Pediatric Emergencies IN EMS Anatomical Differences Head and


- Slides: 49
Pediatric Emergencies IN EMS
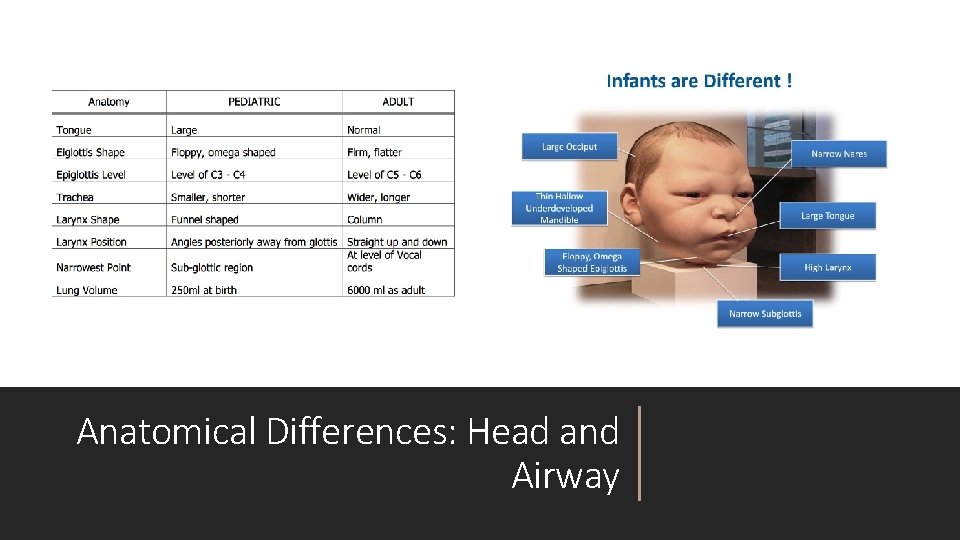
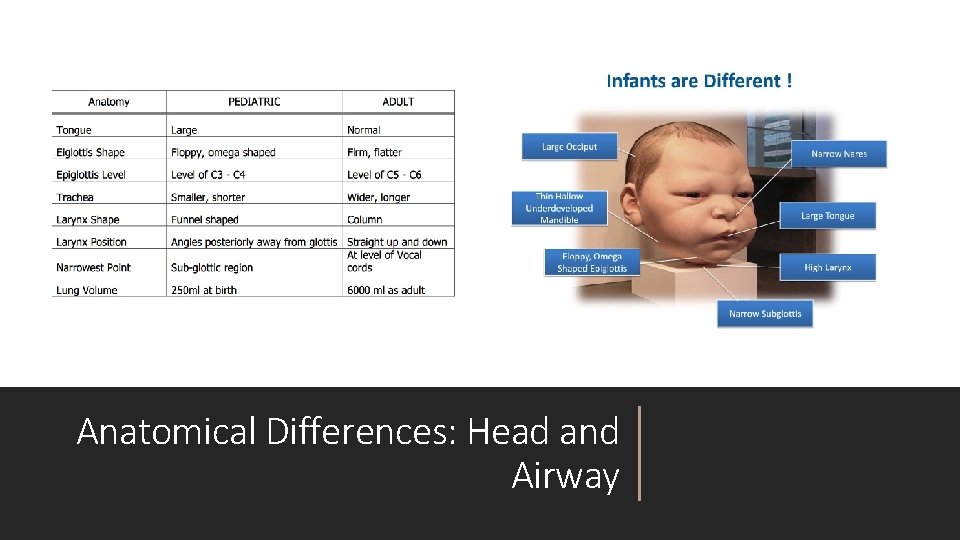
Anatomical Differences: Head and Airway
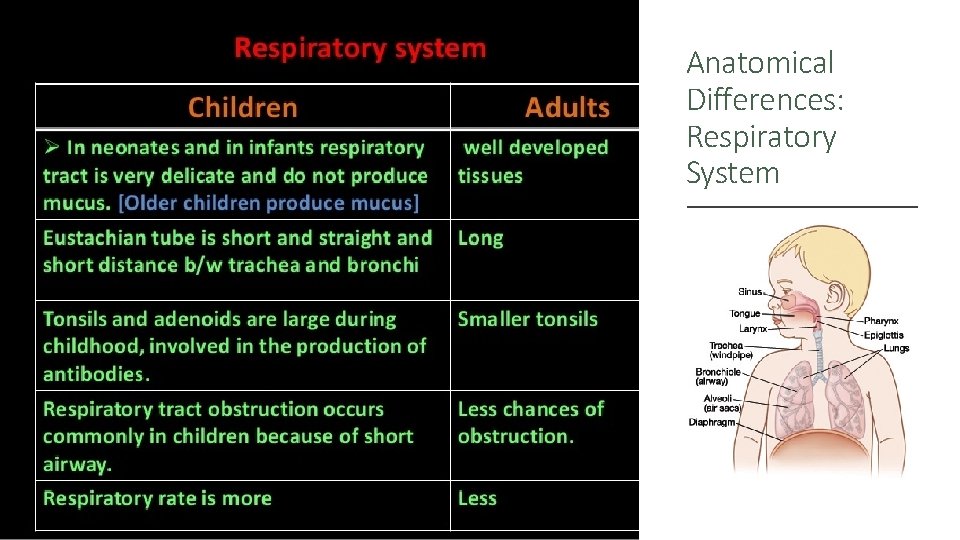
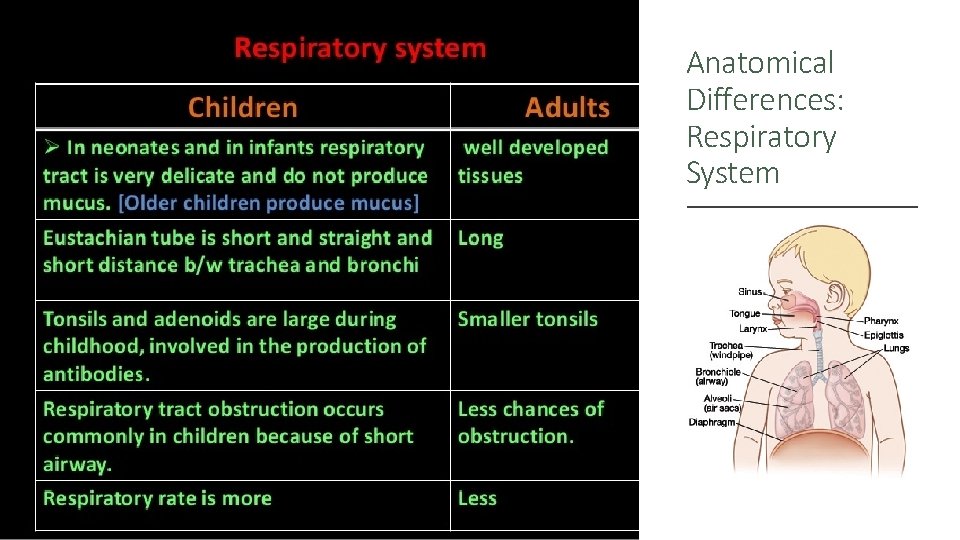
Anatomical Differences: Respiratory System
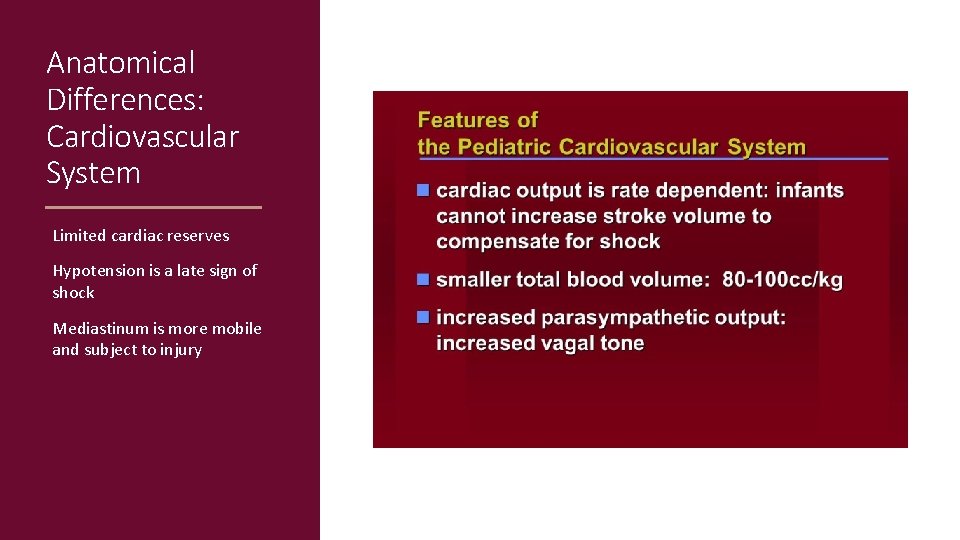
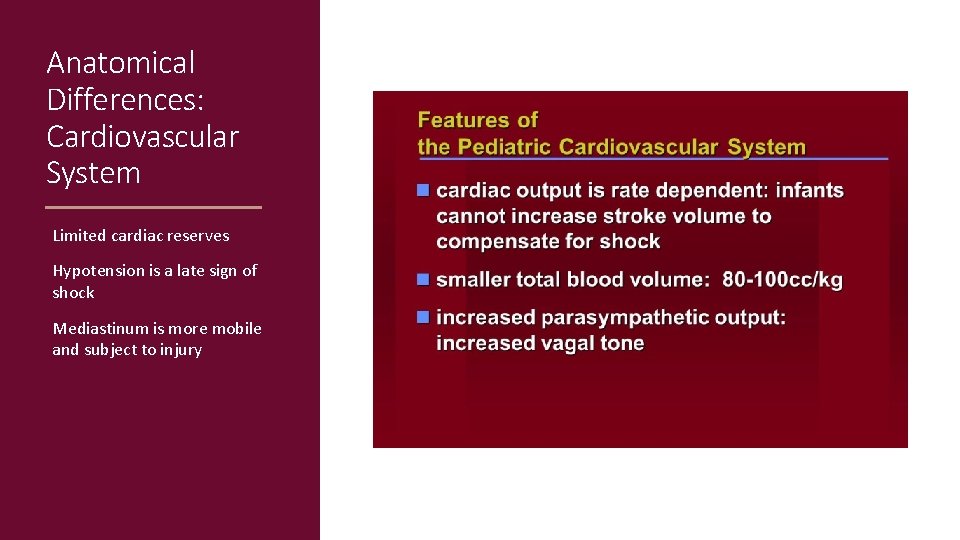
Anatomical Differences: Cardiovascular System Limited cardiac reserves Hypotension is a late sign of shock Mediastinum is more mobile and subject to injury
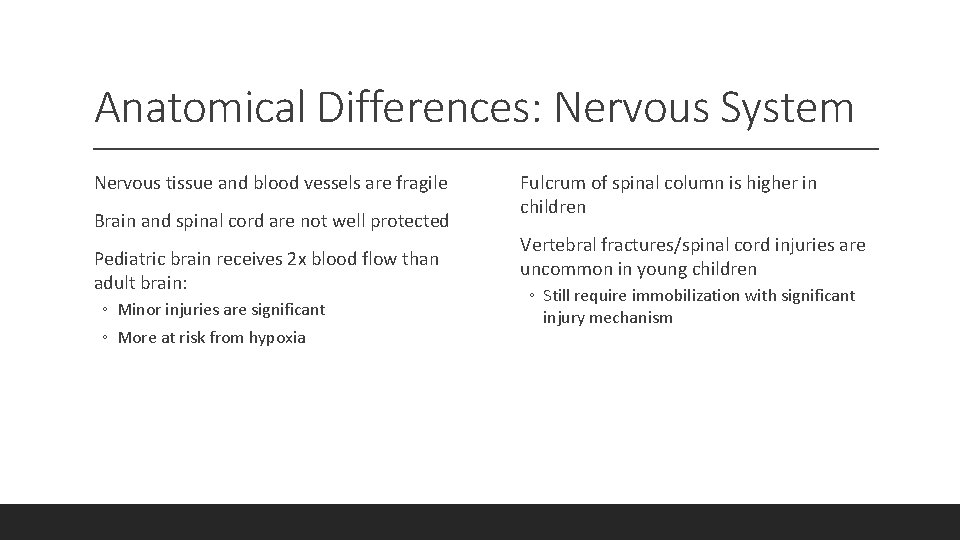
Anatomical Differences: Nervous System Nervous tissue and blood vessels are fragile Brain and spinal cord are not well protected Pediatric brain receives 2 x blood flow than adult brain: ◦ Minor injuries are significant ◦ More at risk from hypoxia Fulcrum of spinal column is higher in children Vertebral fractures/spinal cord injuries are uncommon in young children ◦ Still require immobilization with significant injury mechanism
