Teaching Core Concepts in Family Medicine Using the

- Slides: 40
Teaching Core Concepts in Family Medicine Using the Electronic Health Record Douglas J. Bower, MD, Jim H. Shropshire, MD, Kayleen Papin, MD, Jennifer Frank, MD, Sabina Diehr, MD Medical College of Wisconsin & University of Wisconsin – School of Medicine and Public Health
Why are We Here? Family Physicians recognize that … l EHRs are here to stay l Emerging & evolving technology will be in our students’ future practices. l Technology must be integrated into our teaching Technical – “how to” l Utilization - “FM core principles” l
Session Objectives l Identify opportunities to teach core family medicine principles in the context of an EHR framed within the ACGME competencies. l Discuss strategies for preceptors to optimize their clinical teaching in the context of an EHR. l Discuss strategies for teaching students how to optimally utilize the EHR in patientcentered clinical encounters.
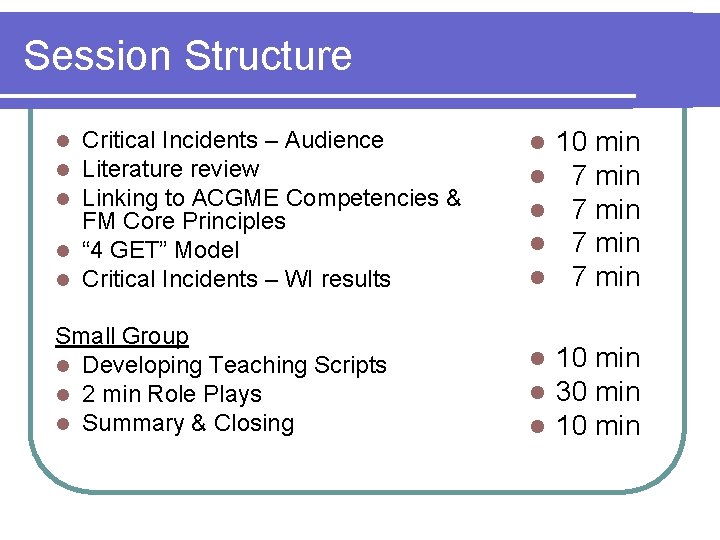
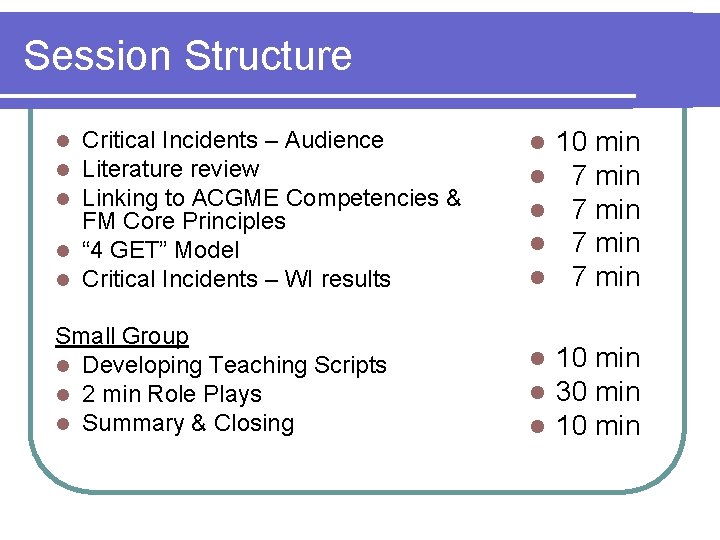
Session Structure Critical Incidents – Audience Literature review Linking to ACGME Competencies & FM Core Principles l “ 4 GET” Model l Critical Incidents – WI results l l l 10 min 7 min Small Group l Developing Teaching Scripts l 2 min Role Plays l Summary & Closing l l l 10 min 30 min 10 min l l l
Critical Incidents
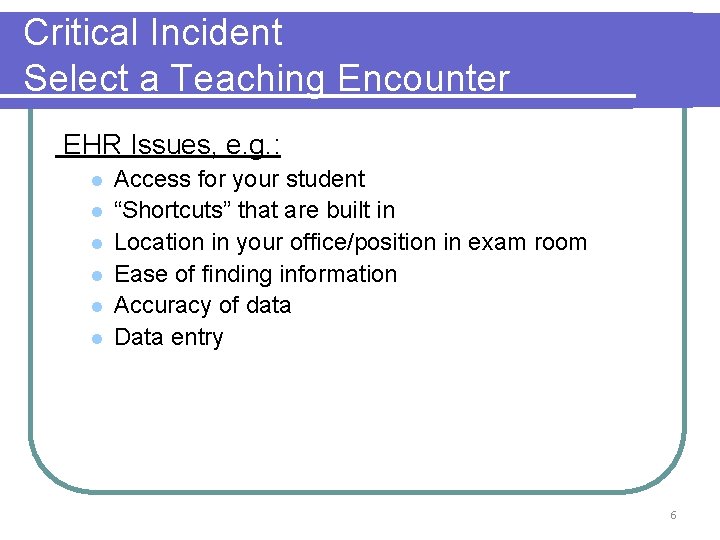
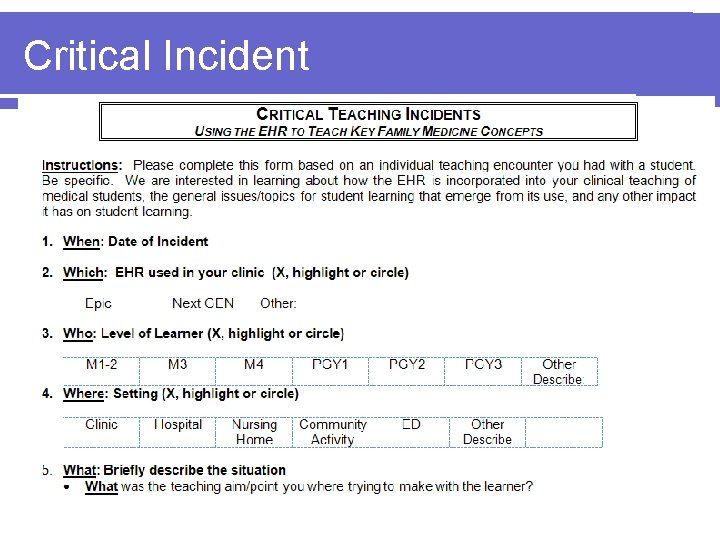
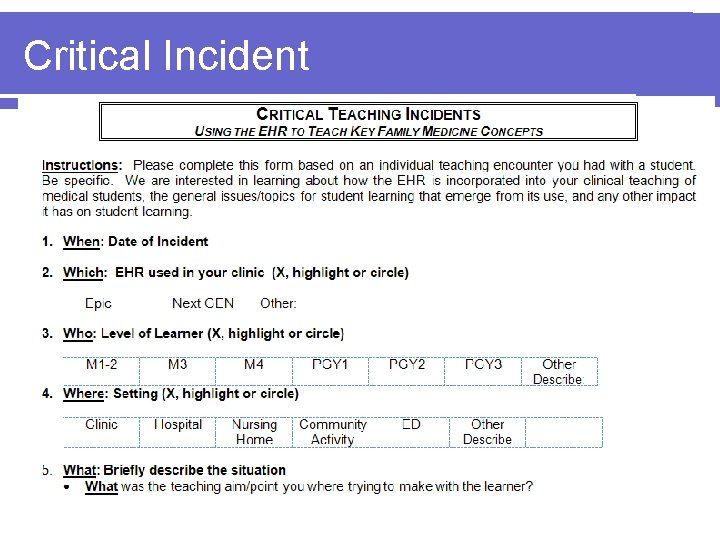
