Ortopedick klinika UK 2 LF a FN Motol









- Slides: 40

Ortopedická klinika UK. 2. LF a FN Motol Dětská a dospělá ortopedie a traumatologie
Ostheosynthesis
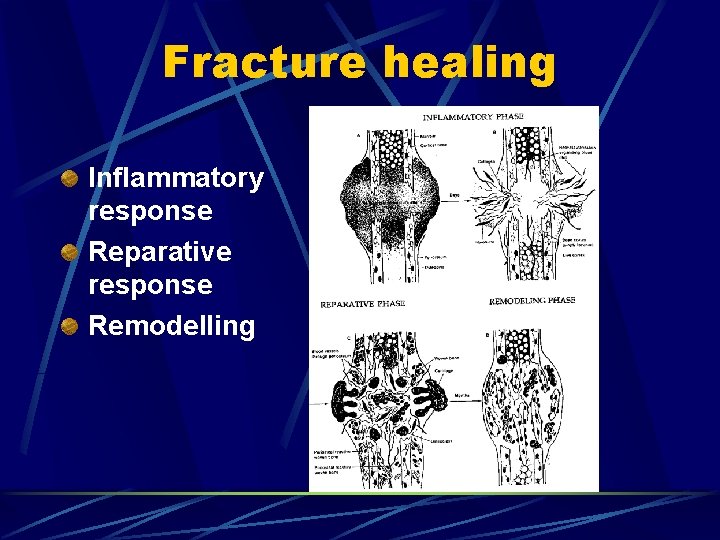
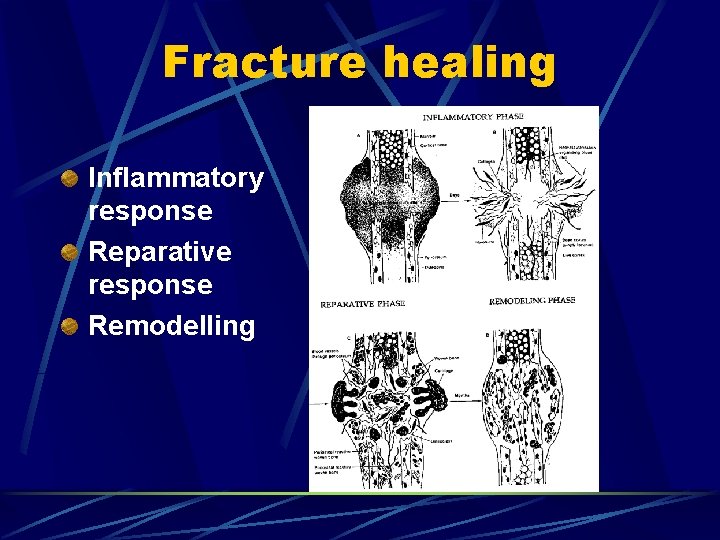
Fracture healing Inflammatory response Reparative response Remodelling
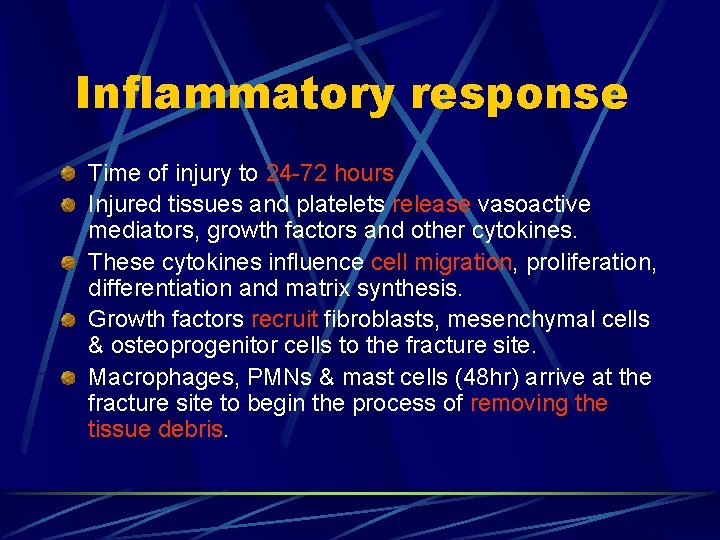
Inflammatory response Time of injury to 24 -72 hours Injured tissues and platelets release vasoactive mediators, growth factors and other cytokines. These cytokines influence cell migration, proliferation, differentiation and matrix synthesis. Growth factors recruit fibroblasts, mesenchymal cells & osteoprogenitor cells to the fracture site. Macrophages, PMNs & mast cells (48 hr) arrive at the fracture site to begin the process of removing the tissue debris.
