Holes Human Anatomy and Physiology Eleventh Edition Shier







- Slides: 46

Hole’s Human Anatomy and Physiology Eleventh Edition Shier w Butler w Lewis Chapter 22 Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. 1
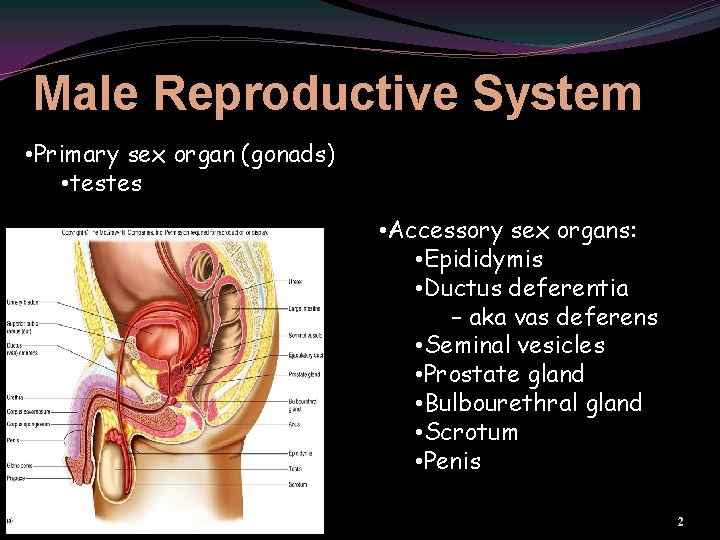
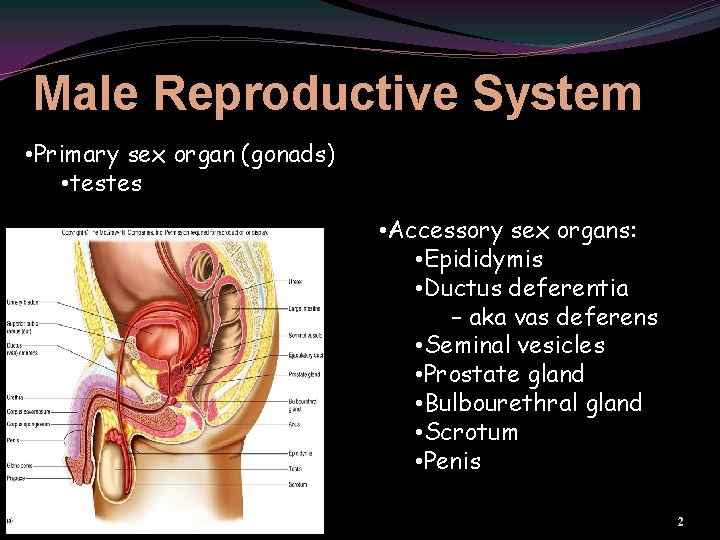
Male Reproductive System • Primary sex organ (gonads) • testes • Accessory sex organs: • Epididymis • Ductus deferentia – aka vas deferens • Seminal vesicles • Prostate gland • Bulbourethral gland • Scrotum • Penis 2
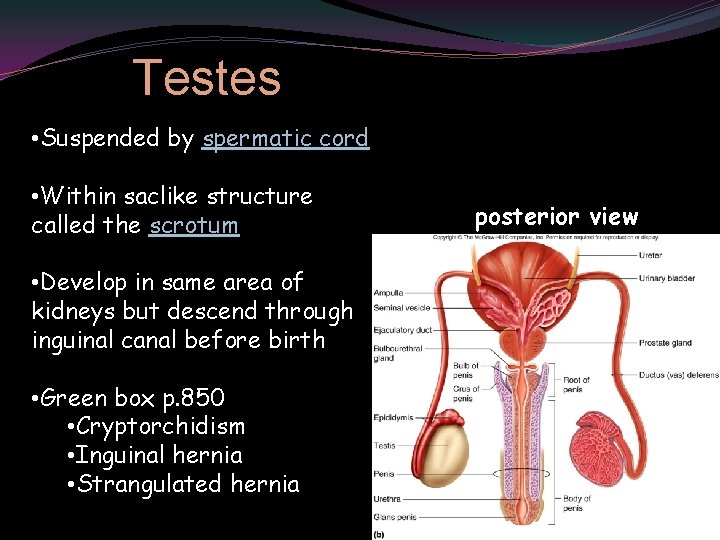
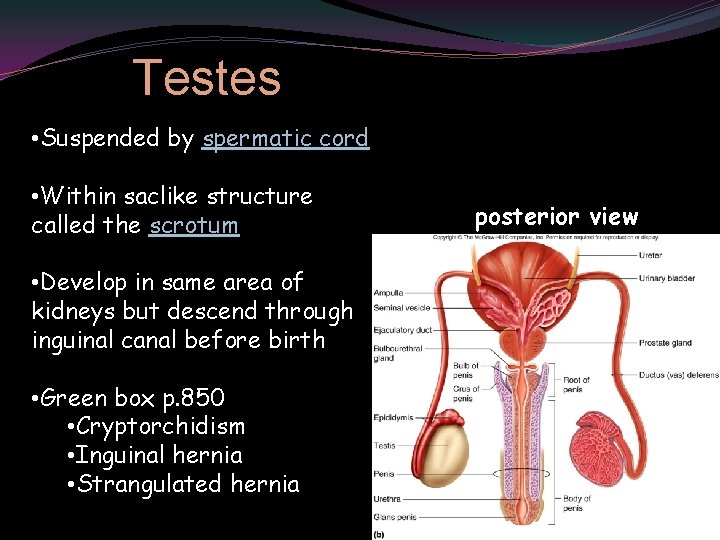
Testes • Suspended by spermatic cord • Within saclike structure called the scrotum posterior view • Develop in same area of kidneys but descend through inguinal canal before birth • Green box p. 850 • Cryptorchidism • Inguinal hernia • Strangulated hernia 3
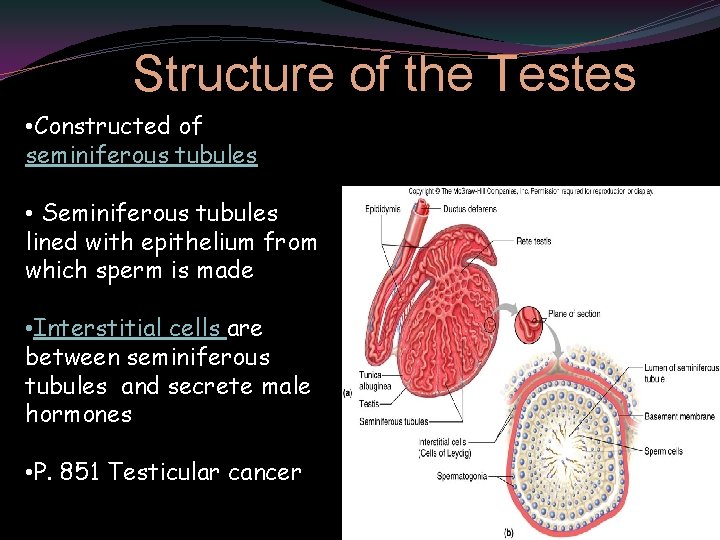
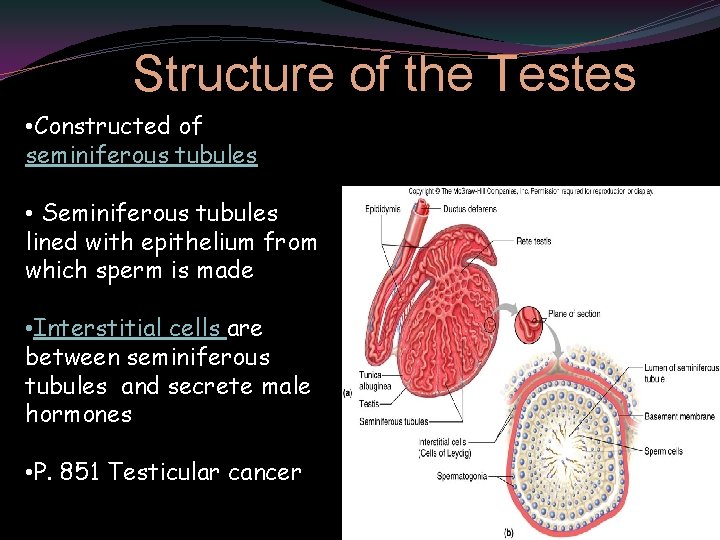
Structure of the Testes • Constructed of seminiferous tubules • Seminiferous tubules lined with epithelium from which sperm is made • Interstitial cells are between seminiferous tubules and secrete male hormones • P. 851 Testicular cancer 4
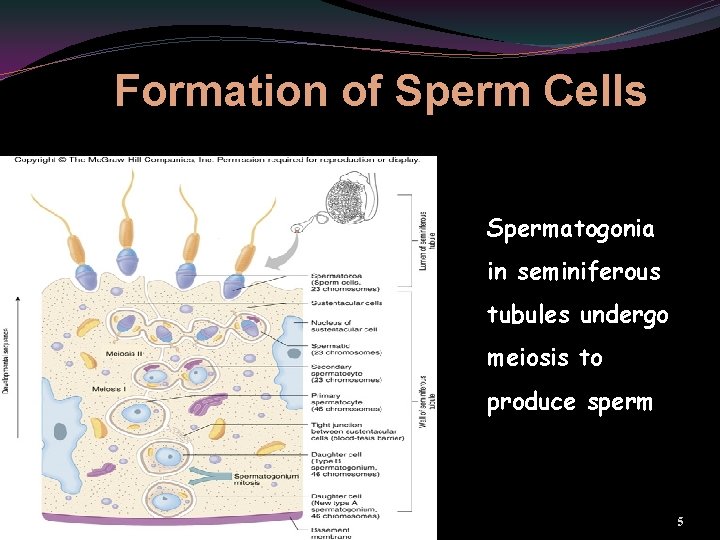
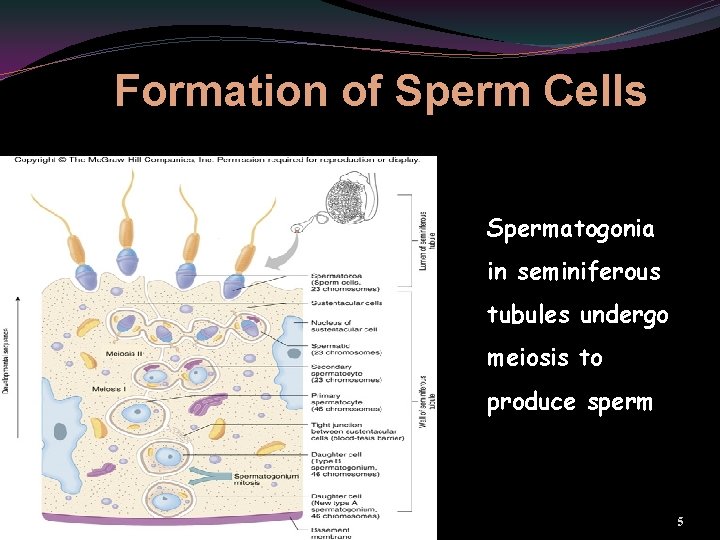
Formation of Sperm Cells Spermatogonia in seminiferous tubules undergo meiosis to produce sperm 5

Spermatogenesis Through meiosis one primary spermatocyte will produce 4 sperm cells. 6
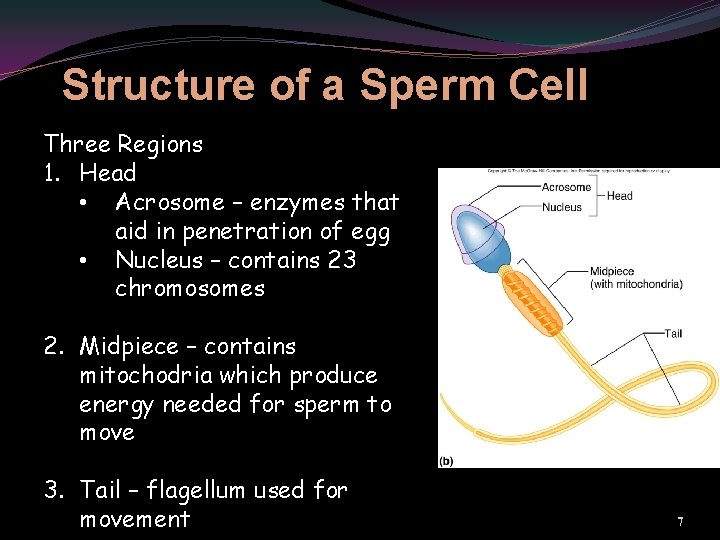
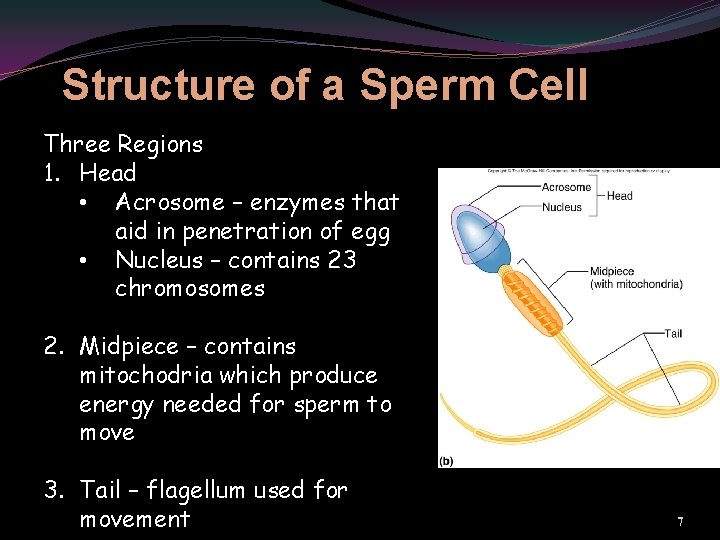
Structure of a Sperm Cell Three Regions 1. Head • Acrosome – enzymes that aid in penetration of egg • Nucleus – contains 23 chromosomes 2. Midpiece – contains mitochodria which produce energy needed for sperm to move 3. Tail – flagellum used for movement 7
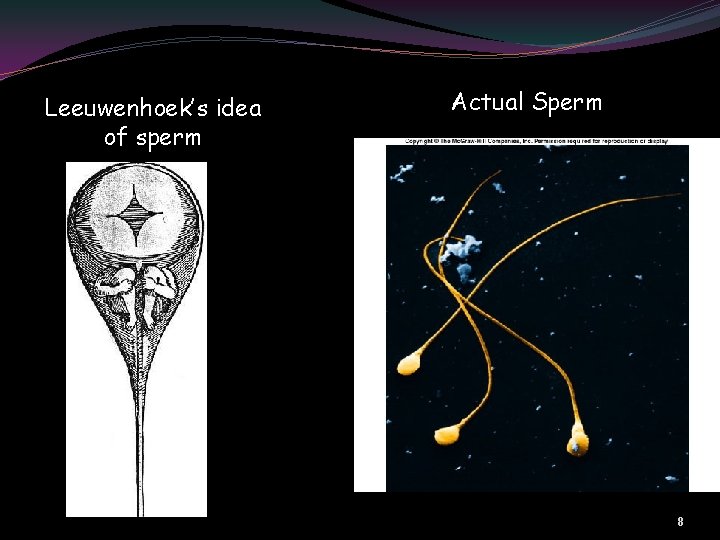
Leeuwenhoek’s idea of sperm Actual Sperm 8
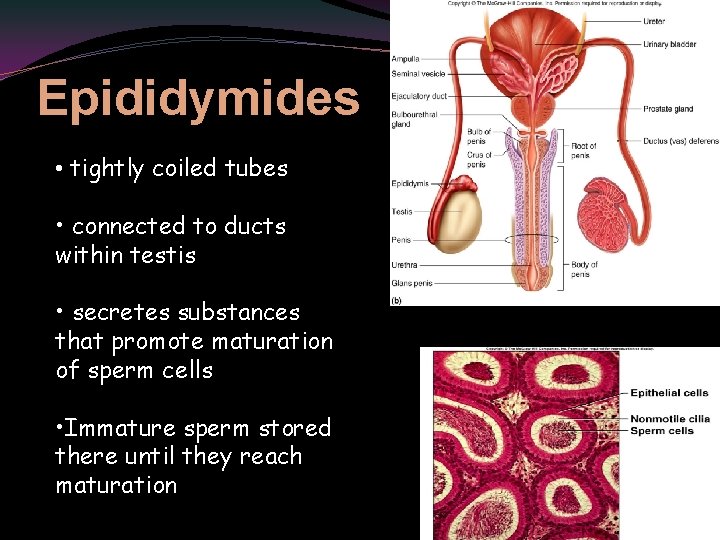
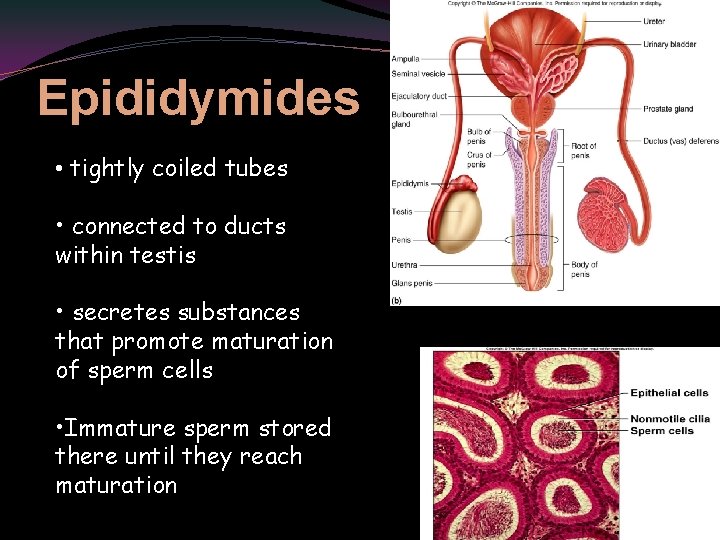
Epididymides • tightly coiled tubes • connected to ducts within testis • secretes substances that promote maturation of sperm cells • Immature sperm stored there until they reach maturation 9
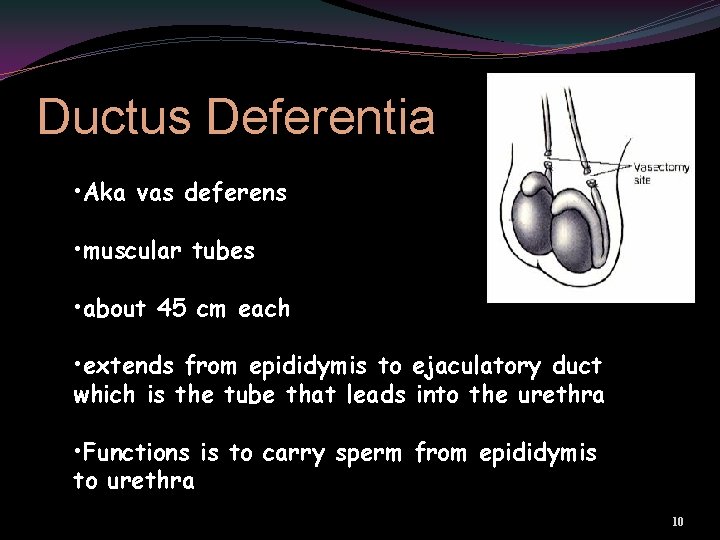
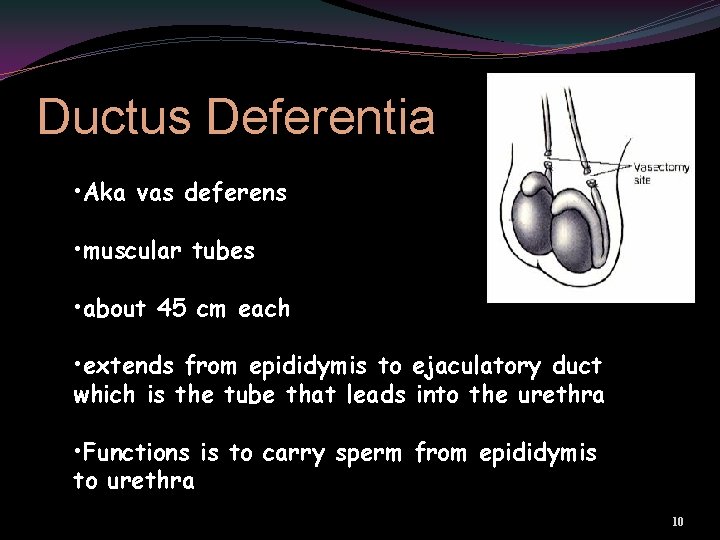
Ductus Deferentia • Aka vas deferens • muscular tubes • about 45 cm each • extends from epididymis to ejaculatory duct which is the tube that leads into the urethra • Functions is to carry sperm from epididymis to urethra 10
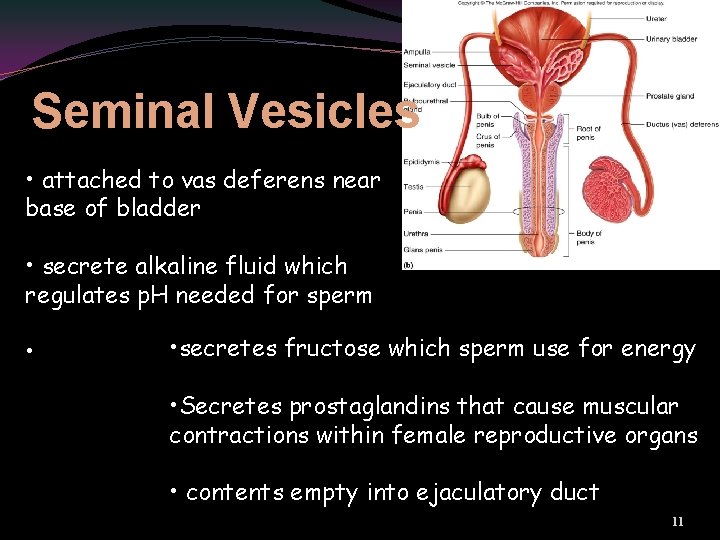
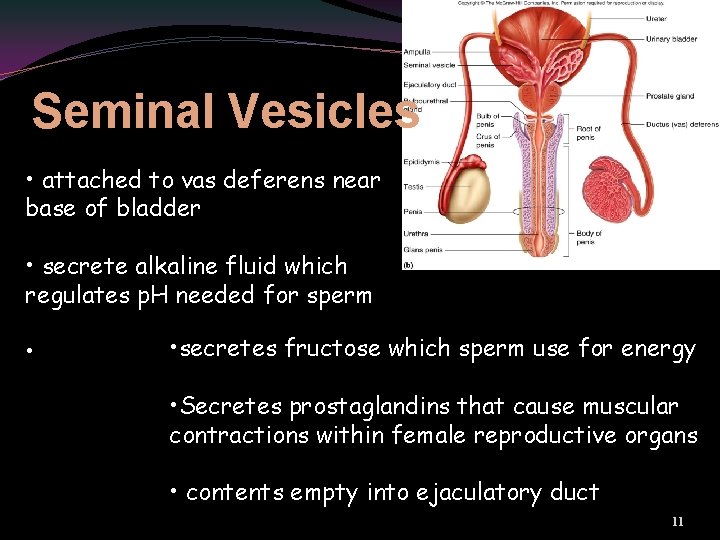
Seminal Vesicles • attached to vas deferens near base of bladder • secrete alkaline fluid which regulates p. H needed for sperm • • secretes fructose which sperm use for energy • Secretes prostaglandins that cause muscular contractions within female reproductive organs • contents empty into ejaculatory duct 11
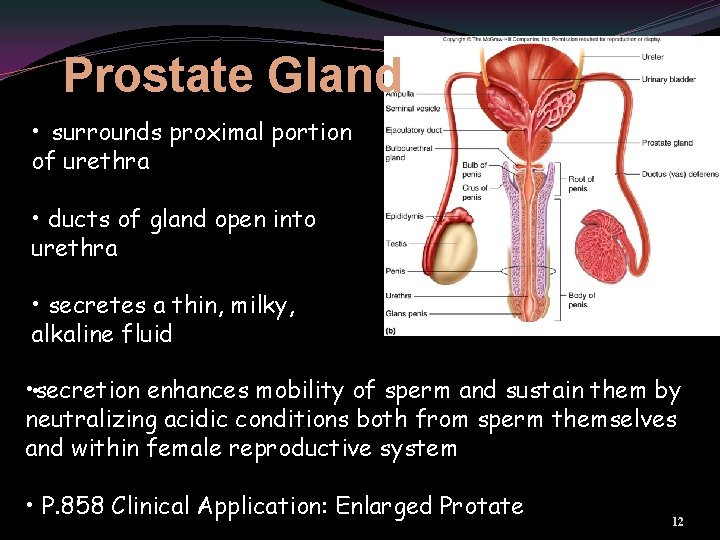
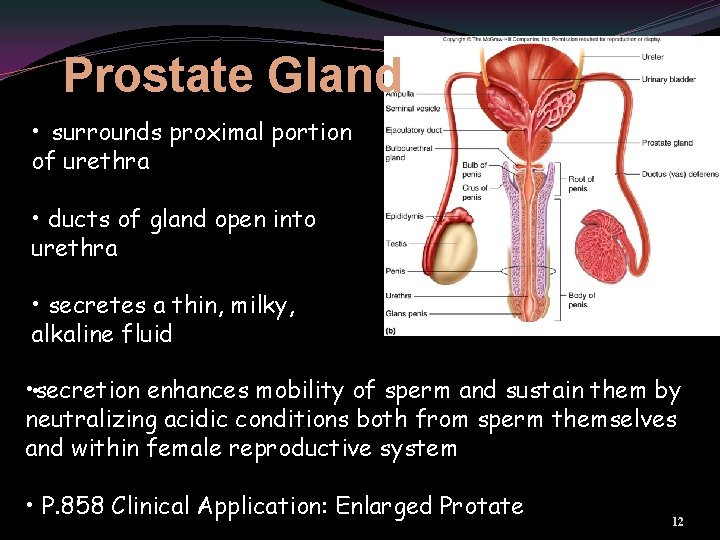
Prostate Gland • surrounds proximal portion of urethra • ducts of gland open into urethra • secretes a thin, milky, alkaline fluid • • secretion enhances mobility of sperm and sustain them by neutralizing acidic conditions both from sperm themselves and within female reproductive system • P. 858 Clinical Application: Enlarged Protate 12

Study links finger length to prostate cancer risk http: //www. msnbc. msn. com/id/40442341/ns/health-cancer/ LONDON — Men with long index fingers have a lower risk of prostate cancer, British scientists said on Wednesday, a finding that could be used to help select those who need regular screening for the disease. More likely Less likely 13
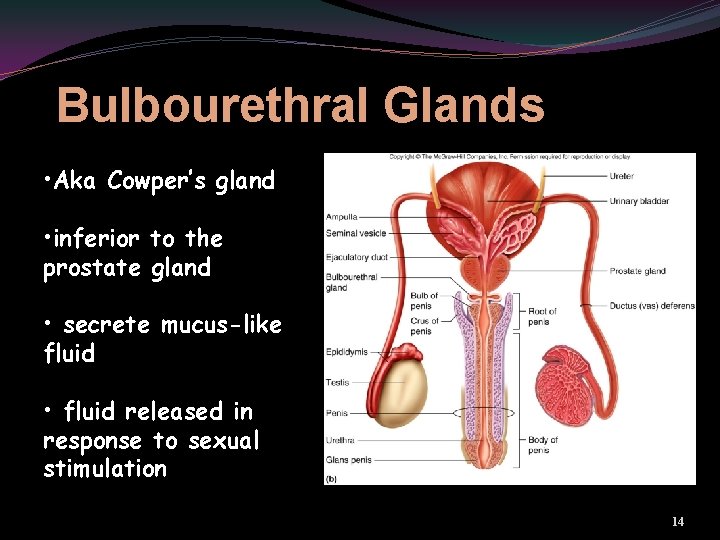
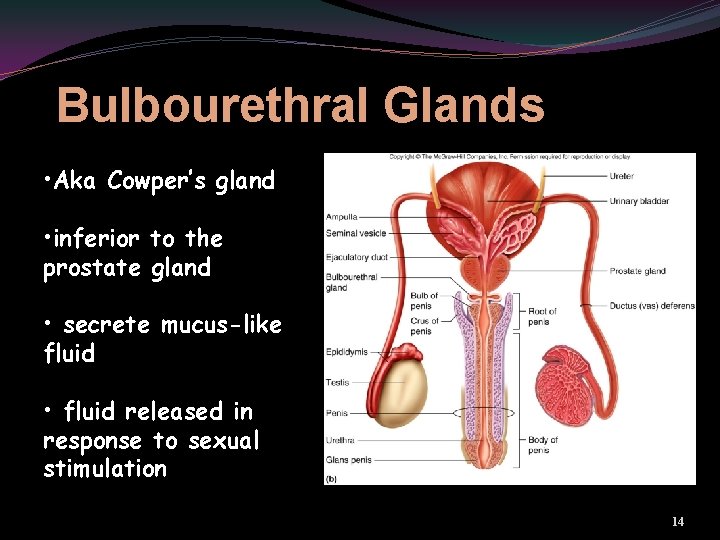
Bulbourethral Glands • Aka Cowper’s gland • inferior to the prostate gland • secrete mucus-like fluid • fluid released in response to sexual stimulation 14
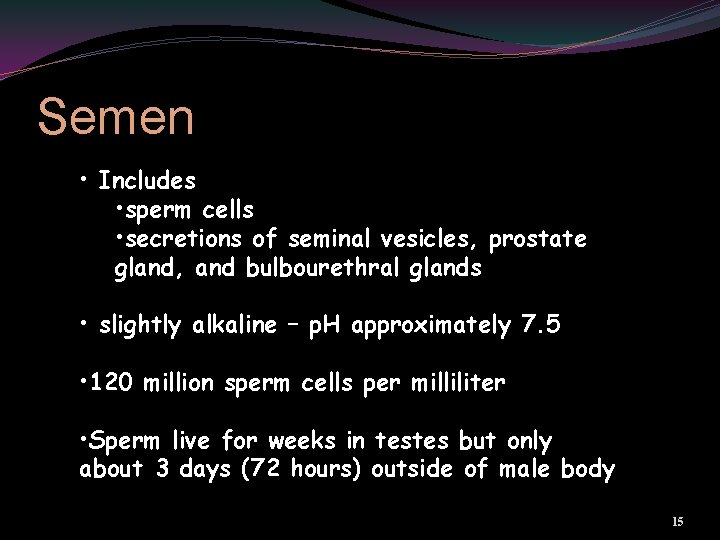
Semen • Includes • sperm cells • secretions of seminal vesicles, prostate gland, and bulbourethral glands • slightly alkaline – p. H approximately 7. 5 • 120 million sperm cells per milliliter • Sperm live for weeks in testes but only about 3 days (72 hours) outside of male body 15
• Scrotum • pouch of skin and subcutaneous tissue • dartos muscle • smooth muscle in subcutaneous tissue • Helps maintain optimal temperature for sperm by moving testes closer or further away from body • medial septum divides scrotum into two chambers • each chamber houses a testis and epididymis 16
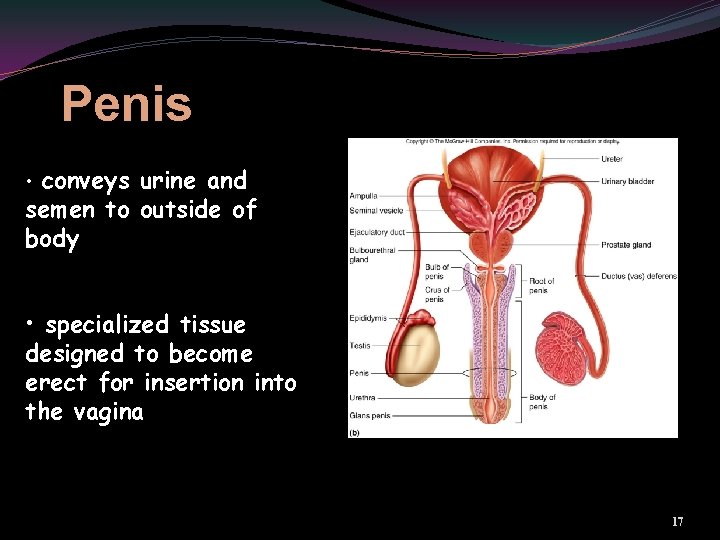
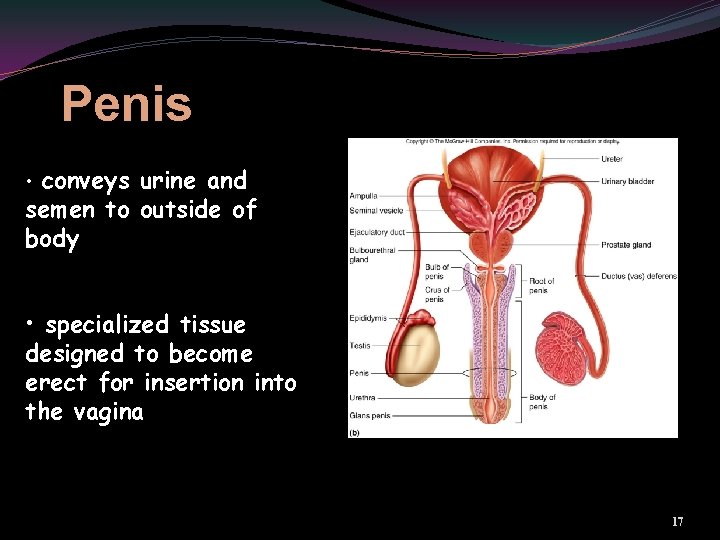
Penis • conveys urine and semen to outside of body • specialized tissue designed to become erect for insertion into the vagina 17
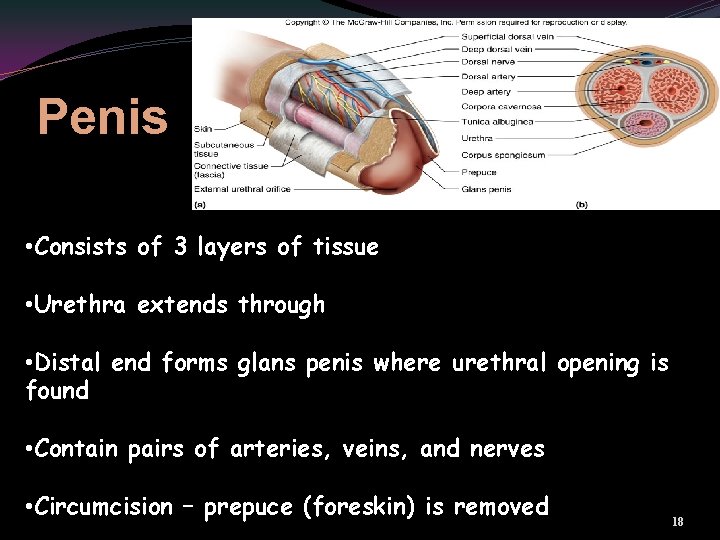
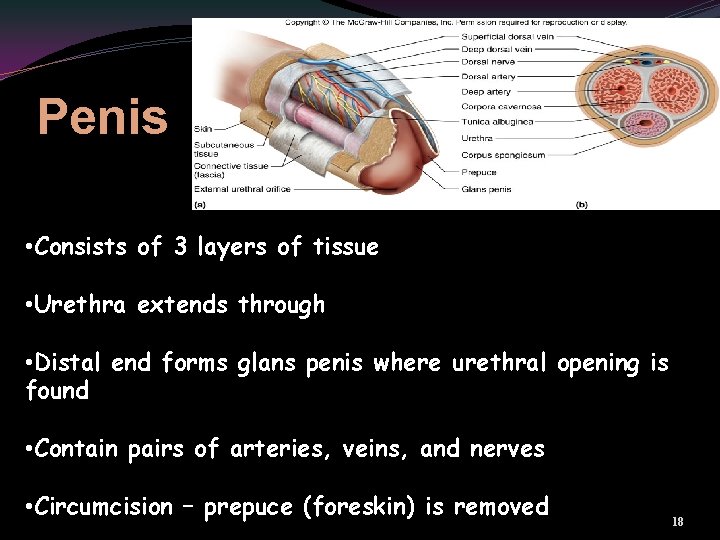
Penis • Consists of 3 layers of tissue • Urethra extends through • Distal end forms glans penis where urethral opening is found • Contain pairs of arteries, veins, and nerves • Circumcision – prepuce (foreskin) is removed 18
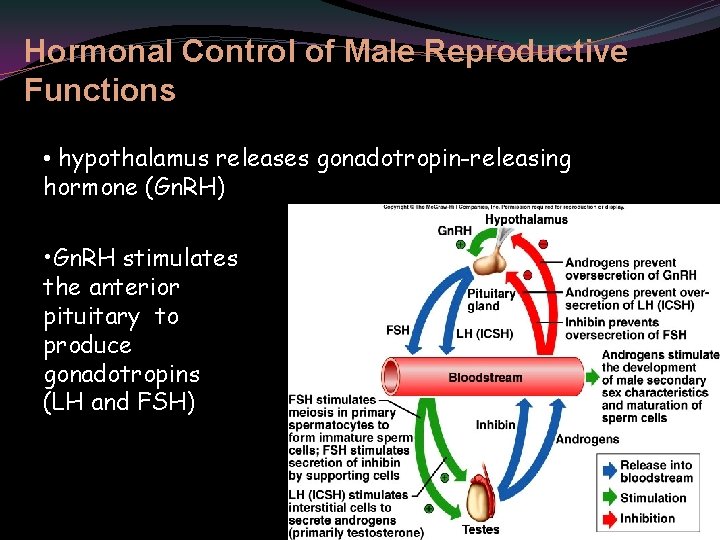
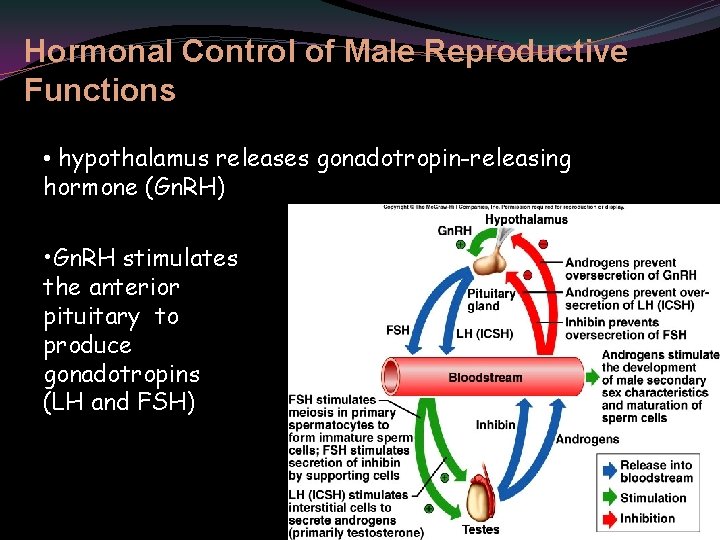
Hormonal Control of Male Reproductive Functions • hypothalamus releases gonadotropin-releasing hormone (Gn. RH) • Gn. RH stimulates the anterior pituitary to produce gonadotropins (LH and FSH) 19
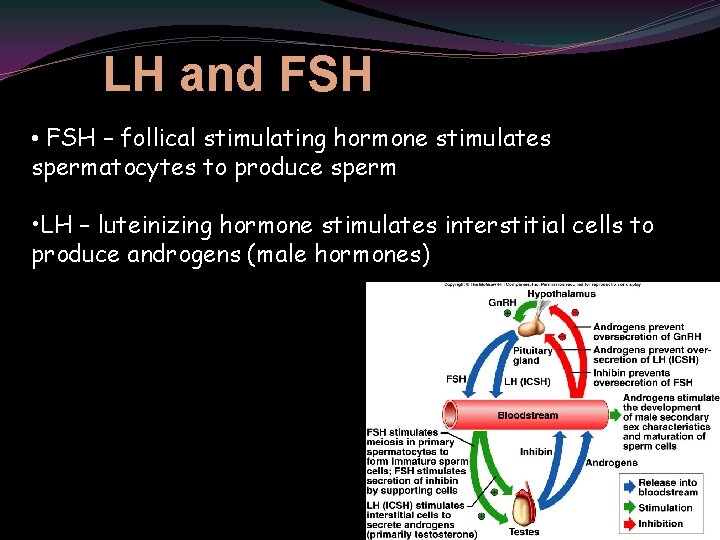
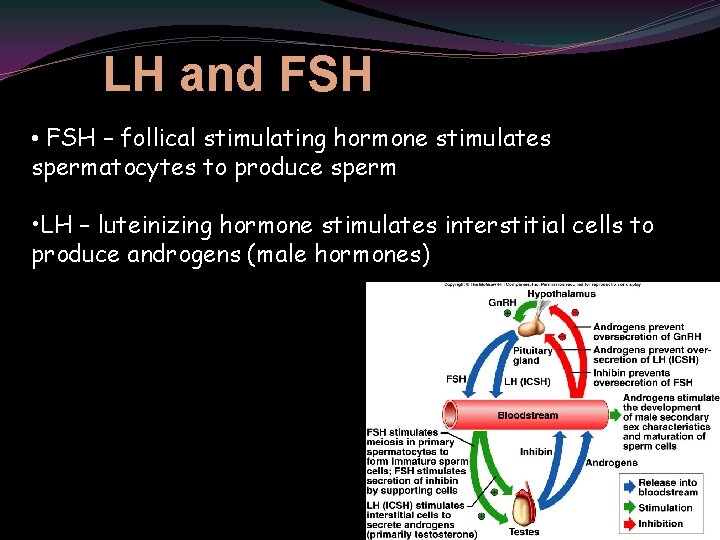
LH and FSH • FSH – follical stimulating hormone stimulates spermatocytes to produce sperm • LH – luteinizing hormone stimulates interstitial cells to produce androgens (male hormones) 20

Actions of Testosterone The androgen testosterone is responsible for secondary sex characteristics. • increased growth of body hair • sometimes decreased growth of scalp hair • enlargement of larynx and thickening of vocal cords • thickening of skin • increased muscular growth • thickening and strengthening of the bones 21
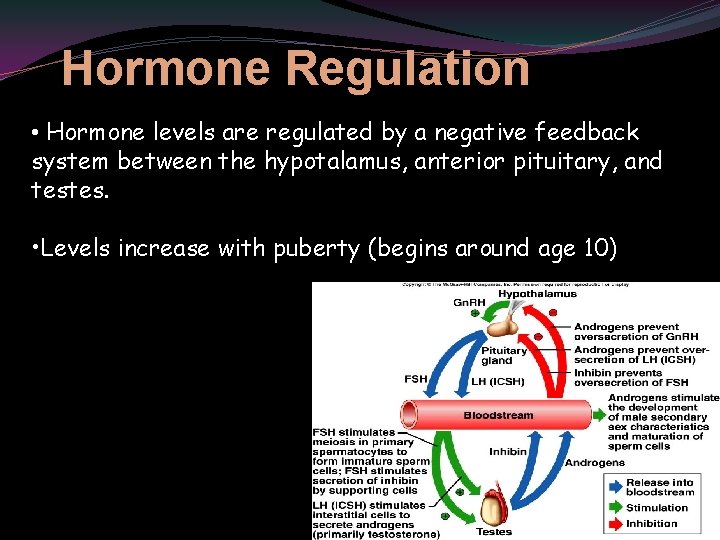
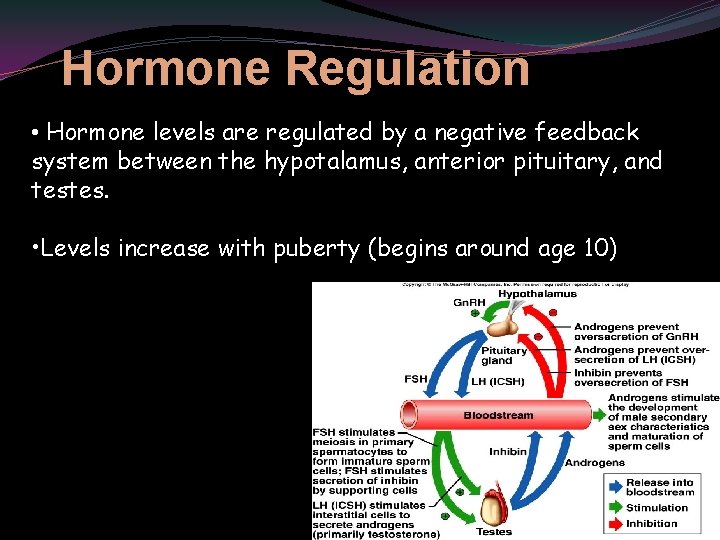
Hormone Regulation • Hormone levels are regulated by a negative feedback system between the hypotalamus, anterior pituitary, and testes. • Levels increase with puberty (begins around age 10) 22
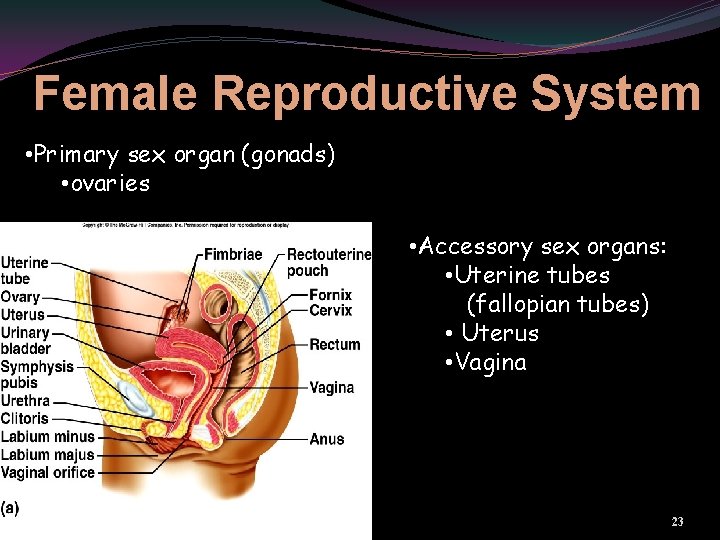
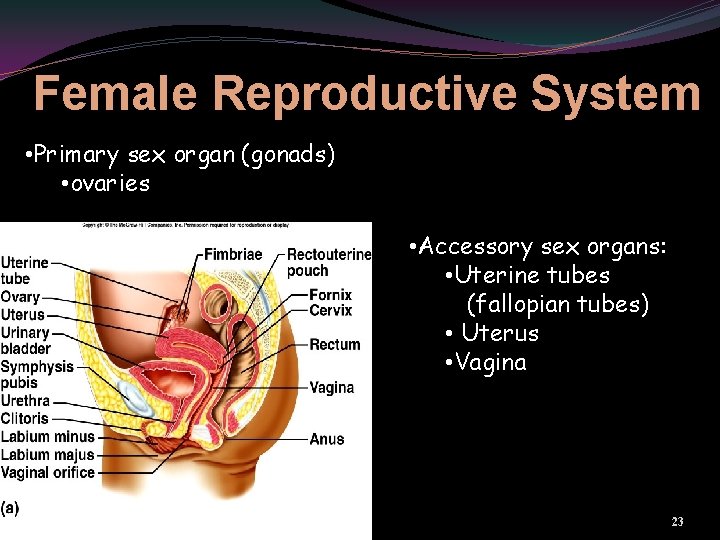
Female Reproductive System • Primary sex organ (gonads) • ovaries • Accessory sex organs: • Uterine tubes (fallopian tubes) • Uterus • Vagina 23
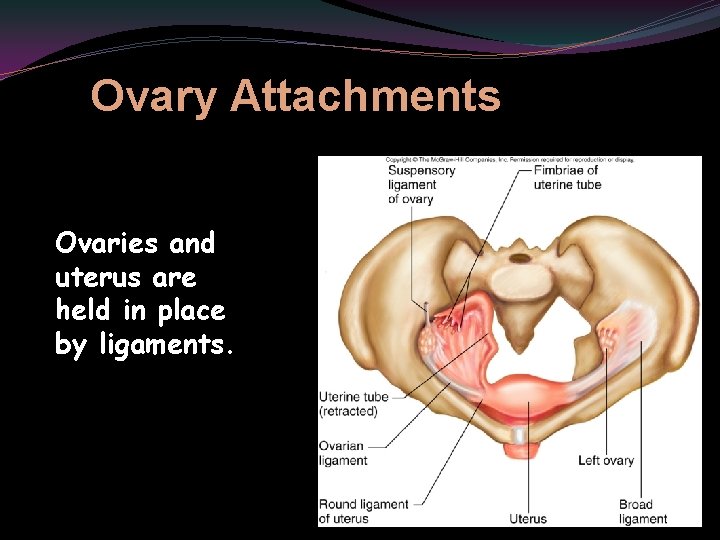
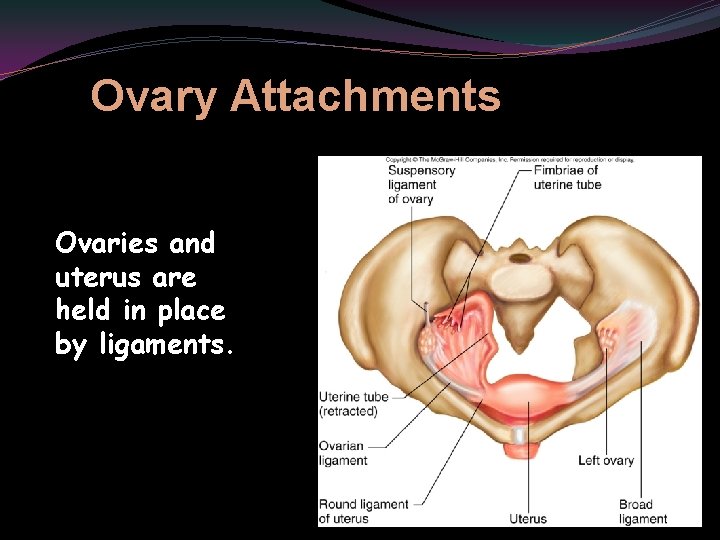
Ovary Attachments Ovaries and uterus are held in place by ligaments. 24
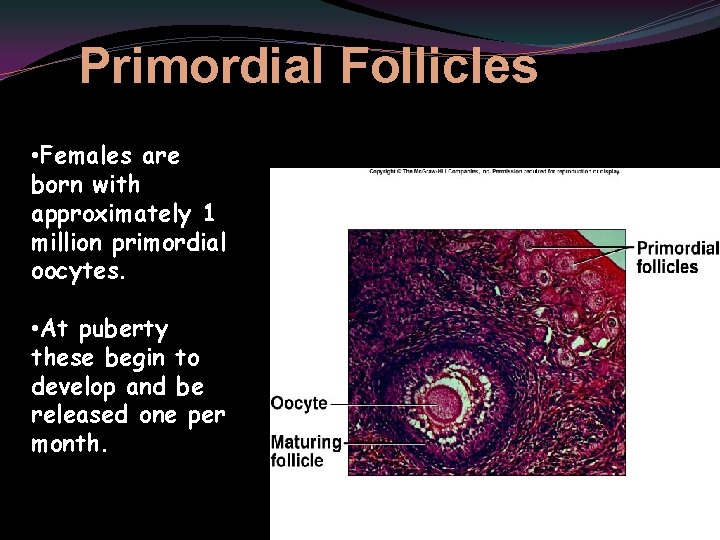
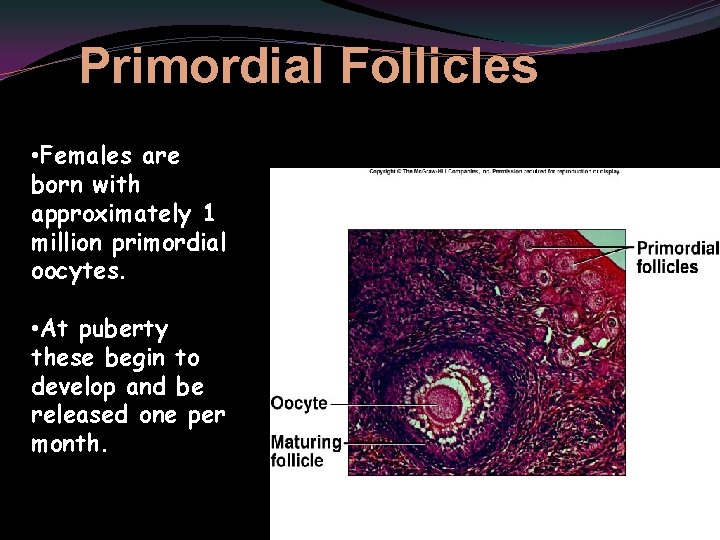
Primordial Follicles • Females are born with approximately 1 million primordial oocytes. • At puberty these begin to develop and be released one per month. 25
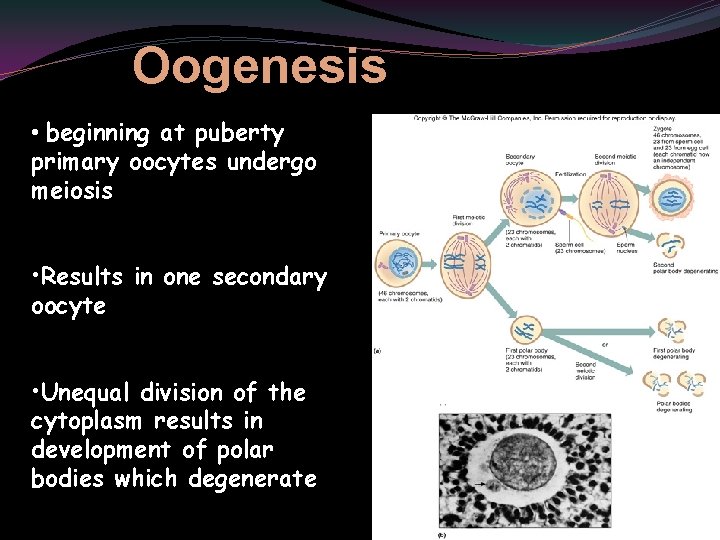
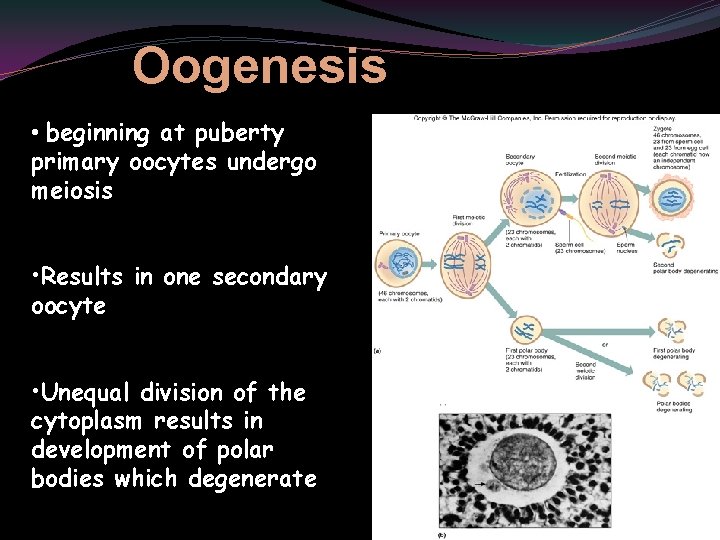
Oogenesis • beginning at puberty primary oocytes undergo meiosis • Results in one secondary oocyte • Unequal division of the cytoplasm results in development of polar bodies which degenerate 26
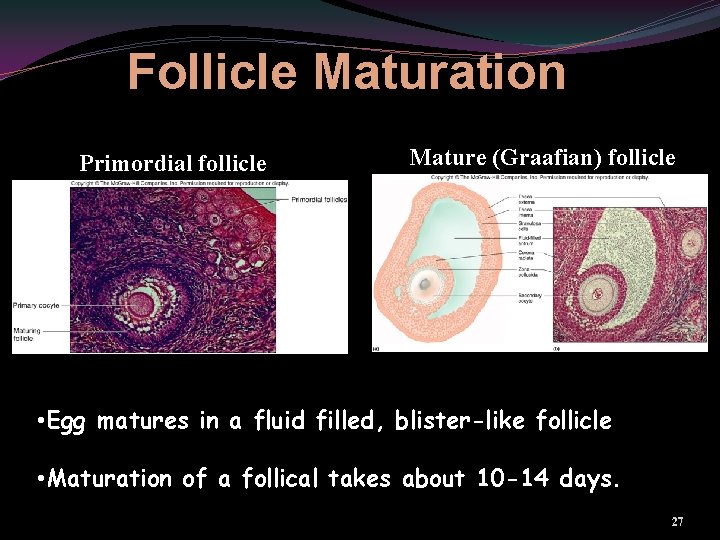
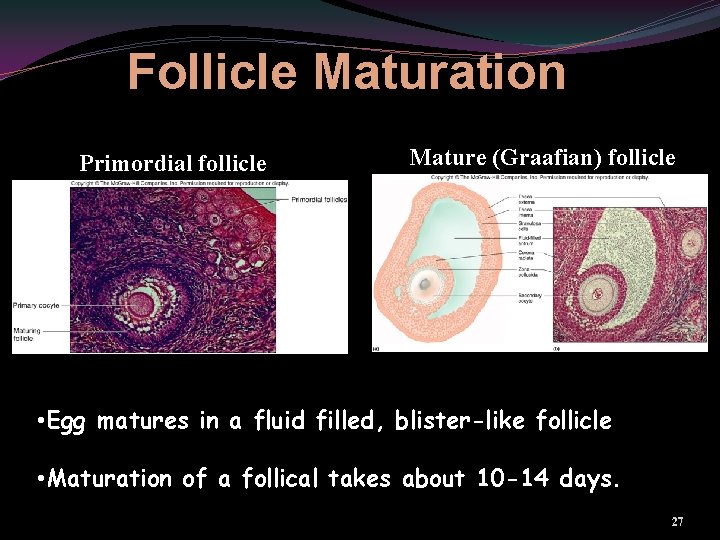
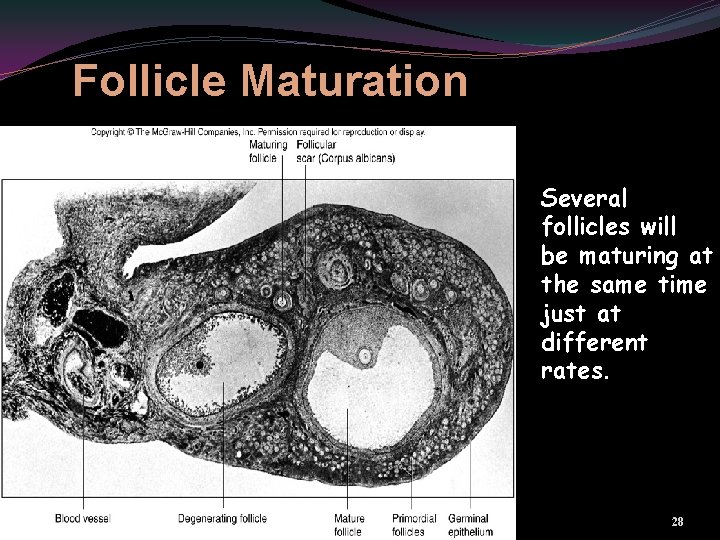
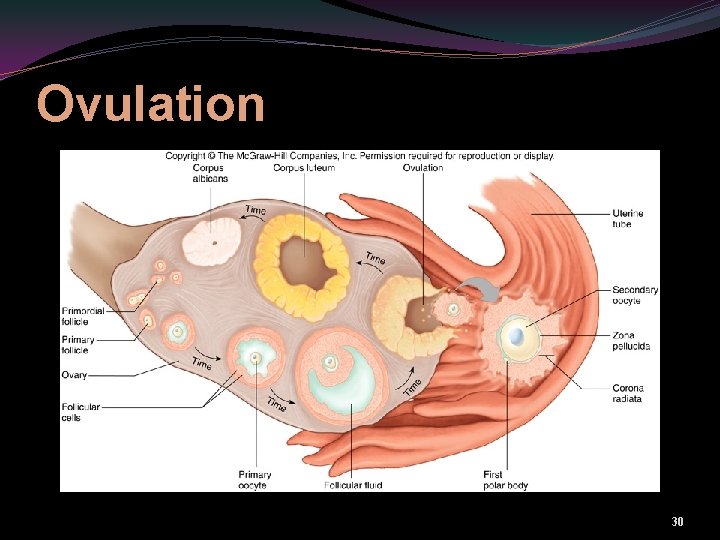
Follicle Maturation Primordial follicle Mature (Graafian) follicle • Egg matures in a fluid filled, blister-like follicle • Maturation of a follical takes about 10 -14 days. 27
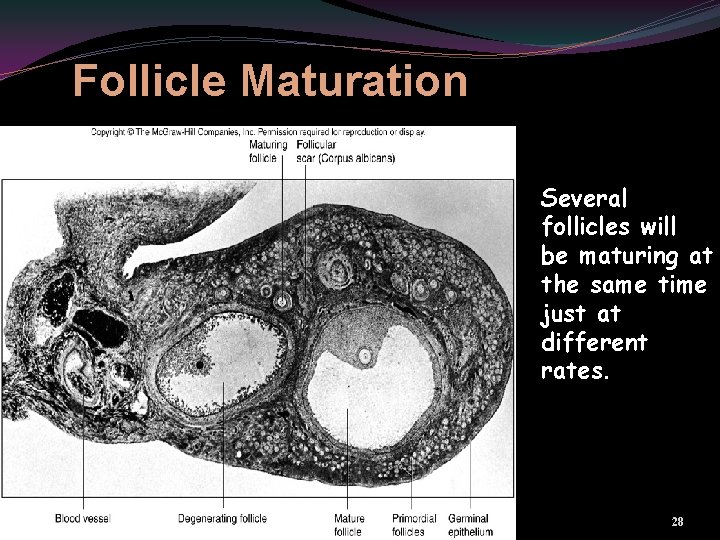
Follicle Maturation Several follicles will be maturing at the same time just at different rates. 28
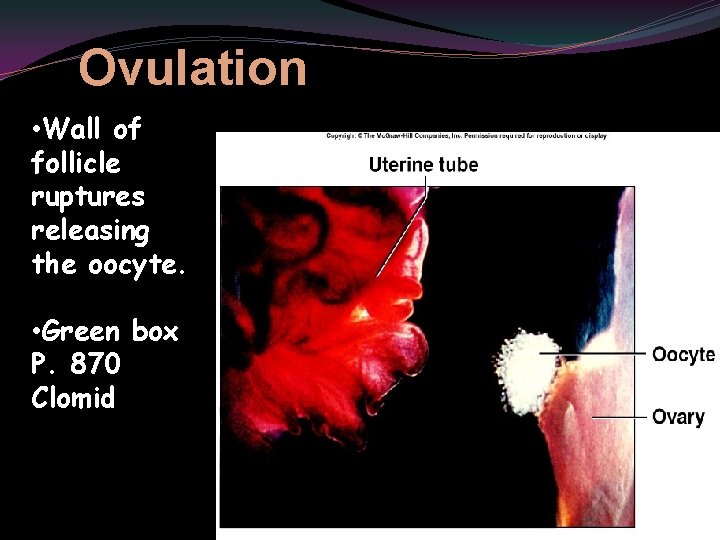
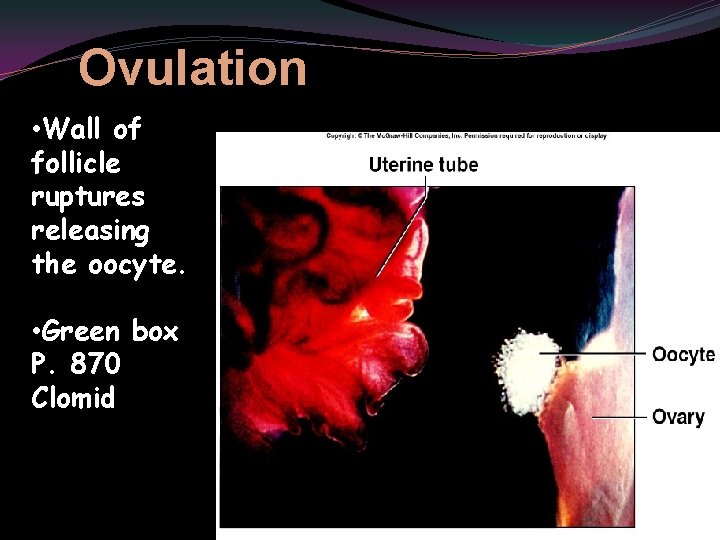
Ovulation • Wall of follicle ruptures releasing the oocyte. • Green box P. 870 Clomid 29
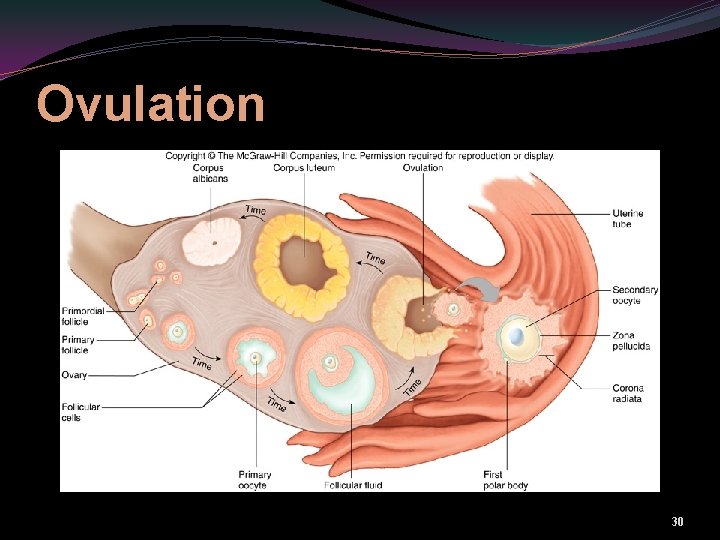
Ovulation 30

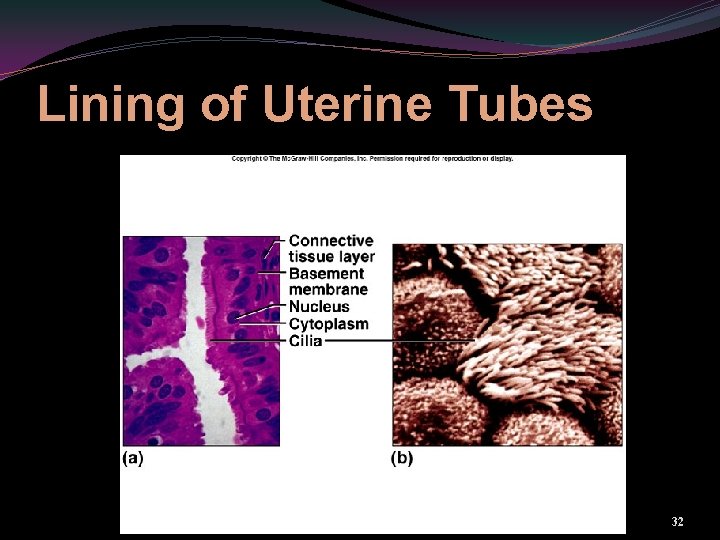
Uterine Tubes aka Fallopian Tubes • About 10 cm long • convey eggs toward the uterus • Fingerlike projections called fimbriae direct egg into tube • Lining has cilia that help move egg downward 31
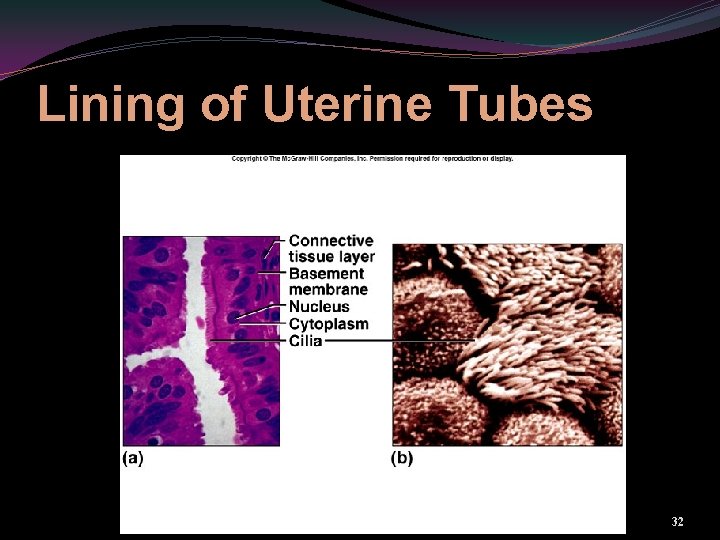
Lining of Uterine Tubes 32
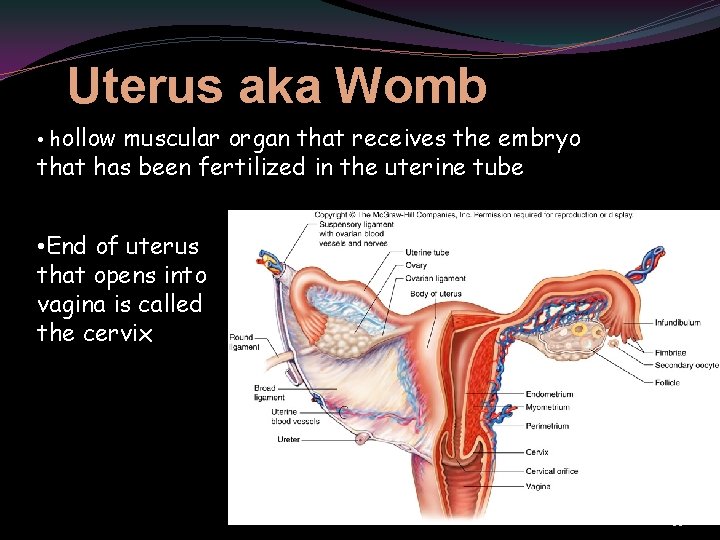
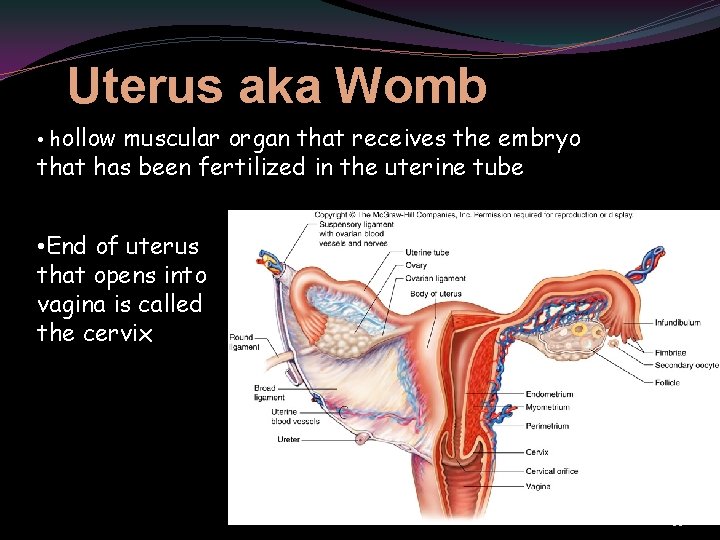
Uterus aka Womb • hollow muscular organ that receives the embryo that has been fertilized in the uterine tube • End of uterus that opens into vagina is called the cervix 33
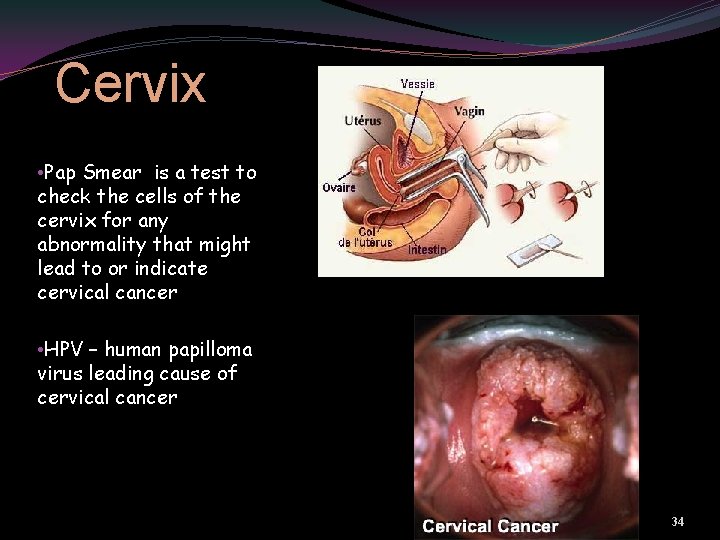
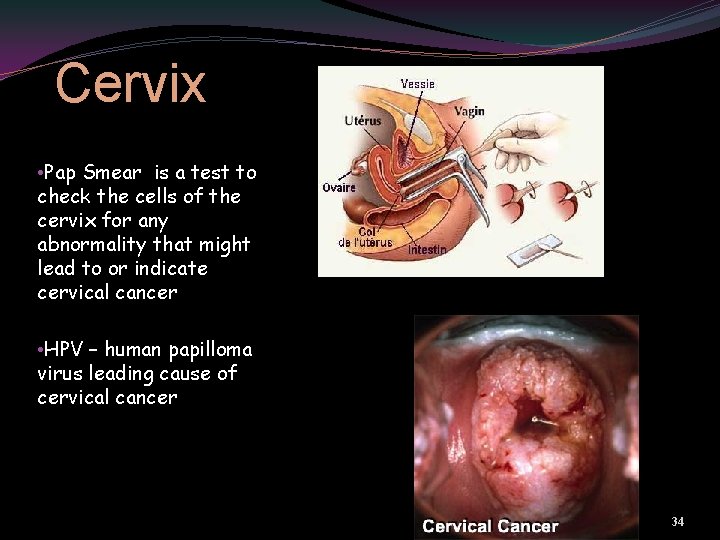
Cervix • Pap Smear is a test to check the cells of the cervix for any abnormality that might lead to or indicate cervical cancer • HPV – human papilloma virus leading cause of cervical cancer 34
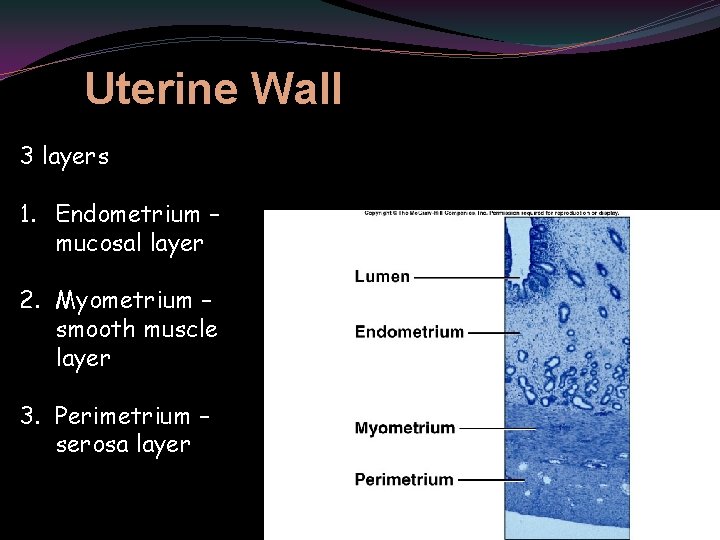
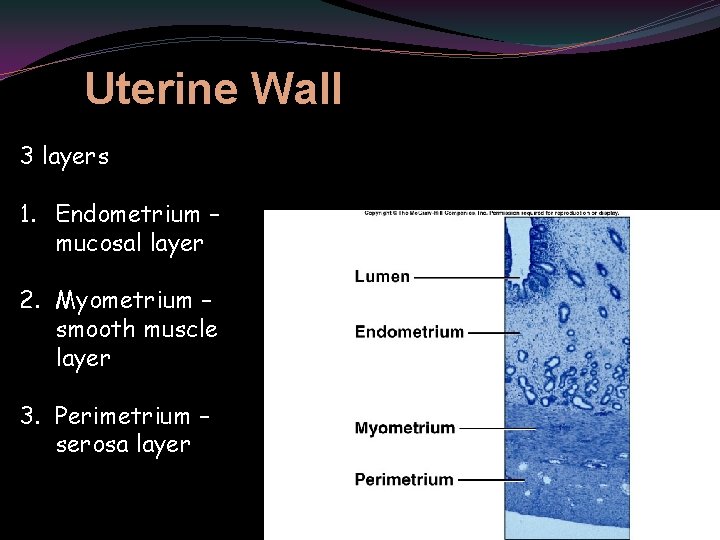
Uterine Wall 3 layers 1. Endometrium – mucosal layer 2. Myometrium – smooth muscle layer 3. Perimetrium – serosa layer 35
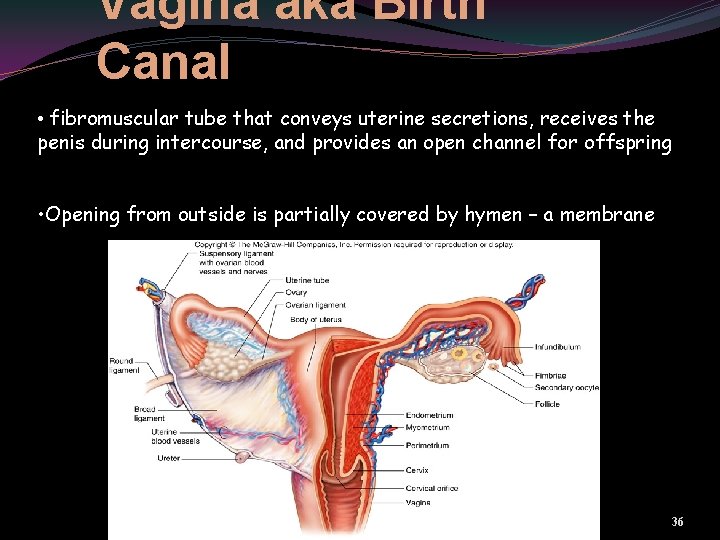
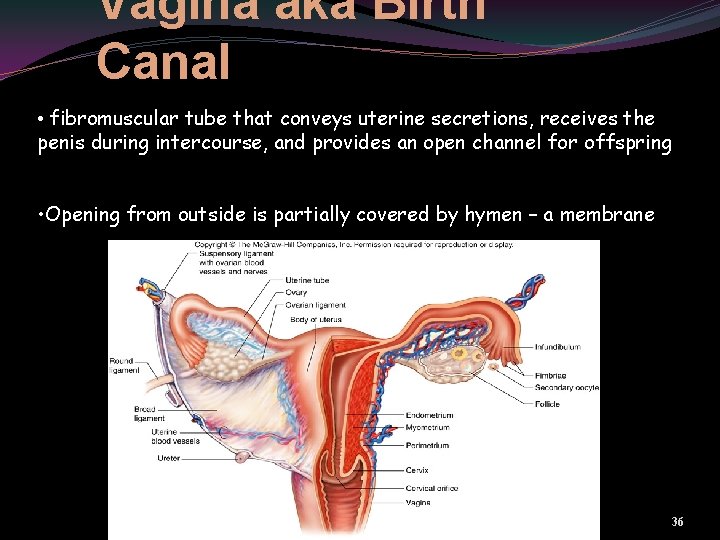
Vagina aka Birth Canal • fibromuscular tube that conveys uterine secretions, receives the penis during intercourse, and provides an open channel for offspring • Opening from outside is partially covered by hymen – a membrane 36
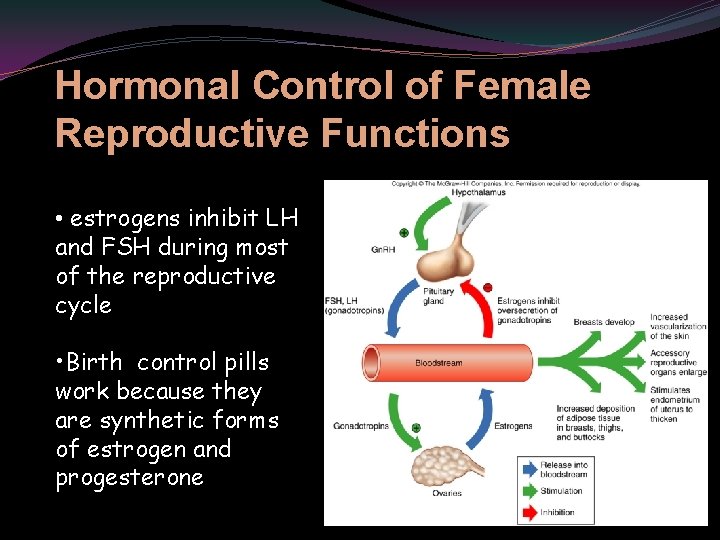
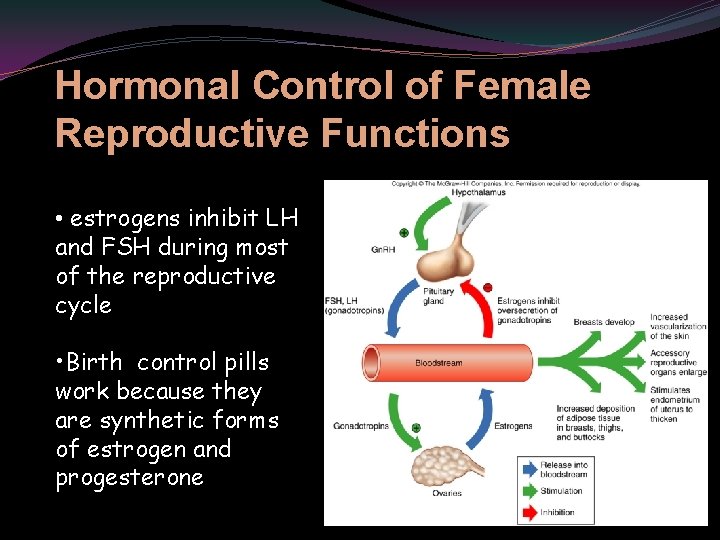
Hormonal Control of Female Reproductive Functions • estrogens inhibit LH and FSH during most of the reproductive cycle • Birth control pills work because they are synthetic forms of estrogen and progesterone 37
Effects of Estrogens • development of breasts and ductile system of the mammary glands • increased adipose tissue in breasts, thighs, and buttocks • increases vascularization of skin • Body hair growth is due to androgens that increase at puberty 38
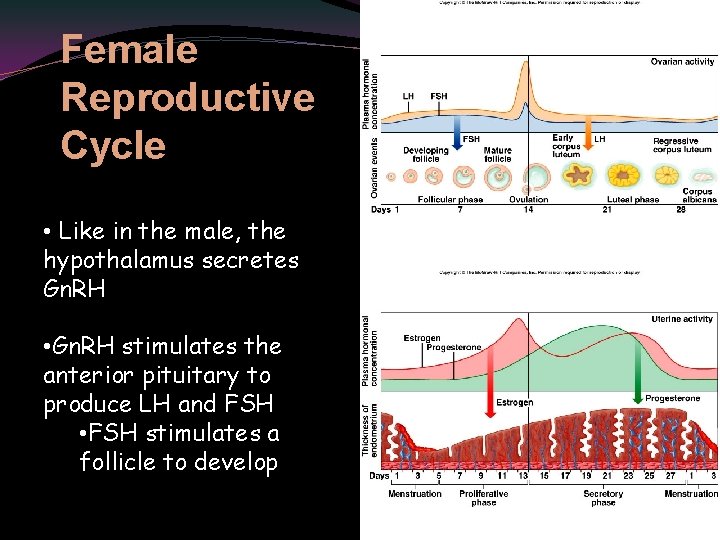
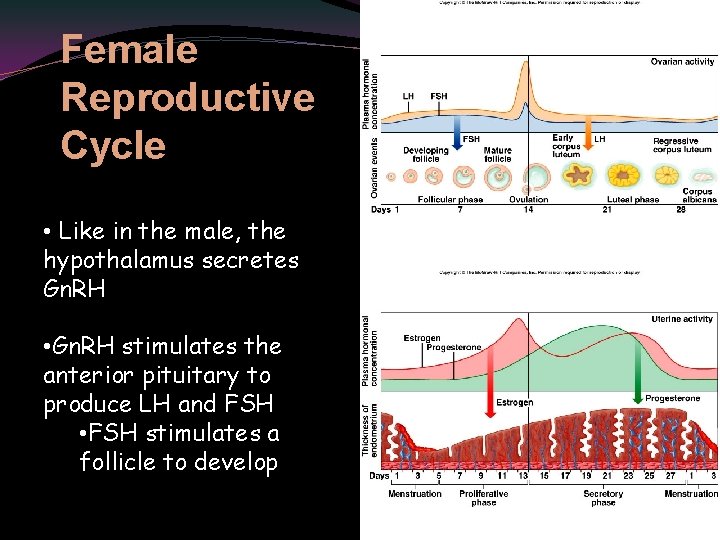
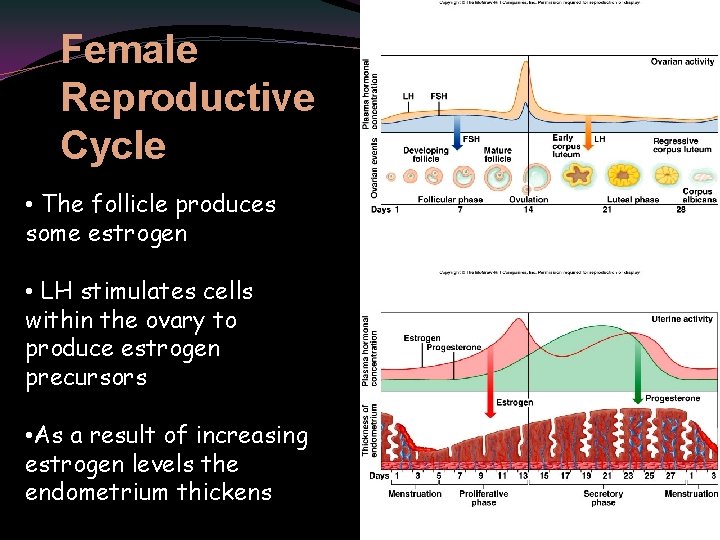
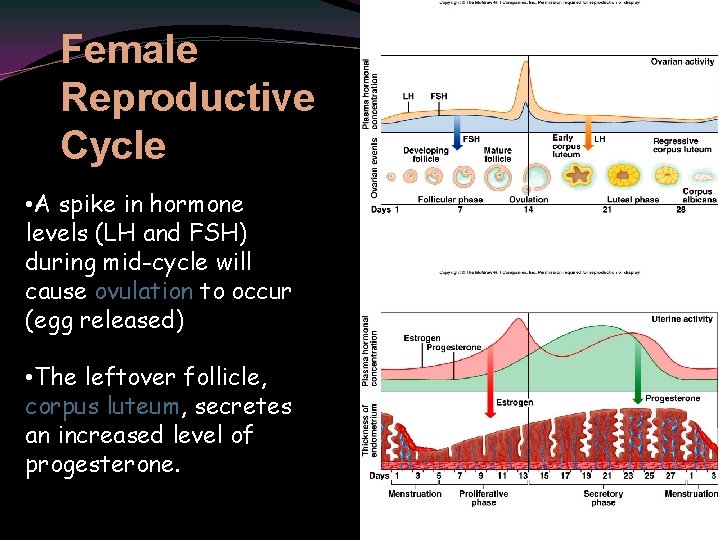
Female Reproductive Cycle • Like in the male, the hypothalamus secretes Gn. RH • Gn. RH stimulates the anterior pituitary to produce LH and FSH • FSH stimulates a follicle to develop 39
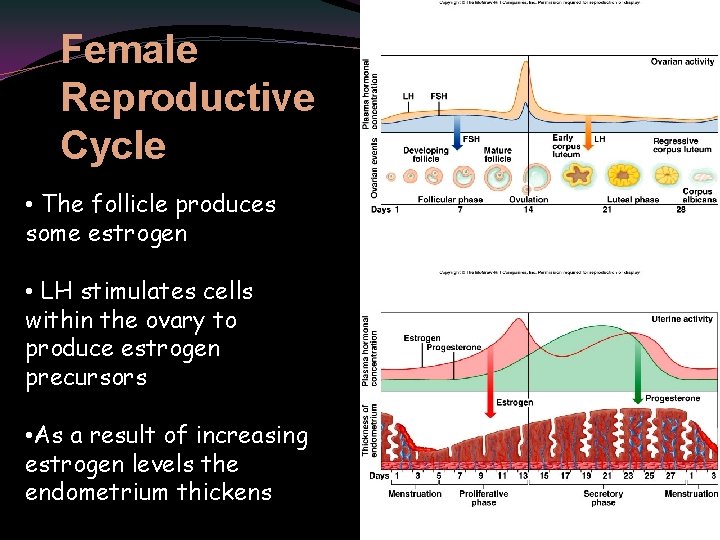
Female Reproductive Cycle • The follicle produces some estrogen • LH stimulates cells within the ovary to produce estrogen precursors • As a result of increasing estrogen levels the endometrium thickens 40
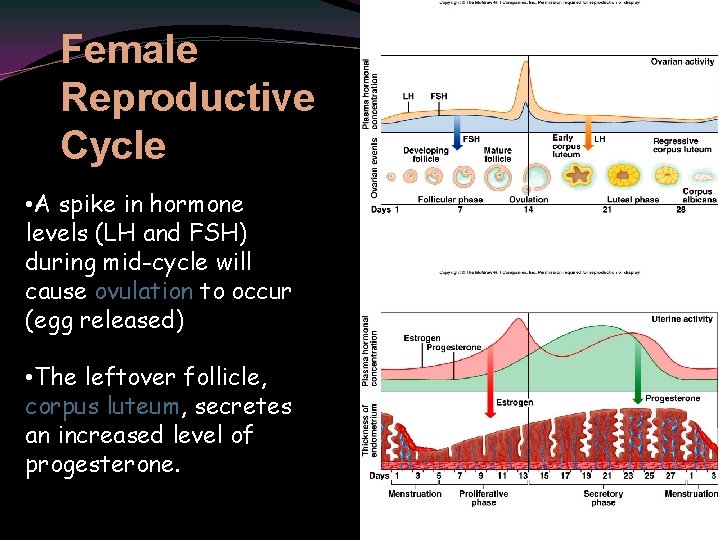
Female Reproductive Cycle • A spike in hormone levels (LH and FSH) during mid-cycle will cause ovulation to occur (egg released) • The leftover follicle, corpus luteum, secretes an increased level of progesterone. 41

Female Reproductive Cycle • Progesterone causes the endometrium to become more vascular. • If pregnancy does NOT occur the corpus luteum dries up and the hormone levels drop drastically • As a result of the drop in hormone levels the endometrium is shed 42
Menopause • usually occurs in late 40 s or early 50 s • reproductive cycles stop • ovaries no longer produce as much estrogens and progesterone • some female secondary sex characteristics may disappear • may produce hot flashes and fatigue • hormone therapy may prevent effects on bone tissue 43
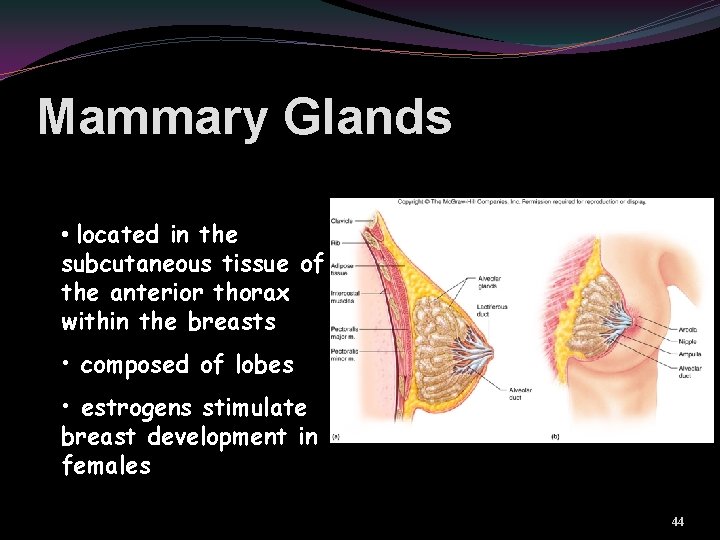
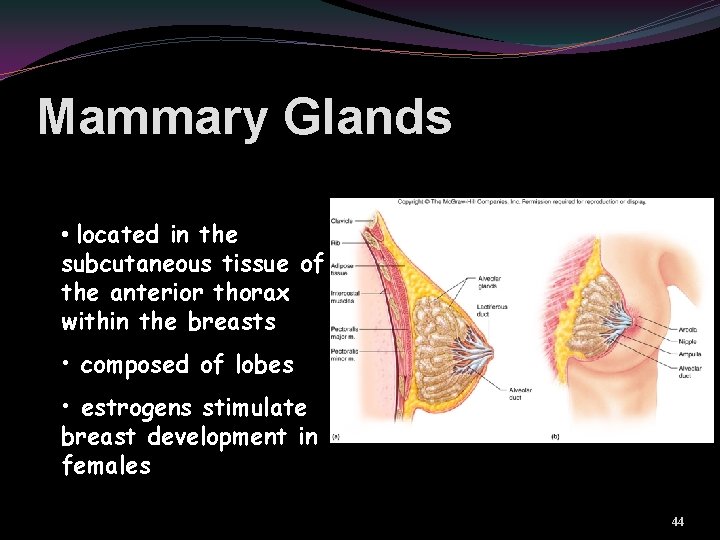
Mammary Glands • located in the subcutaneous tissue of the anterior thorax within the breasts • composed of lobes • estrogens stimulate breast development in females 44
Birth Control • coitus interruptus • rhythm method • mechanical barriers • condom • diaphragm • cervical cap • spermicidal foams or jellies • chemical barriers • spermicides • oral contraceptives • hormonal • injectable contraception • hormonal • intrauterine devices • surgical methods • vasectomy • tubal ligation 45

Surgical Methods of Birth Control Vasectomy Tubal ligation 46
 Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Human anatomy and physiology seventh edition marieb
Human anatomy and physiology seventh edition marieb Uterus perimetrium
Uterus perimetrium Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 Anatomy and physiology ninth edition
Anatomy and physiology ninth edition Management eleventh edition stephen p robbins
Management eleventh edition stephen p robbins Management eleventh edition stephen p robbins
Management eleventh edition stephen p robbins Management eleventh edition
Management eleventh edition Management eleventh edition
Management eleventh edition Waistline
Waistline Medial lateral distal proximal
Medial lateral distal proximal Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Peter shier
Peter shier Criterios de gurd
Criterios de gurd степени сравнения shy
степени сравнения shy Human anatomy fifth edition
Human anatomy fifth edition Human anatomy fifth edition
Human anatomy fifth edition Physiology of sport and exercise 5th edition
Physiology of sport and exercise 5th edition Eleventh 5 year plan
Eleventh 5 year plan Eleventh 5 year plan
Eleventh 5 year plan Thfive
Thfive For his eleventh birthday elvis presley
For his eleventh birthday elvis presley Lower respiratory structures
Lower respiratory structures Tattoo anatomy and physiology
Tattoo anatomy and physiology Anatomy science olympiad
Anatomy science olympiad Crown plants examples
Crown plants examples Anatomy and physiology of bone
Anatomy and physiology of bone Anatomy of peptic ulcer
Anatomy of peptic ulcer Cantlie line
Cantlie line Epigastric region
Epigastric region Iliac regions
Iliac regions Red blood cells anatomy and physiology
Red blood cells anatomy and physiology Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology Http://anatomy and physiology
Http://anatomy and physiology Physiology of appendix
Physiology of appendix Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomy and physiology of swine
Anatomy and physiology of swine Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition Science olympiad anatomy and physiology 2020 cheat sheet
Science olympiad anatomy and physiology 2020 cheat sheet Chapter 2 basic chemistry anatomy and physiology
Chapter 2 basic chemistry anatomy and physiology Stomach anatomy corpus
Stomach anatomy corpus Pancreas anatomy and physiology
Pancreas anatomy and physiology Chapter 7 anatomy and physiology
Chapter 7 anatomy and physiology Chapter 14 the digestive system and body metabolism
Chapter 14 the digestive system and body metabolism