Pathology of Pulmonary Hypertension Wolter J Mooi Department



- Slides: 14
Pathology of Pulmonary Hypertension Wolter J. Mooi Department of Pathology, VUmc Amsterdam WJ. Mooi@VUmc. nl

Pulmonary arterial hypertension (WHO definition) • Sustained elevation of pulmonary arterial pressure to more than 25 mm Hg at rest, or to more than 30 mm Hg with exercise • Mean pulmonary wedge pressure and left ventricular end-diastolic pressure less than 15 mm Hg
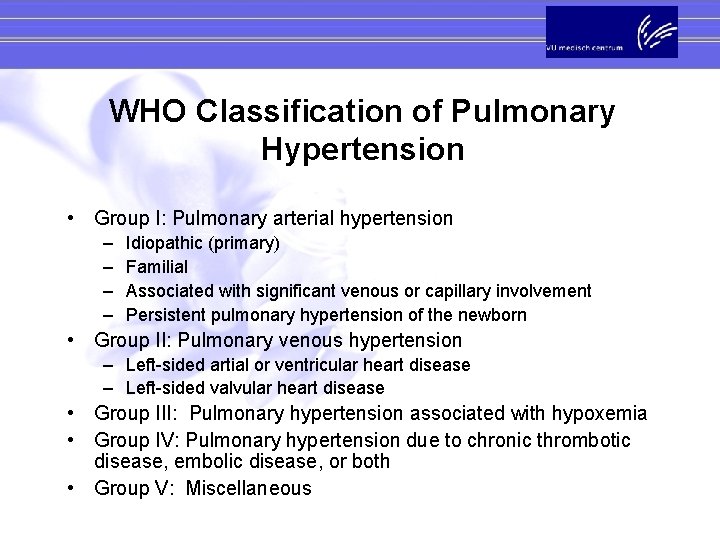
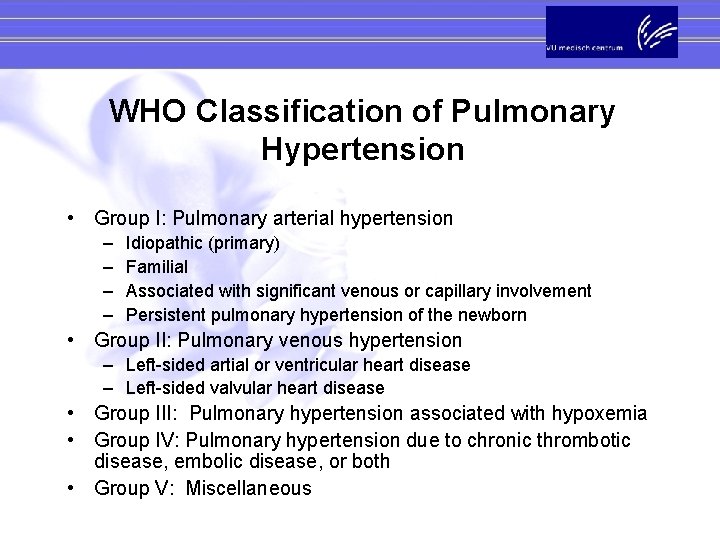
WHO Classification of Pulmonary Hypertension • Group I: Pulmonary arterial hypertension – – Idiopathic (primary) Familial Associated with significant venous or capillary involvement Persistent pulmonary hypertension of the newborn • Group II: Pulmonary venous hypertension – Left-sided artial or ventricular heart disease – Left-sided valvular heart disease • Group III: Pulmonary hypertension associated with hypoxemia • Group IV: Pulmonary hypertension due to chronic thrombotic disease, embolic disease, or both • Group V: Miscellaneous
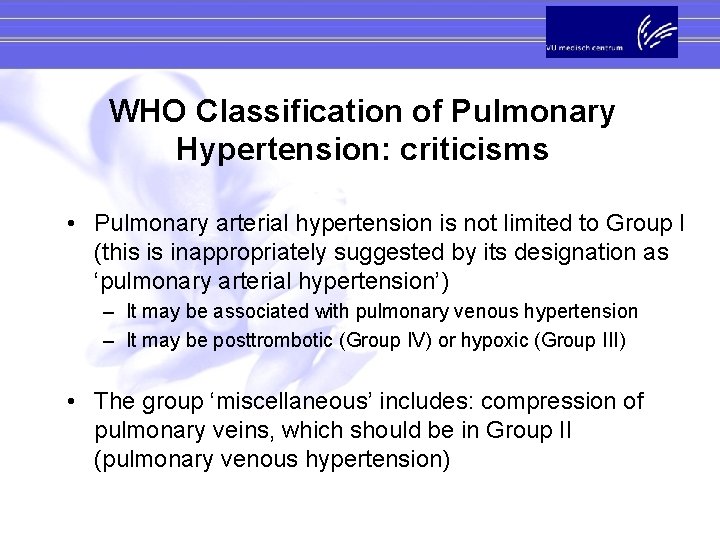
WHO Classification of Pulmonary Hypertension: criticisms • Pulmonary arterial hypertension is not limited to Group I (this is inappropriately suggested by its designation as ‘pulmonary arterial hypertension’) – It may be associated with pulmonary venous hypertension – It may be posttrombotic (Group IV) or hypoxic (Group III) • The group ‘miscellaneous’ includes: compression of pulmonary veins, which should be in Group II (pulmonary venous hypertension)
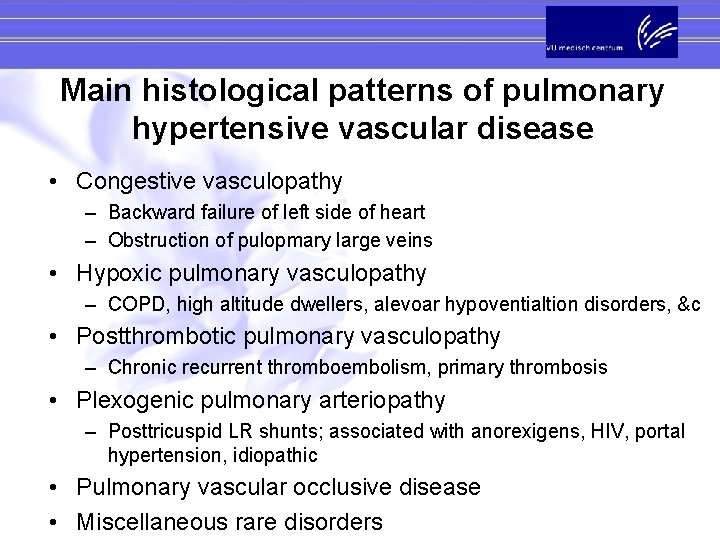
Main histological patterns of pulmonary hypertensive vascular disease • Congestive vasculopathy – Backward failure of left side of heart – Obstruction of pulopmary large veins • Hypoxic pulmonary vasculopathy – COPD, high altitude dwellers, alevoar hypoventialtion disorders, &c • Postthrombotic pulmonary vasculopathy – Chronic recurrent thromboembolism, primary thrombosis • Plexogenic pulmonary arteriopathy – Posttricuspid LR shunts; associated with anorexigens, HIV, portal hypertension, idiopathic • Pulmonary vascular occlusive disease • Miscellaneous rare disorders
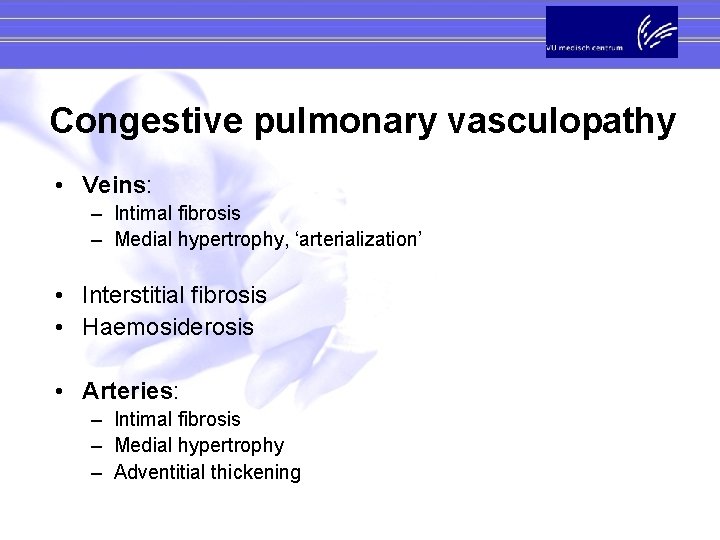
Congestive pulmonary vasculopathy • Veins: – Intimal fibrosis – Medial hypertrophy, ‘arterialization’ • Interstitial fibrosis • Haemosiderosis • Arteries: – Intimal fibrosis – Medial hypertrophy – Adventitial thickening
Hypoxic pulmonary vasculopathy • Arteries and arterioles: – Medial hypertrophy (accentuated in smaller branches) – Muscularization of arterioles – Longitudinal smooth muscle bundles – Mild intimal thickening • Veins: – Mild thickening of venule walls (mild smooth medial hypertrophy, mild fibrosis)
Postthrombotic pulmonary arteriopathy • Arteries: – – – Eccentric intimal fibrosis Concentric intimal fibrosis (not concentric laminar) Bands and webs Medial atrophy, fibrosis Arterial obliteration; fibroelastic scars NB-1: abnormalities are focal, so that many arteries may appear normal or near normal, even in the presence of severe obstruction NB-2: arterial changes in fibrosing lung disease are very similar if not identical to postthrombotic arteriopathy
Plexogenic pulmonary arteriopathy • Early phase: – Medial thickening of elastic and muscular pulmonary arteries – Muscularization of pulmonary arterioles – Mild intimal fibrosis • Late phase: – – Concentric laminar intimal fibrosis Fibrinoid necrosis, arteritis Dilatation lesions Plexifom lesions

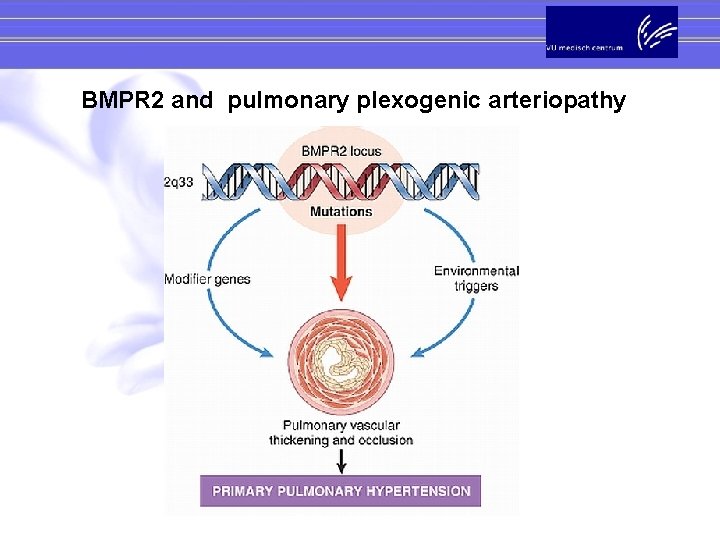
BMPR 2 germline mutations and familial pulmonary plexogenic arteriopathy Deng et al. , Am J Hum Genet 2000; 67: 737 -44; Lane et al. , Nat Genet 2000; 26: 81 -84
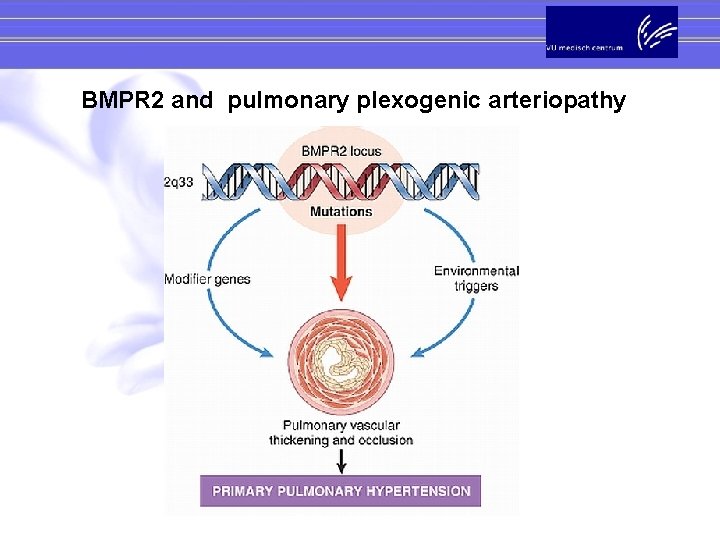
BMPR 2 and pulmonary plexogenic arteriopathy
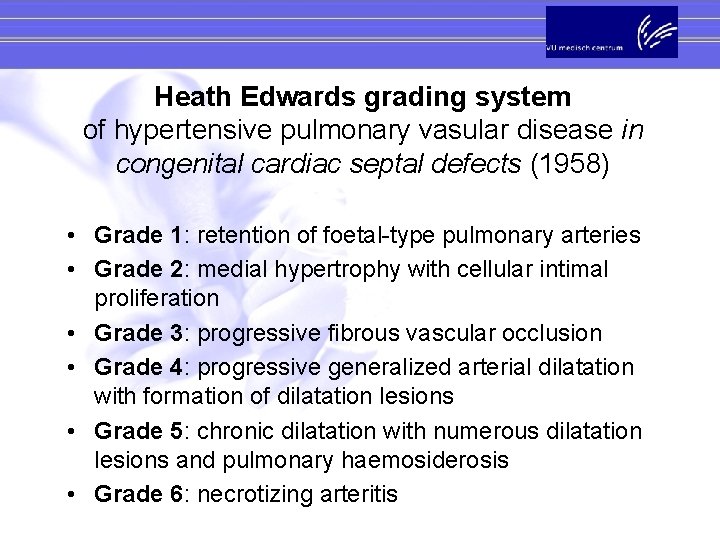
Heath Edwards grading system of hypertensive pulmonary vasular disease in congenital cardiac septal defects (1958) • Grade 1: retention of foetal-type pulmonary arteries • Grade 2: medial hypertrophy with cellular intimal proliferation • Grade 3: progressive fibrous vascular occlusion • Grade 4: progressive generalized arterial dilatation with formation of dilatation lesions • Grade 5: chronic dilatation with numerous dilatation lesions and pulmonary haemosiderosis • Grade 6: necrotizing arteritis

Heath Edwards grading system Grade 1 Intimal reaction None 2 3 4 Fibrous and fibroelastic changes Plexiform lesion hypertrophy Medial changes 6 Cellular proliferation 5 Some generalized dilatation Local dilatation lesions Haemosidereosis Necrotizing arteritis
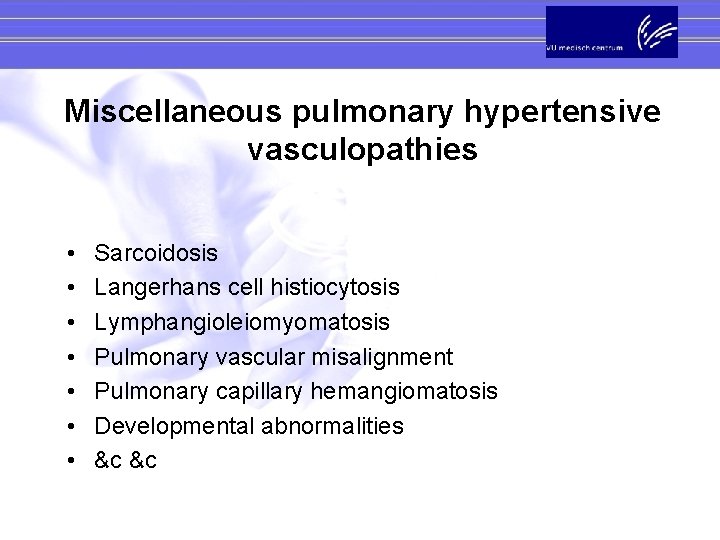
Miscellaneous pulmonary hypertensive vasculopathies • • Sarcoidosis Langerhans cell histiocytosis Lymphangioleiomyomatosis Pulmonary vascular misalignment Pulmonary capillary hemangiomatosis Developmental abnormalities &c &c
 Nt pro brain natriuretic peptide
Nt pro brain natriuretic peptide Pulmonary hypertension
Pulmonary hypertension Pulmonary hypertension
Pulmonary hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Sachin gupta md
Sachin gupta md Medslide
Medslide Nervous mechanism for regulation of blood pressure
Nervous mechanism for regulation of blood pressure Pulmonary hypertension causes
Pulmonary hypertension causes Pulmonary hypertension
Pulmonary hypertension Rvsp calculation
Rvsp calculation Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Stages of pulmonary hypertension
Stages of pulmonary hypertension Kristoffer wolter
Kristoffer wolter Capado ia
Capado ia Wolter monteskiusz
Wolter monteskiusz