Infectious Disease I Gastrointestinal Infections and Enterotoxigenic Poisonings
- Slides: 40
Infectious Disease I: Gastrointestinal Infections and Enterotoxigenic Poisonings Courses in Therapeutics and Disease State Management Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 1 of 3) • Define and distinguish between watery diarrhea and dysenteric diarrhea. • Discuss the common clinical presentations of GI infections. • Describe the typical microbiology of GI infections. • Describe the appropriate indications for stool culture and its limitations. • Assess the degree of dehydration based on clinical presentation. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 2 of 3) • Choose the method of rehydration therapy based on dehydration status. • Recommend antibiotic therapy for GI infections. • Provide recommendation on the proper duration of treatment of GI infections given details of the patient condition and type of infection. • Describe the rationale and indication for antimotility agent use in diarrheal illnesses. • Describe the proper assessment of patients during treatment of GI infections. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 3 of 3) • Recommend prevention and treatment strategies for GI infections. • Outline a treatment strategy for C. difficile–related pseudomembranous colitis. • Identify the appropriate patient population and clinical situation in which antibiotics should be used for the treatment of traveler’s diarrhea. • Outline a prevention strategy for traveler’s diarrhea. • Describe the temporal timing relationships of bacterial causes of food poisoning and the severity and onset of symptoms. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Required Reading • Martin S, Jung R. Chapter 91. Gastrointestinal Infections and Enterotoxigenic Poisonings. In: Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 9 e. New York, NY: Mc. Graw-Hill; 2014. • Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31: 431– 55. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
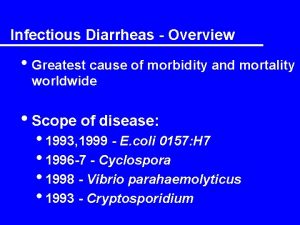
Overview • GI infections and enterotoxigenic poisonings encompass a wide variety of medical conditions characterized by inflammation of the GI tract • Vomiting and diarrhea are commonly associated with GI inflammation • Dehydration is responsible for the majority of morbidity and mortality • Diarrhea is defined as a decrease in consistency of bowel movements and an increase in frequency of stools to ≥ 3 per day • Acute disease is commonly associated with diarrhea lasting ≤ 14 • Persistent disease is associated with diarrhea that lasts >14 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
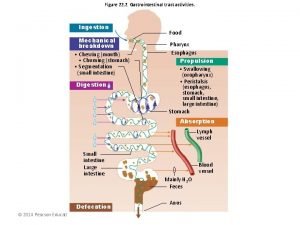
Pathophysiology • The gastrointestinal (GI) tract has the tremendous ability to absorb large amounts of fluids and electrolytes • Invading pathogens use differing mechanisms to alter the movement of ions and water across the lining of the GI tract, causing diarrhea • • Toxin production Changes in transepithelial fluid balance Mucosal invasion Acute inflammatory reactions Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Most Common Pathogens • Pathogens responsible for watery diarrhea • • Rotavirus Norovirus Enterotoxigenic Escherichia coli (ETEC) Cholera • Pathogens commonly associated with dysenteric or bloody diarrhea • • • Shigella spp. Salmonella spp. Campylobacter spp. Enterohemorrhagic E. coli (EHEC) Yersinia enterocolitica C. difficile Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
