Ocular Myasthenia Gravis Diagnostic Studies and Long Term

- Slides: 40
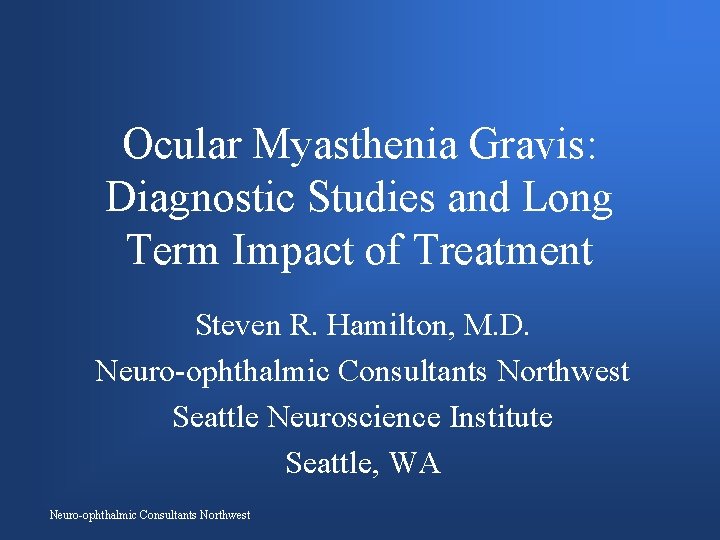
Ocular Myasthenia Gravis: Diagnostic Studies and Long Term Impact of Treatment Steven R. Hamilton, M. D. Neuro-ophthalmic Consultants Northwest Seattle Neuroscience Institute Seattle, WA Neuro-ophthalmic Consultants Northwest
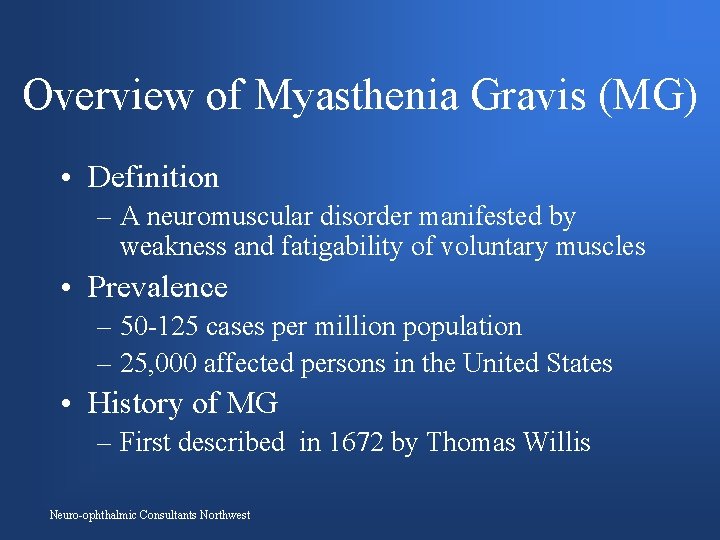
Overview of Myasthenia Gravis (MG) • Definition – A neuromuscular disorder manifested by weakness and fatigability of voluntary muscles • Prevalence – 50 -125 cases per million population – 25, 000 affected persons in the United States • History of MG – First described in 1672 by Thomas Willis Neuro-ophthalmic Consultants Northwest
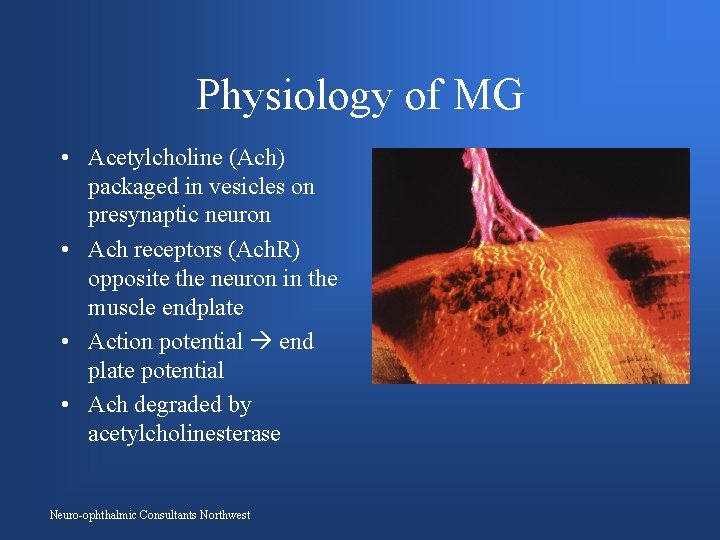
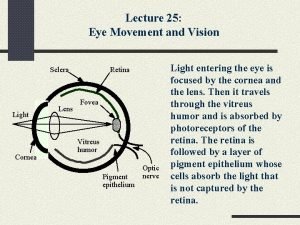
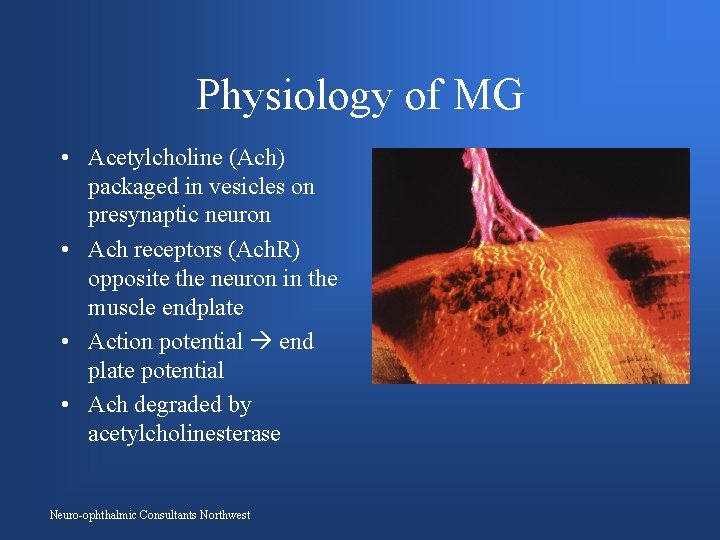
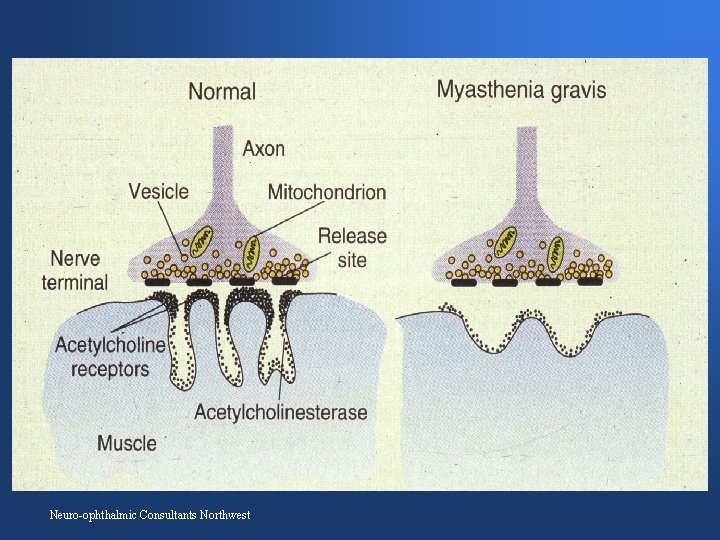
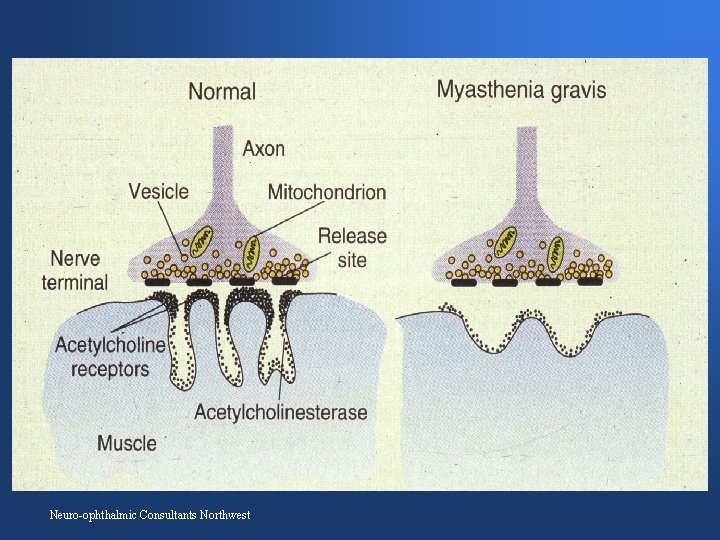
Physiology of MG • Acetylcholine (Ach) packaged in vesicles on presynaptic neuron • Ach receptors (Ach. R) opposite the neuron in the muscle endplate • Action potential end plate potential • Ach degraded by acetylcholinesterase Neuro-ophthalmic Consultants Northwest
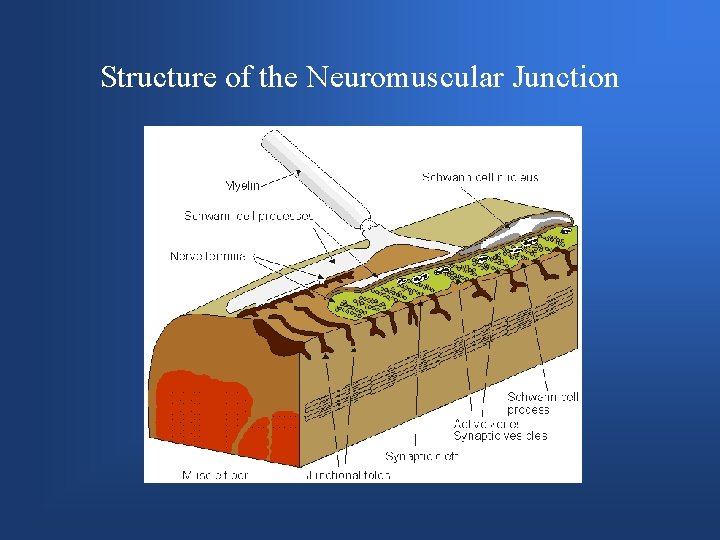
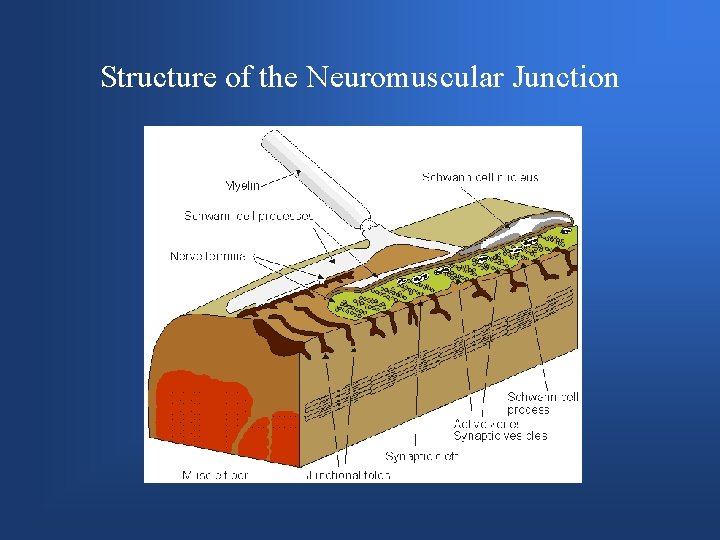
Structure of the Neuromuscular Junction
Neuro-ophthalmic Consultants Northwest
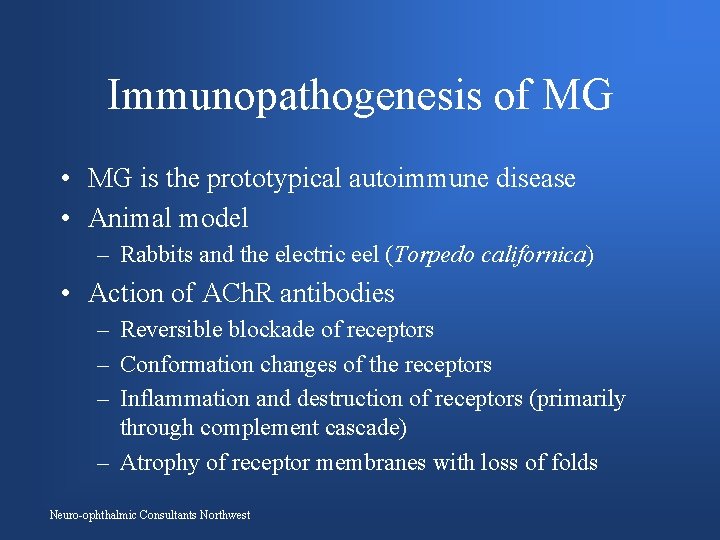
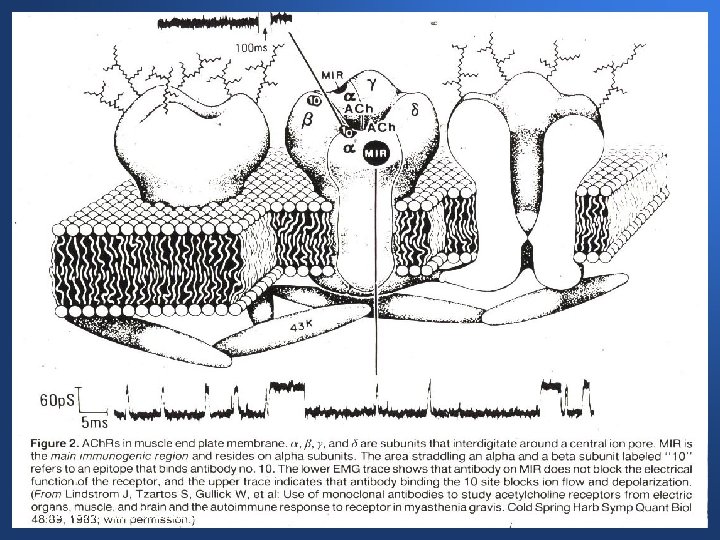
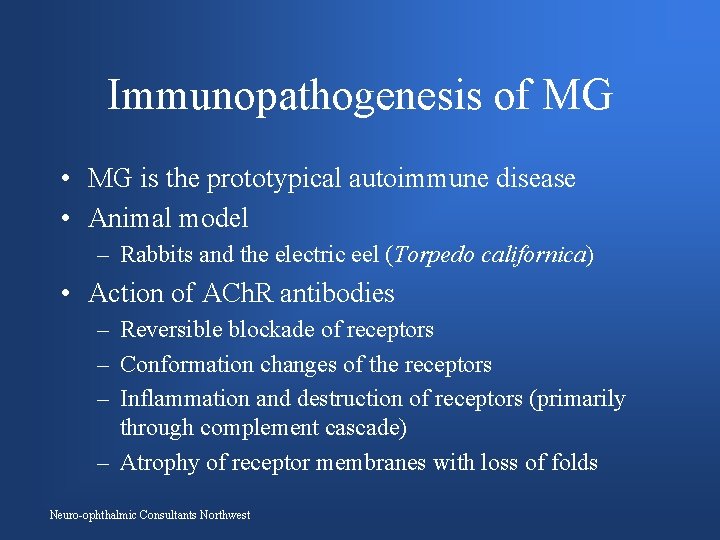
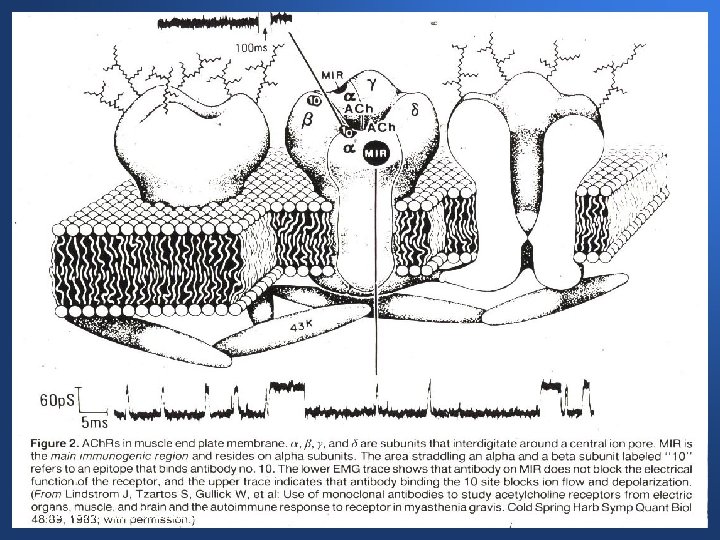
Immunopathogenesis of MG • MG is the prototypical autoimmune disease • Animal model – Rabbits and the electric eel (Torpedo californica) • Action of ACh. R antibodies – Reversible blockade of receptors – Conformation changes of the receptors – Inflammation and destruction of receptors (primarily through complement cascade) – Atrophy of receptor membranes with loss of folds Neuro-ophthalmic Consultants Northwest
Neuro-ophthalmic Consultants Northwest
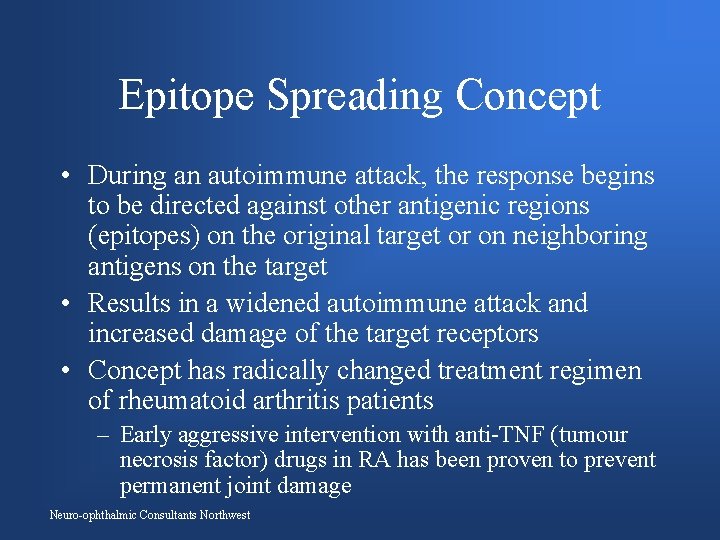
