Family Medicine Resident School Lecture 4517 Ashley Crum







- Slides: 71
Family Medicine Resident School Lecture 4/5/17 Ashley Crum, MD Emergency Medicine/Sports Medicine Fellow
§ Identify common fractures in upper and lower extremities § Treatment § Urgent vs Non-urgent referal
§ Try to understand the mechanism of injury from the history § Always do a neurovascular exam before and after any manipulation § Do not push for ROM testing if you suspect a fracture until you have x-rays
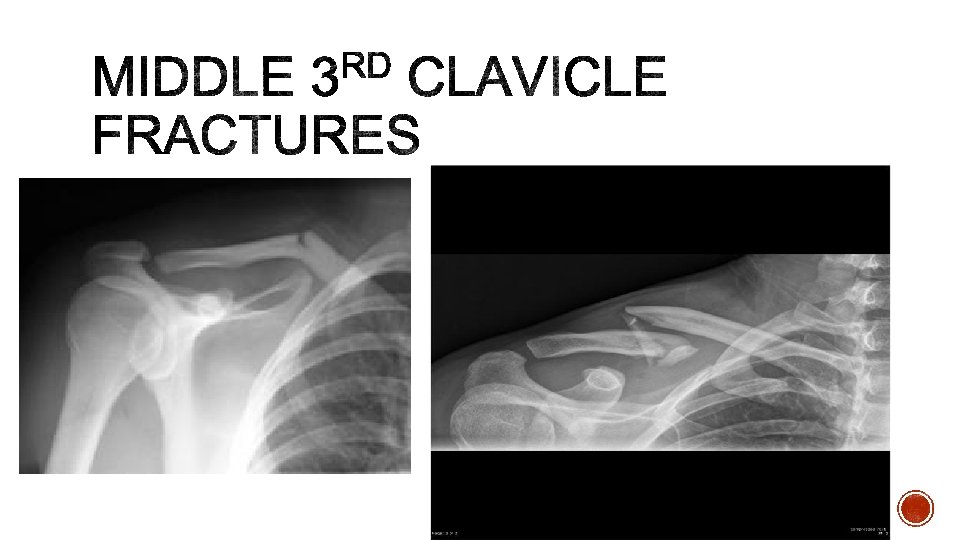
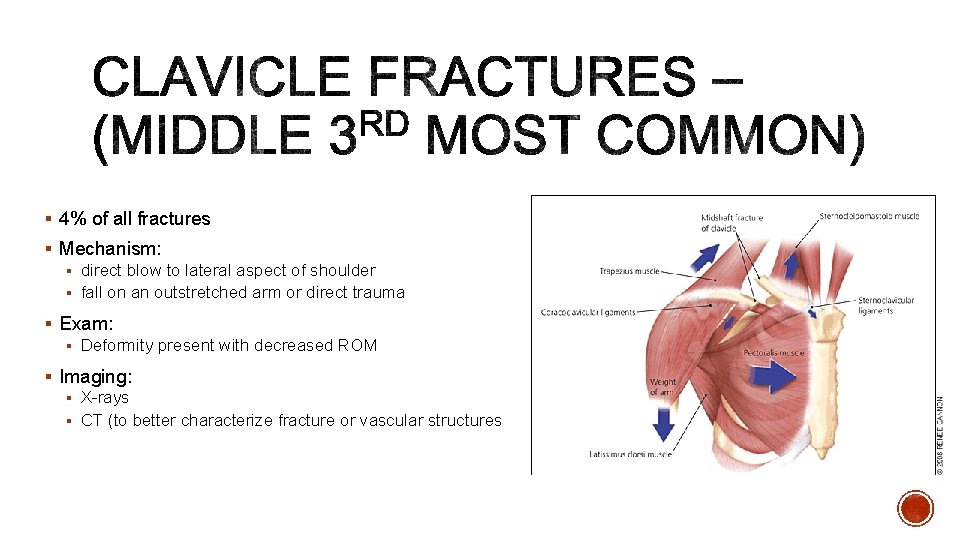
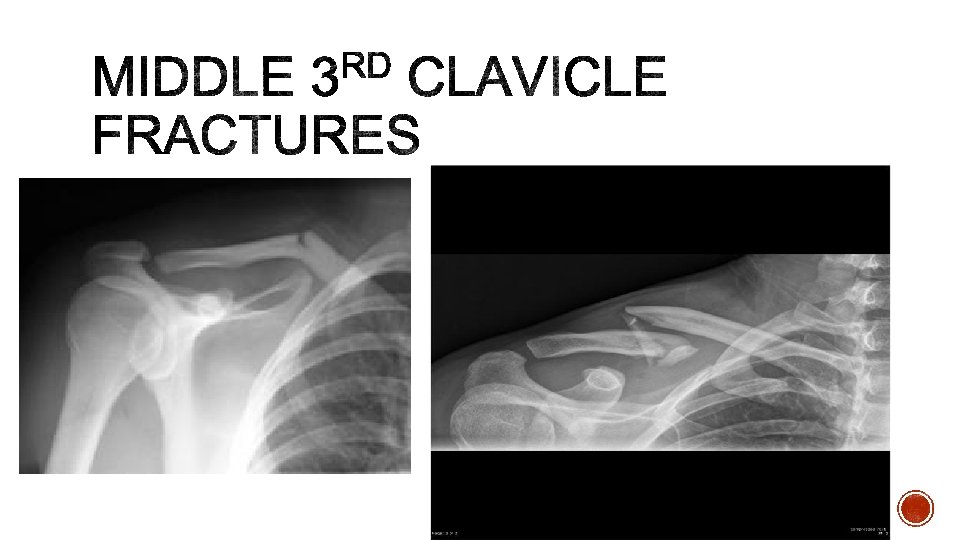
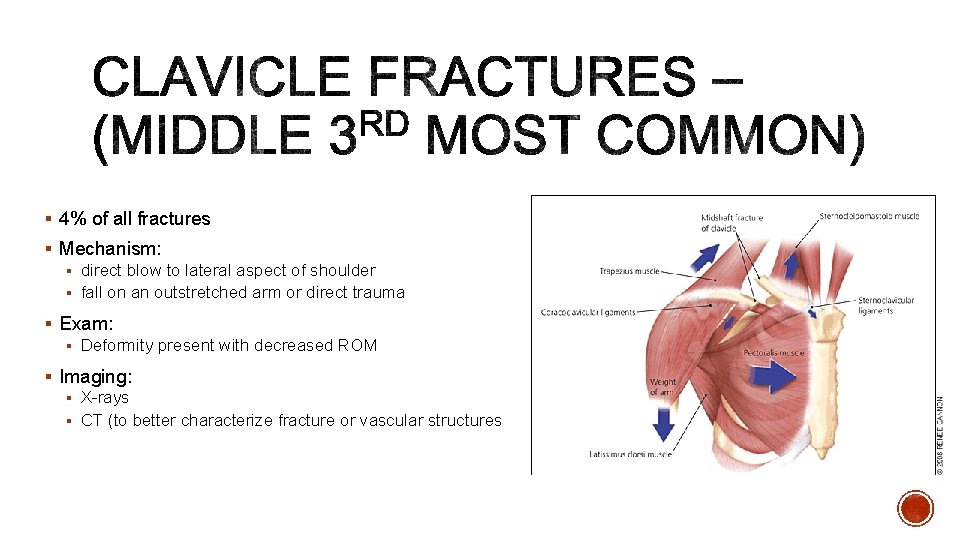
§ 4% of all fractures § Mechanism: § direct blow to lateral aspect of shoulder § fall on an outstretched arm or direct trauma § Exam: § Deformity present with decreased ROM § Imaging: § X-rays § CT (to better characterize fracture or vascular structures
§ Sling immobilization with gentle ROM exercises at 2 -4 weeks and strengthening at 6 - 10 weeks § Non-displaced middle third § Most pediatric § Stable lateral third § Operative § Open § Non-union symptomatic § Skin tenting § Vascular injury § Unstable fractures (posterior medial third, most lateral third § Ortho referral: Non-emergent for most
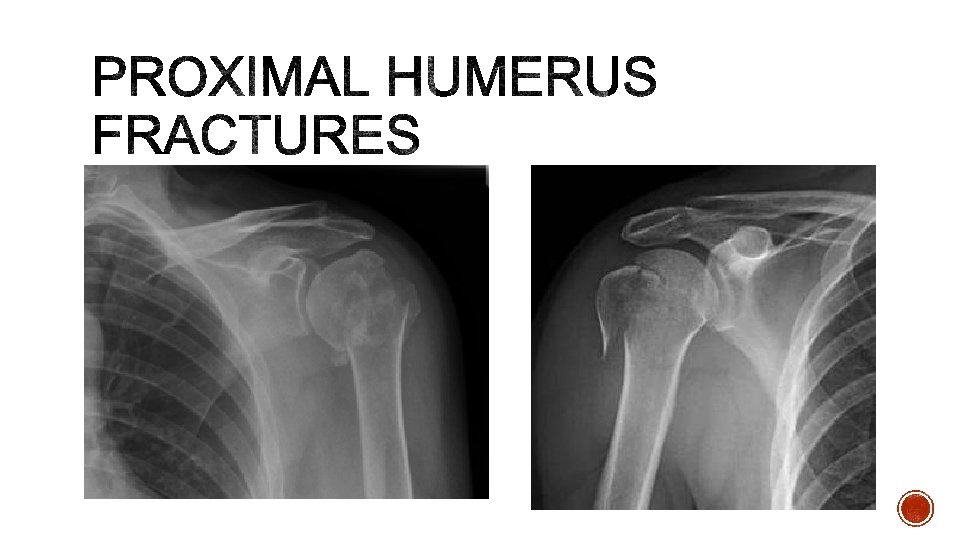
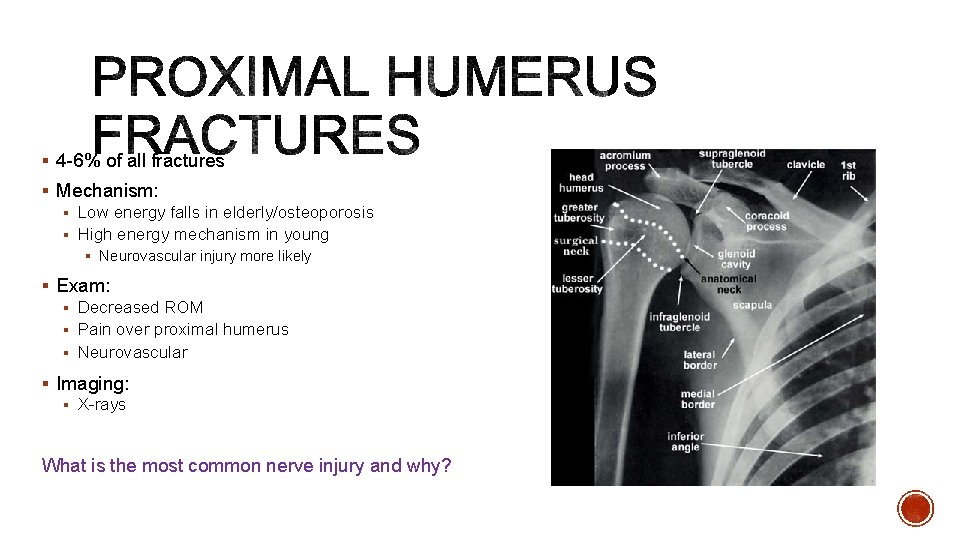
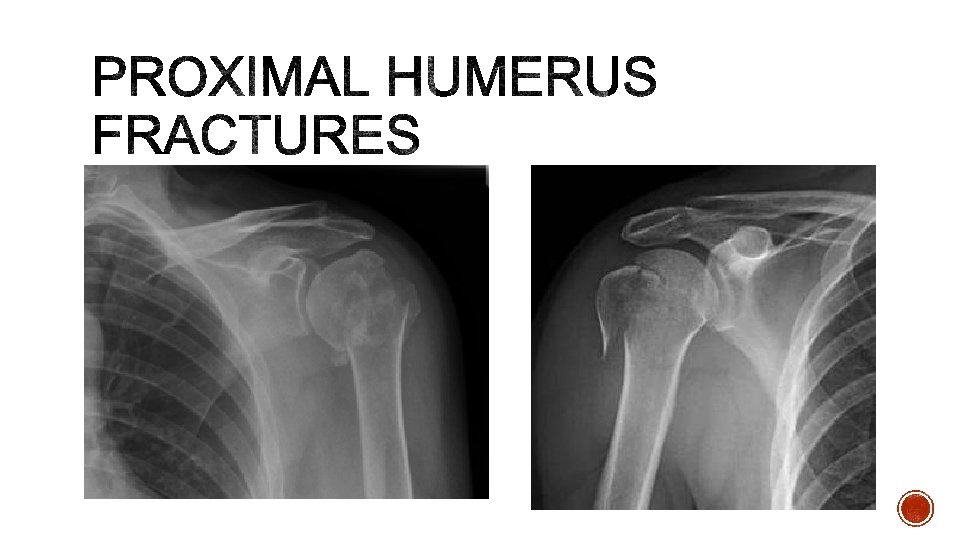
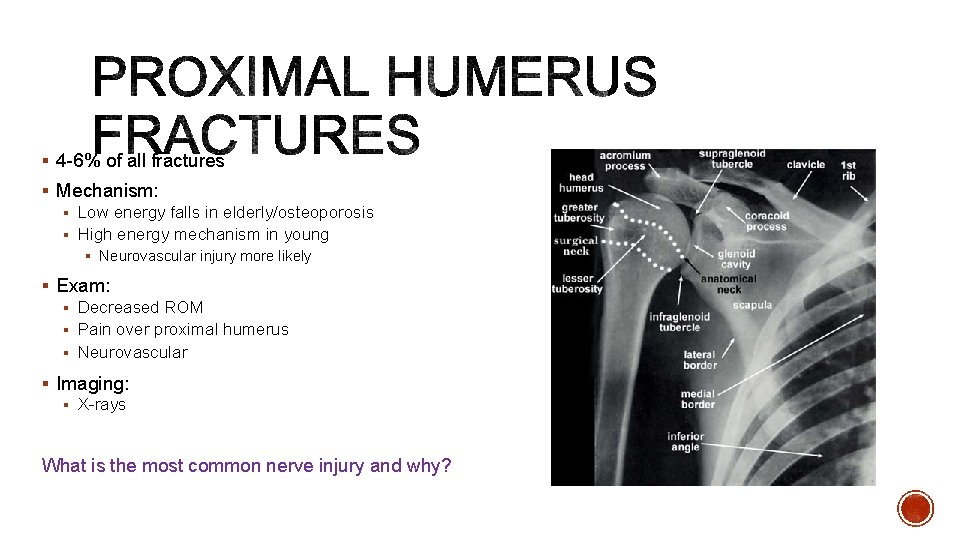
§ 4 -6% of all fractures § Mechanism: § Low energy falls in elderly/osteoporosis § High energy mechanism in young § Neurovascular injury more likely § Exam: § Decreased ROM § Pain over proximal humerus § Neurovascular § Imaging: § X-rays What is the most common nerve injury and why?

