How to interpret lung function tests Roles of





- Slides: 48
How to interpret lung function tests
Roles of Lung Function Tests of FUNCTION Diagnosis: support (exclude) pattern recognition Quantifying severity Monitoring: progress treatment Prognosis
Choice of Tests WHAT IS THE QUESTION? eg compatibility with specific diagnosis? how severe is the functional defect? has there been improvement/deterioration?
Collateral Information Clinical Radiographic BMI Smoking Haemoglobin
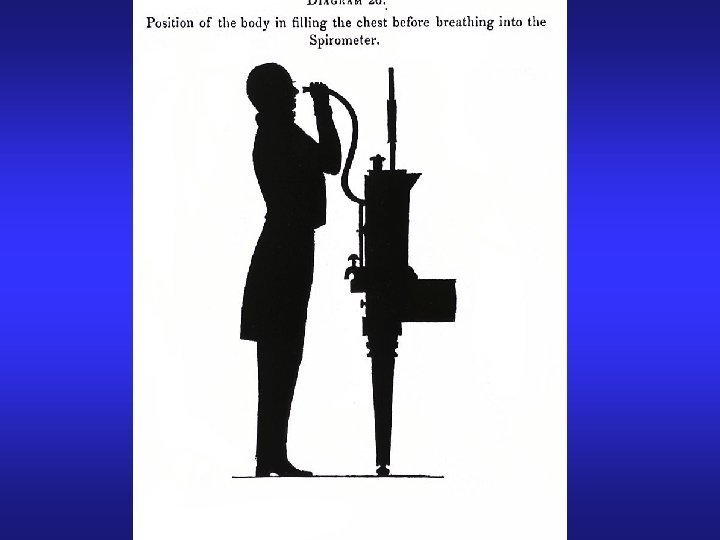
Spirometry KEEP IT SIMPLE! FEV 1 } (F)VC } usually suffice FEV 1/(F)VC }
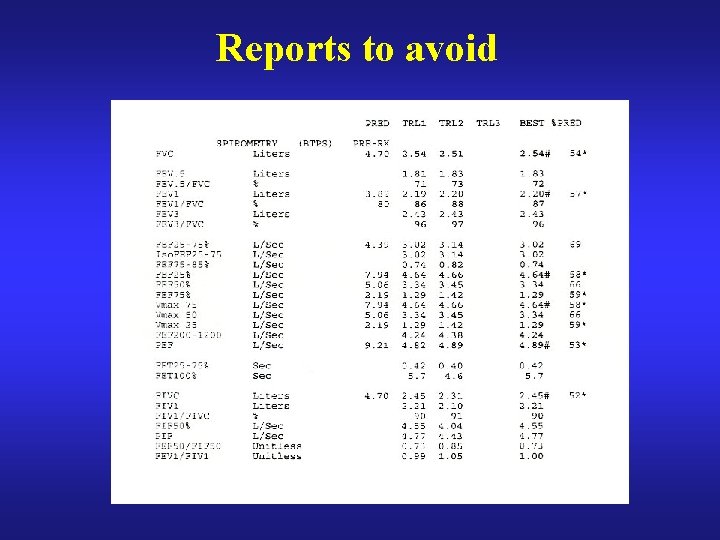
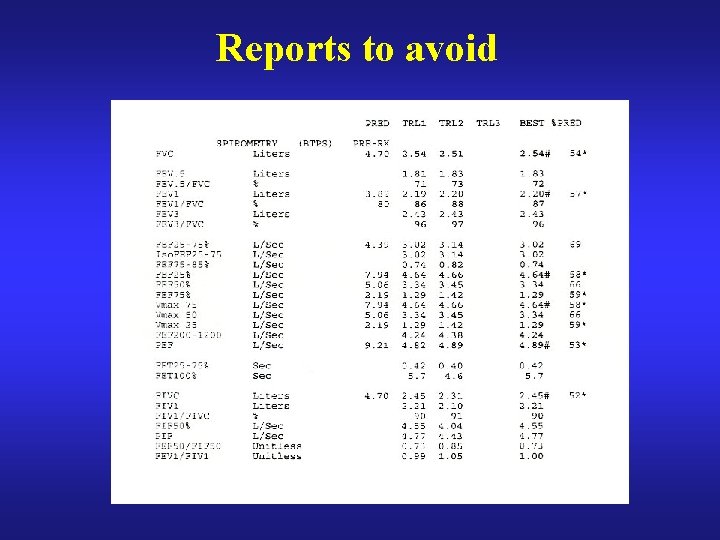
Reports to avoid
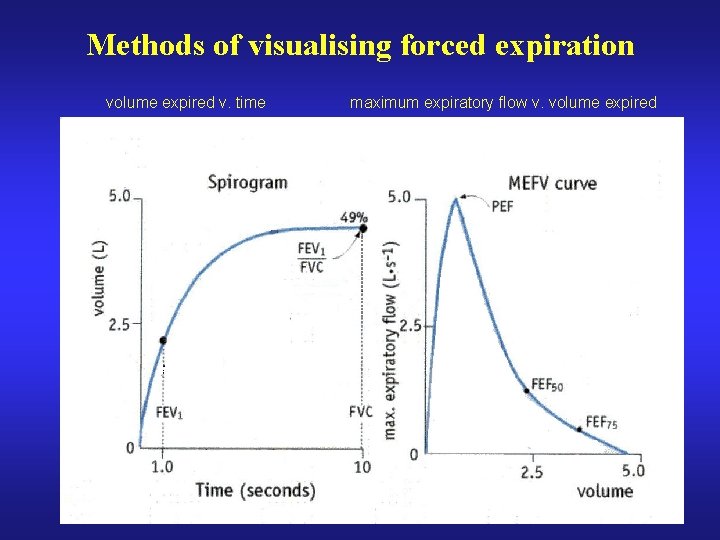
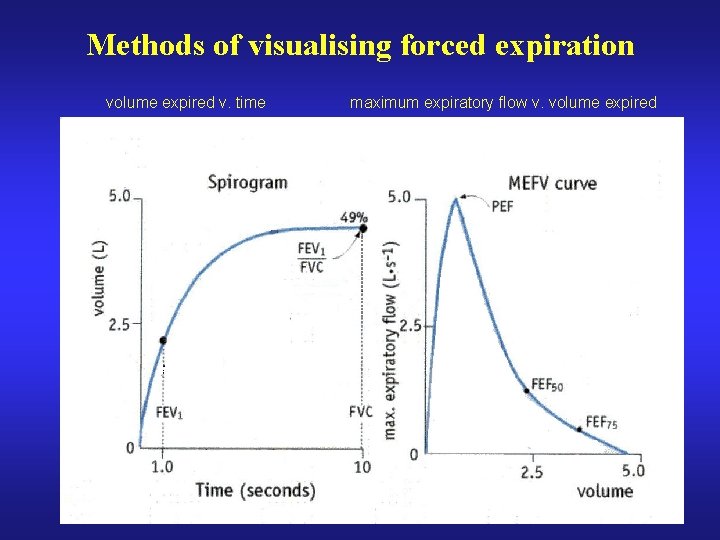
Methods of visualising forced expiration volume expired v. time maximum expiratory flow v. volume expired
Maximum Flow-Volume Curves Recognition of central airway narrowing Useful to visualise effort Longitudinal changes within subject BUT Seductive and easily overinterpreted
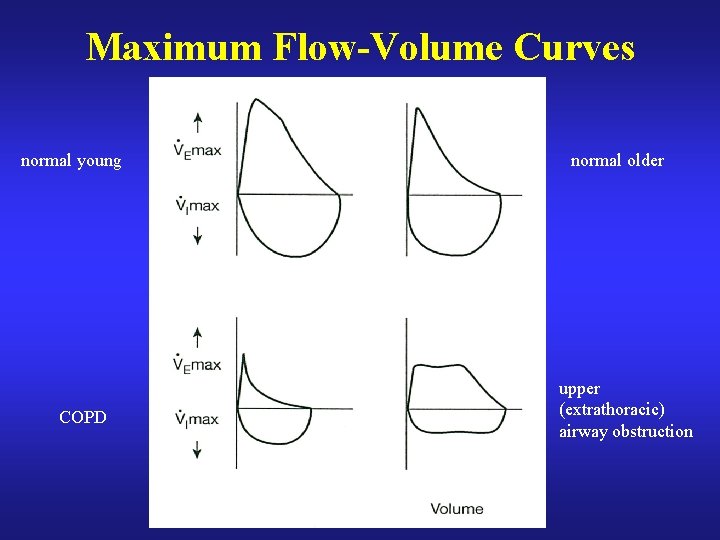
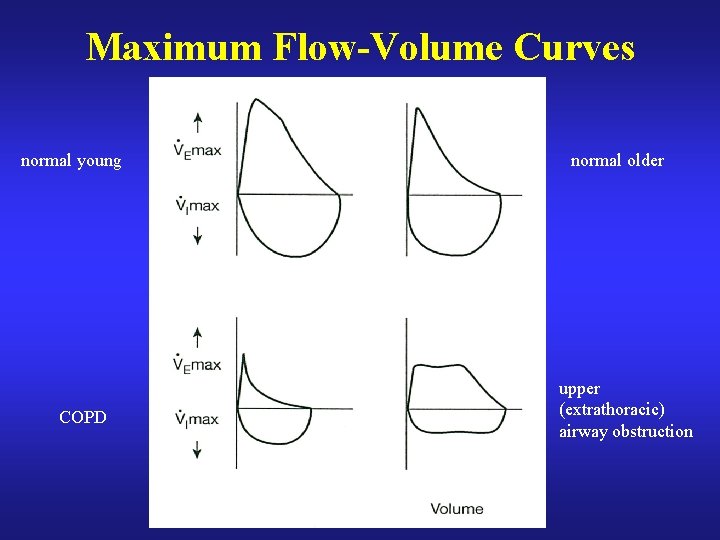
