HCC Capture NC HFMA Presentation Roadmap HCC Defined
- Slides: 27
HCC Capture NC HFMA
Presentation Roadmap • HCC Defined • Professional Coding Team • Provider Engagement & Partnership with Coding Team • Workflow and Technology • Measuring Results 2
HCC Defined 3
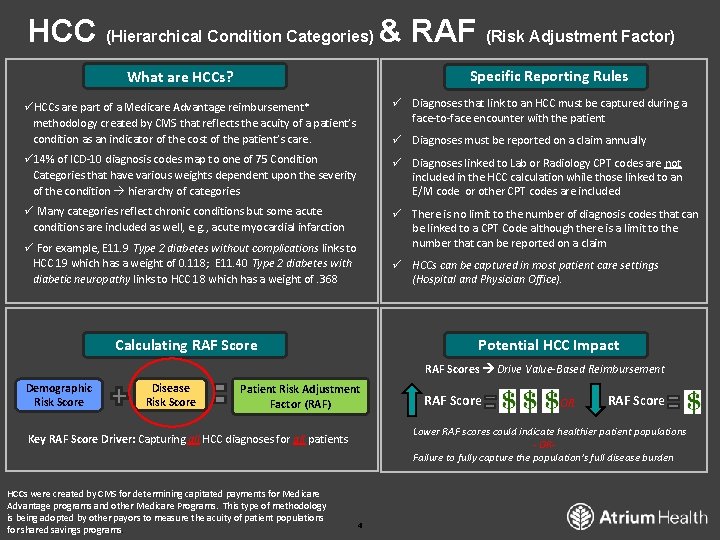
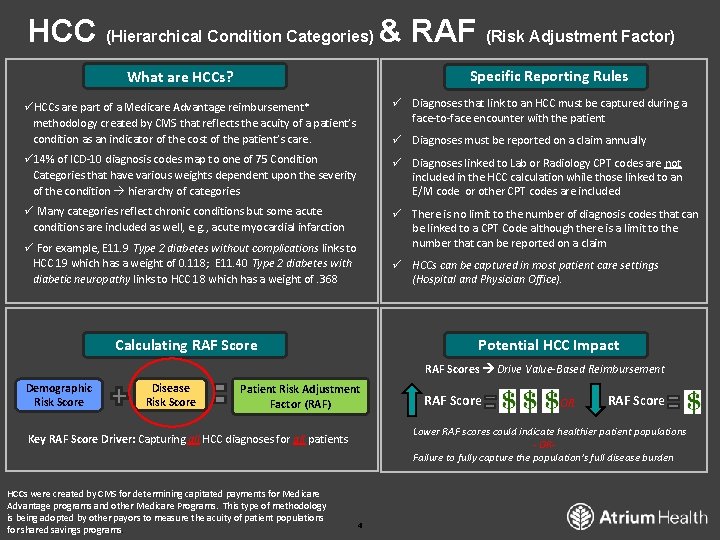
HCC (Hierarchical Condition Categories) & RAF (Risk Adjustment Factor) Specific Reporting Rules What are HCCs? üHCCs are part of a Medicare Advantage reimbursement* methodology created by CMS that reflects the acuity of a patient’s condition as an indicator of the cost of the patient’s care. ü Diagnoses that link to an HCC must be captured during a face-to-face encounter with the patient ü 14% of ICD-10 diagnosis codes map to one of 75 Condition Categories that have various weights dependent upon the severity of the condition hierarchy of categories ü Diagnoses linked to Lab or Radiology CPT codes are not included in the HCC calculation while those linked to an E/M code or other CPT codes are included ü Many categories reflect chronic conditions but some acute conditions are included as well, e. g. , acute myocardial infarction ü There is no limit to the number of diagnosis codes that can be linked to a CPT Code although there is a limit to the number that can be reported on a claim ü Diagnoses must be reported on a claim annually ü For example, E 11. 9 Type 2 diabetes without complications links to HCC 19 which has a weight of 0. 118; E 11. 40 Type 2 diabetes with diabetic neuropathy links to HCC 18 which has a weight of. 368 ü HCCs can be captured in most patient care settings (Hospital and Physician Office). Calculating RAF Score Potential HCC Impact RAF Scores Drive Value-Based Reimbursement Demographic Risk Score Disease Risk Score Patient Risk Adjustment Factor (RAF) OR RAF Score Lower RAF scores could indicate healthier patient populations - ORFailure to fully capture the population’s full disease burden Key RAF Score Driver: Capturing all HCC diagnoses for all patients HCCs were created by CMS for determining capitated payments for Medicare Advantage programs and other Medicare Programs. This type of methodology is being adopted by other payors to measure the acuity of patient populations for shared savings programs. RAF Score 4
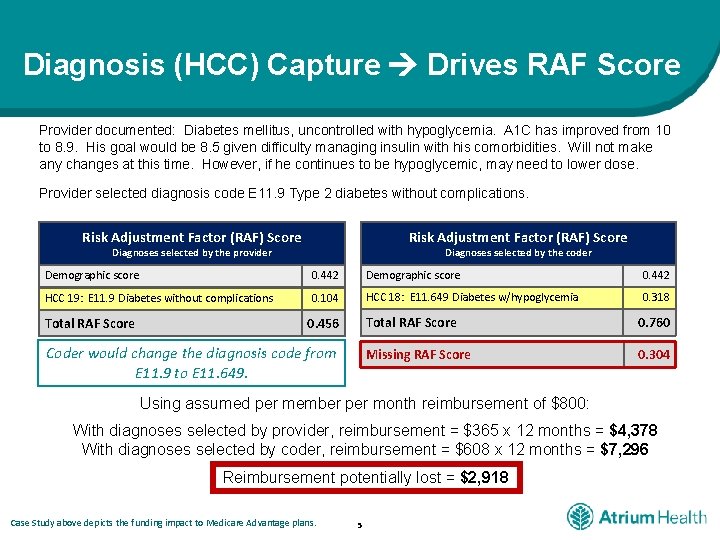
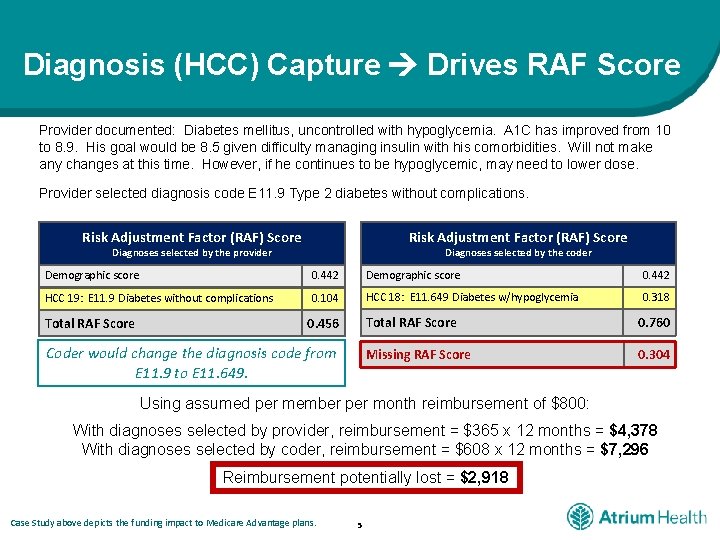
Diagnosis (HCC) Capture Drives RAF Score Provider documented: Diabetes mellitus, uncontrolled with hypoglycemia. A 1 C has improved from 10 to 8. 9. His goal would be 8. 5 given difficulty managing insulin with his comorbidities. Will not make any changes at this time. However, if he continues to be hypoglycemic, may need to lower dose. Provider selected diagnosis code E 11. 9 Type 2 diabetes without complications. Risk Adjustment Factor (RAF) Score Diagnoses selected by the provider Diagnoses selected by the coder Demographic score 0. 442 HCC 19: E 11. 9 Diabetes without complications 0. 104 HCC 18: E 11. 649 Diabetes w/hypoglycemia 0. 318 Total RAF Score 0. 456 Coder would change the diagnosis code from E 11. 9 to E 11. 649. Total RAF Score 0. 760 Missing RAF Score 0. 304 Using assumed per member per month reimbursement of $800: With diagnoses selected by provider, reimbursement = $365 x 12 months = $4, 378 With diagnoses selected by coder, reimbursement = $608 x 12 months = $7, 296 Reimbursement potentially lost = $2, 918 Case Study above depicts the funding impact to Medicare Advantage plans. 5
Professional Coding Team Role 6
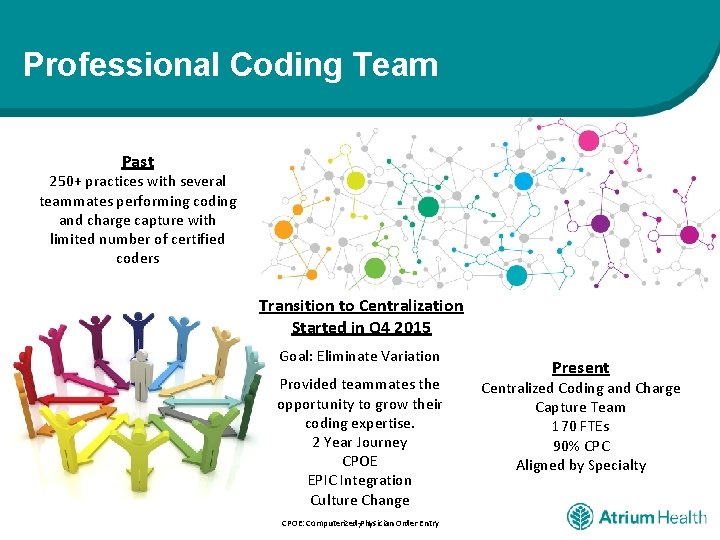
