IN THE NAME OF GOD THE COMPASSIONATE THE




























- Slides: 66

IN THE NAME OF GOD THE COMPASSIONATE THE MERCIFUL
Histology Lecture 22 Female Reproductive System
Female Reproductive System Female reproductive system comprises of the following organs: 1 Ovaries 1 Oviducts 1 Uterus 1 Vagina 1 External Genitalia Ø Mammary Gland is a skin appendix but due to its close relation to reproductive system explains here

Ovary IOvaries are small almond shaped organs lying in pelvic cavities IThe surface epithelium is simple cuboidal and known as germinal epithelium I Tunica albuginea is a dense irregular connective tissue that is directly beneath epithelium IThe ovary can be divided into two components: cortex and medulla IHilum is the route whereby vessels and nerves enter and leave the ovary IMedulla is the core of ovary contains loose connective tissue and vessels IRemnants of Wollfian ducts persists from embryonic period and are irregular tubules lined by a cuboidal epithelium

Ovary IHilus cells are identical to Leydig cells, and may contain Reinke’s crystalloids ISmall clumps of hilus cells are often found near blood vessels IMedulla contains stromal cells identical to those which are in the cortex ECortex has two components a stroma and structures that producing gametes ECortical stroma has closely packed spindle shaped fibroblast-like cells which are arranged in a whorled pattern ECollagen fibers between stromal cells are prominent in outer cortex and with time the amount of collagen will increase


Ovary ü Stroma provides structural support, forms theca interna and externa around follicles, and secretes steroid hormone ü There is three types of stromal steroid secreting cells: I. Scattered luteinized stromal cells which are numerous during pregnancy II. Stromal cells that form theca layers III. Enzymically active stromal cells (EASC)which are numerous in postmenopausal women and secret testosterone
Ovarian Follicles ã Ovarian follicles located in cortex and surrounded by stromal cells ã A follicle consists of an oocyte surrounded by one or more layers of follicular cells ã 2 ovaries of young adult female have about 400, 000 follicles; most of them will degenerate (atresia) ã About 450 follicles will cycle to ovulation in lifetime

Types of Ovarian Follicles ü According to morphological characteristic follicles can be categorized into: ÖPrimordial Follicles ÖGrowing Follicles ÖUnilaminar primary follicles ÖMultilaminar primary follicles ÖSecondary follicles ÖMature Follicles (Tertiary or Graafian Follicles)

Primordial Follicle • Primordial follicles contain a primary oocyte that entered the prophase of first mitotic division • Primary oocyte surrounded with one layer of flattened follicular cells which are separated by a basal lamina from the stroma • Many of them degenerate during lifetime • Most numerous in fetus (several million) • One million at birth • At the onset of the buberty their number reduced to about a quarter of a million • Oocyte about 25 µm diameter • Euchromatic nucleus, large nucleolus

Growing Follicles ÔOocyte diameter increases to 100 to 150 µm ÔNucleus enlarges and called germinal vesicle(GV) ÔOrganelles increase in number and amount (mitochondria, several golgi complexes, RER, free ribosomes) ÔFollicular cells become cuboidal ÔUnilaminar primary follicle has one layer of cuboidal follicular cells ÔMultilaminar primary follicle has several layers of follicular (granulosa) cells
Growing Follicles ï Zona pellucida secreted by oocyte and is composed of 3 glycoproteins ZP 1, ZP 2, ZP 3 forms just outside oocyte membrane, thick basal lamina ï Follicle cell filopodia extend into Zona pellucida as do oocyte microvilli, joined by gap junctions ï Stromal cells differentiate into theca folliculi that has a theca interna and theca externa ï A thickened basal lamina separated theca interna from granulosa cells

Theca Interna & Theca Externa v. Theca Interna § Cells are more cuboidal with round nuclei § steroid producing cell features § SER, mitochondria with tubular cristae and lipid droplets § produce androstenedione which is converted to estradiol by granulosa cells § highly vascularized v. Theca externa Ø Ø Composed of connective tissue and stromal cells with vessels forming a plexus cells are flattened
Secondary Follicles Ü Granulosa and theca cells increase in number Ü Fluid-filled spaces in granulosa layer fuse to form the antrum that become filled with liquor folliculi Ü This fluid is an exudates of plasma and produced by granulosa cells. It contains GAGs, proteoglycans, steroid binding protein, steroids and some hormones. Ü Cumulus oophorus is a small group of granulosa cells that surround primary oocyte and project into antrum Ü A single layer of granulosa cells that immediately surround the primary oocyte is known as corona radiata Ü Most of follicle at this stage become atretic Ü Some granulosa cells of atretic follicles do not degenerate and form interstitial glands which secret androgens

Mature (Graafian) Follicles ° Mature follicle develops due to continued proliferation of granulosa cells and production of more liquor folliculi which undergo ovulation ° By the time of ovulation it may be over 2. 5 cm in diameter ° Bulge from ovary surface ° Because of continued formation of liquor folliculi cumulus oophorus detaches and float freely in liquor folliculi


Oocyte Meiotic Divisions ÞFirst meiotic division occurs just prior to ovulation under the influence of meiosis inducing factor ÞSecond meiotic division then begins and stops at metaphase ÞSecond meiotic division is completed after fertilization
Ovulation ÏFluid pressure builds up until follicle ruptures due to formation of proteoglycans and hyaluronic acid and attraction of water ÏBefore ovulation the surface of ovary loses its blood supply just where the follicle pressing it and known as stigma ÏPerifollicular connective tissue broken down by proteases ÏOvum (Secondary oocyte) is drawn into open end of oviduct (fallopian tube) ÏOvum remains viable about 24 hours after ovulation ÏRemnants of graafian follicle are converted to corpus hemorrhagicum
Corpus Hemorrhagicum Ø Following ovulation the remainder of follicle collapses and some ruptured blood vessels leak into follicular cavity and forming a clot that is known as corpus hemorrhagicum Corpus Luteum ² After removing the clot by phagocytes a temporary hormone secreting structure formed by granulosa cells and theca interna cells known as corpus luteum ² Granulosa cells hypertrophy into large pale staining granulosa-lutein cells with organelles necessary for steroid production ² They constitute about 80% of the cells of corpus luteum ² These cells produce progesterone and convert androgen produced by theca-lutein cells into estrogens

Corpus Luteum J Theca interna cells form theca-lutein cells which are smaller and darker staining than granulosa-lutein cells J Located in folds of cells in perimeter of corpus luteum form about 20% of cells population and are highly vascularized J Produce estrogen, progesterone androgens J If pregnancy does not occur corpus luteum of mensturation survives only 10 -14 days J In pregnancy it enlarges greatly due to HCG and lasts 6 months and called corpus luteum of pregnancy J Corpus luteum of pregnancy grows to a 5 cm diameter structure


Corpus Albicans [When the corpus luteum degenerate it is invaded by fibroblasts which manufacture collagen type I and form a fibrous structure known as corpus albicans [Large ones form after pregnancy and smaller ones after each ovulation [On the surface of ovary remnants of corpus albicans is visible as a scar

Oviduct àUterine tube is a muscular tube, 12 cm long àIt is the site of fertilization àUpper end opens into peritoneal cavity near ovary àLower end passes through the uterus wall àOviduct has 4 segments îintramural part in uterine wall îisthmus is adjacent to uterine wall îampulla is dilated part îinfundibulum is funnel-shaped part near ovary with fimbriae

Oviduct { Mucosa has many longitudinal folds which are pronounced in the ampulla { Mucosa has a simple columnar epithelium consist of ciliated cell and nonciliated peg cell { Ciliated cells are numerous near ovarian end of the tube { Peg cells are secretory cells that produce a watery tubal fluid contains normal serum proteins, chloride and potassium ions { Cilia near ovary beat toward uterus but cilia near uterus beat toward ovary { Lamina propria composed of loose connective tissue
Oviduct i Muscularis consists of poorly defined Inner circular layer and outer longitudinal layer of smooth muscle cells i Muscularis peristaltic movements with the beating of the cilia of epithelium help to propel oocyte to the uterus i Serosa is a connective tissue layer lined by a simple squamous epithelium contains blood vessels, and nerves


Uterus ª Uterus is a pear-shaped structure attached to oviducts at upper end and to vagina at lower end ª Uterus is divided into three regions: Body Fundus Cervix ª Wall of body and fundus has 3 layers • Endometrium • Myometrium • Adventitia/Serosa

ø Anterior portion of body covered by adventitia which is composed of areolar connective tissue ø The remaining portion of uterus covered by serosa composed of a layer of simple squamous cells (mesothelium) resting on an areolar connective tissue
Myometrium ¯ Myometrium is the thickest layer and composed of four poorly defined layers of smooth muscle separated by connective tissue ¯ Inner and outer layers are mostly longitudinal in orientation ¯ Middle layers are highly vascularized and consist of mostly circularly arranged bundle of smooth muscle cells ¯ Arcuate arteries located in this layers and is known as Stratum Vasculare ¯ Middle layers thicken during pregnancy with more and large smooth muscle cells (hyperplasia and hypertrophy) and increased collagen fibers ¯ Myometrium is estrogen dependent in absent of estrogen smooth muscle cell atrophies and some of the begin to apoptosis
Endometrium áEndometrium is mucosal lining of uterus composed of a simple columnar epithelium áEpithelium has ciliated columnar cells and secretory columnar cells áLamina propria composed of dense irregular connective tissue and vessels supports epithelium and houses simple tubular glands áThe glands have not ciliated cells áEndometrium has 2 zones w. Functional layer w. Basal layer

Endometrial Layers Functional layer is a thick superficial layer sloughed off during menstruation and replaced during each menstrual cycle Functional layer vascularized by coiled helical arteries that originate from arcuate arteries in stratum vasculare Basal layer is a deep narrow layer retained after menstruation whose glands epithelium and connective tissue element regenerate functional layer Basal layer supplied by short straight arteries which originate from arcuate arteries in stratum vasculare

Menstrual Cycle ÜEstrogen and progesterone from ovary stimulate changes in the endometrium ÜThe average menstrual cycle is 28 day ÜBegins age is about 12 -15 y/o and ends age is about 45 -50 y/o ÜThe menstrual cycle has 3 main phases ü Menstrual phase: days 1 -4 ü Proliferative (follicular) phase: days 5 -14 ü Ovulation around day 14 ü Secretory (luteal) phase: days 15 -28
Proliferative (Follicular) Phase ÷ Days 5 -14 leading up to ovulation ÷ Estrogen produced by theca cells of ovarian follicle ÷ Cells of gland bases proliferate forming simple columnar epithelium and tubular glands of endometrium ÷ Connective tissue cells proliferate in lamina propria ÷ Coiled arteries grow into regenerated lamina propria ÷ Functionalis of endometrium become 2 -3 mm in thickness ÷ glands have a straight tubes with narrow lumens but their cells accumulate glycogen ÷ At the day 14 the functional layer has been fully restored

Secretory (Luteal) Phase í Begins after ovulation, days 15 -28 í Corpus luteum forms and produces progesterone í Glands develop further, become highly coiled, branched and begin to secrete í Coiled arteries also attain full development í Endometrium reaches 5 mm in thickness due to edema and accumulated glycogen secretions of the glands

Menstrual Phase /If fertilization does not take place the corpus luteum stops secreting hormones after about 14 days /Progesterone and estrogen decrease causing coiled arteries to intermittently constrict cutting off blood flow to the functional layer of endometrium /Endometrial cells die and the functional layer is sloughed off /Then coiled arteries dilate once again, because they are weakened they rupture /The disgorged blood removes patches of the functional layer as menses /Vessels distal to constrictions are shed with the functional layer causing some bleeding /About 35 ml blood loss occur during mensturation

Uterine Cervix U Cervix is the lower part of uterus that protrude into vagina U It is lined by mucous secreting simple columnar epithelium U Part of cervix in upper vagina has stratified squamous nonkeratinized epithelium U Lamina propria composed of mostly dense connective tissue and many elastic fibers and a few smooth muscle cells U Mucosa do not slough off during menstruation U Cervical mucosa contains branched cervical glands U At time of ovulation cervical glands secrete a serous fluid U At other time the secretion become viscous and during pregnancy forming a plug U Softening of cervix during parturition is due to lysis of collagen
Vagina • A thick stratified squamous nonkeratinized epithelium lines the vaginal mucosa • Estrogen stimulates epithelium to synthesize glycogen • Mucosa has not glands but increment of fluid during sexual arousal is due to transudate from vessels of lamina propria and secretion of cervical glands • Underlying lamina propria composed of loose connective tissue that highly vascularized with many elastic fibers • Muscular layer of circular and a prominent longitudinal smooth muscle fibers • Adventitia of dense irregular connective tissue with elastic fibers, many vessels and vast venous plexus and nerves

Female Urethra §Female urethra is about 5 cm in length §It is lined by transitional epithelium near bladder and stratified squamous nonkeratinized in reminder portion §Patches of pseudostratified columnar is interspersed §Lamina propria is a fibroelastic connective tissue §Mucous secreting glands of Littre are numerous along its length §Muscular layers is composed of an outer circular and an inner longitudinal smooth muscle fibers §When urethra pierce urogenital diaphragm a sphincter of skeletal muscle surrounds it
External Genitalia(Vulva) External genitalia is consists of mons pubis, labia majora, labia minora, clitoris, Bartholin’s glands, minor vestibular glands, and hymen Mons pubis is the are overlying symphysis pubis covered by skin that underneath it is a pad of fat Labia majora are skin folds with an adipose core and a thin layer of smooth muscle skin with coarse hair on their external surface, sweat and sebaceous glands, many nerve fibers Labia minora are folds of skin without hair and with core of spongy connective tissue with elastic fibers skin with sebaceous and sweat glands, and many nerve fibers
External Genitalia ÖClitoris is embryonic homologue of penis Öcontains 2 erectile tissue bodies Öcovered by stratified squamous epithelium Öheavily innervated ÖBartholin’s glands are mucous secreting glands with ducts opening into the vestibule of vagina ÖMinor vestibular glands are also opened into vestibule ÖHymen is a thin fold of epithelially enclosed fibrovascular connective tissue that narrow the orifice of vagina in virgin
Mammary Glands ÒMammary gland consists of 15 -25 lobes of compund tubuloacinar glands similar to apocrine sweat glands ÒGlands secrete by apocrine mechanism (lipids) and exocytosis (proteins) ÒEach lobe surrounded by dense irregular connective tissue and adipose tissue ÒConnective tissue surrounding acini has many plasma cells and lymphocytes, sources of milk immunoglobulins ÒEach lobe has its own duct leading into lactiferous ducts of nipple ÒInterlobular ducts have simple cuboidal epithelium surrounded by myoepithelial cells ÒLactiferous sinuses lined by stratified squamous epithelium that changes to stratified columnar or cuboidal deeper in lactiferous ducts ÒGlandular cells proliferate during pregnancy

Areola & Nipple • Areola is a circular highly pigmented skin around nipple; color darkens during pregnancy due to increased melanin production by melanocytes • Areola contains sweat and sebaceous glands and also areolar glands of Montgomery that resemble both sweat and mammary glands • Nipple is a protuberance at the center of areola that is covered by stratified squamous keratinized epithelium • Terminal portion of lactiferous ducts end at nipple • The core of nipple is composed of dense collagenous CT with abundant elastic fibers connected to skin • Abundant smooth muscle fibers arrange in circular way around nipple and in longitudinal way along axis of the nipple

Department of Histology F. Rajaei
 In the name of allah the compassionate the merciful
In the name of allah the compassionate the merciful Uoa aegrotat
Uoa aegrotat Example of compassionate letter to yourself
Example of compassionate letter to yourself Compassionate ottawa
Compassionate ottawa Allah the compassionate
Allah the compassionate Allah the compassionate
Allah the compassionate Compassionate respectful and caring
Compassionate respectful and caring The most compassionate
The most compassionate Compassionate capitalism definition
Compassionate capitalism definition Pallatie
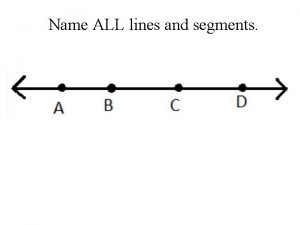
Pallatie Draw three noncollinear points j k and l
Draw three noncollinear points j k and l Our god is an awesome god vine
Our god is an awesome god vine Our god is an awesome god he reigns
Our god is an awesome god he reigns Our god is an awesome god medley
Our god is an awesome god medley God is good god is great speed
God is good god is great speed O god you are my god earnestly i seek you
O god you are my god earnestly i seek you God-given virtues that direct us to our loving, triune god.
God-given virtues that direct us to our loving, triune god. God-given virtues that direct us to our loving, triune god.
God-given virtues that direct us to our loving, triune god. My god's bigger than your god
My god's bigger than your god Don't covet your neighbor's
Don't covet your neighbor's God's promises
God's promises O lord how excellent
O lord how excellent In the name of god amen mayflower compact
In the name of god amen mayflower compact In the name of god most gracious prayer
In the name of god most gracious prayer 馮定華神父2020
馮定華神父2020 Hermes roman name
Hermes roman name In the name of god the beneficent the merciful
In the name of god the beneficent the merciful In the name of god the beneficent the merciful
In the name of god the beneficent the merciful The most gracious
The most gracious Toy story 2 repairman
Toy story 2 repairman Colossians 1:17-19
Colossians 1:17-19 Name
Name God saves name
God saves name In the name of god the most gracious the most merciful
In the name of god the most gracious the most merciful In the name of god the merciful
In the name of god the merciful His name is the word of god
His name is the word of god What was apollo's realm
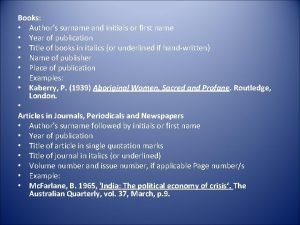
What was apollo's realm Authors by initials
Authors by initials Name above every other name
Name above every other name Angle names
Angle names Class person string name
Class person string name What is name
What is name Name of presentation company name
Name of presentation company name Name of presentation company name
Name of presentation company name Name teachers name class date
Name teachers name class date Her name is betty
Her name is betty How old is
How old is Name class section subject
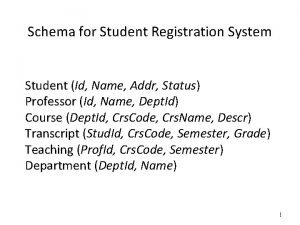
Name class section subject Student id name department name
Student id name department name Git user name
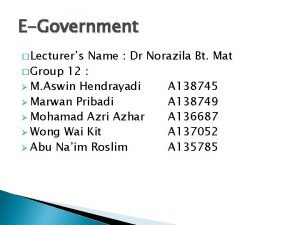
Git user name Lecturer's name or lecturer name
Lecturer's name or lecturer name Agile inception
Agile inception Name class teacher date
Name class teacher date First name last name tpu
First name last name tpu Stock name and classical name of elements
Stock name and classical name of elements Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Thang điểm glasgow
Thang điểm glasgow Hát lên người ơi alleluia
Hát lên người ơi alleluia Kể tên các môn thể thao
Kể tên các môn thể thao Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