Maximum Flow-Volume Curves normal young COPD normal older upper (extrathoracic) airway obstruction
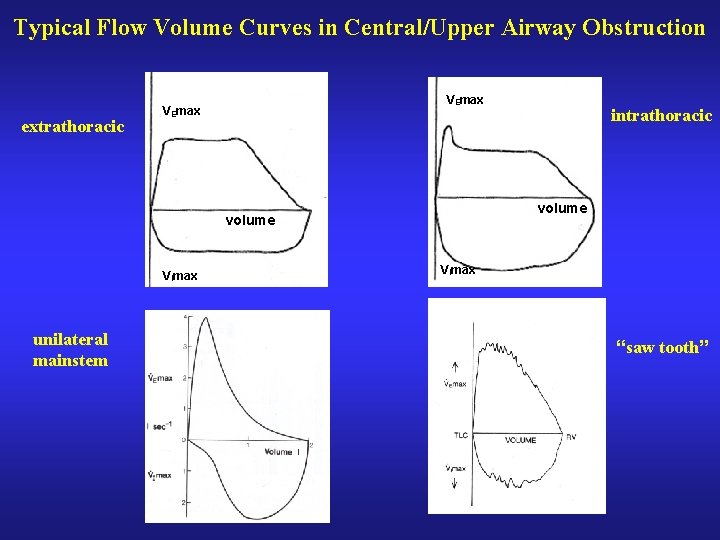
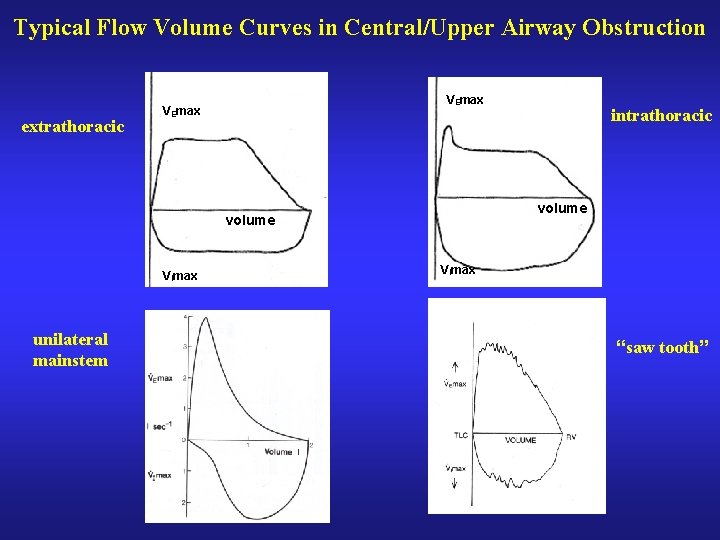
Typical Flow Volume Curves in Central/Upper Airway Obstruction extrathoracic VEmax volume VImax unilateral mainstem intrathoracic VImax “saw tooth”

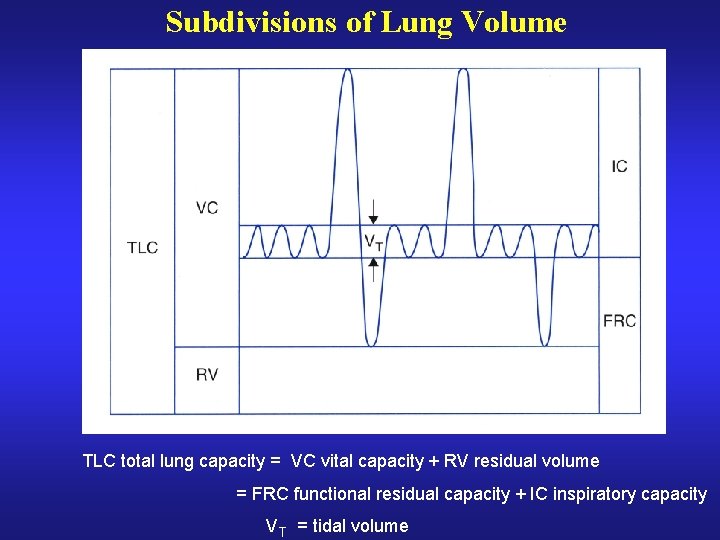
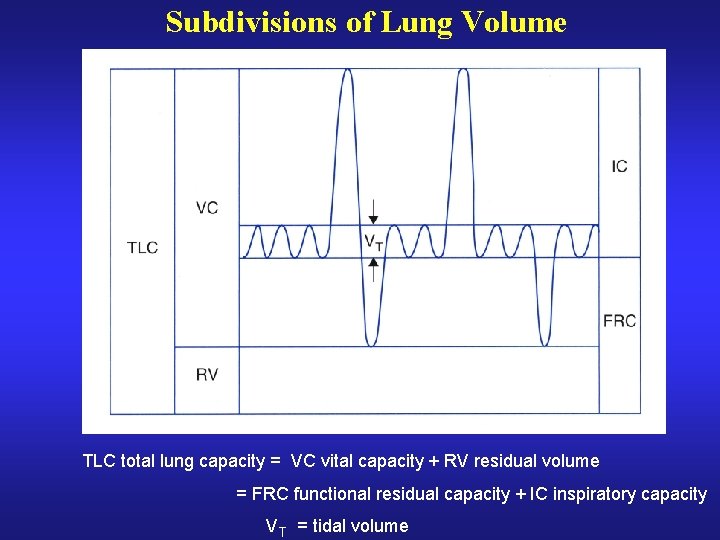
Subdivisions of Lung Volume TLC total lung capacity = VC vital capacity + RV residual volume = FRC functional residual capacity + IC inspiratory capacity V T = tidal volume
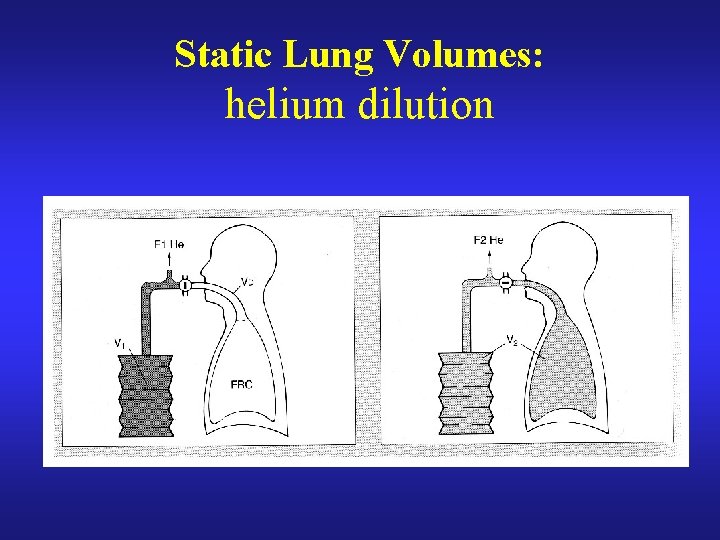
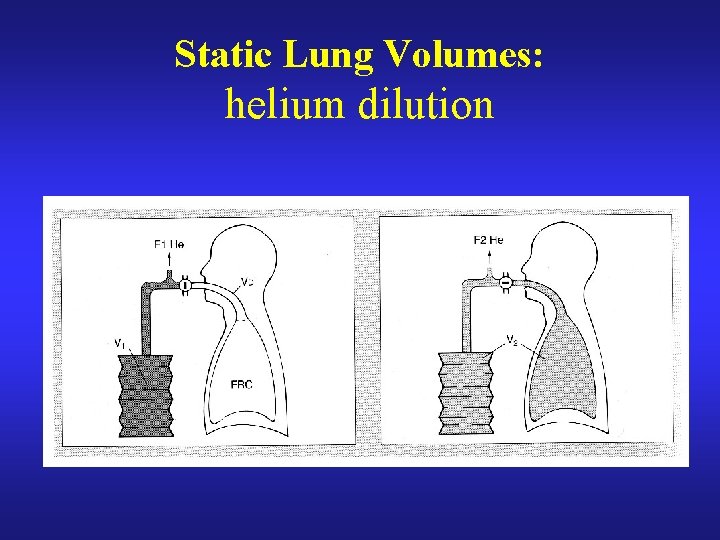
Static Lung Volumes: helium dilution
Inert Gas Dilution – practicalities (1) closed circuit rebreathing CO 2 absorbed oxygen added to maintain constant FRC level equilibration recognised by stable helium concentration TLC/RV by immediate inspiration from/ expiration into spirometer with healthy lungs equilibration takes c. 5 minutes
Inert Gas Dilution – practicalities (2) Due to uneven ventilation in patients with airway obstruction: equilibration is very slow the endpoint may be unclear TLC and RV are often underestimated repeat measurements may be impracticable
