Lecture 20 1 PHYSIOPATHOLOGY OF THE FEMALE REPRODUCTIVE

- Slides: 28
Lecture 20 1. PHYSIOPATHOLOGY OF THE FEMALE REPRODUCTIVE SYSTEM. 2. HIPOTALAMO-PITUITARYOVARIAN AXIS. 3. ENDOMETRIAL CYCLE AND MENSTRUATION Prof. Vlad TICA, MD, Ph. D
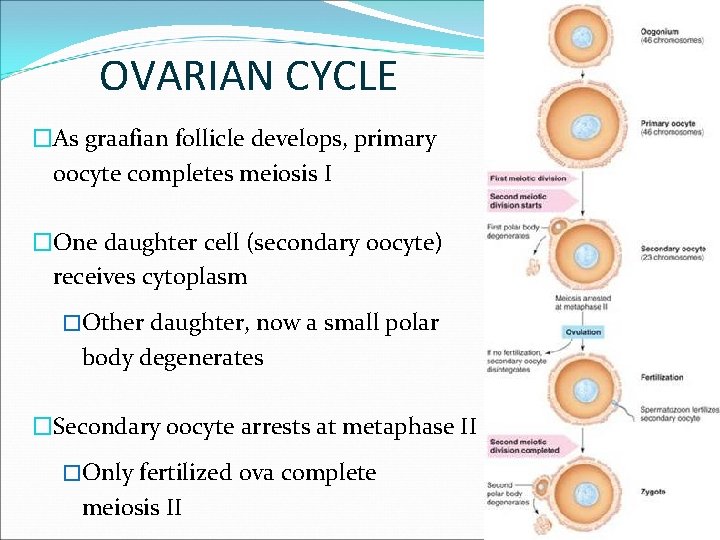
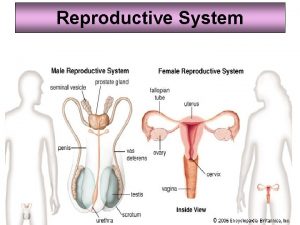
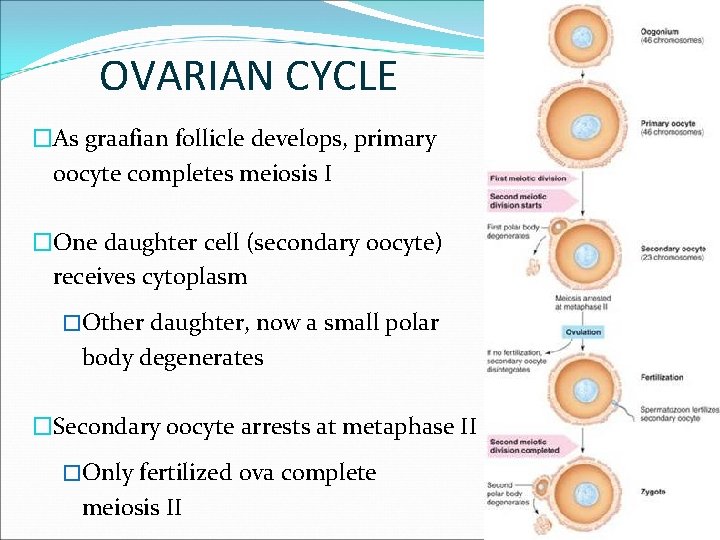
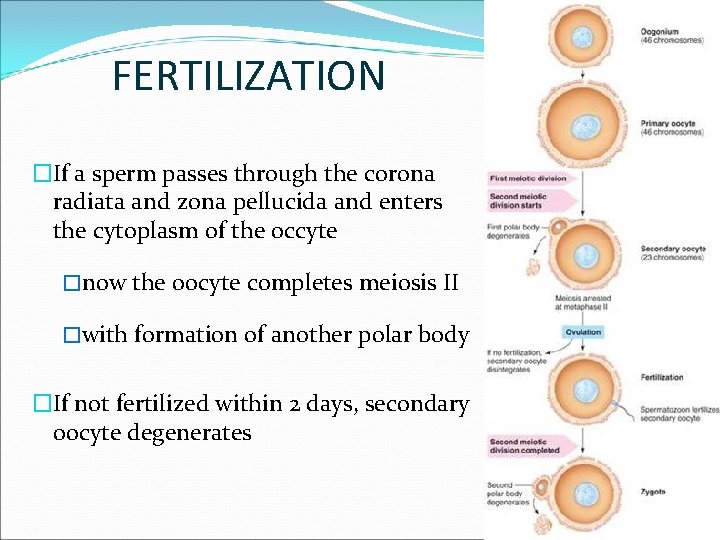
OVARIAN CYCLE �As graafian follicle develops, primary oocyte completes meiosis I �One daughter cell (secondary oocyte) receives cytoplasm �Other daughter, now a small polar body degenerates �Secondary oocyte arrests at metaphase II �Only fertilized ova complete meiosis II
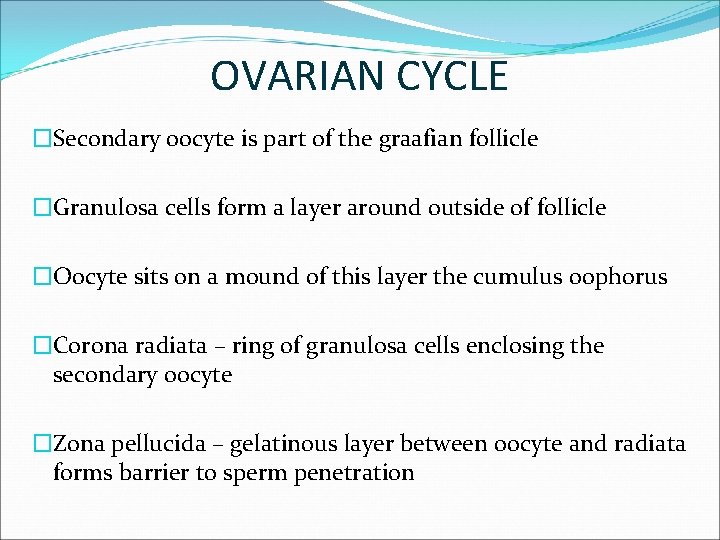
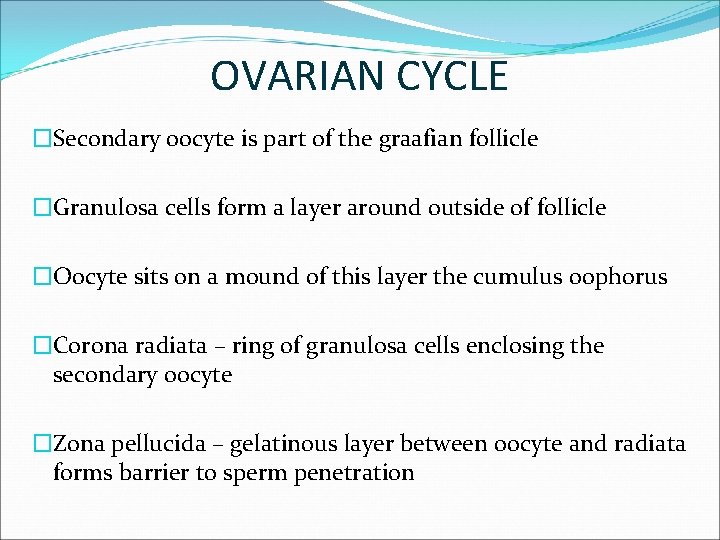
OVARIAN CYCLE �Secondary oocyte is part of the graafian follicle �Granulosa cells form a layer around outside of follicle �Oocyte sits on a mound of this layer the cumulus oophorus �Corona radiata – ring of granulosa cells enclosing the secondary oocyte �Zona pellucida – gelatinous layer between oocyte and radiata forms barrier to sperm penetration
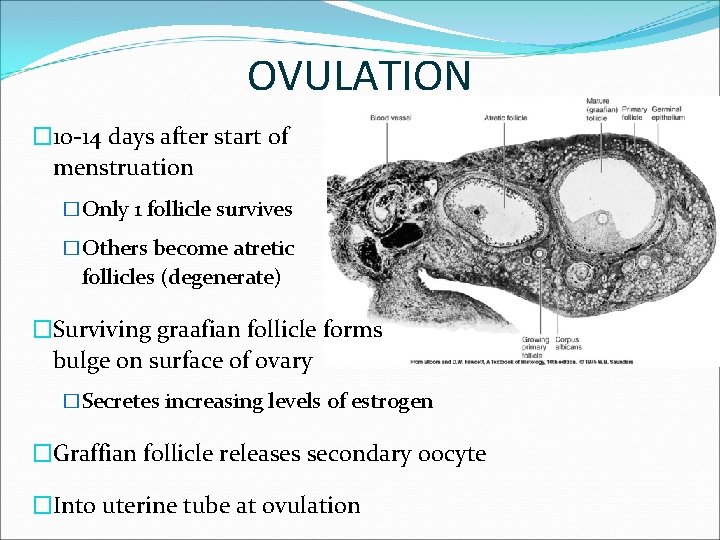
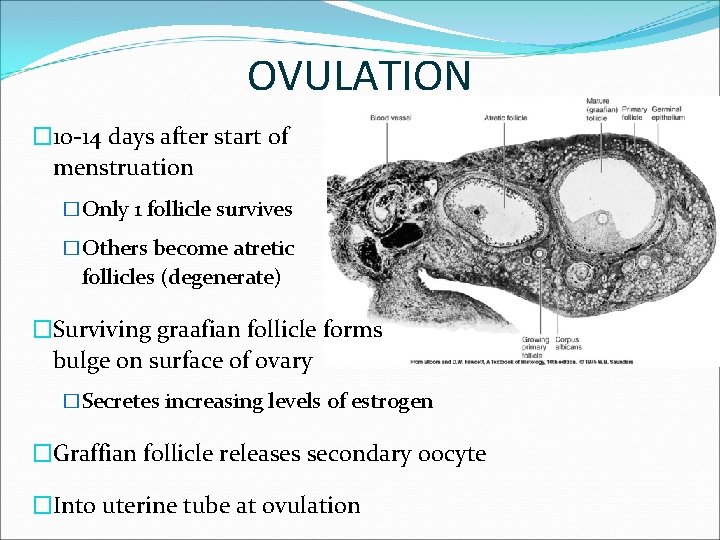
OVULATION � 10 -14 days after start of menstruation �Only 1 follicle survives �Others become atretic follicles (degenerate) �Surviving graafian follicle forms bulge on surface of ovary �Secretes increasing levels of estrogen �Graffian follicle releases secondary oocyte �Into uterine tube at ovulation
