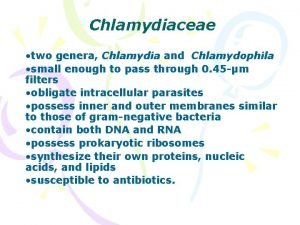
Chlamydia Mycoplasma and Rickettsia CHLAMYDIA The family Chlamydiaceae




- Slides: 17
Chlamydia Mycoplasma and Rickettsia
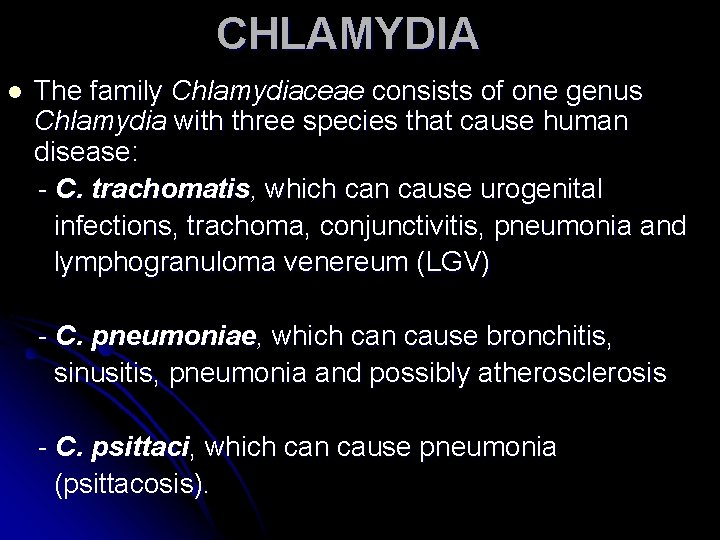
CHLAMYDIA The family Chlamydiaceae consists of one genus Chlamydia with three species that cause human disease: - C. trachomatis, which can cause urogenital infections, trachoma, conjunctivitis, pneumonia and lymphogranuloma venereum (LGV) - C. pneumoniae, which can cause bronchitis, sinusitis, pneumonia and possibly atherosclerosis - C. psittaci, which can cause pneumonia (psittacosis). l
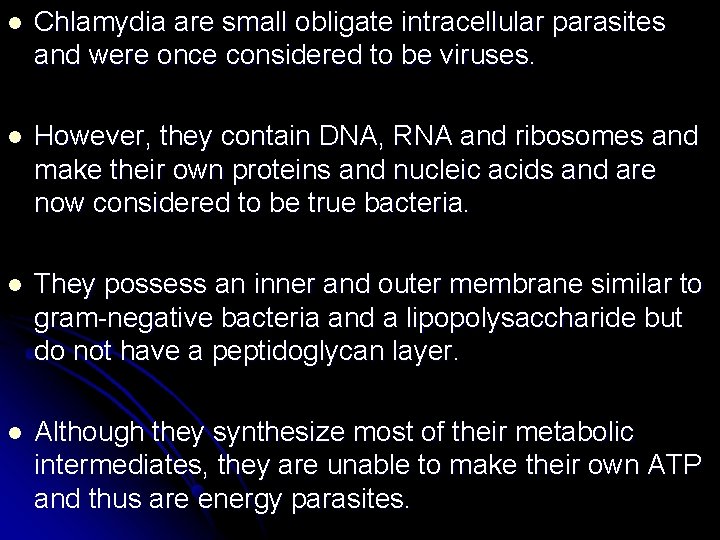
l Chlamydia are small obligate intracellular parasites and were once considered to be viruses. l However, they contain DNA, RNA and ribosomes and make their own proteins and nucleic acids and are now considered to be true bacteria. l They possess an inner and outer membrane similar to gram-negative bacteria and a lipopolysaccharide but do not have a peptidoglycan layer. l Although they synthesize most of their metabolic intermediates, they are unable to make their own ATP and thus are energy parasites.
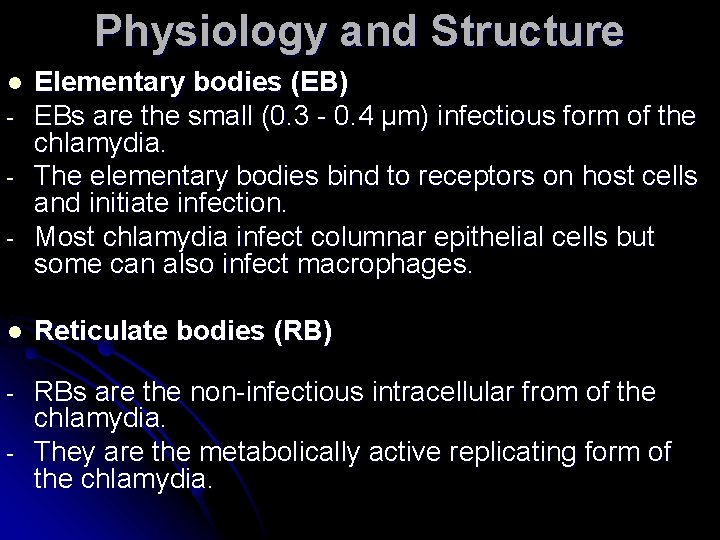
Physiology and Structure l - Elementary bodies (EB) EBs are the small (0. 3 - 0. 4 μm) infectious form of the chlamydia. The elementary bodies bind to receptors on host cells and initiate infection. Most chlamydia infect columnar epithelial cells but some can also infect macrophages. l Reticulate bodies (RB) - RBs are the non-infectious intracellular from of the chlamydia. They are the metabolically active replicating form of the chlamydia. -

The developmental cycle of chlamydia l The EBs are internalized by endocytosis and/or by phagocytosis. Within the host cell endosome the EBs reorganize and become RBs. l The chlamydia inhibit the fusion of the endosome with the lysosomes and thus resist intracellular killing. The entire intracellular life cycle of the chlamydia occurs within the endosome. l RBs replicate by binary fission and