Body Plethysmography
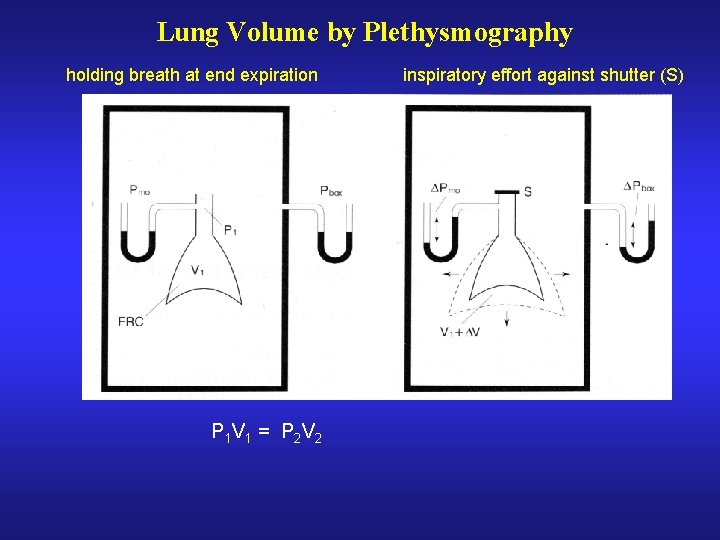
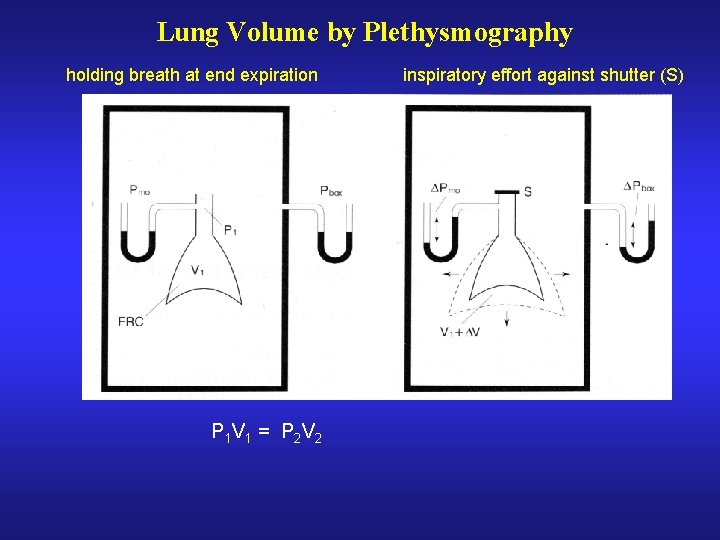
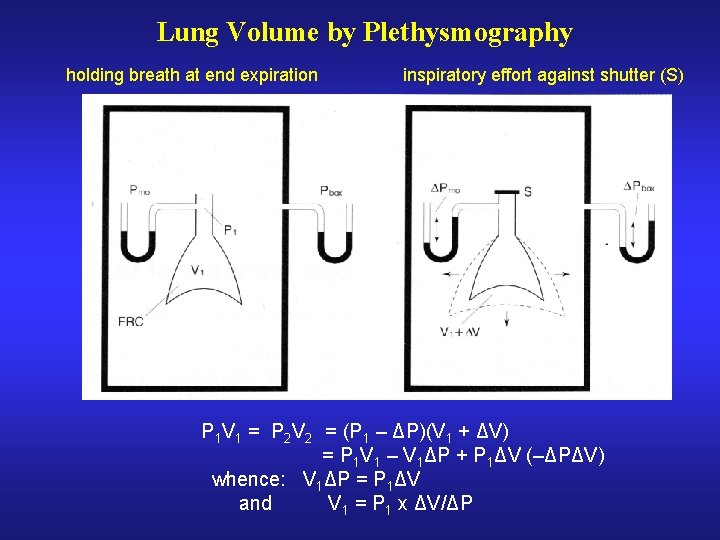
Lung Volume by Plethysmography holding breath at end expiration P 1 V 1 = P 2 V 2 inspiratory effort against shutter (S)
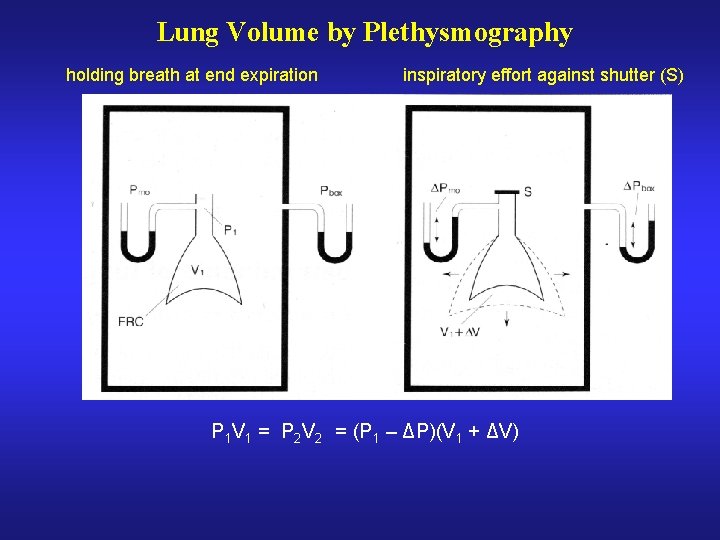
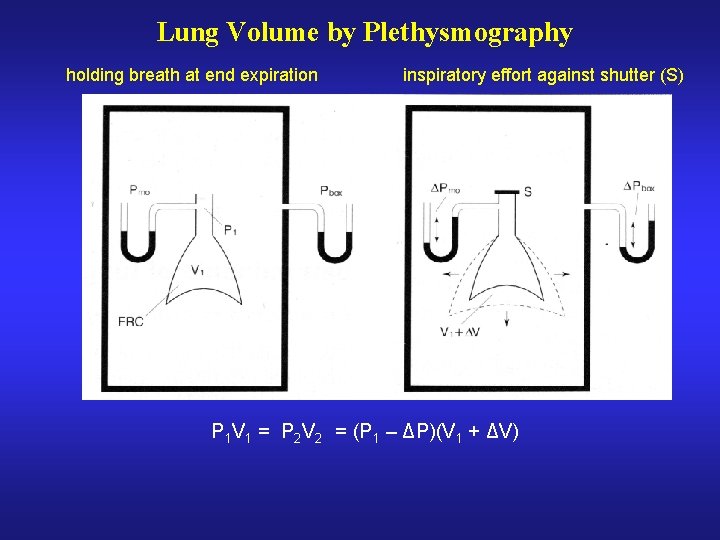
Lung Volume by Plethysmography holding breath at end expiration inspiratory effort against shutter (S) P 1 V 1 = P 2 V 2 = (P 1 – ΔP)(V 1 + ΔV)
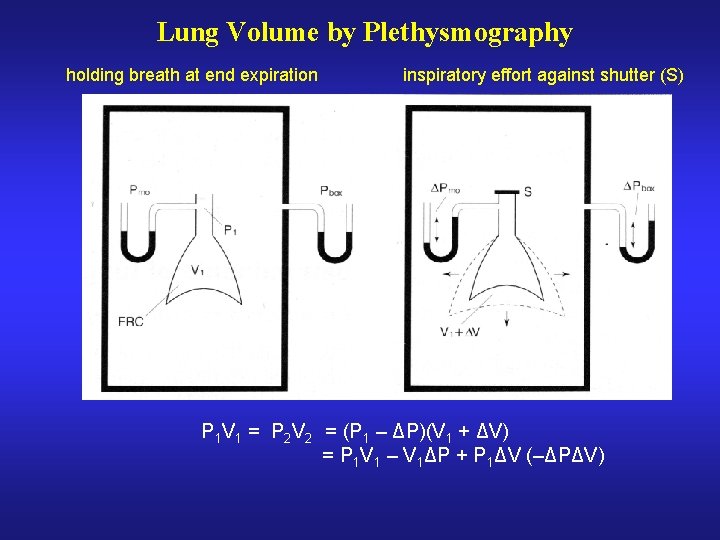
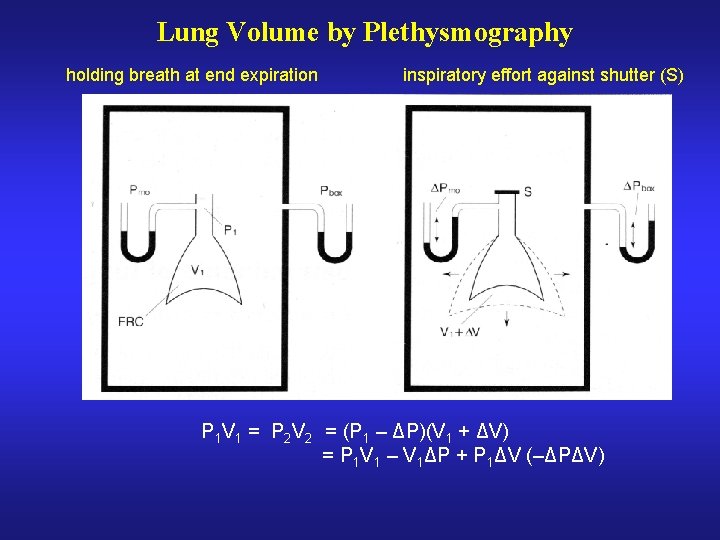
Lung Volume by Plethysmography holding breath at end expiration inspiratory effort against shutter (S) P 1 V 1 = P 2 V 2 = (P 1 – ΔP)(V 1 + ΔV) = P 1 V 1 – V 1ΔP + P 1ΔV (–ΔPΔV)
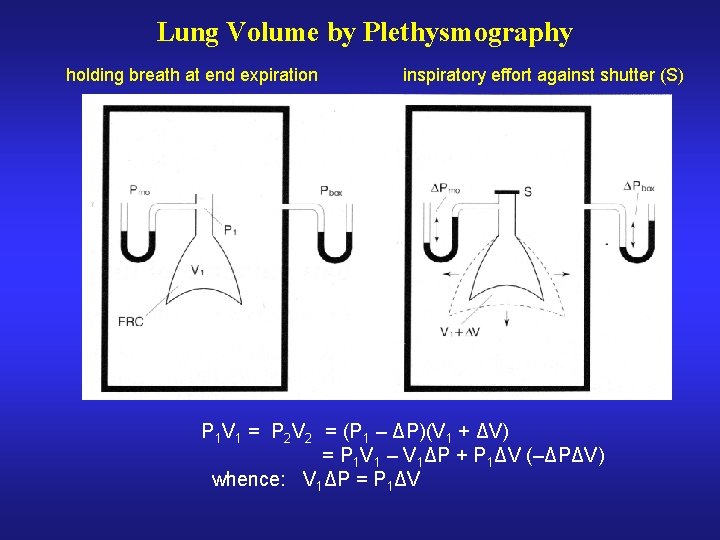
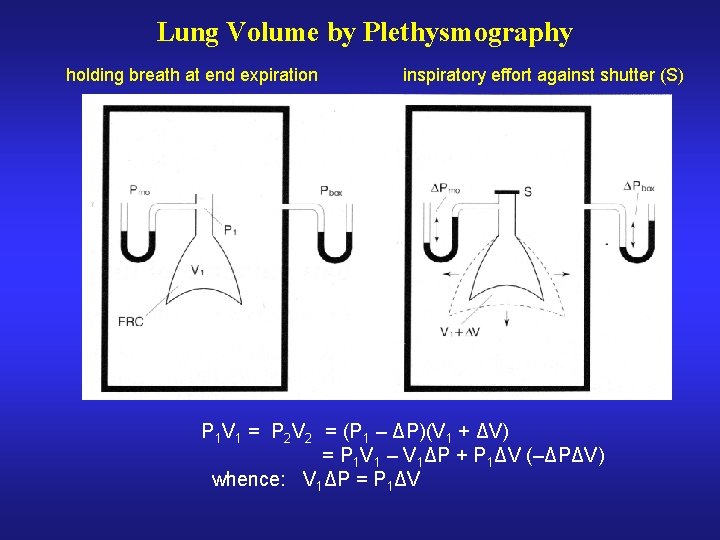
Lung Volume by Plethysmography holding breath at end expiration inspiratory effort against shutter (S) P 1 V 1 = P 2 V 2 = (P 1 – ΔP)(V 1 + ΔV) = P 1 V 1 – V 1ΔP + P 1ΔV (–ΔPΔV) whence: V 1ΔP = P 1ΔV
