NY STATE OF HEATH ASSISTOR CERTIFICATION TRAINING MODULE







- Slides: 83
NY STATE OF HEATH ASSISTOR CERTIFICATION TRAINING MODULE FOUR: NY STATE OF HEALTH TERMS & PROGRAM INFORMATION nystateofhealth. ny. gov
LEARNING OBJECTIVES By the end of this lesson, you will be able to… • Define Common Health Care Terms. • Define Essential Health Benefits (EHBs). • Describe Medicaid, Essential Plan and Child Health Plus. • Define Qualified Health Plans (QHPs). • Define the Metal Levels. • Describe Advance Premium Tax Credits and Cost Sharing Reductions.
HEALTH CARE TERMS • Premium • In-Network • Deductible • Out-of-Network • Co-Payment • Formulary • Co-Insurance • Maximum Out-of-Pocket Cost (MOOP)
HEALTH CARE TERMS - SCENARIO Jane has Good. Care. She must pay $15 each time she sees her primary care doctor and $35 each time she sees a specialist. Jane can find out ahead of time how much she would pay for each service covered through her insurance. What does Jane pay every time she sees a provider? Co-pay
HEALTH CARE TERMS - SCENARIO José has Right. Care insurance and must cover the first $1, 750 of health care costs before Right. Care covers additional care. This amount may not apply to all services. After reaching the $1, 750, Right. Care will pay for additional care, but José must still pay any co-pays or co-insurance associated with his plan. What is the name of the amount he has to meet before his insurance covers additional care? Deductible

HEALTH CARE TERMS - SCENARIO Mary has Best. Care insurance and pays $100 a month for her insurance, regardless of whether she sees a doctor once a year or twice a month. What is Mary paying on a monthly basis? Premium
HEALTH CARE TERMS - SCENARIO Peter got a prescription from his primary care provider and he wants to know is it is covered by his insurance plan. How can he verify that his prescription is covered? Formulary
HEALTH CARE TERMS - SCENARIO Tom has insurance through Great. Care and has to pay 10% for a hearing aid. If Tom has met his deductible and wants a hearing aid that costs the insurance company $1, 000, Tom would pay 10% of that cost, or $100. What do you call a percent of the cost? Co-Insurance
HEALTH CARE TERMS - SCENARIO Peter has insurance through Paramount. Care. With this insurance plan he has access to 500 primary care providers and over 600 specialists. How do you call this group of doctors that have agreed to provide services to Paramount. Care’s members? In-network
HEALTH CARE TERMS - SCENARIO Rosie has insurance through Perfect. Care. With this insurance plan, she will only have to pay out of her own pocket up to the point where she spent $3, 000 within the calendar year. After this amount is reached, Perfect. Care will cover 100% of all costs. What would you call this amount? Maximum Out-of-Pocket Cost (MOOP)
HEALTH CARE TERMS - SCENARIO As a part of his coverage with Paramount Care, Peter is not allowed to see a doctor outside of his network of over 1, 000 providers, unless: • His plan has coverage for out-of-network providers. • He has obtained permission from the insurance company to see an out-ofnetwork provider. • He wants to pay the full cost of seeing the out-of-network provider.
TYPE OF INSURANCE • Commercial Insurance - unsubsidized health insurance • Public Insurance -subsidized insurance

ESSENTIAL HEALTH BENEFITS (EHBS) • • • Ambulatory Patient Services Emergency Services Hospitalization Maternity and Newborn Care Mental Health & Substance Use Disorder Services, including behavioral health treatment Rehabilitative and Habilitative Services and Devices Prescription Drugs Laboratory Services Preventive and Wellness and Chronic Disease Management Pediatric Services, including Oral and Vision Care
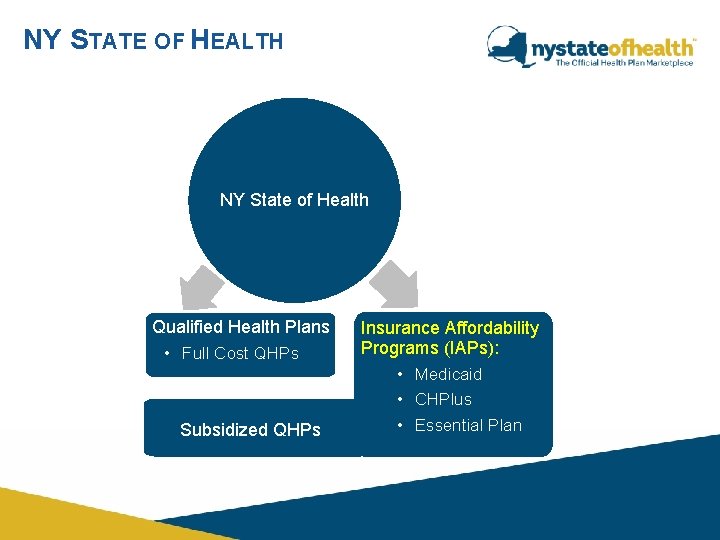
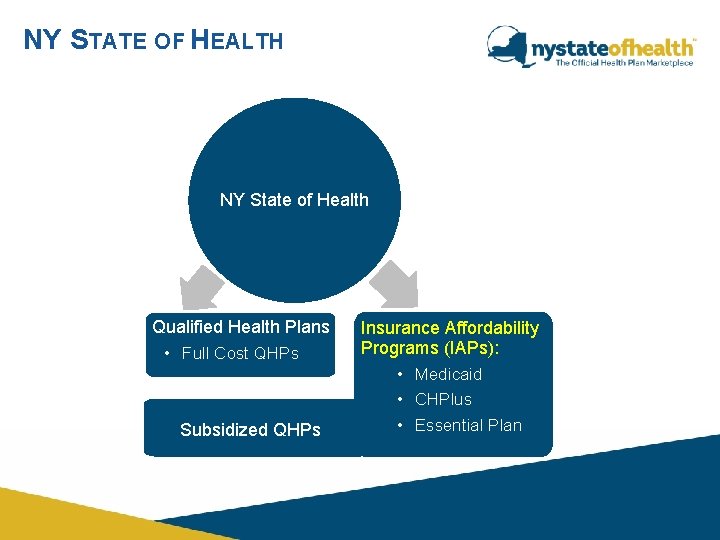
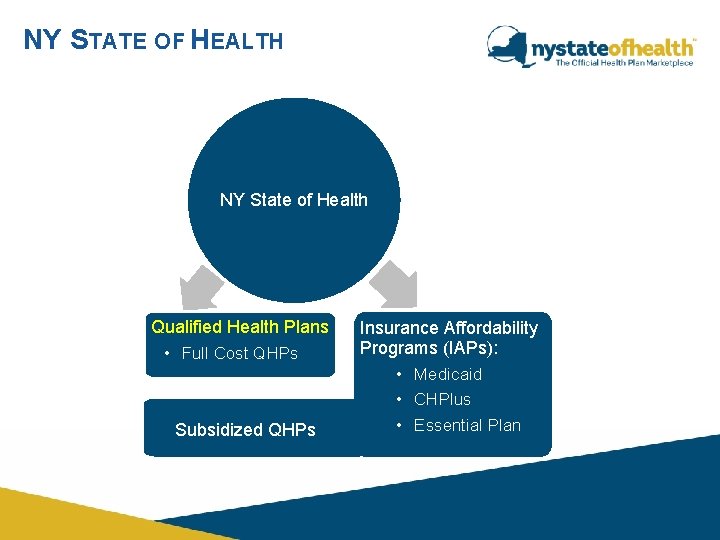
NY STATE OF HEALTH NY State of Health Qualified Health Plans • Full Cost QHPs Subsidized QHPs Insurance Affordability Programs (IAPs): • Medicaid • CHPlus • Essential Plan
MEDICAID - BASICS New York State’s Medicaid program is a state and federally funded program that provides health insurance for NYS residents who meet eligibility requirements. • To be Medicaid eligible, individuals would need to meet income eligibility. Income eligibility is: ü up to 138% of the FPL for adults ages 19 through 64 ü up to 154% of the FPL for children ages 1 through 18. ü Up to 155% of the FPL for 19 -20 years old living with parents. ü up to 223% of the FPL for pregnant women and infants under the age of 1. • There are no premiums or other forms of cost sharing for Medicaid, except for some co-payments for prescriptions in Medicaid Managed Care.
