Empanelment The New Primary Care Measurement NC HFMA
- Slides: 18
Empanelment The New Primary Care Measurement NC HFMA
Key Takaways • Definitions and Determinates of Provider Panels • How Empanelment can align the work • Industry view on Panels • Lessons Learned…one point of view
Why Panel Management? The “care model” and “patient-centered medical home” concepts require a different approach. Patients are assigned to particular clinicians or care teams; this in turn fosters ongoing relationships, and makes it possible for care teams to “manage” care — not just for individual patients as they appear, but for all of the patients assigned to their panel. . (Source: DHHS Agency for Healthcare Research and Quality website (http: //www. ahrq. gov/professionals/prevention-chroniccare/improve/system/pfhandbook/mod 20. html. ) 3
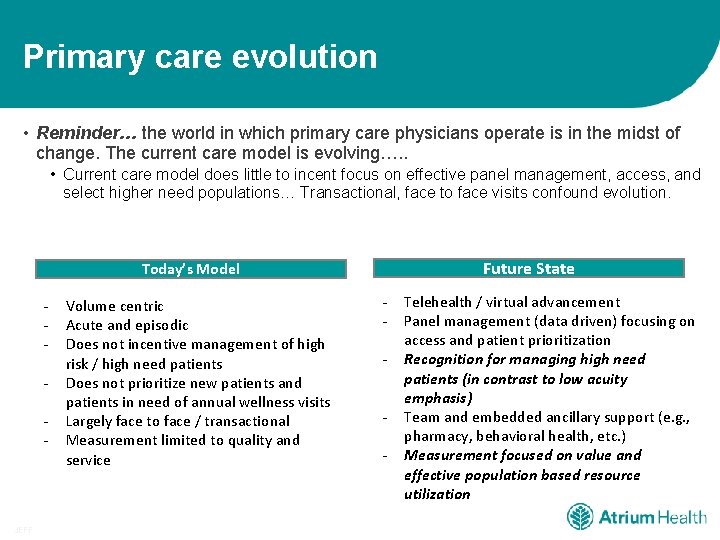
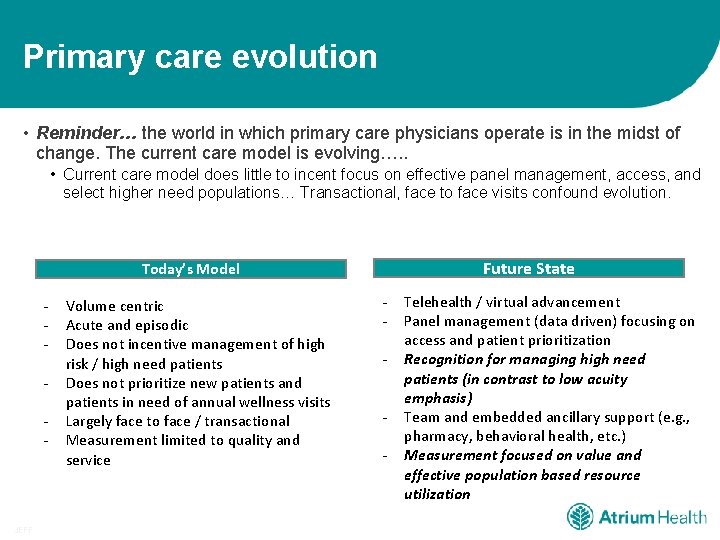
Primary care evolution • Reminder… the world in which primary care physicians operate is in the midst of change. The current care model is evolving…. . • Current care model does little to incent focus on effective panel management, access, and select higher need populations… Transactional, face to face visits confound evolution. Future State Today’s Model - JEFF Volume centric Acute and episodic Does not incentive management of high risk / high need patients Does not prioritize new patients and patients in need of annual wellness visits Largely face to face / transactional Measurement limited to quality and service - Telehealth / virtual advancement Panel management (data driven) focusing on access and patient prioritization Recognition for managing high need patients (in contrast to low acuity emphasis) Team and embedded ancillary support (e. g. , pharmacy, behavioral health, etc. ) Measurement focused on value and effective population based resource utilization