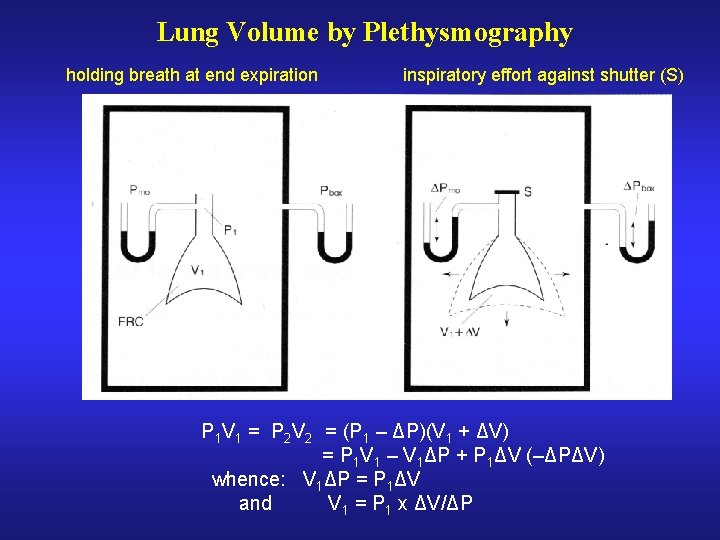
Lung Volume by Plethysmography holding breath at end expiration inspiratory effort against shutter (S) P 1 V 1 = P 2 V 2 = (P 1 – ΔP)(V 1 + ΔV) = P 1 V 1 – V 1ΔP + P 1ΔV (–ΔPΔV) whence: V 1ΔP = P 1ΔV and V 1 = P 1 x ΔV/ΔP
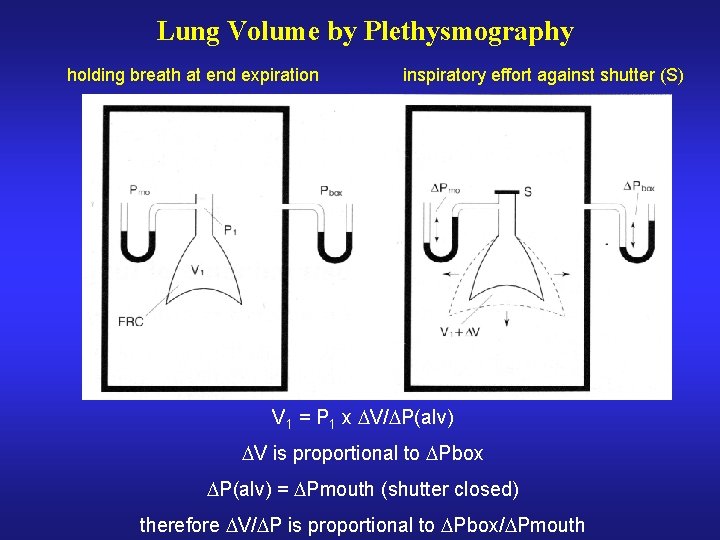
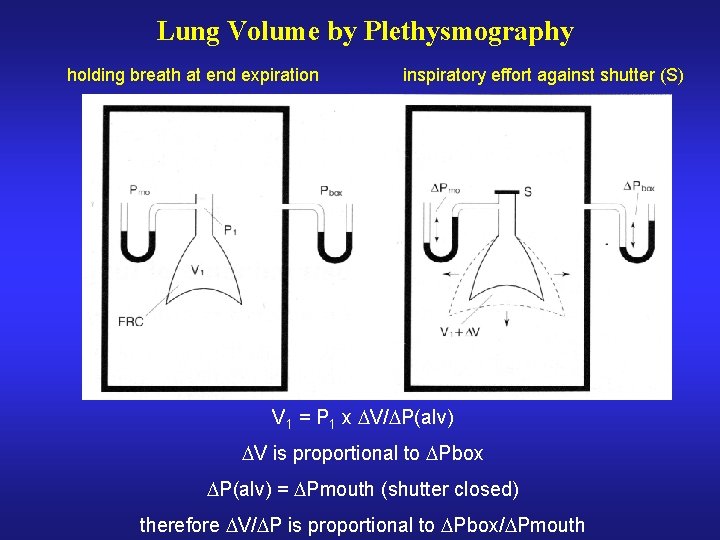
Lung Volume by Plethysmography holding breath at end expiration inspiratory effort against shutter (S) V 1 = P 1 x V/ P(alv) V is proportional to Pbox P(alv) = Pmouth (shutter closed) therefore V/ P is proportional to Pbox/ Pmouth
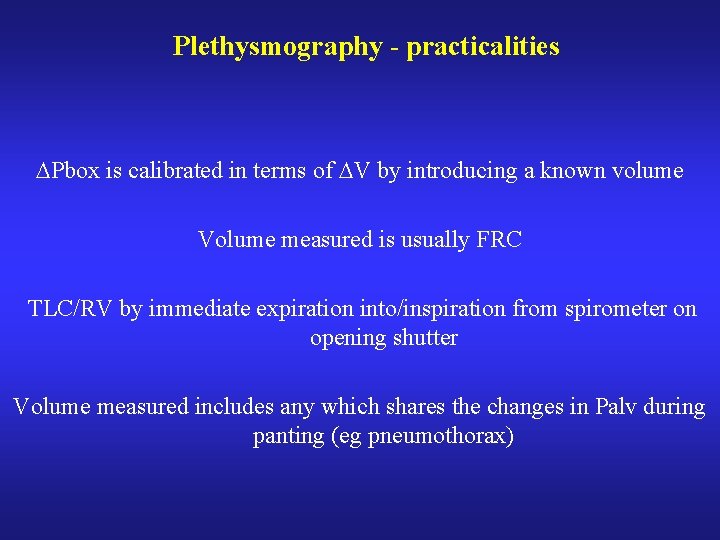
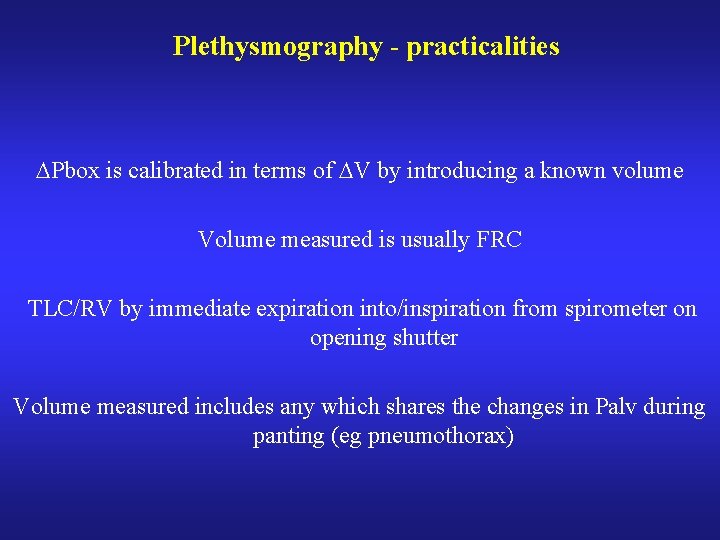
Plethysmography - practicalities Pbox is calibrated in terms of V by introducing a known volume Volume measured is usually FRC TLC/RV by immediate expiration into/inspiration from spirometer on opening shutter Volume measured includes any which shares the changes in Palv during panting (eg pneumothorax)
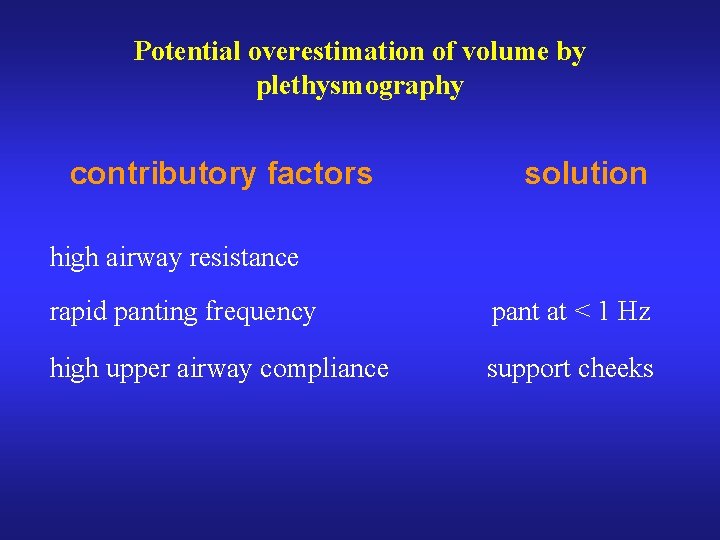
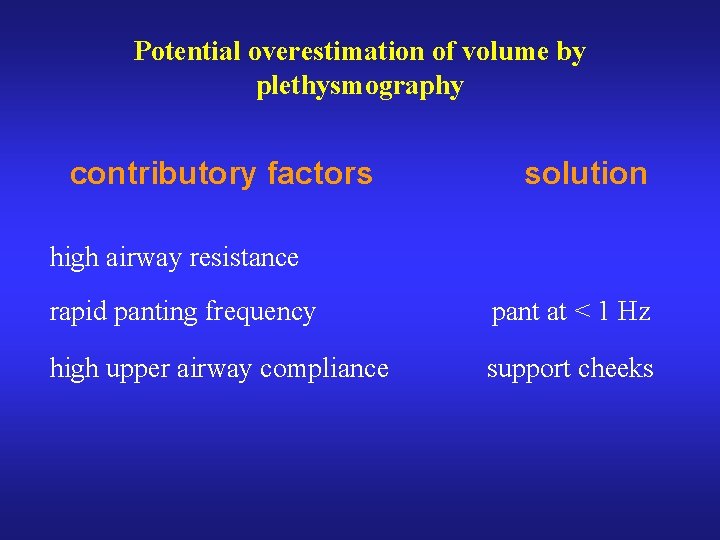
