And Then There Were None Family Medicine Residency






- Slides: 43
And Then There Were None… Family Medicine Residency Program Closures, Mergers & Transitions

Panelists: Michael J. Petrizzi, M. D. , Program Director, Hanover Family Physicians Margaret Wiedmann, M. D. , Program Director, UIC/IL Masonic Family Practice Residency Crystal Cash, M. D. , Program Director, Cook County-Loyola-Provident Family Practice Residency Eugene Hong, M. D. Program Director, Drexel University College of Medicine Janet Fleetwood, Ph. D, . Professor & Vice Chair for Academic Affairs, Drexel University College of Medicine (Moderator)
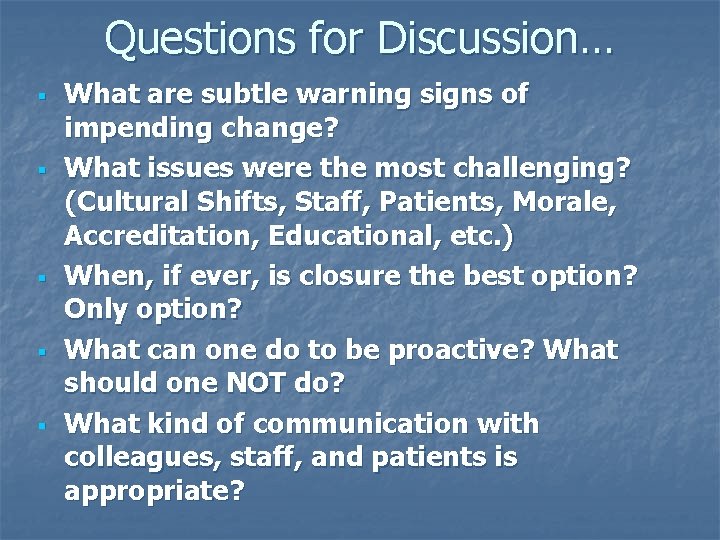
Questions for Discussion… § § § What are subtle warning signs of impending change? What issues were the most challenging? (Cultural Shifts, Staff, Patients, Morale, Accreditation, Educational, etc. ) When, if ever, is closure the best option? Only option? What can one do to be proactive? What should one NOT do? What kind of communication with colleagues, staff, and patients is appropriate?

What Do Data Show? n n n Community based programs disproportionately affected Most hospitals were private, nonprofit Most had underserved focus Most open for 11+ years Board pass rates average 98% Financial, political and institutional changes have major impact Gonzalez, E. et. al. “A Study of Closure of Family Practice Residency Programs, ” Family Medicine, November-December 2003
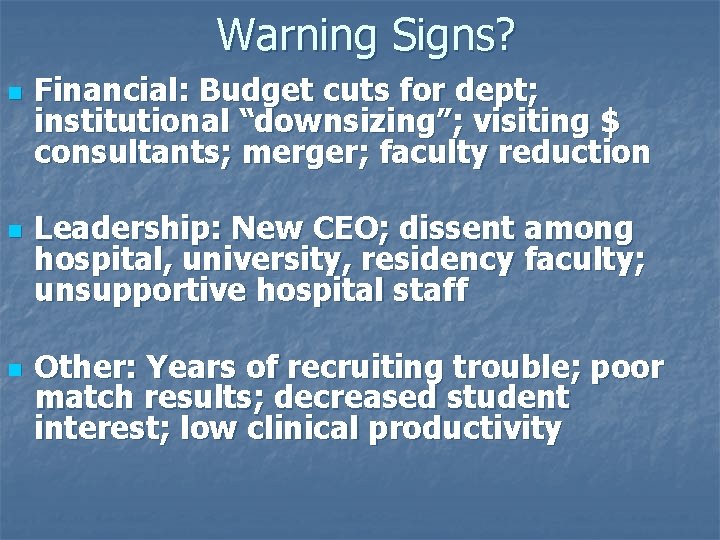
