Medical Nutrition Therapy for Renal Disorders Functions of














- Slides: 86
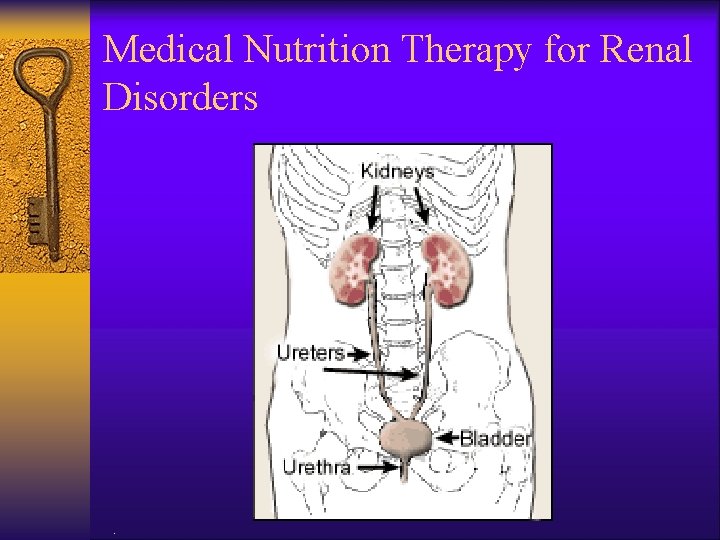
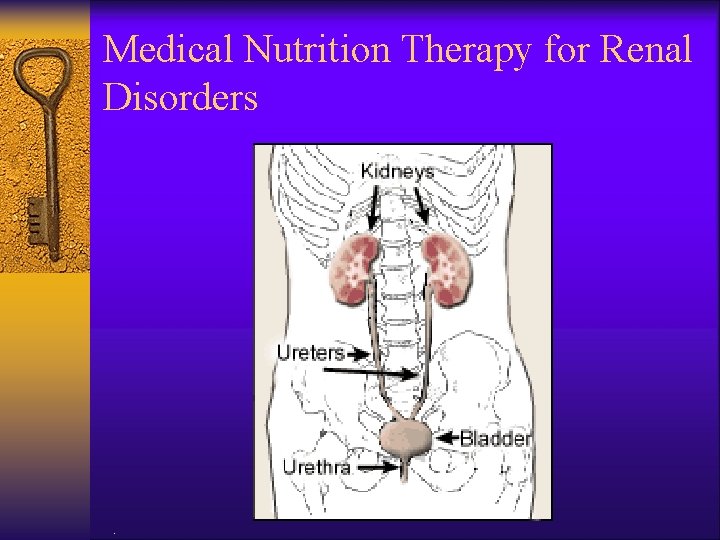
Medical Nutrition Therapy for Renal Disorders .
Functions of the Kidney ¨ Excretory ¨ Acid-base balance ¨ Endocrine ¨ Fluid and electrolyte balance .
Excretory Functions ¨ Removal of excess fluid and waste products ¨ 180 L of filtrate pass through the kidneys each day producing 1 -2 L of urine ¨ Wastes excreted from the body in urine include urea (byproduct of protein metabolism); excess vitamins and minerals; metabolites of some drugs and poisons .
Acid-Base Functions ¨ Acid-base balance is maintained through a buffer system, which maintains blood at p. H of 7. 4 ¨ Bicarbonate carries hydrogen ions to the kidneys where they are removed from extracellular fluid in the tubules, returned to the bloodstream as needed ¨ Phosphate buffers intracellular fluid Source: Byham-Gray, Wiesen, eds. A Clinical Guide to Nutrition Care in Kidney Disease. ADA, 2004.
Acid-Base Balance Functions ¨ When fluid volume is low, anti-diuretic hormone (ADH) or vasopressin is released from the anterior pituitary; increases absorption of water in the collecting duct ¨ When extracellular volume (ECV) decreases, the renin-angiotensin-aldosterone system is activated excretes less sodium chloride Source: Byham-Gray, Wiesen, eds. A Clinical Guide to Nutrition Care in Kidney Disease. ADA, 2004.
Endocrine Functions ¨ 1, 25 -dihydroxy-vitamin D 3 or calcitriol is produced in the kidney; enhances calcium absorption ¨ Activation of Vitamin D and excretion of excess phosphate maintain healthy bones ¨ Erythropoietin: acts on the bone marrow to increase production of red blood cells Source: Byham-Gray, Wiesen, eds. A Clinical Guide to Nutrition Care in Kidney Disease. ADA, 2004.
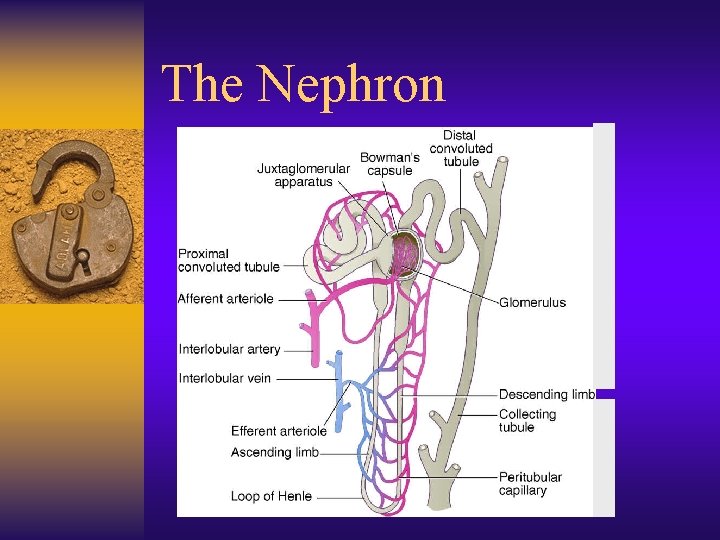
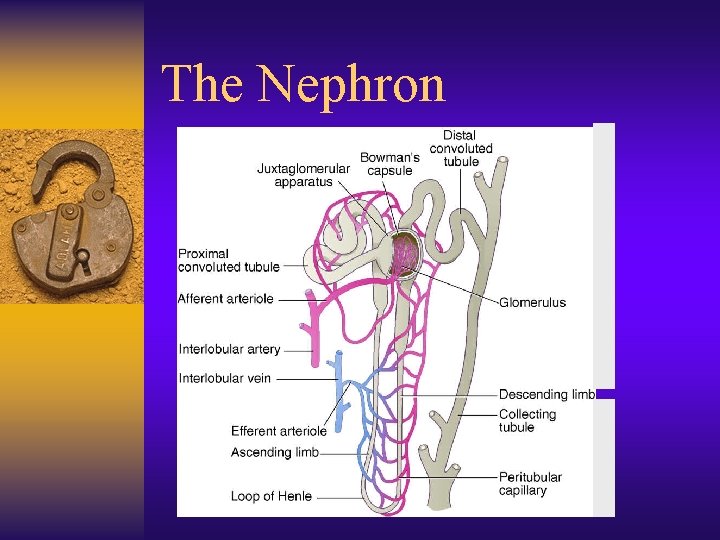
The Nephron
The Most Common Kidney Diseases ¨ Diabetic Nephropathy damage to the nephrons in the kidneys from unused sugar in the blood, usually due to Diabetes. ¨ High Blood Pressure can damage the small blood vessels in the kidneys. The damaged vessels cannot filter poison from the blood as they are supposed to. ¨ Polycystic Kidney Disease (PKD) is a hereditary kidney disease in which many cysts grow in the kidneys. These cysts may lead to kidney failure. .
The Most Common Kidney Diseases ¨ Acute Renal Failure - Sudden kidney failure caused by blood loss, drugs or poisons. If the kidneys are not seriously damaged, acute renal failure may be reversed. ¨ Chronic Renal Failure - Gradual loss of kidney function is called Chronic Renal Failure or Chronic Renal Disease. ¨ End-Stage Renal Disease - The condition of total or nearly total and permanent kidney failure. .
Kidney Diseases ¨ Glomerular diseases – Nephrotic syndrome – Nephritic syndrome—tubular or interstitial ¨ Tubular defects – Acute renal failure (ARF) ¨ Other – End-stage renal disease (ESRD) – Kidney stones .
Nephrotic Syndrome ¨ Alterations of the glomerular basement membrane allows persistent loss of large amounts of protein in the urine ¨ Associated with diabetes, glomerulonephritis, amyloidosis, lupus ¨ High risk for cardiovascular disease ¨ Hypercoagulability ¨ Abnormal bone metabolism .
Nephrotic Syndrome ¨ Albuminuria: more than 3 g/day urinary albumin losses, with proportionally lesser amounts for children ¨ Hypoalbuminemia ¨ Hypertension ¨ Hyperlipidemia ¨ Edema .
Medical Mgt of Nephrotic Syndrome ¨ Corticosteroids ¨ Immunosuppressants ¨ ACE inhibitors/angiotensin receptor blockers to reduce protein losses, control blood pressure and fluid balance ¨ Coenzyme A reductase inhibitors to control hyperlipidemia .
MNT in Nephrotic Syndrome ¨ ¨ ¨ Protein 0. 8 to 1 g/kg IBW 80% HBV Sodium based on fluid status Potassium and other minerals (calcium, phosphorus) monitored and individualized Fluid unrestricted Diet therapy probably not effective for hyperlipidemia; may require medication Byham-Gray L, Wiesen K. A clinical guide to nutrition care in kidney disease. ADA, 2004.
Nephritic syndrome ¨ Acute glomerulonephritis (inflammation of the glomerulus ¨ Sudden onset, often after streptococcus infections ¨ Symptoms include hematuria, hypertension ¨ Usually resolve on their own or advance to nephrotic syndrome or ESRD .
Nephritic syndrome: Nutritional Management ¨ Diet to treat underlying disease ¨ Restrict diet if necessary to control symptoms ¨ Protein restricted in uremia ¨ Sodium restriction in hypertension ¨ Potassium restriction in hyperkalemia .
Acute Renal Failure ¨ Rapid, often reversible deterioration of renal function ¨ GFR declines over hours to days ¨ Most commonly occurs during hospitalization (5% of hospitalized pts; 30% of ICU pts) ¨ Associated with major in-hospital morbidity and mortality (7 to 80%) Byham-Gray L, Wiesen K. A clinical guide to nutrition care in kidney disease. ADA, 2004.
Causes of Acute Renal Failure ¨ Pre-renal: caused by intravascular volume depletion, decreased cardiac output ¨ Post-renal: benign prostatic hypertrophy, prostate cancer, cervical cancer, colorectal cancer, neurogenic bladder, urethral strictures ¨ Intrinsic or parenchymal ARF: vascular disease, interstitial nephritis, glomerular disease, acute tubular necrosis Byham-Gray L, Wiesen K. A clinical guide to nutrition care in kidney disease. ADA, 2004.
Causes of Acute Renal Failure ¨ Ischemic Injury (50% of all incidence) d/t loss of blood supply to the kidneys secondary to surgical complications, thrombosis, hypotension, hypovolemia ¨ Nephrotoxic injury: medications, contrast medium, chemotherapy, poisons (35%) ¨ Multiorgan system failure, particularly liver failure ¨ Sepsis, especially bacterial ¨ Obstructive uropathy (trauma during surgery, urolithiasis, enlarged prostate) ¨ Acute glomerular nephritis.