Potential overestimation of volume by plethysmography contributory factors solution high airway resistance rapid panting frequency pant at < 1 Hz high upper airway compliance support cheeks
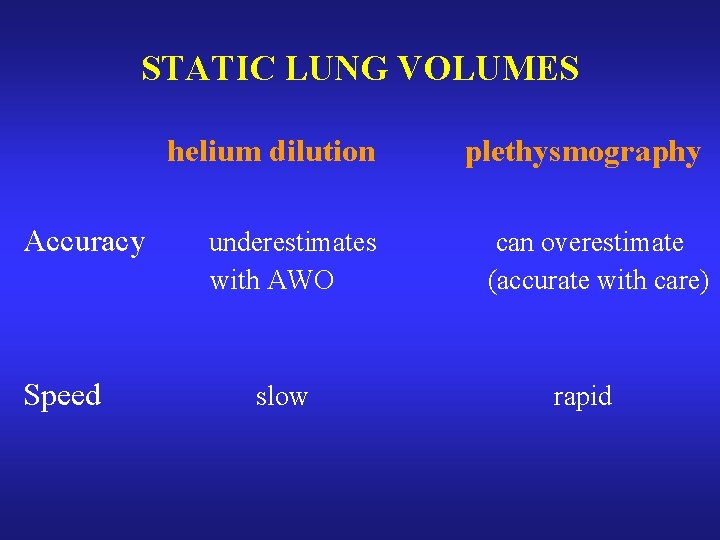
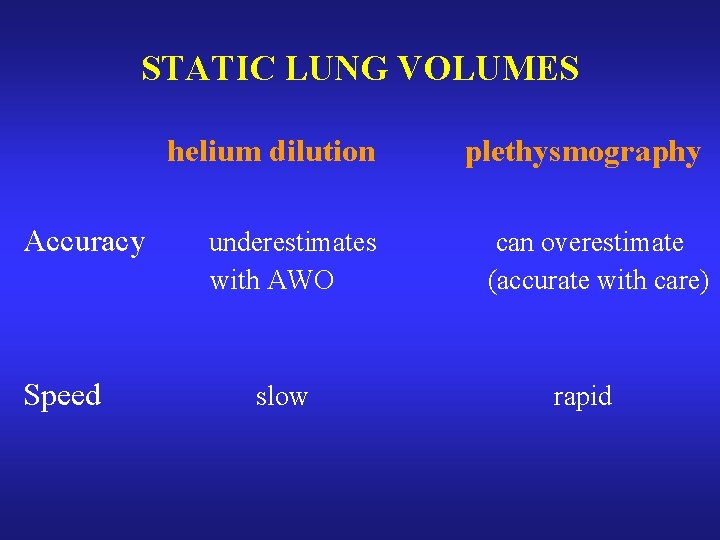
STATIC LUNG VOLUMES Accuracy Speed helium dilution plethysmography underestimates with AWO can overestimate (accurate with care) slow rapid

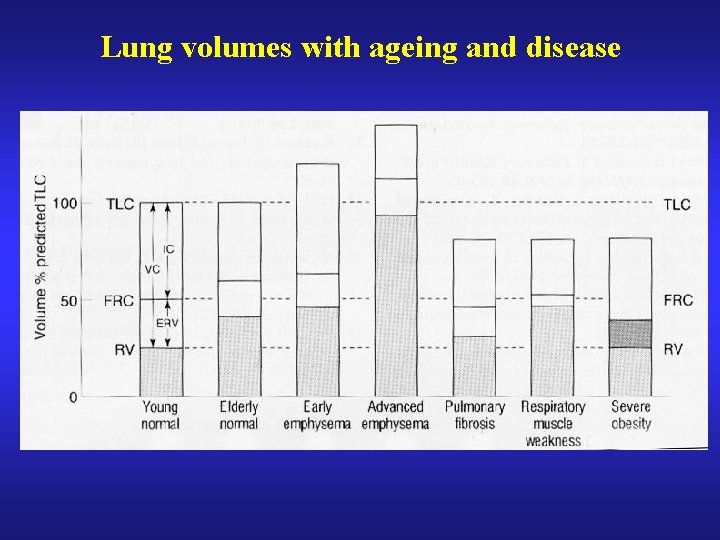
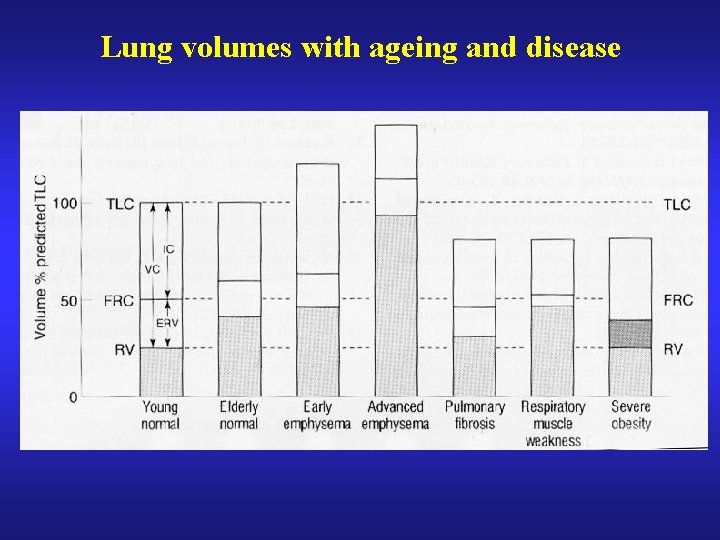
Lung volumes with ageing and disease
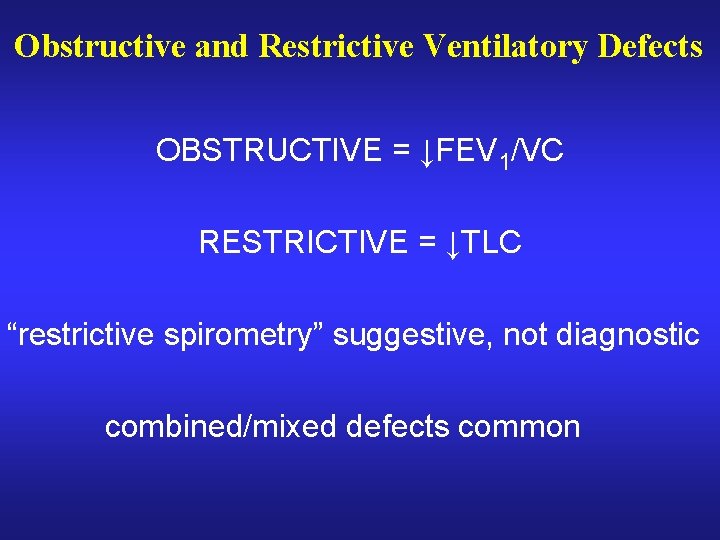
Obstructive and Restrictive Ventilatory Defects OBSTRUCTIVE = ↓FEV 1/VC RESTRICTIVE = ↓TLC “restrictive spirometry” suggestive, not diagnostic combined/mixed defects common
CO Diffusing Capacity - DLCO (CO Transfer Factor - TLCO)
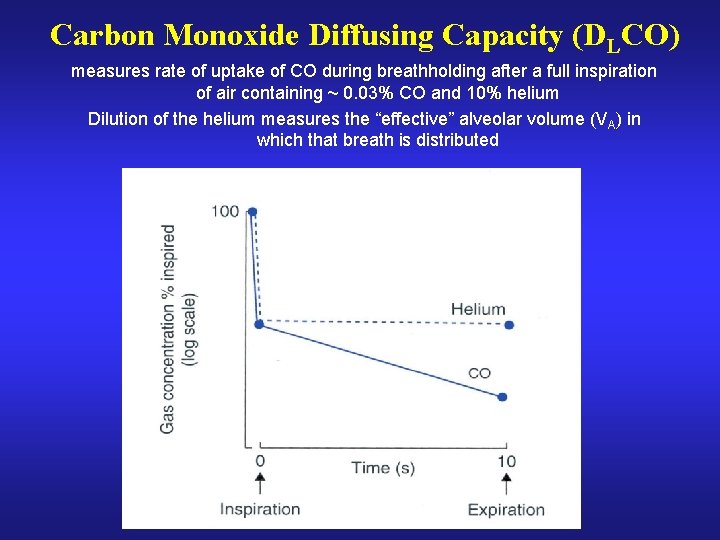
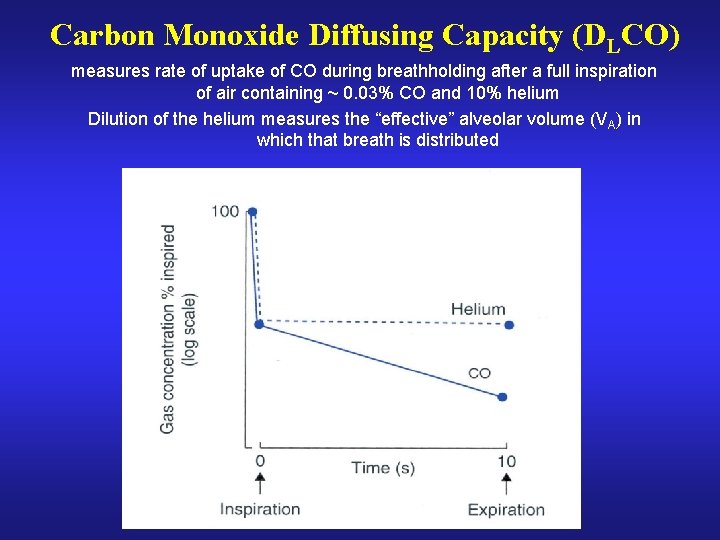
Carbon Monoxide Diffusing Capacity (DLCO) measures rate of uptake of CO during breathholding after a full inspiration of air containing ~ 0. 03% CO and 10% helium Dilution of the helium measures the “effective” alveolar volume (VA) in which that breath is distributed
Factors affecting DLCO distribution of inspired gas integrity and number of alveoli (total surface area) thickness of alveolar-capillary membrane function of pulmonary capillaries haemoglobin concentration sensitive but poor specificity
KCO - “Transfer Coefficient” DLCO = KCO x VA KCO = DLCO/VA VA is the “effective” alveolar volume KCO is the rate of uptake of CO per litre of ventilated lung
Volume Dependence of DLCO and KCO Measured during breathholding at full inflation (TLC) If measured sub-TLC less alveolar-capillary surface is exposed so total CO uptake (DLCO) is reduced But capillary blood volume unaffected therefore CO uptake per litre of lung (ie KCO) is increased Pattern of extrapulmonary volume restriction
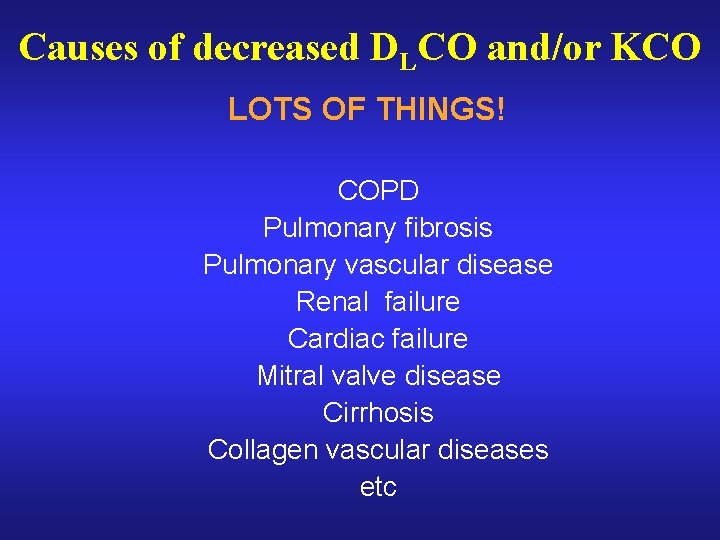
Causes of decreased DLCO and/or KCO LOTS OF THINGS! COPD Pulmonary fibrosis Pulmonary vascular disease Renal failure Cardiac failure Mitral valve disease Cirrhosis Collagen vascular diseases etc
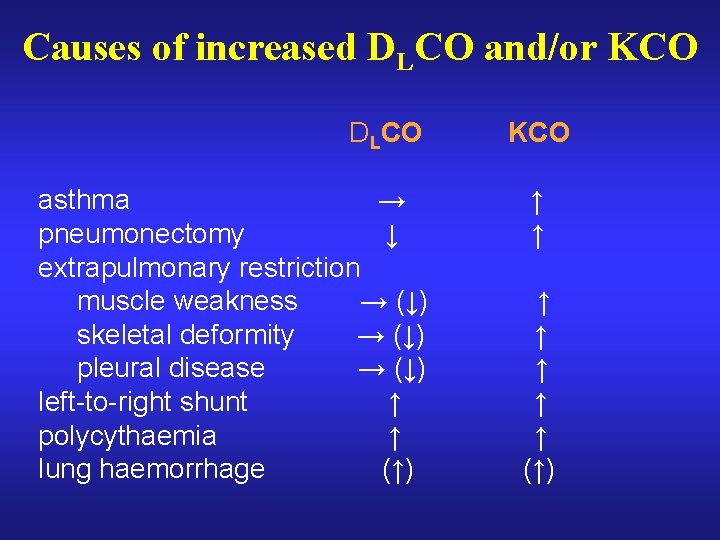
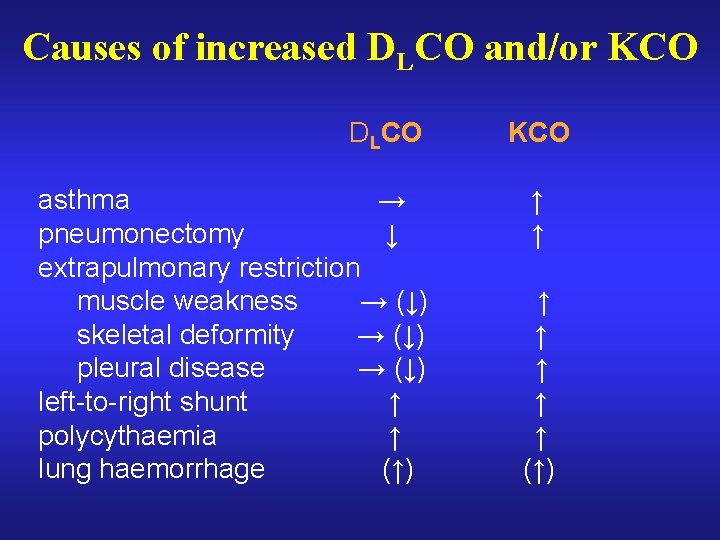
Causes of increased DLCO and/or KCO DLCO asthma → pneumonectomy ↓ extrapulmonary restriction muscle weakness → (↓) skeletal deformity → (↓) pleural disease → (↓) left-to-right shunt ↑ polycythaemia ↑ lung haemorrhage (↑) KCO ↑ ↑ ↑ ↑ (↑)