MEDICAID – BASICS CONTINUED Consumers may be eligible for Medicaid if they are income eligible using Modified Adjusted Gross Income (MAGI) budgeting and meet Medicaid income and all other eligibility criteria. MAGI Population includes: • Pregnant Women • Children • Parents/Caretaker Relative • Adults under age 65, not on Medicare
MEDICAID – BASICS CONTINUED Consumers, who are eligible for Medicaid due to non-financial criteria or are categorically eligible for Medicaid, must be referred to the Local Department of Social Services (LDSS) or Human Resource Administration (HRA). Non-MAGI Population includes: • Categorically eligible (e. g. TANF, SSl, Foster Care) • Individuals 65 and older when given conditional eligibility • Individuals whose eligibility is based on being blind or disabled • Medically Needy • Medicaid Buy-ln for Working Persons with Disabilities • Cancer Services Program
MEDICAID – NON-MAGI First determine whether the applicants are MAGI – Pregnant women – Children through age 18 – Parent/Caretaker relative of a dependent child under age 19 – Age 19 -64 and not eligible for Medicare Part A or B All other applicants are non-MAGI, e. g. , single adult who is age 65 or older and not a parent or caretaker relative. Among the MAGI population and prior to starting the online application, assess for non-MAGI to determine whether anyone requires: – Nursing facility services – Congregate Care Level 1, 2 or 3 – Waiver Services – Medicaid Buy-In for Working People with Disabilities
MEDICAID – EMERGENCY SERVICES Medicaid Emergency Services -Individuals applying for coverage in the NY State of Health, who do not have a satisfactory citizenship or immigration status, may be eligible for treatment for an emergency medical condition if they meet other Medicaid eligibility criteria and their medical condition meets the definition of an emergency medical condition. *No Immigration Eligibility Criteria
MEDICAID MANAGED CARE New York State pays a monthly premium to the health plan on behalf of the individual.
MEDICAID EXEMPT POPULATION Exempt Populations have the option to stay with Fee-for-Service Medicaid: • People in long-term alcohol or drug residential programs • People who live in facilities for the developmentally disabled • People who are in regular Medicaid and are being treated for a chronic medical condition for 6 months or more by a fee-for-service Medicaid specialist who is not in a Medicaid health plan. • People in waivered programs, such as Care At Home and TBI • American Indians/Alaska Natives

MEDICAID EXCLUDED POPULATION Excluded populations MUST stay with Fee-for-Service Medicaid: • Children or adults who live in state psychiatric or Residential Treatment Facilities • People who will get Medicaid only after they spend some of their own money for medical needs (spend-down cases) • People with other full benefit health insurance • Infants living with their mothers in jail or prison • All foster care children living in an institutional setting outside of NYC • NYS places in foster care setting by contract agency
MEDICAID MANAGED CARE- SNPS Starting on January 15 th, the Medicaid Managed Care Special Needs Plans (SNPs) will be displayed on the NY State of Health site as a plan selection option for all Medicaid eligible applicants that reside in the SNPs’ service areas. Currently, the SNPs’ service area includes the five (5) boroughs of New York City only.
MEDICAID MANAGED CARE- HARPS Starting in June, 2018 eligible consumers may now enroll in Health and Recovery Plans (HARPs). A HARP is a voluntary Medicaid Managed Care health insurance product for adults aged 21 and over who need physical and/or behavioral health services. Consumers are eligible for HARPs if they meet the following conditions: • They are 21 or older • They are insured only by Medicaid and eligible for Medicaid Managed Care • They are living with a mental health or substance use disorder • They are not participating in a program with the Office for People with Developmental Disabilities • They are not recipients of Traumatic Brain Injury (TBI), Nursing Home Transition and Diversion (NHTD), or Office of Mental Health (OMH) waiver services
MEDICAID MANAGED CARE - BENEFITS Medicaid Managed Care offers additional benefits that go above the Essential Health Benefits (EHB): • Transportation to medical appointments, including public transportation and car mileage. ü Plan coverage for this benefit is individual by county. Please be sure to advise the consumer to contact their health plan to verify this benefit. If the benefit is not offered through the plan, it is available under Fee-for-Service Medicaid.
MEDICAID MANAGED CARE - BENEFITS For NYS residents who are temporarily out of state (such as to go to school), Medicaid coverage is provided only under the following circumstances: • Residents of the district customarily use medical facilities in another district, state or area (these are across the State border nursing home situations); • There are limited medical services available in the district of residence and the district gives prior approval; or • Emergency Medical attention is needed as a result of accident or sudden illness. Per regulation Medicaid will only provide out of state benefits under the above listed circumstances. A provider must be enrolled in NYS Medicaid in order to order, provide, refer, or attend (OPRA) a Medicaid beneficiary (or their services) and be paid.
MEDICAID MANAGED CARE - COSTS Some services require a co-payment be made at the point-of-service. Examples include: • Brand Name Prescription Drugs – $3 • Generic Prescription Drugs - $1 • Over-the-Counter Drugs - $. 50 Each individual has a co-pay maximum of $200 in a service year. The following populations will not pay a co-pay: • Pregnant women • Children under the age of 21 • Family Planning • Residents of a Nursing Home Consumers cannot be denied care or services because they cannot pay their co-payment.

MEDICAID CONTINUOUS COVERAGE New York State Social Services Law provides continuous coverage for certain Medicaid beneficiaries for a period of 12 months from the date of initial eligibility and subsequent redetermination of eligibility. Continuous Coverage will provide stability and continuity of coverage and care to adults in the same way that it has for children on Medicaid.
MEDICAID REIMBURSEMENT Medicaid program enrollees may apply for reimbursement of medical bills they paid while waiting for their Medicaid coverage to begin, as long as their eligibility period covers the date the service was provided. • Reimbursement is most commonly requested when an individual is approved for retroactive Medicaid. • Also, since Medicaid coverage gets dated back to the first of the month of application submission, an individual may request reimbursement for bills paid earlier in the application month. • Individuals requesting reimbursement to their premiums will only be reimbursed if the premium meets a cost effectiveness test.
ESSENTIAL PLAN - BASICS The Essential Plan (Basic Health Program) is a new Insurance Affordability Program starting in 2016, that will offer qualified individuals and families a choice of plans from high-quality private health insurers through NY State of Heath.