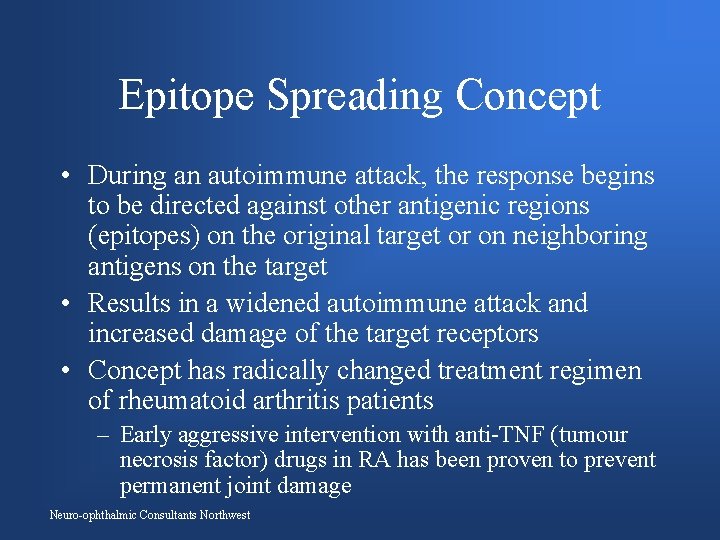
Epitope Spreading Concept • During an autoimmune attack, the response begins to be directed against other antigenic regions (epitopes) on the original target or on neighboring antigens on the target • Results in a widened autoimmune attack and increased damage of the target receptors • Concept has radically changed treatment regimen of rheumatoid arthritis patients – Early aggressive intervention with anti-TNF (tumour necrosis factor) drugs in RA has been proven to prevent permanent joint damage Neuro-ophthalmic Consultants Northwest
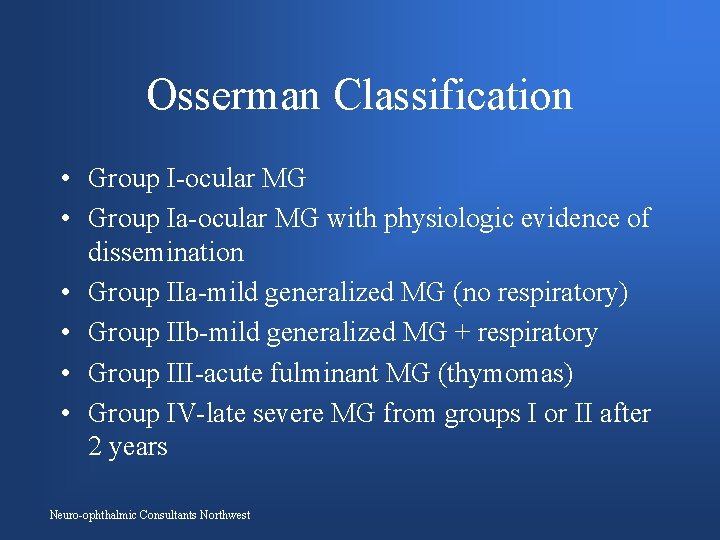
Osserman Classification • Group I-ocular MG • Group Ia-ocular MG with physiologic evidence of dissemination • Group IIa-mild generalized MG (no respiratory) • Group IIb-mild generalized MG + respiratory • Group III-acute fulminant MG (thymomas) • Group IV-late severe MG from groups I or II after 2 years Neuro-ophthalmic Consultants Northwest
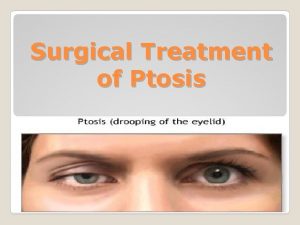
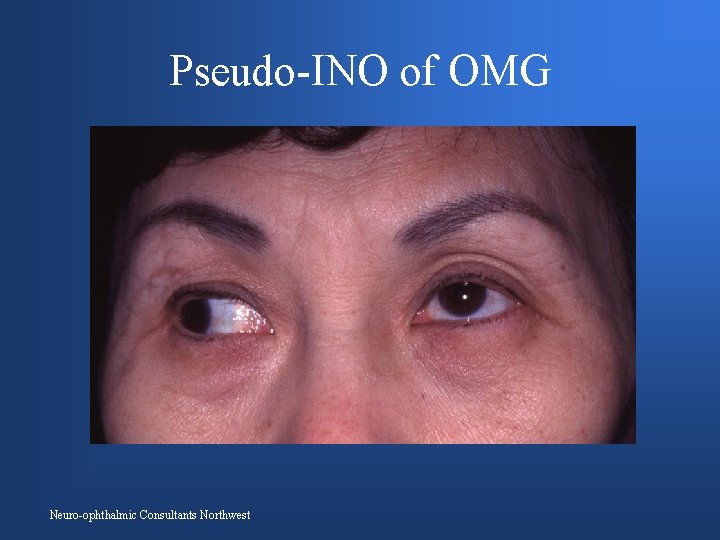
Ocular Myasthenia Gravis • Variable ptosis and diplopia – Presenting symptoms in 50 -70% of patients – Eventually present in 90% of MG patients • • Lid twitch and enhanced ptosis Weakness of orbicularis oculi muscles Pseudo-internuclear ophthalmoplegia Normal pupils Neuro-ophthalmic Consultants Northwest
“My left eyelid droops” • 66 -year-old man with thyroidectomy 40 years earlier • Residual proptosis without diplopia • Droopy left lid for one month, worse at night • Transient double vision recently Neuro-ophthalmic Consultants Northwest

Neuro-ophthalmic Consultants Northwest
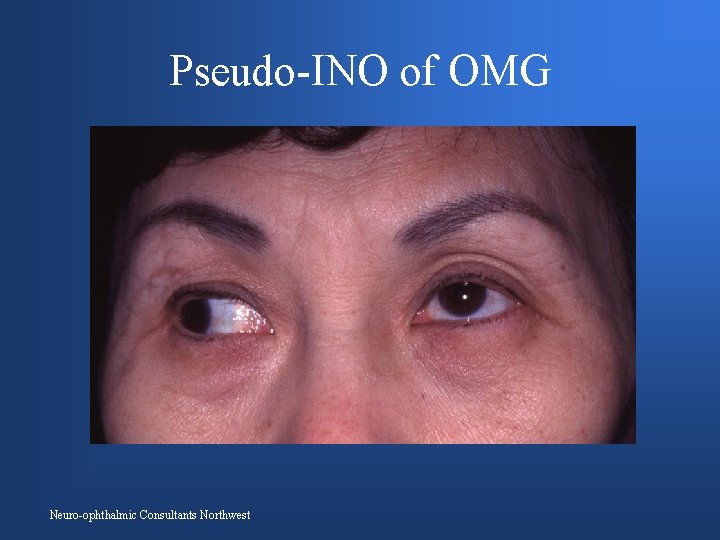
Pseudo-INO of OMG Neuro-ophthalmic Consultants Northwest
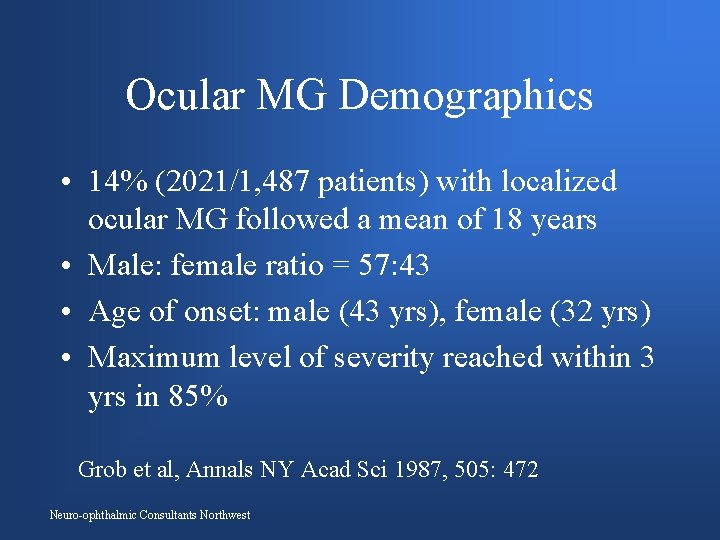
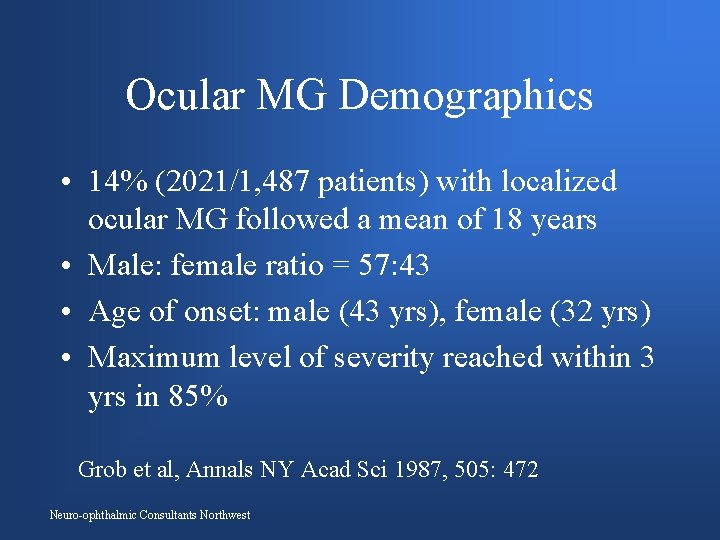
Ocular MG Demographics • 14% (2021/1, 487 patients) with localized ocular MG followed a mean of 18 years • Male: female ratio = 57: 43 • Age of onset: male (43 yrs), female (32 yrs) • Maximum level of severity reached within 3 yrs in 85% Grob et al, Annals NY Acad Sci 1987, 505: 472 Neuro-ophthalmic Consultants Northwest
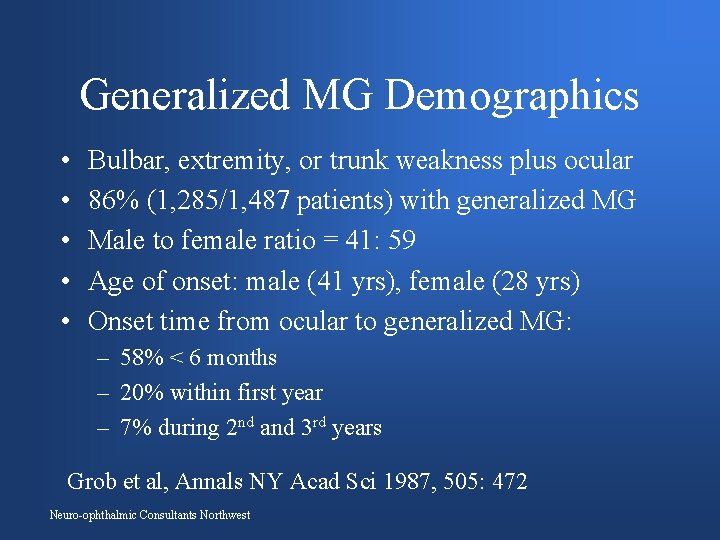
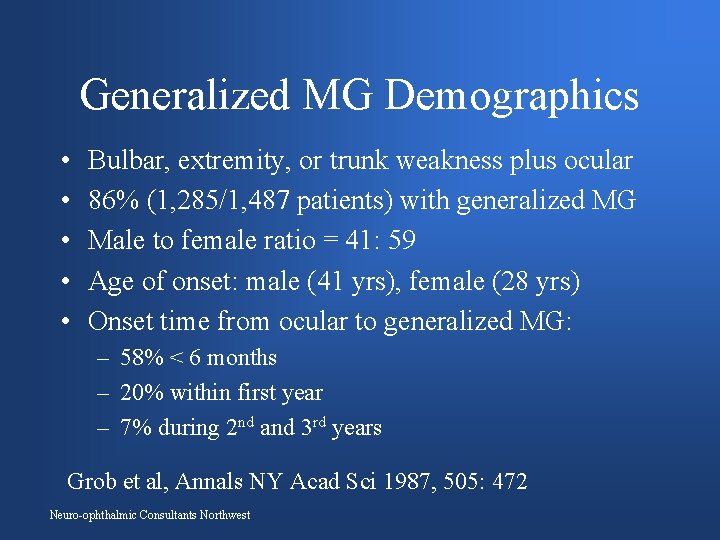
Generalized MG Demographics • • • Bulbar, extremity, or trunk weakness plus ocular 86% (1, 285/1, 487 patients) with generalized MG Male to female ratio = 41: 59 Age of onset: male (41 yrs), female (28 yrs) Onset time from ocular to generalized MG: – 58% < 6 months – 20% within first year – 7% during 2 nd and 3 rd years Grob et al, Annals NY Acad Sci 1987, 505: 472 Neuro-ophthalmic Consultants Northwest
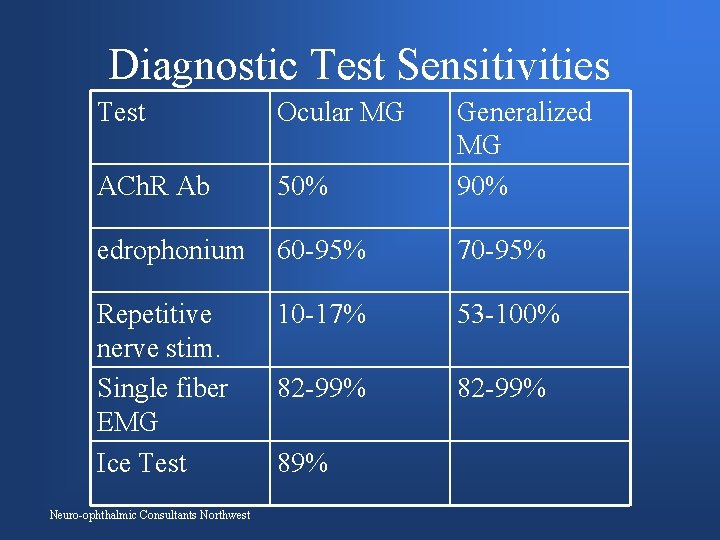
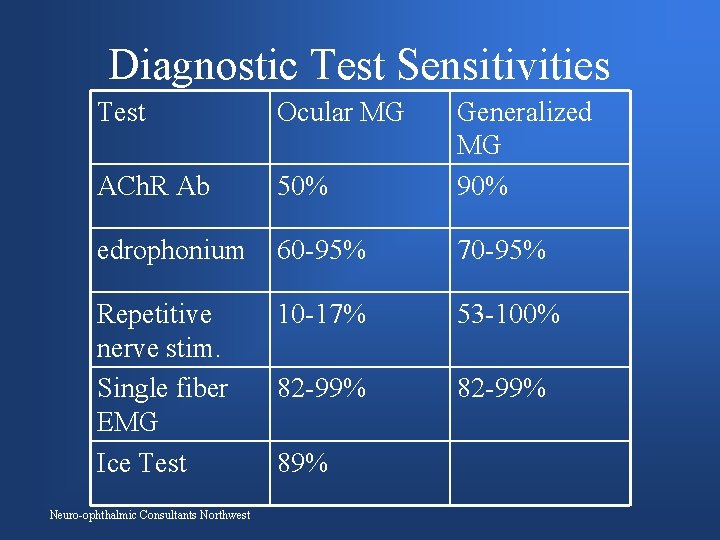
Diagnostic Test Sensitivities Test Ocular MG ACh. R Ab 50% Generalized MG 90% edrophonium 60 -95% 70 -95% Repetitive nerve stim. Single fiber EMG Ice Test 10 -17% 53 -100% 82 -99% Neuro-ophthalmic Consultants Northwest 89%
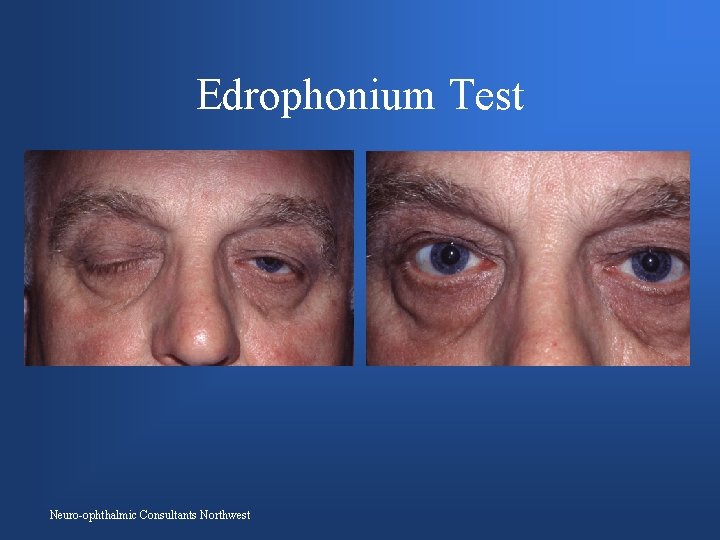
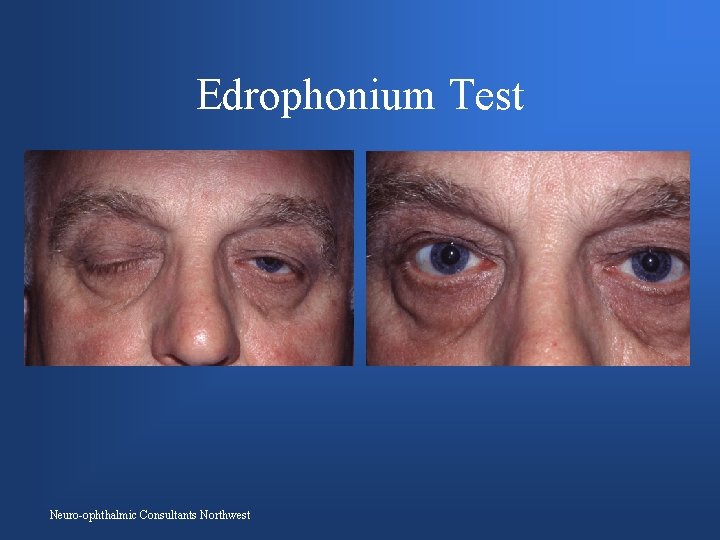
Edrophonium Test Neuro-ophthalmic Consultants Northwest
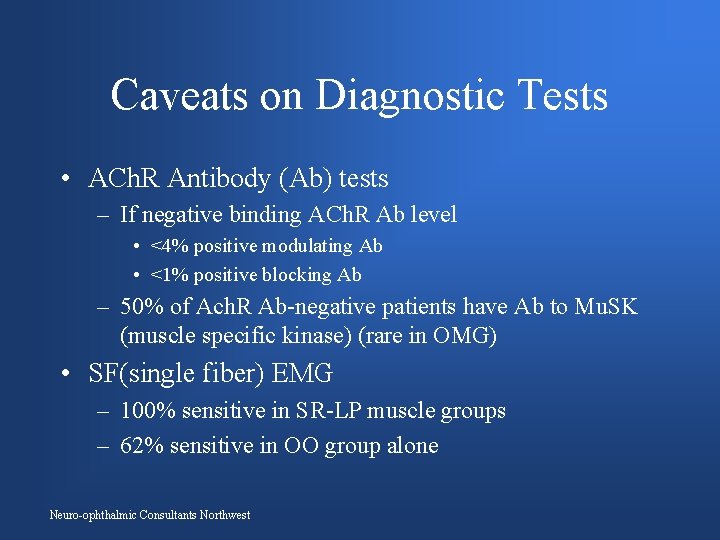
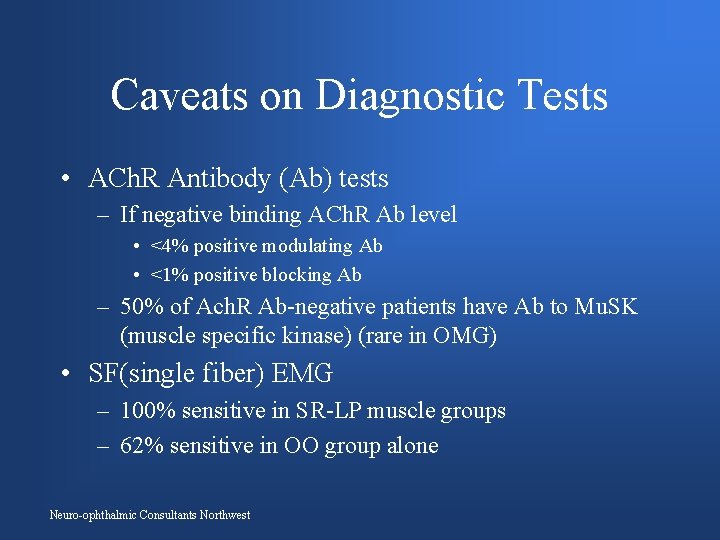
Caveats on Diagnostic Tests • ACh. R Antibody (Ab) tests – If negative binding ACh. R Ab level • <4% positive modulating Ab • <1% positive blocking Ab – 50% of Ach. R Ab-negative patients have Ab to Mu. SK (muscle specific kinase) (rare in OMG) • SF(single fiber) EMG – 100% sensitive in SR-LP muscle groups – 62% sensitive in OO group alone Neuro-ophthalmic Consultants Northwest
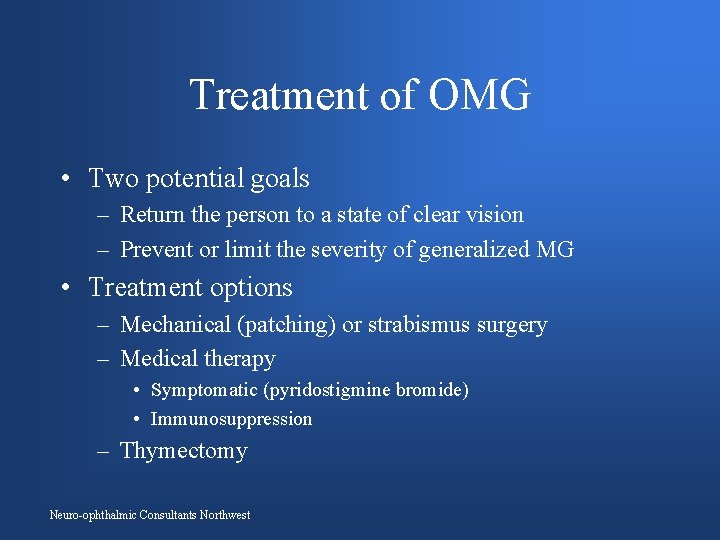
Treatment of OMG • Two potential goals – Return the person to a state of clear vision – Prevent or limit the severity of generalized MG • Treatment options – Mechanical (patching) or strabismus surgery – Medical therapy • Symptomatic (pyridostigmine bromide) • Immunosuppression – Thymectomy Neuro-ophthalmic Consultants Northwest
The Dangers of Patching ocular MG Patients • Too often patients are abandoned to poor quality of life without the chance of binocular vision • An easy fix for the treating neurologist without consideration of the long-term implications for quality of life and the risk of generalization of the disease Neuro-ophthalmic Consultants Northwest
Pyridostigmine Therapy of ocular MG • Improves visual disability in 20 -40% of OMG patients • Most effective for isolated variable ptosis • No immunomodulatory effect to prevent generalization of disease • May actually mask underlying progression of disease or even permit epitope spreading Neuro-ophthalmic Consultants Northwest
Immunosuppressive Therapies for Ocular MG • Cochrane Review 2006 – “There are no data from randomized controlled trials on the impact of any form of treatment on the risk of progression from ocular to generalized myasthenia gravis. ” • Observational studies (cohort and case studies) suggest corticosteroids and azathioprine may reduce the risk of generalization of ocular MG Neuro-ophthalmic Consultants Northwest
Corticosteroids for Ocular MG • Kupersmith et al. Arch Neurol. 2003 Feb; 60(2): 243 -8 – 147 pts with ocular MG – Treated with 6 weeks of 40 -60 mg prednisone per day with gradual taper to once-a-day or alternate-day low-dose therapy (2. 5 -10 mg) – 2 years follow-up data – 7% vs. 36% development of generalized MG Neuro-ophthalmic Consultants Northwest
Corticosteroid Therapy for ocular MG • Monsul et al. J Neurol Sci. 2004 Feb 15; 217(2): 131 -3 – 56 ocular MG patients • Treated patients received 60 mg prednisone per day with slow taper over 3 -6 months • 2 year follow-up • 11% vs. 35% development of generalized MG Neuro-ophthalmic Consultants Northwest
Combined Therapies for Ocular MG • Sommer et al. J Neurol Neurosurg Psychiatry. 1997 Feb; 62(2): 156 -62 – 78 pts with ocular MG with mean duration of disease of 8 years – Only 12% generalized if on corticosteroids (45), azathioprine (27), or both (23) – 64% generalized if on no immunosuppression • Thymectomy for abnormal chest CT also correlated with good outcome Neuro-ophthalmic Consultants Northwest
