Grampian Naloxone Programme Training for Staff The following

- Slides: 35
Grampian Naloxone Programme Training for Staff The following information aims to refresh knowledge on the causes, risk factors and management of opioid overdose. It has been adapted from national materials supplied with the kind permission of Scottish Drugs Forum Staff should ensure they are familiar with this information as it forms the basis of delivering the naloxone intervention. A recap quiz based on the information within this presentation will be used to ensure staff have retained and understood the information provided. There are films embedded within the document where you see the following symbol click on it to play the films The SDF booklet “Drug Related Deaths: What should you know” should be used in conjunction with this material
Purpose of Training For many professionals working with individuals who use drugs, discussing overdose risks may already be a key focus for discussion The naloxone programme ensures that key messages are discussed consistently and extend it to allow the supply of naloxone For clients who find themselves in an overdose situation the intervention will equip them to take the correct course of action and dispel any pre-existing myths Training will focus on the delivery of the specific intervention and help you find your own style of delivery. If you would like to learn more about formal adult learning techniques follow the link at the end of the presentation
Key Learning Outcomes Refresh knowledge – Opioid overdose risks Understand the importance, relevance and need for the Take Home Naloxone programme Refresh Basic Life Support knowledge highlighting respiratory events Introduce and understand naloxone administration and good practice Improve awareness of naloxone promotion & resources Understand need to communicate key points with clients
What is an overdose? Overdose happens when a person takes more of a drug or combination of drugs than the body can handle. As a result the central nervous system is not able to properly control basic life functions. The person may pass out, stop breathing, have heart failure or experience seizures. Overdose can be fatal. Non-fatal overdose, which can be associated with several health harms, is also a cause for concerns.
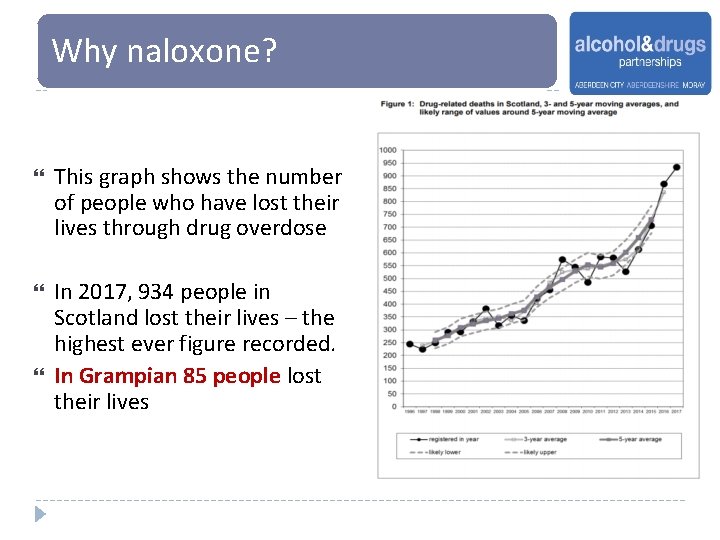
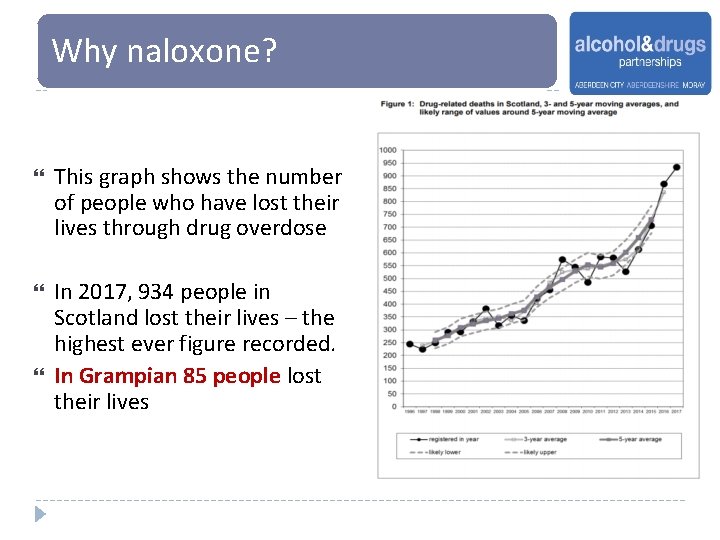
Why naloxone? This graph shows the number of people who have lost their lives through drug overdose In 2017, 934 people in Scotland lost their lives – the highest ever figure recorded. In Grampian 85 people lost their lives
Why naloxone? Of those individuals who died More than 70% were over the age of 35 years. These were generally people with a long history in drug use rather than young, inexperienced individuals Research has suggested that the majority of deaths occur in the homes of themselves or another. Another person was often present At time of death almost 90% of individuals were found to have an opioid drug present in their system What does this mean? If naloxone had been available and those present equipped to use it, some of these lives may have been saved
Drug Overdose Associated Drugs – Depressant Drugs The most common drug identified in a drug-related death are DEPRESSANTS sometimes known as “DOWNERS” These include: The OPIOID group of drugs which includes heroin, prescription medications such as methadone, Suboxone® , morphine and dihydrocodeine and some ‘Over the Counter’ (OTC) medicines (e. g. those containing codeine) BENZODIAZEPINES (examples include diazepam, alprazolam (Xanax) and temazepam) ALCOHOL Depressant drugs act on the Central Nervous System (CNS) causing respiratory depression which can lead to organ failure and death Combining more than one depressant drug increases the risk of overdose There are further substances which are becoming more commonly used and have an unknown or unpredictable effect on overdose risk e. g. Gabapentin, phenazepam, etizolam and the new psychoactive substances.