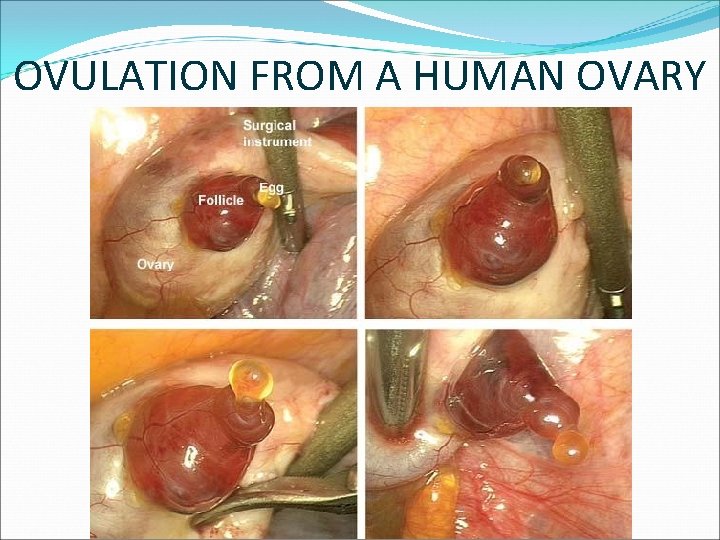
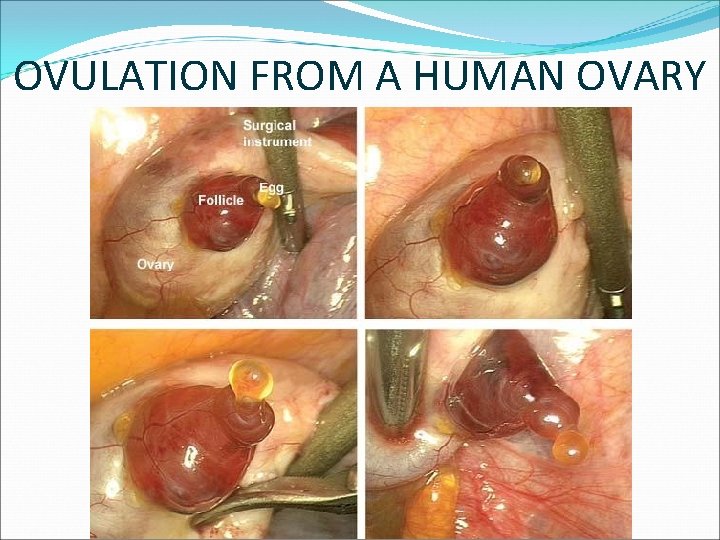
OVULATION FROM A HUMAN OVARY
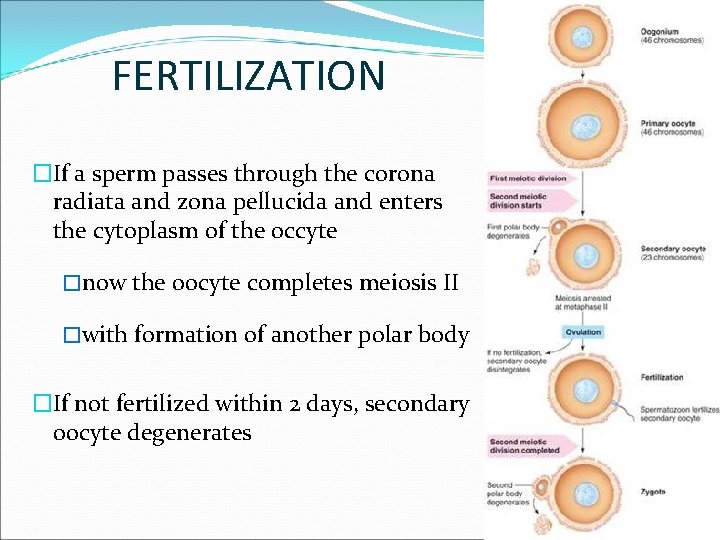
FERTILIZATION �If a sperm passes through the corona radiata and zona pellucida and enters the cytoplasm of the occyte �now the oocyte completes meiosis II �with formation of another polar body �If not fertilized within 2 days, secondary oocyte degenerates
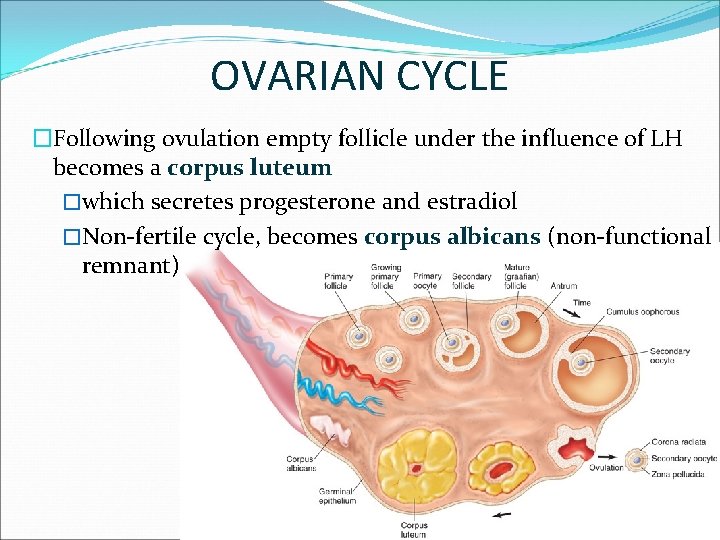
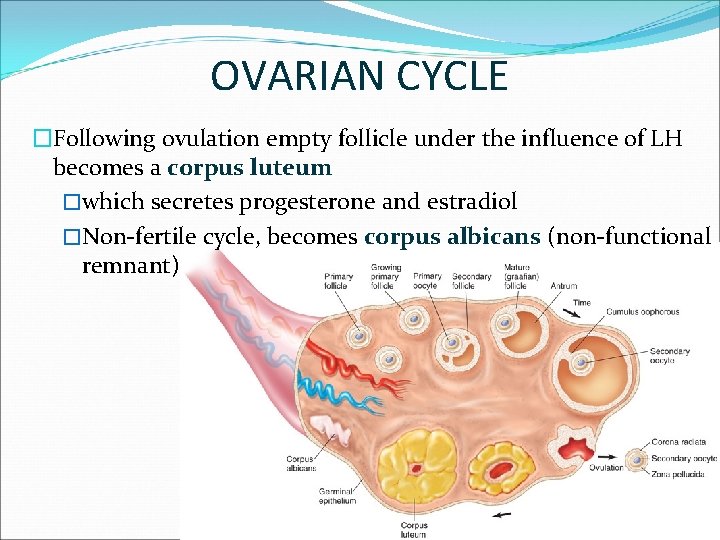
OVARIAN CYCLE �Following ovulation empty follicle under the influence of LH becomes a corpus luteum �which secretes progesterone and estradiol �Non-fertile cycle, becomes corpus albicans (non-functional remnant)
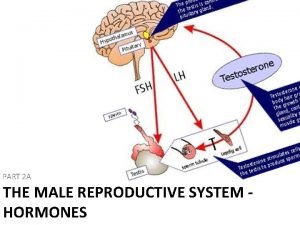
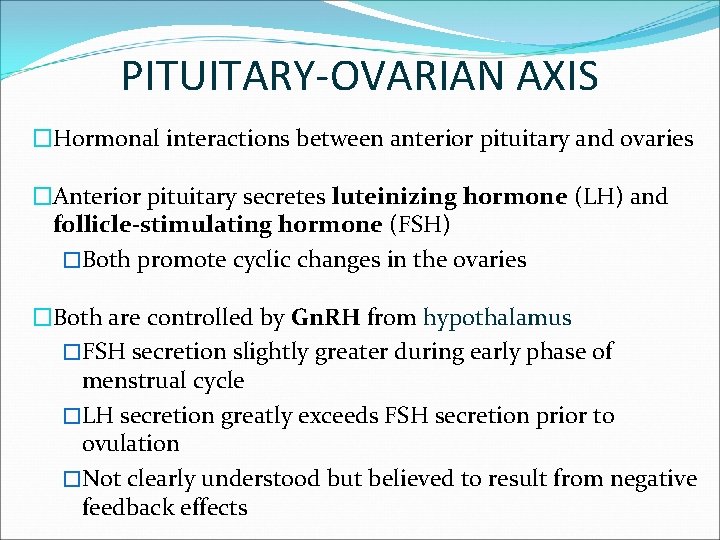
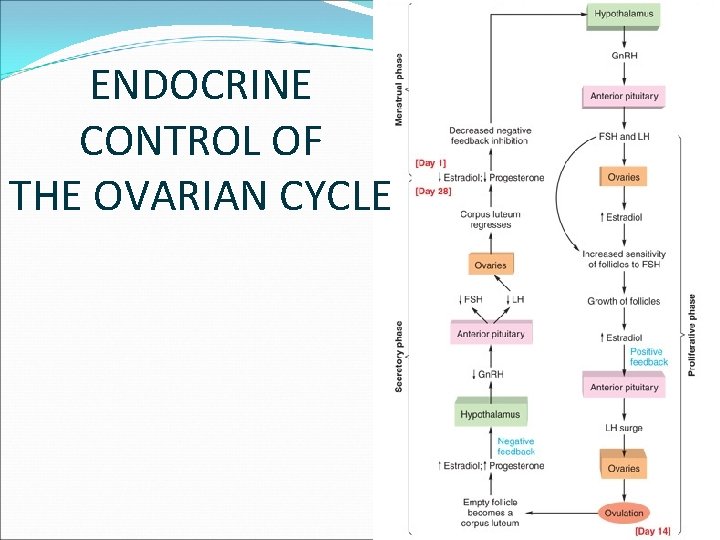
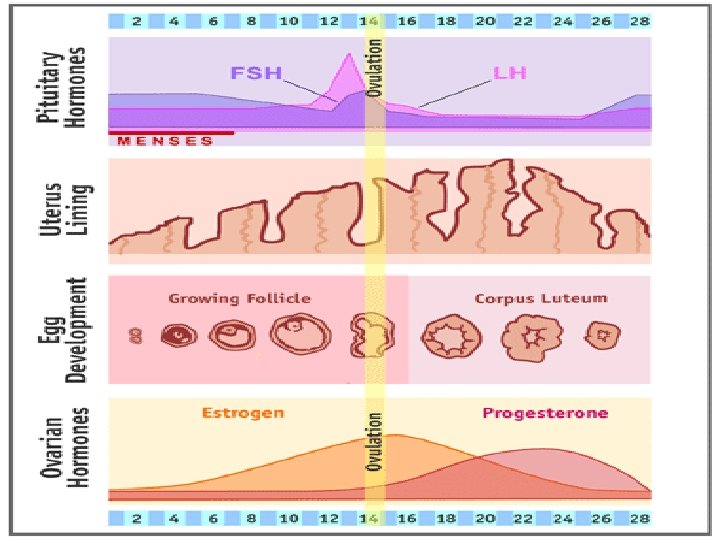
PITUITARY-OVARIAN AXIS �Hormonal interactions between anterior pituitary and ovaries �Anterior pituitary secretes luteinizing hormone (LH) and follicle-stimulating hormone (FSH) �Both promote cyclic changes in the ovaries �Both are controlled by Gn. RH from hypothalamus �FSH secretion slightly greater during early phase of menstrual cycle �LH secretion greatly exceeds FSH secretion prior to ovulation �Not clearly understood but believed to result from negative feedback effects
