Early Detection and Prevention of ICU Delirium Are




- Slides: 31

Early Detection and Prevention of ICU Delirium Are you doing your part?
Instructions § This program awards 0. 5 CE. § Before proceeding to the posttest, thoroughly review the following Power. Point© program. – For best learning experience, view in “Slide Show” otherwise link(s) will not work. – The posttest is a test, not an Acknowledgement. § When complete, close the program and “Take Test”. There is not need to submit an Attendance Record; successful completion of the posttest will automatically record your completion in the Edu. Tracker system. § Print a certificate for your CE records. St. Luke’s University Health Network
Objectives At the conclusion of this program, the learner will be able to: § Describe Delirium § Discuss the potential causes of Delirium § Identify the interventions that should be employed in the ICU setting to prevent Delirium § Assimilate the use of the CAM-ICU into practice St. Luke’s University Health Network
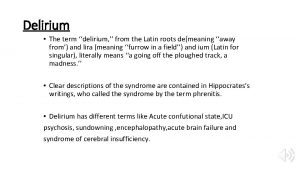
What is Delirium? § “…a clinical syndrome characterized by disturbance in consciousness, attention, cognition, and perception”, (Alexander, 2009). § …is a syndrome of several different etiologies characterized by a disturbance of consciousness combined with a change in cognition. Factoid: the incidence of delirium in the ICU ranges from 45 to 87% and seems to vary between intubated patients and non intubated patients. St. Luke’s University Health Network
Pathophysiology Different mechanisms have been proposed: § These mechanisms are not mutually exclusive and likely act in concert with each other. § One hypothesis speculates that decreased cholinergic activity may lead to delirium. § There is an imbalance between inflammatory and antiinflammatory mediators. § Both increased and relative serotonin deficiencies have been associated with delirium. § Patients with underlying central nervous system disease may have a heightened response to inflammatory mediators. St. Luke’s University Health Network
Clinical Manifestations Typically manifests as a constellation of symptoms with an acute onset and fluctuating course. Symptoms have been organized into cognitive and behavioral groups: § Common cognitive symptoms: – – – inability to sustain attention impaired short term memory impaired visuospatial ability reduced level of consciousness preservation § Common behavioral symptoms: – – sleep wake cycle disturbance irritability hallucinations delusions St. Luke’s University Health Network
Symptoms of Delirium Symptoms may appear over a few hours to several days in the ICU and may including but are not limited to: § Visual and/or auditory hallucinations § Impulsive behavior § Disoriented § Acute confusion, decreased focus, inability to maintain attention § Aggressive behavior Waxing/waning of symptoms is also possible… St. Luke’s University Health Network
Types of Delirium As defined by Balas, et al (2012): § Hyperactive – “…screaming out in fear, describing hallucinations, pulling at tubes, trying to climb out of bed, and attempting to hit staff…” § Hypoactive – “…may be missed in the absence of active monitoring and is more common in older, seriously ill patients…” § Mixed – combination of the above (also the most common form) St. Luke’s University Health Network
Causes of Delirium can be caused by singular or multiple factors. Factors can be pharmacological and/or non-pharmacological. Delirium can be present prior to admission, or can develop quickly in the elderly population and/or the patients with history of recent substance abuse. St. Luke’s University Health Network
Pharmacologic Causes Including but not limited to: § Polypharmacy § Anxiolytics (i. e. lorazepam) § Antibiotics (i. e. floroquinalones) § Opioids/Narcotics (i. e. morphine) § Antidepressants (i. e. amitriptyline) § Corticosteroids (i. e. hydrocortisone) § Anesthesia St. Luke’s University Health Network

Non-pharmacological causes Predisposing factors, including, but not limited to: – – Age (elderly/older adults) History of recent substance abuse (i. e. illicit drugs, tobacco, etc. ) History of recent alcohol abuse Other pre-existing conditions that may alter consciousness St. Luke’s University Health Network
Non-pharmacological causes Including but not limited to: • Nutritional/Hydration status • Baseline mental status Environmental • Ambient noise level during sleeping hours • Lighting level during sleeping hours • Change in sleeping hours • Sleep deprivation • Staff –faces unfamiliar to the patient
Non-pharmacological causes Factors directly related to severity of illness/ICU stay, including but not limited to: – – – Electrolyte imbalance Hypotension Hypoxia Anemia Acid/Base imbalance St. Luke’s University Health Network
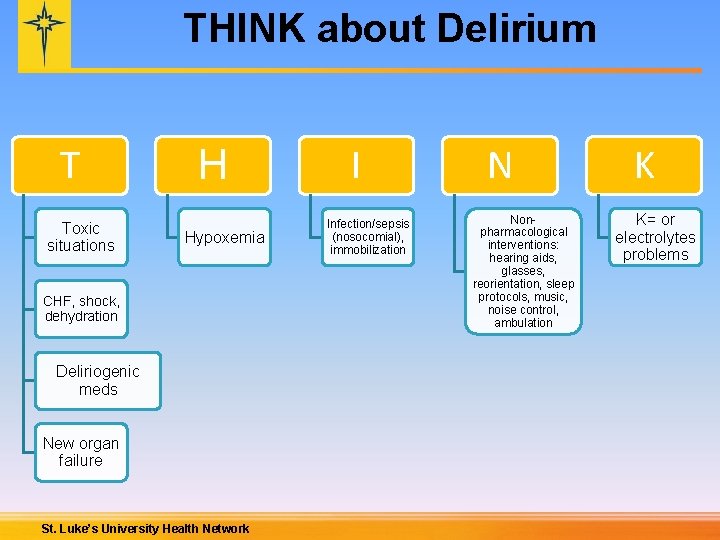
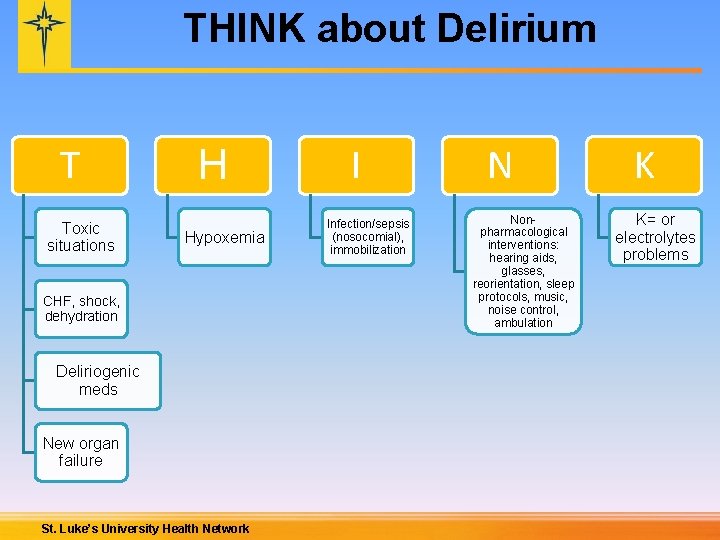
THINK about Delirium T Toxic situations H Hypoxemia CHF, shock, dehydration Deliriogenic meds New organ failure St. Luke’s University Health Network I Infection/sepsis (nosocomial), immobilization N Nonpharmacological interventions: hearing aids, glasses, reorientation, sleep protocols, music, noise control, ambulation K K= or electrolytes problems
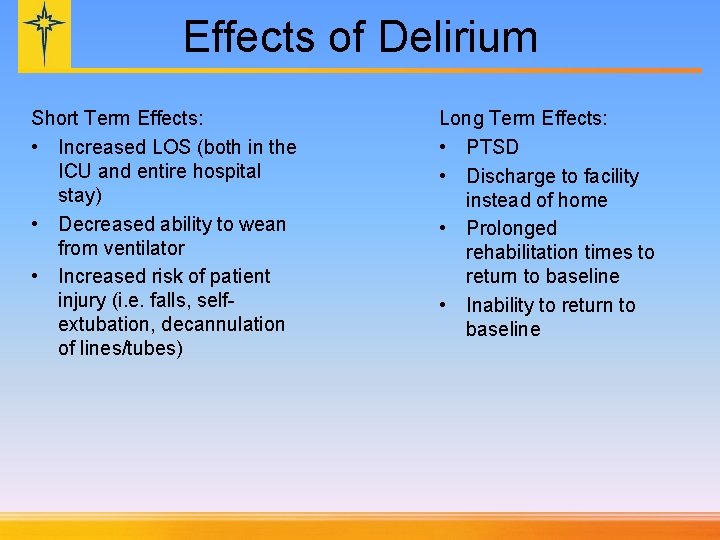
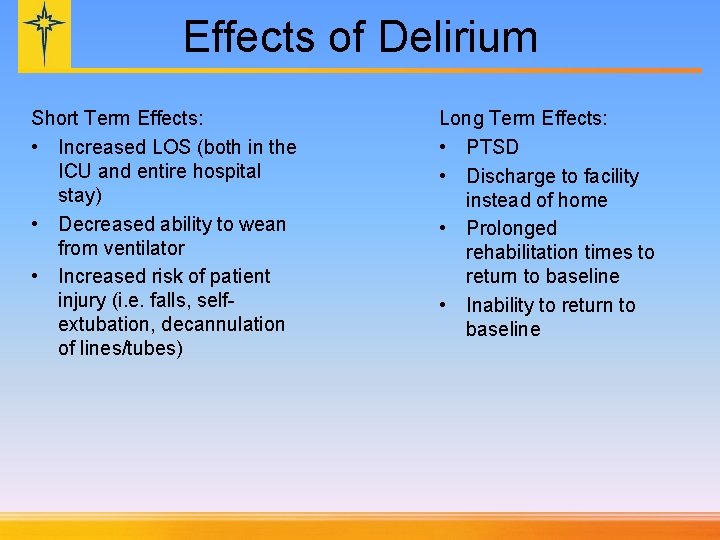
Effects of Delirium Short Term Effects: • Increased LOS (both in the ICU and entire hospital stay) • Decreased ability to wean from ventilator • Increased risk of patient injury (i. e. falls, selfextubation, decannulation of lines/tubes) Long Term Effects: • PTSD • Discharge to facility instead of home • Prolonged rehabilitation times to return to baseline • Inability to return to baseline
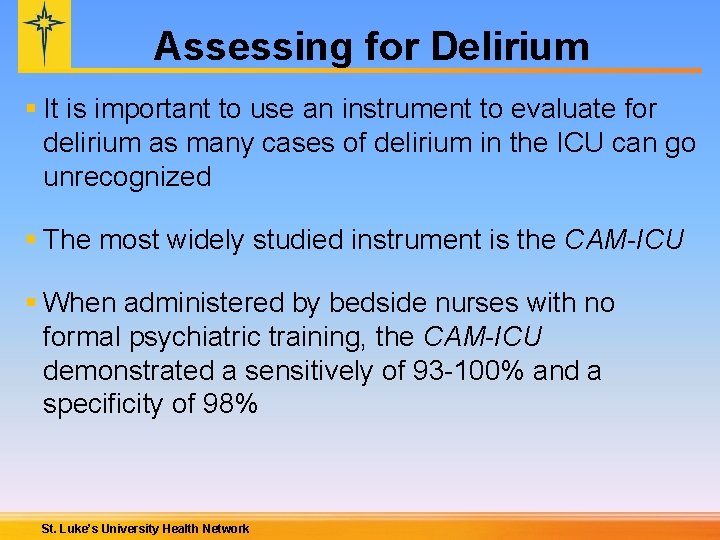
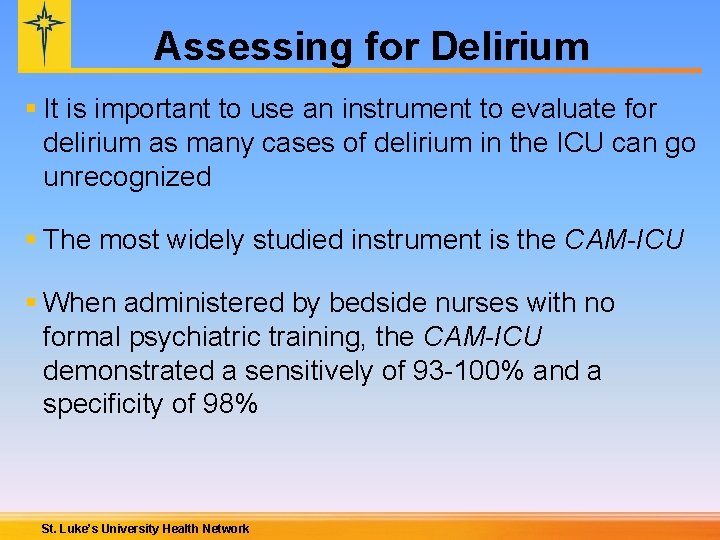
Assessing for Delirium § It is important to use an instrument to evaluate for delirium as many cases of delirium in the ICU can go unrecognized § The most widely studied instrument is the CAM-ICU § When administered by bedside nurses with no formal psychiatric training, the CAM-ICU demonstrated a sensitively of 93 -100% and a specificity of 98% St. Luke’s University Health Network
CAM-ICU Scoring Confusion Assessment Method for the ICU http: //www. youtube. com/watch? v=6 Wy. J 0 z. L 7 Vk. I St. Luke’s University Health Network

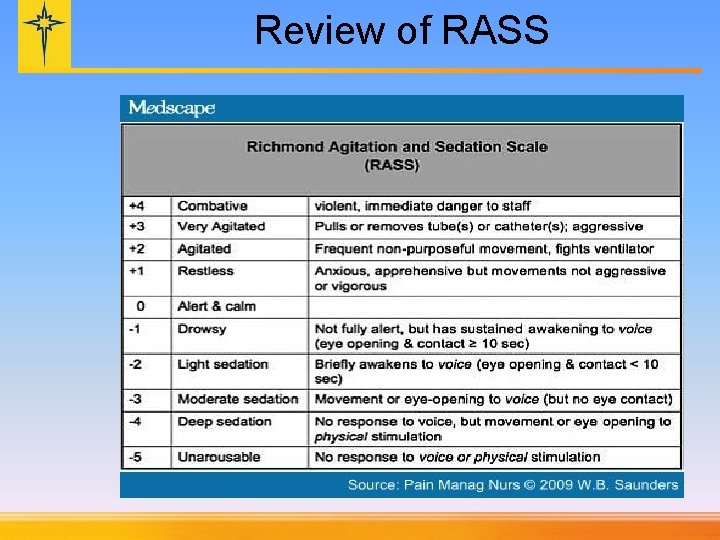
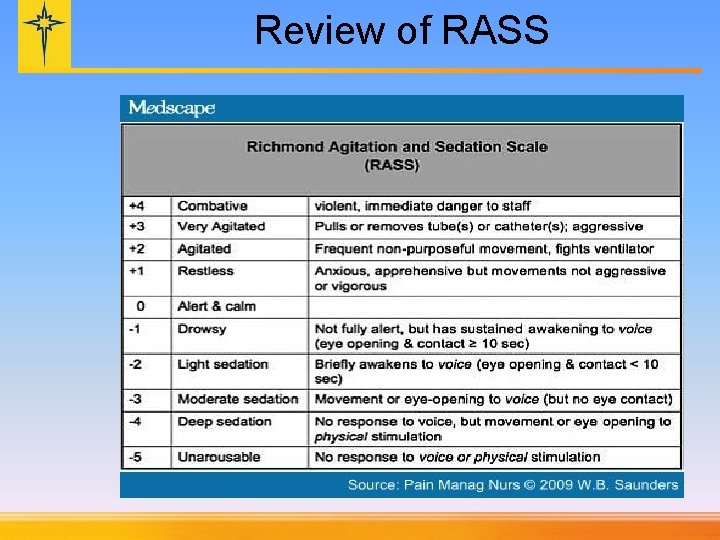
Review of RASS
Assessing for Delirium § Baseline on admission § Every Q 12 H with 08: 00 and 20: 00 assessments § With any noted or suspected changes in patient’s mental status St. Luke’s University Health Network
Sample Charting Screens

Sample Charting Screens
Interventions § Primary prevention is key! § Nursing staff will be scoring CAM-ICU scales q 12 hours and with any change in mental status. § Nursing staff will discuss CAM-ICU findings on rounds and communicate changes as necessary. § Any and all interventions should be employed as the patient tolerates. – This will be part of the nursing assessments. – Interventions can be non-pharmacologic or pharmacologic. St. Luke’s University Health Network
Interventions: Non-Pharmacologic § Decrease sleep deprivation – Lights out, shades closed, TVs off, baths done, etc. all well before 11 pm; to promote longer periods of uninterrupted sleep – Decrease staff noise after 11 pm § Increase day time activity/early mobilization – Lights on, window shades open, OOB (vented and non-vented patients), early and consistent Rehabilitation Services involvement as appropriate – Eye glasses on, hearing aids in § Improve nutrition/hydration status – UCAT § Monitor mental status – Report changes to care team § Family involvement – Encourage families/friends to conclude visiting by 8: 30 pm, also not waking patients in the middle of the night. St. Luke’s University Health Network
Interventions: Pharmacologic § The first step is to look at the patients current medication list for potential drugs that increase risk of delirium development: – Benzodiazepines (Alcohol withdrawal delirium still treated with benzodiazepines) – Narcotics – Levaquin – Pepcid § Although there is not a lot of good data to support the routine use of Haldol in the treatment of delirium, there is also insufficient evidence to recommend against it. – Currently really only drug available – Need to monitor QT interval St. Luke’s University Health Network
Goals § Decrease the number of incidences of delirium in the ICU populations § Decrease sequelae related to delirium – Decrease LOS – Decrease ventilator days /invasive device days § Ensure consistency of clinical practices related to Delirium prevention, recognition, assessment and treatment across all St. Luke’s University Health Network ICU settings St. Luke’s University Health Network
Why is this so important? …because Delirium happens to our patients… St. Luke’s University Health Network
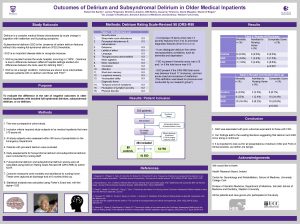
Example of Current MICU Delirium Data § Our sample size was obtained twice a day over a 5 week period – 55 patients • 26 male • 29 female – 5 patients were excluded due to comatose state – 44% of MICU patients at some point tested positive for delirium Further breakdown of data coming… St. Luke’s University Health Network
Summary: Putting it all together… § Assess each patient on admission for his/her functional & cognitive status prior to admission. § Employ non-pharmacological interventions for the prevention of delirium development. Every patient, Every Time! § Employ early, progressive mobility for all patients once hemodynamically stable. § If delirium is suspected, perform CAM-ICU. § If CAM-ICU is positive, report to critical care team. § Use pharmacological intervention strategies when delirium is identified. St. Luke’s University Health Network
Literature Lat, I. , Mc. Millian, W. , Taylor, S. (2009). The impact of delirium on clinical outcomes in mechanically ventilated surgical and trauma patients. Critical Care Med. 37(6): 1898 -1906. Milbrandt, E. , Deppen, S. , et al. (2004). Costs associated with delirium in mehanically ventilated patients. Crit Care Med. 32(4): 955 -962. Thomason, J. , Shintani, A. , et al. (2005). Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Critical Care. 9(4): R 375 -81. Ely, E. , Inouye, S. , et al. (2001). Delirium in mechanically ventilated patients: Validity and reliability of the Confusion Assessment Method for the Intensive Care Unite (CAM-ICU). JAMA. 286: 2703 -2710 St. Luke’s University Health Network
Thank you! § Thank you to the Allentown ICU/Rapid Response Teams for their initial work called the ICU EPIC project; some of this program is based on their work. § Thank you to MICU nurses Nicole Gieniec and Erica Moulding and to Donna Martonik and the Allentown ICU Team for developing this program. § Contact your patient care manager or educator with questions about this program. St. Luke’s University Health Network
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Insidan region jh
Insidan region jh Starvation deadlock
Starvation deadlock Deadlock prevention avoidance and detection
Deadlock prevention avoidance and detection National breast and cervical cancer early detection program
National breast and cervical cancer early detection program National breast and cervical cancer early detection program
National breast and cervical cancer early detection program Difference between dementia and delirium
Difference between dementia and delirium Difference between delirium and dementia ppt
Difference between delirium and dementia ppt Amnesia
Amnesia Ekd system
Ekd system Lucie big delirium
Lucie big delirium Dr rose dinda martini
Dr rose dinda martini Nash delirium
Nash delirium Terminalt delirium
Terminalt delirium Escala cam delirium
Escala cam delirium Delirium care pathways
Delirium care pathways Delirium definition
Delirium definition Delirium definition
Delirium definition Excited delirium перевод
Excited delirium перевод Escala de cam
Escala de cam Delirium case presentation
Delirium case presentation Flocculation delirium
Flocculation delirium Tingkat kesadaran
Tingkat kesadaran Driver diagram palliative care
Driver diagram palliative care Early cpr and early defibrillation can: *
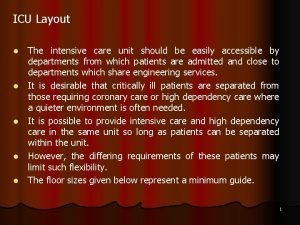
Early cpr and early defibrillation can: * Icu layout and design
Icu layout and design Rumus depkes menghitung tenaga perawat
Rumus depkes menghitung tenaga perawat Escalas de sedacion
Escalas de sedacion Icu localization
Icu localization Icu tersier
Icu tersier Emphancy
Emphancy Icu indication
Icu indication