ESSENTIAL PLAN - ELIGIBILITY • Be over 18 years old or below age 65 at the beginning of the plan year • Reside in New York State • Not eligible for Medicaid or Child Health Plus (CHPlus) • Have income above 138% and at or below 200% of the FPL or at or below 138% of the FPL and ineligible for Medicaid due to immigration status. • Not eligible for affordable Minimum Essential Coverage (MEC) • Individuals eligible for the Essential Plan are not eligible to receive Advance Premium Tax Credits Pregnant women are NOT eligible for Essential Plan because they will qualify for Medicaid. Consumers are required to report their pregnancy and NY State of Health will re-determine their eligibility for Medicaid.
ALIESSA IMMIGRATION STATUS The 2001 Aliessa v. Novello court decision, requires legal immigrants in the federal 5 -year ban and some categories of PRUCOL, to be eligible for New York State-funded Medicaid, if they meet the income eligibility guidelines.
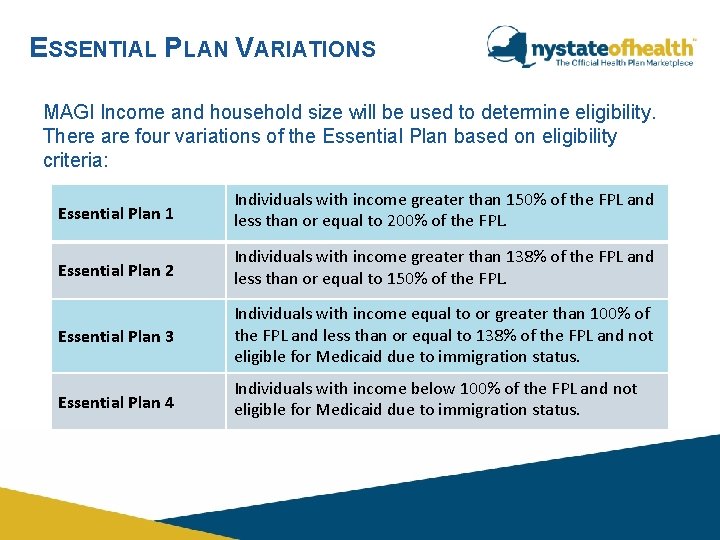
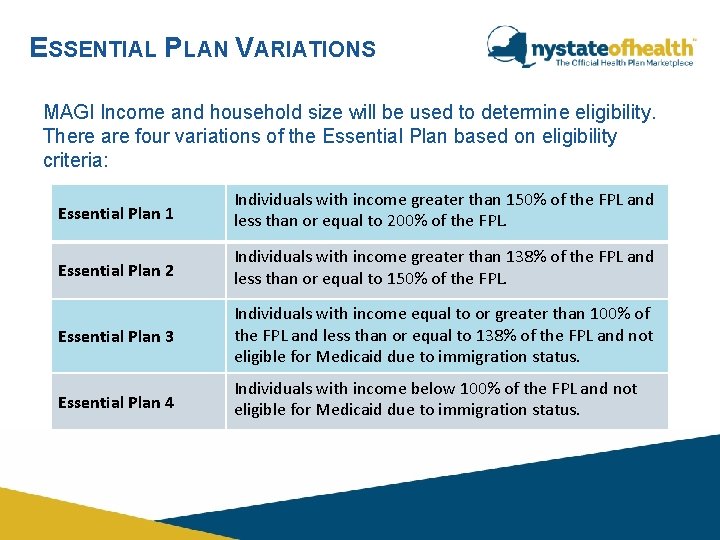
ESSENTIAL PLAN VARIATIONS MAGI Income and household size will be used to determine eligibility. There are four variations of the Essential Plan based on eligibility criteria: Essential Plan 1 Individuals with income greater than 150% of the FPL and less than or equal to 200% of the FPL. Essential Plan 2 Individuals with income greater than 138% of the FPL and less than or equal to 150% of the FPL. Essential Plan 3 Individuals with income equal to or greater than 100% of the FPL and less than or equal to 138% of the FPL and not eligible for Medicaid due to immigration status. Essential Plan 4 Individuals with income below 100% of the FPL and not eligible for Medicaid due to immigration status.
ESSENTIAL PLAN - COST • Individuals with income at or below 138% of the FPL will have no premium. • Individuals with income greater than 138% and less than or equal to 150% of the FPL will have no premium, unless they select a plan with dental and vision. • Individuals with income greater than 150% and less than or equal to 200% of the FPL will have a premium of $20 per individual per month and a higher premium if selecting dental and vision plan.
ESSENTIAL PLAN - BENEFITS • Each of the standard Essential Plan carriers will cover the same benefits. o Enrollees with incomes greater than 138% of the FPL will have the option of purchasing adult vision and adult dental benefits at an additional cost. o Enrollees with incomes at or below 138% of the FPL will enroll in plans with additional benefits including dental and vision. • All plans in the Essential Plan will cover the essential health benefits. They will also include the following: o No annual deductible o Low out-of-pocket costs o Preventive care will be free o American Indian/Alaskan Natives will have a $0 cost sharing
ESSENTIAL PLAN - BENEFITS Population with income at or below 138% of the FPL are also eligible for the following additional services: • • • Non-Emergency Transportation Non-Prescription Drugs Adult Dental Care Vision Care Orthotic Services Orthopedic Footwear
ESSENTIAL PLAN - BENEFITS Essential Plan enrollees must select a health plan at the time of enrollment. Enrollees will: • Receive a Plan ID Card to access services. • Those with income at or below the 138% FPL will also receive a NY State Benefits Card (CBIC) to access additional services mirroring Medicaid. This include services like: o Non-emergency transportation o Family planning services § Consumers have the option of using either their CBIC or plan card to access family planning services.
CHILD HEALTH PLUS - BASICS Child Health Plus is a subsidized insurance program for uninsured New York State children under the age of 19, who are not Medicaid eligible and do not have access to a state health benefits plan. • Children with income at or below 400% of the FPL receive subsidized coverage. • Children with income above 400% of the FPL can purchase CHPlus at full cost.
