Infectious Disease I Central Nervous System Infections Courses

- Slides: 44
Infectious Disease I: Central Nervous System Infections Courses in Therapeutics and Disease State Management Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 1 of 3) • Define meningitis and encephalitis • List, in order of relative incidence, the most common age-dependent bacterial causes of meningitis, and identify the fatality rate associated with each • Analyze laboratory values of CSF components and describe the values as normal or as indicative of a specific infective condition • Identify the common signs and symptoms of bacterial meningitis • Select appropriate empirical therapy directed against suspected bacterial meningitis according to age group Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 2 of 3) • List the antibiotic of first choice and alternatives to treat meningitis secondary to Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae • Identify general principles of chemoprophylaxis after exposure to H. influenzae and N. meningitidis index cases • List the physiochemical properties associated with increased penetration of antibiotics into the CNS • Classify antibiotics according to level of penetration into the CNS • List three reasons why corticosteroid use in bacterial meningitis is controversial Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 3 of 3) • Assess the value of dexamethasone as adjunctive therapy in meningitis • Discuss the role vaccination plays in the prevention of meningitis and what impact vaccination is having on the epidemiology of meningitis • Select appropriate antifungal therapy to treat Cryptococcus neoformans • List the viruses most commonly associated with encephalitis and meningoencephalitis and provide recommendations for therapy as appropriate Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Required Reading • Elshaboury RH, Hermsen ED, Holt JS, Mitropoulos IF, Rotschafer JC. Chapter 84. Central Nervous System Infections In: Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 9 e. New York, NY: Mc. Graw-Hill; 2014. • Tunkel AR, Hartman BJ, Kaplan SL, et. al. . 2004. Practice guidelines for the management of bacterial meningitis. Clin. Infect. Dis. 39: 1267 -1284. • Tunkel AR, Hasbun R, Bhimraj A, et. al. . 2017 Infectious Diseases Society of America’s Clinical Practice Guidelines for Healthcare. Associated Ventriculitis and Meningitis. Clin Infect Dis 2017; 64 (6): e 34 -e 65. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
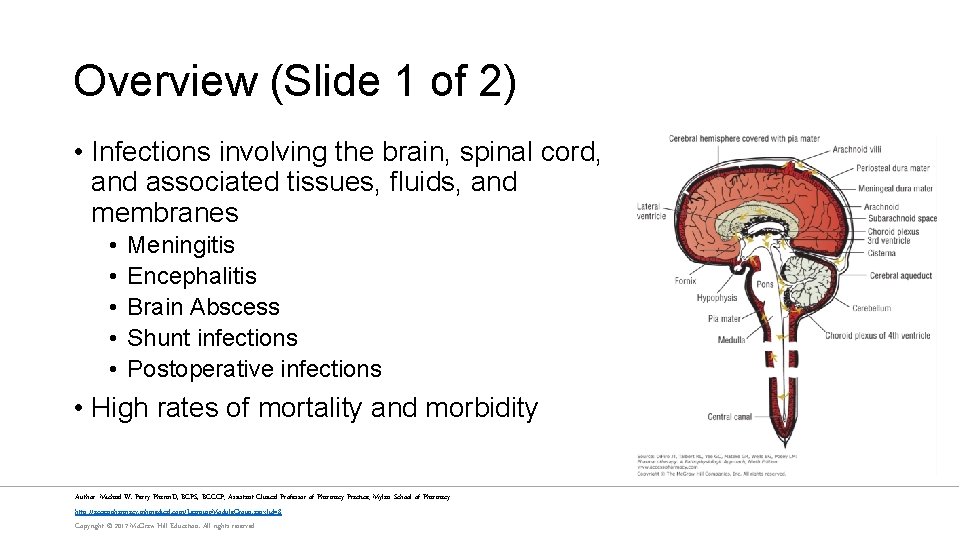
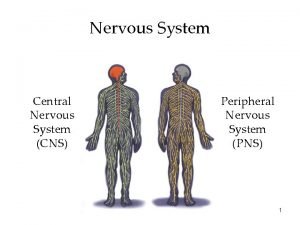
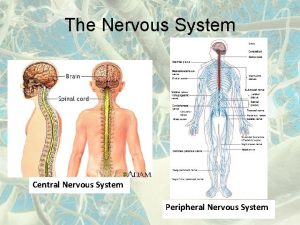
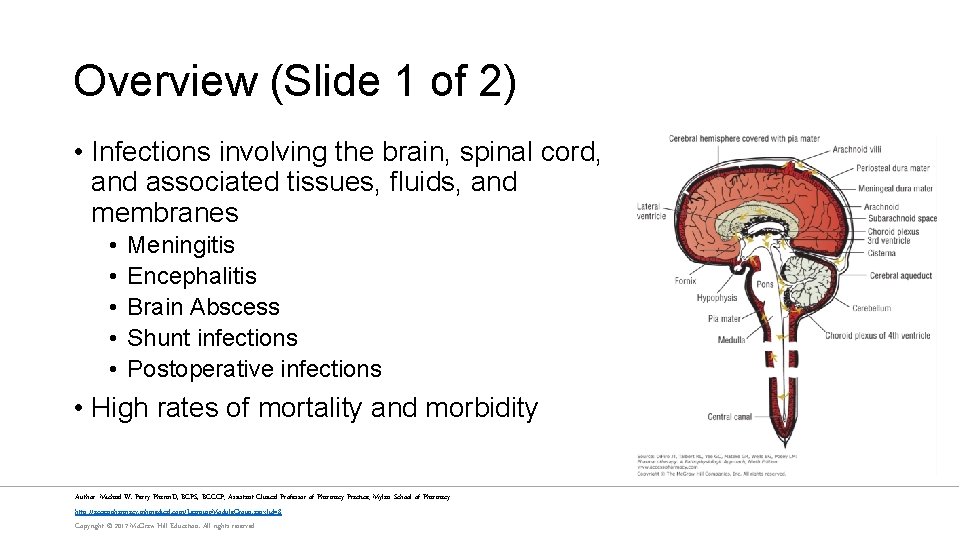