Acute Tubular Necrosis Most common cause of ARF ¨ Ischemia: due to major surgery, hypotension, cardiogenic, septic, or hypovolemic shock ¨ Nephrotoxicity: drugs, chemotherapeutic agents, organic solvents, heavy metals, cocaine .
Acute Tubular Necrosis Initiating phase ¨ Period between onset and established renal failure ¨ Usually reversible by treating the underlying disorder or removing offending agent ¨ Time frame: hours or days Byham-Gray L, Wiesen K. A clinical guide to nutrition care in kidney disease. ADA, 2004.
Acute Tubular Necrosis Maintenance Phase ¨ Epithelial cell injury ¨ Urine output is at its lowest; complications associated with uremia, fluid overload, electrolyte imbalance (decreased sodium, increased potassium levels) ¨ Time frame: 10 -16 days in oliguric patients; 5 -8 days in nonoliguric patients.

Acute Tubular Necrosis Recovery Phase ¨ Tubule cell regeneration and gradual return of GFR ¨ BUN and creatinine return to near normal ¨ May be complicated by marked diuresis, dehydration and fluid and electrolyte imbalance (increased sodium, decreased potassium) ¨ Time frame: days to months.
Renal Replacement Therapies in ARF ¨ Recommended for patients with pronounced azotemia, electrolyte imbalance, fluid overload, severe acidosis ¨ Used in 85% of patients with oliguric ARF and 30% of nonoliguric ¨ Purpose is to correct imbalances as well as provide sufficient renal support to other organs.
Renal Replacement Therapies in ARF ¨ Hemodialysis: standard treatment if patient is hemodynamically stable – However, risk of hypotension and wide swings in body weight in unstable patients ¨ Continuous hemofiltration provides slow, continuous filtration across a membrane, driven by arterial pressure or pump .

Renal Replacement Therapies in ARF ¨ Continuous hemodialysis , uses an ultrafiltrate fluid similar to plasma – Clearance occurs through diffusion from high concentration (blood) to low concentration ¨ Peritoneal dialysis: less often used in the US; not as effective when large volume or solute clearances needed. .
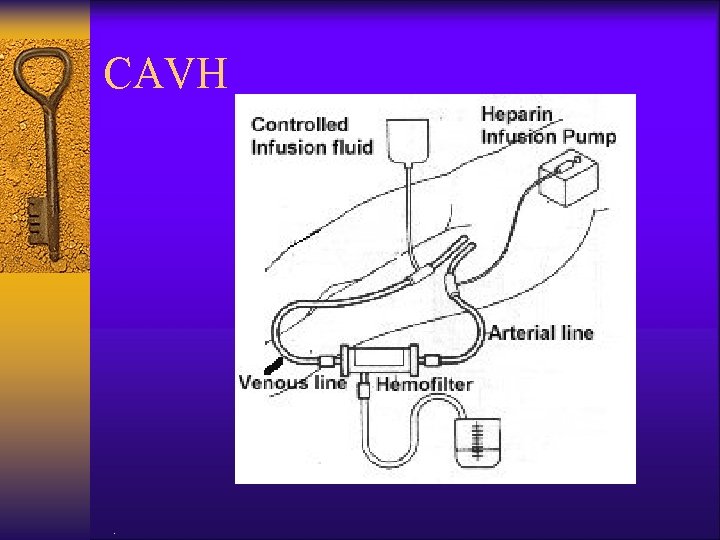
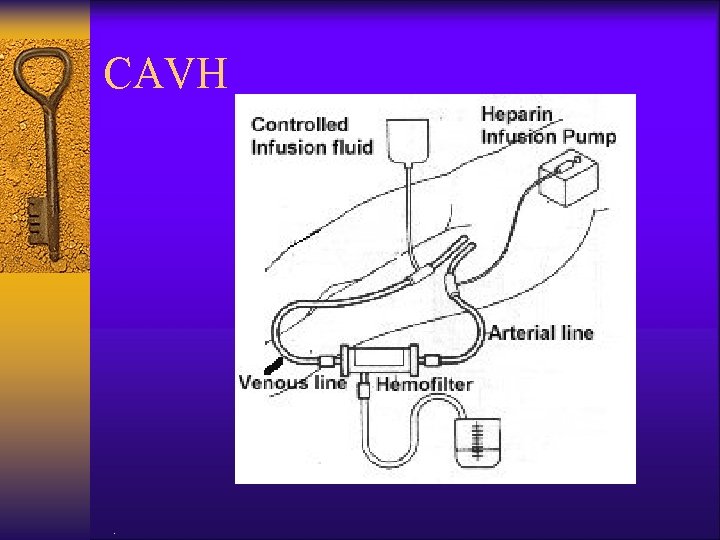
CAVH .
Chronic Kidney Disease .
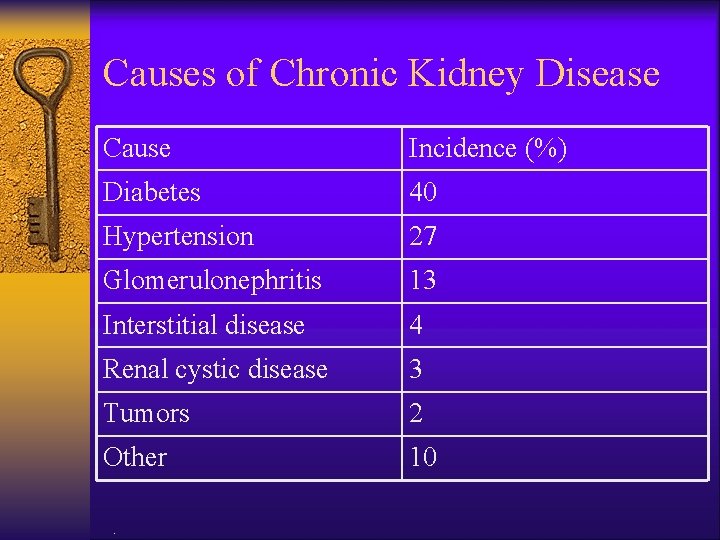
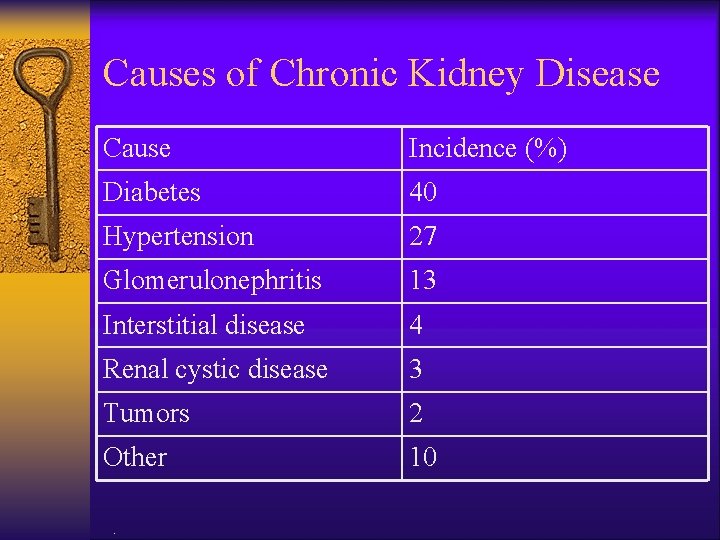
Causes of Chronic Kidney Disease Cause Incidence (%) Diabetes 40 Hypertension 27 Glomerulonephritis 13 Interstitial disease 4 Renal cystic disease 3 Tumors 2 Other 10 .
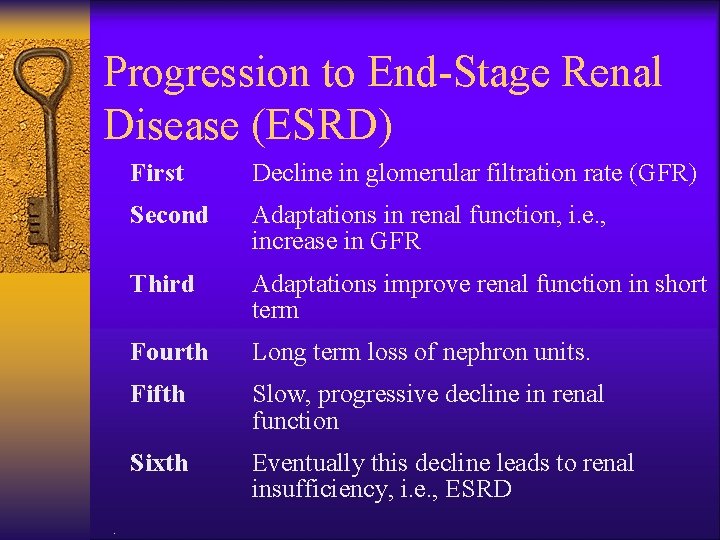
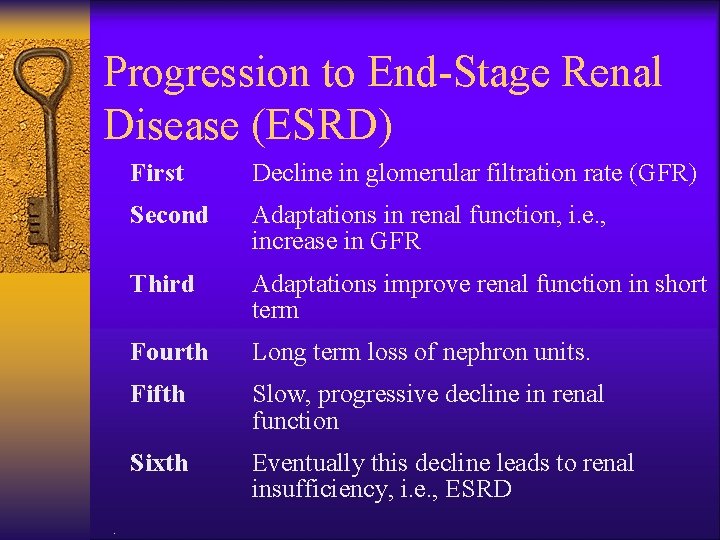
Progression to End-Stage Renal Disease (ESRD) . First Decline in glomerular filtration rate (GFR) Second Adaptations in renal function, i. e. , increase in GFR Third Adaptations improve renal function in short term Fourth Long term loss of nephron units. Fifth Slow, progressive decline in renal function Sixth Eventually this decline leads to renal insufficiency, i. e. , ESRD
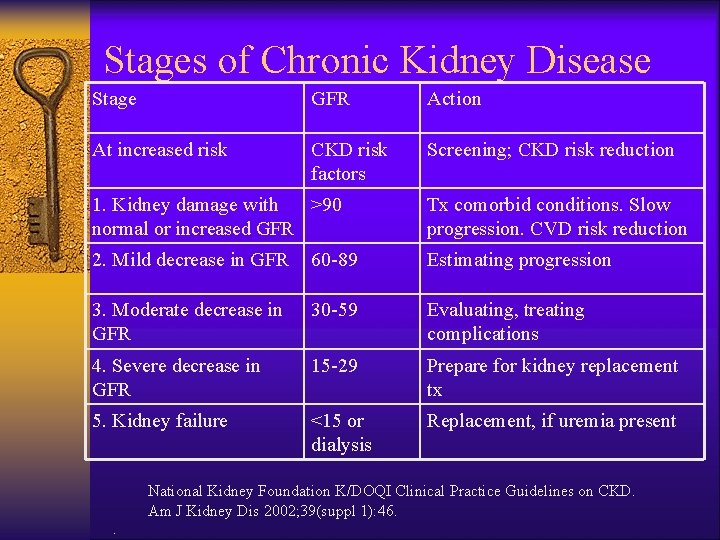
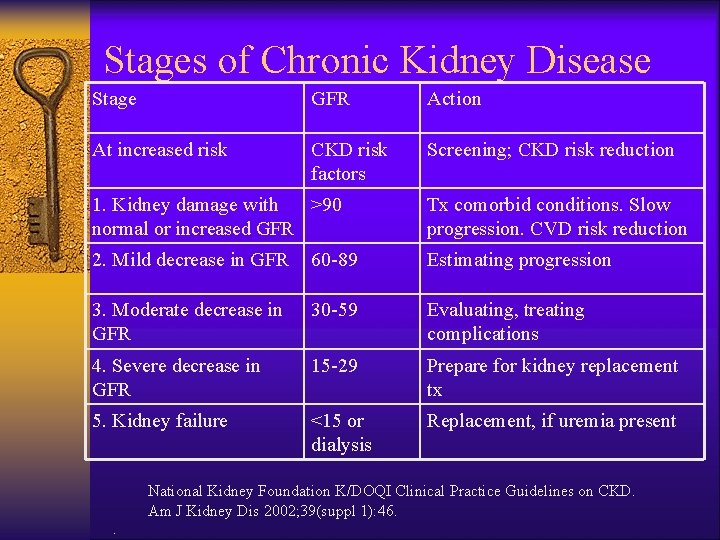
Stages of Chronic Kidney Disease Stage GFR Action At increased risk CKD risk factors Screening; CKD risk reduction 1. Kidney damage with >90 normal or increased GFR Tx comorbid conditions. Slow progression. CVD risk reduction 2. Mild decrease in GFR 60 -89 Estimating progression 3. Moderate decrease in GFR 30 -59 Evaluating, treating complications 4. Severe decrease in GFR 15 -29 Prepare for kidney replacement tx 5. Kidney failure <15 or dialysis Replacement, if uremia present National Kidney Foundation K/DOQI Clinical Practice Guidelines on CKD. Am J Kidney Dis 2002; 39(suppl 1): 46. .

ESRD: Medical Management ¨ Dialysis ¨ Immunosuppressant drugs ¨ Kidney transplant ¨ Psychological support .
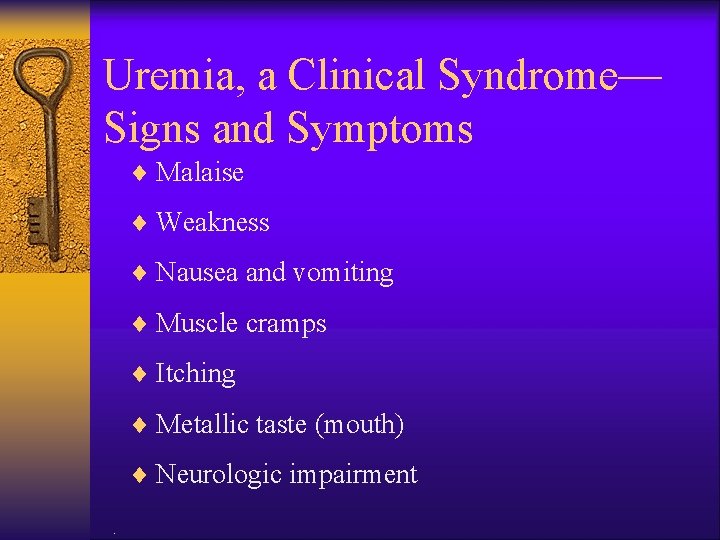
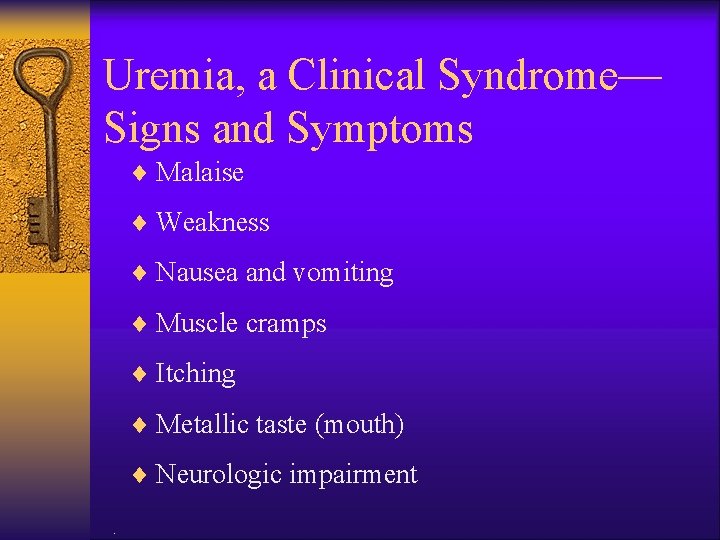
Uremia, a Clinical Syndrome— Signs and Symptoms ¨ Malaise ¨ Weakness ¨ Nausea and vomiting ¨ Muscle cramps ¨ Itching ¨ Metallic taste (mouth) ¨ Neurologic impairment.
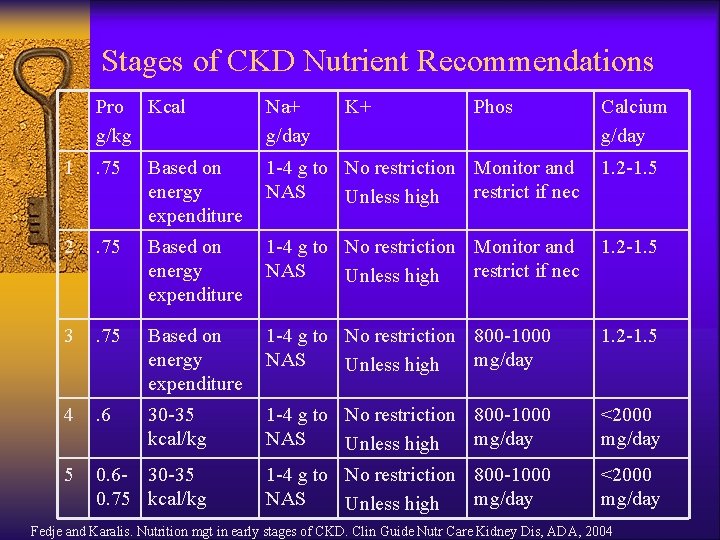
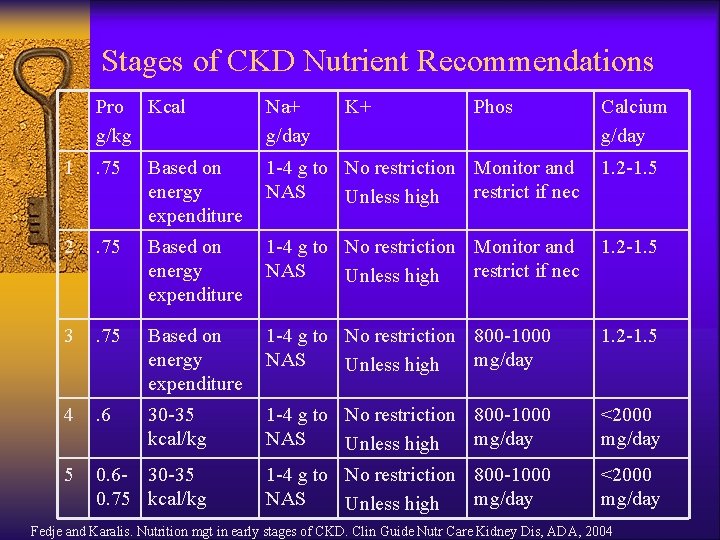
Stages of CKD Nutrient Recommendations Pro Kcal g/kg Na+ g/day K+ Phos Calcium g/day 1 . 75 Based on energy expenditure 1 -4 g to No restriction Monitor and NAS restrict if nec Unless high 1. 2 -1. 5 2 . 75 Based on energy expenditure 1 -4 g to No restriction Monitor and NAS restrict if nec Unless high 1. 2 -1. 5 3 . 75 Based on energy expenditure 1 -4 g to No restriction 800 -1000 NAS mg/day Unless high 1. 2 -1. 5 4 . 6 30 -35 kcal/kg 1 -4 g to No restriction 800 -1000 NAS mg/day Unless high <2000 mg/day 5 0. 6 - 30 -35 0. 75 kcal/kg 1 -4 g to No restriction 800 -1000 NAS mg/day Unless high <2000 mg/day . Fedje and Karalis. Nutrition mgt in early stages of CKD. Clin Guide Nutr Care Kidney Dis, ADA, 2004
Nutrition Assessment and Monitoring in the CKD Pt .
Anthropometric Measurements ¨ % usual body weight (%UBW) ¨ % standard body weight (%SBW) ¨ Height ¨ Skeletal frame size ¨ BMI ¨ Skinfold thickness ¨ Mid-arm muscle area, circumference, or diameter .
Blood Urea Nitrogen (BUN) ¨ Measure of the nitrogenous waste products of protein ¨ High BUN in CKD may reflect high protein intake, GI bleeding or inadequate dialysis, increased catabolism due to infection, surgery, poor nutrition ¨ Decreased BUN may mean protein anabolism, overhydration, protein loss, low dietary protein Source: Byham-Gray, Wiesen, eds. A Clinical Guide to Nutrition Care in Kidney Disease. ADA, 2004.
Creatinine (nl 0. 5 -1. 4 mg/d. L) ¨ Nitrogenous waste product of muscle metabolism ¨ Produced proportionate to muscle mass ¨ Unrelated to dietary protein intake (DPI) ¨ Sensitive marker of renal function: the higher the serum creatinine, the greater the loss of renal function; may reflect inadequate dialysis or muscle catabolism ¨ A decrease in creatinine over time may reflect loss of lean body mass Source: Byham-Gray, Wiesen, eds. A Clinical Guide to Nutrition Care in Kidney Disease. ADA, 2004.
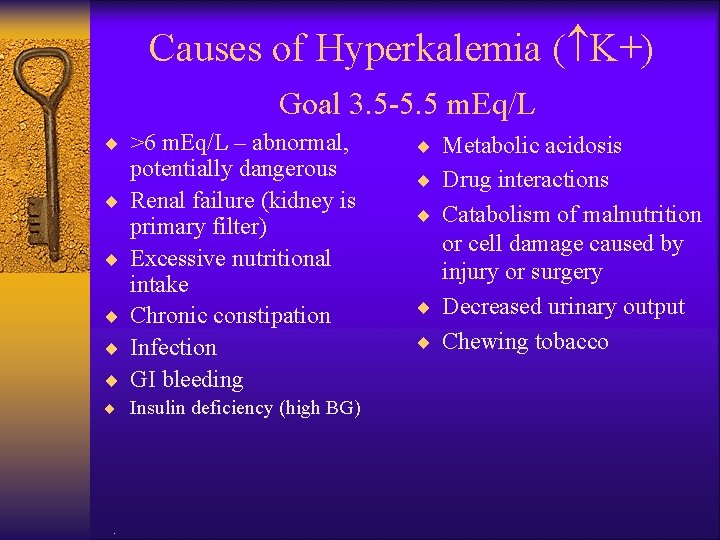
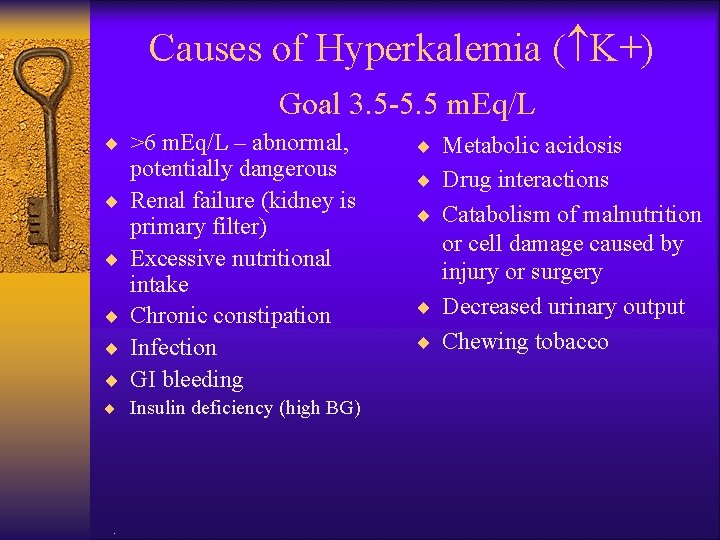
Causes of Hyperkalemia ( K+) Goal 3. 5 -5. 5 m. Eq/L ¨ >6 m. Eq/L – abnormal, ¨ ¨ ¨ potentially dangerous Renal failure (kidney is primary filter) Excessive nutritional intake Chronic constipation Infection GI bleeding ¨ Insulin deficiency (high BG) . ¨ Metabolic acidosis ¨ Drug interactions ¨ Catabolism of malnutrition or cell damage caused by injury or surgery ¨ Decreased urinary output ¨ Chewing tobacco
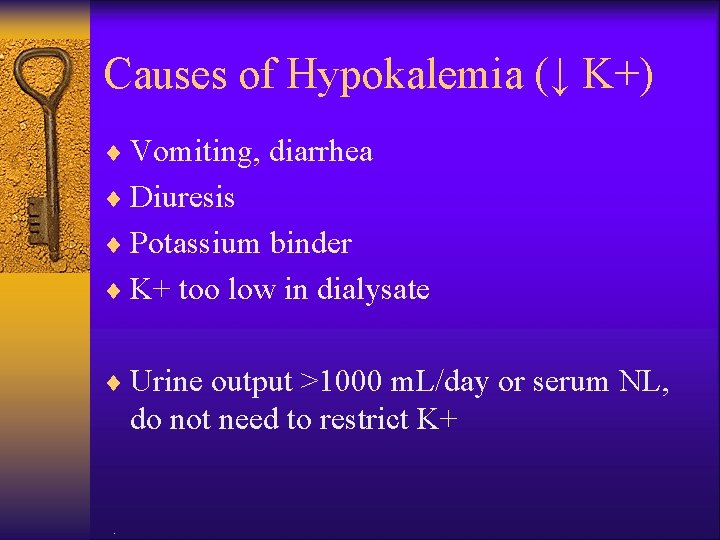
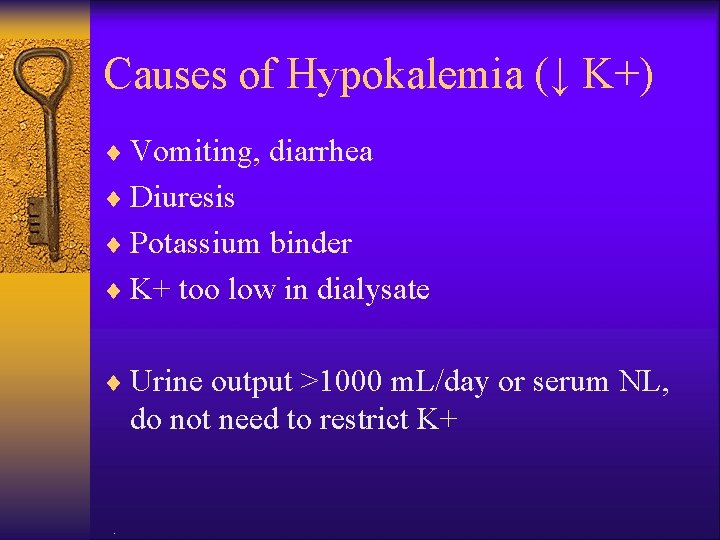
Causes of Hypokalemia (↓ K+) ¨ Vomiting, diarrhea ¨ Diuresis ¨ Potassium binder ¨ K+ too low in dialysate ¨ Urine output >1000 m. L/day or serum NL, do not need to restrict K+ .
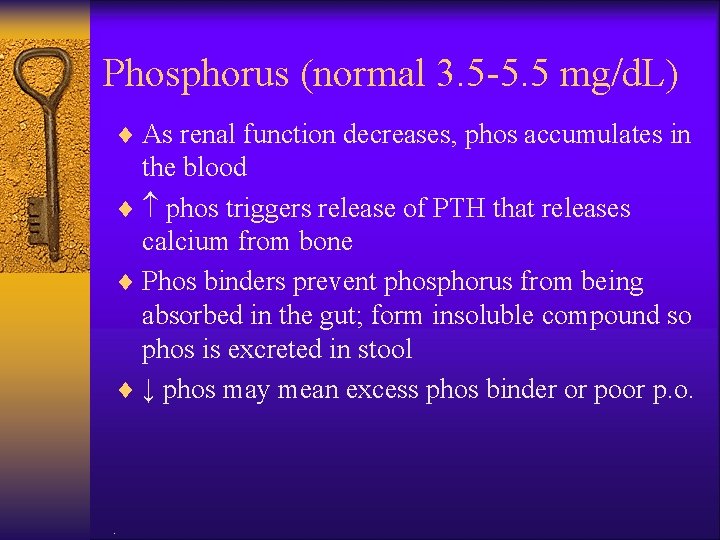
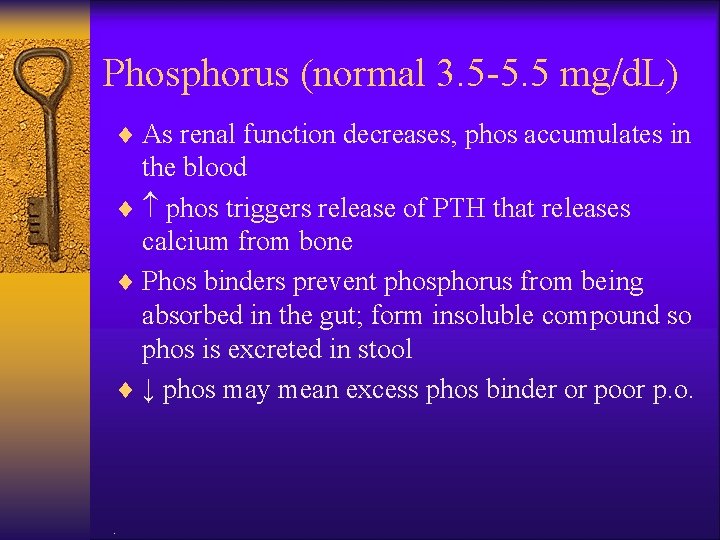
Phosphorus (normal 3. 5 -5. 5 mg/d. L) ¨ As renal function decreases, phos accumulates in the blood ¨ phos triggers release of PTH that releases calcium from bone ¨ Phos binders prevent phosphorus from being absorbed in the gut; form insoluble compound so phos is excreted in stool ¨ ↓ phos may mean excess phos binder or poor p. o. .
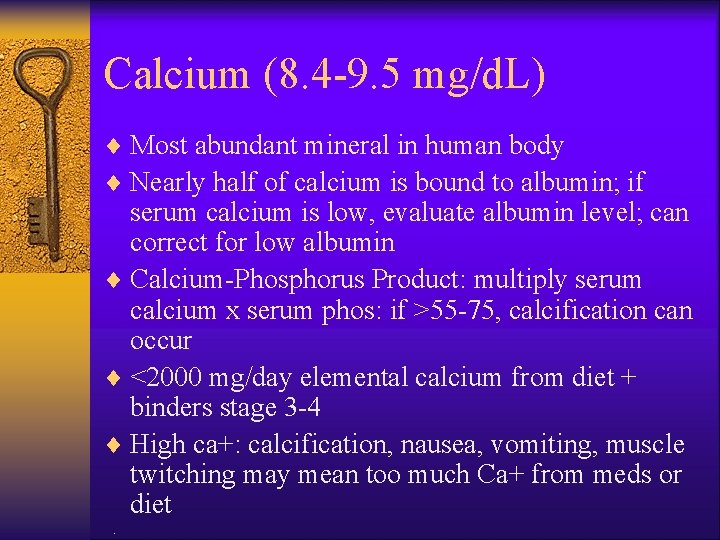
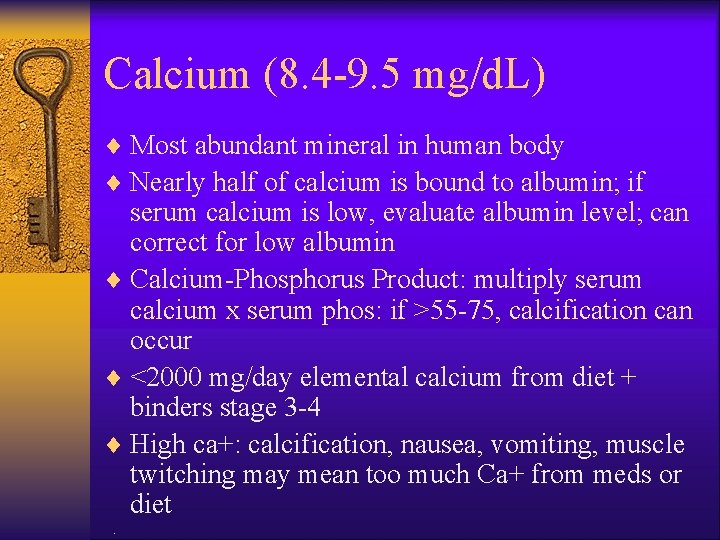
Calcium (8. 4 -9. 5 mg/d. L) ¨ Most abundant mineral in human body ¨ Nearly half of calcium is bound to albumin; if serum calcium is low, evaluate albumin level; can correct for low albumin ¨ Calcium-Phosphorus Product: multiply serum calcium x serum phos: if >55 -75, calcification can occur ¨ <2000 mg/day elemental calcium from diet + binders stage 3 -4 ¨ High ca+: calcification, nausea, vomiting, muscle twitching may mean too much Ca+ from meds or diet.
Serum Sodium (nl 133 -145 m. Eq/L) ¨ Not a reliable indicator of sodium intake in CKD ¨ Fluid retention due to decreased urine production can dilute an elevated level ¨ Serum levels must be evaluated in conjunction with fluid status .
Lipids ¨ Cardiovascular disease is the most common cause of death in people with CKD ¨ Kidney disease is considered the equivalent of a risk factor, like diabetes ¨ HD: often have normal LDL, TC, ↑ triglycerides, ↓ HDL ¨ PD: have ↑ LDL/TC + ↑ TG ¨ Renal Tx: ↑ LDL/TC/TG, normal HDL, often due to medications.
Cholesterol in CKD ¨ High • High risk TC 200 -300 mg/dl (non-fasting) • LDL goal < 100 mg/dl ¨ Low • <150 -180, evaluate for pro-energy malnutrition • Increased mortality .
Hematological Indicators ¨ Hemoglobin: ↓ due to lack of erythropoetin, produced by the kidney; pts receive synthetic EPO tx (Epogen) ¨ May have anemia of chronic disease ¨ Ferritin: may be indicator of iron overload; ↑ ferritin may mean EPO resistance .
Glomerular Filtration Rate (GFR) ¨ Best index of kidney function ¨ Used to establish stage of CKD ¨ GFR is the amount of filtrate formed per minute based on total surface area available for filtration (number of functioning glomeruli) ¨ Can be determined using injected isotope (inulin) measurement in urine ¨ Can be calculated from serum creatinine using standard equations.

Interdialytic Weight Gain ¨ Pts on dialysis gain several kg of fluid between HD treatments ¨ If pts gain >5%, may reflect excessive fluid intake, leading to hypertension, edema, ascites, pleural effusion ¨ Fluid gains of <2% reflect minimal fluid and food intake, may be losing body mass .
Pre-ESRD (DM) ¨ Primary Prevention – Glycemic control (DCCT) • Aim for Euglycemia • Watch for low B. S. – B. P. control • 130/80 • Na+ restrict – Base on comorbidities (~2 -3 g. ) – Medications may increase or decrease K+; monitor • Wt. loss (gradual)/exercise – Meds: ACE inhibitors and ARB’s .
Pre-ESRD ¨ Secondary Prevention (overt nephropathy; GFR ~ 25) – Protein normalization – 0. 6 g/kg - RDA 0. 8 g/kg ( minimum for DM) – Delay need for dialysis, control uremic symptoms, reduce acidosis ¨ Stage 4 CKD: monitor labs, may need to limit K+, Phos. , Ca++, Mg++ .
MNT in Patients on Hemodialysis .
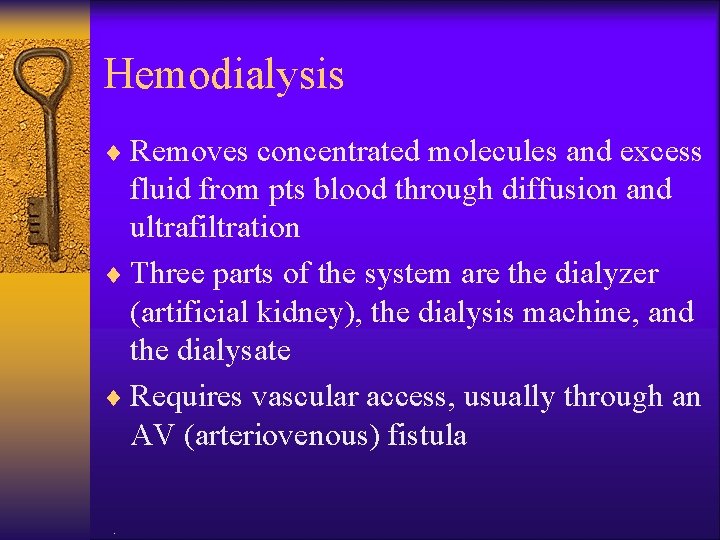
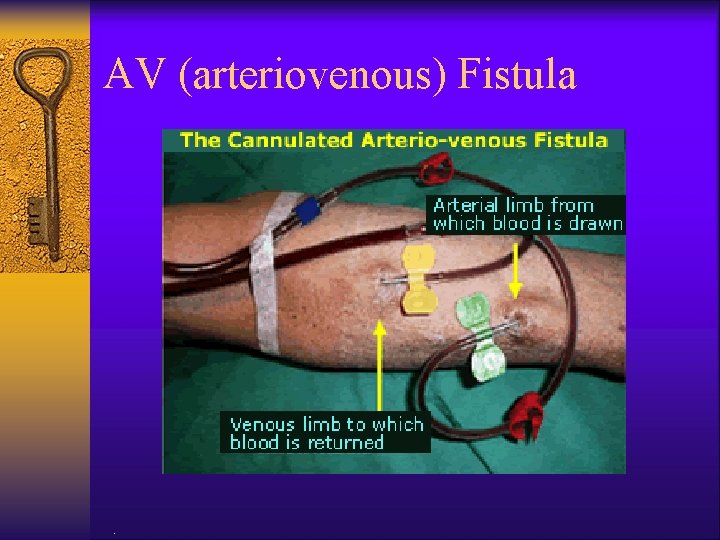
Hemodialysis ¨ Removes concentrated molecules and excess fluid from pts blood through diffusion and ultrafiltration ¨ Three parts of the system are the dialyzer (artificial kidney), the dialysis machine, and the dialysate ¨ Requires vascular access, usually through an AV (arteriovenous) fistula.
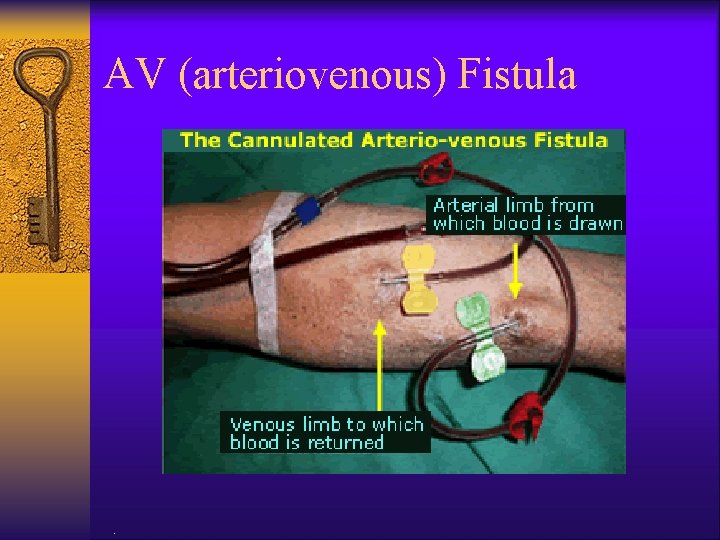
AV (arteriovenous) Fistula .
ESRD: Nutritional Management ¨ Prevent deficiencies ¨ Control edema and serum electrolytes ¨ Prevent renal osteodystrophy ¨ Provide an attractive and palatable diet .
MNT in HD: Protein ¨ 10 -12 g free amino acids lost per treatment during dialysis ¨ Greater amino acid losses with glucose-free dialysate and high flux dialyzers ¨ 1. 2 g protein/kg standard body weight (SBW) with 50% high biological value (meat, poultry, fish, eggs, soy, dairy) ¨ Most HD patients take in less than 1 g/day NKF K/DOQI practice guidelines. Am J Kid Dis 2000; 35(suppl): S 40 -S 41, Cited in Byham. Gray, p. 45 -46.
MNT in HD: Energy ¨ Adults <60 years: 35 kcal/kg SBW ¨ Adults > 60 or obese: 30 -35 kcals/kg body weight ¨ Actual intakes of HD patients in studies are lower than that (mean 23 kcals/kg in HEMO study) NKF K/DOQI practice guidelines. Am J Kid Dis 2000; 35(suppl): S 40 -S 41, Cited in Byham-Gray, p. 46 .

MNT in HD: Lipids ¨ HD patients at risk for lipid disorders ¨ Recommended fat intake<30% of calories and saturated fat<10%; cholesterol <300 mg/day ¨ Optimum fiber intake 20 -25 g/day ¨ These restrictions are difficult to achieve along with other restrictions of HD diet .
MNT in HD: sodium and fluid ¨ ≥ 1 L fluid output: 2 -4 g Na and 2 L fluid ¨ ≤ 1 L fluid output: 2 g Na and 1 -1. 5 L fluid ¨ Anuria: 2 g Na and 1 L fluid ¨ Restrict Na+ if ↑ interdialytic wt gain, CHF, edema, HTN, low serum sodium.
MNT in HD: Potassium ¨ Potassium needs related to urinary output ¨ Most patients on HD can tolerate 2. 5 g of K+ ¨ Stricter diet may be indicated for pts w/ insulin deficiency, metabolic acidosis, treated with beta blockers or aldosterone antagonists, hypercatabolic ¨ Individuals: 40 mg/kg edema-free IBW or SBW.

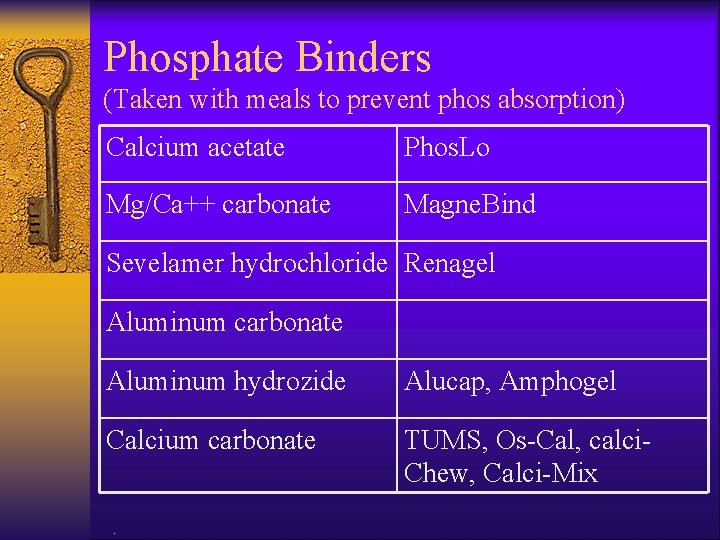
MNT in HD: Phosphorus ¨ Maintain s. phos 3. 5 -5. 5 mg/d. L ¨ Usually ok until GFR ↓ to 20 -30 m. L/min ¨ Dialysis removes 500 -1000 mg/treatment ¨ Use phosphorus binders with meals: absorb 50% of dietary phosphorus ¨ Dietary intake: 800 to 1000 mg/day or <17 mg/kg IBW or SBW ¨ Identify high protein, low phos food sources.
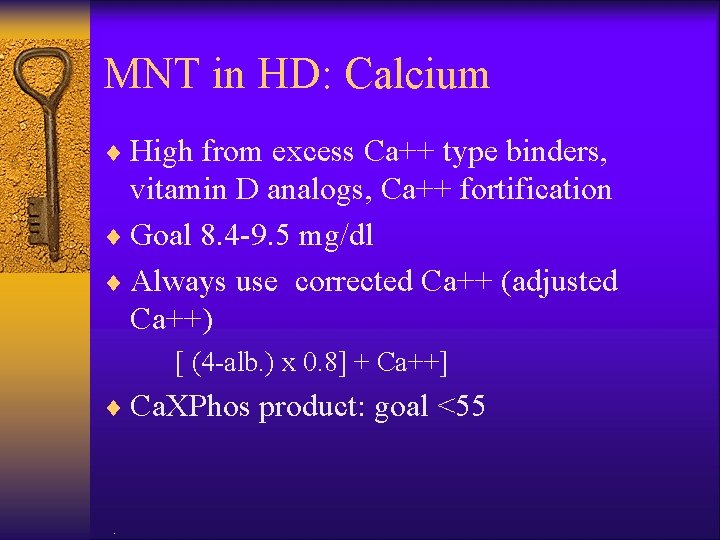
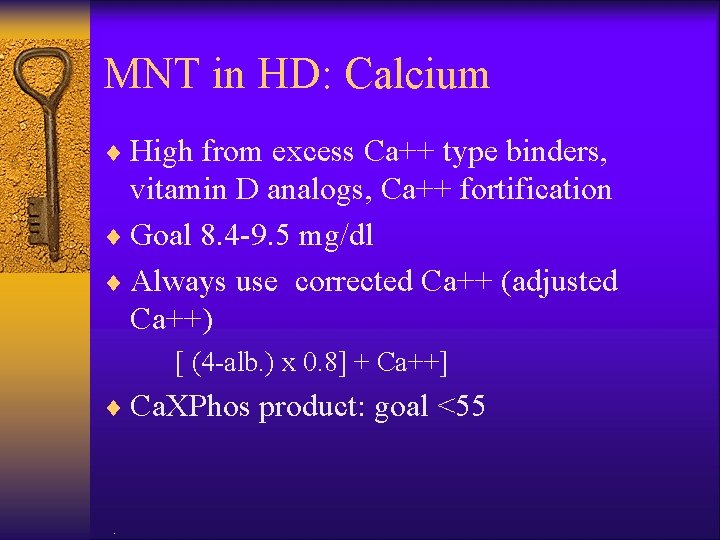
MNT in HD: Calcium ¨ High from excess Ca++ type binders, vitamin D analogs, Ca++ fortification ¨ Goal 8. 4 -9. 5 mg/dl ¨ Always use corrected Ca++ (adjusted Ca++) [ (4 -alb. ) x 0. 8] + Ca++] ¨ Ca. XPhos product: goal <55 .
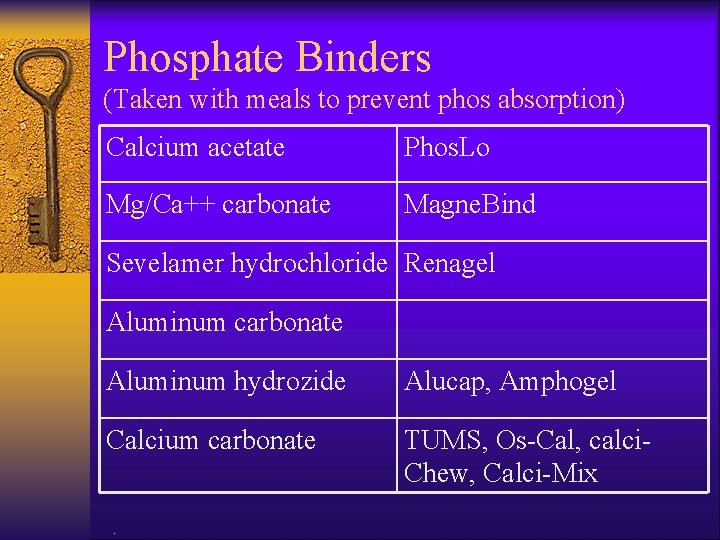
Phosphate Binders (Taken with meals to prevent phos absorption) Calcium acetate Phos. Lo Mg/Ca++ carbonate Magne. Bind Sevelamer hydrochloride Renagel Aluminum carbonate Aluminum hydrozide Alucap, Amphogel Calcium carbonate TUMS, Os-Cal, calci. Chew, Calci-Mix .
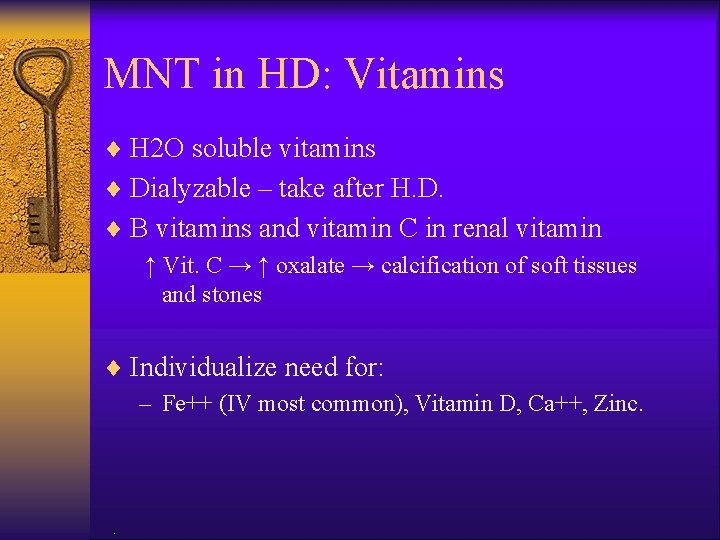
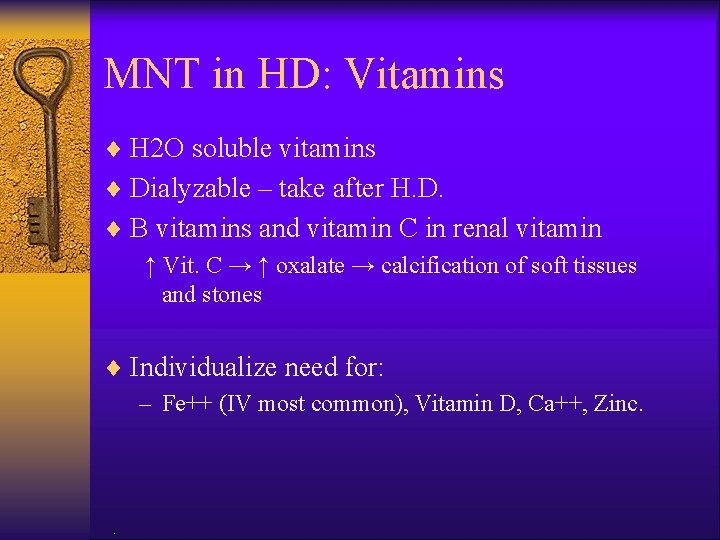
MNT in HD: Vitamins ¨ H 2 O soluble vitamins ¨ Dialyzable – take after H. D. ¨ B vitamins and vitamin C in renal vitamin ↑ Vit. C → ↑ oxalate → calcification of soft tissues and stones ¨ Individualize need for: – Fe++ (IV most common), Vitamin D, Ca++, Zinc. .

MNT in HD: Vitamin D ¨ Vitamin D is activated in the kidney to calcitriol, or vitamin D 3 ¨ As D 3 levels fall, calcium absorption ↓ and phos excretion ↓ ¨ Vitamin D 3 therapy helps prevent renal bone disease but may cause hypercalcemia ¨ Renal pts should use calcitriol supplements under the supervision of a physician.
Hemodialysis ¨ Typical diet order – 2000 calorie, 80 g protein, 2 g Na+, 3 g K+, low phosphorus, 1500 cc fluid restriction .
Skeletal Effects of Chronic Renal Failure ¨ Hyperphosphatemia ¨ Hypocalcemia ¨ Hyperparathyroidism ¨ Low bone mass and density ¨ Osteitis fibrosa cystica—hyperplastic demineralized bone .
Monitor Patient Status 1. 2. 3. 4. 5. BP >140/90 Edema Weight changes Urine output Urine analysis: —Albumin —Protein .
Monitor Patient Status (cont) 6. 7. . Kidney function Creatinine clearance Glomerular filtration rate (GFR) Blood values BUN 10 to 20 mg/dl (<100 mg/dl) Creatinine 0. 7 to 1. 5 mg/dl (10 -15 mg/dl) Potassium 3. 5 to 5. 5 m. Eq/L Phosphorus 3. 0 to 4. 5 mg/dl Albumin 3. 5 -5. 5 g/dl Calcium 9 -11 mg/dl
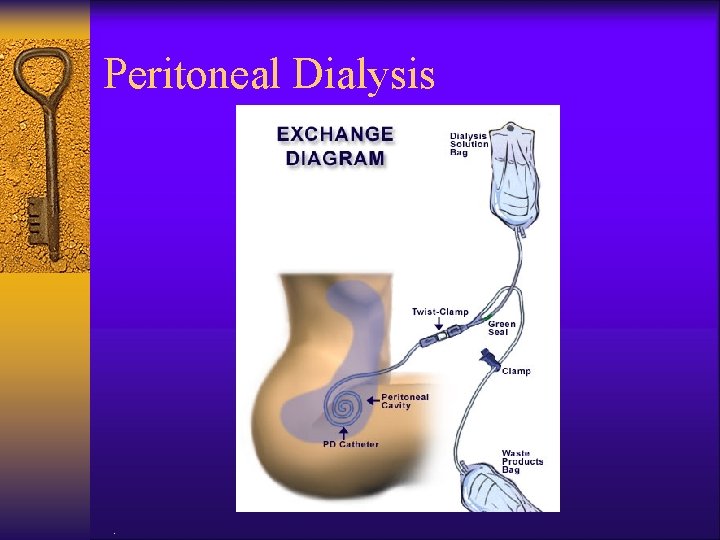
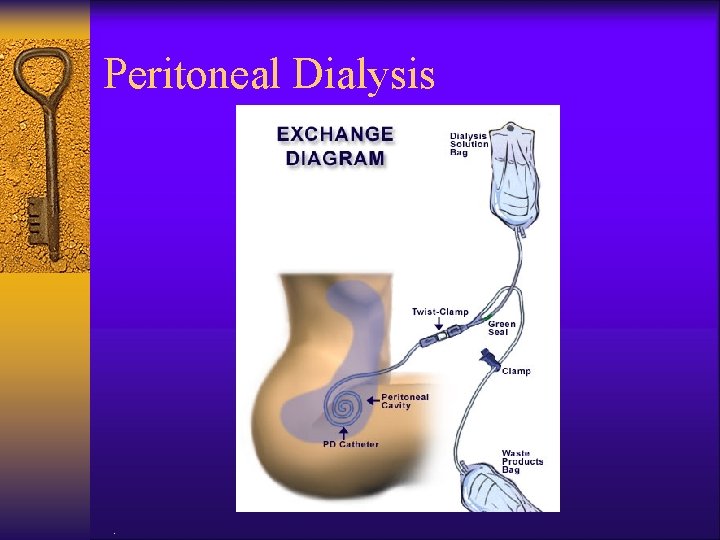
Peritoneal Dialysis .
CAPD (continuous ambulatory peritoneal dialysis) ¨ Most patients do 4 -5 exchanges per day ¨ A specific volume of dialysate (1500 -3000 ml) is infused into the peritoneal cavity via a catheter ¨ The dialysate dwells for 4 hours as excess fluid and toxins diffuse through peritoneal membrane ¨ Dialysate and wastes are drained from the body and the process repeated. .
Peritoneal Dialysis (home dialysis) ¨ ¨ ¨ Blood cleansed by passive movement from capillaries to dialysate (diffusion) Ultra-filtration (UF): fluid removed by osmosis due to high osmolality of dextrose in dialysate Better control of labs, fluid balance and B. P. Advantages for those with heart failure, access problems. Diet liberal, independence. Disadvantages: , anorexia, a. a. losses in dialysate, peritionitis→ catabolism, anorexia, long- term wasting, high B. S. , wt. gain, lack of socialization .
MNT for PD: Energy ¨ Energy: 35 kcals/kg/day SBW or adjusted body weight for pts<60 years; 30 kcals/kg for those >60 ¨ Calories provided in the dialysate should be included in total intake (may absorb as much as 1/3 of daily energy needs) .

MNT for PD: Protein ¨ PD patients lose 5 -15 grams of protein a day, primarily as albumin ¨ Goal 1. 2 -1. 3 g/kg SBW or ABW/day .
MNT for PD: Sodium ¨ PD clears sodium very well, so sodium can be fairly liberal ¨ However, high salt diets increase thirst and may make adherence to fluid limits more difficult ¨ General recommendation is 2 -4 grams sodium .
MNT for PD ¨ Potassium: is easily cleared by PD; some patients may need K+ supplementation ¨ Calcium: limit to 2000 mg elemental calcium – Generally pts get ~1500 mg from calciumbased phosphate binders – Serum calcium should be maintained in low normal range (8. 4 -9. 5 mg/dl) .
MNT for PD ¨ Phosphorus: limited to 800 -1000 mg/day which is difficult with high protein diet – Use phosphate binders ¨ Fluid: can be adjusted by varying the dextrose concentrations of the dialysate – May need to be restricted if pts cannot achieve fluid balance without frequent hypertonic exchanges .

PD: weight gain, hypertriglyceridemia, hyperglycemia ¨ Increase exercise as allowed by MD ¨ Limit sodium and fluid to minimize hypertonic exchanges ¨ Modify energy intake to facilitate wt loss ¨ Modify intake of sugars and fats, especially saturated fats .
PD: Protein Losses, Malnutrition ¨ Patient education regarding protein goals and ways to meet them ¨ Suggest pt eat protein foods first and limit fluids at mealtime ¨ Frequent smaller portions of protein and easy to eat proteins such as egg white, cottage cheese, etc ¨ Education on sterile technique to avoid peritonitis.
Kidney Transplant 1. Types: related donor or cadaver 2. Posttransplant management: Corticosteroids Cyclosporine 3. Diet while on high-dose steroids: 1. 3 to 2 g/kg BW protein 30 to 35 kcal/kg BW energy 80 to 100 m. Eq Na 4. Diet after steroids: 1 g/kg BW protein Kcal to achieve IBW Individualize Na level .
Well Mr. Osborne, it may not be kidney stones after all. .

Kidney Stones 1. Particulate matter crystallizes Ca salts (Ca oxalate or Ca phosphate) Uric acid Cystine Struvite (NH 4, magnesium and phosphate) 2. Ca salts in stones—Rx: high fluid; evaluate calcium from diet; may need more! 3. Treat metabolic problem; low-oxalate diet may be needed; acid-ash diet is sometimes useful but not proven totally effective .

Kidney Stones—cont’d 4. Uric acid stones Alter p. H of urine to more alkaline Use high-alkaline-ash diet Food list in Krause text 5. Cystine stones (rare) 6. Struvite (infection stones) antibiotics and/or surgery .

Acid-Ash Diet ¨ Increases acidity of urine (contains chloride, phosphorus, and sulfur) ¨ Meats, cheese, grains emphasized ¨ Fruits and vegetables limited (exceptions are corn, lentils, cranberries, plums, prunes) .
Alkaline-Ash Diet ¨ Increases alkalinity of urine (contains sodium, potassium, calcium, and magnesium) ¨ Fruits and vegetables emphasized (exceptions are corn, lentils, cranberries, plums, prunes) ¨ Meats and grains limited .

Summary ¨ Renal diseases—delicate balance of nutrients ¨ Regular monitoring of lab values, with altered dietary interventions accordingly .
 Res extra commercium
Res extra commercium Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Small bowel obstruction parenteral nutrition
Small bowel obstruction parenteral nutrition Distinguish between renal corpuscle and renal tubule
Distinguish between renal corpuscle and renal tubule Aeiou renal replacement therapy
Aeiou renal replacement therapy Nutrition fundamentals of nursing
Nutrition fundamentals of nursing Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Bioness integrated therapy system price
Bioness integrated therapy system price What are the major humanistic therapies
What are the major humanistic therapies Medical family therapy
Medical family therapy Iso 22301 utbildning
Iso 22301 utbildning Typiska novell drag
Typiska novell drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Ekologiskt fotavtryck
Ekologiskt fotavtryck Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Tidbok yrkesförare
Tidbok yrkesförare Anatomi organ reproduksi
Anatomi organ reproduksi Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Boverket ka
Boverket ka Hur skriver man en tes
Hur skriver man en tes Delegerande ledarskap
Delegerande ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Formel för lufttryck
Formel för lufttryck Publik sektor
Publik sektor Kyssande vind
Kyssande vind Presentera för publik crossboss
Presentera för publik crossboss Jiddisch
Jiddisch Plats för toran ark
Plats för toran ark Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter Luftstrupen för medicinare
Luftstrupen för medicinare Claes martinsson
Claes martinsson Centrum för kunskap och säkerhet
Centrum för kunskap och säkerhet Byggprocessen steg för steg
Byggprocessen steg för steg Bra mat för unga idrottare
Bra mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Referatmarkeringar
Referatmarkeringar Redogör för vad psykologi är
Redogör för vad psykologi är Stål för stötfångarsystem
Stål för stötfångarsystem Tack för att ni har lyssnat
Tack för att ni har lyssnat Borra hål för knoppar
Borra hål för knoppar Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Formel standardavvikelse
Formel standardavvikelse Tack för att ni har lyssnat
Tack för att ni har lyssnat Rita perspektiv
Rita perspektiv Informationskartläggning
Informationskartläggning Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Toppslätskivling effekt
Toppslätskivling effekt Gibbs reflekterande cykel
Gibbs reflekterande cykel Egg för emanuel
Egg för emanuel Elektronik för barn
Elektronik för barn Antikt plagg i rom
Antikt plagg i rom Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Ellika andolf
Ellika andolf Romarriket tidslinje
Romarriket tidslinje Tack för att ni lyssnade
Tack för att ni lyssnade Enheter för massa
Enheter för massa Dikt om ljus
Dikt om ljus Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Rådet för byggkompetens
Rådet för byggkompetens Ledarskapsteorier
Ledarskapsteorier Skivepiteldysplasi
Skivepiteldysplasi Myndigheten för delaktighet
Myndigheten för delaktighet Trög för kemist
Trög för kemist Sju principer för tillitsbaserad styrning
Sju principer för tillitsbaserad styrning Läkarutlåtande för livränta
Läkarutlåtande för livränta Karttecken färger
Karttecken färger Skapa med geometriska former
Skapa med geometriska former Vishnuiter
Vishnuiter Meios steg för steg
Meios steg för steg Bris för vuxna
Bris för vuxna Bamse för de yngsta
Bamse för de yngsta Doctors license number
Doctors license number Gbmc medical records
Gbmc medical records Hepburn osteometric board
Hepburn osteometric board Torrance memorial medical center medical records
Torrance memorial medical center medical records Cartersville medical center medical records
Cartersville medical center medical records