CHILD HEALTH PLUS - ELIGIBILITY • Under the age of 19 • Ineligible for Medicaid • Resident of New York State • Do not have other health insurance coverage • Do not have access to NYSHIP state health benefit
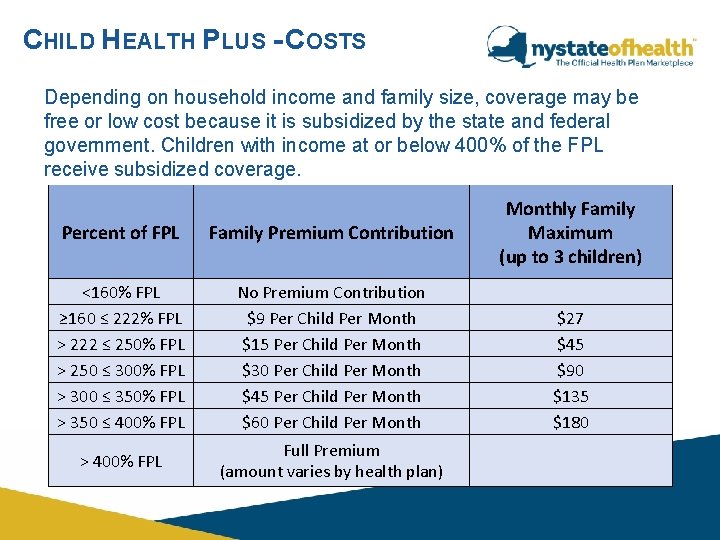
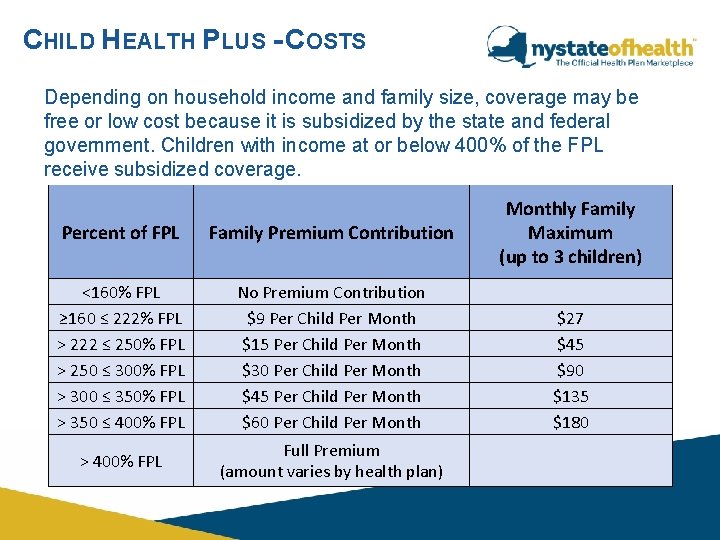
CHILD HEALTH PLUS - COSTS Depending on household income and family size, coverage may be free or low cost because it is subsidized by the state and federal government. Children with income at or below 400% of the FPL receive subsidized coverage. Percent of FPL Family Premium Contribution <160% FPL ≥ 160 ≤ 222% FPL > 222 ≤ 250% FPL > 250 ≤ 300% FPL > 300 ≤ 350% FPL > 350 ≤ 400% FPL No Premium Contribution $9 Per Child Per Month $15 Per Child Per Month $30 Per Child Per Month $45 Per Child Per Month $60 Per Child Per Month > 400% FPL Full Premium (amount varies by health plan) Monthly Family Maximum (up to 3 children) $27 $45 $90 $135 $180
CHILD HEALTH PLUS – CONTINUOUS COVERAGE • Children have 12 months of continuous coverage in the Child Health Plus Program. The 12 -month period of continuous coverage is subject to exclusions. • The period of eligibility shall begin on the first day of the month an eligible child is enrolled or recertified for enrollment on an annual basis, based on all required documentation, and shall continue for twelve (12) months ending on the last day of the twelfth month. • Presumptive enrollees are not eligible for 12 months of continuous coverage until all required documentation is submitted and a child is determined fully eligible for CHPlus at which time the 12 months of continuous coverage will begin on the day presumptive eligibility began.
CHILD HEALTH PLUS – NEWBORN POLICY Families must apply for coverage within 60 days of the newborn’s date of birth in order to be eligible to have the coverage to go retroactive to the first of the newborns birth month. • Newborns will be enrolled in the same CHplus plan as their siblings, if applicable. • If no siblings, families must select and enroll in a plan within 60 days of the newborn's DOB. • Coverage start date options: • 1 st of the newborn’s birth month • 1 st of the month after the newborn’s birth month • 1 st of the second month after the newborn’s birth month • Following the 15 th of the month rule when applying
NYSHIP State Health Benefits Plans provide health insurance through the New York State Health Insurance Program (NYSHIP). • Coverage is offered to employees/retirees of NYS government, the State Legislature and the Unified Court System. Some local government agencies and school districts also elect to participate in NYSHIP. • If the applicant is not sure, they can check with their employer. If the child has access to State Health Insurance Benefits through NYSHIP, he/she will not be able to enroll in Child Health Plus.
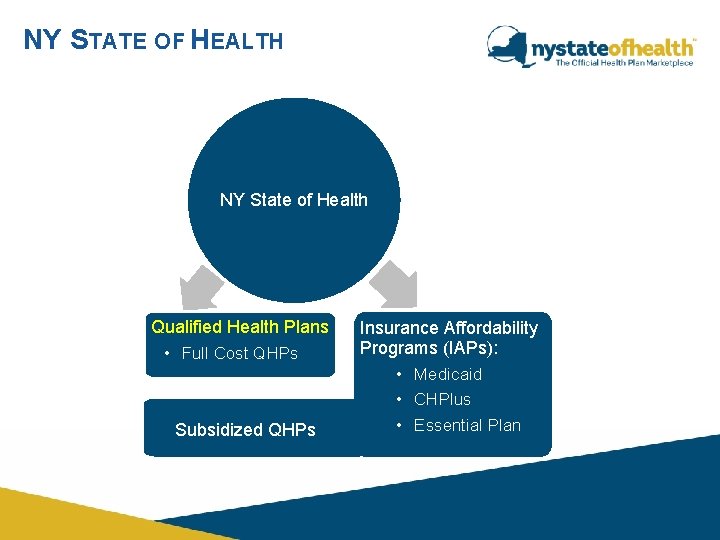
NY STATE OF HEALTH NY State of Health Qualified Health Plans • Full Cost QHPs Subsidized QHPs Insurance Affordability Programs (IAPs): • Medicaid • CHPlus • Essential Plan

QUALIFIED HEALTH PLANS (QHP) Licensed, commercial health plans that have been approved by the NY State of Health to provide comprehensive coverage, follow limits on out-of-pocket expenses (such as deductibles, co-payments, and out-of-pocket maximums), and meet other requirements.

QHP STANDARD PRODUCTS Insurers must offer: • The exact same benefits. • The exact same cost sharing. • Different prescription formularies/networks/quality ratings.
QHP NON-STANDARD PRODUCTS Insurers may offer: • Additional benefits not included in EHB. • Variations on standard cost sharing. • Different networks. • Limited substitutions in two benefit categories: o Rehabilitative and Habilitative o Preventive/Wellness/Chronic Disease Management
QHP NETWORK ADEQUACY STANDARDS QHPs must ensure the provider network meets the following standards: – Network of sufficient types of providers – Offers a directory of providers Out-of-Network Benefits − Allows the consumer to use providers outside of the QHP’s network – Cost sharing amount may be different when using Out-of. Network providers
CHECK FOR UNDERSTANDING 1. Standard QHPs must offer the exact same benefits and the exact same cost sharing. What are the ways in which Standard QHPs could be different? (select all that apply) A. B. C. D. E. They can have different networks They can choose different benefits to offer They can have different prescription formularies They can have different quality ratings They can have different deductibles across the same metal levels
CHECK FOR UNDERSTANDING 2. Non-Standard QHPs are different than Standard QHPs. What are the differences? (check all that apply) A. They can have different networks B. They can have variations on standard cost sharing C. They can cover additional benefits not included in the EHBs D. They can offer limited substitutions in two benefit categories
CHECK FOR UNDERSTANDING True or False? 3. All QHPs cover the Ten Essential Health Benefits True
CHECK FOR UNDERSTANDING 4. Please identify which statements below are accurate. (Select all that apply) A. All QHPs could have different networks, as long as those networks meet adequacy standards. B. All QHPs cover exactly the same benefits C. All QHPs have the same prescription formularies D. None of the QHPs offer out-of-network benefits E. Standard and Non-Standard QHPs have different cost sharing amounts for different benefits F. Every Silver & Platinum QHP will offer out-of-network benefits G. Some QHPs will offer out-of-network benefits
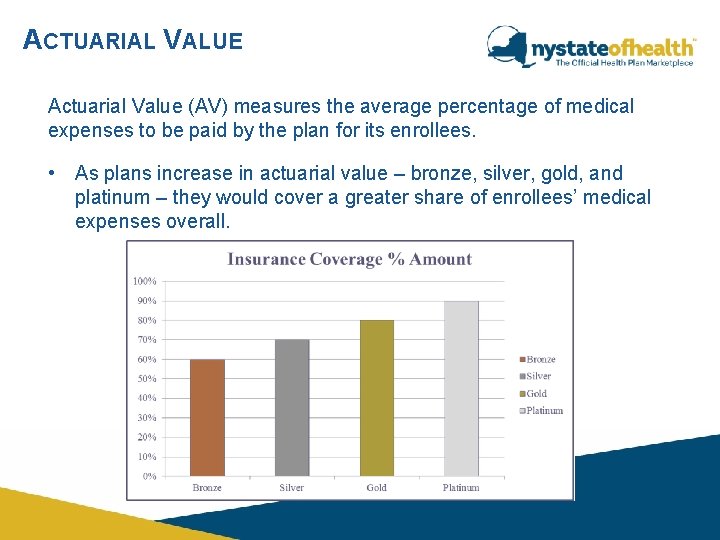
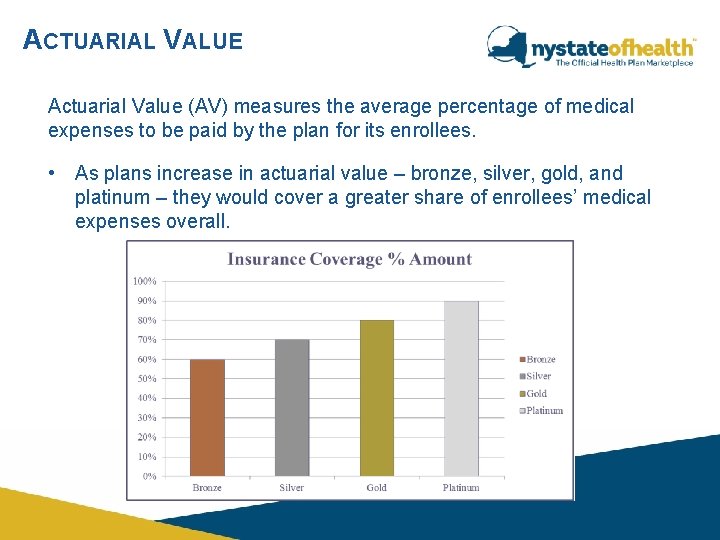
ACTUARIAL VALUE Actuarial Value (AV) measures the average percentage of medical expenses to be paid by the plan for its enrollees. • As plans increase in actuarial value – bronze, silver, gold, and platinum – they would cover a greater share of enrollees’ medical expenses overall.
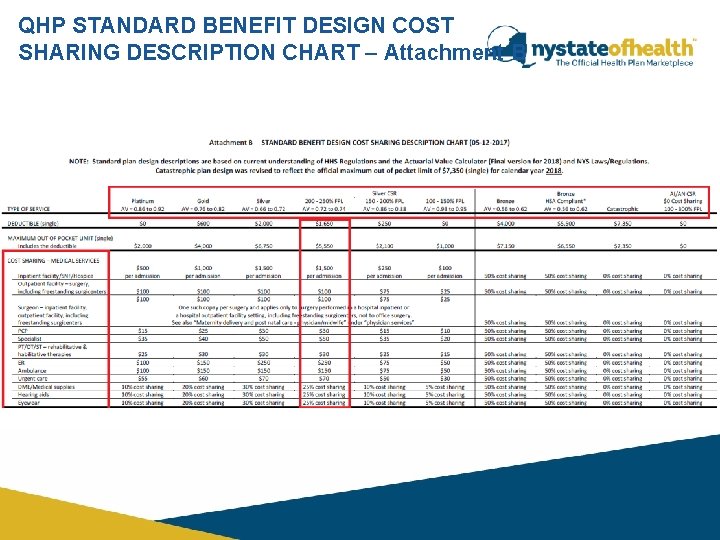
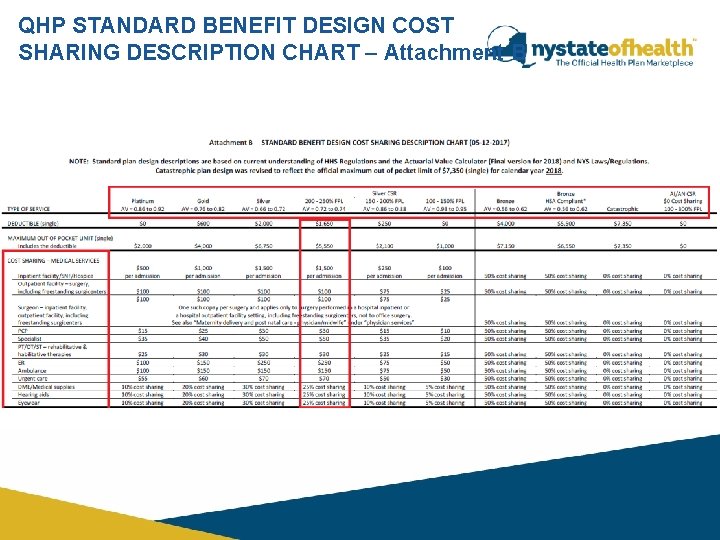
QHP STANDARD BENEFIT DESIGN COST SHARING DESCRIPTION CHART – Attachment B
NY STATE OF HEALTH NY State of Health Qualified Health Plans • Full Cost QHPs Subsidized QHPs Insurance Affordability Programs (IAPs): • Medicaid • CHPlus • Essential Plan
INSURANCE AFFORDABILITY PROGRAMS WITHIN QHPS • Advance Premium Tax Credits (APTC) – lower the cost of monthly health insurance premiums • Cost-Sharing Reductions (CSR) – reduce out of pocket costs o Co-pays o Co-insurance o Deductibles o Maximum Out of Pocket
ADVANCE PREMIUM TAX CREDIT (APTC) • Available to eligible individuals who enroll in QHPs • Individuals and families with income greater than 200% to 400% FPL • Consumers that would be eligible for Medicaid, Essential Plan or CHPlus are ineligible for tax credits • Consumers who are offered Employer Sponsored Health Insurance that is considered affordable are ineligible for tax credits Applicants have the option to choose how their credit is applied: • Can go towards lowering monthly premium • Can be received in lump sum when filing taxes • Split their tax credit by receiving some each month and some at tax time
ADVANCE PREMIUM TAX CREDIT (APTC) CONTINUED When applicants apply in the Marketplace, they report their estimated annual income. If the actual annual income is different than the estimated income, and an enrollee uses all or some of the APTC for which they were eligible, the enrollee may have to pay back some or all of the APTC to the IRS at tax time or may be due a federal refund. Consumers must know that if their circumstances change, it is their responsibility to notify the NY State of Health so that their eligibility can be redetermined. Individuals can report changes on-line, through the NY State of Health Customer Service Center, or with the help of the Assistor.
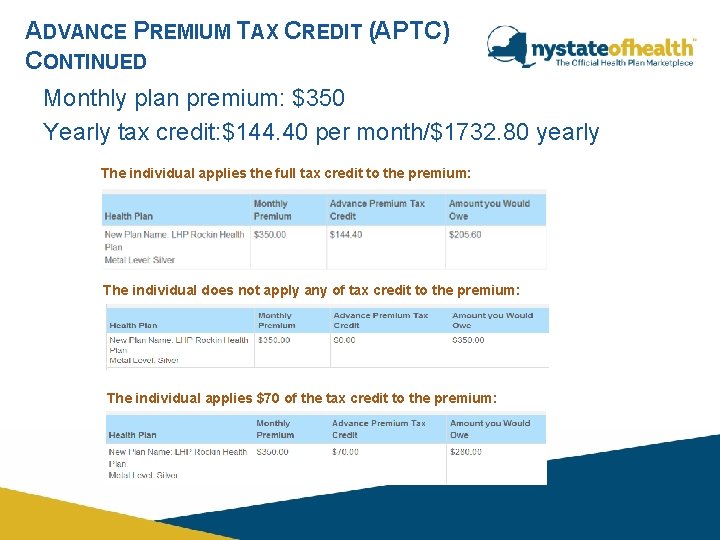
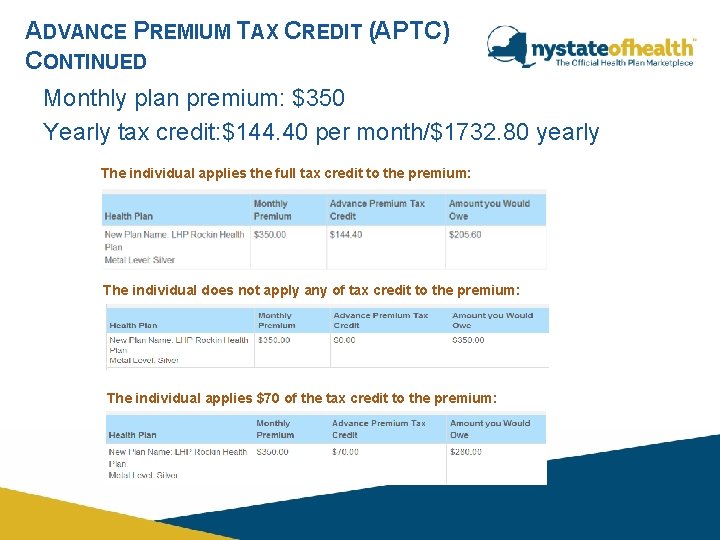
ADVANCE PREMIUM TAX CREDIT (APTC) CONTINUED Monthly plan premium: $350 Yearly tax credit: $144. 40 per month/$1732. 80 yearly The individual applies the full tax credit to the premium: The individual does not apply any of tax credit to the premium: The individual applies $70 of the tax credit to the premium:
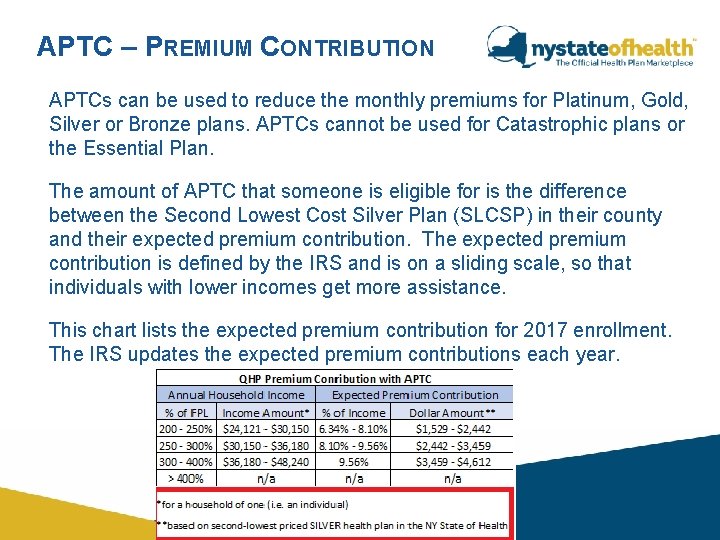
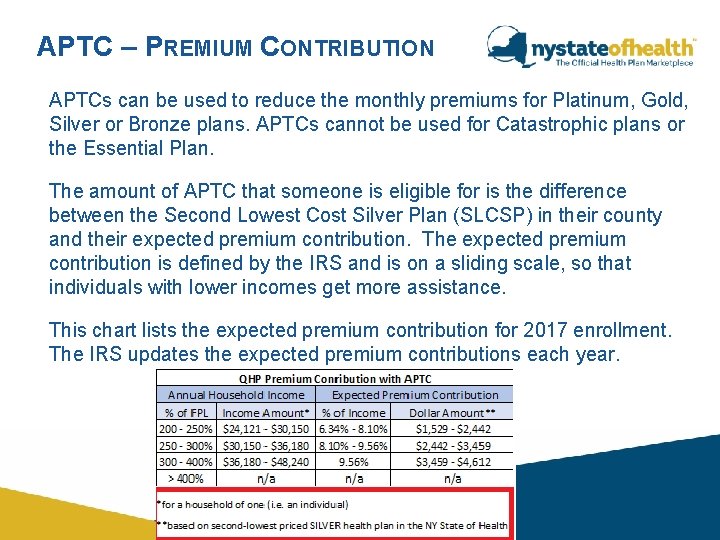
APTC – PREMIUM CONTRIBUTION APTCs can be used to reduce the monthly premiums for Platinum, Gold, Silver or Bronze plans. APTCs cannot be used for Catastrophic plans or the Essential Plan. The amount of APTC that someone is eligible for is the difference between the Second Lowest Cost Silver Plan (SLCSP) in their county and their expected premium contribution. The expected premium contribution is defined by the IRS and is on a sliding scale, so that individuals with lower incomes get more assistance. This chart lists the expected premium contribution for 2017 enrollment. The IRS updates the expected premium contributions each year.
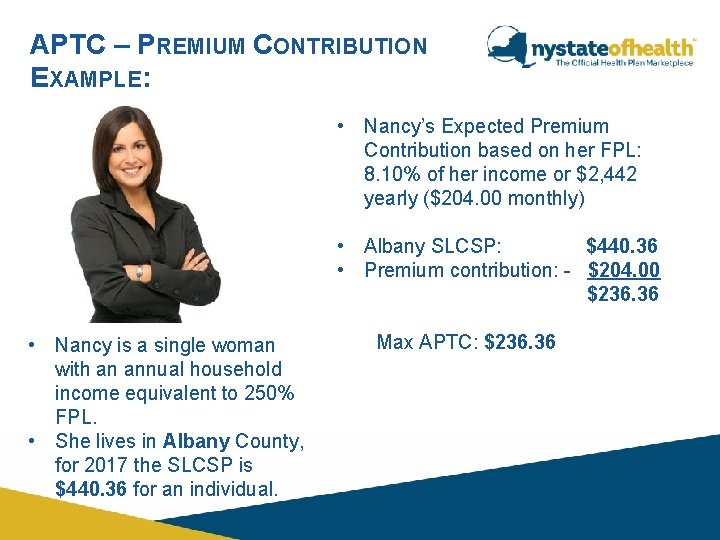
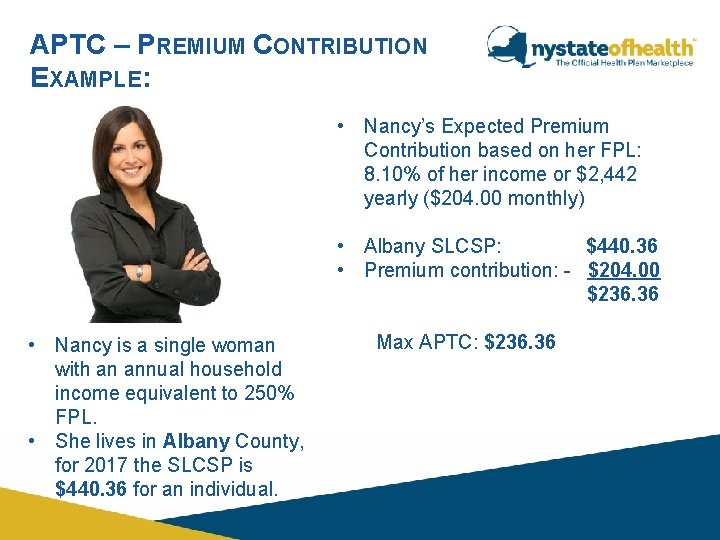
APTC – PREMIUM CONTRIBUTION EXAMPLE: • Nancy’s Expected Premium Contribution based on her FPL: 8. 10% of her income or $2, 442 yearly ($204. 00 monthly) • Albany SLCSP: $440. 36 • Premium contribution: - $204. 00 $236. 36 • Nancy is a single woman with an annual household income equivalent to 250% FPL. • She lives in Albany County, for 2017 the SLCSP is $440. 36 for an individual. Max APTC: $236. 36
APTC - ELIGIBILITY Consumers who become eligible to receive APTC must: • Attest to filing taxes in the upcoming tax year. • If married, the household must file jointly. • Report changes to the NY State of Health. *APTC is reconciled by the IRS at tax time. Note: Victims of domestic violence who are married but are unable to file taxes jointly with their spouses may be eligible for QHP subsidies.
COST SHARING REDUCTIONS (CSRS) Reduce the out-of-pocket costs for health care services at the point-of-care. Sliding Scale based on calculations performed by NY State of Health. Allows the consumer to pay a percentage of out-of-pocket costs, and the federal government covers the rest. Covers: • Deductibles • Co-pays • Co-insurance *Must enroll in Silver Metal Level Plan
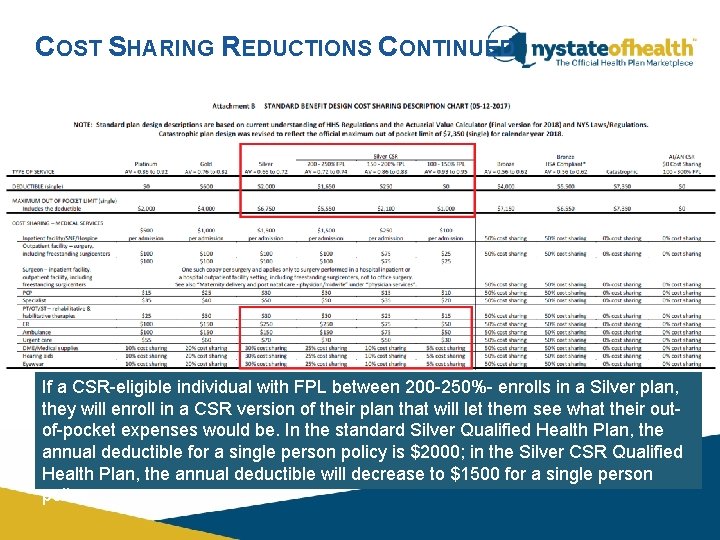
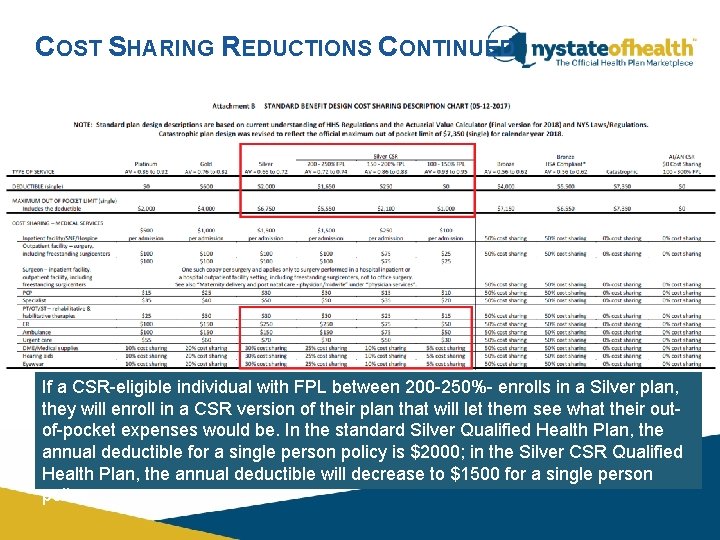
COST SHARING REDUCTIONS CONTINUED If a CSR-eligible individual with FPL between 200 -250%- enrolls in a Silver plan, they will enroll in a CSR version of their plan that will let them see what their outof-pocket expenses would be. In the standard Silver Qualified Health Plan, the annual deductible for a single person policy is $2000; in the Silver CSR Qualified Health Plan, the annual deductible will decrease to $1500 for a single person policy.
CHECK FOR UNDERSTANDING True or False? 1. A consumer who becomes eligible for CSR will receive the same amount of CSR for 12 months regardless of a change in income. False
CHECK FOR UNDERSTANDING True or False? 2. A consumer, who is legally married and becomes eligible for CSR, must attest that they will file their taxes jointly with their spouse in the upcoming tax year in order to remain eligible for CSR. True
AMERICAN INDIAN/ALASKAN NATIVE ELIGIBILITY • AI/AN with income at or below 300% FPL are eligible for a CSR plan with no out-of-pocket costs. Bronze plans will be the most affordable plans for these consumers. • AI/AN with income above 300% FPL are eligible for limited cost sharing, with no out-of-pocket costs for I/T/U providers, or through a referral with contract health services.
