Selected Neurological and Respiratory Disorders Neurological Disorders Muscle
- Slides: 45
Selected Neurological and Respiratory Disorders
Neurological Disorders • • • Muscle Paralysis Neural Tube Disorders Cerebrovascular Accidents (Stroke) Transient Ischemia Attack Aneurysm
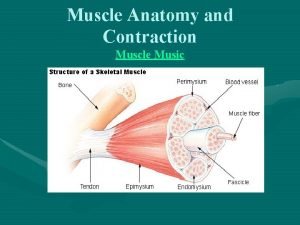
Muscle Paralysis • Flaccid paralysis – – – Destruction of motor neurons by disease Interruption of reflex arc responsible for muscle tone Muscle deprived of innervation Low muscle tone Peripheral nerve destruction • Spastic paralysis – – Reflex arc not disturbed Injury to cortical neurons stops voluntary control Muscle retains innervation Increased muscle tone
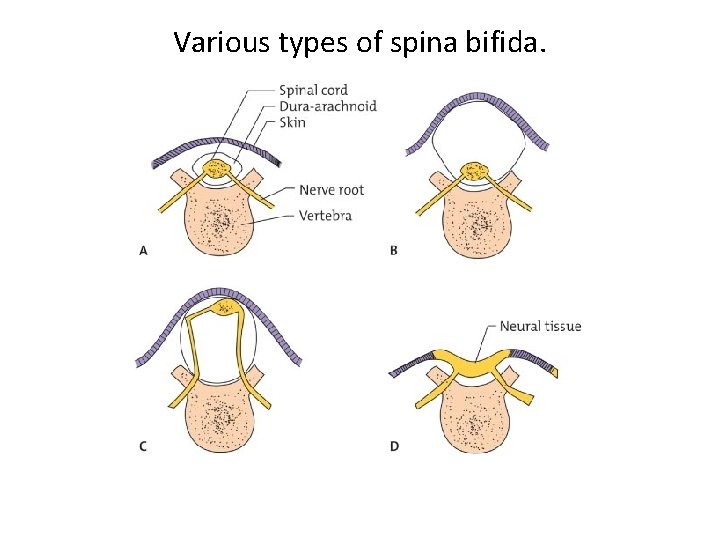
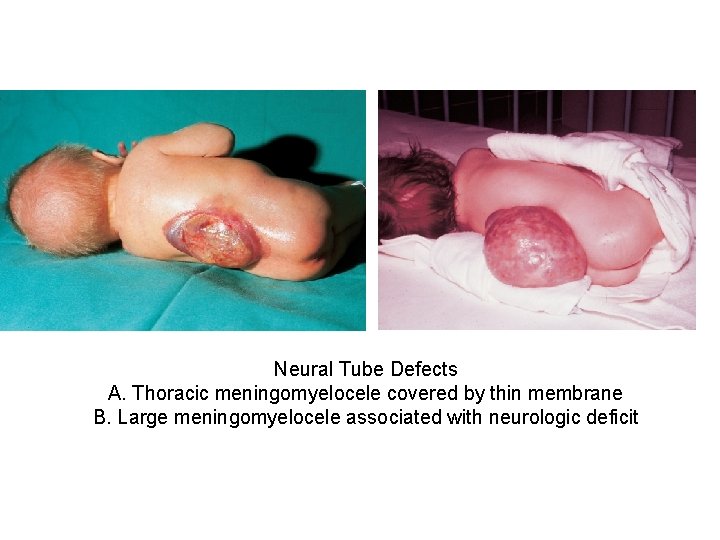
Neural Tube Defects • Anencephaly – Failure of normal development of brain and cranial cavity – Multifactorial inheritance • Spina bifida – Diagnosis: amniocentesis and alpha-fetoprotein levels – Alpha-fetoprotein leaks from fetal blood into amnionic fluid through open neural tube defect; high levels found in amnionic fluid • Occult • Meningocele • Meningomyelocele
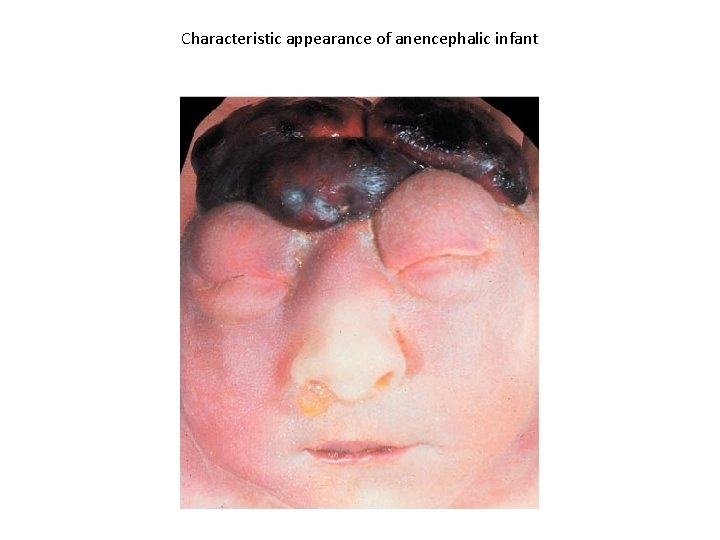
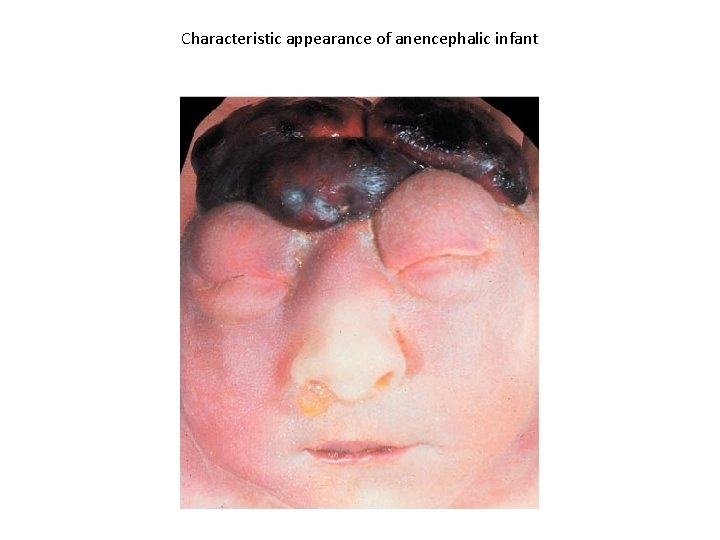
Characteristic appearance of anencephalic infant
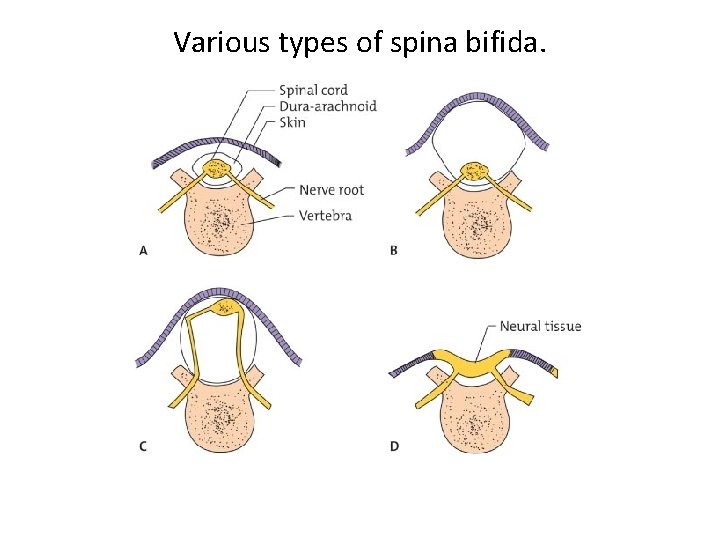
Various types of spina bifida.
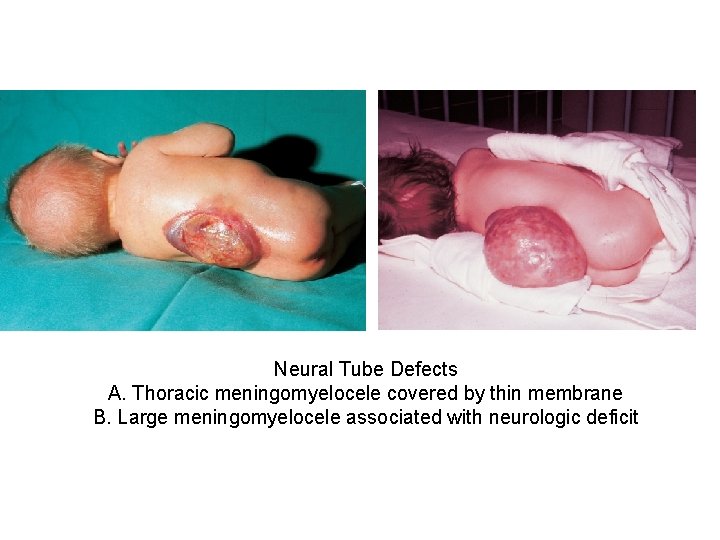
Neural Tube Defects A. Thoracic meningomyelocele covered by thin membrane B. Large meningomyelocele associated with neurologic deficit
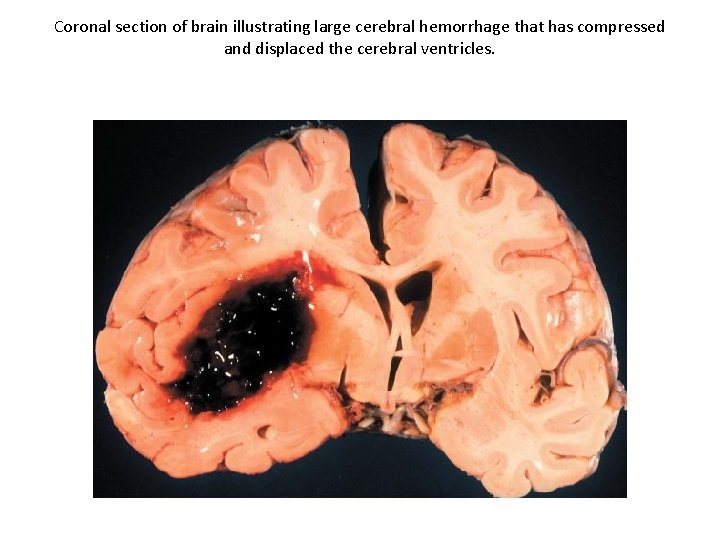
Stroke: Cerebrovascular Accident (1 of 5) • Any injury to brain tissue from disturbance of blood supply to brain • Types of stroke – Cerebral thrombosis: most common; thrombosis of cerebral artery narrowed by arteriosclerosis – Cerebral embolus: occurs less frequently; blockage of