Professional Coding Team Past 250+ practices with several teammates performing coding and charge capture with limited number of certified coders Transition to Centralization Started in Q 4 2015 Goal: Eliminate Variation Provided teammates the opportunity to grow their coding expertise. 2 Year Journey CPOE EPIC Integration Culture Change CPOE: Computerized 7 Physician Order Entry Present Centralized Coding and Charge Capture Team 170 FTEs 90% CPC Aligned by Specialty
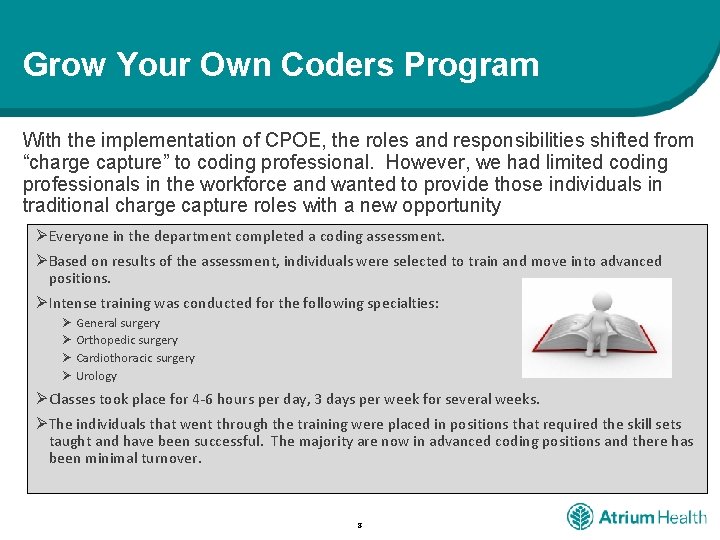
Grow Your Own Coders Program With the implementation of CPOE, the roles and responsibilities shifted from “charge capture” to coding professional. However, we had limited coding professionals in the workforce and wanted to provide those individuals in traditional charge capture roles with a new opportunity ØEveryone in the department completed a coding assessment. ØBased on results of the assessment, individuals were selected to train and move into advanced positions. ØIntense training was conducted for the following specialties: Ø General surgery Ø Orthopedic surgery Ø Cardiothoracic surgery Ø Urology ØClasses took place for 4 -6 hours per day, 3 days per week for several weeks. ØThe individuals that went through the training were placed in positions that required the skill sets taught and have been successful. The majority are now in advanced coding positions and there has been minimal turnover. 8
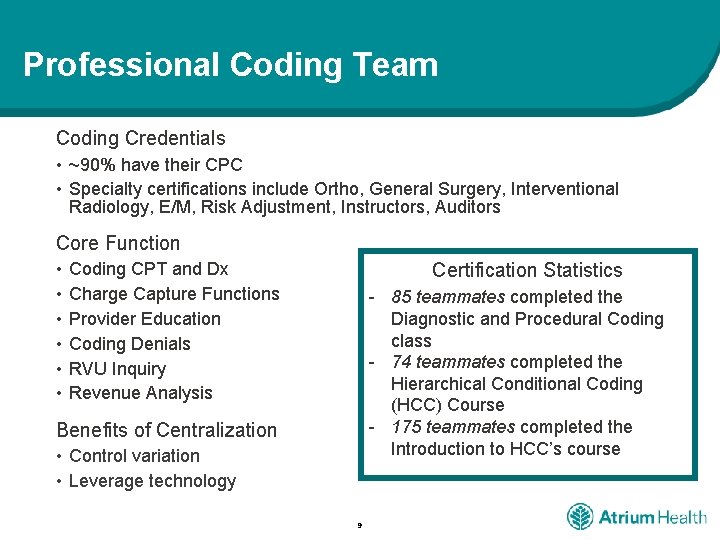
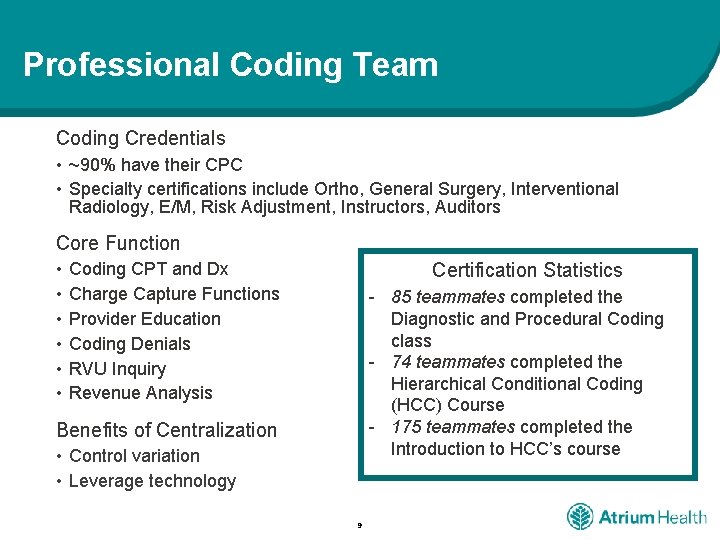
Professional Coding Team Coding Credentials • ~90% have their CPC • Specialty certifications include Ortho, General Surgery, Interventional Radiology, E/M, Risk Adjustment, Instructors, Auditors Core Function • • • Certification Statistics Coding CPT and Dx Charge Capture Functions Provider Education Coding Denials RVU Inquiry Revenue Analysis - 85 teammates completed the Diagnostic and Procedural Coding class - 74 teammates completed the Hierarchical Conditional Coding (HCC) Course - 175 teammates completed the Introduction to HCC’s course Benefits of Centralization • Control variation • Leverage technology 9
