ENFERMEDADES PULMONARES INTERSTICIALES DR ALFREDO DE LA CRUZ
![� IPF (IDIOPATHIC PULMONARY FIBROSIS) AND CFA (CRYPTOGENIC FIBROSING ALVEOLITIS ) ARE SYNONYMOUS[2] AND � IPF (IDIOPATHIC PULMONARY FIBROSIS) AND CFA (CRYPTOGENIC FIBROSING ALVEOLITIS ) ARE SYNONYMOUS[2] AND](https://slidetodoc.com/presentation_image_h2/4d3621b00699aaff72c8257290123733/image-10.jpg)
![FACTORES DE RIEZGO � IPF/UIP is more common in males[43, 56, 75, 78, 83] FACTORES DE RIEZGO � IPF/UIP is more common in males[43, 56, 75, 78, 83]](https://slidetodoc.com/presentation_image_h2/4d3621b00699aaff72c8257290123733/image-15.jpg)

- Slides: 24
ENFERMEDADES PULMONARES INTERSTICIALES DR. ALFREDO DE LA CRUZ MUÑOZ Neumologo Internista Guatemala C. A.
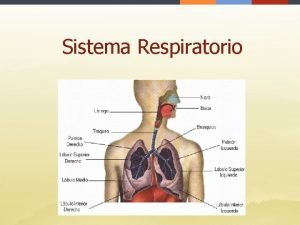
INFILTRACION INTERSTICIAL DIFUSA PULMONAR (IIDP) � Las enfermedades pulmonares intersticiales (interstitial lung diseases, ILD) � incluyen un gran número de enfermedades que afectan al parénquima del pulmón (los alvéolos, el epitelio alveolar, el endotelio capilar y los espacios entre estas estructuras, así como a los tejidos perivasculares y linfáticos).
� Un criterio de utilidad para la clasificación consiste en separar a las ILD en dos grupos con base en la histopatología mayor subyacente: � 1) las que se acompañan de inflamación y fibrosis predominantes, y � 2) las que tienen como aspectos que predominan reacciones granulomatosas en las zonas intersticiales o vasculares
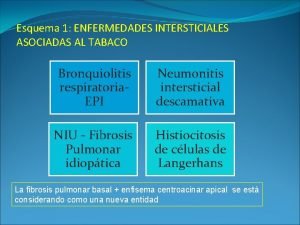
1. ALVEOLITIS, INFLAMACIÓN INTERSTICIAL Y FIBROSIS a. causa conocida � Amianto/Asbesto � Humos, gases � Fármacos (antibióticos, amiodarona, oro) y agentes quimioterápicos � Radiación � Neumonía por aspiración � Secuela del síndrome apneico del adulto
b. CAUSA DESCONOCIDA � � � � Neumonías intersticiales idiopáticas Fibrosis pulmonar idiopática (neumonía intersticial ordinaria) Neumonía intersticial descamativa Enfermedad pulmonar intersticial asociada a bronquiolitis respiratoria Neumonía intersticial aguda (lesión alveolar difusa) Neumonía organizativa criptógena (bronquiolitis obliterante con neumonía organizativa) Neumonía intersticial inespecífica
Enfermedades del tejido conjuntivo Lupus eritematoso diseminado, artritis reumatoide, espondilitis anquilosante, esclerosis sistémica, síndrome de Sjögren, polimiositis-dermatomiositis Síndromes de hemorragia pulmonar � Síndrome de Goodpasture, hemosiderosis pulmonar idiopática, capilaritis pulmonar aislada Proteinosis pulmonar alveolar � Trastornos infiltrativos linfocitarios (neumonitis intersticial linfocítica asociada a una enfermedad del tejido conjuntivo) � Neumonías eosinófilas � Linfangioleiomiomatosis � Amiloidosis �
Enfermedades heredadas Esclerosis tuberosa, neurofibromatosis, enfermedad de Niemann-Pick, enfermedad de Gaucher, síndrome de Hermansky-Pudlak � Enfermedades digestivas o hepáticas (enfermedad de Crohn, cirrosis biliar primaria, hepatitis crónica activa, colitis ulcerosa) � Enfermedad del injerto contra hospedador (trasplante de médula ósea; trasplante de órganos sólidos) �
2. RESPUESTA PULMONAR: GRANULOMATOSA � A. CAUSA CONOCIDA � Neumonitis por hipersensibilidad (polvos orgánicos) � Polvos inorgánicos: silicato de berilio
B. CAUSA DESCONOCIDA Sarcoidosis � Granulomatosis de células de Langerhans (granuloma eosinófilo del pulmón) � Vasculitis granulomatosa � Granulomatosis de Wegener, granulomatosis alérgica de Churg-Strauss � Granulomatosis broncocéntrica � Granulomatosis linfomatoide �
![IPF IDIOPATHIC PULMONARY FIBROSIS AND CFA CRYPTOGENIC FIBROSING ALVEOLITIS ARE SYNONYMOUS2 AND � IPF (IDIOPATHIC PULMONARY FIBROSIS) AND CFA (CRYPTOGENIC FIBROSING ALVEOLITIS ) ARE SYNONYMOUS[2] AND](https://slidetodoc.com/presentation_image_h2/4d3621b00699aaff72c8257290123733/image-10.jpg)
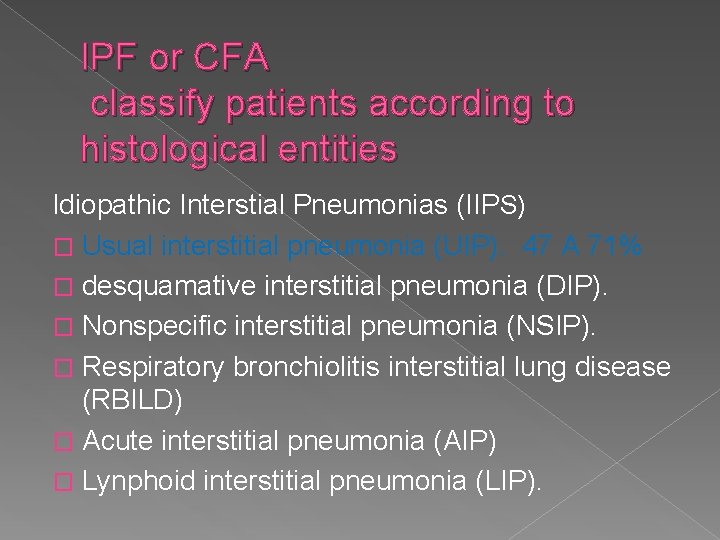
� IPF (IDIOPATHIC PULMONARY FIBROSIS) AND CFA (CRYPTOGENIC FIBROSING ALVEOLITIS ) ARE SYNONYMOUS[2] AND ARE ASSOCIATED WITH THE HISTOPATHOLOGICAL PATTERN UIP. [
IPF or CFA classify patients according to histological entities Idiopathic Interstial Pneumonias (IIPS) � Usual interstitial pneumonia (UIP). 47 A 71% � desquamative interstitial pneumonia (DIP). � Nonspecific interstitial pneumonia (NSIP). � Respiratory bronchiolitis interstitial lung disease (RBILD) � Acute interstitial pneumonia (AIP) � Lynphoid interstitial pneumonia (LIP).
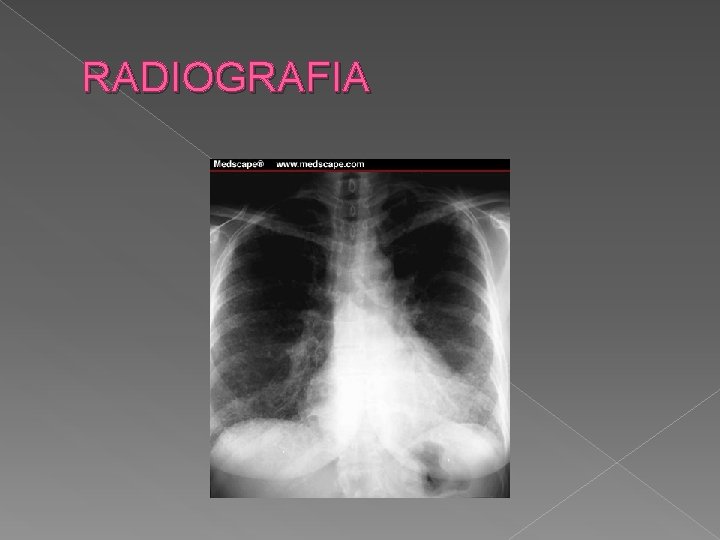
� Cardinal features of IPF/UIP include dry cough, exertional dyspnea, end-inspiratory velcro rales, diffuse parenchymal infiltrates on chest radiographs, honeycombing on HRCT, a restrictive defect on pulmonary function tests (PFTs), and impaired oxygenation. [2, 3, 42, 43] Exertional dyspnea progresses inexorably over months to years. [
HISTORIA NATURAL � The onset is indolent, but IPF/UIP progresses inexorably over months to years, with progressive fibrosis and destruction of lung parenchyma. [58] Spontaneous remissions do not occur, [5, 56, 63, 64] but some patients stabilize following an initial decline. [53, 56, 58] Most patients die of respiratory failure within 3 to 8 years of onset of symptoms; mean survival is 2. 8 to 3. 6 years. [
EPIDEMIOLOGIA � Idiopathic pulmonary fibrosis is rare, but precise data regarding incidence and prevalence are lacking. In 1988, 4, 851 deaths in the United States were attributed to pulmonary fibrosis (ICD-9, 515, n = 4, 694) and idiopathic pulmonary fibrosis (ICD-9, 516. 3, n = 157). [46
![FACTORES DE RIEZGO IPFUIP is more common in males43 56 75 78 83 FACTORES DE RIEZGO � IPF/UIP is more common in males[43, 56, 75, 78, 83]](https://slidetodoc.com/presentation_image_h2/4d3621b00699aaff72c8257290123733/image-15.jpg)
FACTORES DE RIEZGO � IPF/UIP is more common in males[43, 56, 75, 78, 83] and in current or former smokers. [53, 65, 76, 8385] Other risk factors include exposure to dusts or metals, [75] organic solvents, [86] and residence in agricultural or polluted urban areas
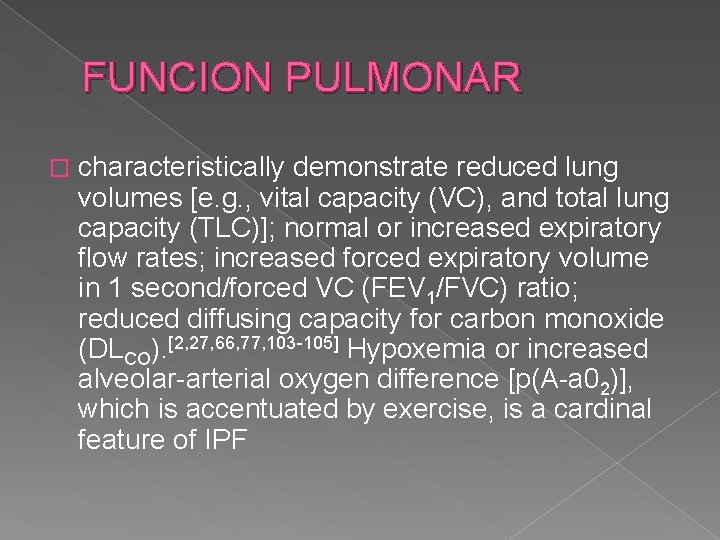
GENETICA � The mode of transmission of familial IPF is not known, but is believed to be autosomal dominant with variable penetrance in approximately 70% of cases; there is no clear mode of transmission in the remaining 30%
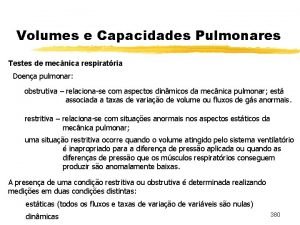
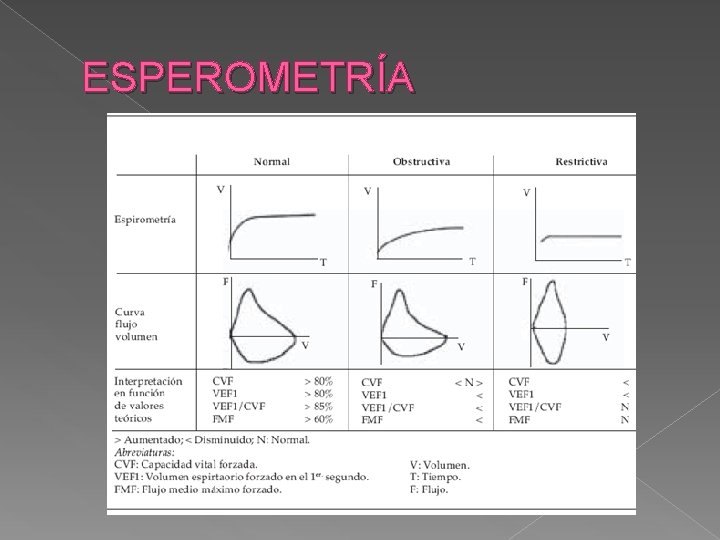
FUNCION PULMONAR � characteristically demonstrate reduced lung volumes [e. g. , vital capacity (VC), and total lung capacity (TLC)]; normal or increased expiratory flow rates; increased forced expiratory volume in 1 second/forced VC (FEV 1/FVC) ratio; reduced diffusing capacity for carbon monoxide (DLCO). [2, 27, 66, 77, 103 -105] Hypoxemia or increased alveolar-arterial oxygen difference [p(A-a 02)], which is accentuated by exercise, is a cardinal feature of IPF
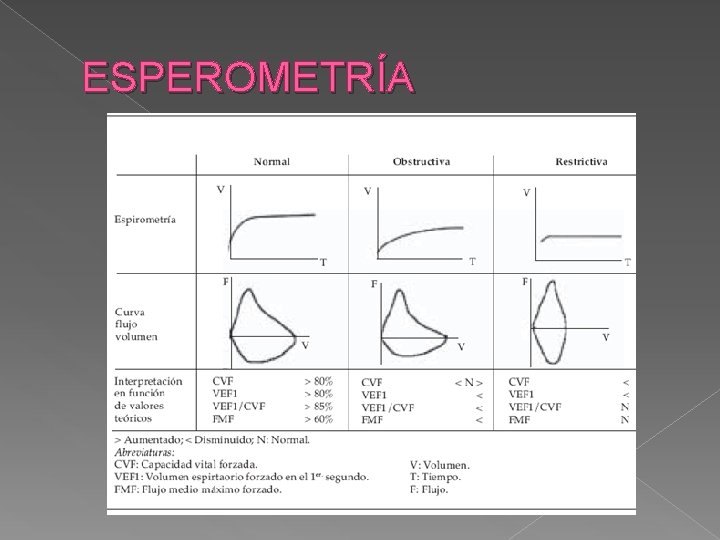
ESPEROMETRÍA
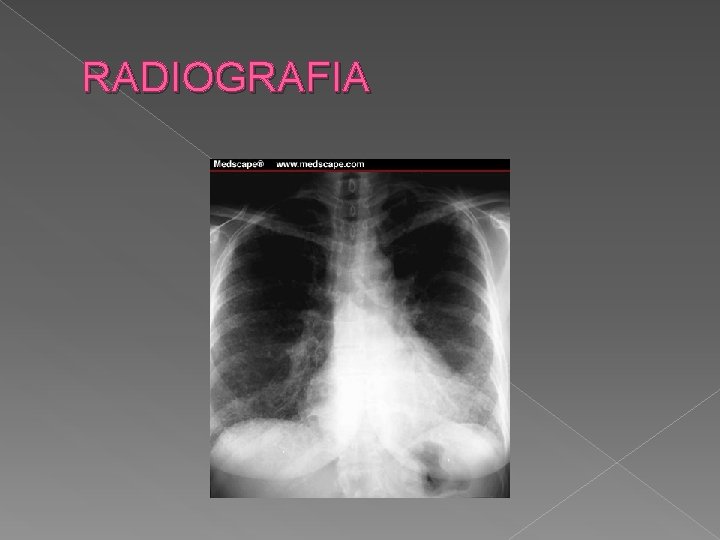
RADIOGRAFIA

HRCT
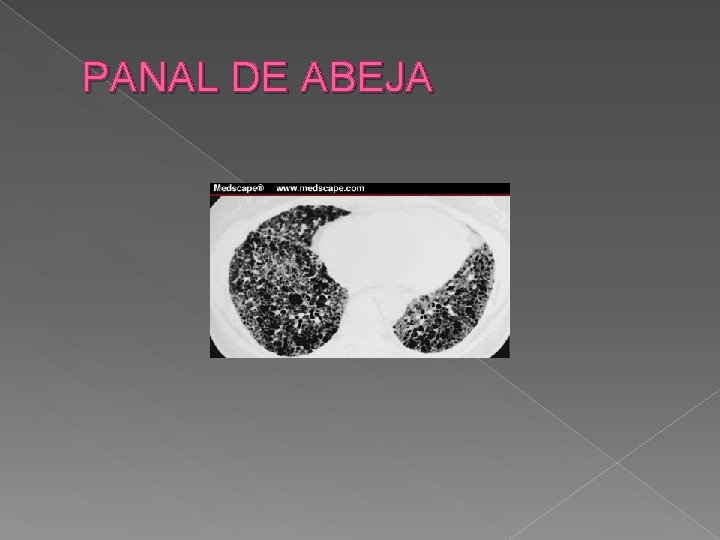
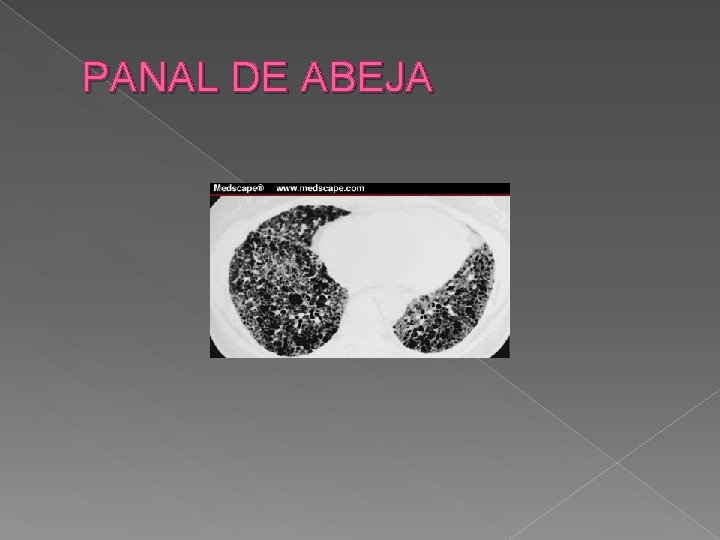
PANAL DE ABEJA
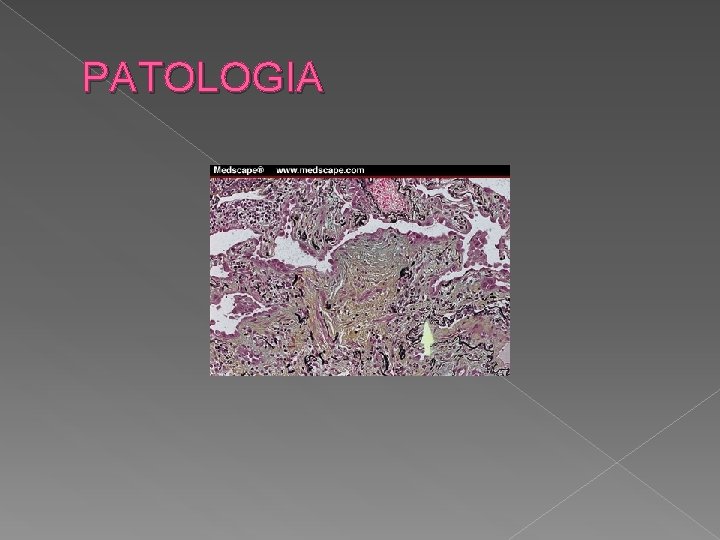
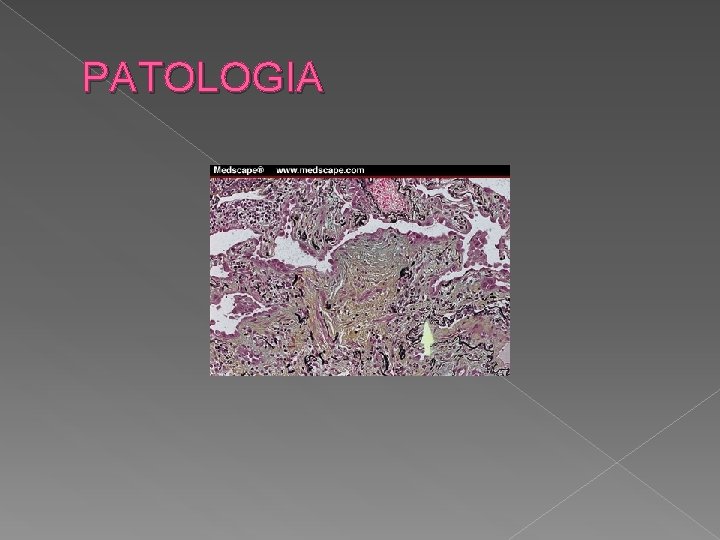
PATOLOGIA
TRATAMIENTO � In one clinical survey, 61% of IPF patients under age 70 were treated with corticosteroids, compared with 28% of patients over age 70. [44] Immunosuppressive or cytotoxic agents are used in only 2 to 17% of patients with IPF/CFA. [42, 44, 47, 65] Other treatment options (albeit unproven) include colchicine, [47, 127, 179, 245] D-penicillamine, [245] perfenidone, [41] Nacetylcysteine (NAC), [179] and gamma-interferon
� Treatment for IPF needs to be individualized � AZA (2 -3 mg/kg/day, maximum daily dose 150 mg � oral CP (dose 1 -2 mg/kg/day; maximum dose 150 mg/day) plus prednisone � corticosteroids (e. g. , 0. 5 mg/kg/day) can be tried.
 Espirometria normal y epoc
Espirometria normal y epoc Endocrinocitos
Endocrinocitos Solucion solida
Solucion solida Mario ademar cruz cruz
Mario ademar cruz cruz Volumenes y capacidades pulmonares
Volumenes y capacidades pulmonares Esbozos pulmonares
Esbozos pulmonares Epicondrio
Epicondrio Volumes e capacidades pulmonares - fisiologia
Volumes e capacidades pulmonares - fisiologia Crioablacion de venas pulmonares
Crioablacion de venas pulmonares Silueta cardiotimica hasta que edad
Silueta cardiotimica hasta que edad Tumores pulmonares benignos
Tumores pulmonares benignos Abdomen bdi medicina
Abdomen bdi medicina Aparatos
Aparatos Anhidrasa carbónica
Anhidrasa carbónica Capacidad vital y capacidad vital forzada
Capacidad vital y capacidad vital forzada Alterações fibrocicatriciais nos apices pulmonares
Alterações fibrocicatriciais nos apices pulmonares Cuerdas vocales verdaderas
Cuerdas vocales verdaderas Volume capacidade pulmonar
Volume capacidade pulmonar ápices pulmonares
ápices pulmonares Segmentos pulmonares
Segmentos pulmonares Enfermedades del sistema endocrino
Enfermedades del sistema endocrino Enfermedades mentales de los signos del zodiaco
Enfermedades mentales de los signos del zodiaco Enfermedades restrictivas
Enfermedades restrictivas Edgar lopategui corsino
Edgar lopategui corsino Enfermedades del sistema urinario
Enfermedades del sistema urinario