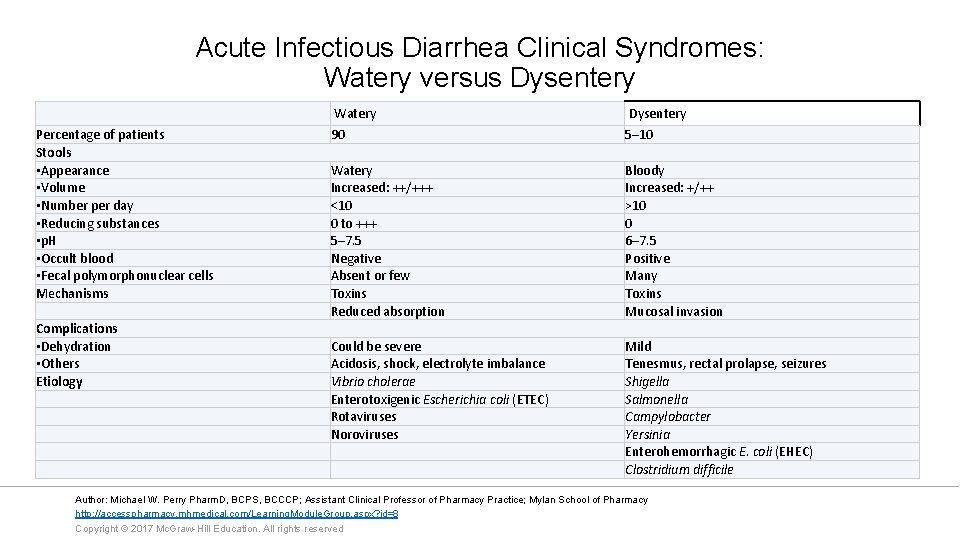
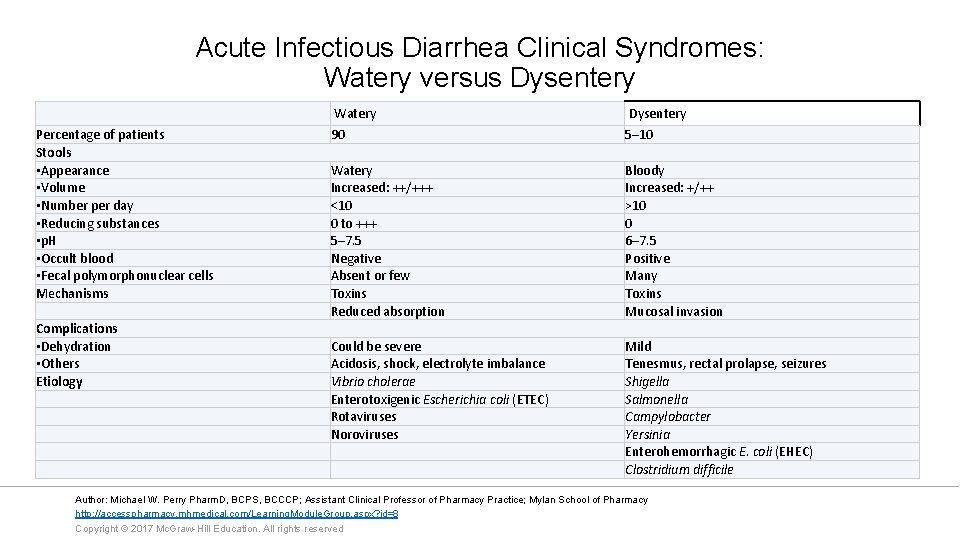
Acute Infectious Diarrhea Clinical Syndromes: Watery versus Dysentery Percentage of patients Stools • Appearance • Volume • Number per day • Reducing substances • p. H • Occult blood • Fecal polymorphonuclear cells Mechanisms Complications • Dehydration • Others Etiology Watery Dysentery 90 5– 10 Watery Increased: ++/+++ <10 0 to +++ 5– 7. 5 Negative Absent or few Toxins Reduced absorption Bloody Increased: +/++ >10 0 6– 7. 5 Positive Many Toxins Mucosal invasion Could be severe Acidosis, shock, electrolyte imbalance Vibrio cholerae Enterotoxigenic Escherichia coli (ETEC) Rotaviruses Noroviruses Mild Tenesmus, rectal prolapse, seizures Shigella Salmonella Campylobacter Yersinia Enterohemorrhagic E. coli (EHEC) Clostridium difficile Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
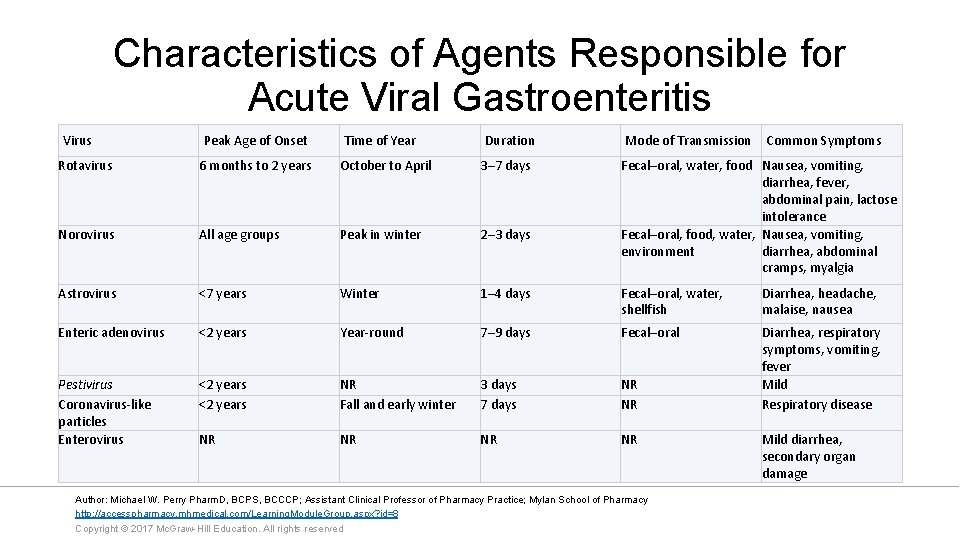
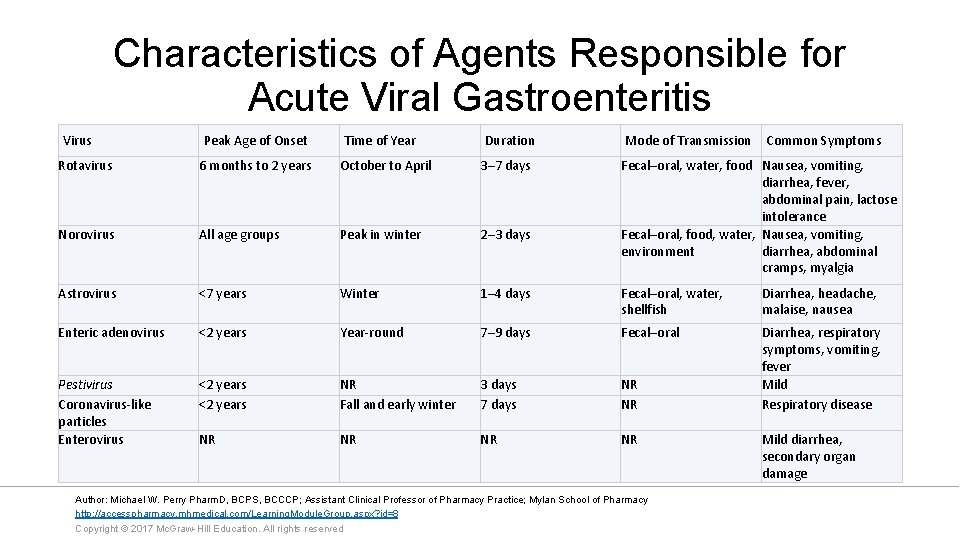
Characteristics of Agents Responsible for Acute Viral Gastroenteritis Virus Peak Age of Onset Time of Year Duration Mode of Transmission Common Symptoms Rotavirus 6 months to 2 years October to April 3– 7 days Fecal–oral, water, food Nausea, vomiting, diarrhea, fever, abdominal pain, lactose intolerance Fecal–oral, food, water, Nausea, vomiting, environment diarrhea, abdominal cramps, myalgia Norovirus All age groups Peak in winter 2– 3 days Astrovirus <7 years Winter 1– 4 days Fecal–oral, water, shellfish Diarrhea, headache, malaise, nausea Enteric adenovirus <2 years Year-round 7– 9 days Fecal–oral Pestivirus Coronavirus-like particles Enterovirus <2 years NR Fall and early winter 3 days 7 days NR NR Diarrhea, respiratory symptoms, vomiting, fever Mild Respiratory disease NR NR Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved Mild diarrhea, secondary organ damage
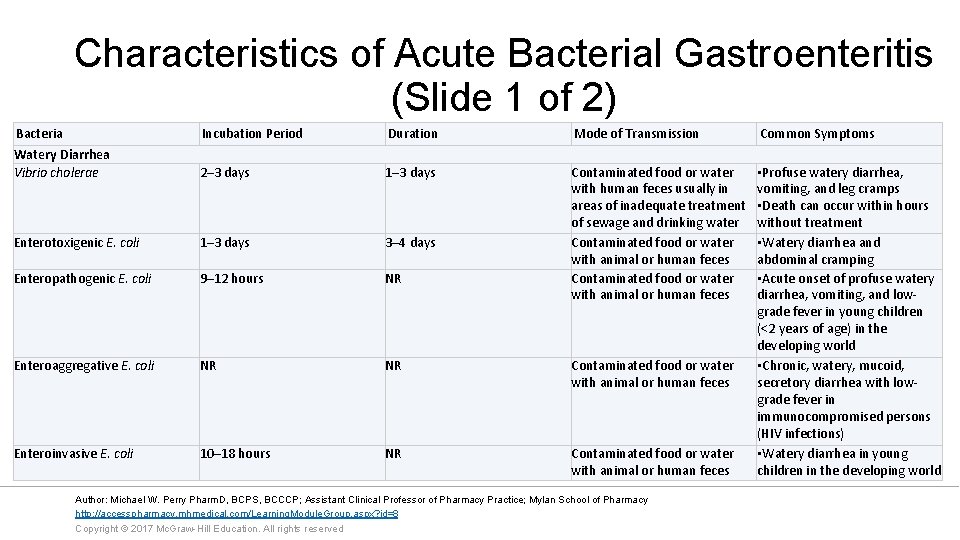
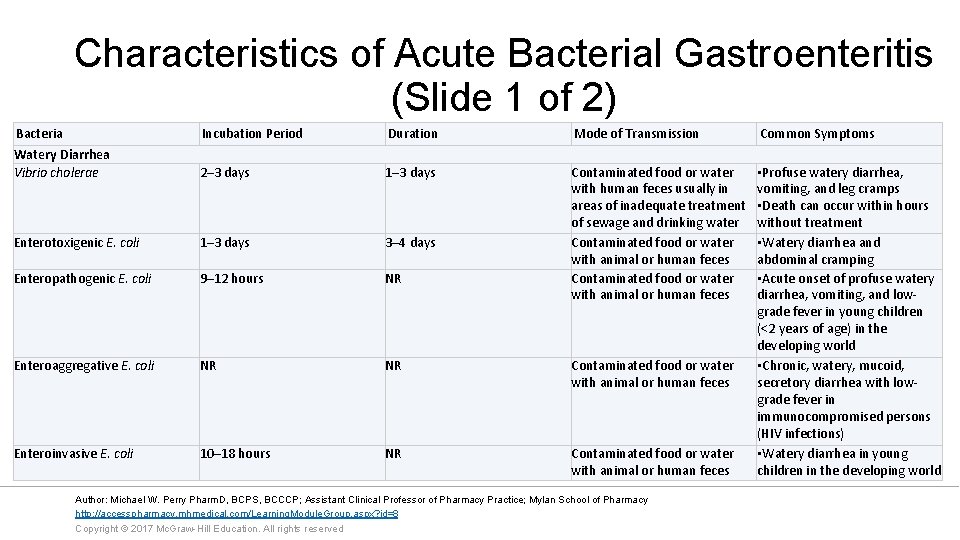
Characteristics of Acute Bacterial Gastroenteritis (Slide 1 of 2) Bacteria Watery Diarrhea Vibrio cholerae Incubation Period Duration Mode of Transmission Common Symptoms 2– 3 days 1– 3 days Enterotoxigenic E. coli 1– 3 days 3– 4 days Enteropathogenic E. coli 9– 12 hours NR Contaminated food or water with human feces usually in areas of inadequate treatment of sewage and drinking water Contaminated food or water with animal or human feces Enteroaggregative E. coli NR NR Contaminated food or water with animal or human feces Enteroinvasive E. coli 10– 18 hours NR Contaminated food or water with animal or human feces • Profuse watery diarrhea, vomiting, and leg cramps • Death can occur within hours without treatment • Watery diarrhea and abdominal cramping • Acute onset of profuse watery diarrhea, vomiting, and lowgrade fever in young children (<2 years of age) in the developing world • Chronic, watery, mucoid, secretory diarrhea with lowgrade fever in immunocompromised persons (HIV infections) • Watery diarrhea in young children in the developing world Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
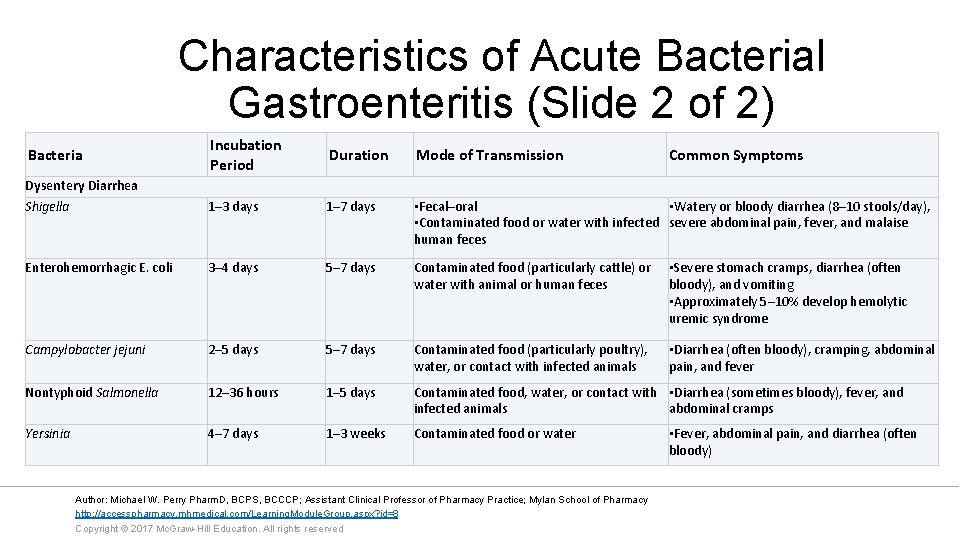
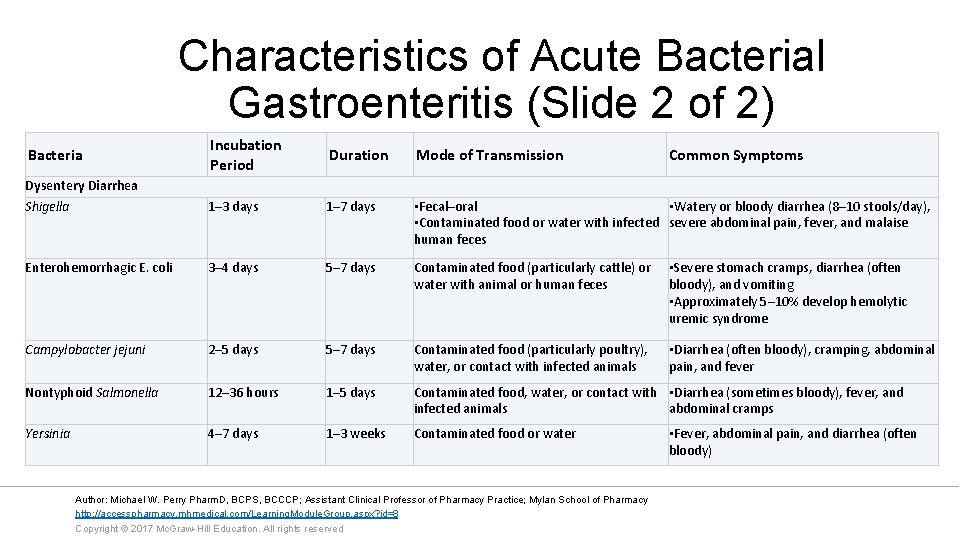