Overview (Slide 1 of 2) • Infections involving the brain, spinal cord, and associated tissues, fluids, and membranes • • • Meningitis Encephalitis Brain Abscess Shunt infections Postoperative infections • High rates of mortality and morbidity Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Overview (Slide 2 of 2) • Community Acquired Meningitis • Healthcare-associated Ventriculitis and Meningitis • • • Cerebrospinal fluid (CSF) shunts CSF drains Intrathecal infusion pumps Deep brain stimulation hardware Neurosurgery or Head Trauma Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
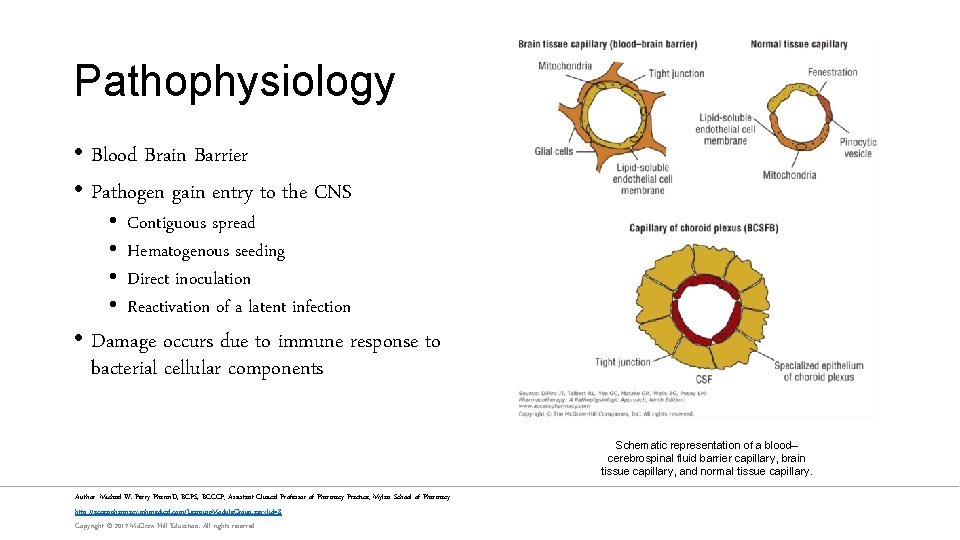
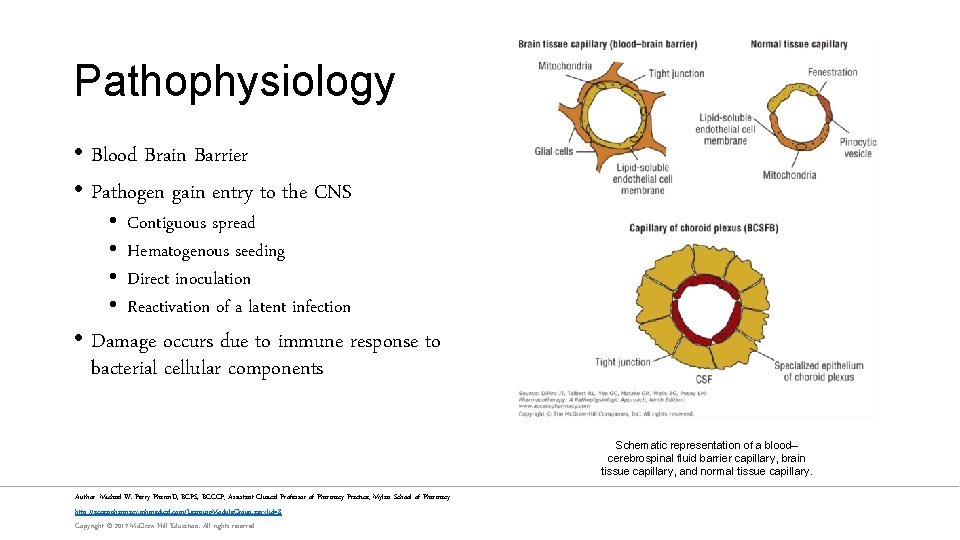
Pathophysiology • Blood Brain Barrier • Pathogen gain entry to the CNS • • Contiguous spread Hematogenous seeding Direct inoculation Reactivation of a latent infection • Damage occurs due to immune response to bacterial cellular components Schematic representation of a blood– cerebrospinal fluid barrier capillary, brain tissue capillary, and normal tissue capillary. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
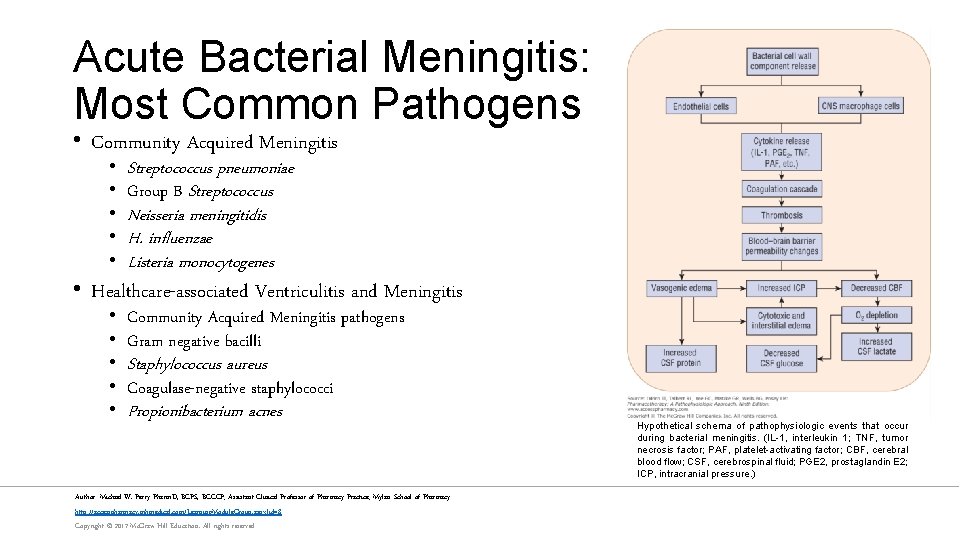
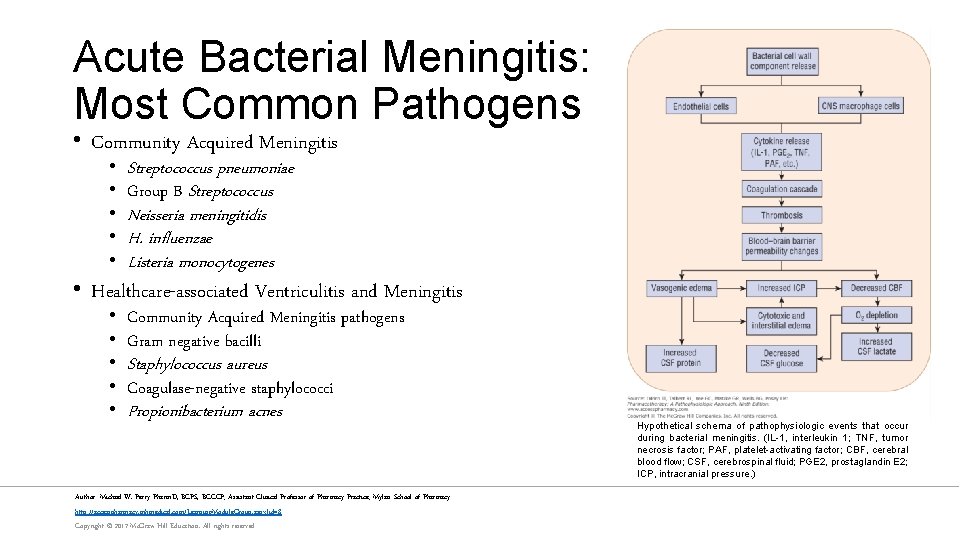
Acute Bacterial Meningitis: Most Common Pathogens • Community Acquired Meningitis • • • Streptococcus pneumoniae Group B Streptococcus Neisseria meningitidis H. influenzae Listeria monocytogenes • Healthcare-associated Ventriculitis and Meningitis • • • Community Acquired Meningitis pathogens Gram negative bacilli Staphylococcus aureus Coagulase-negative staphylococci Propionibacterium acnes Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved Hypothetical schema of pathophysiologic events that occur during bacterial meningitis. (IL-1, interleukin 1; TNF, tumor necrosis factor; PAF, platelet-activating factor; CBF, cerebral blood flow; CSF, cerebrospinal fluid; PGE 2, prostaglandin E 2; ICP, intracranial pressure. )
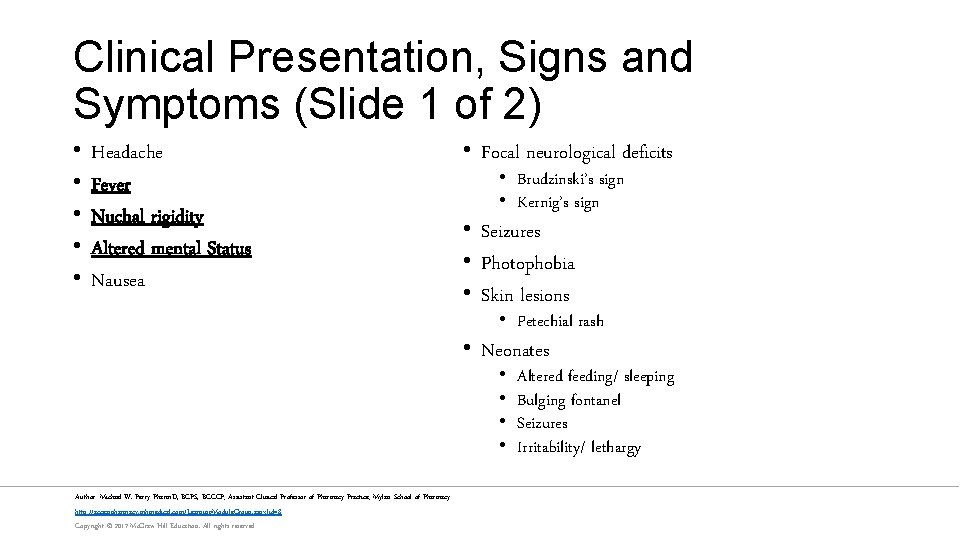
Clinical Presentation, Signs and Symptoms (Slide 1 of 2) • • • Headache Fever Nuchal rigidity Altered mental Status Nausea • Focal neurological deficits • Brudzinski’s sign • Kernig’s sign • Seizures • Photophobia • Skin lesions • Petechial rash • Neonates • • Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved Altered feeding/ sleeping Bulging fontanel Seizures Irritability/ lethargy
Clinical Presentation, Signs and Symptoms (Slide 2 of 2) Link: Schematic of Brudzinski’s signs Link: Schematic of Kernig’s sign Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Laboratory Tests • Lumbar Puncture • • Opening Pressure CSF composition CSF gram stain CSF culture • Blood Cultures • Scraping of skin lesions • WBC Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved • Cranial Imaging • Magnetic resonance imaging (MRI) • Computed tomography (CT) scan
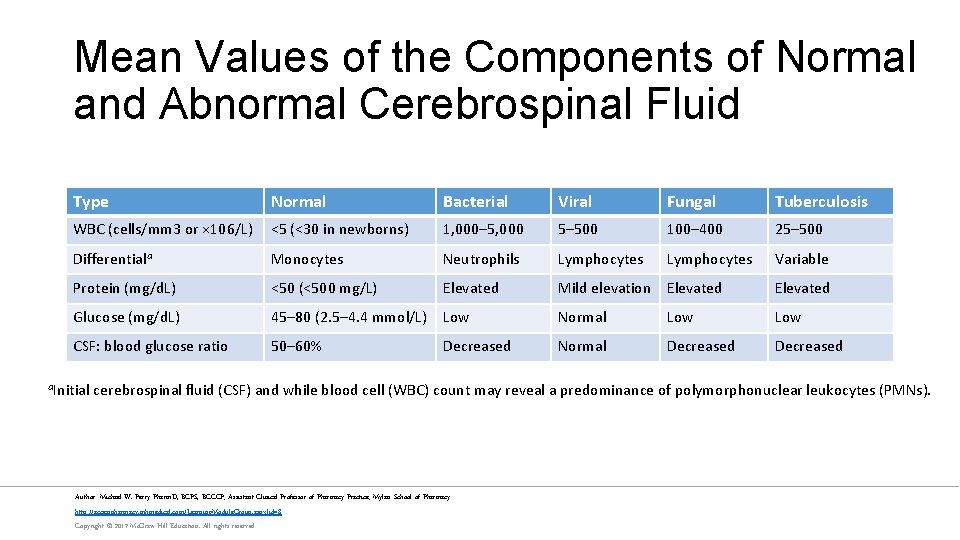
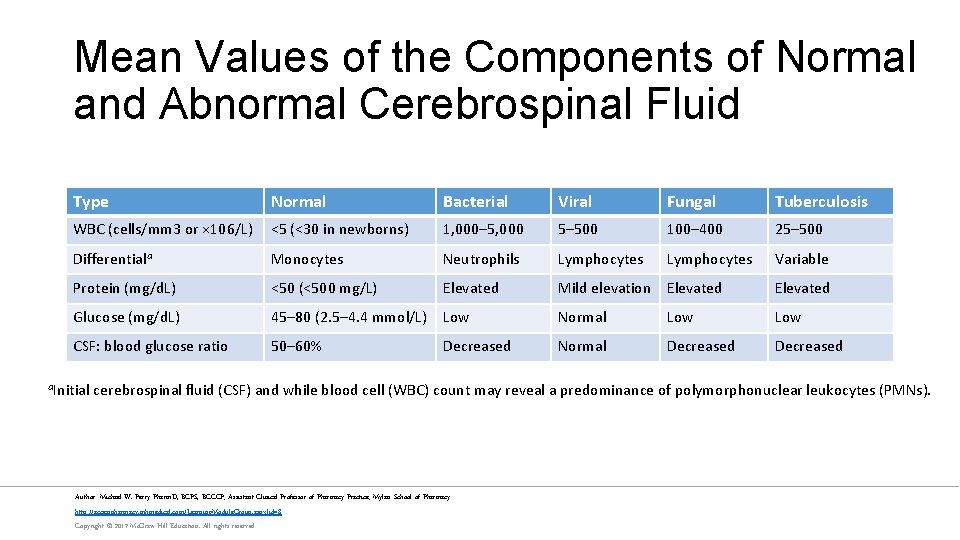