cerebral artery by fragment of blood clot from an arteriosclerotic plaque or from heart – Cerebral hemorrhage: most serious type of stroke; usually from rupture of a cerebral artery in person with hypertension
Stroke: Cerebrovascular Accident (2 of 5) • Predisposing Factors – 1. Mural thrombus formed on wall of left ventricle adjacent to a healing myocardial infarction – 2. Thrombus formed on rough surface of diseased mitral or aortic valve – 3. Small thrombus in left atrium of person with atrial fibrillation
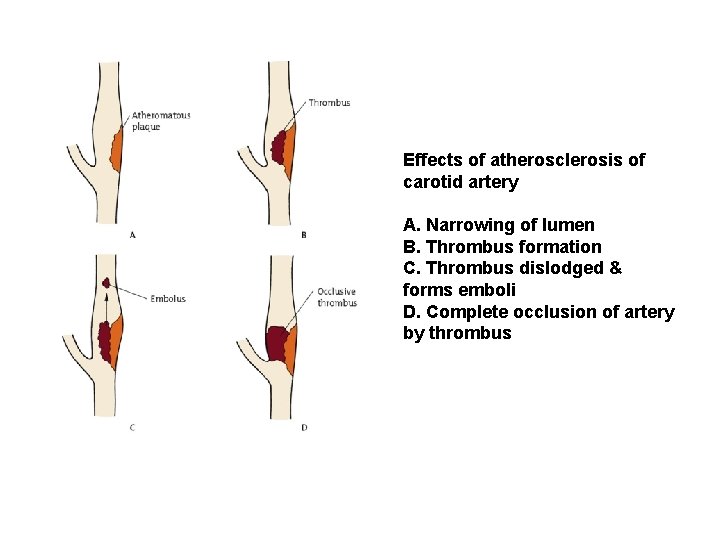
Stroke: Cerebrovascular Accident (3 of 5) • Ischemic infarct: no blood leaks into brain • Hemorrhagic infarct: blood leaks into damaged brain tissue • Arteriosclerosis of extracranial arteries – Sclerosis of a major artery from aorta that supply brain – Common affected site: carotid artery in neck; arteriosclerotic plaque may narrow lumen and reduce cerebral blood flow
