GET SMART A Radiologists Guide to SMART Syndrome












- Slides: 40
GET SMART: A Radiologist’s Guide to SMART Syndrome e. Ed. E-79 1: Department of Radiology 2. Department of Pathology Wilson Altmeyer, MD 1 Achint Singh, MD 1 Bundhit Tantiwongkosi, MD 1 Viet Nguyen, MD 1 Carlos Bazan, MD 1 James Henry, MD 2
Disclosure Statement • The authors have no financial interests to disclose
Table of Contents Click on below to proceed directly to section of choice. BACKGROUND CLINICAL MANIFESTATIONS RADIOLOGICAL APPEARANCE HISTIOLOGICAL APPEARANCE TREATMENT PROGNOSIS CASES TAKE HOME POINTS
What is SMART Syndrome • Stroke-like Migraine Attacks after Radiation Therapy • Approximately 50 reported cases in literature • SMART syndrome is a presumed DELAYED manifestation of cranial radiation (whole brain or focal XRT) • Patients present with complex neurological symptoms
History of SMART Syndrome • 1995: “Migraine-like episodes” and pediatric cranial radiation are linked • 2003: The term “stroke-like migraine attacks” is first coined and the delayed relationship (years to decades) between radiation and syndrome is elucidated • 2006: “SMART Syndrome” acronym is adopted
Clinical Manifestations • Subacute onset of symptoms 1. Migraine type headaches 2. Seizures 3. Stroke-like deficits • • Hemiplegia Aphasia Visual field defect Altered mental status • Delayed time interval between radiation and SMART syndrome development: 2 to 30 years

Irradiated Tumors Smart syndrome has followed cranial radiation for the treatment of a wide range of intracranial neoplasms, including: • • • Medulloblastoma Ependymoma Astrocytoma Pineoblastoma Dysgerminoma • • • Astroblastoma Lymphoma Oligoastrocytoma PNET Metastatic disease

Radiographic Appearance • HALLMARKS: 1. Cortical T 2 hyperintensity 2. Gyriform, cortical enhancement – Location • Does not respect vascular borders • Typically located in the occipital and dorsal temporoparietal lobes • Spares the subcortical white matter • Spares the frontal lobes • +/- Associated restricted diffusion • MRI abnormalities typically resolve with clinical improvement
