MYCOPLASMA and Ureaplasma Dr R K Kalyan Associate


- Slides: 41
MYCOPLASMA and Ureaplasma Dr. R. K. Kalyan Associate Professor Microbiology Dept. KGMU
MYCOPLASMA ¬ Smallest free-living micro organisms, lack cell wall. ¬ Size varies from spherical shape(125250 nm to longer branching filaments 5001000 nm in size. Many can pass through a bacterial filter. ¬ 1 st member of this group – isolated by Nocard & Roux (1898) – caused bovine pleuropneumonia. ¬ Later, many similar isolates were obtained from animals, human beings, plants & environmental sources – called as “pleuropneumonia like organisms”(PPLO).
MYCOPLASMA ¬ Eaton (1944) first isolated the causative agent of the disease in hamsters and cotton rates. ¬ Also known as Eaton agent. ¬ 1956 - PPLO replaced by Mycoplasma. – Myco : fungus like branching filaments – Plasma : plasticity ¬ highly pleomorphic – no fixed shape or size - Lack cell wall.
Morphology and Physiology ¬ Small genome size (M. pneumoniae is ~800 Kbp) – Require complex media for growth ¬ Facultative anaerobes – Except M. pneumoniae - strict aerobe • No cell wall means these are resistant to penicillins, cephalosporins and vancomycin, etc. • Grow slowly by binary fission ¬ Doubling time can be as long as 16 hours, extended incubation needed
Morphology and Physiology cont’ • Require complex media for growth, including sterols • Major antigenic determinants are glycolipids and proteins, some cross reaction with human tissues. • Requirements for growth allow one to differentiate between species
Morphology and Physiology cont’ • M. pneumoniae - glucose • M. hominis - arginine • U. urealyticum - urea (buffered media due to growth inhibition by alkaline media) • M. genitalium - difficult to culture
Mycoplasmas of Humans ¬ 1. 2. 3. ¬ Parasitic Established pathogens: M. pneumoniae Presumed pathogens: M. hominis, U. urealyticum Non pathogenic: M. orale, M. buccale, M. genitalium, M. fermentans Saprophytic – present mainly on skin & in mouth.
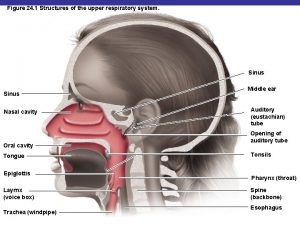
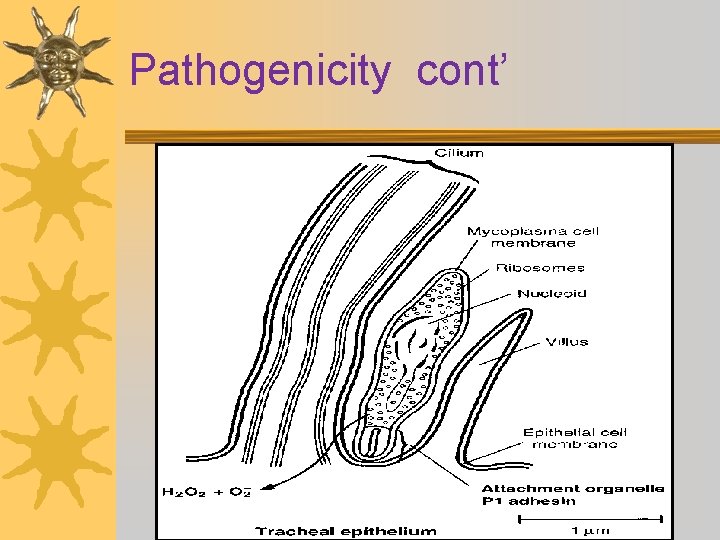
Pathogenicity ¬ Produce surface infections – adhere to the mucosa of respiratory, gastrointestinal & genitourinary tracts with the help of adhesin. ¬ 1. 2. Two types of diseases: Atypical Pneumonia Genital infections
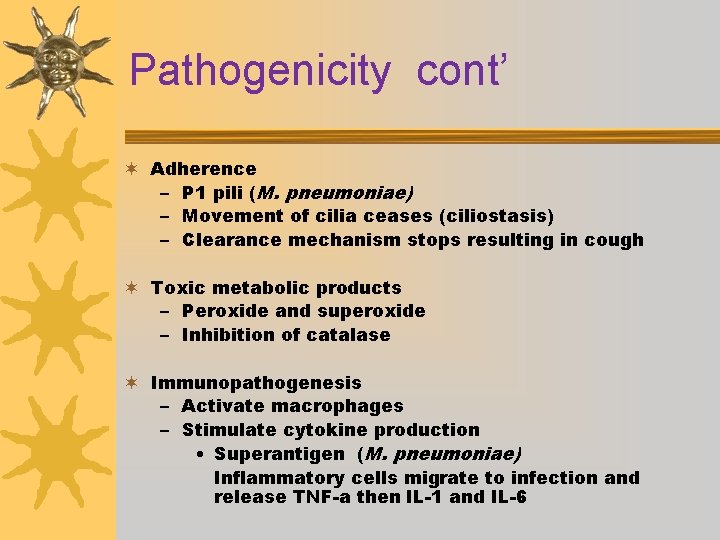
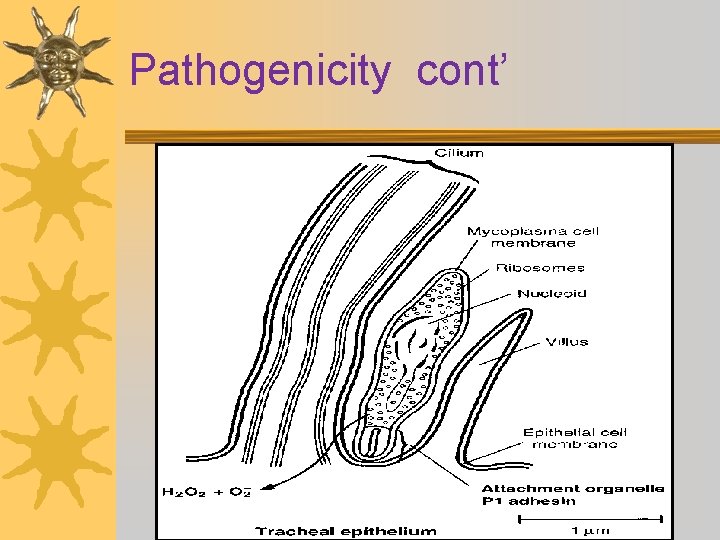
Pathogenicity cont’ ¬ Adherence – P 1 pili (M. pneumoniae) – Movement of cilia ceases (ciliostasis) – Clearance mechanism stops resulting in cough ¬ Toxic metabolic products – Peroxide and superoxide – Inhibition of catalase ¬ Immunopathogenesis – Activate macrophages – Stimulate cytokine production • Superantigen (M. pneumoniae) Inflammatory cells migrate to infection and release TNF-a then IL-1 and IL-6
Pathogenicity cont’
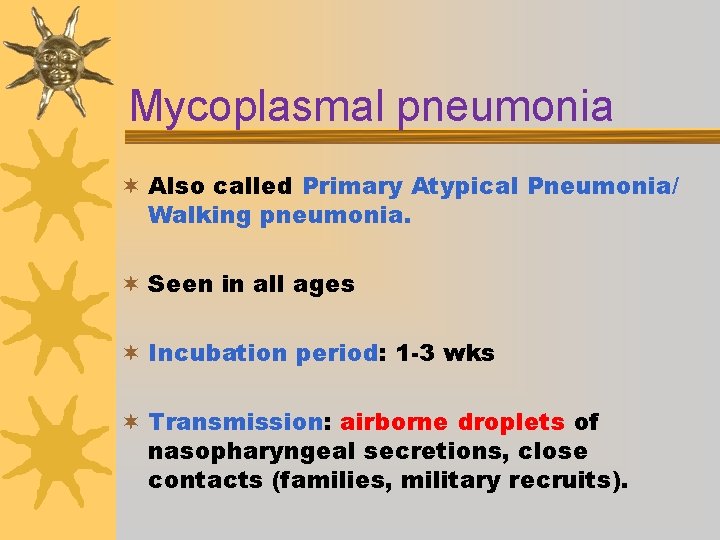
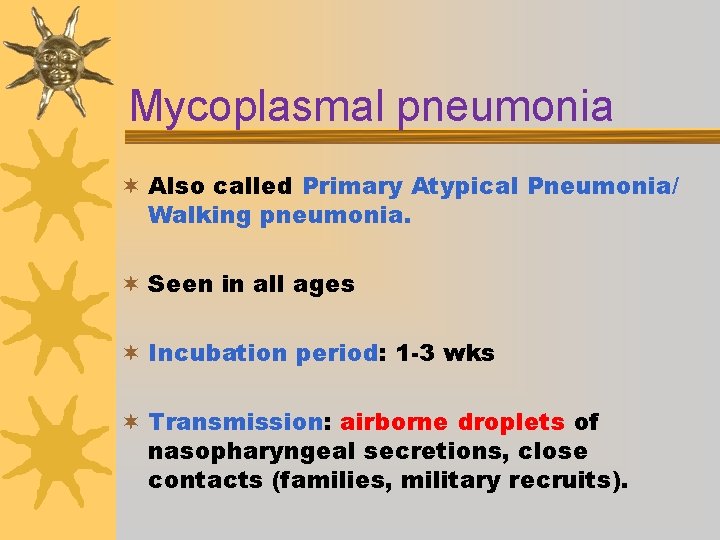
Mycoplasmal pneumonia ¬ Also called Primary Atypical Pneumonia/ Walking pneumonia. ¬ Seen in all ages ¬ Incubation period: 1 -3 wks ¬ Transmission: airborne droplets of nasopharyngeal secretions, close contacts (families, military recruits).
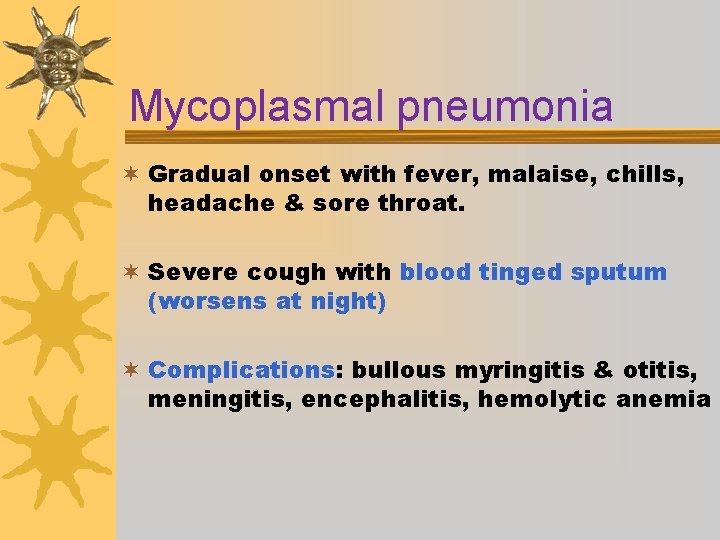
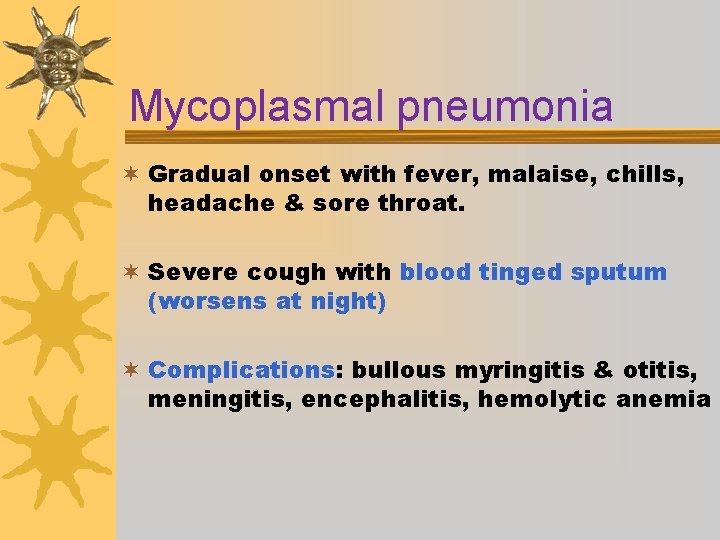
Mycoplasmal pneumonia ¬ Gradual onset with fever, malaise, chills, headache & sore throat. ¬ Severe cough with blood tinged sputum (worsens at night) ¬ Complications: bullous myringitis & otitis, meningitis, encephalitis, hemolytic anemia
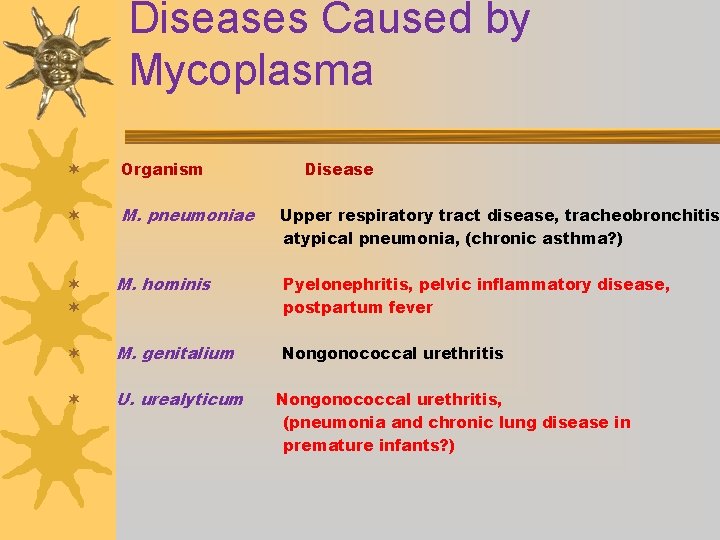
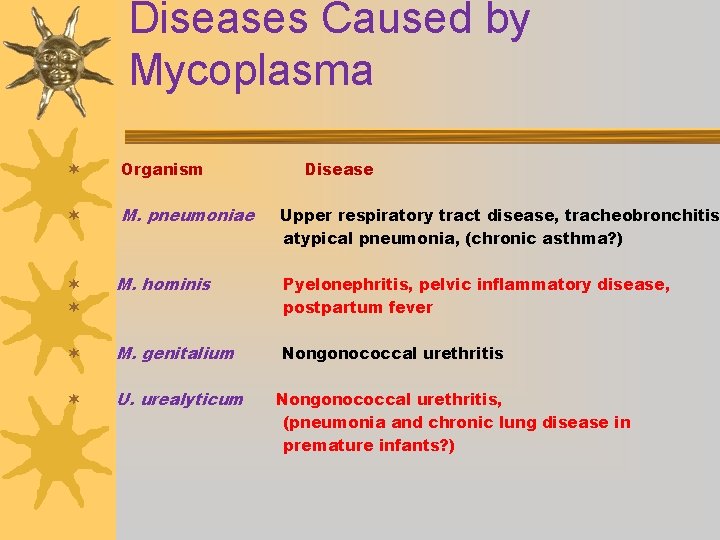
Diseases Caused by Mycoplasma ¬ Organism ¬ M. pneumoniae Disease Upper respiratory tract disease, tracheobronchitis atypical pneumonia, (chronic asthma? ) ¬ ¬ M. hominis Pyelonephritis, pelvic inflammatory disease, postpartum fever ¬ M. genitalium Nongonococcal urethritis ¬ U. urealyticum Nongonococcal urethritis, (pneumonia and chronic lung disease in premature infants? )
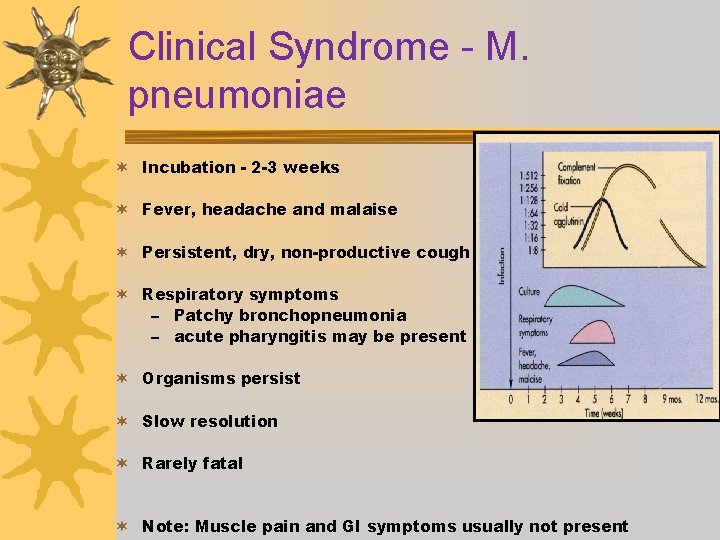
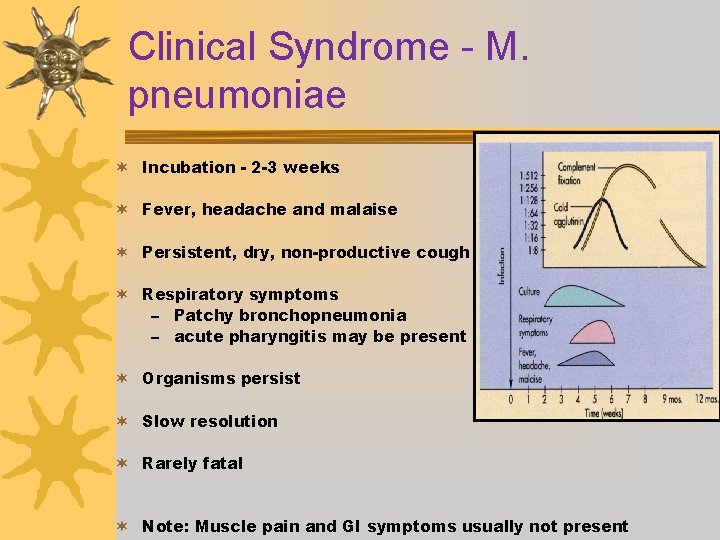
Clinical Syndrome - M. pneumoniae ¬ Incubation - 2 -3 weeks ¬ Fever, headache and malaise ¬ Persistent, dry, non-productive cough ¬ Respiratory symptoms – Patchy bronchopneumonia – acute pharyngitis may be present ¬ Organisms persist ¬ Slow resolution ¬ Rarely fatal ¬ Note: Muscle pain and GI symptoms usually not present
Epidemiology - M. pneumoniae ¬ Occurs worldwide ¬ No seasonal variation – Proportionally higher in summer and fall ¬ Epidemics occur every 4 -8 year ¬ Spread by aerosol route (Confined populations). ¬ Disease of the young (5 -20 years), although all ages are at risk
Laboratory Diagnosis - M. pneumoniae ¬ Microscopy – Difficult to stain – This process can help eliminate other organisms ¬ Culture (definitive diagnosis) – Sputum (usually scant) or throat washings – Special transport medium needed • Must suspect M. pneumoniae – May take 2 -3 weeks or longer, 6 hour doubling time with glucose and p. H indicator included – Incubation with antisera to look for inhibition.
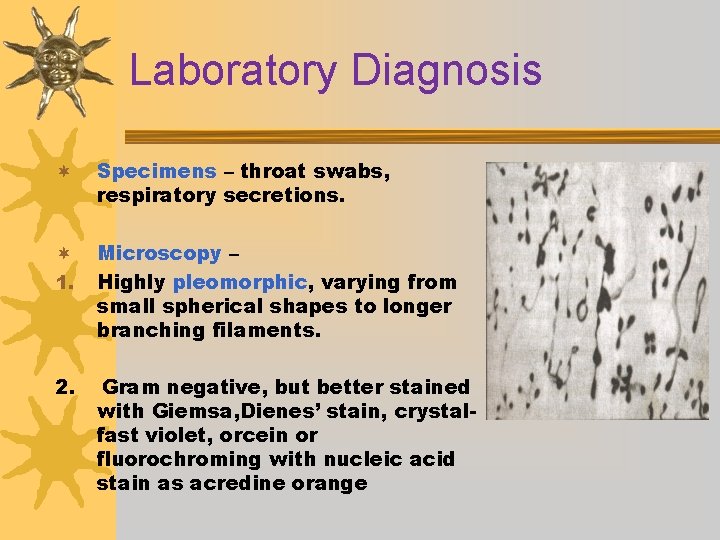
Laboratory Diagnosis ¬ Specimens – throat swabs, respiratory secretions. ¬ 1. Microscopy – Highly pleomorphic, varying from small spherical shapes to longer branching filaments. 2. Gram negative, but better stained with Giemsa, Dienes’ stain, crystalfast violet, orcein or fluorochroming with nucleic acid stain as acredine orange
Laboratory Diagnosis ¬ Isolation of Mycoplasma (Culture) – 1. Semi solid enriched medium containing 20% horse or human serum, yeast extract & DNA. Penicillium & Thallium acetate are selective agents. (serum – source of cholesterol & other lipids) 2. Incubate aerobically for 7 -12 days with 5– 10% CO 2 at 35 -37°C. (temp range 22 - 41°C, parasites 35 - 37°C, saprophytes – lower temp)
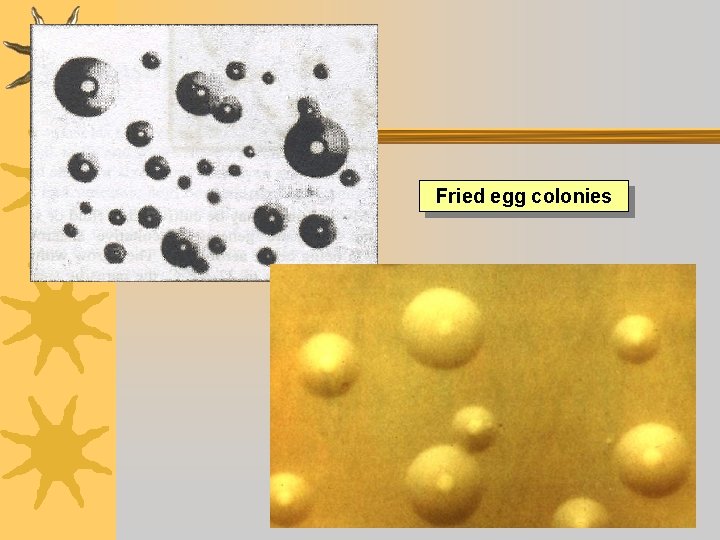
Laboratory Diagnosis 3. Typical “fried egg” appearance of colonies - Central opaque granular area of growth extending into the depth of the medium, surrounded by a flat, translucent peripheral zone. 4. Colonies best seen with a hand lens after staining with Diene’s method. 5. Produce beta hemolytic colonies, can agglutinate guinea pig erythrocytes.
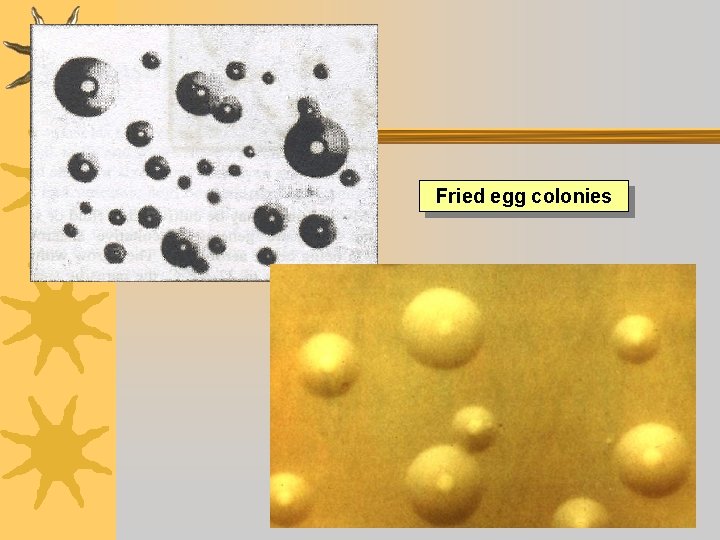
Fried egg colonies Dr Ekta, Microbiology, GMCA
Except for M. pneumoniae colonies which have a granular appearance, described as being mulberry shaped
Identification of Isolates ¬ Growth Inhibition Test – inhibition of growth around discs impregnated with specific antisera. ¬ Immunofluorescence on colonies transferred to glass slides. ¬ Molecular diagnosis – PCR-based tests are being developed and these are expected to be the diagnostic test of choice in the future. – These should have good sensitivity and be specific
Identification of Isolates ¬ Serological diagnosis 1. Specific tests – IF, HAI 2. Non specific serological tests – cold agglutination tests (Abs agglutinate human group O red cells at low temperature, 4 C). 1: 32 titer or above is significant.
Ureaplasma urealyticum ¬ Strains of mycoplasma isolated from the urogenital tract of human beings & animals. ¬ Form very tiny colonies - hence called T strain or T form of mycoplasmas. ¬ Hydrolyzes urea
Genital Infections ¬ Caused by M. hominis & U. urealyticum ¬ Transmitted by sexual contact ¬ Men - Nonspecific urethritis, proctitis, balanoposthitis & Reiter’s syndrome ¬ Women – acute salpingitis, PID, cervicitis, vaginitis ¬ Also associated with infertility, abortion, postpartum fever, chorioamnionitis & low birth weight infants
Mycoplasma & HIV infection ¬ Severe & prolonged infections in HIV infected & other immunodeficient individuals
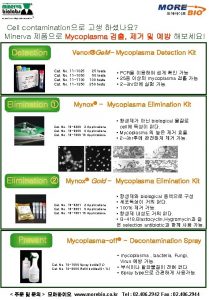
Mycoplasma as cell culture contaminants ¬ Contaminates continuous cell cultures maintained in laboratories ¬ Interferes with the growth of viruses in these cultures. ¬ Mistaken for viruses. ¬ Eradication from infected cells is difficult.
Treatment and Prevention M. pneumoniae ¬ Treatment – Tetracycline in adults (doxycycline) or erythromycin (children) • Newer fluoroquinolones (in adults) – Resistant to cell wall synthesis inhibitors. ¬ Prevention – Avoid close contact – Isolation is not practical due to length of illness – No vaccine, although attempted
Treatment ¬ Tetracycline, Erythromycin & Clarithromycin – drug of choice ¬ Resistant to antibiotics which interfere with bacterial cell wall synthesis. ¬ Newer macrolides & quinolones being used now.
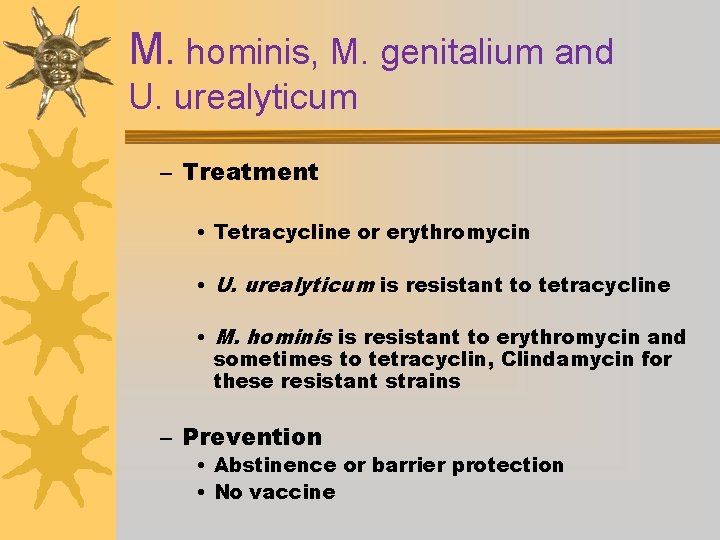
M. hominis, M. genitalium and U. urealyticum – Treatment • Tetracycline or erythromycin • U. urealyticum is resistant to tetracycline • M. hominis is resistant to erythromycin and sometimes to tetracyclin, Clindamycin for these resistant strains – Prevention • Abstinence or barrier protection • No vaccine
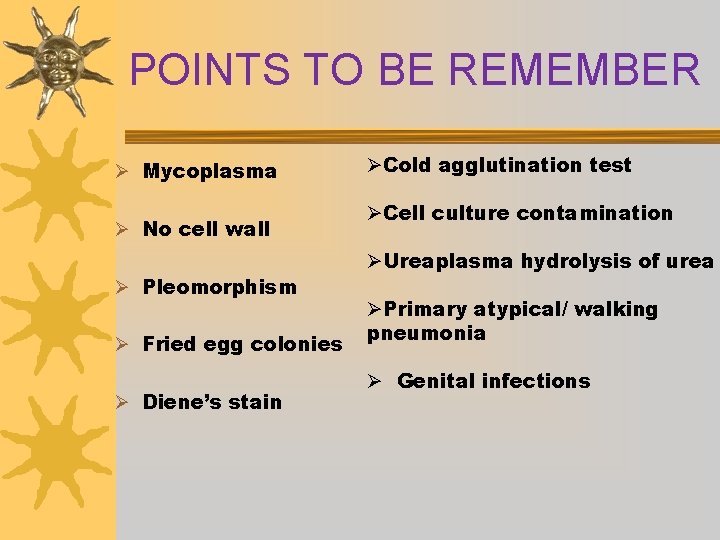
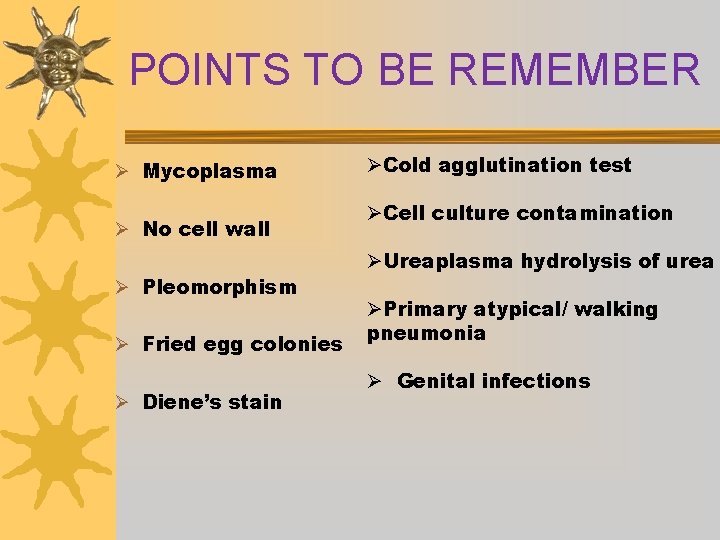
POINTS TO BE REMEMBER Ø Mycoplasma Ø No cell wall Ø Pleomorphism Ø Fried egg colonies Ø Diene’s stain ØCold agglutination test ØCell culture contamination ØUreaplasma hydrolysis of urea ØPrimary atypical/ walking pneumonia Ø Genital infections

Dienes stain ¬ Azure II ¬ Methylene blue ¬ Maltose ¬ Na 2 co 3 ¬ Benzoic acid ¬ DW
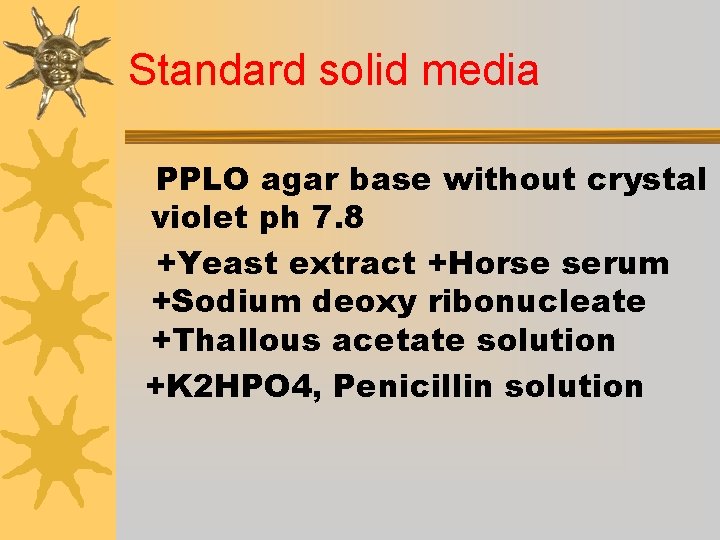
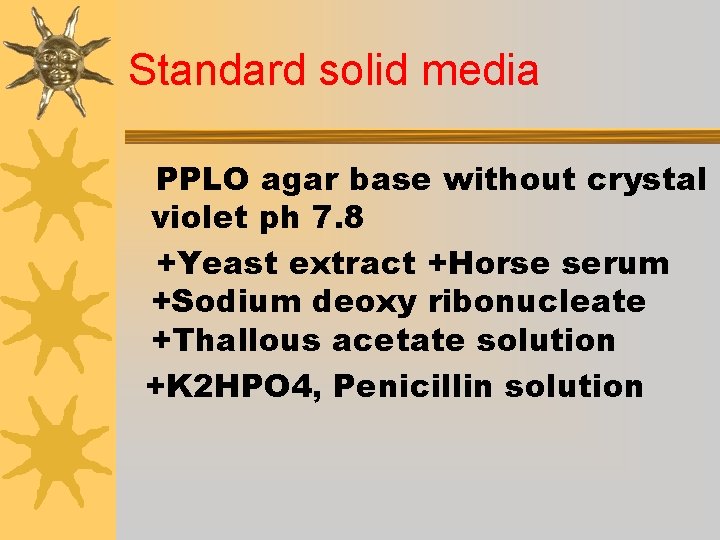
Standard solid media PPLO agar base without crystal violet ph 7. 8 +Yeast extract +Horse serum +Sodium deoxy ribonucleate +Thallous acetate solution +K 2 HPO 4, Penicillin solution
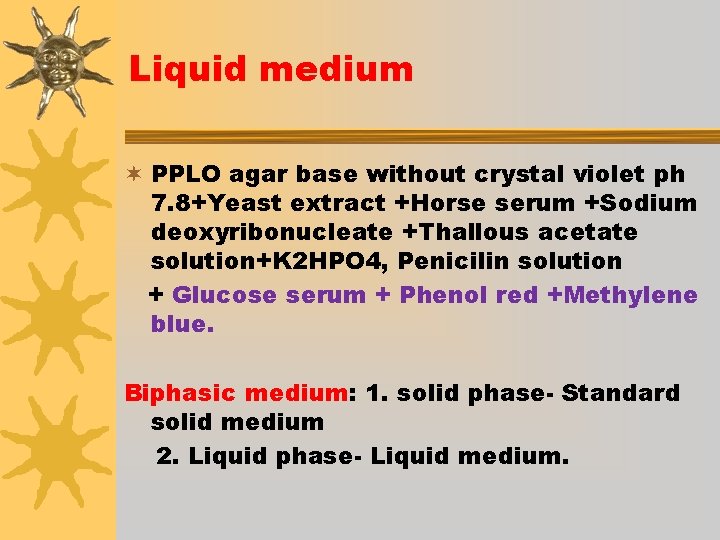
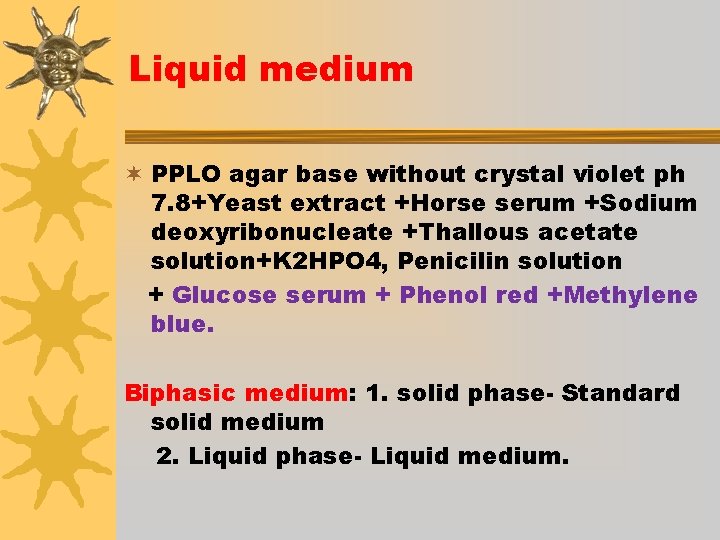
Liquid medium ¬ PPLO agar base without crystal violet ph 7. 8+Yeast extract +Horse serum +Sodium deoxyribonucleate +Thallous acetate solution+K 2 HPO 4, Penicilin solution + Glucose serum + Phenol red +Methylene blue. Biphasic medium: 1. solid phase- Standard solid medium 2. Liquid phase- Liquid medium.