Stroke: Cerebrovascular Accident (4 of 5) • Diagnosis – Cerebral angiogram – Carotid endarterectomy – Less invasive methods: similar to balloon angioplasty and stent insertion procedures used to treat coronary artery plaques
Stroke: Cerebrovascular Accident (5 of 5) • CT scan: can distinguish a cerebral infarct from cerebral hemorrhage • Magnetic resonance imaging (MRI): provides similar information and is equally effective
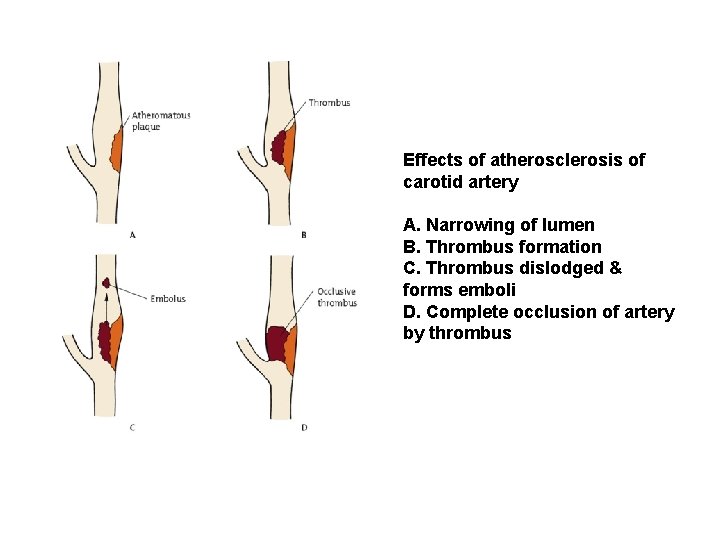
Effects of atherosclerosis of carotid artery A. Narrowing of lumen B. Thrombus formation C. Thrombus dislodged & forms emboli D. Complete occlusion of artery by thrombus
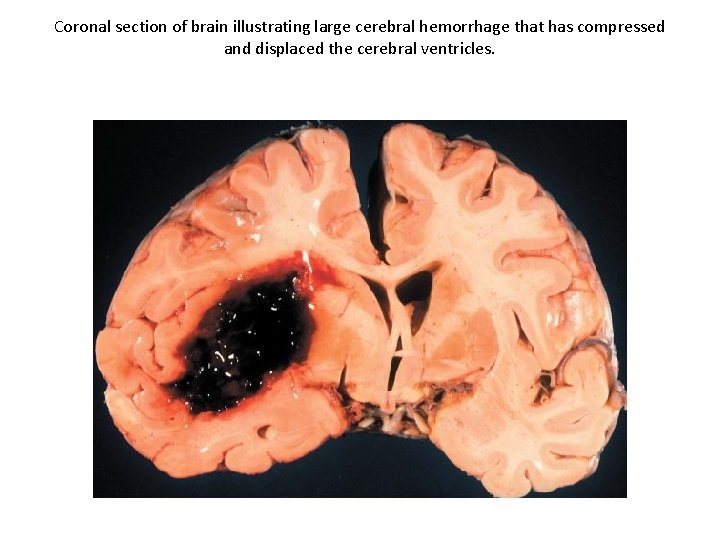
Coronal section of brain illustrating large cerebral hemorrhage that has compressed and displaced the cerebral ventricles.