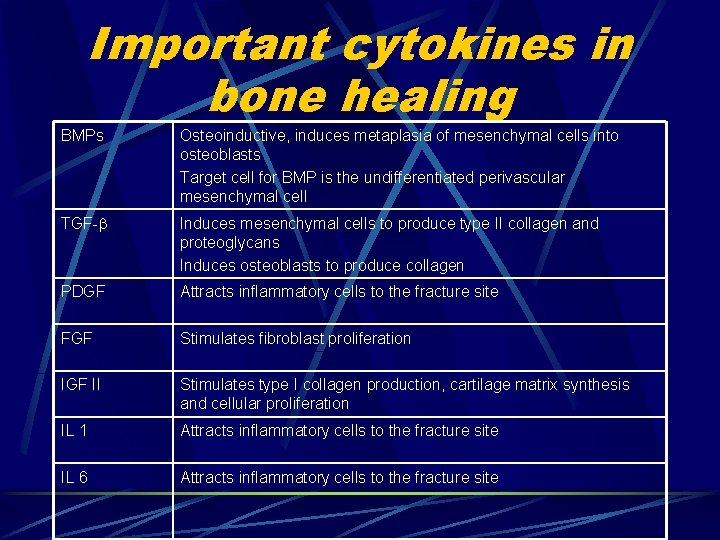
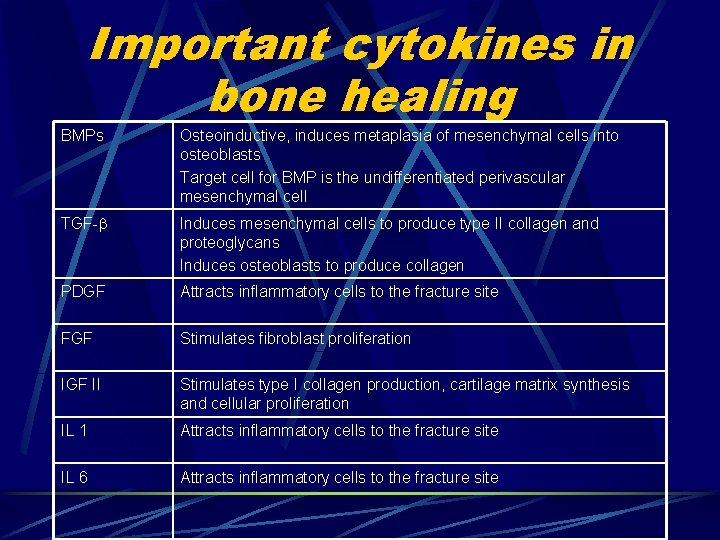
Important cytokines in bone healing BMPs Osteoinductive, induces metaplasia of mesenchymal cells into osteoblasts Target cell for BMP is the undifferentiated perivascular mesenchymal cell TGF- Induces mesenchymal cells to produce type II collagen and proteoglycans Induces osteoblasts to produce collagen PDGF Attracts inflammatory cells to the fracture site FGF Stimulates fibroblast proliferation IGF II Stimulates type I collagen production, cartilage matrix synthesis and cellular proliferation IL 1 Attracts inflammatory cells to the fracture site IL 6 Attracts inflammatory cells to the fracture site
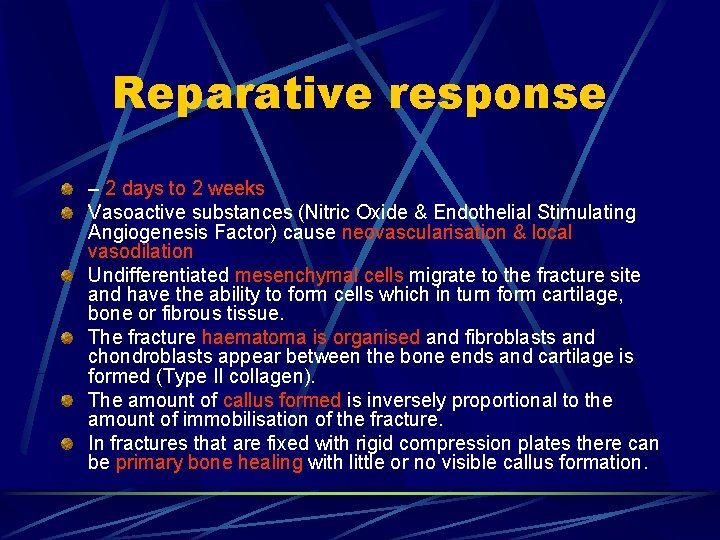
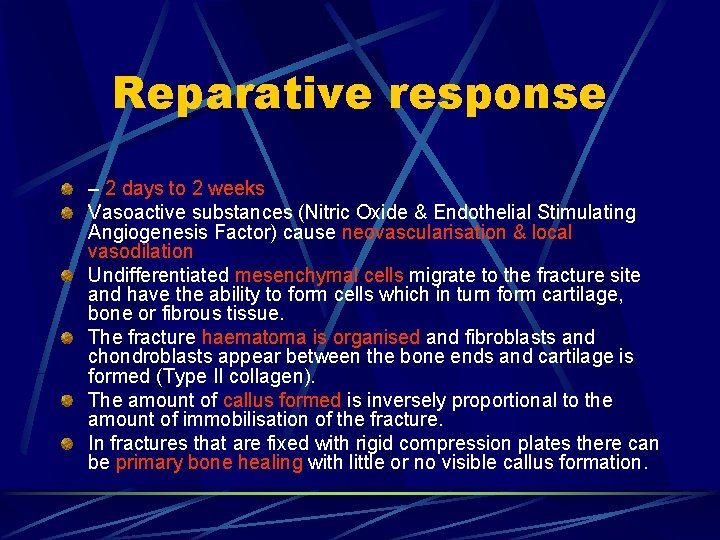
Reparative response – 2 days to 2 weeks Vasoactive substances (Nitric Oxide & Endothelial Stimulating Angiogenesis Factor) cause neovascularisation & local vasodilation Undifferentiated mesenchymal cells migrate to the fracture site and have the ability to form cells which in turn form cartilage, bone or fibrous tissue. The fracture haematoma is organised and fibroblasts and chondroblasts appear between the bone ends and cartilage is formed (Type II collagen). The amount of callus formed is inversely proportional to the amount of immobilisation of the fracture. In fractures that are fixed with rigid compression plates there can be primary bone healing with little or no visible callus formation.
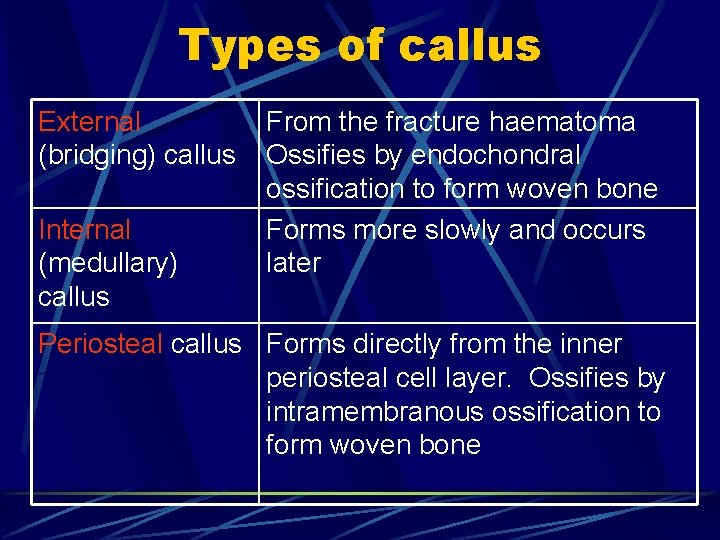
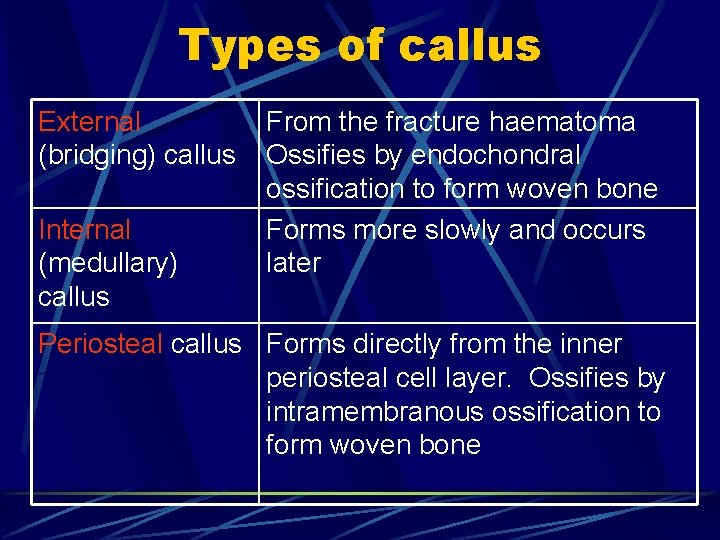