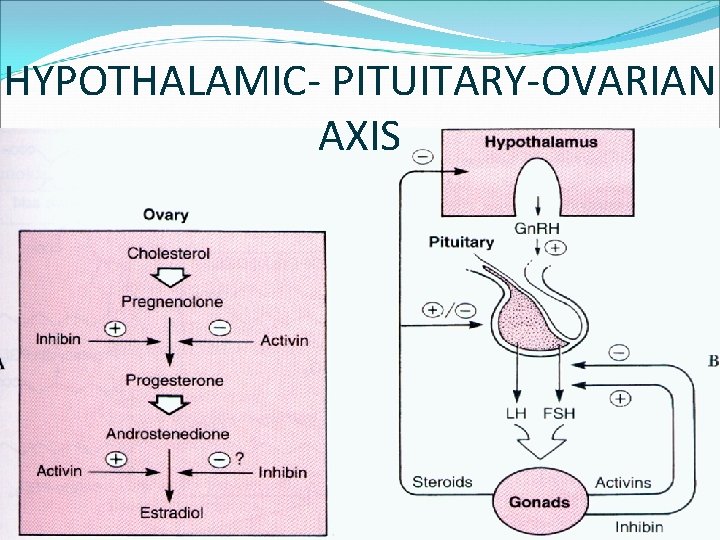
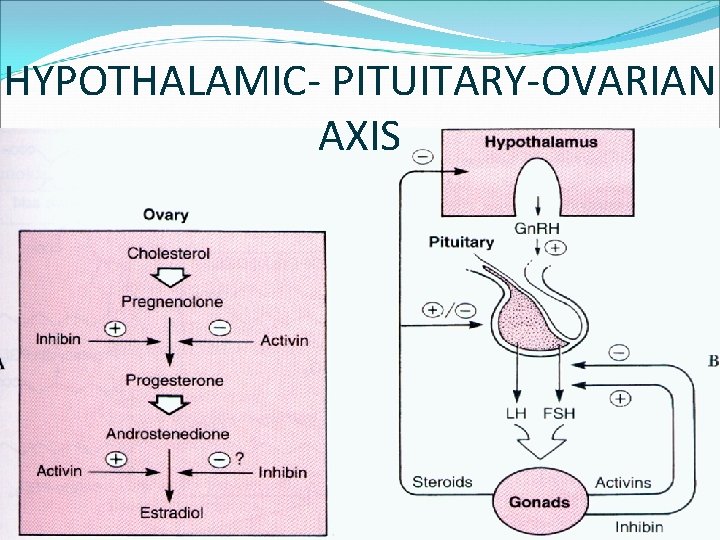
HYPOTHALAMIC- PITUITARY-OVARIAN AXIS
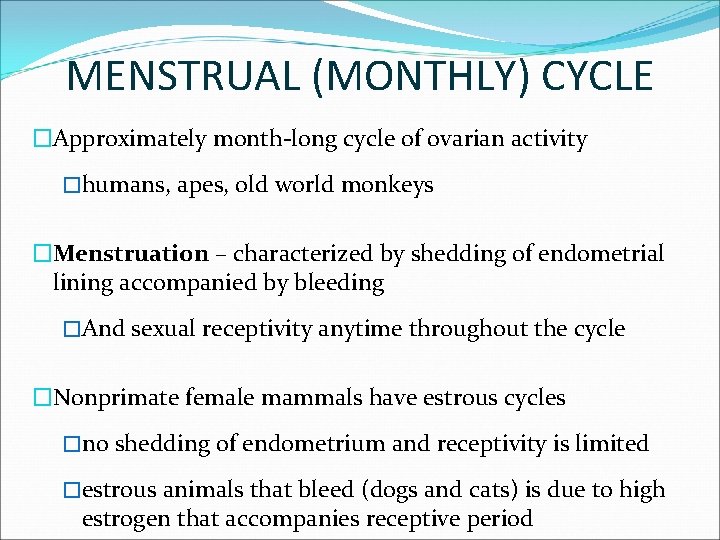
MENSTRUAL (MONTHLY) CYCLE �Approximately month-long cycle of ovarian activity �humans, apes, old world monkeys �Menstruation – characterized by shedding of endometrial lining accompanied by bleeding �And sexual receptivity anytime throughout the cycle �Nonprimate female mammals have estrous cycles �no shedding of endometrium and receptivity is limited �estrous animals that bleed (dogs and cats) is due to high estrogen that accompanies receptive period
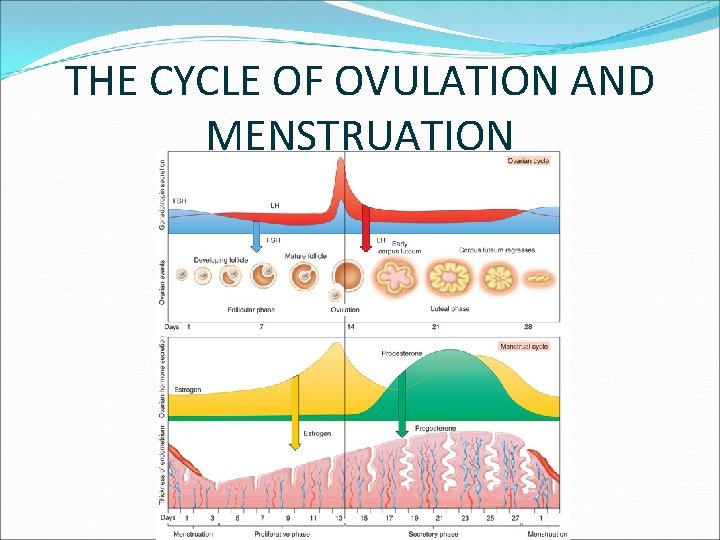
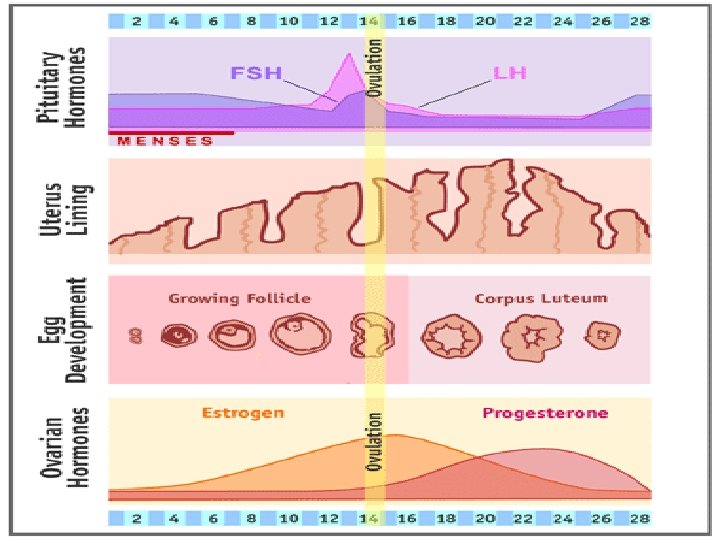
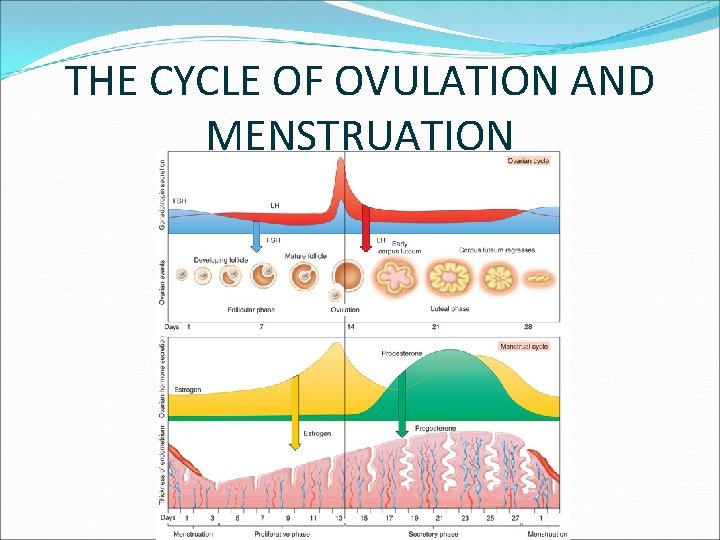
MENSTRUAL CYCLE �In humans is about 28 days �Day 1 is taken to be the first day of menstruation �Days 1 thru ovulation constitutes the follicular phase �Time from ovulation to menstruation is luteal phase �Endometrial changes are called: menstrual, proliferative and secretory phases
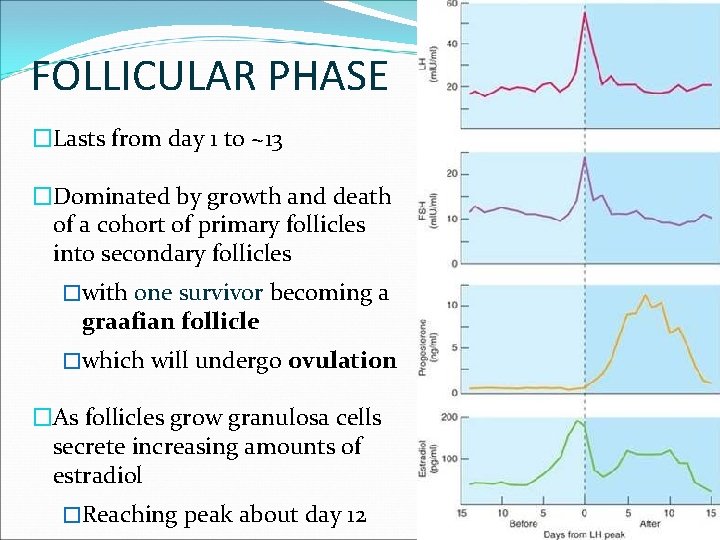
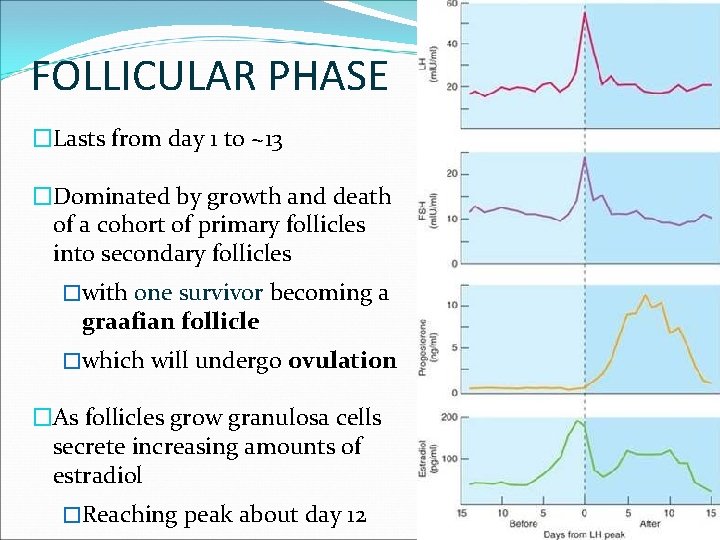
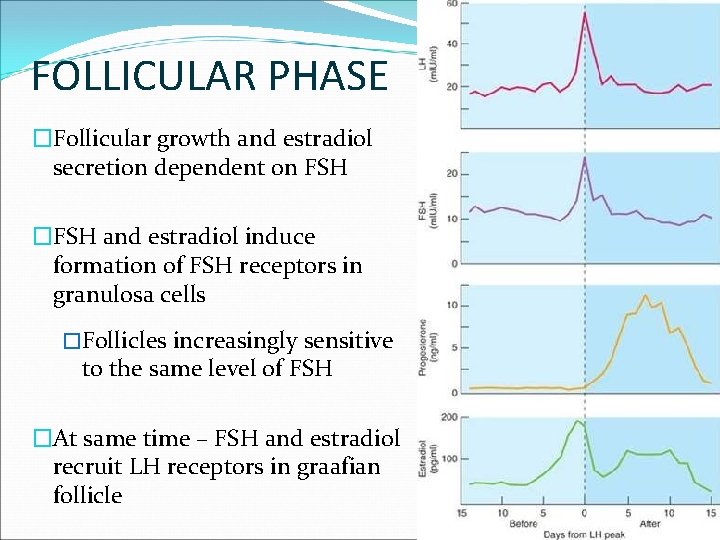
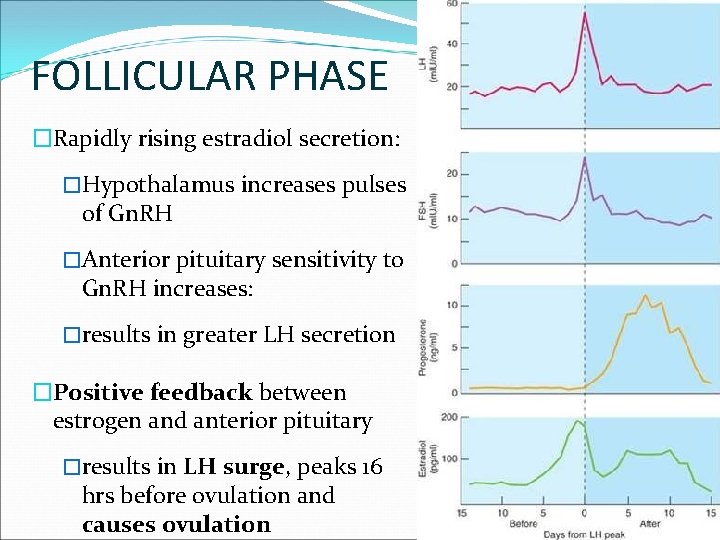