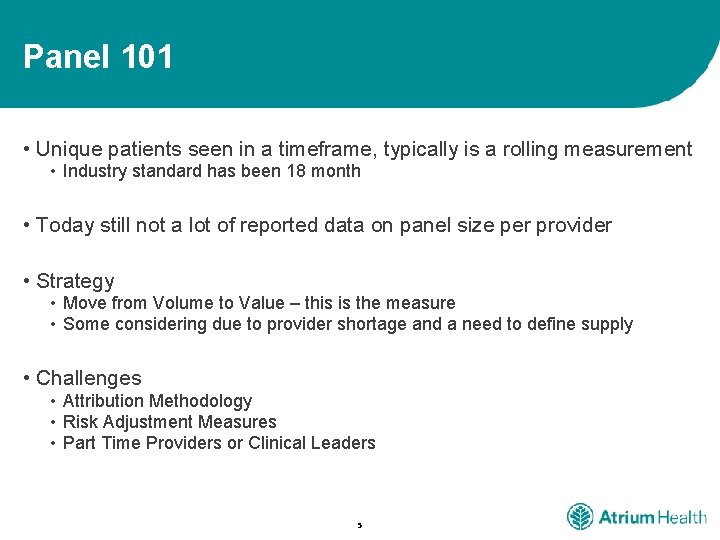
Panel 101 • Unique patients seen in a timeframe, typically is a rolling measurement • Industry standard has been 18 month • Today still not a lot of reported data on panel size per provider • Strategy • Move from Volume to Value – this is the measure • Some considering due to provider shortage and a need to define supply • Challenges • Attribution Methodology • Risk Adjustment Measures • Part Time Providers or Clinical Leaders 5
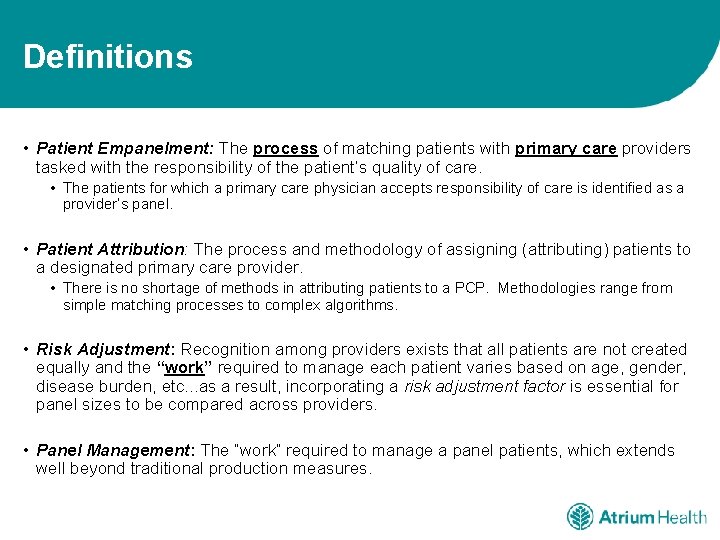
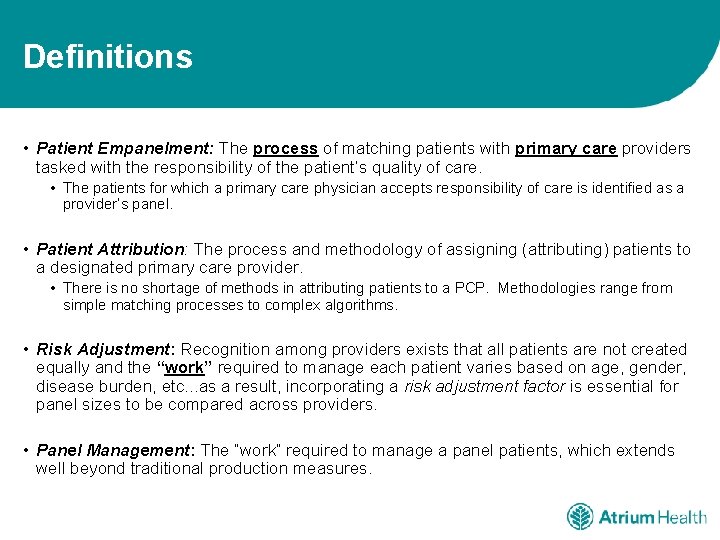
Definitions • Patient Empanelment: The process of matching patients with primary care providers tasked with the responsibility of the patient’s quality of care. • The patients for which a primary care physician accepts responsibility of care is identified as a provider’s panel. • Patient Attribution: The process and methodology of assigning (attributing) patients to a designated primary care provider. • There is no shortage of methods in attributing patients to a PCP. Methodologies range from simple matching processes to complex algorithms. • Risk Adjustment: Recognition among providers exists that all patients are not created equally and the “work” required to manage each patient varies based on age, gender, disease burden, etc. . . as a result, incorporating a risk adjustment factor is essential for panel sizes to be compared across providers. • Panel Management: The “work” required to manage a panel patients, which extends well beyond traditional production measures.
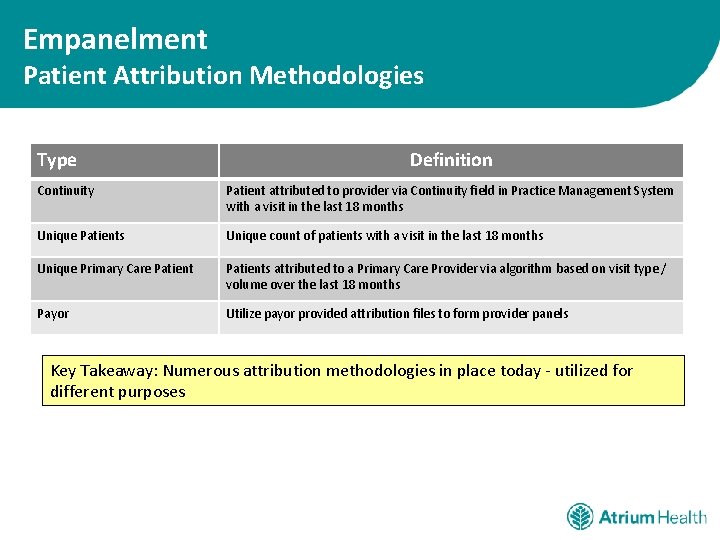
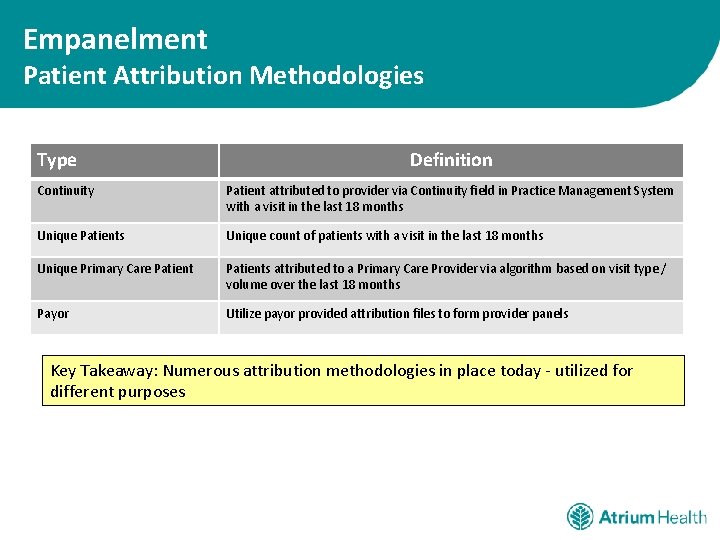
Empanelment Patient Attribution Methodologies Type Definition Continuity Patient attributed to provider via Continuity field in Practice Management System with a visit in the last 18 months Unique Patients Unique count of patients with a visit in the last 18 months Unique Primary Care Patients attributed to a Primary Care Provider via algorithm based on visit type / volume over the last 18 months Payor Utilize payor provided attribution files to form provider panels Key Takeaway: Numerous attribution methodologies in place today - utilized for different purposes
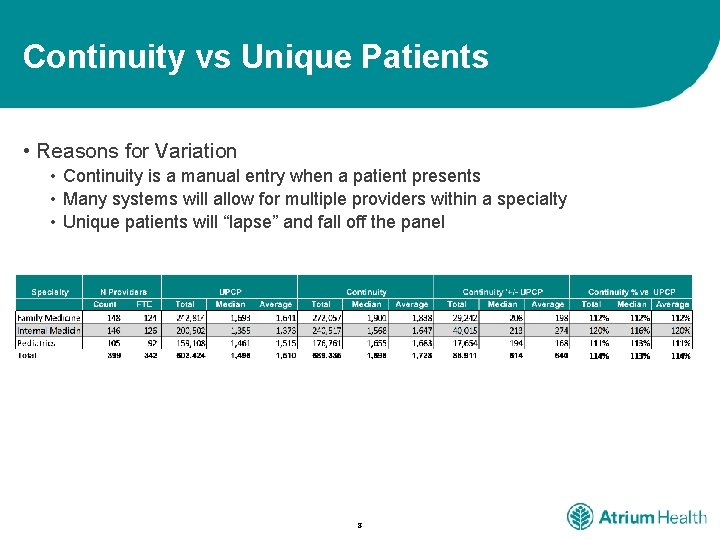
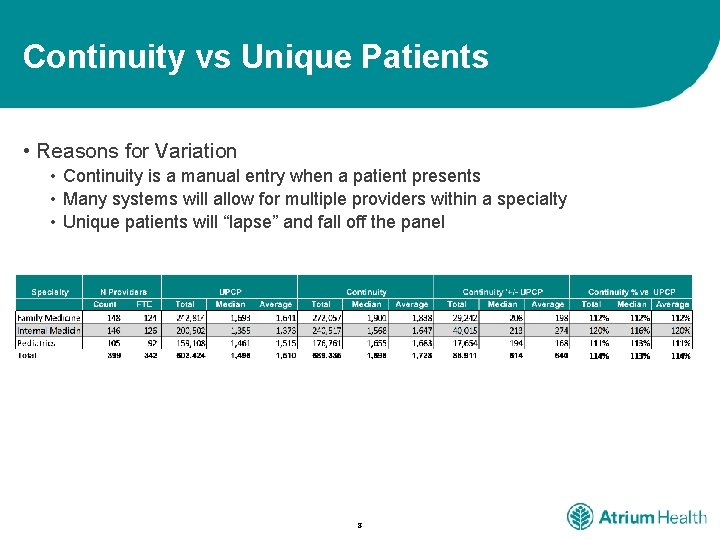
Continuity vs Unique Patients • Reasons for Variation • Continuity is a manual entry when a patient presents • Many systems will allow for multiple providers within a specialty • Unique patients will “lapse” and fall off the panel 8
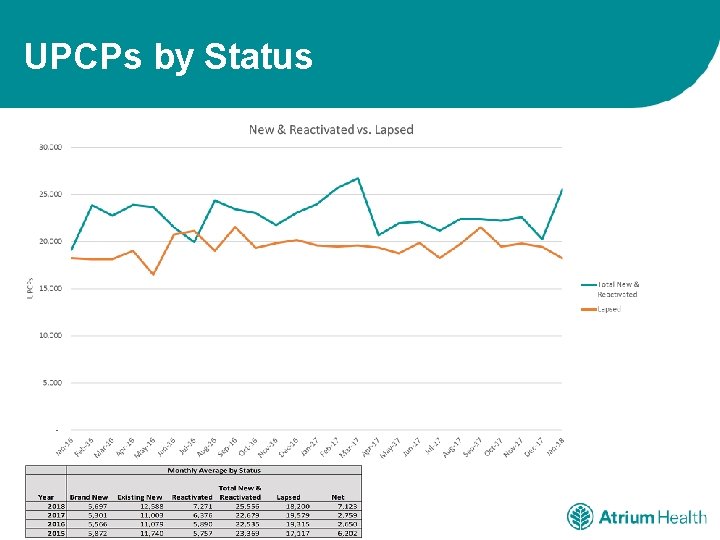
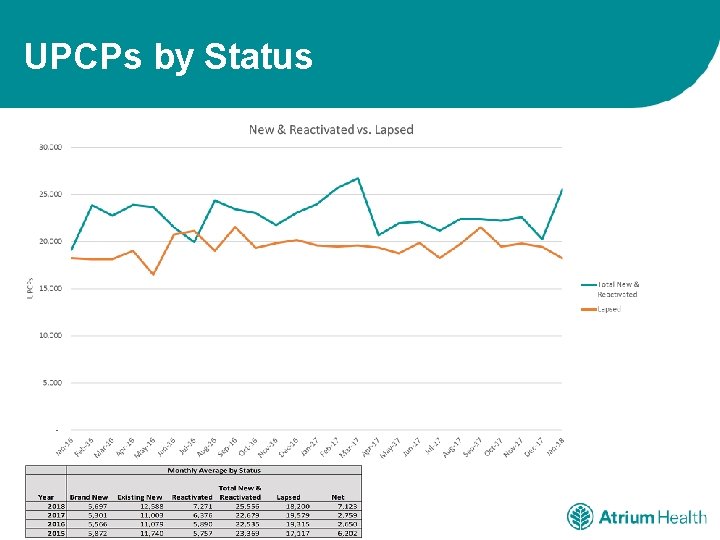
UPCPs by Status
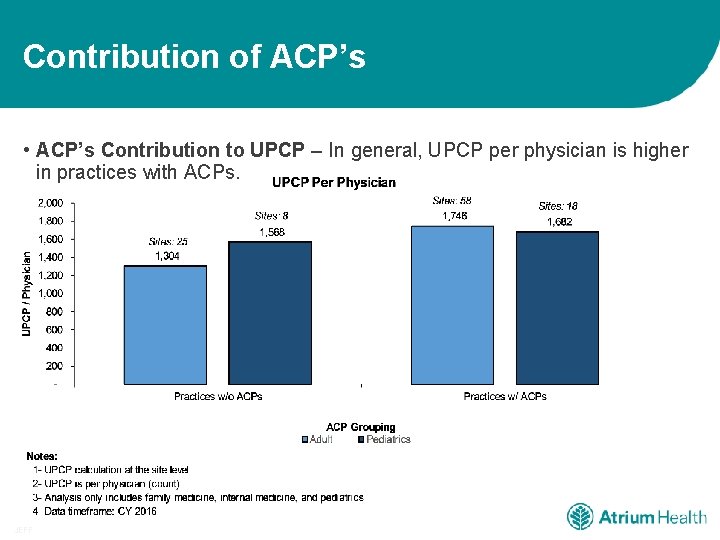
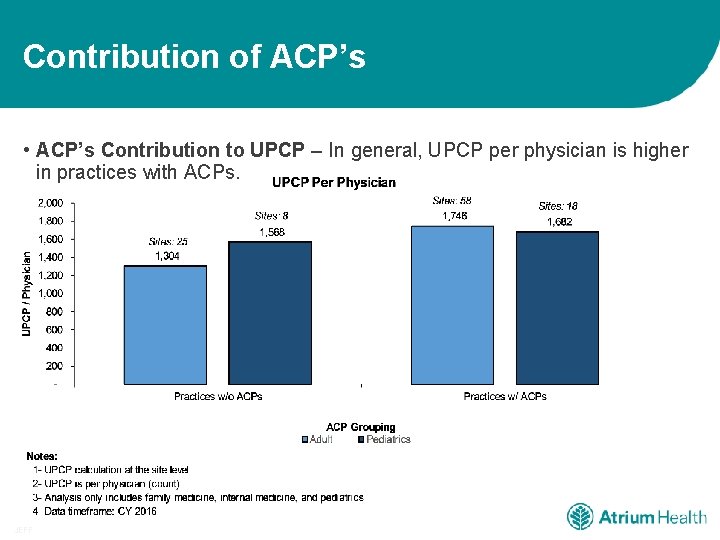
Contribution of ACP’s • ACP’s Contribution to UPCP – In general, UPCP per physician is higher in practices with ACPs. JEFF
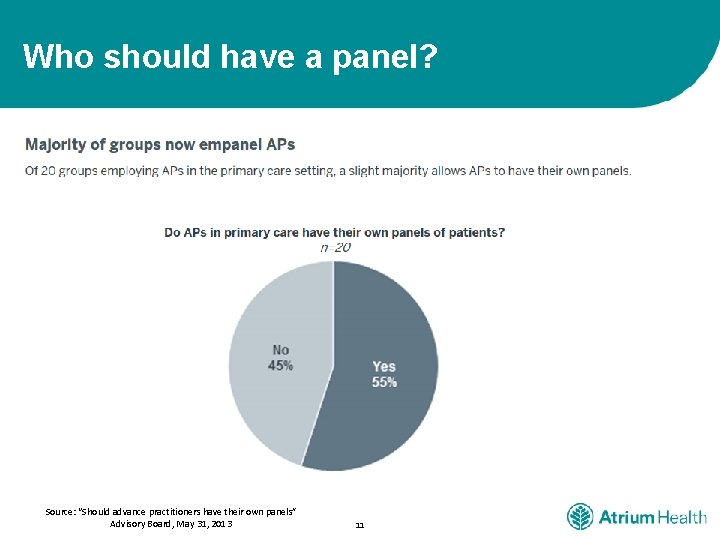
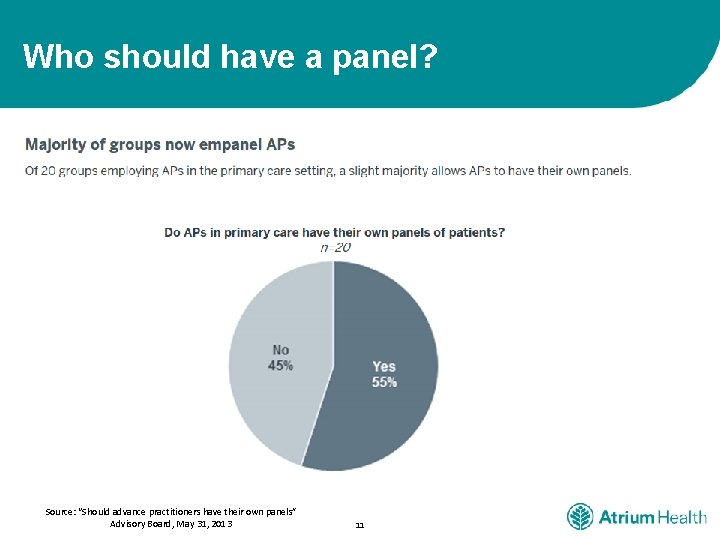
Who should have a panel? Source: “Should advance practitioners have their own panels” Advisory Board, May 31, 2013 11
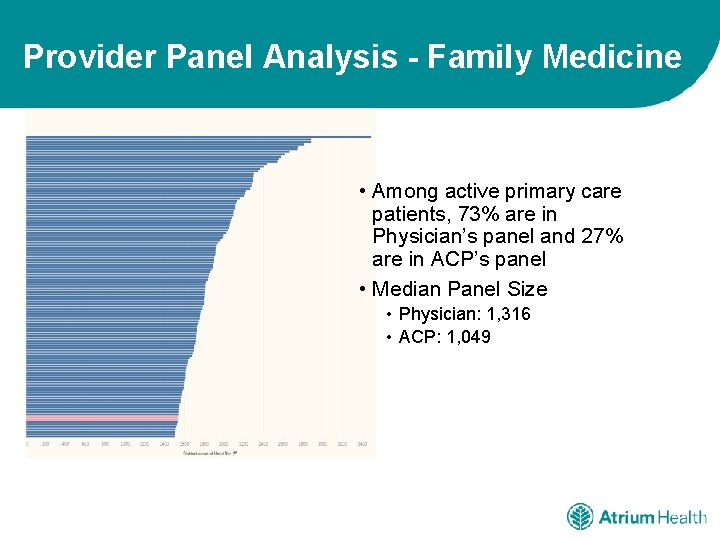
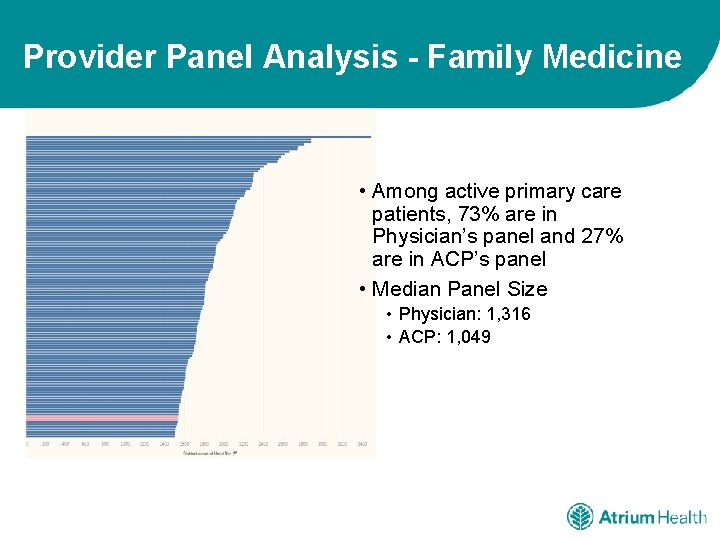
Provider Panel Analysis - Family Medicine • Among active primary care patients, 73% are in Physician’s panel and 27% are in ACP’s panel • Median Panel Size • Physician: 1, 316 • ACP: 1, 049
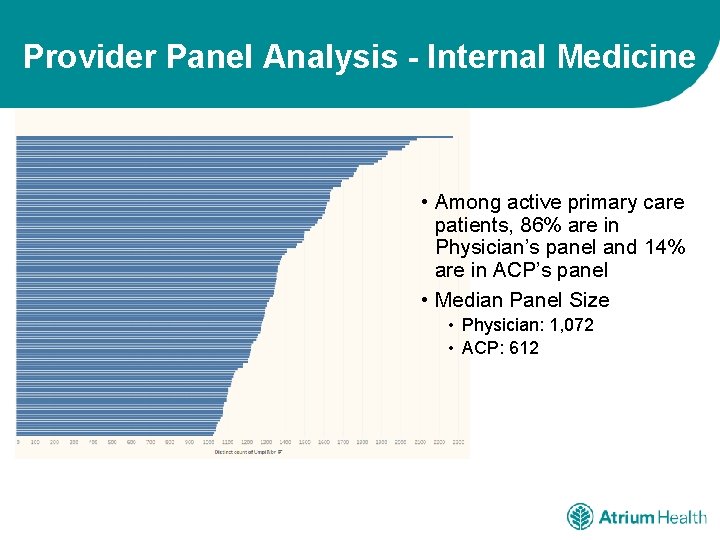
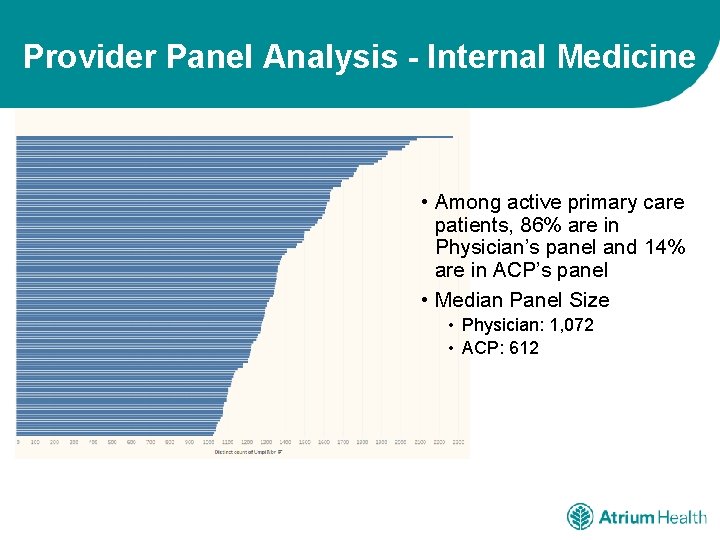
Provider Panel Analysis - Internal Medicine • Among active primary care patients, 86% are in Physician’s panel and 14% are in ACP’s panel • Median Panel Size • Physician: 1, 072 • ACP: 612
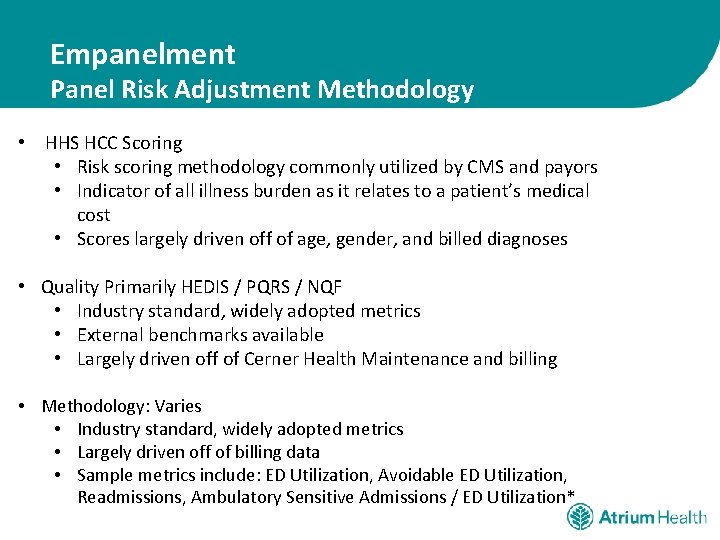