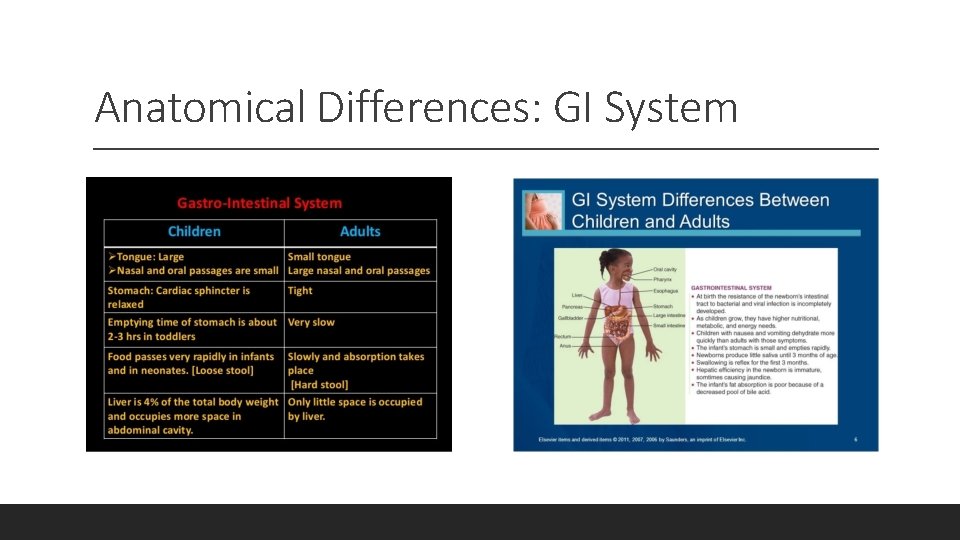
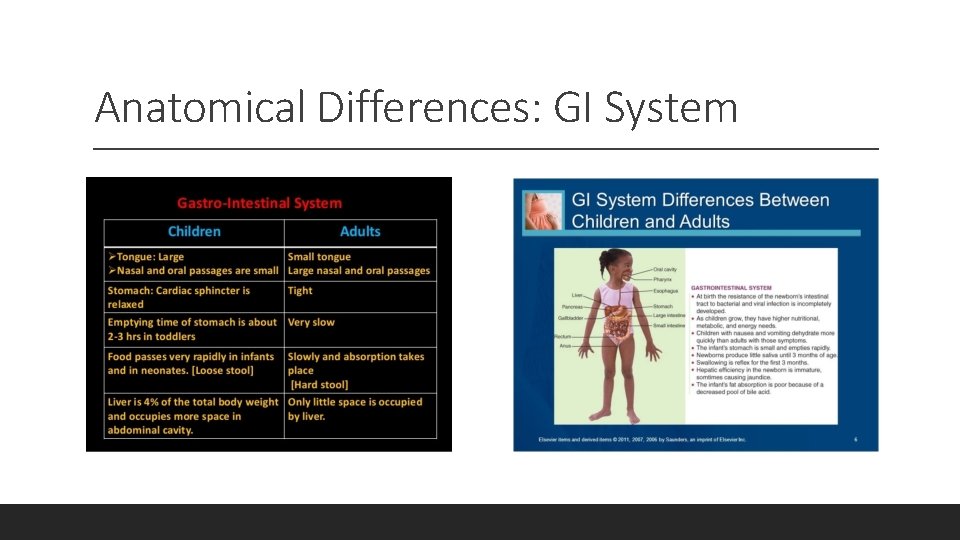
Anatomical Differences: GI System
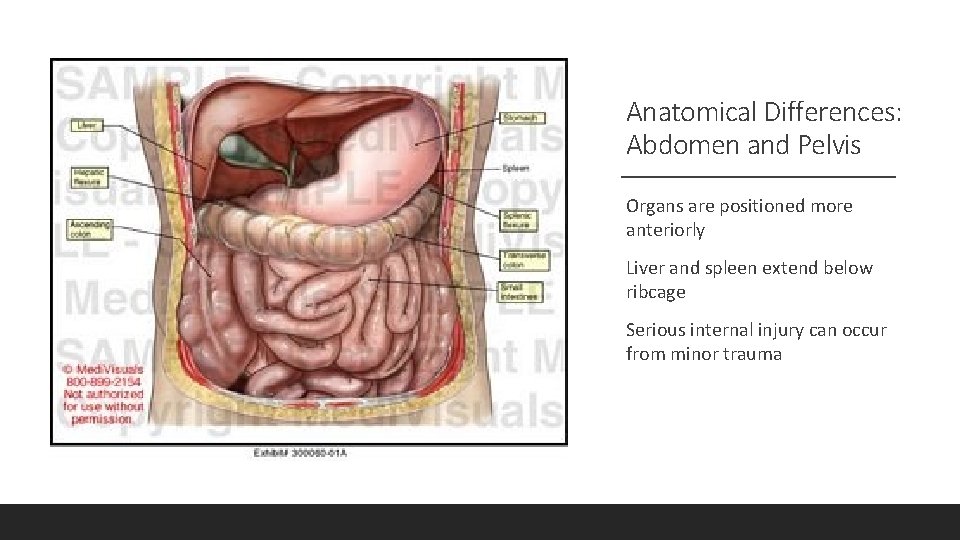
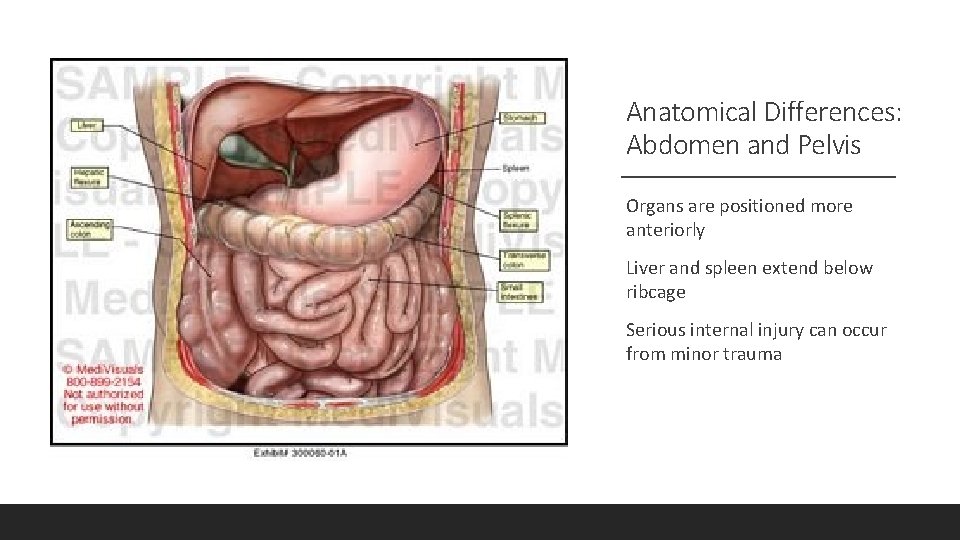
Anatomical Differences: Abdomen and Pelvis Organs are positioned more anteriorly Liver and spleen extend below ribcage Serious internal injury can occur from minor trauma
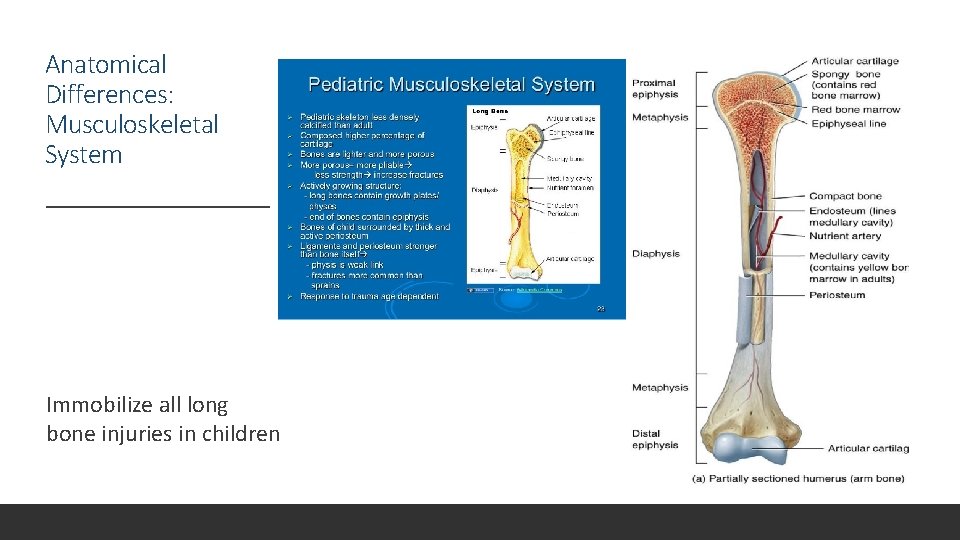
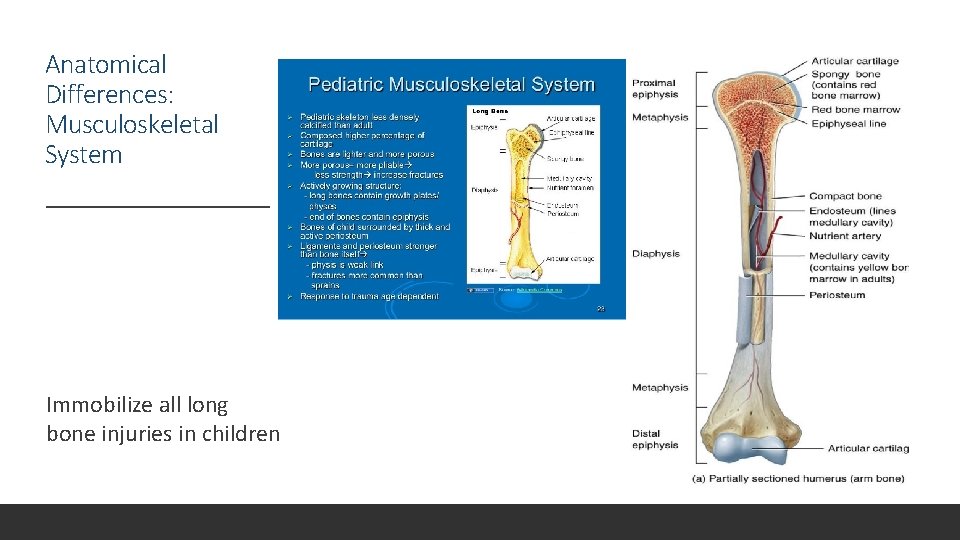
Anatomical Differences: Musculoskeletal System Immobilize all long bone injuries in children
Pediatric Assessment Address all life-threatening abnormalities as you encounter them during your assessment Use a weight-based resuscitation tape if you do not know the patient’s weight Ensure that you have age-appropriate equipment with you Establish rapport with parents/caregivers while remembering that the patient is your first priority
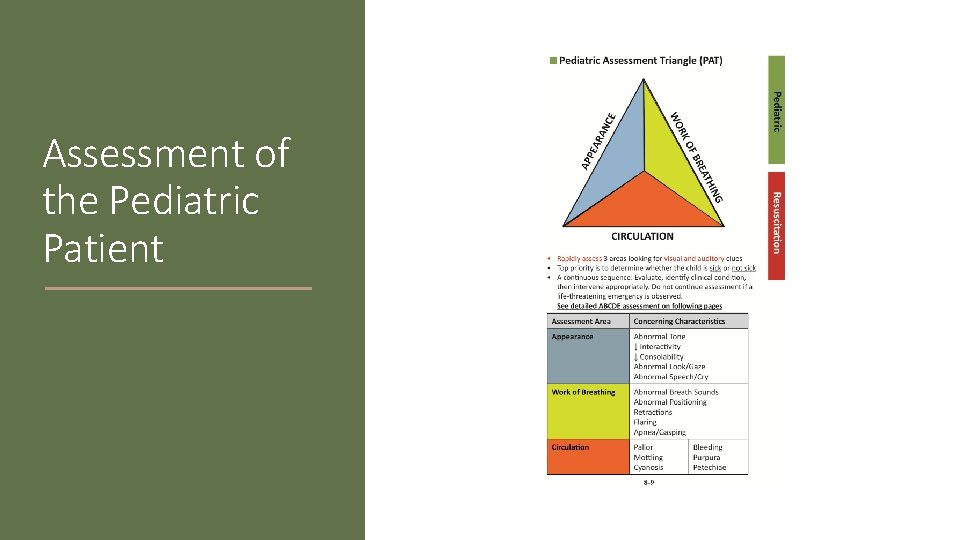
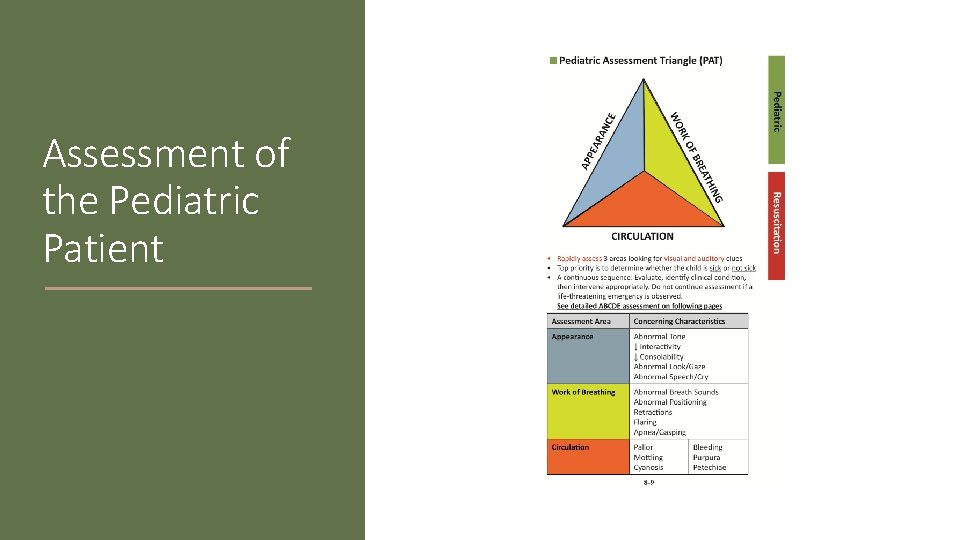
Assessment of the Pediatric Patient
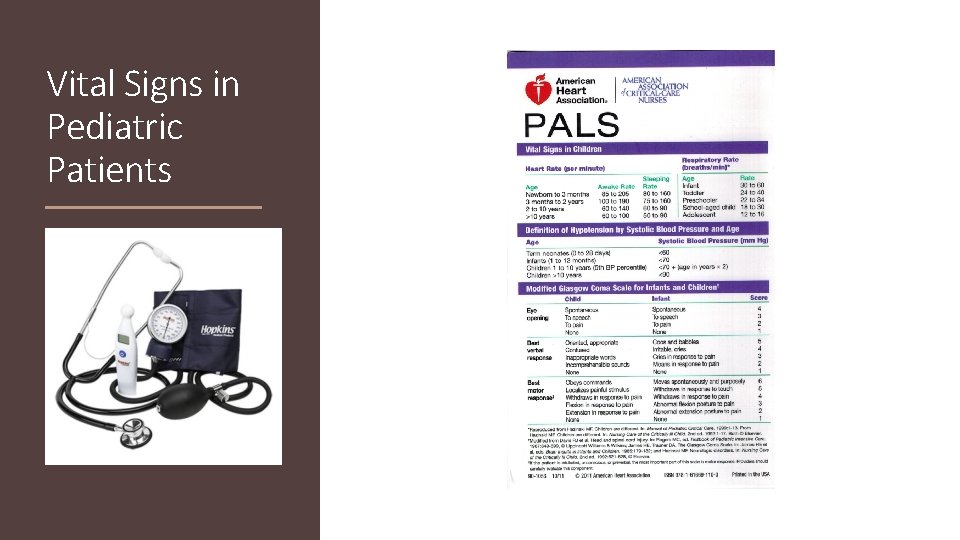
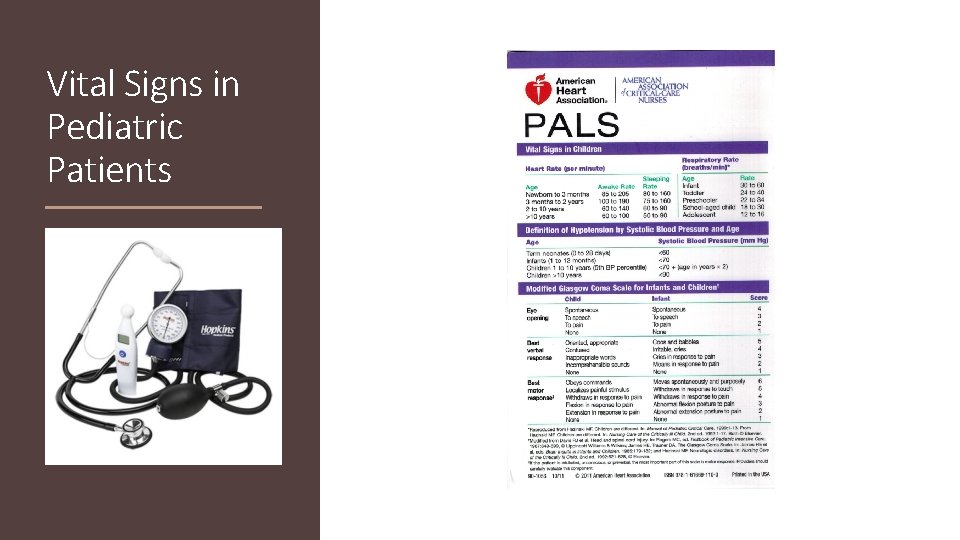
Vital Signs in Pediatric Patients
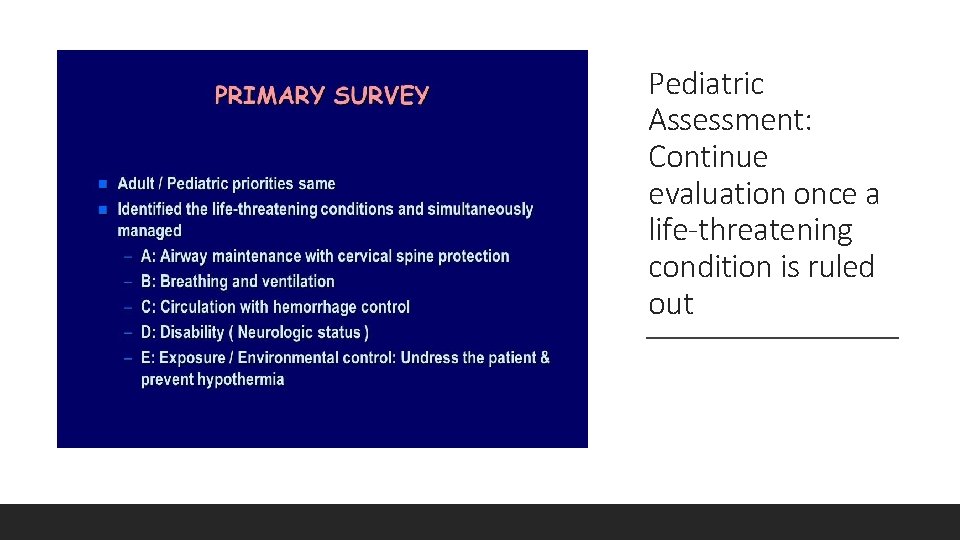
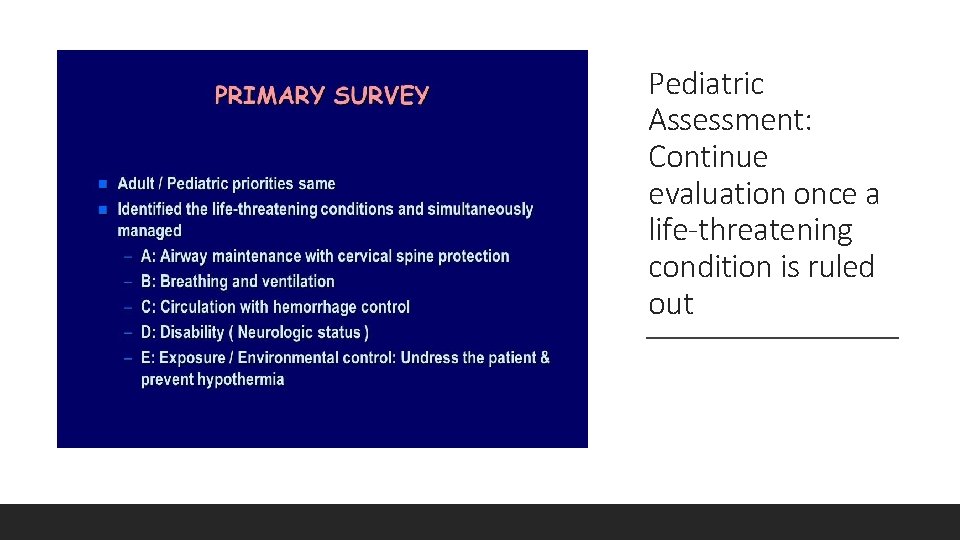
Pediatric Assessment: Continue evaluation once a life-threatening condition is ruled out
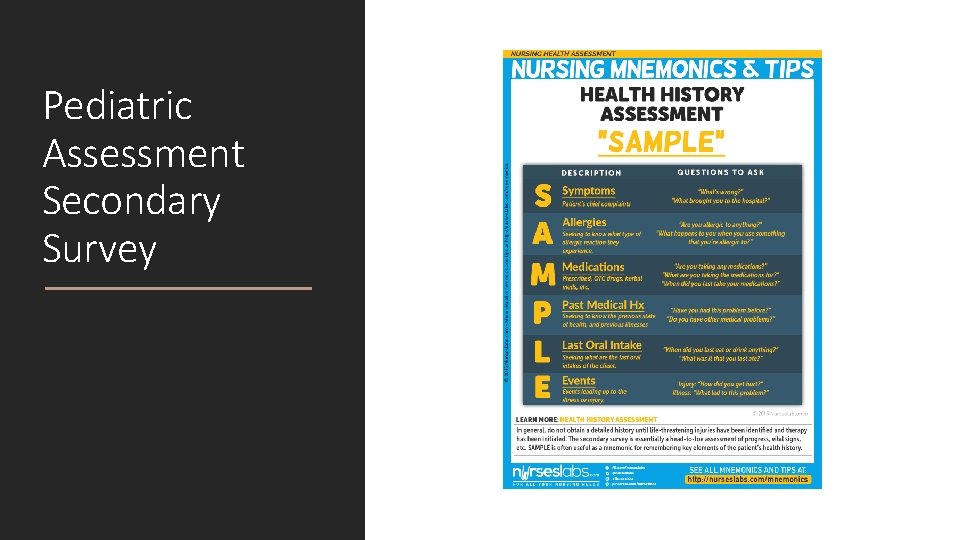
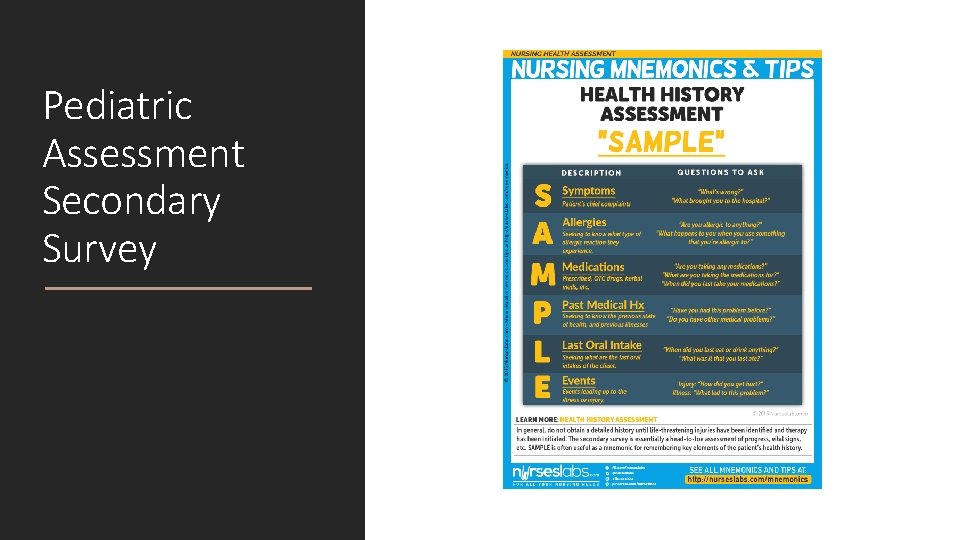
Pediatric Assessment Secondary Survey
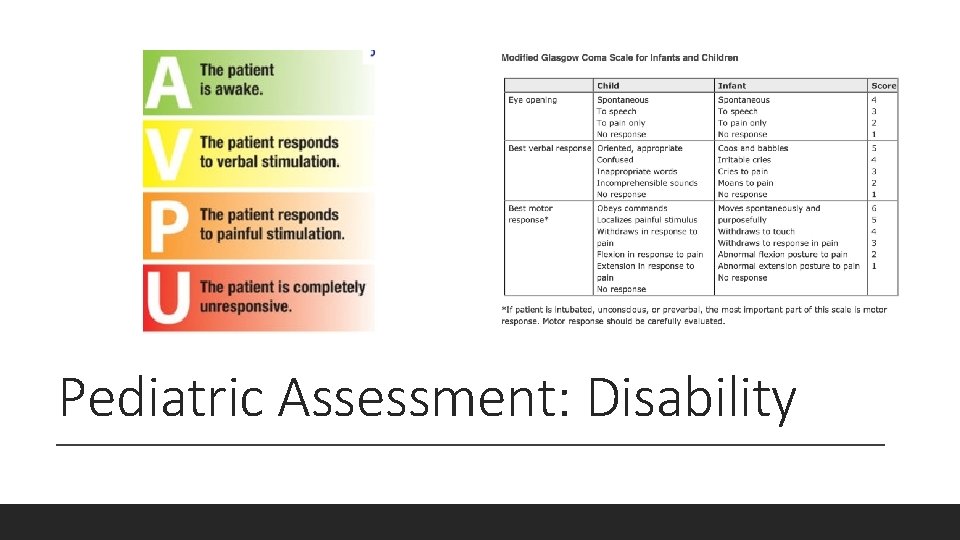
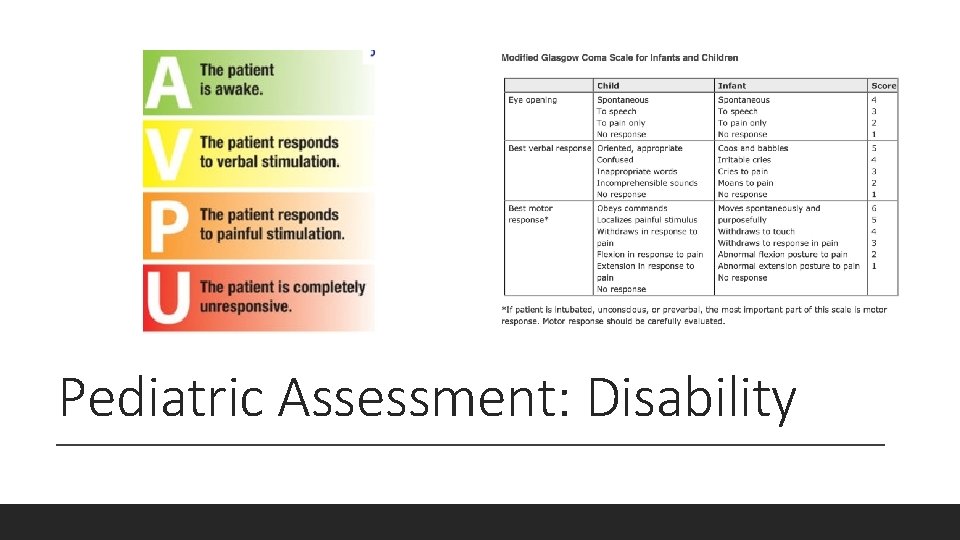
Pediatric Assessment: Disability
Transport Decisions Return to Pediatric Assessment Triangle frequently Continue to assess ABCs Treat life-threatening conditions In unstable patients, transport sooner rather than later In stable patients, continue with assessment
Pediatric Emergencies RESPIRATORY
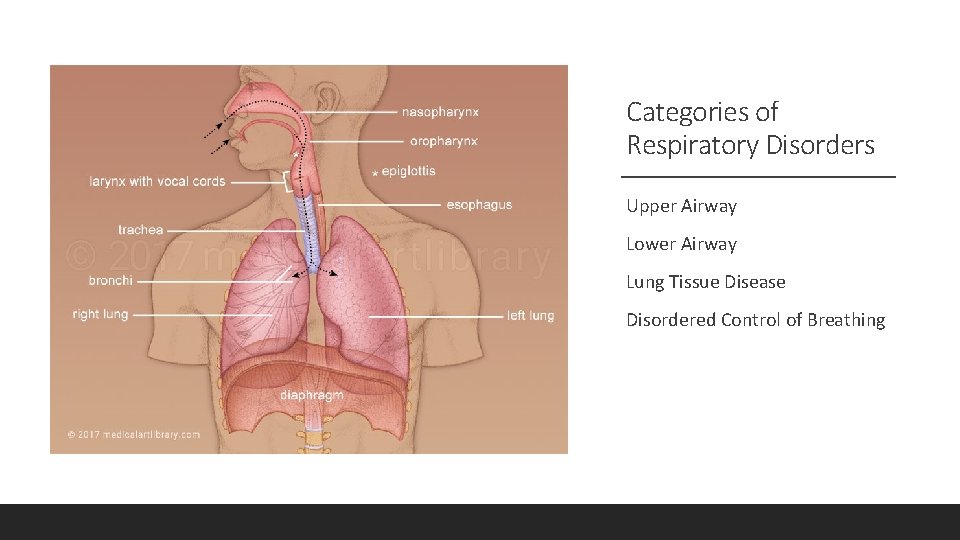
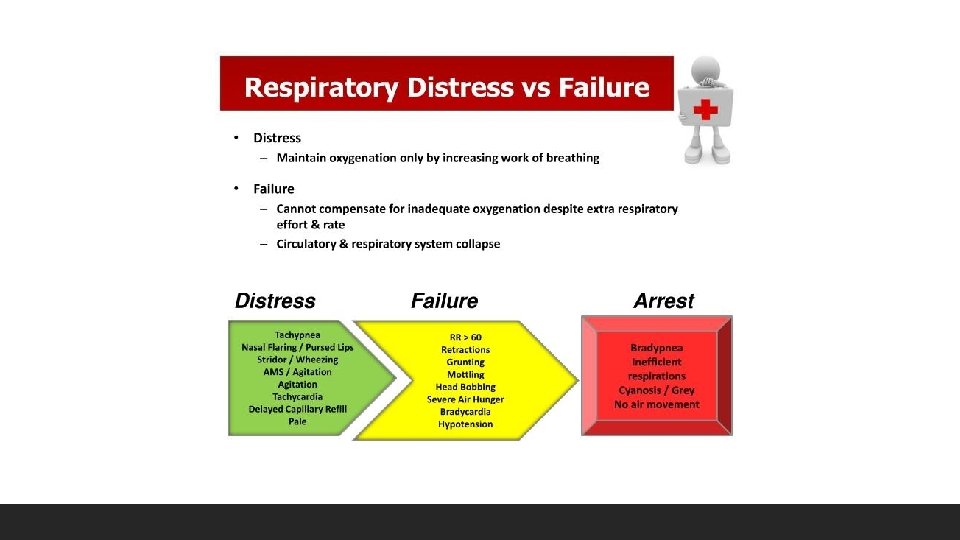
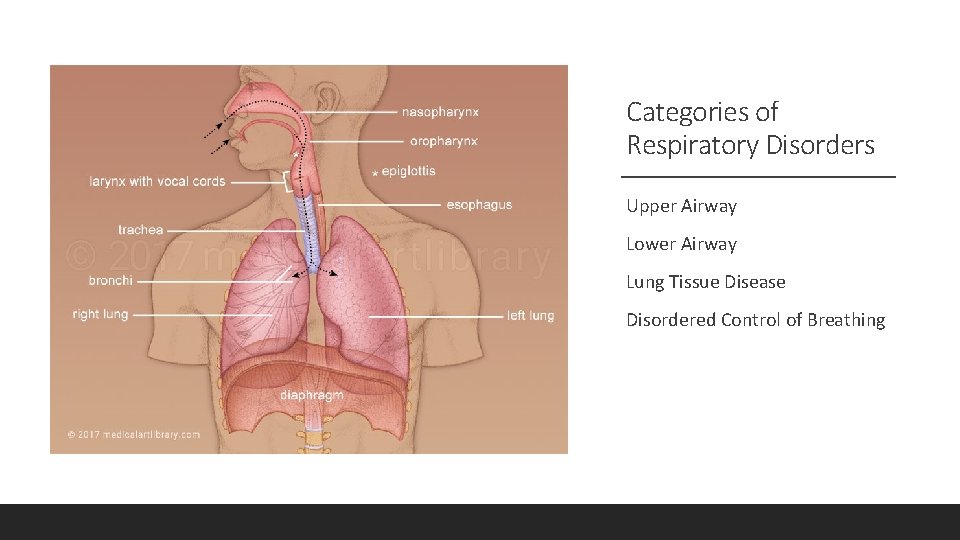
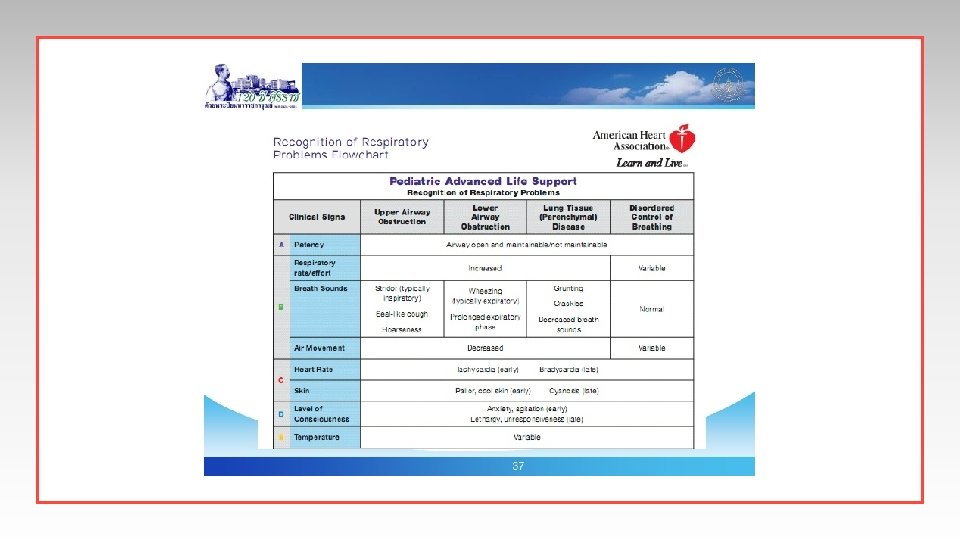
Categories of Respiratory Disorders Upper Airway Lower Airway Lung Tissue Disease Disordered Control of Breathing
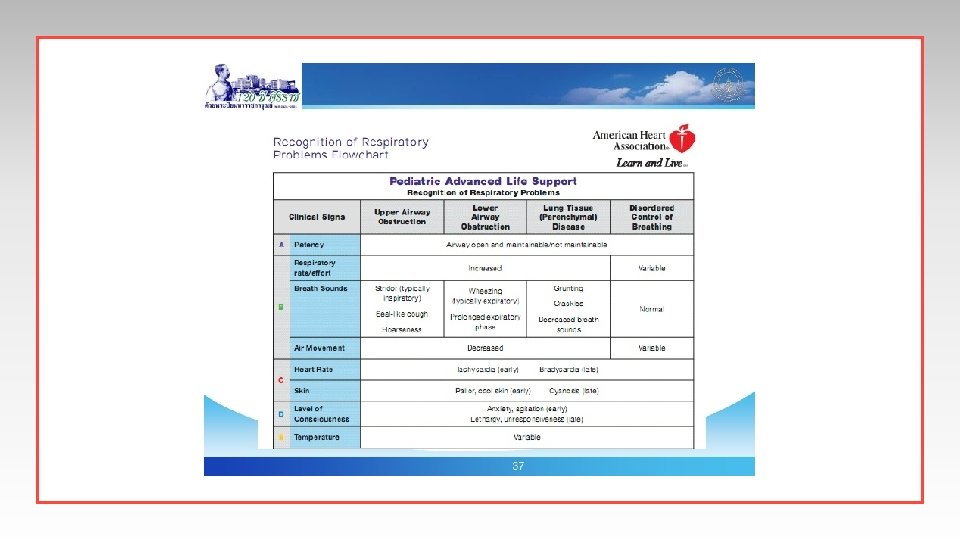
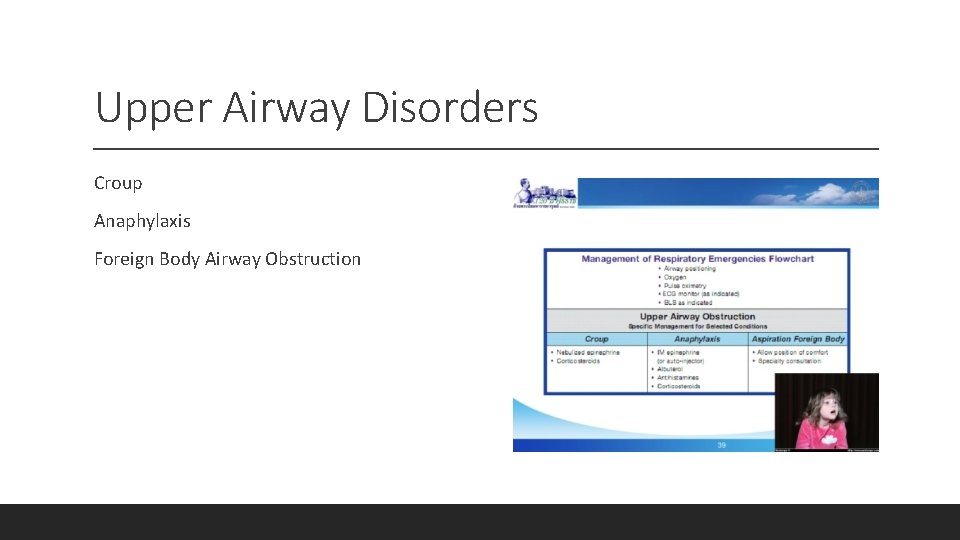
Upper Airway Disorders Croup Anaphylaxis Foreign Body Airway Obstruction
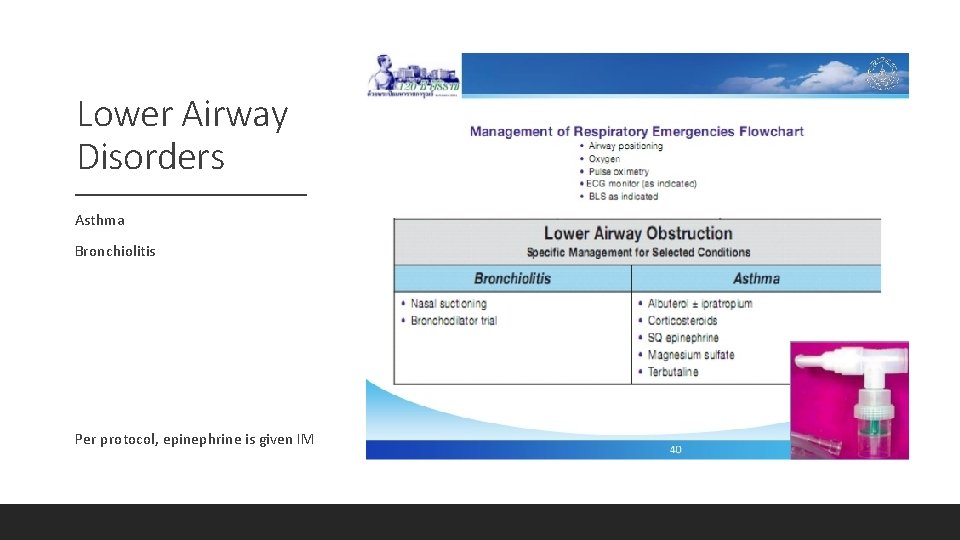
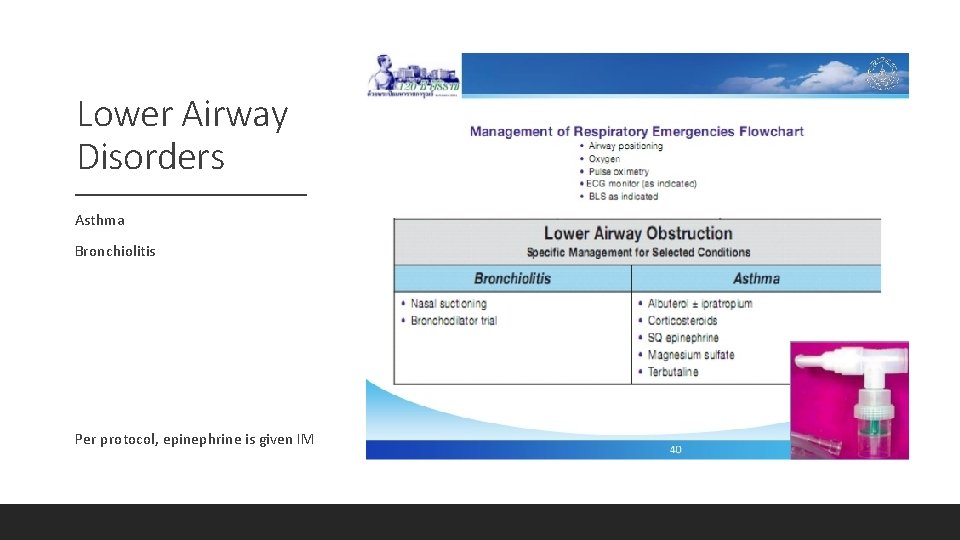
Lower Airway Disorders Asthma Bronchiolitis Per protocol, epinephrine is given IM
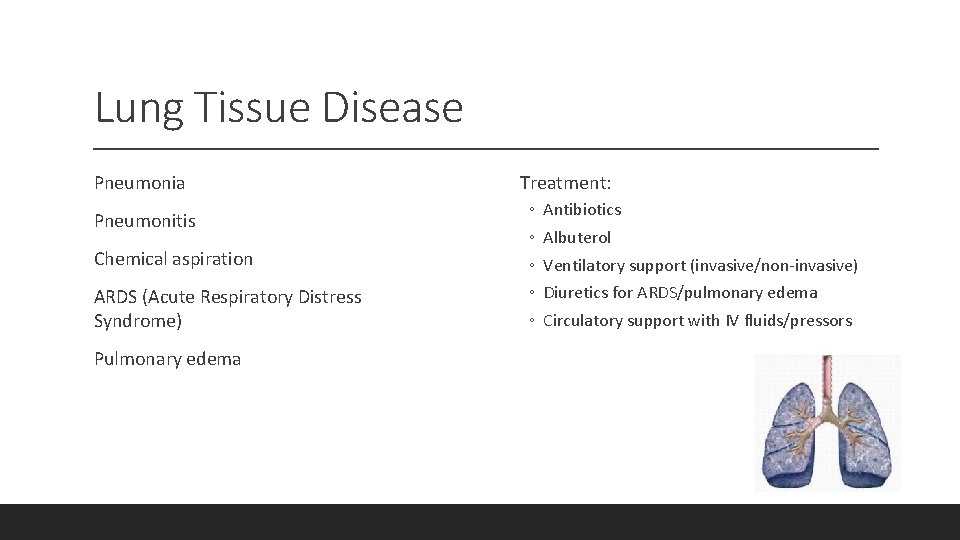
Lung Tissue Disease Pneumonia Pneumonitis Chemical aspiration ARDS (Acute Respiratory Distress Syndrome) Pulmonary edema Treatment: ◦ ◦ ◦ Antibiotics Albuterol Ventilatory support (invasive/non-invasive) Diuretics for ARDS/pulmonary edema Circulatory support with IV fluids/pressors
Disordered Work of Breathing Increased ICP (intracranial pressure) Poisoning/overdose Neuromuscular Disease Treatment: ◦ ◦ ◦ Avoid hypoxemia Avoid hypercarbia Avoid hyperthermia Ventilatory support (invasive/non-invasive) Antidote (if poisoning) Never give naloxone to a neonate
Pediatric Emergencies SHOCK
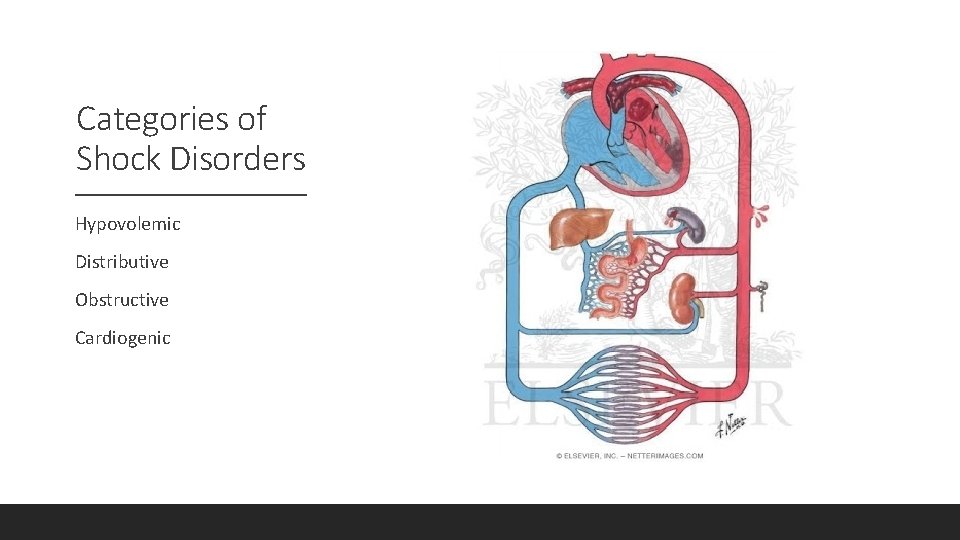
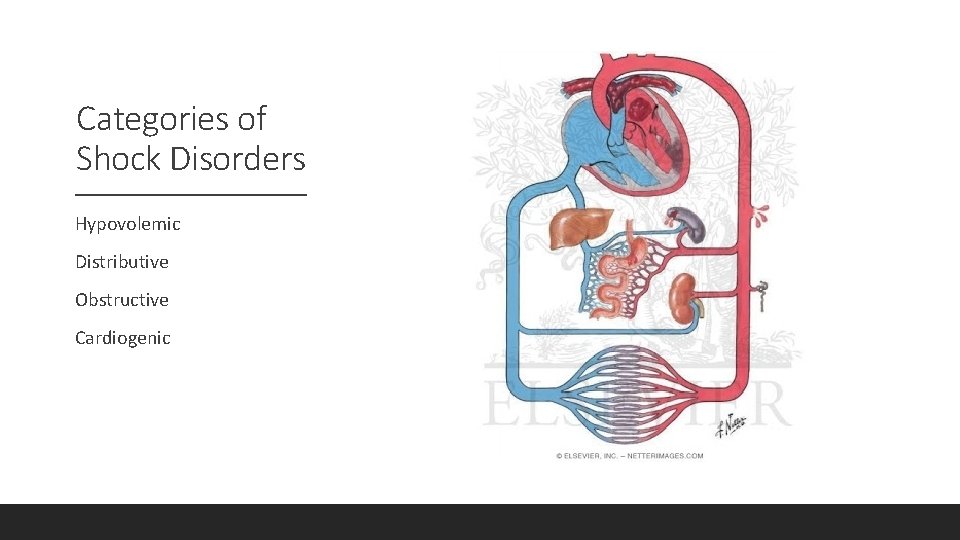
Categories of Shock Disorders Hypovolemic Distributive Obstructive Cardiogenic
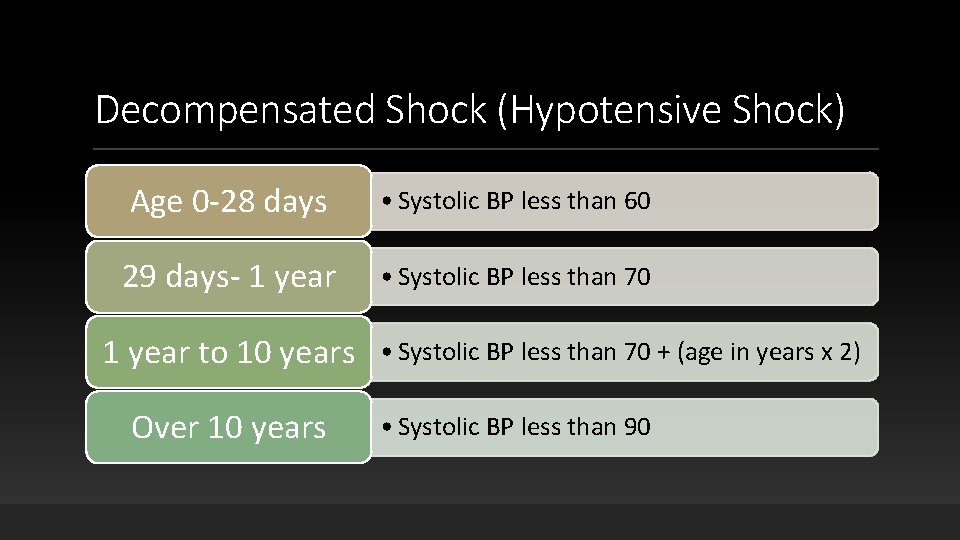
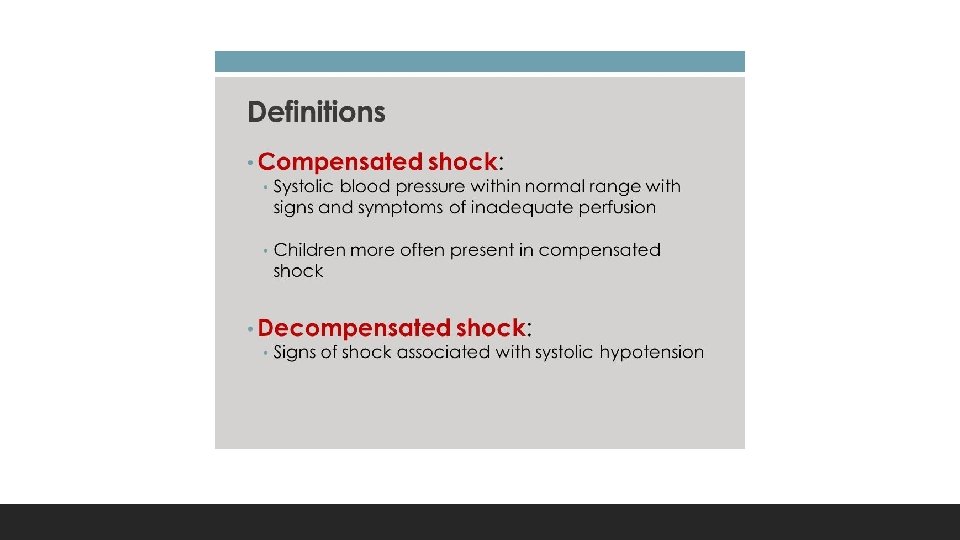