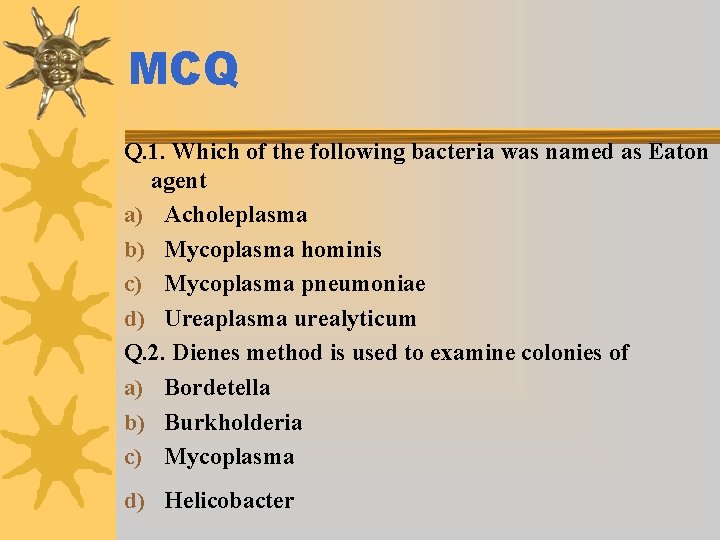
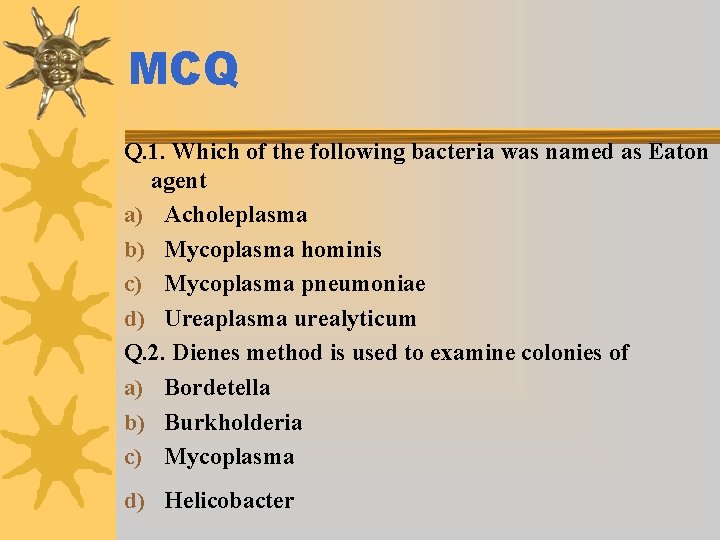
MCQ Q. 1. Which of the following bacteria was named as Eaton agent a) Acholeplasma b) Mycoplasma hominis c) Mycoplasma pneumoniae d) Ureaplasma urealyticum Q. 2. Dienes method is used to examine colonies of a) Bordetella b) Burkholderia c) Mycoplasma d) Helicobacter
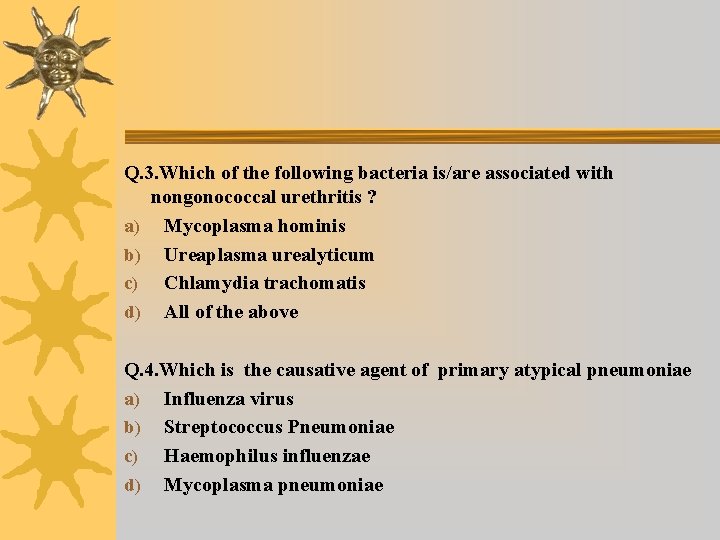
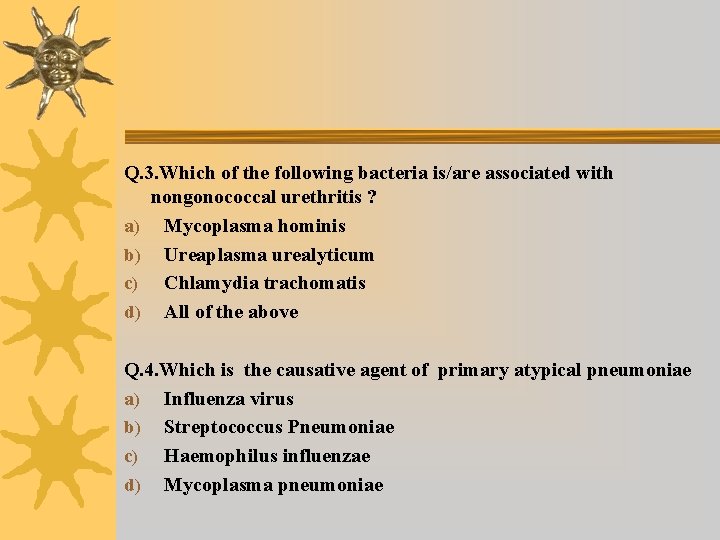
Q. 3. Which of the following bacteria is/are associated with nongonococcal urethritis ? a) Mycoplasma hominis b) Ureaplasma urealyticum c) Chlamydia trachomatis d) All of the above Q. 4. Which is the causative agent of primary atypical pneumoniae a) Influenza virus b) Streptococcus Pneumoniae c) Haemophilus influenzae d) Mycoplasma pneumoniae
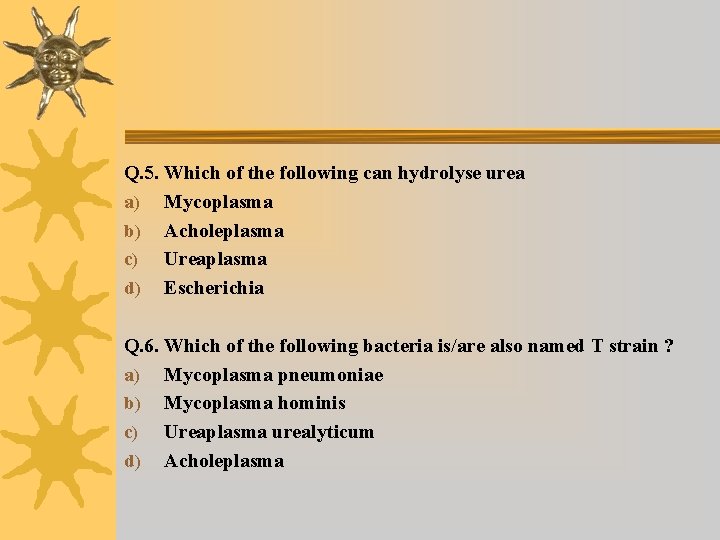
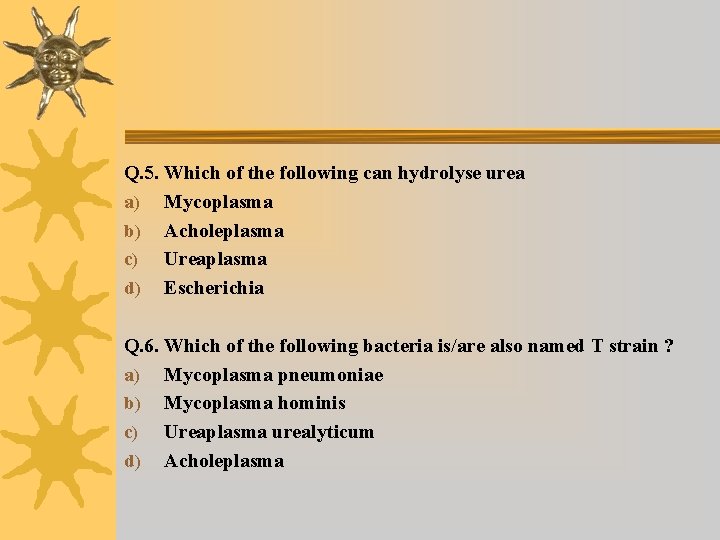
Q. 5. Which of the following can hydrolyse urea a) Mycoplasma b) Acholeplasma c) Ureaplasma d) Escherichia Q. 6. Which of the following bacteria is/are also named T strain ? a) Mycoplasma pneumoniae b) Mycoplasma hominis c) Ureaplasma urealyticum d) Acholeplasma
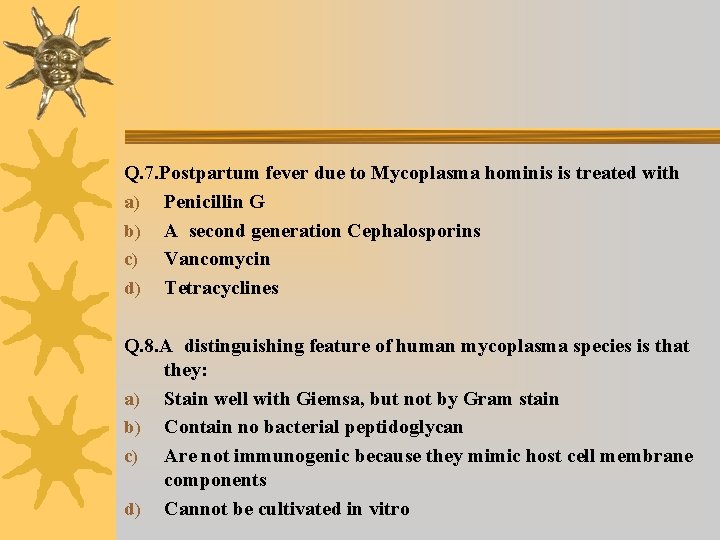
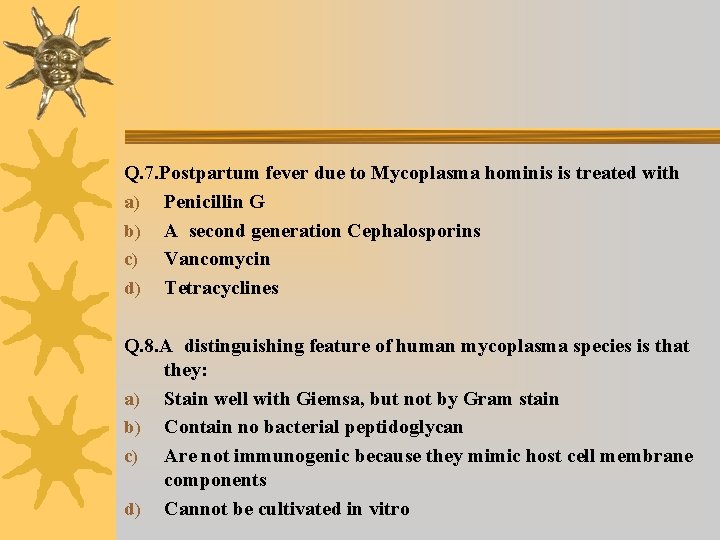
Q. 7. Postpartum fever due to Mycoplasma hominis is treated with a) Penicillin G b) A second generation Cephalosporins c) Vancomycin d) Tetracyclines Q. 8. A distinguishing feature of human mycoplasma species is that they: a) Stain well with Giemsa, but not by Gram stain b) Contain no bacterial peptidoglycan c) Are not immunogenic because they mimic host cell membrane components d) Cannot be cultivated in vitro
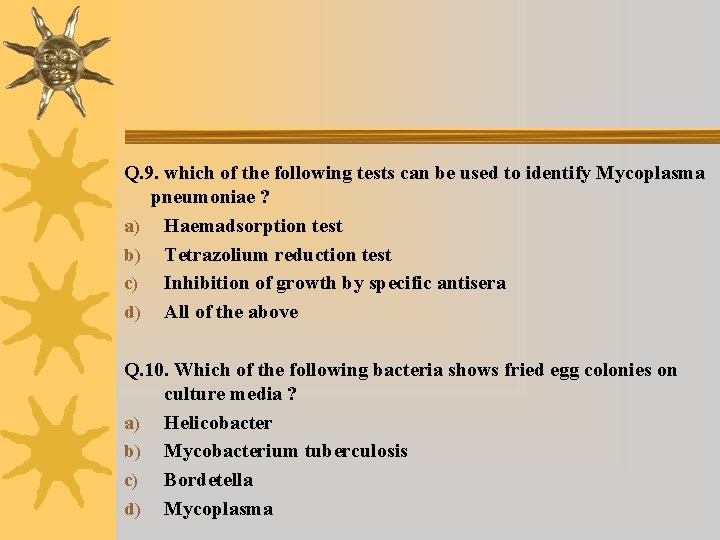
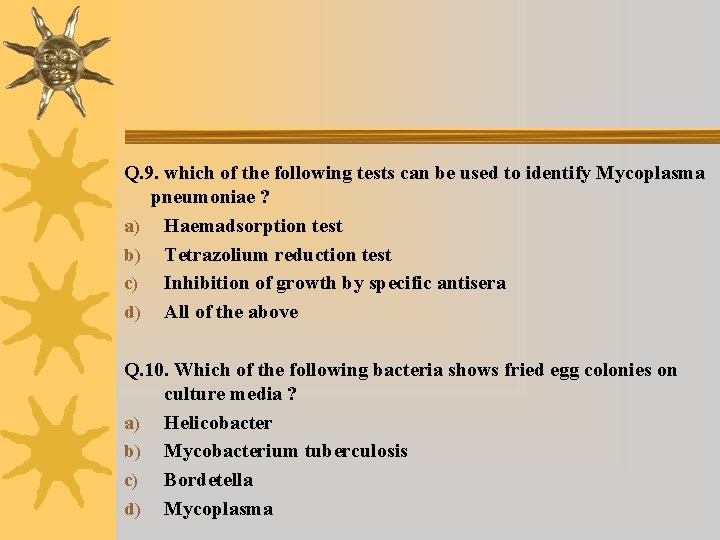
Q. 9. which of the following tests can be used to identify Mycoplasma pneumoniae ? a) Haemadsorption test b) Tetrazolium reduction test c) Inhibition of growth by specific antisera d) All of the above Q. 10. Which of the following bacteria shows fried egg colonies on culture media ? a) Helicobacter b) Mycobacterium tuberculosis c) Bordetella d) Mycoplasma
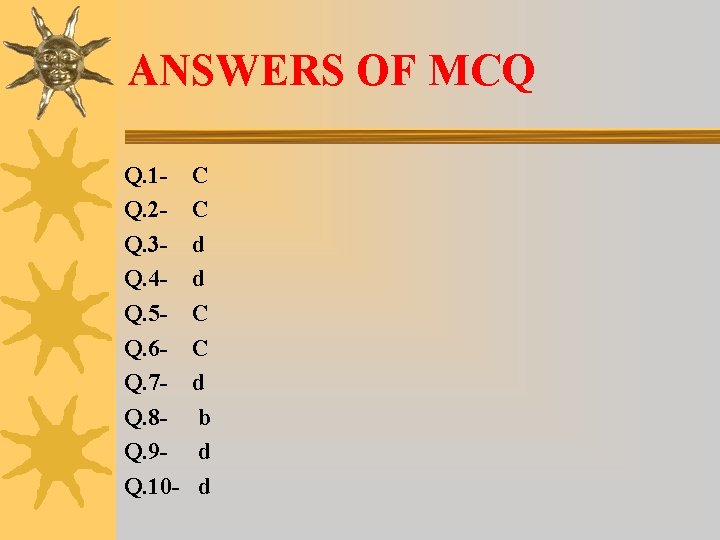
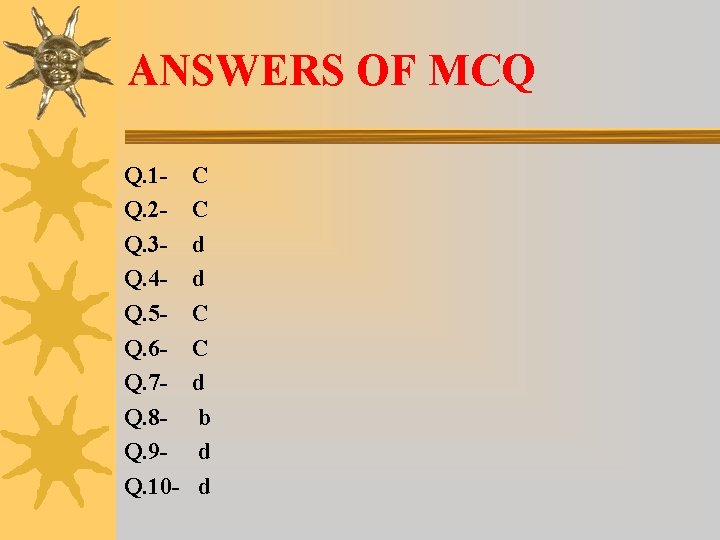
ANSWERS OF MCQ Q. 1 Q. 2 Q. 3 Q. 4 Q. 5 Q. 6 Q. 7 Q. 8 Q. 9 Q. 10 - C C d d C C d b d d

! Thanks for attention !
 Swollen lymph nodes
Swollen lymph nodes Mycoplasma pneumoniae
Mycoplasma pneumoniae Rocky mountain fever
Rocky mountain fever Migrants
Migrants Ureaplasma pozitiva
Ureaplasma pozitiva Rez. cystitiden
Rez. cystitiden Ureaplasma sintomas
Ureaplasma sintomas Kalyan kumar hcl
Kalyan kumar hcl Dhamma vahini titwala contact number
Dhamma vahini titwala contact number Krishi kalyan abhiyan phase 3
Krishi kalyan abhiyan phase 3 Nirman shramik kalyan yojana
Nirman shramik kalyan yojana Nishant samaj kalyan foundation samiti chandauli
Nishant samaj kalyan foundation samiti chandauli Bcs professional membership
Bcs professional membership Promotion from assistant to associate professor
Promotion from assistant to associate professor Tecniche associate al pensiero computazionale:
Tecniche associate al pensiero computazionale: The pyramid at chichen itza is most closely associate with
The pyramid at chichen itza is most closely associate with Lone star college nursing program requirements
Lone star college nursing program requirements Incose asep certification
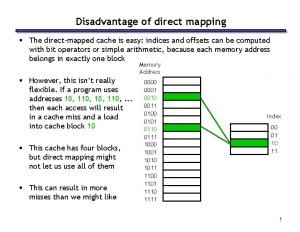
Incose asep certification Direct mapped cache
Direct mapped cache Project associate cern
Project associate cern Associate degree netherlands
Associate degree netherlands Laser alignment
Laser alignment Physician associate lecturer
Physician associate lecturer Rcog associate
Rcog associate Tio collegegeld
Tio collegegeld Associate director meaning
Associate director meaning Harper college
Harper college Iter project associate
Iter project associate Aad program
Aad program Harbor city community college
Harbor city community college Why is critical reading an active process of discovery
Why is critical reading an active process of discovery Delta chi flag
Delta chi flag Associate degree rmit
Associate degree rmit Adobe audition certification
Adobe audition certification Cincinnati state associate degrees
Cincinnati state associate degrees Safety associate
Safety associate Associate warden
Associate warden Associate degree startdag
Associate degree startdag Imeche associate membership
Imeche associate membership To associate
To associate Hea associate fellowship
Hea associate fellowship Associate consultant in capgemini
Associate consultant in capgemini