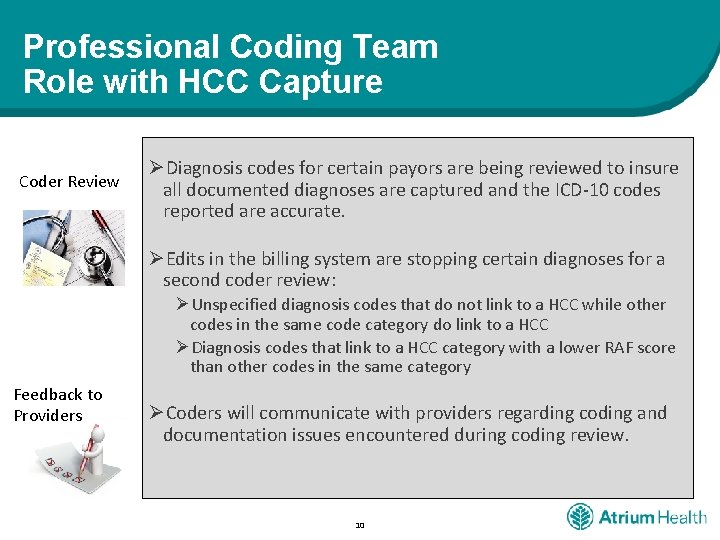
Professional Coding Team Role with HCC Capture Coder Review ØDiagnosis codes for certain payors are being reviewed to insure all documented diagnoses are captured and the ICD-10 codes reported are accurate. ØEdits in the billing system are stopping certain diagnoses for a second coder review: ØUnspecified diagnosis codes that do not link to a HCC while other codes in the same code category do link to a HCC ØDiagnosis codes that link to a HCC category with a lower RAF score than other codes in the same category Feedback to Providers ØCoders will communicate with providers regarding coding and documentation issues encountered during coding review. 10
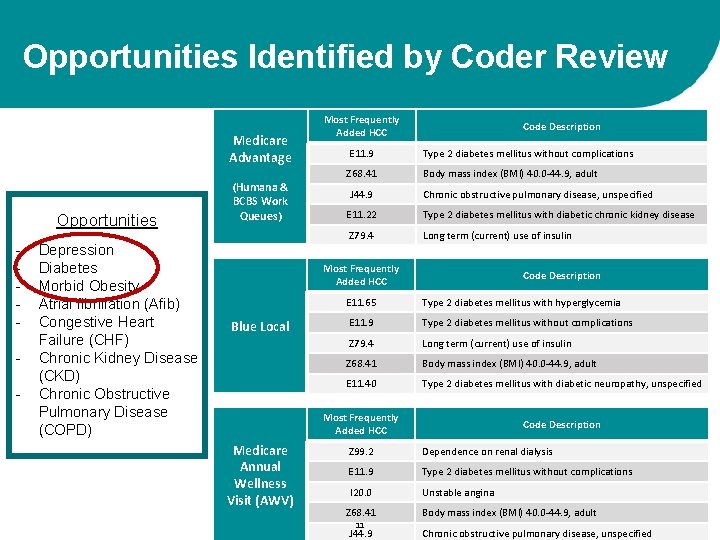
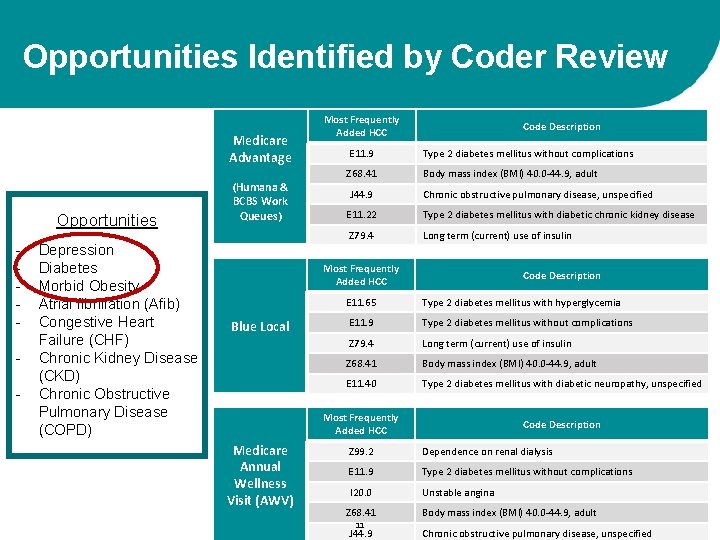
Opportunities Identified by Coder Review Medicare Advantage Opportunities - Depression Diabetes Morbid Obesity Atrial fibrillation (Afib) Congestive Heart Failure (CHF) Chronic Kidney Disease (CKD) Chronic Obstructive Pulmonary Disease (COPD) (Humana & BCBS Work Queues) Most Frequently Added HCC Code Description E 11. 9 Type 2 diabetes mellitus without complications Z 68. 41 Body mass index (BMI) 40. 0 -44. 9, adult J 44. 9 Chronic obstructive pulmonary disease, unspecified E 11. 22 Type 2 diabetes mellitus with diabetic chronic kidney disease Z 79. 4 Long term (current) use of insulin Most Frequently Added HCC Blue Local Medicare Annual Wellness Visit (AWV) Code Description E 11. 65 Type 2 diabetes mellitus with hyperglycemia E 11. 9 Type 2 diabetes mellitus without complications Z 79. 4 Long term (current) use of insulin Z 68. 41 Body mass index (BMI) 40. 0 -44. 9, adult E 11. 40 Type 2 diabetes mellitus with diabetic neuropathy, unspecified Most Frequently Added HCC Code Description Z 99. 2 Dependence on renal dialysis E 11. 9 Type 2 diabetes mellitus without complications I 20. 0 Unstable angina Z 68. 41 11 J 44. 9 Body mass index (BMI) 40. 0 -44. 9, adult Chronic obstructive pulmonary disease, unspecified
Provider Engagement & Partnership with Coding Team 12
Provider Engagement Critical to have Provider Engagement and Leadership • Medical Risk Adjustment Committee • Provider-led committee responsible for executing the plan to improve our capture of HCC diagnoses and appropriately reflect the risk of our patients. • Multidisciplinary group of 35 members • 10+ physicians • Specialties represented: Internal Medicine, Family Medicine, Endocrinology, Surgery, Emergency Medicine, Cardiology, etc. 30+ physicians participated in HCC Bootcamp • Half Day Training Session taught by HCPro • Significant Discussion and Questions from the Providers 13
Provider Resources The One-Stop Shop for all things HCC: HCC Site on Atrium Health Physician Connect 14
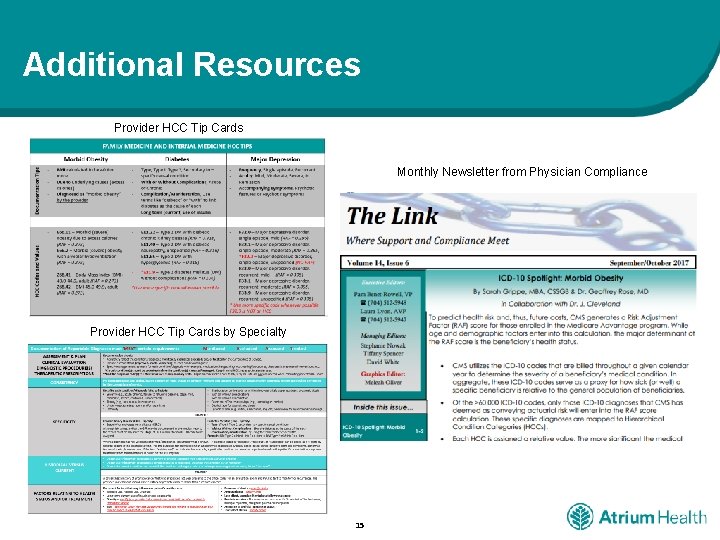
Additional Resources Provider HCC Tip Cards Monthly Newsletter from Physician Compliance Provider HCC Tip Cards by Specialty 15
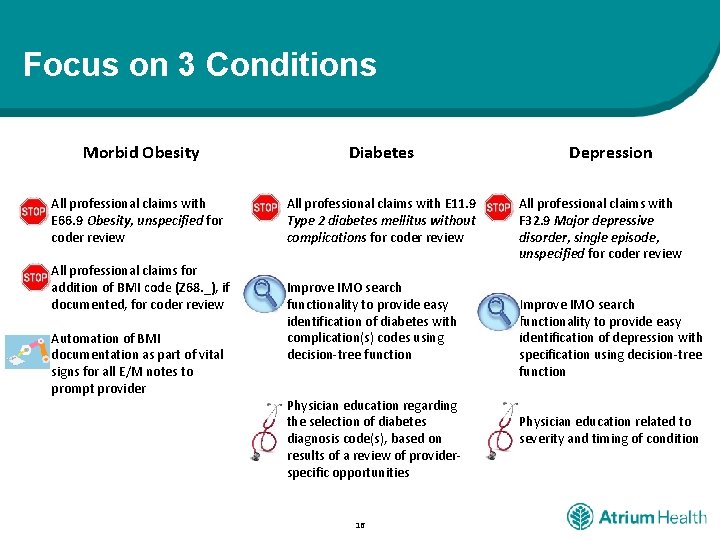
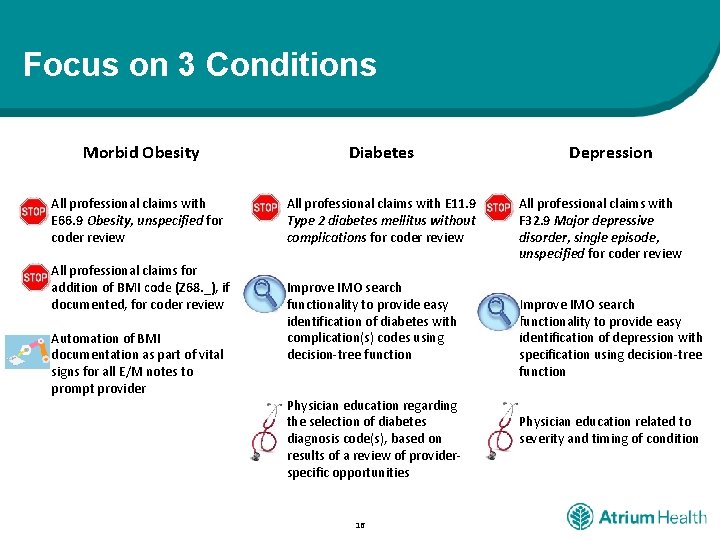
Focus on 3 Conditions Morbid Obesity Diabetes All professional claims with E 66. 9 Obesity, unspecified for coder review All professional claims with E 11. 9 Type 2 diabetes mellitus without complications for coder review All professional claims for addition of BMI code (Z 68. _), if documented, for coder review Automation of BMI documentation as part of vital signs for all E/M notes to prompt provider Improve IMO search functionality to provide easy identification of diabetes with complication(s) codes using decision-tree function Physician education regarding the selection of diabetes diagnosis code(s), based on results of a review of providerspecific opportunities 16 Depression All professional claims with F 32. 9 Major depressive disorder, single episode, unspecified for coder review Improve IMO search functionality to provide easy identification of depression with specification using decision-tree function Physician education related to severity and timing of condition
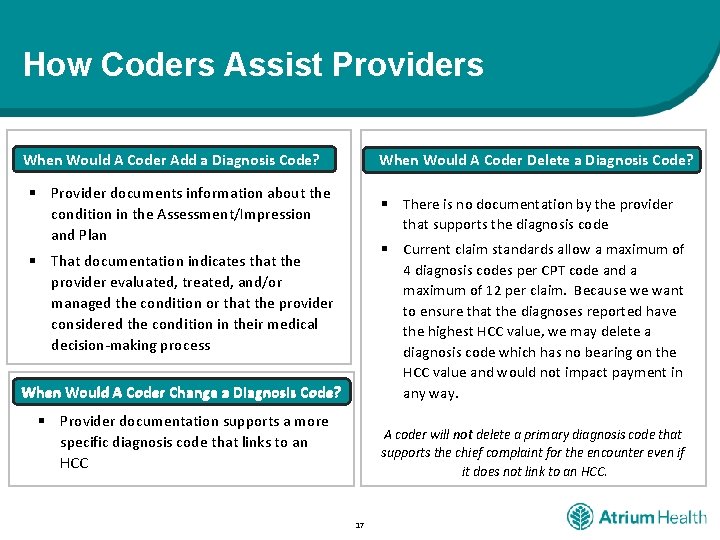
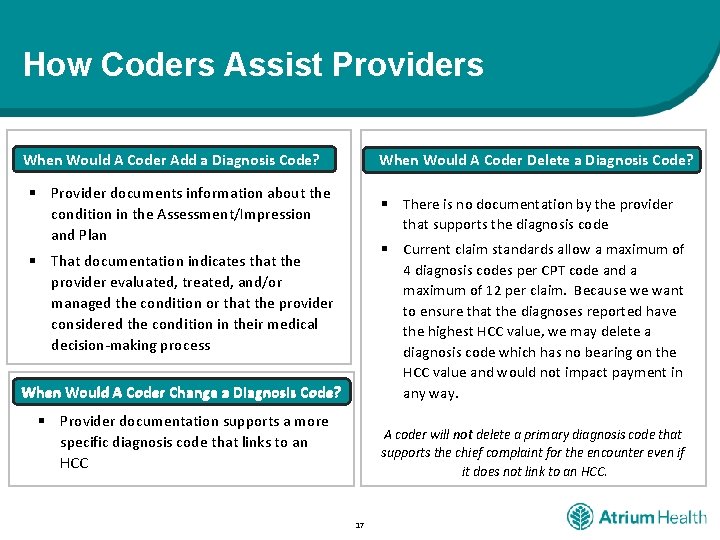
How Coders Assist Providers When Would A Coder Delete a Diagnosis Code? When Would A Coder Add a Diagnosis Code? § Provider documents information about the condition in the Assessment/Impression and Plan § There is no documentation by the provider that supports the diagnosis code § Current claim standards allow a maximum of 4 diagnosis codes per CPT code and a maximum of 12 per claim. Because we want to ensure that the diagnoses reported have the highest HCC value, we may delete a diagnosis code which has no bearing on the HCC value and would not impact payment in any way. § That documentation indicates that the provider evaluated, treated, and/or managed the condition or that the provider considered the condition in their medical decision-making process When Would A Coder Change a Diagnosis Code? § Provider documentation supports a more specific diagnosis code that links to an HCC A coder will not delete a primary diagnosis code that supports the chief complaint for the encounter even if it does not link to an HCC. 17
Workflow & Technology 18
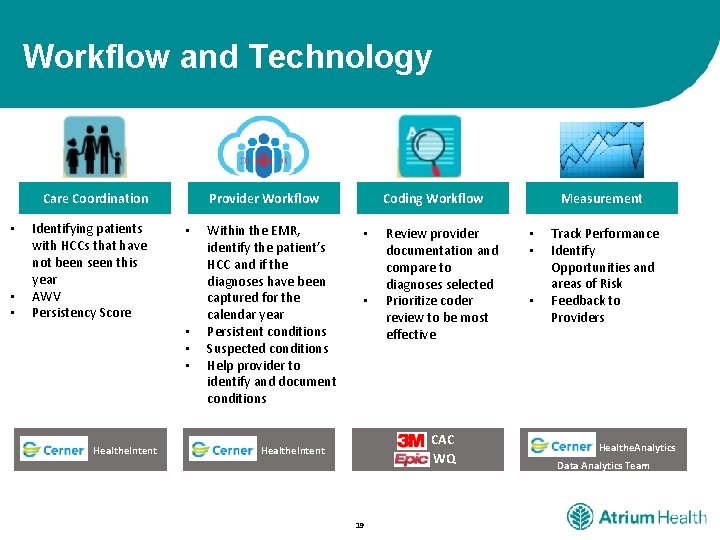
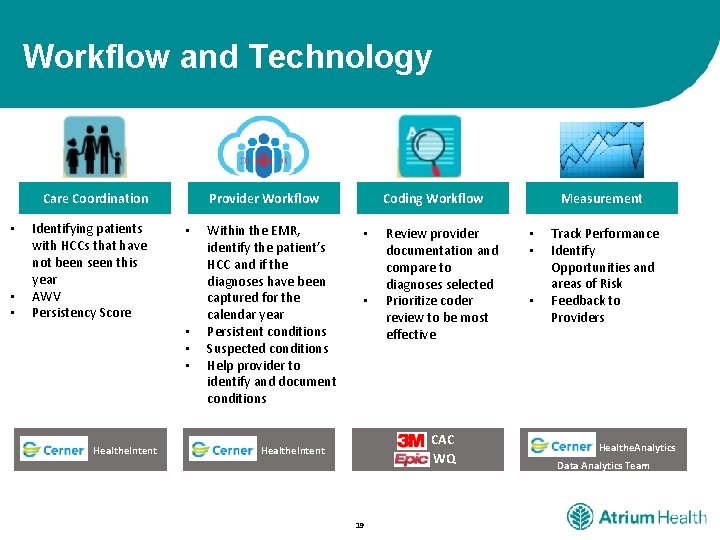