Critical Incident Select a Teaching Encounter EHR Issues, e. g. : l l l Access for your student “Shortcuts” that are built in Location in your office/position in exam room Ease of finding information Accuracy of data Data entry 6
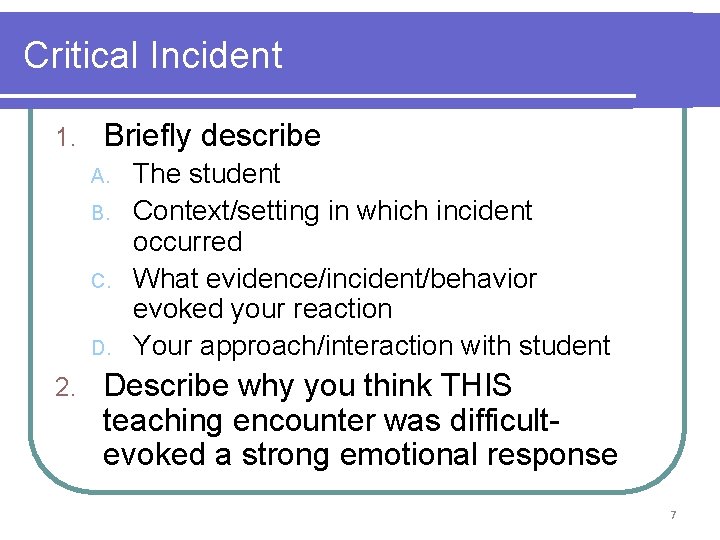
Critical Incident 1. Briefly describe A. B. C. D. 2. The student Context/setting in which incident occurred What evidence/incident/behavior evoked your reaction Your approach/interaction with student Describe why you think THIS teaching encounter was difficultevoked a strong emotional response 7
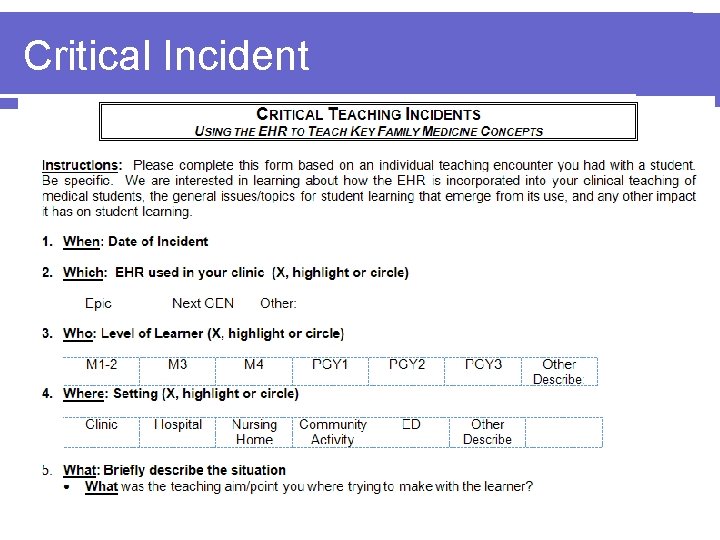
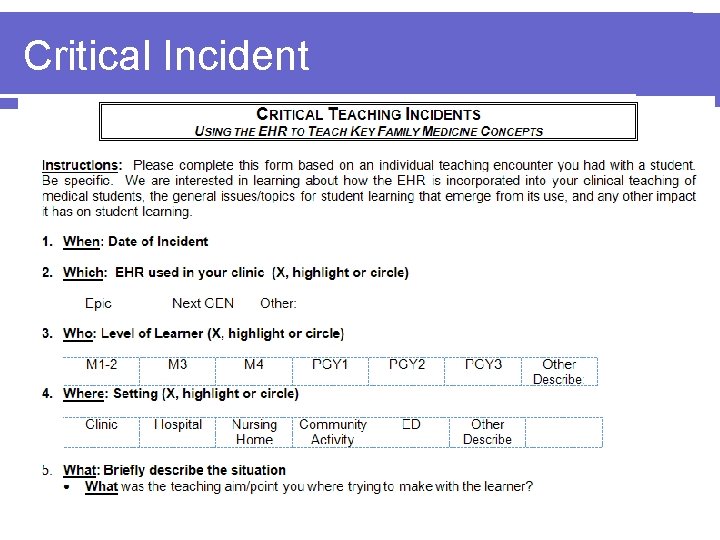
Critical Incident
Literature Review Jennifer Frank, MD
The Evidence out there… l No formal, proven way to teach the EHR l What are barriers you have seen to a “standard” curriculum? No standard EMR l Different practice styles l Different types of technological tools l Different comfort levels among preceptors l
A Conceptual Framework l Organizing the challenges Geographical l Relational l Educational l Structural l
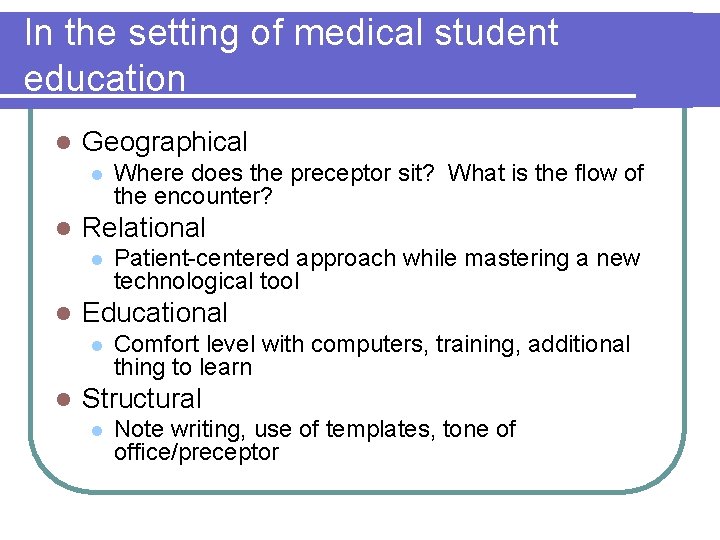
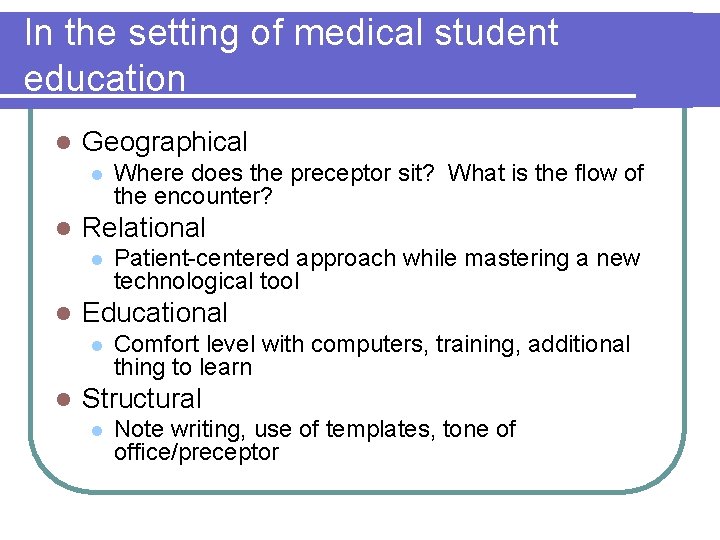
In the setting of medical student education l Geographical l l Relational l l Patient-centered approach while mastering a new technological tool Educational l l Where does the preceptor sit? What is the flow of the encounter? Comfort level with computers, training, additional thing to learn Structural l Note writing, use of templates, tone of office/preceptor
