Medical Nutrition Therapy in Neurological Disorders Part 2

- Slides: 67
Medical Nutrition Therapy in Neurological Disorders Part 2
Epilepsy • • Intermittent derangement of the nervous system caused by sudden discharge of cerebral neurons 2. 3 million Americans have epilepsy; 15% under age 15 May be caused by head injury, congenital defects, metabolic disorders, other illnesses Many are idiopathic (cause unknown)
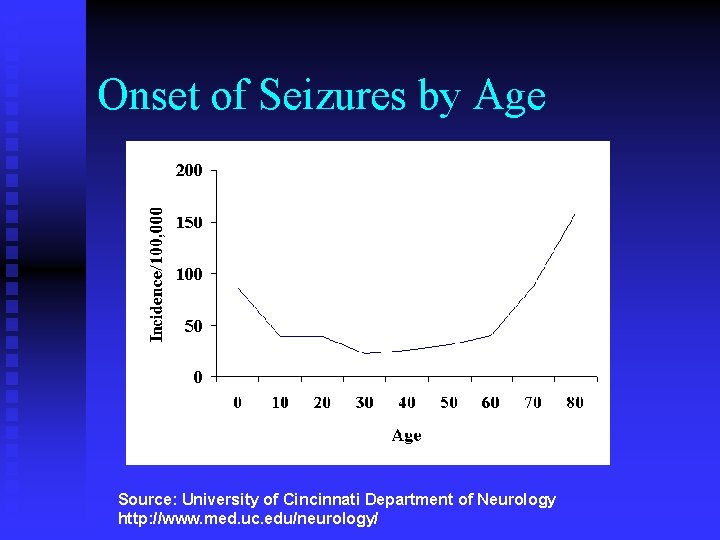
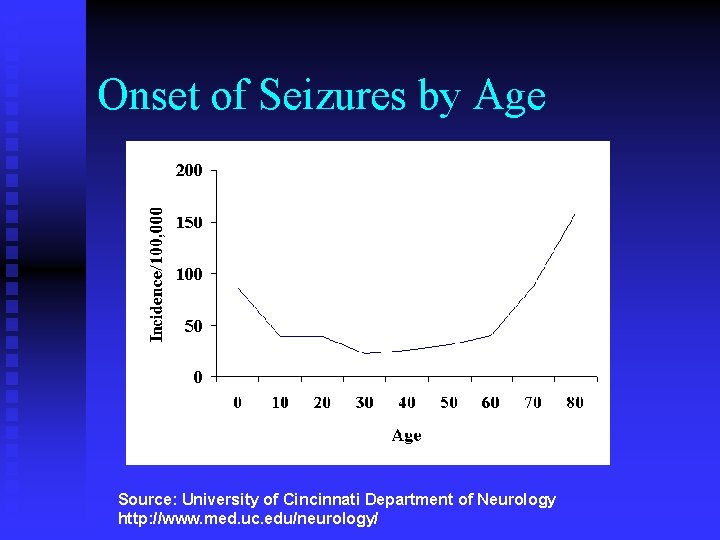
Onset of Seizures by Age Source: University of Cincinnati Department of Neurology http: //www. med. uc. edu/neurology/
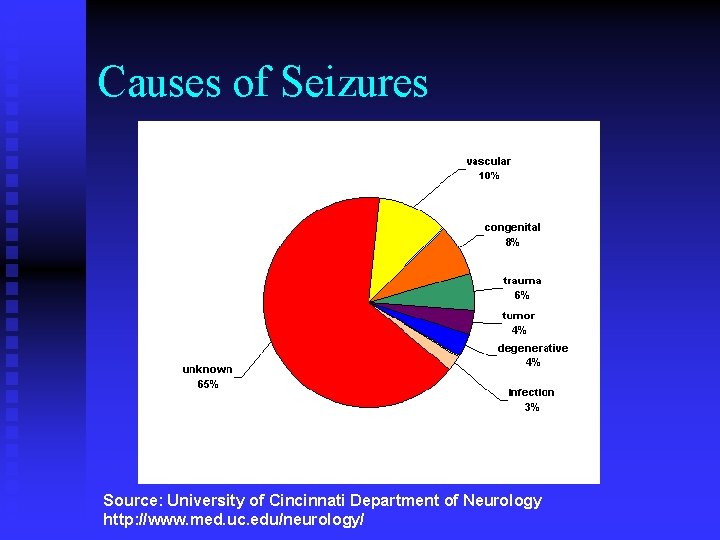
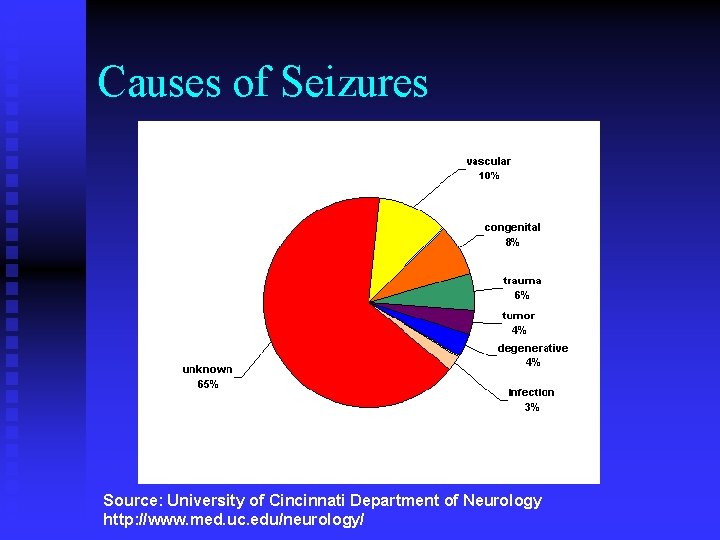
Causes of Seizures Source: University of Cincinnati Department of Neurology http: //www. med. uc. edu/neurology/
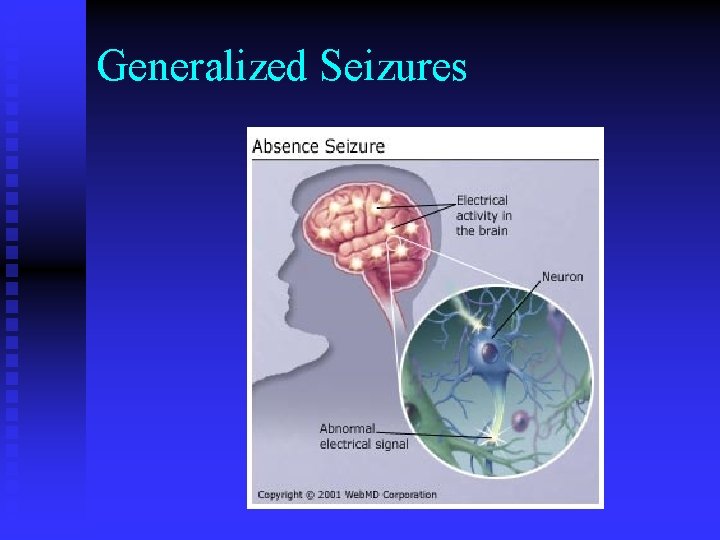
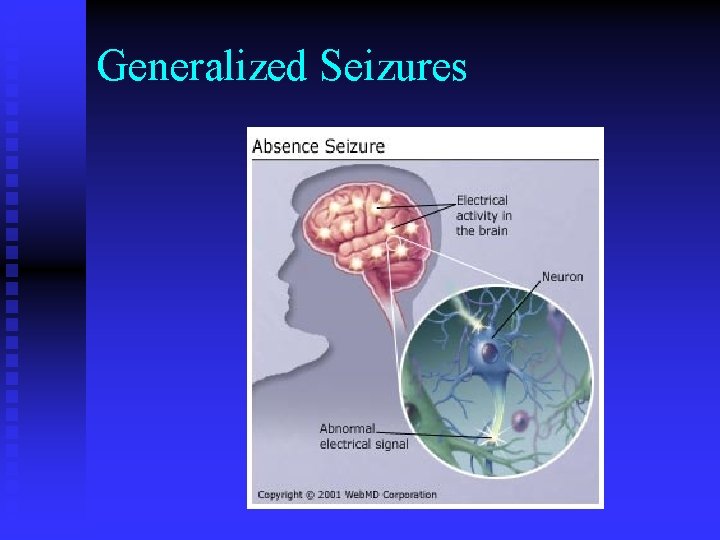
Generalized Seizures
Epilepsy: Tonic-Clonic Seizure • • Formerly called grand mal. Generalized seizure that lasts 1 -2 minutes Involves complete loss of muscle tone and consciousness More common in children
Epilepsy: Absence Seizure • • Formerly called petit mal Also generalized May appear to be daydreaming, but recovers after a few seconds with no postictal fatigue or disorientation More common in children
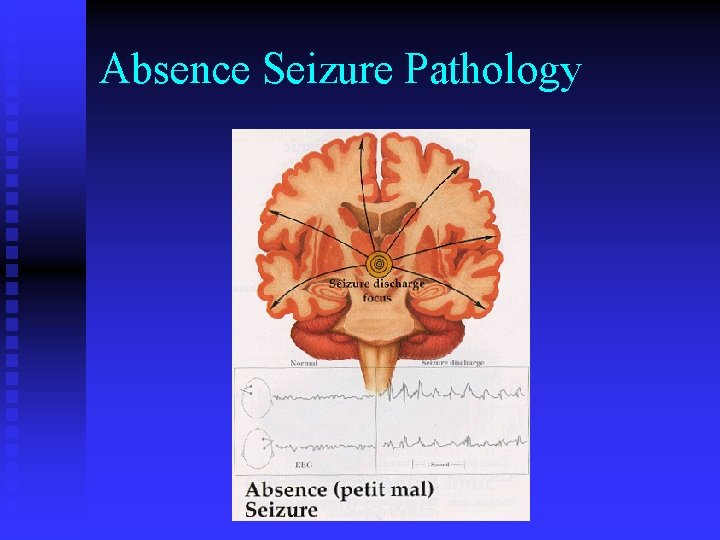
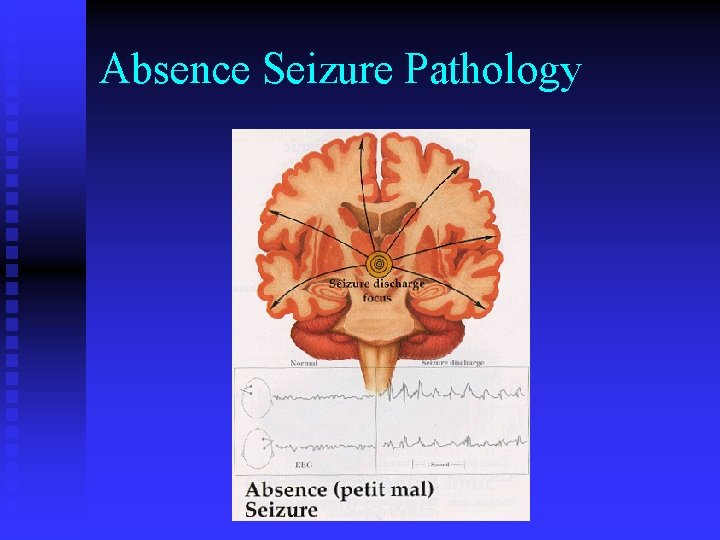
Absence Seizure Pathology
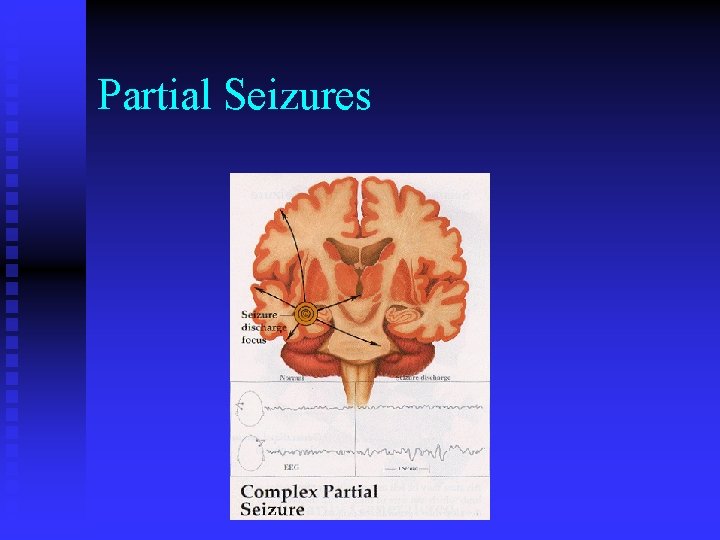
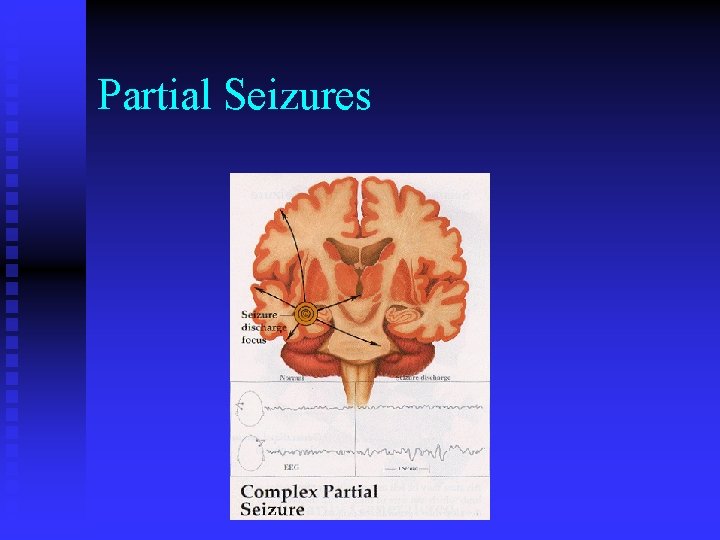
Partial Seizures
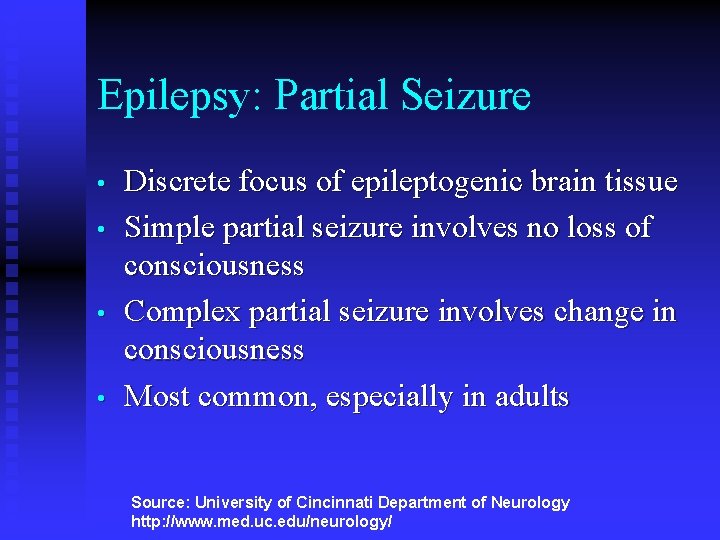
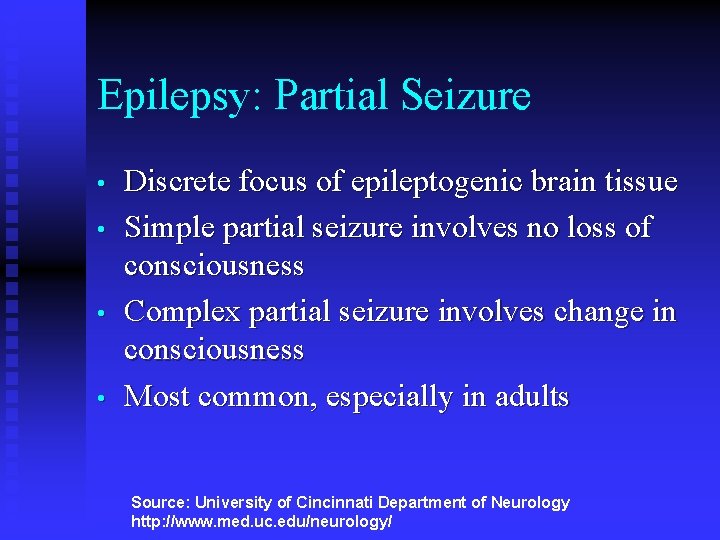
Epilepsy: Partial Seizure • • Discrete focus of epileptogenic brain tissue Simple partial seizure involves no loss of consciousness Complex partial seizure involves change in consciousness Most common, especially in adults Source: University of Cincinnati Department of Neurology http: //www. med. uc. edu/neurology/
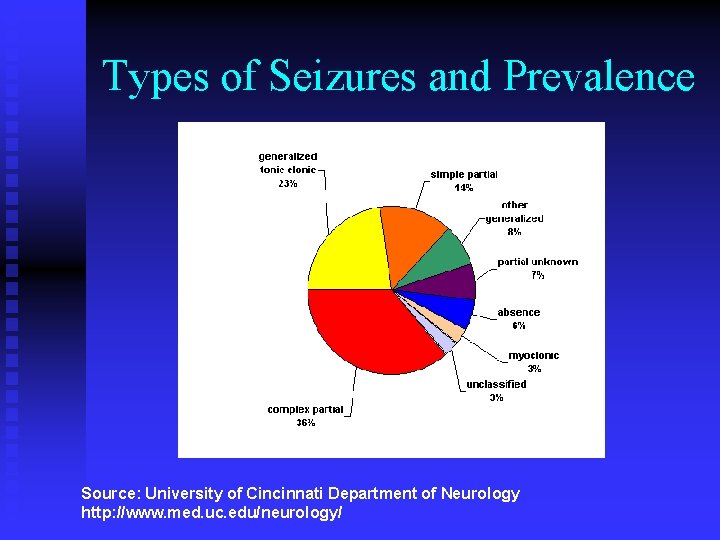
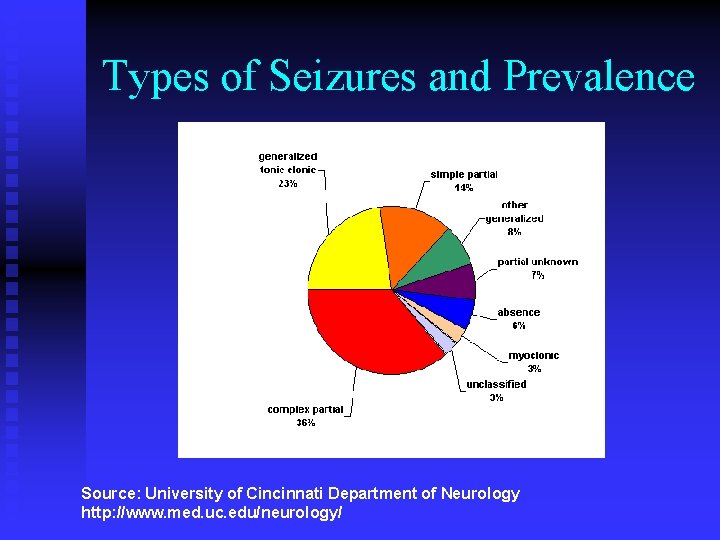
Types of Seizures and Prevalence Source: University of Cincinnati Department of Neurology http: //www. med. uc. edu/neurology/
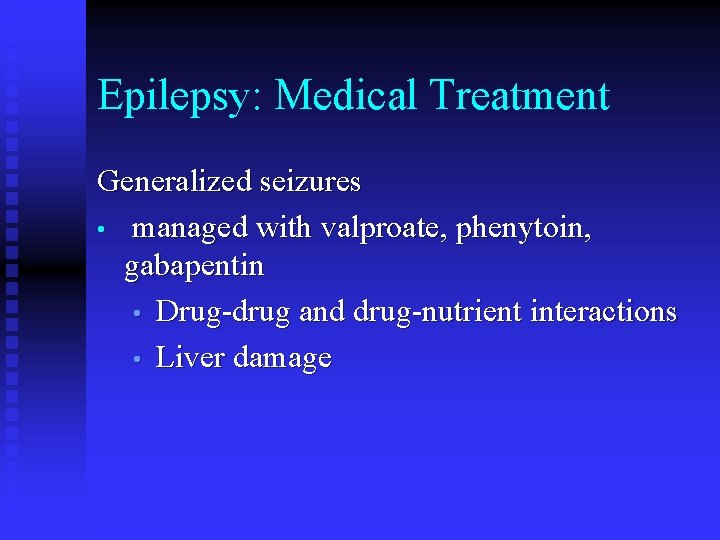
Epilepsy: Medical Treatment Generalized seizures • managed with valproate, phenytoin, gabapentin • Drug-drug and drug-nutrient interactions • Liver damage
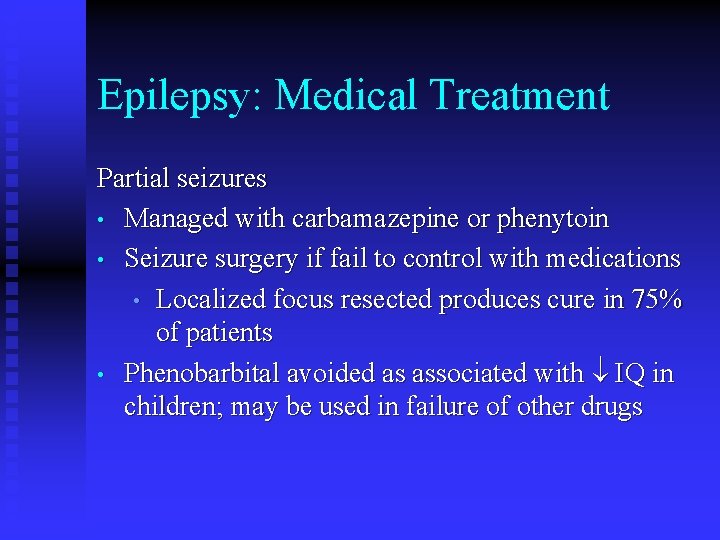
Epilepsy: Medical Treatment Partial seizures • Managed with carbamazepine or phenytoin • Seizure surgery if fail to control with medications • Localized focus resected produces cure in 75% of patients • Phenobarbital avoided as associated with IQ in children; may be used in failure of other drugs
Epilepsy: Drug-Nutrient Interactions • • • Phenobarbital, phenytoin, primidone interfere with absorption of calcium by increasing vitamin D metabolism Long term therapy may lead to osteomalacia in adults or rickets in children Vitamin D supplementation is essential
Epilepsy: Drug-Nutrient Interactions • • • Folic acid supplementation interferes with phenytoin metabolism; may not reach therapeutic levels Phenytoin and phenobarbital are bound to albumin in the bloodstream; malnutrition results in free drug and possible toxicity Alcohol interferes with phenytoin, possibly resulting in seizures
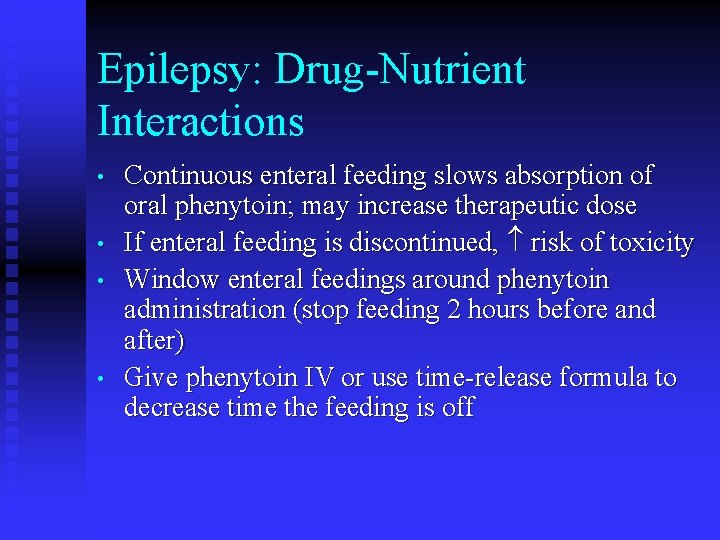
Epilepsy: Drug-Nutrient Interactions • • Continuous enteral feeding slows absorption of oral phenytoin; may increase therapeutic dose If enteral feeding is discontinued, risk of toxicity Window enteral feedings around phenytoin administration (stop feeding 2 hours before and after) Give phenytoin IV or use time-release formula to decrease time the feeding is off