Workflow and Technology Care Coordination • • • Identifying patients Stakeholders with. Key HCCs that have not been seen this year AWV Persistency Score Provider Workflow • • Healthe. Intent Within the EMR, identify the patient’s HCC and if the diagnoses have been captured for the calendar year Persistent conditions Suspected conditions Help provider to identify and document conditions Measurement Coding Workflow • • Review provider Analytics documentation and compare to diagnoses selected Prioritize coder review to be most effective CAC WQ Healthe. Intent 19 • • • Track Performance Identify. Value Add Opportunities and areas of Risk Feedback to Providers Healthe. Analytics Data Analytics Team
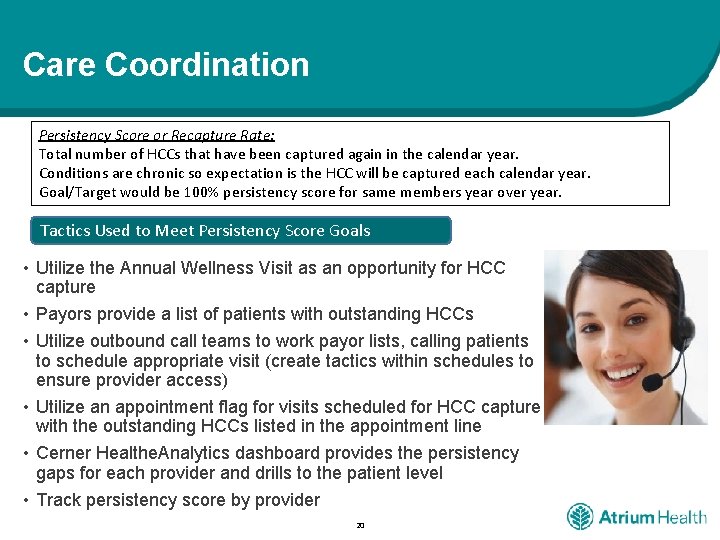
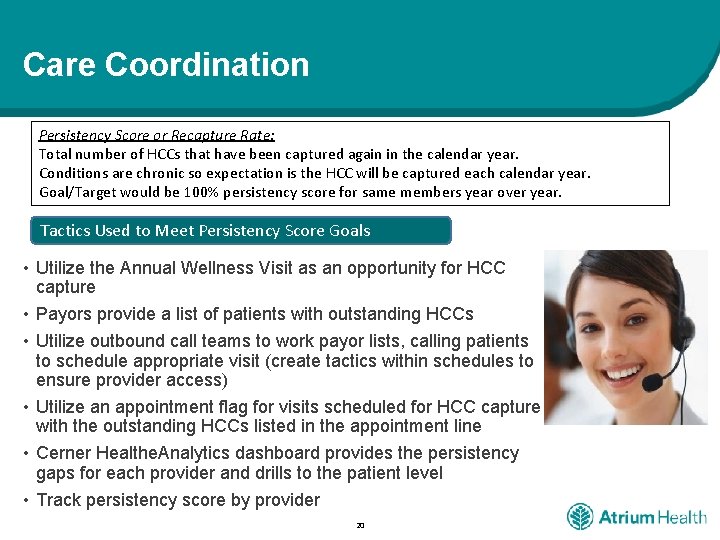
Care Coordination Persistency Score or Recapture Rate: Total number of HCCs that have been captured again in the calendar year. Conditions are chronic so expectation is the HCC will be captured each calendar year. Goal/Target would be 100% persistency score for same members year over year. Tactics Used to Meet Persistency Score Goals • Utilize the Annual Wellness Visit as an opportunity for HCC capture • Payors provide a list of patients with outstanding HCCs • Utilize outbound call teams to work payor lists, calling patients to schedule appropriate visit (create tactics within schedules to ensure provider access) • Utilize an appointment flag for visits scheduled for HCC capture with the outstanding HCCs listed in the appointment line • Cerner Healthe. Analytics dashboard provides the persistency gaps for each provider and drills to the patient level • Track persistency score by provider 20
Metrics/Performance Tracking 21
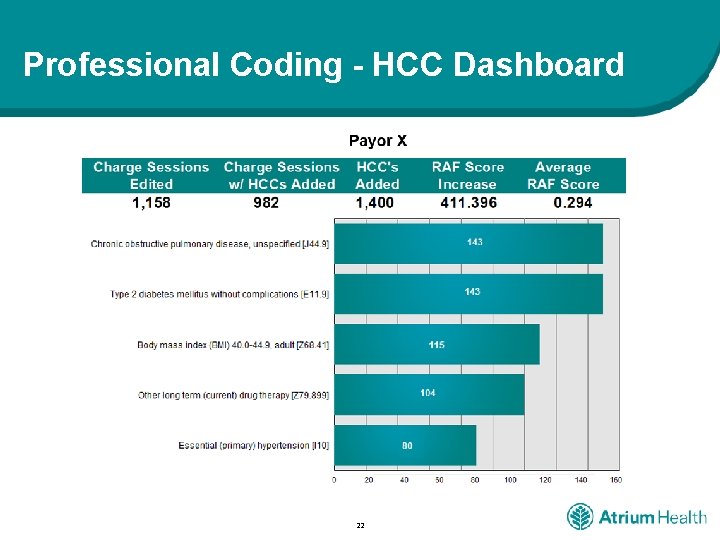
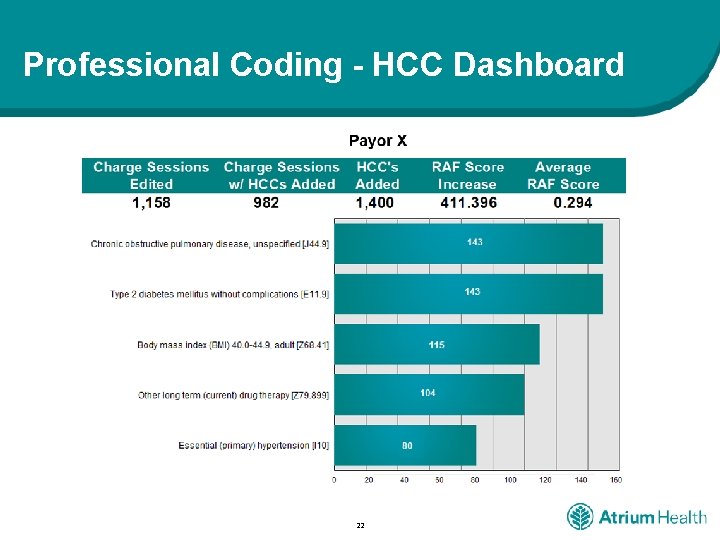
Professional Coding - HCC Dashboard 22
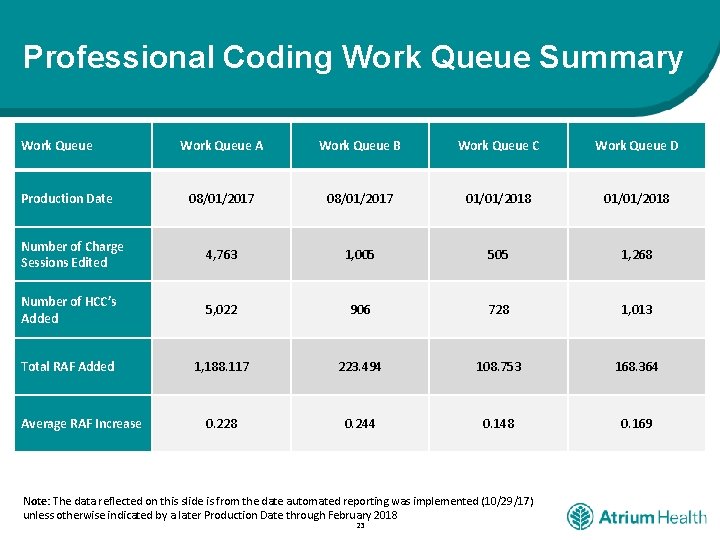
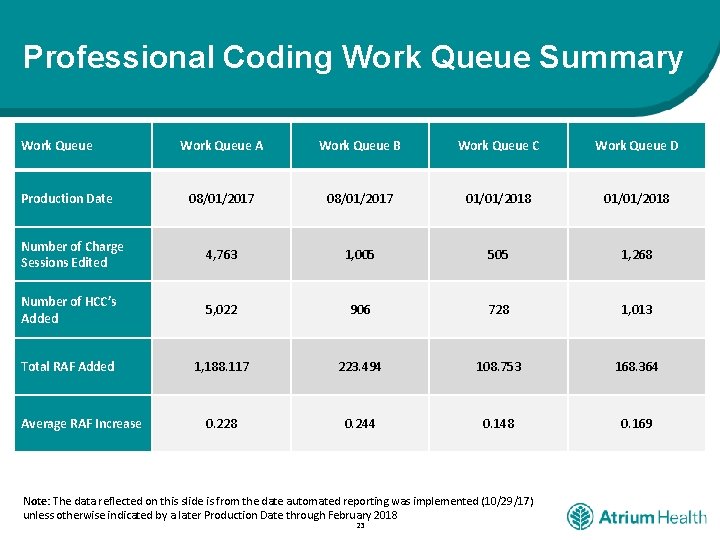