Types of callus External (bridging) callus Internal (medullary) callus From the fracture haematoma Ossifies by endochondral ossification to form woven bone Forms more slowly and occurs later Periosteal callus Forms directly from the inner periosteal cell layer. Ossifies by intramembranous ossification to form woven bone
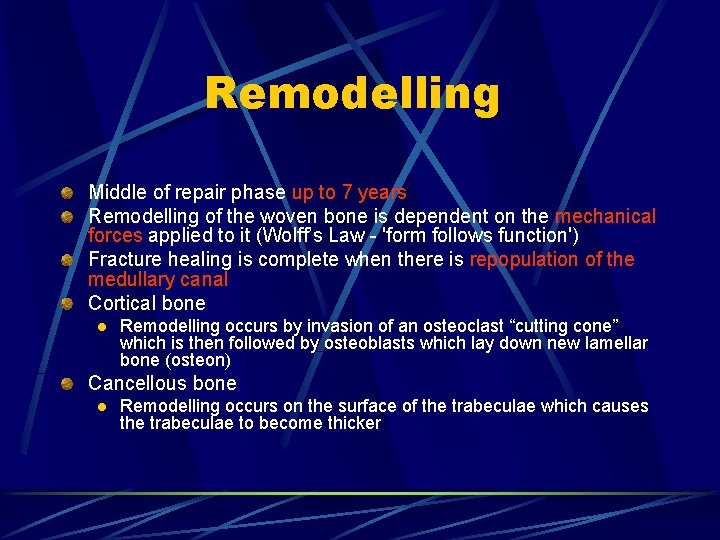
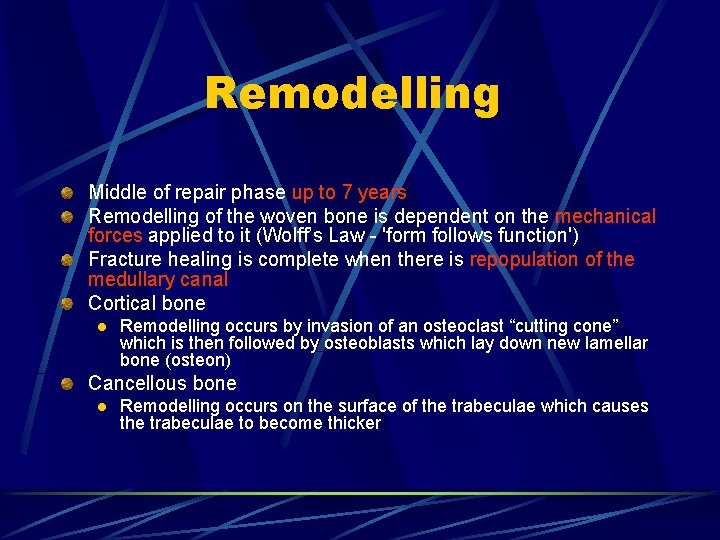
Remodelling Middle of repair phase up to 7 years Remodelling of the woven bone is dependent on the mechanical forces applied to it (Wolff’s Law - 'form follows function') Fracture healing is complete when there is repopulation of the medullary canal Cortical bone l Remodelling occurs by invasion of an osteoclast “cutting cone” which is then followed by osteoblasts which lay down new lamellar bone (osteon) Cancellous bone l Remodelling occurs on the surface of the trabeculae which causes the trabeculae to become thicker
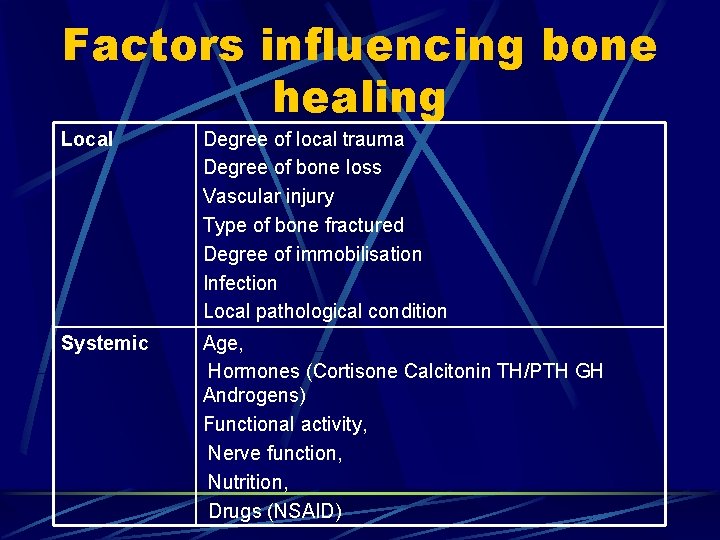
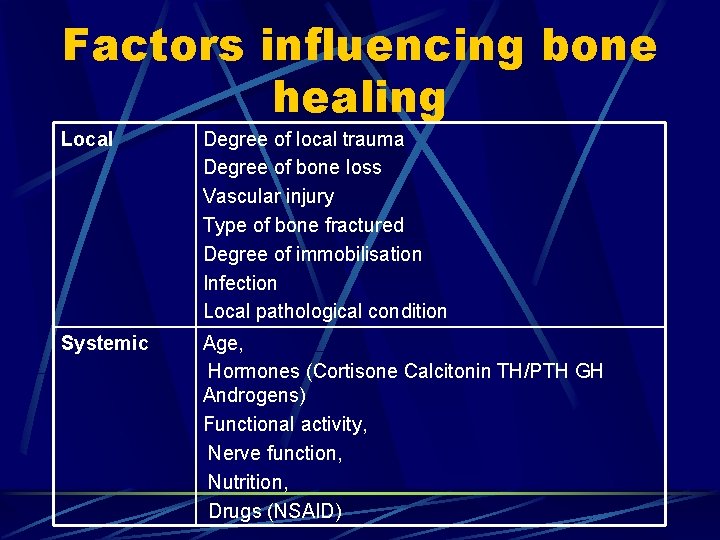
Factors influencing bone healing Local Degree of local trauma Degree of bone loss Vascular injury Type of bone fractured Degree of immobilisation Infection Local pathological condition Systemic Age, Hormones (Cortisone Calcitonin TH/PTH GH Androgens) Functional activity, Nerve function, Nutrition, Drugs (NSAID)
Fracture managemet first aid - immobilisation conservative operative
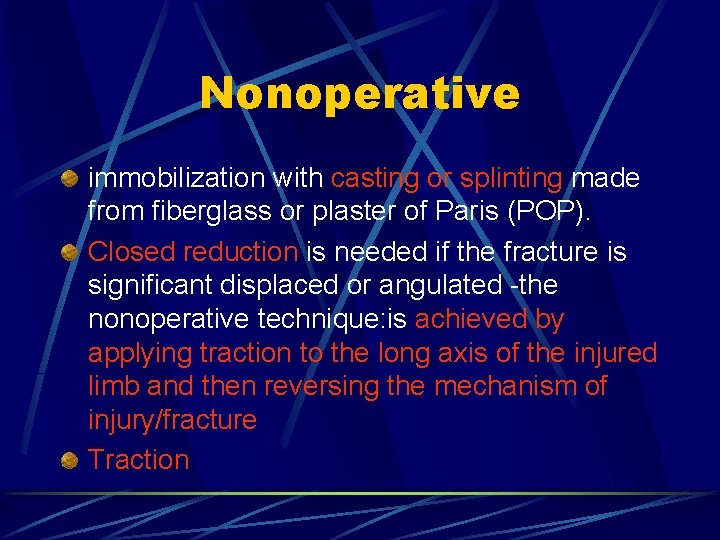
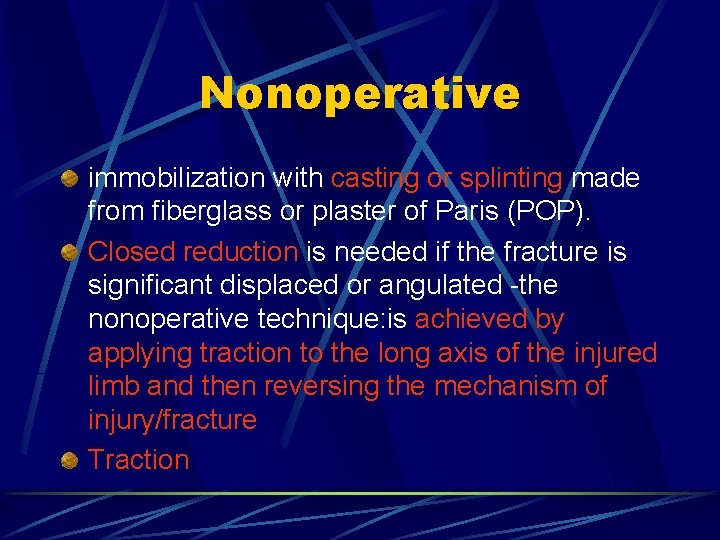
Nonoperative immobilization with casting or splinting made from fiberglass or plaster of Paris (POP). Closed reduction is needed if the fracture is significant displaced or angulated -the nonoperative technique: is achieved by applying traction to the long axis of the injured limb and then reversing the mechanism of injury/fracture Traction