§ Sling immobilization followed by progressive rehab at 14 days § minimally displaced surgical neck fracture § greater tuberosity fracture displaced < 5 mm § Surgical management § Greater tuberosity fracture displaced >5 mm § Displaced surgical neck fractures § Compacted fractures with good bone quality § Ortho referral: § Urgent follow up (may call to review x-ray with) § Emergent if vascular compromise
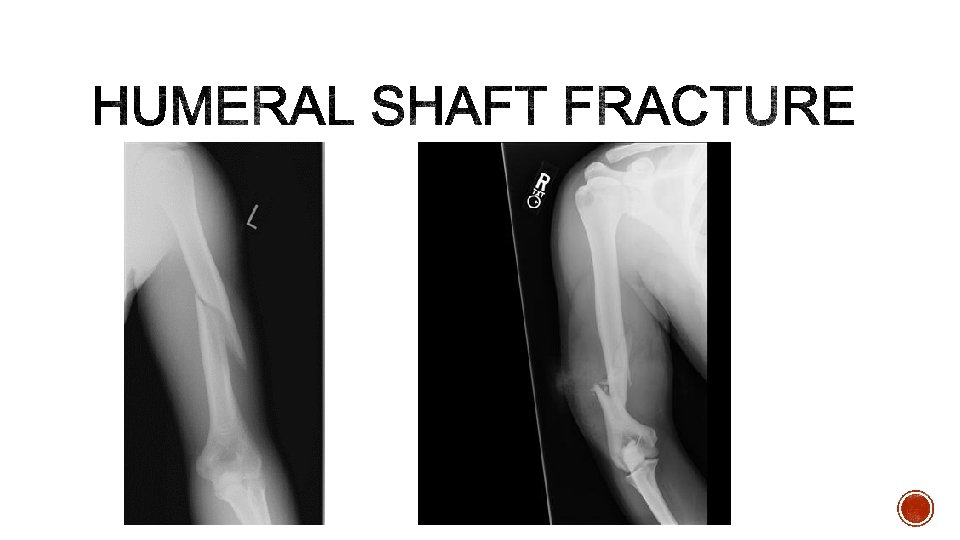
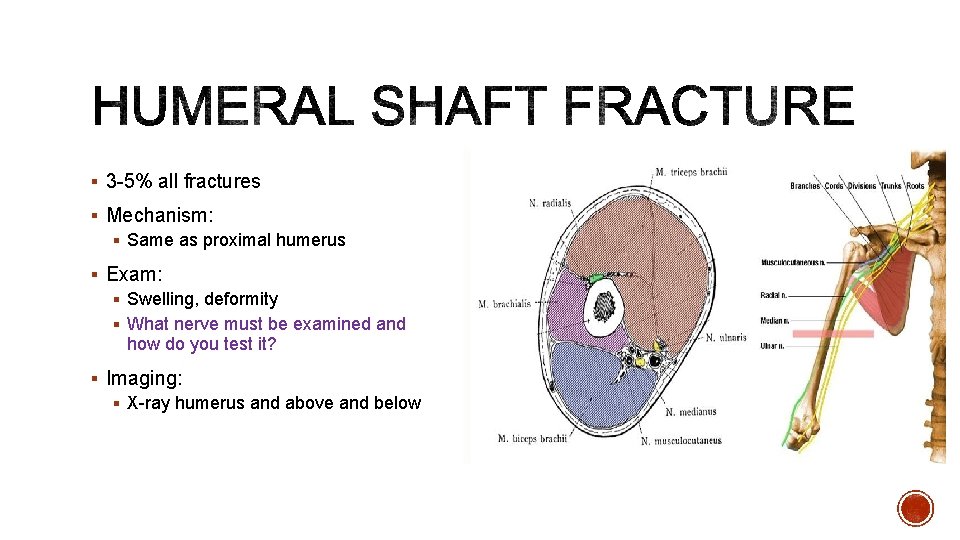
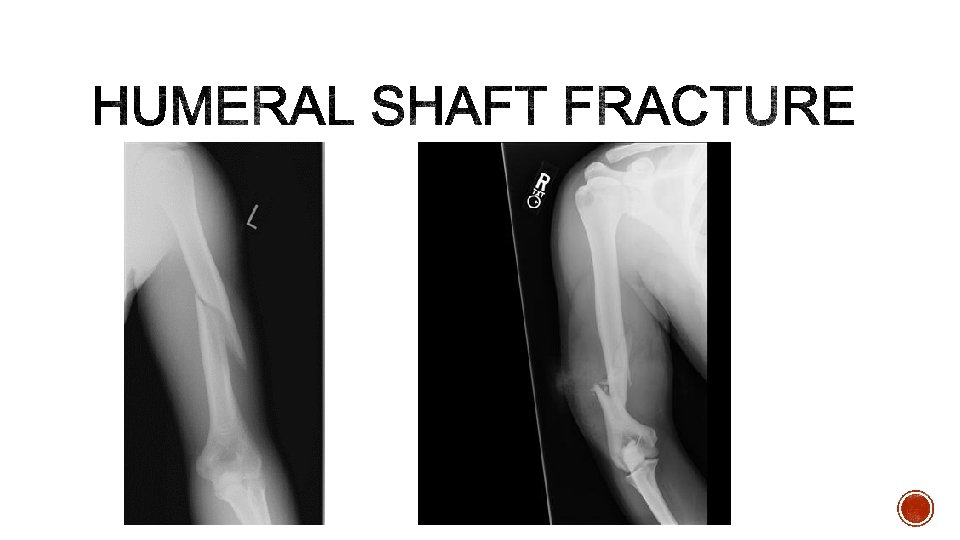
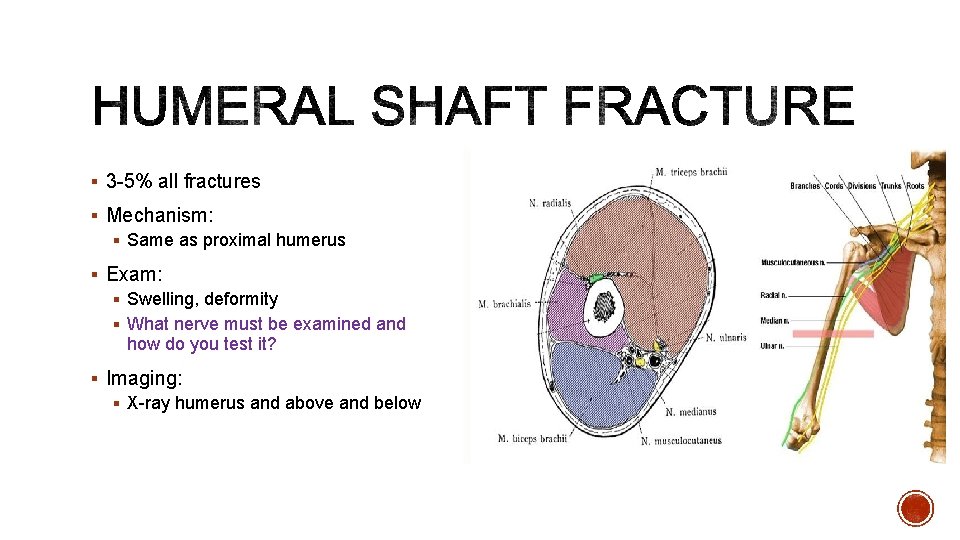
§ 3 -5% all fractures § Mechanism: § Same as proximal humerus § Exam: § Swelling, deformity § What nerve must be examined and how do you test it? § Imaging: § X-ray humerus and above and below
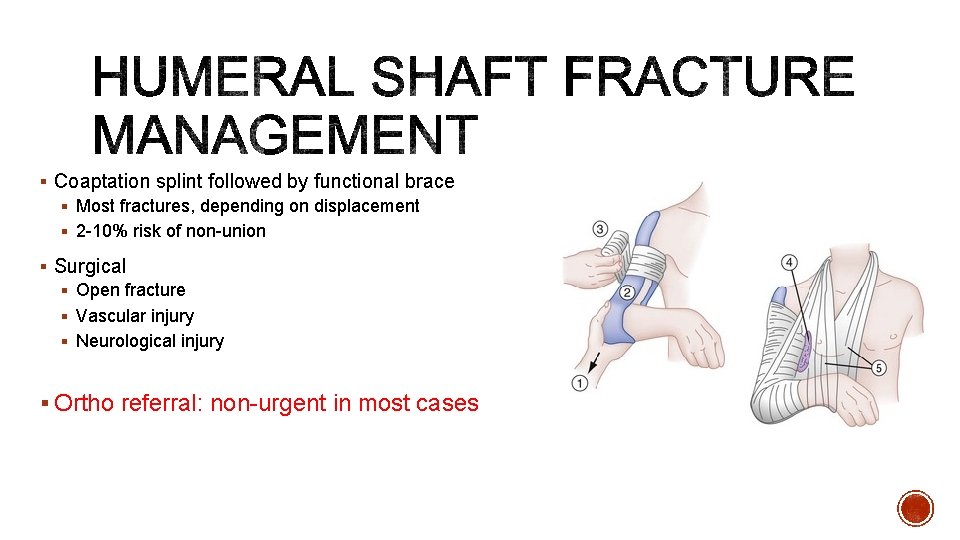
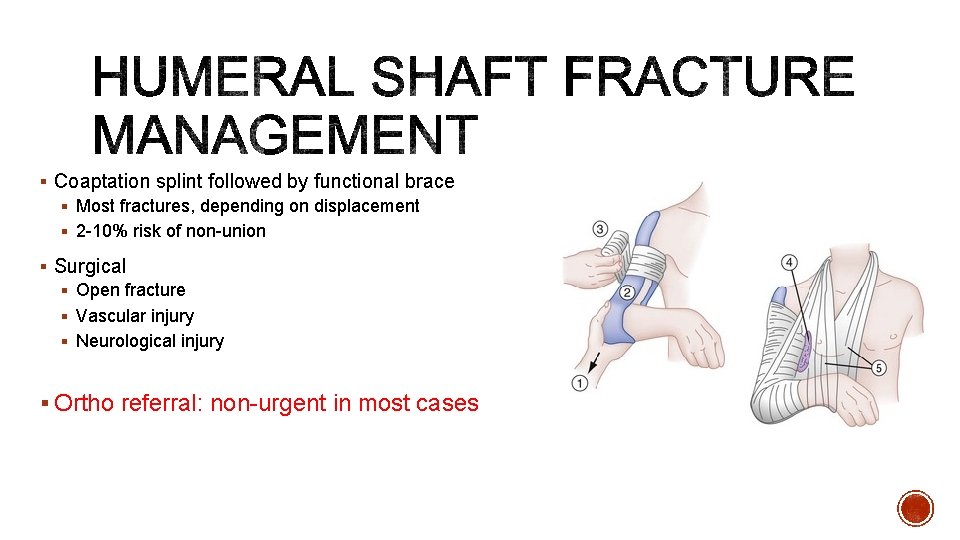
§ Coaptation splint followed by functional brace § Most fractures, depending on displacement § 2 -10% risk of non-union § Surgical § Open fracture § Vascular injury § Neurological injury § Ortho referral: non-urgent in most cases
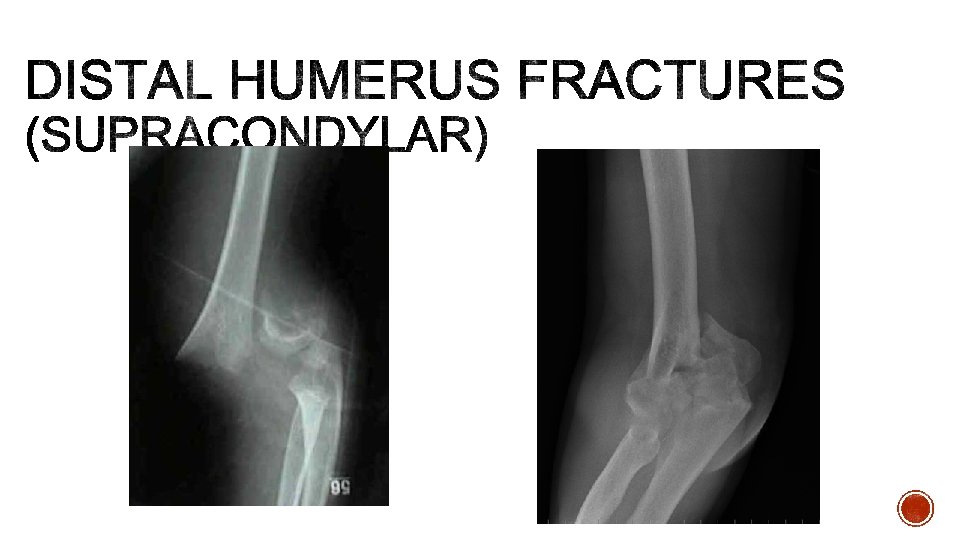
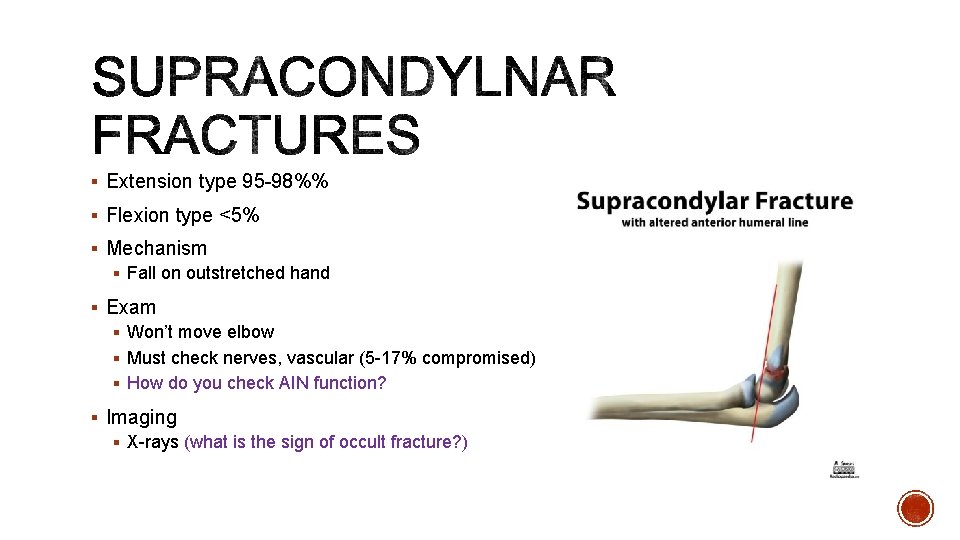
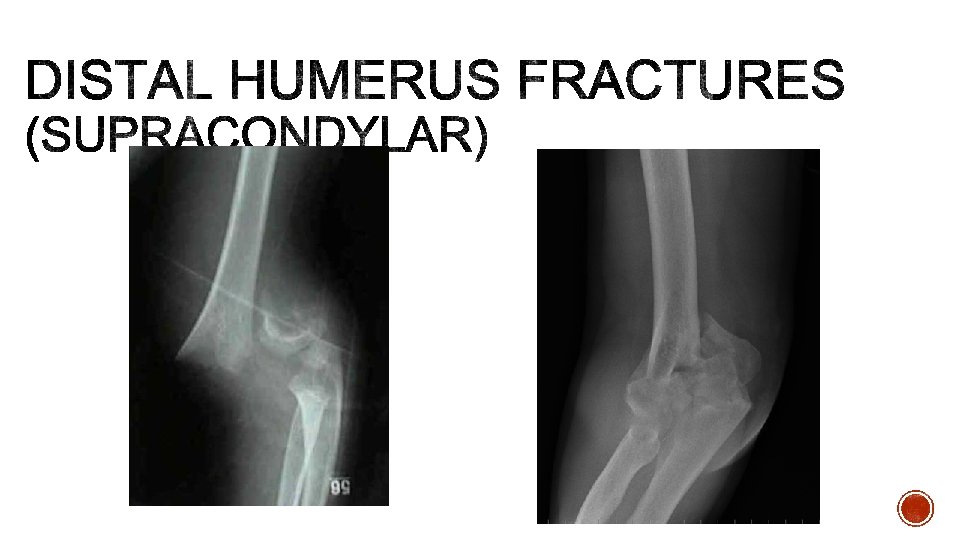
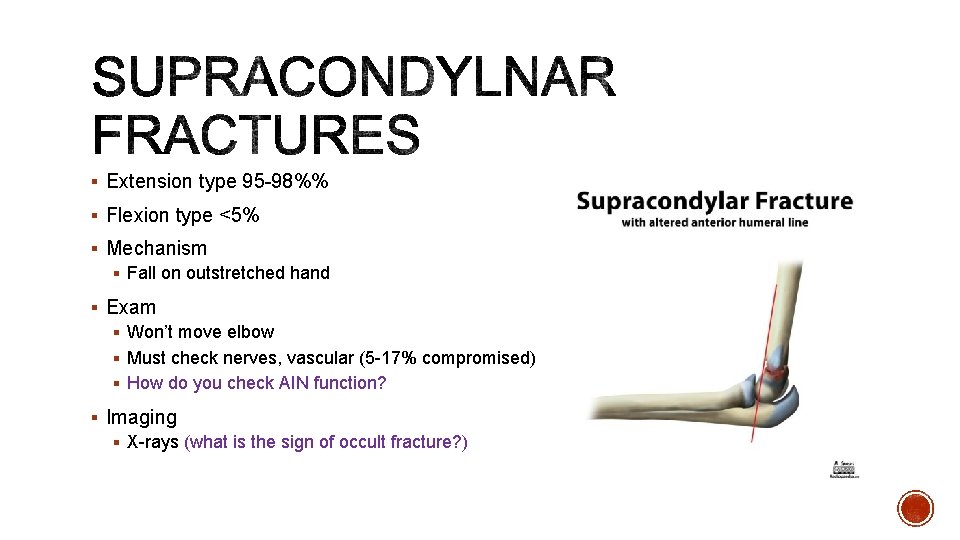
§ Extension type 95 -98%% § Flexion type <5% § Mechanism § Fall on outstretched hand § Exam § Won’t move elbow § Must check nerves, vascular (5 -17% compromised) § How do you check AIN function? § Imaging § X-rays (what is the sign of occult fracture? )
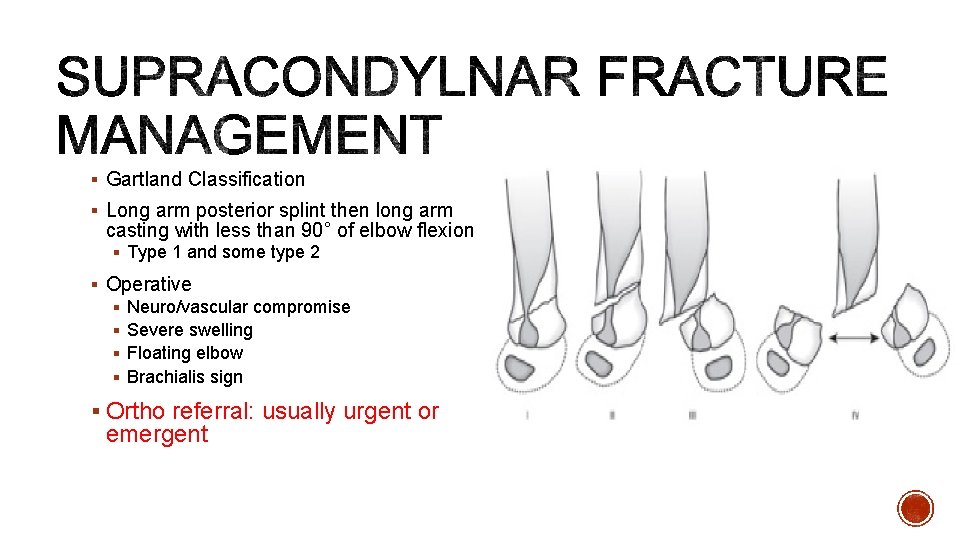
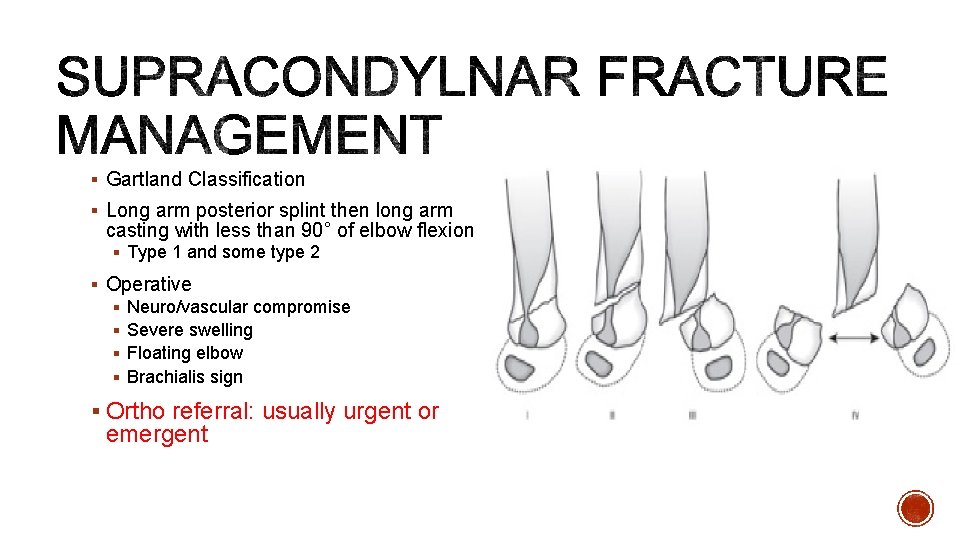
§ Gartland Classification § Long arm posterior splint then long arm casting with less than 90° of elbow flexion § Type 1 and some type 2 § Operative § Neuro/vascular compromise § Severe swelling § Floating elbow § Brachialis sign § Ortho referral: usually urgent or emergent
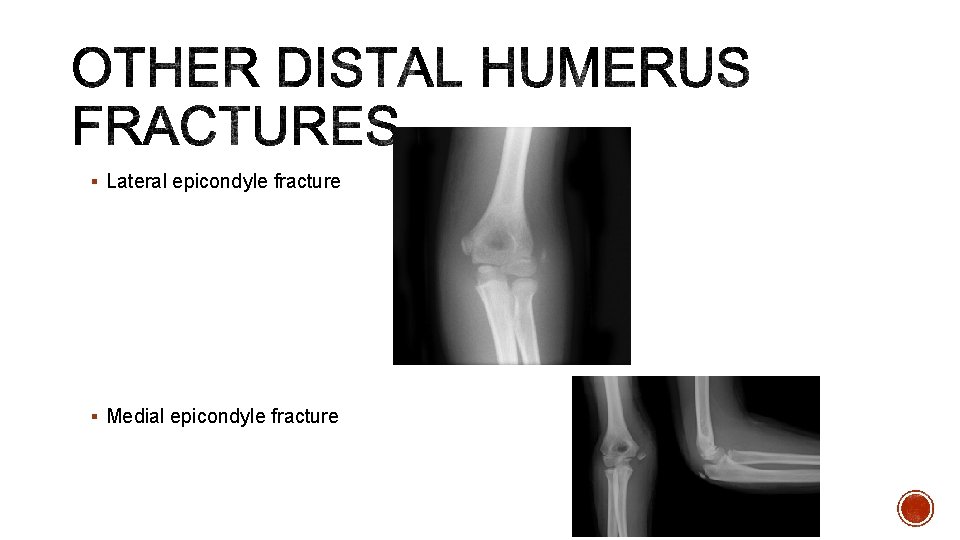
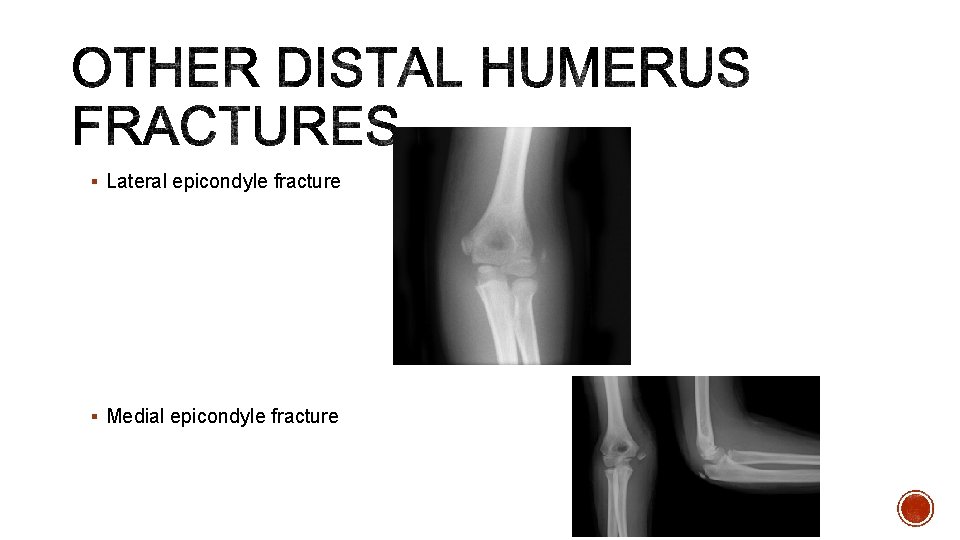
§ Lateral epicondyle fracture § Medial epicondyle fracture
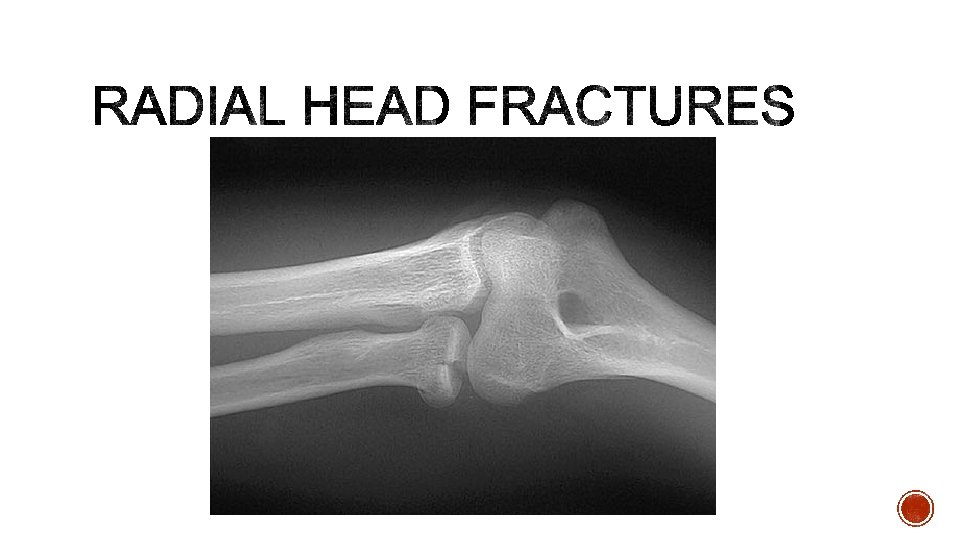
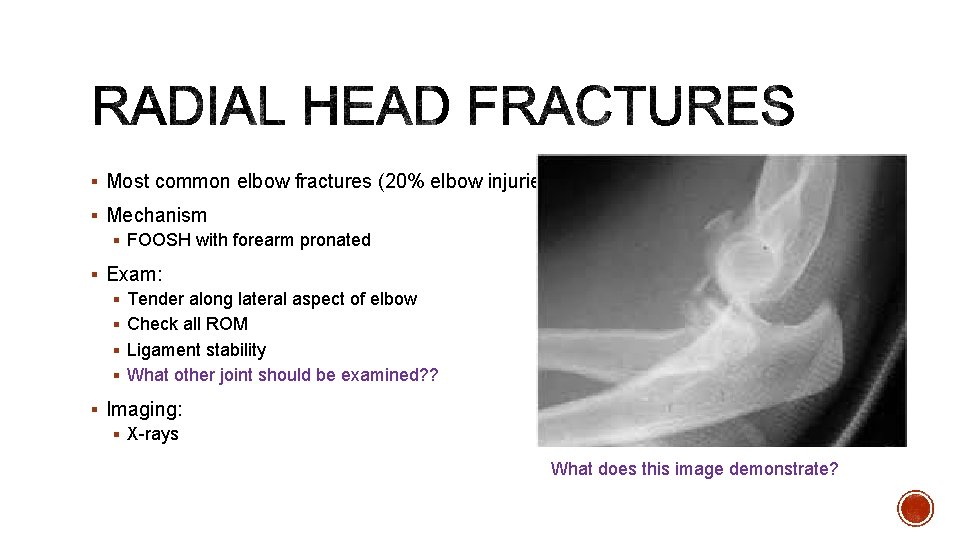
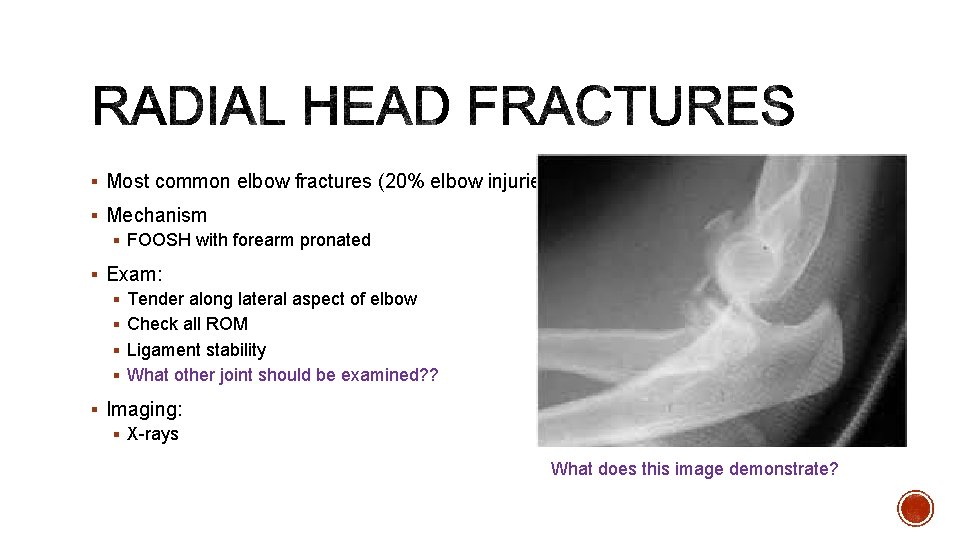
§ Most common elbow fractures (20% elbow injuries) § Mechanism § FOOSH with forearm pronated § Exam: § Tender along lateral aspect of elbow § Check all ROM § Ligament stability § What other joint should be examined? ? § Imaging: § X-rays What does this image demonstrate?
§ Short period of immobilization followed by early ROM § Isolated, minimally displaced, no mechanical blocks § Can get elbow stiffness with prolonged immobilization § Surgical § Mechanical block § Other injuries § Ortho Referral: close follow up for most