Transient Ischemic Attack, TIA • Brief episodes of neurologic disfunction – From embolization of material from plaque in carotid artery – One-third of patients eventually suffer major stroke • Treatment: endarterectomy or medical therapy
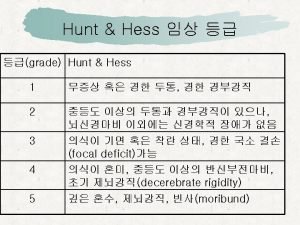
Cerebral Aneurysm • Congenital aneurysm of circle of Willis – – – Congenital weakness in arterial wall allows lining to protrude Weakness is congenital but aneurysm develops in adult life Rupture causes subarachnoid hemorrhage Hypertension predisposes Treatment: aneurysm occluded surgically • Arteriosclerotic aneurysm – Cerebral artery dilates and compresses adjacent tissue – Rupture uncommon
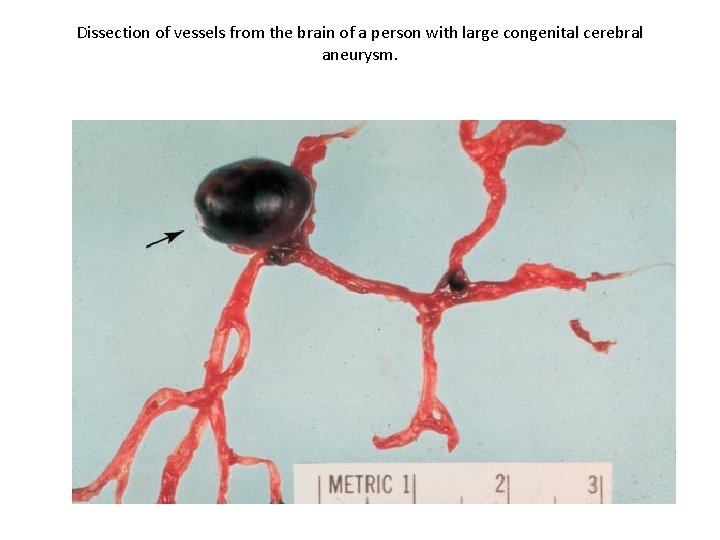
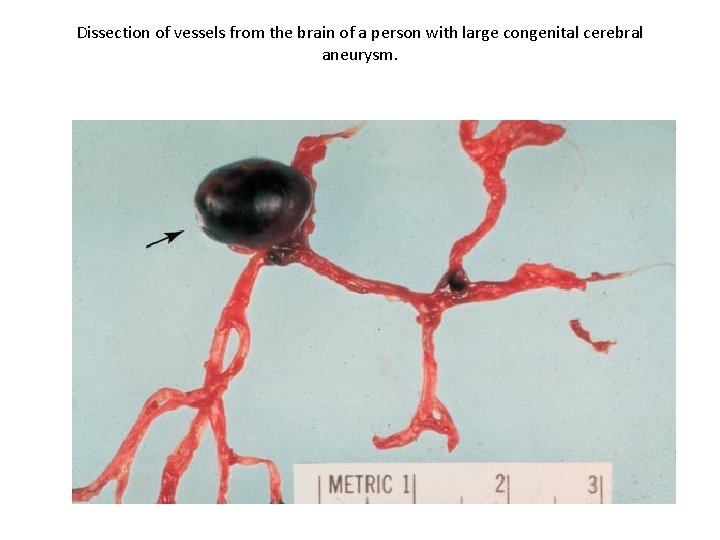
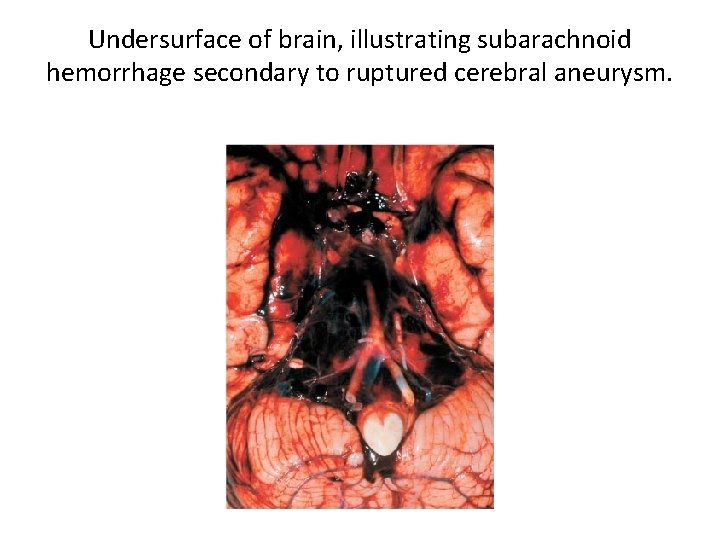
Dissection of vessels from the brain of a person with large congenital cerebral aneurysm.
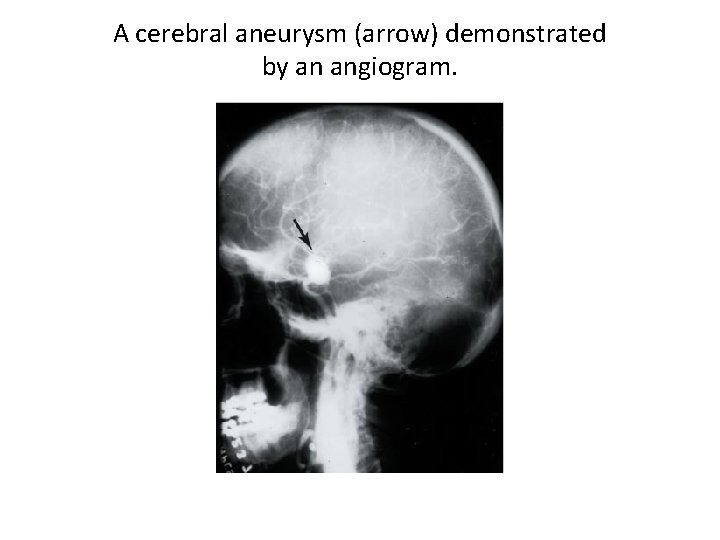
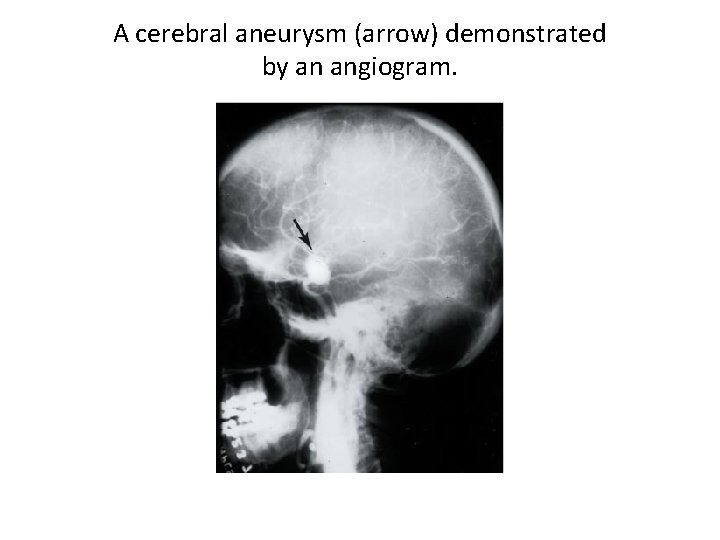
A cerebral aneurysm (arrow) demonstrated by an angiogram.
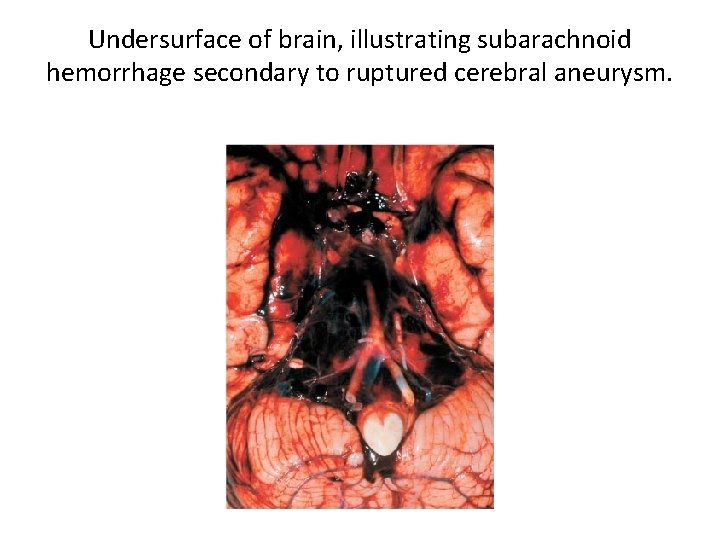
Undersurface of brain, illustrating subarachnoid hemorrhage secondary to ruptured cerebral aneurysm.
Respiratory Disorders Pneumothorax Atelectasis Pneumonia Tuberculosis Bronchitis Chronic Obstructive Pulmonary Disease (COPD) Emphysema Bronchial Asthma
Pneumothorax Pathogenesis/Manifestations Pathogenesis • Lung injury or pulmonary disease that allows air to escape into the pleural space • Stab wound or penetrating injury to the chest wall • Spontaneous – generally in young healthy persons Manifestations • Chest pain • Shortness of breath • Air in pleural cavity • Tension pneumothorax
Tension Pneumothorax • Development of a higher than atmospheric pressure in the pleural cavity – creating a tension • Can accompany type of pneumothorax • Upon inhalation air enters pleural space – due to drop in intrapleural pressure • On exhalation – air gets trapped due to the edges of the tear compressing as a result of the increased intrapleural pressure – thus the pressure in the intrapleural space is getting greater and greater • Heart and Mediastinal structures shifted away from pneumothorax
Atelectasis An incomplete expansion of the lung, a collapse of a part of the lung There are two types 1. Obstructive atelectasis: complete bronchial obstruction by • Mucous secretions, tumor, foreign object • Resulting in collapse of the part of the lung supplied by the blocked bronchus • Can also develop as a postoperative complication, where because of the pain, the patient does not cough or breathe deeply, accumulating mucous secretions
Atelectasis 2. Compression atelectasis – External compression on the lung • Fluid, air, or blood in the pleural cavity, reducing its volume and preventing lung expansion
Pneumonia An inflammation of the lung • The exudate spreads unimpeded through the lung • Filling the alveoli • The affected portions of the lung become relatively solid (consolidation) • At times, the exudate reaches the pleural surface
Pneumonia Classification 1. Etiology: most important because it serves as a guide for treatment – Bacteria, chlamydia, mycoplasmas, rickettsiae, viruses, fungi 2. Anatomic distribution of the inflammatory processdescribes what part of the lung is involved – Lobar: entire lung (bacteria, neutrophil infiltration) – Bronchopneumonia (bacteria, neutrophil infiltration): parts of one or more lobes adjacent to the bronchi – bronchopulmonary segments
Pneumonia Classification – Interstitial pneumonia or primary atypical pneumonia (virus or mycoplasma; lymphocyte, monocyte, and plasma cell infiltration): alveolar septa affected 3. Predisposing factors that lead to its development • Any condition associated with poor lung ventilation and retention of bronchial secretions – Postoperative – atelectasis and secondary bacterial infection – Aspiration – Obstruction
– Clinical features of pneumonia • Manifestations of systemic infection – Feeling ill – Elevated temperature – Increased white blood cell count • Manifestations of lung inflammation – – Cough Purulent sputum Pain on respiration if involves pleura Shortness of breath
Tuberculosis • It is a special type of pneumonia caused by Mycobacterium tuberculosis – an acid – fast bacteria • Because the tubercle bacillus has a capsule composed of waxes and fatty substances, it is more resistant to destruction than others – thick cell wall • As a result of this organism’s resistance – monocytes accumulate around the bacteria – many fuse with the bacteria attempting phagocytosis – but the fusion produces a large multinucleated “giant cell”. Lymphocytes and plasma cells surround the area – followed by fibrous tissue proliferation. The central portion becomes necrotic – thus a granuloma is formed. TB is termed a granulomatous disease.
– Manifestations • Course of infection – Acquired from organisms inhaled in airborne droplets – Organisms lodge within pulmonary alveoli where they proceed to multiply – Initially the organisms do not elicit a marked inflammatory reaction because they do not produce any toxins or destructive enzymes – Macrophage phagocytose the bacteria but are unable to destroy them – they may even carry the organisms to other parts of the lung and into regional lymph nodes. – After several weeks cell-mediated immunity develops – Sensitized T- cytotoxic lymphocytes attract and activate macrophages – the activated macrophages attack and destroy many of the organisms forming the characteristic granulomas formed – In the majority of cases the person is unaware they have been infected – no symptoms – Infection arrested in majority of cases • Outcome depends – Number of organisms inhaled – State of body’s defenses – May heal by scarring or progress to cavitation
• Sometimes the granuloma is large enough to be seen on X-ray but most of the times it is too small • The positive skin test reveals the infection • Cell-mediated immunity generally controls the infection • The healed granuloma may contain small numbers of viable organisms and the infection may become reactivated when the immune system drops • In some individuals the primary infection does not respond favorably to the immune system fight • The granuloma may extend into a nearby bronchus and necrotic inflammatory tissue is discharged into it • A cavity may form • If the person gets reactivation of the bacteria (becomes active) and they have cavitation (into bronchus) their sputum can be infectious to others
• Most cases of active TB do not result from the initial infection – but rather by a reactivation – however some are due to a reinfection (new case) • How does reactivation occur- it is due to a drop in the immune system action as a result of AIDS, other debilitating diseases, treatment with corticosteroids, treatment with immunosuppressive therapy
• Extrapulmonary tuberculosis – Result of hematogenous spread of tubercle bacilli – thus a secondary infection – Sites » Kidneys » Bone » Uterus » Fallopian tubes Sometimes the secondary infection may progress even though the pulmonary infection has healed leading to an active extrapulmonary TB without clinically apparent pulmonary TB
Tuberculosis Diagnosis – Skin test (Mantoux): a positive test reveals recent infection – chest x-ray: when the granuloma is large enough to be detected – or see pulmonary infiltrates – sputum culture – acid fast bacteria
• The tuberculosis skin test (also known as the tuberculin test or PPD test) is a test used to determine if someone has developed an immune response to the bacterium that causes tuberculosis (TB). This response can occur if someone currently has TB, if they were exposed to it in the past, or if they received the BCG vaccine against TB (which is not performed in the U. S. ). • The tuberculin skin test is based on the fact that infection with M. tuberculosis produces a delayed-type hypersensitivity skin reaction to certain components of the bacterium.
Tuberculosis Treatment • Cell-mediated immunity generally controls the infection • The healed granulomas, however, may contain small numbers of viable organisms, and the infection may become reactivated • Not all primary infections respond as favorably – If a large number of organisms are inhaled or if the host is compromised (body’s defenses are inadequate), the inflammation will progress, causing more destruction of lung tissue
Tuberculosis – People who have active progressive tuberculosis with a tuberculous cavity can infect others because they can discharge large numbers of tubercle bacilli in the sputum – Treatment • Antibiotics and Chemotherapeutic agents • Drug-resistant tuberculosis treatment – More prolonged – Results less satisfactory • Drugs recommended – Following conversion of a negative into positive skin test reaction – Patients with inactive tuberculosis who have increased risk •
Bronchitis An inflammation of the tracheobronchial mucosa • Acute bronchitis – Common and self-limiting • Chronic bronchitis – often associated with emphysema in COPD – Secondary to chronic irritation by smoking or atmospheric pollution
• Bronchiectasis – Walls weakened by inflammation and dilate – Distended bronchi retain secretions » Chronic cough » Production of large amounts of purulent sputum – Diagnosed with bronchogram – A specialized X-ray which consists of taking films after instilling a radiopaque oil into the trachea and bronchi. The oil covers the mucosa of the bronchi, and the abnormal bronchi can be recognized as dilated – Only effective treatment is surgical resection of affected segments of lung
• Upper Respiratory System – From nose and mouth down to Lungs – (includes nose, mouth, pharynx, larynx, and trachea • Lower Respiratory System – Mainstem bronchus to Alveoli • Upper Airway – From nose and mouth to and inclusive of larynx (voice box) • Lower Airway – Trachea down to alveoli
Chronic Obstructive Pulmonary Disease • • Emphysema and chronic bronchitis occur together so frequently that they are usually considered a single entity, designated COPD Emphysema is characterized by loss of elasticity (increased pulmonary compliance) of the lung tissue caused by destruction of structures feeding the alveoli • Chronic bronchitis – Secondary to chronic irritation by smoking or atmospheric pollution Clinical manifestations • Dyspnea • Cyanosis
• • • Emphysema The air spaces distal to the terminal bronchioles are enlarged and their walls are destroyed The normally fine alveolar structure of the lung is destroyed The large cystic air spaces form throughout the lung The destructive process usually begins in the upper lobes but eventually may affect all lobes Once emphysema has developed, the damaged lungs cannot be restored to normal
Bronchial Asthma • Spasmodic contraction of smooth muscles in the walls of the smaller bronchi and bronchioles • It causes shortness of breath and wheezing respiration • Exerts a greater effect on expiration than on inspiration • Attacks are precipitated by allergens: inhalation of dust, pollens, animal dander, or other allergens • Treated with drugs such as epinephrine or theophylline that relax bronchospasms and block the release of mediators from mast cells
• Bronchial Asthma – Pathogenesis • Spasmodic contraction of smooth muscles in walls of smaller bronchi and bronchioles • Associated with increased secretions from bronchial mucous glands – Clinical manifestations • Shortness of breath • Wheezing respirations • Air flow impeded more on expiration than on inspiration – Air trapped in lungs – Lungs become overinflated
– Attacks precipitated by allergens • Interact with mast cells coated with Ig. E antibody • Release chemical mediators that induce bronchospasm – Treatment • Drugs that relax bronchospasm – Epinephrine – Theophylline • Drugs that block release of mediators from mast cells
 Neurological examination
Neurological examination Muscle power neurological examination
Muscle power neurological examination Respiratory zone vs conducting zone
Respiratory zone vs conducting zone Esoohagus
Esoohagus Muscle refractory period
Muscle refractory period Powerful shoulder abductor used to raise the arm overhead
Powerful shoulder abductor used to raise the arm overhead Wfns scale
Wfns scale Neuro checks pupil size
Neuro checks pupil size Motor function neurological assessment
Motor function neurological assessment What is focal neurological signs
What is focal neurological signs Trapezium squeeze
Trapezium squeeze Is adhd a neurological disorder
Is adhd a neurological disorder Haapsalu neurological rehabilitation centre
Haapsalu neurological rehabilitation centre Neurological based behavior
Neurological based behavior Neurological examination
Neurological examination Ao classification system
Ao classification system Compare and contrast first and second language acquisition
Compare and contrast first and second language acquisition Trait theory in criminology
Trait theory in criminology Stoneham centre physiotherapy
Stoneham centre physiotherapy Fudoscopy
Fudoscopy Neurological disease
Neurological disease Uw neurosurgery residents
Uw neurosurgery residents Normal pressure hydrocephalus triad
Normal pressure hydrocephalus triad Neurological observations glasgow coma scale
Neurological observations glasgow coma scale Qualitative vs quantitative data analysis
Qualitative vs quantitative data analysis Qualitative quantitative
Qualitative quantitative Removes selected text and places it on the clipboard
Removes selected text and places it on the clipboard 8255 control word
8255 control word Survivorship curve for k selected species
Survivorship curve for k selected species Selected response questions
Selected response questions Vba combobox selected item
Vba combobox selected item K selected species survivorship curve
K selected species survivorship curve Example of r selected species
Example of r selected species Weights of the backpacks of first graders on a school bus
Weights of the backpacks of first graders on a school bus Ann arbor mi population pyramid
Ann arbor mi population pyramid Neither of my two suitcases is adequate for this trip
Neither of my two suitcases is adequate for this trip Delete it
Delete it Selected response tasks
Selected response tasks Congratulations you have been selected
Congratulations you have been selected Three randomly selected households are surveyed 2 6 7
Three randomly selected households are surveyed 2 6 7 K selected
K selected R-selected species
R-selected species Aluminum ion symbol
Aluminum ion symbol Definition of measures of dispersion
Definition of measures of dispersion Gwen harwood: selected poems
Gwen harwood: selected poems Dreamweaver php extensions
Dreamweaver php extensions