Mean Values of the Components of Normal and Abnormal Cerebrospinal Fluid Type Normal Bacterial Viral Fungal Tuberculosis WBC (cells/mm 3 or × 106/L) <5 (<30 in newborns) 1, 000– 5, 000 5– 500 100– 400 25– 500 Differentiala Monocytes Neutrophils Lymphocytes Variable Protein (mg/d. L) <50 (<500 mg/L) Elevated Mild elevation Elevated Glucose (mg/d. L) 45– 80 (2. 5– 4. 4 mmol/L) Low Normal Low CSF: blood glucose ratio 50– 60% Decreased Normal Decreased a. Initial cerebrospinal fluid (CSF) and while blood cell (WBC) count may reveal a predominance of polymorphonuclear leukocytes (PMNs). Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Goals of Therapy • Prevent Death • Prevent residual neurological deficits • Eradicate or control invading organism by starting appropriate antimicrobial therapy • Ameliorate clinical signs and symptoms • Provide supportive care • Prevent future infections through timely introduction of vaccination and chemoprophylaxis Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Nonpharmacological Treatment • Respiratory and Circulatory Support as needed Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
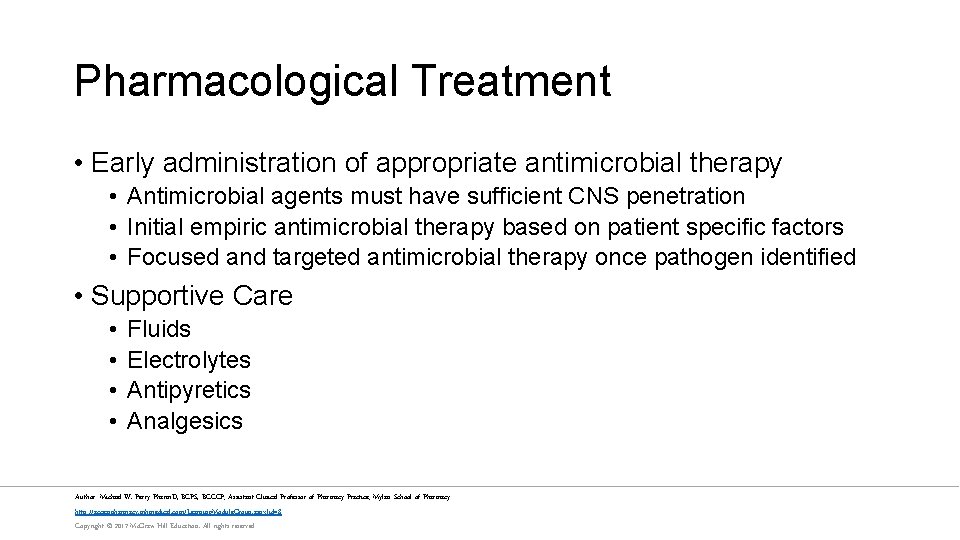
Pharmacological Treatment • Early administration of appropriate antimicrobial therapy • Antimicrobial agents must have sufficient CNS penetration • Initial empiric antimicrobial therapy based on patient specific factors • Focused and targeted antimicrobial therapy once pathogen identified • Supportive Care • • Fluids Electrolytes Antipyretics Analgesics Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
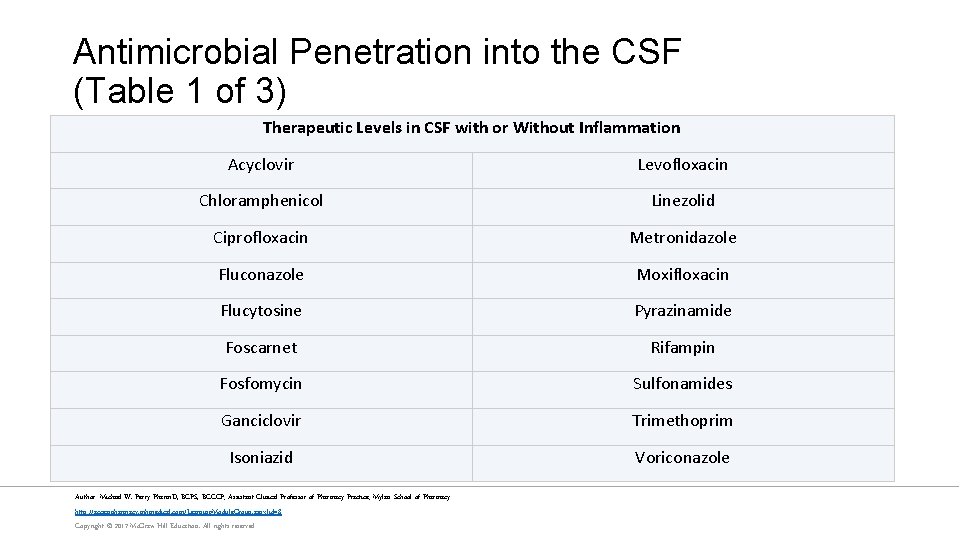
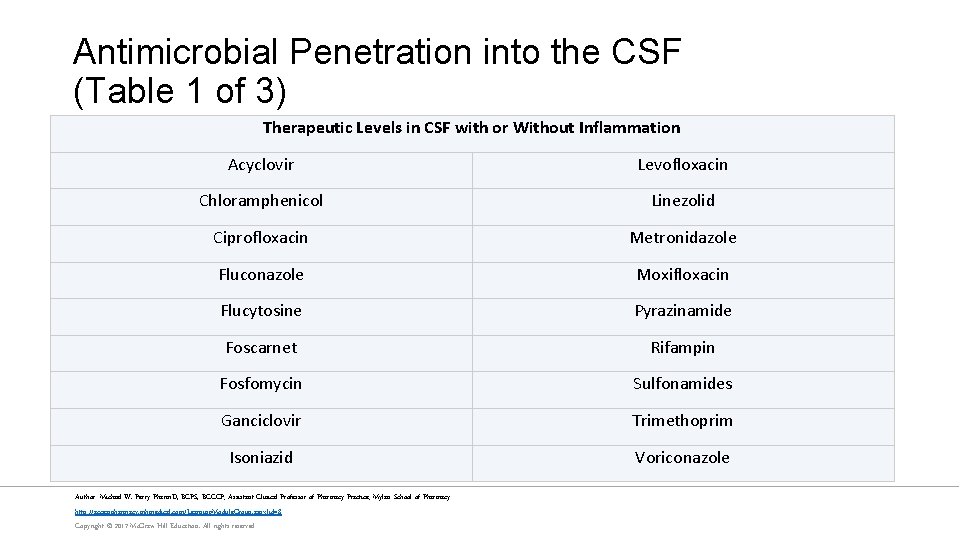
Antimicrobial Penetration into the CSF (Table 1 of 3) Therapeutic Levels in CSF with or Without Inflammation Acyclovir Levofloxacin Chloramphenicol Linezolid Ciprofloxacin Metronidazole Fluconazole Moxifloxacin Flucytosine Pyrazinamide Foscarnet Rifampin Fosfomycin Sulfonamides Ganciclovir Trimethoprim Isoniazid Voriconazole Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
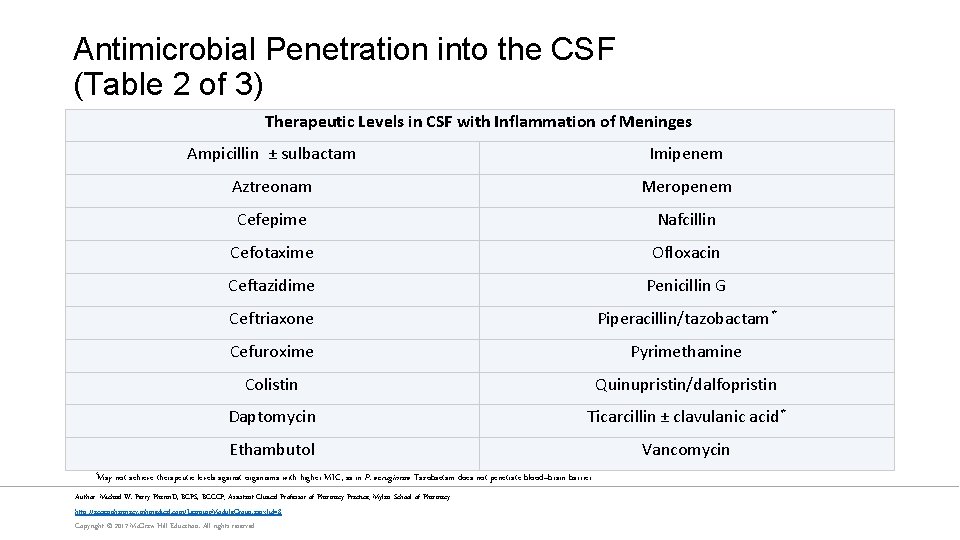
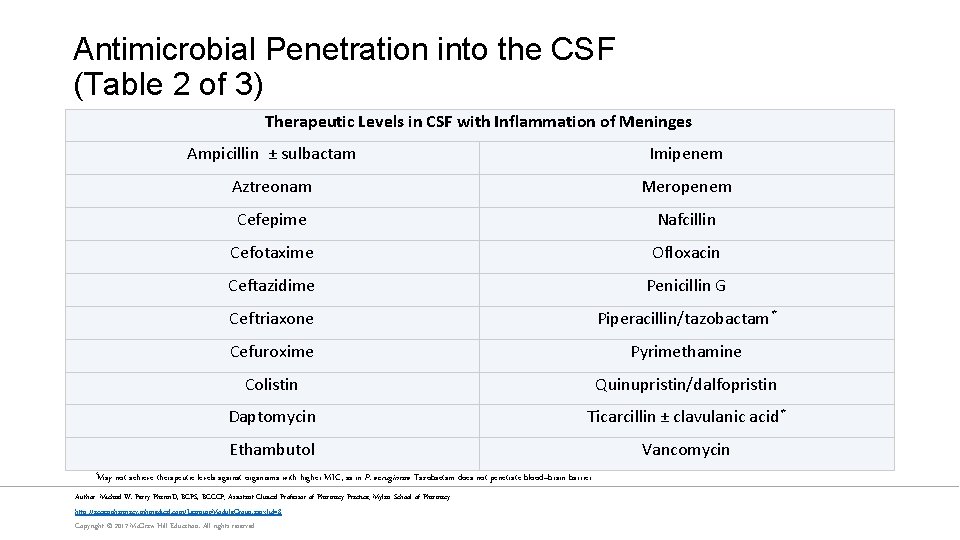
Antimicrobial Penetration into the CSF (Table 2 of 3) Therapeutic Levels in CSF with Inflammation of Meninges *May Ampicillin ± sulbactam Imipenem Aztreonam Meropenem Cefepime Nafcillin Cefotaxime Ofloxacin Ceftazidime Penicillin G Ceftriaxone Piperacillin/tazobactam* Cefuroxime Pyrimethamine Colistin Quinupristin/dalfopristin Daptomycin Ticarcillin ± clavulanic acid* Ethambutol Vancomycin not achieve therapeutic levels against organisms with higher MIC, as in P. aeruginosa. Tazobactam does not penetrate blood–brain barrier. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
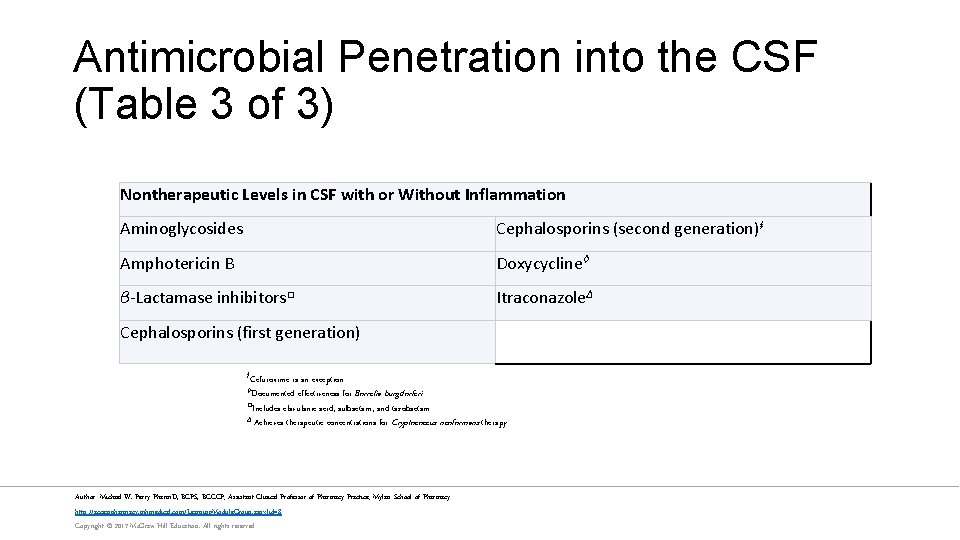
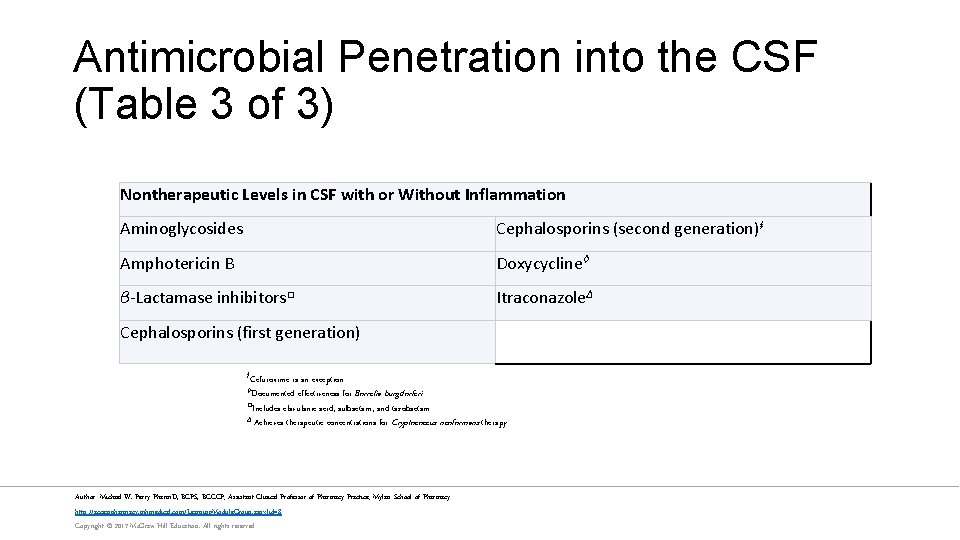
