Liver diseases III Cholestatic Diseases Cholestasis is caused











- Slides: 35
Liver diseases III
Cholestatic Diseases • Cholestasis is caused by impaired bile formation and bile flow that gives rise to accumulation of bile pigment in the hepatic parenchyma. • It can be caused by extrahepatic or intrahepatic obstruction of bile channels, or by defects in hepatocyte bile secretion.
• Bile is produced continuously by the liver and stored and concentrated in the gallbladder. After eating, this stored bile is discharged into duodenum. • Composition of bile: Water (97%), bile salts (0. 7%), bilirubin (0. 2%), fat/cholesterol/fatty acids/lecithin (0. 5%). About 400 -800 ml of bile is produced/day in adults (can reach 1 L/day).
• Two thirds of the organic materials in bile are bile salts, which are formed by the conjugation of bile acids with taurine or glycine. • The primary human bile acids are cholic acid and chenodeoxycholic acid. • Bile acids in bile salts are highly effective detergents. Their primary physiologic role is to solubilize water-insoluble lipids secreted by hepatocytes into bile, and also to solubilize dietary lipids in the gut lumen. • Ninety-five percent of secreted bile acids, conjugated or unconjugated, are reabsorbed from the gut lumen and recirculate to the liver (enterohepatic circulation), thus helping to maintain a large endogenous pool of bile acids for digestive and excretory purposes.
• Hepatic bile serves two major functions: (1) the emulsification of dietary fat in the lumen of the gut through the detergent action of bile salts (2) the elimination of bilirubin, excess cholesterol, xenobiotics, and other waste products that are insufficiently water-soluble to be excreted into urine. *Tissue deposition of bile becomes clinically evident as: - yellow discoloration of the skin and sclera (jaundice and icterus, respectively) due to retention of bilirubin, - and as cholestasis, when there is systemic retention of not only bilirubin but also other solutes eliminated in bile.
• Patients may have: jaundice, pruritus, skin xanthomas (focal accumulation of cholesterol), symptoms related to intestinal malabsorption, including nutritional deficiencies of the fat-soluble vitamins A, D, or K. A characteristic laboratory finding is elevated serum alkaline phosphatase and γ-glutamyl transpeptidase (GGT), enzymes present on the apical (canalicular) membranes of hepatocytes and bile duct epithelial cells.
• Common to both obstructive and nonobstructive cholestasis is the accumulation of bile pigment (green-brown) within the hepatic parenchyma.




• Causes: Large Bile Duct Obstruction: - The most common cause of bile duct obstruction in adults is extrahepatic cholelithiasis (gallstones) followed by malignancies of the biliary tree or head of the pancreas, and strictures resulting from previous surgical procedures. - Obstructive conditions in children include biliary atresia, cystic fibrosis, choledochal cysts and syndromes in which there are insufficient intrahepatic bile ducts. - Subtotal or intermittent obstruction may promote ascending cholangitis, a secondary bacterial infection of the biliary tree that aggravates the inflammatory injury. Enteric organisms such as coliforms and enterococci are common culprits. Cholangitis usually presents with fever, chills, abdominal pain, and jaundice.
• Since extrahepatic biliary obstruction is frequently amenable to surgical alleviation, correct and prompt diagnosis is imperative. • In contrast, cholestasis due to diseases of the intrahepatic biliary tree or hepatocellular secretory failure (collectively termed intrahepatic cholestasis) is not benefited by surgery (short of transplantation), and the patient’s condition may be worsened by an operative procedure. There is thus some urgency in making a correct diagnosis of the cause of jaundice and cholestasis. • Left uncorrected, secondary inflammation resulting from chronic biliary obstruction and ductular reactions initiate periportal fibrosis, eventually leading to hepatic scarring and nodule formation, generating secondary or obstructive biliary cirrhosis.

- Primary Hepatolithiasis: is a disorder of intrahepatic gallstone formation that leads to repeated bouts of ascending cholangitis, progressive inflammatory destruction of hepatic parenchyma, and predisposes to biliary neoplasia.
• Neonatal Cholestasis: Prolonged conjugated hyperbilirubinemia in the neonate (beyond 14 -21 days after birth). The major causes are: (1) cholangiopathies, primarily biliary atresia (complete or partial obstruction of the lumen of the extrahepatic biliary tree within the first 3 months of life). (2) A variety of disorders causing conjugated hyperbilirubinemia in the neonate, collectively referred to as neonatal hepatitis. Differentiation of biliary atresia from nonobstructive neonatal cholestasis is very important, since definitive treatment of biliary atresia requires surgical intervention (Kasai procedure), whereas surgery may adversely affect the clinical course of a child with other disorders. Affected infants have jaundice, dark urine, light or acholic stools, and hepatomegaly