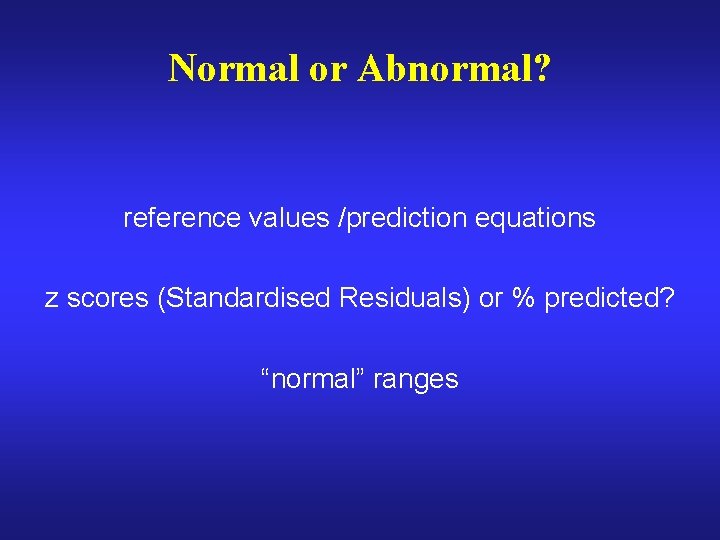
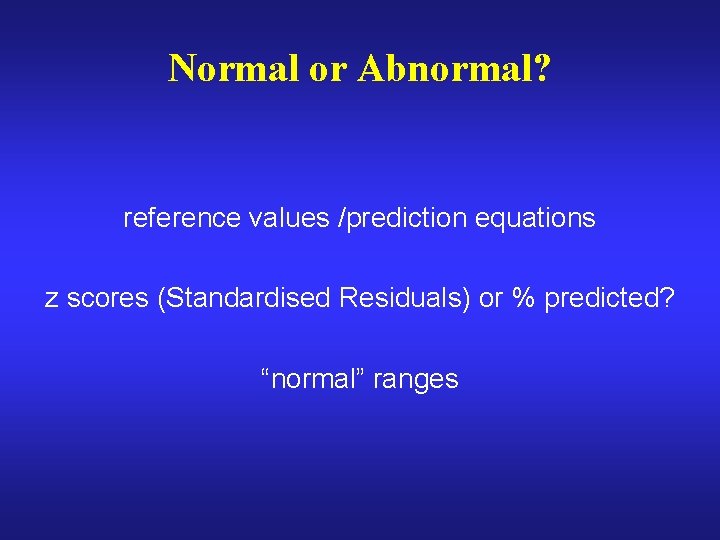
Normal or Abnormal? reference values /prediction equations z scores (Standardised Residuals) or % predicted? “normal” ranges
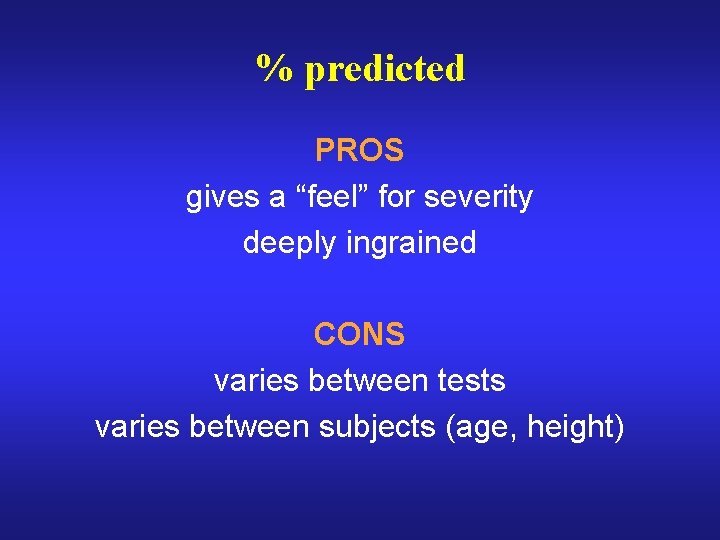
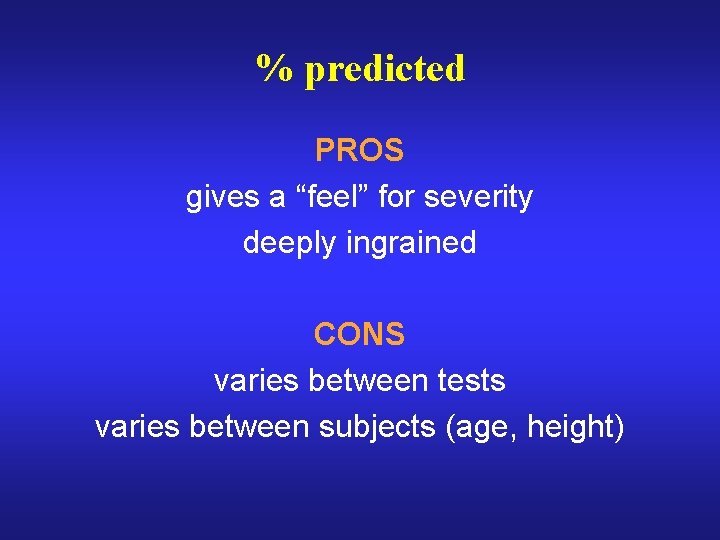
% predicted PROS gives a “feel” for severity deeply ingrained CONS varies between tests varies between subjects (age, height)
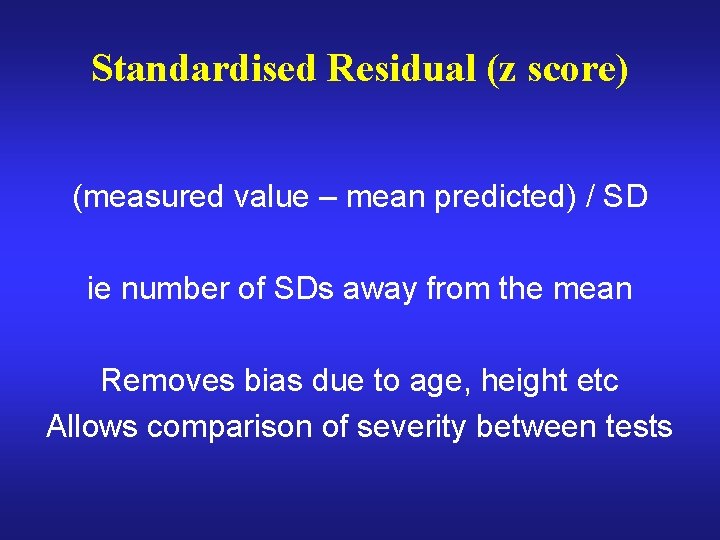
Standardised Residual (z score) (measured value – mean predicted) / SD ie number of SDs away from the mean Removes bias due to age, height etc Allows comparison of severity between tests
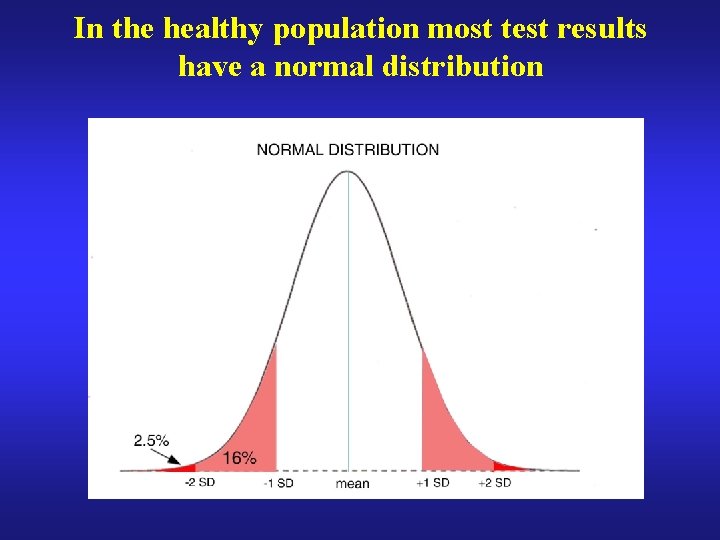
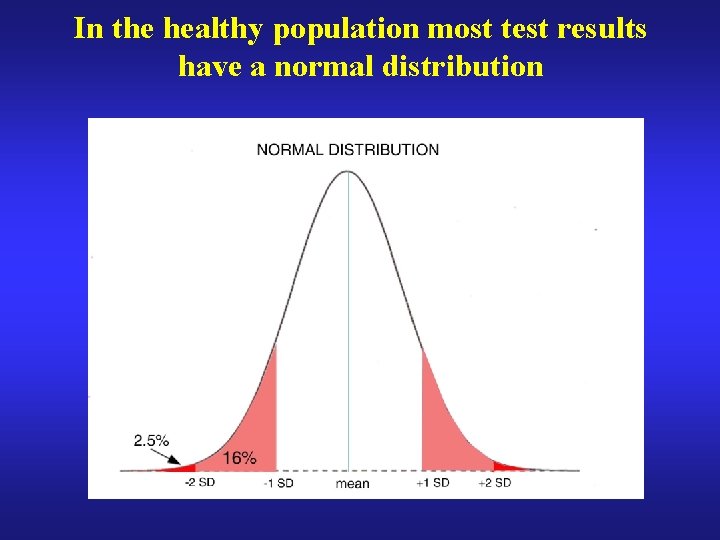
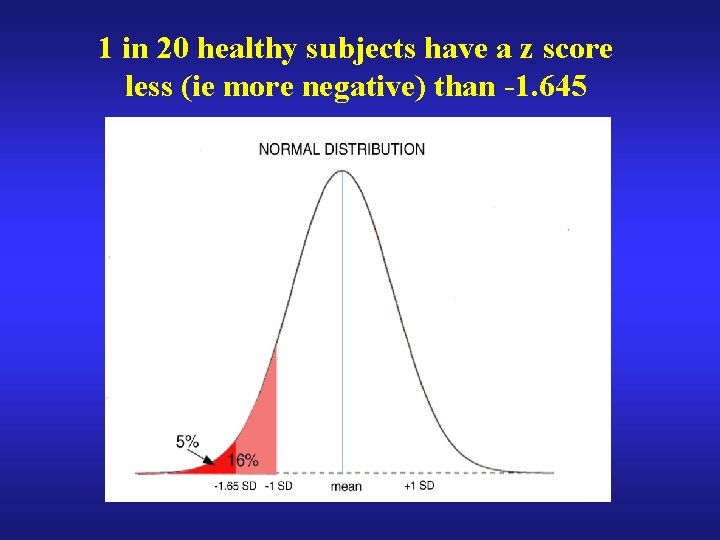
In the healthy population most test results have a normal distribution
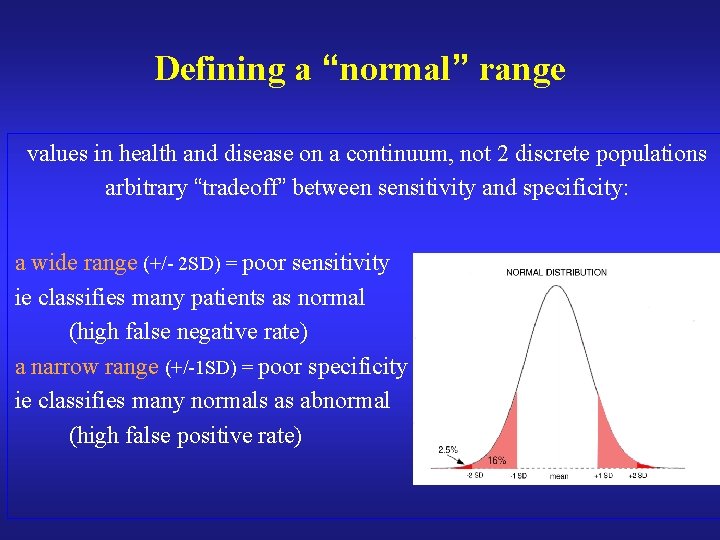
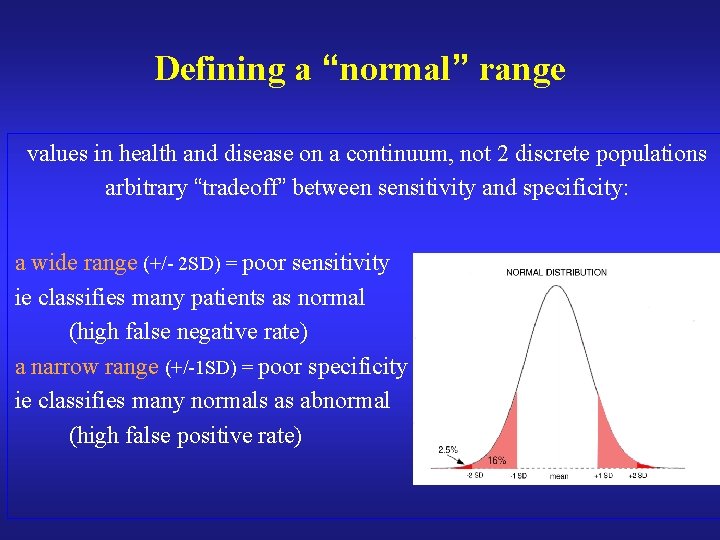