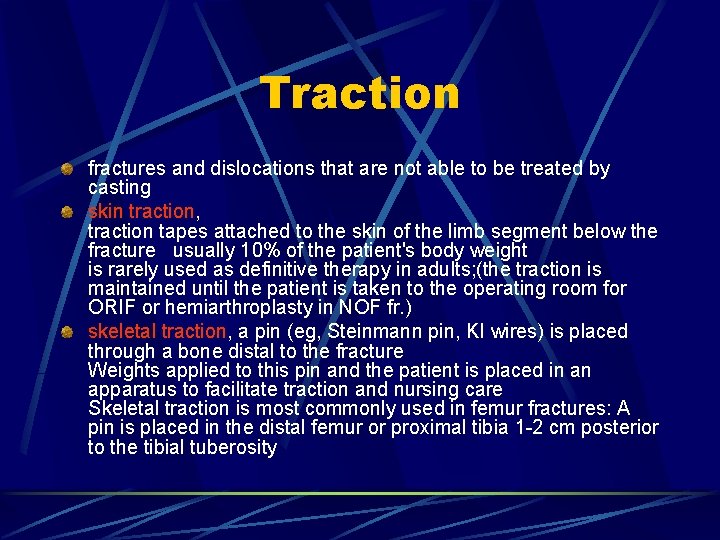
Traction fractures and dislocations that are not able to be treated by casting skin traction, traction tapes attached to the skin of the limb segment below the fracture usually 10% of the patient's body weight is rarely used as definitive therapy in adults; (the traction is maintained until the patient is taken to the operating room for ORIF or hemiarthroplasty in NOF fr. ) skeletal traction, a pin (eg, Steinmann pin, KI wires) is placed through a bone distal to the fracture Weights applied to this pin and the patient is placed in an apparatus to facilitate traction and nursing care Skeletal traction is most commonly used in femur fractures: A pin is placed in the distal femur or proximal tibia 1 -2 cm posterior to the tibial tuberosity
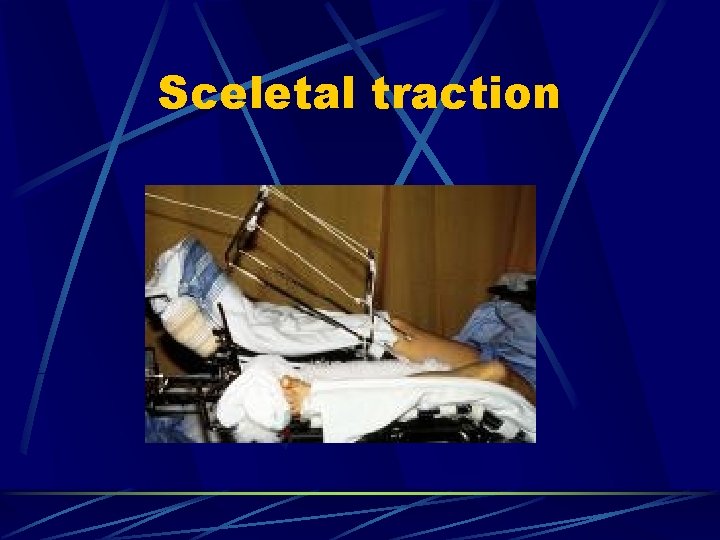
Sceletal traction
Operative Failed nonoperative (closed) management Unstable fractures that cannot be adequately maintained in a reduced position Displaced intra-articular fractures (>2 mm) Patients with fractures that are known to heal poorly following nonoperative management (eg, femoral neck fractures) Large avulsion fractures that disrupt the muscle-tendon or ligamentous function of an affected joint (eg, patella, olecranon fracture, ) Impending pathologic fractures Multiple traumatic injuries with fractures involving the pelvis, femur, or vertebrae Unstable open fractures or complicated open fractures Fractures in individuals who are poor candidates for nonoperative management that