reorganize into EBs. The resulting inclusions may contain 100 - 500 progeny l Eventually the cells and inclusions lyse (C. psittaci) or the inclusion is extruded by reverse endocytosis (C. trachomatis and C. pneumoniae)

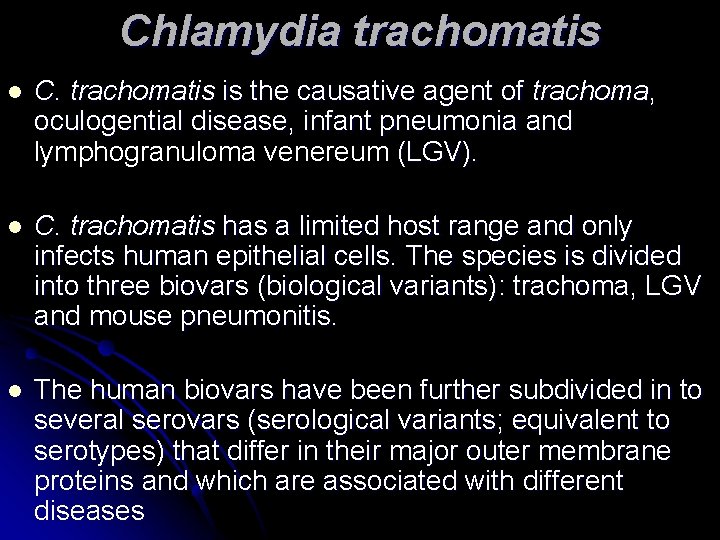
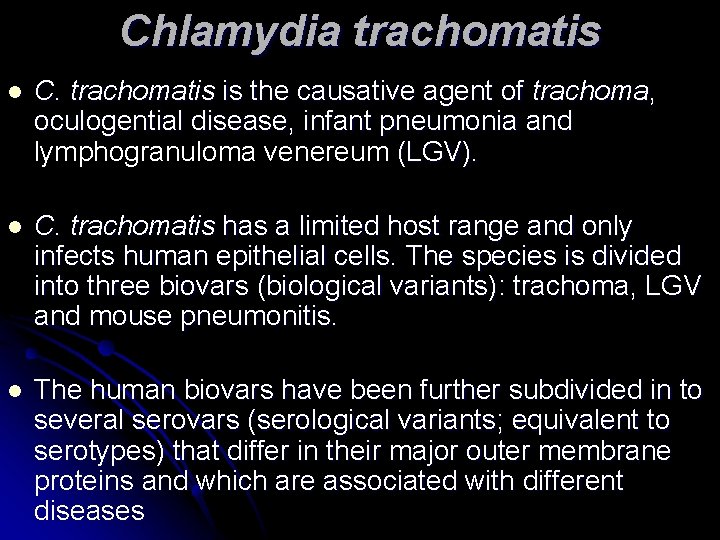
Chlamydia trachomatis l C. trachomatis is the causative agent of trachoma, oculogential disease, infant pneumonia and lymphogranuloma venereum (LGV). l C. trachomatis has a limited host range and only infects human epithelial cells. The species is divided into three biovars (biological variants): trachoma, LGV and mouse pneumonitis. l The human biovars have been further subdivided in to several serovars (serological variants; equivalent to serotypes) that differ in their major outer membrane proteins and which are associated with different diseases
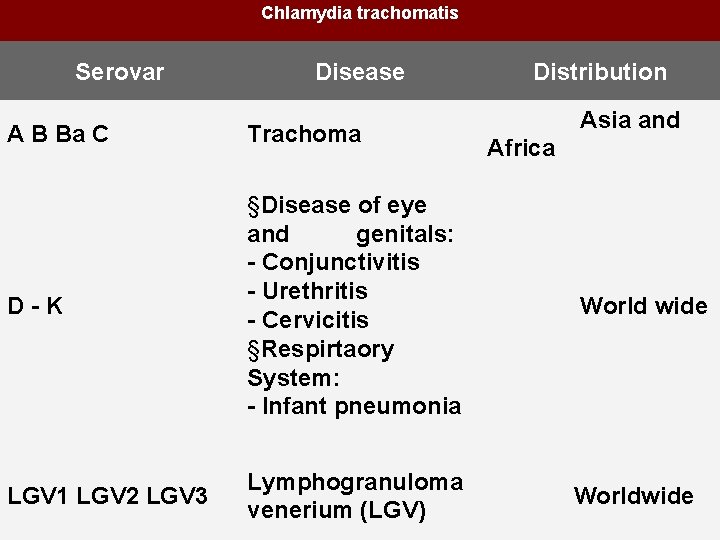