Antimicrobial Penetration into the CSF (Table 3 of 3) Nontherapeutic Levels in CSF with or Without Inflammation Aminoglycosides Cephalosporins (second generation)ⱡ Amphotericin B Doxycycline◊ β-Lactamase inhibitors□ Itraconazole∆ Cephalosporins (first generation) ⱡCefuroxime is an exception. effectiveness for Borrelia burgdorferi. □Includes clavulanic acid, sulbactam, and tazobactam. ∆ Achieves therapeutic concentrations for Cryptococcus neoformans therapy. ◊Documented Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
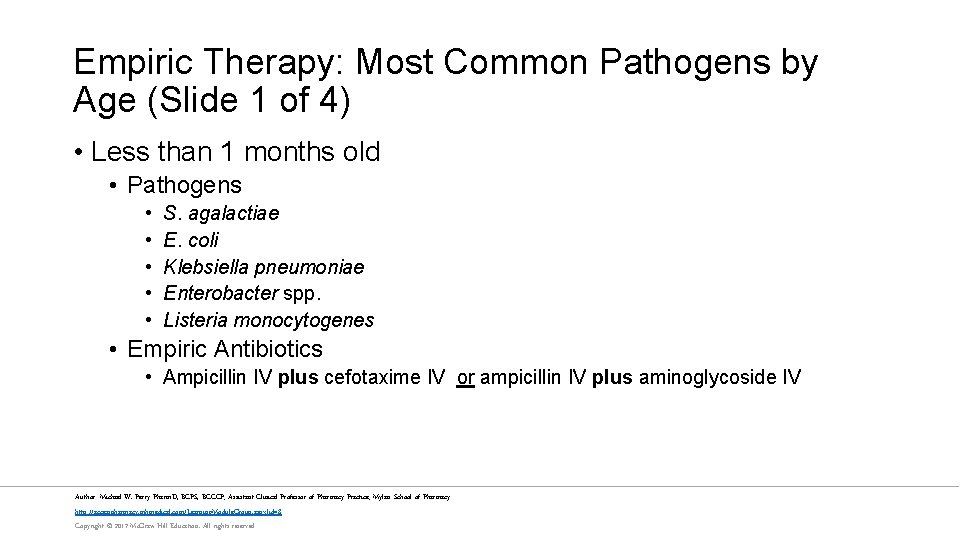
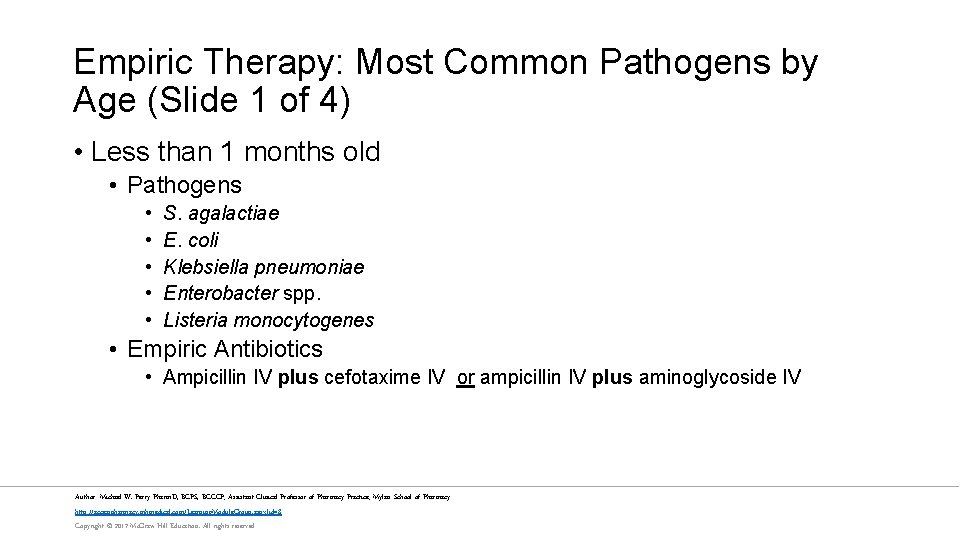
Empiric Therapy: Most Common Pathogens by Age (Slide 1 of 4) • Less than 1 months old • Pathogens • • • S. agalactiae E. coli Klebsiella pneumoniae Enterobacter spp. Listeria monocytogenes • Empiric Antibiotics • Ampicillin IV plus cefotaxime IV or ampicillin IV plus aminoglycoside IV Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
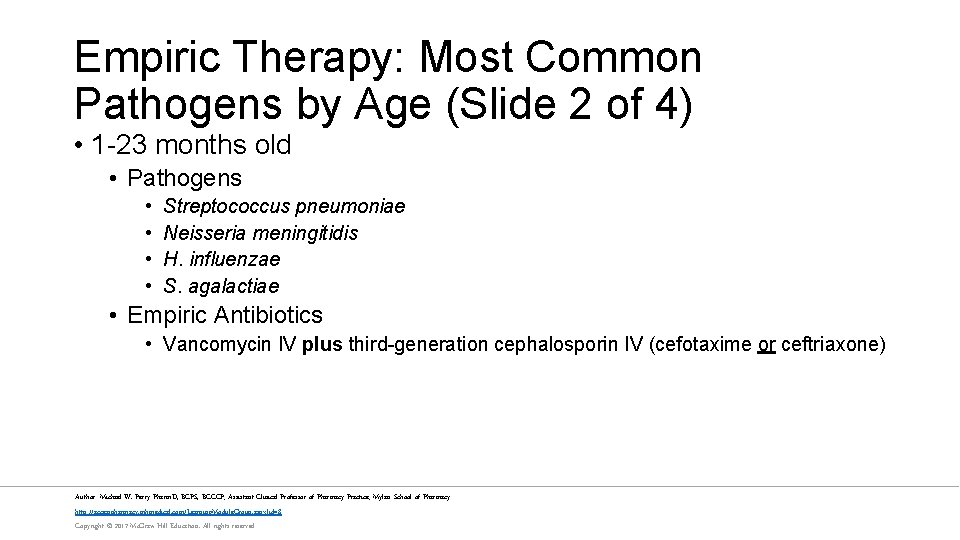
Empiric Therapy: Most Common Pathogens by Age (Slide 2 of 4) • 1 -23 months old • Pathogens • • Streptococcus pneumoniae Neisseria meningitidis H. influenzae S. agalactiae • Empiric Antibiotics • Vancomycin IV plus third-generation cephalosporin IV (cefotaxime or ceftriaxone) Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
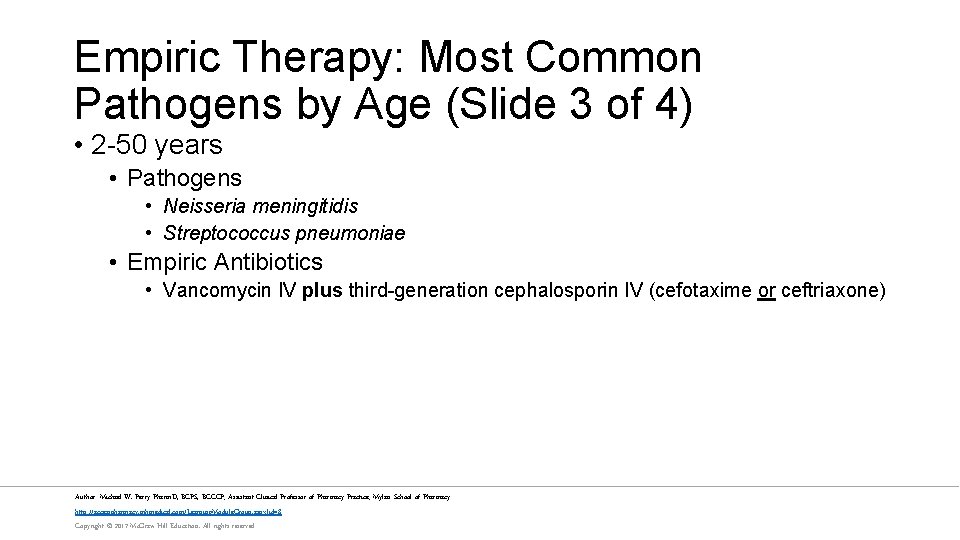
Empiric Therapy: Most Common Pathogens by Age (Slide 3 of 4) • 2 -50 years • Pathogens • Neisseria meningitidis • Streptococcus pneumoniae • Empiric Antibiotics • Vancomycin IV plus third-generation cephalosporin IV (cefotaxime or ceftriaxone) Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
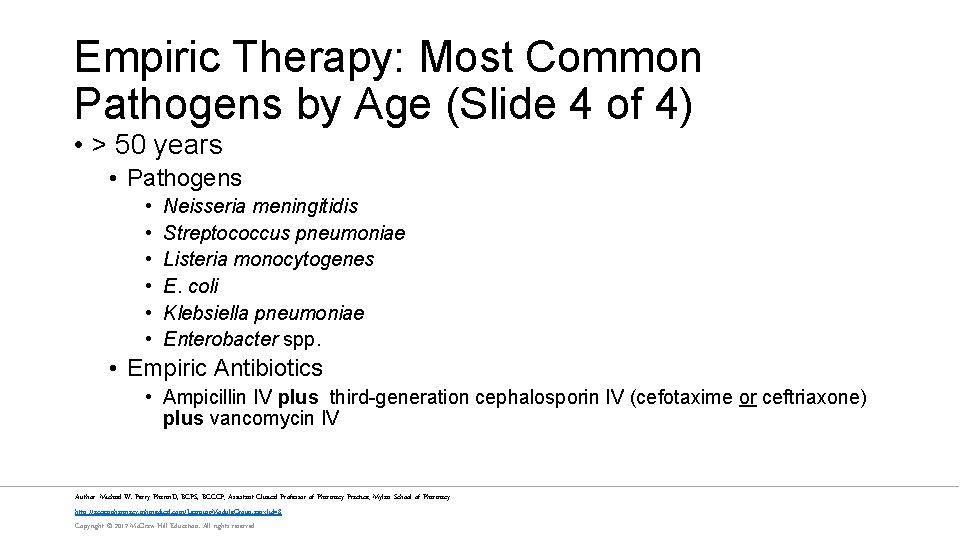
Empiric Therapy: Most Common Pathogens by Age (Slide 4 of 4) • > 50 years • Pathogens • • • Neisseria meningitidis Streptococcus pneumoniae Listeria monocytogenes E. coli Klebsiella pneumoniae Enterobacter spp. • Empiric Antibiotics • Ampicillin IV plus third-generation cephalosporin IV (cefotaxime or ceftriaxone) plus vancomycin IV Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
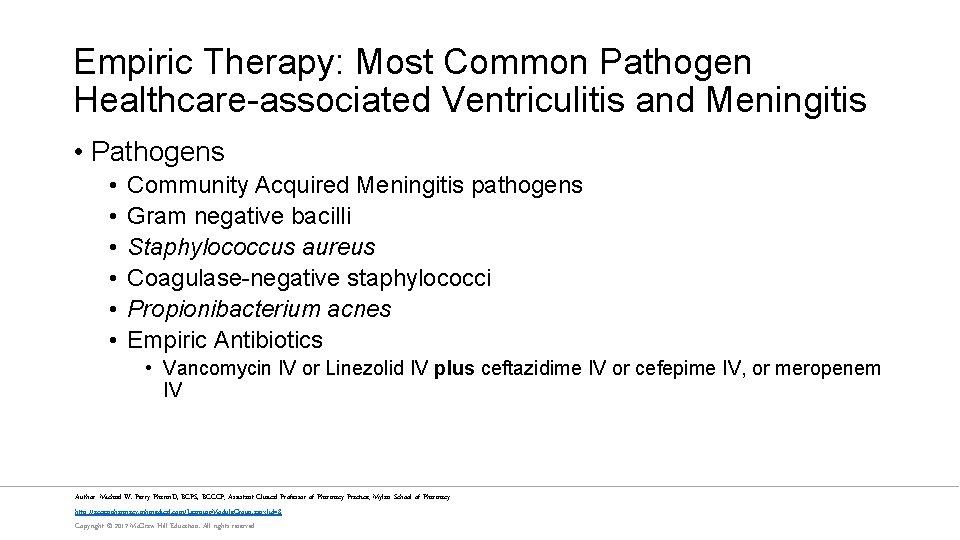
Empiric Therapy: Most Common Pathogen Healthcare-associated Ventriculitis and Meningitis • Pathogens • • • Community Acquired Meningitis pathogens Gram negative bacilli Staphylococcus aureus Coagulase-negative staphylococci Propionibacterium acnes Empiric Antibiotics • Vancomycin IV or Linezolid IV plus ceftazidime IV or cefepime IV, or meropenem IV Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
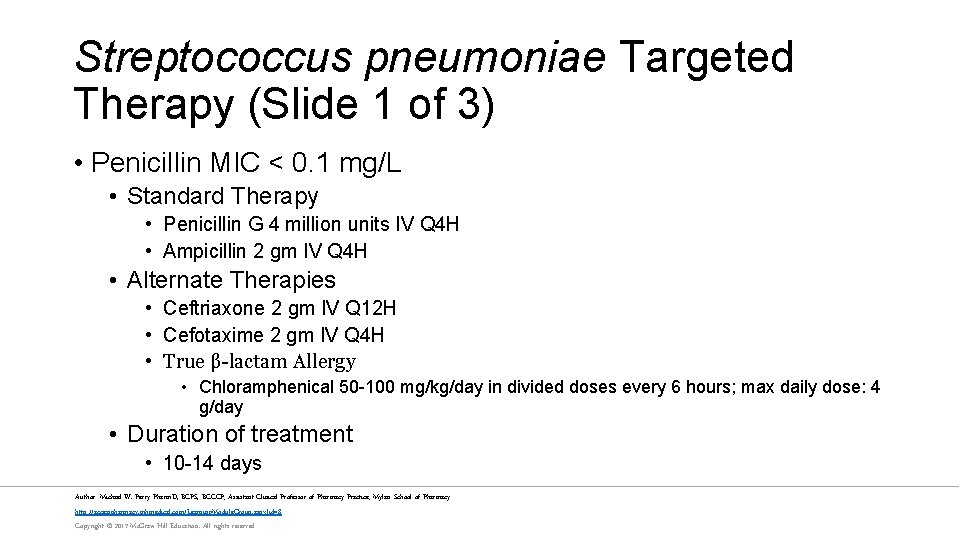
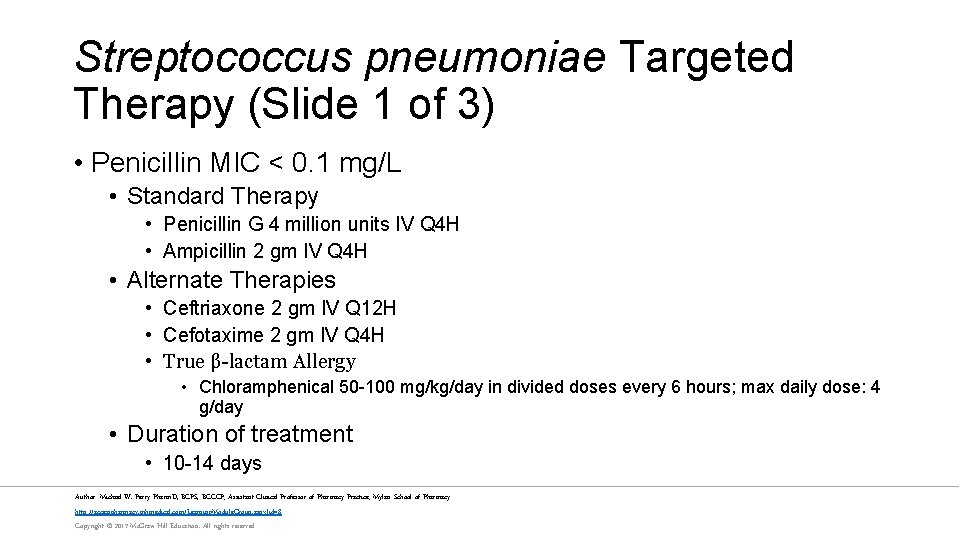
Streptococcus pneumoniae Targeted Therapy (Slide 1 of 3) • Penicillin MIC < 0. 1 mg/L • Standard Therapy • Penicillin G 4 million units IV Q 4 H • Ampicillin 2 gm IV Q 4 H • Alternate Therapies • Ceftriaxone 2 gm IV Q 12 H • Cefotaxime 2 gm IV Q 4 H • True β-lactam Allergy • Chloramphenical 50 -100 mg/kg/day in divided doses every 6 hours; max daily dose: 4 g/day • Duration of treatment • 10 -14 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