Laboratory & Histologic Findings • Laboratory Findings – Normal in SMART syndrome – Lumbar puncture is unremarkable – Helpful in excluding infection • Histological Findings – Nonspecific – Pathophysiology poorly understood – Gliosis with perivascular infiltrates reported
Treatment • Very little data on the treatment of SMART syndrome • No clear consensus on treatment regimen • Treatments reported in the literature – Steroids – Anti-epileptic agents – Pain medication (for headaches)
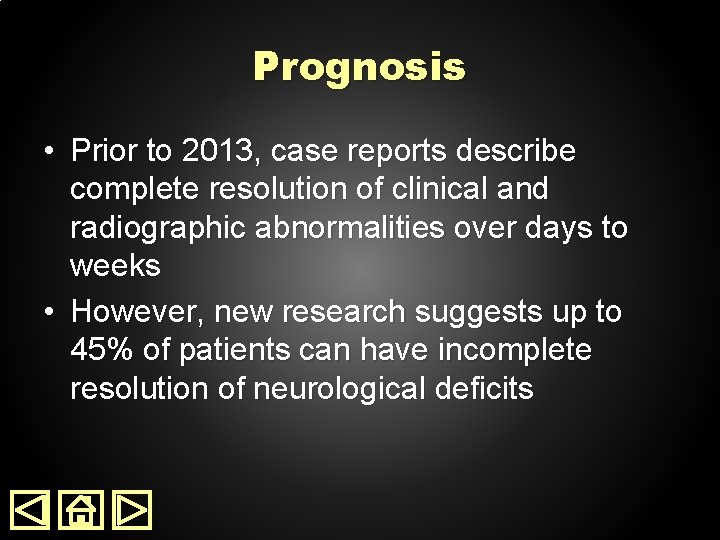
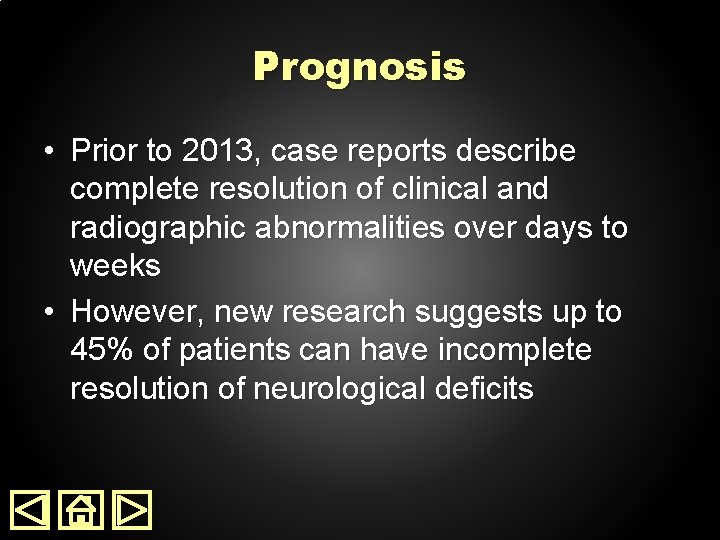
Prognosis • Prior to 2013, case reports describe complete resolution of clinical and radiographic abnormalities over days to weeks • However, new research suggests up to 45% of patients can have incomplete resolution of neurological deficits

Case #1 • 26 y/o with 5 -day history of – Vision disturbance • Loss of color progressing to frank blindness – Severe frontal headaches – Worsening seizures • Past medical history – Left parietal neurocytoma resected at age 7 – Patient received chemotherapy and radiation

Case #1 • Physical Examination – Ophthalmological examination • 0/15 recognition of color plates • Impaired visual acuity • Normal pupillary reflex color plate – Otherwise, neurologically intact. • Laboratory Work-up – Unremarkable – RPR, HIV, SS-A, SS-B, ANA, ACE, Lyme test all negative
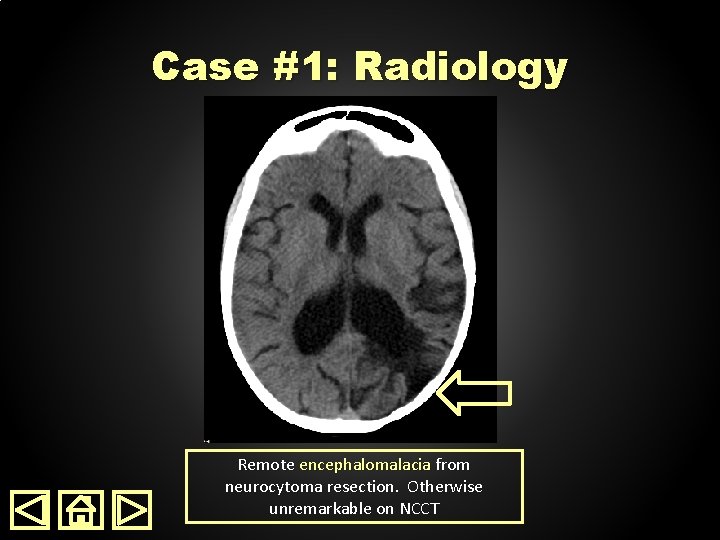
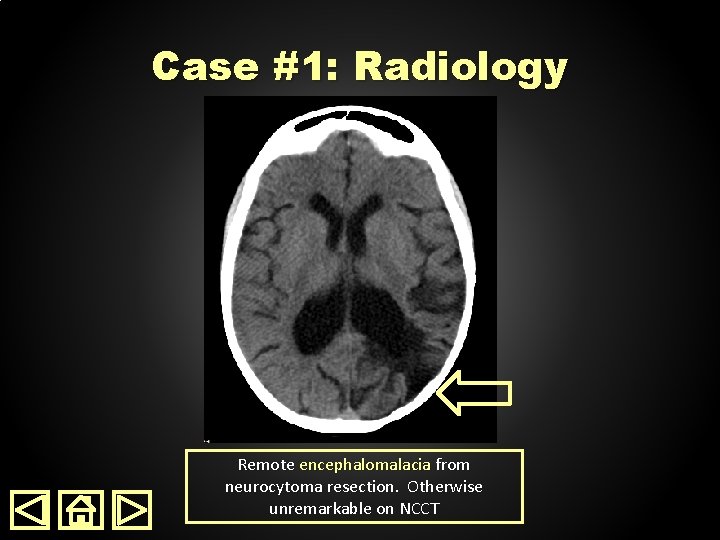
Case #1: Radiology Remote encephalomalacia from neurocytoma resection. Otherwise unremarkable on NCCT
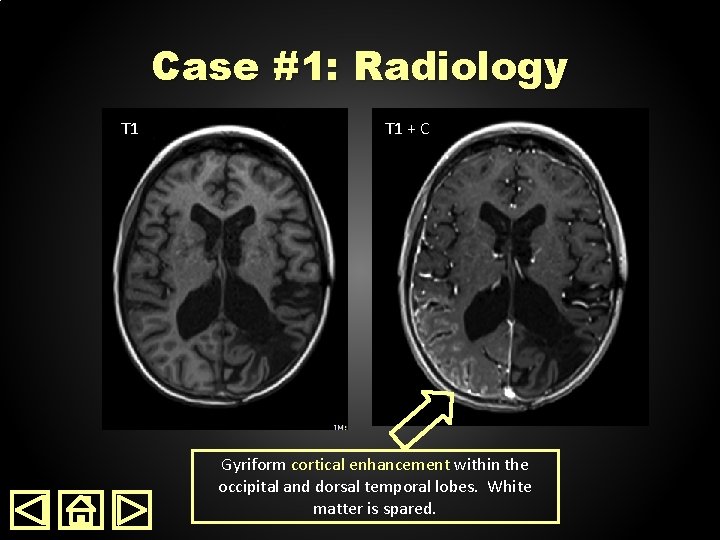
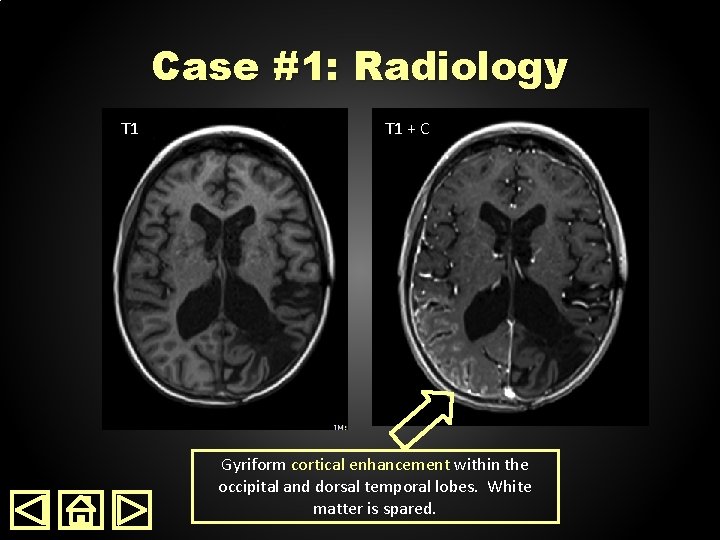
Case #1: Radiology T 1 + C Gyriform cortical enhancement within the occipital and dorsal temporal lobes. White matter is spared.