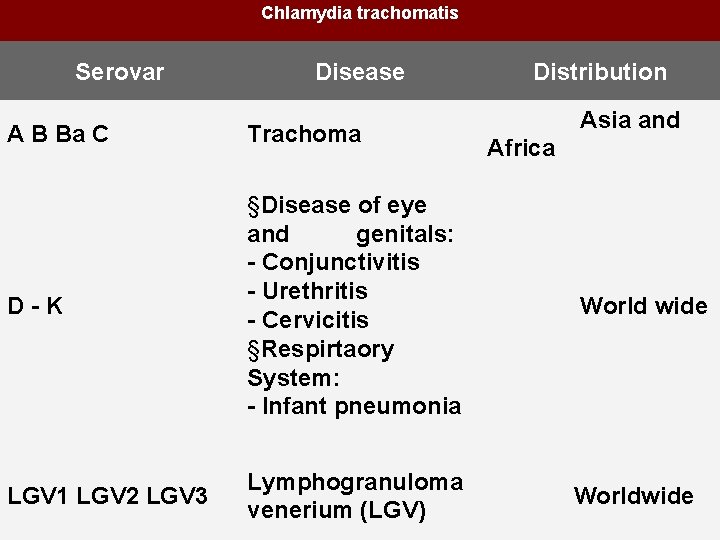
Chlamydia trachomatis Serovar Disease Distribution A B Ba C Trachoma Asia and Africa D - K §Disease of eye and genitals: - Conjunctivitis - Urethritis - Cervicitis §Respirtaory System: - Infant pneumonia World wide LGV 1 LGV 2 LGV 3 Lymphogranuloma Worldwide venerium (LGV)
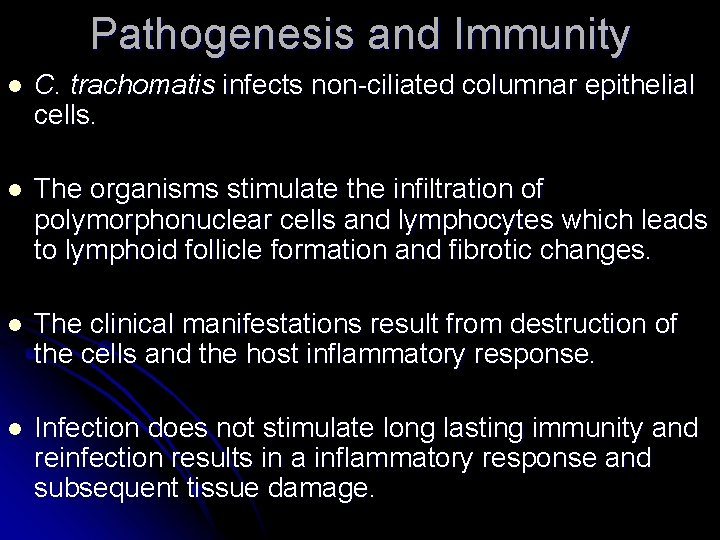
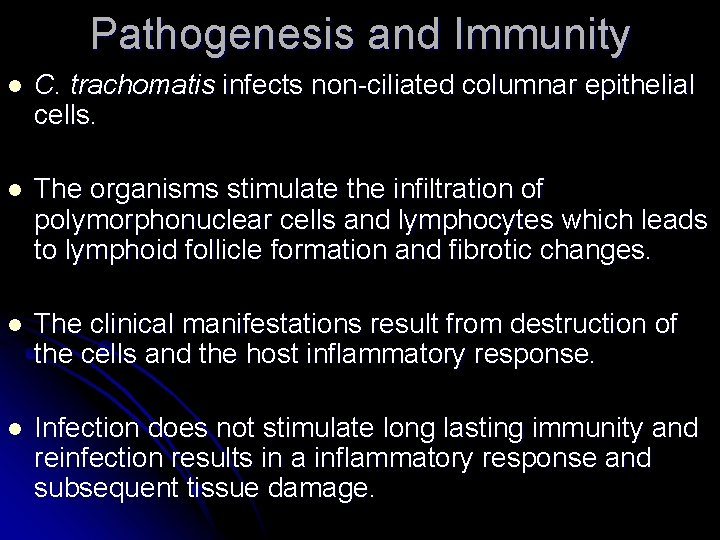
Pathogenesis and Immunity l C. trachomatis infects non-ciliated columnar epithelial cells. l The organisms stimulate the infiltration of polymorphonuclear cells and lymphocytes which leads to lymphoid follicle formation and fibrotic changes. l The clinical manifestations result from destruction of the cells and the host inflammatory response. l Infection does not stimulate long lasting immunity and reinfection results in a inflammatory response and subsequent tissue damage.