Drug Overdose Associated Drugs – Stimulant drugs In Scotland, stimulant drugs feature much less commonly in drug deaths than depressant drugs Death through use of stimulant drugs is more likely to be as a result of an acute cardiac event, grossly increased body temperature or convulsions The risk of drug death increases when used in combination with other drugs including depressant drugs and alcohol STIMULANT drugs include (but are not limited to): Cocaine, Crack Cocaine, MDMA (Ecstasy), Amphetamines (e. g. Speed), many new psychoactive substances (formerly known as “legal highs”) Naloxone will NOT reverse the effects of stimulant drugs
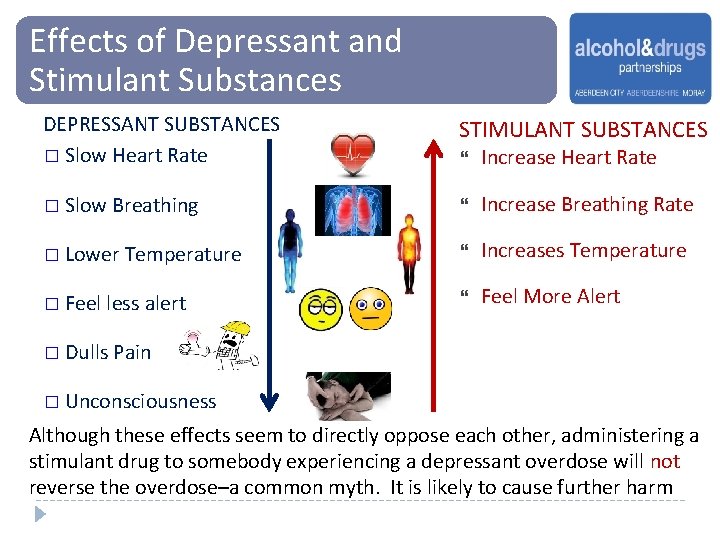
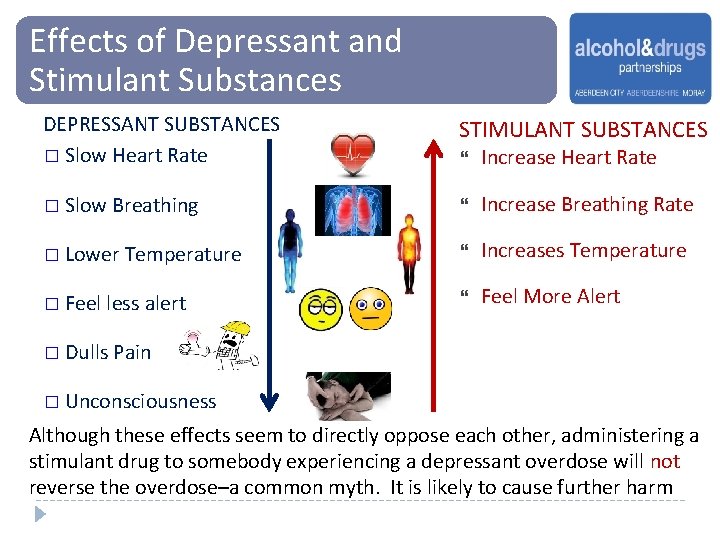
Effects of Depressant and Stimulant Substances DEPRESSANT SUBSTANCES � Slow Heart Rate STIMULANT SUBSTANCES Increase Heart Rate � Slow Breathing Increase Breathing Rate � Lower Temperature Increases Temperature � Feel less alert Feel More Alert � Dulls Pain � Unconsciousness Although these effects seem to directly oppose each other, administering a stimulant drug to somebody experiencing a depressant overdose will not reverse the overdose–a common myth. It is likely to cause further harm
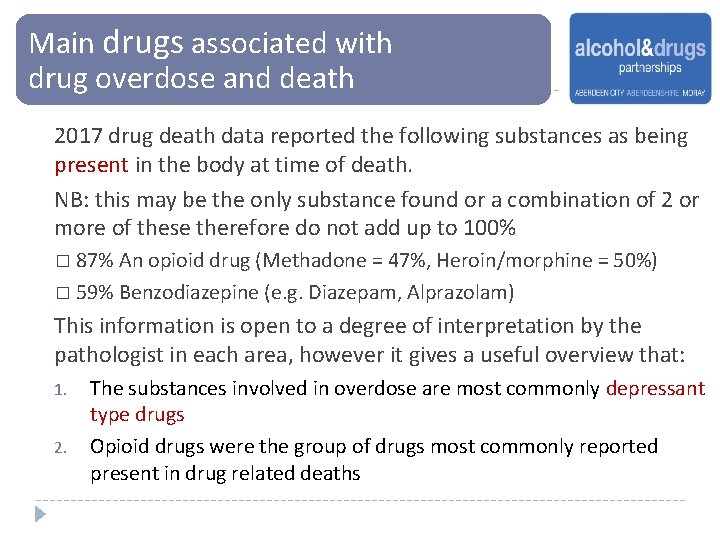
Main drugs associated with drug overdose and death 2017 drug death data reported the following substances as being present in the body at time of death. NB: this may be the only substance found or a combination of 2 or more of these therefore do not add up to 100% � 87% An opioid drug (Methadone = 47%, Heroin/morphine = 50%) � 59% Benzodiazepine (e. g. Diazepam, Alprazolam) This information is open to a degree of interpretation by the pathologist in each area, however it gives a useful overview that: 1. 2. The substances involved in overdose are most commonly depressant type drugs Opioid drugs were the group of drugs most commonly reported present in drug related deaths
Risk Factors The two key risk factors in overdose and drug death are reduced tolerance and poly-drug use 1. REDUCED TOLERANCE As our bodies get used to the repeated presence of a drug and learn to tolerate it, a higher dose is needed to maintain the same effect. Tolerance will be reduced if there is a break or reduction in drug use for a period. There will be a risk of overdose if individuals return to high levels of drug use following a break or reduction in consumption. This is a key cause of overdose and drug death
Risk Factors Risk 2. POLY-DRUG USE (INCLUDING ALCOHOL) Mixing drugs, especially depressants, is extremely dangerous. Each depressant on its own can slow down breathing and heart rate – but when used in combination these physical effects become enhanced and much more dangerous. The long-acting nature of some depressant drugs can also lead to the risk of unintentional “topping up” or poly-drug misuse