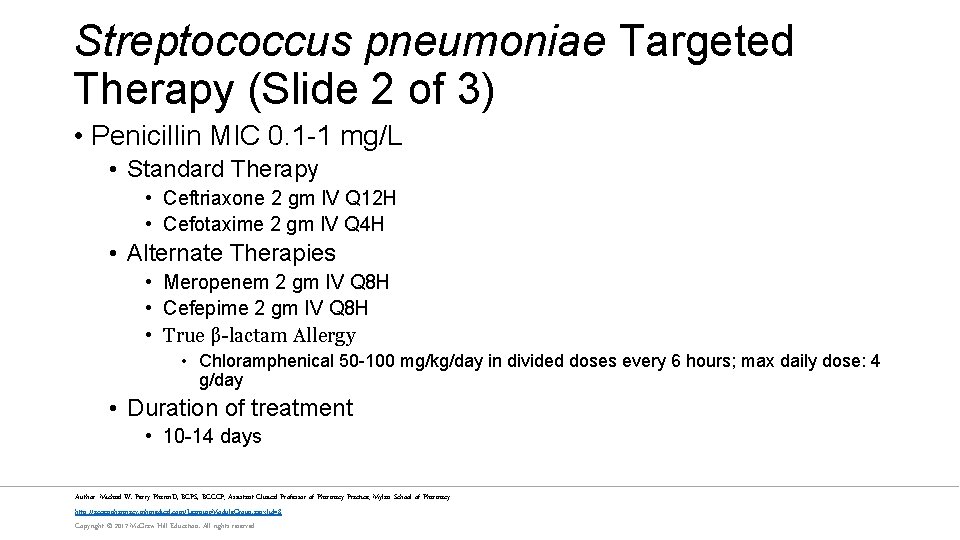
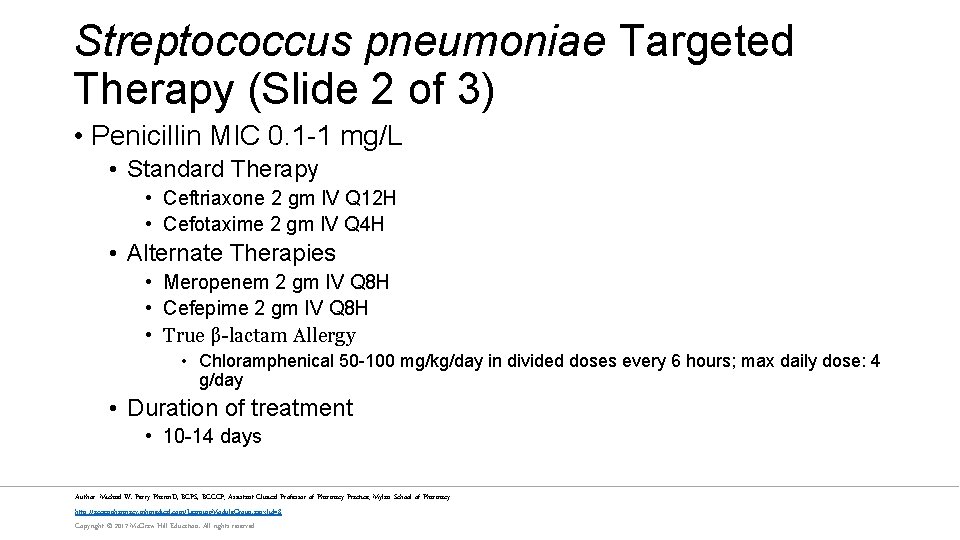
Streptococcus pneumoniae Targeted Therapy (Slide 2 of 3) • Penicillin MIC 0. 1 -1 mg/L • Standard Therapy • Ceftriaxone 2 gm IV Q 12 H • Cefotaxime 2 gm IV Q 4 H • Alternate Therapies • Meropenem 2 gm IV Q 8 H • Cefepime 2 gm IV Q 8 H • True β-lactam Allergy • Chloramphenical 50 -100 mg/kg/day in divided doses every 6 hours; max daily dose: 4 g/day • Duration of treatment • 10 -14 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
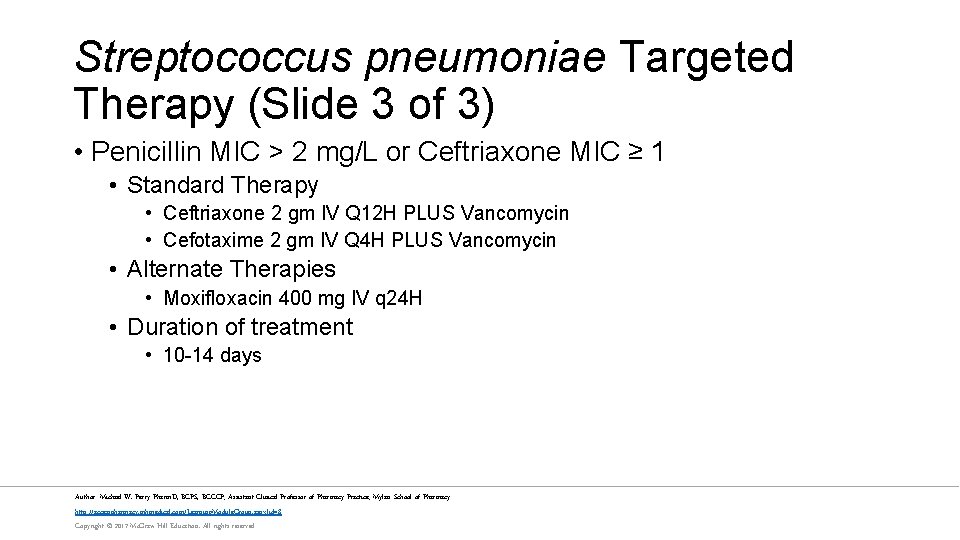
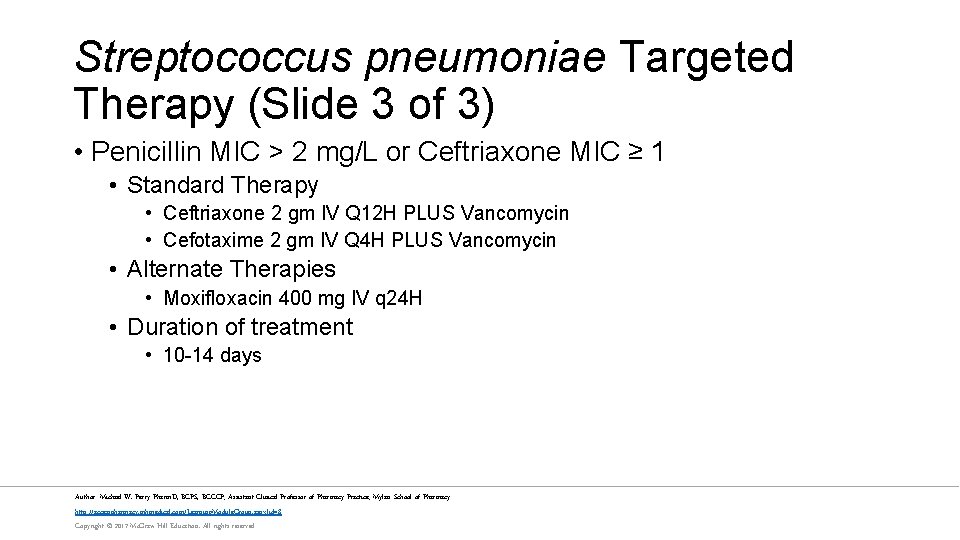
Streptococcus pneumoniae Targeted Therapy (Slide 3 of 3) • Penicillin MIC > 2 mg/L or Ceftriaxone MIC ≥ 1 • Standard Therapy • Ceftriaxone 2 gm IV Q 12 H PLUS Vancomycin • Cefotaxime 2 gm IV Q 4 H PLUS Vancomycin • Alternate Therapies • Moxifloxacin 400 mg IV q 24 H • Duration of treatment • 10 -14 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
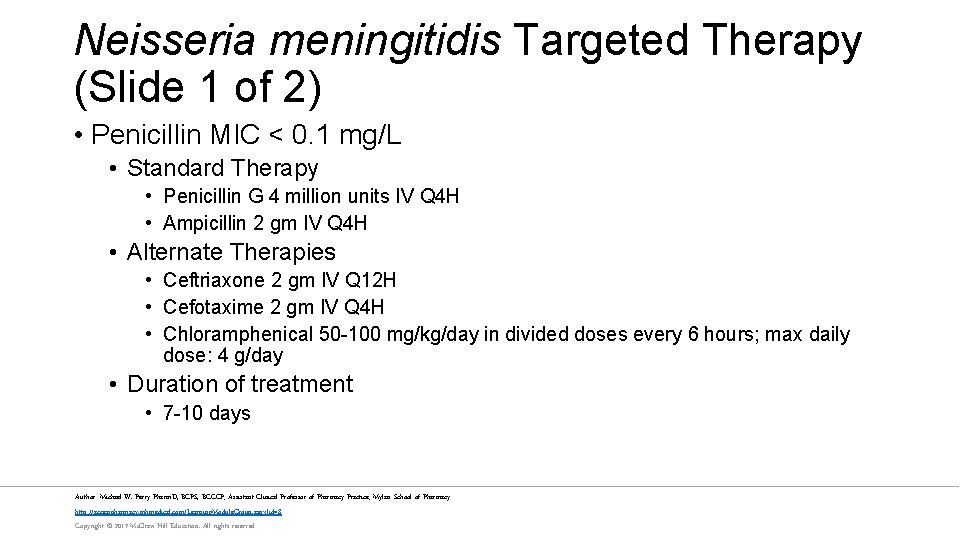
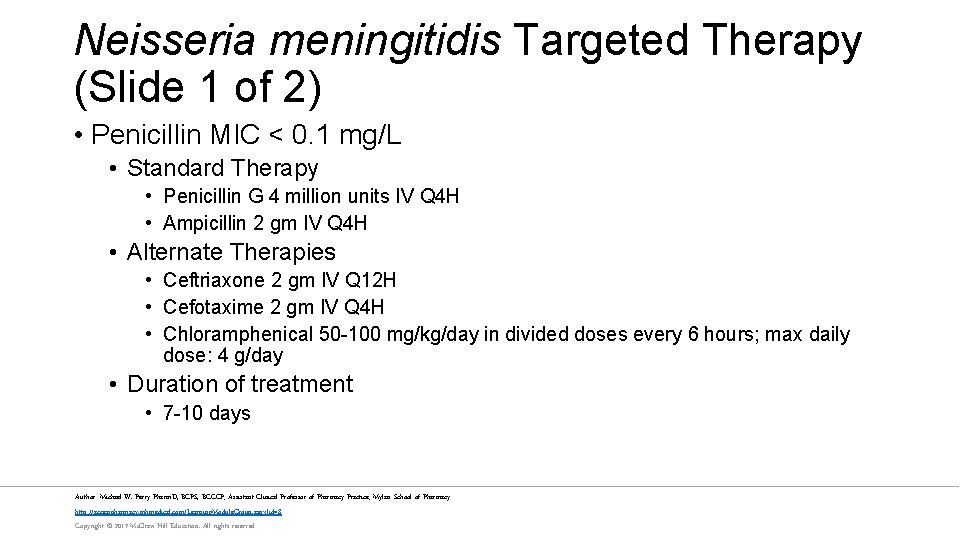
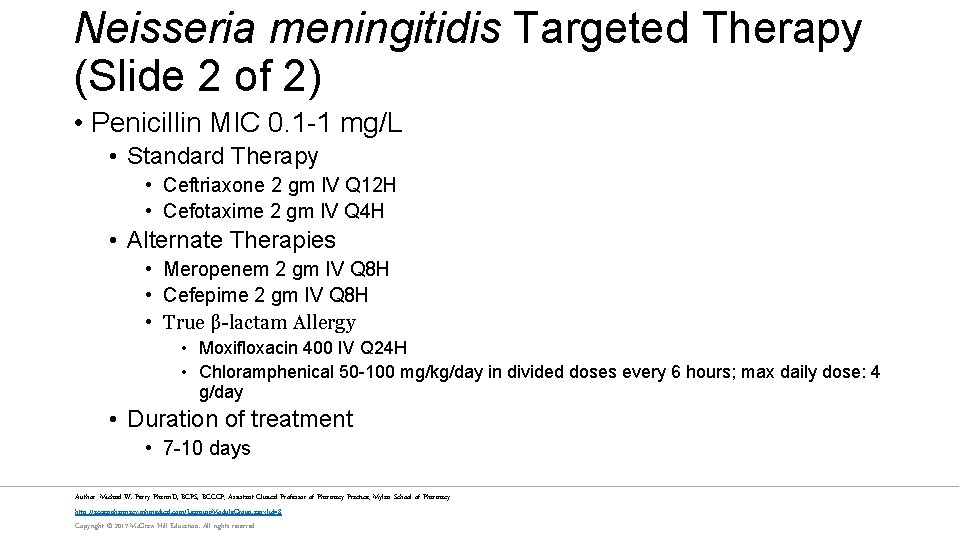
Neisseria meningitidis Targeted Therapy (Slide 1 of 2) • Penicillin MIC < 0. 1 mg/L • Standard Therapy • Penicillin G 4 million units IV Q 4 H • Ampicillin 2 gm IV Q 4 H • Alternate Therapies • Ceftriaxone 2 gm IV Q 12 H • Cefotaxime 2 gm IV Q 4 H • Chloramphenical 50 -100 mg/kg/day in divided doses every 6 hours; max daily dose: 4 g/day • Duration of treatment • 7 -10 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
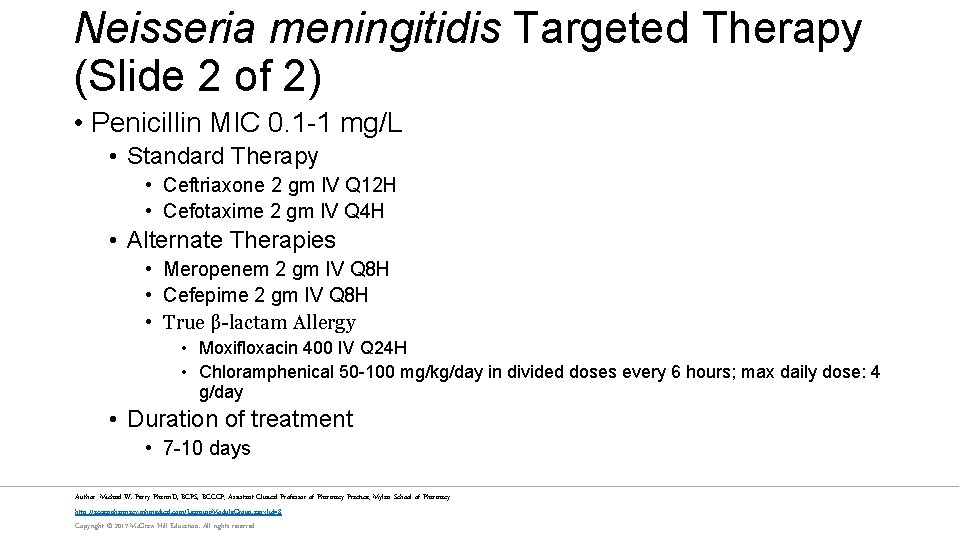
Neisseria meningitidis Targeted Therapy (Slide 2 of 2) • Penicillin MIC 0. 1 -1 mg/L • Standard Therapy • Ceftriaxone 2 gm IV Q 12 H • Cefotaxime 2 gm IV Q 4 H • Alternate Therapies • Meropenem 2 gm IV Q 8 H • Cefepime 2 gm IV Q 8 H • True β-lactam Allergy • Moxifloxacin 400 IV Q 24 H • Chloramphenical 50 -100 mg/kg/day in divided doses every 6 hours; max daily dose: 4 g/day • Duration of treatment • 7 -10 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
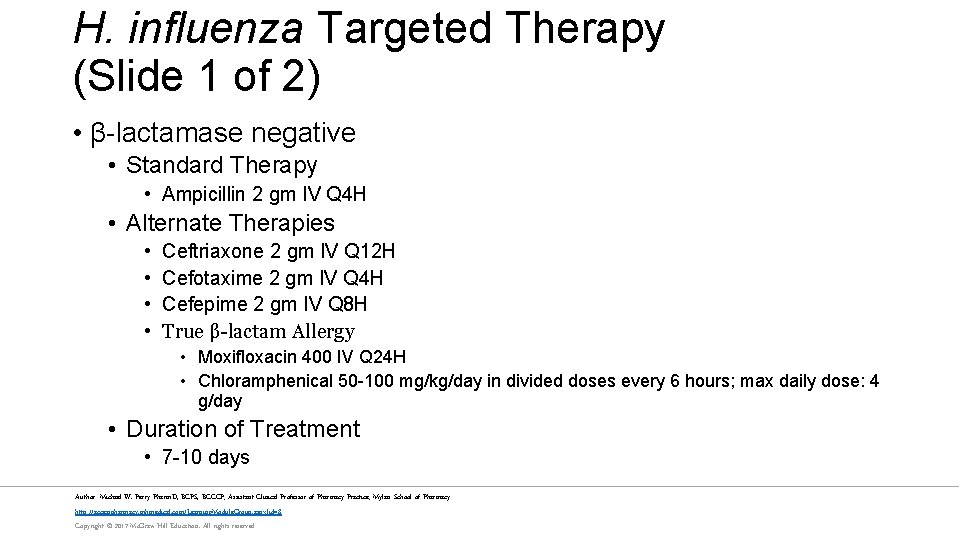
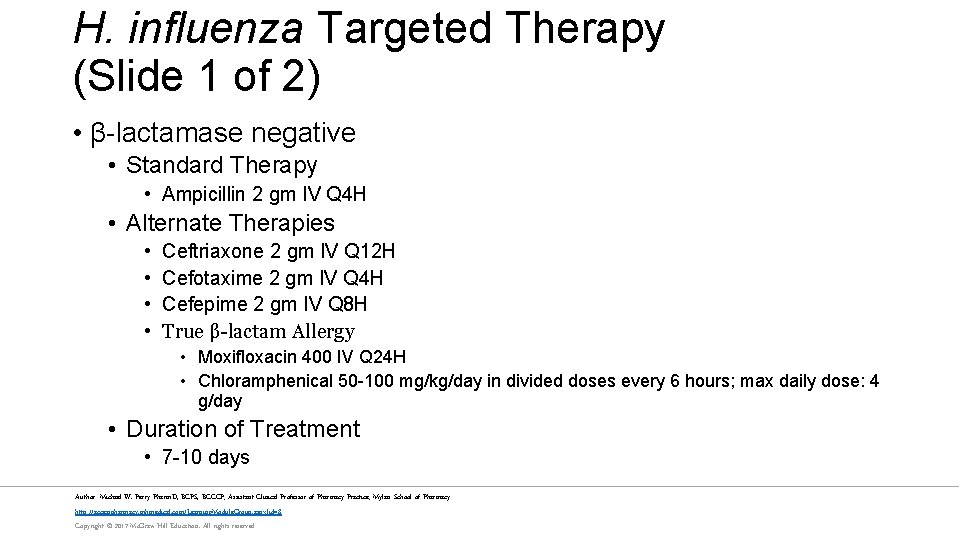
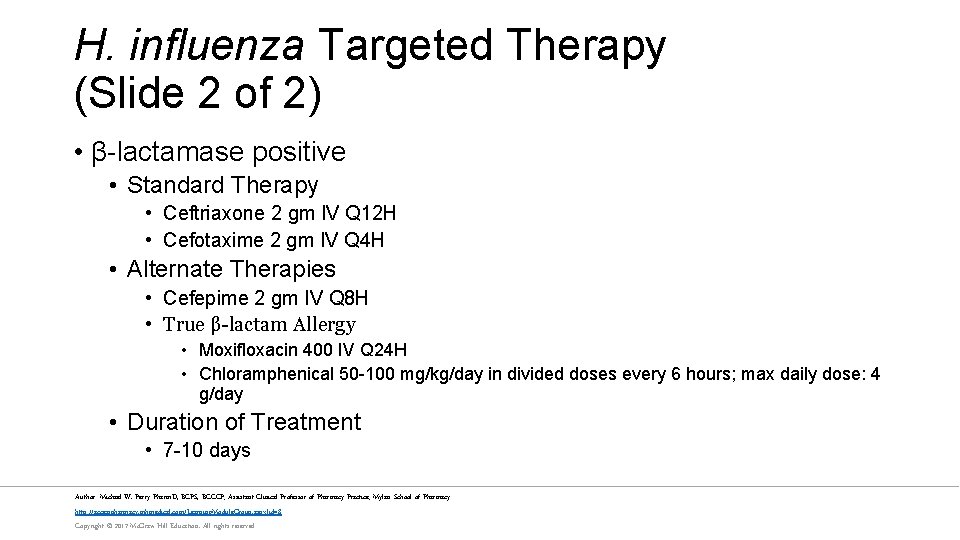
H. influenza Targeted Therapy (Slide 1 of 2) • β-lactamase negative • Standard Therapy • Ampicillin 2 gm IV Q 4 H • Alternate Therapies • • Ceftriaxone 2 gm IV Q 12 H Cefotaxime 2 gm IV Q 4 H Cefepime 2 gm IV Q 8 H True β-lactam Allergy • Moxifloxacin 400 IV Q 24 H • Chloramphenical 50 -100 mg/kg/day in divided doses every 6 hours; max daily dose: 4 g/day • Duration of Treatment • 7 -10 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
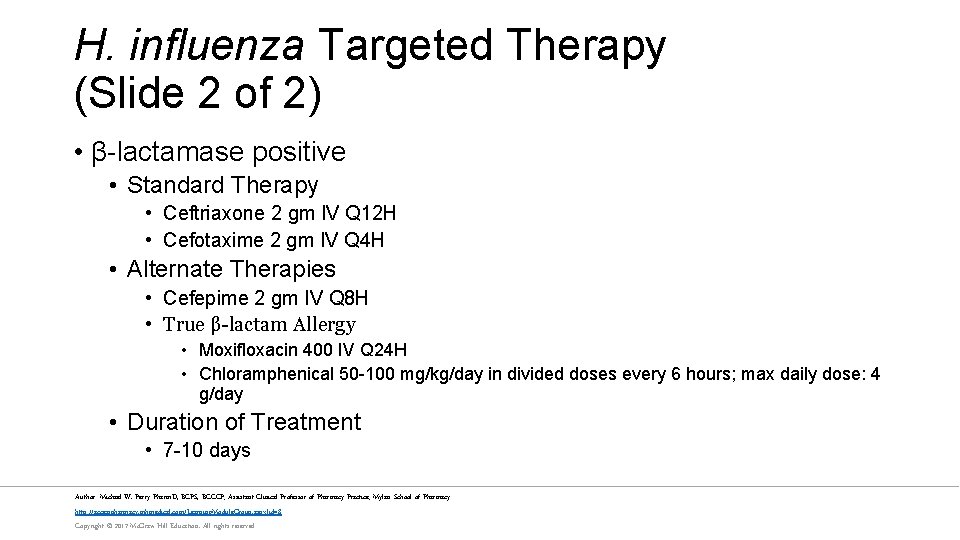