Case #1: Radiology FLAIR T 2 & FLAIR demonstrate no obvious changes in the region of gyriform enhancement
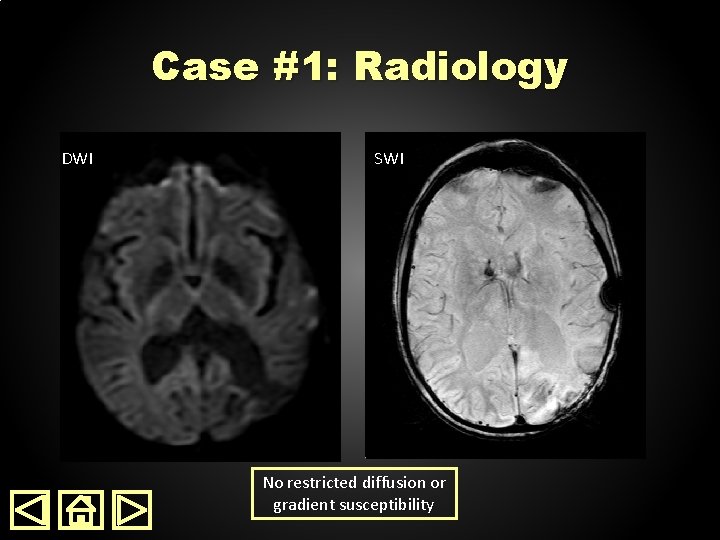
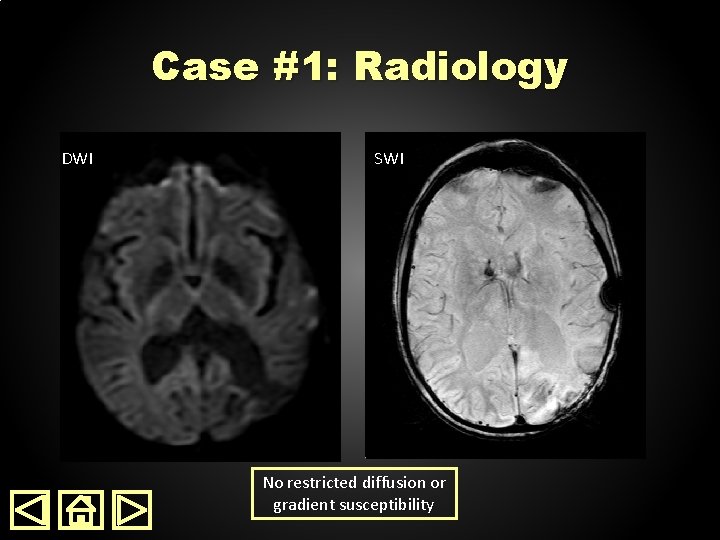
Case #1: Radiology DWI SWI No restricted diffusion or gradient susceptibility
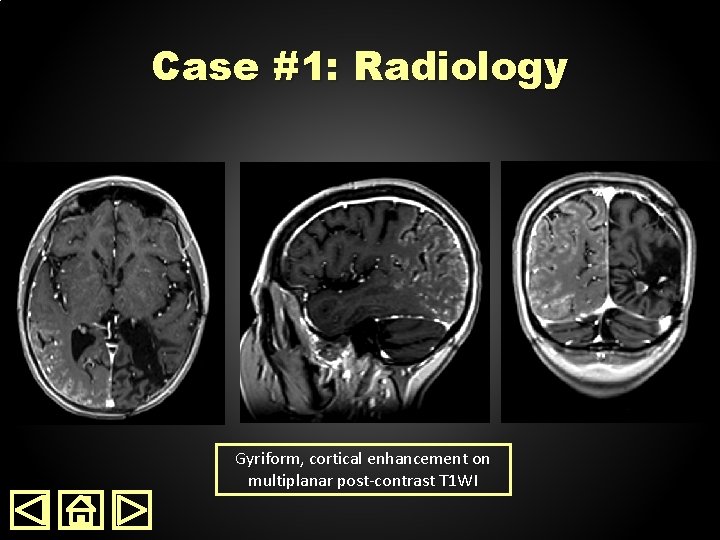
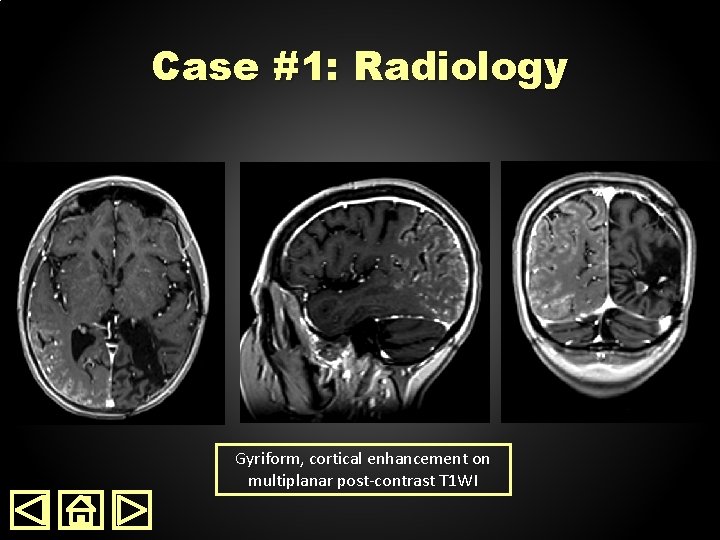
Case #1: Radiology Gyriform, cortical enhancement on multiplanar post-contrast T 1 WI
Radiology DDx Provided • • • Meningoencephalitis Post ictal/migraine change SMART Syndrome
Hospital Course • Treatment – Dexamethasone – Keppra BID • Patient hospitalized for 5 days • Headaches resolved • Vision deficit showed incomplete resolution • No brain biopsy (as patient was presumptively given diagnosis of SMART Syndrome)
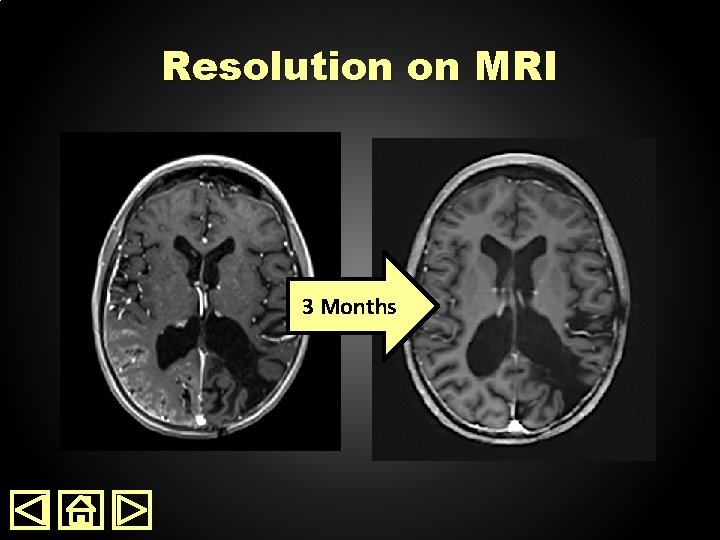
3 Month Follow Up • All symptoms have completely resolved • Repeat MRI showed resolution of cortical enhancement
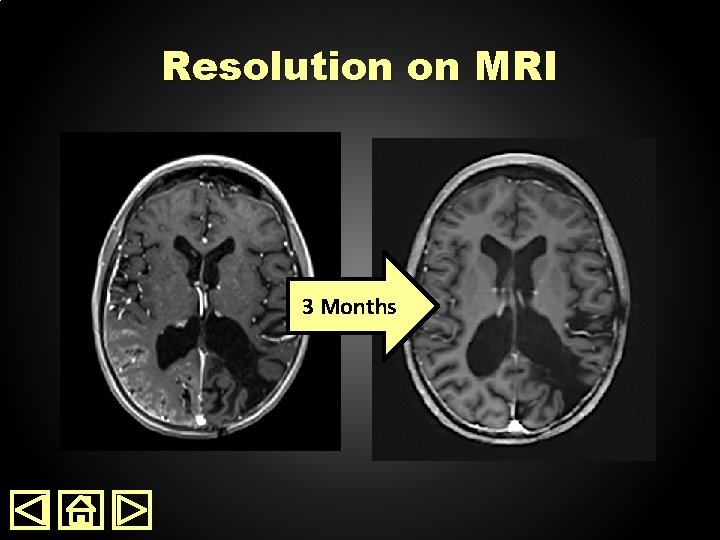
Resolution on MRI 3 Months

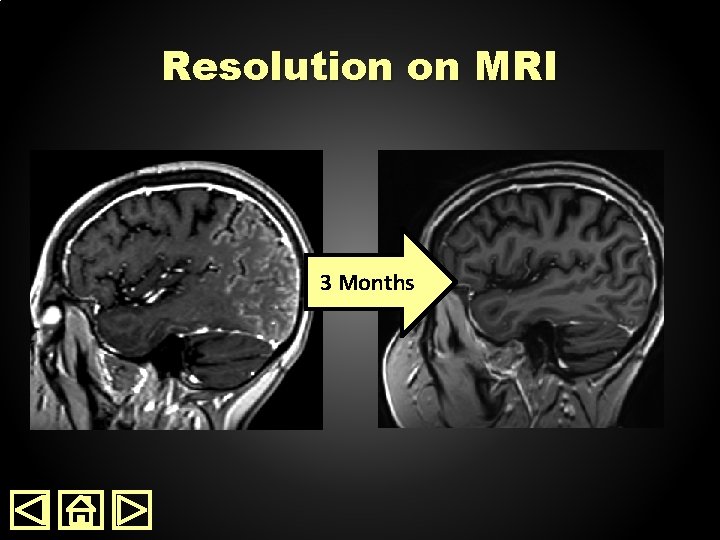
Resolution on MRI 3 Months
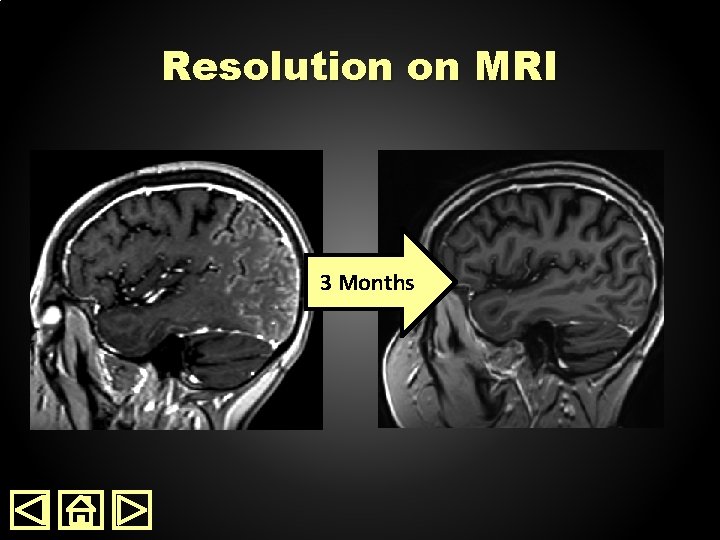
Resolution on MRI 3 Months
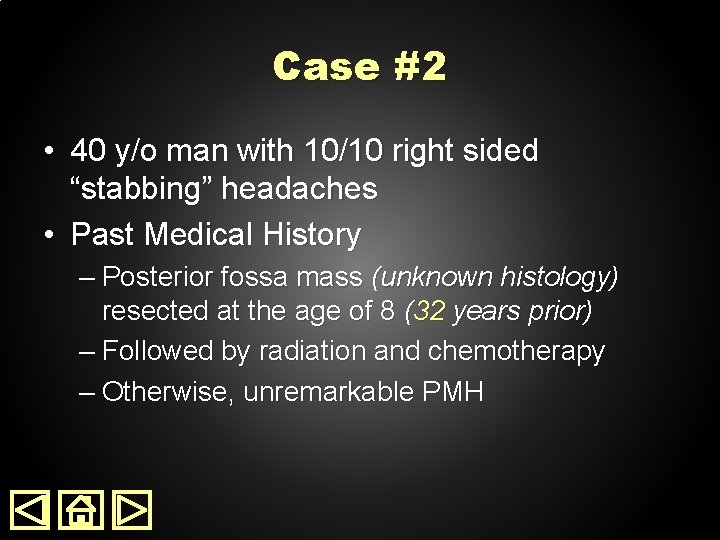
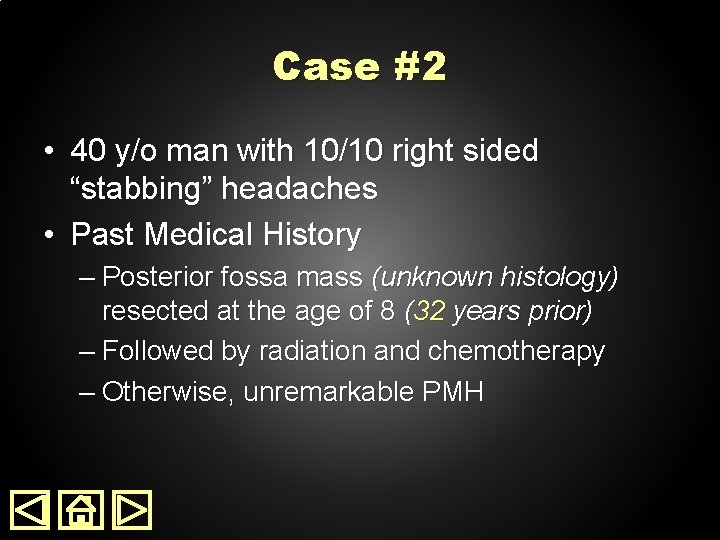
Case #2 • 40 y/o man with 10/10 right sided “stabbing” headaches • Past Medical History – Posterior fossa mass (unknown histology) resected at the age of 8 (32 years prior) – Followed by radiation and chemotherapy – Otherwise, unremarkable PMH

Case #2 • Physical Examination – Unremarkable except minimal psychomotor slowing – Vital signs normal • Laboratory Evaluation – Serology normal • CMP, CBC, ANA panel, B 12, TSH, Ammonia, UA, ESR all normal – Lumbar puncture normal

Case #2: Radiology CT CT + C Non-contrast CT is unremarkable. Post contrast CT reveals subtle gyriform enhancement (particularly when displayed with narrow windows)

Case #2: Radiology T 1 FLAIR Remote encephalomalacia from posterior fossa mass resection 32 years prior
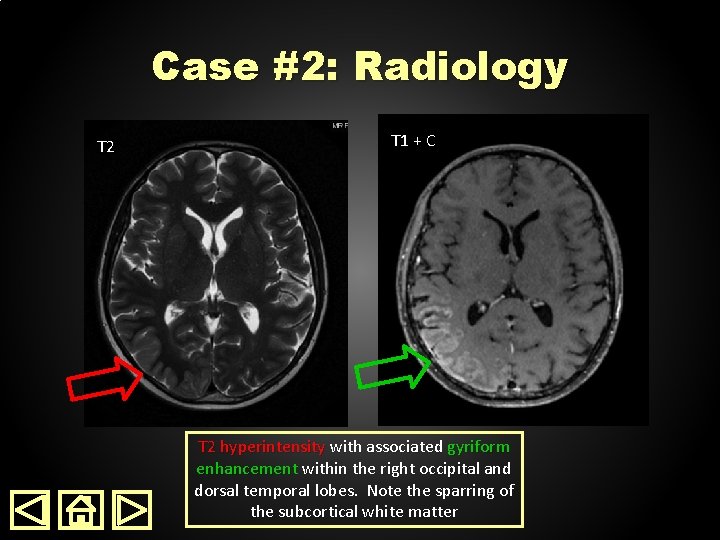
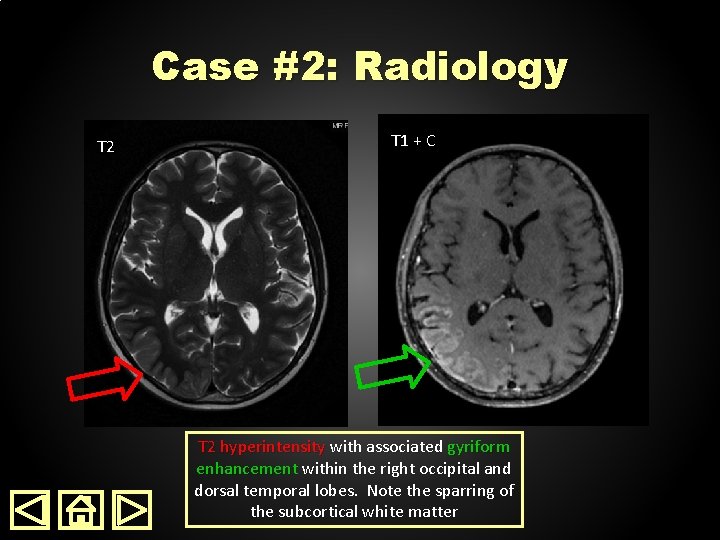
Case #2: Radiology T 2 T 1 + C T 2 hyperintensity with associated gyriform enhancement within the right occipital and dorsal temporal lobes. Note the sparring of the subcortical white matter

Case #2: Radiology DWI ADC Associated restricted diffusion on DWI and ADC map
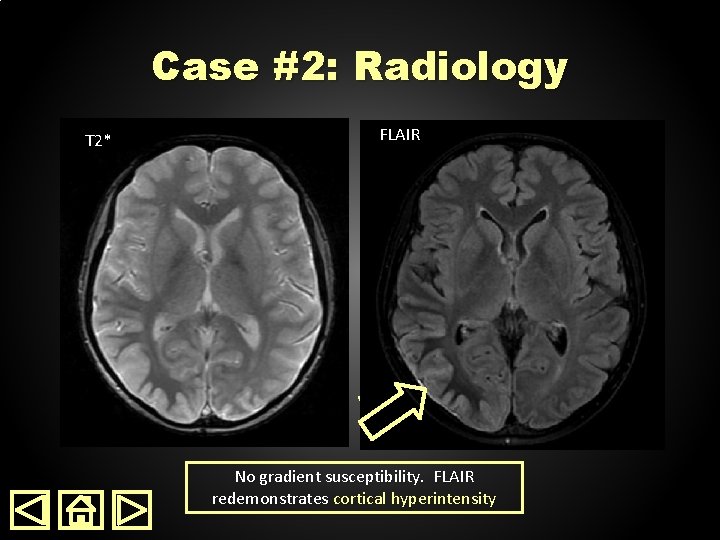
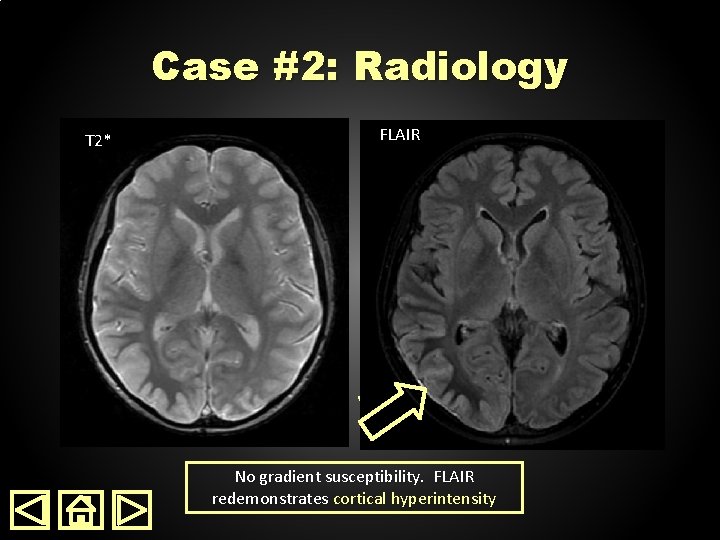
Case #2: Radiology T 2* FLAIR No gradient susceptibility. FLAIR redemonstrates cortical hyperintensity
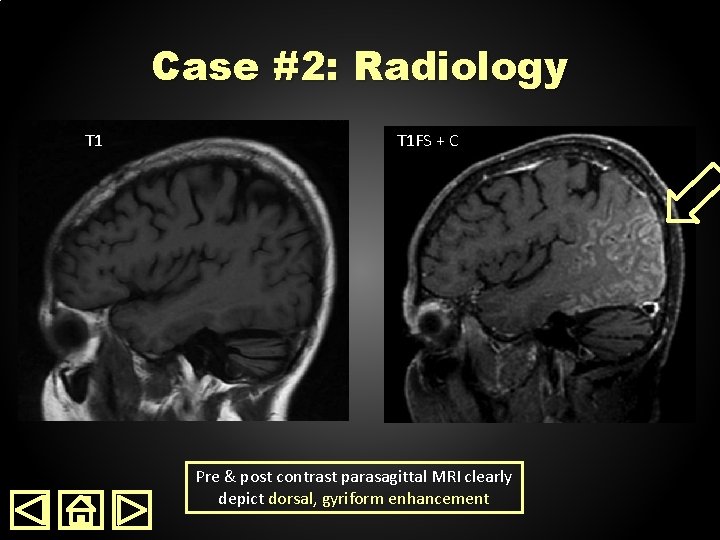
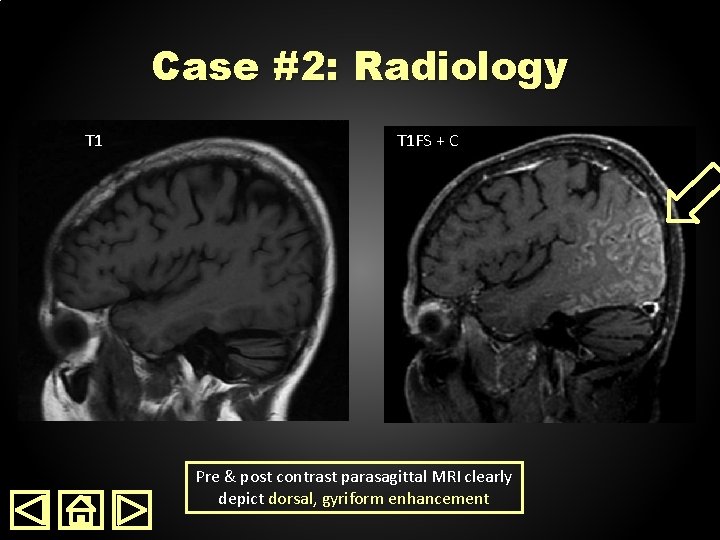
Case #2: Radiology T 1 FS + C Pre & post contrast parasagittal MRI clearly depict dorsal, gyriform enhancement