Combined Therapies for OMG • Mee et al. J Neuro-ophthalmol. 2003 Dec; 23(4): 24950 – Retrospective review of 34 patients who are positive for ACh. R Antibodies – Treatment with corticosteroids and/or azathioprine – 2 years of follow-up – 21/34 (62%) patients generalized • 9% of those on immunomodulatory therapy generalized • 86% of those on pyridostigmine alone generalized Neuro-ophthalmic Consultants Northwest
Mycophenolate mofetil • Pro-drug of mycophenolic acid – first isolated in 1898 from Penicillium • Inhibits lymphocyte purine synthesis by reversibly and noncompetitively blocking inosine monophosphate dehydrogenase. • Highly specific for lymphocytes • Side effects: gastrointestinal upset, increased liver function tests. Rare bone marrow suppression. • Better tolerated than azathioprine and cyclosporine (less nephrotoxic) Neuro-ophthalmic Consultants Northwest
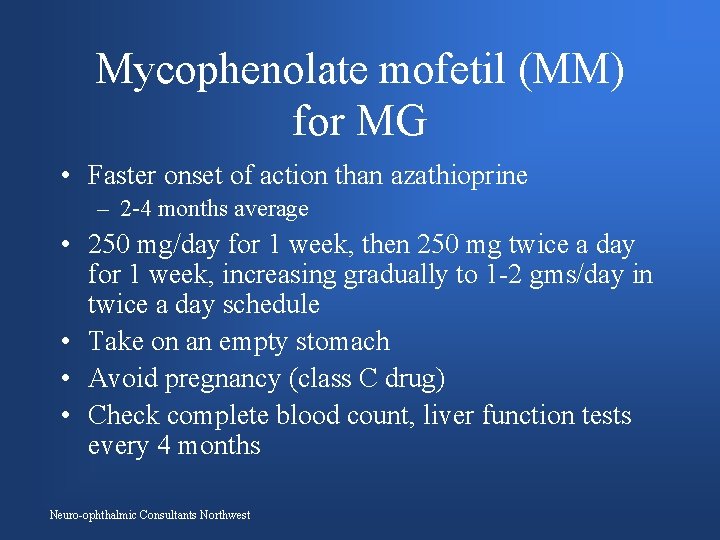
Mycophenolate mofetil (MM) for MG • Faster onset of action than azathioprine – 2 -4 months average • 250 mg/day for 1 week, then 250 mg twice a day for 1 week, increasing gradually to 1 -2 gms/day in twice a day schedule • Take on an empty stomach • Avoid pregnancy (class C drug) • Check complete blood count, liver function tests every 4 months Neuro-ophthalmic Consultants Northwest
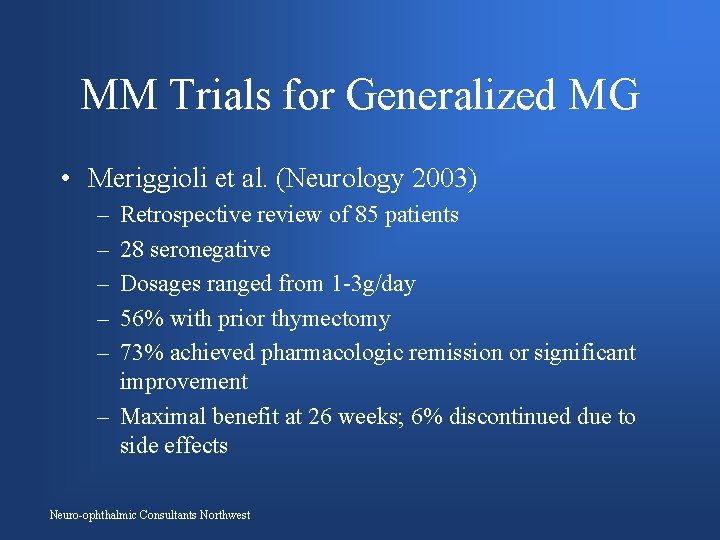
MM Trials for Generalized MG • Meriggioli et al. (Neurology 2003) – – – Retrospective review of 85 patients 28 seronegative Dosages ranged from 1 -3 g/day 56% with prior thymectomy 73% achieved pharmacologic remission or significant improvement – Maximal benefit at 26 weeks; 6% discontinued due to side effects Neuro-ophthalmic Consultants Northwest
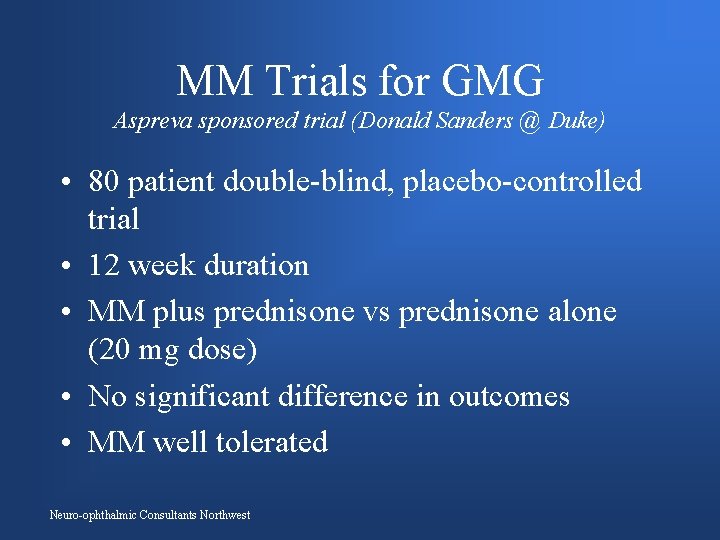