requires prolonged immobilization (eg, elderly patients with proximal femur fractures) Fractures in growth areas in skeletally immature individuals that have increased risk for growth arrest (eg, Salter-Harris types III-V) Nonunions or malunions that have failed to respond to nonoperative treatment

Surgical therapy In 1958, the Association for the Study of Internal Fixation (ASIF) OA( Arbeitsgemeinschaft für Osteosynthesefragen) 4 treatment goals 1. Anatomic reduction of the fracture fragments: diaphysis: anatomical alignment assuring length, angulation, and rotation intra-articular fractures: anatomic reduction of all fragments. 2. Stable internal fixation to fulfill biomechanical demands 3. Preservation of blood supply to the injured area of the extremity 4. Active pain-free mobilization of adjacent muscles and joints
Surgical therapy ORIF - Open reduction and internal fixation Kirschner wires (K- wires) Plates and screws Intramedullary nailing External fixation
Open reduction and internal fixation exposing the fracture site and obtaining a reduction of the fracture must be stabilized and maintained
AO principles System Fixation elements Surgical technique Complications resolving Manual
New technique
Kirschner wires commonly used in fractures around joints. resist only changes in alignment, they do not resist rotation and have poor resistance to torque and bending forces used as adjunctive fixation for screws or plates and screws casting or splinting is used in conjunction. can be placed percutaneously adequate for small fragments in metaphyseal and epiphyseal regions, especially in fractures of the distal foot, wrist, and hand, ( Colles fractures, and in displaced metacarpal and phalangeal fractures after closed reduction )