FOLLICULAR PHASE �Lasts from day 1 to ~13 �Dominated by growth and death of a cohort of primary follicles into secondary follicles �with one survivor becoming a graafian follicle �which will undergo ovulation �As follicles grow granulosa cells secrete increasing amounts of estradiol �Reaching peak about day 12
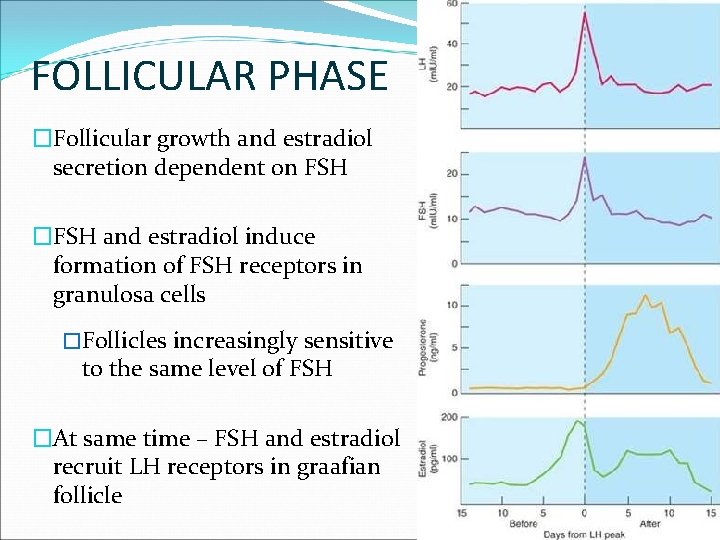
FOLLICULAR PHASE �Follicular growth and estradiol secretion dependent on FSH �FSH and estradiol induce formation of FSH receptors in granulosa cells �Follicles increasingly sensitive to the same level of FSH �At same time – FSH and estradiol recruit LH receptors in graafian follicle
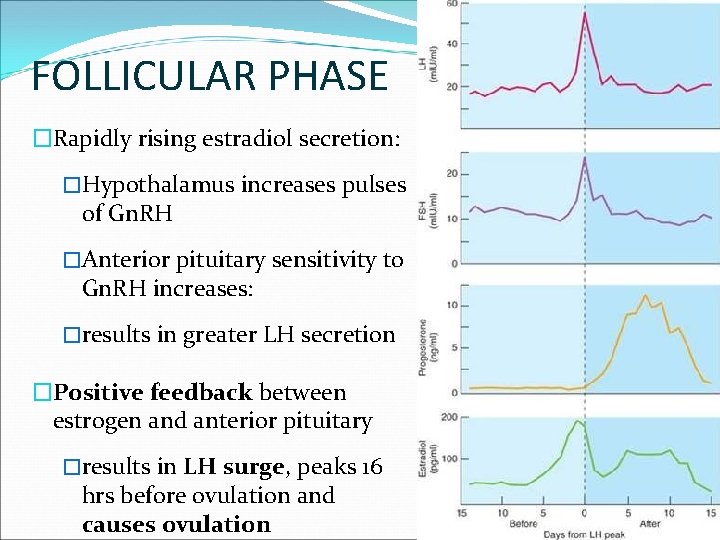
FOLLICULAR PHASE �Rapidly rising estradiol secretion: �Hypothalamus increases pulses of Gn. RH �Anterior pituitary sensitivity to Gn. RH increases: �results in greater LH secretion �Positive feedback between estrogen and anterior pituitary �results in LH surge, peaks 16 hrs before ovulation and causes ovulation
THE CYCLE OF OVULATION AND MENSTRUATION
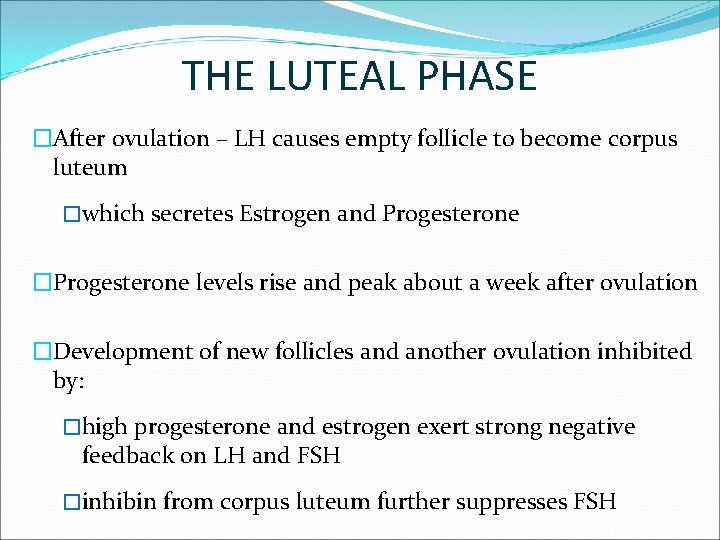
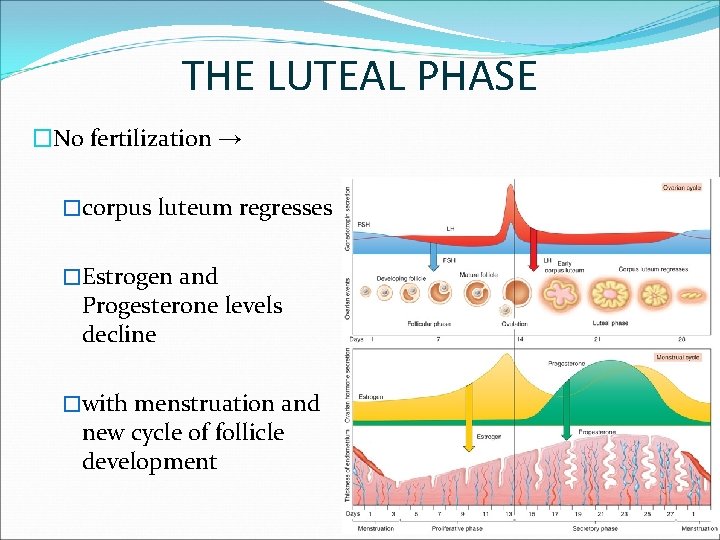
THE LUTEAL PHASE �After ovulation – LH causes empty follicle to become corpus luteum �which secretes Estrogen and Progesterone �Progesterone levels rise and peak about a week after ovulation �Development of new follicles and another ovulation inhibited by: �high progesterone and estrogen exert strong negative feedback on LH and FSH �inhibin from corpus luteum further suppresses FSH