Characteristics of Acute Bacterial Gastroenteritis (Slide 2 of 2) Incubation Period Duration Mode of Transmission Dysentery Diarrhea Shigella 1– 3 days 1– 7 days • Fecal–oral • Watery or bloody diarrhea (8– 10 stools/day), • Contaminated food or water with infected severe abdominal pain, fever, and malaise human feces Enterohemorrhagic E. coli 3– 4 days 5– 7 days Contaminated food (particularly cattle) or water with animal or human feces • Severe stomach cramps, diarrhea (often bloody), and vomiting • Approximately 5– 10% develop hemolytic uremic syndrome Campylobacter jejuni 2– 5 days 5– 7 days Contaminated food (particularly poultry), water, or contact with infected animals • Diarrhea (often bloody), cramping, abdominal pain, and fever Nontyphoid Salmonella 12– 36 hours 1– 5 days Contaminated food, water, or contact with • Diarrhea (sometimes bloody), fever, and infected animals abdominal cramps Yersinia 4– 7 days 1– 3 weeks Contaminated food or water Bacteria Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved Common Symptoms • Fever, abdominal pain, and diarrhea (often bloody)
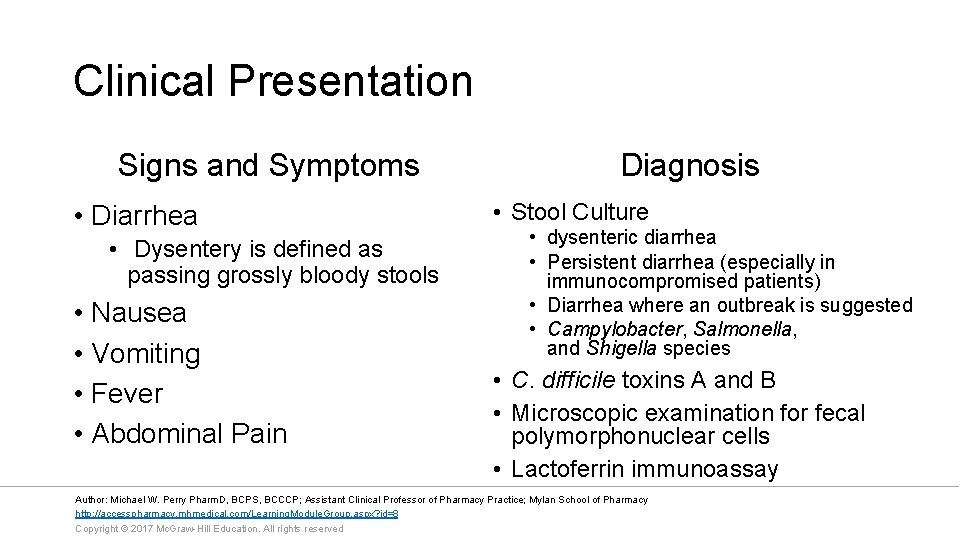
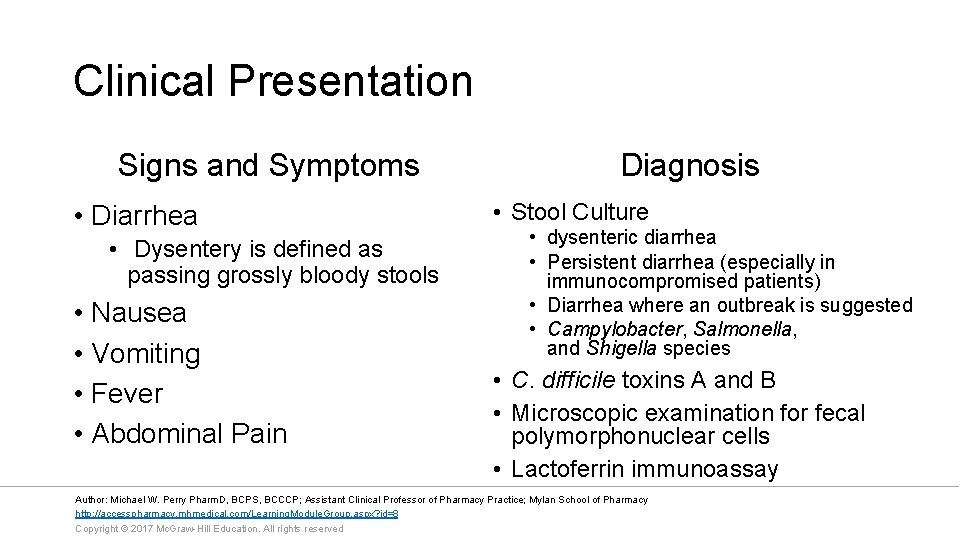
Clinical Presentation Signs and Symptoms • Diarrhea • Dysentery is defined as passing grossly bloody stools • Nausea • Vomiting • Fever • Abdominal Pain Diagnosis • Stool Culture • dysenteric diarrhea • Persistent diarrhea (especially in immunocompromised patients) • Diarrhea where an outbreak is suggested • Campylobacter, Salmonella, and Shigella species • C. difficile toxins A and B • Microscopic examination for fecal polymorphonuclear cells • Lactoferrin immunoassay Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
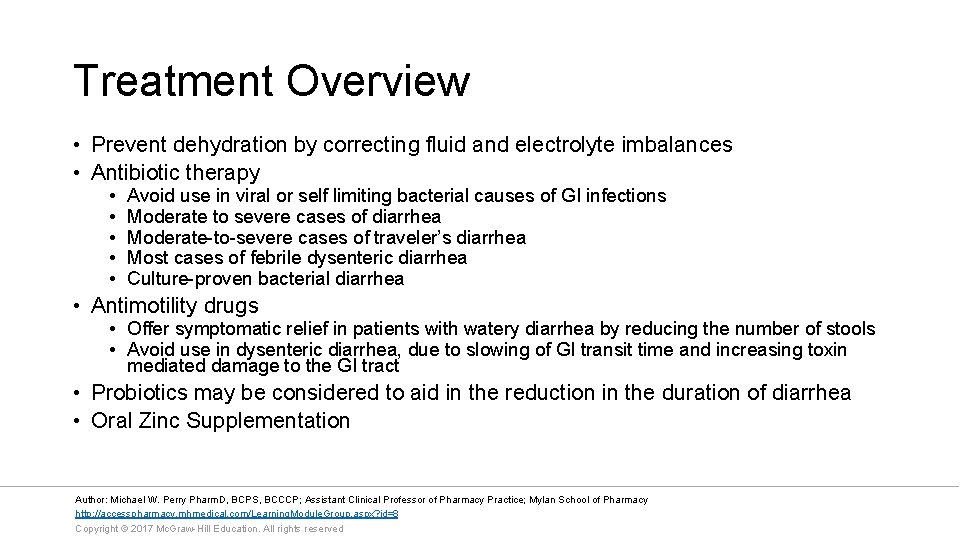
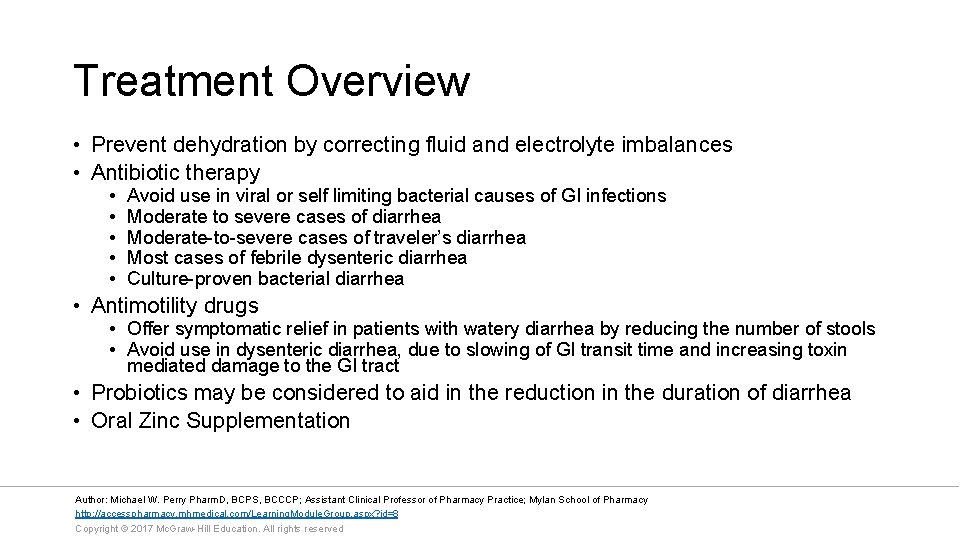
Treatment Overview • Prevent dehydration by correcting fluid and electrolyte imbalances • Antibiotic therapy • • • Avoid use in viral or self limiting bacterial causes of GI infections Moderate to severe cases of diarrhea Moderate-to-severe cases of traveler’s diarrhea Most cases of febrile dysenteric diarrhea Culture-proven bacterial diarrhea • Antimotility drugs • Offer symptomatic relief in patients with watery diarrhea by reducing the number of stools • Avoid use in dysenteric diarrhea, due to slowing of GI transit time and increasing toxin mediated damage to the GI tract • Probiotics may be considered to aid in the reduction in the duration of diarrhea • Oral Zinc Supplementation Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
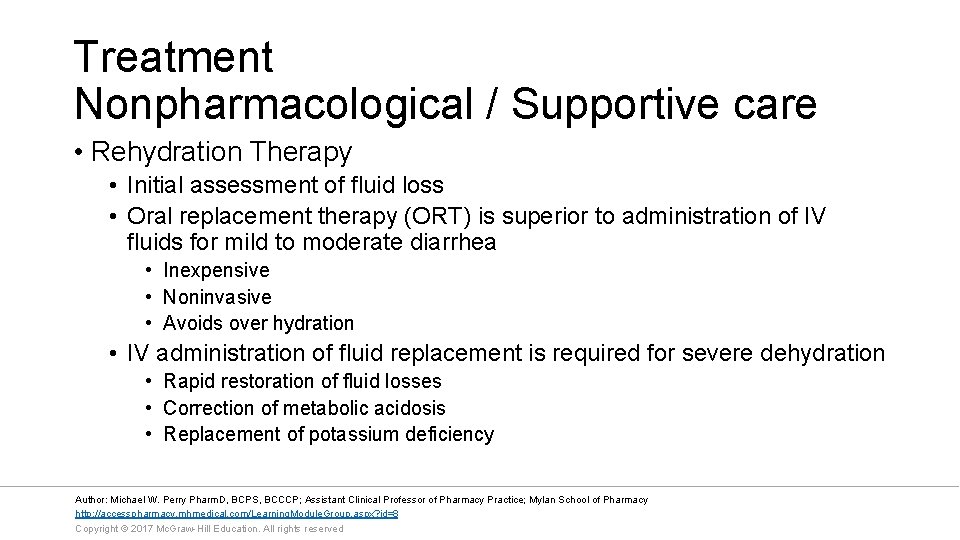
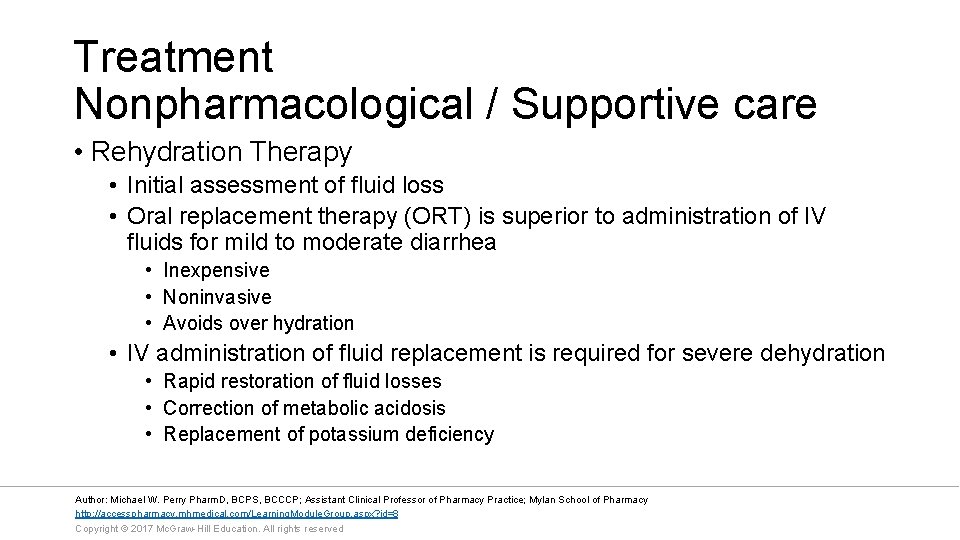
Treatment Nonpharmacological / Supportive care • Rehydration Therapy • Initial assessment of fluid loss • Oral replacement therapy (ORT) is superior to administration of IV fluids for mild to moderate diarrhea • Inexpensive • Noninvasive • Avoids over hydration • IV administration of fluid replacement is required for severe dehydration • Rapid restoration of fluid losses • Correction of metabolic acidosis • Replacement of potassium deficiency Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
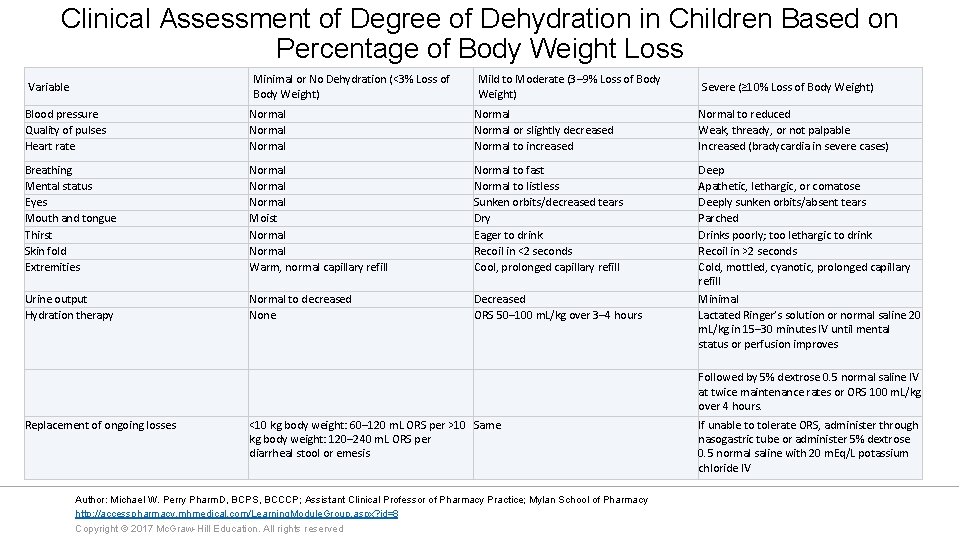
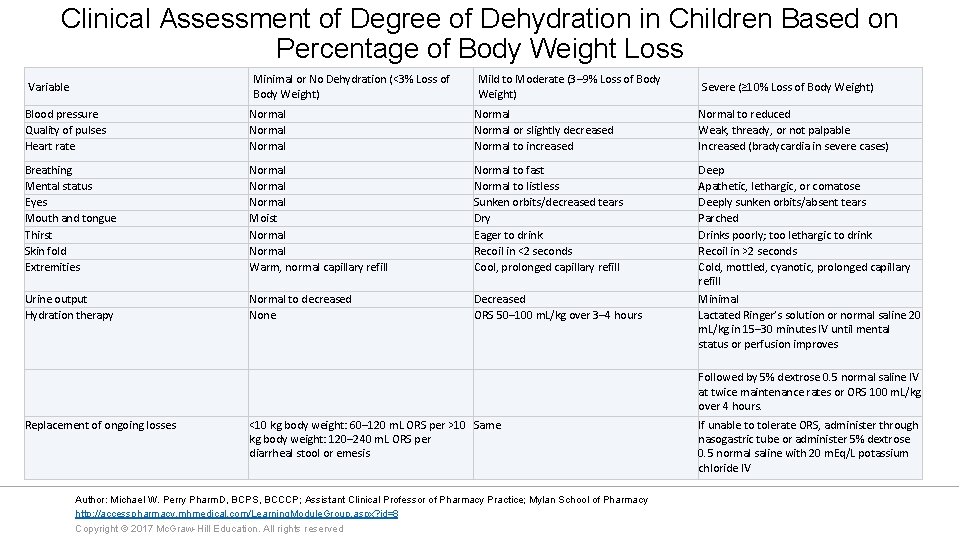
Clinical Assessment of Degree of Dehydration in Children Based on Percentage of Body Weight Loss Minimal or No Dehydration (<3% Loss of Body Weight) Variable Mild to Moderate (3– 9% Loss of Body Weight) Severe (≥ 10% Loss of Body Weight) Blood pressure Quality of pulses Heart rate Normal Normal or slightly decreased Normal to increased Normal to reduced Weak, thready, or not palpable Increased (bradycardia in severe cases) Breathing Mental status Eyes Mouth and tongue Thirst Skin fold Extremities Normal Moist Normal Warm, normal capillary refill Normal to fast Normal to listless Sunken orbits/decreased tears Dry Eager to drink Recoil in <2 seconds Cool, prolonged capillary refill Urine output Hydration therapy Normal to decreased None Decreased ORS 50– 100 m. L/kg over 3– 4 hours Deep Apathetic, lethargic, or comatose Deeply sunken orbits/absent tears Parched Drinks poorly; too lethargic to drink Recoil in >2 seconds Cold, mottled, cyanotic, prolonged capillary refill Minimal Lactated Ringer’s solution or normal saline 20 m. L/kg in 15– 30 minutes IV until mental status or perfusion improves Followed by 5% dextrose 0. 5 normal saline IV at twice maintenance rates or ORS 100 m. L/kg over 4 hours. Replacement of ongoing losses <10 kg body weight: 60– 120 m. L ORS per >10 Same kg body weight: 120– 240 m. L ORS per diarrheal stool or emesis Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved If unable to tolerate ORS, administer through nasogastric tube or administer 5% dextrose 0. 5 normal saline with 20 m. Eq/L potassium chloride IV
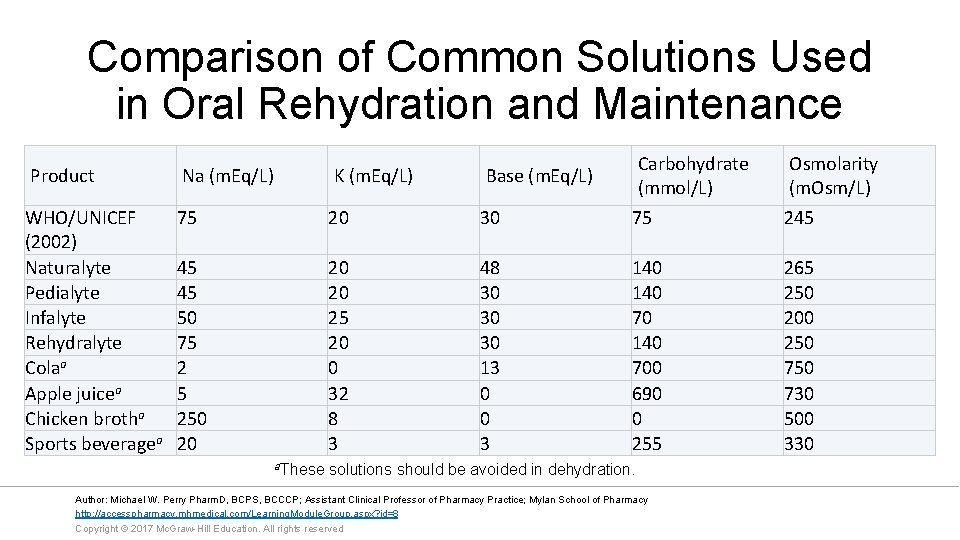
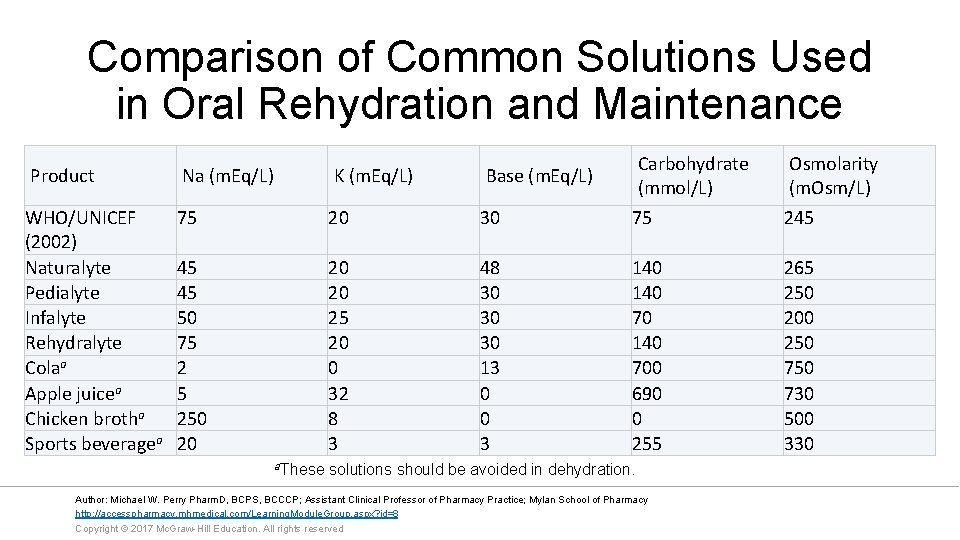
Comparison of Common Solutions Used in Oral Rehydration and Maintenance Product Na (m. Eq/L) K (m. Eq/L) Base (m. Eq/L) Carbohydrate (mmol/L) Osmolarity (m. Osm/L) WHO/UNICEF (2002) Naturalyte Pedialyte Infalyte Rehydralyte Colaa Apple juicea Chicken brotha Sports beveragea 75 20 30 75 245 45 45 50 75 2 5 250 20 25 20 0 32 8 3 48 30 30 30 13 0 0 3 140 700 690 0 255 265 250 200 250 730 500 330 a. These solutions should be avoided in dehydration. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
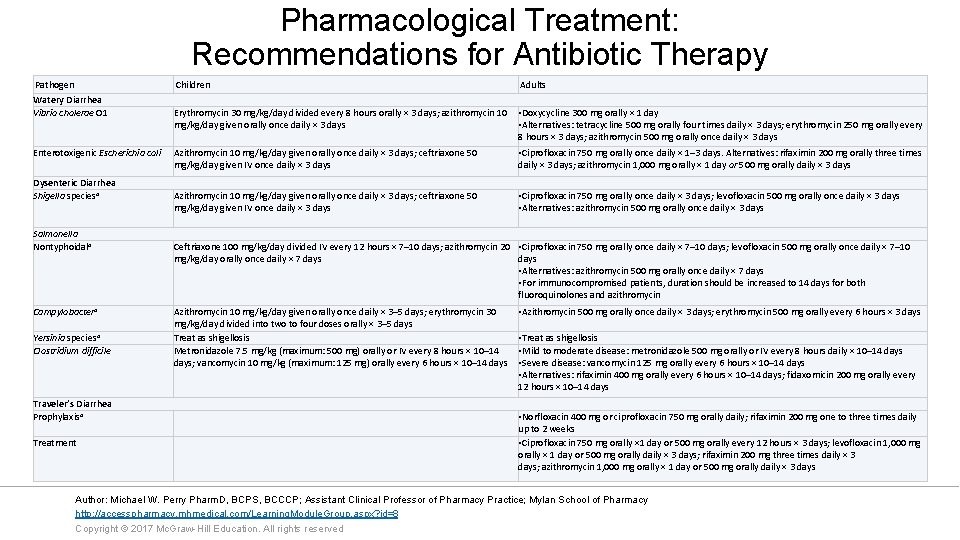
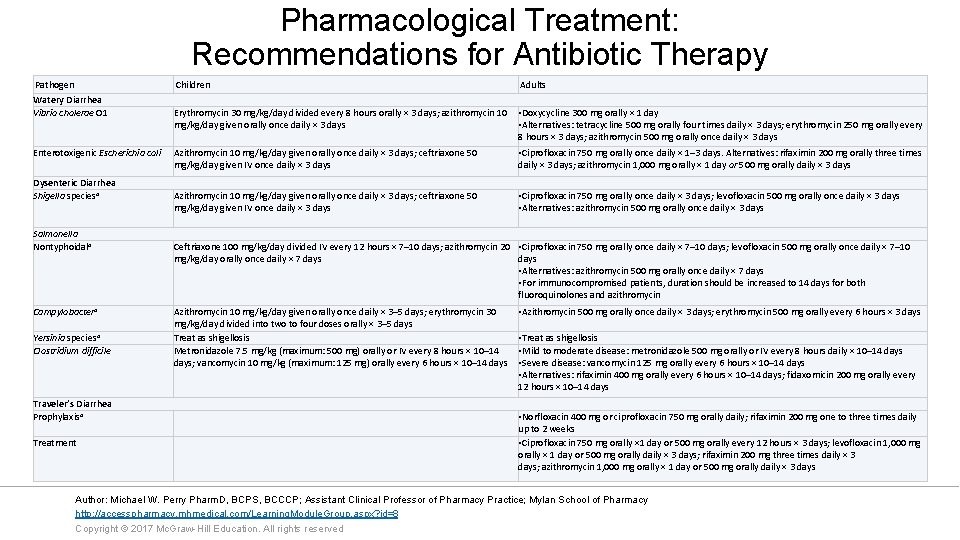
Pharmacological Treatment: Recommendations for Antibiotic Therapy Pathogen Children Watery Diarrhea Vibrio cholerae O 1 Enterotoxigenic Escherichia coli Dysenteric Diarrhea Shigella speciesa Salmonella Nontyphoidala Campylobactera Yersinia speciesa Clostridium difficile Traveler’s Diarrhea Prophylaxisa Treatment Adults Erythromycin 30 mg/kg/day divided every 8 hours orally × 3 days; azithromycin 10 • Doxycycline 300 mg orally × 1 day mg/kg/day given orally once daily × 3 days • Alternatives: tetracycline 500 mg orally four times daily × 3 days; erythromycin 250 mg orally every 8 hours × 3 days; azithromycin 500 mg orally once daily × 3 days Azithromycin 10 mg/kg/day given orally once daily × 3 days; ceftriaxone 50 mg/kg/day given IV once daily × 3 days • Ciprofloxacin 750 mg orally once daily × 1– 3 days. Alternatives: rifaximin 200 mg orally three times daily × 3 days; azithromycin 1, 000 mg orally × 1 day or 500 mg orally daily × 3 days Azithromycin 10 mg/kg/day given orally once daily × 3 days; ceftriaxone 50 mg/kg/day given IV once daily × 3 days • Ciprofloxacin 750 mg orally once daily × 3 days; levofloxacin 500 mg orally once daily × 3 days • Alternatives: azithromycin 500 mg orally once daily × 3 days Ceftriaxone 100 mg/kg/day divided IV every 12 hours × 7– 10 days; azithromycin 20 • Ciprofloxacin 750 mg orally once daily × 7– 10 days; levofloxacin 500 mg orally once daily × 7– 10 mg/kg/day orally once daily × 7 days • Alternatives: azithromycin 500 mg orally once daily × 7 days • For immunocompromised patients, duration should be increased to 14 days for both fluoroquinolones and azithromycin Azithromycin 10 mg/kg/day given orally once daily × 3– 5 days; erythromycin 30 mg/kg/day divided into two to four doses orally × 3– 5 days Treat as shigellosis Metronidazole 7. 