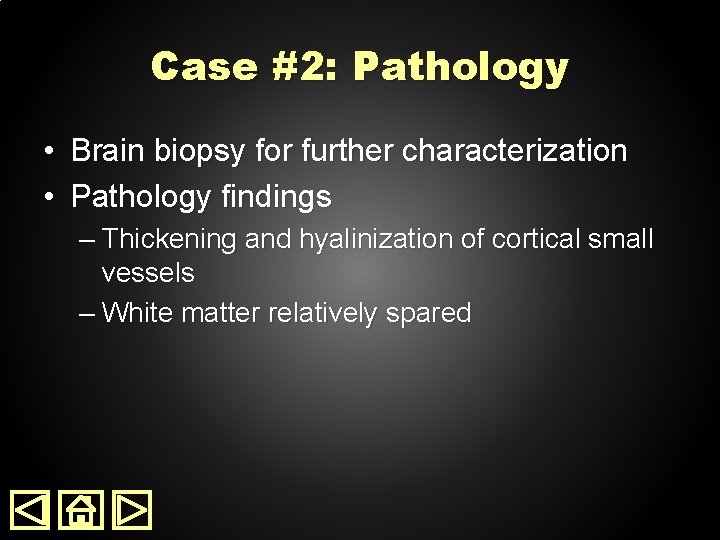
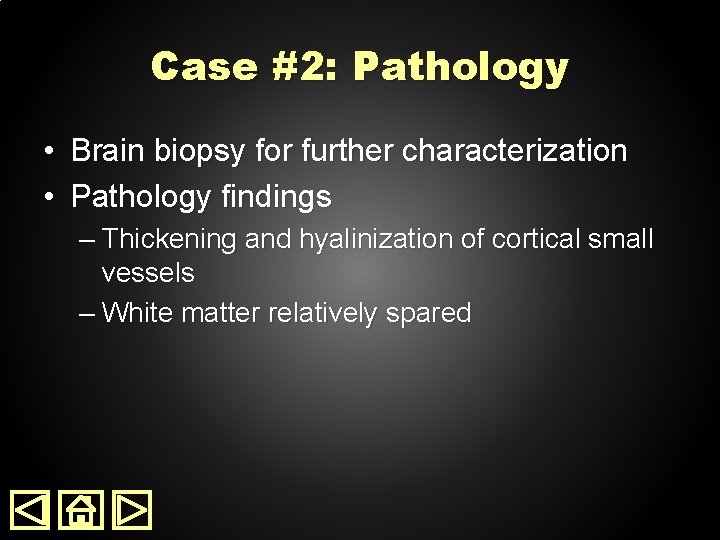
Case #2: Pathology • Brain biopsy for further characterization • Pathology findings – Thickening and hyalinization of cortical small vessels – White matter relatively spared
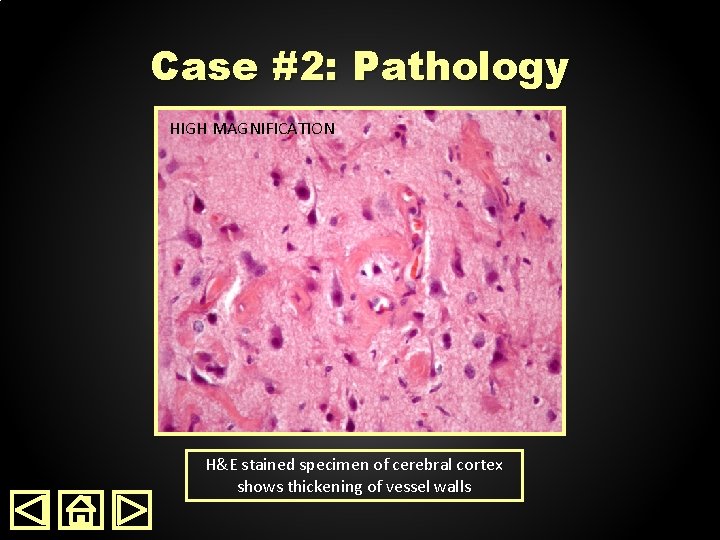
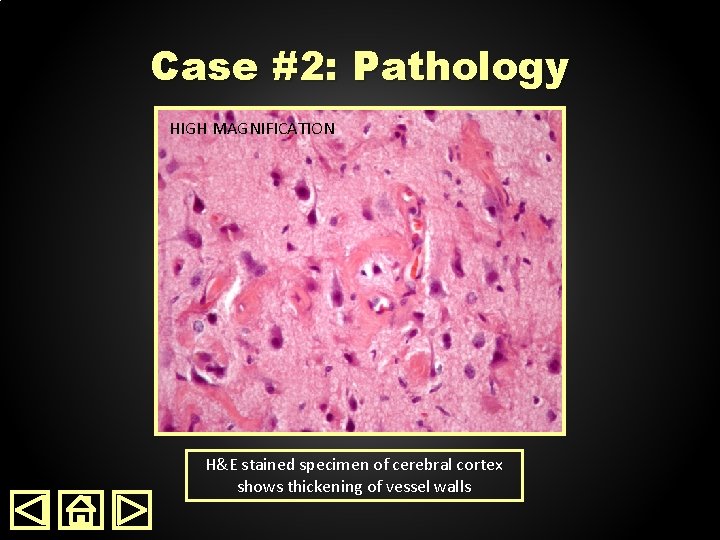
Case #2: Pathology HIGH LOWMAGNIFICATION H&E stained specimen of cerebral cortex shows thickening of vessel walls

Case #2: Pathology HIGH LOWMAGNIFICATION H&E stained specimen of cerebral cortex shows thickening of vessel walls
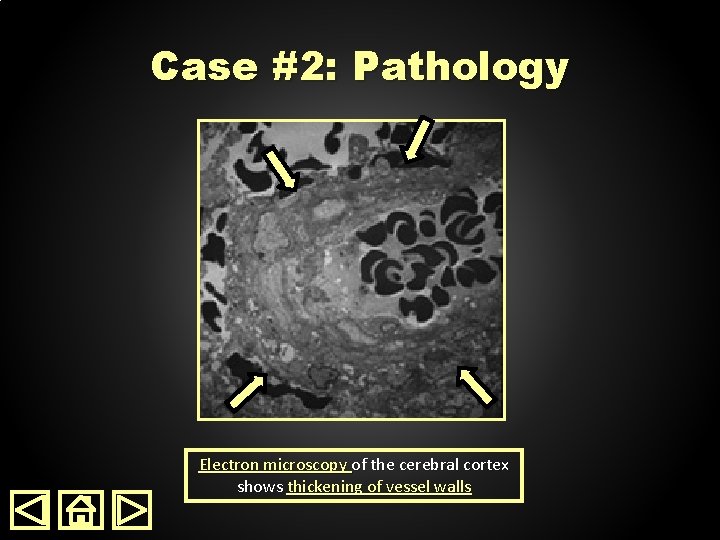
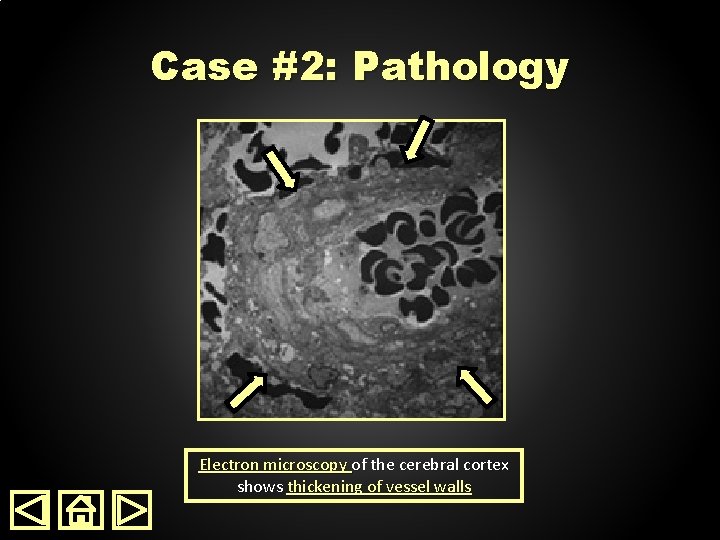
Case #2: Pathology Electron microscopy of the cerebral cortex shows thickening of vessel walls