Professional Coding Work Queue Summary Work Queue A Work Queue B Work Queue C Work Queue D 08/01/2017 01/01/2018 Number of Charge Sessions Edited 4, 763 1, 005 505 1, 268 Number of HCC’s Added 5, 022 906 728 1, 013 Total RAF Added 1, 188. 117 223. 494 108. 753 168. 364 0. 228 0. 244 0. 148 0. 169 Production Date Average RAF Increase Note: The data reflected on this slide is from the date automated reporting was implemented (10/29/17) unless otherwise indicated by a later Production Date through February 2018 23
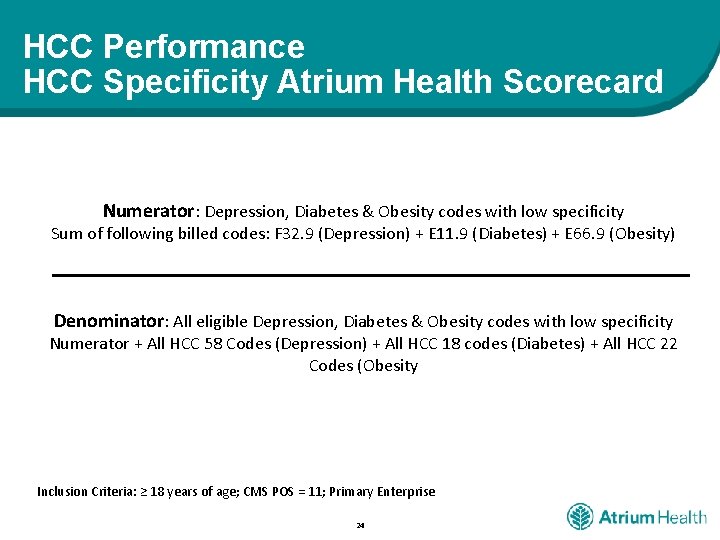
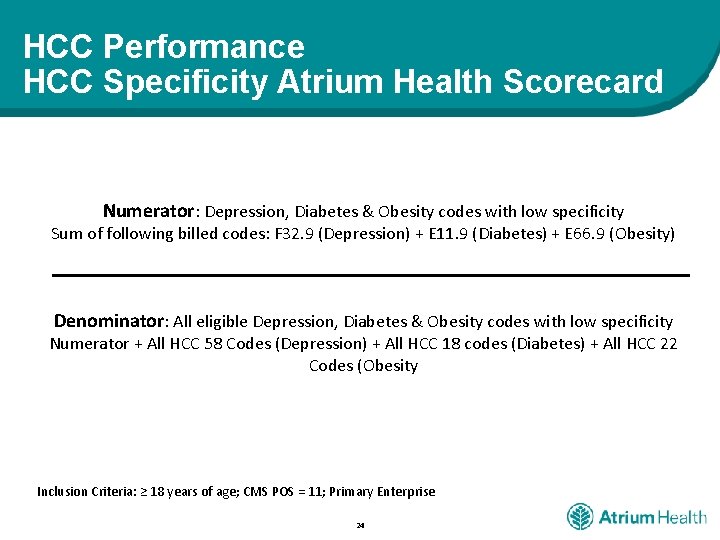
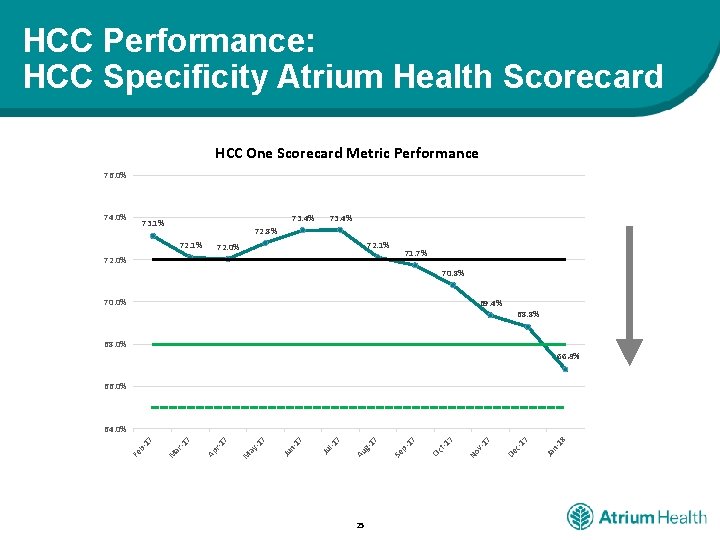
HCC Performance HCC Specificity Atrium Health Scorecard Numerator: Depression, Diabetes & Obesity codes with low specificity Sum of following billed codes: F 32. 9 (Depression) + E 11. 9 (Diabetes) + E 66. 9 (Obesity) Denominator: All eligible Depression, Diabetes & Obesity codes with low specificity Numerator + All HCC 58 Codes (Depression) + All HCC 18 codes (Diabetes) + All HCC 22 Codes (Obesity Inclusion Criteria: ≥ 18 years of age; CMS POS = 11; Primary Enterprise 24
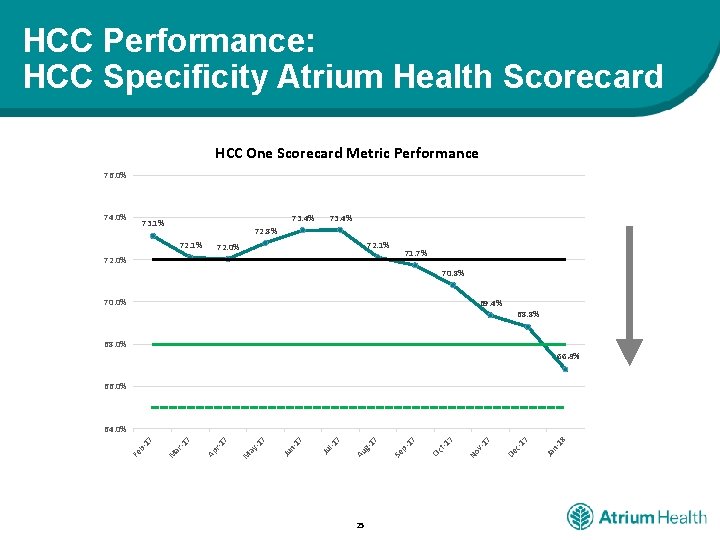
HCC Performance: HCC Specificity Atrium Health Scorecard HCC One Scorecard Metric Performance 76. 0% 74. 0% 73. 4% 73. 1% 73. 4% 72. 8% 72. 1% 72. 0% 71. 7% 72. 0% 70. 8% 70. 0% 69. 4% 68. 8% 68. 0% 66. 8% 66. 0% 25 18 n. Ja 17 c. De 17 v. No 7 t-1 Oc 17 p. Se 7 g 1 Au 7 l-1 Ju 7 -1 Ju n 7 M ay -1 7 r-1 Ap 7 -1 ar M Fe b- 17 64. 0%
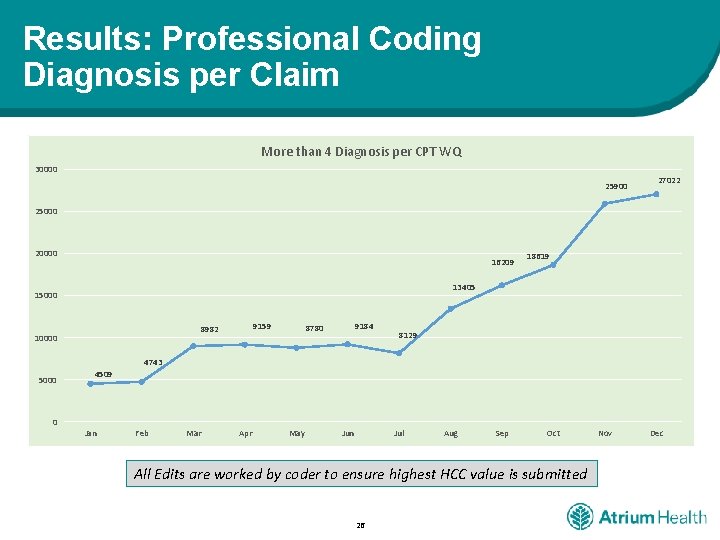
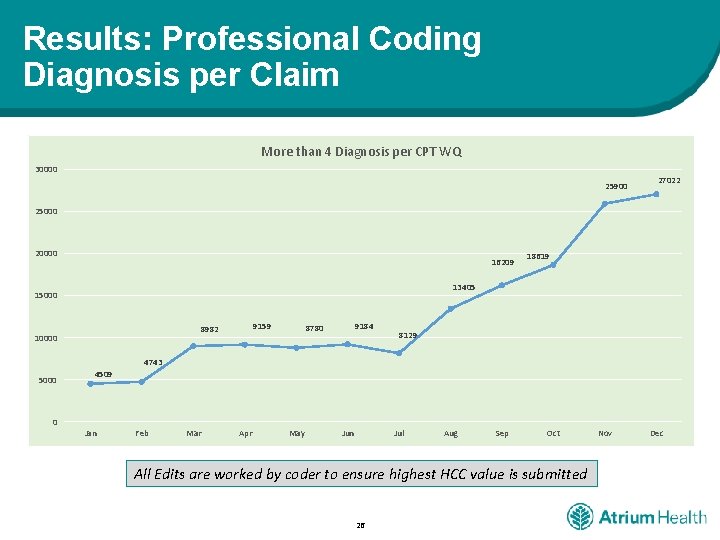
Results: Professional Coding Diagnosis per Claim More than 4 Diagnosis per CPT WQ 30000 25900 27022 25000 20000 16209 18619 13405 15000 9159 8982 10000 9184 8780 8129 4743 5000 0 4509 Jan Feb Mar Apr May Jun Jul Aug Sep Oct All Edits are worked by coder to ensure highest HCC value is submitted 26 Nov Dec
Questions? 27