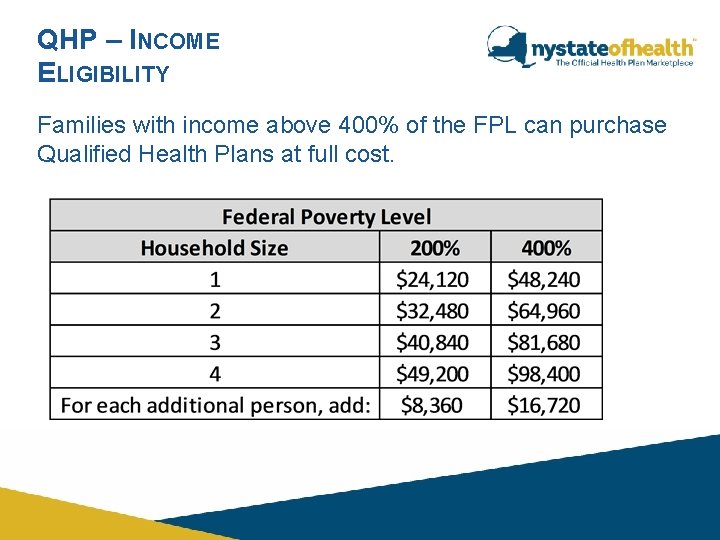
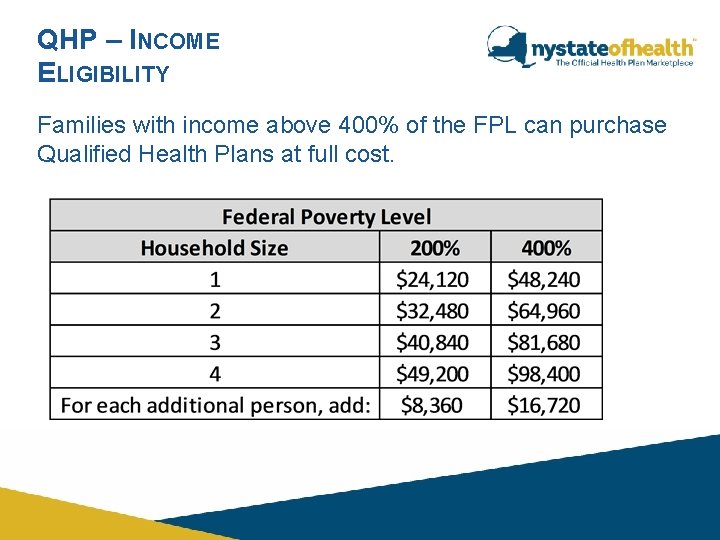
QHP – INCOME ELIGIBILITY Families with income above 400% of the FPL can purchase Qualified Health Plans at full cost.
CATASTROPHIC COVERAGE A health insurance policy that is designed to give protection against catastrophic events. Who is Eligible? • Young adults under 30 • Individuals exempt from the Individual Mandate because they cannot find affordable insurance.
QUALITY AND ENROLLEE SATISFACTION All health plans offered through the NY State of Health will be assigned a quality rating based on: • • • Effectiveness Access and availability of care Cost of care Use and frequency of services Satisfaction with the experience of care Certifications or other descriptive information
PREMIUM PAYMENT – NEXT STEPS Upon completion of the enrollment, the consumer will be provided with options to make their first monthly premium payment. Consumers will be given a Grace Period to pay their premiums: • Subsidized QHP Consumers - Will have 10 -day grace period for the first month’s premium and 90 days every month after. • Full Pay QHP Consumers - will have a 10 -day grace period for the first month’s premium and will have a 30 -day grace period for premiums in subsequent months • Essential Plan Consumers - will have a 10 -day grace period for the first month’s premium and will have a 30 -day grace period for premiums in subsequent months. • CHPlus Consumers – Coverage is not effectuated until the premium is paid. On the consumer’s eligibility results, the individual will receive a confirmation number and the health plan’s mailing address if they would like to send in the premium contribution prior to receipt of a bill.
QHP OPEN ENROLLMENT PERIOD Unlike other healthcare programs you might be familiar with, there will be specific enrollment periods for QHPs. • The Annual Enrollment Period is November 1, 2016 to January 31, 2017. • Individuals may also qualify for Special Enrollment Period if they experience certain events.
QHP SPECIAL ENROLLMENT PERIOD Outside of the Annual Open Enrollment Period, during which individuals who meet specific qualifying criteria may enroll in or change QHPs. • Specific Qualifying Life Events • Pregnancy • Birth of Child • Marriage • Death • Adoption • American Indians and Alaskan Natives may enroll in a QHP at any time and may change from one QHP to another once per month. • Some SEPs can be requested online; others must be requested by calling the Service Center.
SPECIAL ENROLLMENT PERIOD In the case of a qualifying event or life status change, in most circumstances, individuals have 60 days from the event to enroll in or change from one Qualified Health Plan to another. Coverage effective date during SEPs, unless specified otherwise, the coverage will be effective based on the date plan selection was completed according to the 15 th of the month rule. Enrollees with the following SEPs have the option of selecting the standard coverage effective date or selecting a different coverage effective date: • Loss of Essential Coverage • Marriage/Domestic Partnership • Gained a dependent due to birth, adoption or placement for adoption, or placement in foster care
SPECIAL ENROLLMENT PERIOD If the SEP qualifies for an alternative start date, the Plan Selection Dashboard will include a Plan Start Date drop-down menu after selecting a plan. If the Plan Selection Start Date drop-down is presented, the consumer may choose the enrollment start date. • The available dates depend on the type of SEP the consumer qualified for and whether plan selection is done before or after the 15 th. • It is important to note that if consumers choose an earlier start date, they will be billed the full premium for each covered month. • The health plan will not pay for any services that were rendered before coverage is effectuated.
PREGNANCY SEP Pregnancy is an option on the SEP screen which functions differently than other SEPs. The option to choose “Pregnancy” on the SEP screen is available to newly applying consumers who are over income for Medicaid. The consumer will then be able to check the box on the SEP screen that their pregnancy is the reason they are applying for health care coverage today. The consumer will then need to enter the information on the date the pregnancy was certified by a medical professional.
SPECIAL ENROLLMENT PERIOD What Consumers Need to Know About SEPs: • New applicants for QHPs must meet SEP requirements. • When a current enrollee applies for a SEP, the NY State of Health will re-calculate their eligibility based on the life change. • In most cases, consumers will not need to submit documentation to request a SEP. • Consumers who enroll in a QHP mid-year must meet the entire annual deductible and the full maximum out-of-pocket limit. • Current enrollees who change plans will start over with a new deductible and maximum out-of-pocket limit. • Current enrollees who choose to remain in the same QHP continue paying towards their deductible and out of pocket maximum.
MEDICAID ENROLLMENT PERIOD Medicaid has continuous enrollment. • All consumers who are determined eligible for Medicaid through the NY State of Health, coverage is effective back to the first of the month from the date of application. • Consumers who are eligible for Medicaid Managed Care will have FFS until they select a plan or are auto enrolled in a plan. • If a consumer selects a Managed Care Plan or is auto enrolled in a Managed Care plan on or before the 15 th of the month, the Managed Care coverage will start the first of the following month. • Retroactive coverage can be requested by the consumer.
ESSENTIAL PLAN AND CHPLUS ENROLLMENT PERIOD Essential Plan and CHPlus both have continuous open enrollment. Applicants are able to enroll all year long and change their plan at any time throughout the year. Essential Plan • For individuals with income at or below 138% of the FPL and do not qualify for Medicaid due to their immigration status, the effective date of coverage will be on the first of the month in which an Essential Plan is selected. • For individuals with incomes above 138% of the FPL, the effective date of coverage will follow the “ 15 th of the month” rule. CHPlus • An application received between the 1 st and the 15 th of a month, will be effective the first day of the following month.
CHECK FOR UNDERSTANDING True or False? 1. A consumer who does not file their taxes is not eligible to enroll through the NY State of Health. False
CHECK FOR UNDERSTANDING 2. What plan options do consumers have if they make over 400% of the Federal Poverty Level? A. They cannot get coverage through the NY State of Health B. They need to submit documentation to prove why they need coverage C. They can enroll through the Small Business Marketplace D. They can enroll in a Full-Pay QHP
CHECK FOR UNDERSTANDING True or False? 3. A consumer who becomes eligible for a QHP can enroll in that plan anytime throughout the year. False

WHAT QUESTIONS DO YOU HAVE?