Risk Factors The following circumstances increase likelihood of overdose and death: Using too much of a substance/substances Varying levels of purity of the substance(s) Using alone (No-one around to help or administer naloxone. Isolation and loneliness are also contributing factors) Injecting Drug Use (Overdose is still a risk with other routes but marginally less e. g. Smoking may help control rate/amount of drug consumed a bit better) Longer history of drug use & history of non-fatal overdose - older people can be an especially vulnerable group Poor mental and/or physical health Homelessness (consider environment where person is using) Not being in treatment/supported/disconnected
Risk Factors The following are higher risk times when individuals may be more at risk of overdose: On release from prison (tolerance low, fail to access service etc) On leaving residential rehabilitation or hospital Following recent detoxification During a period of relapse After a recent life event (May be positive e. g. coming into money or negative e. g. bereavement, relationship breakdown etc) Following a change in social circumstances e. g. Loss of tenancy or job During festive periods, weekends & holidays (Positive e. g. Celebration/“reward” or negative e. g. Loneliness, isolation, services not available etc)
Commonly held myths on how to reverse an opioid overdose Clients often have their own beliefs about what reverses an overdose. This can be based on previous personal experience or that of their peers. Common myths include, but are not limited to: Walking the casualty around (risk of further injury) Inflicting pain (will not be felt by someone who is unconscious or who has taken a strong painkiller such as heroin) Injecting stimulant drugs (stimulant drugs cannot counteract or reverse effects of opioid overdose) Injecting salty water (there is sometimes (client) confusion that this is similar to a hospital saline drip) Throwing water or put casualty in bath / shower (trigger shock or accidental drowning) Putting the casualty outside (risk of hypothermia)
Addressing Client Myths It is important to investigate and set straight any myths. Even if these actions appear to have worked in the past this is likely to be coincidental and the amount of drugs consumed was not enough to result in a fatal overdose Stress the importance of taking immediate action if faced with an overdose situation and encourage clients to take the actions described in the next few slides.
How does opioid overdose kill? Opioid drugs (and other respiratory depressants) depress the Central Nervous System which can lead to: Dyspnoea (breathing difficult or laboured can sound like snoring or rattle in chest) Apnoea (breathing stops) Cardiac Arrest (heart stops due to lack of oxygen) Circulatory Collapse (circulation of blood around the body and to the brain stops) Body can no longer function and death occurs

Observable Signs &Symptoms Watch film “Signs and symptoms of an opioid overdose” (Click Logo)
What are Appropriate Actions? Follow the “S. A. F. E. ” approach: SHOUT for help APPROACH with care Ensure area is FREE from danger EVALUATE if safe to take action Be vigilant of any present hazards to both yourself and the casualty e. g. discarded needles
What are Appropriate Actions? Dial 999 Ask calmly for an ambulance Give the location and status of the casualty. EITHER. . “. . . unconscious but breathing” OR. . “. . . unconscious and not breathing” Stay with the person until the ambulance arrives
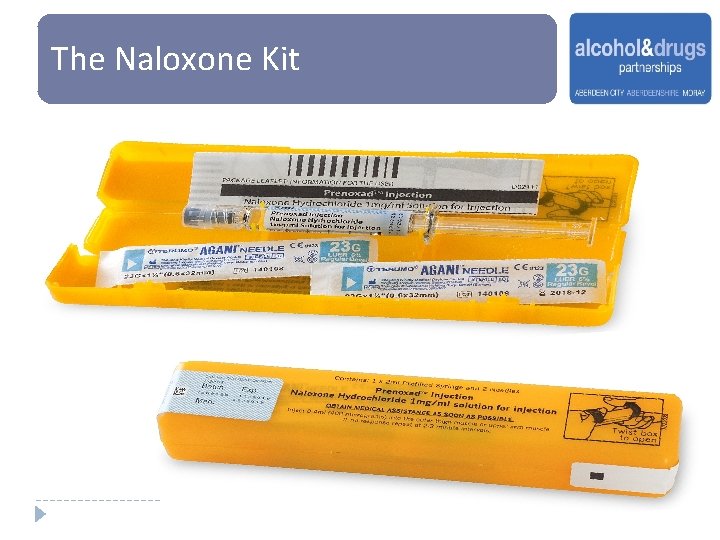
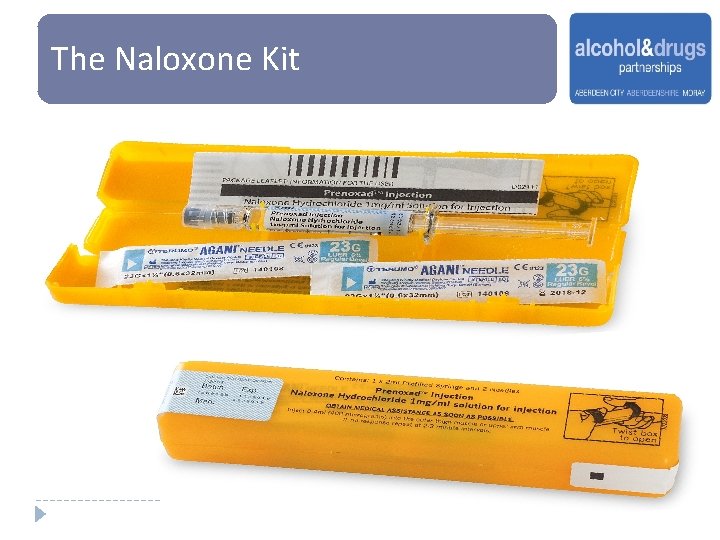
The Naloxone Kit
What is Naloxone? Naloxone is a pure opioid antagonist It is intended for administration to people who are not responding following an overdose of opioid drugs It works by attaching onto opioid receptors in brain and will remove, replace and block any opioid drugs which are on these receptors This can help restore consciousness and breathing It can temporarily reverse the effects of overdose if used soon enough There are no exclusions from using naloxone if opioid overdose is suspected. Failing to administer naloxone may result in death
Naloxone - FACTS Naloxone cannot make someone intoxicated / high It is a very safe drug which has been used for decades to reverse the effects of opioid overdose It is a Prescription only Medication for opioid overdose currently licensed for administration subcutaneous, intramuscular or intravenous injection Legislation now exists which allows it to be supplied by any drug treatment service, including needle exchanges and community pharmacies without the need for a prescription or Patient Group Direction It can be supplied to individuals at risk of overdose, their significant others and services in contact with those at risk
Naloxone - FACTS The effects of naloxone will begin to wear off after approximately 30 minutes. Opioid drugs can then reattach to the receptors and the effects of the opioid drug can return It will not reverse the effect of benzodiazepines or alcohol (although these may of course contribute to the overdose effect) It does not rid the body of opioid drugs It can buy time until an ambulance arrives
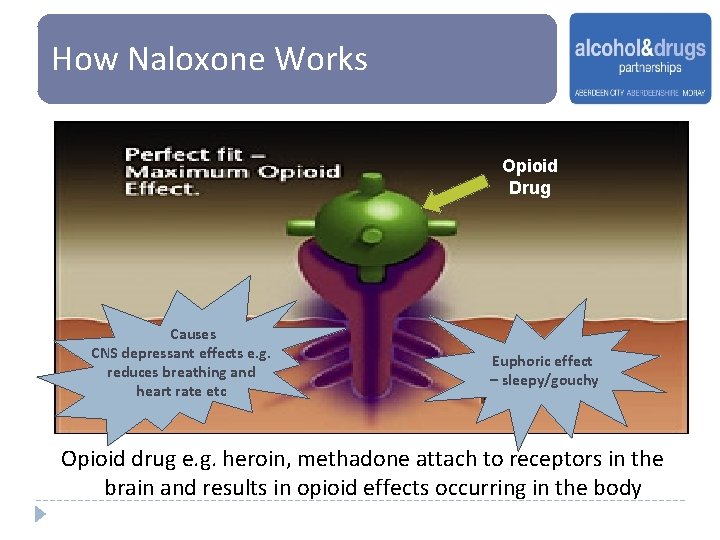
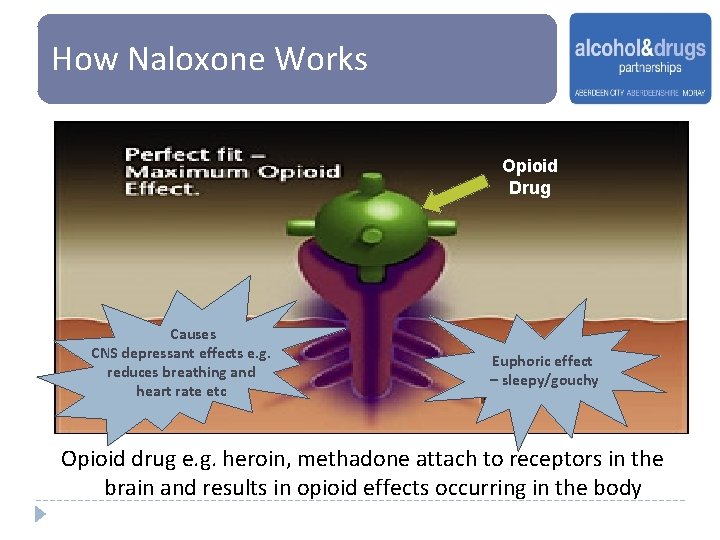
How Naloxone Works Opioid Drug Causes CNS depressant effects e. g. reduces breathing and heart rate etc Euphoric effect – sleepy/gouchy Opioid drug e. g. heroin, methadone attach to receptors in the brain and results in opioid effects occurring in the body
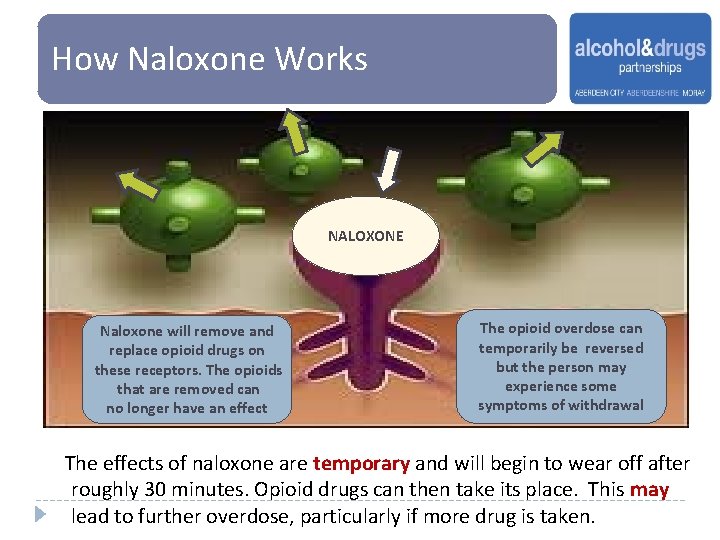
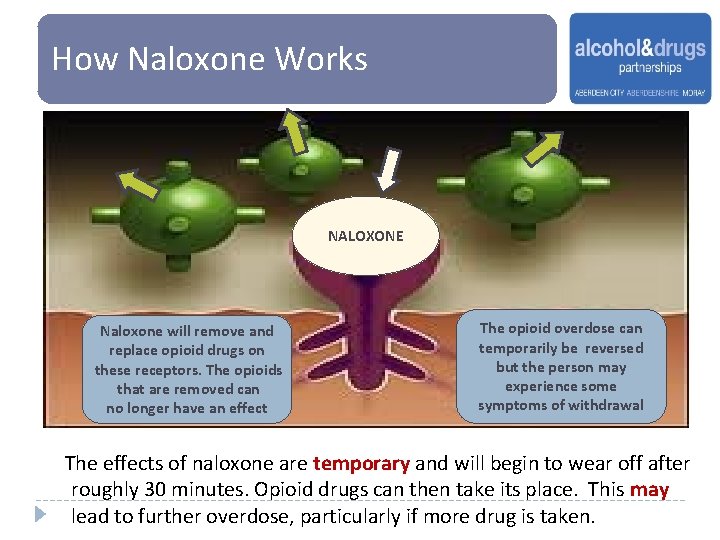
How Naloxone Works NALOXONE Naloxone will remove and replace opioid drugs on these receptors. The opioids that are removed can no longer have an effect The opioid overdose can temporarily be reversed but the person may experience some symptoms of withdrawal The effects of naloxone are temporary and will begin to wear off after roughly 30 minutes. Opioid drugs can then take its place. This may lead to further overdose, particularly if more drug is taken.
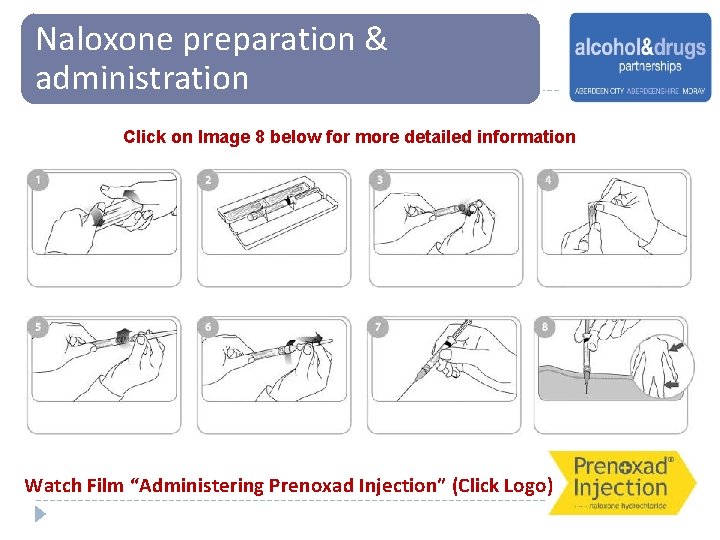
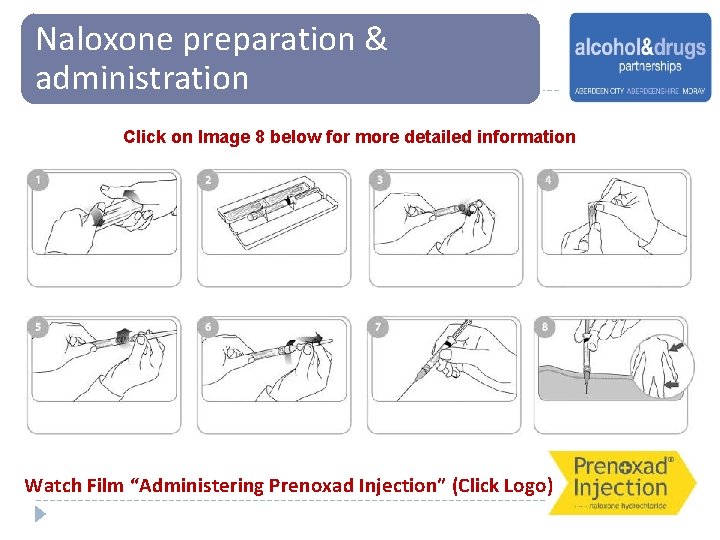
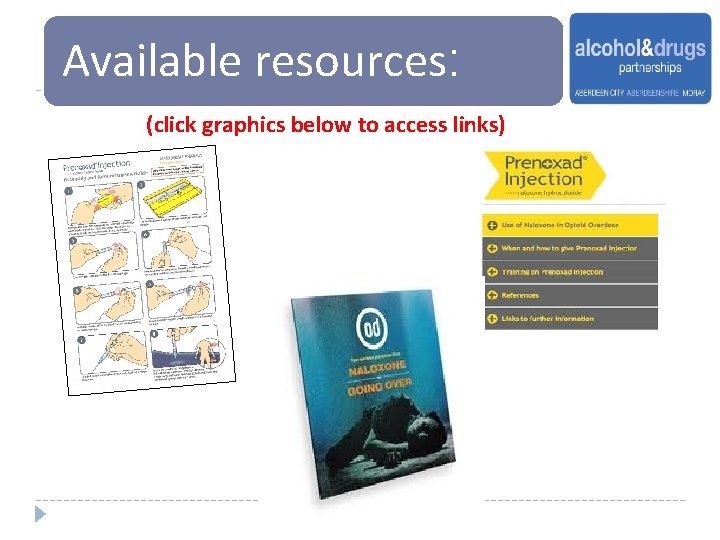
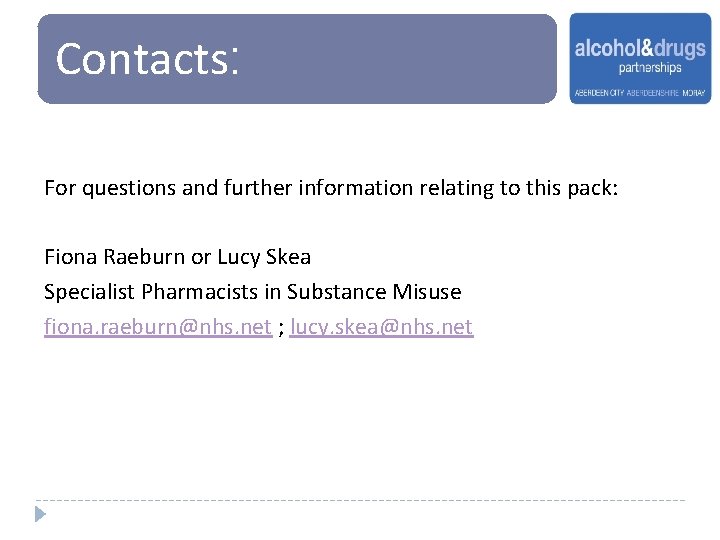
Naloxone preparation & administration Click on Image 8 below for more detailed information Watch Film “Administering Prenoxad Injection” (Click Logo)
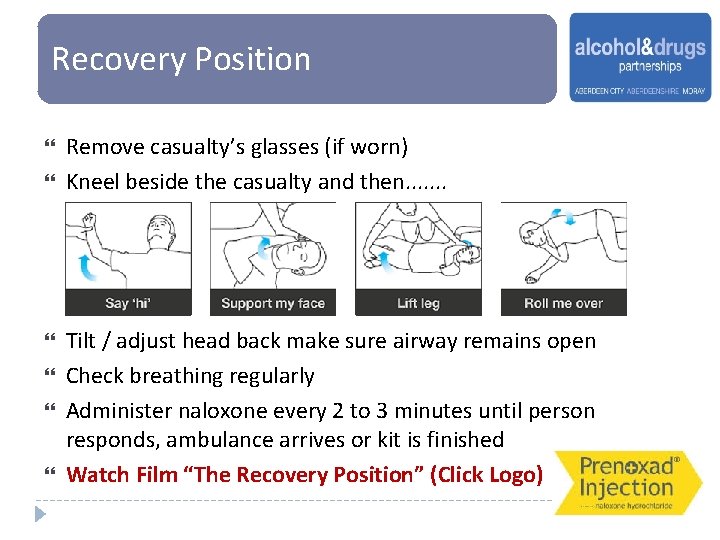
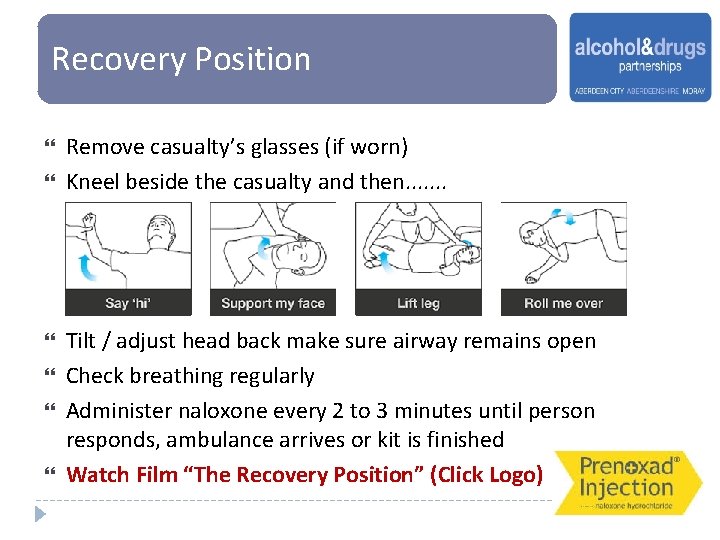
Recovery Position Remove casualty’s glasses (if worn) Kneel beside the casualty and then. . . . Tilt / adjust head back make sure airway remains open Check breathing regularly Administer naloxone every 2 to 3 minutes until person responds, ambulance arrives or kit is finished Watch Film “The Recovery Position” (Click Logo)
Principles of Basic Life Support To maintain a clear airway To support breathing – using rescue breaths The person is at risk of dying from a lack of oxygen due to respiratory depression therefore rescue breaths are recommended wherever possible To support circulation – using chest compressions
Basic Life Support Actions Look, Listen & Feel for normal breathing Watch chest for signs of movement – no more than 10 seconds is required No evidence of breathing 30 Compressions followed by 2 Rescue Breaths Continue process until emergency services arrive or casualty’s condition improves Watch Film “Performing CPR” (Click Logo) start resuscitation
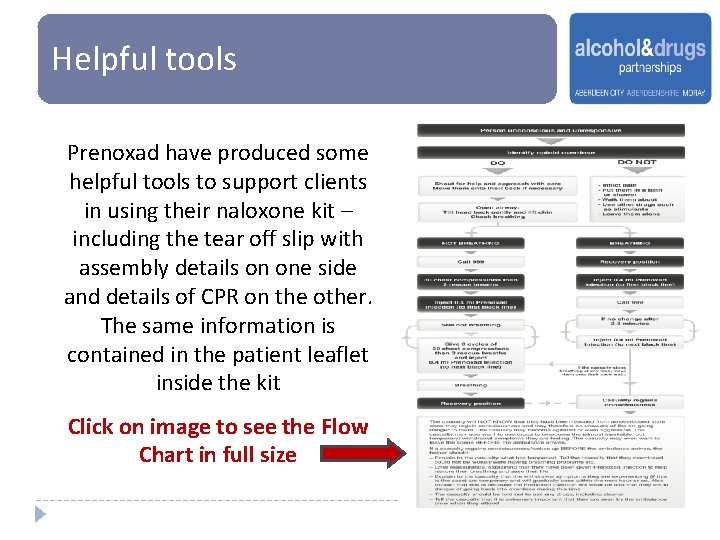
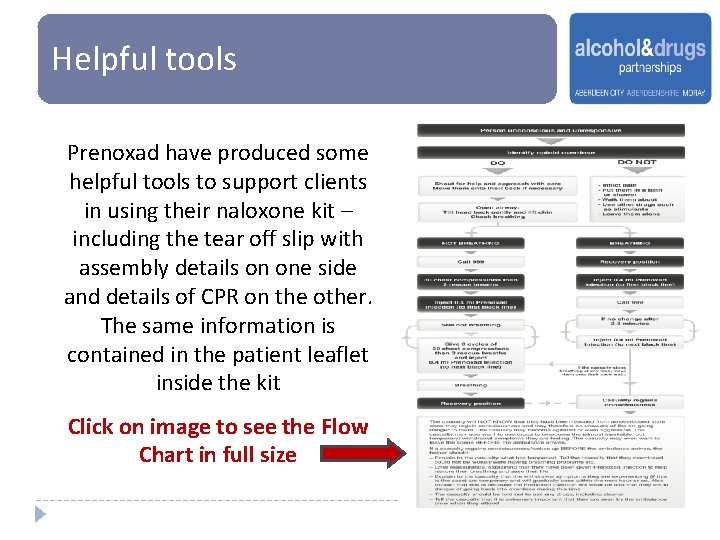
Helpful tools Prenoxad have produced some helpful tools to support clients in using their naloxone kit – including the tear off slip with assembly details on one side and details of CPR on the other. The same information is contained in the patient leaflet inside the kit Click on image to see the Flow Chart in full size
Preparation – Face 2 Face Training Session On completion of Pre-reading, a face-2 -face session will take place. This will cover: Pre-reading recap & quiz How to use the Naloxone kit Recovery Position & Basic Life Support demonstration How to deliver the intervention in practice Making naloxone supplies Guidance and Documentation
