Differential Diagnosis Infantile Stridor Amy Stinson MS IV










- Slides: 32
Differential Diagnosis: Infantile Stridor Amy Stinson MS IV KCUMB
Stridor l An expression of partial respiratory tract obstruction 2° to external compression or partial occlusion within the airway 1 l Character & Intensity: – Site & Degree of obstruction – Airflow velocity & Pressure gradient – Stridor
Stridor l Inspiratory – problem at or above vocal cords, usually high pitched at cords, low pitched above cords – Laryngomalacia, unilateral cord paralysis l Expiratory – problem is below cords – tracheobronchial tree, more prolonged – Vascular compression l Biphasic – usually subglottic – Subglottic stenosis, subglottic hemangioma, bilateral cord paralysis
Laryngomalacia Most common cause of stridor l Most common congenital laryngeal abnormality l “Congenital flaccid larynx” or “Inspiratory laryngeal collapse” l Inspiration: l – Prolapse of supraglottic structures – Extreme infolding of “Omega-shaped” epiglottis and aryepiglottic folds
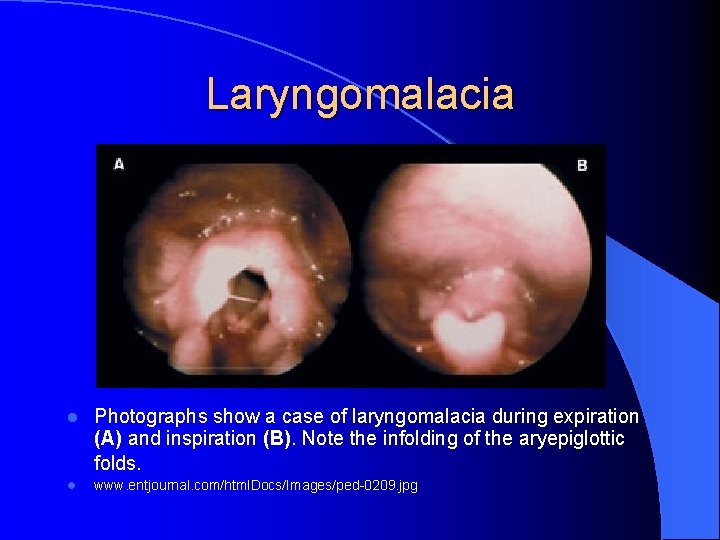
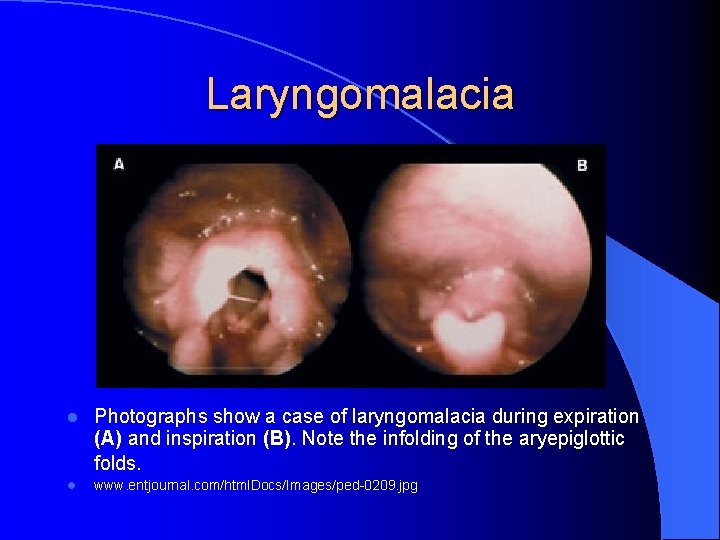
Laryngomalacia l Photographs show a case of laryngomalacia during expiration (A) and inspiration (B). Note the infolding of the aryepiglottic folds. l www. entjournal. com/html. Docs/Images/ped-0209. jpg

Laryngomalacia l l Normal Vs Abnormal www. meei. harvard. edu/. . . /images/laryngomal. jpg