Warning Signs? n n n Financial: Budget cuts for dept; institutional “downsizing”; visiting $ consultants; merger; faculty reduction Leadership: New CEO; dissent among hospital, university, residency faculty; unsupportive hospital staff Other: Years of recruiting trouble; poor match results; decreased student interest; low clinical productivity
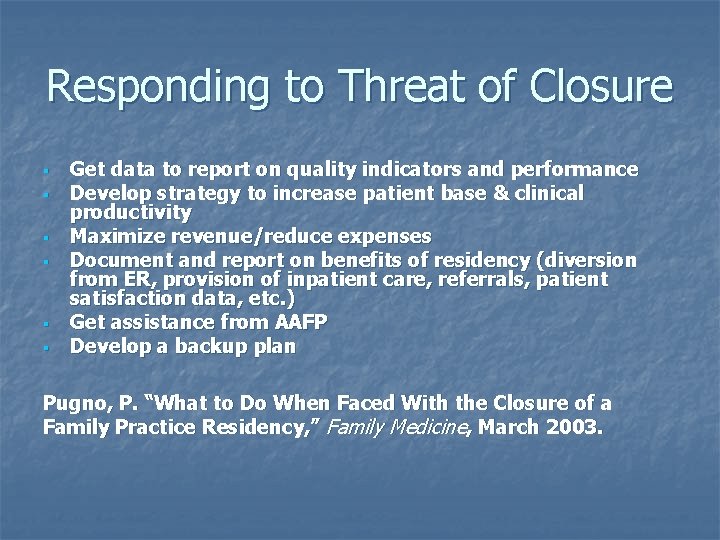
Responding to Threat of Closure § § § Get data to report on quality indicators and performance Develop strategy to increase patient base & clinical productivity Maximize revenue/reduce expenses Document and report on benefits of residency (diversion from ER, provision of inpatient care, referrals, patient satisfaction data, etc. ) Get assistance from AAFP Develop a backup plan Pugno, P. “What to Do When Faced With the Closure of a Family Practice Residency, ” Family Medicine, March 2003.
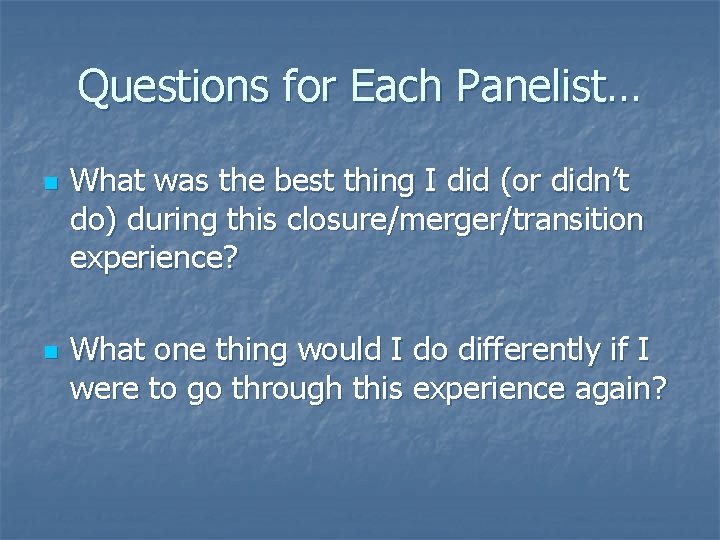
Questions for Each Panelist… n n What was the best thing I did (or didn’t do) during this closure/merger/transition experience? What one thing would I do differently if I were to go through this experience again?
Michael Petrizzi, M. D. n n Program Director Hanover Family Physicians Program Closing n Today’s Theme: “Mike – Title? ” n
Hanover Family Physicians Michael J. Petrizzi, MD Associate Professor of Family Medicine
Background n n n 1987 – Dean at MCV asked Dept. of Family Medicine to start new FP Residency at the University 1988 – Provisional Accreditation 1989 – First class interns arrive

Program Design n n All 3 -years at University Hospital Outpatient training at a private practice Private practice has teaching contract with Commonwealth of Virginia PGY I slots funded via pass throughs PGY II and III funded through state contract.