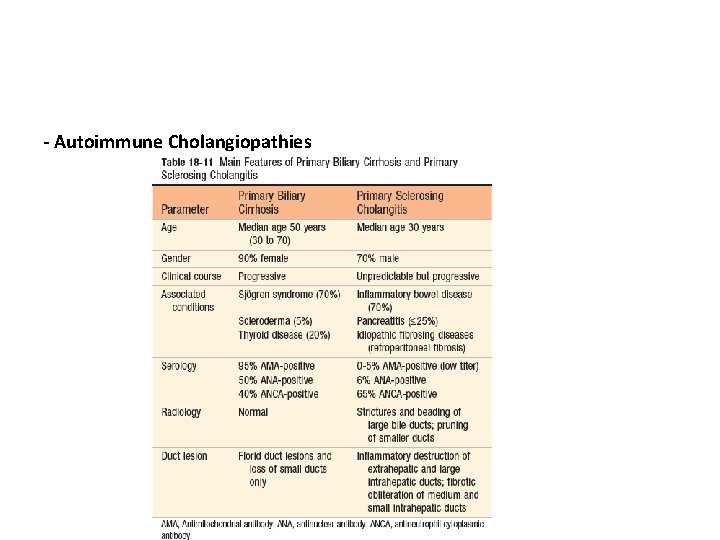
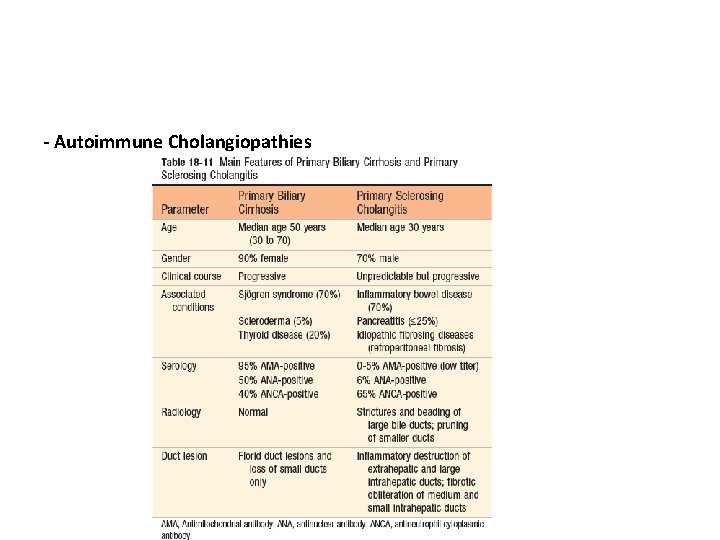
- Autoimmune Cholangiopathies


- intrahepatic bile ducts are frequently damaged as part of other liver diseases, including viral hepatitis, drug- or toxin-induced liver injury, liver transplantation, and graft-versus-host disease that follows hematopoietic stem cell transplantation.
Liver tumors Involvement of the liver by metastatic malignancy is far more common than primary hepatic neoplasia. • Hepatic masses: - Nodular Hyperplasias (focal nodular hyperplasia and nodular regenerative hyperplasia). - True neoplasm: Benign Neoplasms: Cavernous hemangiomas (m. c) Hepatocellular Adenomas (OCP) Malignant neoplasms: Hepatoblastoma (children) Hepatocellular Carcinoma (adult) Cholangiocarcinoma (biliary tree)
GALLBLADDER Between meals, bile is stored in the gallbladder, where it is concentrated. The adult gallbladder has a capacity of about 50 m. L. The organ is not essential for biliary function, since humans do not suffer from indigestion or malabsorption of fat after cholecystectomy.
Cholelithiasis (Gallstones) • More than 95% of biliary tract disease is attributable to cholelithiasis (gallstones). There are two general classes of gallstones: cholesterol stones: containing more than 50% of crystalline cholesterol monohydrate, pigment stones: composed predominantly of bilirubin calcium salts.