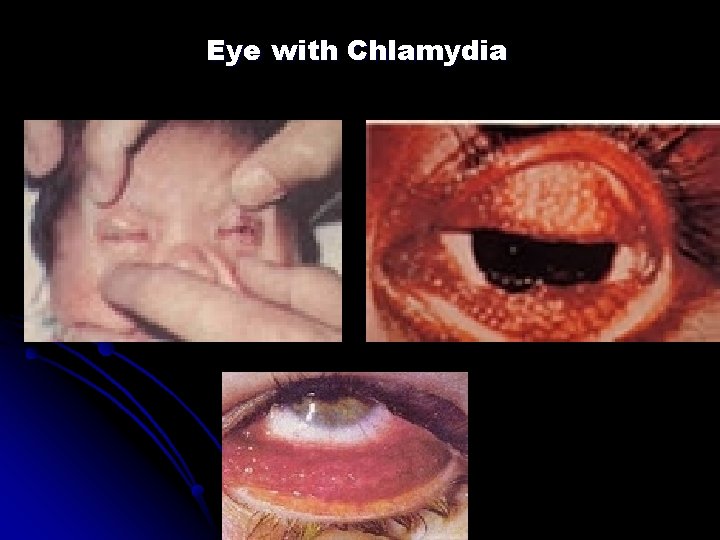
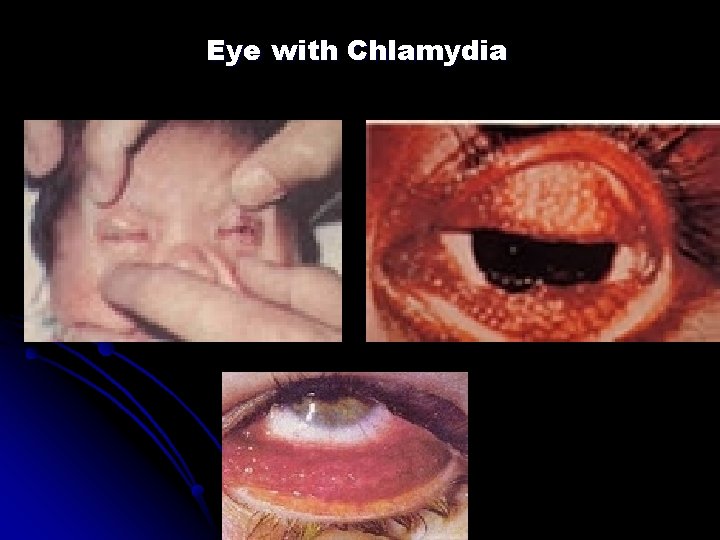
Eye with Chlamydia
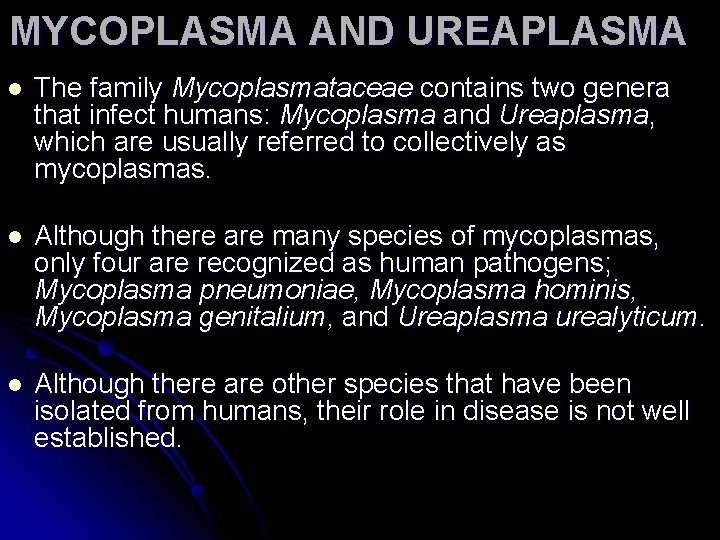
MYCOPLASMA AND UREAPLASMA l The family Mycoplasmataceae contains two genera that infect humans: Mycoplasma and Ureaplasma, which are usually referred to collectively as mycoplasmas. l Although there are many species of mycoplasmas, only four are recognized as human pathogens; Mycoplasma pneumoniae, Mycoplasma hominis, Mycoplasma genitalium, and Ureaplasma urealyticum. l Although there are other species that have been isolated from humans, their role in disease is not well established.
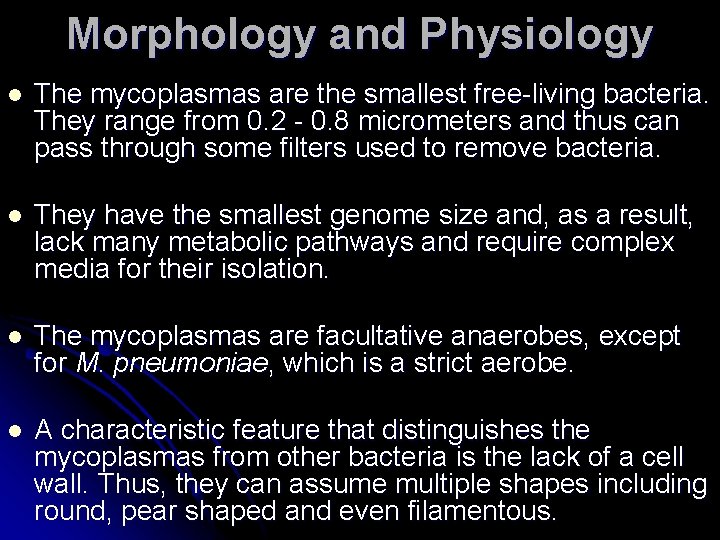
Morphology and Physiology l The mycoplasmas are the smallest free-living bacteria. They range from 0. 2 - 0. 8 micrometers and thus can pass through some filters used to remove bacteria. l They have the smallest genome size and, as a result, lack many metabolic pathways and require complex media for their isolation. l The mycoplasmas are facultative anaerobes, except for M. pneumoniae, which is a strict aerobe. l A characteristic feature that distinguishes the mycoplasmas from other bacteria is the lack of a cell wall. Thus, they can assume multiple shapes including round, pear shaped and even filamentous.
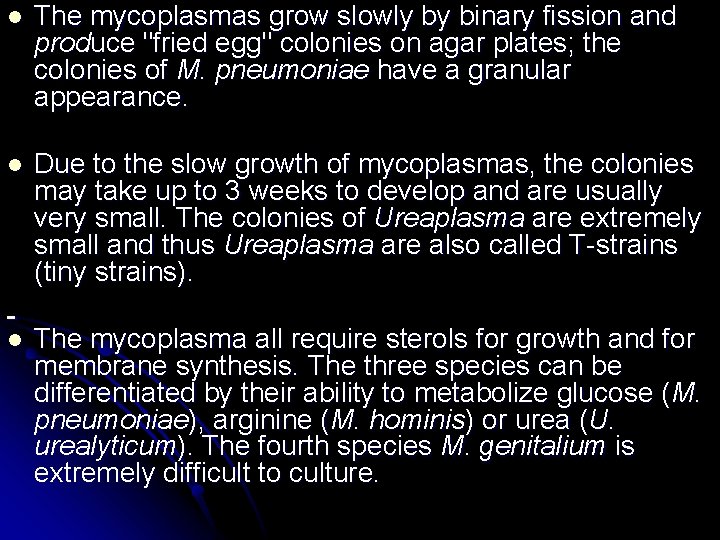
l The mycoplasmas grow slowly by binary fission and produce "fried egg" colonies on agar plates; the colonies of M. pneumoniae have a granular appearance. l Due to the slow growth of mycoplasmas, the colonies may take up to 3 weeks to develop and are usually very small. The colonies of Ureaplasma are extremely small and thus Ureaplasma are also called T-strains (tiny strains). l The mycoplasma all require sterols for growth and for membrane synthesis. The three species can be differentiated by their ability to metabolize glucose (M. pneumoniae), arginine (M. hominis) or urea (U. urealyticum). The fourth species M. genitalium is extremely difficult to culture.

The diseases caused by M. pneumoniae, M. hominis, M. genitalium and U. urealyticum Organism Disease M. pneumoniae Upper respiratory tract disease, tracheobronchitis, atypical pneumonia M. hominis Pyelonephritis, pelvic inflammatory disease, postpartum fever M. genitalium Nongonococcl urethritis U. urealyticum Nongonococcl urethritis

RICKETTSIA, ORIENTIA, EHRLICHIA, ANAPLASMA, COXIELLA AND BARTONELLA
l Howard Ricketts described the causative agent of Rocky Mountain Spotted Fever and was able to culture it in laboratory animals. l The Rickettsia, Ehrlichia, Anaplasma and Coxiella are all small obligate intracellular parasites which were once thought to be part of the same family. l Like the Chlamydia these bacteria were once thought to be viruses because of their small size and intracellular life cycle. However, they are true bacteria, structurally similar to Gram negative bacteria. l They are small Gram negative coccobacilli that are normally stained with Giemsa since they stain poorly with the Gram stain. Humans are accidentally infected with these organisms.