Laryngomalacia l Signs & symptoms: – Inspiratory stridor within a few days of birth – Initially mild more pronounced with a peak at 6 – 9 – – mo 4 Stridor is worse when supine and neck flexion: better when prone and neck extension 1 Symptoms worse when sleeping, feeding, or on exertion Most commonly – mild stridor that is self limited Most cases spontaneously resolve by 2 yrs of age
Laryngomalacia l More Severe: – Severe stridor, apneic episodes, feeding problems, & FTT – pulmonary HTN & cor pulmonale l Presumed etiologies: 4 – Abnormally pliable supraglottic cartilage – Neuromuscular abnormalities – GER
Laryngomalacia l DX: – Endoscopy under local anesthesia – Laryngotracheobronchoscopy to R/O other path – Polysomnography to detect desaturations w/hypoxia or hypercapnia l Treatment: – OBSERVE – Temp trach in severe cases – Sx for 10% supraglottoplasty which reduces amount of laryngeal mucosa – Anti-reflux meds
Laryngomalacia l “State Dependent” Laryngomalacia 6 – Neurogenic factors would cause at states of awareness – often paradoxical. – Direct stimulation resolves l Discoordinate Pharyngolaryngomalacia 6 – Assoc. with severe collapse and poor outcomes – Need CPAP & nasal stents and poss. trach
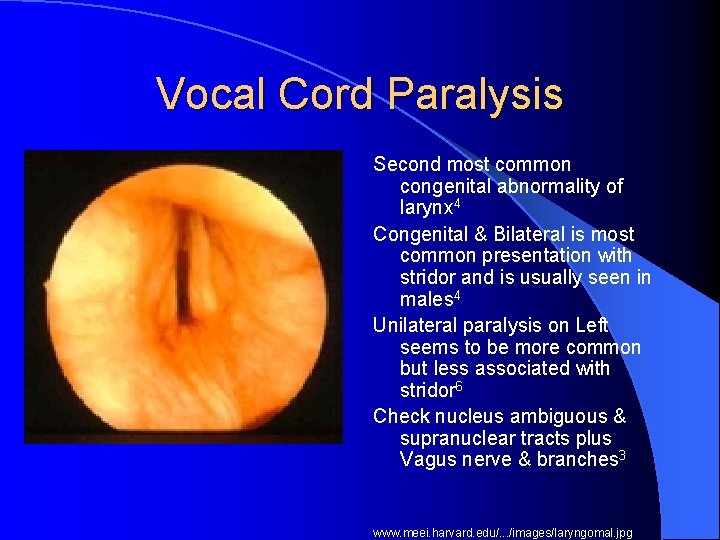
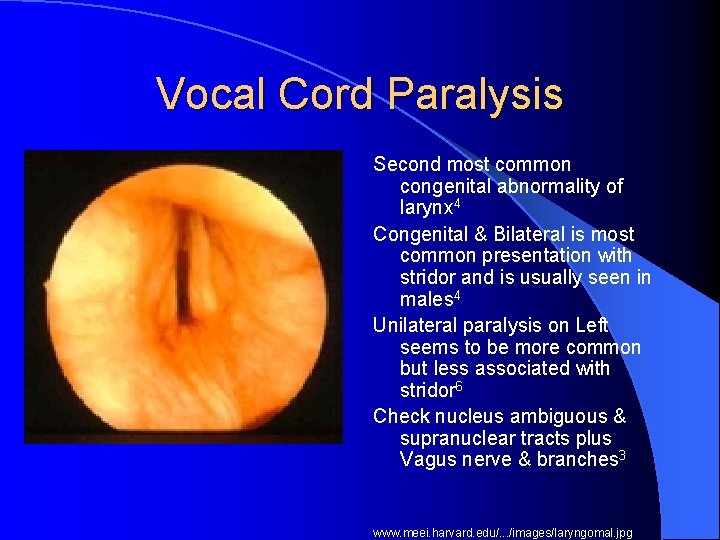