Pathogenesis of Cholesterol Stones: 1) Supersaturation of bile with cholesterol; (2) hypomotility of the gallbladder; (3) accelerated cholesterol crystal nucleation; (4) and hypersecretion of mucus in the gallbladder, which traps the nucleated crystals, Pathogenesis of Pigment Stones: elevated levels of unconjugated bilirubin in bile,


Clinical features: • 70% to 80% of patients remain asymptomatic throughout their lives. • biliary colic (constant and not colicky right upper quadrant pain radiate to the right shoulder, usually follows a fatty meal) • Cholecystitis----- pain • Complications: empyema, perforation, fistulas, cholangitis, obstructive cholestasis and pancreatitis. • increased risk of gallbladder carcinoma
Cholecystitis • Inflammation of the gallbladder may be: acute, chronic, acute superimposed on chronic. • It almost always occurs in association with gallstones.
• Acute Cholecystitis: Calculous cholecystitis: is precipitated in 90% of cases by obstruction of the neck or the cystic duct by a stone. It is the primary complication of gallstones and the most common reason for emergency cholecystectomy-----chemical irritation and inflammation (not infection)of a gallbladder. acalculous cholecystitis: Cholecystitis without gallstones, may occur in severely ill patients and accounts for about 10% of patients with cholecystitis----- result from ischemia (cystic artery), Contributing factors may include inflammation and edema of the wall compromising blood flow, gallbladder stasis, and accumulation of microcrystals of cholesterol (biliary sludge), viscous bile, and gallbladder mucus, causing cystic duct obstruction in the absence of stones.
• Clinical symptoms of acute acalculous cholecystitis tend to be more insidious, since they are obscured by the underlying conditions precipitating the attacks. • As a result of either delay in diagnosis or the disease itself, the incidence of gangrene and perforation is much higher in acalculous than in calculous cholecystitis.
• Chronic Cholecystitis: Chronic cholecystitis may be a sequel to repeated bouts of mild to severe acute cholecystitis, but in many instances it develops in the apparent absence of antecedent attacks. Since it is associated with cholelithiasis in more than 90% of cases, the at-risk patient population is the same as that for gallstones. Unlike acute calculous cholecystitis, obstruction of gallbladder outflow is not a requisite.
• Diagnosis of both acute and chronic cholecystitis is important because of the following complications: - Bacterial superinfection with cholangitis or sepsis - Gallbladder perforation and local abscess formation - Gallbladder rupture with diffuse peritonitis - Biliary enteric (cholecystenteric) fistula, with drainage of bile into adjacent organs, entry of air and bacteria into the biliary tree, and potentially, gallstone-induced intestinal obstruction (ileus) - Aggravation of preexisting medical illness, with cardiac, pulmonary, renal, or liver decompensation - Porcelain gallbladder, with increased risk of cancer
Gallbladder carcinoma • The most important risk factor for gallbladder cancer is gallstones which are present in 95% of cases. • Gallbladder cancer is at least twice as common in women than in men.
 Cholestatic pattern
Cholestatic pattern Neonatal cholestasis naspghan
Neonatal cholestasis naspghan Neonatal cholestasis definition
Neonatal cholestasis definition Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Microbes
Microbes Diseases caused by dust
Diseases caused by dust Hamlet act iii scene iii
Hamlet act iii scene iii R
R Main lobar fissure of the liver
Main lobar fissure of the liver Bare area of liver
Bare area of liver Toronto liver centre
Toronto liver centre Aflp in pregnancy
Aflp in pregnancy Esophagogastric junction
Esophagogastric junction Perisinusoidal space
Perisinusoidal space Liversoc
Liversoc Pacr uwe
Pacr uwe Gallbladder and spleen location
Gallbladder and spleen location Normal range alkaline phosphatase in child
Normal range alkaline phosphatase in child Pancreas location
Pancreas location Profile
Profile Hepatic encephalopathy staging
Hepatic encephalopathy staging Continental gum method
Continental gum method Liver injury grading
Liver injury grading Stigmata of chronic liver disease
Stigmata of chronic liver disease Complication of liver cirrhosis
Complication of liver cirrhosis Traub's area percussion
Traub's area percussion Peristaltic waves
Peristaltic waves Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Hepatic encephalopathy treatment guidelines
Hepatic encephalopathy treatment guidelines Bloodborne pathogens attacking the liver are
Bloodborne pathogens attacking the liver are Liver defenition
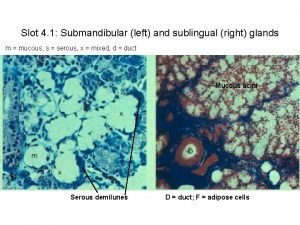
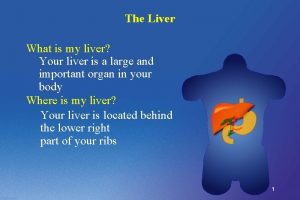
Liver defenition Bile canaliculi
Bile canaliculi Ovarian cyst size chart in mm
Ovarian cyst size chart in mm Where are liver flukes found
Where are liver flukes found Normal size of liver
Normal size of liver What is the primary function of the liver
What is the primary function of the liver