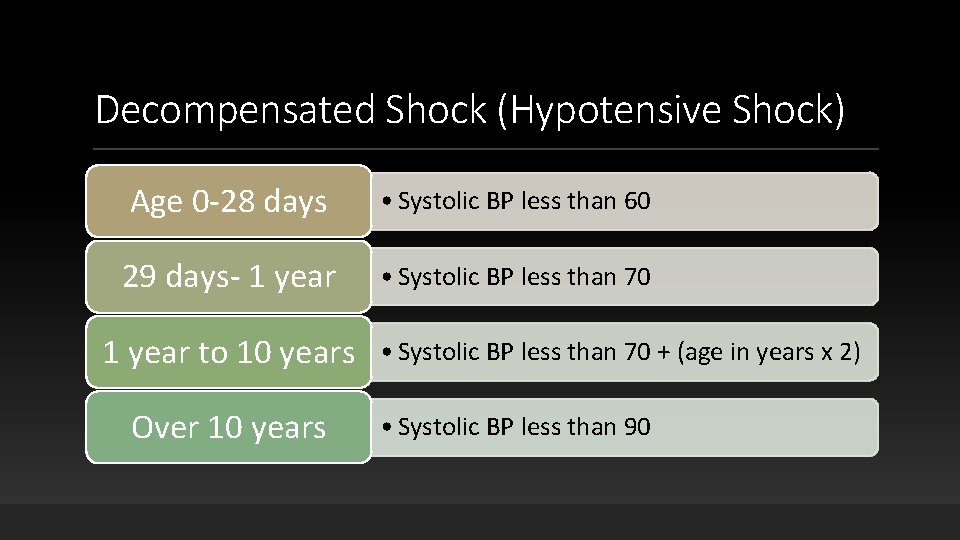
Decompensated Shock (Hypotensive Shock) Age 0 -28 days • Systolic BP less than 60 29 days- 1 year • Systolic BP less than 70 1 year to 10 years Over 10 years • Systolic BP less than 70 + (age in years x 2) • Systolic BP less than 90
Hypovolemic Shock Non-hemorrhagic ◦ Vomiting ◦ Diarrhea ◦ Poor intake Fluid bolus: 20 ml/kg Control bleeding Consider TXA if > 16 years old, less than 3 hours post injury (hemorrhagic shock) Blood Transfusion (hemorrhagic shock) Hemorrhagic
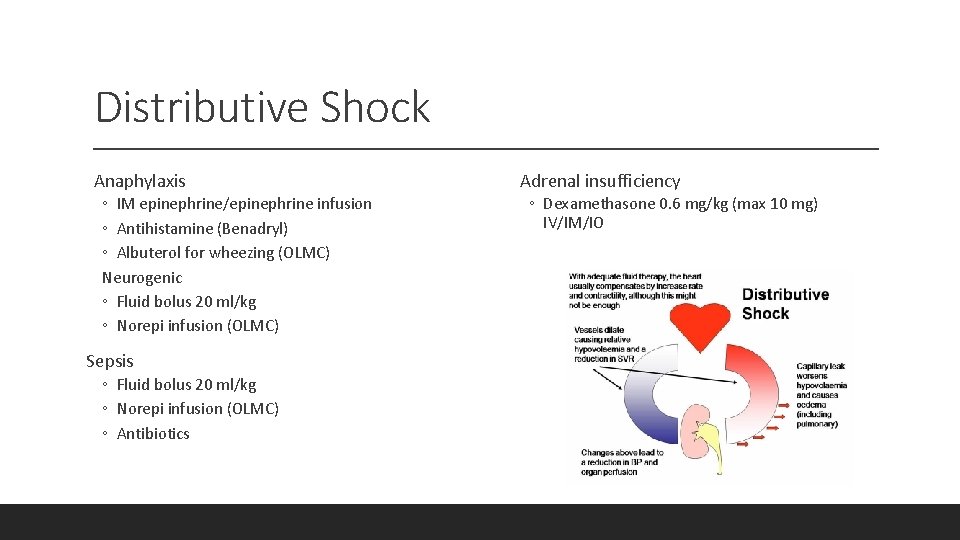
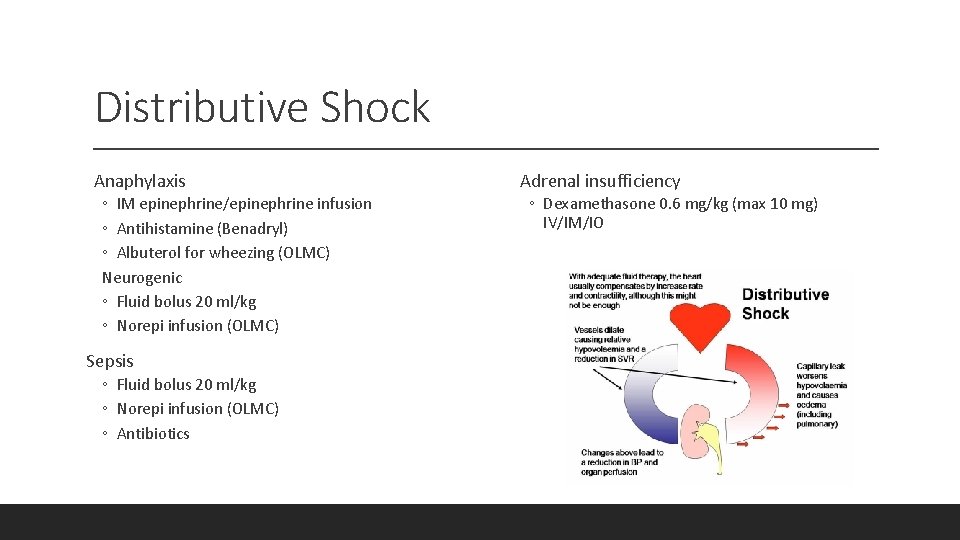
Distributive Shock Anaphylaxis ◦ IM epinephrine/epinephrine infusion ◦ Antihistamine (Benadryl) ◦ Albuterol for wheezing (OLMC) Neurogenic ◦ Fluid bolus 20 ml/kg ◦ Norepi infusion (OLMC) Sepsis ◦ Fluid bolus 20 ml/kg ◦ Norepi infusion (OLMC) ◦ Antibiotics Adrenal insufficiency ◦ Dexamethasone 0. 6 mg/kg (max 10 mg) IV/IM/IO
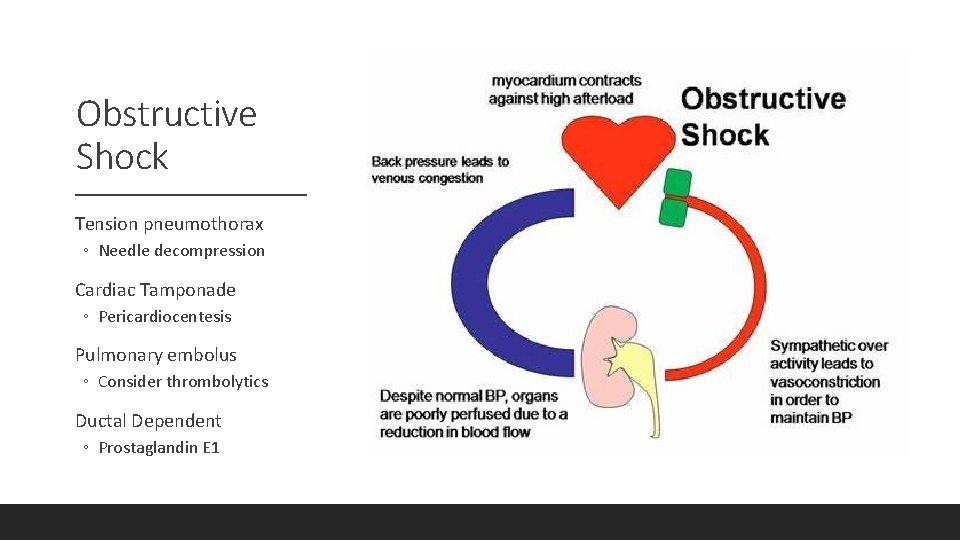
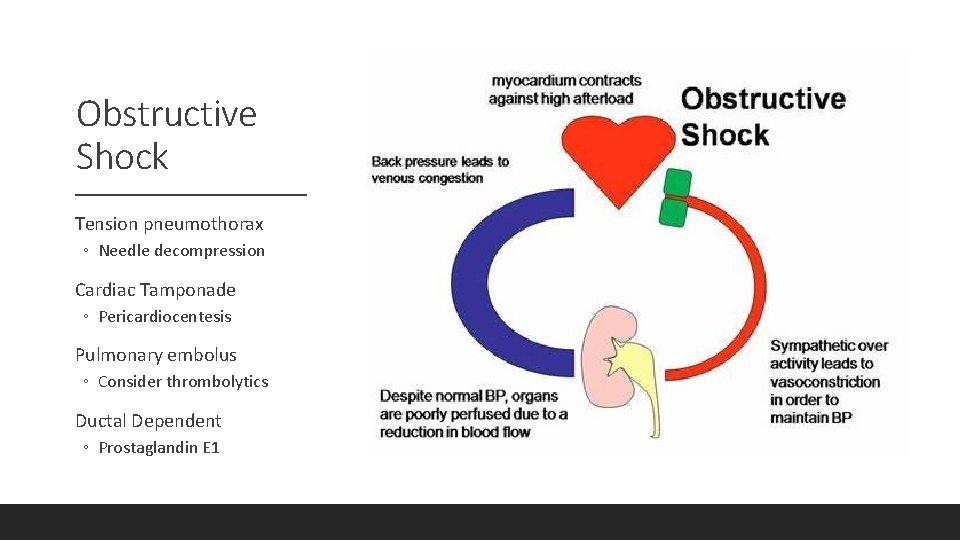
Obstructive Shock Tension pneumothorax ◦ Needle decompression Cardiac Tamponade ◦ Pericardiocentesis Pulmonary embolus ◦ Consider thrombolytics Ductal Dependent ◦ Prostaglandin E 1
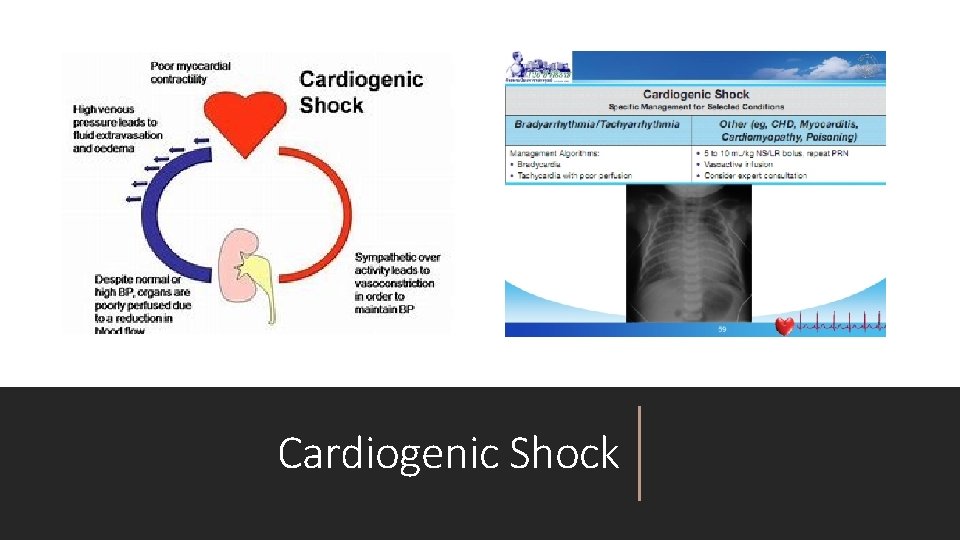
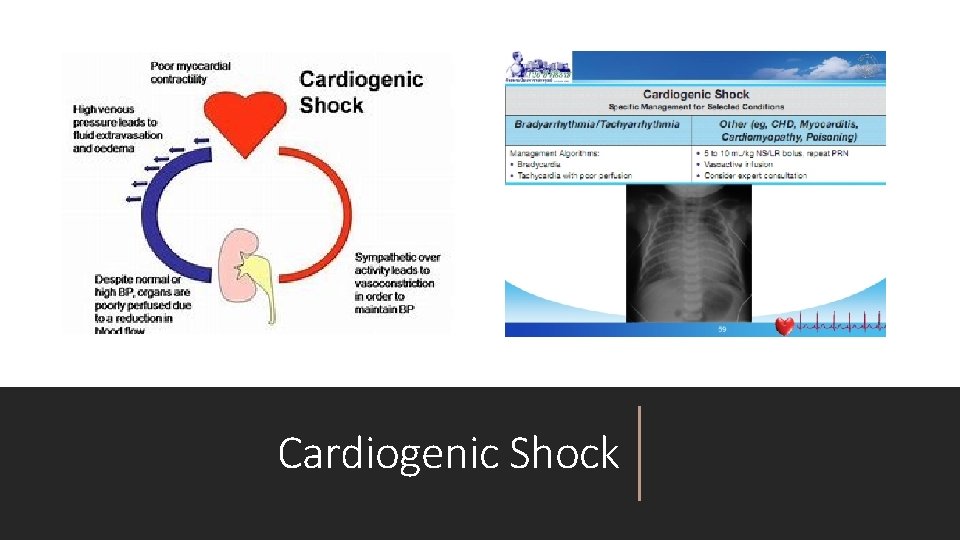
Cardiogenic Shock
Pediatric Emergencies BRIEF RESOLVED UNEXPLAINED EVENT
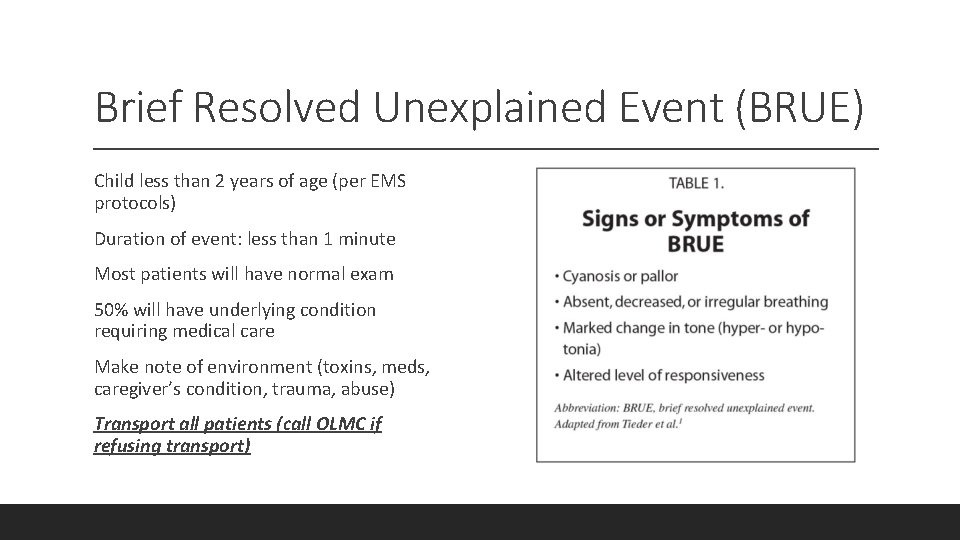
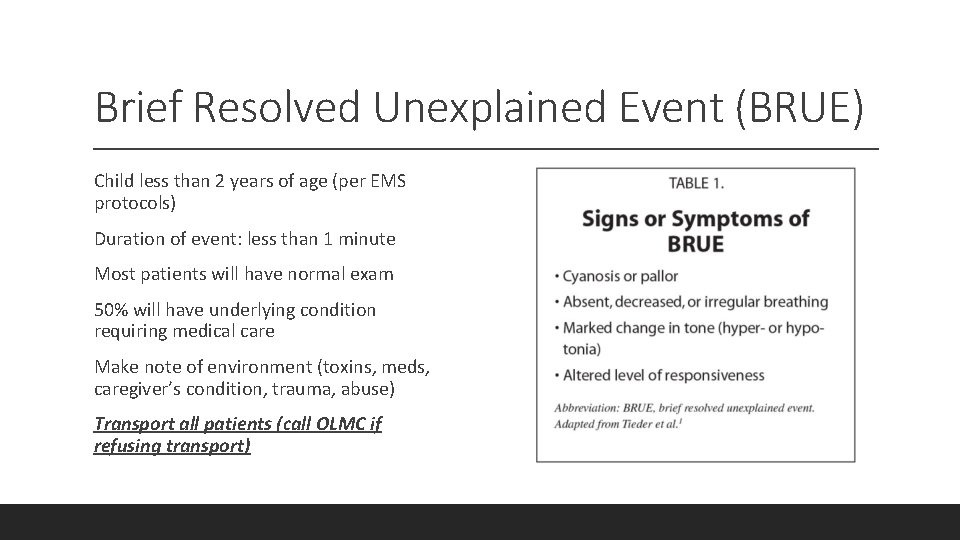
Brief Resolved Unexplained Event (BRUE) Child less than 2 years of age (per EMS protocols) Duration of event: less than 1 minute Most patients will have normal exam 50% will have underlying condition requiring medical care Make note of environment (toxins, meds, caregiver’s condition, trauma, abuse) Transport all patients (call OLMC if refusing transport)

Pediatric Emergencies NEONATAL AND YOUNG INFANT FEVER
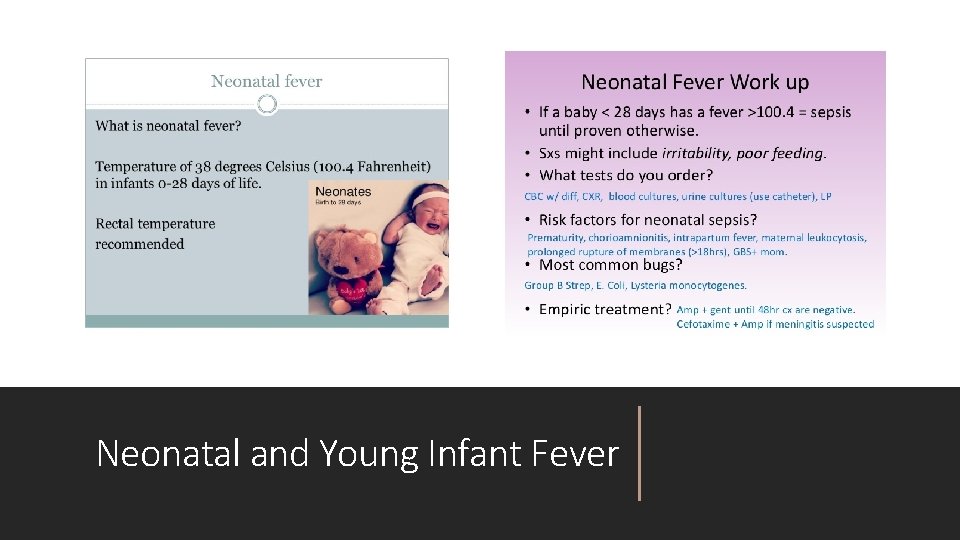
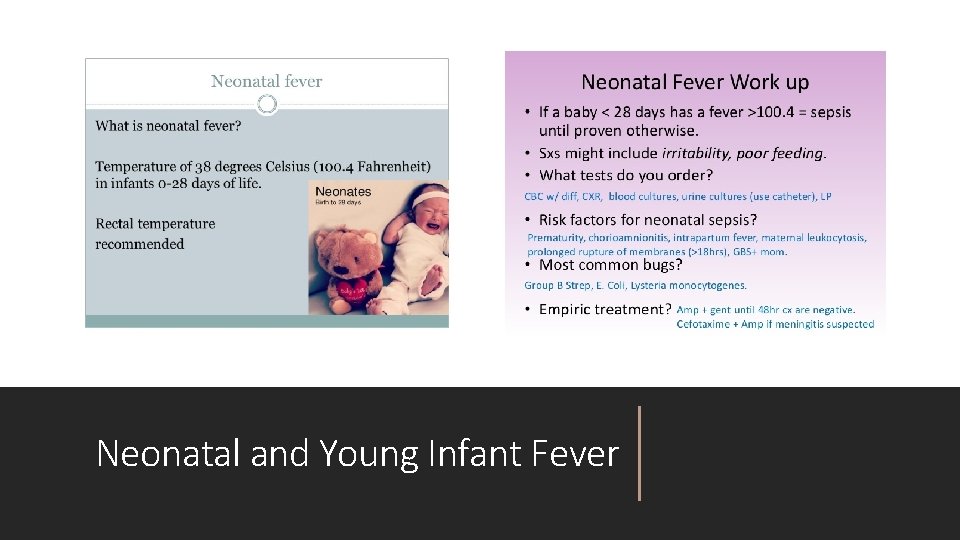
Neonatal and Young Infant Fever
Fever in Neonates and Young Infants Transport all patients less than 90 days old with measured or reported fever (taken by any route by any caregiver) Call OLMC for assistance if caregiver/guardian refuses care/transport!

Pediatric Emergencies HYPOGLYCEMIA
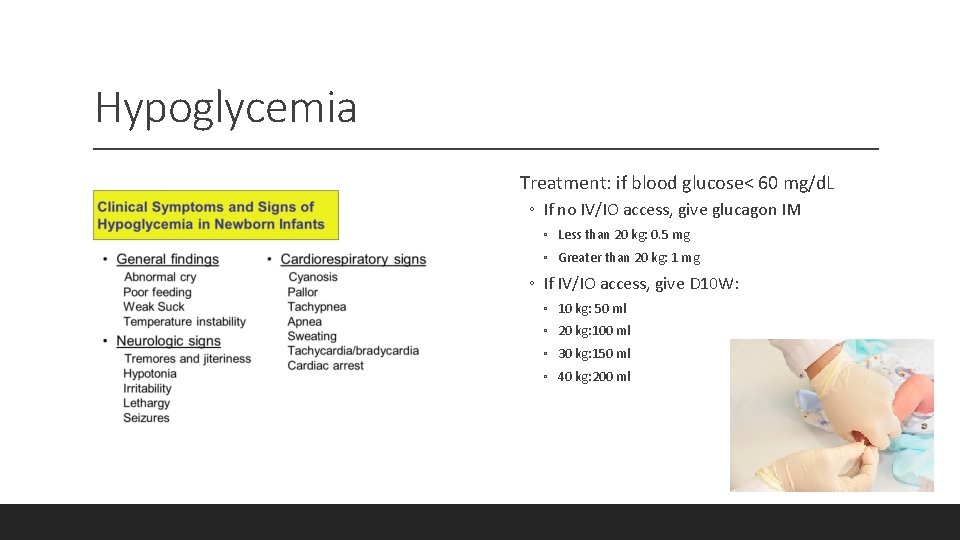
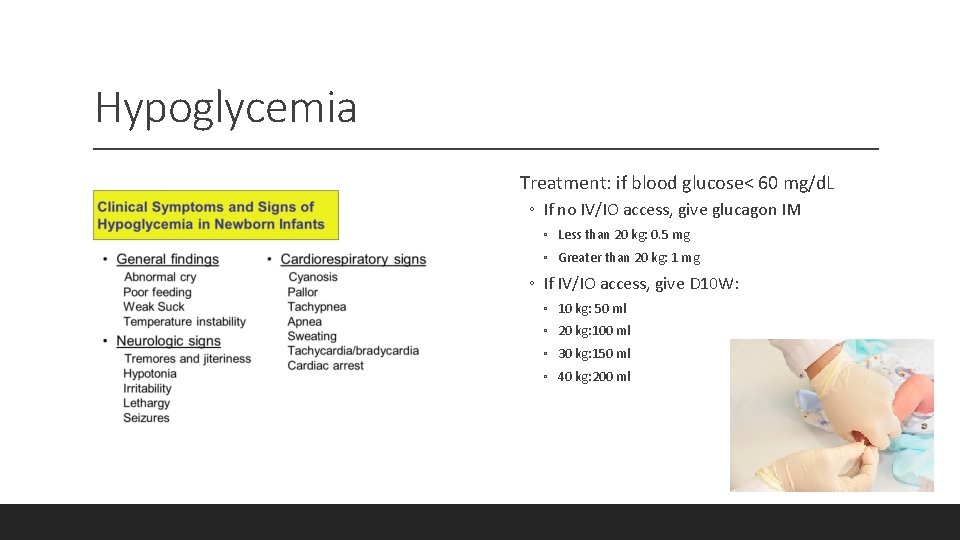
Hypoglycemia Treatment: if blood glucose< 60 mg/d. L ◦ If no IV/IO access, give glucagon IM ◦ Less than 20 kg: 0. 5 mg ◦ Greater than 20 kg: 1 mg ◦ If IV/IO access, give D 10 W: ◦ 10 kg: 50 ml ◦ 20 kg: 100 ml ◦ 30 kg: 150 ml ◦ 40 kg: 200 ml
Pediatric Emergencies PALS ALGORITHMS
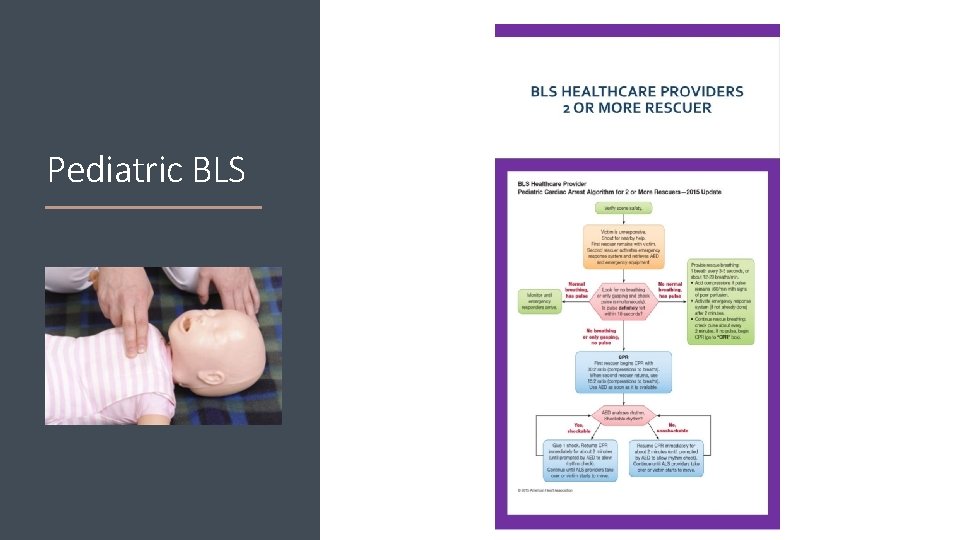
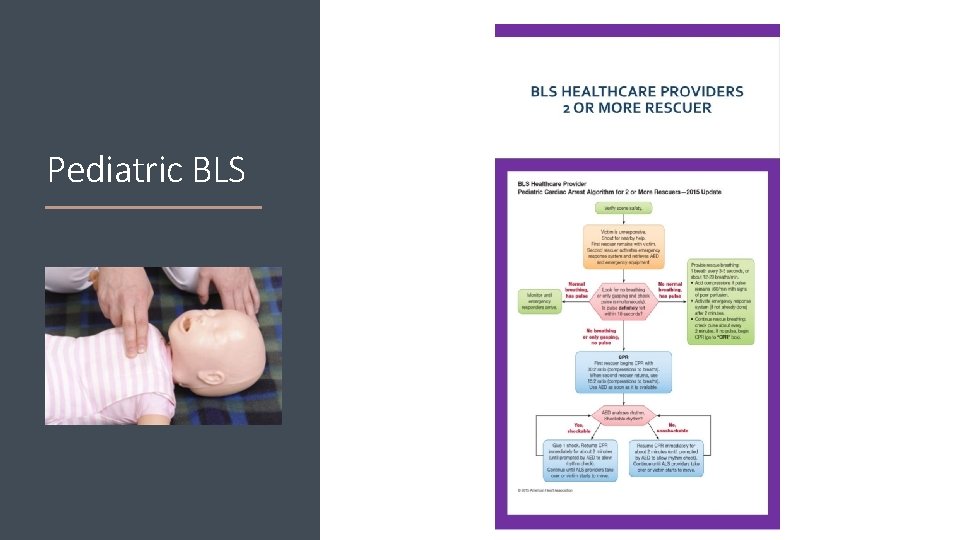
Pediatric BLS
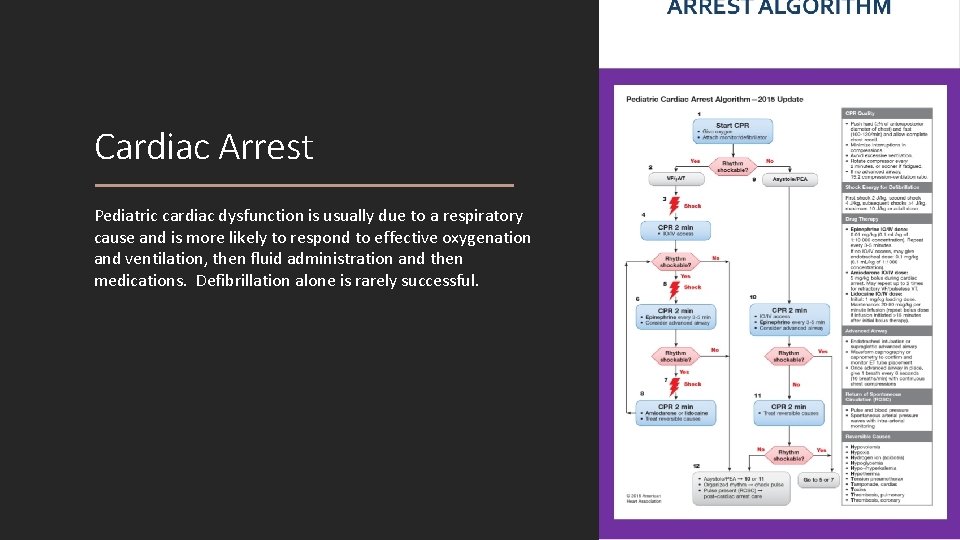
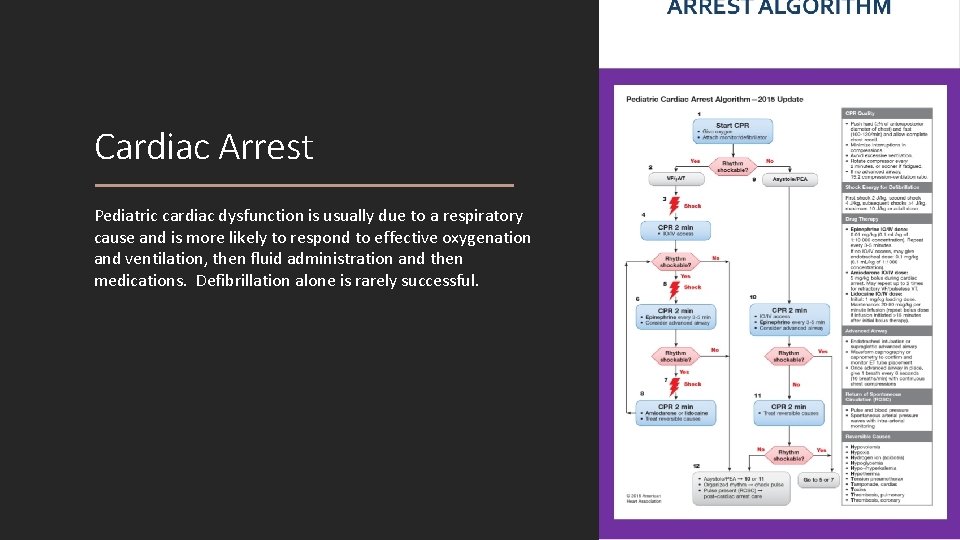
Cardiac Arrest Pediatric cardiac dysfunction is usually due to a respiratory cause and is more likely to respond to effective oxygenation and ventilation, then fluid administration and then medications. Defibrillation alone is rarely successful.