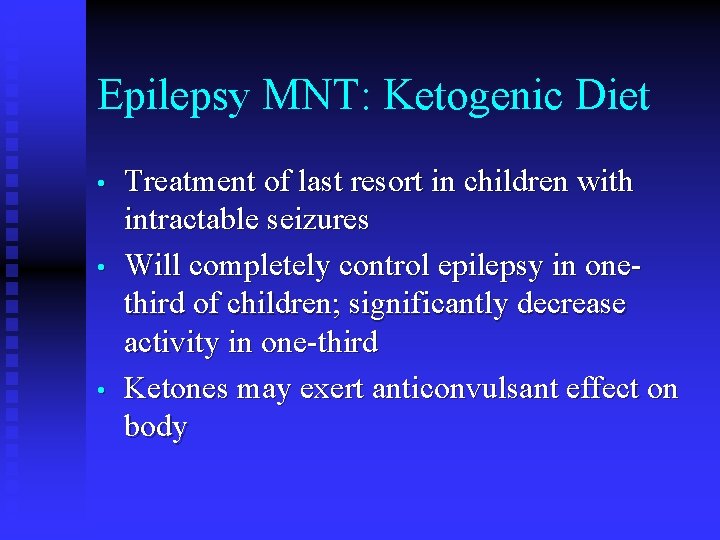
Epilepsy MNT: Ketogenic Diet • • • Treatment of last resort in children with intractable seizures Will completely control epilepsy in onethird of children; significantly decrease activity in one-third Ketones may exert anticonvulsant effect on body
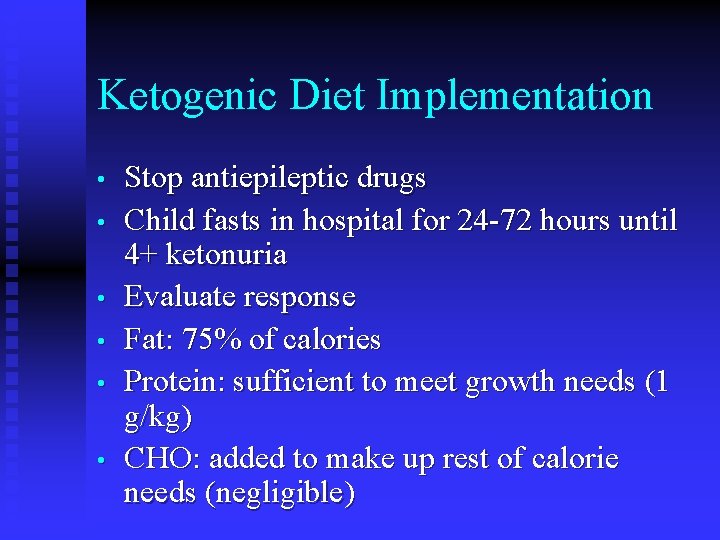
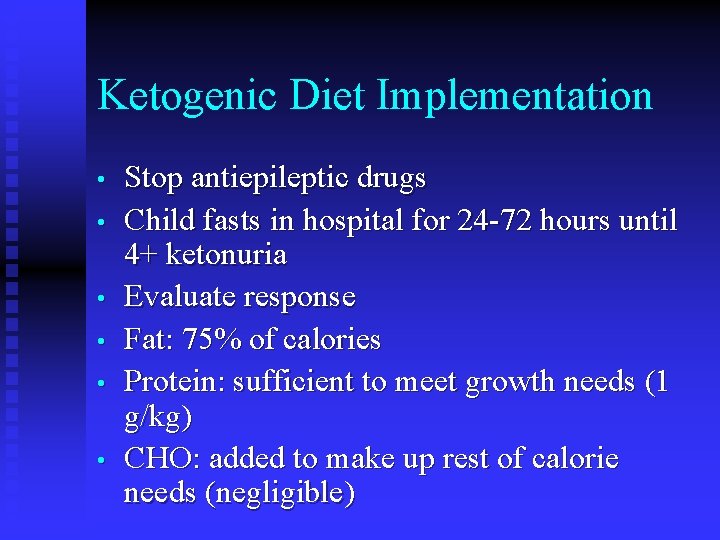
Ketogenic Diet Implementation • • • Stop antiepileptic drugs Child fasts in hospital for 24 -72 hours until 4+ ketonuria Evaluate response Fat: 75% of calories Protein: sufficient to meet growth needs (1 g/kg) CHO: added to make up rest of calorie needs (negligible)
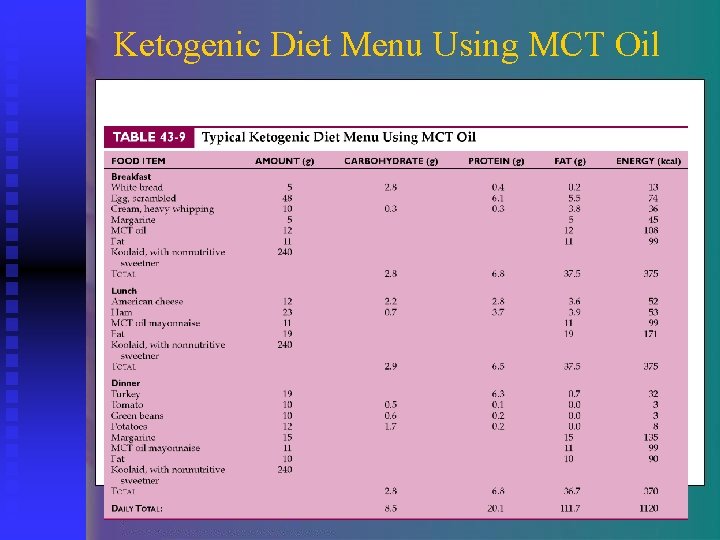
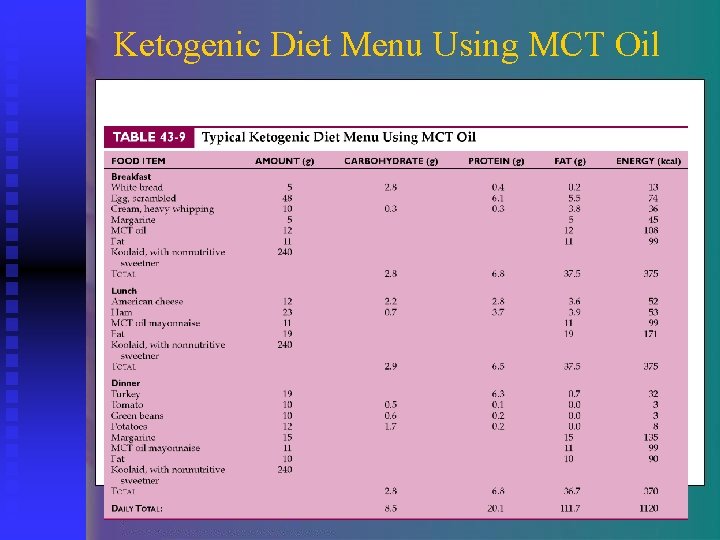
Ketogenic Diet Menu Using MCT Oil
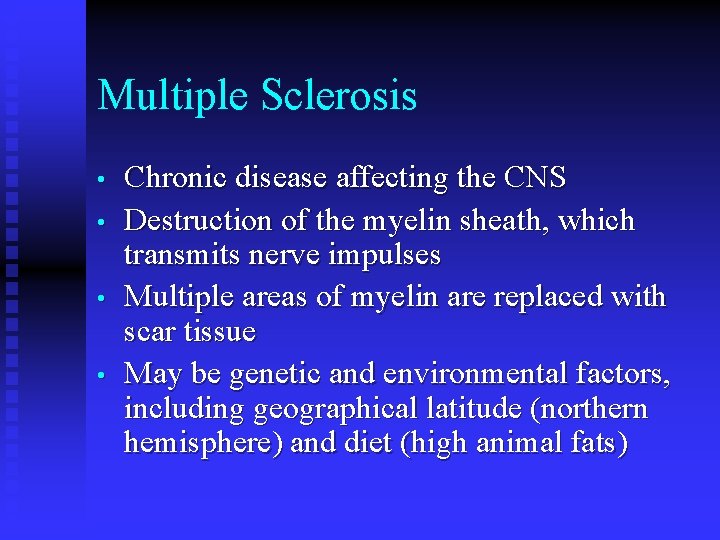
Multiple Sclerosis • • Chronic disease affecting the CNS Destruction of the myelin sheath, which transmits nerve impulses Multiple areas of myelin are replaced with scar tissue May be genetic and environmental factors, including geographical latitude (northern hemisphere) and diet (high animal fats)
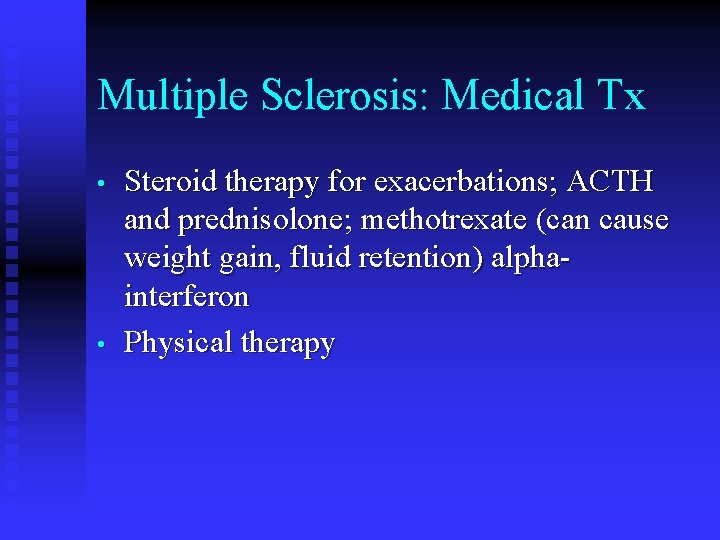
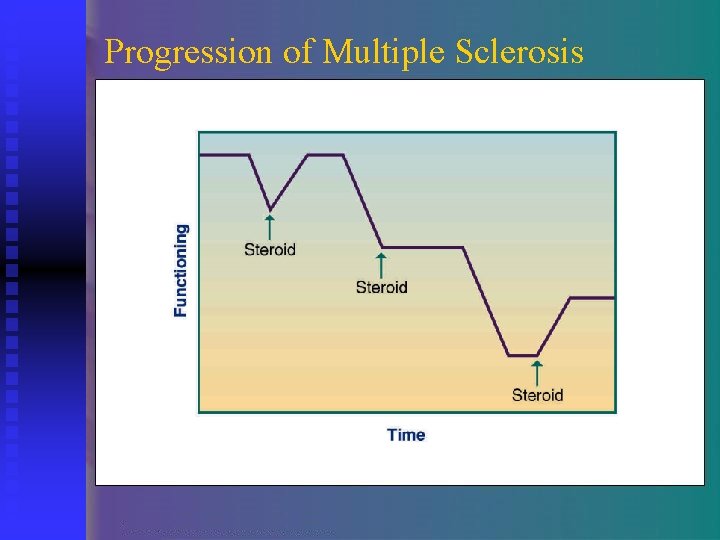
Multiple Sclerosis: Medical Tx • • Steroid therapy for exacerbations; ACTH and prednisolone; methotrexate (can cause weight gain, fluid retention) alphainterferon Physical therapy
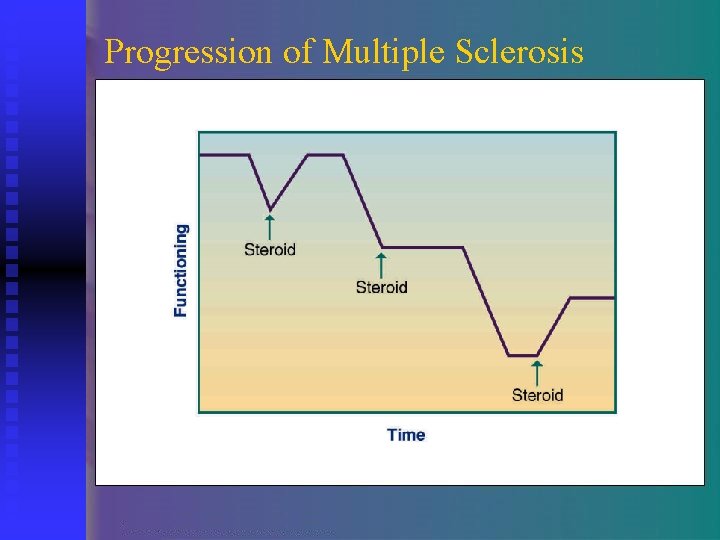
Progression of Multiple Sclerosis
MS Controversial Therapies • • Shank diet: low in saturated fat Mac. Dougal diet: no gluten, low sugar, and no refined sugar Allergen-free, gluten-free, pectin-free, fructose-restricted, raw food Evers diet Low fat diet high in linoleic acid may have some beneficial effects
MNT in MS • • • Diet consistency modifications as needed if dysphagia develops Suggest prepackaged, single-serving or convenience foods if meal preparation becomes difficult due to impaired vision, poor ambulation High fiber diet for constipation Counseling regarding fluid intake, cranberry juice to prevent UTIs Enteral nutrition support in end stage
Nutrition Guidelines for Parkinson’s Disease • • Eat a variety of healthy foods consistent with the US Dietary Guidelines Maintain a healthy body weight Balance food with exercise Eat foods high in fiber
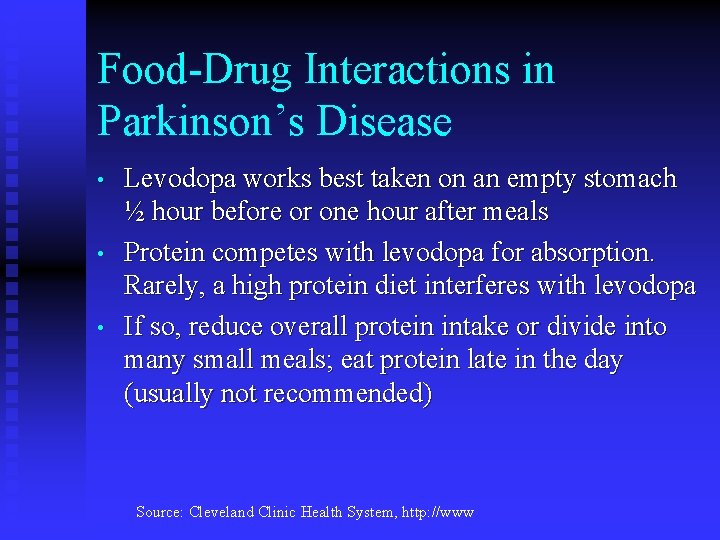
Food-Drug Interactions in Parkinson’s Disease • • • Levodopa works best taken on an empty stomach ½ hour before or one hour after meals Protein competes with levodopa for absorption. Rarely, a high protein diet interferes with levodopa If so, reduce overall protein intake or divide into many small meals; eat protein late in the day (usually not recommended) Source: Cleveland Clinic Health System, http: //www
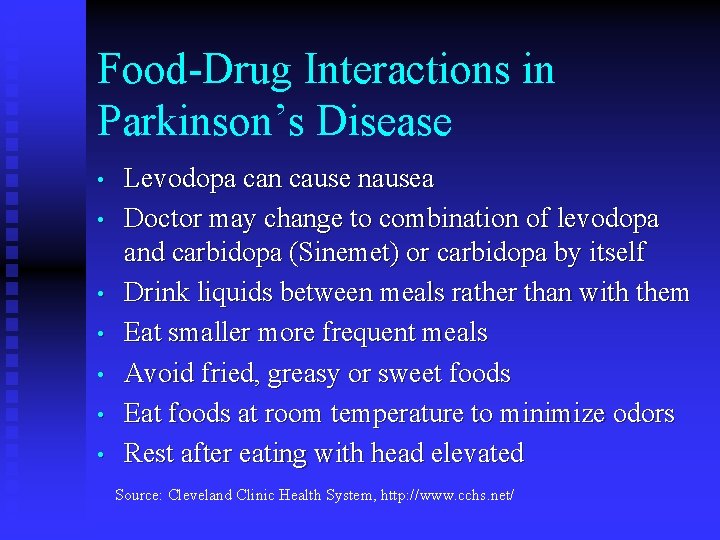
Food-Drug Interactions in Parkinson’s Disease • • Levodopa can cause nausea Doctor may change to combination of levodopa and carbidopa (Sinemet) or carbidopa by itself Drink liquids between meals rather than with them Eat smaller more frequent meals Avoid fried, greasy or sweet foods Eat foods at room temperature to minimize odors Rest after eating with head elevated Source: Cleveland Clinic Health System, http: //www. cchs. net/
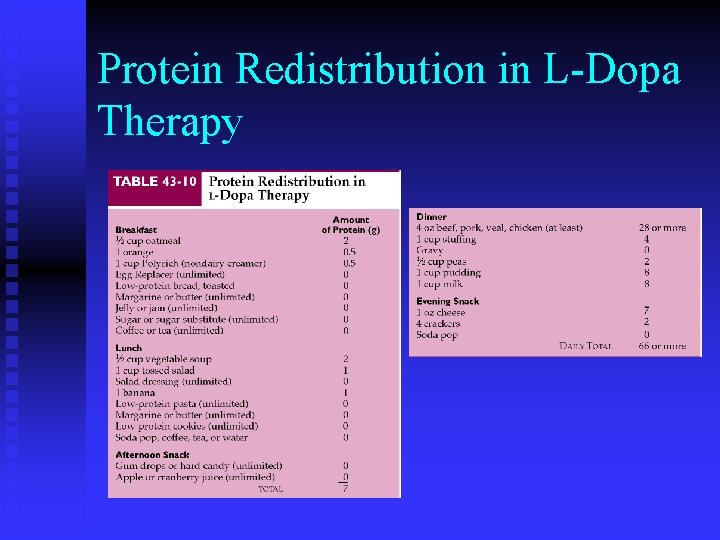
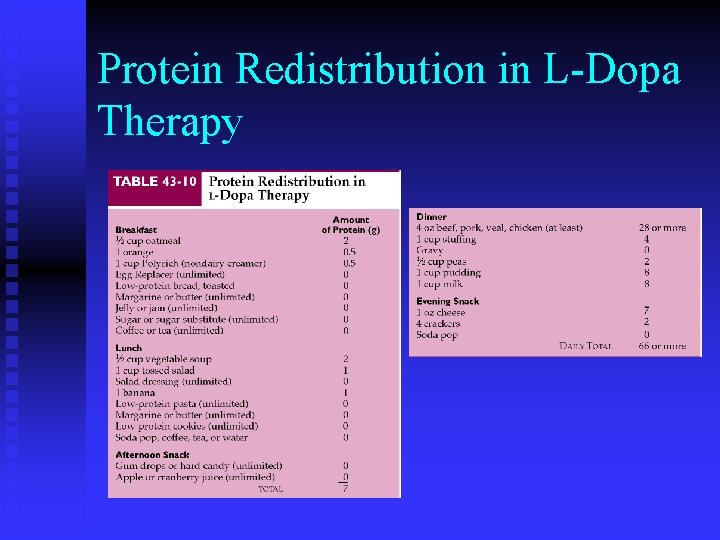
Protein Redistribution in L-Dopa Therapy
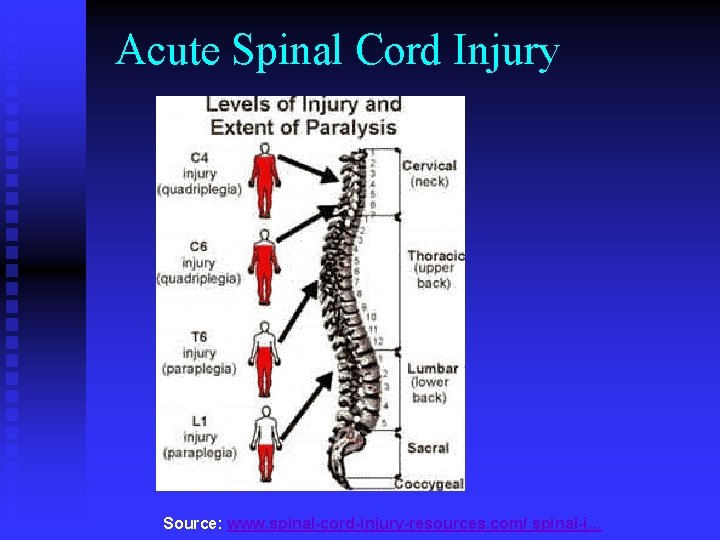
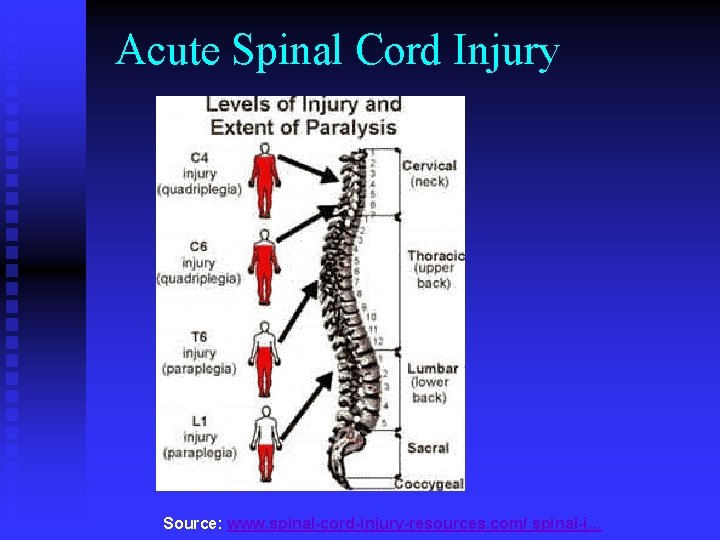
Acute Spinal Cord Injury Source: www. spinal-cord-injury-resources. com/ spinal-i. . .
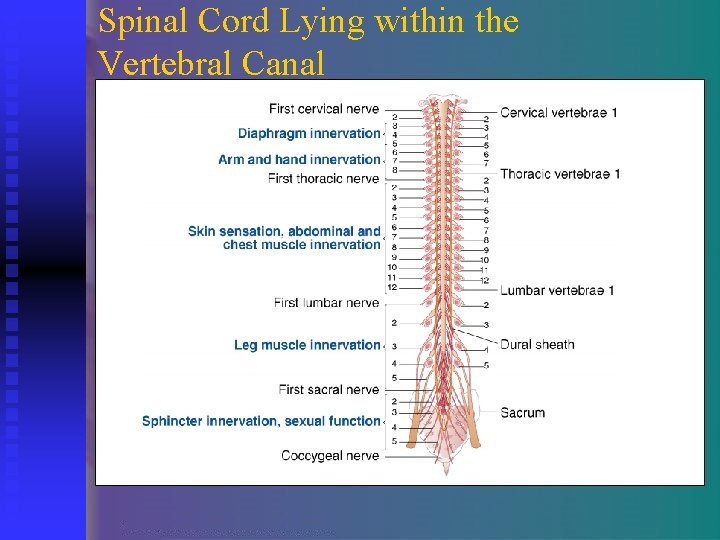
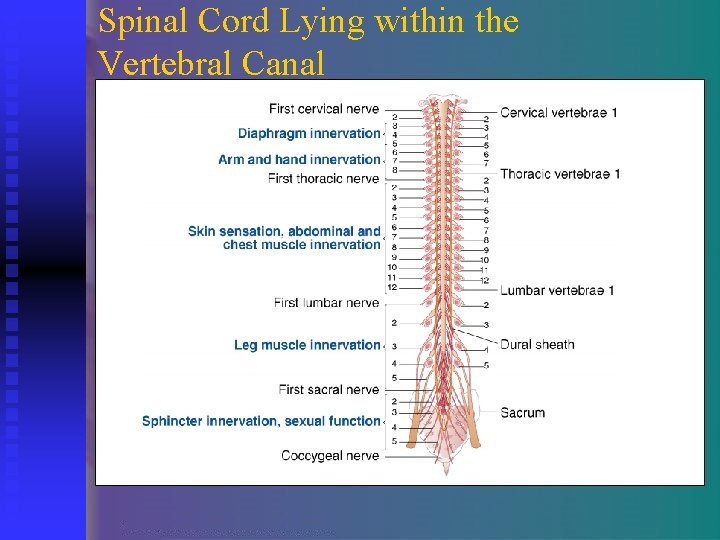
Spinal Cord Lying within the Vertebral Canal
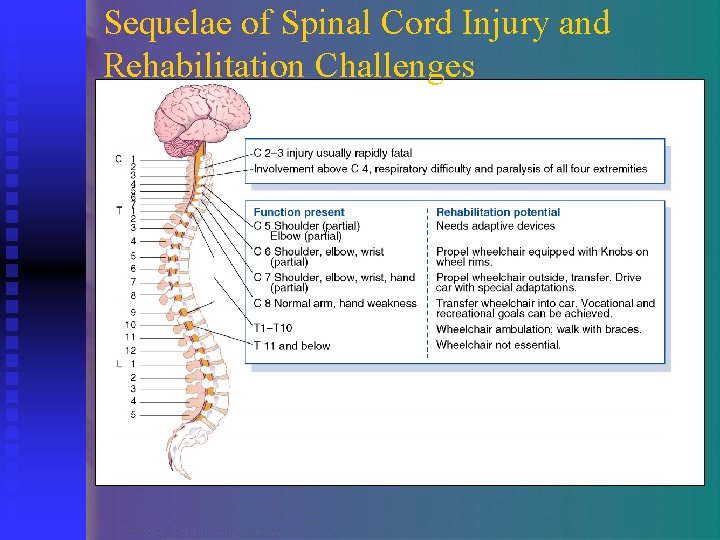
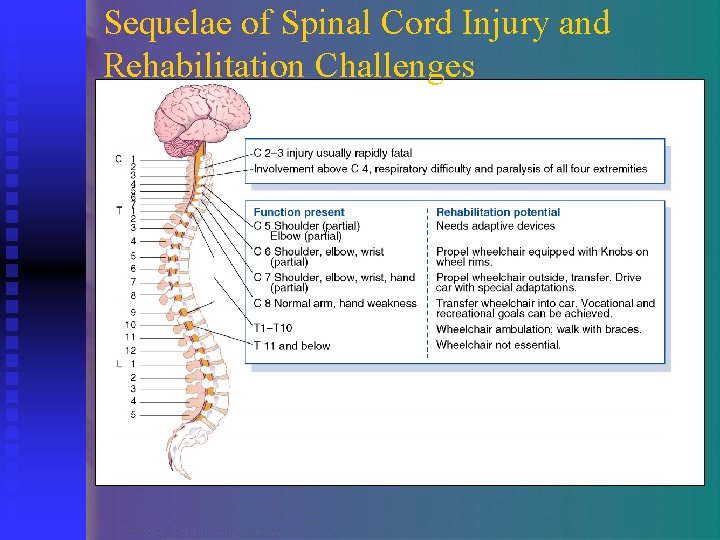
Sequelae of Spinal Cord Injury and Rehabilitation Challenges
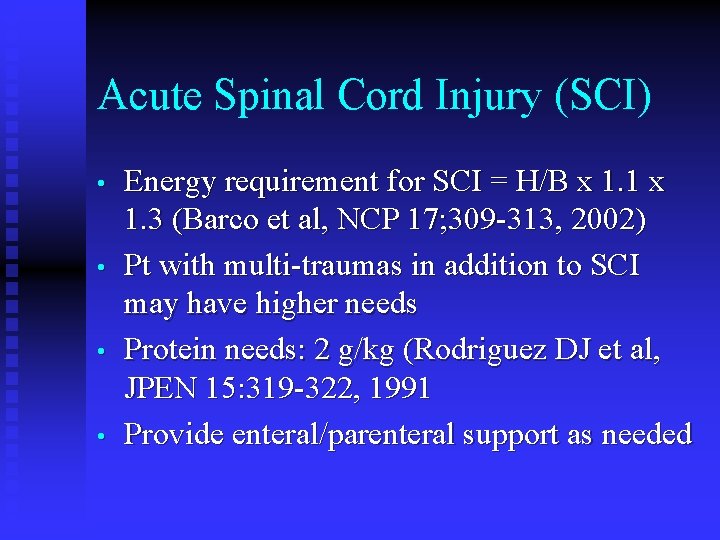
Acute Spinal Cord Injury (SCI) • • Energy requirement for SCI = H/B x 1. 1 x 1. 3 (Barco et al, NCP 17; 309 -313, 2002) Pt with multi-traumas in addition to SCI may have higher needs Protein needs: 2 g/kg (Rodriguez DJ et al, JPEN 15: 319 -322, 1991 Provide enteral/parenteral support as needed
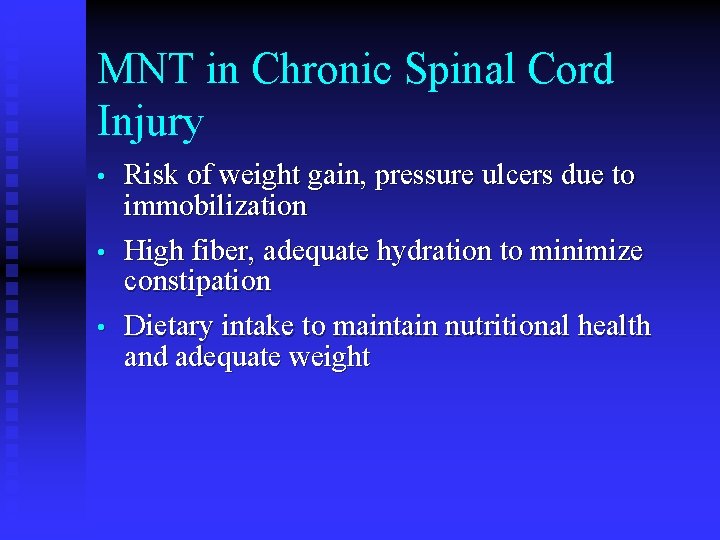
MNT in Chronic Spinal Cord Injury • • • Risk of weight gain, pressure ulcers due to immobilization High fiber, adequate hydration to minimize constipation Dietary intake to maintain nutritional health and adequate weight
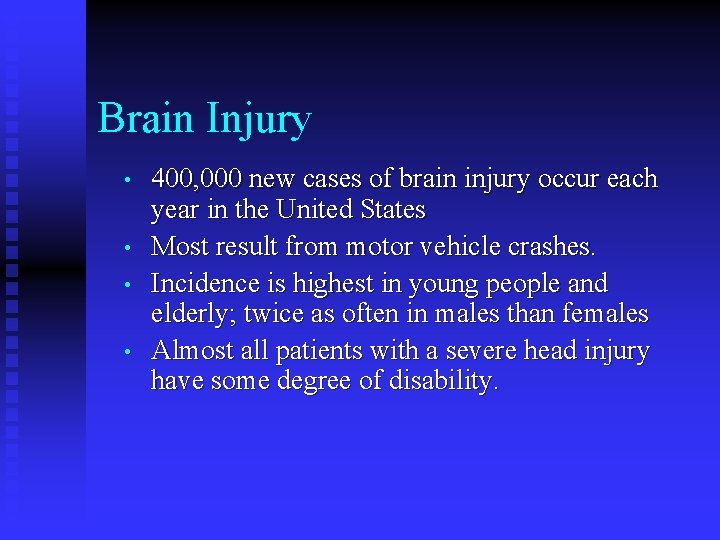
Brain Injury • • 400, 000 new cases of brain injury occur each year in the United States Most result from motor vehicle crashes. Incidence is highest in young people and elderly; twice as often in males than females Almost all patients with a severe head injury have some degree of disability.
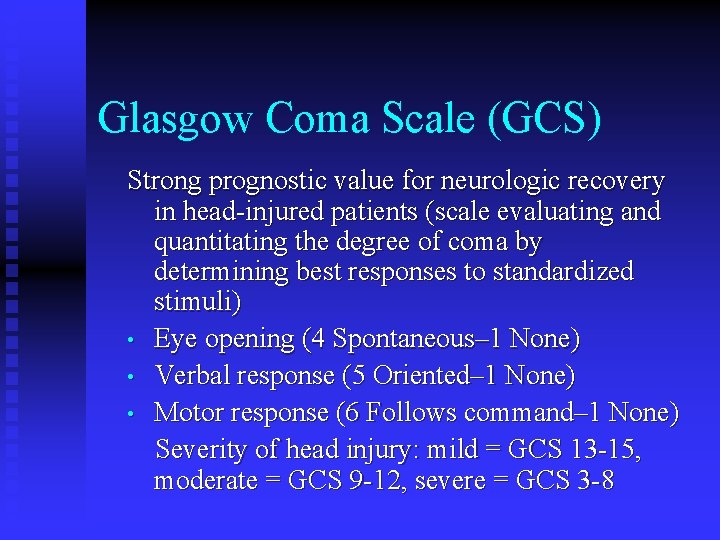
Glasgow Coma Scale (GCS) Strong prognostic value for neurologic recovery in head-injured patients (scale evaluating and quantitating the degree of coma by determining best responses to standardized stimuli) • Eye opening (4 Spontaneous– 1 None) • Verbal response (5 Oriented– 1 None) • Motor response (6 Follows command– 1 None) Severity of head injury: mild = GCS 13 -15, moderate = GCS 9 -12, severe = GCS 3 -8
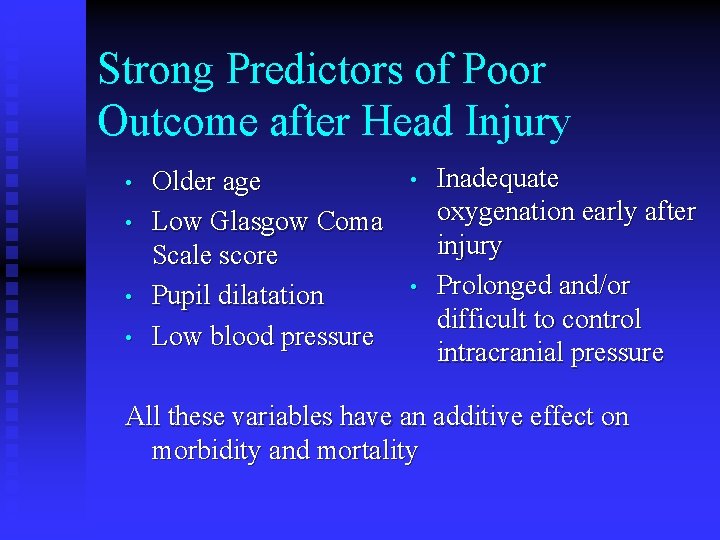
Strong Predictors of Poor Outcome after Head Injury • • Older age Low Glasgow Coma Scale score Pupil dilatation Low blood pressure • • Inadequate oxygenation early after injury Prolonged and/or difficult to control intracranial pressure All these variables have an additive effect on morbidity and mortality

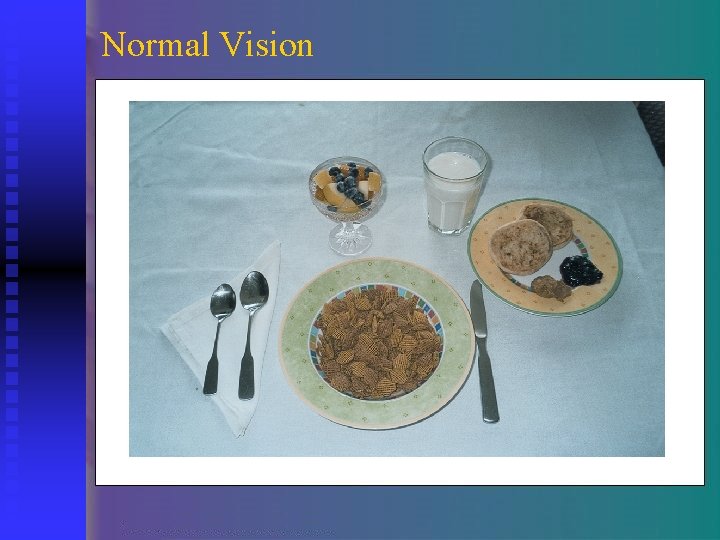
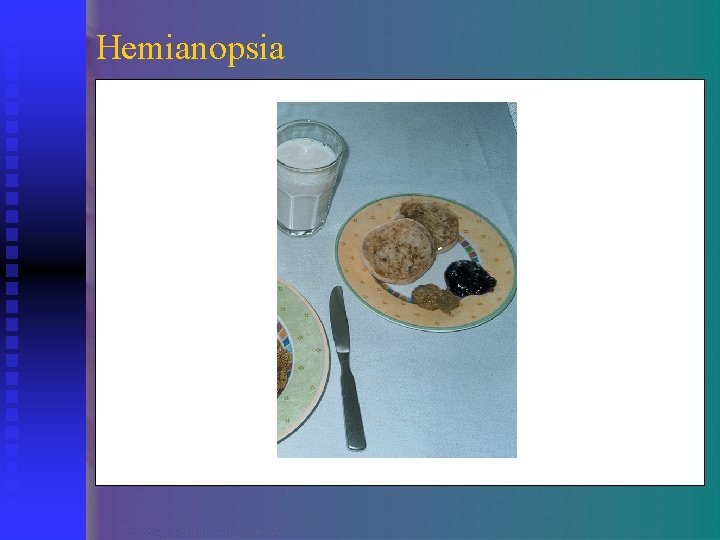
Neurological Deficits That Affect Nutritional Status • • Hemiparesis: weakness that affects one side of the body • May increase risk of aspiration Hemianopsia: blindness in one half of field of vision. • Must compensate by turning his head
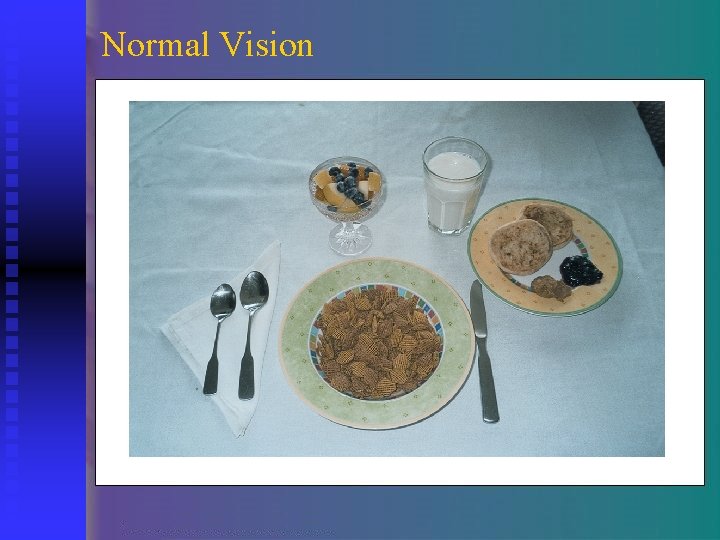
Normal Vision
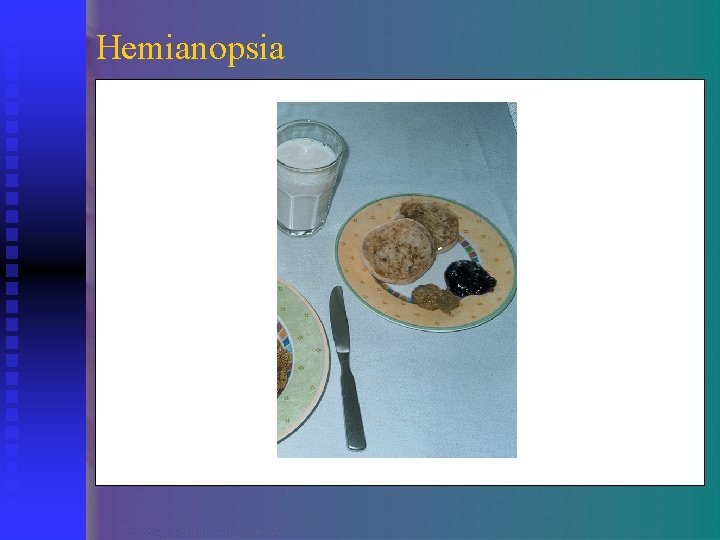
Hemianopsia
Neurological Deficits That Affect Nutritional Status • • Apraxia • Patient has difficulty with perceptual motor planning Dysphagia • Difficulty swallowing
Symptoms of Dysphagia • • • Drooling Choking or coughing during or following meals Inability to suck from a straw Gurgly voice quality Holding pockets of food in the buccal recesses (patient may not be aware)
Symptoms of Dysphagia • • • Absent gag reflex Chronic upper respiratory infections Weight loss and anorexia
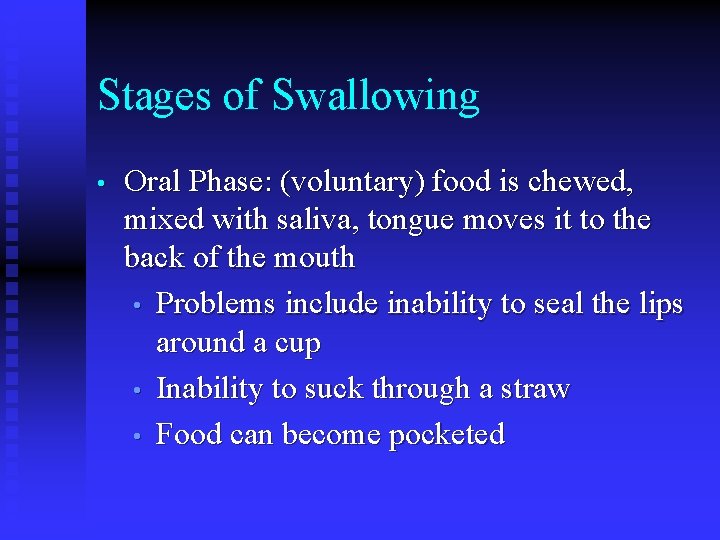
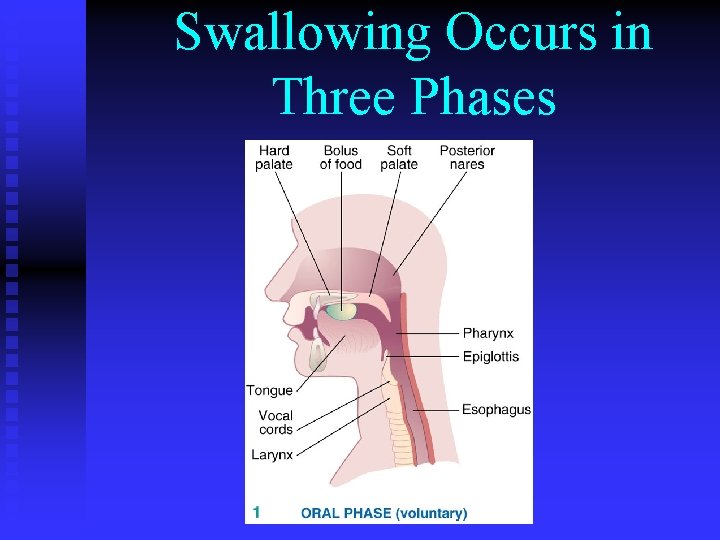
Stages of Swallowing • Oral Phase: (voluntary) food is chewed, mixed with saliva, tongue moves it to the back of the mouth • Problems include inability to seal the lips around a cup • Inability to suck through a straw • Food can become pocketed
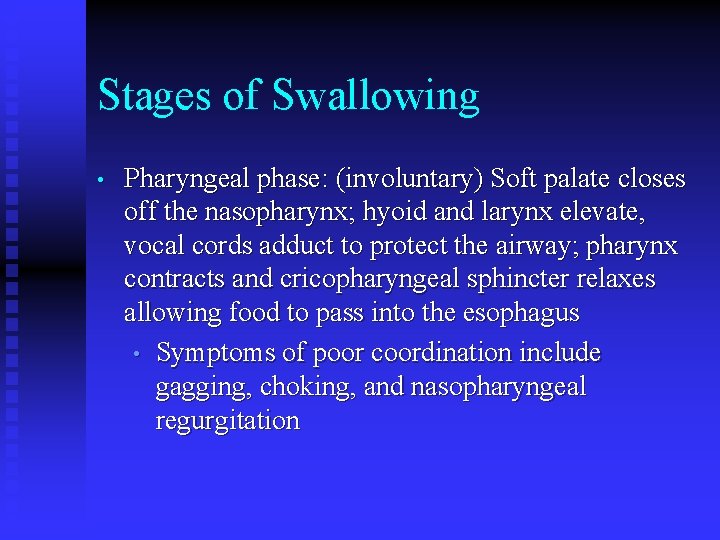
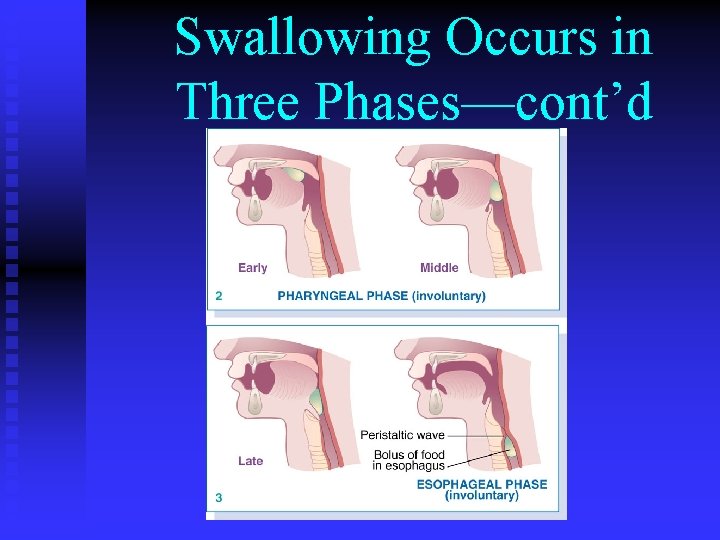
Stages of Swallowing • Pharyngeal phase: (involuntary) Soft palate closes off the nasopharynx; hyoid and larynx elevate, vocal cords adduct to protect the airway; pharynx contracts and cricopharyngeal sphincter relaxes allowing food to pass into the esophagus • Symptoms of poor coordination include gagging, choking, and nasopharyngeal regurgitation
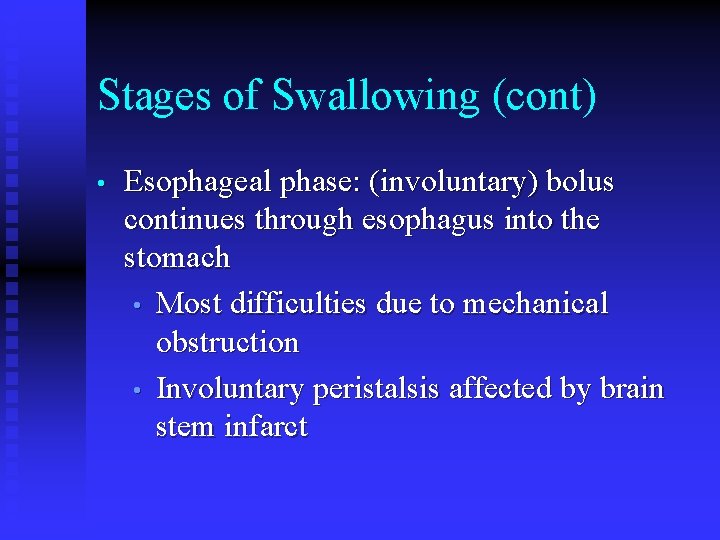
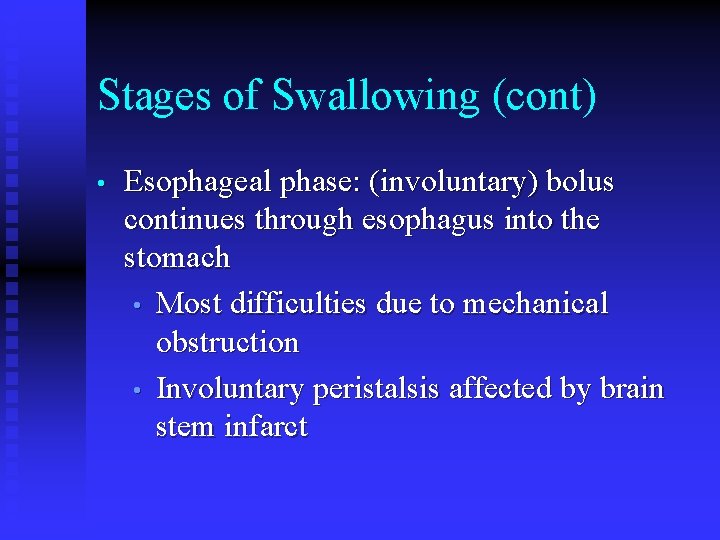
Stages of Swallowing (cont) • Esophageal phase: (involuntary) bolus continues through esophagus into the stomach • Most difficulties due to mechanical obstruction • Involuntary peristalsis affected by brain stem infarct
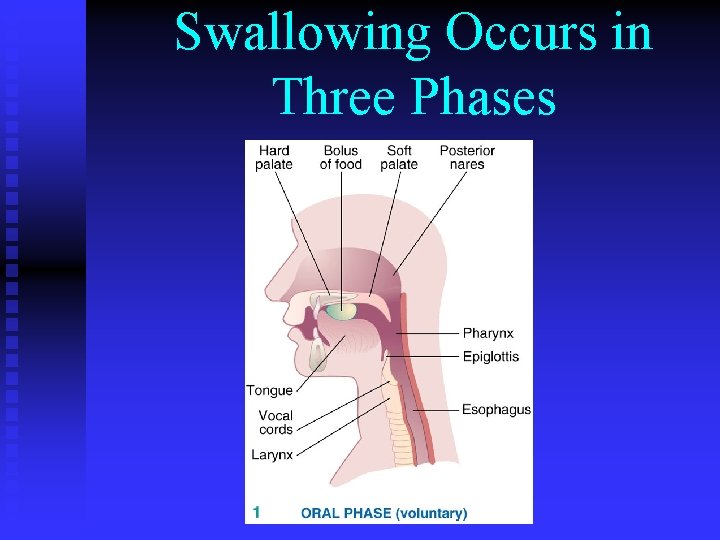
Swallowing Occurs in Three Phases
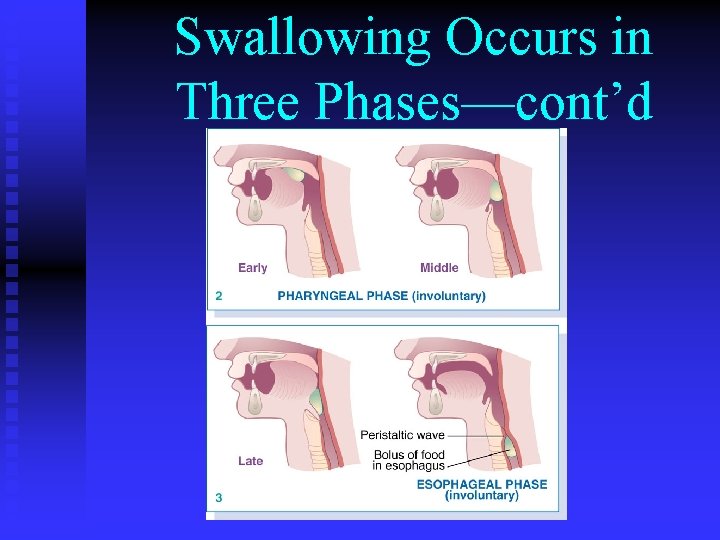
Swallowing Occurs in Three Phases—cont’d
Swallow Animation http: //greenfield. fortunecity. com/rattler/46/upali 4. htm
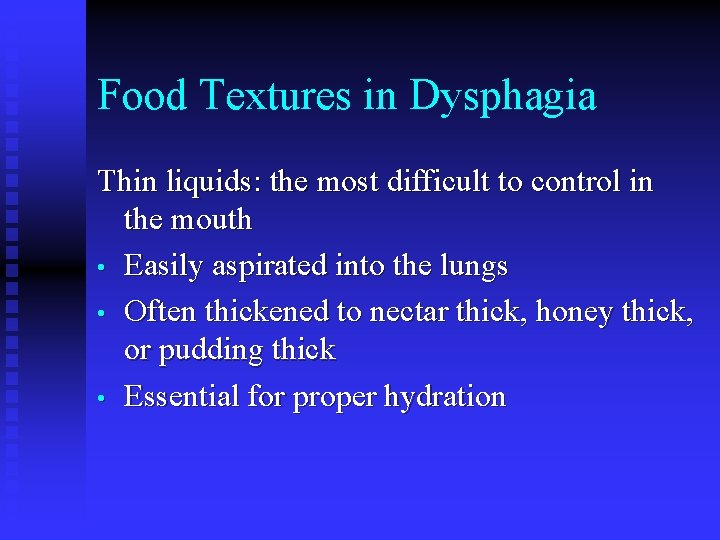
Food Textures in Dysphagia Thin liquids: the most difficult to control in the mouth • Easily aspirated into the lungs • Often thickened to nectar thick, honey thick, or pudding thick • Essential for proper hydration
National Dysphagia Diet Survey • • Diet covered in Oral and Dental Health lecture ADA and ASHA surveyed RDs and SLPs regarding use of NDD 30% had implemented NDD Of those not using it, some were using modifications of it Reported at FNCE 2007; Shirley L. Mc. Callum
Thickened Liquids Issues • • • No consistency across product lines within manufacturers or between competitors Continuous hydration of the thickening agent in pre-thickened products Issues with instant food thickener continuing to thicken
Randomized Study of Two Interventions for Liquid Aspiration Short and Long-term Effects (“Protocol 201”) NIH-Funded Dysphagia Clinical Trial Presented at FNCE, Oct. 2007 Jo. Anne Robbins, Ph. D, CCC-SLP
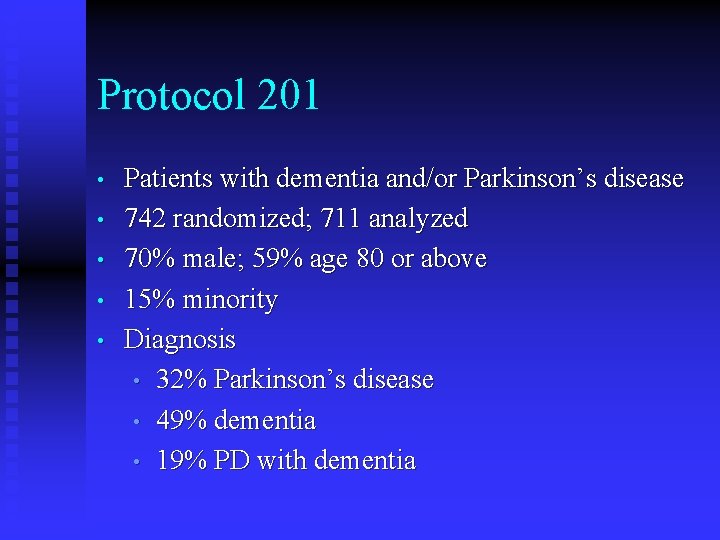
Protocol 201 • • • Patients with dementia and/or Parkinson’s disease 742 randomized; 711 analyzed 70% male; 59% age 80 or above 15% minority Diagnosis • 32% Parkinson’s disease • 49% dementia • 19% PD with dementia
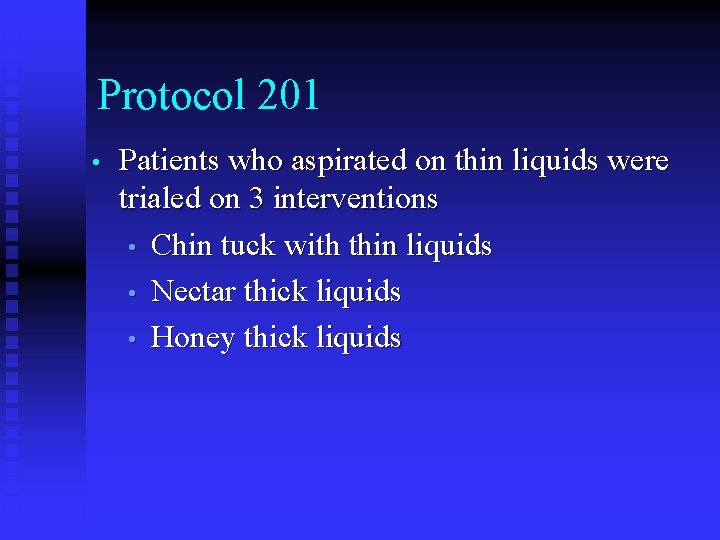
Protocol 201 • Patients who aspirated on thin liquids were trialed on 3 interventions • Chin tuck with thin liquids • Nectar thick liquids • Honey thick liquids
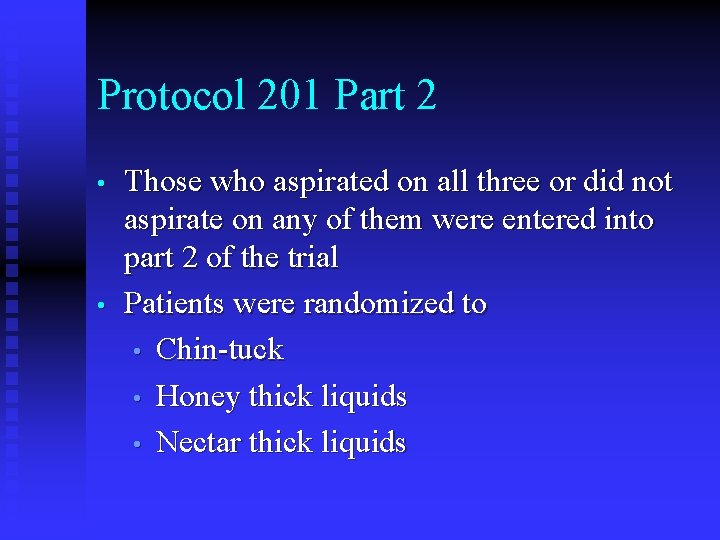
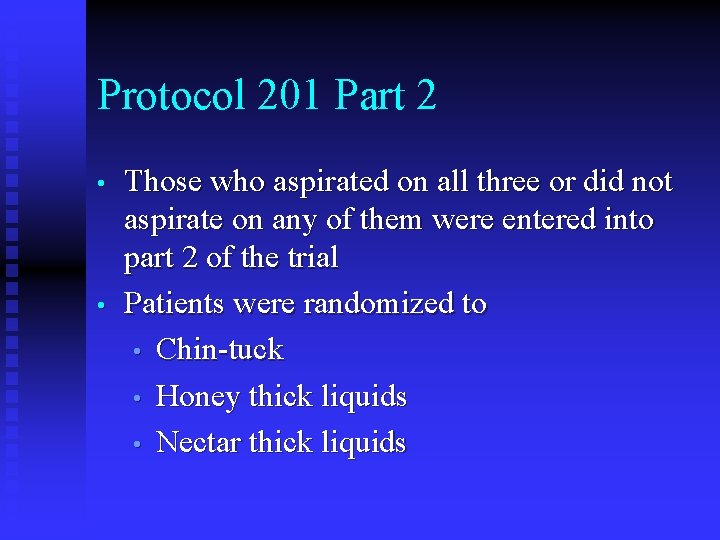
Protocol 201 Part 2 • • Those who aspirated on all three or did not aspirate on any of them were entered into part 2 of the trial Patients were randomized to • Chin-tuck • Honey thick liquids • Nectar thick liquids
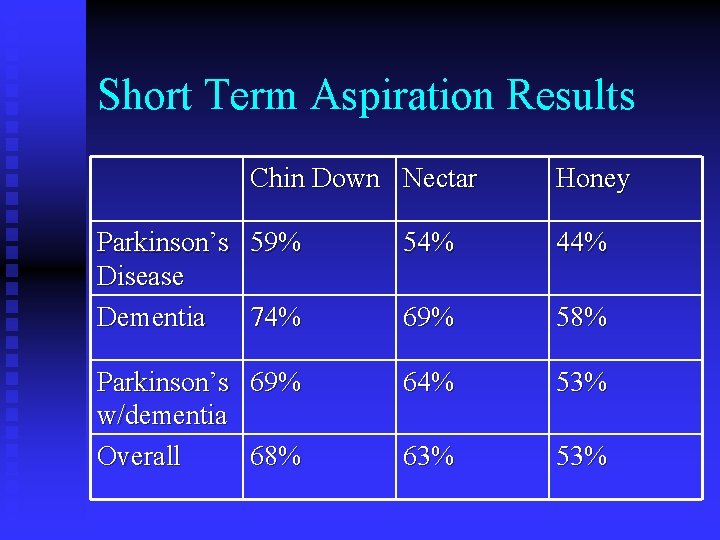
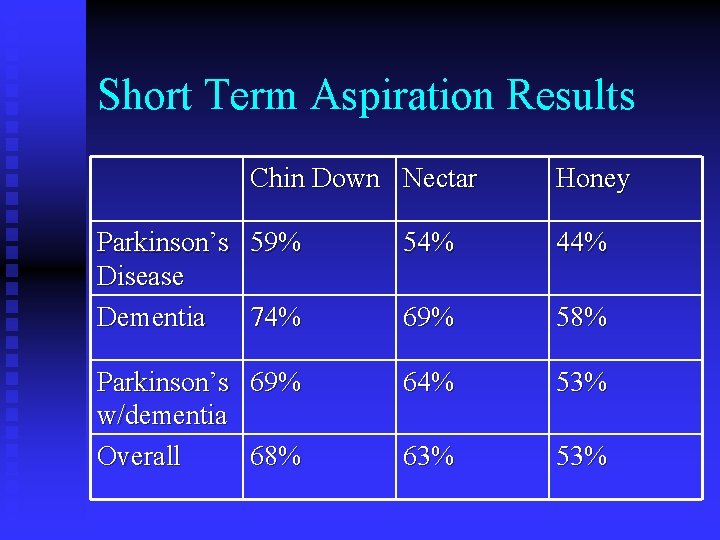
Short Term Aspiration Results Chin Down Nectar Honey Parkinson’s 59% Disease Dementia 74% 54% 44% 69% 58% Parkinson’s 69% w/dementia Overall 68% 64% 53% 63% 53%
Summary • • • Higher proportion of dementia patients aspirated on all interventions Aspiration frequency: Chin down, nectar, then honey Satisfaction: chin down or nectar, then honey
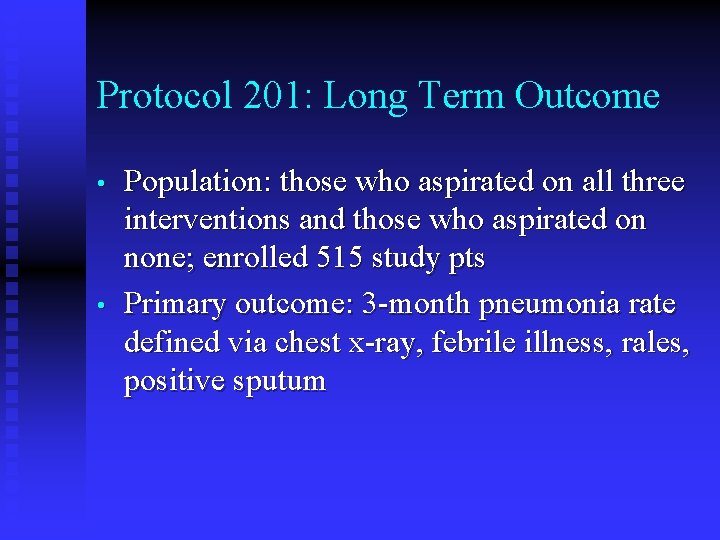
Protocol 201: Long Term Outcome • • Population: those who aspirated on all three interventions and those who aspirated on none; enrolled 515 study pts Primary outcome: 3 -month pneumonia rate defined via chest x-ray, febrile illness, rales, positive sputum
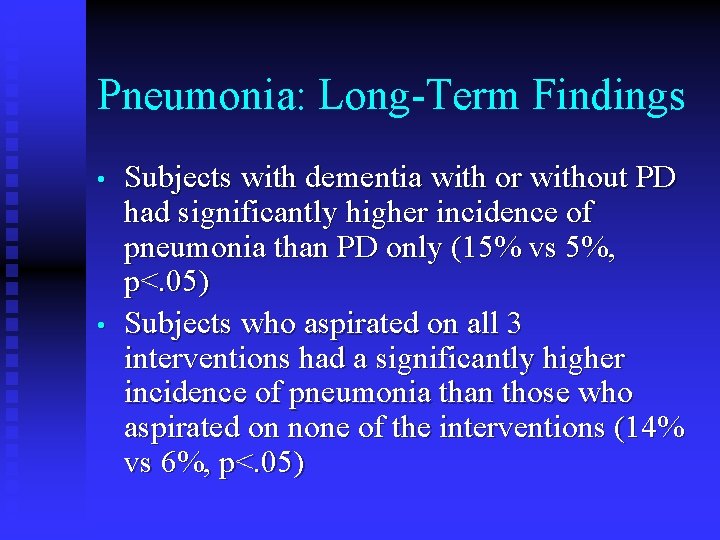
Pneumonia: Long-Term Findings • • Subjects with dementia with or without PD had significantly higher incidence of pneumonia than PD only (15% vs 5%, p<. 05) Subjects who aspirated on all 3 interventions had a significantly higher incidence of pneumonia than those who aspirated on none of the interventions (14% vs 6%, p<. 05)
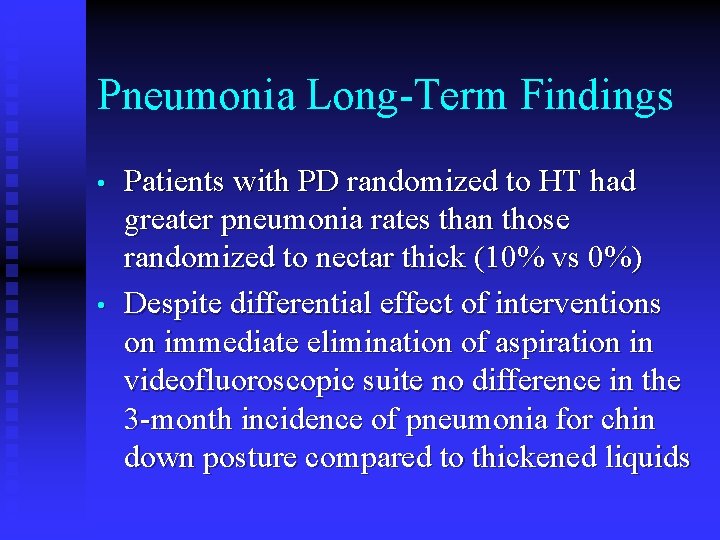
Pneumonia Long-Term Findings • • Patients with PD randomized to HT had greater pneumonia rates than those randomized to nectar thick (10% vs 0%) Despite differential effect of interventions on immediate elimination of aspiration in videofluoroscopic suite no difference in the 3 -month incidence of pneumonia for chin down posture compared to thickened liquids
Current Assumption • • “The thicker the liquid, the safer the swallow. ” Not true in pts who aspirate thick liquids – worse health outcomes
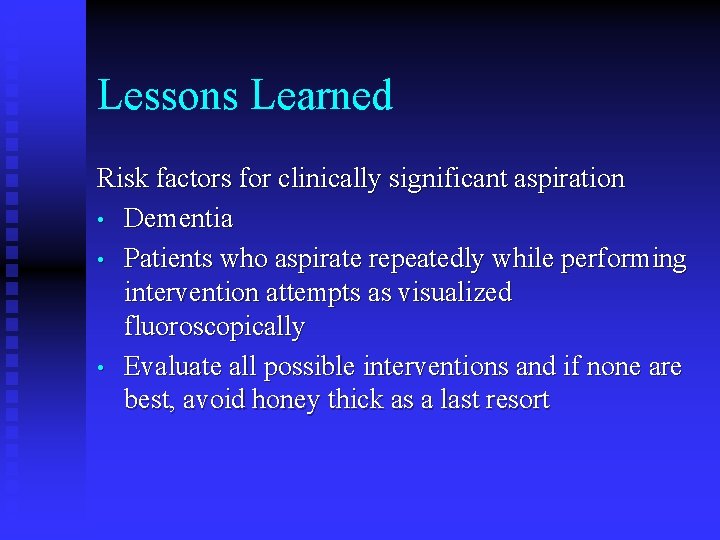
Lessons Learned Risk factors for clinically significant aspiration • Dementia • Patients who aspirate repeatedly while performing intervention attempts as visualized fluoroscopically • Evaluate all possible interventions and if none are best, avoid honey thick as a last resort
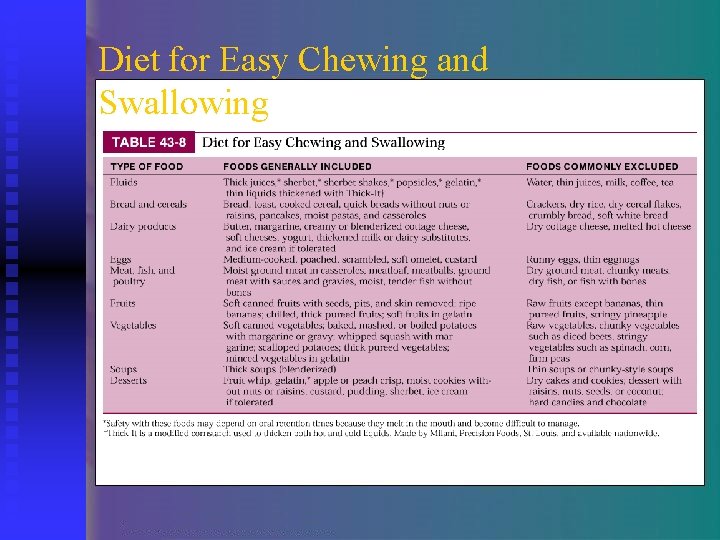
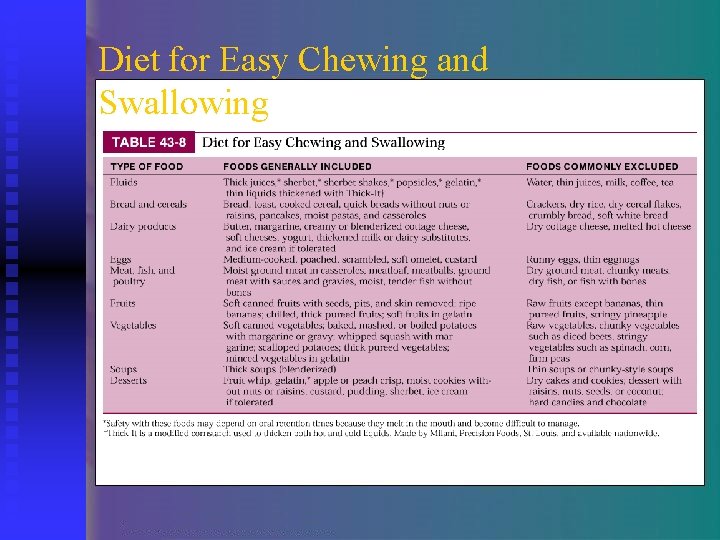
Diet for Easy Chewing and Swallowing
Techniques for Improving Acceptance • • Aroma Seasoning Layering/swirling Piping • • • Molding Slurries Garnishing
Localizing Signs of Mass Lesion • • • Lesions in the central portion of the frontal lobes may cause speech impairment. Lesions of the occipital lobes affect the visual field. Lesions of the cerebellum and brainstem affect the cranial nerves. Lesions in the spinal cord affect motor neurons Lesions of the pituitary gland hypothalamus may induce electrolyte or metabolic abnormalities and/or visual disturbances.
Medical Nutrition Therapy • • Cognitive and swallowing dysfunction usually affect nutritional management and place neurologic patients at risk for malnutrition. The nutritional assessment should emphasize patterns of normal chewing, swallowing, and ingestion in addition to traditional assessment components.
Nutritional Support • Enteral nutrition support is the preferred modality for nutrition support in patients who cannot swallow or eat because of deteriorating neurologic disease.
 Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Small bowel obstruction
Small bowel obstruction Fundamentals of nursing nutrition
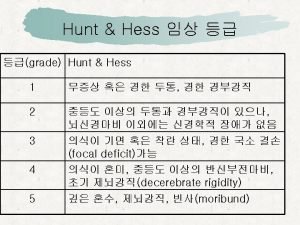
Fundamentals of nursing nutrition Grade wfns
Grade wfns Neuro checks flowsheet
Neuro checks flowsheet Motor function neurological assessment
Motor function neurological assessment What is focal neurological signs
What is focal neurological signs Level of consciousness assessment
Level of consciousness assessment Is adhd a neurological disorder
Is adhd a neurological disorder Muscle power grading scale
Muscle power grading scale Villa fridheim haapsalu
Villa fridheim haapsalu Neurological based behavior
Neurological based behavior Neurological examination
Neurological examination Muscle power neurological examination
Muscle power neurological examination Neurological exam
Neurological exam Contrasting acquisition
Contrasting acquisition Trait theory of criminology
Trait theory of criminology Snowdon neurological rehabilitation unit
Snowdon neurological rehabilitation unit Fudoscopy
Fudoscopy Neurological disease
Neurological disease Uw neurological surgery
Uw neurological surgery Normal pressure hydrocephalus triad
Normal pressure hydrocephalus triad Glasgow coma scale video
Glasgow coma scale video Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Humanistic therapies aim to boost
Humanistic therapies aim to boost Medical family therapy
Medical family therapy Family therapy part 2
Family therapy part 2 Ossr physical therapy
Ossr physical therapy Ptal california medical board
Ptal california medical board Gbmc infoweb
Gbmc infoweb Hepburn osteometric board
Hepburn osteometric board Torrance memorial cardiac rehab
Torrance memorial cardiac rehab Cartersville medical center medical records
Cartersville medical center medical records Part whole model subtraction
Part whole model subtraction Unit ratio definition
Unit ratio definition Part part whole
Part part whole Part by part technical description example
Part by part technical description example What are the 3 parts of the bar
What are the 3 parts of the bar The part of a shadow surrounding the darkest part
The part of a shadow surrounding the darkest part Minitab adalah
Minitab adalah Health and social care level 3 unit 14
Health and social care level 3 unit 14 Physiological disorders unit 14
Physiological disorders unit 14 Neurocognitive disorder
Neurocognitive disorder Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders The flinders model
The flinders model Assistive technology for emotional and behavioral disorders
Assistive technology for emotional and behavioral disorders Somatization disorder
Somatization disorder Egodystonic
Egodystonic Types of sensory disorders
Types of sensory disorders Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Chapter 18 psychological disorders review worksheet
Chapter 18 psychological disorders review worksheet Different personality disorders
Different personality disorders Paranoid personality disorder
Paranoid personality disorder Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Avoidant personality disorder
Avoidant personality disorder Dsm v personality disorders
Dsm v personality disorders Group c personality disorders
Group c personality disorders Cluster c
Cluster c Cluster traits
Cluster traits Anankastic personality disorder
Anankastic personality disorder Eat disorder york
Eat disorder york Neurotic stress related and somatoform disorders
Neurotic stress related and somatoform disorders Neurocognitive disorders
Neurocognitive disorders