H. influenza Targeted Therapy (Slide 2 of 2) • β-lactamase positive • Standard Therapy • Ceftriaxone 2 gm IV Q 12 H • Cefotaxime 2 gm IV Q 4 H • Alternate Therapies • Cefepime 2 gm IV Q 8 H • True β-lactam Allergy • Moxifloxacin 400 IV Q 24 H • Chloramphenical 50 -100 mg/kg/day in divided doses every 6 hours; max daily dose: 4 g/day • Duration of Treatment • 7 -10 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
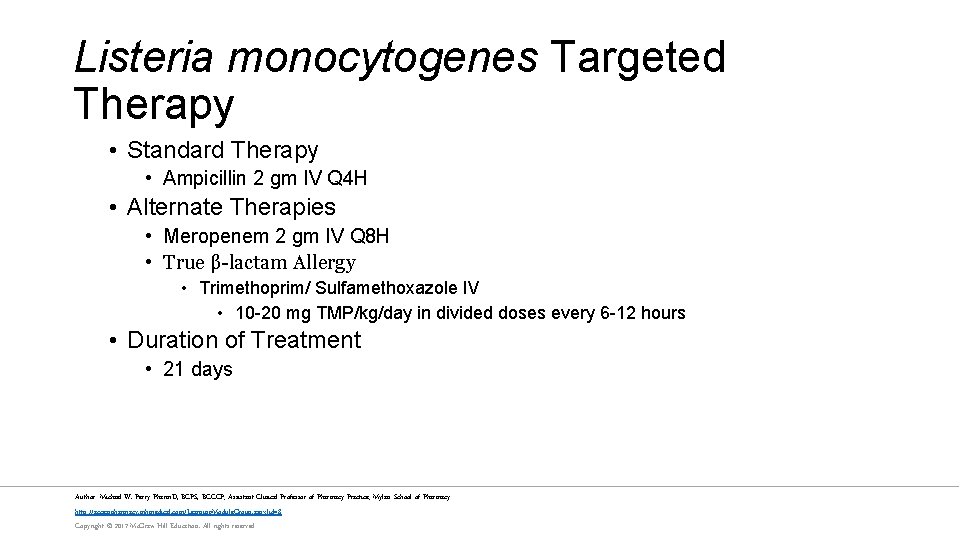
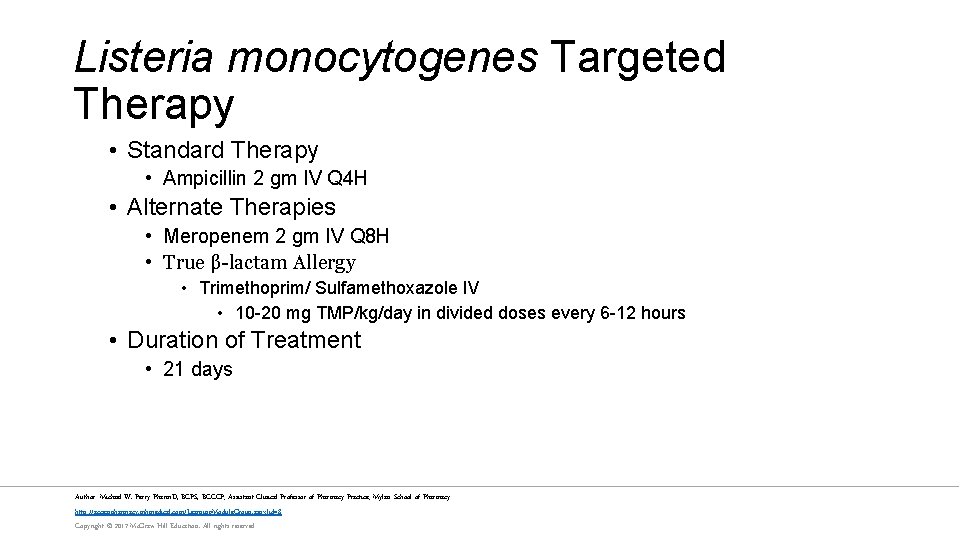
Listeria monocytogenes Targeted Therapy • Standard Therapy • Ampicillin 2 gm IV Q 4 H • Alternate Therapies • Meropenem 2 gm IV Q 8 H • True β-lactam Allergy • Trimethoprim/ Sulfamethoxazole IV • 10 -20 mg TMP/kg/day in divided doses every 6 -12 hours • Duration of Treatment • 21 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
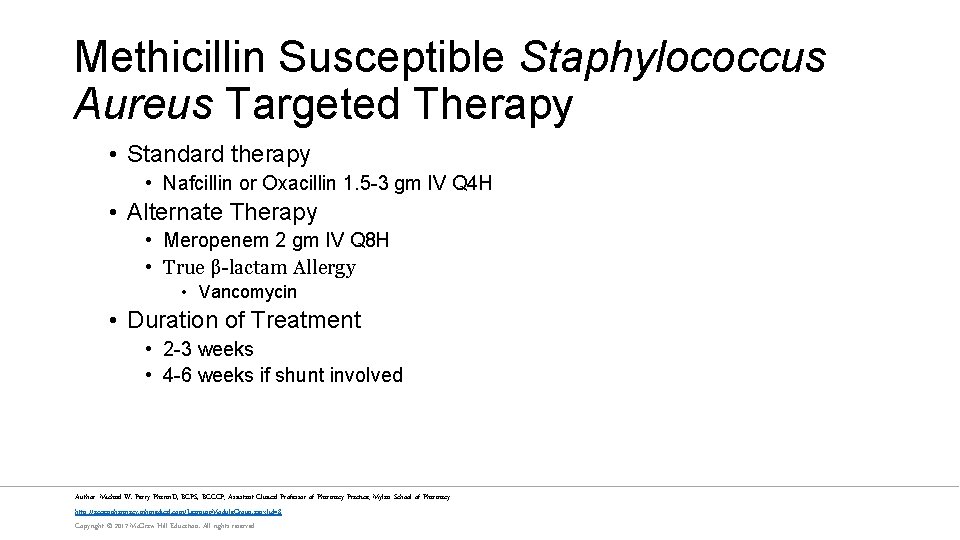
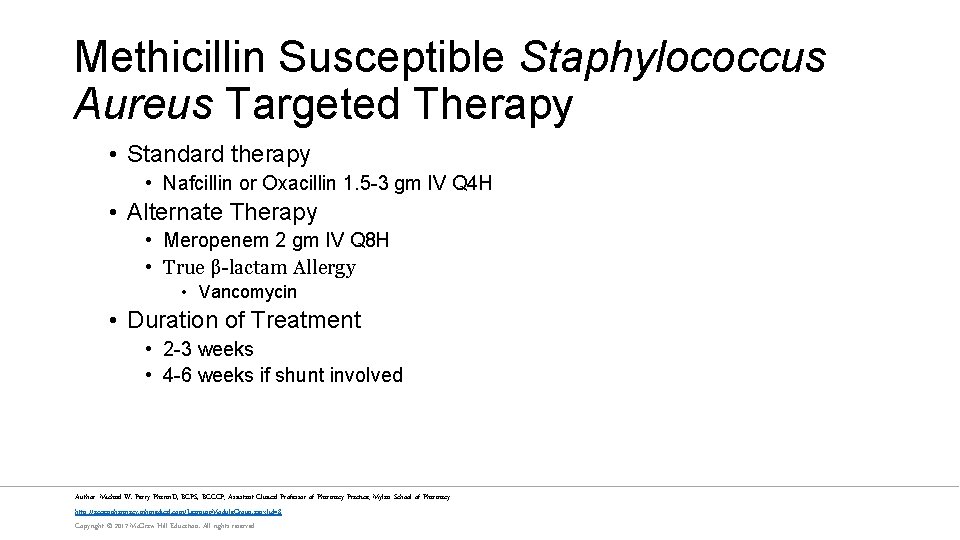
Methicillin Susceptible Staphylococcus Aureus Targeted Therapy • Standard therapy • Nafcillin or Oxacillin 1. 5 -3 gm IV Q 4 H • Alternate Therapy • Meropenem 2 gm IV Q 8 H • True β-lactam Allergy • Vancomycin • Duration of Treatment • 2 -3 weeks • 4 -6 weeks if shunt involved Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
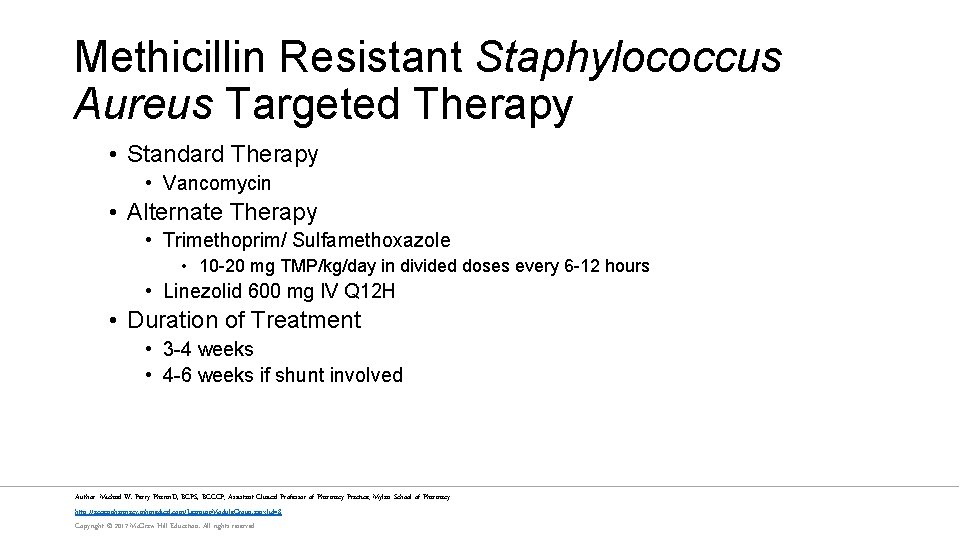
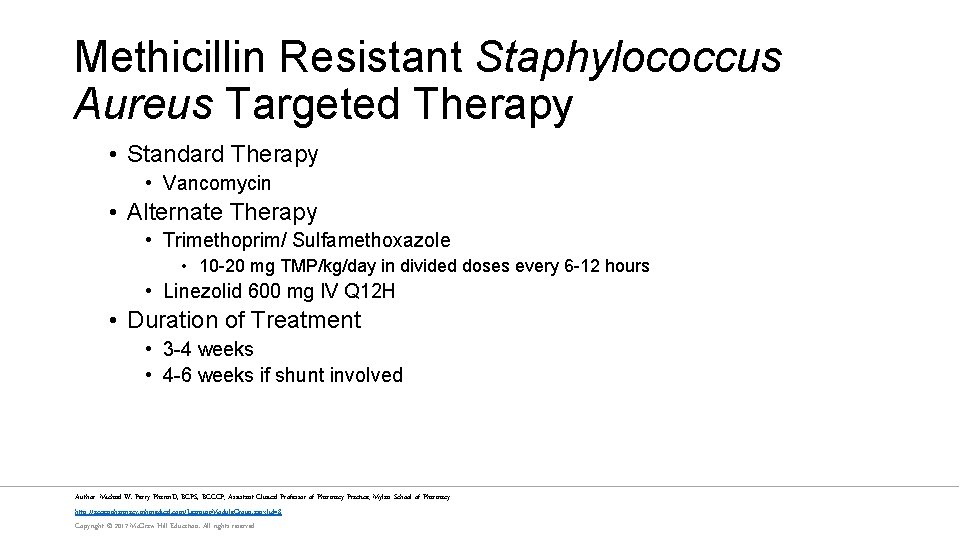
Methicillin Resistant Staphylococcus Aureus Targeted Therapy • Standard Therapy • Vancomycin • Alternate Therapy • Trimethoprim/ Sulfamethoxazole • 10 -20 mg TMP/kg/day in divided doses every 6 -12 hours • Linezolid 600 mg IV Q 12 H • Duration of Treatment • 3 -4 weeks • 4 -6 weeks if shunt involved Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
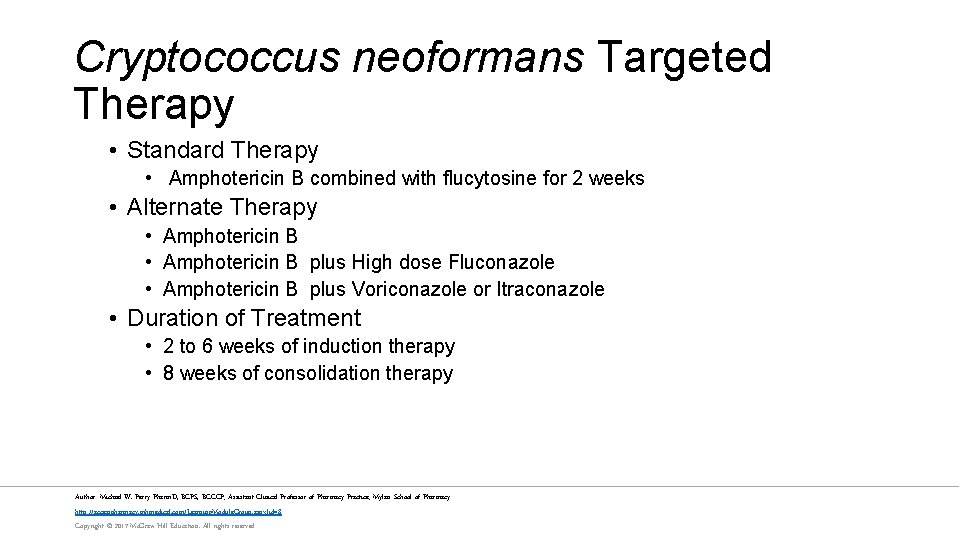
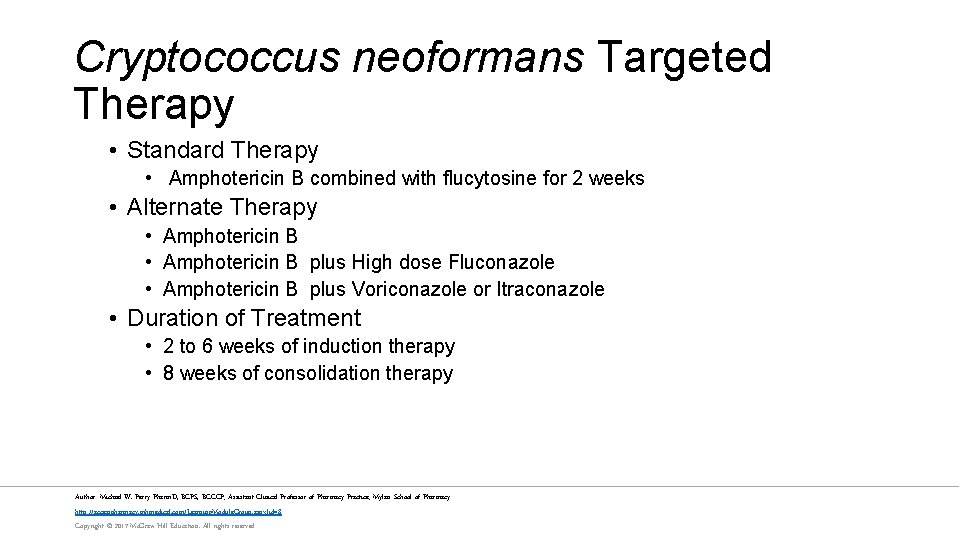
Cryptococcus neoformans Targeted Therapy • Standard Therapy • Amphotericin B combined with flucytosine for 2 weeks • Alternate Therapy • Amphotericin B plus High dose Fluconazole • Amphotericin B plus Voriconazole or Itraconazole • Duration of Treatment • 2 to 6 weeks of induction therapy • 8 weeks of consolidation therapy Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
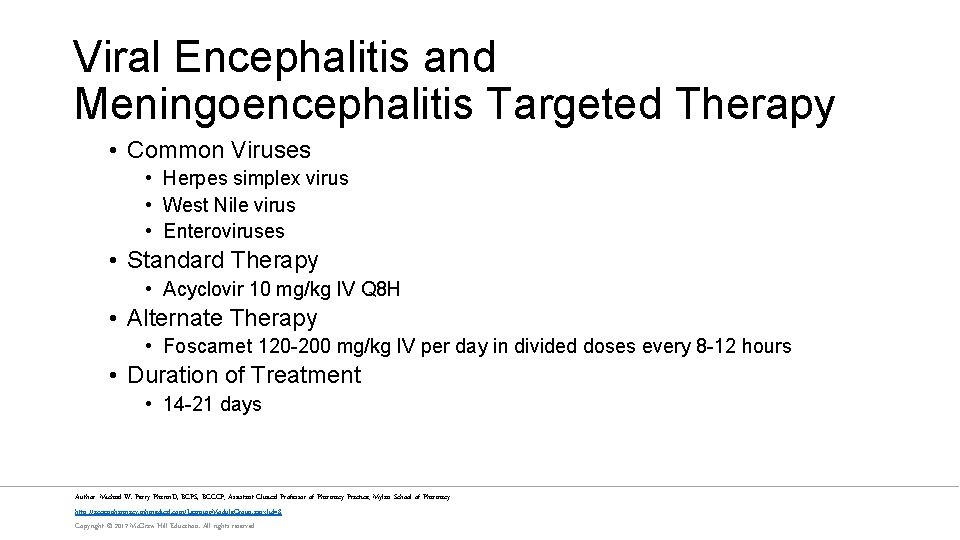
Viral Encephalitis and Meningoencephalitis Targeted Therapy • Common Viruses • Herpes simplex virus • West Nile virus • Enteroviruses • Standard Therapy • Acyclovir 10 mg/kg IV Q 8 H • Alternate Therapy • Foscarnet 120 -200 mg/kg IV per day in divided doses every 8 -12 hours • Duration of Treatment • 14 -21 days Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Dexamethasone • Corticosteroids inhibit the production of pro-inflammatory cytokines • Clinical trial data surrounding the benefits of corticosteroids in meningitis is conflicting • A series trials and systematic review showed steroids