Empanelment Panel Risk Adjustment Methodology • HHS HCC Scoring • Risk scoring methodology commonly utilized by CMS and payors • Indicator of all illness burden as it relates to a patient’s medical cost • Scores largely driven off of age, gender, and billed diagnoses • Quality Primarily HEDIS / PQRS / NQF • Industry standard, widely adopted metrics • External benchmarks available • Largely driven off of Cerner Health Maintenance and billing • Methodology: Varies • Industry standard, widely adopted metrics • Largely driven off of billing data • Sample metrics include: ED Utilization, Avoidable ED Utilization, Readmissions, Ambulatory Sensitive Admissions / ED Utilization*
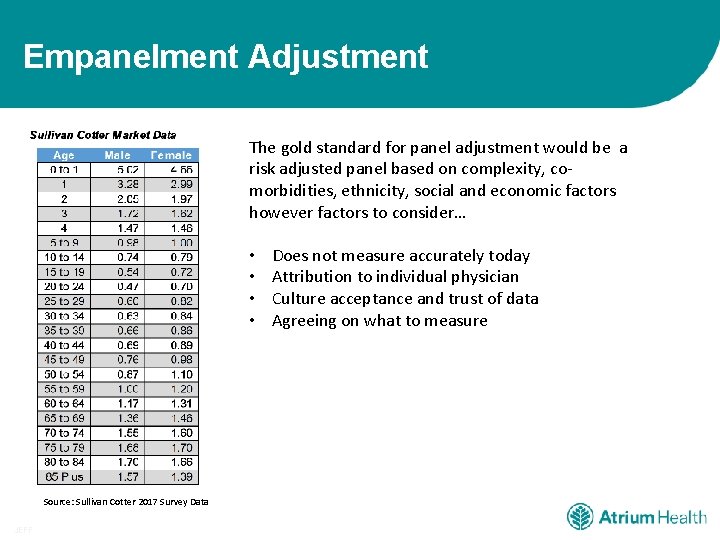
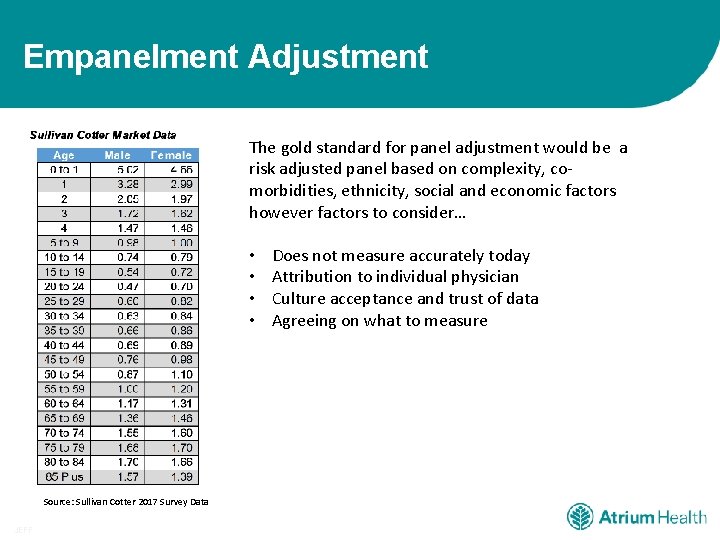
Empanelment Adjustment The gold standard for panel adjustment would be a risk adjusted panel based on complexity, comorbidities, ethnicity, social and economic factors however factors to consider… • • Source: Sullivan Cotter 2017 Survey Data JEFF Does not measure accurately today Attribution to individual physician Culture acceptance and trust of data Agreeing on what to measure
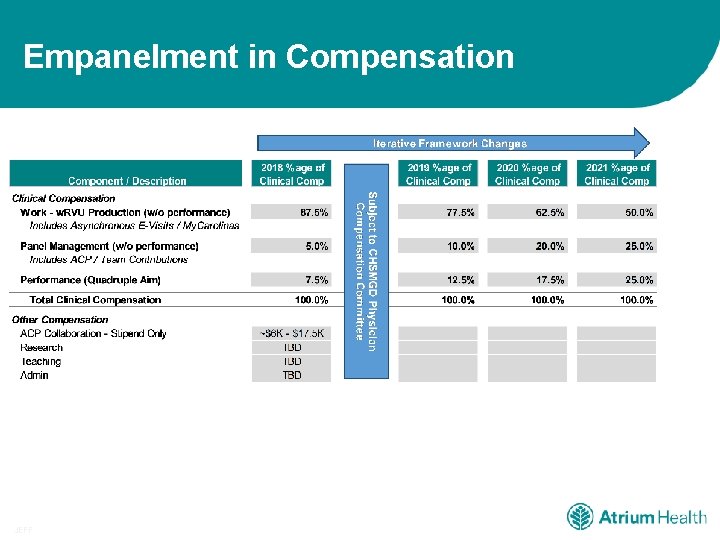
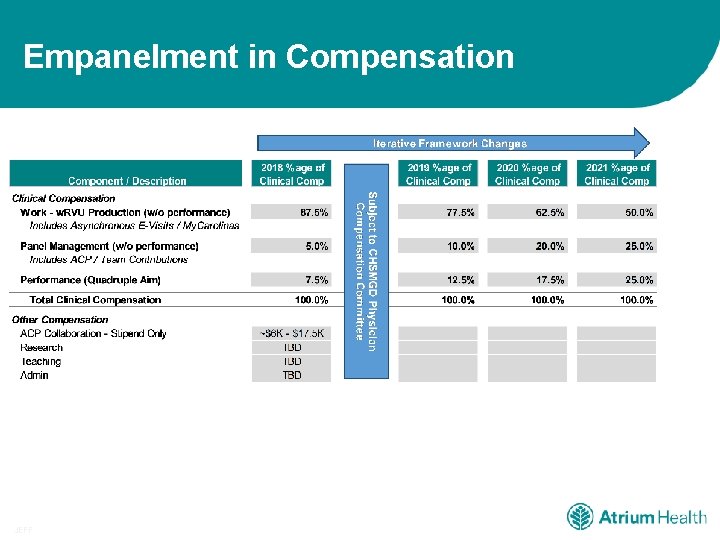
Empanelment in Compensation JEFF
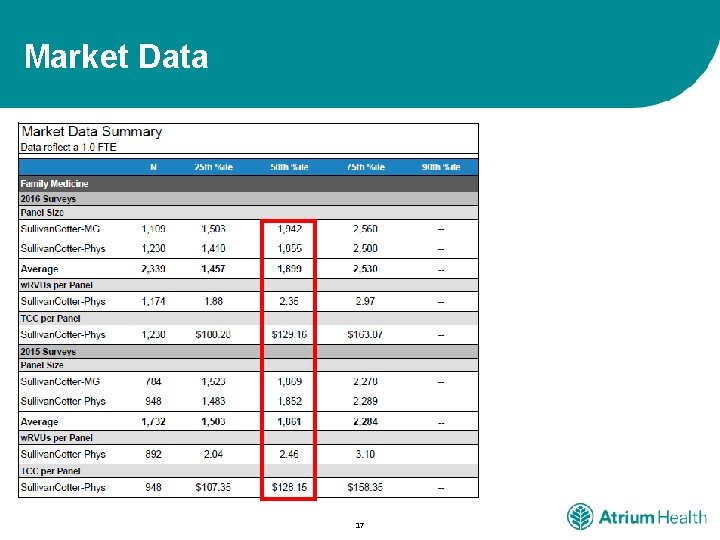
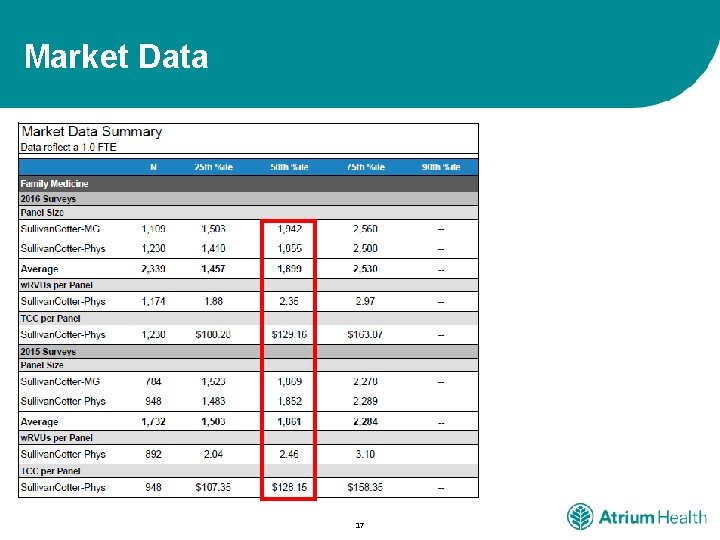
Market Data 17
Questions? 18
 Primary secondary tertiary medical care
Primary secondary tertiary medical care Nc hfma
Nc hfma Hcc recapture rate
Hcc recapture rate Wv hfma
Wv hfma Primary scales of measurement in marketing research
Primary scales of measurement in marketing research Scales of measurement
Scales of measurement Measurement scales
Measurement scales Nrm rics
Nrm rics New rules of measurement
New rules of measurement Measurement standards laboratory of new zealand
Measurement standards laboratory of new zealand Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Glasgow thang điểm
Glasgow thang điểm Chúa yêu trần thế
Chúa yêu trần thế Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất