ENT 318 Artificial Organs Artificial kidney Lecturer Normahira
- Slides: 46
ENT 318 Artificial Organs Artificial kidney Lecturer: Normahira Mamat @ Mohamad Nor 1
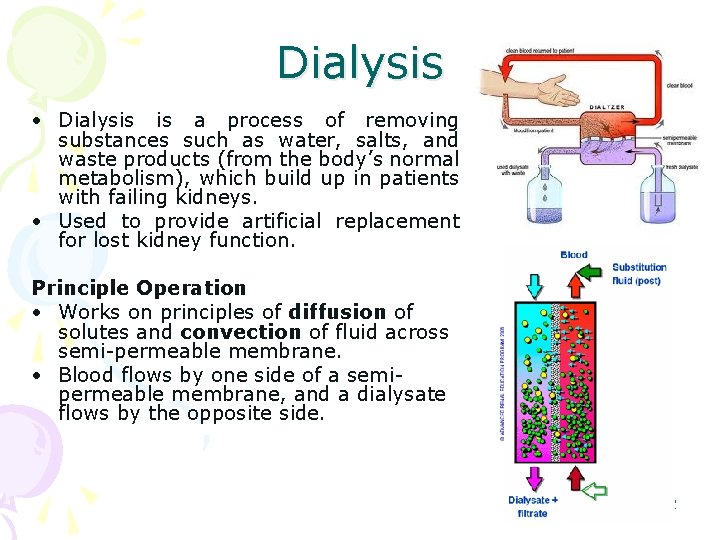
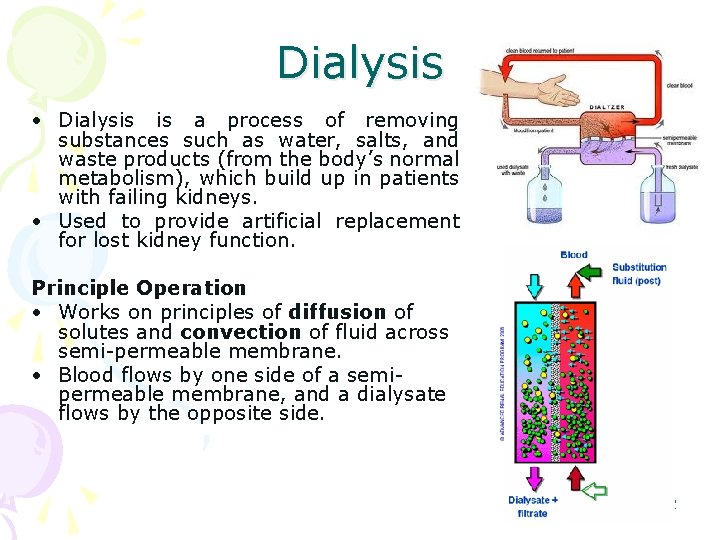
Dialysis • Dialysis is a process of removing substances such as water, salts, and waste products (from the body’s normal metabolism), which build up in patients with failing kidneys. • Used to provide artificial replacement for lost kidney function. Principle Operation • Works on principles of diffusion of solutes and convection of fluid across semi-permeable membrane. • Blood flows by one side of a semipermeable membrane, and a dialysate flows by the opposite side. 2
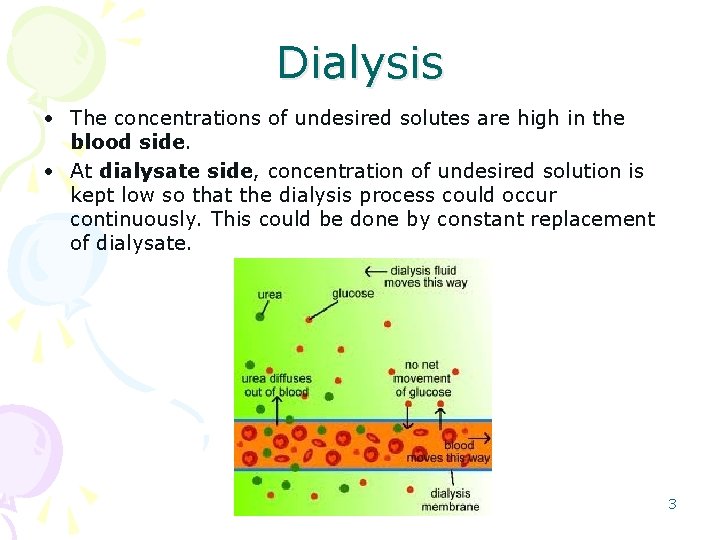
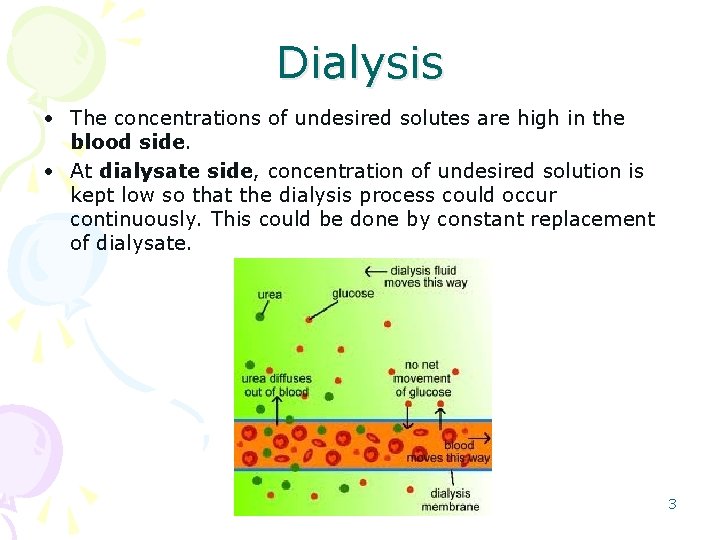
Dialysis • The concentrations of undesired solutes are high in the blood side. • At dialysate side, concentration of undesired solution is kept low so that the dialysis process could occur continuously. This could be done by constant replacement of dialysate. 3
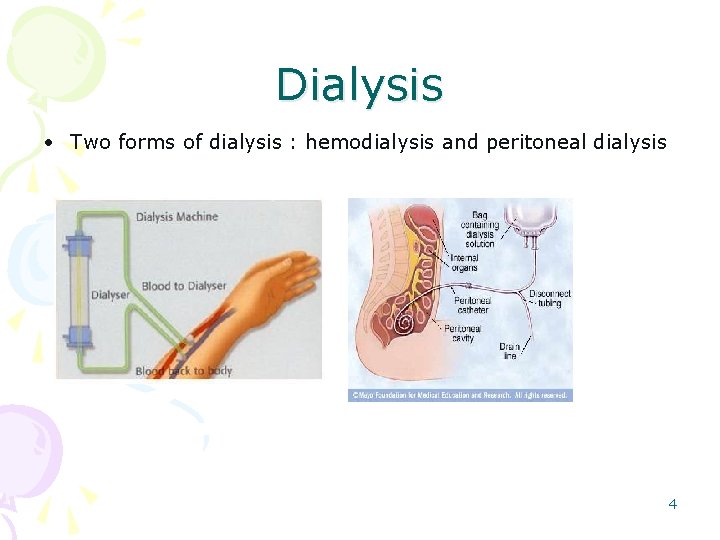
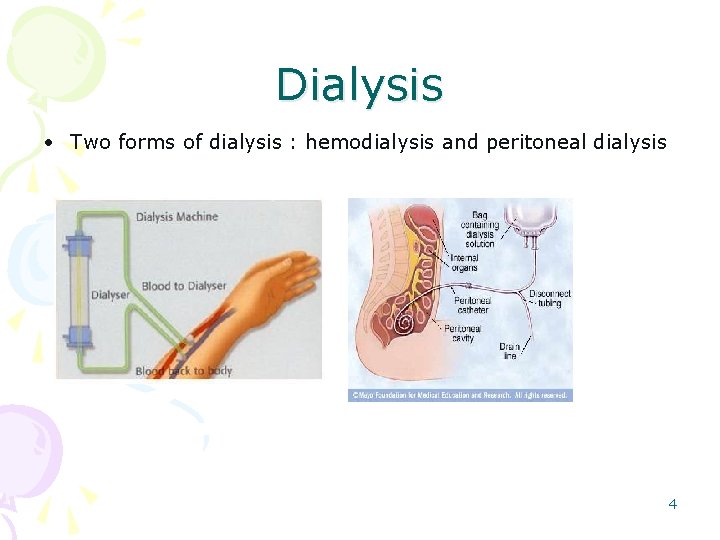
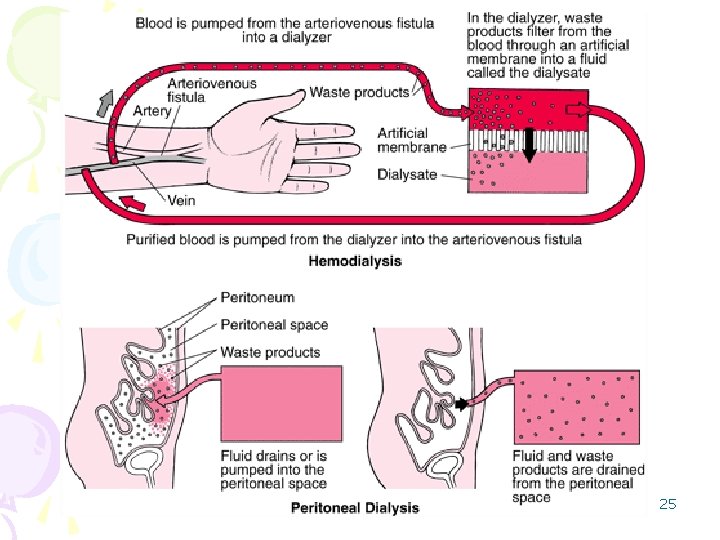
Dialysis • Two forms of dialysis : hemodialysis and peritoneal dialysis 4
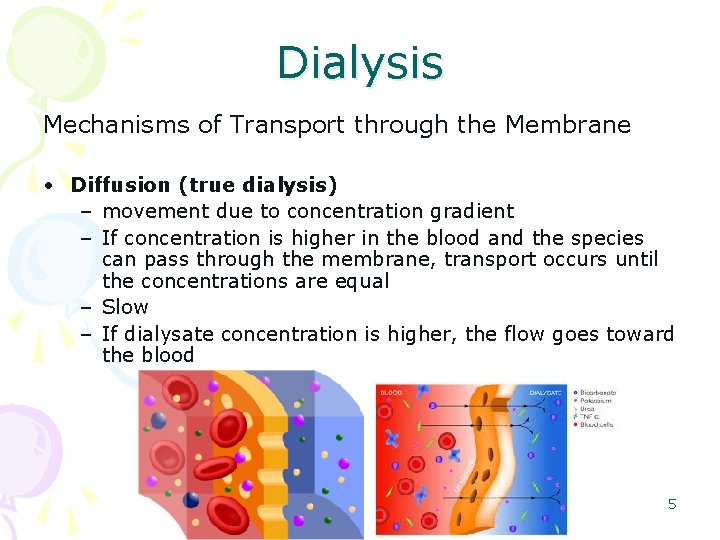
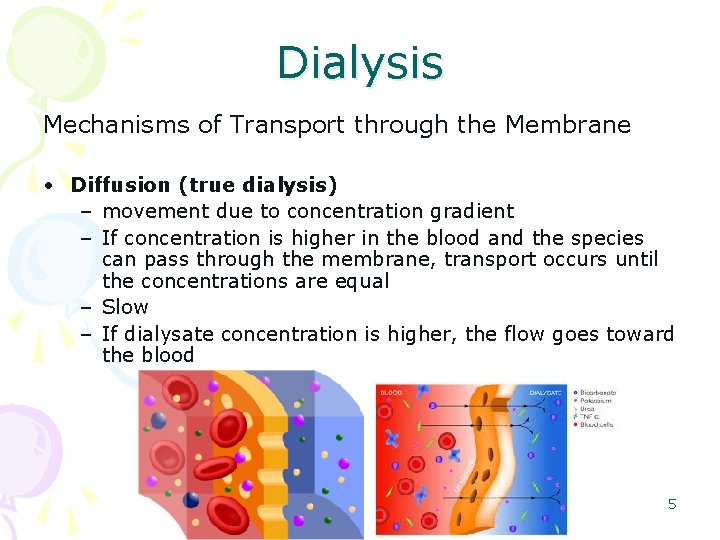
Dialysis Mechanisms of Transport through the Membrane • Diffusion (true dialysis) – movement due to concentration gradient – If concentration is higher in the blood and the species can pass through the membrane, transport occurs until the concentrations are equal – Slow – If dialysate concentration is higher, the flow goes toward the blood 5
Dialysis • Convection – Massive movement of fluid across membrane – Fluid carries dissolved or suspended species that can pass through the membrane – Usually as a result of fluid pressure (both positive and suction pressure) – Principal means of water and electrolyte removal (ultrafiltration) – Can also remove water by adding glucose to dialysate (osmotic gradient) 6
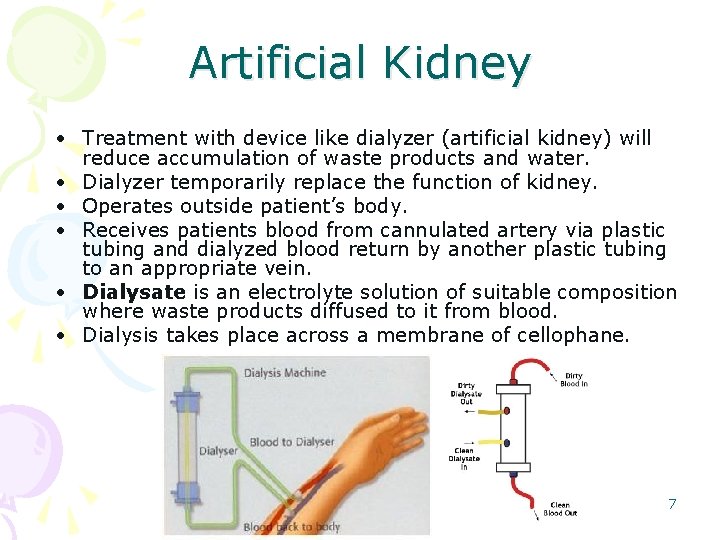
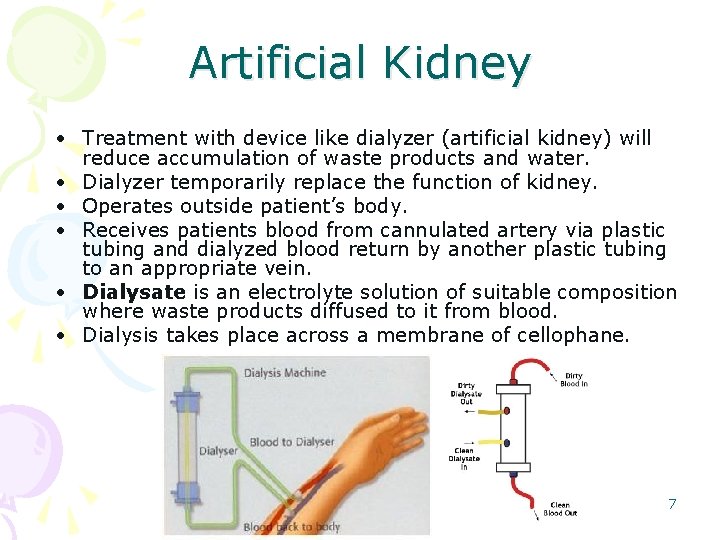
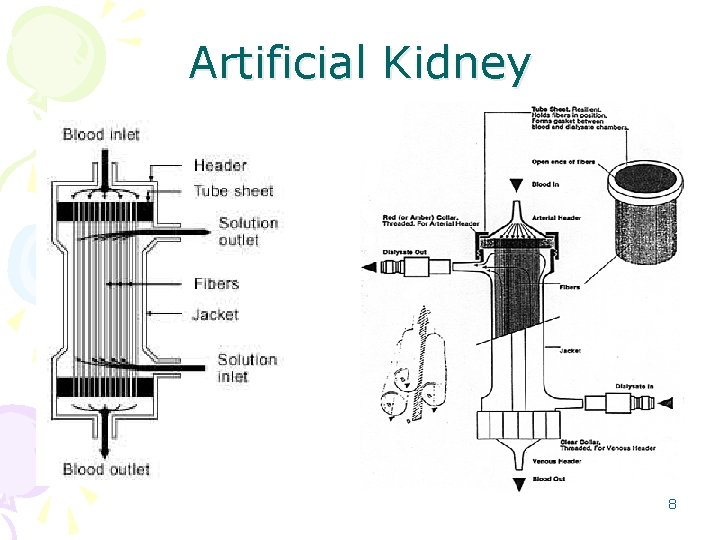
Artificial Kidney • Treatment with device like dialyzer (artificial kidney) will reduce accumulation of waste products and water. • Dialyzer temporarily replace the function of kidney. • Operates outside patient’s body. • Receives patients blood from cannulated artery via plastic tubing and dialyzed blood return by another plastic tubing to an appropriate vein. • Dialysate is an electrolyte solution of suitable composition where waste products diffused to it from blood. • Dialysis takes place across a membrane of cellophane. 7
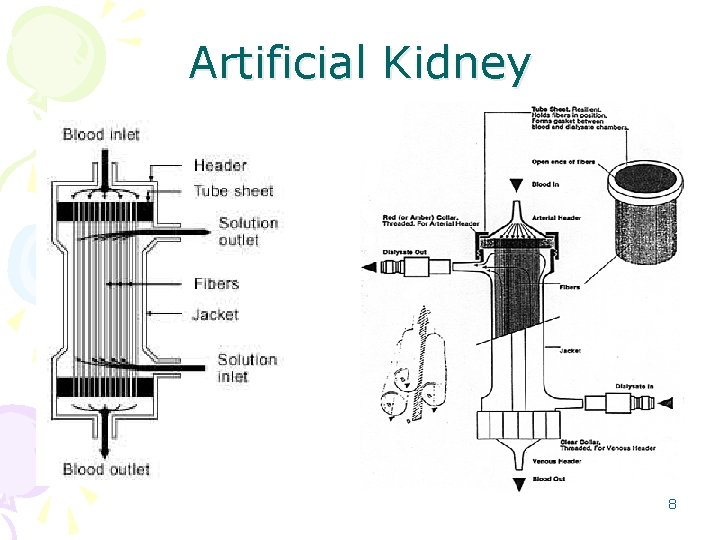
Artificial Kidney 8
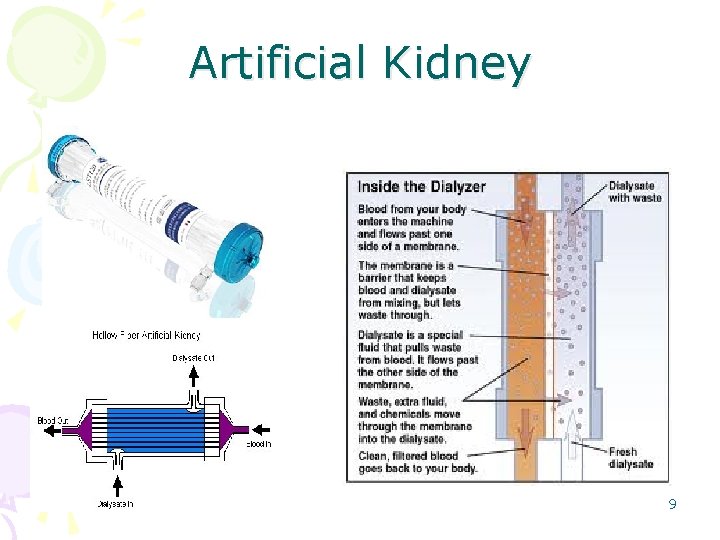
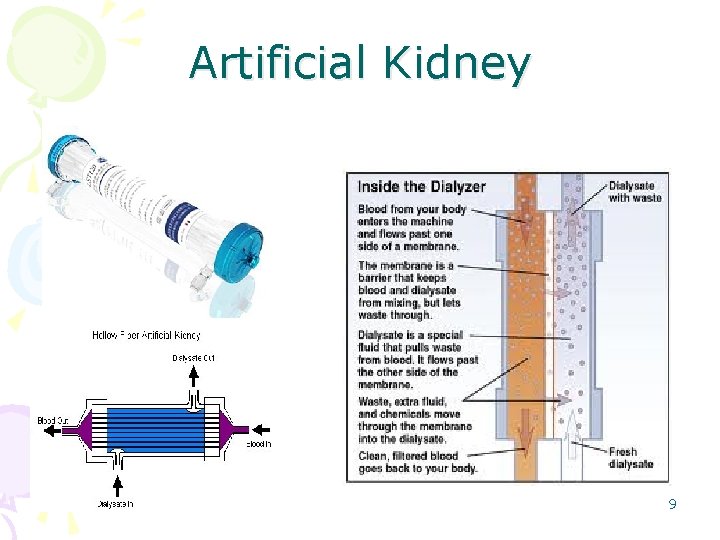
Artificial Kidney 9
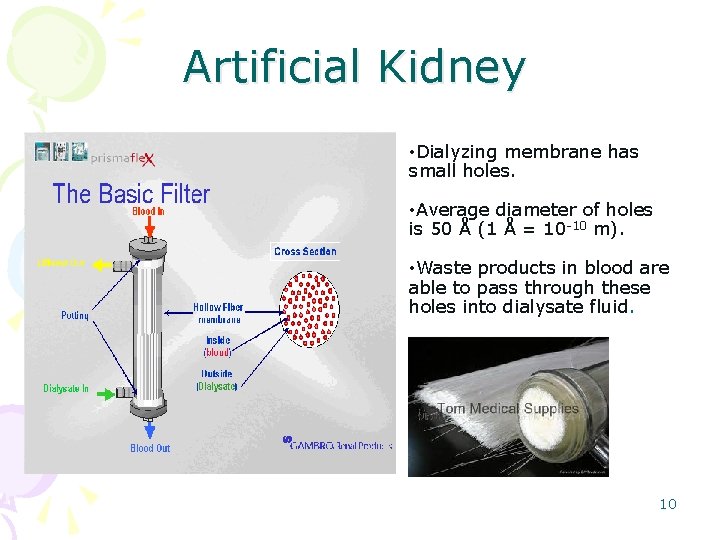
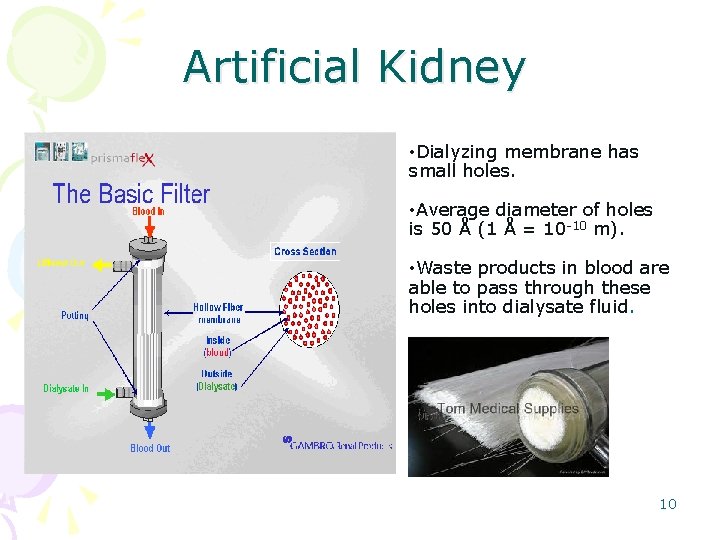
Artificial Kidney • Dialyzing membrane has small holes. • Average diameter of holes is 50 Å (1 Å = 10 -10 m). • Waste products in blood are able to pass through these holes into dialysate fluid. 10
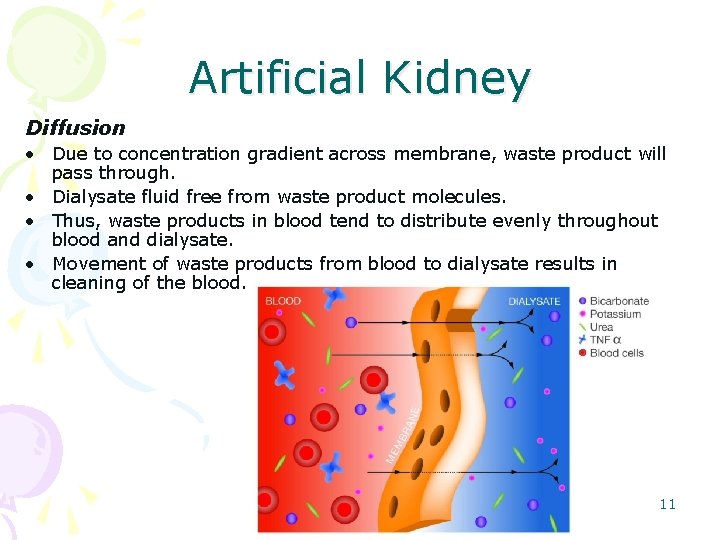
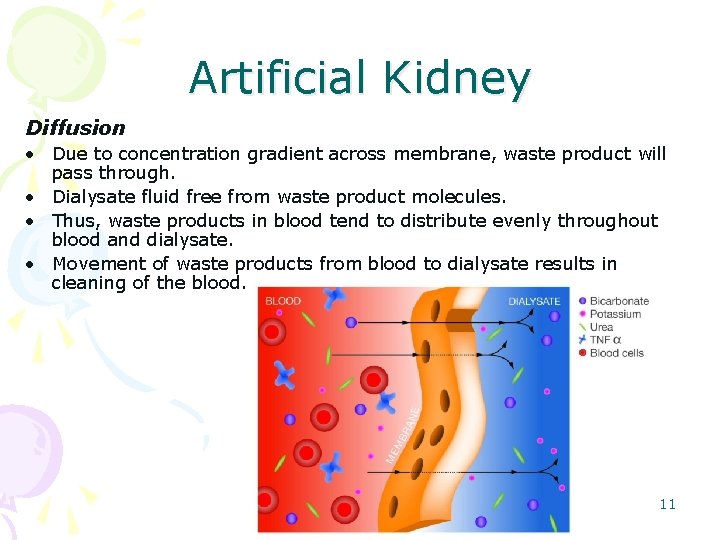
Artificial Kidney Diffusion • Due to concentration gradient across membrane, waste product will pass through. • Dialysate fluid free from waste product molecules. • Thus, waste products in blood tend to distribute evenly throughout blood and dialysate. • Movement of waste products from blood to dialysate results in cleaning of the blood. 11
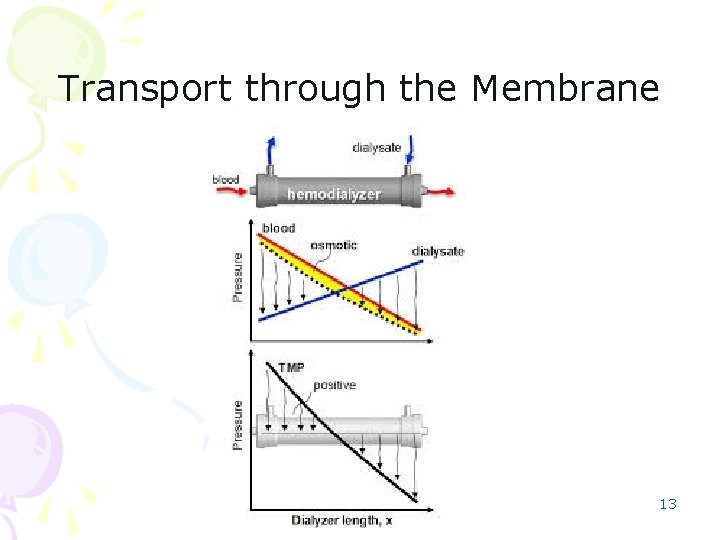
Artificial Kidney Convection • Volume of body fluid cannot be controlled by dialysis. • Ultra-filtration across membrane is employed. • Positive pressure applied to blood compartment. • Or negative pressure established in dialysate compartment. • Thus, fluid (water and electrolytes) will move from blood compartment to dialysate. • Degree of ultra-filtration depends on pressure difference across membrane and ultra-filtration characteristic of membrane. 12
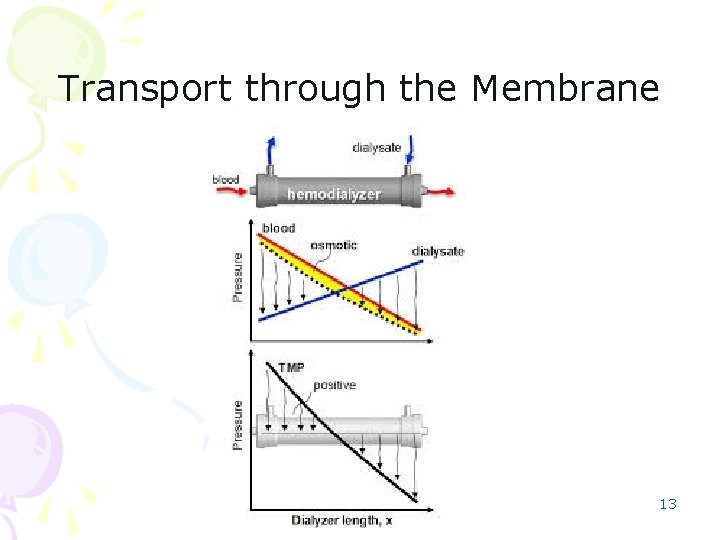
Transport through the Membrane 13
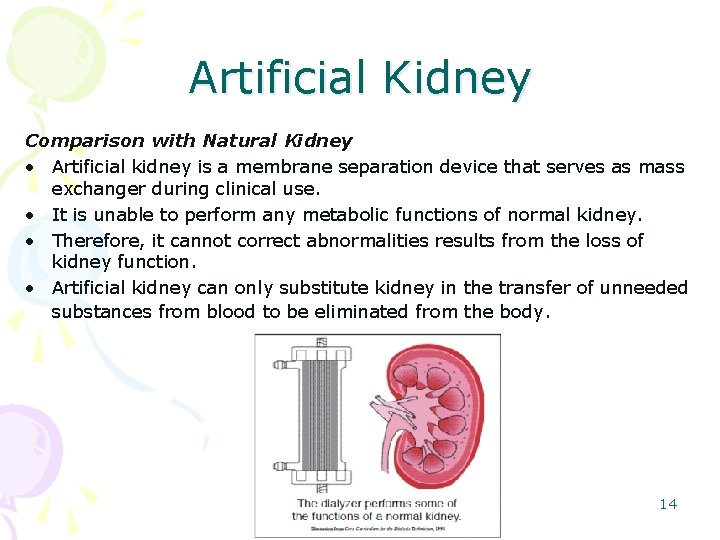
Artificial Kidney Comparison with Natural Kidney • Artificial kidney is a membrane separation device that serves as mass exchanger during clinical use. • It is unable to perform any metabolic functions of normal kidney. • Therefore, it cannot correct abnormalities results from the loss of kidney function. • Artificial kidney can only substitute kidney in the transfer of unneeded substances from blood to be eliminated from the body. 14
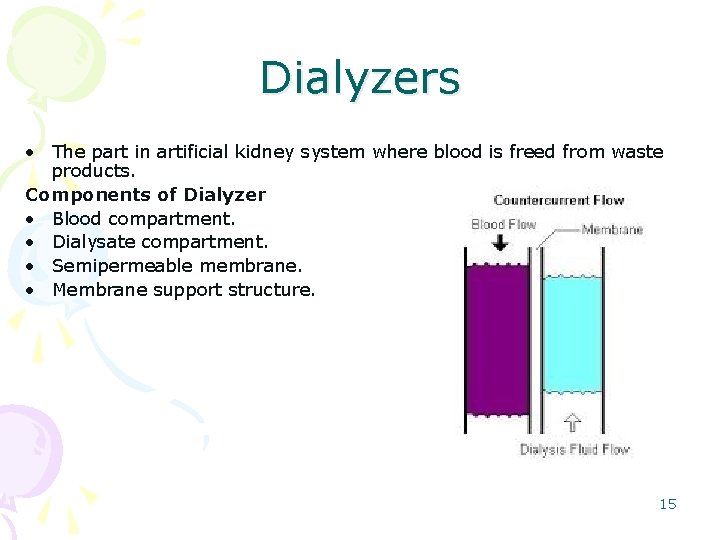
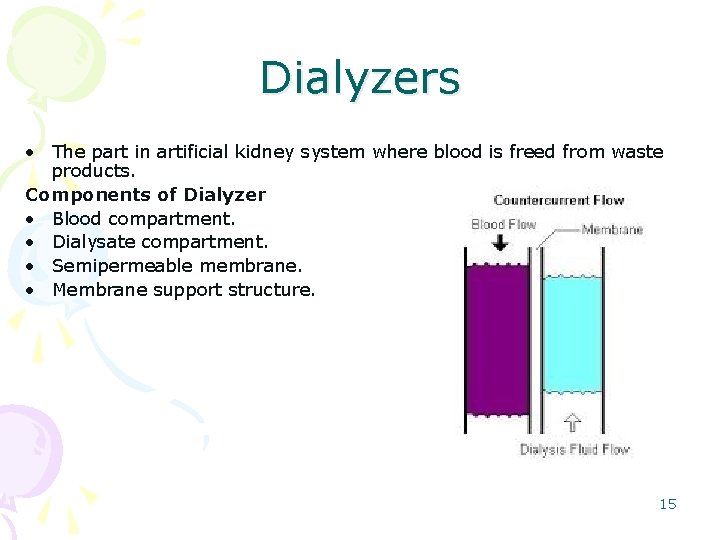
Dialyzers • The part in artificial kidney system where blood is freed from waste products. Components of Dialyzer • Blood compartment. • Dialysate compartment. • Semipermeable membrane. • Membrane support structure. 15
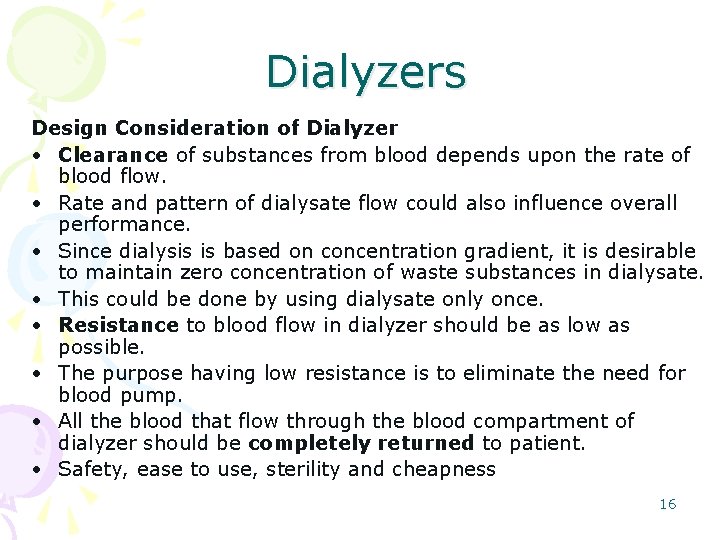