Early History n n n Full spectrum care training All faculty do OB Additional focus on Procedural Training, Sports Medicine, and Geriatrics
Progress Report n n Move into 10, 000 sq. foot facility in 1993 Building owned by MCV Hospitals Full accreditation for 5 years in 1993, 1998, 2003 Greater than two-thirds of graduates stayed in Virginia, meeting departmental and residency goals
Wrinkles in the Sails n n n Community hospital opens 3 miles away in 1998 University’s new President declares need for new identify for VCU and need to reclaim status as research institution and tertiary care center By 2000, University and Hospital funds decreased – Dept. has to provide ALL of the gap funding
What To Do? n n Dean gives permission to seek funding from outside, i. e. community hospital March 2001 – First support check arrives Sept. 2001 – Major increase starts Hospital anticipates 18 -slots pass through, funding based on info from CMS Intermediary
Now What!! n n n Commonwealth of Virginia experienced major budget short fall $1. 8 million dollars cut from Department’s budget – all programs share that burden and ask community hospitals to make up funding One month later, community hospital is told that pre-established cap of ONE is all that they will get
SO n n Decide to merge the Hanover (suburban) and Blackstone (rural) Residencies – both under community hospital system Submit new PIF – 1/2 Site visit Oct. 2003 Recruit to new program
Then n RRC approves suburban portion, but tables vote on rural since too far from hospital Effectively means virtually no pass through funds for other portion February 2004 – Community hospital system informs both – DO NOT take in intern class and close Hanover
Results n n n HFP must close – only 50% of funds would be available Inform “new” interns – no program Place current interns – fortunately found slots Graduate current PGY III’s Secured funds to have one more year for PGY II’s
Reflections n n n It is not location, it is not just mission It is not necessarily even about quality It is about funding and decision regarding PGY II and PGY III as state supported, may have been the right one, yet it also lead to closure
The Future n n n Faculty and administrative assistance to our other residencies in the system Individual academic and professional pursuits Continue to serve over 50, 000 patients in our community
Support Structures n n n Working with Department regarding undergraduate training Relationship with Department was key Relationship and commitment from Chairman will never be forgotten Efforts by AAFP & RRC were also appreciated Fellow Directors in the system were great