Defining a “normal” range values in health and disease on a continuum, not 2 discrete populations arbitrary “tradeoff” between sensitivity and specificity: a wide range (+/- 2 SD) = poor sensitivity ie classifies many patients as normal (high false negative rate) a narrow range (+/-1 SD) = poor specificity ie classifies many normals as abnormal (high false positive rate)
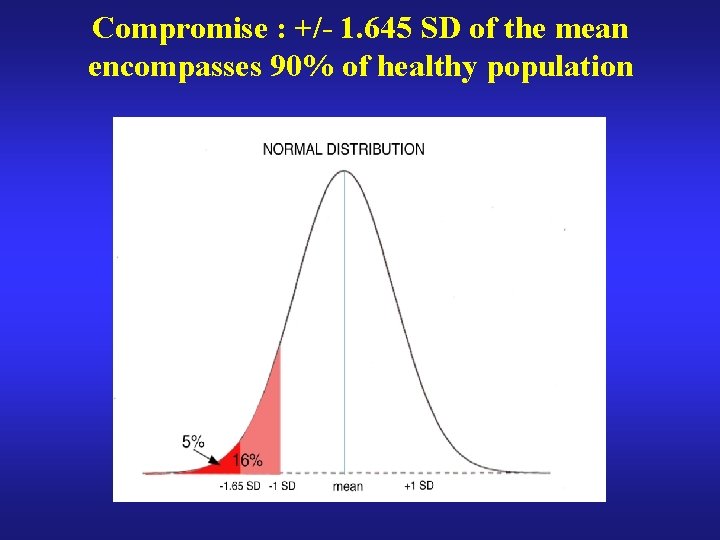
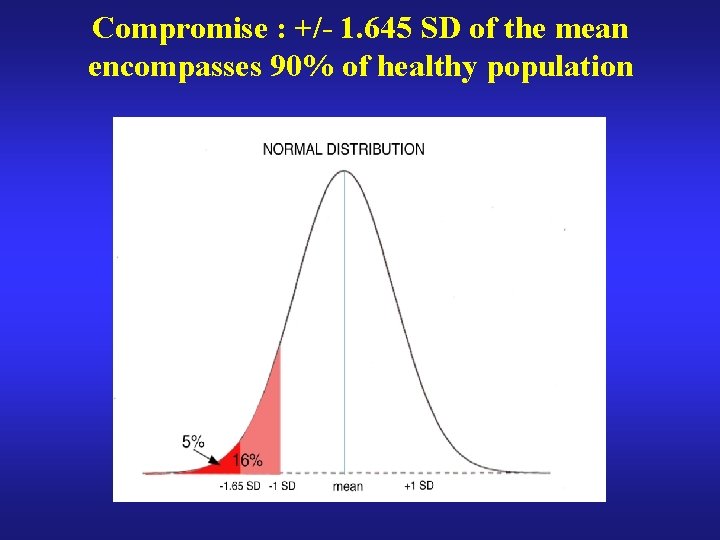
Compromise : +/- 1. 645 SD of the mean encompasses 90% of healthy population
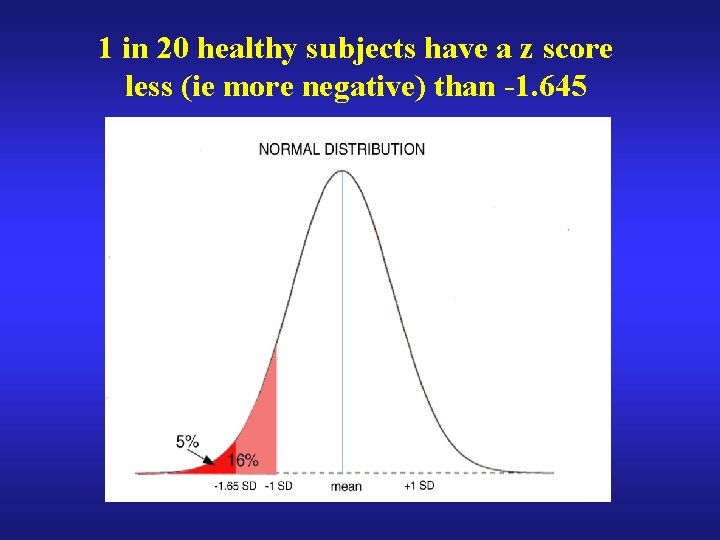
1 in 20 healthy subjects have a z score less (ie more negative) than -1. 645

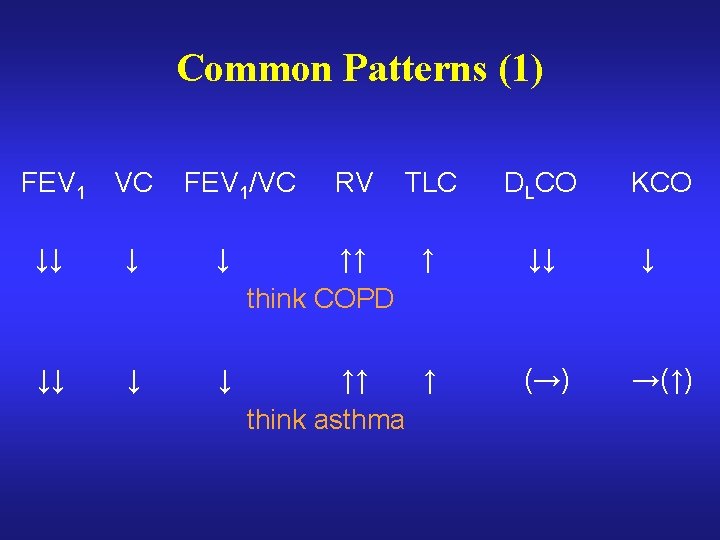
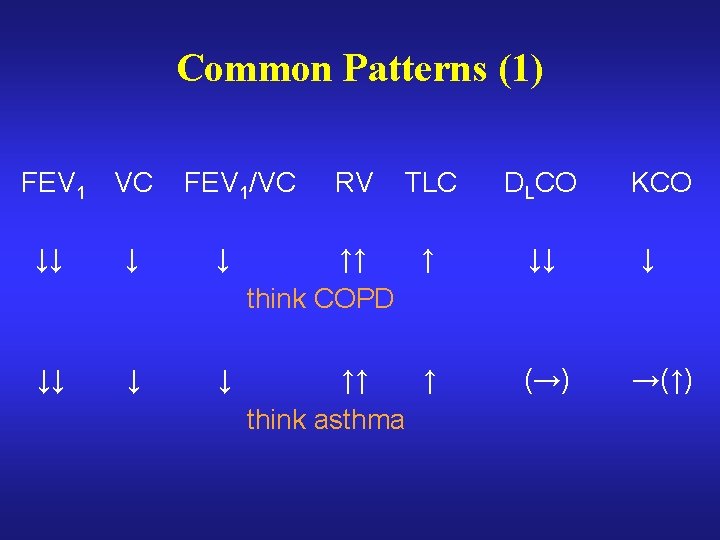
Common Patterns (1) FEV 1 VC FEV 1/VC RV TLC DLCO ↓↓ ↓ ↓ ↑↑ ↑ think COPD ↓↓ ↓↓ ↓ ↓ ↑↑ ↑ think asthma (→) KCO ↓ →(↑)
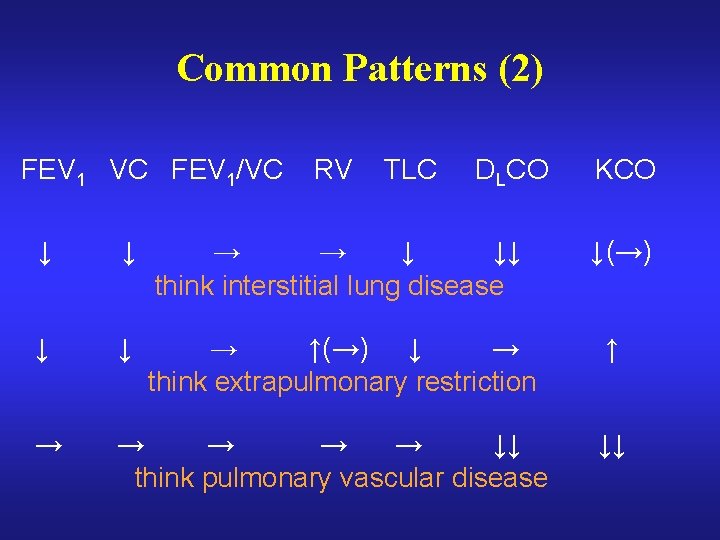
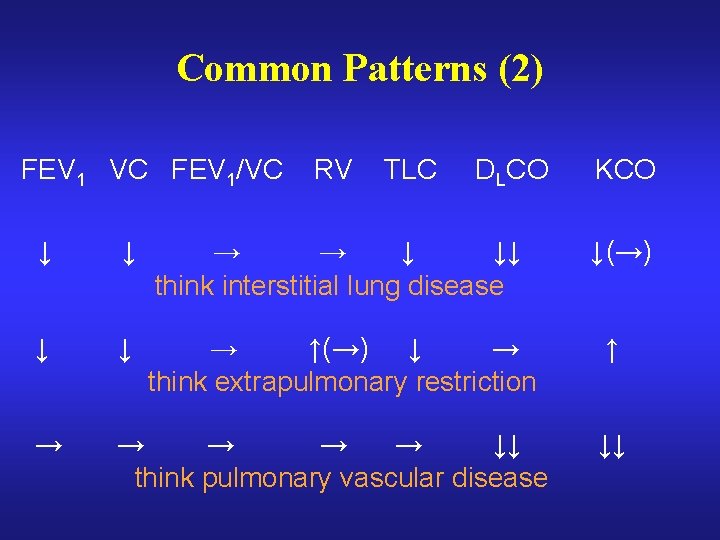
Common Patterns (2) FEV 1 VC FEV 1/VC RV TLC DLCO ↓ ↓ → → ↓ ↓↓ think interstitial lung disease ↓ ↓ → ↑(→) ↓ → think extrapulmonary restriction → → → ↓↓ think pulmonary vascular disease KCO ↓(→) ↑ ↓↓

Common Patterns (3) FEV 1 VC FEV 1/VC ↓↓ ↓ ↓ RV TLC DLCO KCO ↑(→) →(↓) ↓↓ ↓↓ think combined defect eg ILD + COPD