Dialyzers Design Consideration of Dialyzer • Clearance of substances from blood depends upon the rate of blood flow. • Rate and pattern of dialysate flow could also influence overall performance. • Since dialysis is based on concentration gradient, it is desirable to maintain zero concentration of waste substances in dialysate. • This could be done by using dialysate only once. • Resistance to blood flow in dialyzer should be as low as possible. • The purpose having low resistance is to eliminate the need for blood pump. • All the blood that flow through the blood compartment of dialyzer should be completely returned to patient. • Safety, ease to use, sterility and cheapness 16
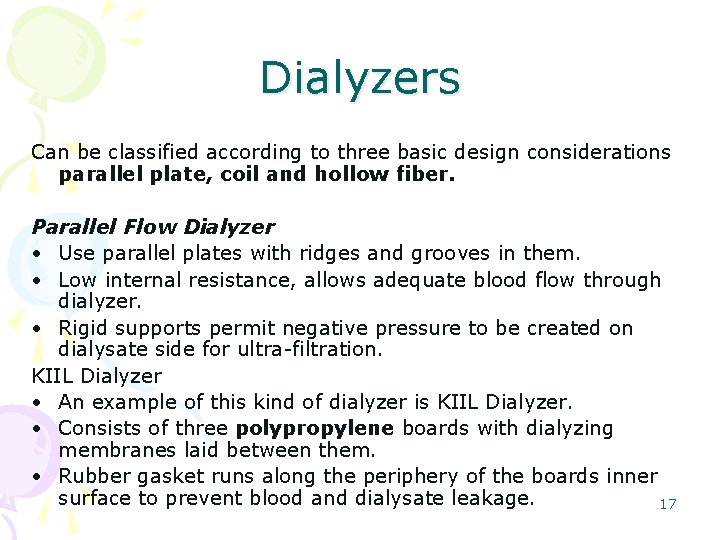
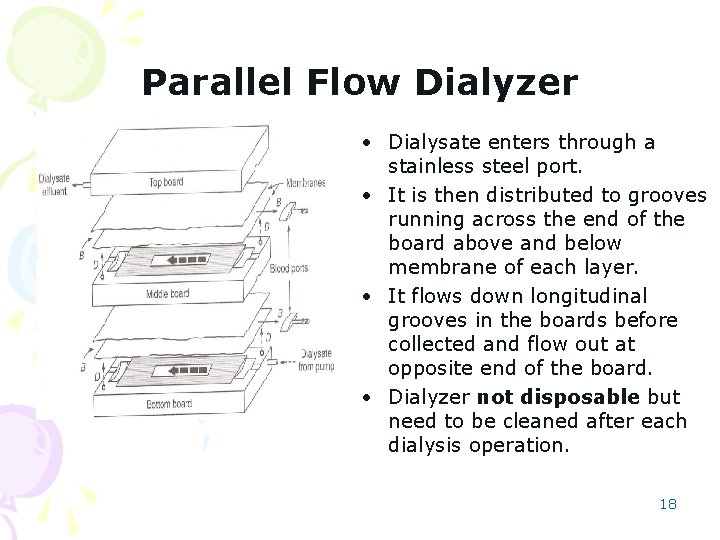
Dialyzers Can be classified according to three basic design considerations parallel plate, coil and hollow fiber. Parallel Flow Dialyzer • Use parallel plates with ridges and grooves in them. • Low internal resistance, allows adequate blood flow through dialyzer. • Rigid supports permit negative pressure to be created on dialysate side for ultra-filtration. KIIL Dialyzer • An example of this kind of dialyzer is KIIL Dialyzer. • Consists of three polypropylene boards with dialyzing membranes laid between them. • Rubber gasket runs along the periphery of the boards inner surface to prevent blood and dialysate leakage. 17
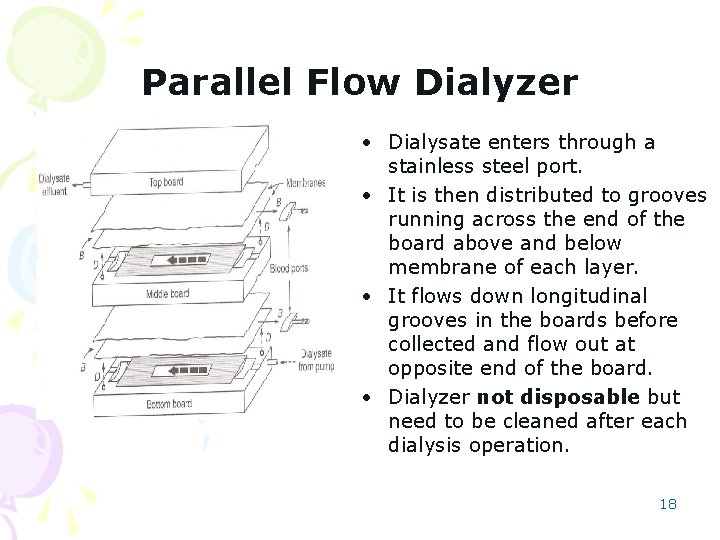
Parallel Flow Dialyzer • Dialysate enters through a stainless steel port. • It is then distributed to grooves running across the end of the board above and below membrane of each layer. • It flows down longitudinal grooves in the boards before collected and flow out at opposite end of the board. • Dialyzer not disposable but need to be cleaned after each dialysis operation. 18
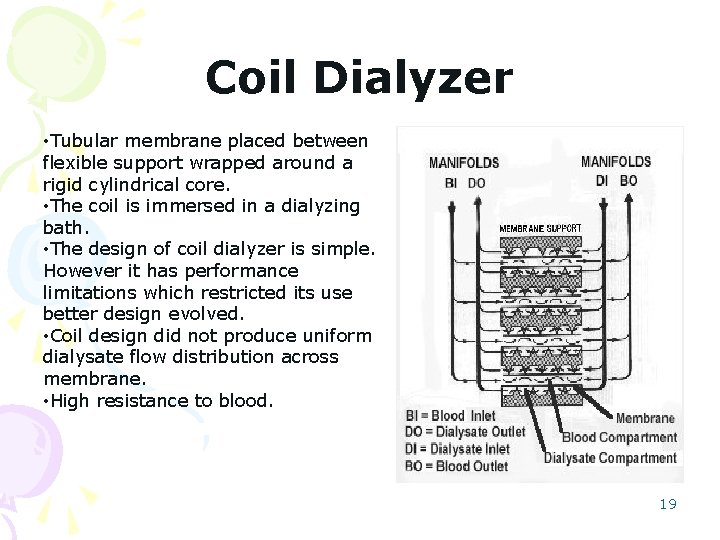
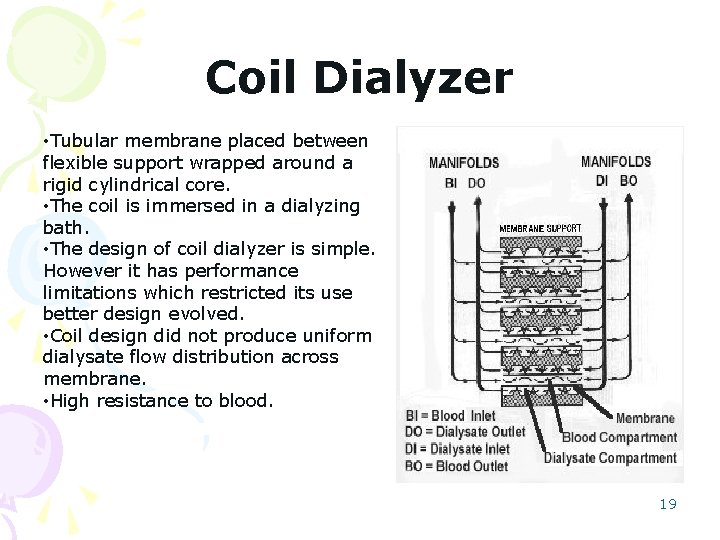
Coil Dialyzer • Tubular membrane placed between flexible support wrapped around a rigid cylindrical core. • The coil is immersed in a dialyzing bath. • The design of coil dialyzer is simple. However it has performance limitations which restricted its use better design evolved. • Coil design did not produce uniform dialysate flow distribution across membrane. • High resistance to blood. 19
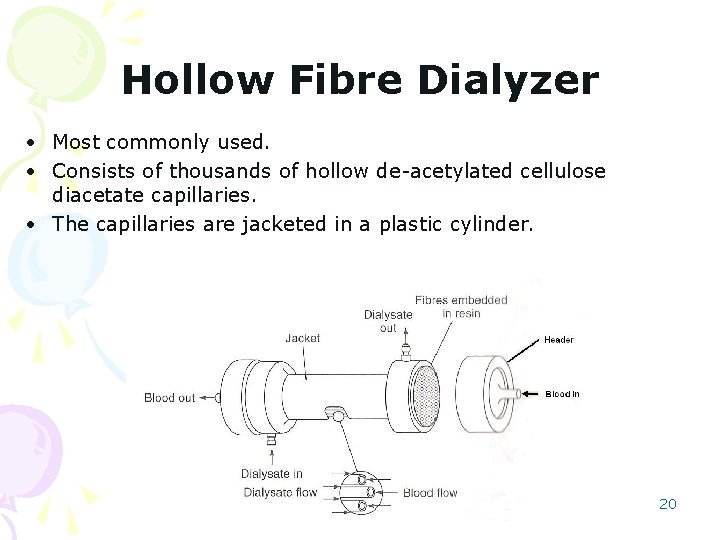
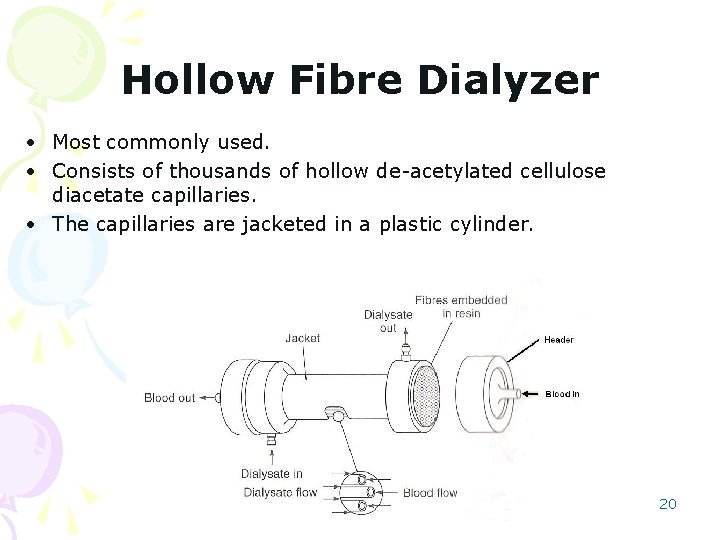
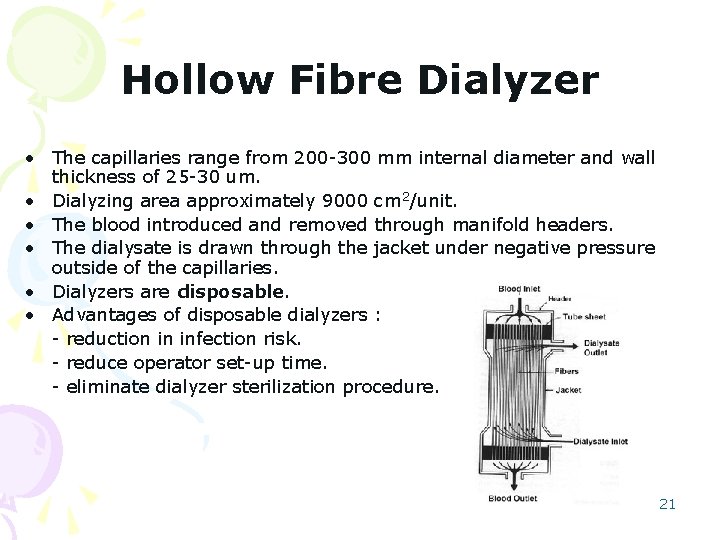
Hollow Fibre Dialyzer • Most commonly used. • Consists of thousands of hollow de-acetylated cellulose diacetate capillaries. • The capillaries are jacketed in a plastic cylinder. 20