5 mg/kg (maximum: 500 mg) orally or IV every 8 hours × 10– 14 days; vancomycin 10 mg/kg (maximum: 125 mg) orally every 6 hours × 10– 14 days • Azithromycin 500 mg orally once daily × 3 days; erythromycin 500 mg orally every 6 hours × 3 days • Treat as shigellosis • Mild to moderate disease: metronidazole 500 mg orally or IV every 8 hours daily × 10– 14 days • Severe disease: vancomycin 125 mg orally every 6 hours × 10– 14 days • Alternatives: rifaximin 400 mg orally every 6 hours × 10– 14 days; fidaxomicin 200 mg orally every 12 hours × 10– 14 days • Norfloxacin 400 mg or ciprofloxacin 750 mg orally daily; rifaximin 200 mg one to three times daily up to 2 weeks • Ciprofloxacin 750 mg orally × 1 day or 500 mg orally every 12 hours × 3 days; levofloxacin 1, 000 mg orally × 1 day or 500 mg orally daily × 3 days; rifaximin 200 mg three times daily × 3 days; azithromycin 1, 000 mg orally × 1 day or 500 mg orally daily × 3 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
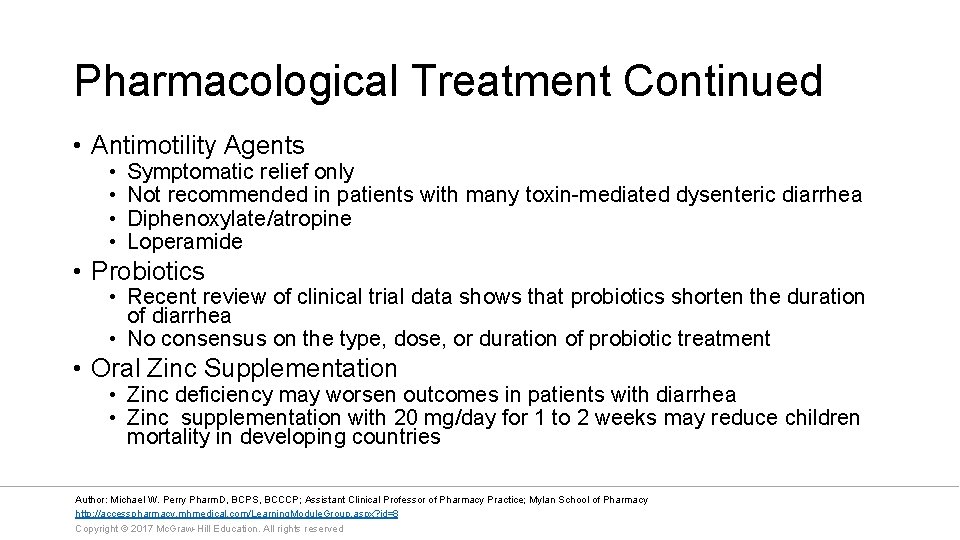
Pharmacological Treatment Continued • Antimotility Agents • • Symptomatic relief only Not recommended in patients with many toxin-mediated dysenteric diarrhea Diphenoxylate/atropine Loperamide • Probiotics • Recent review of clinical trial data shows that probiotics shorten the duration of diarrhea • No consensus on the type, dose, or duration of probiotic treatment • Oral Zinc Supplementation • Zinc deficiency may worsen outcomes in patients with diarrhea • Zinc supplementation with 20 mg/day for 1 to 2 weeks may reduce children mortality in developing countries Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Overall Monitoring • Appropriate follow-up care of patients with acute diarrhea is based on successful restoration of fluid losses • Clinical signs and symptoms should be monitored frequently for improvement or worsening • Electrolytes should be measured in those receiving IV fluids • Repeat stool samples are often unnecessary • Prompt discharge of hospitalized patients is recommended when • Rehydration is achieved • IV fluids have not been required • Oral intake equals or exceeds losses, or adequate education and medical follow-up are ensured • Most patients can be discharged in 16 to 24 hours. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Prevention • • • Clean water supply Sanitation facilities Quality control of commercial products Hand washing with soap and running water Safe food handling and preparation practices Reporting suspected outbreaks and cases of notifiable illness to local health authorities • Vaccination with available vaccines as appropriate • Typhoid fever • Rotavirus • V. cholerae Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Pathophysiology of C. difficile • C. difficile is the most commonly known cause of infectious diarrhea in hospitalized patients in North America and Europe • C. difficile is a gram-positive spore-forming anaerobic bacillus and causes a toxin-mediated disease • Toxin A and B cause diarrhea and colitis • Causes formation of pseudomembranous plaques • Preceded by use of antimicrobial therapy, which disrupts normal colonic flora allowing C. difficile overgrowth Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Clinical Presentation of C. difficile Signs and Symptoms • General • Start of diarrhea during or after antimicrobial use • Abdominal discomfort • Fever • Colitis • • • Malaise Abdominal pain Nausea Anorexia Watery diarrhea Low-grade fever Diagnosis • WBC count (marked leukocytosis) • Detection of toxin A or B • Stool culture for C. difficile • Endoscopic exam • Fulminant disease • Severe abdominal pain • Perfuse diarrhea • High fever Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Treatment Overview for C. difficile • Discontinuation of antibiotic therapy if possible • Fluid and electrolyte replacement as needed • Antimicrobial therapy directed at C. difficile Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Pharmacological Treatment of C. difficile (Slide 1 of 2) • Metronidazole • Mild to moderate CDI: 500 mg PO three times daily for 10 to 14 days • Severe CDI: 500 mg IV three times daily for 10 to 14 days • Vancomycin ORAL • Mild to moderate: 125 mg PO four times daily for 10 to 14 days • Severe: 125 mg PO four times daily for 10 to 14 days • Severe Complicated CDI use combined therapy • Vancomycin 500 mg via enteral route four times daily • Metronidazole 500 mg IV three times daily Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Pharmacological Treatment of C. difficile (Slide 2 of 2) • Recurrence Treatment Strategies • First recurrence: use same agent used to treat the initial episode of CDI • Second recurrence: Vancomycin in a tapered and/or pulse dosing strategy • Otherapies • Fidaxomicin macrocyclic oral antibiotic that has minimal bioavailability, and is bacteriostatic against C. difficile • Bezlotoxumab is a monoclonal antibody that binds to and neutralizes C. difficile toxin B Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Overall Monitoring • Duration of therapy is generally 10 -14 days • Patients with multiple treatment failures should referred to a specialist Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Pathophysiology Traveler’s Diarrhea • Traveler’s diarrhea describes the clinical syndrome manifested by malaise, anorexia, and abdominal cramps followed by the sudden onset of diarrhea that incapacitates many travelers. • Traveler’s diarrhea is caused by contaminated food or water • Symptoms usually occurs during the first week of travel Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Most Common Pathogens • Enterotoxigenic Escherichia coli • Shigella Campylobacter • Salmonella • Viruses • Parasites Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Clinical Presentation: Traveler’s Diarrhea • • Malaise Anorexia Abdominal cramps Sudden onset of diarrhea • Mild diarrhea 1 to 3 loose stools/day that are associated with abdominal cramps lasting less than 14 days. • Moderate diarrhea >4 loose stools daily associated with dehydration • Severe diarrhea is defined as the presence of fever or blood in stools • Viral Pathogen Symptoms • Conjunctivitis • Coryza • Cough • Laboratory Tests • Throat Swab Culture • Rapid antigen-detection test Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Treatment Traveler’s Diarrhea: Nonpharmacological / Supportive care Avoiding high-risk food and beverages • • • Raw or undercooked meat and seafood Moist foods served at room temperature Fruits that cannot be peeled Vegetables Milk from a questionable source Hot sauces on the table Tap water Unsealed bottled water Iced drinks Food from a street vendor Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Pharmacological Prevention of Traveler’s Diarrhea • Bismuth subsalicylate 524 orally four times daily for up to 3 weeks • Prophylactic Antibiotics are not routinely recommended • High-risk individuals or important situations (military operations) may benefit • Fluoroquinolones are the mainstay of prophylactic antibiotics • Azithromycin may be considered when traveling is South Asia and South east Asia due to resistance to Fluoroquinolones • Rifaximin may be considered in patients traveling to areas where E. coli predominates Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Pharmacological Treatment of Traveler’s Diarrhea (Slide 1 of 2) • Fluid and electrolyte replacement should be initiated at the onset of diarrhea • Symptomatic Relief • Loperamide 4 mg orally initially and then 2 mg with each subsequent loose stool to a maximum of 16 mg/day • Do not use if bloody diarrhea and fever is present • Loperamide should be discontinued if symptoms persist for more than 48 hours. • Bismuth subsalicylate 524 mg every 30 minutes for up to eight doses Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
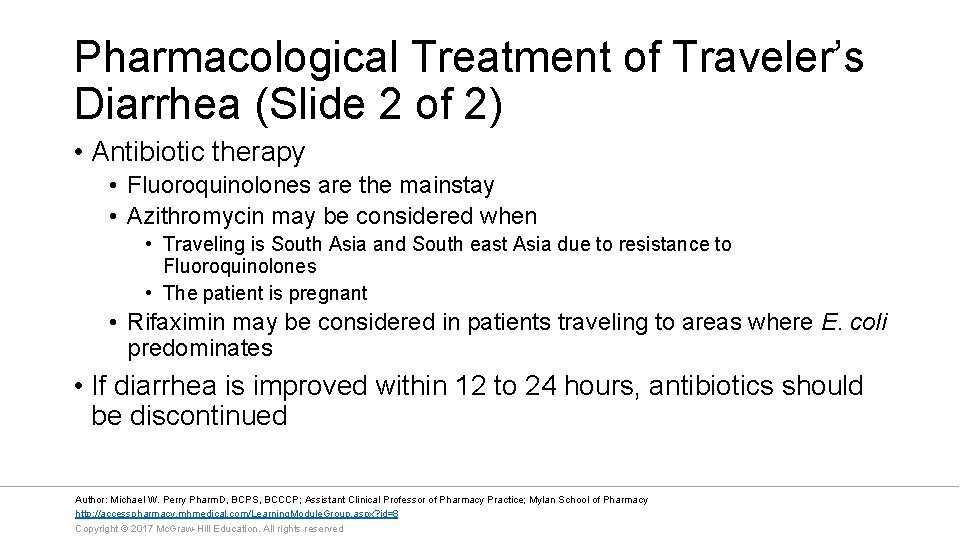
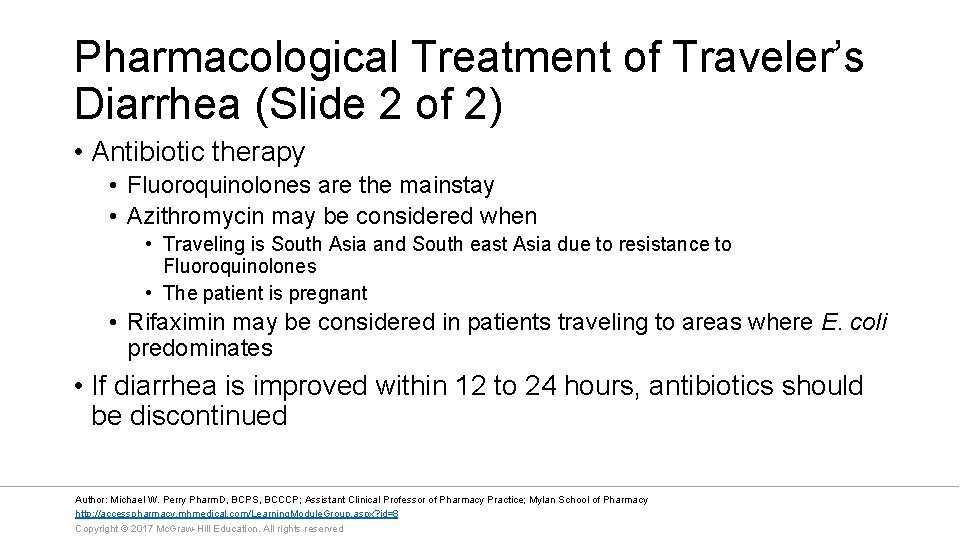
Pharmacological Treatment of Traveler’s Diarrhea (Slide 2 of 2) • Antibiotic therapy • Fluoroquinolones are the mainstay • Azithromycin may be considered when • Traveling is South Asia and South east Asia due to resistance to Fluoroquinolones • The patient is pregnant • Rifaximin may be considered in patients traveling to areas where E. coli predominates • If diarrhea is improved within 12 to 24 hours, antibiotics should be discontinued Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Food Poisoning Overview • Foodborne illnesses result from the ingestion of food containing pathogenic microorganisms that cause GI infections or preformed toxins that were produced by microorganisms that cause enterotoxigenic poisonings Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Most Common Pathogens in Food Poisoning • Staphylococcus aureus • Bacillus cereus • Clostridium perfringens • Clostridium botulinum • Norovirus • nontyphoidal Salmonella • Campylobacter spp. • Shigella • E. coli Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
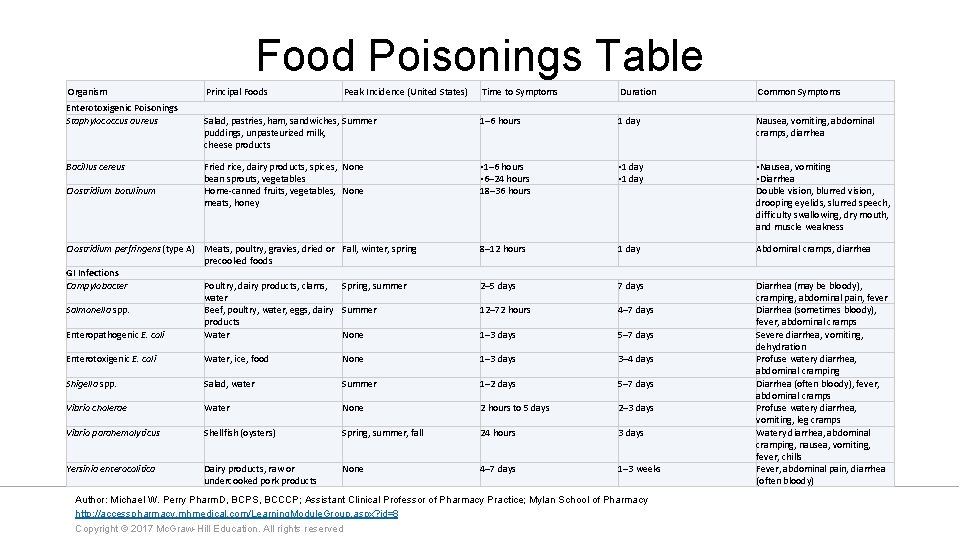
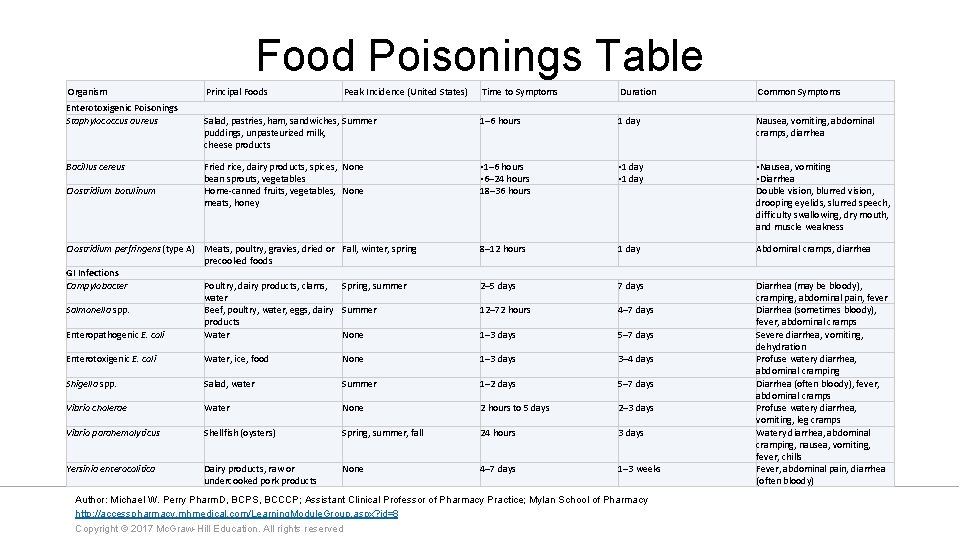
Food Poisonings Table Organism Enterotoxigenic Poisonings Staphylococcus aureus Bacillus cereus Clostridium botulinum Principal Foods Peak Incidence (United States) Time to Symptoms Duration Common Symptoms Salad, pastries, ham, sandwiches, Summer puddings, unpasteurized milk, cheese products 1– 6 hours 1 day Nausea, vomiting, abdominal cramps, diarrhea Fried rice, dairy products, spices, None bean sprouts, vegetables Home-canned fruits, vegetables, None meats, honey • 1– 6 hours • 6– 24 hours 18– 36 hours • 1 day • Nausea, vomiting • Diarrhea Double vision, blurred vision, drooping eyelids, slurred speech, difficulty swallowing, dry mouth, and muscle weakness Clostridium perfringens (type A) Meats, poultry, gravies, dried or precooked foods GI Infections Campylobacter Poultry, dairy products, clams, water Salmonella spp. Beef, poultry, water, eggs, dairy products Enteropathogenic E. coli Water Fall, winter, spring 8– 12 hours 1 day Abdominal cramps, diarrhea Spring, summer 2– 5 days 7 days Summer 12– 72 hours 4– 7 days None 1– 3 days 5– 7 days Enterotoxigenic E. coli Water, ice, food None 1– 3 days 3– 4 days Shigella spp. Salad, water Summer 1– 2 days 5– 7 days Vibrio cholerae Water None 2 hours to 5 days 2– 3 days Vibrio parahemolyticus Shellfish (oysters) Spring, summer, fall 24 hours 3 days Yersinia enterocolitica Dairy products, raw or undercooked pork products None 4– 7 days 1– 3 weeks Diarrhea (may be bloody), cramping, abdominal pain, fever Diarrhea (sometimes bloody), fever, abdominal cramps Severe diarrhea, vomiting, dehydration Profuse watery diarrhea, abdominal cramping Diarrhea (often bloody), fever, abdominal cramps Profuse watery diarrhea, vomiting, leg cramps Watery diarrhea, abdominal cramping, nausea, vomiting, fever, chills Fever, abdominal pain, diarrhea (often bloody) Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Food Poisoning Treatment • Fluid and electrolyte management • Oral Rehydration therapy • IV fluids • Antiemetics and antiperistaltic agents offer symptomatic relief, but the latter should not be given in patients who present with high fever, bloody diarrhea, or fecal leukocytes • Many of the foodborne illnesses can be prevented with proper food selection, preparation, and storage Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Summary • GI infections and enterotoxigenic poisonings encompass a wide variety of medical conditions characterized by inflammation of the GI tract • Rehydration therapy is the main therapy to counteract the detrimental effects of dehydration from vomiting and diarrhea • Symptomatic therapy with antiperistaltic agents may be helpful in some patients, but should not be used in patients with bloody stools or high fever • Antimicrobial therapy should be reserved for patients that are high risk or a pathogen is identified that responds to antimicrobial therapy Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
References • Martin S, Jung R. Chapter 91. Gastrointestinal Infections and Enterotoxigenic Poisonings. In: Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 9 e. New York, NY: Mc. Graw-Hill; 2014. • Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31: 431– 55. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
 Enterotoxigenic
Enterotoxigenic Enterotoxigenic
Enterotoxigenic Conistipation
Conistipation Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Infectious disease quality controls
Infectious disease quality controls Stages of infection
Stages of infection Stages of infectious disease
Stages of infectious disease Infectious disease board review
Infectious disease board review Infectious disease
Infectious disease Hennepin county infectious disease manual
Hennepin county infectious disease manual What is the smallest infectious disease agent
What is the smallest infectious disease agent Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Communicable disease and non communicable disease
Communicable disease and non communicable disease A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Bone and joint infections
Bone and joint infections Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Embriologia del sistema gastrointestinal
Embriologia del sistema gastrointestinal Gastrointestinal tract
Gastrointestinal tract Chemotrypsinogen
Chemotrypsinogen Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Gastrointestinal hormones
Gastrointestinal hormones Dr sigit djuniawan
Dr sigit djuniawan Livores violáceos
Livores violáceos Sefalik faz
Sefalik faz Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Nutrition focused physical assessment
Nutrition focused physical assessment Cloaca
Cloaca Composition of stomach
Composition of stomach Motilidad gastrointestinal
Motilidad gastrointestinal Gastinoma
Gastinoma Sistema digestivo
Sistema digestivo Rins anatomia
Rins anatomia Sublingual ilaç uygulaması
Sublingual ilaç uygulaması Intestinal villus
Intestinal villus Gastrointestinal
Gastrointestinal Metformin and constipation
Metformin and constipation Distal organ
Distal organ Nursing care for gastrointestinal disorders
Nursing care for gastrointestinal disorders Nursing diagnosis for pud
Nursing diagnosis for pud