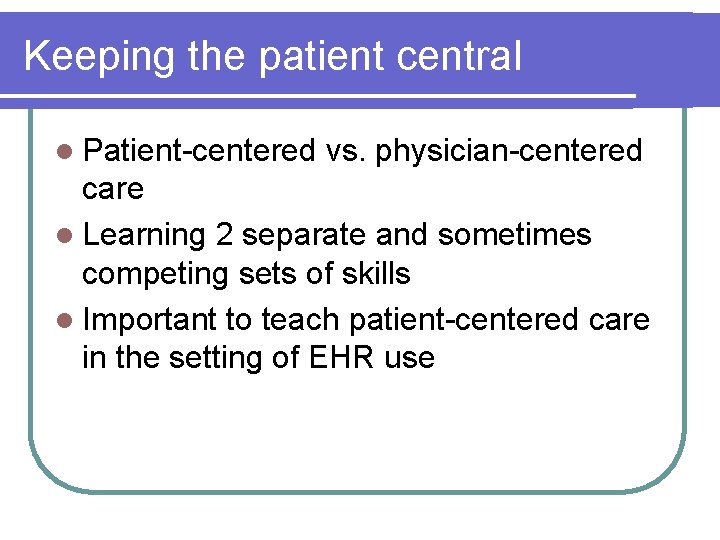
Keeping the patient central l Patient-centered vs. physician-centered care l Learning 2 separate and sometimes competing sets of skills l Important to teach patient-centered care in the setting of EHR use
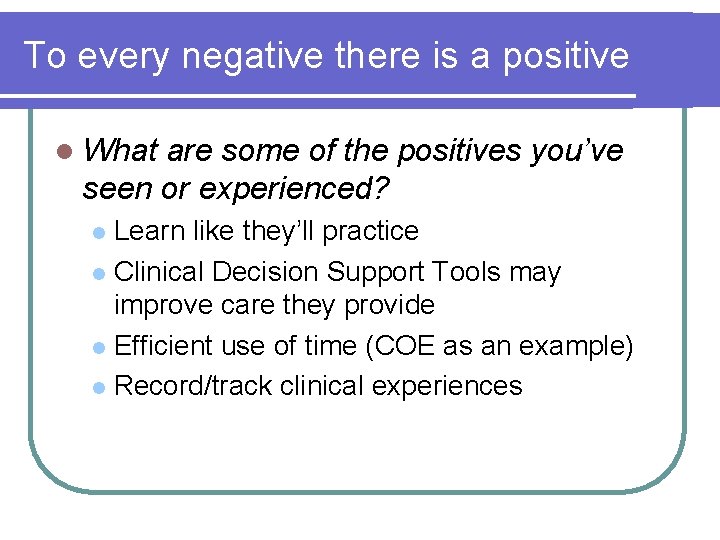
To every negative there is a positive l What are some of the positives you’ve seen or experienced? Learn like they’ll practice l Clinical Decision Support Tools may improve care they provide l Efficient use of time (COE as an example) l Record/track clinical experiences l
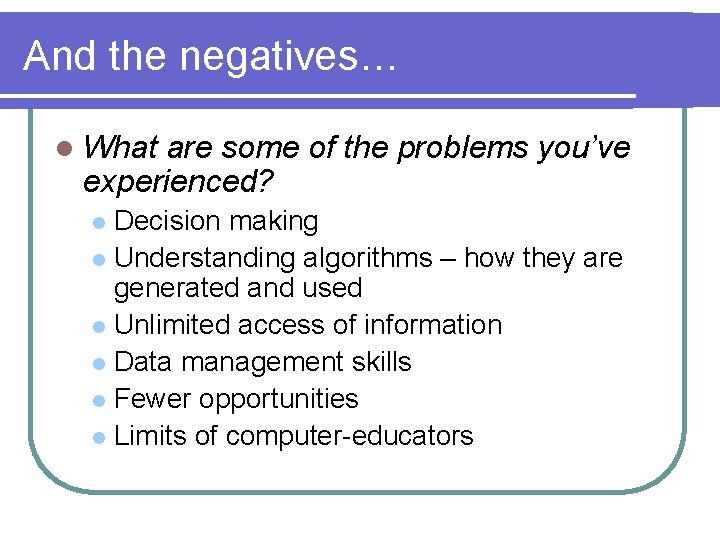
And the negatives… l What are some of the problems you’ve experienced? Decision making l Understanding algorithms – how they are generated and used l Unlimited access of information l Data management skills l Fewer opportunities l Limits of computer-educators l
EHR - ACGME Competencies & Family Medicine Principles Sabina Diehr, MD
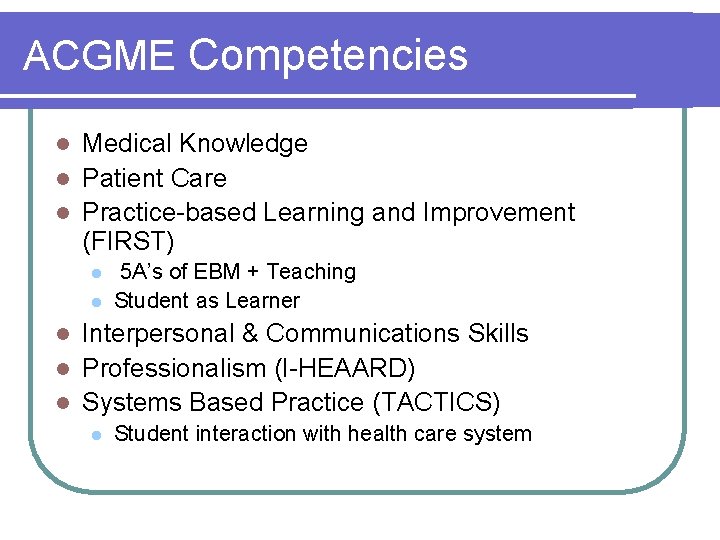
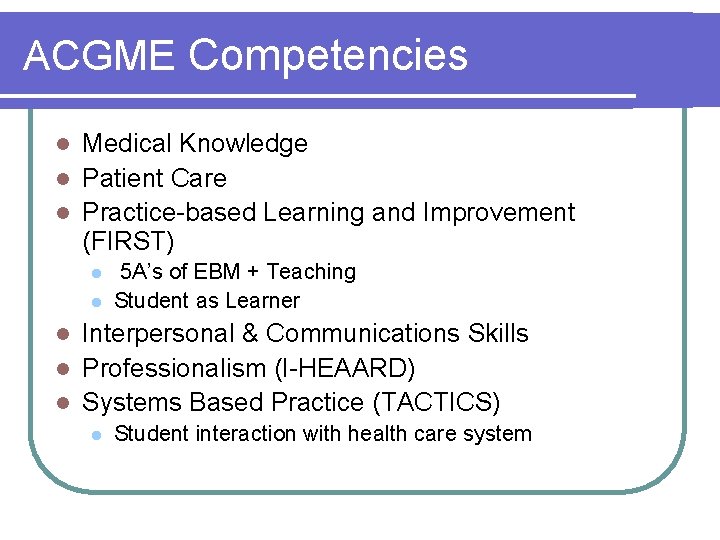
ACGME Competencies Medical Knowledge l Patient Care l Practice-based Learning and Improvement (FIRST) l l l 5 A’s of EBM + Teaching Student as Learner Interpersonal & Communications Skills l Professionalism (I-HEAARD) l Systems Based Practice (TACTICS) l l Student interaction with health care system
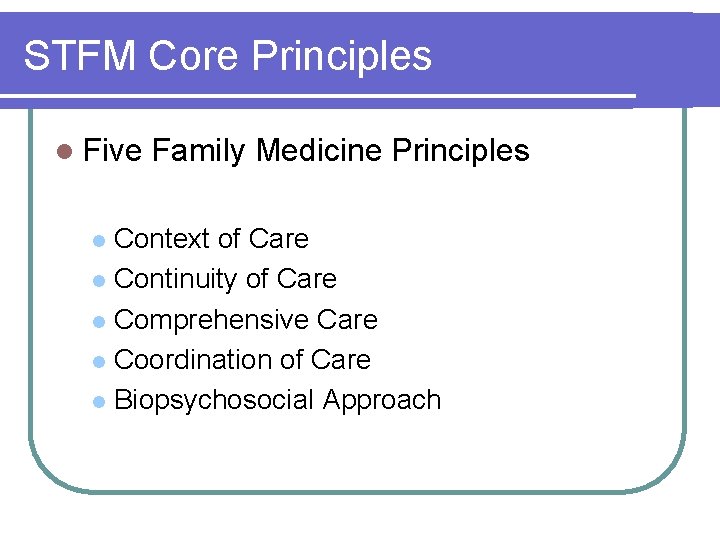
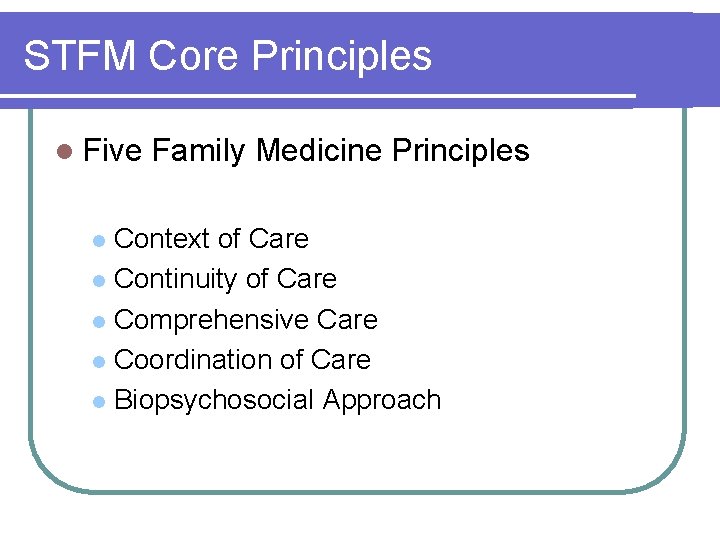