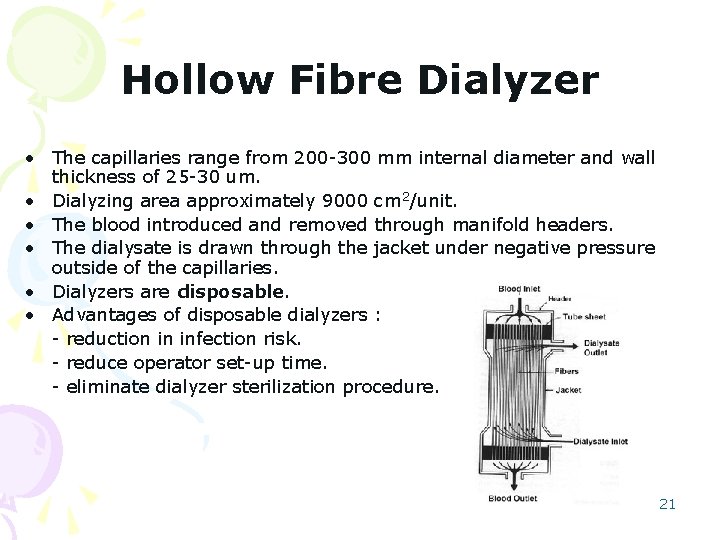
Hollow Fibre Dialyzer • The capillaries range from 200 -300 mm internal diameter and wall thickness of 25 -30 um. • Dialyzing area approximately 9000 cm 2/unit. • The blood introduced and removed through manifold headers. • The dialysate is drawn through the jacket under negative pressure outside of the capillaries. • Dialyzers are disposable. • Advantages of disposable dialyzers : - reduction in infection risk. - reduce operator set-up time. - eliminate dialyzer sterilization procedure. 21
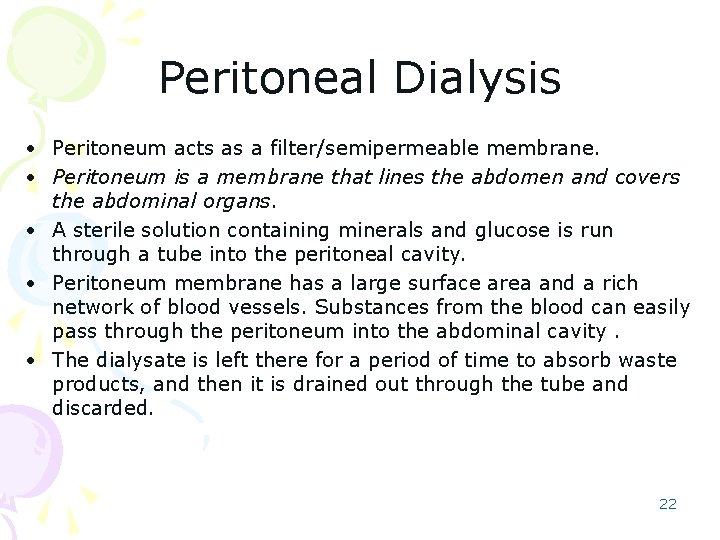
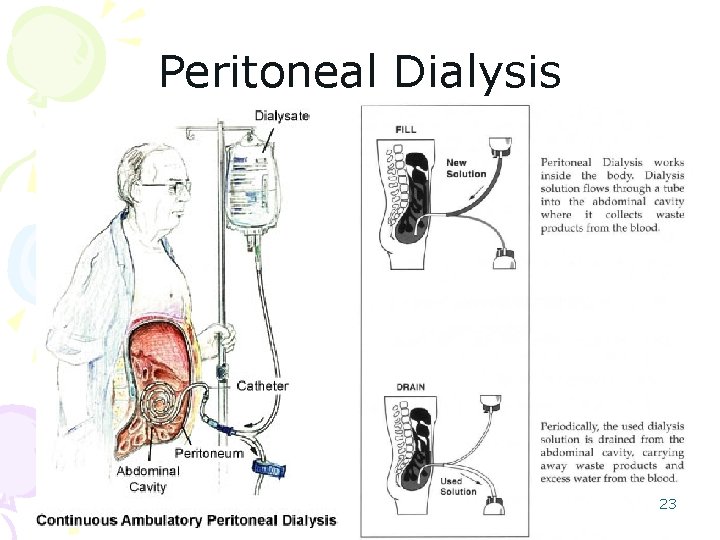
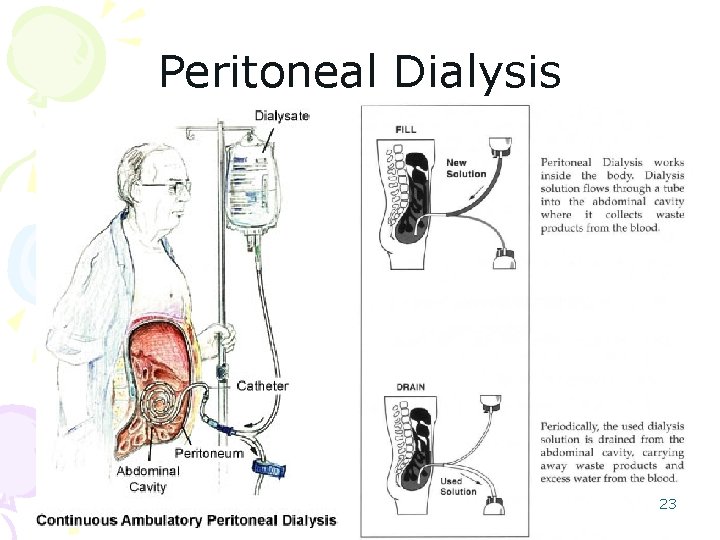
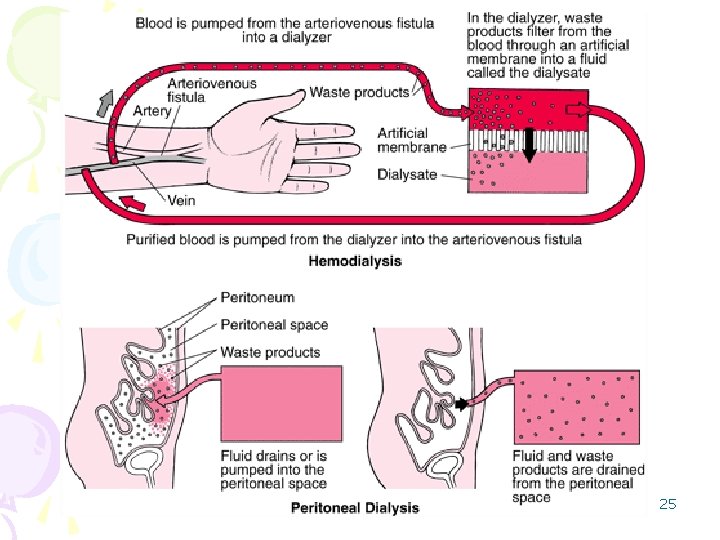
Peritoneal Dialysis • Peritoneum acts as a filter/semipermeable membrane. • Peritoneum is a membrane that lines the abdomen and covers the abdominal organs. • A sterile solution containing minerals and glucose is run through a tube into the peritoneal cavity. • Peritoneum membrane has a large surface area and a rich network of blood vessels. Substances from the blood can easily pass through the peritoneum into the abdominal cavity. • The dialysate is left there for a period of time to absorb waste products, and then it is drained out through the tube and discarded. 22
Peritoneal Dialysis 23
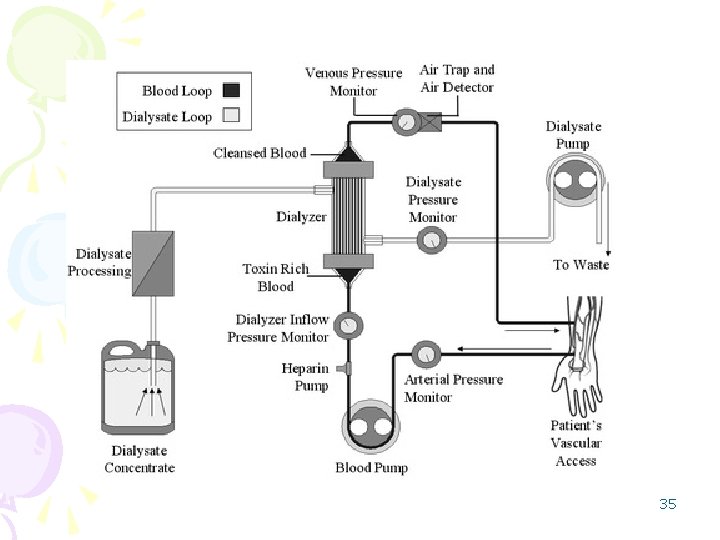
Hemodialysis • Blood is removed from the body and pumped by a machine outside the body into a dialyzer. • Dialyzer filters metabolic waste products from the blood and then returns the purified blood to the person. • Ultrafiltration occurs by increasing the hydrostatic pressure across the dialyzer membrane, usually done by applying a negative pressure to the dialysate compartment of the dialyzer. • Can be an outpatient or inpatient therapy conducted in dialysis centre or hospitals and clinics which have the facilities. • Patients must undergo strict schedule of treatment usually three times a week for 3 to 5 or more hours each visit. 24
25
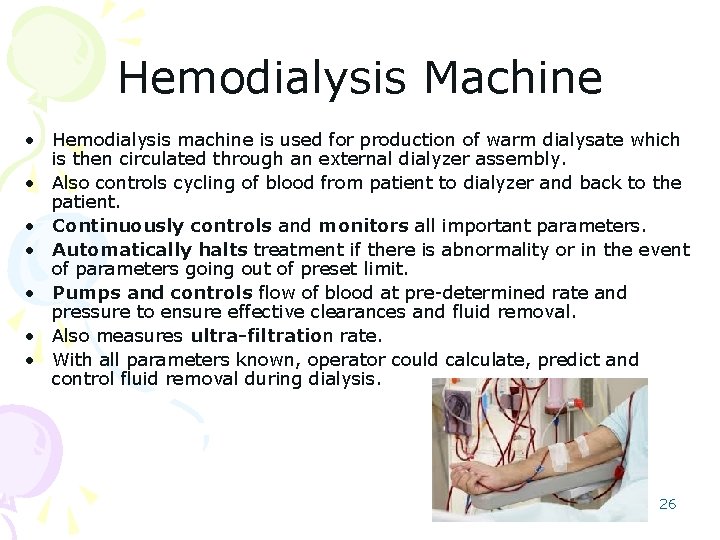
Hemodialysis Machine • Hemodialysis machine is used for production of warm dialysate which is then circulated through an external dialyzer assembly. • Also controls cycling of blood from patient to dialyzer and back to the patient. • Continuously controls and monitors all important parameters. • Automatically halts treatment if there is abnormality or in the event of parameters going out of preset limit. • Pumps and controls flow of blood at pre-determined rate and pressure to ensure effective clearances and fluid removal. • Also measures ultra-filtration rate. • With all parameters known, operator could calculate, predict and control fluid removal during dialysis. 26
Hemodialysis • Yayasan Buah Pinggang Kebangsaan Malaysia – involve in providing facilities for kidney treatment and education for people. (www. nkf. org. my) • Pusat Dialisis Tuanku Syed Putra (NKF) Yayasan Amal Tuanku Hajah Budriah Perlis, Lorong Hilary, Taman Bukit Kaya, Jalan Bukit Lagi, Kangar, 01000 Perlis. 04 -9777411 27
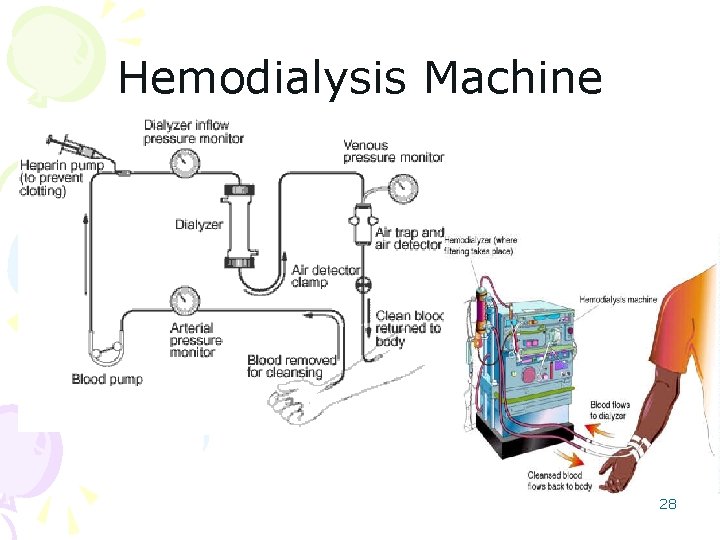
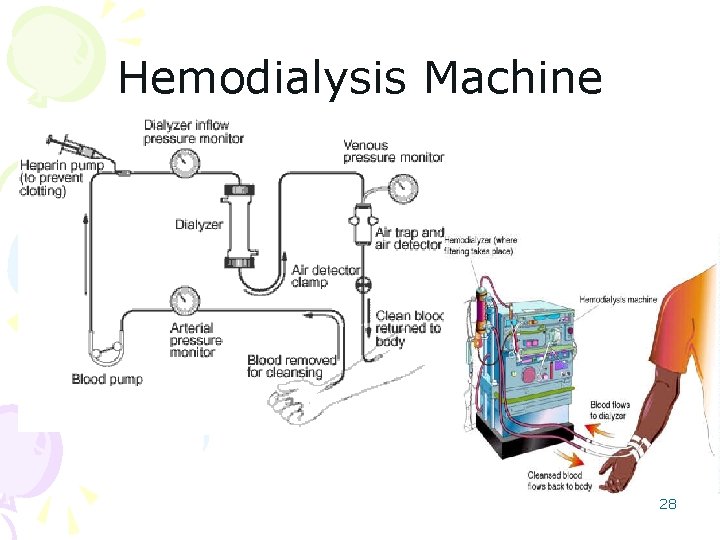
Hemodialysis Machine 28
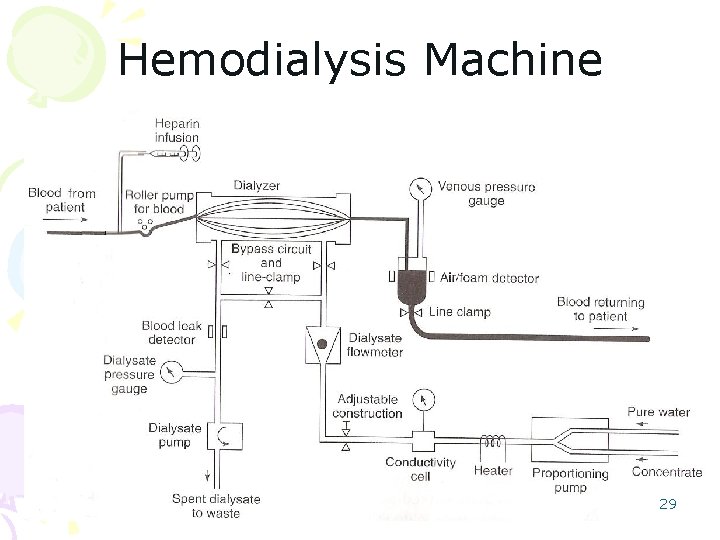
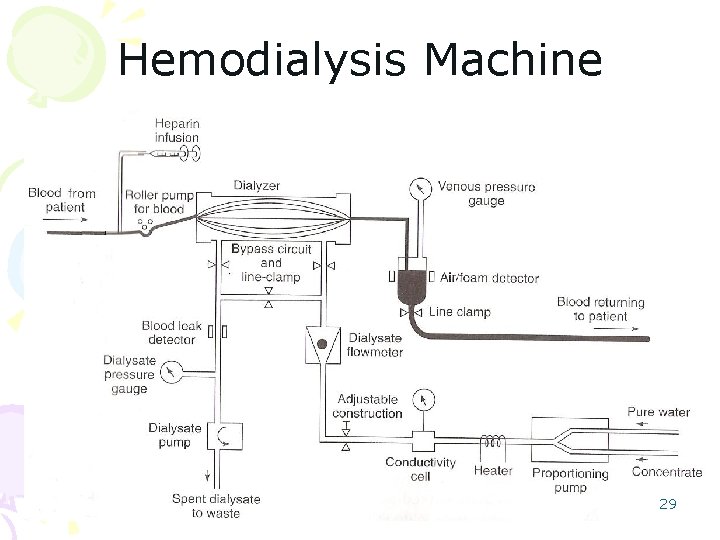
Hemodialysis Machine 29
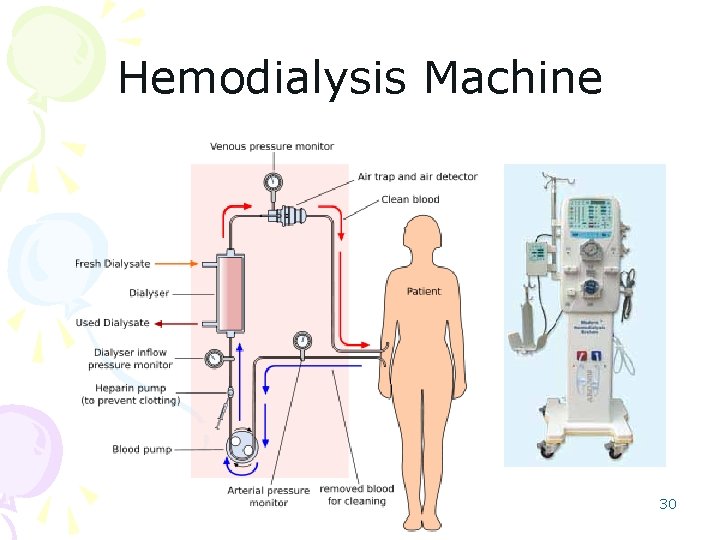
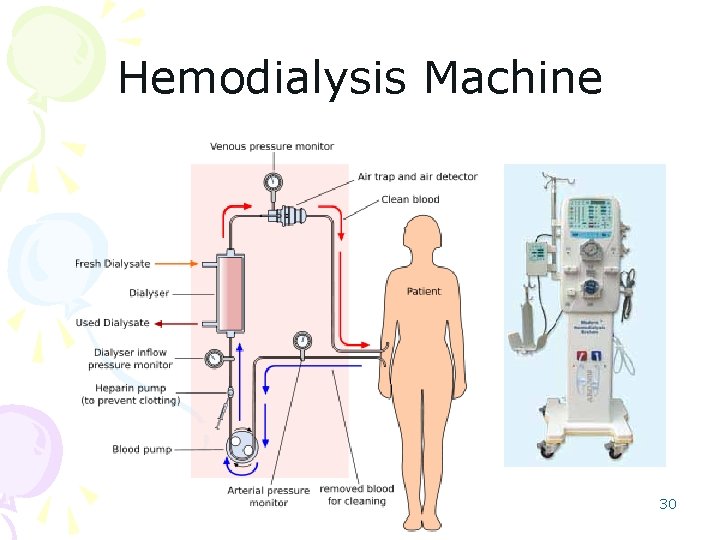
Hemodialysis Machine 30
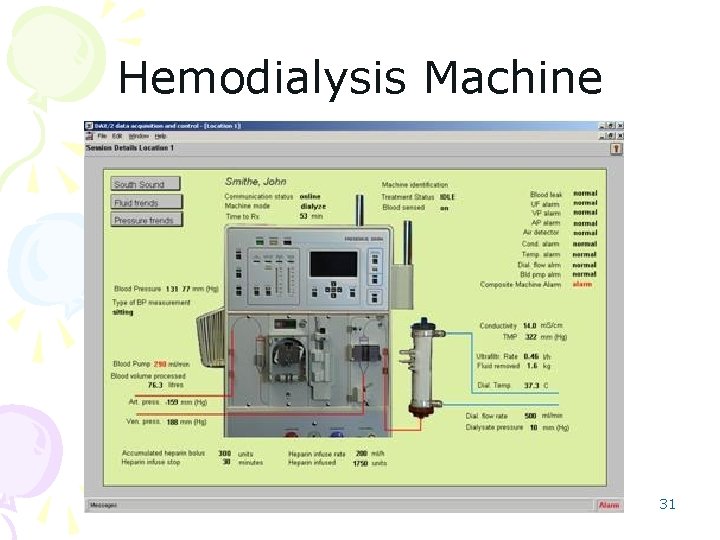
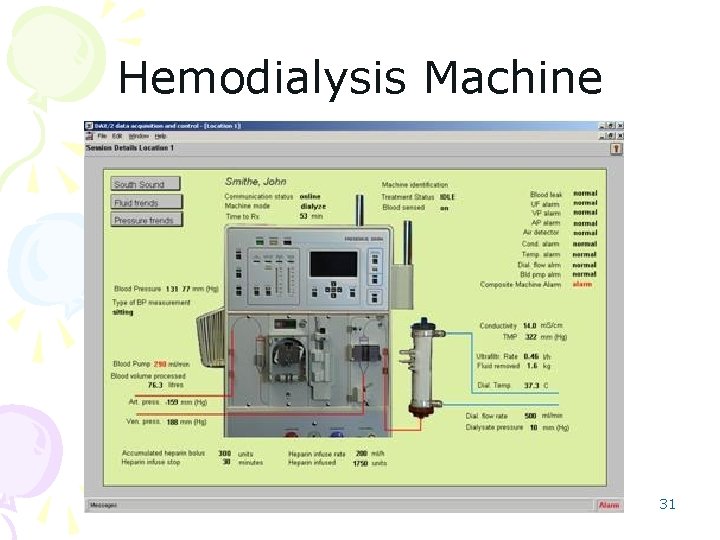
Hemodialysis Machine 31
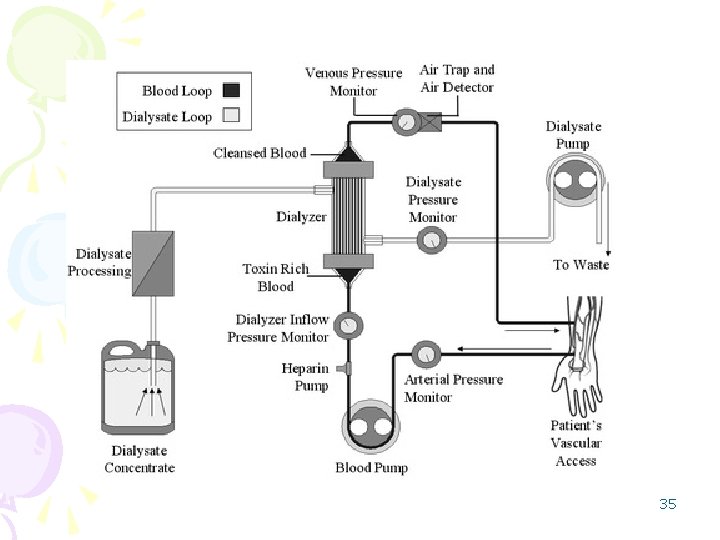
Hemodialysis Machine • Basic Functions of Hemodialysis Machine - Mixes the dialysate. - Monitors the dialysate. - Pump the blood and controls administration of anti-coagulants. - Monitors blood for presence of air. - Monitors ultra-filtration rate. Dialysate Temperature Control and Measurement • Dialysis normally done at body temperature. • Lower than body temperature, dialysis is less efficient and blood has to be warmed before return to patient. • High temperature (>40 o. C) will damage components of blood. • Thus, temperature of dialysate is monitored and controlled before supplied to dialyzer. 32
Hemodialysis Machine • Temperature control system used to raise temperature of dialysate to a required value. • If temperature exceeds, safety cut-out will ensure heater switched off. • Required temperature varied from 36 to 42 o. C. • Two types of circuit for control of temperature : - Bi-metallic thermostat. - Electronic proportional controller. • The latter use thermistor for sensing temperature and triac for control of power to heater. 33
Hemodialysis Machine Dialysate Pressure Control and Measurement • Negative pressure upon dialysate created by effluent pump. • Effluent pump is a fixed-flow, motor-driven gear pump. • Pressure between zero and maximum by adjustment on machine panel. • A relief valve limits maximum negative pressure and minimizing risk of burst in dialyzer membrane. • Pressure adjustment should not produce any significant change in flow rate. • Pressure measured by strain gauge transducer. • Dialysate pressure is measured on one side of membrane and venous pressure on the other side. • Effective pressure across membrane is algebraic sum of dialysate pressure and venous pressure. • This effective pressure important in consideration of filtration and weight control. • If pressure goes beyond limit, effluent pump switched off. • Dialysate by-passed to drain by way of header tank overflow and waste funnel 34
35
Hemodialysis Machine Venous Pressure Measurement • Measured at bubble trap. • A tubing connects the trap to a strain gauge transducer. • If pressure beyond limit, power to blood pump will be isolated and pump will not be used. Bubble trap • Air embolism is serious hazard in dialysis. • Air may be sucked in due to inadequate flow in the line in the pumped dialysis system. • Bubble trap is equipped to diminish air embolism. 36
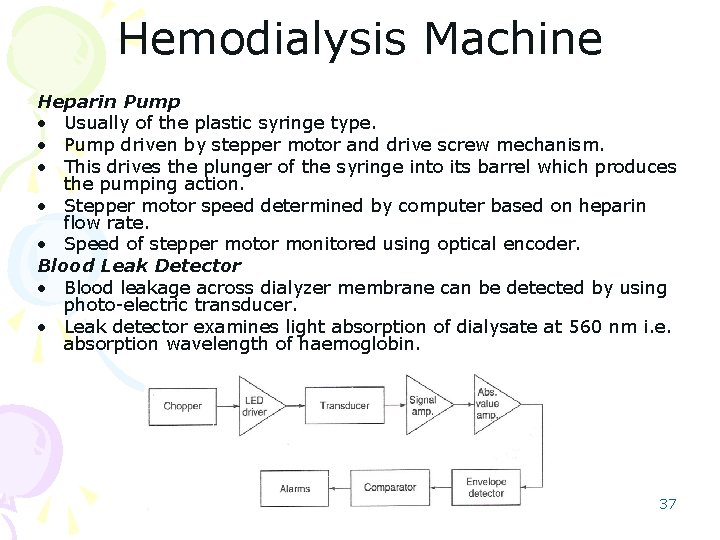
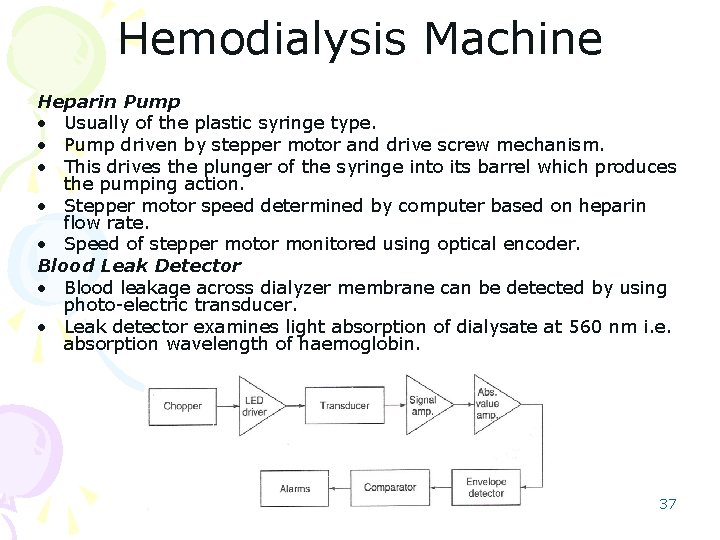
Hemodialysis Machine Heparin Pump • Usually of the plastic syringe type. • Pump driven by stepper motor and drive screw mechanism. • This drives the plunger of the syringe into its barrel which produces the pumping action. • Stepper motor speed determined by computer based on heparin flow rate. • Speed of stepper motor monitored using optical encoder. Blood Leak Detector • Blood leakage across dialyzer membrane can be detected by using photo-electric transducer. • Leak detector examines light absorption of dialysate at 560 nm i. e. absorption wavelength of haemoglobin. 37
Hemodialysis Machine • A chopped light system with AC amplifiers is employed. • Chopping achieved by driving LED with square wave of current. • Compensation thermistor placed in another arm of the bridge. • The light is detected with cadmium sulphide photo-conductive cell. • Absolute value circuit provides signal whose peak value is proportional to the received 560 nm light. • The peak value is compared to a reference voltage which is pre-set. • Maximum setting detects blood leaks at rate of 65 mg/l of dialysate. • If blood leak is detected, the effluent pump switched off automatically. 38
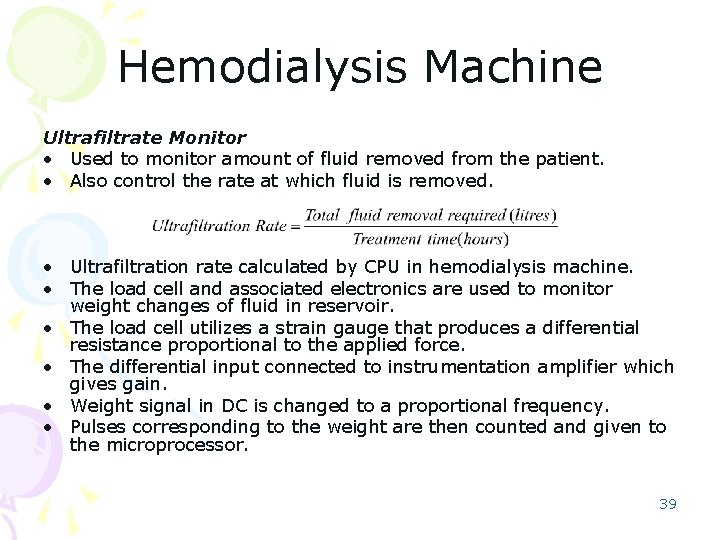
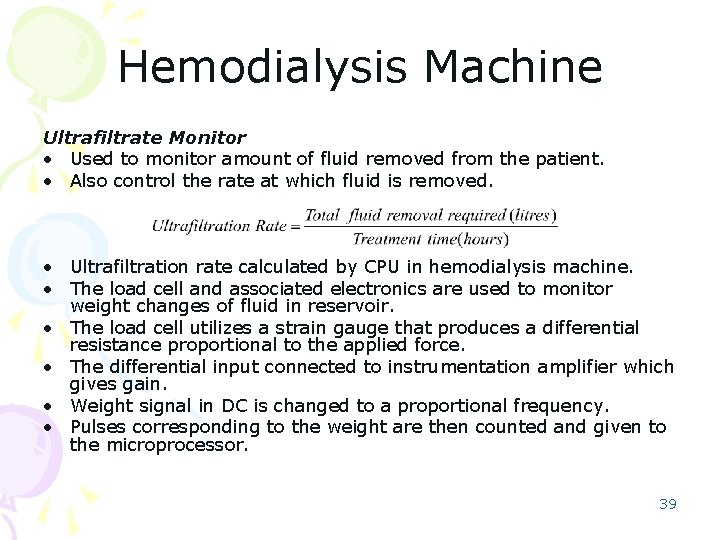
Hemodialysis Machine Ultrafiltrate Monitor • Used to monitor amount of fluid removed from the patient. • Also control the rate at which fluid is removed. • Ultrafiltration rate calculated by CPU in hemodialysis machine. • The load cell and associated electronics are used to monitor weight changes of fluid in reservoir. • The load cell utilizes a strain gauge that produces a differential resistance proportional to the applied force. • The differential input connected to instrumentation amplifier which gives gain. • Weight signal in DC is changed to a proportional frequency. • Pulses corresponding to the weight are then counted and given to the microprocessor. 39
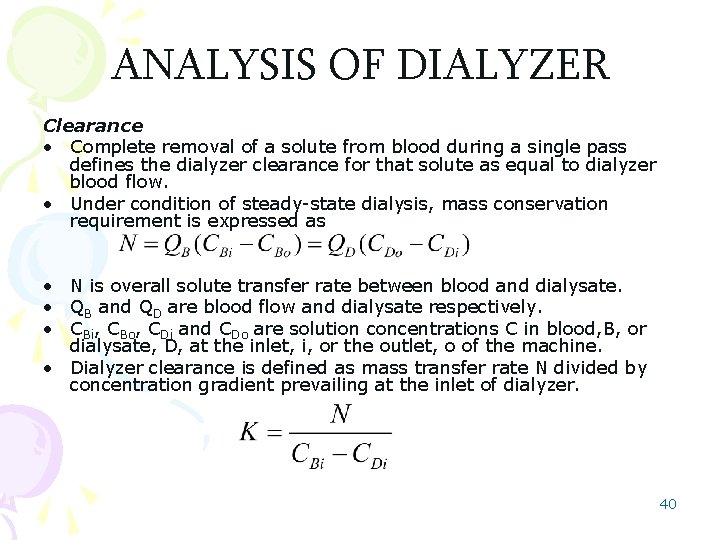
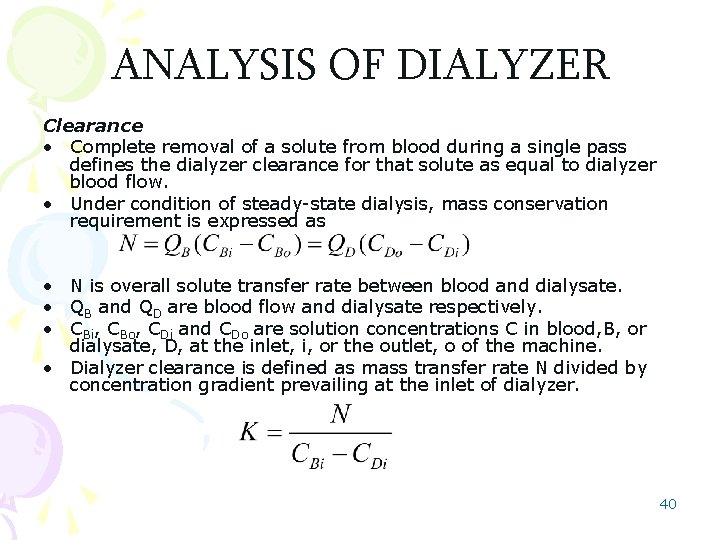
ANALYSIS OF DIALYZER Clearance • Complete removal of a solute from blood during a single pass defines the dialyzer clearance for that solute as equal to dialyzer blood flow. • Under condition of steady-state dialysis, mass conservation requirement is expressed as • N is overall solute transfer rate between blood and dialysate. • QB and QD are blood flow and dialysate respectively. • CBi, CBo, CDi and CDo are solution concentrations C in blood, B, or dialysate, D, at the inlet, i, or the outlet, o of the machine. • Dialyzer clearance is defined as mass transfer rate N divided by concentration gradient prevailing at the inlet of dialyzer. 40
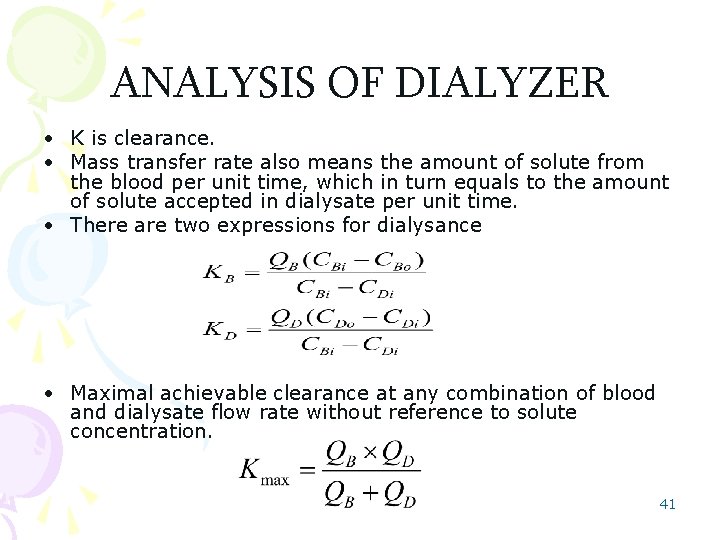
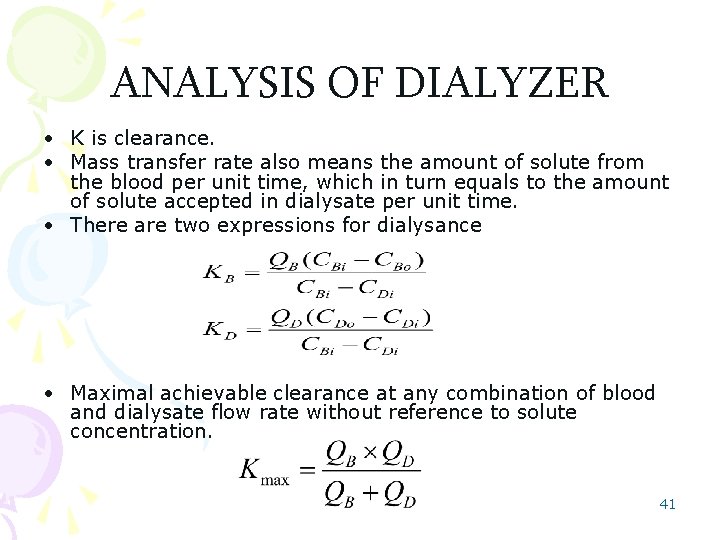
ANALYSIS OF DIALYZER • K is clearance. • Mass transfer rate also means the amount of solute from the blood per unit time, which in turn equals to the amount of solute accepted in dialysate per unit time. • There are two expressions for dialysance • Maximal achievable clearance at any combination of blood and dialysate flow rate without reference to solute concentration. 41
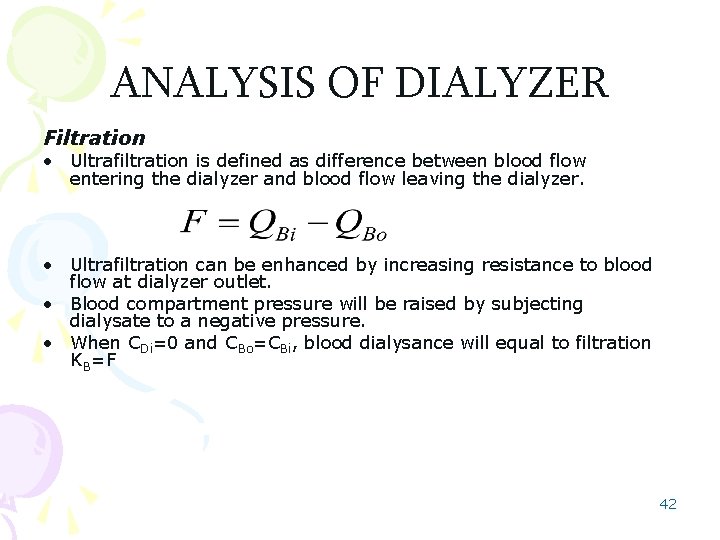
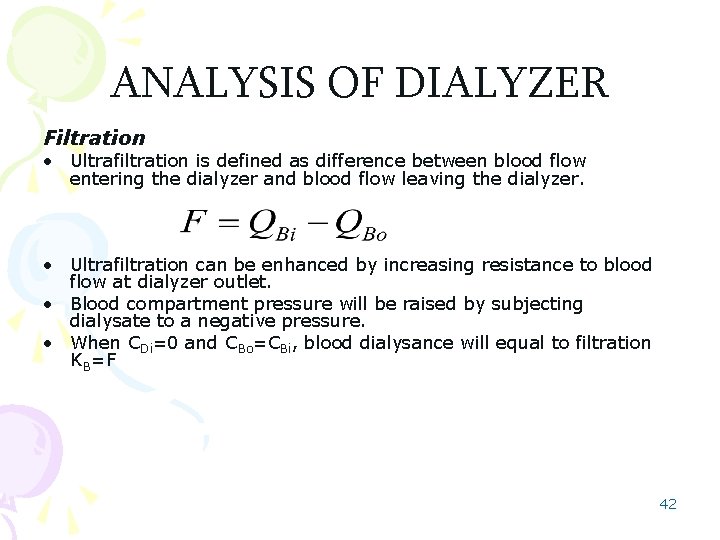
ANALYSIS OF DIALYZER Filtration • Ultrafiltration is defined as difference between blood flow entering the dialyzer and blood flow leaving the dialyzer. • Ultrafiltration can be enhanced by increasing resistance to blood flow at dialyzer outlet. • Blood compartment pressure will be raised by subjecting dialysate to a negative pressure. • When CDi=0 and CBo=CBi, blood dialysance will equal to filtration KB=F 42
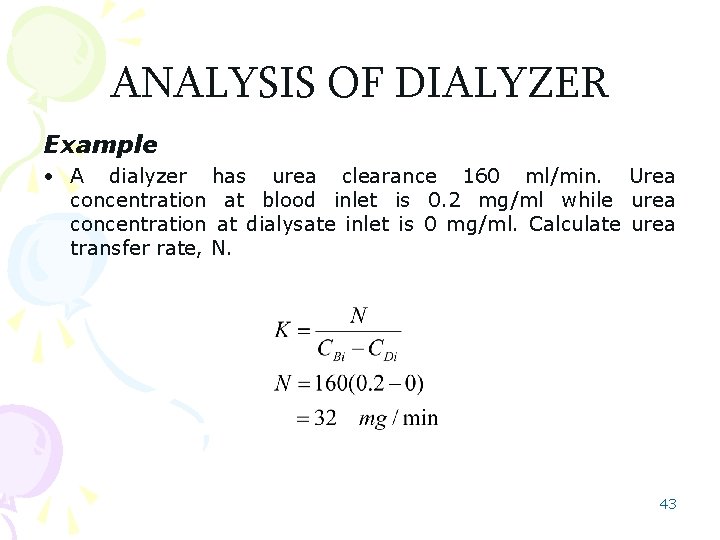
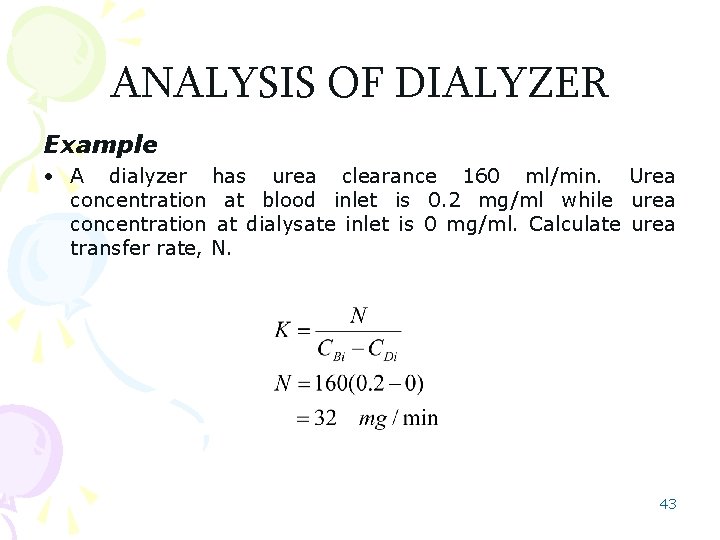
ANALYSIS OF DIALYZER Example • A dialyzer has urea clearance 160 ml/min. Urea concentration at blood inlet is 0. 2 mg/ml while urea concentration at dialysate inlet is 0 mg/ml. Calculate urea transfer rate, N. 43
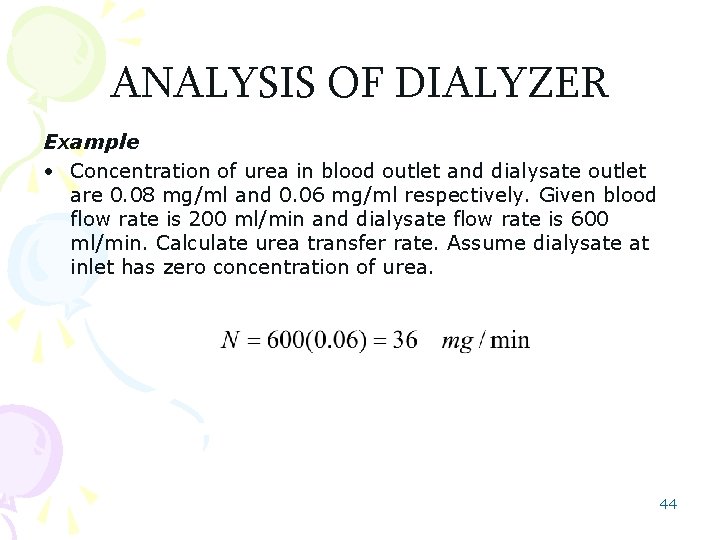
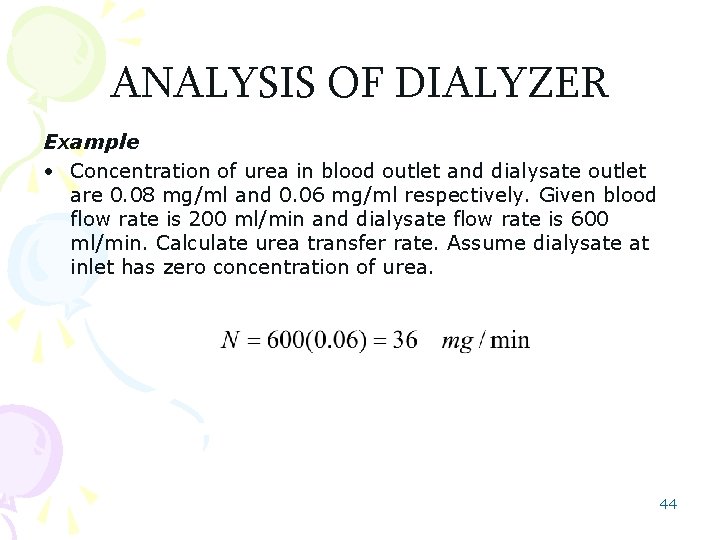
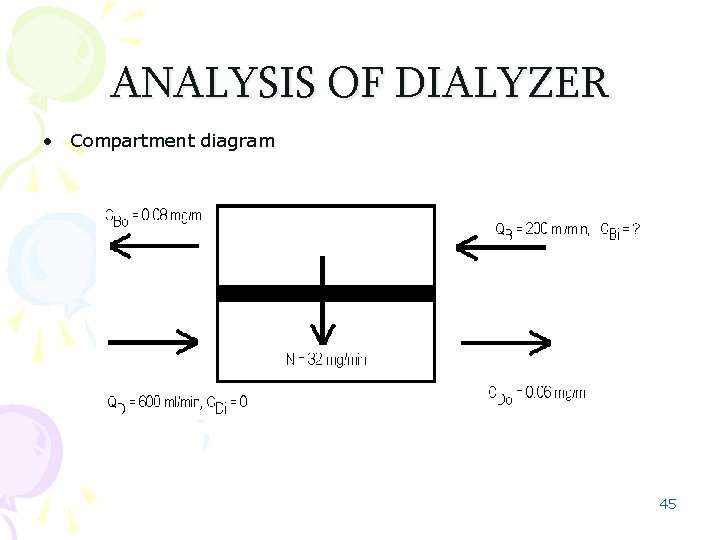
ANALYSIS OF DIALYZER Example • Concentration of urea in blood outlet and dialysate outlet are 0. 08 mg/ml and 0. 06 mg/ml respectively. Given blood flow rate is 200 ml/min and dialysate flow rate is 600 ml/min. Calculate urea transfer rate. Assume dialysate at inlet has zero concentration of urea. 44
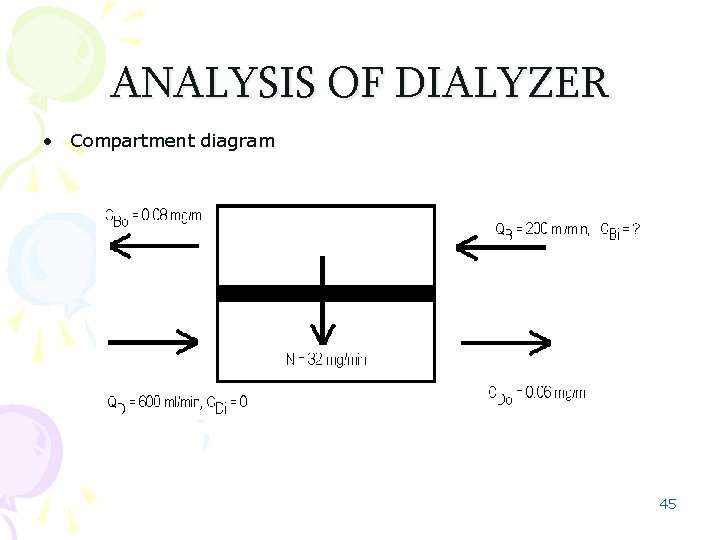
ANALYSIS OF DIALYZER • Compartment diagram 45
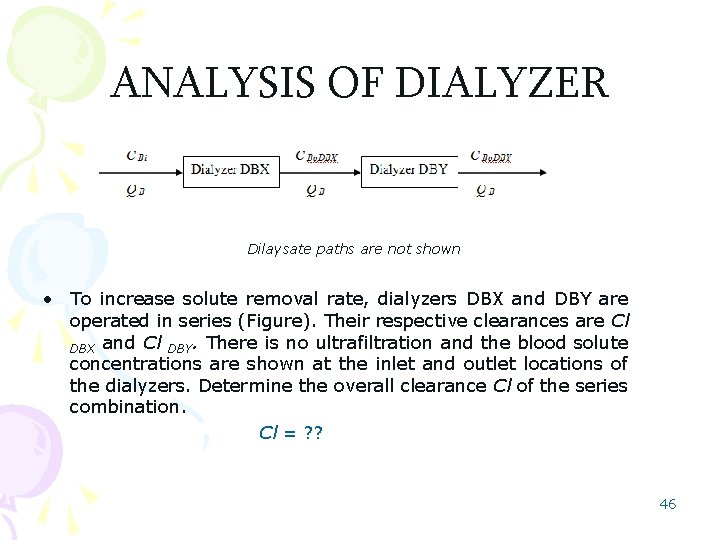
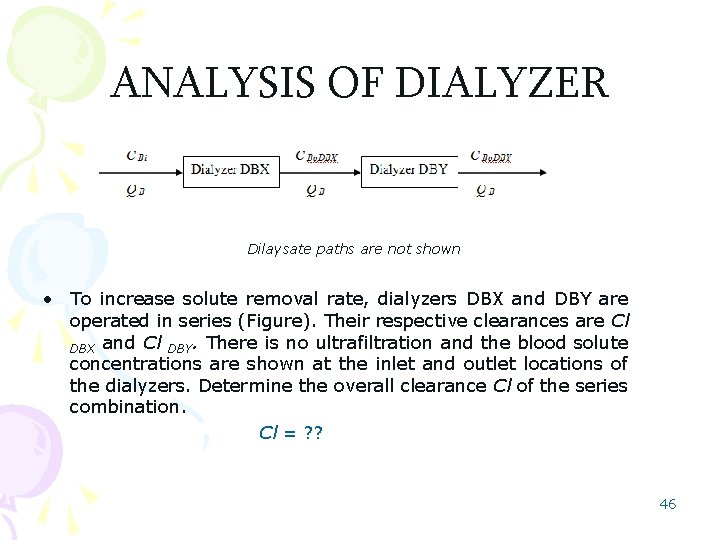
ANALYSIS OF DIALYZER Dilaysate paths are not shown • To increase solute removal rate, dialyzers DBX and DBY are operated in series (Figure). Their respective clearances are Cl DBX and Cl DBY. There is no ultrafiltration and the blood solute concentrations are shown at the inlet and outlet locations of the dialyzers. Determine the overall clearance Cl of the series combination. Cl = ? ? 46
 Lecturer's name or lecturer name
Lecturer's name or lecturer name Biomaterials artificial organs and tissue engineering
Biomaterials artificial organs and tissue engineering Designation of lecturer
Designation of lecturer Spe distinguished lecturer
Spe distinguished lecturer Cfa lecturer handbook
Cfa lecturer handbook Photography lecturer
Photography lecturer Gcwak
Gcwak Physician associate lecturer
Physician associate lecturer Lector vs lecturer
Lector vs lecturer Lecturer asad ali
Lecturer asad ali Lecturer in charge
Lecturer in charge Lecturer name
Lecturer name Spe distinguished lecturer
Spe distinguished lecturer Lecturer in charge
Lecturer in charge Designation lecturer
Designation lecturer Pearson lecturer resources
Pearson lecturer resources Good morning teacher
Good morning teacher Cos 318
Cos 318 Salmo 318
Salmo 318 Salmo 318
Salmo 318 Sia 318
Sia 318 Cos 318
Cos 318 Salmo 318
Salmo 318 Salmo 126
Salmo 126 Cos
Cos Pra onde eu irei salmos
Pra onde eu irei salmos Cos 318
Cos 318 Himno de alabanza oración
Himno de alabanza oración Dios es mi pastor y nada me faltara en hebreo
Dios es mi pastor y nada me faltara en hebreo Salmo 318
Salmo 318 Salmo 72
Salmo 72 Salmo 139:23-24 explicacion
Salmo 139:23-24 explicacion Operating system design issues
Operating system design issues Cos318
Cos318 Salmo 318
Salmo 318 Www.coloradoui.gov.myuiemployer
Www.coloradoui.gov.myuiemployer Salmo 66:19-20
Salmo 66:19-20 Z miasta a i b oddalonych o 510 km
Z miasta a i b oddalonych o 510 km Cos318
Cos318 Salmo 318
Salmo 318 Salmo 318
Salmo 318 Cos318
Cos318 Profgg
Profgg Salmo 318
Salmo 318 Www.coloradoui.gov.myuiemployer
Www.coloradoui.gov.myuiemployer Salmo 318
Salmo 318 Ncgs 14-318
Ncgs 14-318