Further Reading Links SDF Scottish National Naloxone Website: http: //www. naloxone. org. uk Overview of changes in naloxone legislation (PHE, 2015) http: //www. naloxone. org. uk/index. php/lawpolicy/law/uklaw 1 Public Health England (PHE), Health Matters Tool/Website https: //publichealthmatters. blog. gov. uk/2017/03/01/health-matters-preventing-drugmisuse-deaths/ Care Inspectorate - Health Guidance: Take Home Naloxone in Social Care Services http: //www. careinspectorate. com/images/documents/3203/Take%20 Home%20 Naloxon e%20 in%20 Social%20 Care%20 Services. pdf Adult Learning Styles: http: //www. exploreadultlearning. co. uk/the-different-learning-styles-explained. html
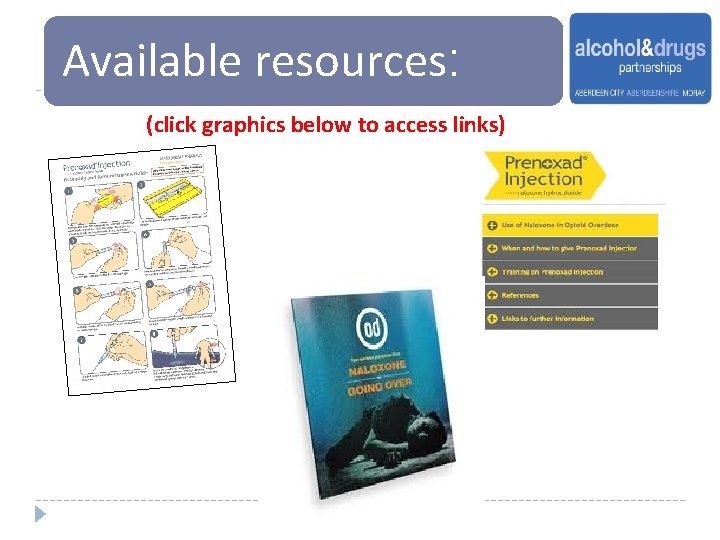
Available resources: (click graphics below to access links)
Contacts: For questions and further information relating to this pack: Fiona Raeburn or Lucy Skea Specialist Pharmacists in Substance Misuse fiona. raeburn@nhs. net ; lucy. skea@nhs. net