Infectious Disease I Overview of Infectious Diseases Courses
- Slides: 40
Infectious Disease I: Overview of Infectious Diseases Courses in Therapeutics and Disease State Management Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 1 of 3) • Recognize general signs, symptoms, laboratory, and microbiologic findings of a patient with an infection • Apply susceptibility data from an institution’s antibiogram in choosing presumptive antimicrobial therapy • Select antimicrobial(s) of choice based on organism and infectious disease • Design an appropriate antimicrobial regimen for a patient-based allergy profile, age, renal and liver function, concomitant disease states, and infection Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 2 of 3) • Propose alternative antimicrobial therapy for a patient with a penicillin allergy • Discuss metabolic and host genetic variations that may affect antimicrobial therapy • Explain key pharmacodynamic relationships to optimize antimicrobial dosing • Recommend antimicrobial agents based on tissue or fluid penetration and site of infection Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Learning Objectives (Slide 3 of 3) • Debate advantages and disadvantages of using combination antimicrobial therapy • Formulate a monitoring plan to assess therapeutic response after initiation of antimicrobial therapy • Evaluate issues including drug selection, host factors, and pathogen(s) in a patient lacking clinical response to antimicrobial therapy • List clinical parameters to consider when switching from parenteral to oral therapy. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Required and Recommended Reading Required Reading Lee GC, Burgess DS. Chapter 83. Antimicrobial Regimen Selection. In: Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 9 e. ` New York, NY: Mc. Graw-Hill; 2014. Recommended Readings • Lampiris HW, Maddix DS. Clinical Use of Antimicrobial Agents. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13 e. New York, NY: Mc. Graw-Hill; 2015. • Rybak MJ, Aeschlimann JR, La. Plante KL. e. Chapter 25. Laboratory Tests to Direct Antimicrobial Pharmacotherapy. In: Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 9 e. New York, NY: Mc. Graw-Hill; 2014. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Antimicrobial Agents (Slide 1 of 4) • Infectious diseases generally are acute, and a delay in antimicrobial therapy can result in serious morbidity or even mortality • Antimicrobial therapy must be initiated swiftly and appropriately in order to prevent serious complications from infectious process and the antimicrobial therapy itself Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Antimicrobial Agents (Slide 2 of 4) Consider the following three patients: • Patient # 1: A 35 -year-old female presents to the emergency room with complaints of fever, cough, and increased green sputum production. She has decreased lung sounds at the bases of his lungs. She does not have a significant past medical history. She has received a 3 -day course of levofloxacin for a urinary tract infection three weeks ago. A complete blood count with differential reveals an elevated white blood cell count of 11, 000 cells/mm 3 • Patient # 2: A 45 -year-old male presents to the emergency room with complaints of fever, cough, increased green sputum production. He has decreased lung sounds at the bases of his lungs. He has a past medical history significant for HTN, hypothyroid, and atrial fibrillation. He has not had any antibiotics in the past 6 months. A complete blood count with differential reveals an elevated white blood cell count of 14, 000 cells/mm 3 • Patient # 3: 62 -year-old male presents to the emergency room with complaints of fever, cough, increased sputum production. He has decreased lung sounds at the bases of his lungs. He has a past medical history of COPD, Diabetes, and HTN. He has not had any antibiotics in the past year. A complete blood count with differential reveals an elevated white blood cell count of 12, 000 cells/mm 3 Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Antimicrobial Agents (Slide 3 of 4) • Confirm the presence of infection • Monitor therapeutic response • Careful history and physical examination • Clinical assessment • Signs and symptoms • Laboratory tests • Predisposing factors • Assessment of therapeutic failure • Identification of the pathogen (see Chap. e 24) • Collection of infected material • Stains • Serologies • Culture and sensitivity • Selection of presumptive therapy considering every infected site • Host factors • Drug factors Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Antimicrobial Agents (Slide 4 of 4) Drawbacks to not following a systematic process include: • Unnecessary use of broad-spectrum antimicrobial therapy that leads to widespread resistance and difficult-to-treat superinfections • Overuse of more expensive or potentially more toxic antimicrobial agents • Administration of antimicrobial agents to patients with infectious processes that are self-limiting (e. g. colds or viral gastritis) Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Confirming the Presence of Infection Signs and Symptoms: Fever • Average normal body temperatures by site are defined as • Oral: 36. 7°C (98°F)- 37°C (98. 6°F) • Rectal: 37. 3°C (99°F)- 37. 6°C (99. 6°F) • Axillary: 36. 1°C (97°F)- 36. 4°C (97. 6°F) • Regulation of body temperature is a complex process, controlled by the hypothalamus, that follows a circadian rhythm • An elevation in temperature above the generally acceptable ranges is considered a hallmark of an infectious process • Clinicians should be aware that there are many non-infectious origins for fever • Medications can prevent a fever in patients with an infectious process Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Confirming the Presence of Infection Signs and Symptoms: White Blood Cell Count • Normal White Blood Cell (WBC) Count range: 4, 000 - 10, 000 cells/mm 3 (4 × 109 -10 × 109/L) • Infections will normally result in a leukocytosis (elevated WBC count) due to an increased production and mobilization of granulocytes and lymphocytes • Patients may have an infection without a leukocytosis • Patients may have a leukocytosis without an infection Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Confirming the Presence of Infection Signs and Symptoms: Local Signs • Pain and inflammation • Swelling • Erythema • Tenderness • Purulent Drainage • Examination of tissues and fluids • Organ specific symptoms Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Confirming the Presence of Infection Signs and Symptoms: Review • All three of the patients in the previous example are presenting with fever as a non-specific symptom of an infection • Each of the patients has an elevated white blood cell count • Patient # 1: 11, 000 cells/mm 3 • Patient # 2: 14, 000 cells/mm 3 • Patient # 3: 12, 000 cells/mm 3 • The following signs and symptoms are more organ specific to respiratory infections • Cough • Increased mucous production • Decreased lung sounds Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Identification of the Pathogen Laboratory Tests: Gram’s Stain • • One of the initial tests completed on a specimen Differentiates between gram-positive and gram-negative organisms Describes the morphology of organisms The Gram’s stain and morphology characteristics of the isolated organisms can be used to categorize stained the organisms into groups • Routinely performed on • • • Sputum Cerebral spinal fluid Blood Bronchial aspirates Urine Mucosal Scrapings Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Identification of the Pathogen Laboratory Tests: Evaluation and Direction Link: Figure on Laboratory Tests to Direct Antimicrobial Pharmacotherapy Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Identification of the Pathogen Laboratory Tests: Culture • Identification of the infecting pathogen by culture is the most definitive method available for the diagnosis and treatment of infection • Samples of fluid or tissues collected from an infected patient will be used to inoculate several types of artificial growth media to identify the causative pathogen • Routinely performed on • • Blood Sputum Bronchial aspirates Urine Cerebral spinal fluid Stool Joint fluid Wound or sinus drainage Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Identification of the Pathogen Laboratory Tests: Other Tests • Rapid Diagnostic Technologies • Can have results within 15 minutes to 4 hours • Genomic testing methodologies • Immunologic Assays • Rapid Strep Test • Rapid Influenza diagnostic test • Enzyme-linked immunosorbent assay (ELISA) tests • Hybridization DNA Probes • Peptide nucleic acid fluorescence in situ hybridization (PNA-FISH) assay • Branched DNA (b. DNA) probe system • Nucleic Acid Amplification Methods • polymerase chain reaction (PCR) • Rapid PCR (r. PCR) • Mass spectrometry Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
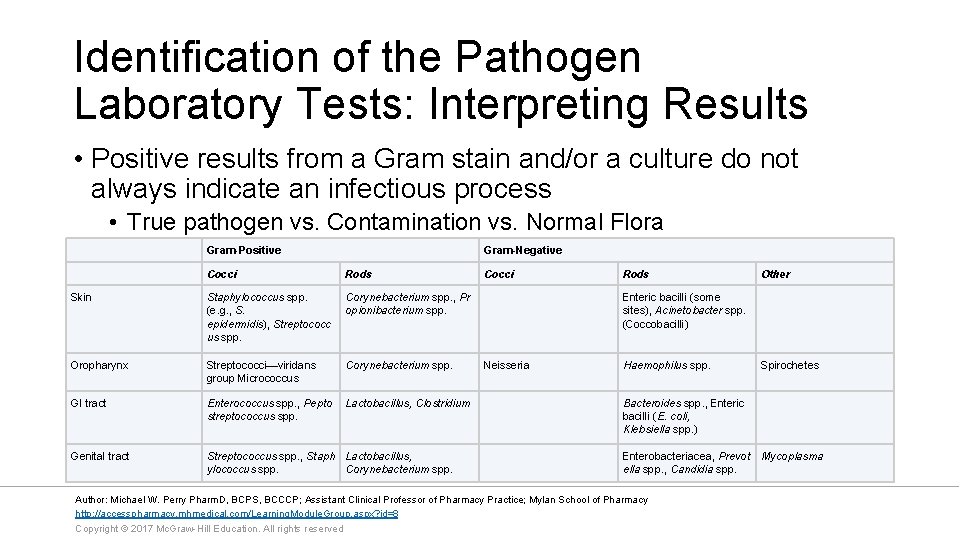
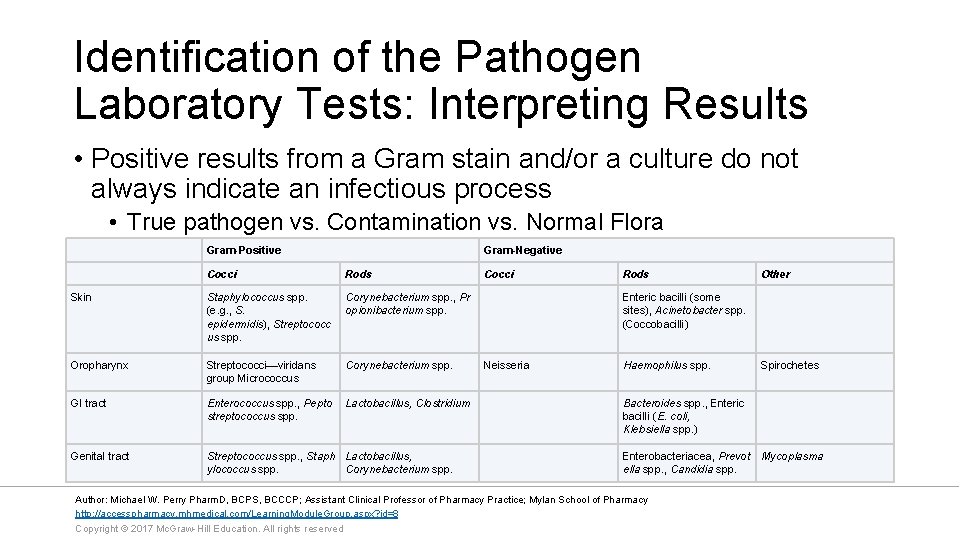
Identification of the Pathogen Laboratory Tests: Interpreting Results • Positive results from a Gram stain and/or a culture do not always indicate an infectious process • True pathogen vs. Contamination vs. Normal Flora Gram-Positive Gram-Negative Cocci Rods Skin Staphylococcus spp. (e. g. , S. epidermidis), Streptococc us spp. Corynebacterium spp. , Pr opionibacterium spp. Oropharynx Streptococci—viridans group Micrococcus Corynebacterium spp. GI tract Enterococcus spp. , Pepto streptococcus spp. Lactobacillus, Clostridium Genital tract Streptococcus spp. , Staph Lactobacillus, ylococcus spp. Corynebacterium spp. Cocci Rods Other Enteric bacilli (some sites), Acinetobacter spp. (Coccobacilli) Neisseria Haemophilus spp. Spirochetes Bacteroides spp. , Enteric bacilli (E. coli, Klebsiella spp. ) Enterobacteriacea, Prevot ella spp. , Candidia spp. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved Mycoplasma
Identification of the Pathogen Laboratory Tests: Patient Examples • Link: Algorithm on Laboratory Tests to Direct Antimicrobial Pharmacotherapy • Sputum gram stain results for the patients were as follows: • Patient #1: Gram negative coccobacilli • Patient #2: Gram positive cocci arranged in pairs • Patient #3: No organism identified Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy: Introduction • After identifying the signs and symptoms of infection and attempting to identify a pathogen, empirical antimicrobial therapy may be initiated depending on • • Disease severity and acuity Patient specific factors Medication related issues Need for multiple antimicrobial agents • Empiric antimicrobial therapy is directed at organisms that are known to cause the infection • Generally accepted drugs of first choice for specific infections are based on several factors • Infection Specific Guidelines • Local antimicrobial susceptibility data via antibiograms Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy: Patient Factors (Slide 1 of 3) • Allergy • Careful assessment of listed medication allergies and reactions must be completed • An “allergy” to a medication with a reaction of nausea is not an allergy • Penicillin allergies are common • Serious reactions (anaphylaxis, laryngospasm, throat swelling) may prevent use of penicillin related compounds • Patients with less serious reactions (rash) may be able to take penicillin related compounds under close supervision • Age • Certain infections are cause by different pathogens based on the patient’s age • Meningitis • Osteomyelitis • Certain medications cannot be processed appropriately in neonates due to underdeveloped hepatic and liver function • Renal function declines with age, which would cause decreased drug clearance in older patients Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy: Patient Factors (Slide 2 of 3) • Pregnancy • Risk of harm to the fetus with teratogenic medications • Altered pharmacokinetics in pregnant patients • Increased intravascular volume • Increased glomerular filtration • Higher hepatic clearance of medication • Metabolic or Genetic Variation • Depending on the genetic variation could lead to increased or decreased drug metabolism • Certain medications require screening for specific genetic variation prior to administration Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy: Patient Factors (Slide 3 of 3) • Organ Dysfunction • Decreases in the renal and/or hepatic function of a patient can lead to accumulation of medications • Medication specific recommendation should be followed when organ dysfunction is present • Concomitant Drugs/ Disease States • Any antimicrobial agent should be screened against a patient’s past medical history and current medication list for drug disease and drug interactions, respectively • Certain disease states will predispose a patient to specific infections and/or pathogens Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy Drug Factors: Pharmacokinetic and Pharmacodynamic Considerations • Pharmacokinetics is used to describe how a medication is processed by the body • Area under the curve (AUC) • Maximum observed concentration (peak) • Half life (t 1/2) • Pharmacodynamics describes the relationship between drug concentration and the effects on the microorganism • AUC: Minimal inhibitory concentration (MIC) ratio (AUC: MIC ratio) • Peak: MIC ratio • Time (T) the concentration is above the MIC (T>MIC) • Utilizing these tools has altered the methods employed to dose and administer medications Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy: Drug Factors • Tissue Penetration • Antimicrobial therapy must be able to get to the site of infection and be active once there • Serious infections are generally treated using intravenous antimicrobial therapy • Outpatient treatment of less serious infectious diseases can be managed using oral medications • Drug Toxicity • Toxicities should be avoided at all costs • Certain medications will require a risk vs. benefit analysis prior to starting therapy Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy: Antimicrobial Regimen Selection Link: Table on Antimicrobial Regimen Selection Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy: Combination Antimicrobial Therapy • Broadening the Spectrum of Coverage • Required for infections caused by multiple pathogens • Required for patients with two concurrent infections with different pathogens • Synergism • Controversial data exists with the use of two antimicrobial agents with differing mechanism of action against a pathogen • Endocarditis is often treated with a combination of an antimicrobial agent that targets the cell wall with an aminoglycoside. • Preventing Resistance • Combining antimicrobials may decrease the development of bacterial resistance • Frequently utilized in the treatment of tuberculosis Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Selection of Presumptive Therapy: Disadvantages of Combination Therapy • Increased Cost • Greater risk of drug toxicity • Superinfection Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
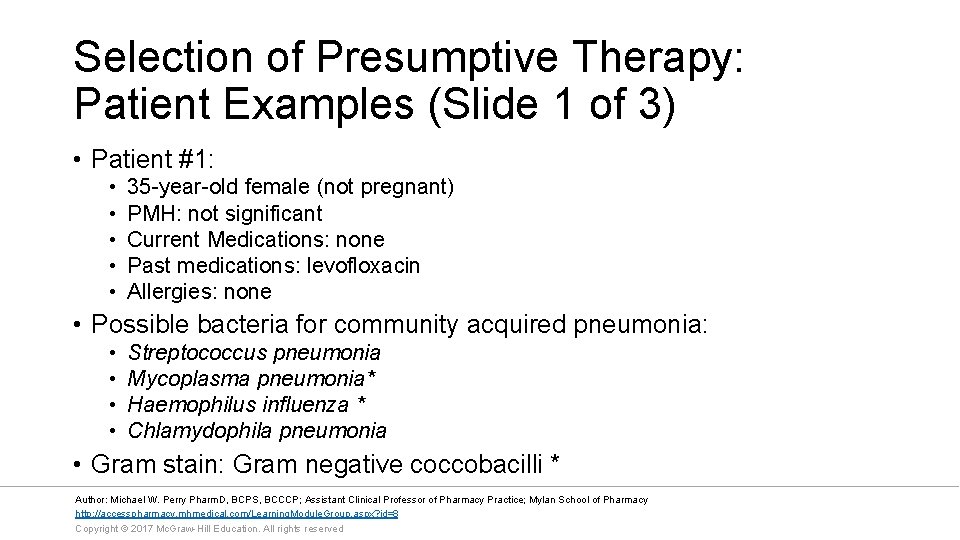
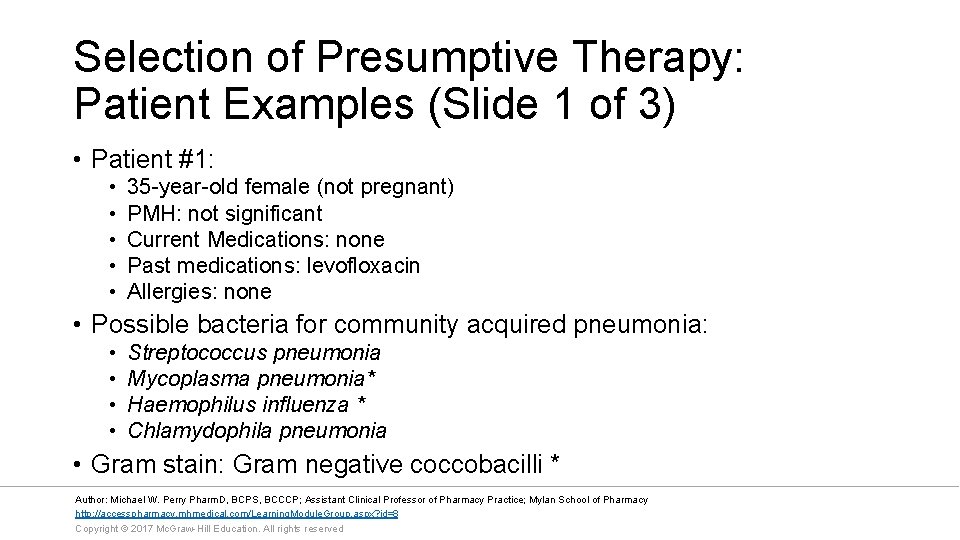
Selection of Presumptive Therapy: Patient Examples (Slide 1 of 3) • Patient #1: • • • 35 -year-old female (not pregnant) PMH: not significant Current Medications: none Past medications: levofloxacin Allergies: none • Possible bacteria for community acquired pneumonia: • • Streptococcus pneumonia Mycoplasma pneumonia* Haemophilus influenza * Chlamydophila pneumonia • Gram stain: Gram negative coccobacilli * Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
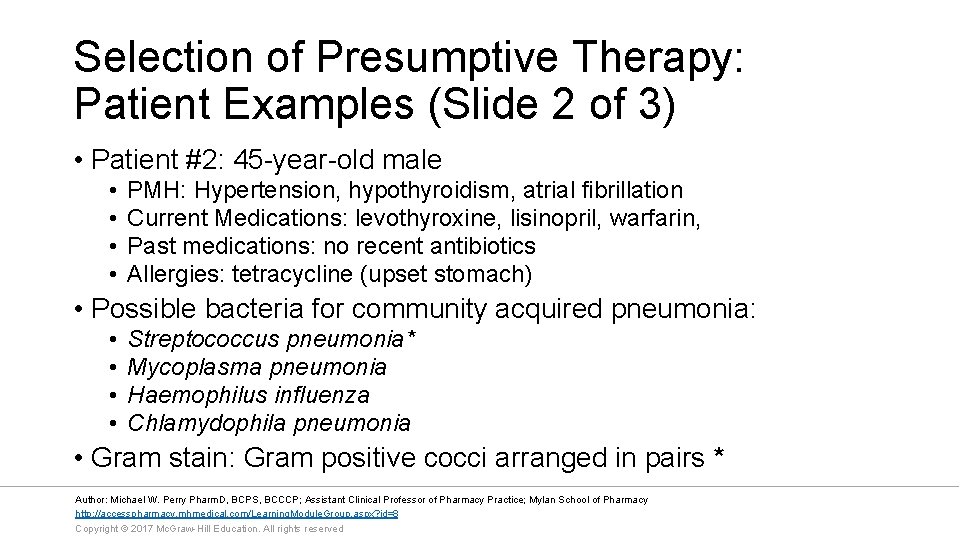
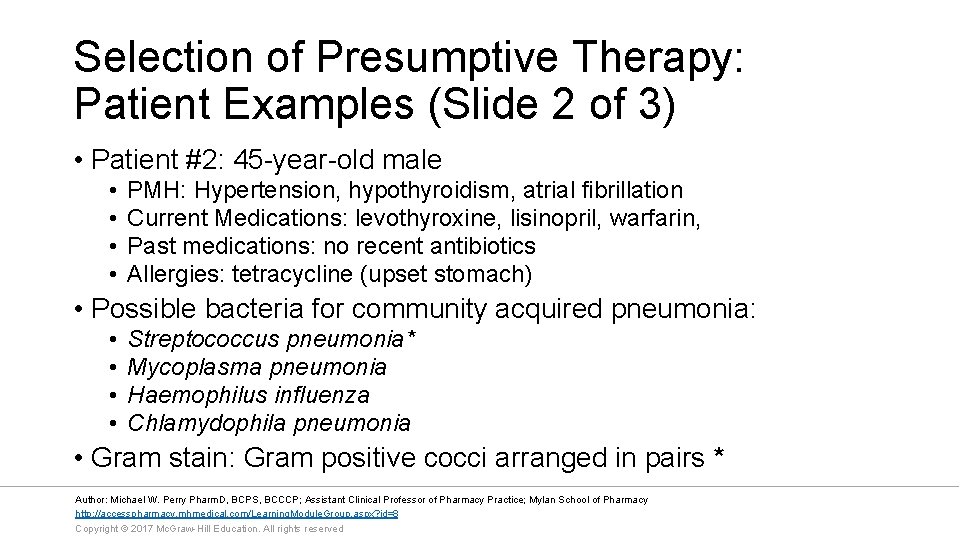
Selection of Presumptive Therapy: Patient Examples (Slide 2 of 3) • Patient #2: 45 -year-old male • • PMH: Hypertension, hypothyroidism, atrial fibrillation Current Medications: levothyroxine, lisinopril, warfarin, Past medications: no recent antibiotics Allergies: tetracycline (upset stomach) • Possible bacteria for community acquired pneumonia: • • Streptococcus pneumonia* Mycoplasma pneumonia Haemophilus influenza Chlamydophila pneumonia • Gram stain: Gram positive cocci arranged in pairs * Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
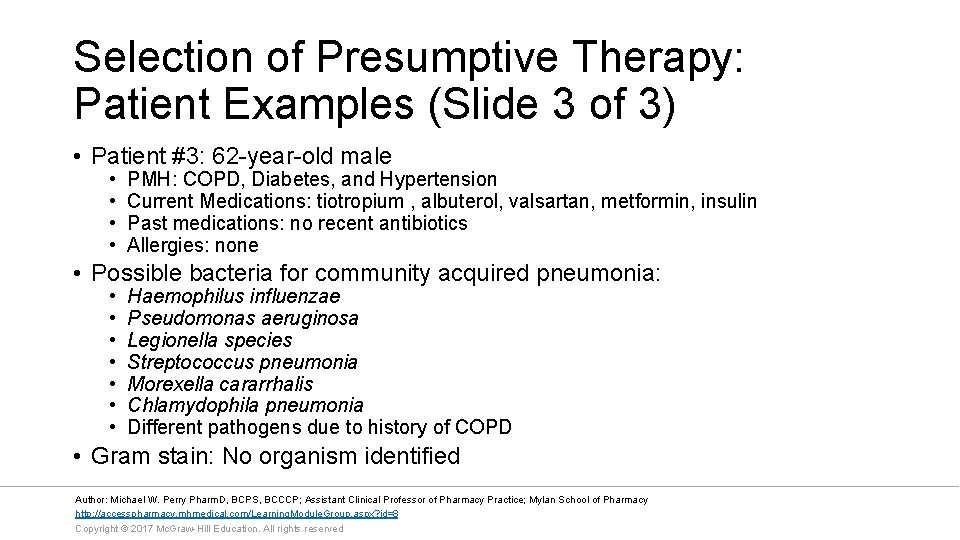
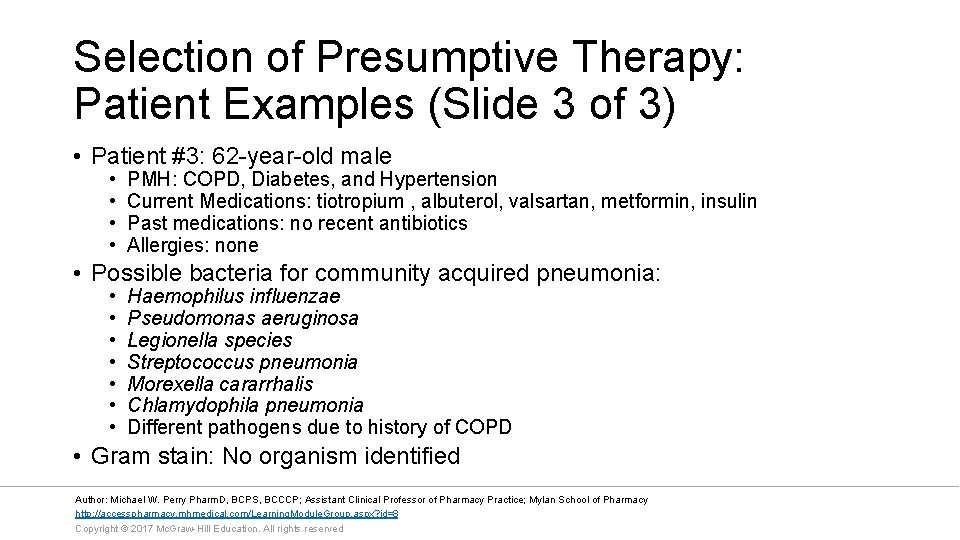
Selection of Presumptive Therapy: Patient Examples (Slide 3 of 3) • Patient #3: 62 -year-old male • • PMH: COPD, Diabetes, and Hypertension Current Medications: tiotropium , albuterol, valsartan, metformin, insulin Past medications: no recent antibiotics Allergies: none • Possible bacteria for community acquired pneumonia: • • Haemophilus influenzae Pseudomonas aeruginosa Legionella species Streptococcus pneumonia Morexella cararrhalis Chlamydophila pneumonia Different pathogens due to history of COPD • Gram stain: No organism identified Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Monitoring Therapeutic Response: Introduction • Patient should be monitored for clinical improvements for two to three days following the initiation of antimicrobial therapy • Decrease in signs and symptoms of infection • Absence of fevers • Correction of WBC count • Patients that fail to respond to therapy should be reevaluated closely Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Monitoring Therapeutic Response: Switching from IV to Oral Therapy • Patients with an overall clinical improvement should be considered to be switched from parenteral to oral antimicrobial therapy • Patients should meet the following criteria • Lack of fever for 8 to 24 hours • Decreased WBC count • Have a functioning Gastrointestinal tract • Oral antimicrobial therapy should have excellent oral bioavailability and activity against the suspected or isolated pathogen Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Monitoring Therapeutic Response: Failure of Antimicrobial Therapy • Drug Selection • • Inappropriate Drug Selection Incorrect dosage Incorrect route Poor penetration into the site of infection • Patient Factors • Immunosuppression • Need for surgical intervention to control source of infection • Microorganisms • Intrinsic resistance • Acquired Resistance • • Alteration in the target site Change in membrane permeability Efflux pump Drug inactivation Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Antibiograms • Institutional differences in pathogen susceptibility • An antibiogram is a periodic summary of antimicrobial susceptibilities of local bacterial isolates submitted to the hospital's clinical microbiology laboratory • The information in the antibiogram aid clinicians in the empiric selection of antimicrobial therapies. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
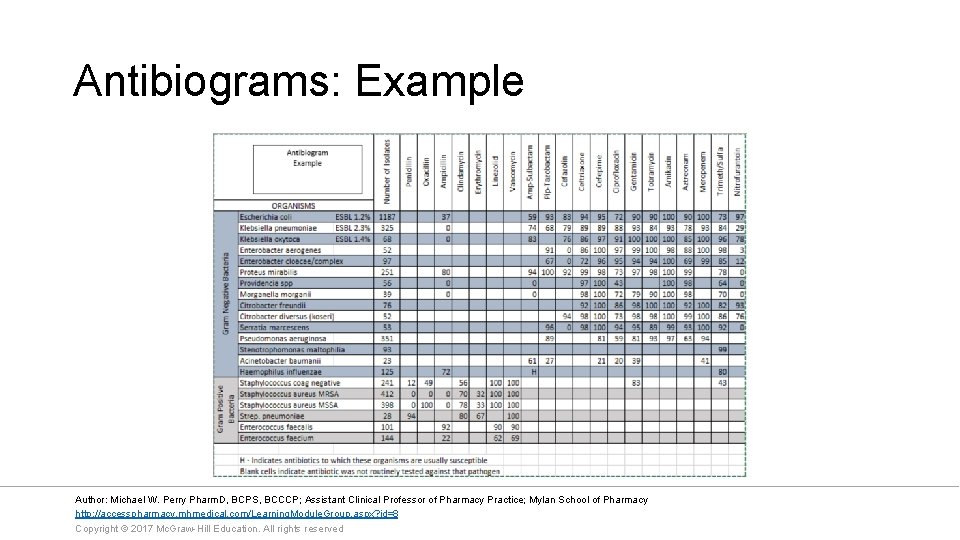
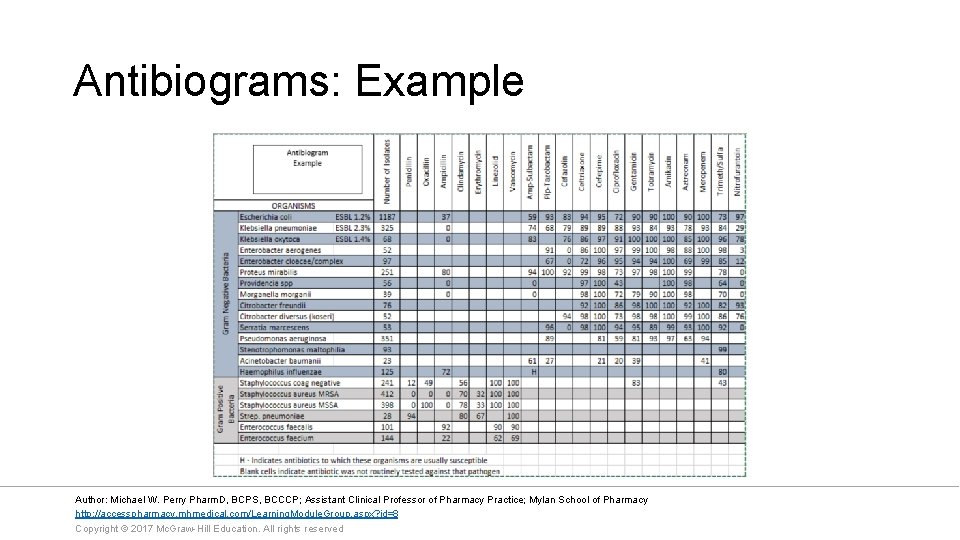
Antibiograms: Example Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Antimicrobial Stewardship • Multidisciplinary team that ensures appropriate and judicious use of antimicrobial therapy in an institution • Make formulary recommendations • Restrict antimicrobial therapies to infectious disease specialists Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Common Bacteria Link: List of Drugs of Choice, First Choice, Alternative(s) Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
Summary • Confirm the presence of infection • Nonspecific signs and symptoms of infection • Fever • WBC count • Pain and inflammation • Site specific symptoms • Identify of the pathogen • Gram Stain • Culture • Rapid test • Select empiric antimicrobial therapy based on suspected infection, patient, medication factors, and local resistance • Monitoring therapeutic response • Improvement of signs and symptoms • Consider changing patient from parenteral to oral therapy Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
References • Lee GC, Burgess DS. Chapter 83. Antimicrobial Regimen Selection. In: Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 9 e. ` New York, NY: Mc. Graw-Hill; 2014. • Lampiris HW, Maddix DS. Clinical Use of Antimicrobial Agents. In: Katzung BG, Trevor AJ. eds. Basic & Clinical Pharmacology, 13 e. New York, NY: Mc. Graw-Hill; 2015. • Rybak MJ, Aeschlimann JR, La. Plante KL. e. Chapter 25. Laboratory Tests to Direct Antimicrobial Pharmacotherapy. In: Di. Piro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L. eds. Pharmacotherapy: A Pathophysiologic Approach, 9 e. New York, NY: Mc. Graw-Hill; 2014. Author: Michael W. Perry Pharm. D, BCPS, BCCCP; Assistant Clinical Professor of Pharmacy Practice; Mylan School of Pharmacy http: //accesspharmacy. mhmedical. com/Learning. Module. Group. aspx? id=8 Copyright © 2017 Mc. Graw-Hill Education. All rights reserved
 Epidemiological triad
Epidemiological triad Icd 10 morbus hansen
Icd 10 morbus hansen Hennepin county infectious disease manual
Hennepin county infectious disease manual Stages of infectious disease
Stages of infectious disease What is the smallest infectious agent
What is the smallest infectious agent Infectious disease quality controls
Infectious disease quality controls Infectious disease board review
Infectious disease board review Types of infection
Types of infection Infectious disease
Infectious disease Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Communicable disease and non communicable disease
Communicable disease and non communicable disease Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Hhps symbols
Hhps symbols Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Noncellular infectious protein particles are called
Noncellular infectious protein particles are called Lead poisoning
Lead poisoning Infectious nucleic acid
Infectious nucleic acid Infectious stunting syndrome
Infectious stunting syndrome Definition of infectious waste
Definition of infectious waste Infectious mononucleosis
Infectious mononucleosis Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Prescriptive screening vs prospective
Prescriptive screening vs prospective Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Types of diseases
Types of diseases What causes genetic diseases
What causes genetic diseases Monocyte derived dendritic cells
Monocyte derived dendritic cells Mastigophora diseases
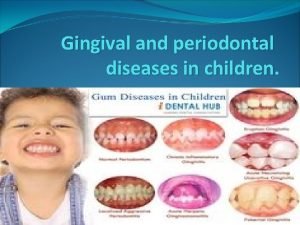
Mastigophora diseases Types of gingiva
Types of gingiva Difference between communicable and noncommunicable
Difference between communicable and noncommunicable Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Diseases in civil war
Diseases in civil war Modern lifestyle and hypokinetic diseases
Modern lifestyle and hypokinetic diseases Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases In what situation should a nail service not be performed?
In what situation should a nail service not be performed? Nutritional diseases
Nutritional diseases Vitamins functions
Vitamins functions Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases