Diphtheria Pertussis and Tetanus Dr Kalyan Diphtheria Epidemiology








- Slides: 28
Diphtheria, Pertussis and Tetanus Dr Kalyan
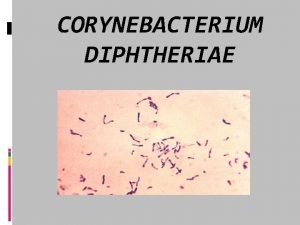
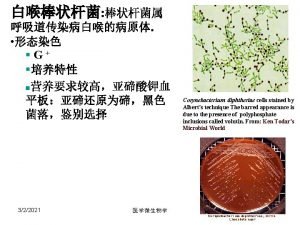
Diphtheria • Epidemiology : • Organism: Gram Positive bacillus, Corynebacterium diphtheriae. • Source of infection: Secretions and discharge from infected person or carrier. • Portal of entry: RT, Skin, Conjunctiva
Pathology • Exotoxin : A and B. • Local lesions: Pseudo-membrane formation. • Systemi Effects: CVS CNS Renal system.

Clinical features • Incubation period: 2 -5 days. • Constitutional symptoms: • Local manifestations: 1. Nasal diphtheria; 2. Faucial diphtheria: 3. Laryngotracheal diphtheria: 4. Unusual sites;
Complications • Myocarditis: End of 1 st week, abdominal pain, vomiting, dyspnea, systemic venous congestion, tachycardia, extrasystoles, thready pulse, soft mufled 1 st heart sound. • Neurological complications; palatal palsy, loss of accommodation, polyneuritis. • Renal: oliguria, proteinuria
Diagnosis • Clinical examination, • Demonstration of organism by Albert”s stain From the lesions • Isolation of organism by culture from the lesions. • Rapid diagnosis by Fluoresent antibody technique

Differential diagnosis • Nasal diphtheria – FB Nose, Congenital syphilis • Faucial diphtheria- Acute membranous tonsilitis. Moniliasis, IMN. • Laryngeal diphtheria—Croup, Acute epiglottis Retropharyngeal abscess

Treatment • Principles: • Antitoxin • Antibiotics • Supportive • Symptomatic • Management of complications
Antitoxin • • • Pharyngeal / laryngeal 20, 000 - 40, 000 U Nasopharyngeal 40, 000 – 60, 000 U Extensive disease 80, 000 - 1, 20, 000 U

Antibiotics • • Procaine penicillin: 3 - 6 lakhs IM 12 th Hrly 14 days (or) Erythromycin 25 – 30 mg/kg /day
Management of complications • Myocarditis; Restriction of fluids and salts Bed rest Diuretics. Digoxin • Respiratory obstruction : Huminified oxygen Tracheostomy • Neurological complications NG feeds Ventilator support

• Prevention: Isolation of the case Disinfection of articles Chemoprophylaxis of close contacts Erythromycin 40 -50 mg/kg /day for 7 days Benzathene penicillin 6 – 12 lakhs IM Single dose • Active Immunization
Whooping cough Pertussis • Epidemiology: Age incidence : < 4 yr Mode of infection- Droplet infection Organism: Non motile Gm Negative bacilllus- Bordetella pertussis
Clinical features • Incubation period: 7 -14 days • Clinical stage 1: Catarrhal stage: Lasts for 7 – 10 days Most infectuous period Clinical features : Cough Which become paroxysmal in the later part of this phase Coryza With little naso pharyngeal secretions
• Clinical stage 2 : Paroxysmal Phase: • Laasts for 2 - 4 weeks • Severe cough in explossive manner ending with whoop, paroxysms of cough are precipitated by cold air, food , cold liquids • Child appear choked, unable to breathe • Anxious with suffused face
• Clinical Stage 3: Convalesent phase: Lasts for 2 - 4 weeks Frequency and severity of paroxysms decreases gradually
Complications • Respiratory: Atelectasis, pneumonia, Bronchiectasis, Pneumothorax, Subcutaneous emphysema, Accentuation of dormant TB focus *Neurological: Convulsions Encephalopathy Focal intracranial Hemorrhages

• GIT; Hernia Rectal Prolapse • Hemorrhagic: Subconjuctival hemorrhage • Malnutrition
Diagnosis • TLC Elevated • Rapid diagnosis by fluoresent antibody staining • Isolation of organism in cultures
Differential diagnosis • • FB in air passages TB hilar lynphadenitis Bronchiolitis Adenovirus infection of RT
Traetment • Erythromycin 40 - 50 mg/kg/day for 14 days • Bronchodilator therapy by nebulisation • Betamethasone in life thretening states O. 75 mg/kg/day
Prevention • Active immunisation: Primary at 6. 10, 14 weeks • booster after 1 year of age.

Tetanus • Some 60% of tetanus deaths occur in neonates and children under the age of 5. • The World Health Organization has repeatedly failed to meet its deadlines for tetanus elimination and the disease remains an important global health concern. • The causative agent of tetanus, Clostridium tetani is a ubiquitous organism, present in the soil and in human and animal faeces.
• Neonatal tetanus usually arises from contamination of the umbilical stump. • Even after maternal immunization, the infant is still at risk in many countries, as malaria and HIV reduce placental transfer of protective antibody.
Clinical manifestation • Tetanus is most often generalized but may also be localized. • Incubation period -2 to 14 days • In generalized tetanus the presenting symptom in about half of cases is trismus (masseter muscle spasm, or lockjaw) • Tetanus toxin does not affect sensory nerves or cortical function, the patient unfortunately remains conscious, in extreme pain, and in fearful anticipation of the next tetanic seizure.
• Neonatal tetanus, the infantile form of generalized tetanus, typically manifests within 3 -12 days of birth. • Localized tetanus results in painful spasms of the muscles adjacent to the wound site and may precede generalized tetanus. • Results of routine laboratory studies are usually normal.

Treatment • Surgical wound excision and debridement. • Surgery should be performed promptly after administration of human tetanus immunoglobulin (TIG) and antibiotics. • Single intramuscular injection of 500 units of TIG to neutralize systemic tetanus toxin, but total doses as high as 3, 000 -6, 000 U are also recommended. • Oral (or intravenous) metronidazole (30 mg/kg/day, given at 6 hr intervals; maximum dose, 4 g/day) decreases the number of vegetative forms of C. tetani and is currently considered the antibiotic of choice. • Diazepam provides both relaxation and seizure control. • The initial dose of 0. 1 -0. 2 mg/kg every 3 -6 hr intravenously.
Thank you
 Lecture etymology
Lecture etymology Dr frank kretsinger
Dr frank kretsinger Corynebacterium
Corynebacterium Bull neck appearance
Bull neck appearance Diphtheria cdc
Diphtheria cdc Diphtheria
Diphtheria Kalyan kumar hcl
Kalyan kumar hcl Titwala vipassana center
Titwala vipassana center Krishi kalyan abhiyan phase 3
Krishi kalyan abhiyan phase 3 Nirman shramik kalyan yojana
Nirman shramik kalyan yojana Samaj kalyan foundation
Samaj kalyan foundation Neuretic
Neuretic Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Nutrition epidemiology definition
Nutrition epidemiology definition Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology How to calculate incidence rate example
How to calculate incidence rate example Cbic recertification
Cbic recertification Person place time epidemiology
Person place time epidemiology Fajar tetanua
Fajar tetanua Kepanjangan sdv paru
Kepanjangan sdv paru Muscle twitch
Muscle twitch The staircase phenomenon
The staircase phenomenon Tetanus lüge
Tetanus lüge Tetanus hondenbeet
Tetanus hondenbeet Direct phosphorylation
Direct phosphorylation Incomplete tetanus muscle contraction
Incomplete tetanus muscle contraction Charles bell tetanus
Charles bell tetanus Risus sardonicus
Risus sardonicus Tetanus hondenbeet
Tetanus hondenbeet