Vocal Cord Paralysis Second most common congenital abnormality of larynx 4 Congenital & Bilateral is most common presentation with stridor and is usually seen in males 4 Unilateral paralysis on Left seems to be more common but less associated with stridor 6 Check nucleus ambiguous & supranuclear tracts plus Vagus nerve & branches 3 www. meei. harvard. edu/. . . /images/laryngomal. jpg

Vocal Cord Paralysis l Etiology: – Idiopathic – CNS: Arnold-Chiari malformation – CV: Congenital abnormalities of heart & great vessels of Sx correction of – Trauma: Repair of TE fistula, birth trauma, head injury – Inflammatory: Guillian-Barre – PNS: myotonic dystrophy, myasthenia gravis
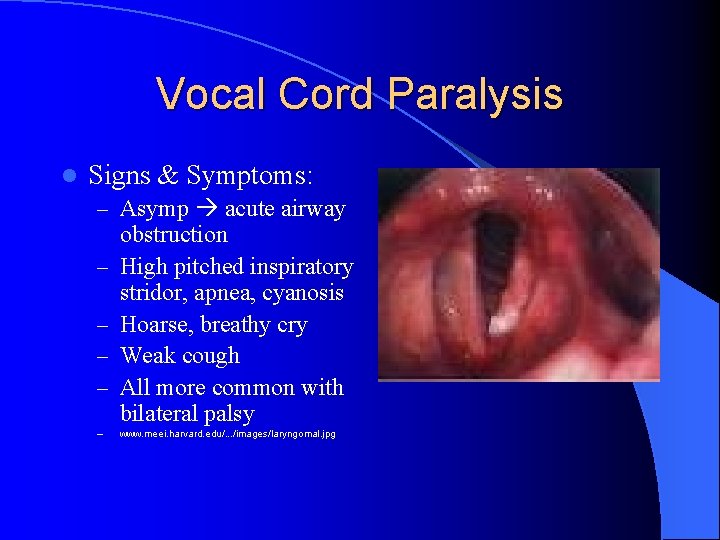
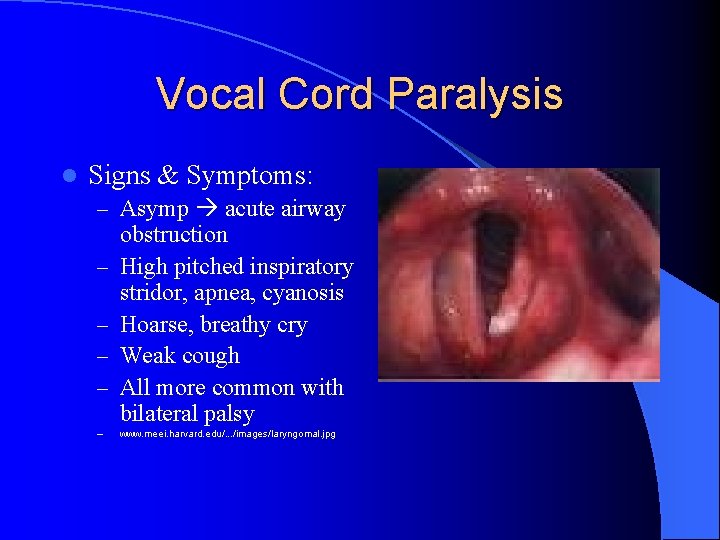
Vocal Cord Paralysis l Signs & Symptoms: – Asymp acute airway – – – obstruction High pitched inspiratory stridor, apnea, cyanosis Hoarse, breathy cry Weak cough All more common with bilateral palsy www. meei. harvard. edu/. . . /images/laryngomal. jpg
Vocal Cord Paralysis l Dx: – Fiberoptic endoscopy – Laryngotracheobronchoscopy – MRI l Tx: – Unilateral: Observe, Speech therapy – Bilateral: Tracheotomy, frequent endoscopies, no Sx for at least a year – maybe longer

Vocal Cord Paralysis www. meei. harvard. edu/. . . /imag es/laryngomal. jpg

Subglottic Stenosis 3 rd most common congenital cause of stridor l Subglottis is the narrowest part of airway & the only complete ring (cricoid cartilage) l Congenital & Acquired l l www. meei. harvard. edu/. . . /images/laryngom al. jpg

Subglottic Stenosis 2, 4, 5 l Congenital: – Soft tissue stenosis or cartilaginous stenosis – Severe: stridor at birth – Mild: intermittent stridor & resp tract infections l Acquired: – Neonatal intubations, external trauma, high trach, infection, burns – Repeated failure of attempted extubation – Gradual onset of stridor after extubation
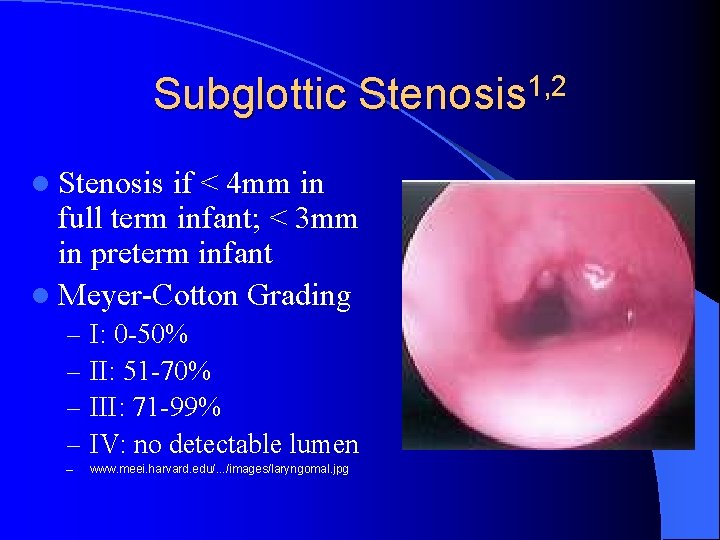
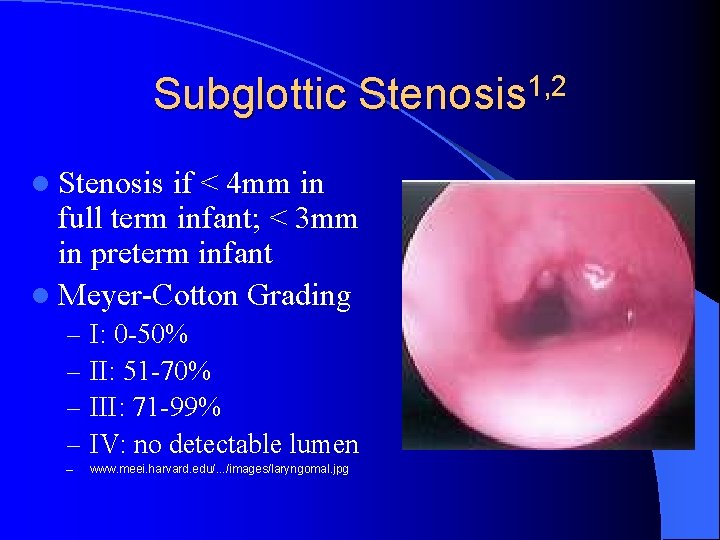
Subglottic Stenosis 1, 2 l Stenosis if < 4 mm in full term infant; < 3 mm in preterm infant l Meyer-Cotton Grading – – I: 0 -50% II: 51 -70% III: 71 -99% IV: no detectable lumen – www. meei. harvard. edu/. . . /images/laryngomal. jpg
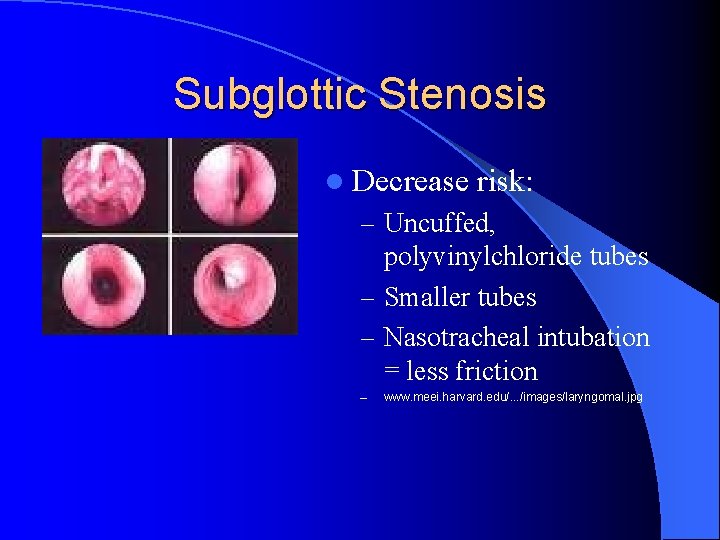
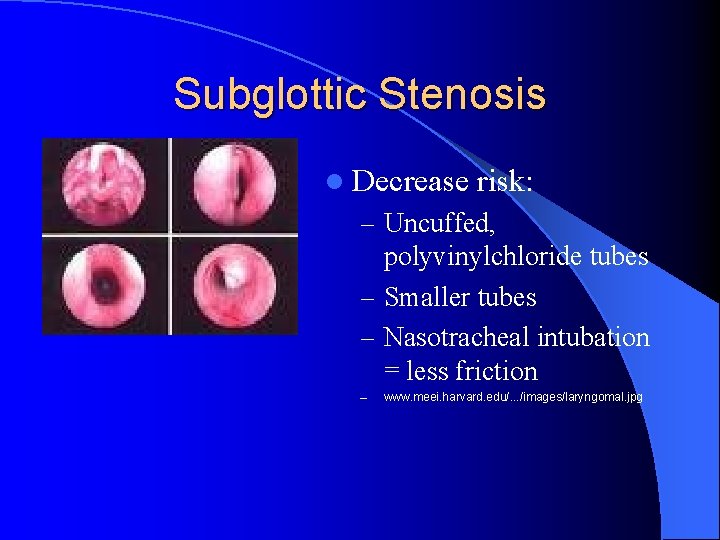
Subglottic Stenosis l Decrease risk: – Uncuffed, polyvinylchloride tubes – Smaller tubes – Nasotracheal intubation = less friction – www. meei. harvard. edu/. . . /images/laryngomal. jpg
Subglottic Stenosis l Treatment: – Observe: Grade I, II, airway can increase with growth – – of child Tracheotomy: until reconstruction Endoscopic: Laser can decrease granulation tissue, can actually worsen with long term scarring Laryngotracheal reconstruction: requires cartilage grafts and stents, enlarges stenosed portion Cricotracheal resection: excises stenosed portion, higher success rate, but increased risk of recurrent laryngeal nerve damage
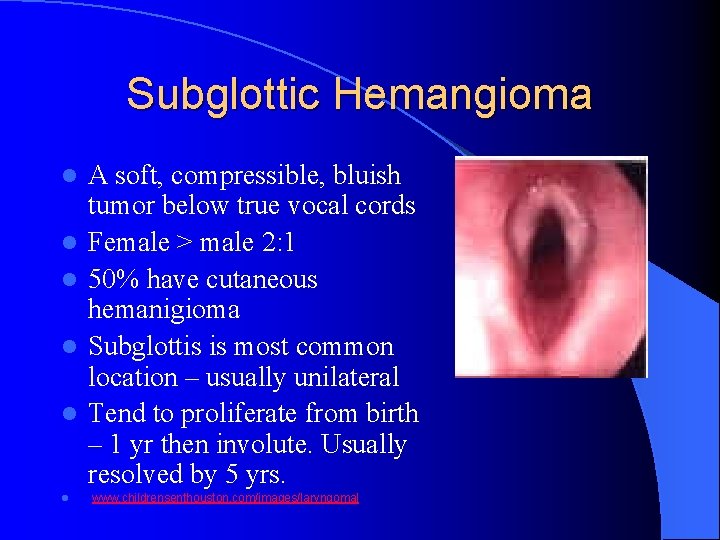
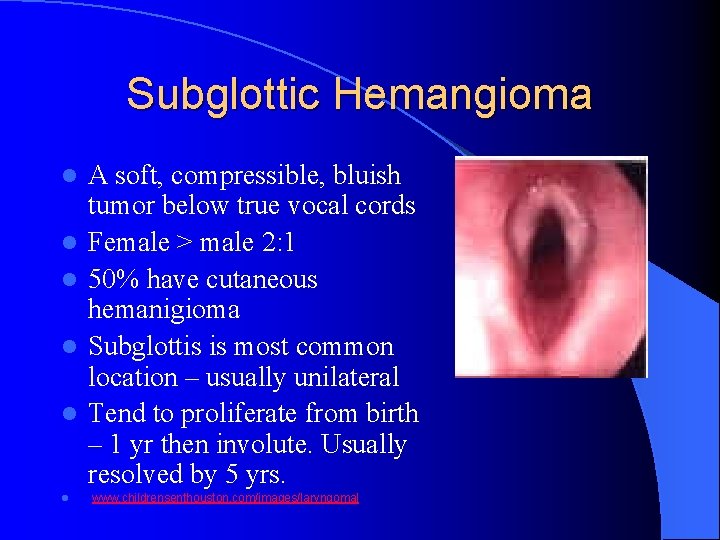
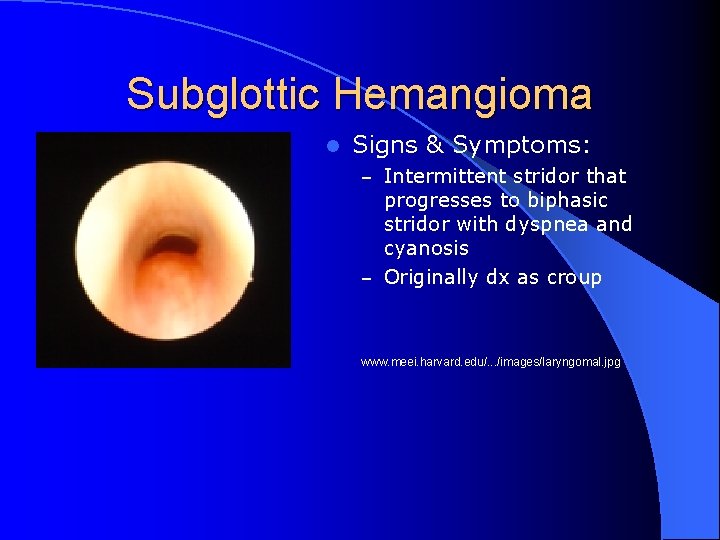
Subglottic Hemangioma l l l A soft, compressible, bluish tumor below true vocal cords Female > male 2: 1 50% have cutaneous hemanigioma Subglottis is most common location – usually unilateral Tend to proliferate from birth – 1 yr then involute. Usually resolved by 5 yrs. www. childrensenthouston. com/images/laryngomal
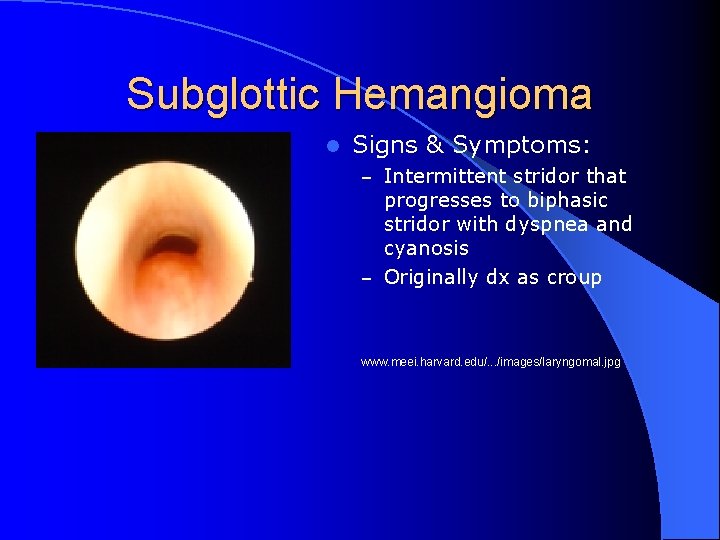
Subglottic Hemangioma l Signs & Symptoms: – Intermittent stridor that progresses to biphasic stridor with dyspnea and cyanosis – Originally dx as croup www. meei. harvard. edu/. . . /images/laryngomal. jpg
Subglottic Hemangioma l Treatment – Observe: if small – Tracheotomy until involution – Steroids – possible estrogen receptor involution – Laser therapy – good for hemostasis – Surgical excision – becoming more common because of stenosis from trach – Interferon – alfa-2 a has antiangiogenic activity when hemangioma in proliferate phase
Less Common Causes of Stridor l Dysphagia lusoria l Laryngeal cysts l Congenital laryngeal webs l Laryngeal foreign bodies l Respiratory papillomatosis
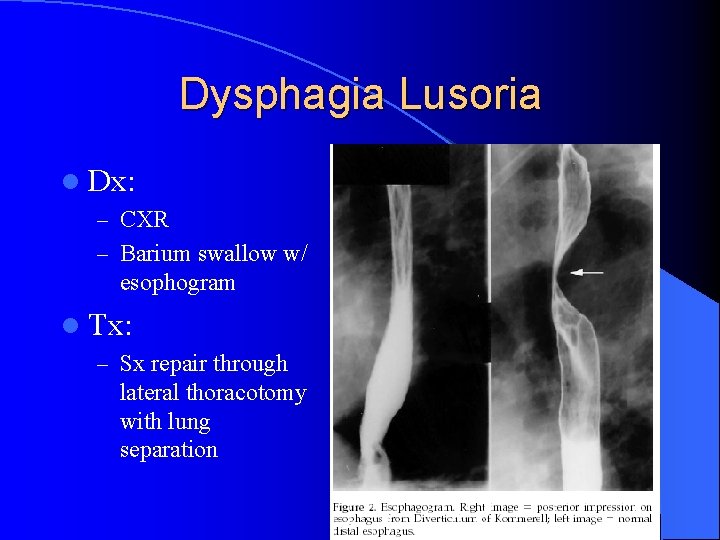
Dysphagia Lusoria “Dysphagia of unclear etiology” l Congenital anomalies of aortic arch: l – Double aortic arch – Anomalous origin of R or L subclavian artery – Kommerell’s Diverticulum – saccular aneurysmal dilation at of ARSA or ALSA – If LA or ductus present between subclavian and pulmonary complete vascular tracheobronchial ring l Presents as respiratory distress, dysphagia & stridor
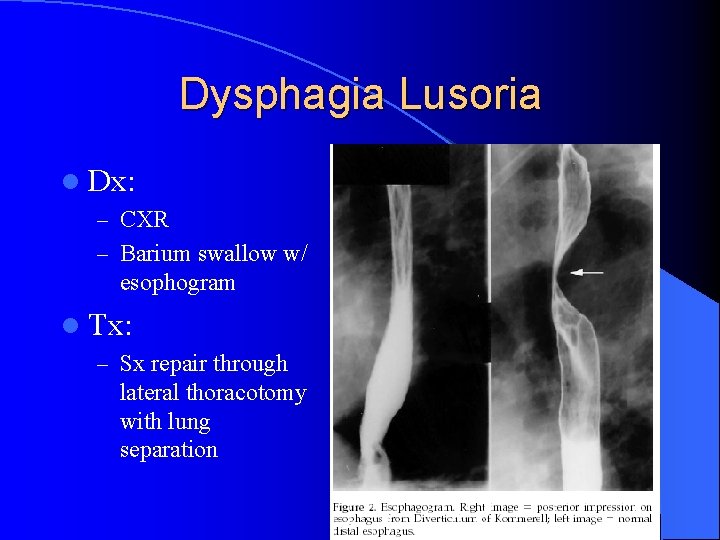
Dysphagia Lusoria l Dx: – CXR – Barium swallow w/ esophogram l Tx: – Sx repair through lateral thoracotomy with lung separation


Laryngeal Cysts 2, 4 l l l Rare cause of Stridor More superficial Fluid filled Ductal: MC, originate from obstruction of submucous gland Saccular: in laryngeal ventricles, usually congenital www. meei. harvard. edu/. . . /images/laryngo mal. jpg
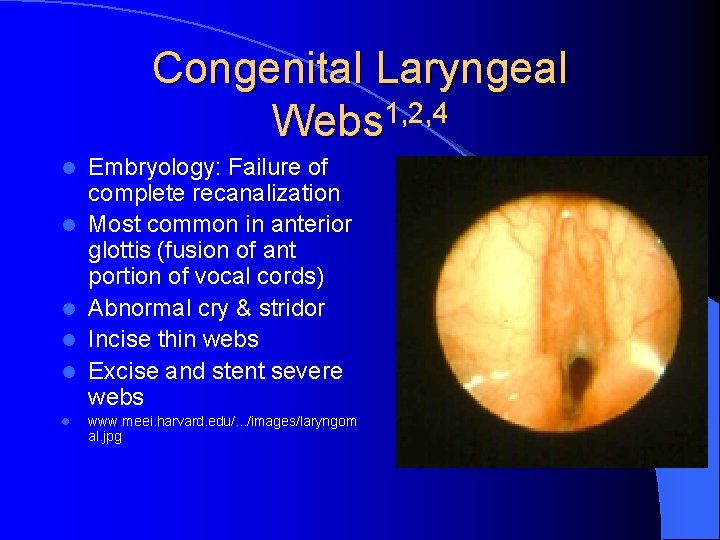
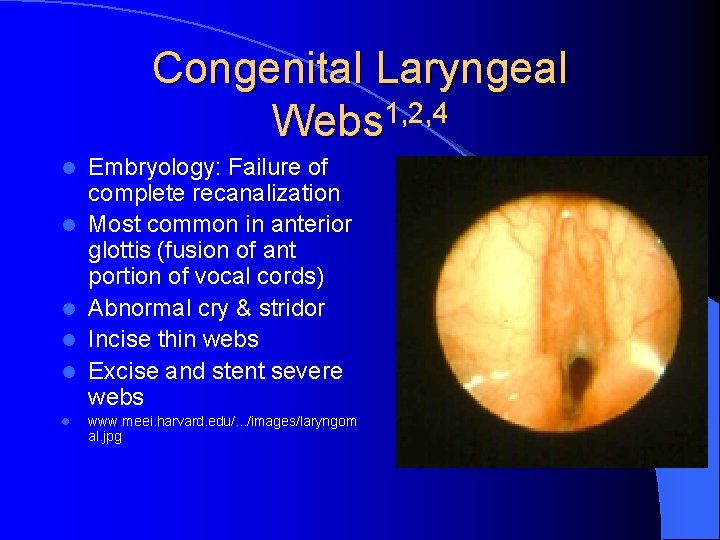
Congenital Laryngeal Webs 1, 2, 4 l l l Embryology: Failure of complete recanalization Most common in anterior glottis (fusion of ant portion of vocal cords) Abnormal cry & stridor Incise thin webs Excise and stent severe webs www. meei. harvard. edu/. . . /images/laryngom al. jpg

Laryngeal Foreign Bodies 4 l MC in kids 1 -3 yrs l Most inhaled objects pass through larynx and lodge distally l If lodged in larynx & partially obstructed – Stridor, hoarseness, and cough – Confirm w/X-ray – Remove in OR
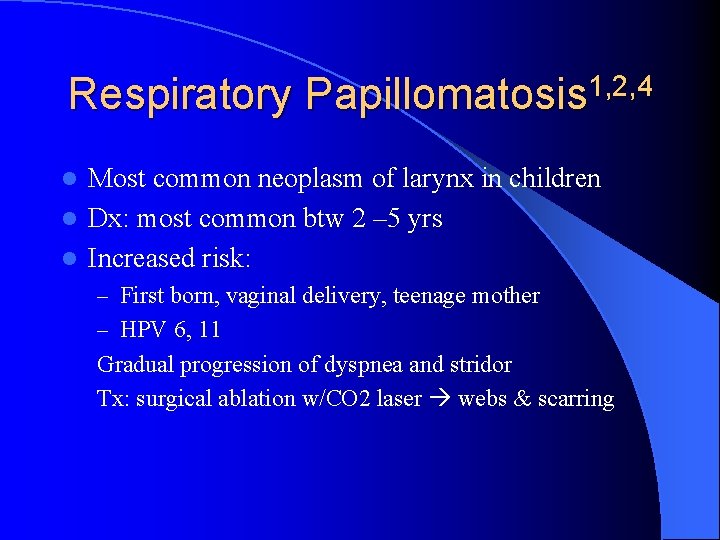
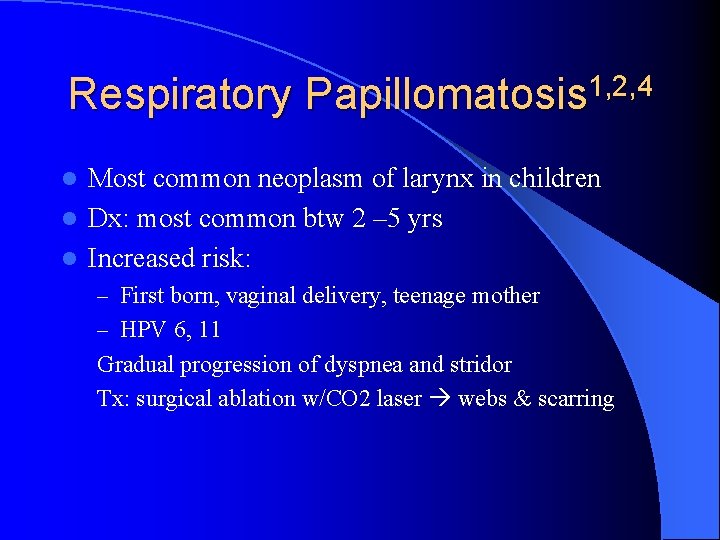
Respiratory Papillomatosis 1, 2, 4 Most common neoplasm of larynx in children l Dx: most common btw 2 – 5 yrs l Increased risk: l – First born, vaginal delivery, teenage mother – HPV 6, 11 Gradual progression of dyspnea and stridor Tx: surgical ablation w/CO 2 laser webs & scarring

References l l l l 1. Rowe, LD. Pediatric Airway Obstruction. Otolaryngology – Head and Neck Surgery. Current Surgery. Chap 38. 2. Kirby, GS. et al. Respiratory Tract and Mediastinum. Current Pediatrics. Chap 18. 3. Gormley, PK. et al. Congenital vascular anomalies and persistent respiratory symptoms in children. International Pediatric Journal of Otorhinolaryngology. Nov 1999: 51: 23 -31. 4. Lange, et al. Current Opinion in Otolaryngology and Head and Neck Surgery. Lippincott, Wilkins and Williams. Dec 1999. p 349. 5. Mossad, E. et al. Diverticulum of Kommerell: A review of a Series and a Report of a Case with Tracheal Deviation Compromising Single Lung Ventilation. Anesth Analog. 2002: 94: 1462 -4 6. Bent, J. Pediatric Laryngotracheal Obstruction: Current Perspectives on Stridor. Laryngoscope. 2006: 116: 1059 -1070 7. Sisk, EA. et al. Tracheotomy in Very Low Birth Weight Neonates: Indications and Outcomes. Laryngoscope. 2006: 116: 928 -933
 Paula stinson
Paula stinson Nathan stinson
Nathan stinson Barney stinson heidi klum
Barney stinson heidi klum Gina stinson
Gina stinson Hayley stinson
Hayley stinson Stridor croup
Stridor croup Croup cough youtube
Croup cough youtube Treatment for stridor
Treatment for stridor Infectious disease board review
Infectious disease board review Approach to stridor
Approach to stridor Dr andrew lipton
Dr andrew lipton Treatment for stridor
Treatment for stridor Steeple sign vs normal
Steeple sign vs normal Dependent intervention nursing
Dependent intervention nursing Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Objectives of nursing process
Objectives of nursing process Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Alarm signs of pud
Alarm signs of pud Differential diagnosis leukocoria
Differential diagnosis leukocoria Intrahepatic jaundice
Intrahepatic jaundice Differential diagnosis of articular syndrome
Differential diagnosis of articular syndrome Brainstem stroke syndromes
Brainstem stroke syndromes Nephrotic syndrome
Nephrotic syndrome Differential diagnosis of dysphagia
Differential diagnosis of dysphagia Differential diagnosis of otitis externa
Differential diagnosis of otitis externa Breast lump differential
Breast lump differential Dka differential diagnosis
Dka differential diagnosis Differential diagnosis red eye
Differential diagnosis red eye Lymphedema differential diagnosis
Lymphedema differential diagnosis Differential diagnosis for premature rupture of membranes
Differential diagnosis for premature rupture of membranes Anisocytosis
Anisocytosis Differential diagnosis for atopic dermatitis
Differential diagnosis for atopic dermatitis