may improve neurological and mortality outcomes in adult patients • A larger trial showed conflicting data • Various antimicrobial agents were used • Dexamethasone was administered at different times in relation to the first antimicrobial dose • Patients had varying levels of illness severity • Overall use of corticosteroids in the setting of meningitis is controversial Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Dexamethasone Recommendations • Infants and children • H. influenza: Dexamethasone 0. 15 mg/kg Q 6 H for 2 -4 days • Administer before or concurrently with the first dose of antibiotics • Pneumococcal: not routinely recommended must weigh risk versus benefit • Adults • Pneumococcal: Dexamethasone 10 mg IV Q 6 H for 2 -4 days • Administer before or concurrently with the first dose of antibiotics • Other bacterial causes of meningitis: not routinely recommended Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Evaluation of Outcomes • Monitor the following every 4 hours for 3 days • • • Fever Headache Meningismus Vital signs Acute changes in Mental Status/ Glasgow Coma Scale • Adjust antimicrobial therapy based on microbiologic findings Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Prophylactic Antibiotics (Slide 1 of 2) • Prophylaxis of close contacts should be started only after consultation with the local health department • Close Contacts • • Members of same household Individuals who share the same sleeping quarters Day care contacts Individuals exposed to oral secretions of infected patient Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved

Prophylactic Antibiotics (Slide 2 of 2) • Neisseria meningitidis • Close contacts • • Rifampin 600 mg PO BID x 2 days Ciprofloxacin 500 mg PO x 1 dose Ceftriaxone 250 mg IM x 1 dose Azithromycin 500 mg PO x 1 dose • H. influenza • Close Contacts • Rifampin 600 mg PO BID x 4 days • Fully vaccinated children do not require prophylactic antibiotics Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Vaccination • Neisseria meningitidis • Meningococcal Polysaccharide Vaccine (Groups A / C / Y and W-135) • Meningococcal (Groups A / C / Y and W-135) Diphtheria Conjugate Vaccine • Meningococcal Group B vaccine • Streptococcus pneumoniae • Pneumococcal Conjugate Vaccines • 7 -valent • 13 -valent • Pneumococcal Polysaccharide Vaccine • 23 -valent • H. influenza • Hib Conjugate vaccine Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Summary • Meningitis is an infection of the central nervous system with high rates of morbidity and mortality • Early identification of meningitis and early initiations of antibiotics is key to improve outcomes • High doses of antimicrobials that penetrate the CNS are required • Adjust therapy as soon as cultures finalized • Prevention with vaccination and prophylactic antibiotics Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
