NCL Low Calorie Diet Service Launch Training Welcome




- Slides: 56
NCL Low Calorie Diet: Service Launch Training
Welcome & Introductions • • • Dr Karl Roberts Pricilla Aboagye Efa Mortty • Clare Driscoll Islington Long-term conditions clinical lead, NCL CCG Independent Clinical Services (ICS) Deputy Head of Medicines Management, Haringey directorate, NCL CCG Primary Care Development Manager, NCL CCG
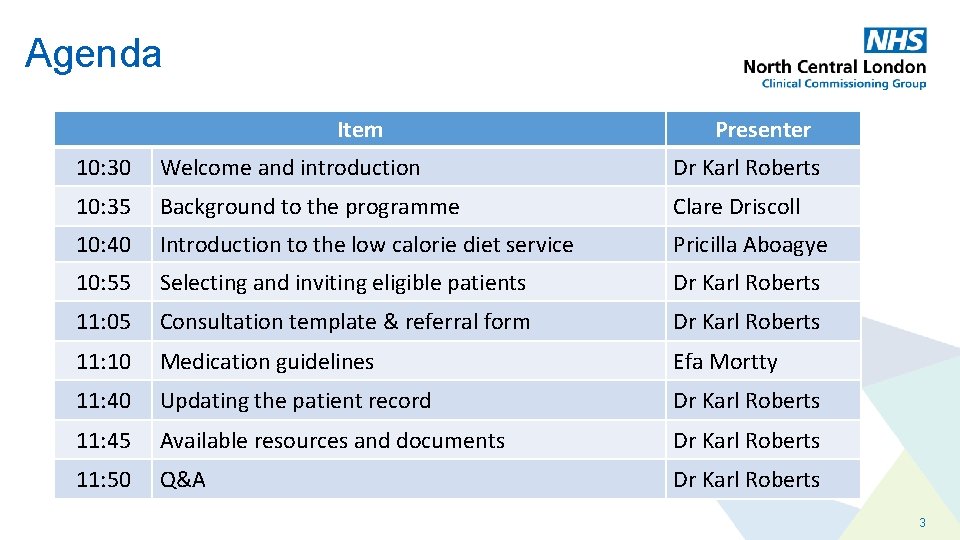
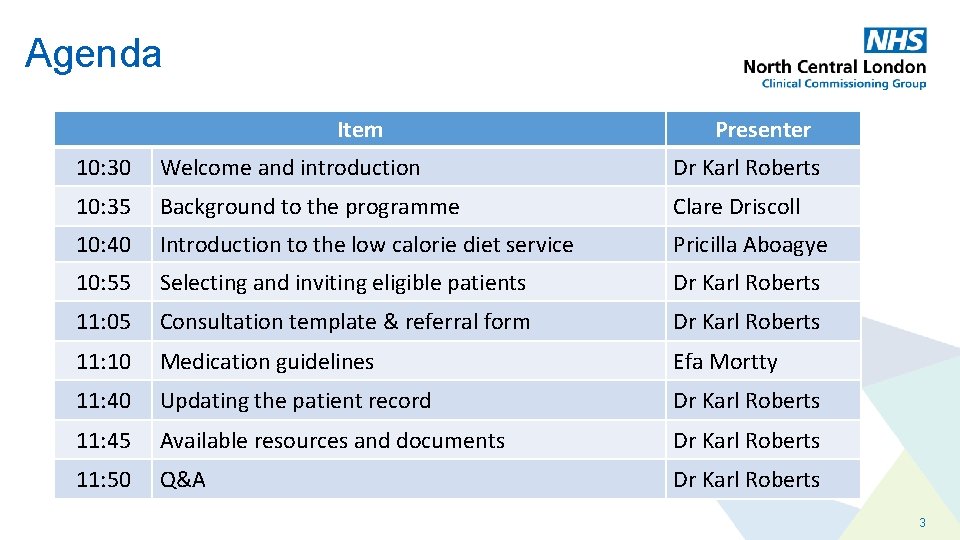
Agenda Item Presenter 10: 30 Welcome and introduction Dr Karl Roberts 10: 35 Background to the programme Clare Driscoll 10: 40 Introduction to the low calorie diet service Pricilla Aboagye 10: 55 Selecting and inviting eligible patients Dr Karl Roberts 11: 05 Consultation template & referral form Dr Karl Roberts 11: 10 Medication guidelines Efa Mortty 11: 40 Updating the patient record Dr Karl Roberts 11: 45 Available resources and documents Dr Karl Roberts 11: 50 Q&A Dr Karl Roberts 3

Programme Background Clare Driscoll
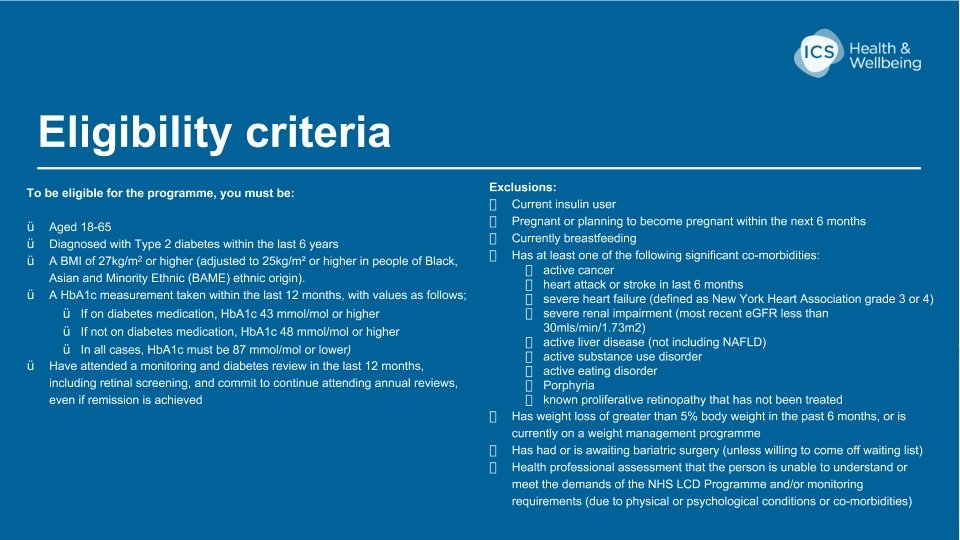
Programme Background • Commissioned by NHS England, NCL CCG is launching a low calorie diet service pilot for people with type 2 diabetes in October 2020 • NCL is one of 10 sites in England chosen to pilot the service for 2 years, with 500 patient places available • The programme is based on the Di. RECT and DROPLET clinical trials which demonstrated that as a result of low calorie diet treatment, people Type 2 diabetes who were overweight could achieve remission • The service will be delivered digitally by Independent Clinical Services (ICS) Health & Wellbeing • There is no cost for the patient and the service will be evaluated by NHS England 5
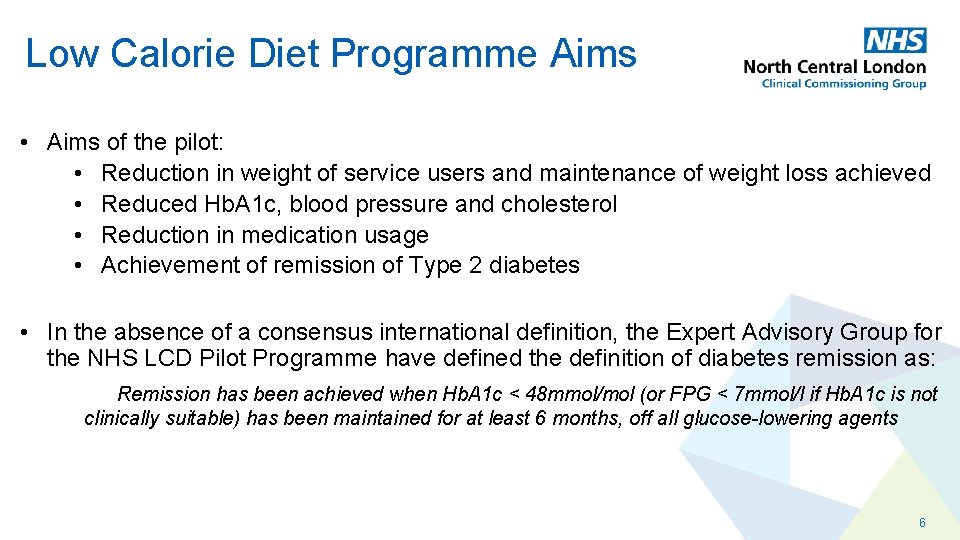
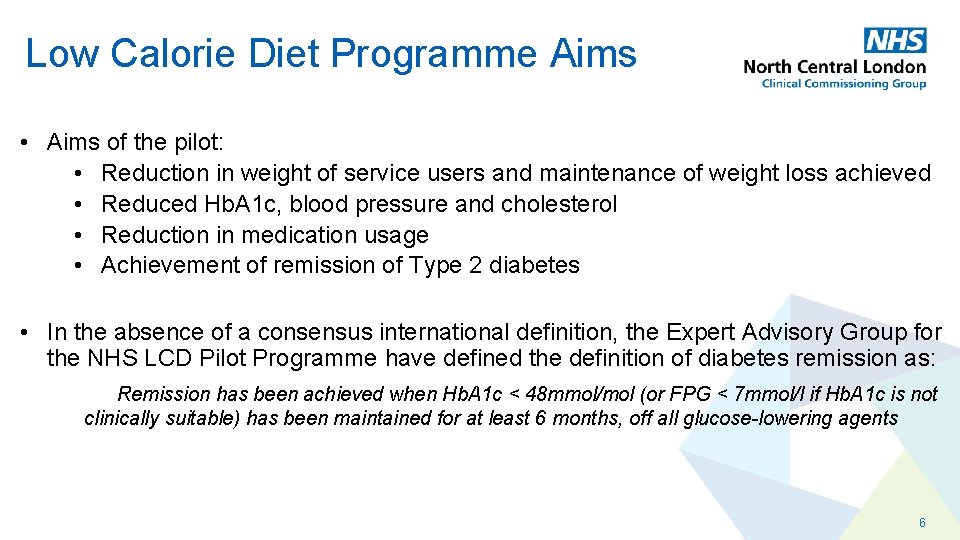
Low Calorie Diet Programme Aims • Aims of the pilot: • Reduction in weight of service users and maintenance of weight loss achieved • Reduced Hb. A 1 c, blood pressure and cholesterol • Reduction in medication usage • Achievement of remission of Type 2 diabetes • In the absence of a consensus international definition, the Expert Advisory Group for the NHS LCD Pilot Programme have defined the definition of diabetes remission as: Remission has been achieved when Hb. A 1 c < 48 mmol/mol (or FPG < 7 mmol/l if Hb. A 1 c is not clinically suitable) has been maintained for at least 6 months, off all glucose-lowering agents 6

ICS Health & Wellbeing 7
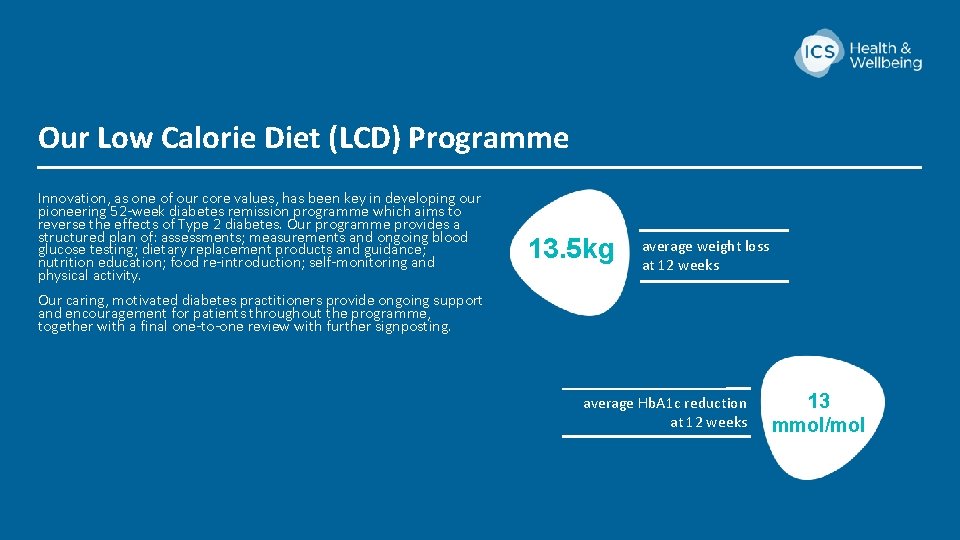
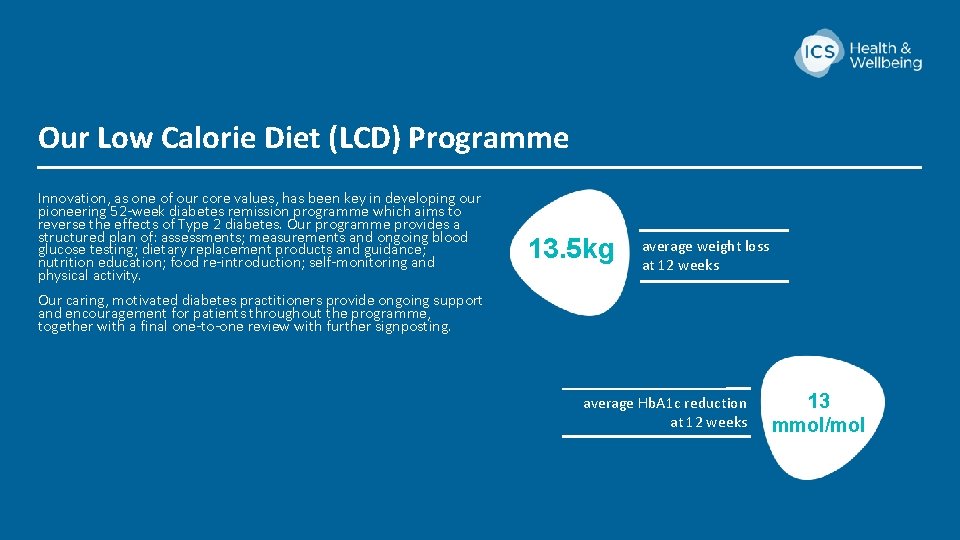
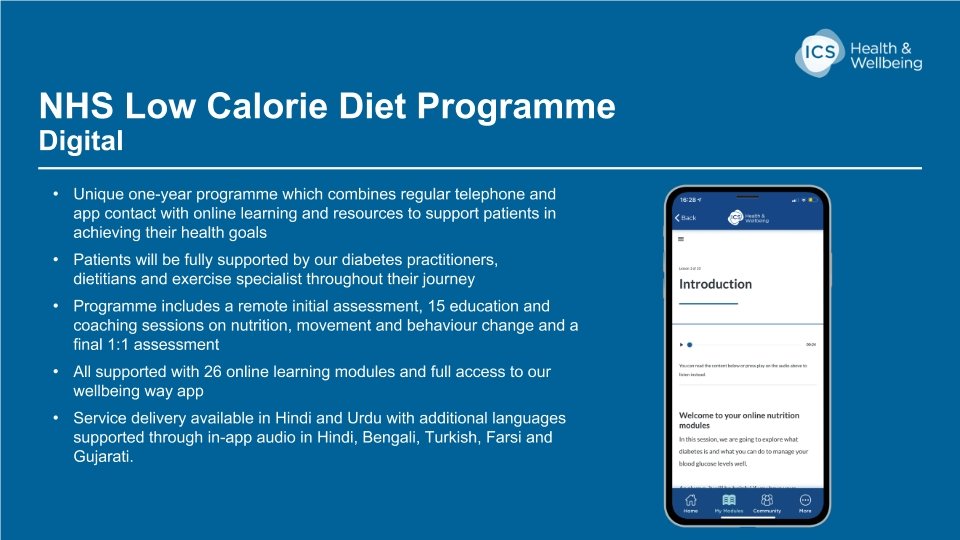
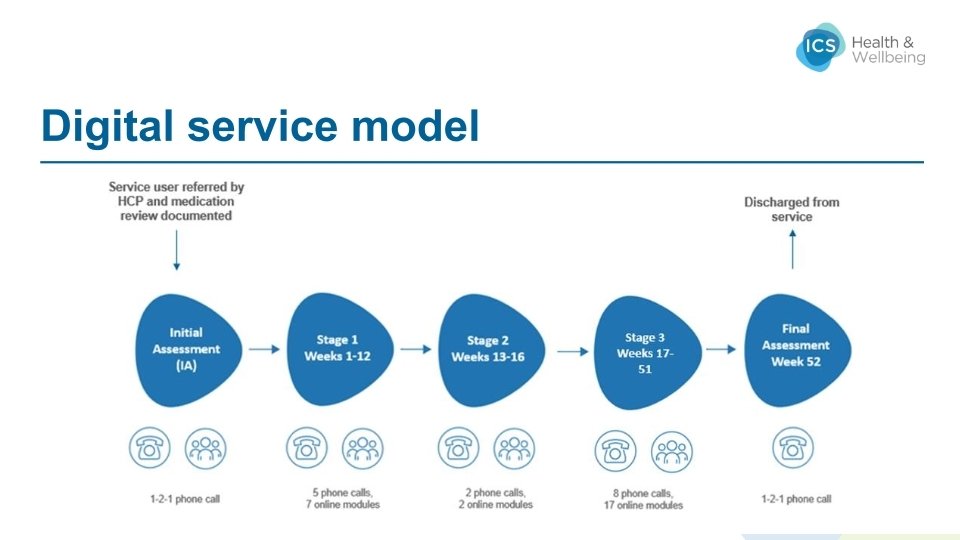
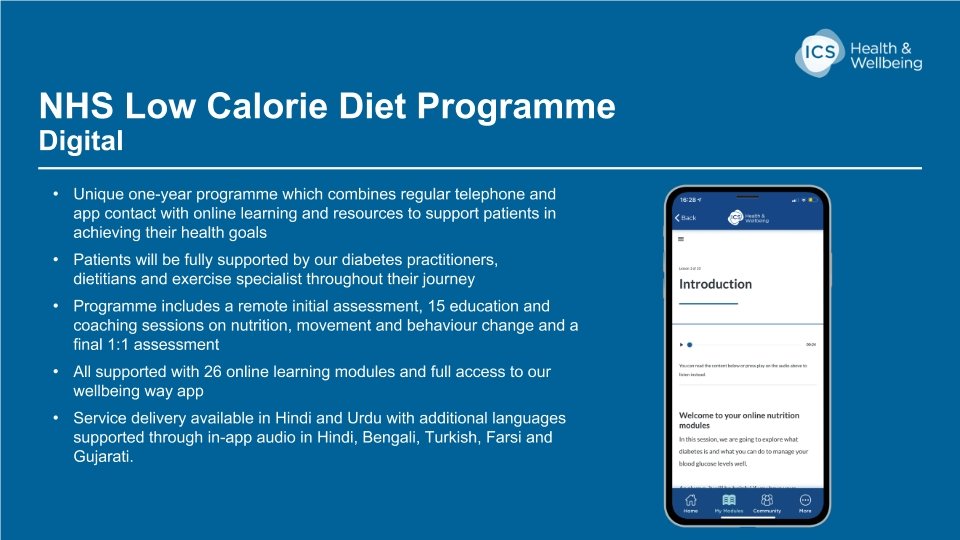
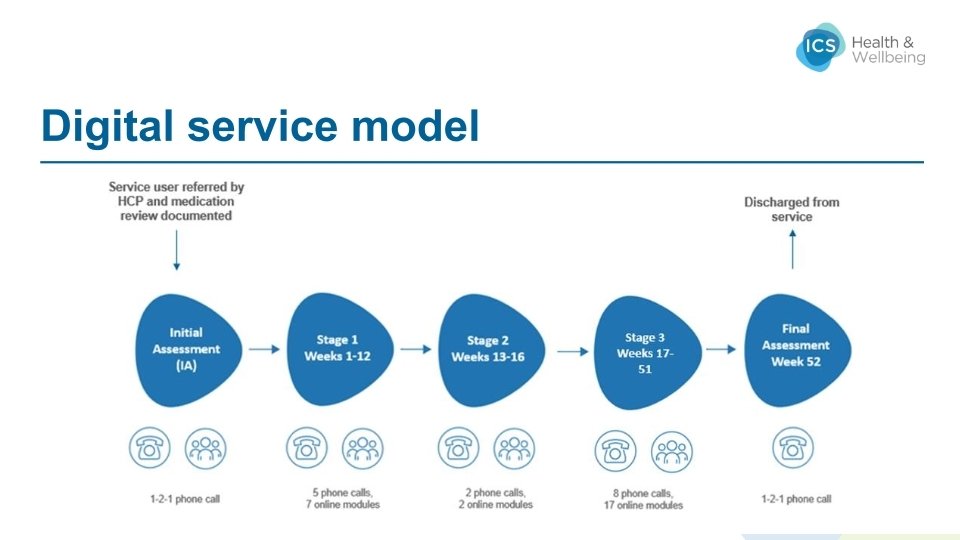
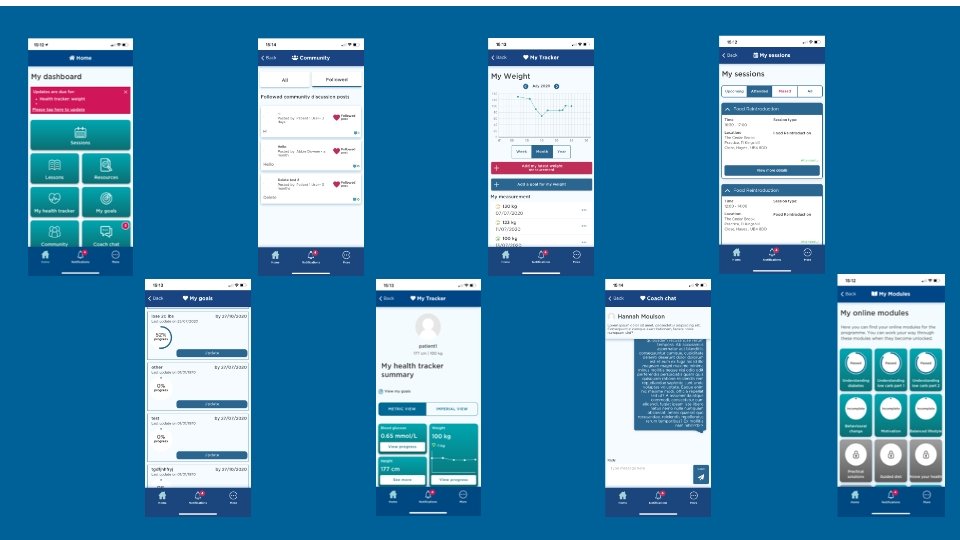
Our Low Calorie Diet (LCD) Programme Innovation, as one of our core values, has been key in developing our pioneering 52 -week diabetes remission programme which aims to reverse the effects of Type 2 diabetes. Our programme provides a structured plan of: assessments; measurements and ongoing blood glucose testing; dietary replacement products and guidance; nutrition education; food re-introduction; self-monitoring and physical activity. 13. 5 kg average weight loss at 12 weeks Our caring, motivated diabetes practitioners provide ongoing support and encouragement for patients throughout the programme, together with a final one-to-one review with further signposting. average Hb. A 1 c reduction at 12 weeks 13 mmol/mol 8