STFM Core Principles l Five Family Medicine Principles Context of Care l Continuity of Care l Comprehensive Care l Coordination of Care l Biopsychosocial Approach l
EHR- Teaching Process The “ 4 GET” Model Jim H. Shropshire, MD
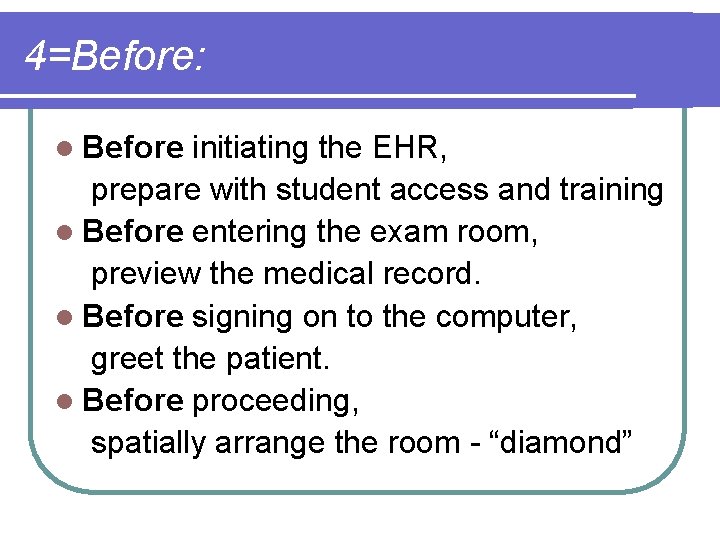
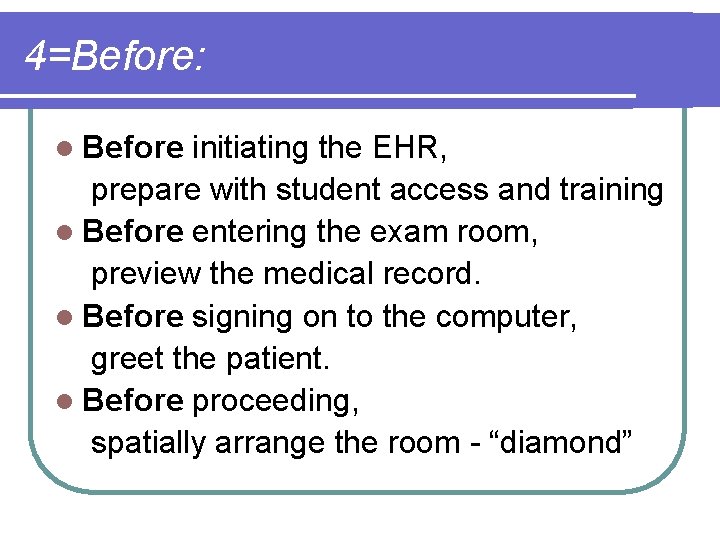
4=Before: l Before initiating the EHR, prepare with student access and training l Before entering the exam room, preview the medical record. l Before signing on to the computer, greet the patient. l Before proceeding, spatially arrange the room - “diamond”
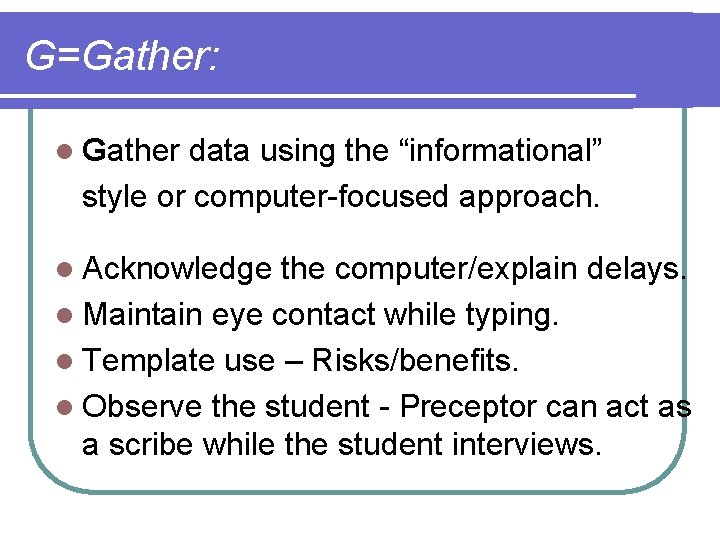
G=Gather: l Gather data using the “informational” style or computer-focused approach. l Acknowledge the computer/explain delays. l Maintain eye contact while typing. l Template use – Risks/benefits. l Observe the student - Preceptor can act as a scribe while the student interviews.
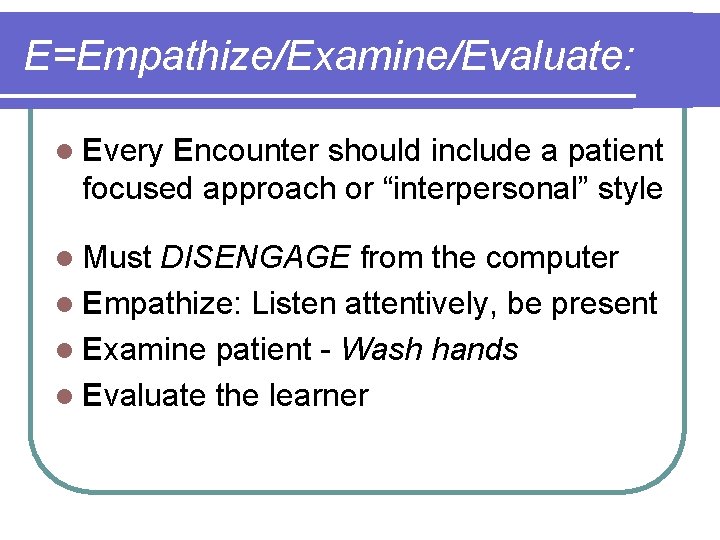
E=Empathize/Examine/Evaluate: l Every Encounter should include a patient focused approach or “interpersonal” style l Must DISENGAGE from the computer l Empathize: Listen attentively, be present l Examine patient - Wash hands l Evaluate the learner
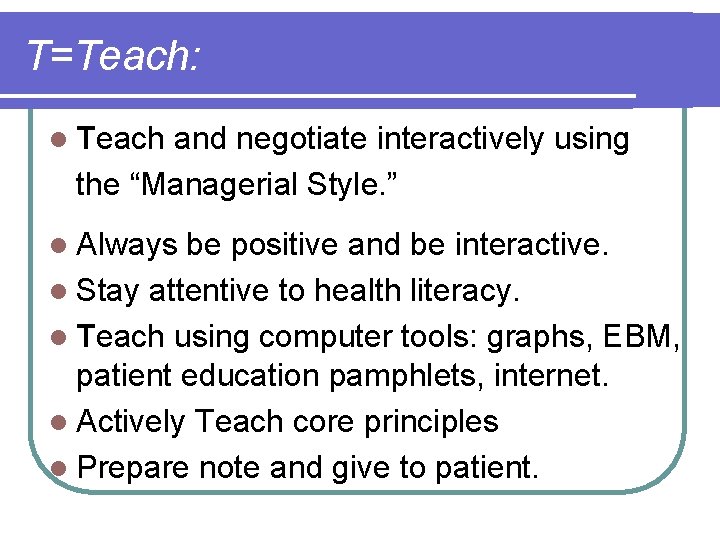
T=Teach: l Teach and negotiate interactively using the “Managerial Style. ” l Always be positive and be interactive. l Stay attentive to health literacy. l Teach using computer tools: graphs, EBM, patient education pamphlets, internet. l Actively Teach core principles l Prepare note and give to patient.