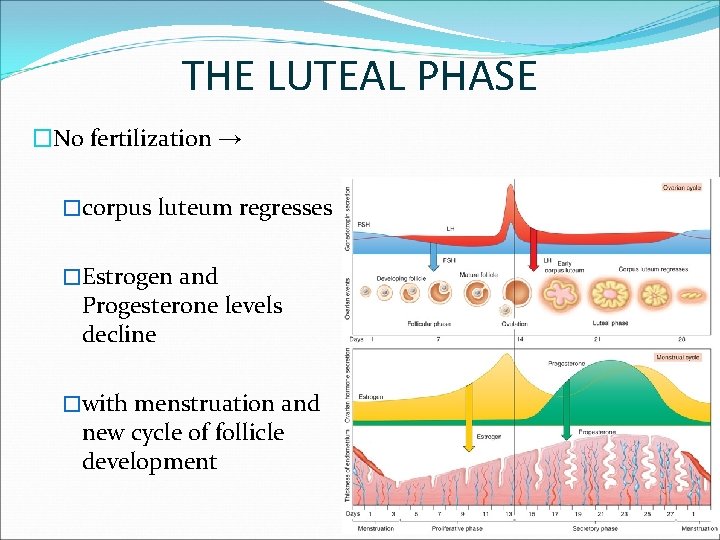
THE LUTEAL PHASE �No fertilization → �corpus luteum regresses �Estrogen and Progesterone levels decline �with menstruation and new cycle of follicle development
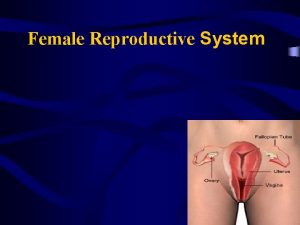
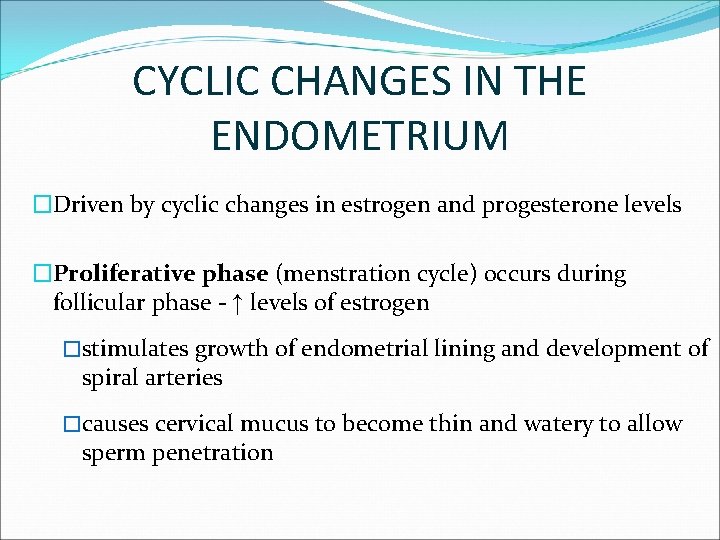
CYCLIC CHANGES IN THE ENDOMETRIUM �Driven by cyclic changes in estrogen and progesterone levels �Proliferative phase (menstration cycle) occurs during follicular phase - ↑ levels of estrogen �stimulates growth of endometrial lining and development of spiral arteries �causes cervical mucus to become thin and watery to allow sperm penetration
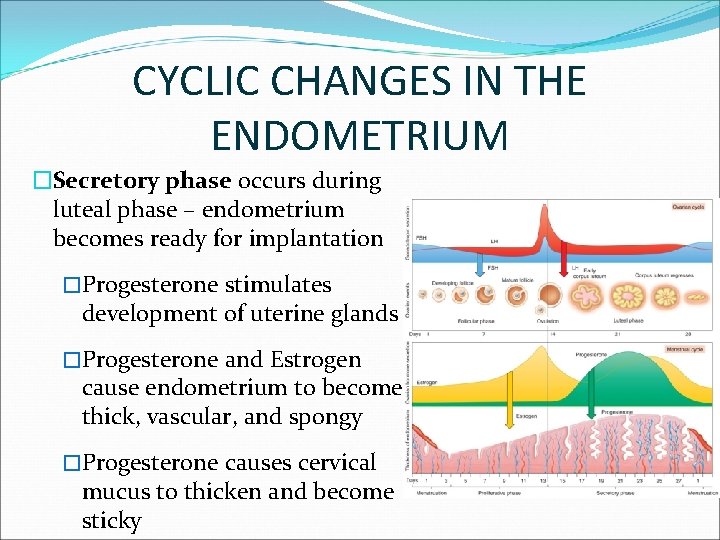
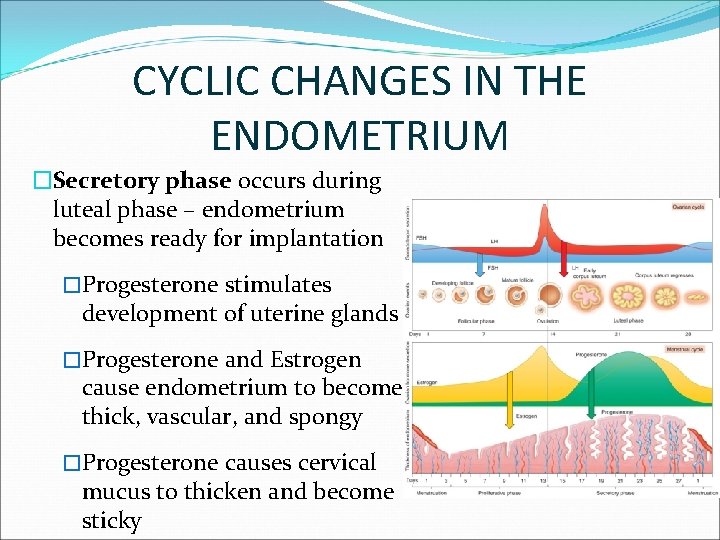
CYCLIC CHANGES IN THE ENDOMETRIUM �Secretory phase occurs during luteal phase – endometrium becomes ready for implantation �Progesterone stimulates development of uterine glands �Progesterone and Estrogen cause endometrium to become thick, vascular, and spongy �Progesterone causes cervical mucus to thicken and become sticky
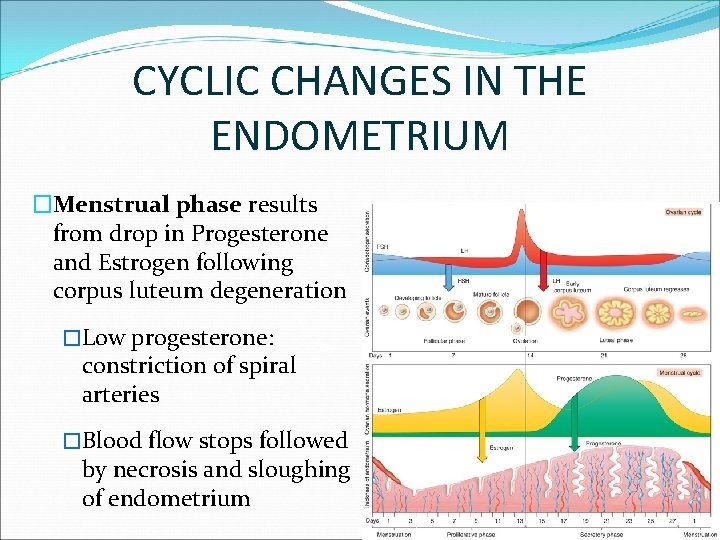
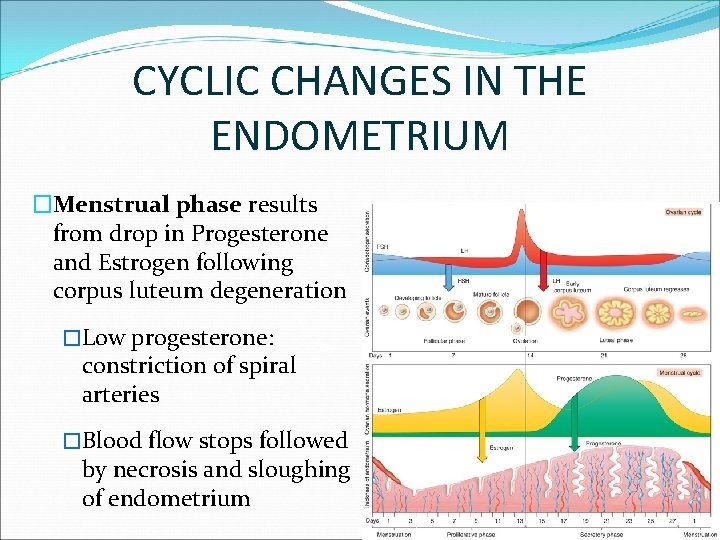