MM Trials for GMG Aspreva sponsored trial (Donald Sanders @ Duke) • 80 patient double-blind, placebo-controlled trial • 12 week duration • MM plus prednisone vs prednisone alone (20 mg dose) • No significant difference in outcomes • MM well tolerated Neuro-ophthalmic Consultants Northwest
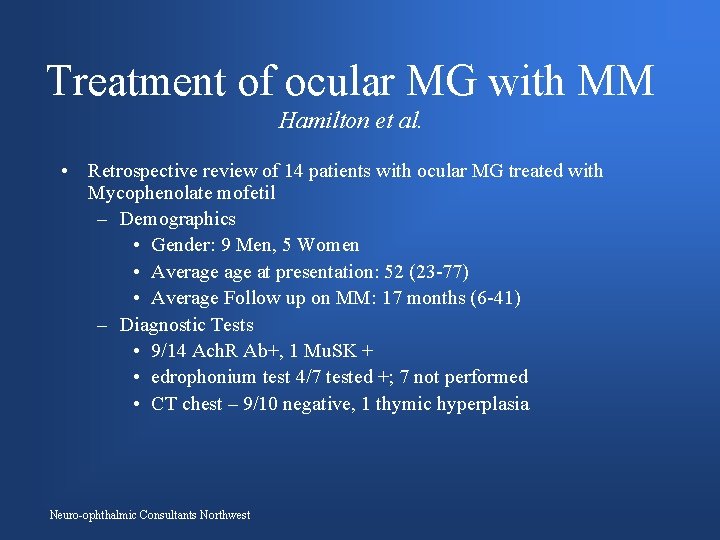
Treatment of ocular MG with MM Hamilton et al. • Retrospective review of 14 patients with ocular MG treated with Mycophenolate mofetil – Demographics • Gender: 9 Men, 5 Women • Average at presentation: 52 (23 -77) • Average Follow up on MM: 17 months (6 -41) – Diagnostic Tests • 9/14 Ach. R Ab+, 1 Mu. SK + • edrophonium test 4/7 tested +; 7 not performed • CT chest – 9/10 negative, 1 thymic hyperplasia Neuro-ophthalmic Consultants Northwest
Study Design • Patients were started on MM for one of three reasons – Primary agent besides pyridostigmine (3/14) – Worsening symptoms on other immunosuppressives (8/14) – Tapering off other immunosuppressives (3/14) Neuro-ophthalmic Consultants Northwest
Study Design • Starting dose MM 250 mg daily with gradual increase to target dose of 1 gm twice a day. • Minimum duration of treatment for at least 6 months. • Blood monitoring of complete blood count with differential and liver function tests. – Initially every 2 weeks – Quarterly when patient reached maintenance Neuro-ophthalmic Consultants Northwest
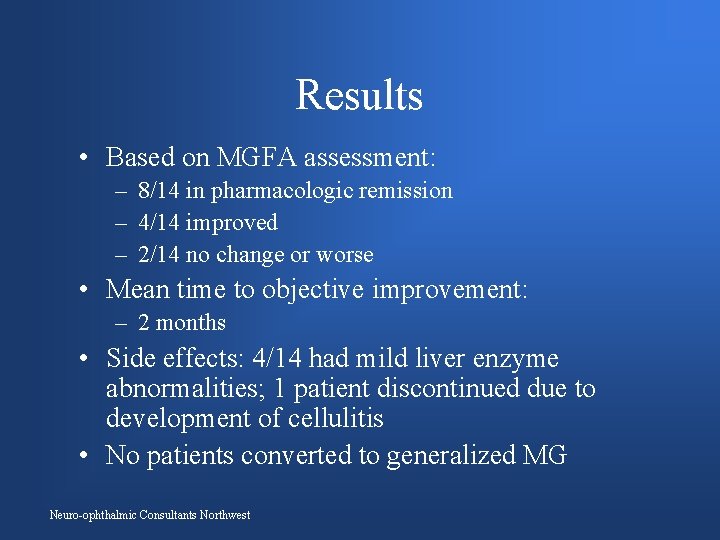
Results • 13/14 patients were able to reach a maintenance dose of 1 g twice a day. 1 patient reached 1, 750 mg daily • 2 patients discontinued the medication – 1 due to development of cellulitis – 1 due to lack of response Neuro-ophthalmic Consultants Northwest
Results • Based on MGFA assessment: – 8/14 in pharmacologic remission – 4/14 improved – 2/14 no change or worse • Mean time to objective improvement: – 2 months • Side effects: 4/14 had mild liver enzyme abnormalities; 1 patient discontinued due to development of cellulitis • No patients converted to generalized MG Neuro-ophthalmic Consultants Northwest
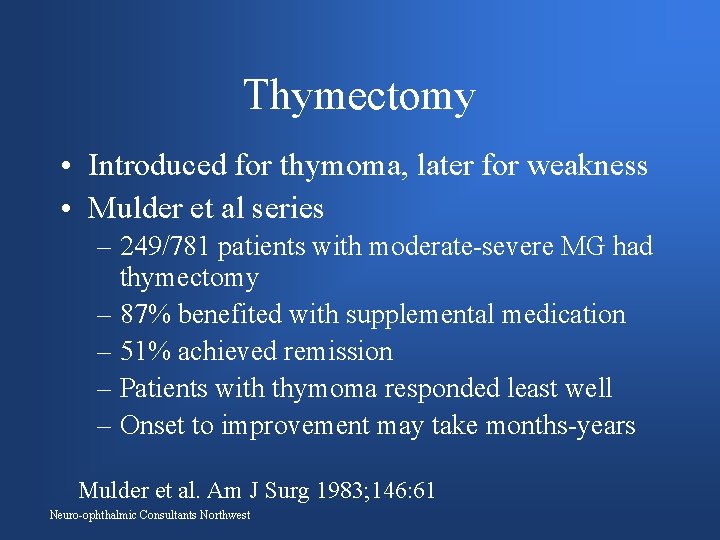
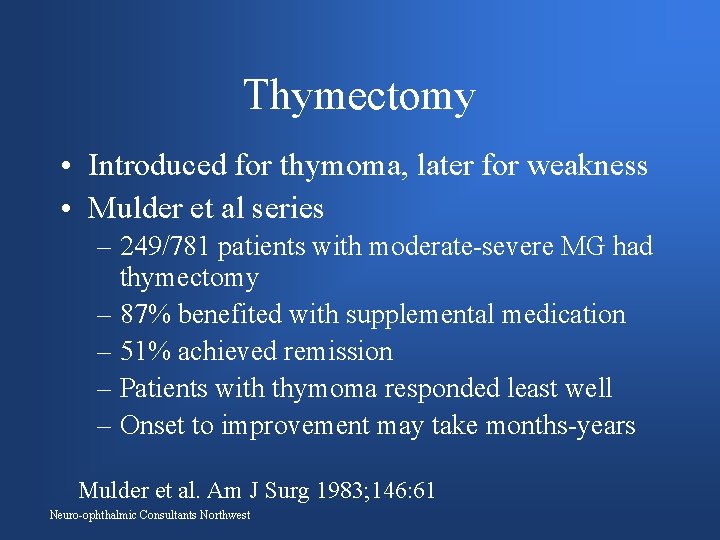
Thymectomy • Introduced for thymoma, later for weakness • Mulder et al series – 249/781 patients with moderate-severe MG had thymectomy – 87% benefited with supplemental medication – 51% achieved remission – Patients with thymoma responded least well – Onset to improvement may take months-years Mulder et al. Am J Surg 1983; 146: 61 Neuro-ophthalmic Consultants Northwest
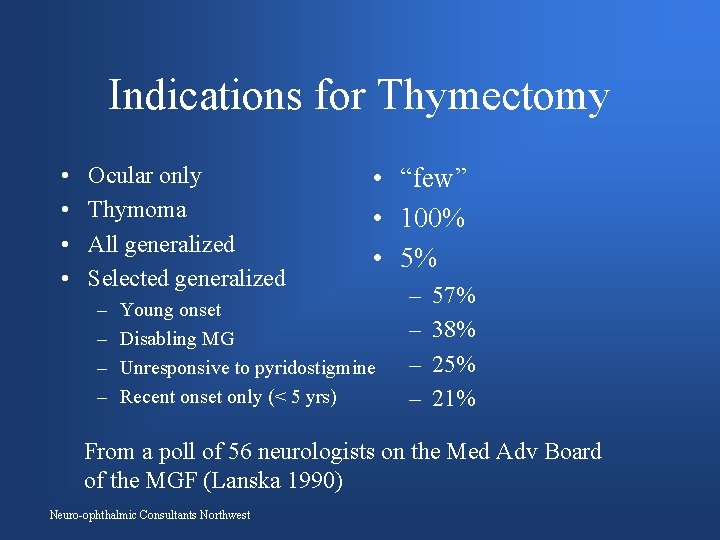
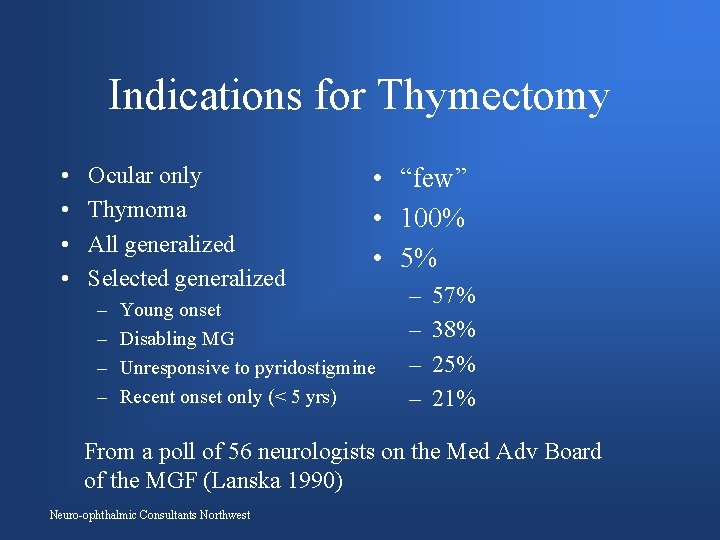
Indications for Thymectomy • • Ocular only Thymoma All generalized Selected generalized – – • “few” • 100% • 5% Young onset Disabling MG Unresponsive to pyridostigmine Recent onset only (< 5 yrs) – – 57% 38% 25% 21% From a poll of 56 neurologists on the Med Adv Board of the MGF (Lanska 1990) Neuro-ophthalmic Consultants Northwest
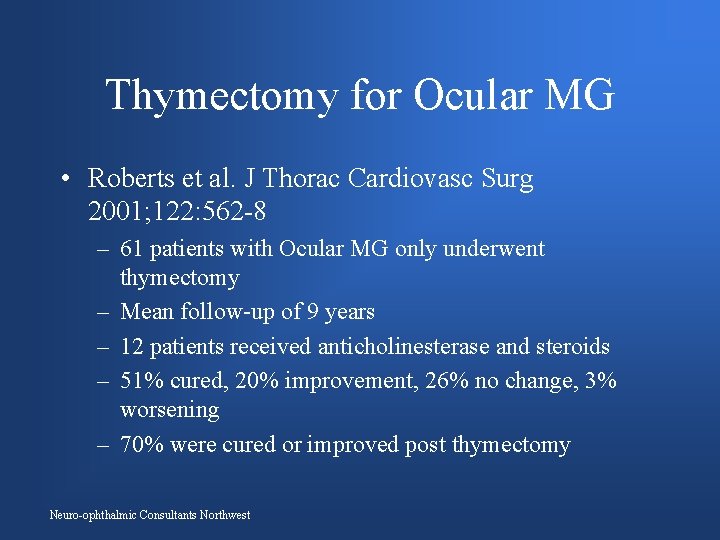
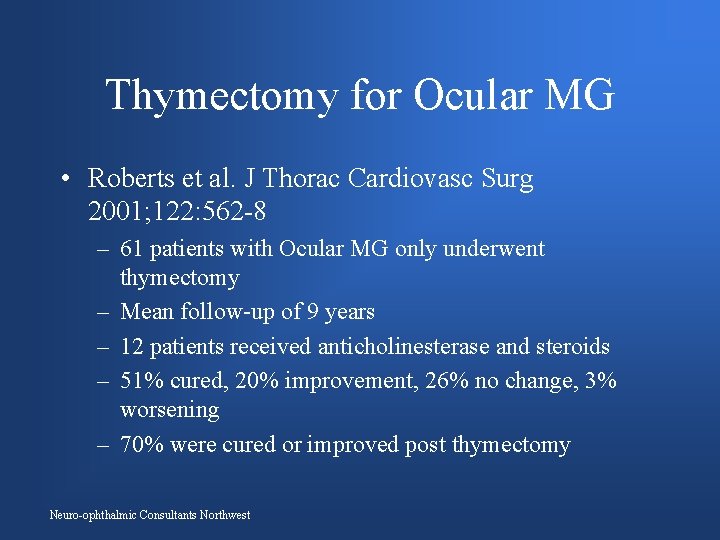
Thymectomy for Ocular MG • Roberts et al. J Thorac Cardiovasc Surg 2001; 122: 562 -8 – 61 patients with Ocular MG only underwent thymectomy – Mean follow-up of 9 years – 12 patients received anticholinesterase and steroids – 51% cured, 20% improvement, 26% no change, 3% worsening – 70% were cured or improved post thymectomy Neuro-ophthalmic Consultants Northwest
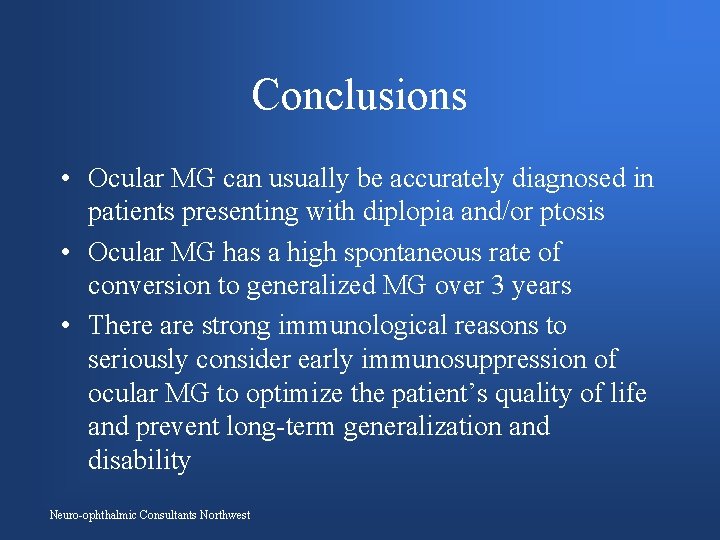
Conclusions • Ocular MG can usually be accurately diagnosed in patients presenting with diplopia and/or ptosis • Ocular MG has a high spontaneous rate of conversion to generalized MG over 3 years • There are strong immunological reasons to seriously consider early immunosuppression of ocular MG to optimize the patient’s quality of life and prevent long-term generalization and disability Neuro-ophthalmic Consultants Northwest
Bryce Canyon, Utah Neuro-ophthalmic Consultants Northwest
 Pictures of ocular myasthenia gravis
Pictures of ocular myasthenia gravis Exercise with myasthenia gravis
Exercise with myasthenia gravis Myasthenia gravis oireet
Myasthenia gravis oireet Concept map for disease process
Concept map for disease process Myasthenia gravis thymectomy
Myasthenia gravis thymectomy High frequency antibodies
High frequency antibodies Tes prostigmin
Tes prostigmin Orgnism
Orgnism Syringomyelia
Syringomyelia Myasthenia gravis eyes
Myasthenia gravis eyes Myasthenia gravis
Myasthenia gravis Myasthenic crisis vs cholinergic crisis
Myasthenic crisis vs cholinergic crisis Imunopatologické reakcie
Imunopatologické reakcie Long medium and short term planning in primary schools
Long medium and short term planning in primary schools Example of short term human resources
Example of short term human resources Difference between long term and short term liabilities
Difference between long term and short term liabilities Accounting for serial bonds
Accounting for serial bonds Long term goal examples
Long term goal examples Long term and short term financial planning
Long term and short term financial planning Long term memory vs short term memory
Long term memory vs short term memory Tall+short h
Tall+short h Once upon a time there lived a
Once upon a time there lived a The diagnostic term anorexia nervosa literally means
The diagnostic term anorexia nervosa literally means Brain weight
Brain weight Miasthenia gravis
Miasthenia gravis Phrenicum
Phrenicum Mythenia gravis
Mythenia gravis Haec precor hanc vocem extremam
Haec precor hanc vocem extremam Miastenia gravis
Miastenia gravis Gravis carter
Gravis carter Latin irregular adverbs
Latin irregular adverbs Paradigm shift from women studies to gender studies
Paradigm shift from women studies to gender studies Epitelio conjuntiva ocular
Epitelio conjuntiva ocular Astaxanthin benefits
Astaxanthin benefits Vagabundeo ocular
Vagabundeo ocular The body tube
The body tube Function of coarse adjustment in microscope
Function of coarse adjustment in microscope Ocular trauma score
Ocular trauma score Vestibulo ocular reflex
Vestibulo ocular reflex Allergies icd 10
Allergies icd 10 Ocular migraine
Ocular migraine