Gratitude n BUT I AM SO THANKFUL FOR OUR STAFF, MY PARTNERS, AND OUR INCREDIBLE FAMILES!!
Margaret Wiedmann. M. D. n n Program Director UIC/IL Masonic Family Practice Residency n n Hospitals Merged 2000 Today’s Themes: “Money & Morale”
Era of Mergers-Late 1990’s Chicago n n Many community hospitals in Chicago with significant actual or projected losses Mergers occurred for financial survival Advocate Health System- not for profit system- 8 hosp, and multiple associated medical groups in Chicago Other competing merged system- Catholic Hospitals
Merger Madness n n n 1998 Ravenswood Merged with Advocate 2000 IL Masonic Merged with Advocate 2000 Advocate combined Ravenswood and Masonic resources and closed Ravenswood
Merger Madness n n 2 Hospitals w/ different cultures, physician characteristics and patient populations, though only 3 miles apart 2 FP residencies UIC(Ravenswood) and Rush(Masonic)-fairly similar Masonic and Rush FPR had agreed to disaffiliate prior to merger but after Rush’s PG’ 1’s graduate UIC/Ravanswood brought in as the new Masonic FPR

Positive Outcome Despite Merger n n n Matched well each year with US grads Expanded from 15 to 24 residents No faculty left because of the merger and most staff stayed despite further distance All residents stayed through merger New, improved FPC
At What Cost n n n All worked harder than ever before Significant worry over $$$- major transition expected by administration for not much expense No faculty raises in past 5 years
Why did we work so hard n n n Mission driven 40% Residents did underserved practices on graduation We make a significant difference to the well being of our ethnically diverse community

Why did we work so hard n n n Special Programs would disappear if we closed High School clinics- 7000 visits/yr Home bound elderly visits- 600/yr Developmental 0 -3 screening and referral program Asthma education clinic Weekly Newborn education clinic(no charge)
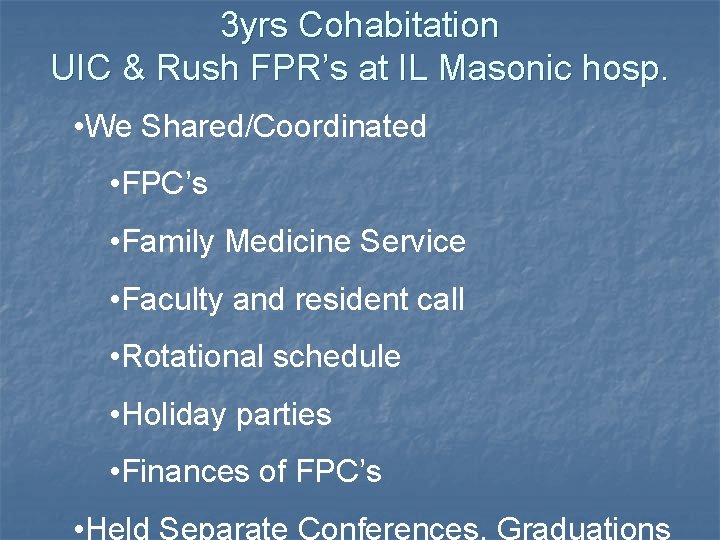
3 yrs Cohabitation UIC & Rush FPR’s at IL Masonic hosp. • We Shared/Coordinated • FPC’s • Family Medicine Service • Faculty and resident call • Rotational schedule • Holiday parties • Finances of FPC’s • Held Separate Conferences, Graduations
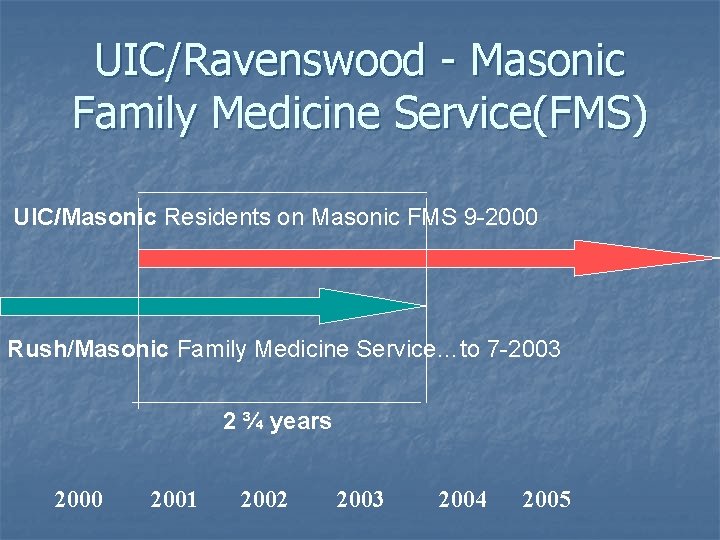
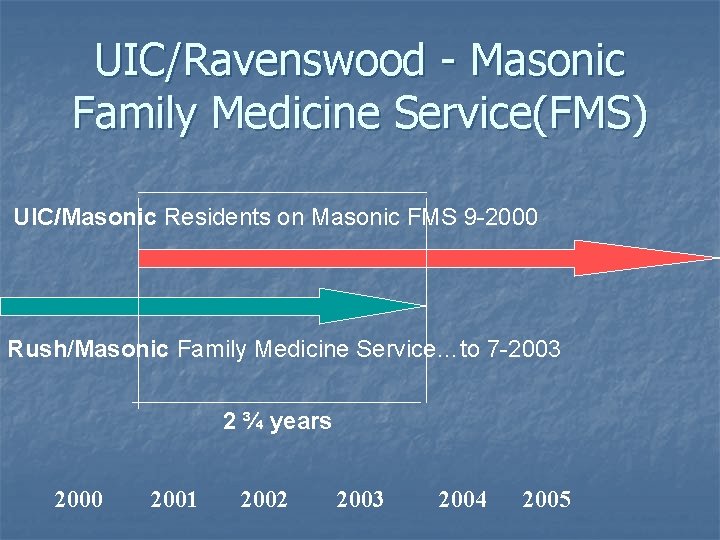
UIC/Ravenswood - Masonic Family Medicine Service(FMS) UIC/Masonic Residents on Masonic FMS 9 -2000 Rush/Masonic Family Medicine Service…to 7 -2003 2 ¾ years 2000 2001 2002 2003 2004 2005
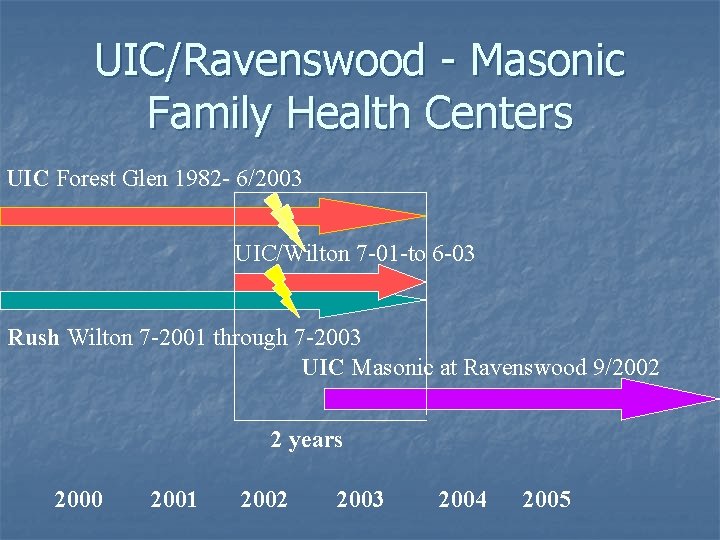
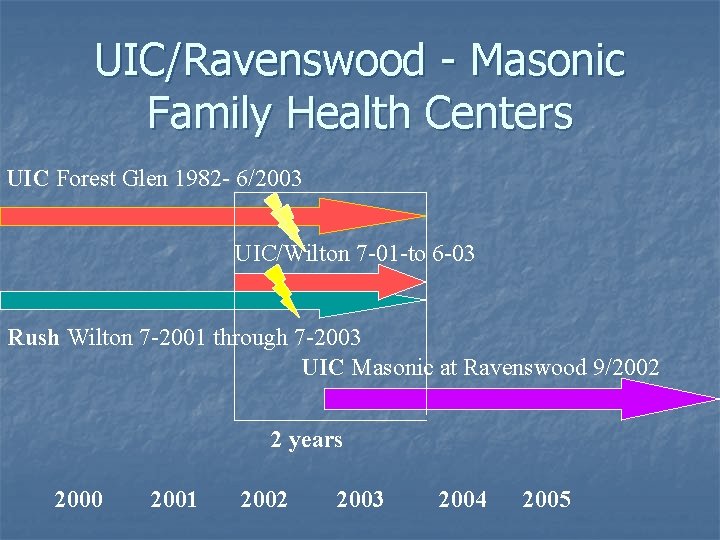
UIC/Ravenswood - Masonic Family Health Centers UIC Forest Glen 1982 - 6/2003 UIC/Wilton 7 -01 -to 6 -03 Rush Wilton 7 -2001 through 7 -2003 UIC Masonic at Ravenswood 9/2002 2 years 2000 2001 2002 2003 2004 2005

New FPC
Biggest Challenges n n n How to manage two residencies and three FPC’s in transition without losing too much money- Strong attention to bottom line was essential to maintain Hospital and Advocate support How to keep morale intact in this rapidly changing environment Recruiting new residents during transition
What we did n n n Attended to the bottom line Practice building- 23, 000 pts/yr Counted on residents, especially chiefs to help us coordinate through the difficult times Lots of talking, retreats, shared planning Everyone had a voice and a valued opinion as we transitioned. Made everyone feel as safe as possible
What we could have done better n n Thoroughly investigate planned end game Be clearer on what the Advocate system and Masonic Hospital wanted to accomplish so we could better understand how we might fit and be clear on what outcomes of the transition were nonnegotiable
Crystal Cash, M. D. n n Program Director Cook County. Loyola-Provident Family Practice Residency n n Program Merged in 2003 Today’s Theme: “Creating a New Culture”
Eugene Hong, M. D. n n Program Director Drexel University College of Medicine, Family Practice Residency n n Program in Transition Today’s Theme: “Challenges and Opportunities”
Conclusions n n n Communicate Develop a Proactive Strategy Lobby for Support
Conclusions n n n Be at the table If not on the radar screen, get on it Ask for help Gonzalez EH, Phillips RL, Pugno PA. “A Study of Closure of Family Practice Residency Programs”, Family Medicine, Nov-Dec 2003. Pugno PA, “What to Do When Faced With the Closure of a Family Practice Residency”, Family Medicine, March 2003.
Questions for Discussion… § § § What are subtle warning signs of impending change? What issues were the most challenging? (Cultural Shifts, Staff, Patients, Morale, Accreditation, Educational, etc. ) When, if ever, is closure the best option? Only option? What can one do to be proactive? What should one NOT do? What kind of communication with colleagues, staff, and patients is appropriate?
 And then there were none mystery elements
And then there were none mystery elements Literary analysis of and then there were none
Literary analysis of and then there were none And then there were none introduction
And then there were none introduction Characteristics of mystery flash fiction
Characteristics of mystery flash fiction Chapter 8 summary and then there were none
Chapter 8 summary and then there were none Halifax family medicine residency
Halifax family medicine residency Unfunded residency positions
Unfunded residency positions Meritus family medicine
Meritus family medicine Kaiser permanente san diego family medicine residency
Kaiser permanente san diego family medicine residency Uthscsa family medicine residency
Uthscsa family medicine residency Slu ent residents
Slu ent residents Margaret wiedmann md
Margaret wiedmann md Unm internal medicine residency
Unm internal medicine residency Umass memorial pharmacy residency
Umass memorial pharmacy residency Neysan pucks
Neysan pucks Brittany shrefler md
Brittany shrefler md Uihc internal medicine residents
Uihc internal medicine residents University of new mexico internal medicine residency
University of new mexico internal medicine residency I am god and there is none like me
I am god and there is none like me Ingilizce gramer zamanlar tablosu
Ingilizce gramer zamanlar tablosu Proof of parent-child relationship letter sample
Proof of parent-child relationship letter sample My jesus my savior
My jesus my savior Lord jesus my savior
Lord jesus my savior You are holy lord of heaven and earth
You are holy lord of heaven and earth Duke medicine grand rounds
Duke medicine grand rounds Five r's of note taking
Five r's of note taking Was/were supposed to
Was/were supposed to Types of family in community medicine
Types of family in community medicine Principles of family medicine
Principles of family medicine Family medicine fellowships
Family medicine fellowships Milestones family medicine
Milestones family medicine Board review family medicine
Board review family medicine Elements of primary health care
Elements of primary health care Wonca definition of family medicine
Wonca definition of family medicine Pediatrics shelf exam percentiles
Pediatrics shelf exam percentiles Ecomap in family medicine
Ecomap in family medicine Af williams family medicine center
Af williams family medicine center Family medicine in ethiopia
Family medicine in ethiopia Cabarrus family medicine concord
Cabarrus family medicine concord Screem family assessment questionnaire
Screem family assessment questionnaire Dr riaz qureshi
Dr riaz qureshi Isu family medicine
Isu family medicine Somatic dysfunction in osteopathic family medicine
Somatic dysfunction in osteopathic family medicine Family medicine meaning
Family medicine meaning