Case #2 • Patient was diagnosed with SMART syndrome on the basis of: – Acute onset of migraine like headaches in the setting of prior cerebral radiation – Characteristic MRI findings – No infection or tumor found during work up – Brain biopsy demonstrating cortical vessel wall hyalinization and thickening – Complete resolution of headaches at follow-up neurology appointment
Take Home Point! • • • Cortical T 2 hyperintensity Gyriform enhancement Dorsal location in brain History of cerebral radiation Migraine type headache • CONSIDER SMART Syndrome
References 1. 2. 3. 4. 5. 6. 7. Bartleson JD, Krecke KN, O’Neill BP, et al. Reversible, strokelike migraine attacks in patients with previous radiation therapy. Neuro Oncol 2003; 5: 121– 7. Black DF, Bartleson JD, Bell ML, et al. SMART: stroke-like migraine attacks after radiation therapy. Cephalalgia 2006; 26: 1137– 42. Kerklaan JP, Lycklama á Nijeholt GJ, Wiggenraad RGJ, et al. SMART syndrome: a late reversible complication after radiation therapy for brain tumours. J Neurol 2011; 258: 1098– 104. Armstrong AE, Gillan E, Di. Mario FJ. SMART Syndrome (Stroke-Like Migraine Attacks After Radiation Therapy) in Adult and Pediatric Patients. J Child Neurol 2014; 29: 336– 41. Black DF, Morris JM, Lindell EP, et al. Stroke-Like Migraine Attacks after Radiation Therapy (SMART) Syndrome Is Not Always Completely Reversible: A Case Series. AJNR Am J Neuroradiol 2013; 34: 2298– 303. Zhang H-N, Zheng Q, Yang L, et al. Stroke-like Migraine Attacks after Radiation Therapy Syndrome. Chinese Medical Journal 2015; 128: 2097. Khanipour Roshan S, Salmela MB, Mc. Kinney AM. Susceptibility-weighted imaging in stroke-like migraine attacks after radiation therapy syndrome. Neuroradiology 2015; 57: 1103– 9.

THANKS FOR VIEWING OUR PRESENTATION Please send questions or comments to: altmeyer@uthscsa. edu