CYCLIC CHANGES IN THE ENDOMETRIUM �Menstrual phase results from drop in Progesterone and Estrogen following corpus luteum degeneration �Low progesterone: constriction of spiral arteries �Blood flow stops followed by necrosis and sloughing of endometrium
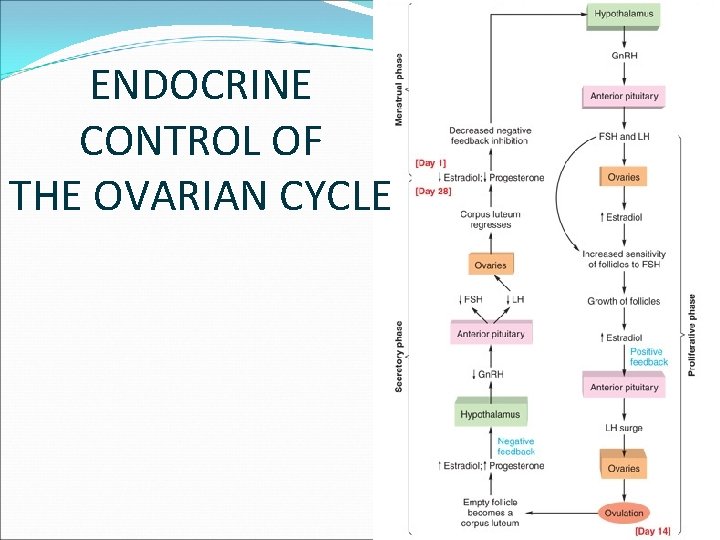
ENDOCRINE CONTROL OF THE OVARIAN CYCLE
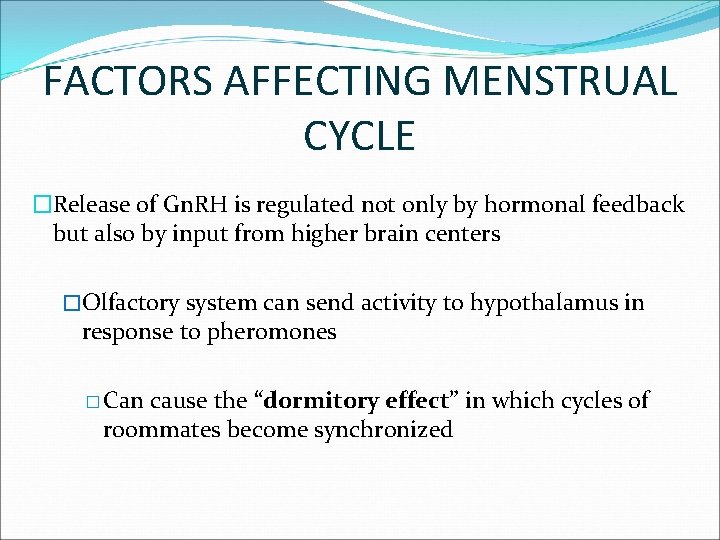
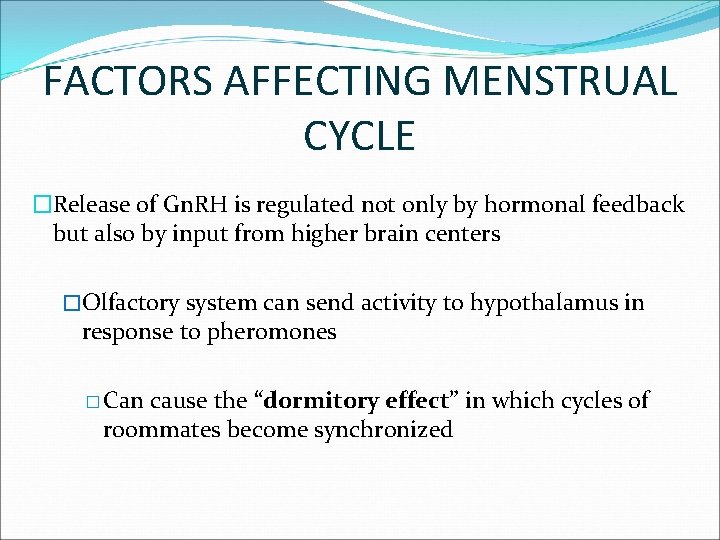
FACTORS AFFECTING MENSTRUAL CYCLE �Release of Gn. RH is regulated not only by hormonal feedback but also by input from higher brain centers �Olfactory system can send activity to hypothalamus in response to pheromones � Can cause the “dormitory effect” in which cycles of roommates become synchronized
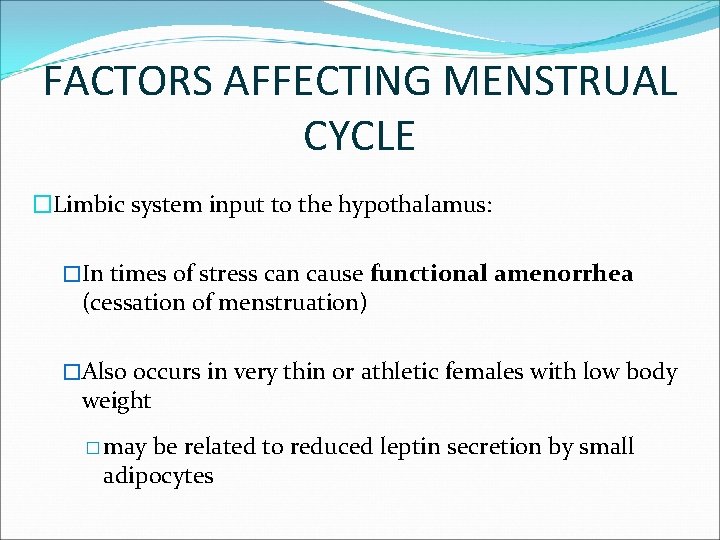
FACTORS AFFECTING MENSTRUAL CYCLE �Limbic system input to the hypothalamus: �In times of stress can cause functional amenorrhea (cessation of menstruation) �Also occurs in very thin or athletic females with low body weight � may be related to reduced leptin secretion by small adipocytes
CONTRACEPTIVE METHODS �Oral contraceptive pills – synthetic estrogen and progesterone �Taken daily for 3 weeks after menstrual period �Mimic corpus luteum, so that negative feedback inhibits ovulation �Placebo pills taken in 4 th wk to permit menstruation
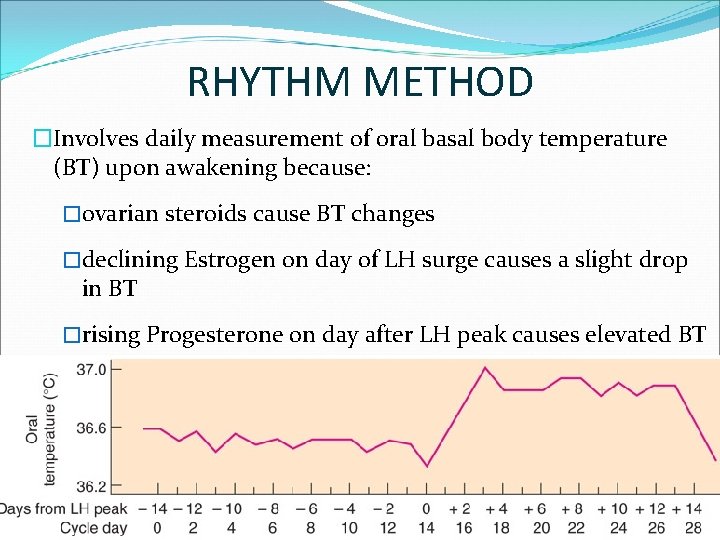
RHYTHM METHOD �Involves daily measurement of oral basal body temperature (BT) upon awakening because: �ovarian steroids cause BT changes �declining Estrogen on day of LH surge causes a slight drop in BT �rising Progesterone on day after LH peak causes elevated BT
MENOPAUSE �Cessation of ovarian activity and menstruation roughly ~50 years �Ovaries depleted of follicles produce no estrogen �LH and FSH are high because of no negative feedback �Lack of Estrogen from ovaries most responsible for: �Hot flashes, osteoporosis, and increased risk of atherosclerosis

THANKS !
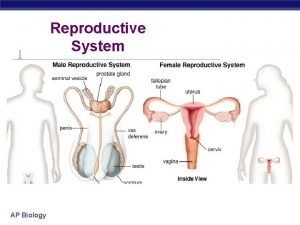
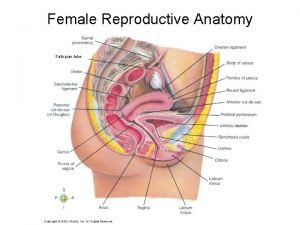
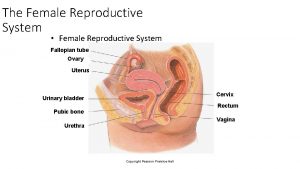
 Female reproductive system internal
Female reproductive system internal Where does mitosis occur in the female reproductive system
Where does mitosis occur in the female reproductive system Female reproductive system with baby
Female reproductive system with baby Diagram of male and female reproductive system of fish
Diagram of male and female reproductive system of fish External genital
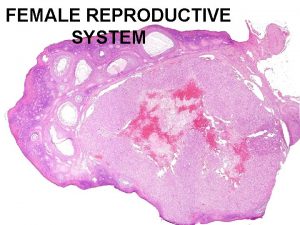
External genital Female reproductive system pathology
Female reproductive system pathology Vagina diagram labeled
Vagina diagram labeled Female reproductive system pathology
Female reproductive system pathology Figure 28-2 the female reproductive system
Figure 28-2 the female reproductive system Inguinal
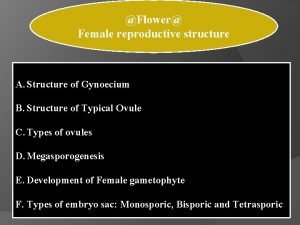
Inguinal Compylotropous ovules are found in
Compylotropous ovules are found in Similarities between male and female reproductive system
Similarities between male and female reproductive system Pea size glands flanking the vagina
Pea size glands flanking the vagina Female anatomy
Female anatomy Uterine seal
Uterine seal Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Uterus is the part of which system in pila...?
Uterus is the part of which system in pila...? Female reproductive system pathology
Female reproductive system pathology What are primary sexual characteristics
What are primary sexual characteristics Ovarian ligament.
Ovarian ligament. Female reproductive anatomy
Female reproductive anatomy Chapter 16 the reproductive system
Chapter 16 the reproductive system Penis circumcised
Penis circumcised Figure 28-2 the female reproductive system
Figure 28-2 the female reproductive system Female reproductive
Female reproductive Female reproductive organs sagittal section
Female reproductive organs sagittal section Female reproductive system pathology
Female reproductive system pathology Unit 5 lesson 3 the female reproductive system
Unit 5 lesson 3 the female reproductive system Female reproductive system color
Female reproductive system color