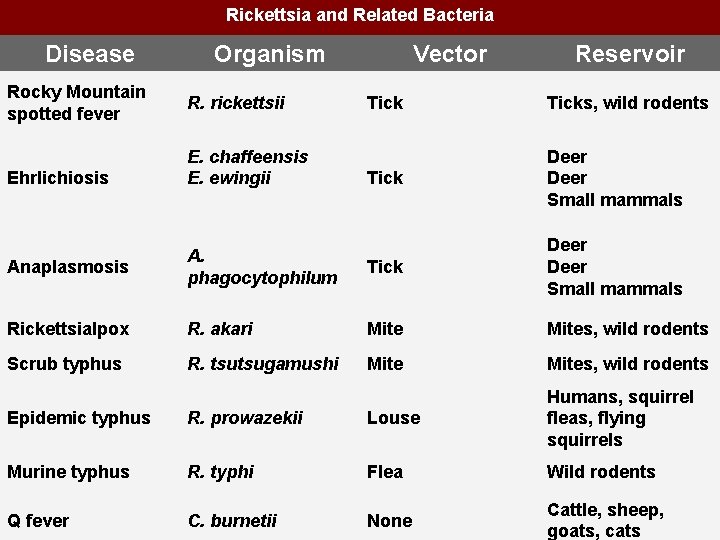
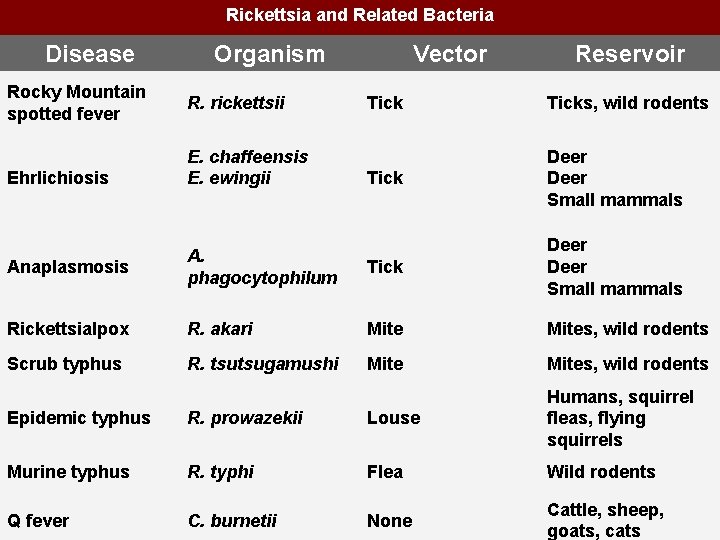
Rickettsia and Related Bacteria Disease Organism Rocky Mountain spotted fever R. rickettsii Ehrlichiosis E. chaffeensis E. ewingii Vector Reservoir Ticks, wild rodents Tick Deer Small mammals Anaplasmosis A. phagocytophilum Tick Deer Small mammals Rickettsialpox R. akari Mites, wild rodents Scrub typhus R. tsutsugamushi Mites, wild rodents Epidemic typhus R. prowazekii Louse Humans, squirrel fleas, flying squirrels Murine typhus R. typhi Flea Wild rodents Q fever C. burnetii None Cattle, sheep, goats, cats
 Dimorphic fungus
Dimorphic fungus Mycoplasma pneumoniae
Mycoplasma pneumoniae Mycoplasmas rickettsiae and chlamydiae are
Mycoplasmas rickettsiae and chlamydiae are Chlamydia trachomatis
Chlamydia trachomatis Neil mooser reaction ppt
Neil mooser reaction ppt Riketsiyalar genel özellikleri
Riketsiyalar genel özellikleri Pediculus humanus
Pediculus humanus Gonore inkubationstid
Gonore inkubationstid Grey cloudy discharge
Grey cloudy discharge Long term effects of chlamydia
Long term effects of chlamydia Chlamydia trachomatis
Chlamydia trachomatis Skinlearning
Skinlearning Doxycycline chlamydia dosage
Doxycycline chlamydia dosage Chlamydia trachomatis diagnosis
Chlamydia trachomatis diagnosis Chlamydia trachomatis diagnosis
Chlamydia trachomatis diagnosis Biovar tric
Biovar tric Chlamydia
Chlamydia Chlamydia symptoms
Chlamydia symptoms