Our Low Calorie Diet (LCD) Programme 9
10
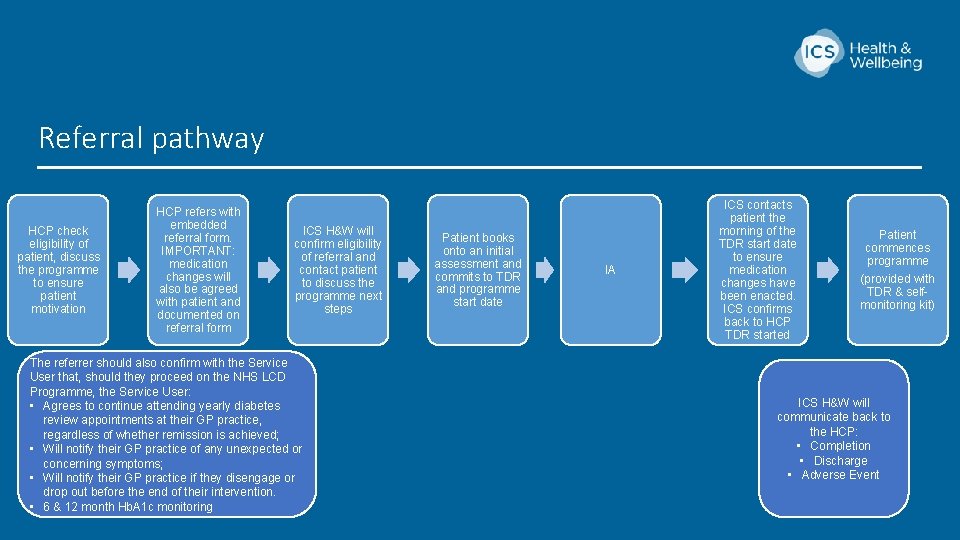
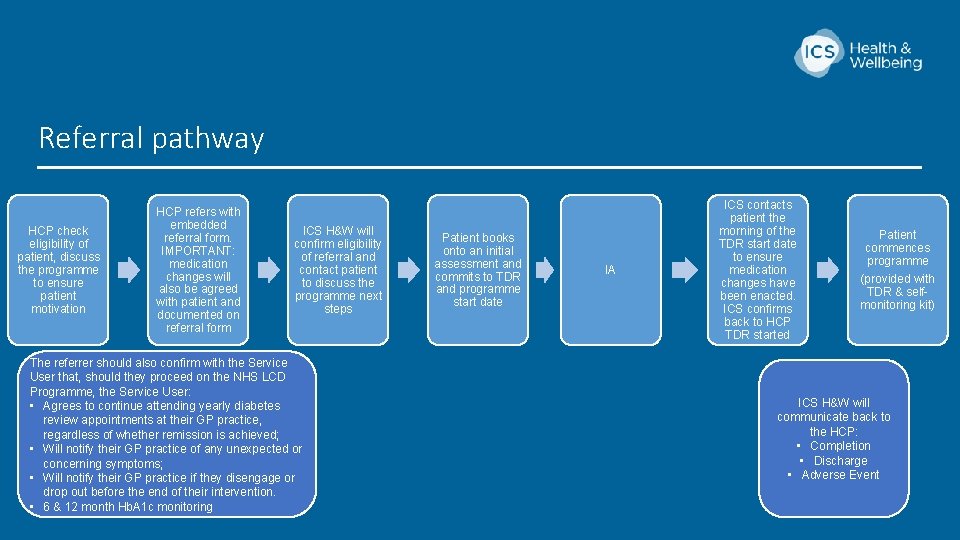
Referral pathway HCP check eligibility of patient, discuss the programme to ensure patient motivation HCP refers with embedded referral form. IMPORTANT: medication changes will also be agreed with patient and documented on referral form ICS H&W will confirm eligibility of referral and contact patient to discuss the programme next steps The referrer should also confirm with the Service User that, should they proceed on the NHS LCD Programme, the Service User: • Agrees to continue attending yearly diabetes review appointments at their GP practice, regardless of whether remission is achieved; • Will notify their GP practice of any unexpected or concerning symptoms; • Will notify their GP practice if they disengage or drop out before the end of their intervention. • 6 & 12 month Hb. A 1 c monitoring Patient books onto an initial assessment and commits to TDR and programme start date IA ICS contacts patient the morning of the TDR start date to ensure medication changes have been enacted. ICS confirms back to HCP TDR started Patient commences programme (provided with TDR & selfmonitoring kit) ICS H&W will communicate back to the HCP: • Completion • Discharge • Adverse Event 11
12
13
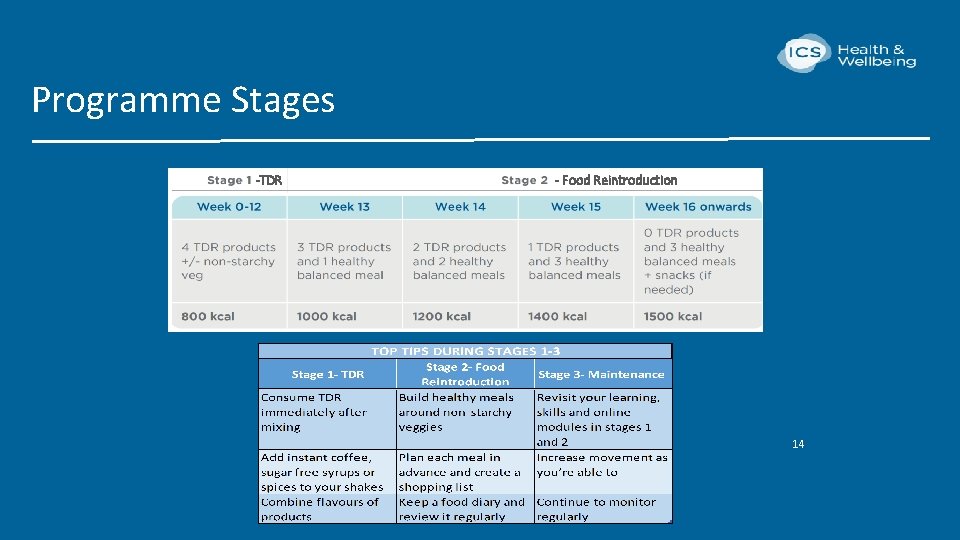
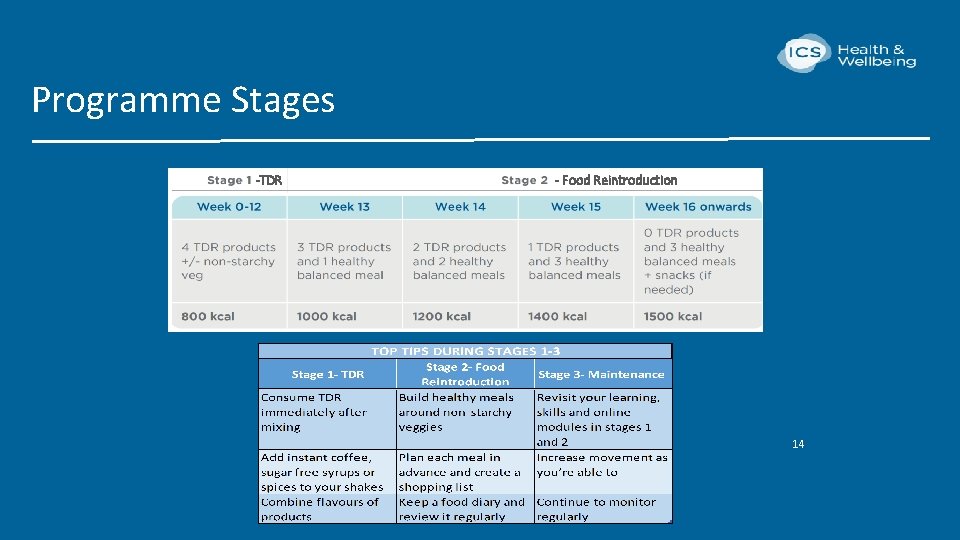
Programme Stages -TDR - Food Reintroduction 14 14
15
Total Diet Replacement Products • Altralife is formulated to provide energy, protein, vitamins and minerals for total diet replacement • Service users consume 4 products per day in the TDR phase (approx. 800 kcals) • Shakes available in 4 different flavours- banana, chocolate, strawberry and vanilla • Soups available in 2 flavours- chicken and vegetable • Halal, kosher and gluten free • Additional fibre supplements also provided • Service users order a sample pack initially to trial flavours and can then order a mixture of products for the full TDR phase 16
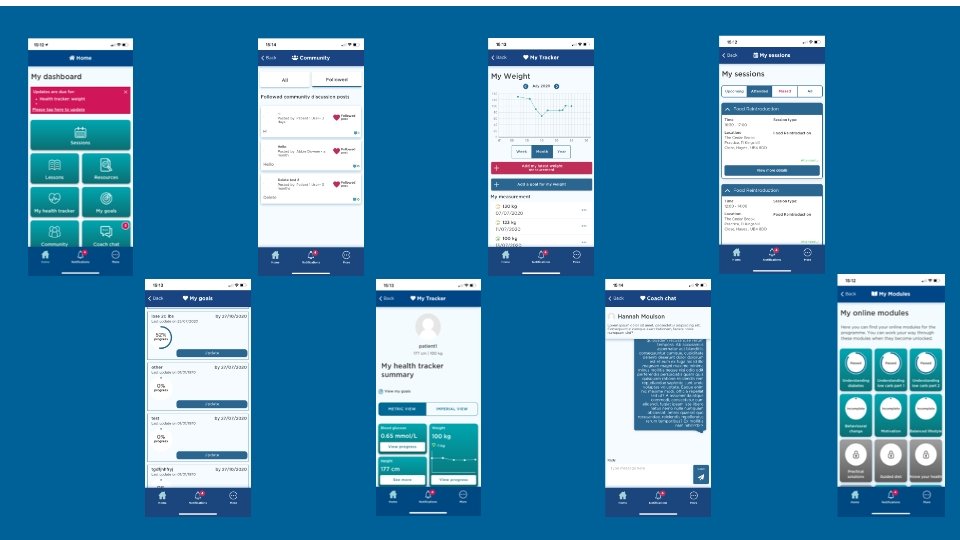
Measurements collected on the programme • Blood Glucose • Weight • Blood Pressure – only if an SU takes blood pressure lowering medication *Height is also a required measurement but will be collected via the referral form. • After the booking call is completed, the patient will be emailed order codes to order a scale, glucometer and blood pressure monitor (only if on BP lowering medication), free of charge. • The patient will also be provided with video guides demonstrating how to accurately use equipment. Practices are NOT expected to provide instruction on equipment use. • Patient will regularly submit data via the app and data will be reviewed during each review call. 17
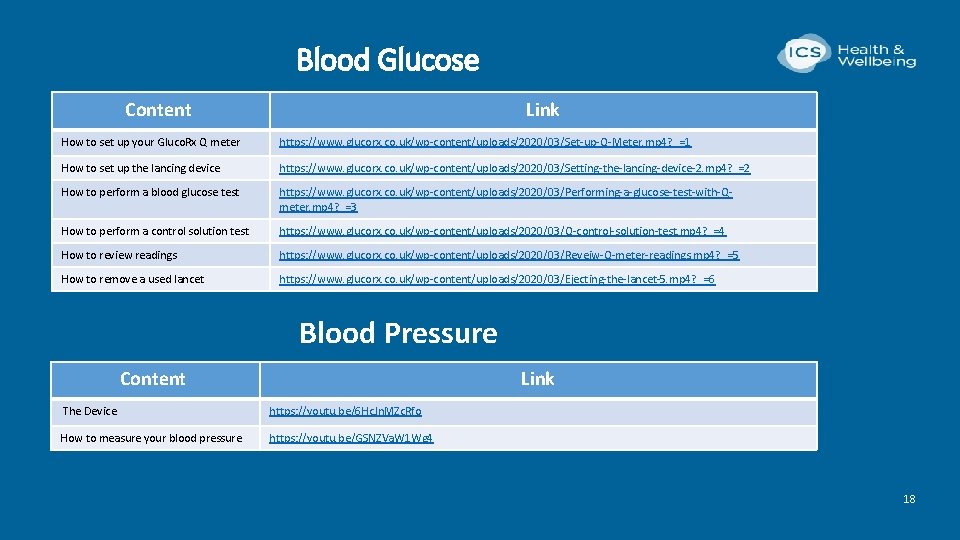
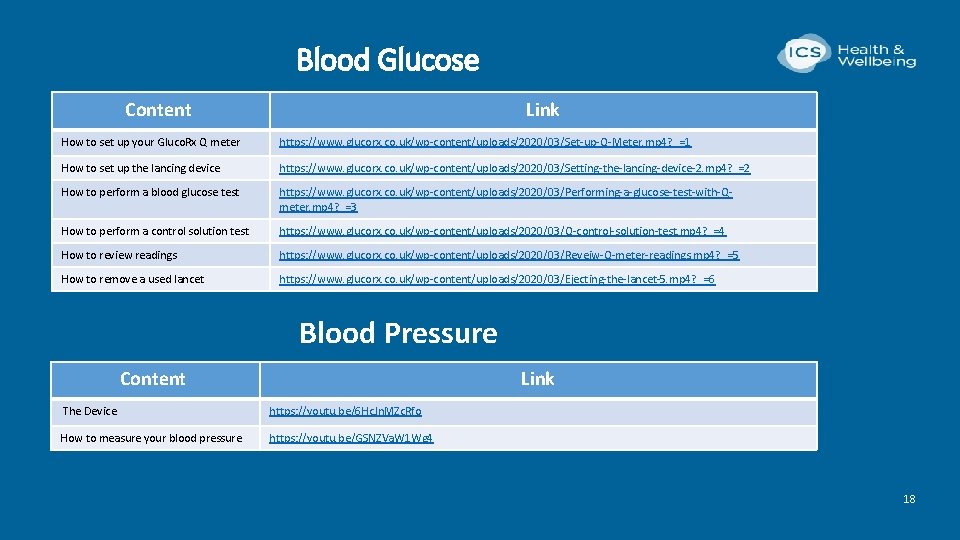
Blood Glucose Content Link How to set up your Gluco. Rx Q meter https: //www. glucorx. co. uk/wp-content/uploads/2020/03/Set-up-Q-Meter. mp 4? _=1 How to set up the lancing device https: //www. glucorx. co. uk/wp-content/uploads/2020/03/Setting-the-lancing-device-2. mp 4? _=2 How to perform a blood glucose test https: //www. glucorx. co. uk/wp-content/uploads/2020/03/Performing-a-glucose-test-with-Qmeter. mp 4? _=3 How to perform a control solution test https: //www. glucorx. co. uk/wp-content/uploads/2020/03/Q-control-solution-test. mp 4? _=4 How to review readings https: //www. glucorx. co. uk/wp-content/uploads/2020/03/Reveiw-Q-meter-readings. mp 4? _=5 How to remove a used lancet https: //www. glucorx. co. uk/wp-content/uploads/2020/03/Ejecting-the-lancet-5. mp 4? _=6 Blood Pressure Content Link The Device https: //youtu. be/6 Hc. Jn. MZc. Rfo How to measure your blood pressure https: //youtu. be/GSNZVa. W 1 Wg 4 18 18
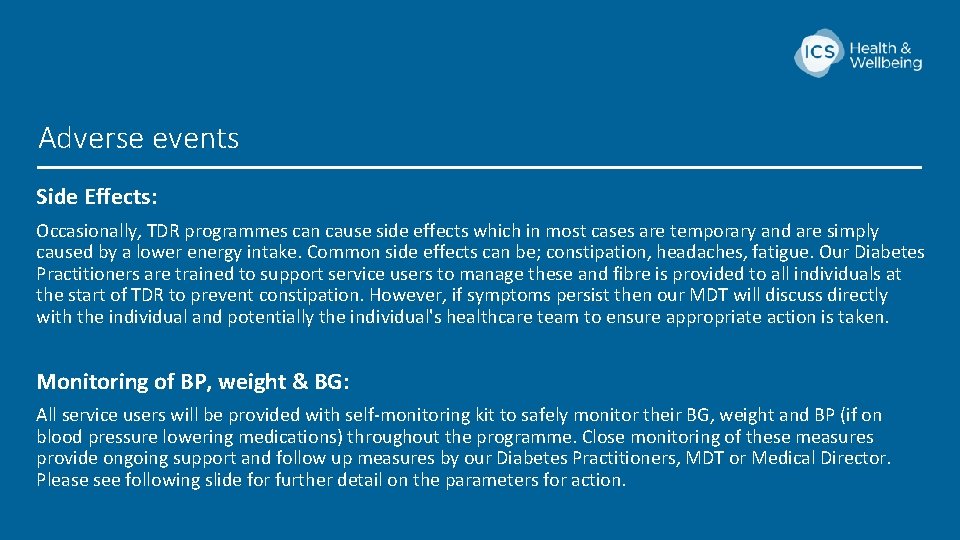
Adverse events Side Effects: Occasionally, TDR programmes can cause side effects which in most cases are temporary and are simply caused by a lower energy intake. Common side effects can be; constipation, headaches, fatigue. Our Diabetes Practitioners are trained to support service users to manage these and fibre is provided to all individuals at the start of TDR to prevent constipation. However, if symptoms persist then our MDT will discuss directly with the individual and potentially the individual's healthcare team to ensure appropriate action is taken. Monitoring of BP, weight & BG: All service users will be provided with self-monitoring kit to safely monitor their BG, weight and BP (if on blood pressure lowering medications) throughout the programme. Close monitoring of these measures provide ongoing support and follow up measures by our Diabetes Practitioners, MDT or Medical Director. Please see following slide for further detail on the parameters for action. 19
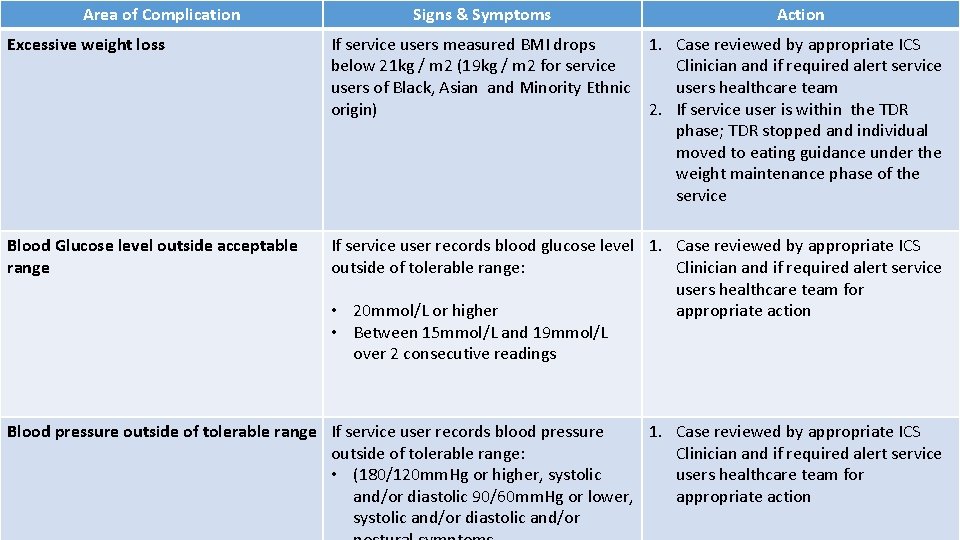
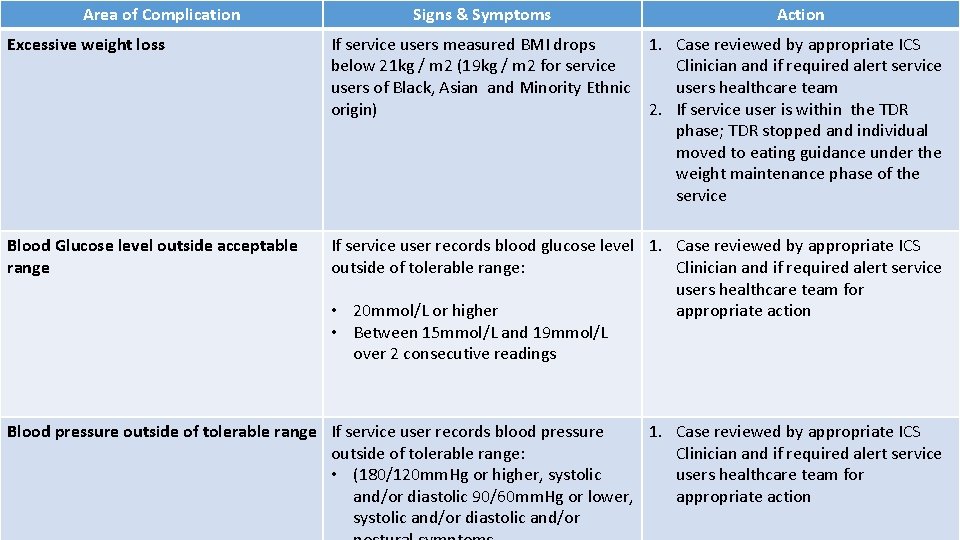
Area of Complication Signs & Symptoms Action Excessive weight loss If service users measured BMI drops 1. Case reviewed by appropriate ICS below 21 kg / m 2 (19 kg / m 2 for service Clinician and if required alert service users of Black, Asian and Minority Ethnic users healthcare team origin) 2. If service user is within the TDR phase; TDR stopped and individual moved to eating guidance under the weight maintenance phase of the service Blood Glucose level outside acceptable range If service user records blood glucose level 1. Case reviewed by appropriate ICS outside of tolerable range: Clinician and if required alert service users healthcare team for • 20 mmol/L or higher appropriate action • Between 15 mmol/L and 19 mmol/L over 2 consecutive readings Blood pressure outside of tolerable range If service user records blood pressure 1. Case reviewed by appropriate ICS outside of tolerable range: Clinician and if required alert service • (180/120 mm. Hg or higher, systolic users healthcare team for and/or diastolic 90/60 mm. Hg or lower, appropriate action systolic and/or diastolic and/or 20
21
Selecting and inviting eligible patients Dr Karl Roberts
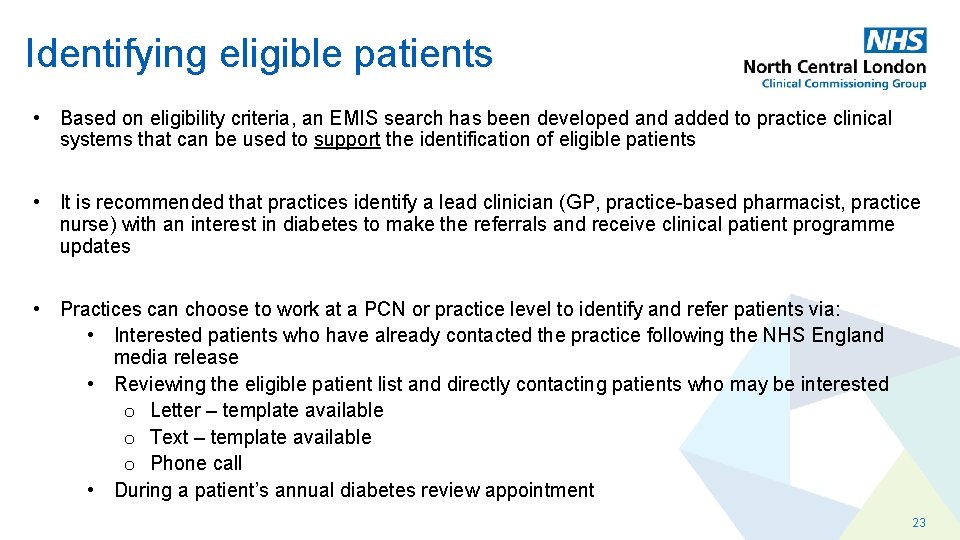
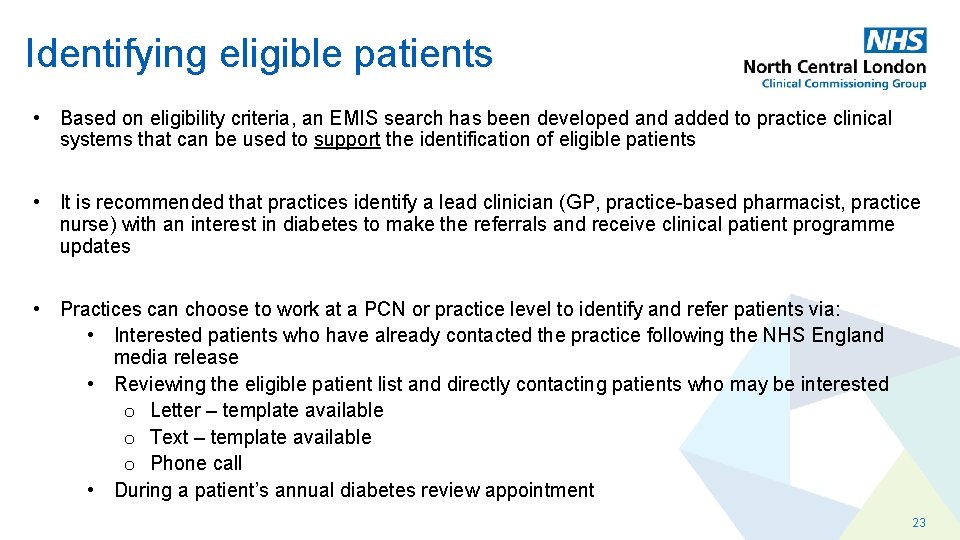
Identifying eligible patients • Based on eligibility criteria, an EMIS search has been developed and added to practice clinical systems that can be used to support the identification of eligible patients • It is recommended that practices identify a lead clinician (GP, practice-based pharmacist, practice nurse) with an interest in diabetes to make the referrals and receive clinical patient programme updates • Practices can choose to work at a PCN or practice level to identify and refer patients via: • Interested patients who have already contacted the practice following the NHS England media release • Reviewing the eligible patient list and directly contacting patients who may be interested o Letter – template available o Text – template available o Phone call • During a patient’s annual diabetes review appointment 23
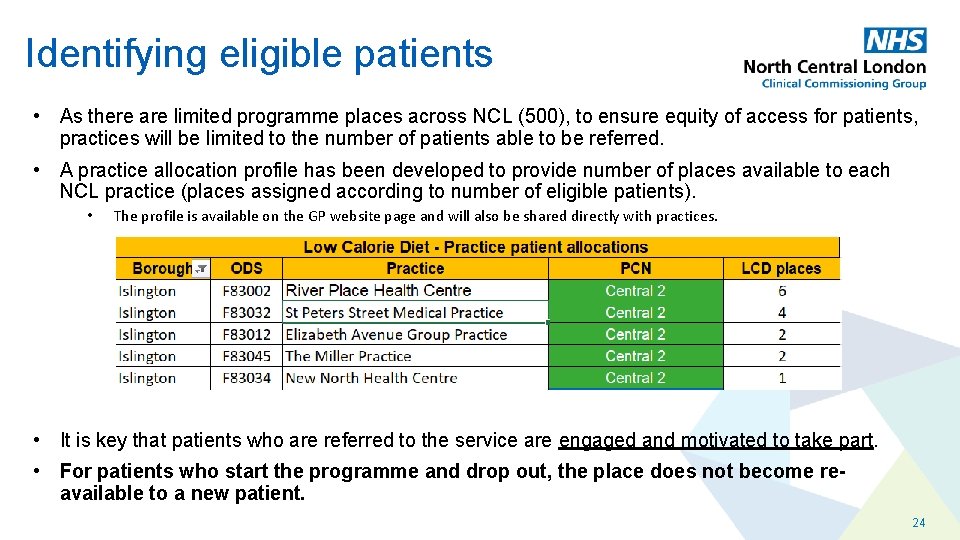
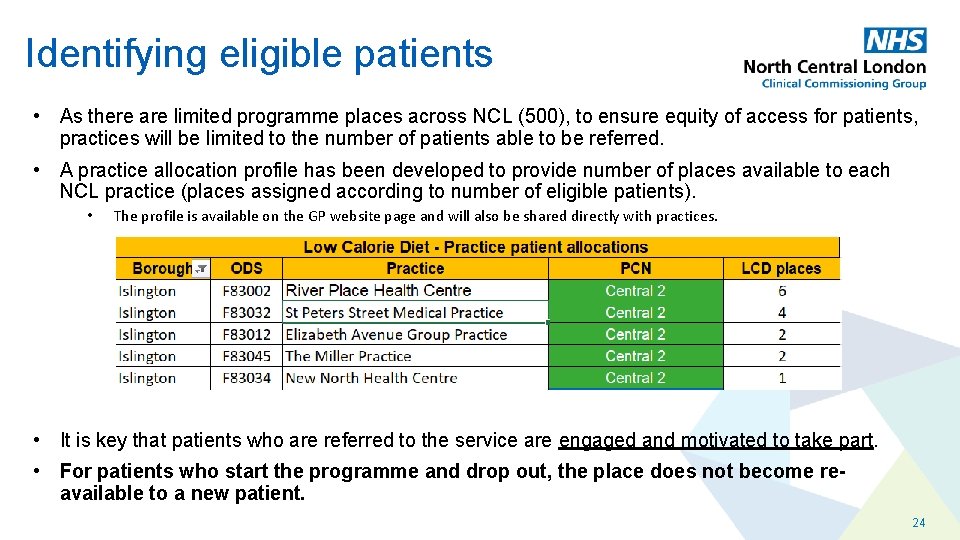
Identifying eligible patients • As there are limited programme places across NCL (500), to ensure equity of access for patients, practices will be limited to the number of patients able to be referred. • A practice allocation profile has been developed to provide number of places available to each NCL practice (places assigned according to number of eligible patients). • The profile is available on the GP website page and will also be shared directly with practices. • It is key that patients who are referred to the service are engaged and motivated to take part. • For patients who start the programme and drop out, the place does not become reavailable to a new patient. 24
Referrer responsibilities • Provide information on concept of remission of Type 2 Diabetes, the LCD service and potential risks and benefits to obtain informed consent • • • Low Calorie Diet patient leaflet available Discuss medication changes to take place on first day of total diet replacement and provide written confirmation of these change to the patient and Provider Respond to any clinical need to further adjust medications according to capillary blood glucose and blood pressure monitoring by the Provider Respond to adverse events if patient contacts practice directly with an urgent clinical need or is directed to the GP practice by the Provider Arrange review of patient at 6 months and 12 months after starting LCD programme with repeat Hb. A 1 c – with further medication adjustment as necessary 25
Enhancing referrals Tips for conversations with interested patients include: • Provided it is clinically appropriate, frame the offer of referral positively as something in which you expect the patient will be interested. Don’t assume the programme won’t be acceptable to a patient • Early in the discussion about the programme, make clear that it is free-of-charge and that there is also no cost to the patient for the TDR products • Make clear that there is ongoing support available for a full year • Most participants report that hunger is not a major problem after the first week • Many people also feel younger with the rapid weight loss and this is self-motivating • Consider motivational interviewing techniques to help patients overcome perceived barriers and support readiness to change 26
Consultation template & referral form Dr Karl Roberts
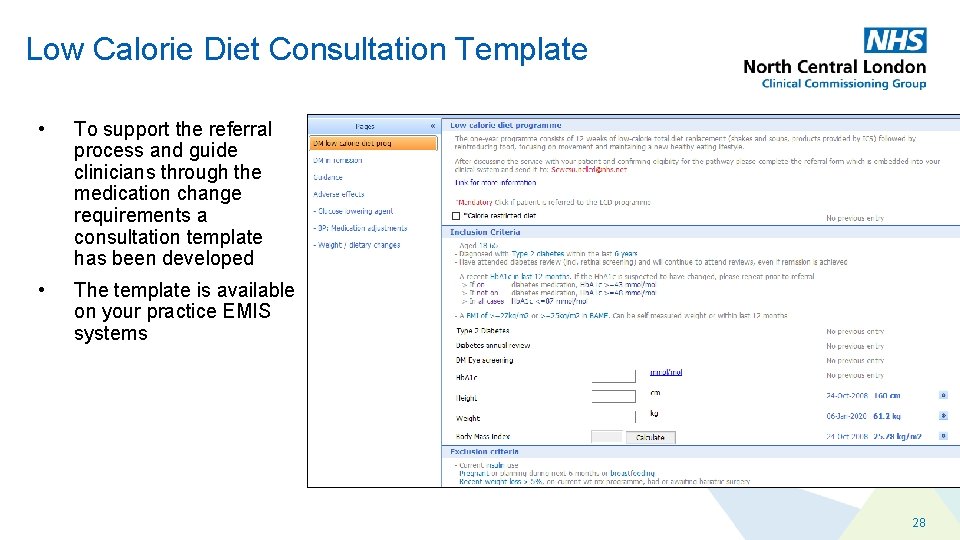
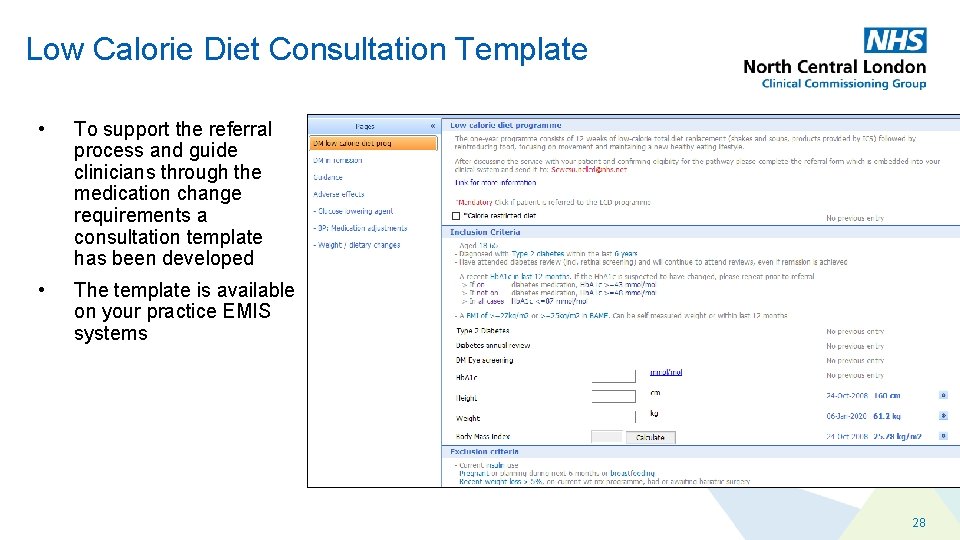
Low Calorie Diet Consultation Template • To support the referral process and guide clinicians through the medication change requirements a consultation template has been developed • The template is available on your practice EMIS systems 28
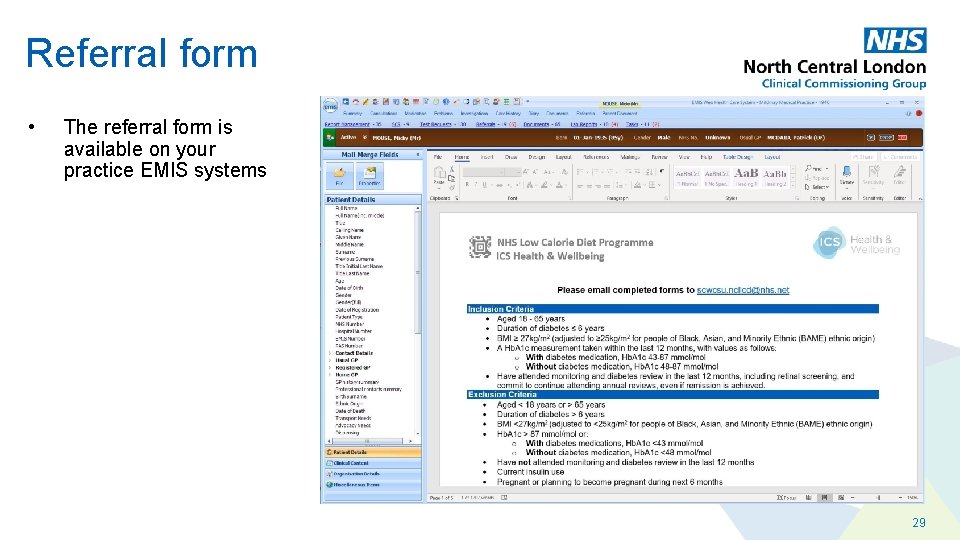
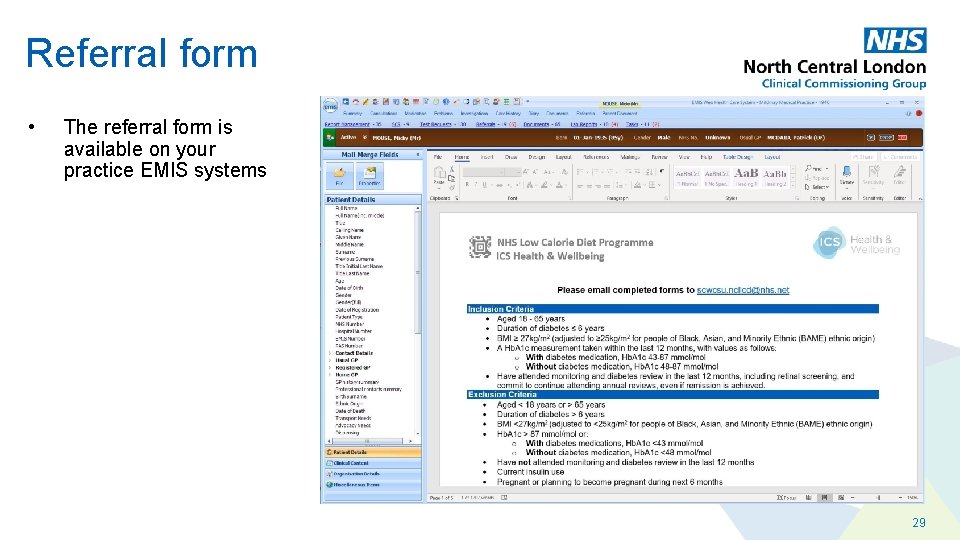
Referral form • The referral form is available on your practice EMIS systems 29
NHS Low Calorie Diet Pilot Programme Adjusting Medicines Efa Mortty Deputy Head of Medicines Management
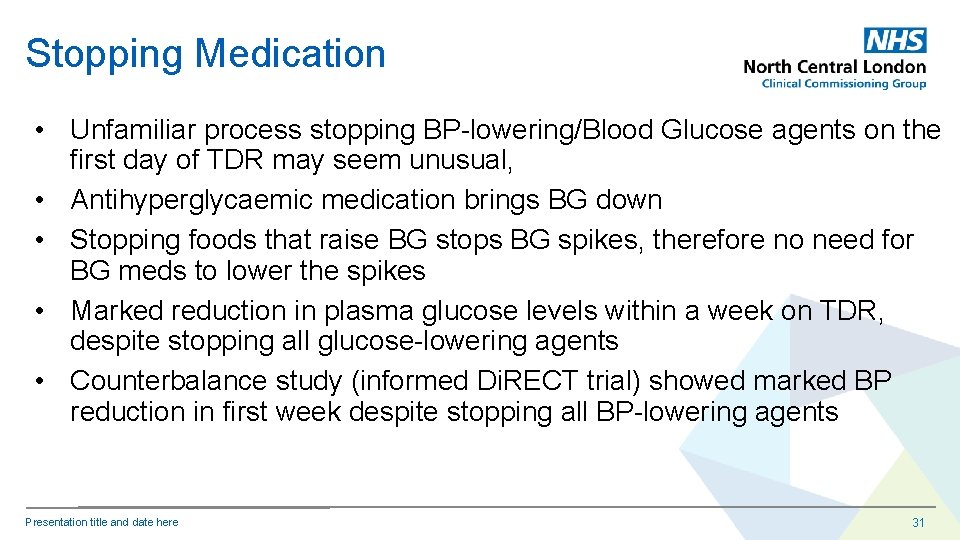
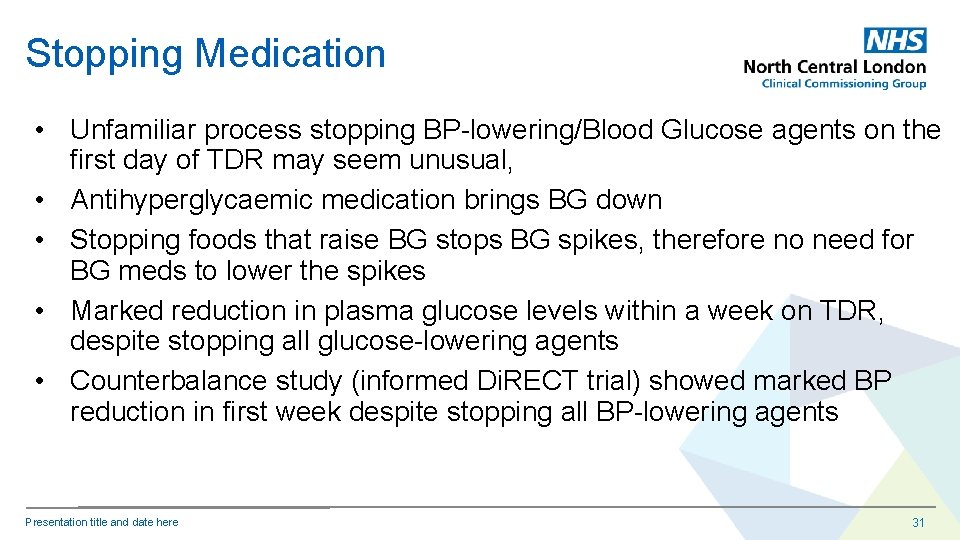
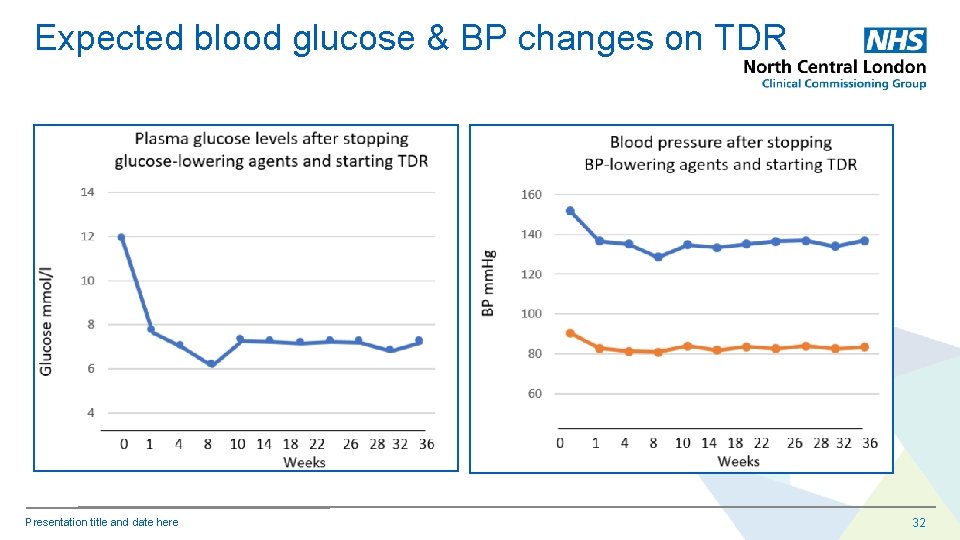
Stopping Medication • Unfamiliar process stopping BP-lowering/Blood Glucose agents on the first day of TDR may seem unusual, • Antihyperglycaemic medication brings BG down • Stopping foods that raise BG stops BG spikes, therefore no need for BG meds to lower the spikes • Marked reduction in plasma glucose levels within a week on TDR, despite stopping all glucose-lowering agents • Counterbalance study (informed Di. RECT trial) showed marked BP reduction in first week despite stopping all BP-lowering agents Presentation title and date here 31
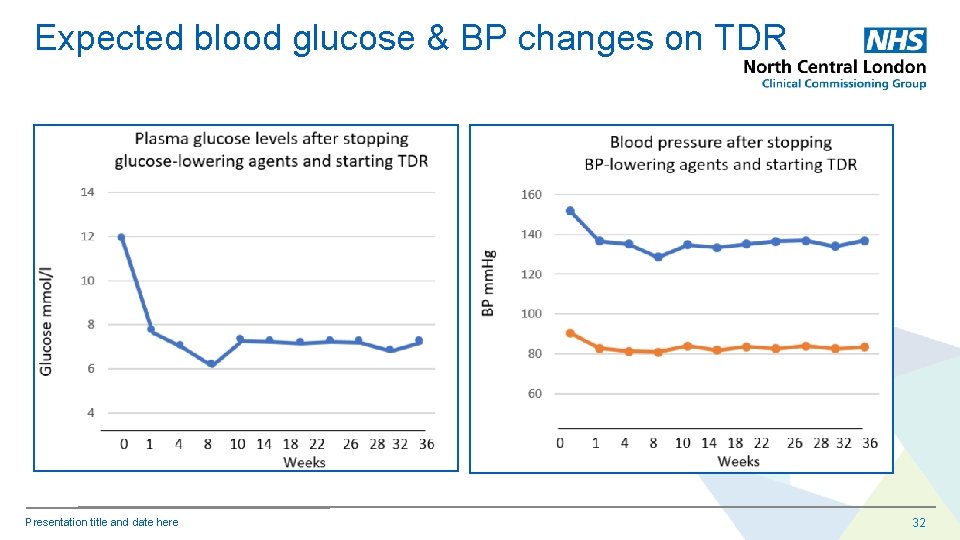
Expected blood glucose & BP changes on TDR Presentation title and date here 32
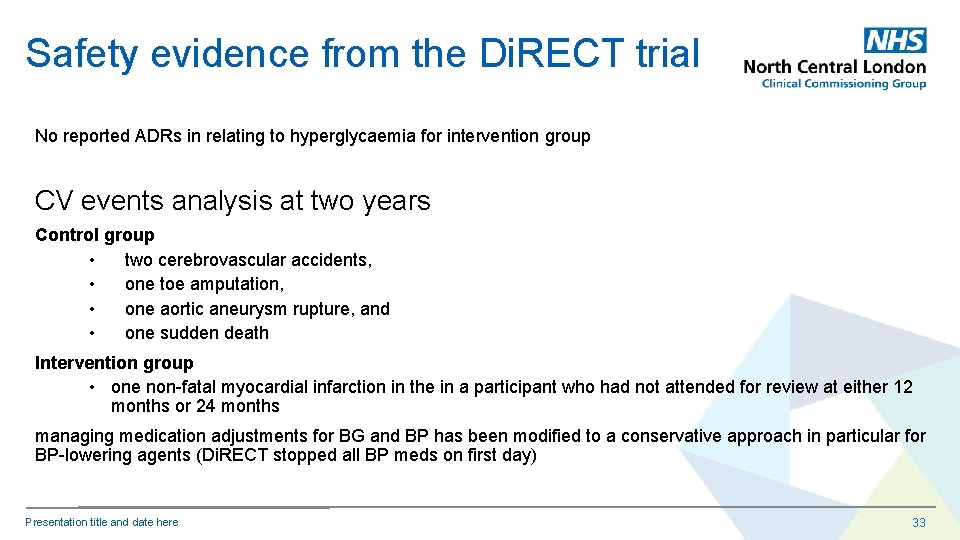
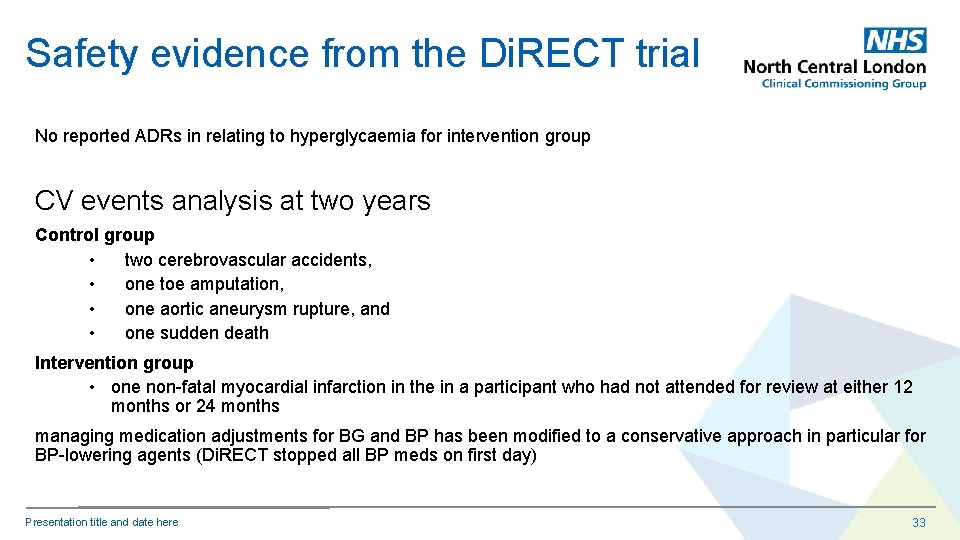
Safety evidence from the Di. RECT trial No reported ADRs in relating to hyperglycaemia for intervention group CV events analysis at two years Control group • two cerebrovascular accidents, • one toe amputation, • one aortic aneurysm rupture, and • one sudden death Intervention group • one non-fatal myocardial infarction in the in a participant who had not attended for review at either 12 months or 24 months managing medication adjustments for BG and BP has been modified to a conservative approach in particular for BP-lowering agents (Di. RECT stopped all BP meds on first day) Presentation title and date here 33
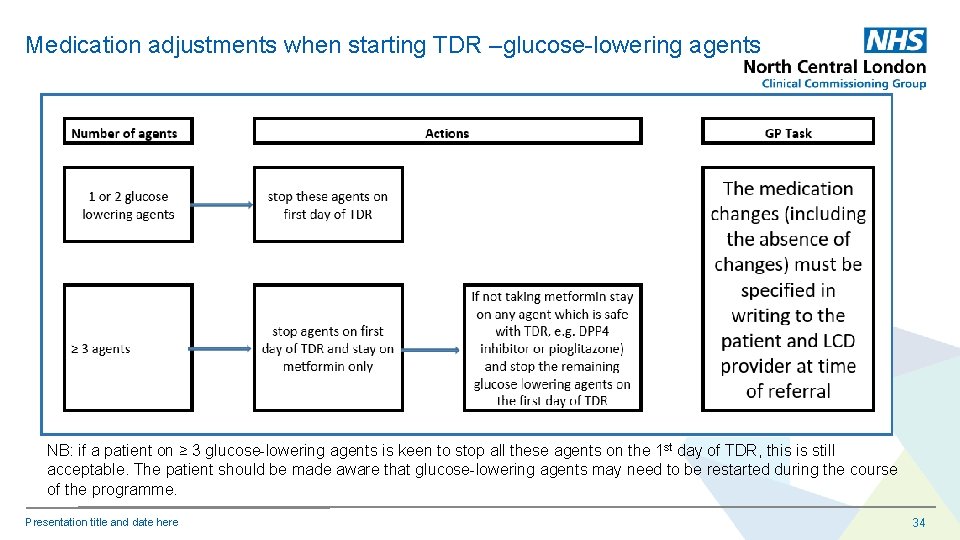
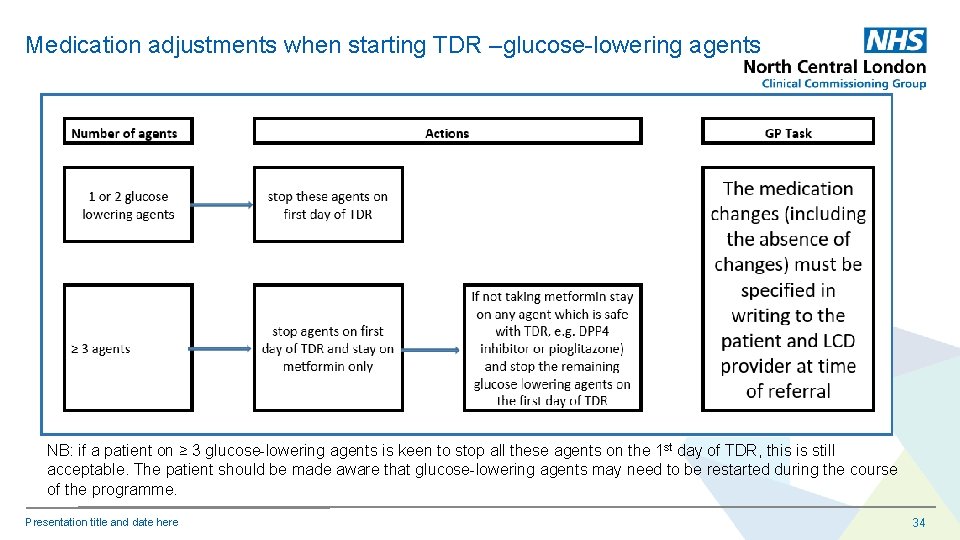
Medication adjustments when starting TDR –glucose-lowering agents NB: if a patient on ≥ 3 glucose-lowering agents is keen to stop all these agents on the 1 st day of TDR, this is still acceptable. The patient should be made aware that glucose-lowering agents may need to be restarted during the course of the programme. Presentation title and date here 34
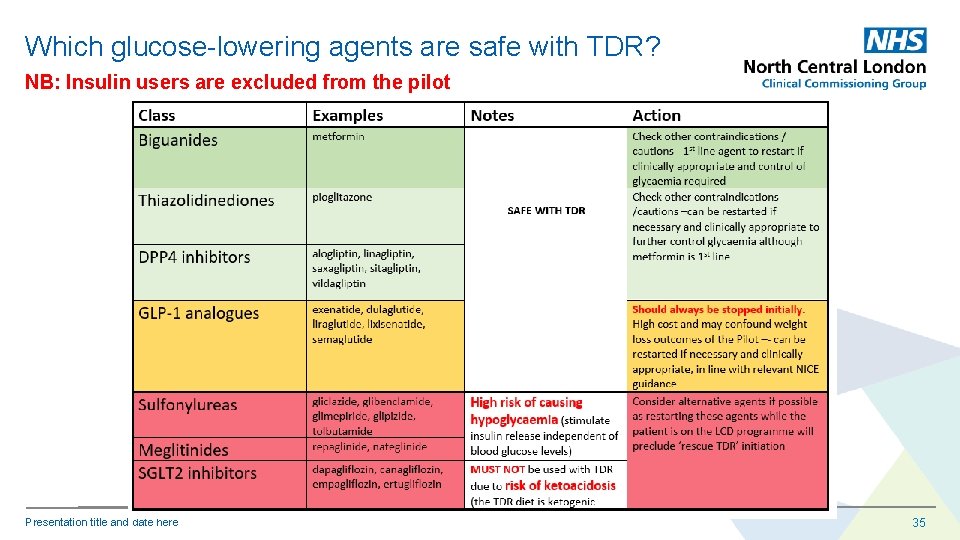
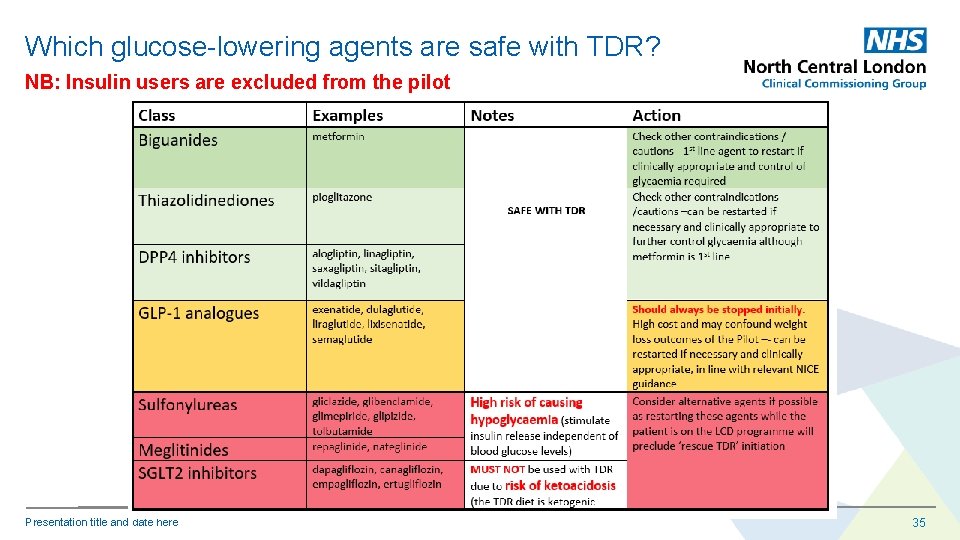
Which glucose-lowering agents are safe with TDR? NB: Insulin users are excluded from the pilot Presentation title and date here 35
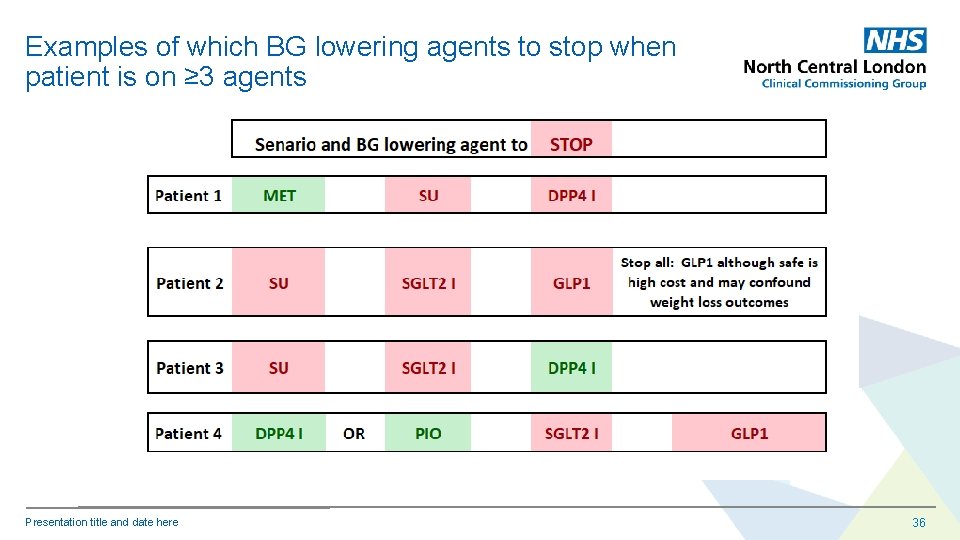
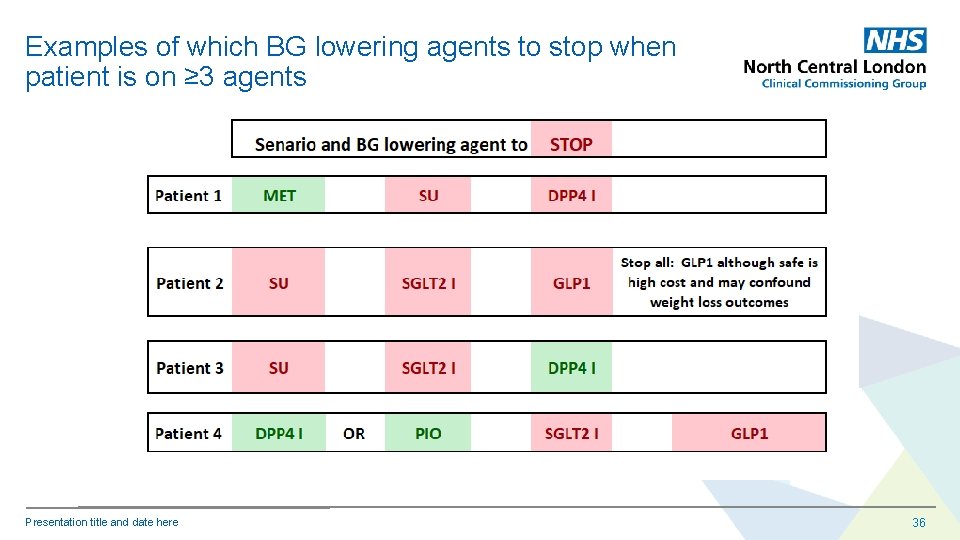
Examples of which BG lowering agents to stop when patient is on ≥ 3 agents Presentation title and date here 36
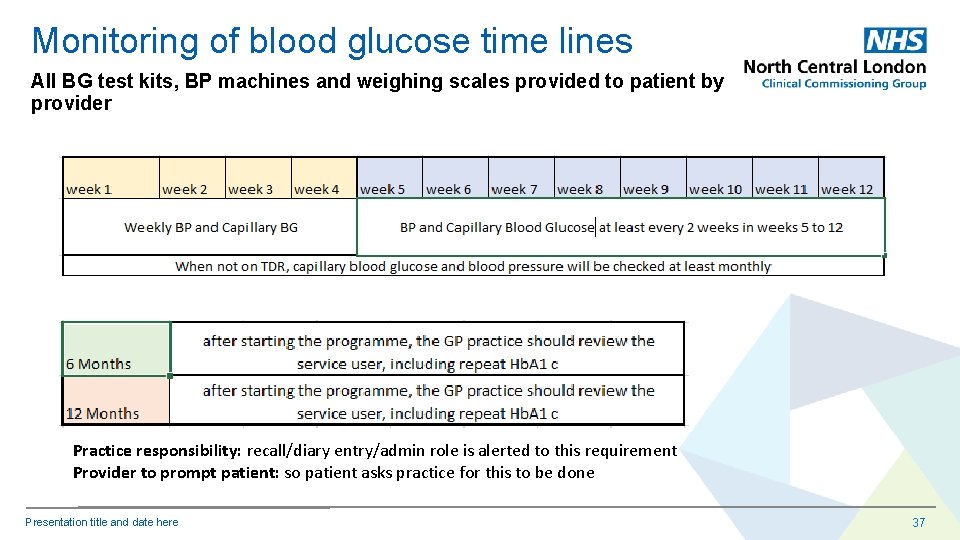
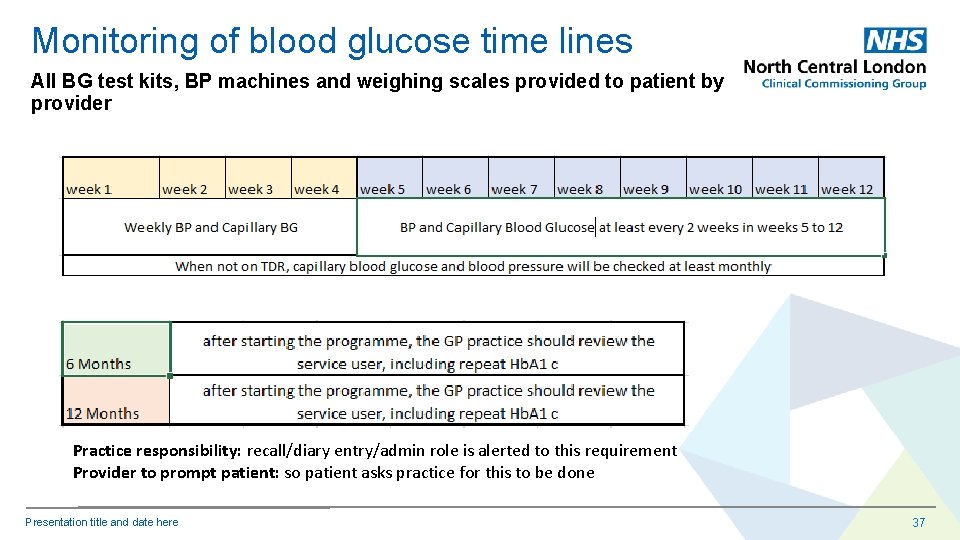
Monitoring of blood glucose time lines All BG test kits, BP machines and weighing scales provided to patient by provider Practice responsibility: recall/diary entry/admin role is alerted to this requirement Provider to prompt patient: so patient asks practice for this to be done Presentation title and date here 37
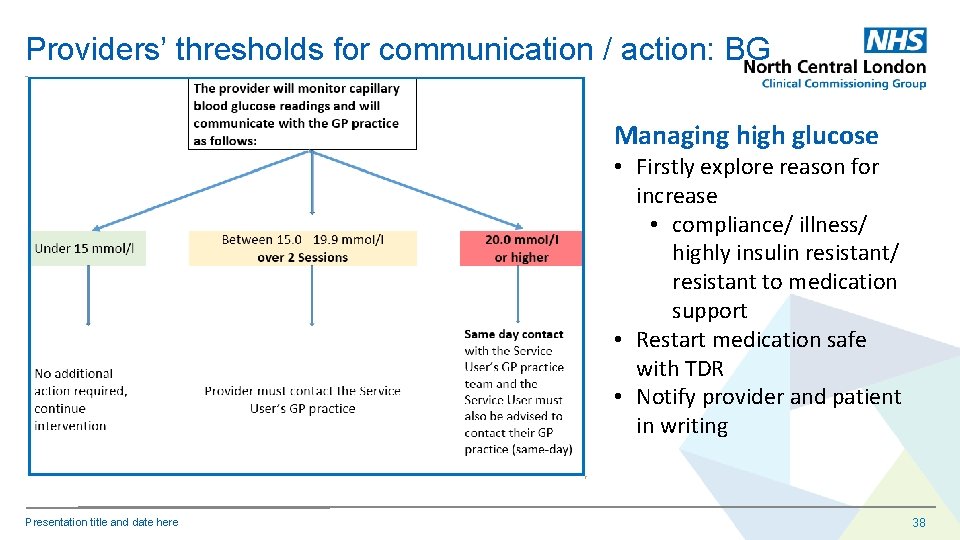
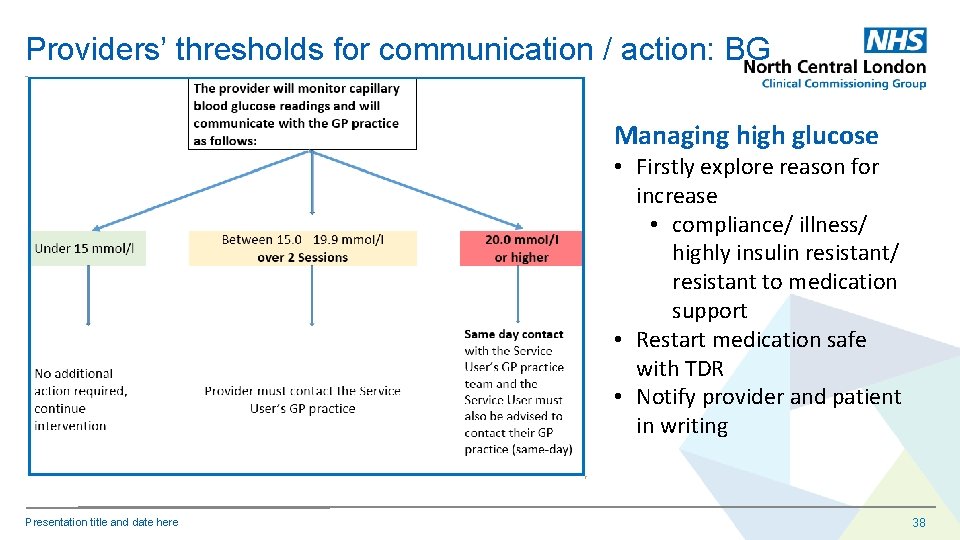
Providers’ thresholds for communication / action: BG Managing high glucose • Firstly explore reason for increase • compliance/ illness/ highly insulin resistant/ resistant to medication support • Restart medication safe with TDR • Notify provider and patient in writing Presentation title and date here 38
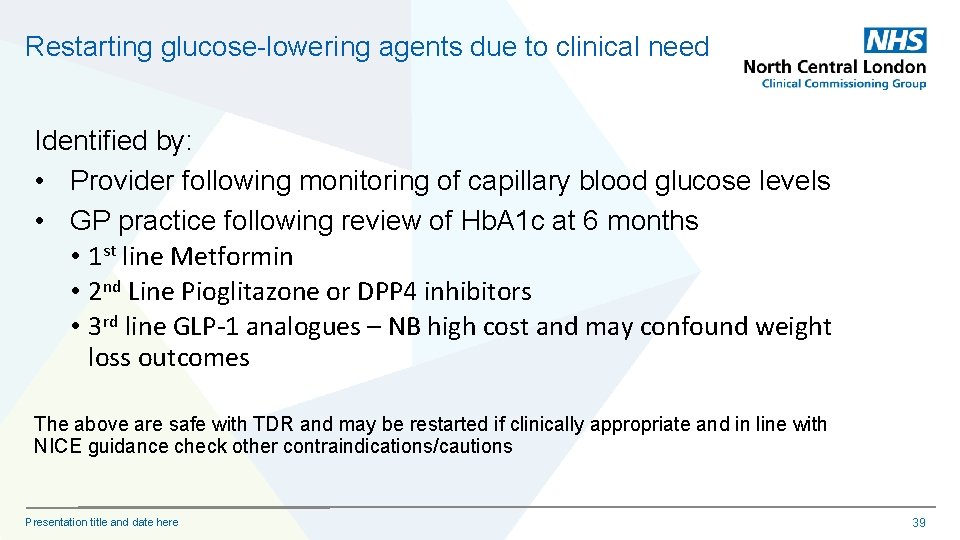
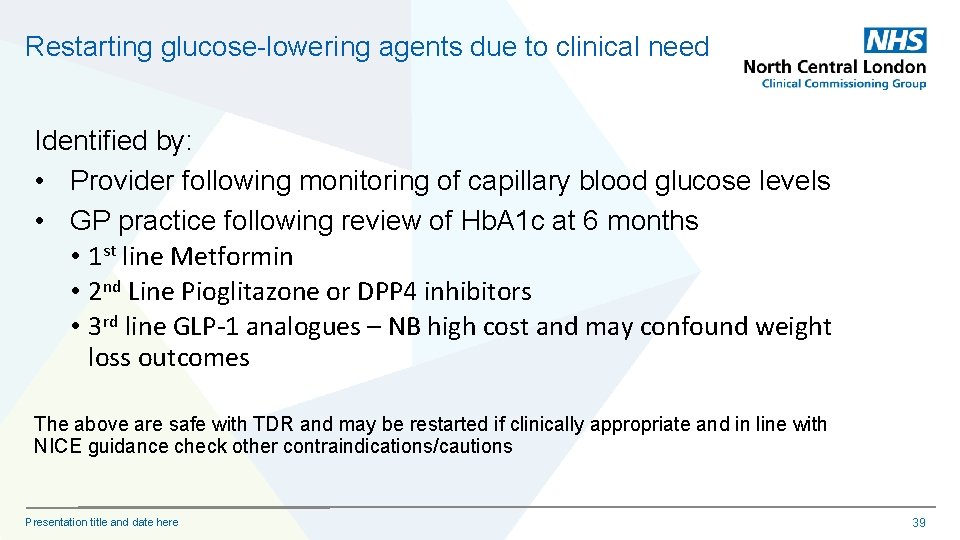
Restarting glucose-lowering agents due to clinical need Identified by: • Provider following monitoring of capillary blood glucose levels • GP practice following review of Hb. A 1 c at 6 months • 1 st line Metformin • 2 nd Line Pioglitazone or DPP 4 inhibitors • 3 rd line GLP-1 analogues – NB high cost and may confound weight loss outcomes The above are safe with TDR and may be restarted if clinically appropriate and in line with NICE guidance check other contraindications/cautions Presentation title and date here 39
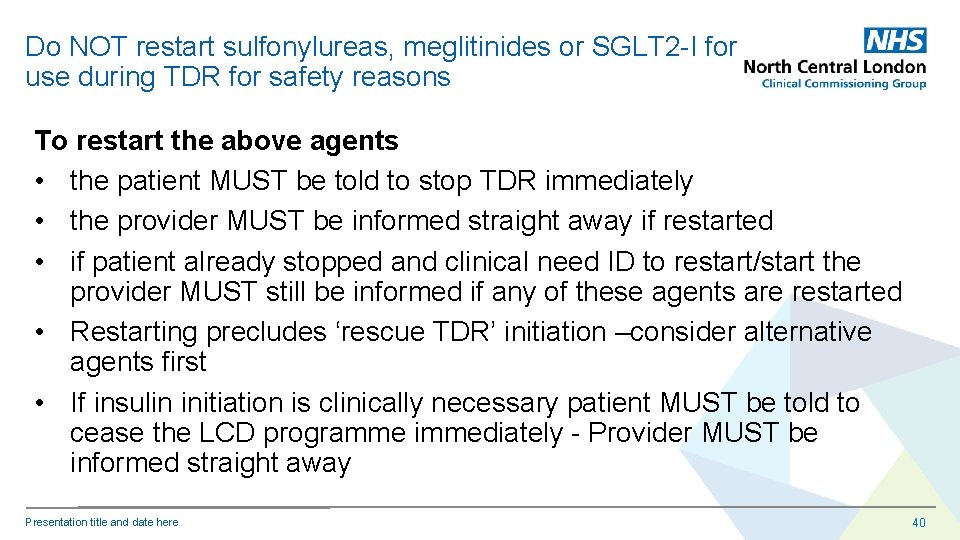
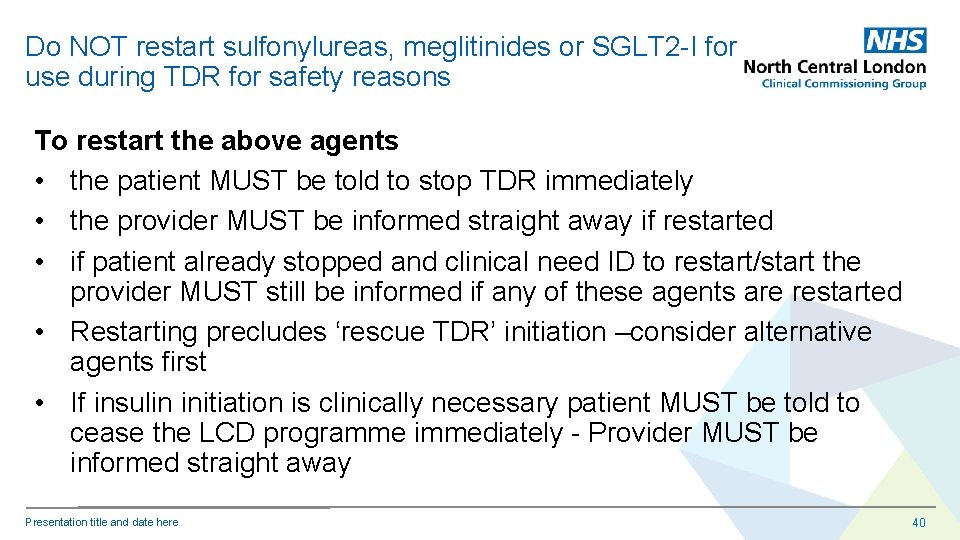
Do NOT restart sulfonylureas, meglitinides or SGLT 2 -I for use during TDR for safety reasons To restart the above agents • the patient MUST be told to stop TDR immediately • the provider MUST be informed straight away if restarted • if patient already stopped and clinical need ID to restart/start the provider MUST still be informed if any of these agents are restarted • Restarting precludes ‘rescue TDR’ initiation –consider alternative agents first • If insulin initiation is clinically necessary patient MUST be told to cease the LCD programme immediately - Provider MUST be informed straight away Presentation title and date here 40
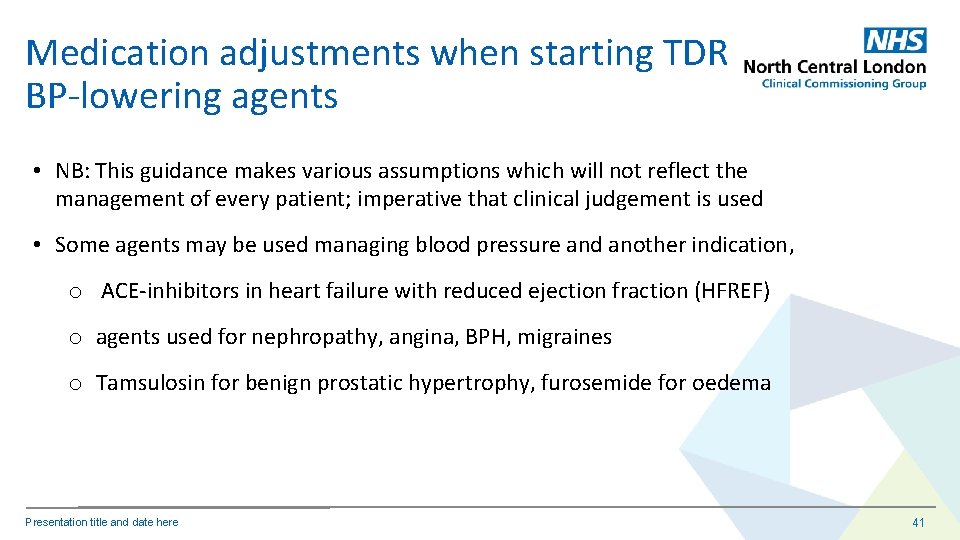
Medication adjustments when starting TDR BP-lowering agents • NB: This guidance makes various assumptions which will not reflect the management of every patient; imperative that clinical judgement is used • Some agents may be used managing blood pressure and another indication, o ACE-inhibitors in heart failure with reduced ejection fraction (HFREF) o agents used for nephropathy, angina, BPH, migraines o Tamsulosin for benign prostatic hypertrophy, furosemide for oedema Presentation title and date here 41
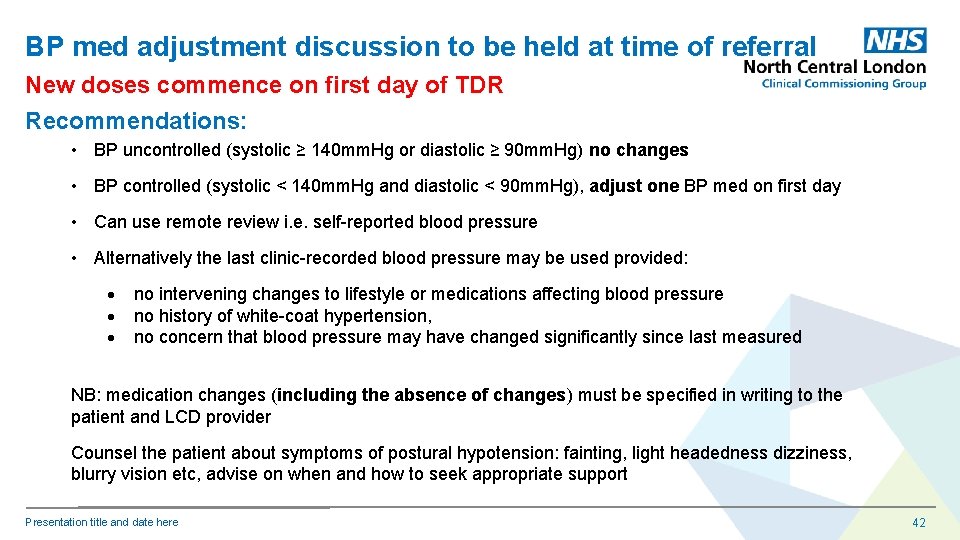
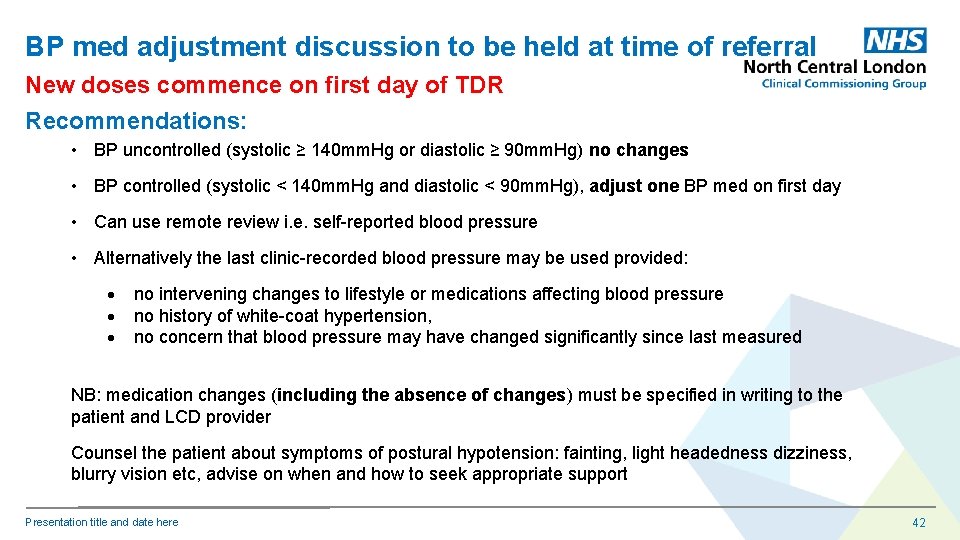
BP med adjustment discussion to be held at time of referral New doses commence on first day of TDR Recommendations: • BP uncontrolled (systolic ≥ 140 mm. Hg or diastolic ≥ 90 mm. Hg) no changes • BP controlled (systolic < 140 mm. Hg and diastolic < 90 mm. Hg), adjust one BP med on first day • Can use remote review i. e. self-reported blood pressure • Alternatively the last clinic-recorded blood pressure may be used provided: no intervening changes to lifestyle or medications affecting blood pressure no history of white-coat hypertension, no concern that blood pressure may have changed significantly since last measured NB: medication changes (including the absence of changes) must be specified in writing to the patient and LCD provider Counsel the patient about symptoms of postural hypotension: fainting, light headedness dizziness, blurry vision etc, advise on when and how to seek appropriate support Presentation title and date here 42
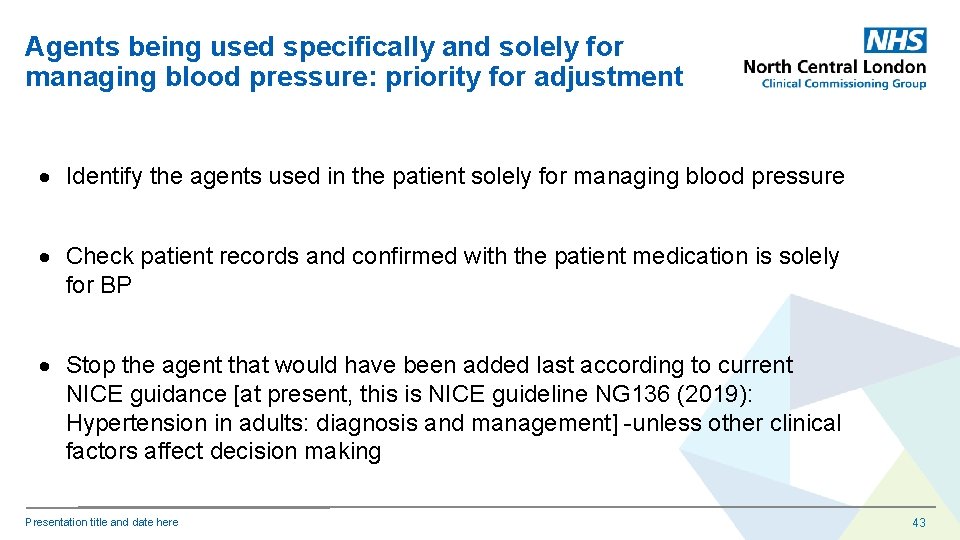
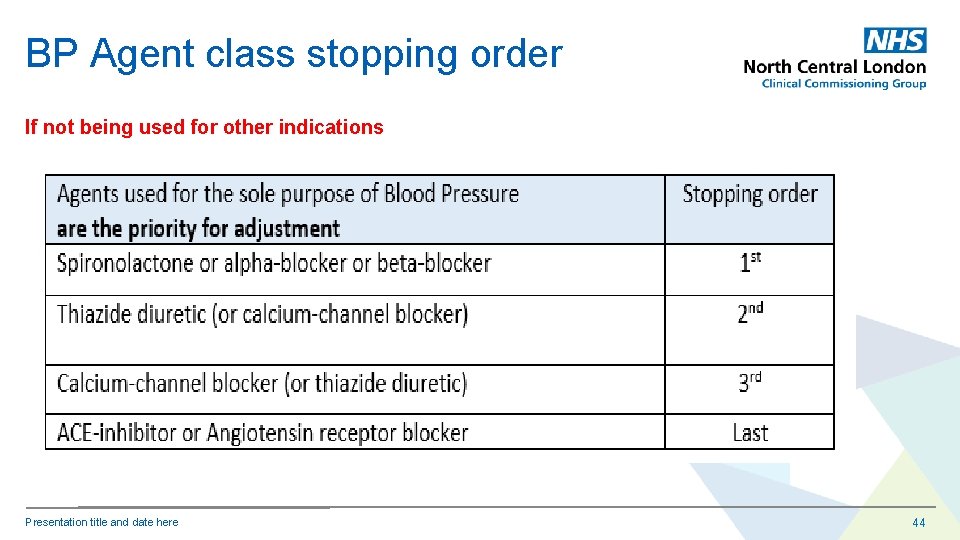
Agents being used specifically and solely for managing blood pressure: priority for adjustment Identify the agents used in the patient solely for managing blood pressure Check patient records and confirmed with the patient medication is solely for BP Stop the agent that would have been added last according to current NICE guidance [at present, this is NICE guideline NG 136 (2019): Hypertension in adults: diagnosis and management] -unless other clinical factors affect decision making Presentation title and date here 43
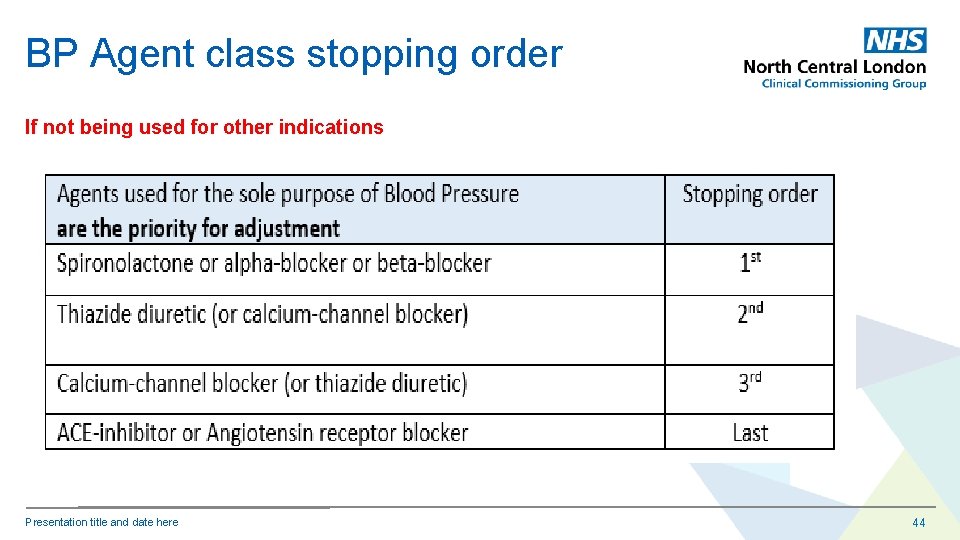
BP Agent class stopping order If not being used for other indications Presentation title and date here 44
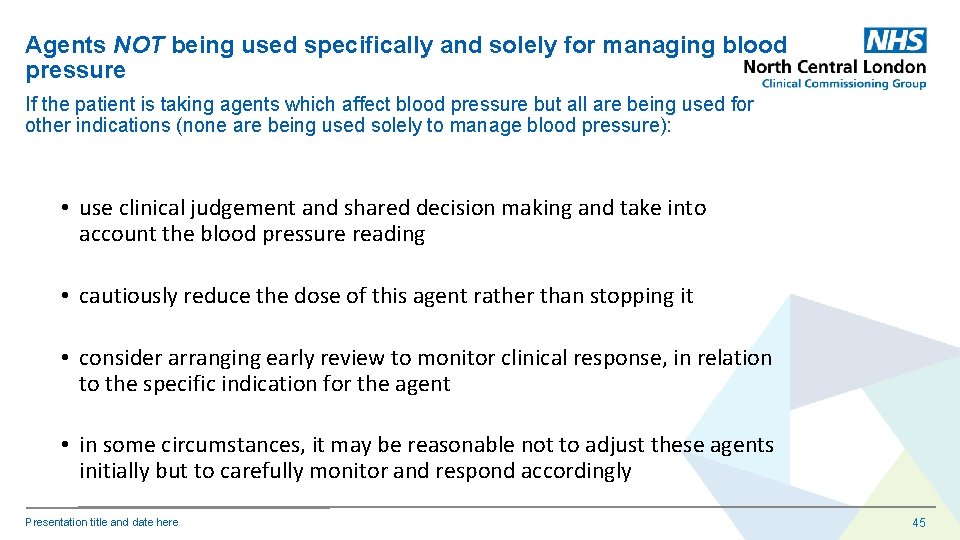
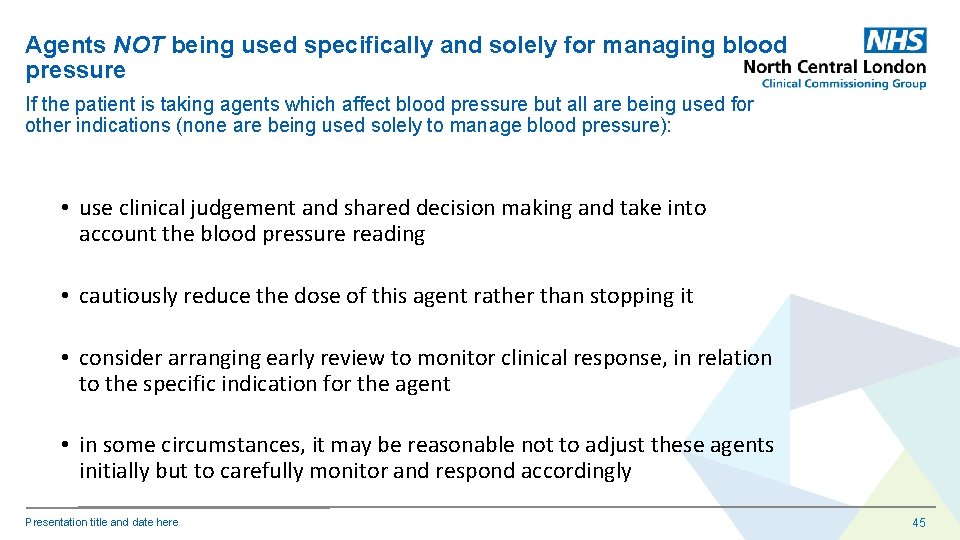
Agents NOT being used specifically and solely for managing blood pressure If the patient is taking agents which affect blood pressure but all are being used for other indications (none are being used solely to manage blood pressure): • use clinical judgement and shared decision making and take into account the blood pressure reading • cautiously reduce the dose of this agent rather than stopping it • consider arranging early review to monitor clinical response, in relation to the specific indication for the agent • in some circumstances, it may be reasonable not to adjust these agents initially but to carefully monitor and respond accordingly Presentation title and date here 45
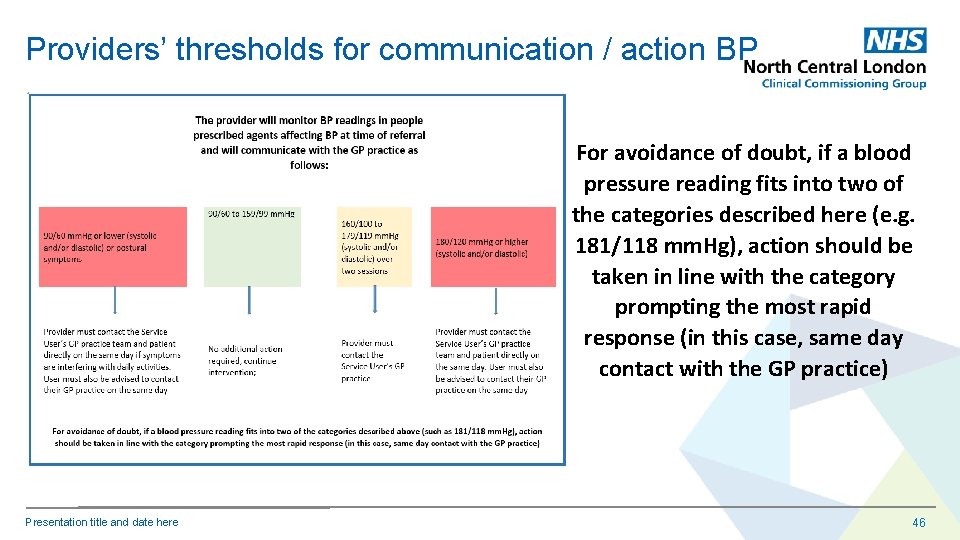
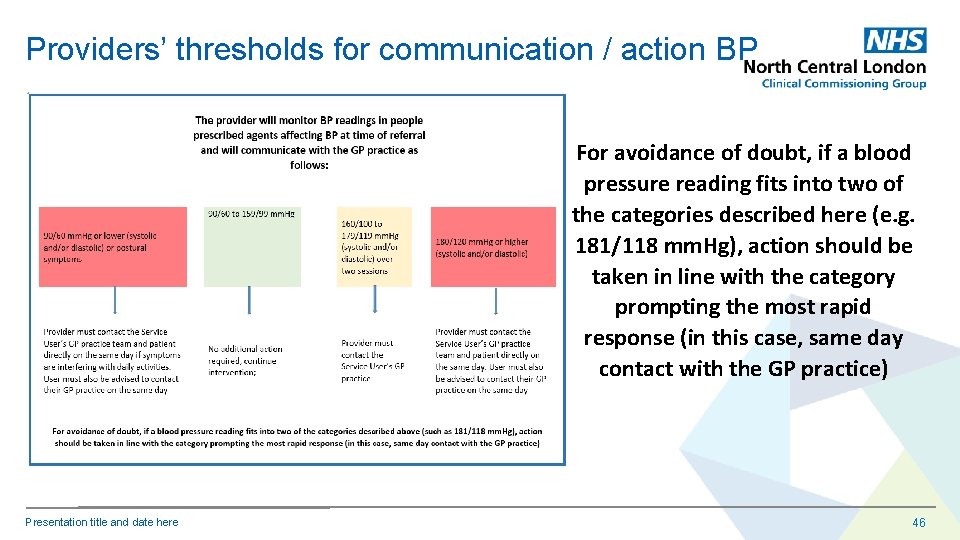
Providers’ thresholds for communication / action BP For avoidance of doubt, if a blood pressure reading fits into two of the categories described here (e. g. 181/118 mm. Hg), action should be taken in line with the category prompting the most rapid response (in this case, same day contact with the GP practice) Presentation title and date here 46
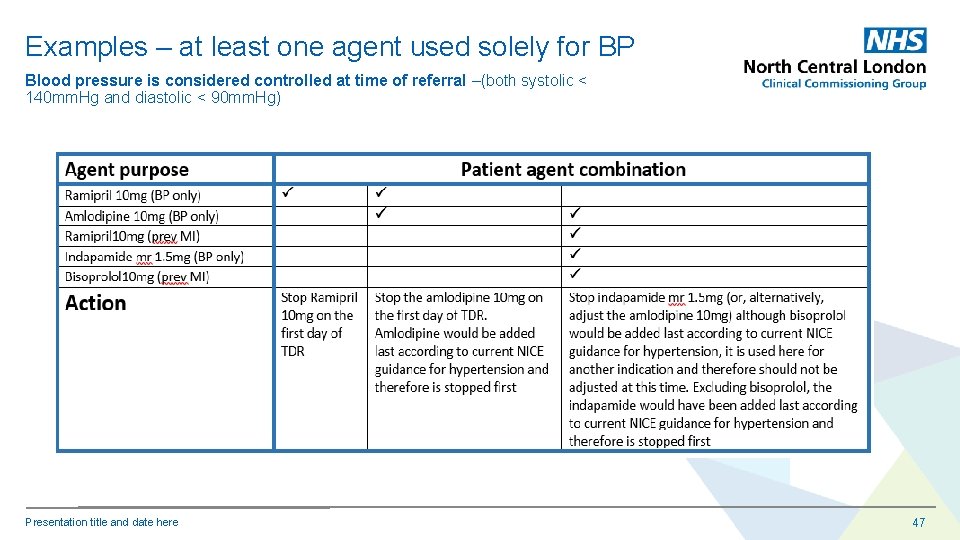
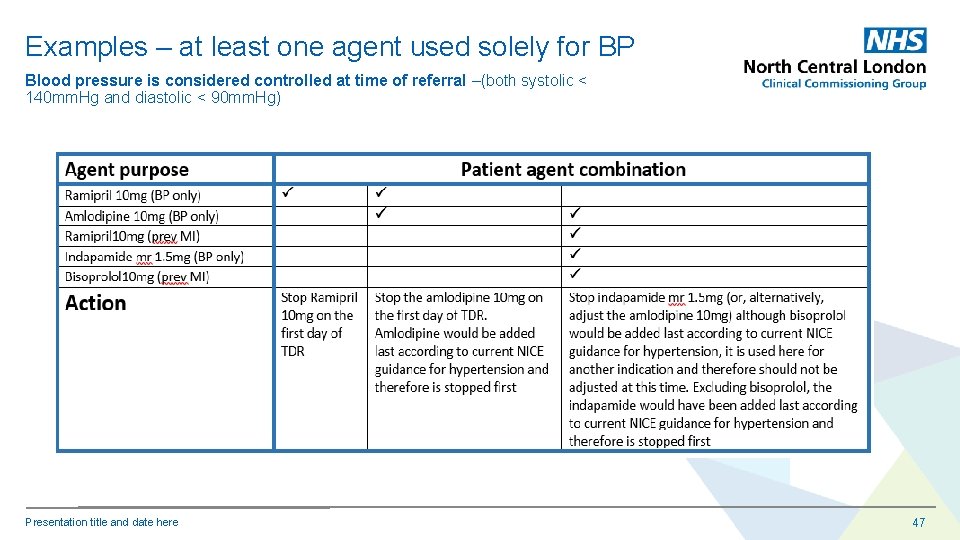
Examples – at least one agent used solely for BP Blood pressure is considered controlled at time of referral –(both systolic < 140 mm. Hg and diastolic < 90 mm. Hg) Presentation title and date here 47
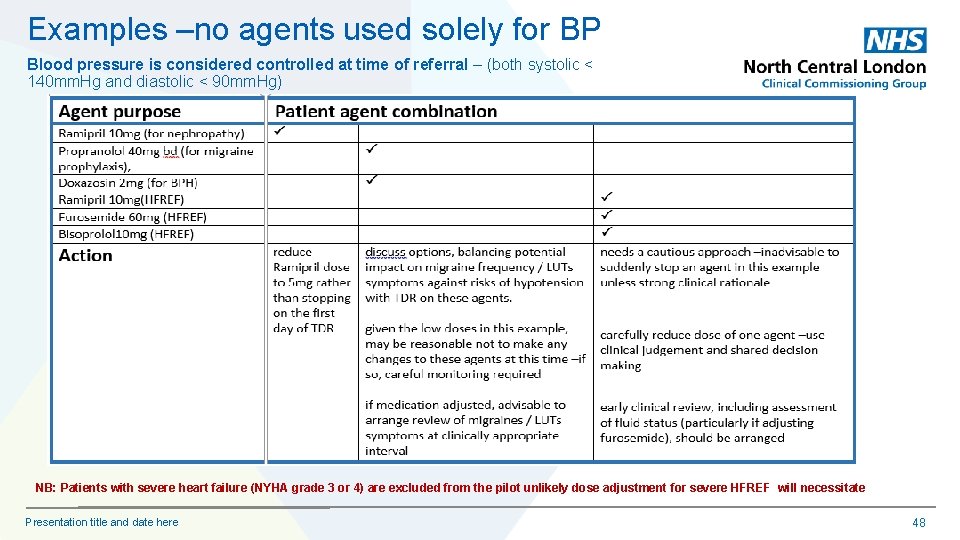
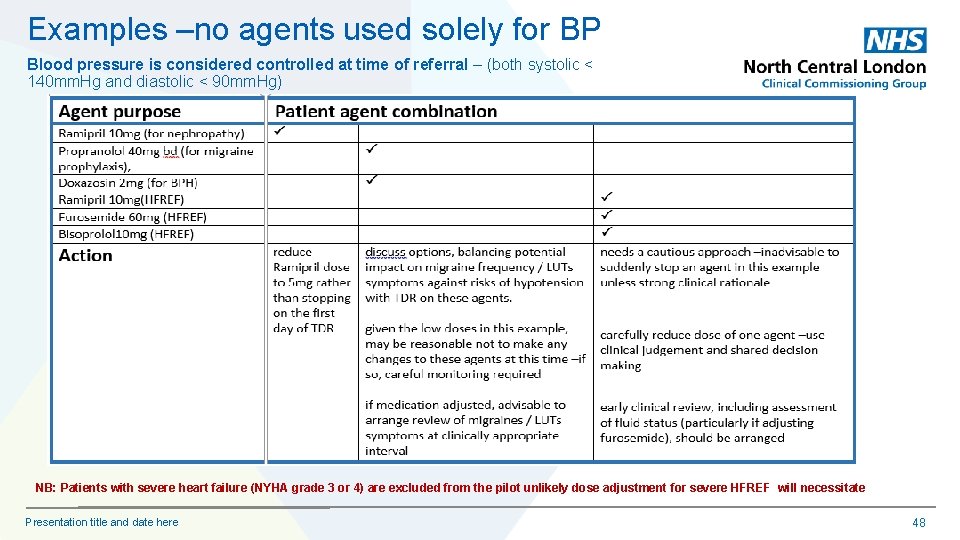
Examples –no agents used solely for BP Blood pressure is considered controlled at time of referral – (both systolic < 140 mm. Hg and diastolic < 90 mm. Hg) NB: Patients with severe heart failure (NYHA grade 3 or 4) are excluded from the pilot unlikely dose adjustment for severe HFREF will necessitate Presentation title and date here 48
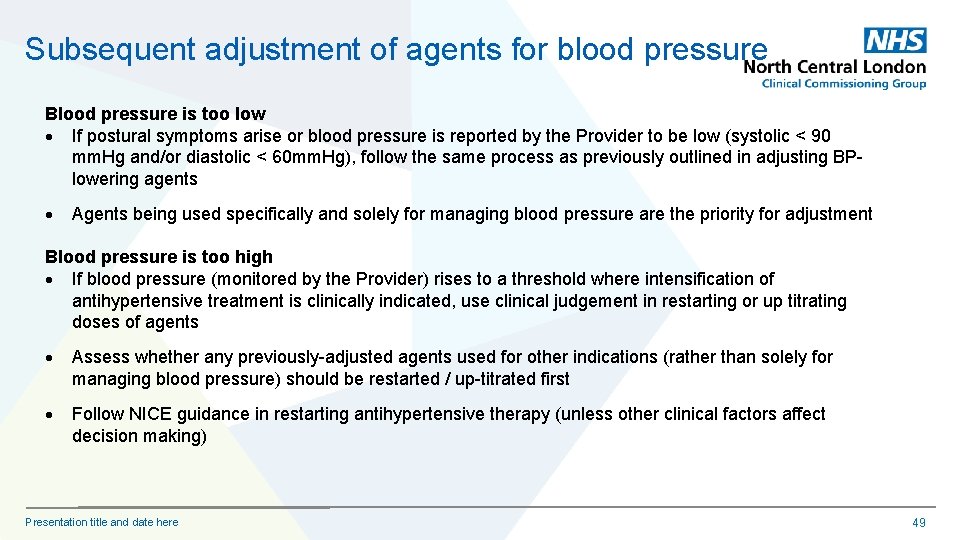
Subsequent adjustment of agents for blood pressure Blood pressure is too low If postural symptoms arise or blood pressure is reported by the Provider to be low (systolic < 90 mm. Hg and/or diastolic < 60 mm. Hg), follow the same process as previously outlined in adjusting BPlowering agents Agents being used specifically and solely for managing blood pressure are the priority for adjustment Blood pressure is too high If blood pressure (monitored by the Provider) rises to a threshold where intensification of antihypertensive treatment is clinically indicated, use clinical judgement in restarting or up titrating doses of agents Assess whether any previously-adjusted agents used for other indications (rather than solely for managing blood pressure) should be restarted / up-titrated first Follow NICE guidance in restarting antihypertensive therapy (unless other clinical factors affect decision making) Presentation title and date here 49
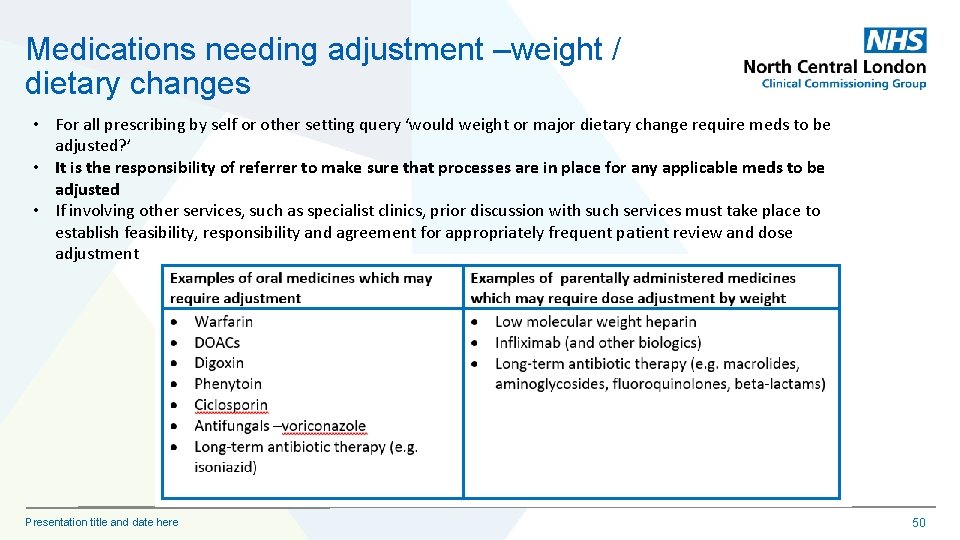
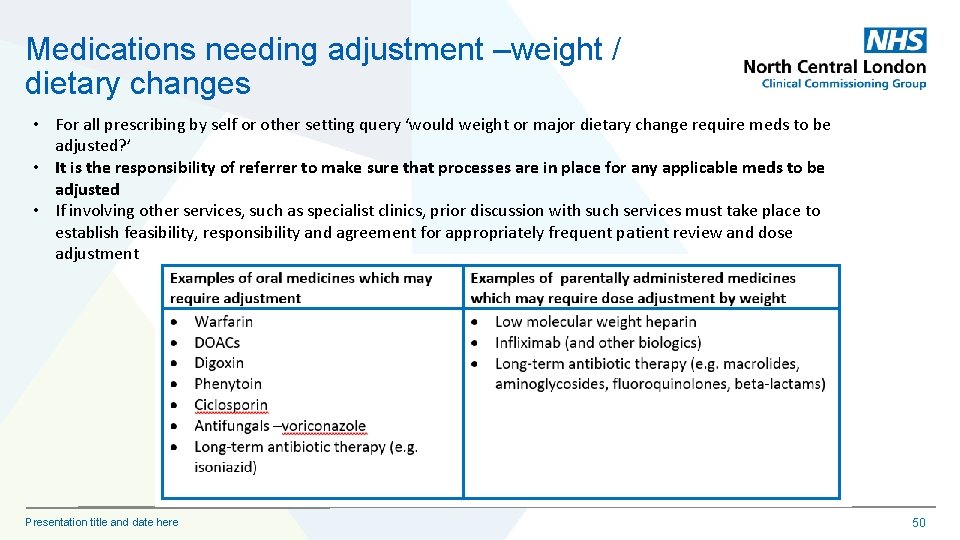
Medications needing adjustment –weight / dietary changes • For all prescribing by self or other setting query ‘would weight or major dietary change require meds to be adjusted? ’ • It is the responsibility of referrer to make sure that processes are in place for any applicable meds to be adjusted • If involving other services, such as specialist clinics, prior discussion with such services must take place to establish feasibility, responsibility and agreement for appropriately frequent patient review and dose adjustment Presentation title and date here 50
Updating the patient record Dr Karl Roberts
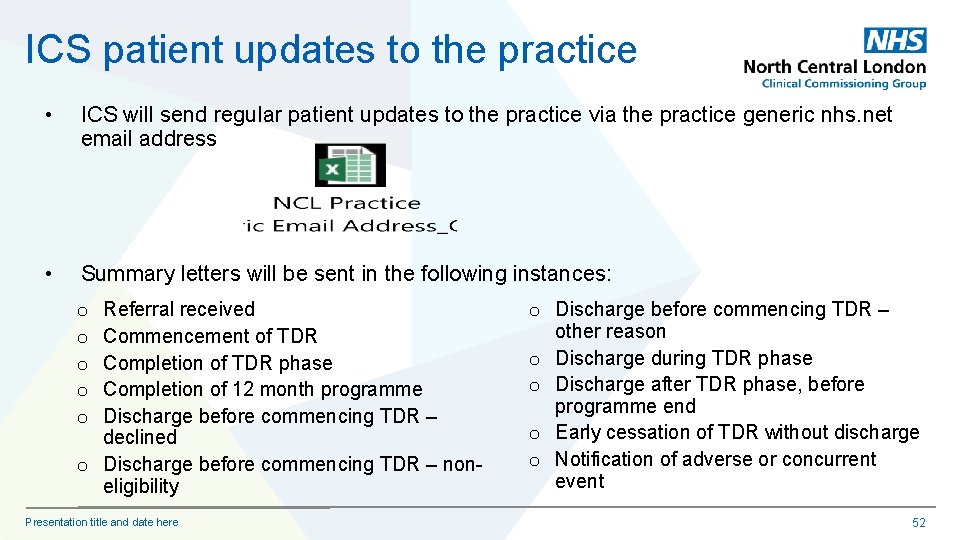
ICS patient updates to the practice • ICS will send regular patient updates to the practice via the practice generic nhs. net email address • Summary letters will be sent in the following instances: Referral received Commencement of TDR Completion of TDR phase Completion of 12 month programme Discharge before commencing TDR – declined o Discharge before commencing TDR – noneligibility o o o Presentation title and date here o Discharge before commencing TDR – other reason o Discharge during TDR phase o Discharge after TDR phase, before programme end o Early cessation of TDR without discharge o Notification of adverse or concurrent event 52
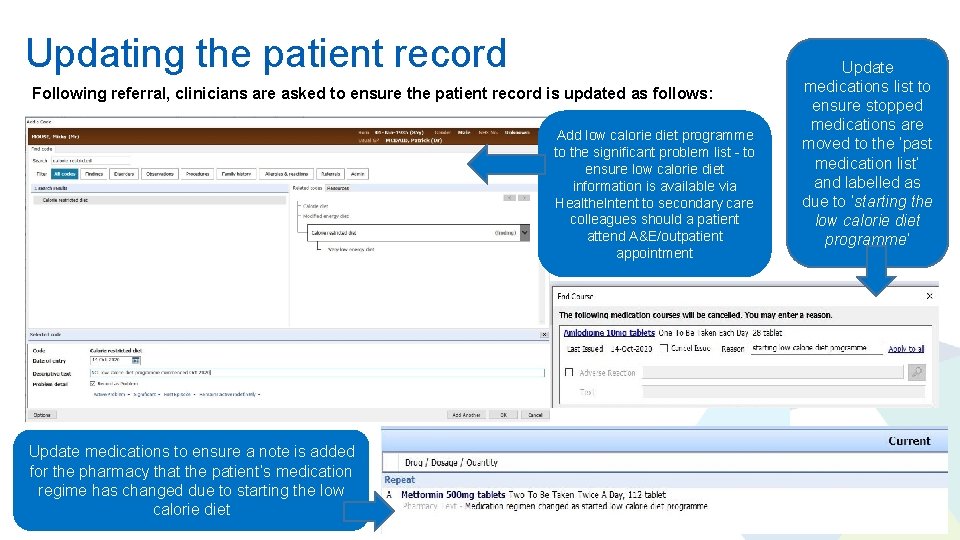
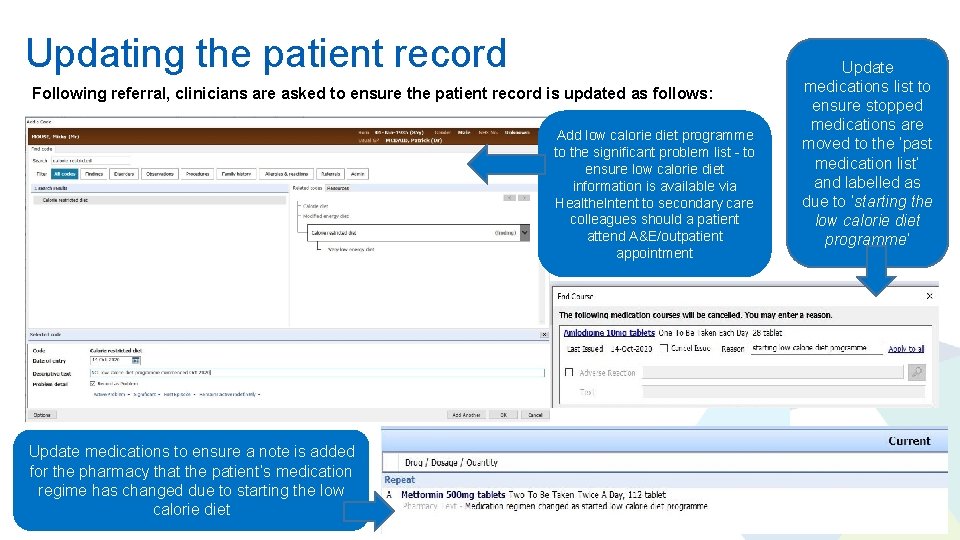
Updating the patient record Following referral, clinicians are asked to ensure the patient record is updated as follows: Add low calorie diet programme to the significant problem list - to ensure low calorie diet information is available via Healthe. Intent to secondary care colleagues should a patient attend A&E/outpatient appointment Update medications to ensure a note is added for the pharmacy that the patient’s medication regime has changed due to starting the low calorie diet Update medications list to ensure stopped medications are moved to the ‘past medication list’ and labelled as due to ‘starting the low calorie diet programme’ 53
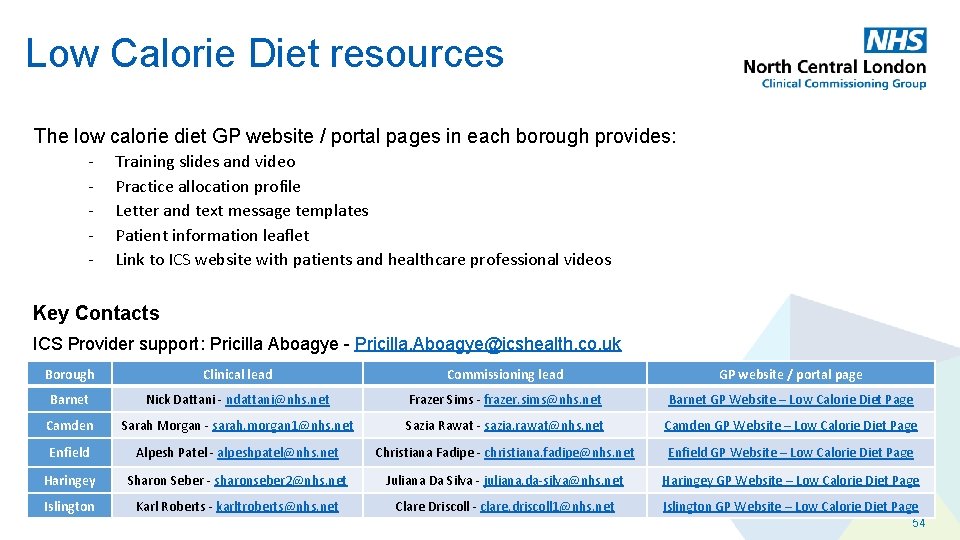
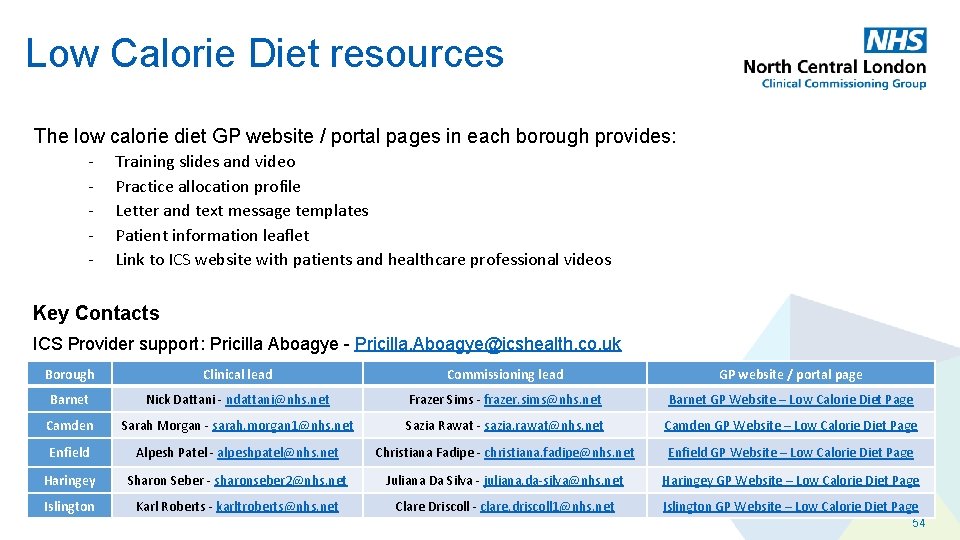
Low Calorie Diet resources The low calorie diet GP website / portal pages in each borough provides: - Training slides and video Practice allocation profile Letter and text message templates Patient information leaflet Link to ICS website with patients and healthcare professional videos Key Contacts ICS Provider support: Pricilla Aboagye - Pricilla. Aboagye@icshealth. co. uk Borough Clinical lead Commissioning lead GP website / portal page Barnet Nick Dattani - ndattani@nhs. net Frazer Sims - frazer. sims@nhs. net Barnet GP Website – Low Calorie Diet Page Camden Sarah Morgan - sarah. morgan 1@nhs. net Sazia Rawat - sazia. rawat@nhs. net Camden GP Website – Low Calorie Diet Page Enfield Alpesh Patel - alpeshpatel@nhs. net Christiana Fadipe - christiana. fadipe@nhs. net Enfield GP Website – Low Calorie Diet Page Haringey Sharon Seber - sharonseber 2@nhs. net Juliana Da Silva - juliana. da-silva@nhs. net Haringey GP Website – Low Calorie Diet Page Islington Karl Roberts - karltroberts@nhs. net Clare Driscoll - clare. driscoll 1@nhs. net Islington GP Website – Low Calorie Diet Page 54

Q&A 55
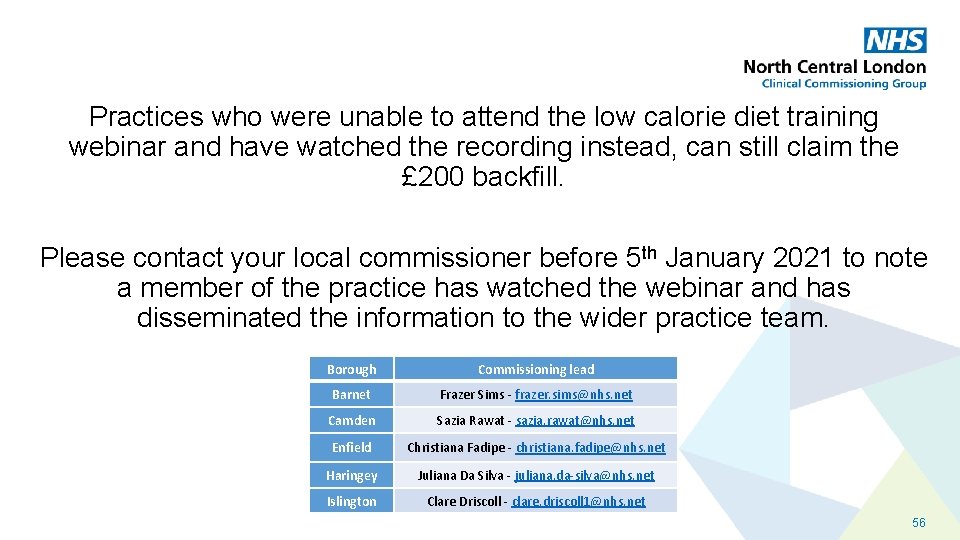
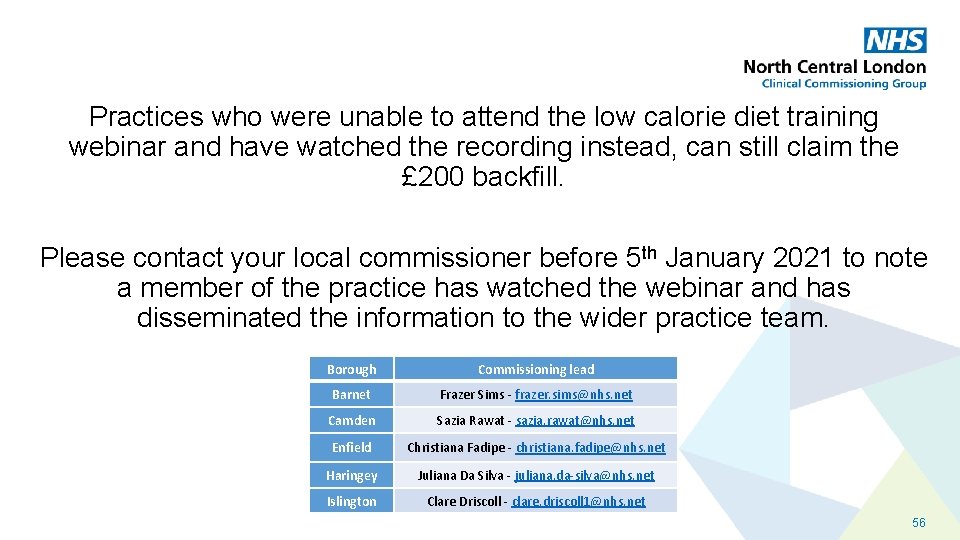
Practices who were unable to attend the low calorie diet training webinar and have watched the recording instead, can still claim the £ 200 backfill. Please contact your local commissioner before 5 th January 2021 to note a member of the practice has watched the webinar and has disseminated the information to the wider practice team. Borough Commissioning lead Barnet Frazer Sims - frazer. sims@nhs. net Camden Sazia Rawat - sazia. rawat@nhs. net Enfield Christiana Fadipe - christiana. fadipe@nhs. net Haringey Juliana Da Silva - juliana. da-silva@nhs. net Islington Clare Driscoll - clare. driscoll 1@nhs. net 56