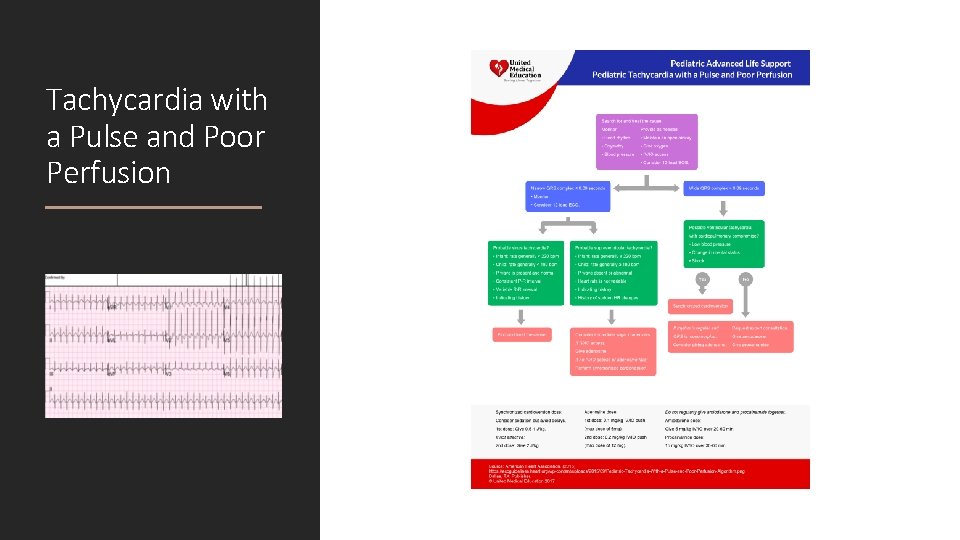
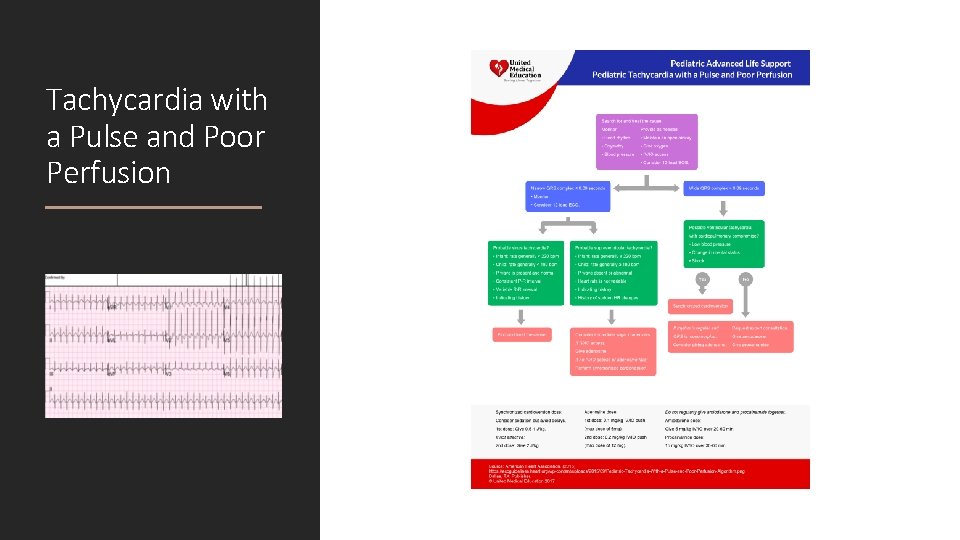
Tachycardia with a Pulse and Poor Perfusion
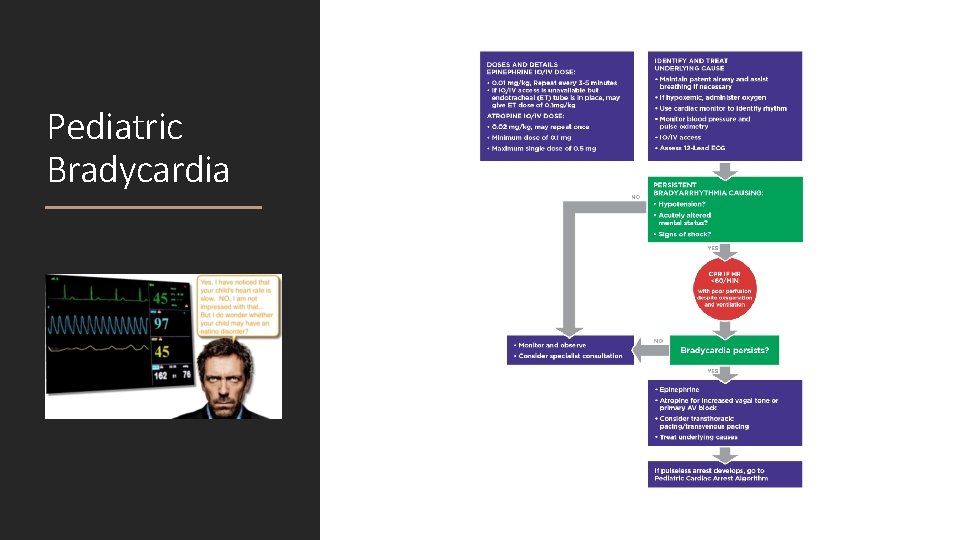
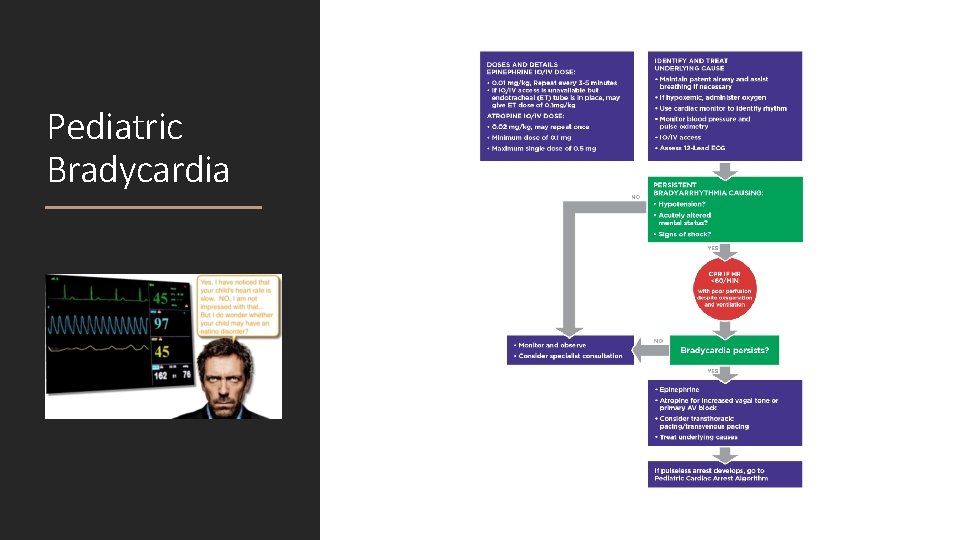
Pediatric Bradycardia
Pediatric Emergencies OPIOID OVERDOSE
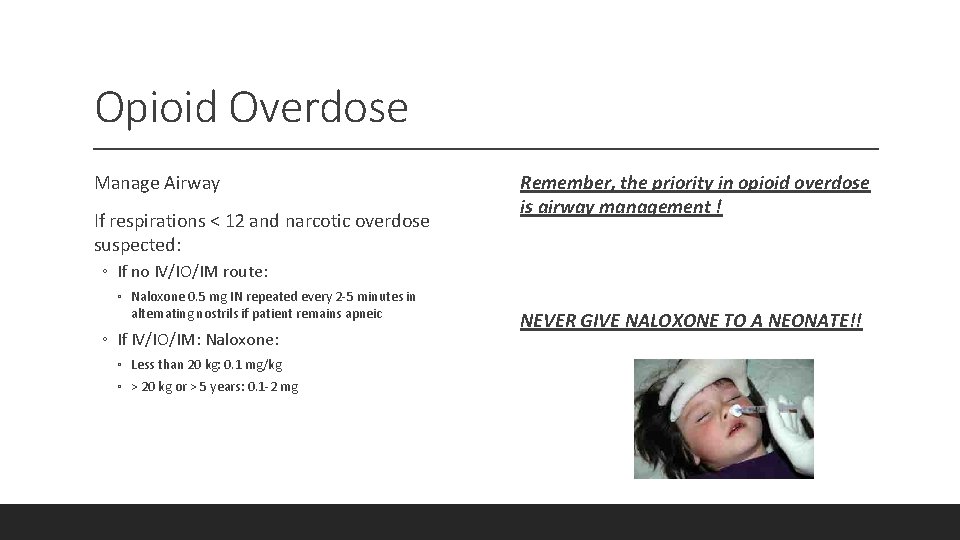
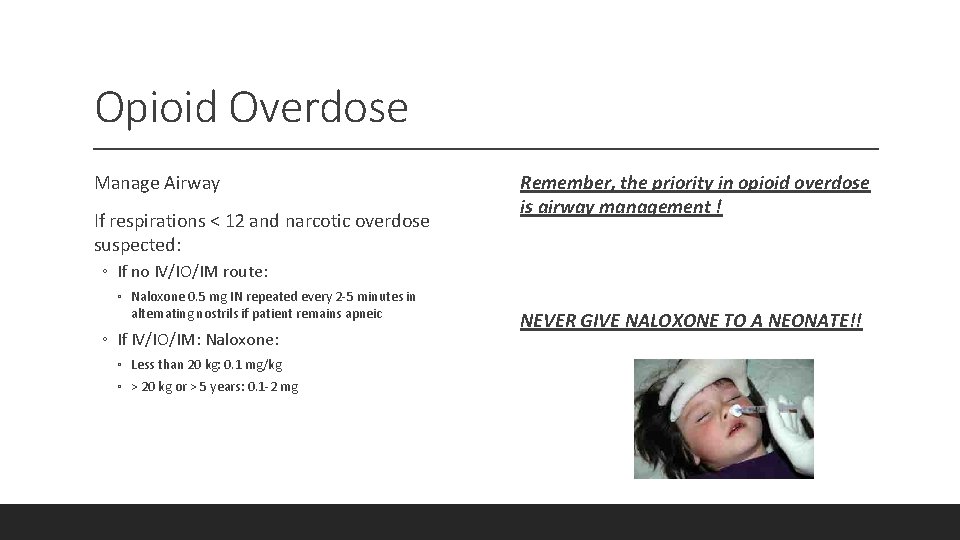
Opioid Overdose Manage Airway If respirations < 12 and narcotic overdose suspected: Remember, the priority in opioid overdose is airway management ! ◦ If no IV/IO/IM route: ◦ Naloxone 0. 5 mg IN repeated every 2 -5 minutes in alternating nostrils if patient remains apneic ◦ If IV/IO/IM: Naloxone: ◦ Less than 20 kg: 0. 1 mg/kg ◦ > 20 kg or > 5 years: 0. 1 -2 mg NEVER GIVE NALOXONE TO A NEONATE!!
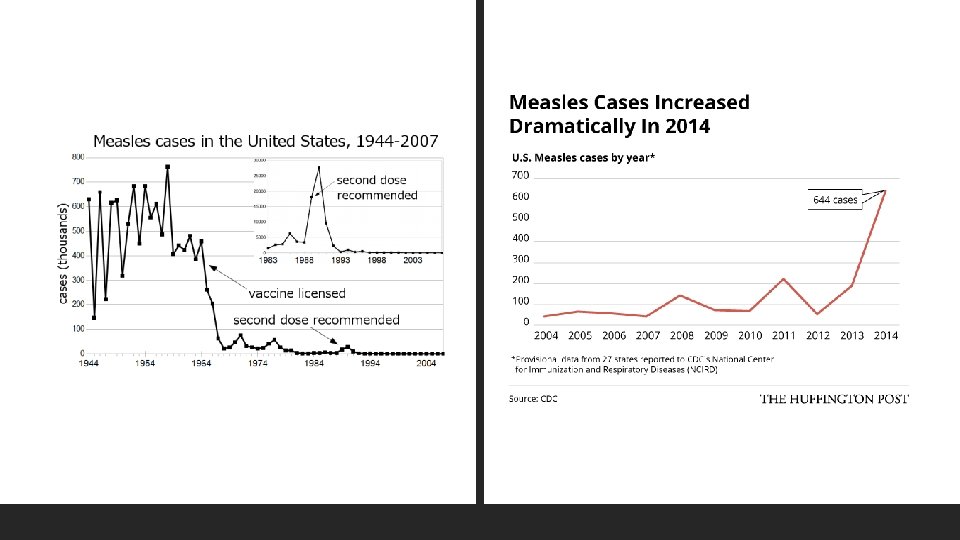
Pediatric Illness MEASLES
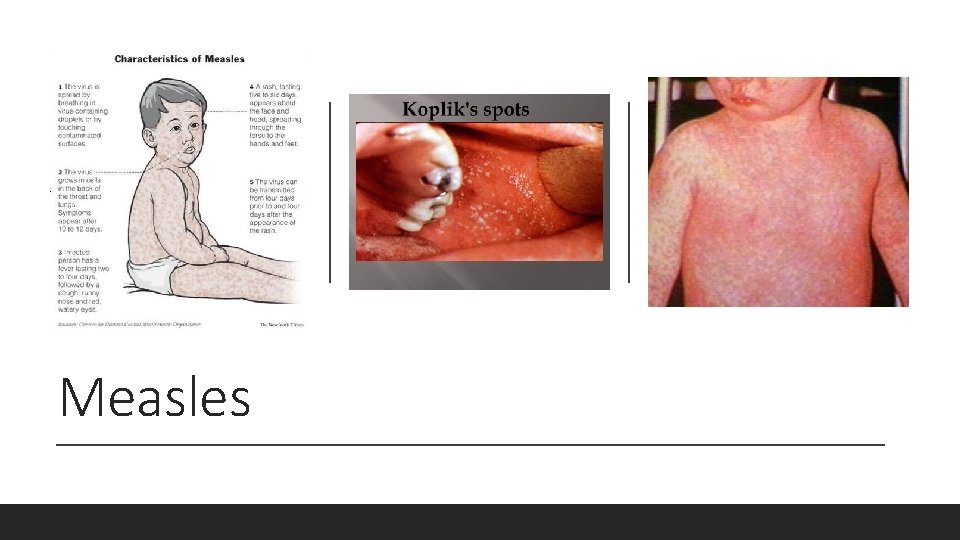
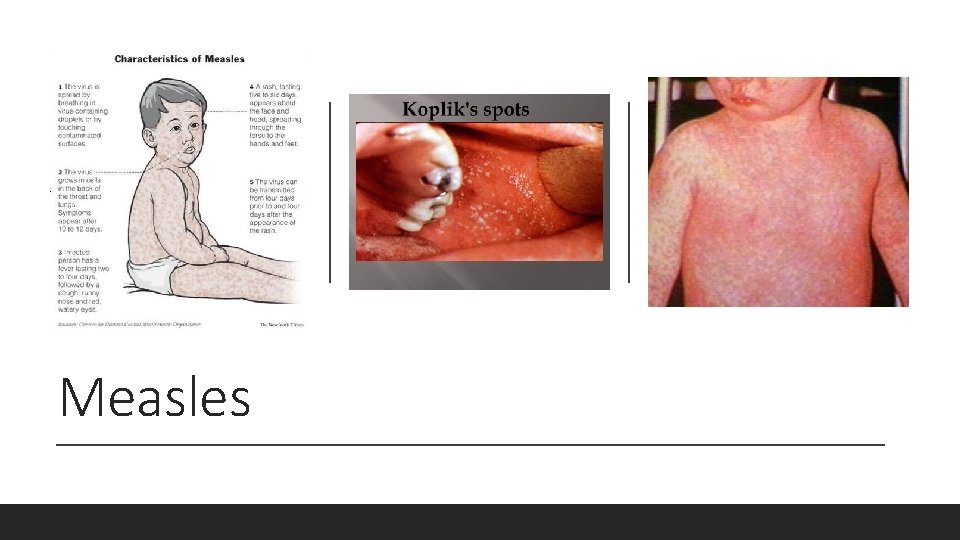
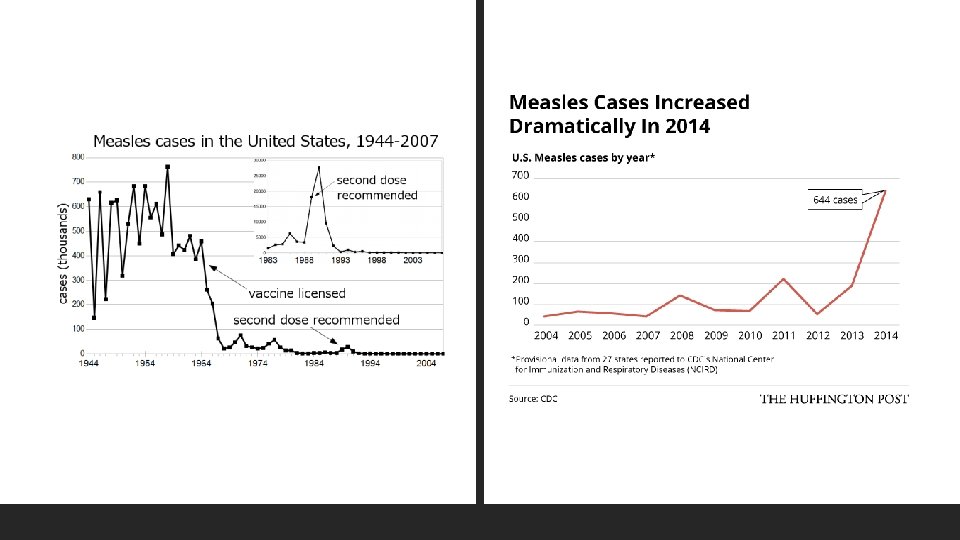
Measles