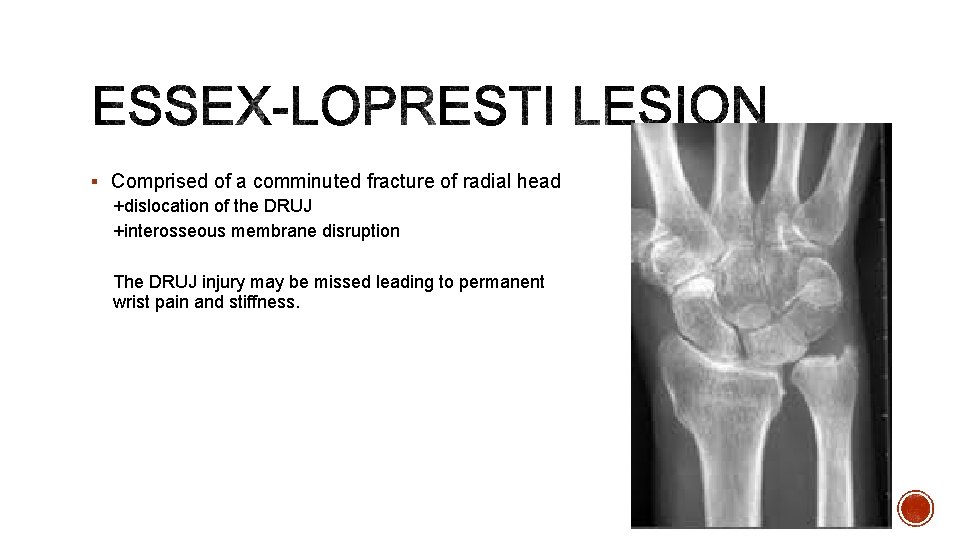
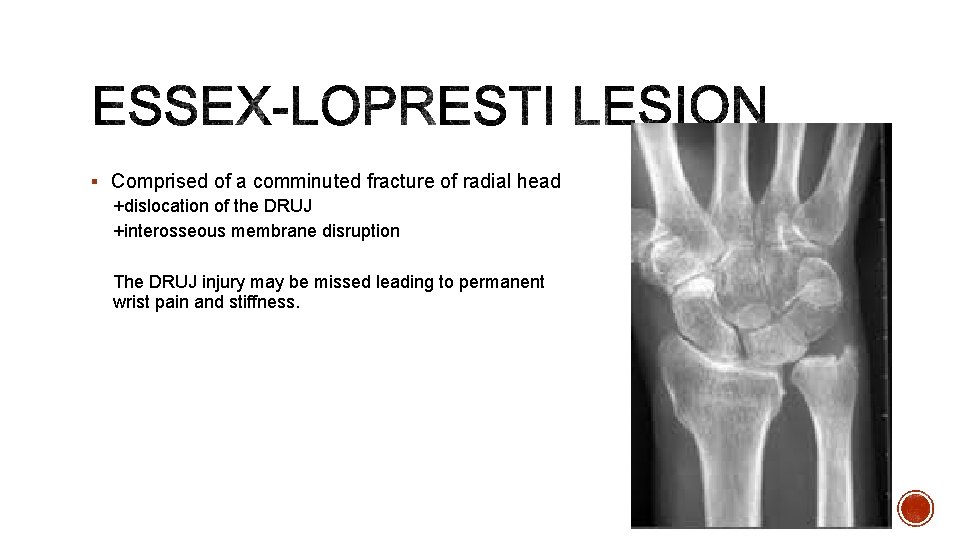
§ Comprised of a comminuted fracture of radial head +dislocation of the DRUJ +interosseous membrane disruption The DRUJ injury may be missed leading to permanent wrist pain and stiffness.

§ Definition § distal 1/3 radius shaft fx AND § associated distal radioulnar joint (DRUJ) injury § Mechanism § direct wrist trauma dorsolateral aspect § fall onto outstretched hand with forearm in pronation § Exam § Tenderness at fracture site § Check pronation/supination for instability § Stress to DRUJ causes wrist or midline pain § Imaging § X-ray forearm, elbow, wrist
§ Is Operative § Better outcomes with sooner rather than later surgery § Ortho referral § Would call for recommendations at time of presentation
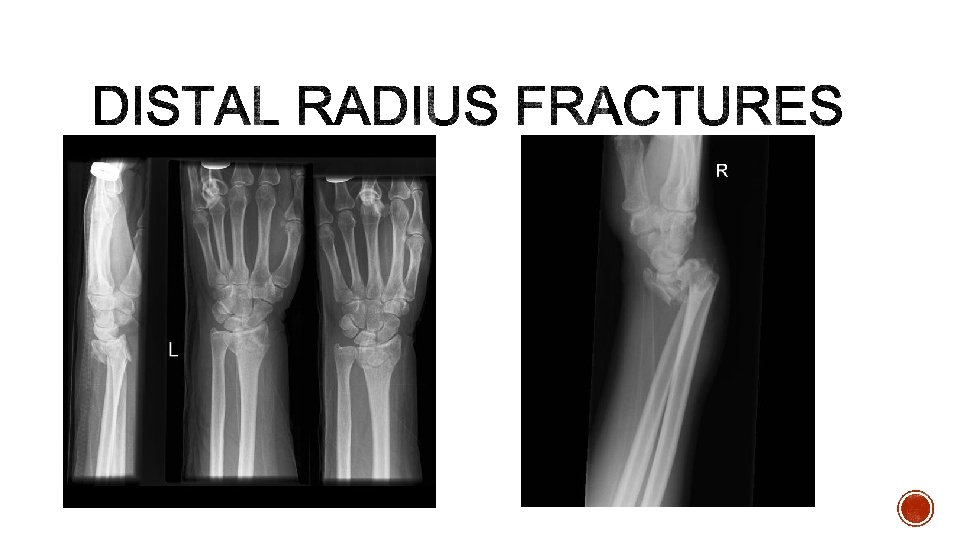
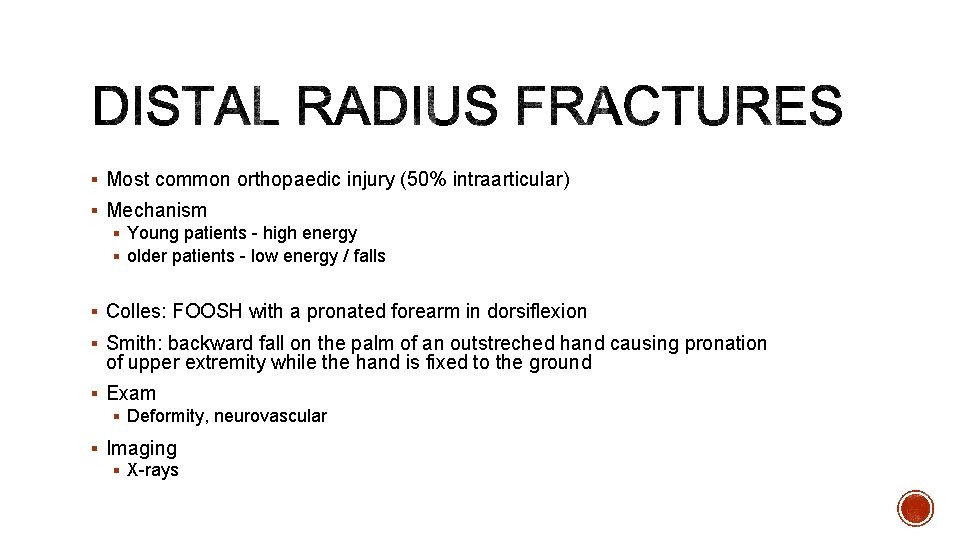
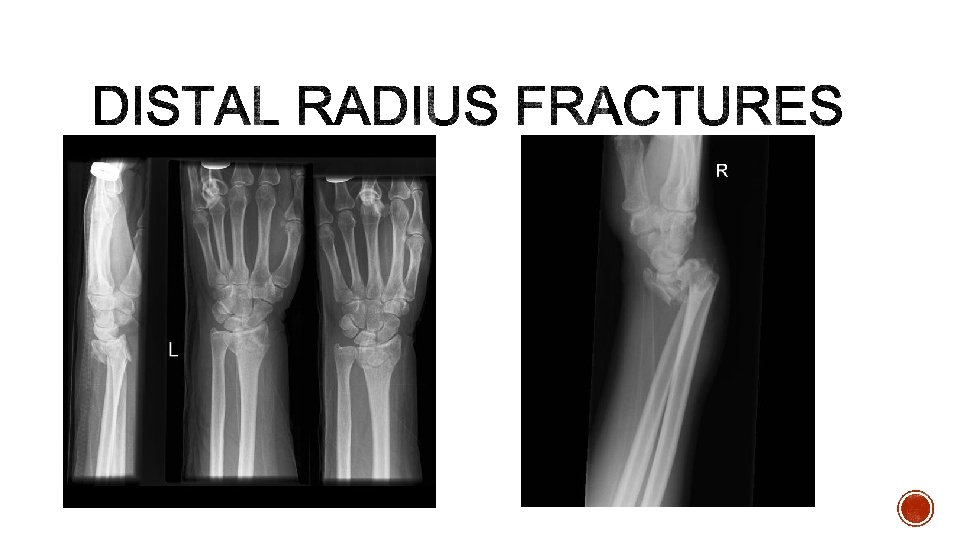
§ Most common orthopaedic injury (50% intraarticular) § Mechanism § Young patients - high energy § older patients - low energy / falls § Colles: FOOSH with a pronated forearm in dorsiflexion § Smith: backward fall on the palm of an outstreched hand causing pronation of upper extremity while the hand is fixed to the ground § Exam § Deformity, neurovascular § Imaging § X-rays
§ Closed reduction and cast immobilization (finger trap is helpful) § extra-articular § <5 mm radial shortening § dorsal angulation <5° or within 20° of contralateral distal radius § Surgical § radiographic findings indicating instability § Ortho Referral: need close follow up after reduction and splint. May need them to help you with a reduction
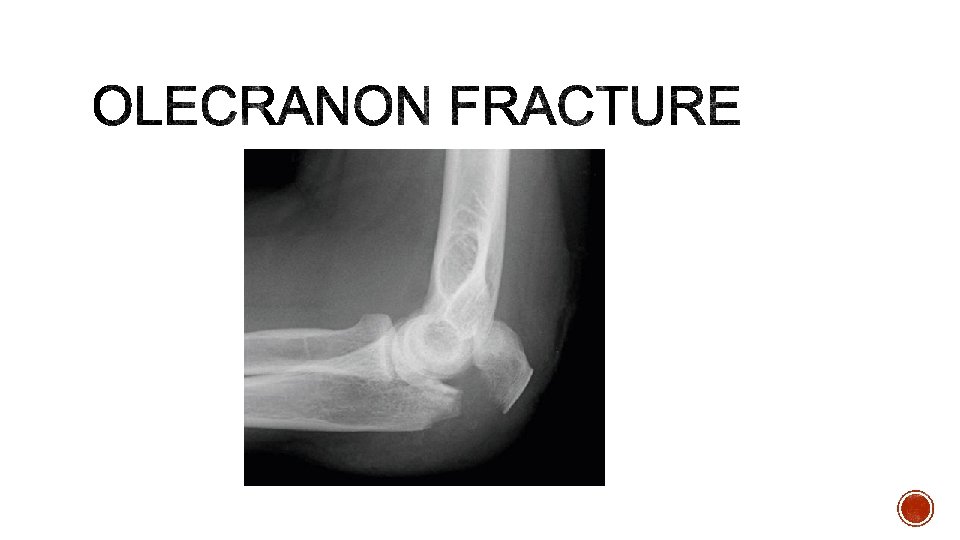
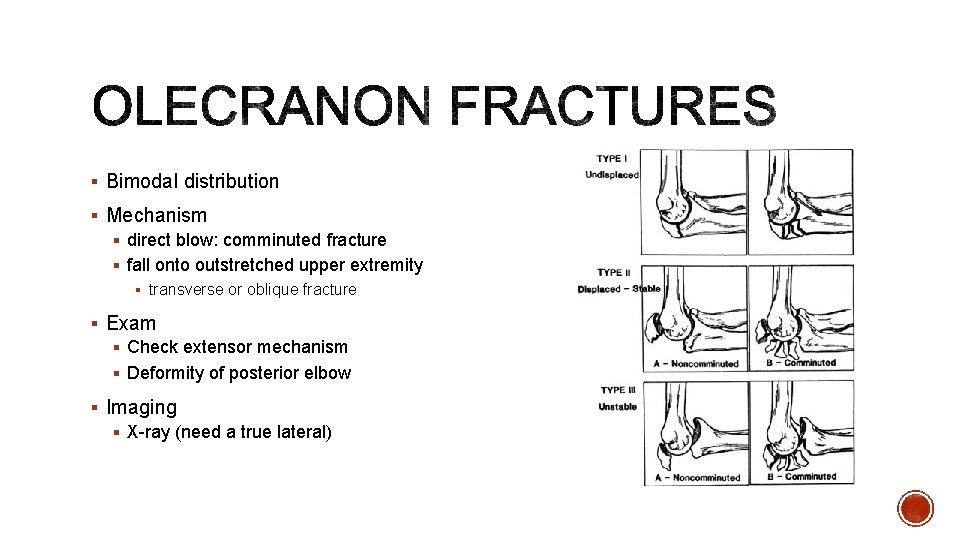
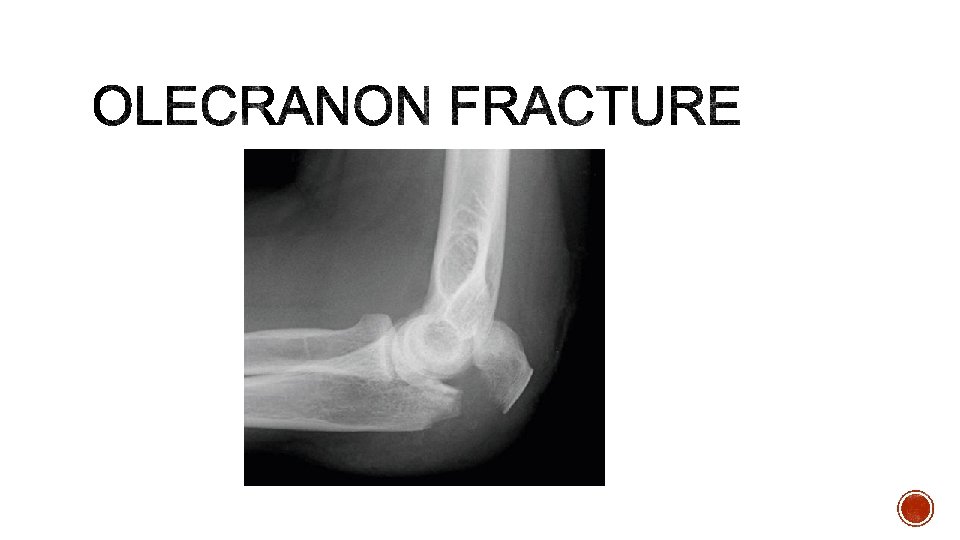
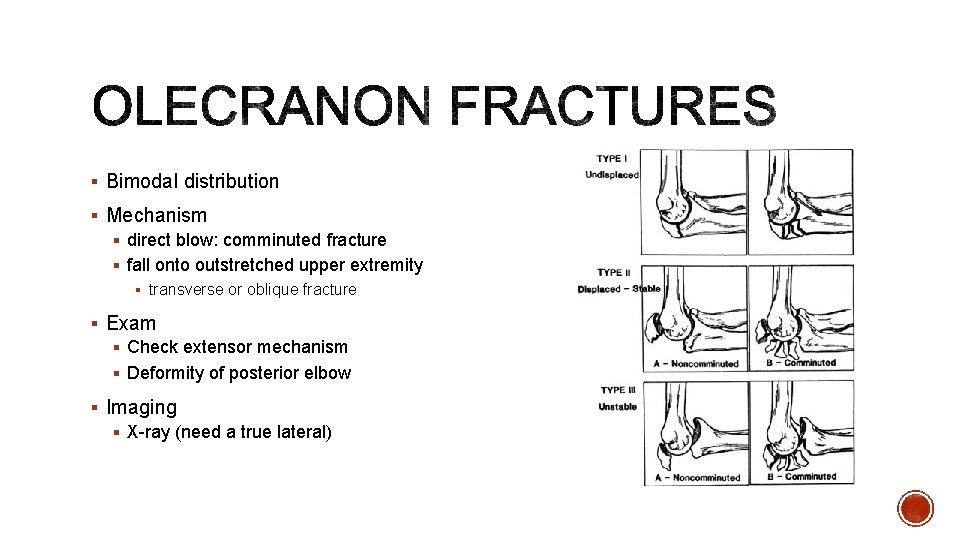
§ Bimodal distribution § Mechanism § direct blow: comminuted fracture § fall onto outstretched upper extremity § transverse or oblique fracture § Exam § Check extensor mechanism § Deformity of posterior elbow § Imaging § X-ray (need a true lateral)
§ Immobilization with early ROM at one week § Non-displaced fractures or low demand elderly individual § Splint in 45 -90% § Surgical § Complex fractures § Ortho referral: close outpatient follow up (unless very complex, problems with extensor mechanism)
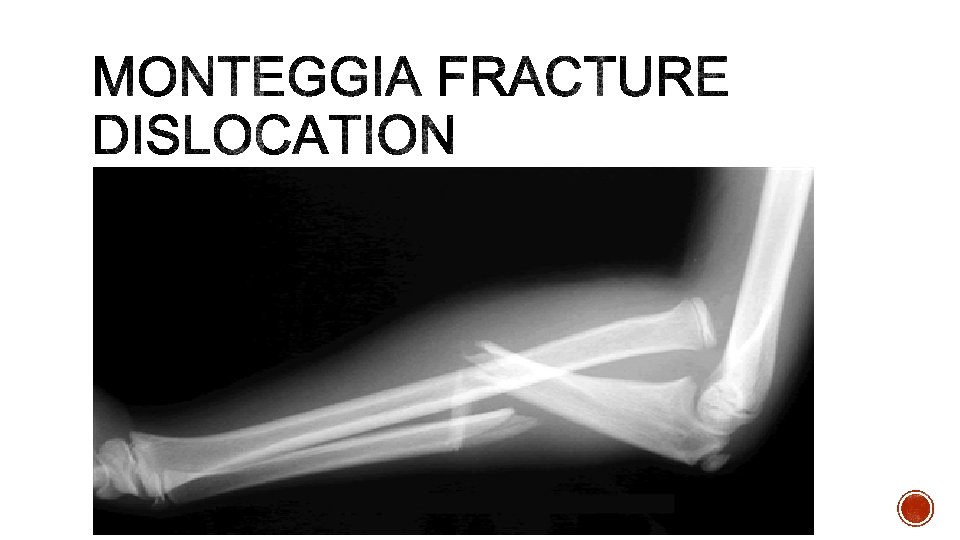
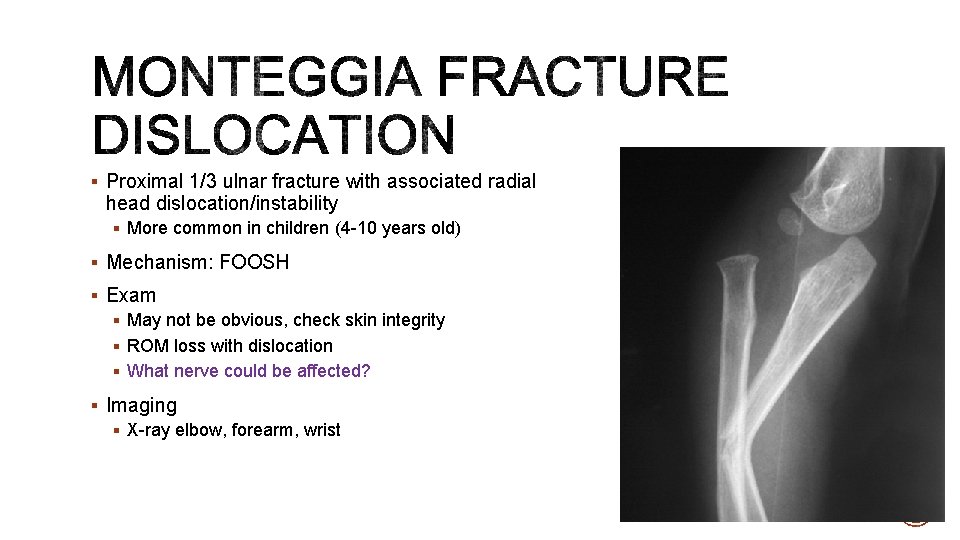
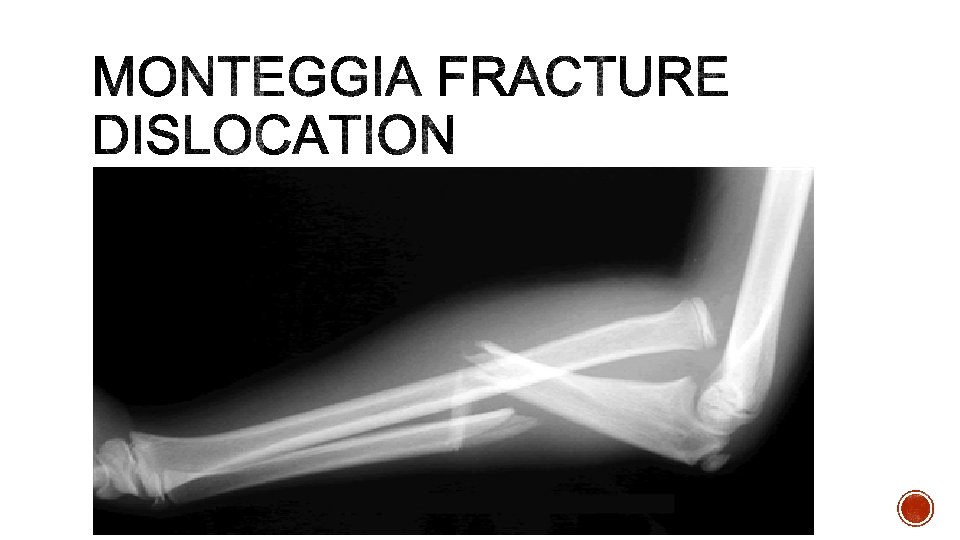
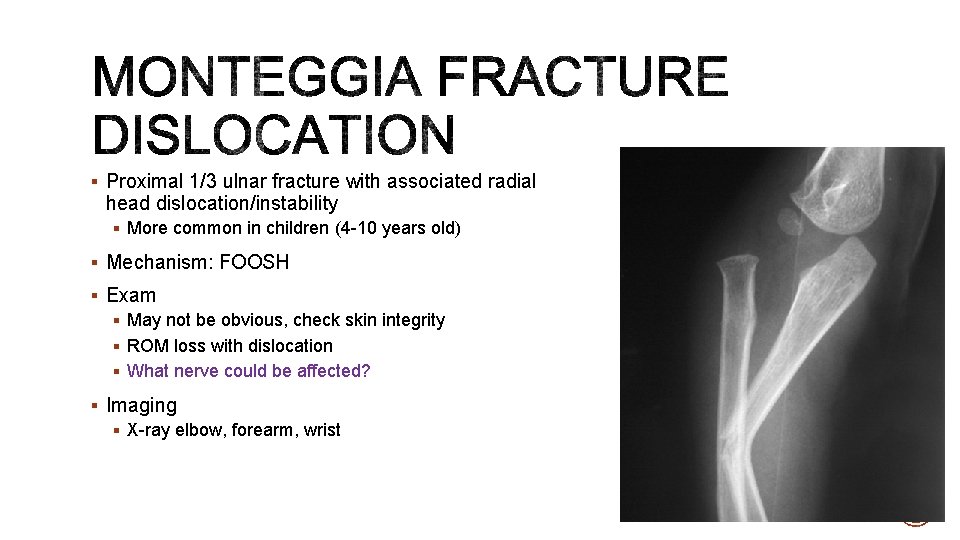
§ Proximal 1/3 ulnar fracture with associated radial head dislocation/instability § More common in children (4 -10 years old) § Mechanism: FOOSH § Exam § May not be obvious, check skin integrity § ROM loss with dislocation § What nerve could be affected? § Imaging § X-ray elbow, forearm, wrist
§ Adult: usually operative § Pediatric: usually closed reduction, immobilization § Can have PIN neuropathy which resolves over time § Ortho Referral: § If possible check with ortho prior to reduction
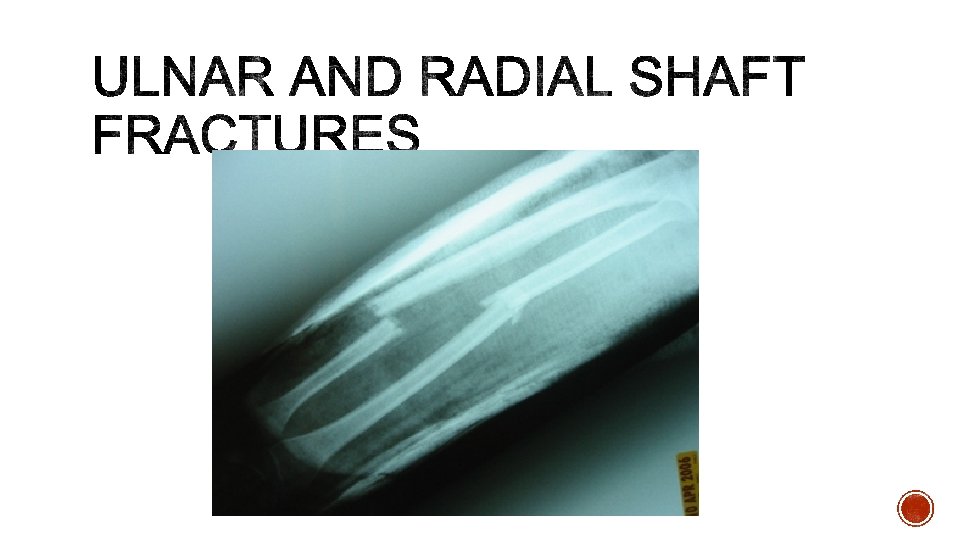
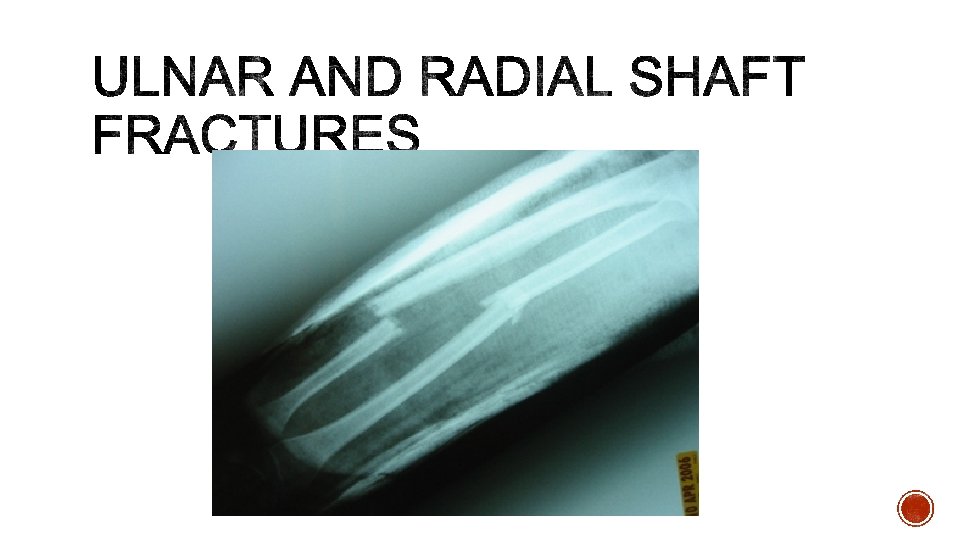
§ Mechanism § Direct trauma, athletic injury, fall from height § Exam § Large deformity § May need to check compartments § Imaging § X-rays § Treatment: § functional fx brace with good interosseous mold for non-displaced ulnar fractures § Surgical: radial fractures, displaced ulnar fractures § Ortho Referral: Urgent if surgical or outpatient if non-displaced
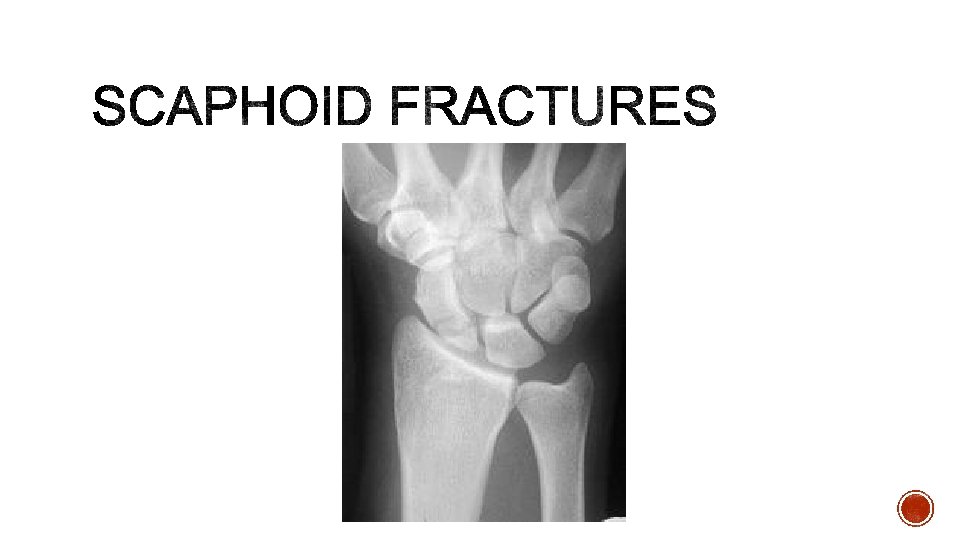
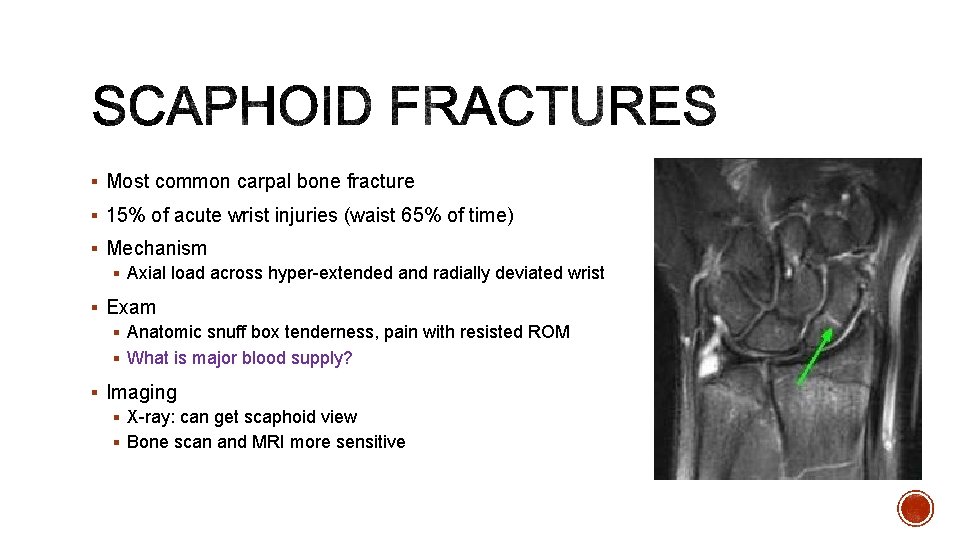
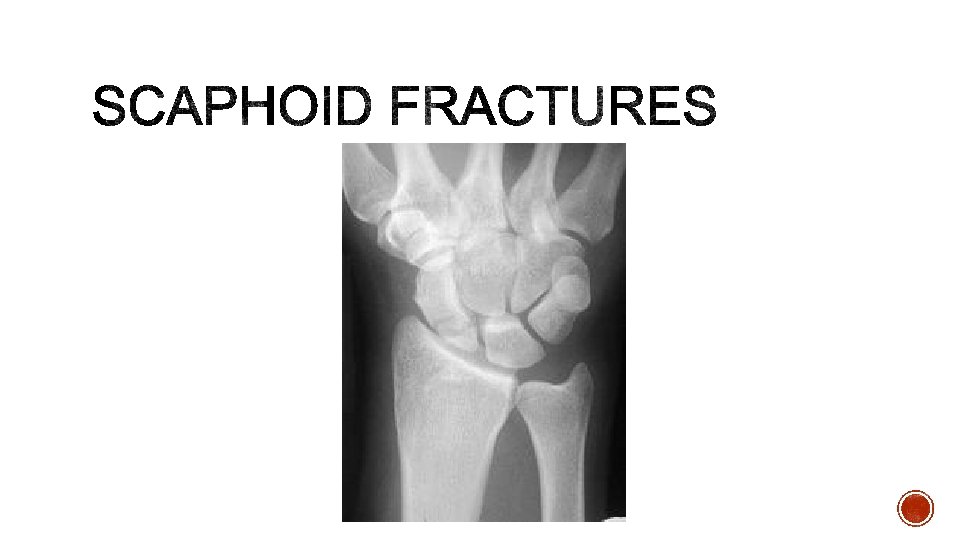
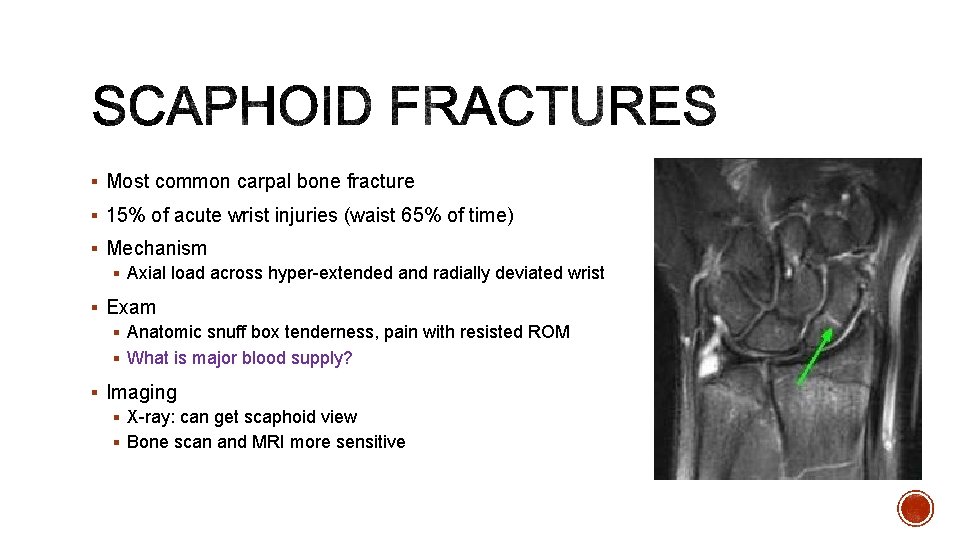
§ Most common carpal bone fracture § 15% of acute wrist injuries (waist 65% of time) § Mechanism § Axial load across hyper-extended and radially deviated wrist § Exam § Anatomic snuff box tenderness, pain with resisted ROM § What is major blood supply? § Imaging § X-ray: can get scaphoid view § Bone scan and MRI more sensitive
§ Thumb spica cast immobilization § Stable, non-displaced fractues § Surgical § Displaced fractures § Ortho referral: close outpatient follow up

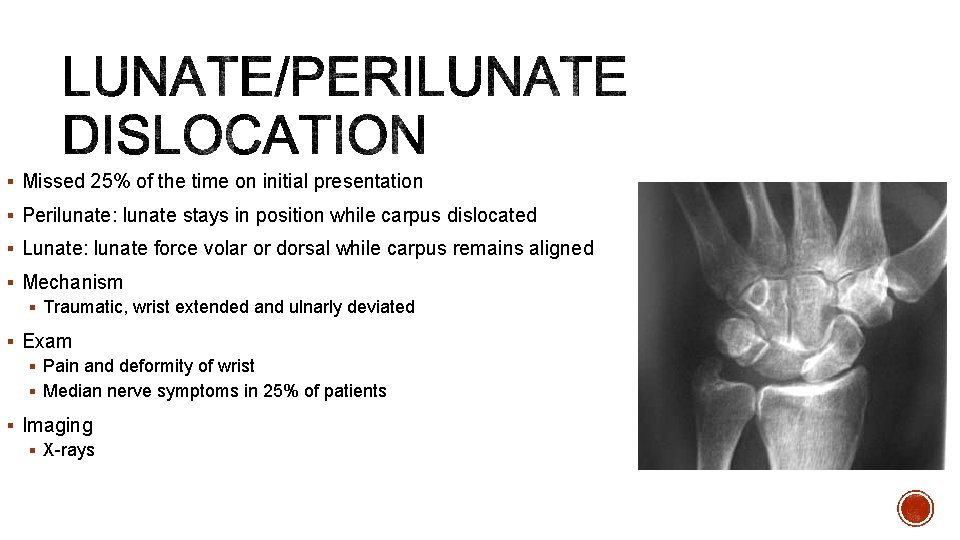
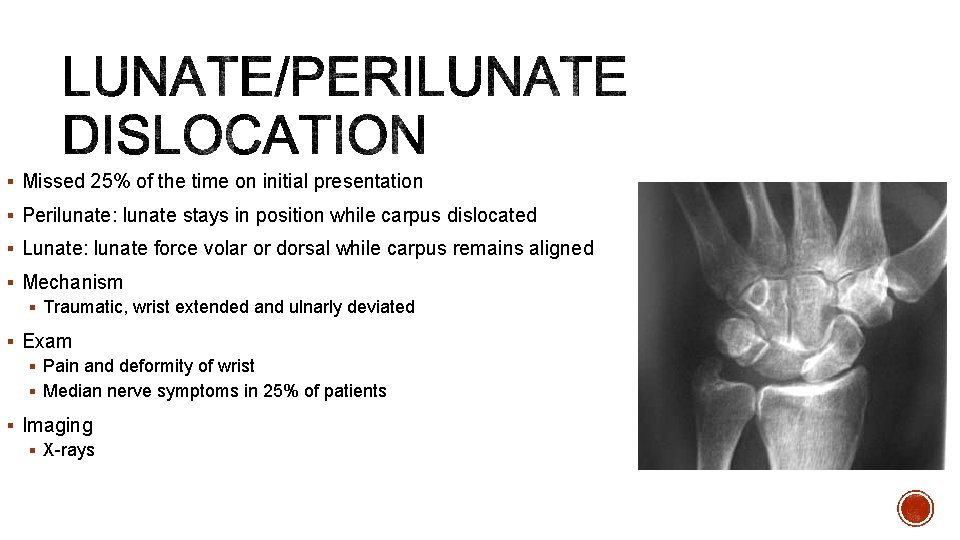
§ Missed 25% of the time on initial presentation § Perilunate: lunate stays in position while carpus dislocated § Lunate: lunate force volar or dorsal while carpus remains aligned § Mechanism § Traumatic, wrist extended and ulnarly deviated § Exam § Pain and deformity of wrist § Median nerve symptoms in 25% of patients § Imaging § X-rays
§ Always needs surgery § Emergent reduction prior to surgery can be done § Ortho referral: Urgent/Emergent

§ Most common variant of base of thumb fractures § Intra-articular fracture/dislocation of base of 1 st metacarpal characterized by volar lip of metacarpal based attached to volar oblique ligament (stays attached to trapezium) § Mechanism § Axial force applied to thumb § Exam § Pain at the base of 1 st metacarpal § Imaging § X-rays
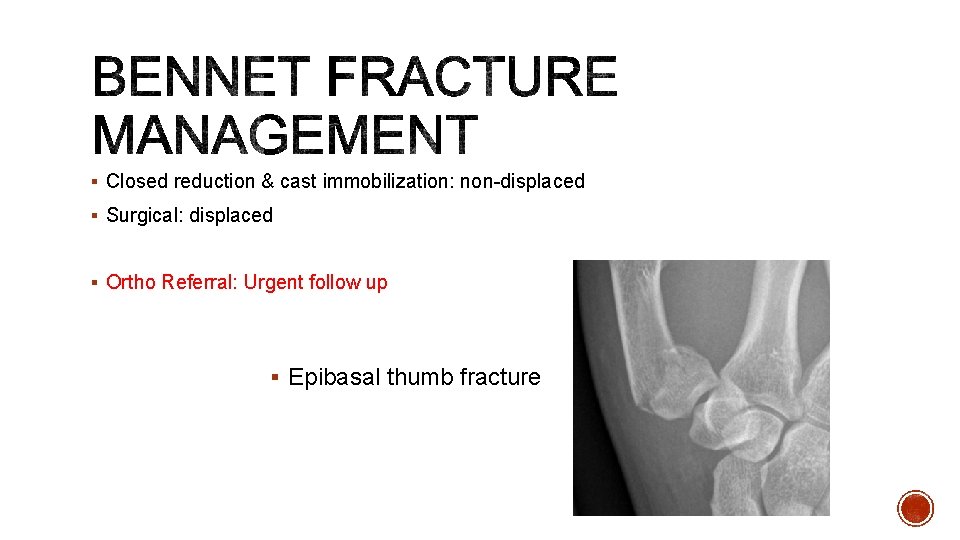
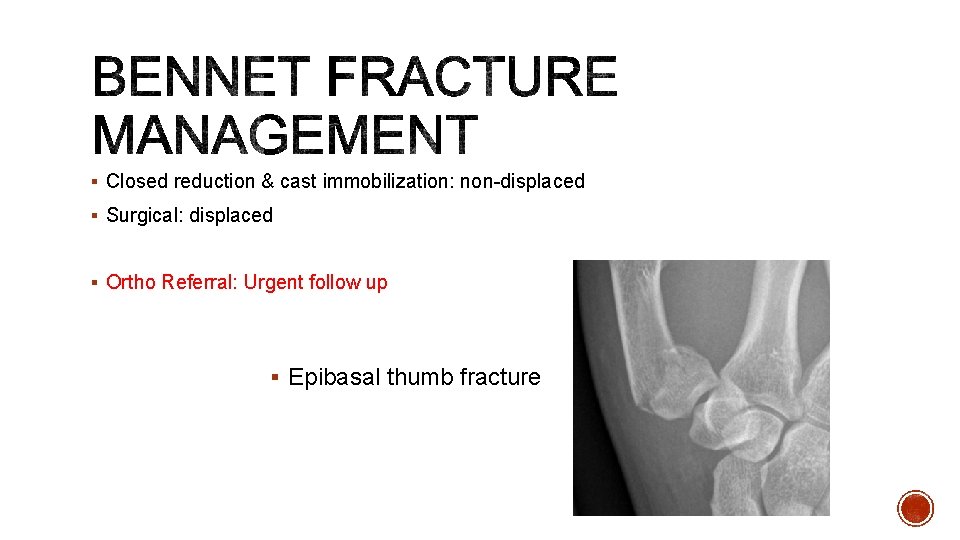
§ Closed reduction & cast immobilization: non-displaced § Surgical: displaced § Ortho Referral: Urgent follow up § Epibasal thumb fracture

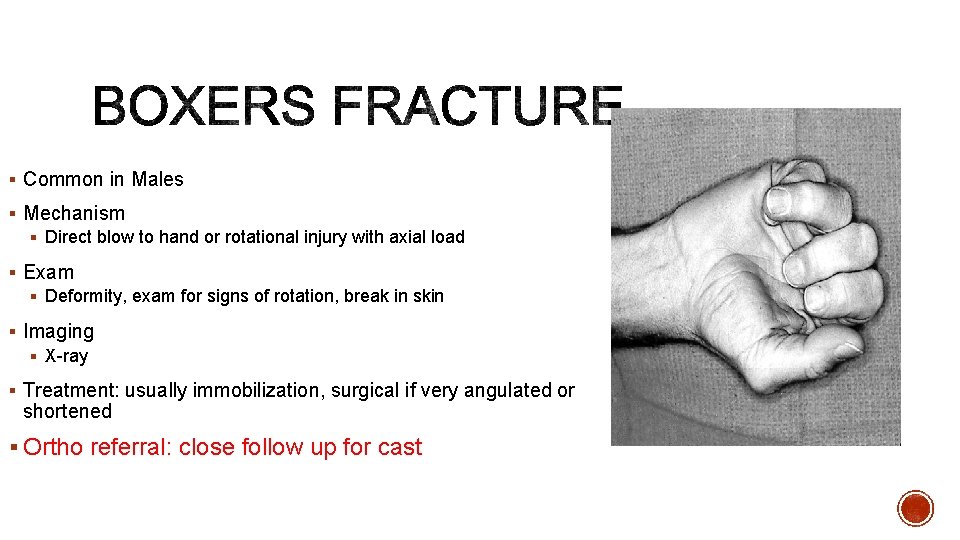
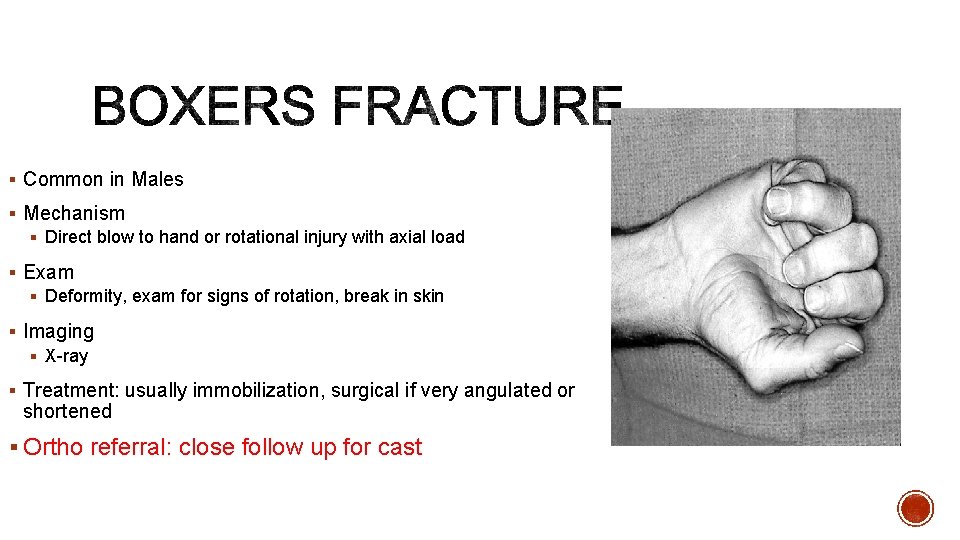
§ Common in Males § Mechanism § Direct blow to hand or rotational injury with axial load § Exam § Deformity, exam for signs of rotation, break in skin § Imaging § X-ray § Treatment: usually immobilization, surgical if very angulated or shortened § Ortho referral: close follow up for cast

§ Deformity caused by disruption of the terminal extensor tendon distal to DIP joint § Mechanism: direct blow to tip of finger causing forced flexion of DIP § Exam: finger tip rest at 45% flexion § Imaging: xrays § Treatment § Extension splinting for 6 -8 weeks with progressive flexion at 6 weeks § Ortho Referral: non-urgent outpatient

§ Avulsion injury of FDP from insertion at base of distal phalanx § Zone I flexor tendon injury § Mechanism: gripping with extension force § Exam: pain over volar distal finger § Imaging: x-ray § Management: Surgical, can splint prior to surgery (<3 weeks) § Ortho Referral: Needs urgent follow up
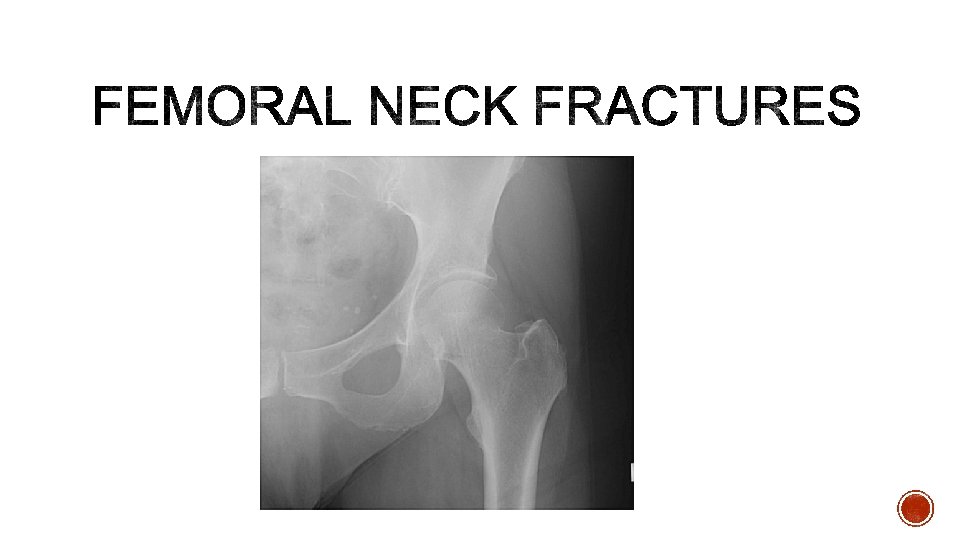
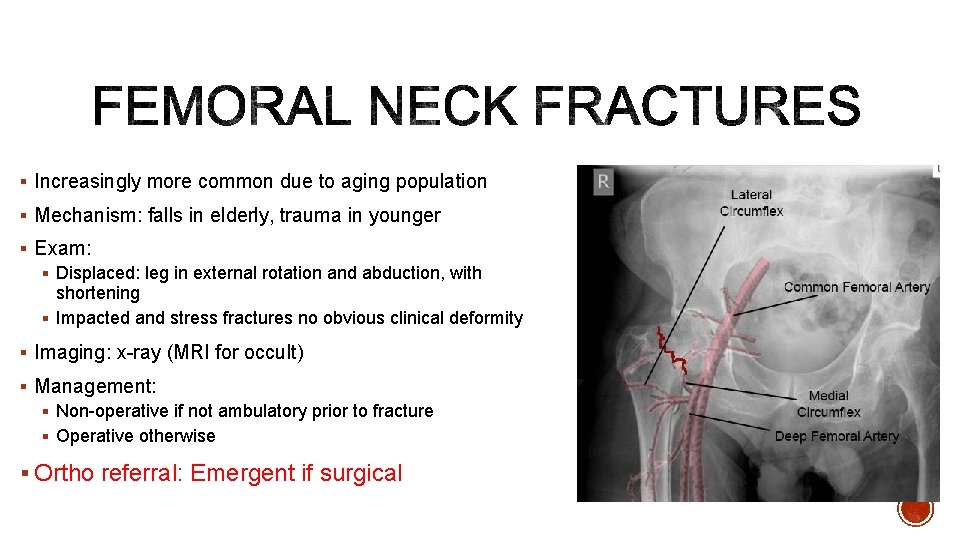
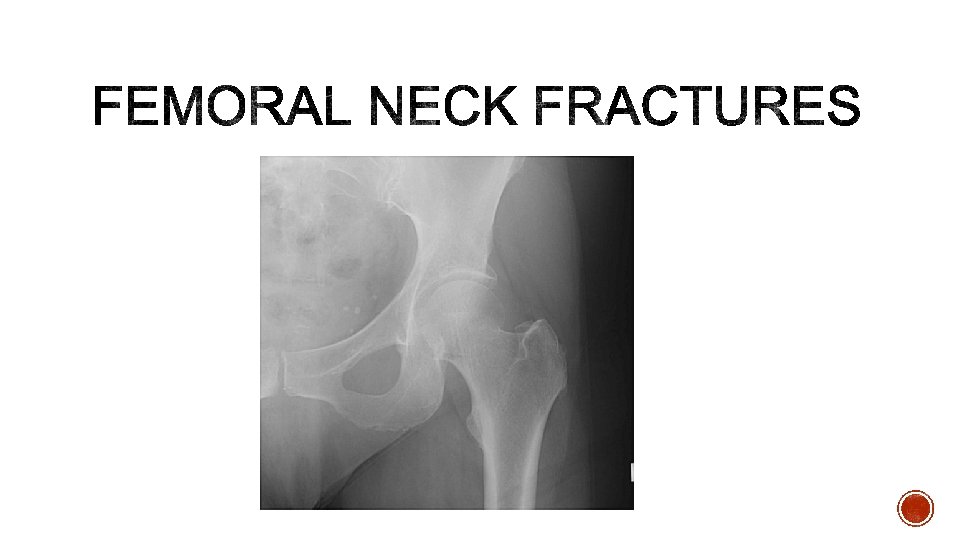
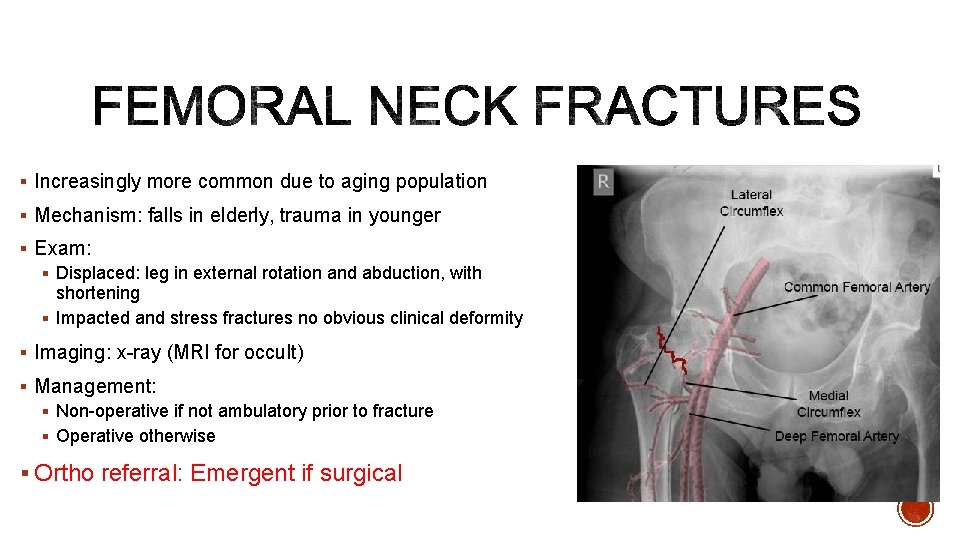
§ Increasingly more common due to aging population § Mechanism: falls in elderly, trauma in younger § Exam: § Displaced: leg in external rotation and abduction, with shortening § Impacted and stress fractures no obvious clinical deformity § Imaging: x-ray (MRI for occult) § Management: § Non-operative if not ambulatory prior to fracture § Operative otherwise § Ortho referral: Emergent if surgical
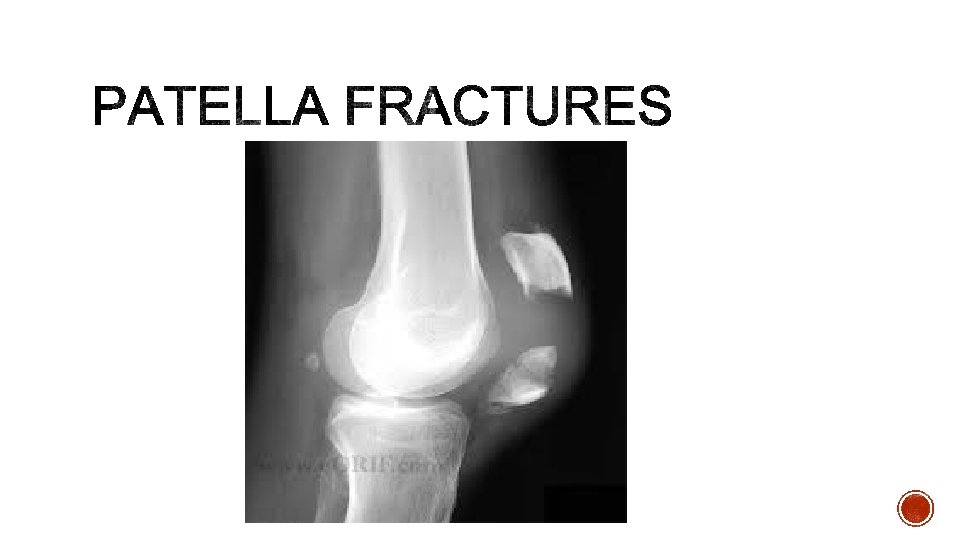
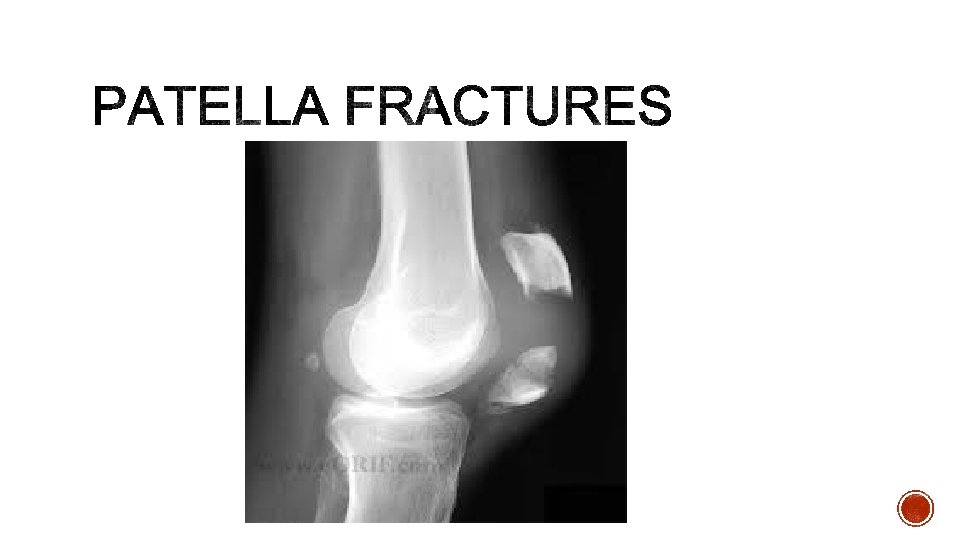
§ Check extensor mechanism § Management § knee immobilized in extension (brace or cylinder cast) and full weight bearing § intact extensor mechanism § nondisplaced or minimally displaced fractures § vertical fracture patterns § Ortho Referral: Urgent follow up
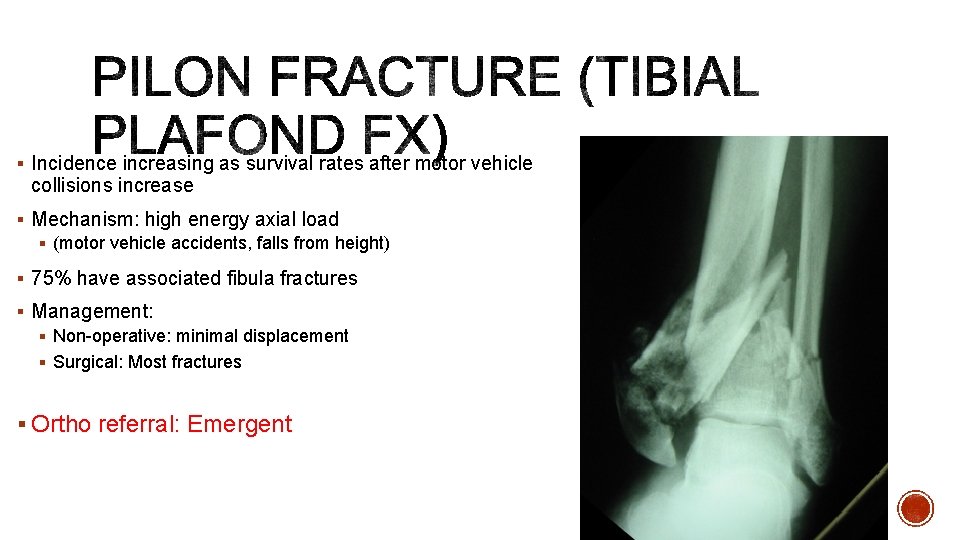
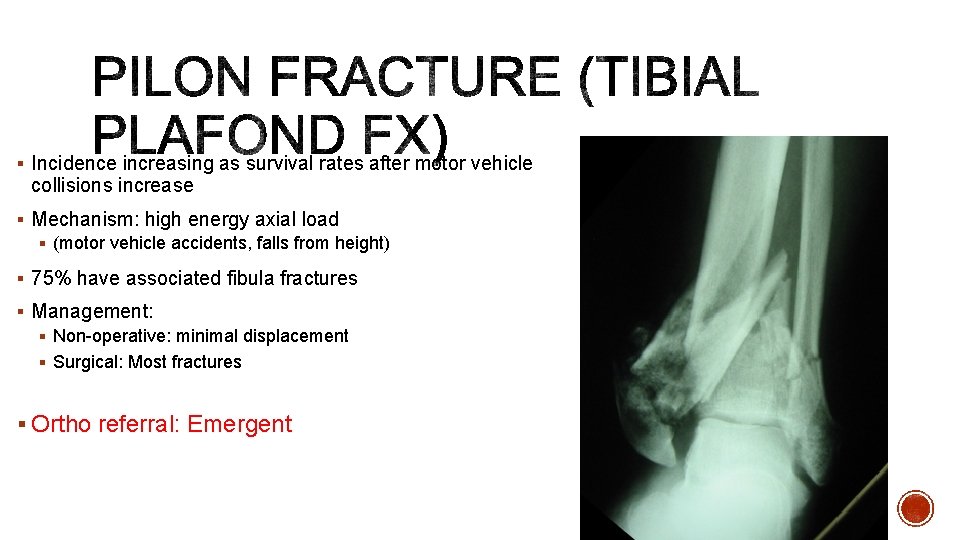
§ Incidence increasing as survival rates after motor vehicle collisions increase § Mechanism: high energy axial load § (motor vehicle accidents, falls from height) § 75% have associated fibula fractures § Management: § Non-operative: minimal displacement § Surgical: Most fractures § Ortho referral: Emergent
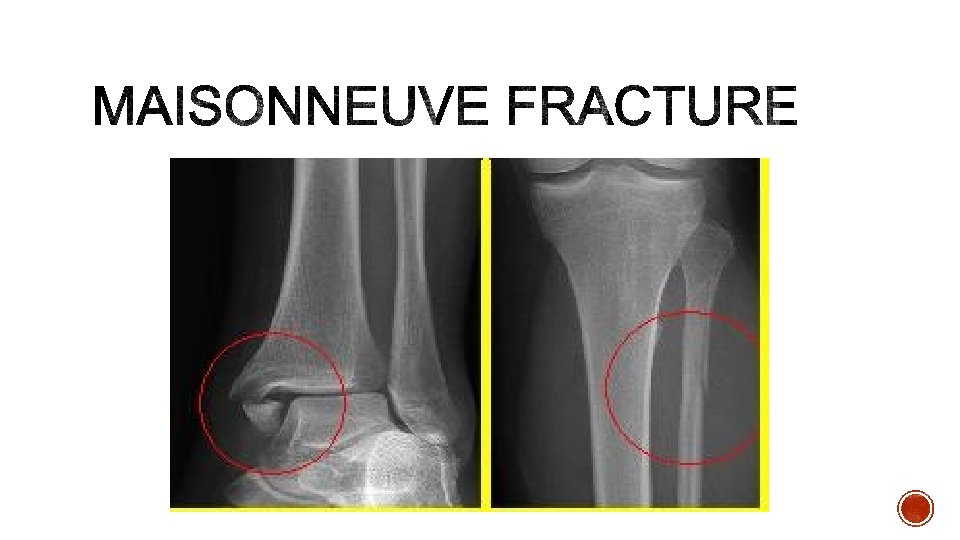
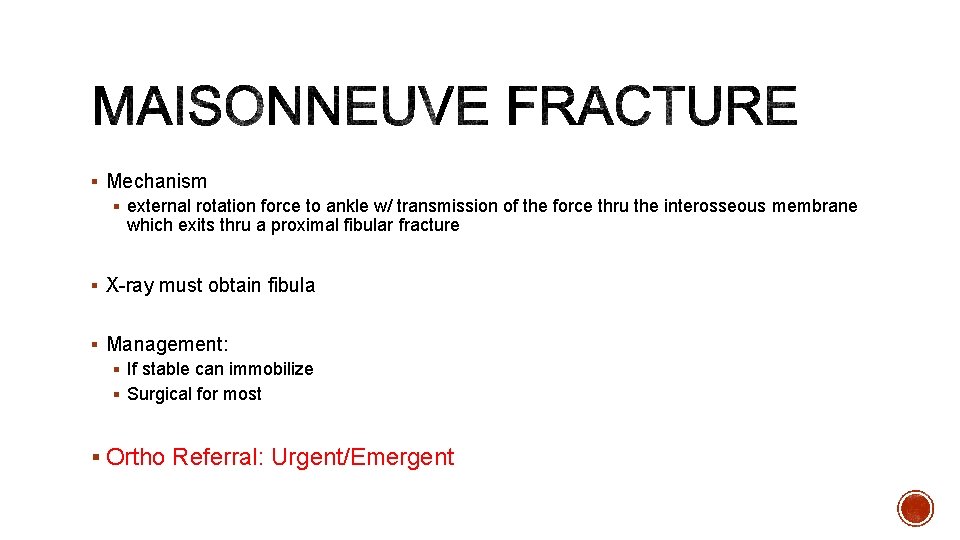
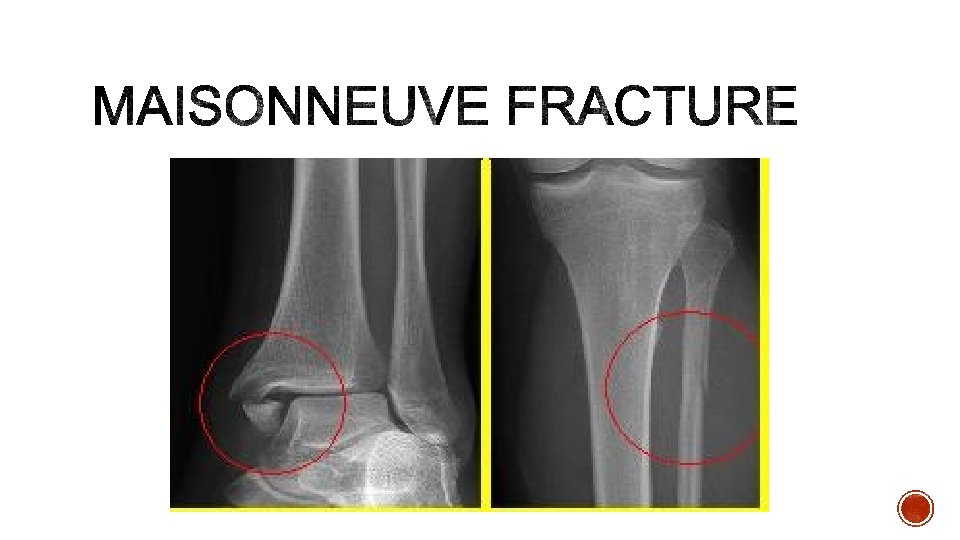
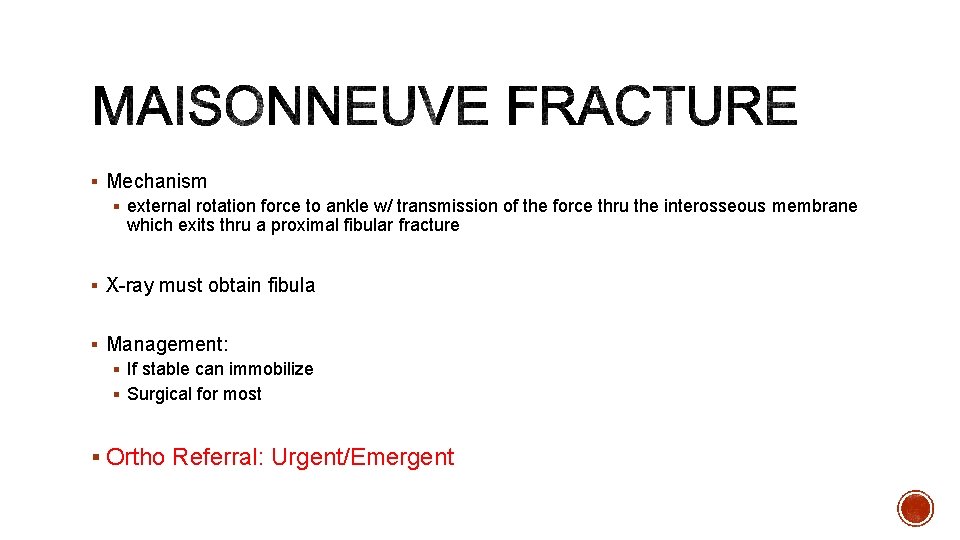
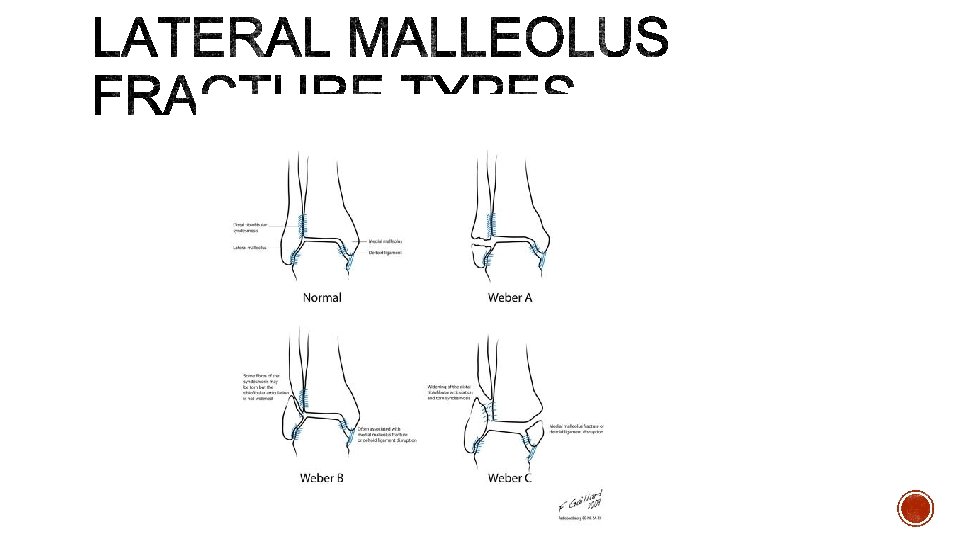
§ Mechanism § external rotation force to ankle w/ transmission of the force thru the interosseous membrane which exits thru a proximal fibular fracture § X-ray must obtain fibula § Management: § If stable can immobilize § Surgical for most § Ortho Referral: Urgent/Emergent
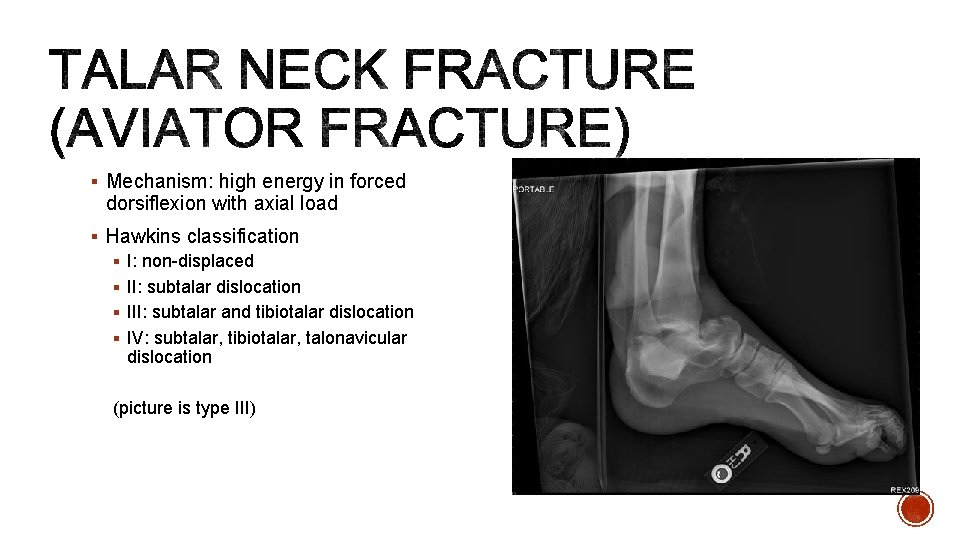
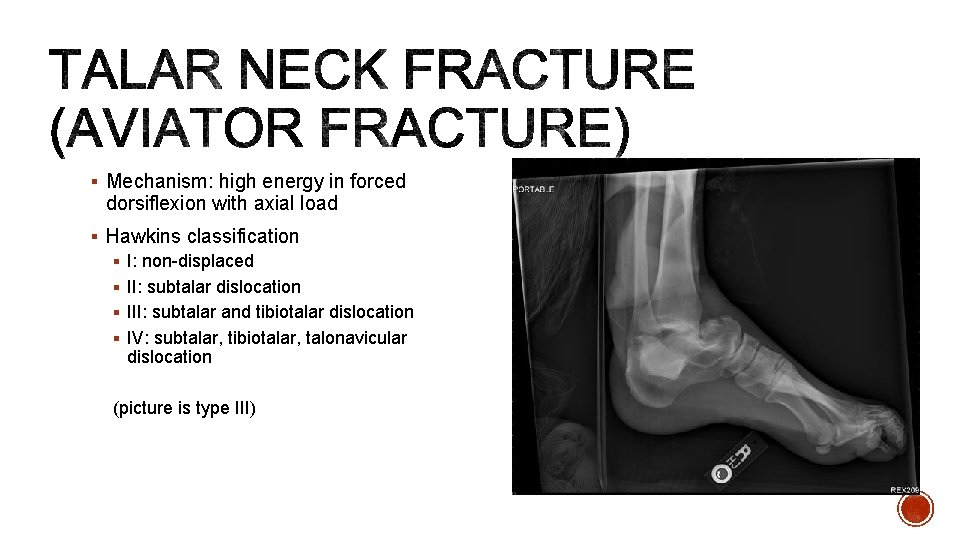
§ Mechanism: high energy in forced dorsiflexion with axial load § Hawkins classification § I: non-displaced § II: subtalar dislocation § III: subtalar and tibiotalar dislocation § IV: subtalar, tibiotalar, talonavicular dislocation (picture is type III)
§ Imaging: § X-ray: Canale View (optimal for neck) § CT scan for displacement § Treatment: § ALL cases require emergent reduction § Non-displaced: short leg cast 8 -12 weeks NWB for 6 weeks § Operative: all displaced fractures § Ortho referral: Emergent
§ Mechanism: traumatic axial loading § Avulsions can be due to different mechanisms (strong gastroc contraction or inversion plantar flexion) § Associated Injuries: § Extension to calcaneocuboid joint 63% § Vertebral injuries 10% § Contralateral Calcaneus 10% § High complication rate
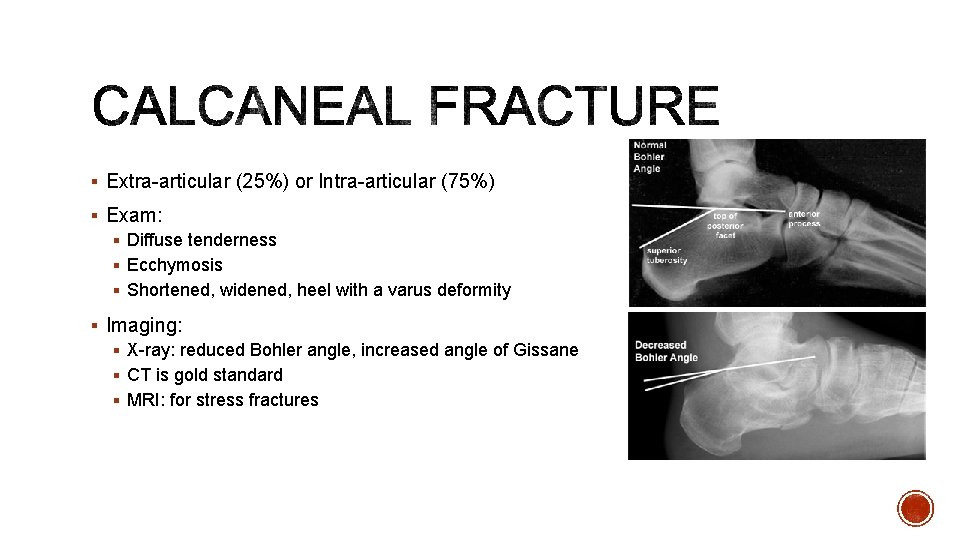
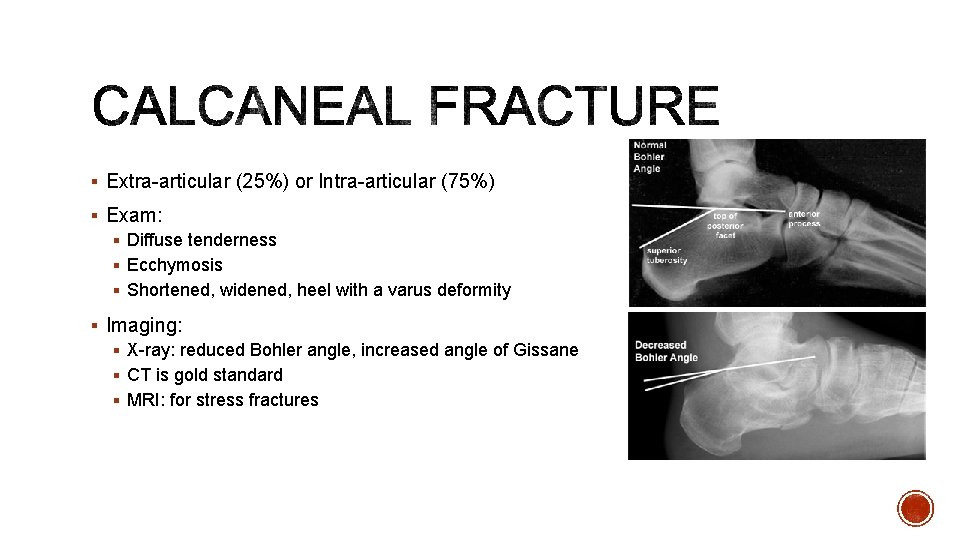
§ Extra-articular (25%) or Intra-articular (75%) § Exam: § Diffuse tenderness § Ecchymosis § Shortened, widened, heel with a varus deformity § Imaging: § X-ray: reduced Bohler angle, increased angle of Gissane § CT is gold standard § MRI: for stress fractures
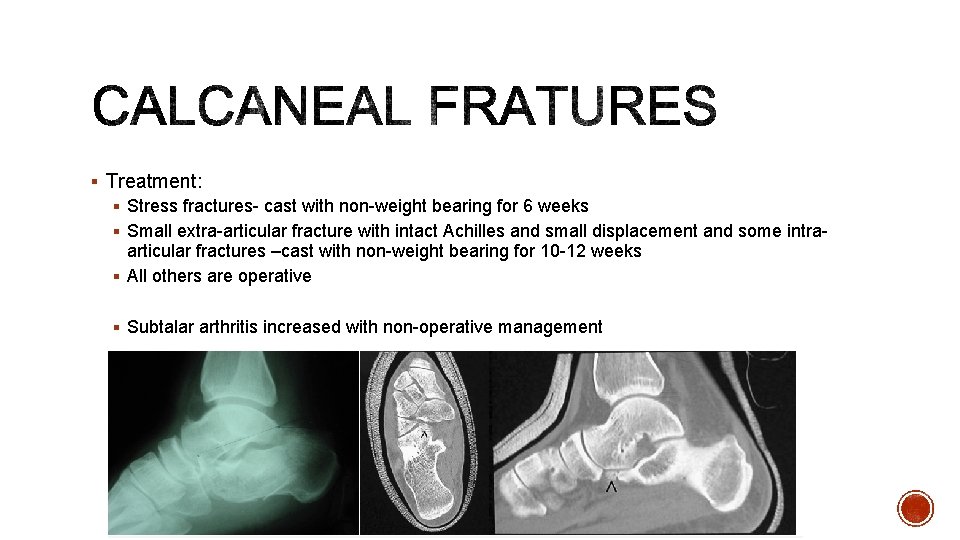
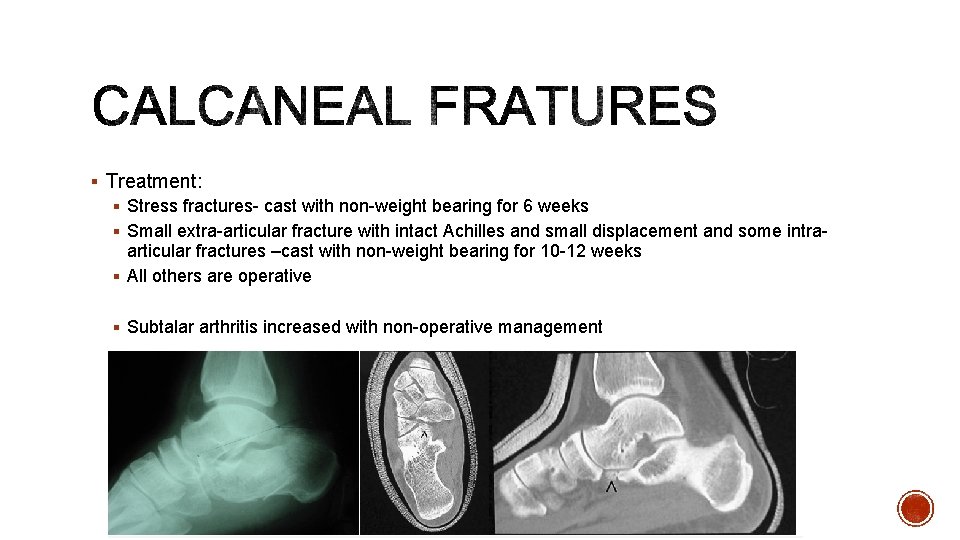
§ Treatment: § Stress fractures- cast with non-weight bearing for 6 weeks § Small extra-articular fracture with intact Achilles and small displacement and some intraarticular fractures –cast with non-weight bearing for 10 -12 weeks § All others are operative § Subtalar arthritis increased with non-operative management
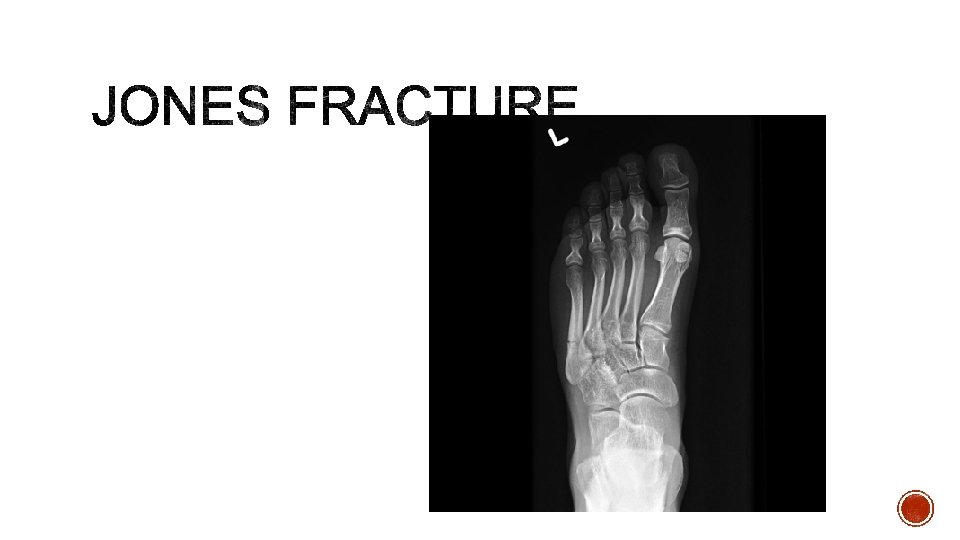
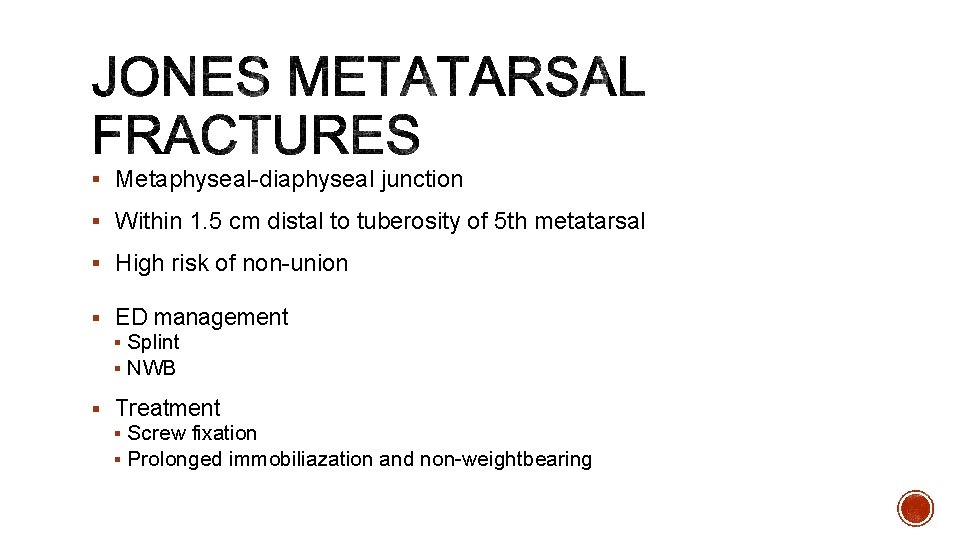
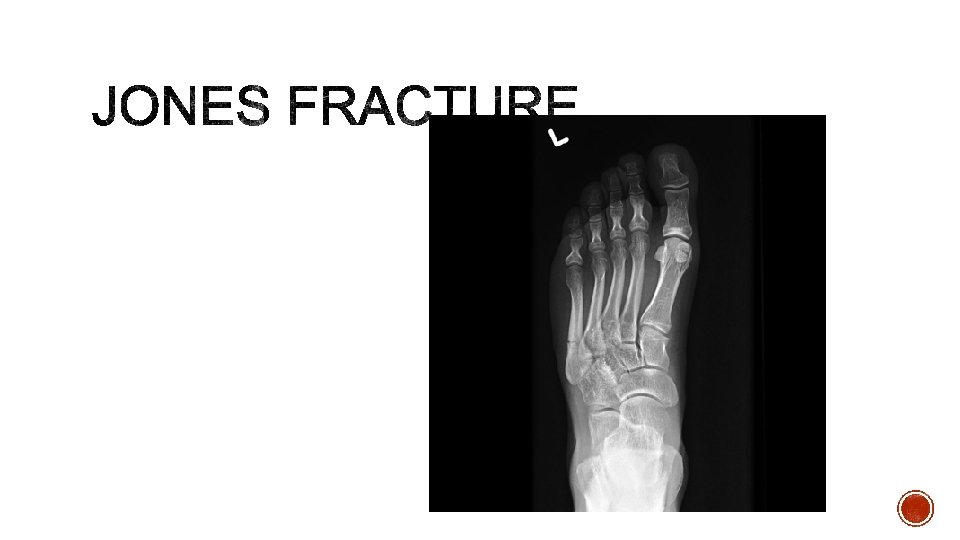
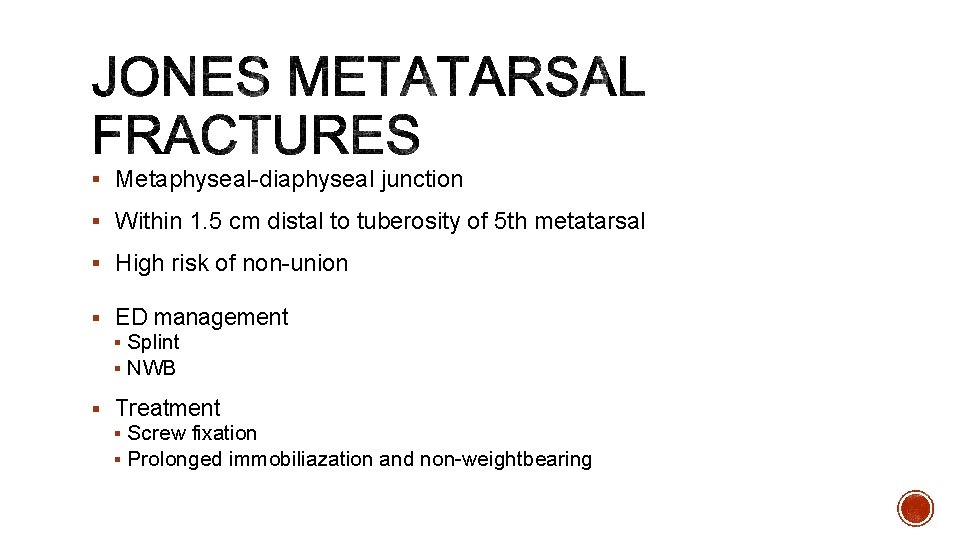
§ Metaphyseal-diaphyseal junction § Within 1. 5 cm distal to tuberosity of 5 th metatarsal § High risk of non-union § ED management § Splint § NWB § Treatment § Screw fixation § Prolonged immobiliazation and non-weightbearing
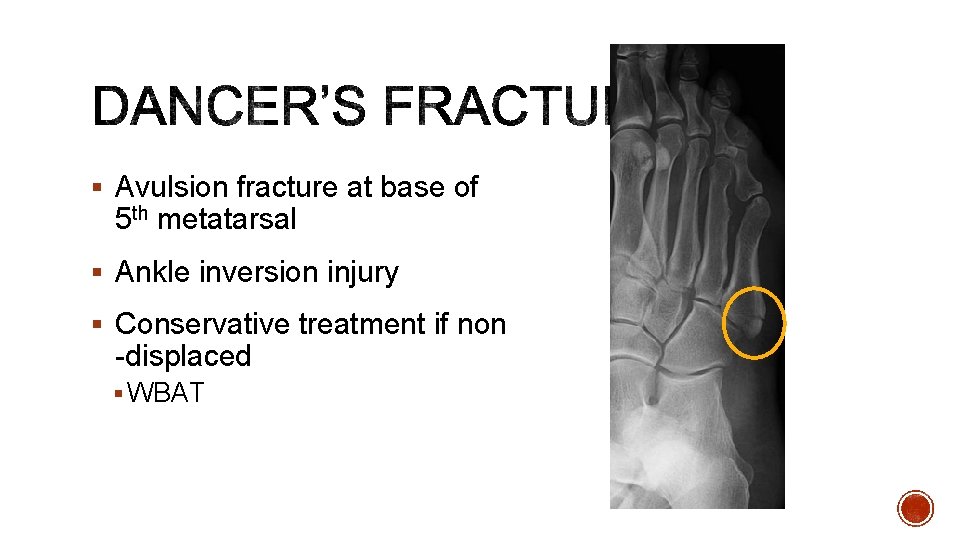
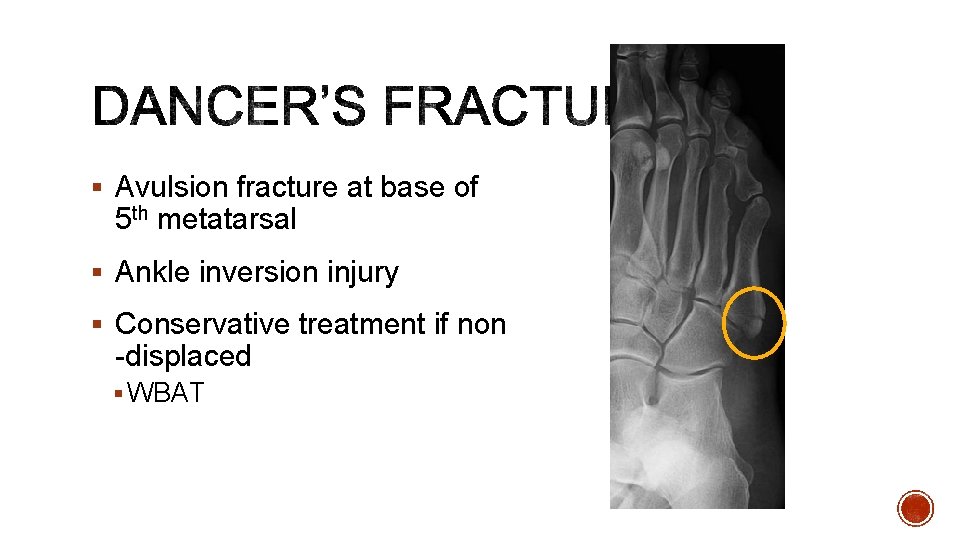
§ Avulsion fracture at base of 5 th metatarsal § Ankle inversion injury § Conservative treatment if non -displaced § WBAT
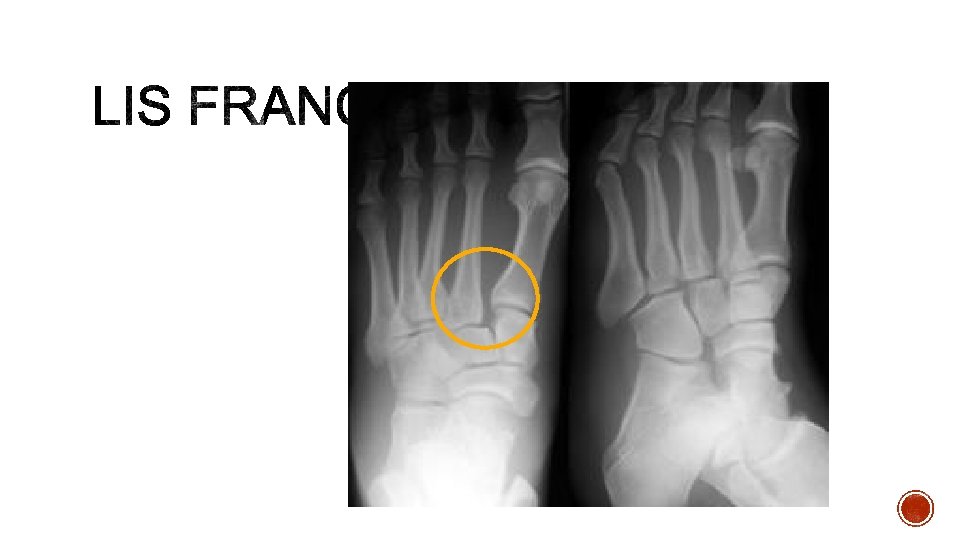
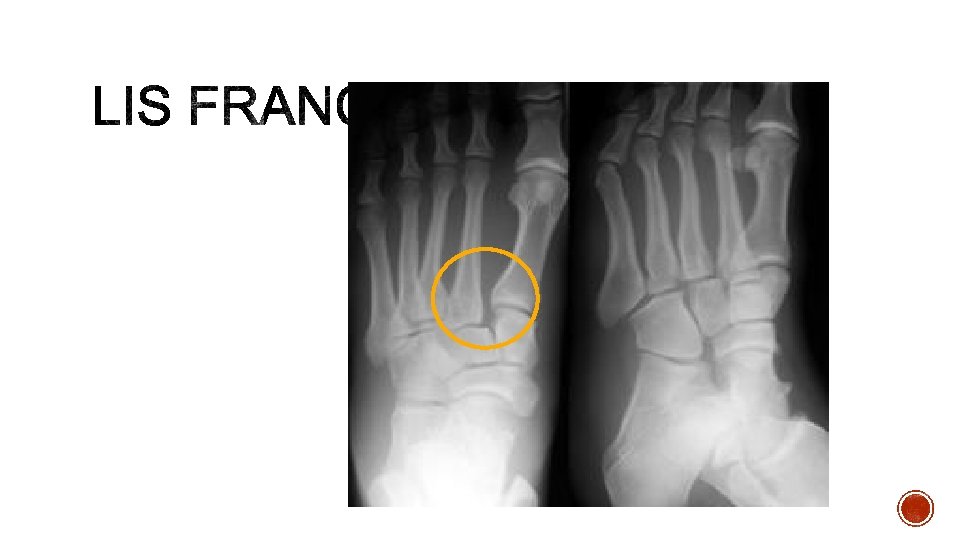
§ Axial load through a hyperplantar flexed foot § Injuries range from mild sprains to severe dislocations § Dislocations often associated with fractures § Metatarsal fractures in 95% § Tarsal fractures in 39%
§ Diagnostic clues § Midfoot swelling § Plantar bruising § Fleck sign § Avulsion of Lisfranc ligament from base of 2 nd metatarsal § Always consider compartment syndrome § Imaging: x-ray, always get stress views if you have high suspicion § MRI: for purely ligamentous injury § Treatment: § Cast for 8 weeks if non-displaced and no fracture § Surgery for most others
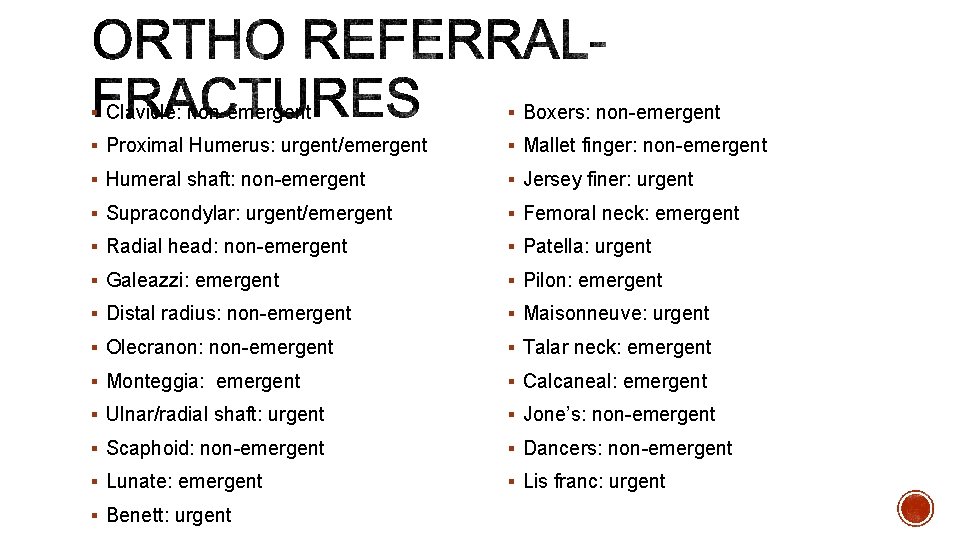
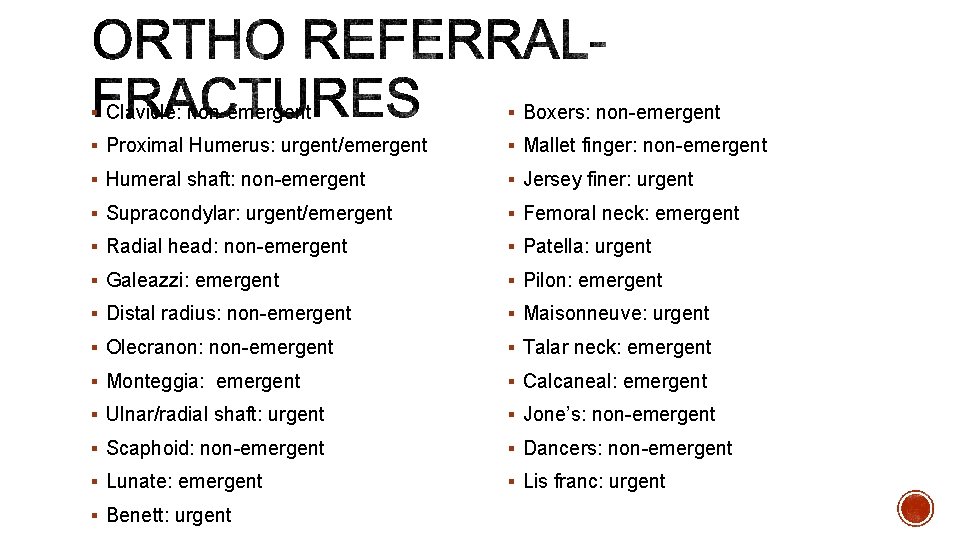
§ Clavicle: non-emergent § Boxers: non-emergent § Proximal Humerus: urgent/emergent § Mallet finger: non-emergent § Humeral shaft: non-emergent § Jersey finer: urgent § Supracondylar: urgent/emergent § Femoral neck: emergent § Radial head: non-emergent § Patella: urgent § Galeazzi: emergent § Pilon: emergent § Distal radius: non-emergent § Maisonneuve: urgent § Olecranon: non-emergent § Talar neck: emergent § Monteggia: emergent § Calcaneal: emergent § Ulnar/radial shaft: urgent § Jone’s: non-emergent § Scaphoid: non-emergent § Dancers: non-emergent § Lunate: emergent § Lis franc: urgent § Benett: urgent
§ Orthobullets. com § Radiopaedia. org § Wheelesonline. com
 Ashley crum
Ashley crum Crum definition
Crum definition Kaylene crum
Kaylene crum Ailsa crum
Ailsa crum Resident and family engagement
Resident and family engagement Resident and family engagement
Resident and family engagement 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad General medicine lecture
General medicine lecture Ashley ridge lockdown
Ashley ridge lockdown Ashley ridge high school parking pass
Ashley ridge high school parking pass Resident set management
Resident set management Resident retention
Resident retention Resident set management
Resident set management Gross income means
Gross income means Divine intervention podcast biostatistics
Divine intervention podcast biostatistics Resident lifecycle
Resident lifecycle Describe the care team and the chain of command
Describe the care team and the chain of command Attending vs resident
Attending vs resident Examples of misappropriation of resident property
Examples of misappropriation of resident property If a resident with ad shows violent behavior the na should
If a resident with ad shows violent behavior the na should Chapter 10 positioning transfers and ambulation
Chapter 10 positioning transfers and ambulation Partially resident textures
Partially resident textures Acgme resident survey
Acgme resident survey Employment of non-resident aliens in the philippines
Employment of non-resident aliens in the philippines Orientation and resident rights quiz
Orientation and resident rights quiz Customer service conflict resolution
Customer service conflict resolution Define resident flora
Define resident flora Magic mask
Magic mask Resident assessment instrument definition
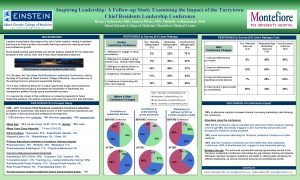
Resident assessment instrument definition Tarrytown chief resident conference
Tarrytown chief resident conference Transamerica estate planning foreign nationals
Transamerica estate planning foreign nationals Yelena bogdan md
Yelena bogdan md Acgme resident survey questions
Acgme resident survey questions Pab ankle fracture
Pab ankle fracture Types of family in community medicine
Types of family in community medicine Principles of family medicine
Principles of family medicine Halifax family medicine residency
Halifax family medicine residency Meritus health family medicine residency
Meritus health family medicine residency Family medicine fellowship
Family medicine fellowship Milestones family medicine
Milestones family medicine Board review family medicine
Board review family medicine Basic requirements for sound phc
Basic requirements for sound phc Define family practice
Define family practice Shelf exam percentiles
Shelf exam percentiles Function of the family
Function of the family Unfunded residency positions
Unfunded residency positions Af williams clinic
Af williams clinic Kaiser permanente san diego family medicine residency
Kaiser permanente san diego family medicine residency Family medicine in ethiopia
Family medicine in ethiopia Cabarrus family medicine concord
Cabarrus family medicine concord Uthscsa family medicine residency
Uthscsa family medicine residency Slu ent residents
Slu ent residents Screem family medicine
Screem family medicine Dr riaz qureshi
Dr riaz qureshi Isu family medicine
Isu family medicine Urt
Urt Family medicine meaning
Family medicine meaning Duke medicine grand rounds
Duke medicine grand rounds Illinois masonic family medicine residency
Illinois masonic family medicine residency Screem res scoring
Screem res scoring Principle of family medicine
Principle of family medicine Challenges facing family medicine
Challenges facing family medicine Primer family medicine
Primer family medicine Monash university master of public health
Monash university master of public health Yong loo lin school of medicine
Yong loo lin school of medicine Medicine hat school district 76
Medicine hat school district 76 Summerschools.suttontrust
Summerschools.suttontrust Coumadin clinic emory
Coumadin clinic emory Morehouse school of medicine registrar
Morehouse school of medicine registrar Mercer med library
Mercer med library Www.hisdchoice.com to apply online
Www.hisdchoice.com to apply online Difference between nuclear family and joint family
Difference between nuclear family and joint family