Plates and screws designs vary depending on the anatomic region and size of the bone used in the management of articular fractures allows early ROM and the use of muscles and joints strength and stability, neutralize forces Buttress plates counteract compression and shear - metaphysis and epiphysis used around joints to support intra-articular fractures Compression plates (DCP – Dinamic commpression plate, LC-DCP low contact dinamic commpression plate) counteract bending, shear, and torsion, eccentrically loaded holes in the plate used in long bones (fibula, radius, and ulna) Neutralization plates combination with interfragmentary screw fixation interfragmentary compression screws provide compression, plate neutralizes torsional, bending, and shear forces ( lag screws increases the stability of the construct) (fibula, radius and ulna, and humerus) Bridge plates - management of multifragmented diaphyseal and metaphyseal fractures.



Contraindications of ORIF Active infection (local or systemic) or osteomyelitis Osteoporotic bone that is too weak to sustain internal or external fixation Soft tissues overlying the fracture or surgical approach that are poor in quality due to burns, surgical scars, or infection (In such scenarios, soft tissue coverage is recommended. ) Medical conditions that contraindicate surgery or anesthesia (eg, recent myocardial infarction) Cases in which amputation would better serve the limb and the patient
Intramedullary nailing widely accepted operate like an internal splint allows for compressive forces at the fracture site, which stimulates bone healing minimally invasive procedures femoral shaft fr. UFN, tibial shaft fr. UTN; humeral shaft fr. UHN. ESIN Elastic stabilization intramedullary nailing TEN – titanium elastic nail Intramedullary nails: 1. flexible or rigid, 2. locked (maintain alignment and length, and limit rotation) or unlocked, 3. reamed or unreamed,


Complications surgical management Neurologic and vascular injury Compartment syndrome Infection Thromboembolic events Avascular necrosis Posttraumatic arthritis
Neurologic and vascular injury nerve injury - patient experiences motor or sensory deficiencies Arterial injury - pulses are diminished or absent - immediate realignment, angiography is indicated - vascular surgeons (knee dislocations, proximal tibial fractures, and supracondylar humerus fractures)
Compartment syndrome reported by von Volkmann in 1872, potentially limb-threatening condition, tissue pressure exceeds perfusion pressure in a closed anatomic space ( hand, forearm, upper arm, most commonly occurs in the anterior compartment of the leg) involves tissue necrosis; functional limb impairment; renal failure secondary to rhabdomyolysis, which may lead to death occur after traumatic injury, after ischemia (eg, after hemorrhage or thromboembolic event); and in rare cases, with exercise Clinically: pain out of proportion to the degree of injury, pain with passive stretch of the involved muscles, pallor, paresthesia, pulselessness is a late finding can be measured greater 30 mm Hg indicates surgical fasciotomy of the affected compartments.
Infection local infection: cellulitis, osteomyelitis, systemic infection, sepsis Early recognition prevents the development of sepsis The most common pathogen is Staphylococcus aureus, group A streptococci, coagulase-negative staphylococci, enterococci ATB should be administered if an infection is suspected, lab: C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) If infection cannot be eradicated with antibiotics, I&D of the surgical wound may be necessary, with removal of the hardware, but only if it is not performing its role.
Thromboembolic events may occur after trauma with prolonged immobilization immobile for 10 or more days have a 67% incidence of thrombosis (Canale, 1998) prophylaxis is effective in decreasing the incidence of deep vein thrombosis, but it has not been shown to be effective in decreasing the incidence of fatal pulmonary embolism. Prophylactic anticoagulation LMWH, Warfarin, early mobilization
Avascular necrosis disruption of blood supply to a region of bone can lead to nonunion, bone collapse, or degenerative changes associated with NOF # and femoral head #, scaphoid, talar neck and body, and proximal humerus.
Posttraumatic arthritis common in intra-articular fractures that are not adequately reduced management: arthroscopic debridement, osteotomy, arthroplasty, or arthrodesis
External fixation In 1907 in Alvin Lambotte, 1952 Ilizarev provides stabilization at a distance from the fracture site without interfering with the soft tissue structures maintains length, alignment, and rotation without requiring casting allows inspection types: Wagner, Orthofix, Unifix, Indications Open fractures with significant soft tissue disruption (eg, type II or III open fractures) Soft tissue injury (eg, burns) Pelvic fractures (temporarily) Severely comminuted and unstable fractures Fractures that are associated with bony deficits Limb-lengthening procedures Fractures associated with infection or nonunion arthrodesis

Complications of external fixation pin tract infection, pin loosening or breakage, interference with joint motion, neurovascular damage when placing pins, malalignment caused by poor placement of the fixator, delayed union and malunion
Spetial types of osteosynthesis LISS ( less invasive stabilisation system) implants for MIPPO (minimal invasive percutane plate osteosynthesis) -Herbert´s screw – scafoid # DHS – NOF# basicervical PFN – NOF # pertrochanteric Phillos –prox. humerus DCS (dinamic condylar screw) and DFN (distal femoral nail) - dist. femur Pilon plate – dist. tibia
 Hypestesie
Hypestesie Ortopedick
Ortopedick Clinica orthopedica lekari
Clinica orthopedica lekari Ortopedick
Ortopedick Reumathoid artritis
Reumathoid artritis Ortopedick
Ortopedick Kyfoscoliosis
Kyfoscoliosis Ppv
Ppv Klinika patologii noworodka zabrze
Klinika patologii noworodka zabrze Emng zotovic
Emng zotovic Lowestoft polska klinika
Lowestoft polska klinika Uroloska klinika kcs
Uroloska klinika kcs Klinika za psihijatriju kcs
Klinika za psihijatriju kcs Neurológiai klinika szeged
Neurológiai klinika szeged Klinika za infektivne bolesti
Klinika za infektivne bolesti Breier klinika
Breier klinika Zagrai ramona
Zagrai ramona Dzintars tīds
Dzintars tīds Szeged klinika mri vizsgálat
Szeged klinika mri vizsgálat Bcb klinika
Bcb klinika Klinika prawa definicja
Klinika prawa definicja Zan mitrev
Zan mitrev Holangit
Holangit Semmelweis egyetem konzerváló fogászati klinika budapest
Semmelweis egyetem konzerváló fogászati klinika budapest Laringotraheobronhitis
Laringotraheobronhitis Klinika za zarazne bolesti veterinarski fakultet
Klinika za zarazne bolesti veterinarski fakultet Grlich
Grlich Boli maligne
Boli maligne Neurologická klinika nitra
Neurologická klinika nitra Friintern
Friintern Semmelweis egyetem szemészeti klinika budapest
Semmelweis egyetem szemészeti klinika budapest Dominika szalewska
Dominika szalewska Klinika xp
Klinika xp