WI Critical Incidents Data Kayleen Papin, MD
Critical Incident
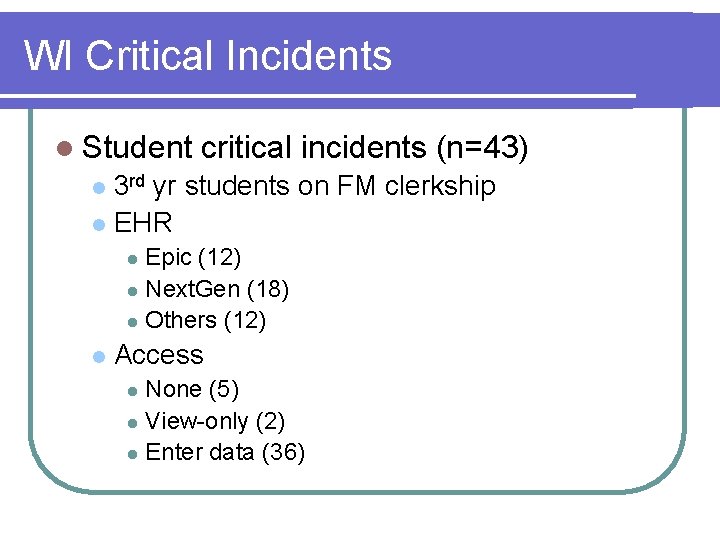
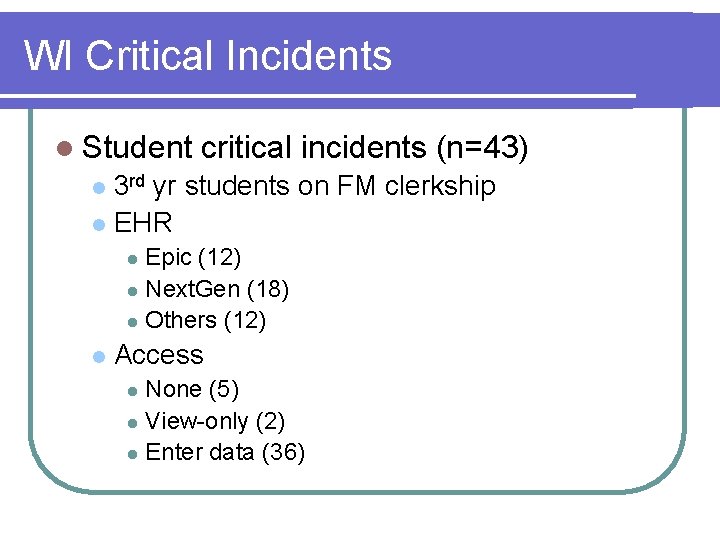
WI Critical Incidents l Student critical incidents (n=43) 3 rd yr students on FM clerkship l EHR l Epic (12) l Next. Gen (18) l Others (12) l l Access None (5) l View-only (2) l Enter data (36) l
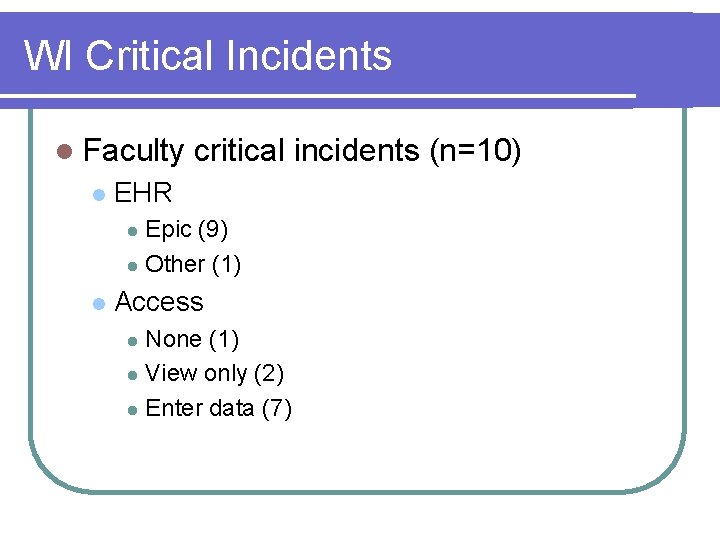
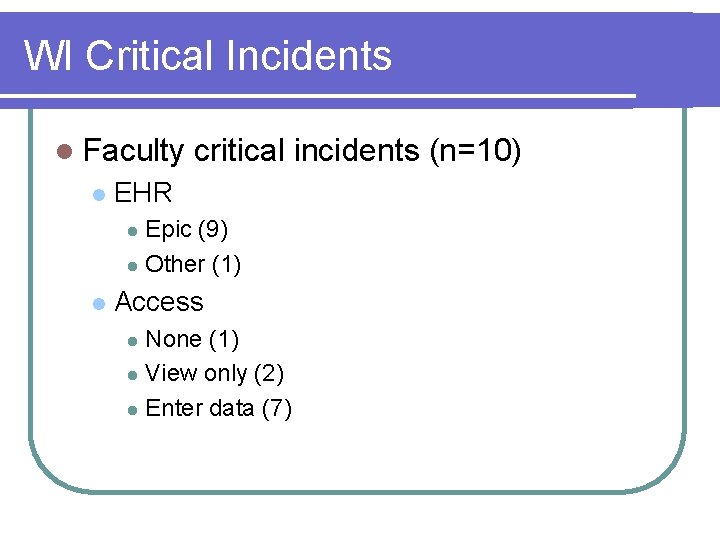
WI Critical Incidents l Faculty l critical incidents (n=10) EHR Epic (9) l Other (1) l l Access None (1) l View only (2) l Enter data (7) l
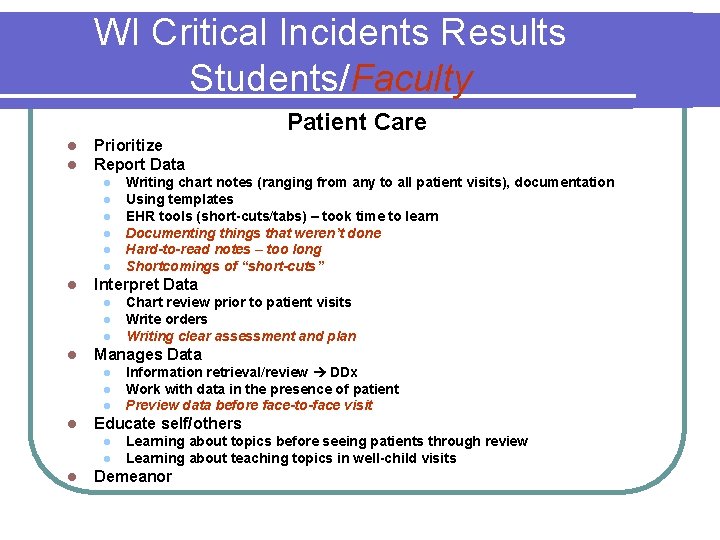
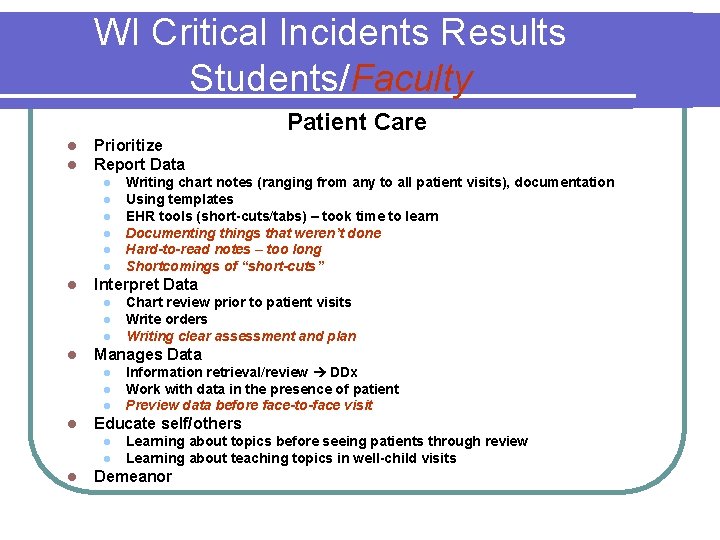
WI Critical Incidents Results Students/Faculty Patient Care l l Prioritize Report Data l l l l Interpret Data l l l Information retrieval/review DDx Work with data in the presence of patient Preview data before face-to-face visit Educate self/others l l l Chart review prior to patient visits Write orders Writing clear assessment and plan Manages Data l l Writing chart notes (ranging from any to all patient visits), documentation Using templates EHR tools (short-cuts/tabs) – took time to learn Documenting things that weren’t done Hard-to-read notes – too long Shortcomings of “short-cuts” Learning about topics before seeing patients through review Learning about teaching topics in well-child visits Demeanor
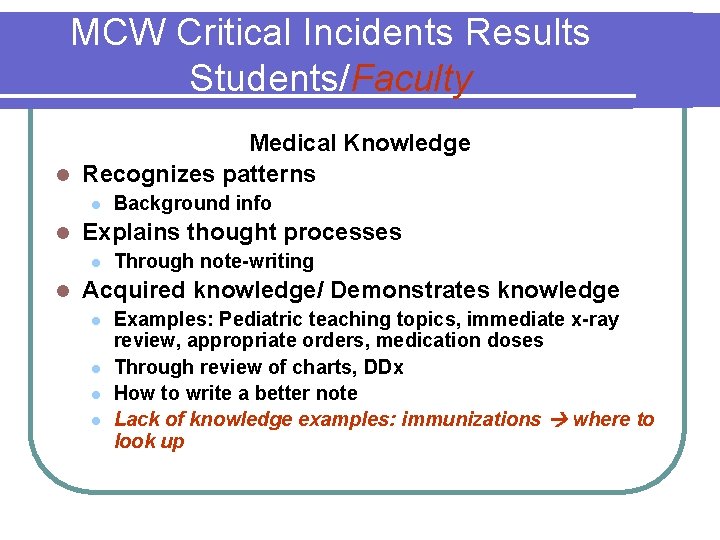
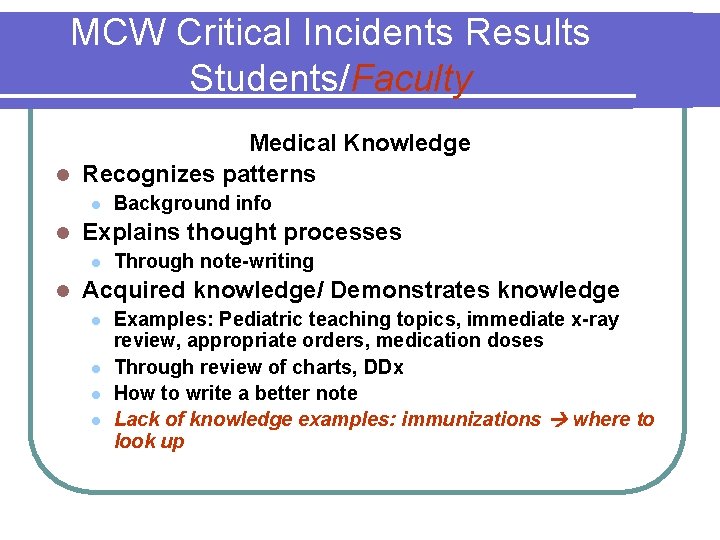
MCW Critical Incidents Results Students/Faculty Medical Knowledge l Recognizes patterns l l Explains thought processes l l Background info Through note-writing Acquired knowledge/ Demonstrates knowledge l l Examples: Pediatric teaching topics, immediate x-ray review, appropriate orders, medication doses Through review of charts, DDx How to write a better note Lack of knowledge examples: immunizations where to look up
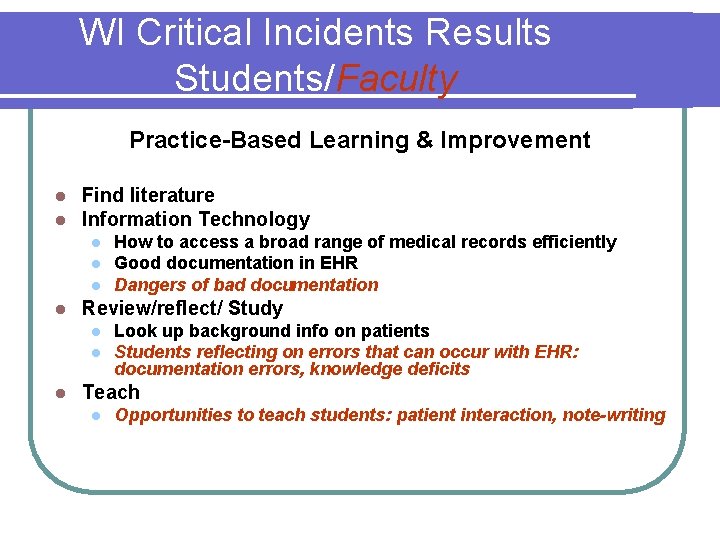
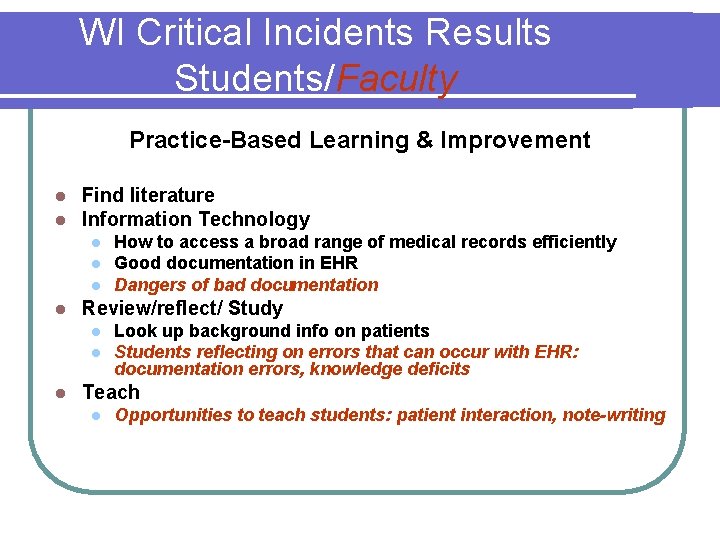
WI Critical Incidents Results Students/Faculty Practice-Based Learning & Improvement l l Find literature Information Technology l l Review/reflect/ Study l l l How to access a broad range of medical records efficiently Good documentation in EHR Dangers of bad documentation Look up background info on patients Students reflecting on errors that can occur with EHR: documentation errors, knowledge deficits Teach l Opportunities to teach students: patient interaction, note-writing
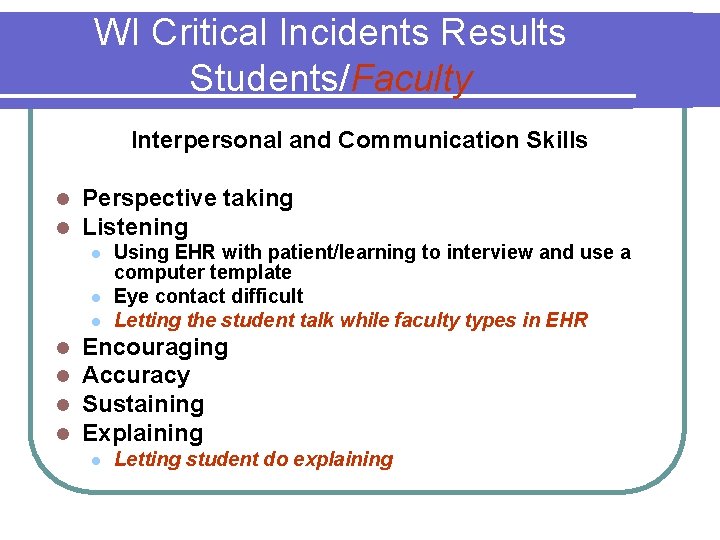
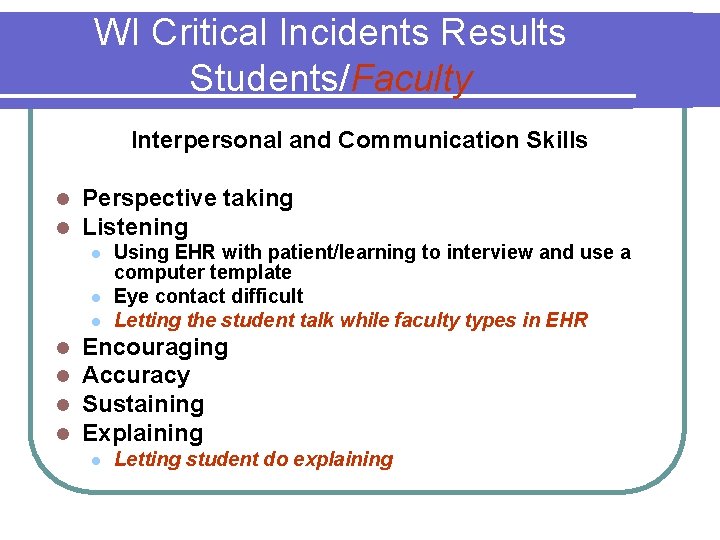
WI Critical Incidents Results Students/Faculty Interpersonal and Communication Skills l l Perspective taking Listening l l l l Using EHR with patient/learning to interview and use a computer template Eye contact difficult Letting the student talk while faculty types in EHR Encouraging Accuracy Sustaining Explaining l Letting student do explaining
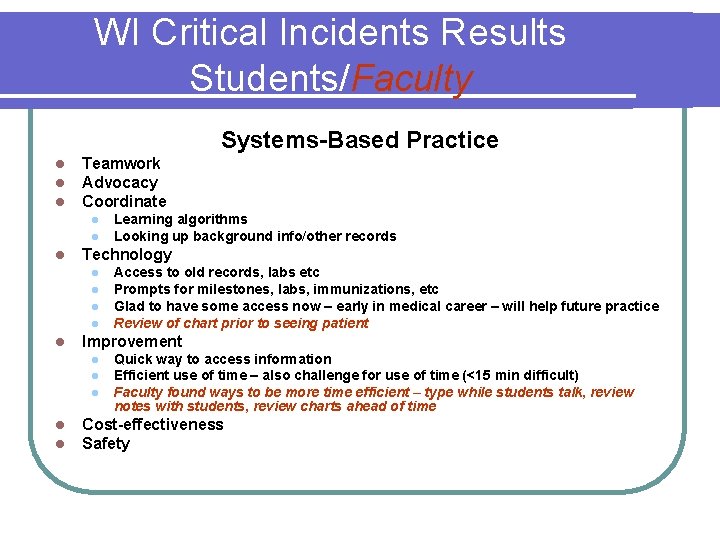
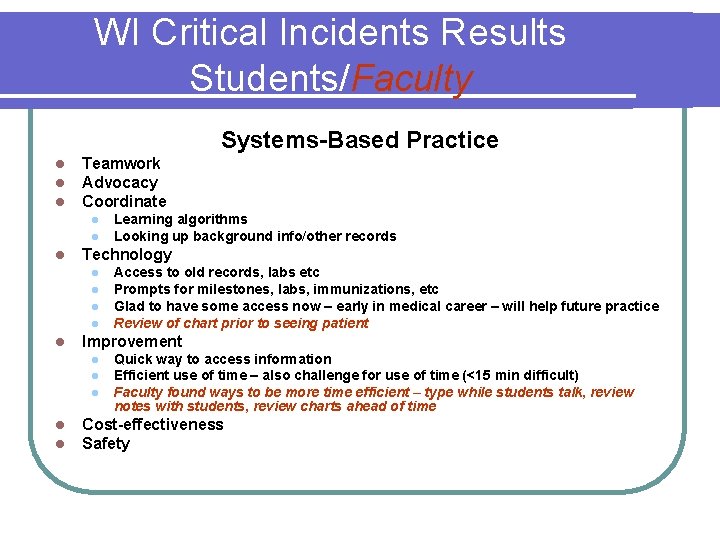
WI Critical Incidents Results Students/Faculty Systems-Based Practice l l l Teamwork Advocacy Coordinate l l l Technology l l l Access to old records, labs etc Prompts for milestones, labs, immunizations, etc Glad to have some access now – early in medical career – will help future practice Review of chart prior to seeing patient Improvement l l l Learning algorithms Looking up background info/other records Quick way to access information Efficient use of time – also challenge for use of time (<15 min difficult) Faculty found ways to be more time efficient – type while students talk, review notes with students, review charts ahead of time Cost-effectiveness Safety
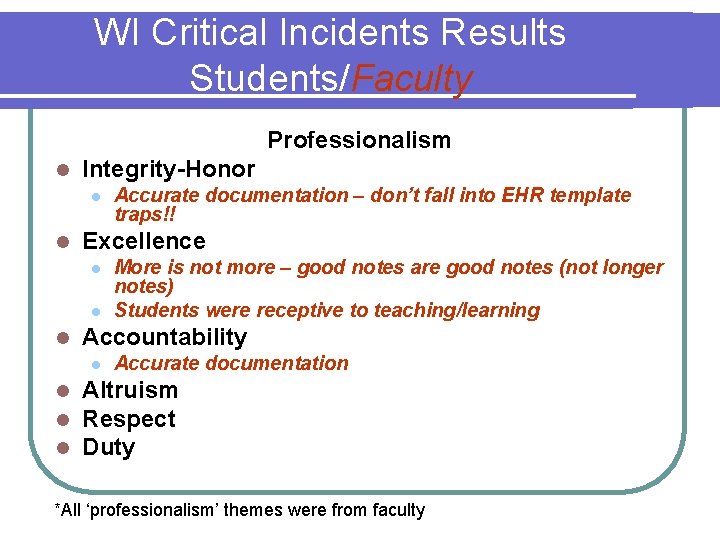
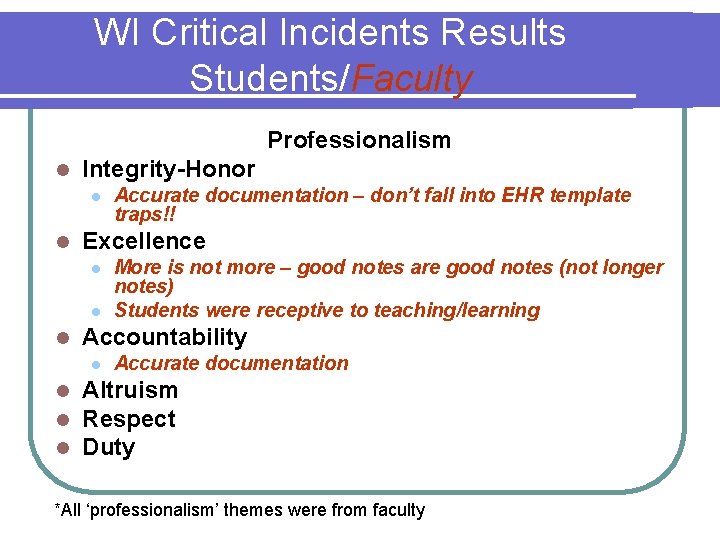
WI Critical Incidents Results Students/Faculty Professionalism l Integrity-Honor l l Excellence l l l More is not more – good notes are good notes (not longer notes) Students were receptive to teaching/learning Accountability l l Accurate documentation – don’t fall into EHR template traps!! Accurate documentation Altruism Respect Duty *All ‘professionalism’ themes were from faculty
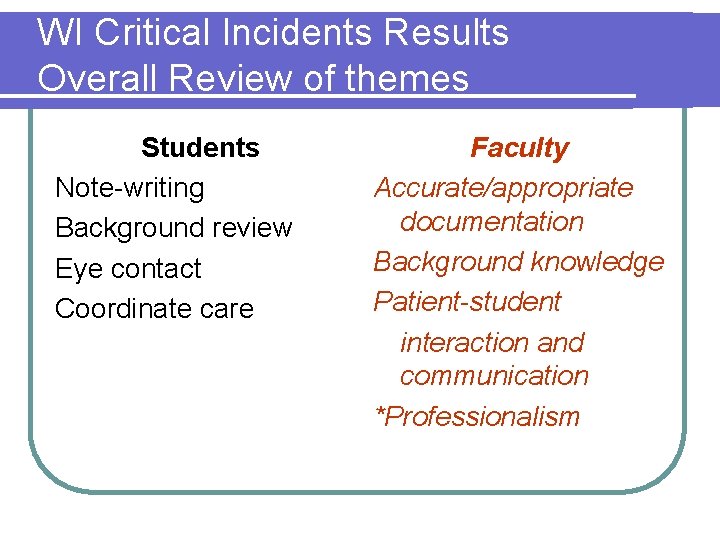
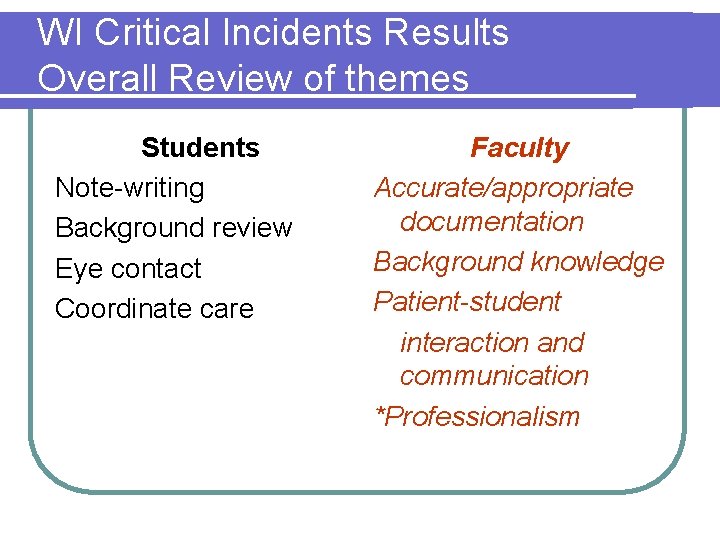
WI Critical Incidents Results Overall Review of themes Students Note-writing Background review Eye contact Coordinate care Faculty Accurate/appropriate documentation Background knowledge Patient-student interaction and communication *Professionalism
Small Groups Developing Teaching Scripts for a Technical and/or Family Medicine Principle involving and EHR.
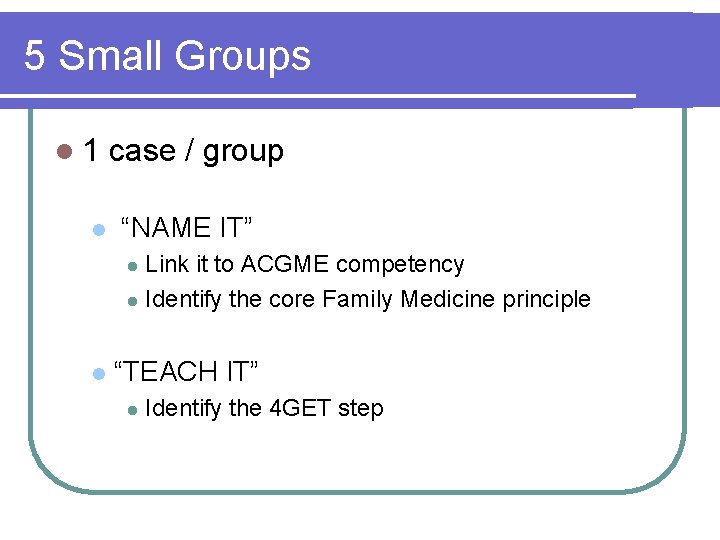
5 Small Groups l 1 l case / group “NAME IT” Link it to ACGME competency l Identify the core Family Medicine principle l l “TEACH IT” l Identify the 4 GET step
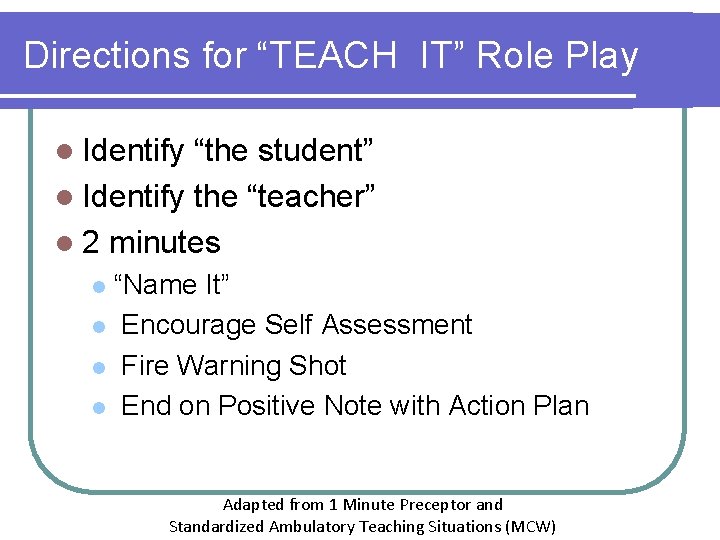
Directions for “TEACH IT” Role Play l Identify “the student” l Identify the “teacher” l 2 minutes “Name It” l Encourage Self Assessment l Fire Warning Shot l End on Positive Note with Action Plan l Adapted from 1 Minute Preceptor and Standardized Ambulatory Teaching Situations (MCW)
Role Plays DEBRIEF

Summary l EHRs are here to stay! l Identify opportunities to teach. l Identify teaching strategies. l 4 GET, but don’t 4 GET about the student
THANKS Everyone! PLEASE fill out your evaluations.
 A company's resources and capabilities represent
A company's resources and capabilities represent 5 core customer and marketplace concepts
5 core customer and marketplace concepts Core concepts of management
Core concepts of management What is the core concept of marketing
What is the core concept of marketing Understanding core database concepts
Understanding core database concepts Core concepts
Core concepts Core concepts of accounting information systems
Core concepts of accounting information systems Core payroll concepts
Core payroll concepts Inner core and outer core
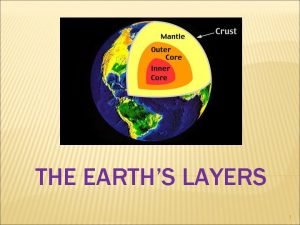
Inner core and outer core Mantle earth meaning
Mantle earth meaning Which layer is the least dense
Which layer is the least dense Core rigidity
Core rigidity Danielson framework summary
Danielson framework summary Bryan zaharko
Bryan zaharko Technical core
Technical core Types of family in community medicine
Types of family in community medicine Principles of family medicine
Principles of family medicine Halifax family medicine residency
Halifax family medicine residency Meritus family practice
Meritus family practice Family medicine fellowships
Family medicine fellowships Milestones family medicine
Milestones family medicine Dr janalynn beste
Dr janalynn beste Principles of primary health care
Principles of primary health care Define family medicine
Define family medicine Internal medicine shelf percentile
Internal medicine shelf percentile Ecomap examples
Ecomap examples St cloud family medicine residency
St cloud family medicine residency Af williams family medicine center
Af williams family medicine center Kaiser permanente san diego family medicine residency
Kaiser permanente san diego family medicine residency Family medicine in ethiopia
Family medicine in ethiopia Cabarrus family medicine concord
Cabarrus family medicine concord Uthscsa internal medicine residents
Uthscsa internal medicine residents St louis university family medicine residency
St louis university family medicine residency Medical genogram symbols
Medical genogram symbols Dr riaz qureshi
Dr riaz qureshi Isu family medicine
Isu family medicine Urt
Urt Family medicine meaning
Family medicine meaning Duke family medicine and community health
Duke family medicine and community health Margaret wiedmann md
Margaret wiedmann md Screem res scoring
Screem res scoring