References • Elshaboury RH, Hermsen ED, Holt JS, Mitropoulos IF, Rotschafer JC. Chapter 84. Central Nervous System Infections In: Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 9 e. New York, NY: Mc. Graw-Hill; 2014. • Tunkel AR, Hartman BJ, Kaplan SL, et. al. . 2004. Practice guidelines for the management of bacterial meningitis. Clin. Infect. Dis. 39: 1267 -1284. • Tunkel AR, Hasbun R, Bhimraj A, et. al. . 2017 Infectious Diseases Society of America’s Clinical Practice Guidelines for Healthcare. Associated Ventriculitis and Meningitis. Clin Infect Dis 2017; 64 (6): e 34 -e 65. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
 Infectious disease quality controls
Infectious disease quality controls Stages of infection
Stages of infection Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Stages of infectious disease
Stages of infectious disease Infectious disease board review
Infectious disease board review Infectious disease
Infectious disease Hennepin county infectious disease manual
Hennepin county infectious disease manual What is the smallest infectious disease agent
What is the smallest infectious disease agent Identify each type of neuronal pool
Identify each type of neuronal pool Sensory input and motor output
Sensory input and motor output Neuronal processes
Neuronal processes Nervous system major divisions
Nervous system major divisions Central nervous system amusement park
Central nervous system amusement park Nervous system brain
Nervous system brain Nervous system vocabulary
Nervous system vocabulary Hydras
Hydras Bser aer
Bser aer Neuroglia
Neuroglia Central nervous system for kids
Central nervous system for kids Communicable disease and non communicable disease
Communicable disease and non communicable disease Nervous system and digestive system
Nervous system and digestive system Endocrine system and nervous system
Endocrine system and nervous system Amino acid-based hormones
Amino acid-based hormones Endocrine system and nervous system
Endocrine system and nervous system Opportunistic infections
Opportunistic infections Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Opportunistic infections
Opportunistic infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Infections opportunistes digestives
Infections opportunistes digestives Eye infections
Eye infections Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Amber blumling
Amber blumling Opsonization
Opsonization Acute gingival infections
Acute gingival infections Central nervous sysytem
Central nervous sysytem Infectious waste meaning
Infectious waste meaning Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Icd 10 morbus hansen
Icd 10 morbus hansen Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs