Approach to stridor in a 6 year old


- Slides: 41
Approach to stridor in a 6 year old child Jacques le Roux 24/08/2012
APPROACH TO STRIDOR IN 6 YEAR OLD CHILD • Anatomy (upper airways) • General reminders • Etiology • Approach - Imaging options - Imaging findings
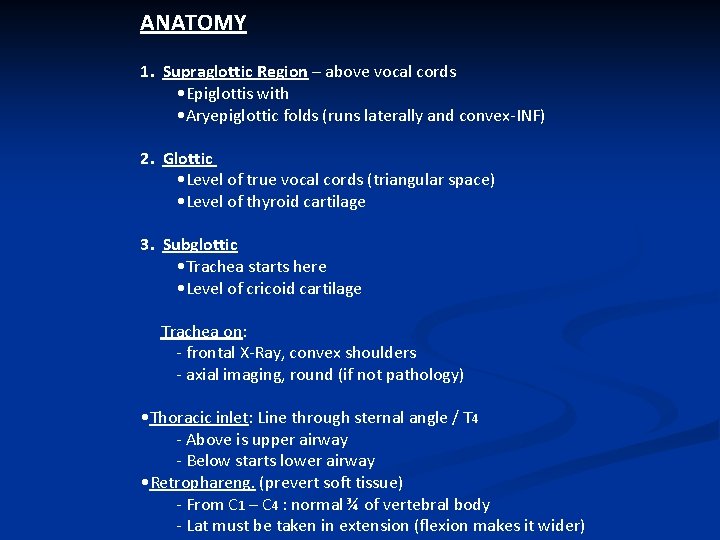
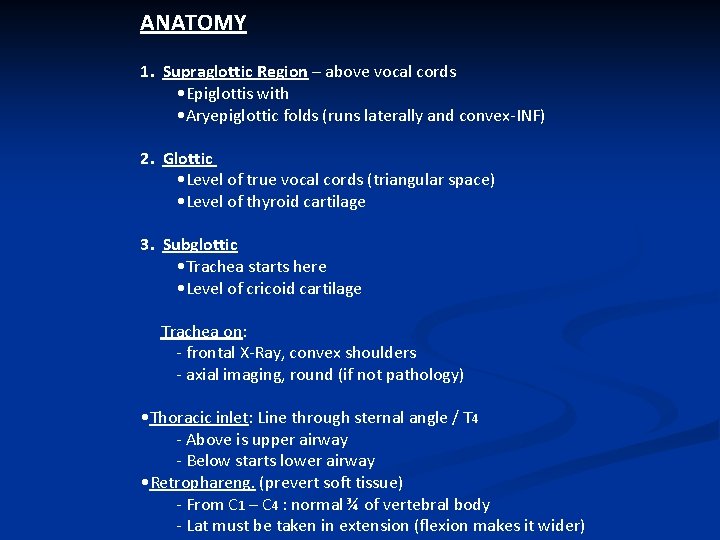
ANATOMY 1. Supraglottic Region – above vocal cords • Epiglottis with • Aryepiglottic folds (runs laterally and convex-INF) 2. Glottic • Level of true vocal cords (triangular space) • Level of thyroid cartilage 3. Subglottic • Trachea starts here • Level of cricoid cartilage Trachea on: - frontal X-Ray, convex shoulders - axial imaging, round (if not pathology) • Thoracic inlet: Line through sternal angle / T 4 - Above is upper airway - Below starts lower airway • Retrophareng. (prevert soft tissue) - From C 1 – C 4 : normal ¾ of vertebral body - Lat must be taken in extension (flexion makes it wider)
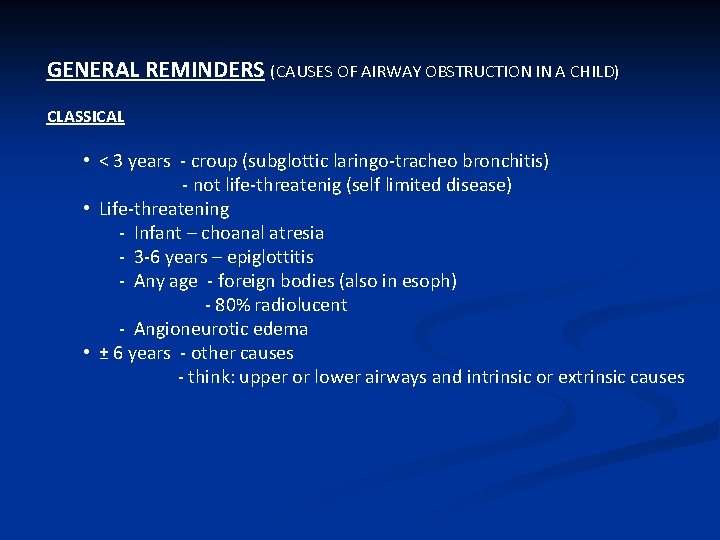
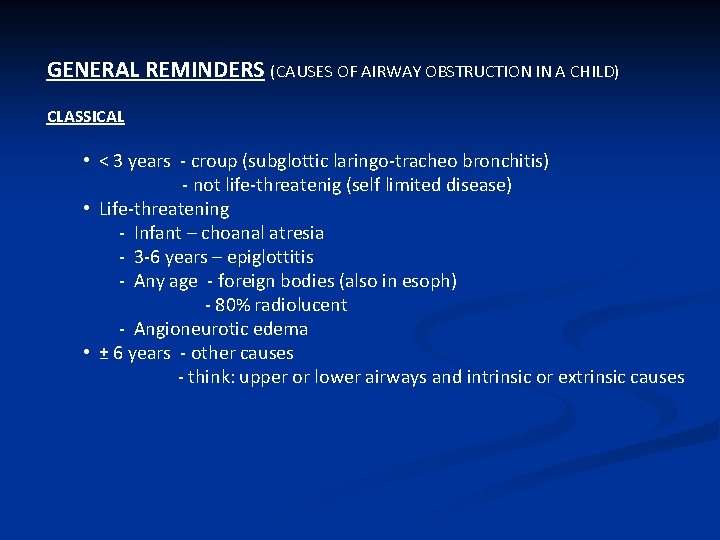
GENERAL REMINDERS (CAUSES OF AIRWAY OBSTRUCTION IN A CHILD) CLASSICAL • < 3 years - croup (subglottic laringo-tracheo bronchitis) - not life-threatenig (self limited disease) • Life-threatening - Infant – choanal atresia - 3 -6 years – epiglottitis - Any age - foreign bodies (also in esoph) - 80% radiolucent - Angioneurotic edema • ± 6 years - other causes - think: upper or lower airways and intrinsic or extrinsic causes
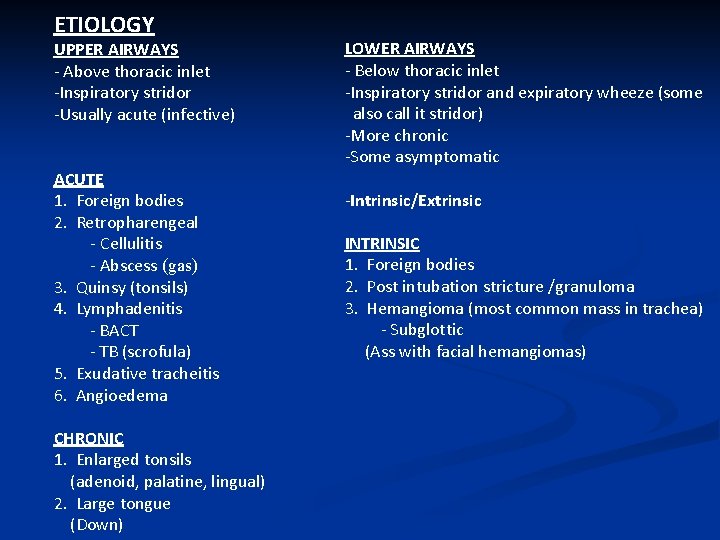
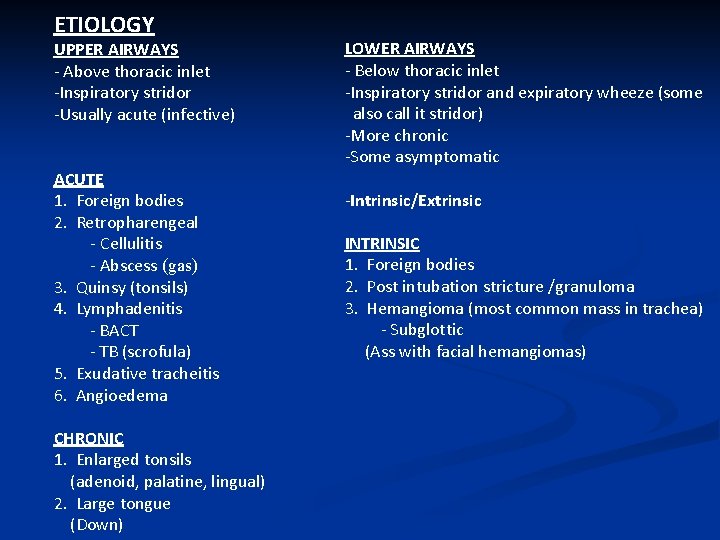
ETIOLOGY UPPER AIRWAYS - Above thoracic inlet -Inspiratory stridor -Usually acute (infective) ACUTE 1. Foreign bodies 2. Retropharengeal - Cellulitis - Abscess (gas) 3. Quinsy (tonsils) 4. Lymphadenitis - BACT - TB (scrofula) 5. Exudative tracheitis 6. Angioedema CHRONIC 1. Enlarged tonsils (adenoid, palatine, lingual) 2. Large tongue (Down) LOWER AIRWAYS - Below thoracic inlet -Inspiratory stridor and expiratory wheeze (some also call it stridor) -More chronic -Some asymptomatic -Intrinsic/Extrinsic INTRINSIC 1. Foreign bodies 2. Post intubation stricture /granuloma 3. Hemangioma (most common mass in trachea) - Subglottic (Ass with facial hemangiomas)
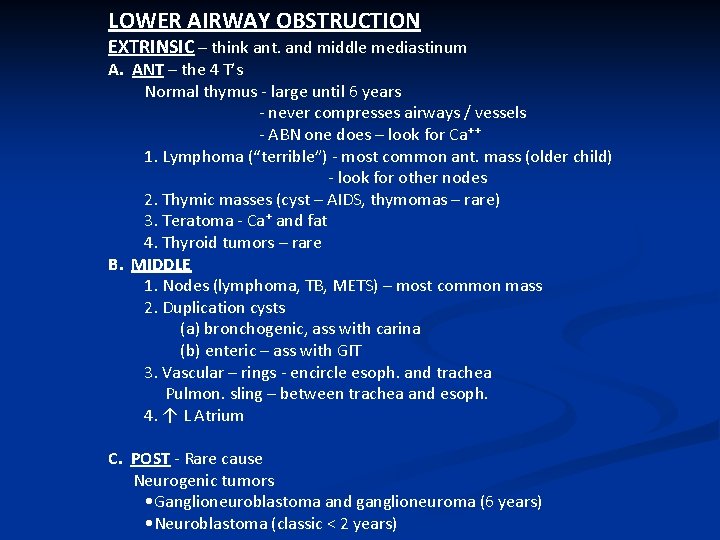
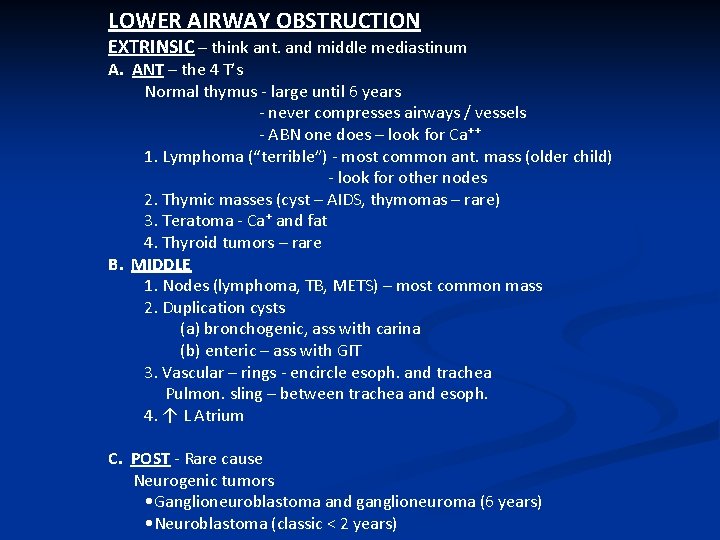
LOWER AIRWAY OBSTRUCTION EXTRINSIC – think ant. and middle mediastinum A. ANT – the 4 T’s Normal thymus - large until 6 years - never compresses airways / vessels - ABN one does – look for Ca⁺⁺ 1. Lymphoma (“terrible”) - most common ant. mass (older child) - look for other nodes 2. Thymic masses (cyst – AIDS, thymomas – rare) 3. Teratoma - Ca⁺ and fat 4. Thyroid tumors – rare B. MIDDLE 1. Nodes (lymphoma, TB, METS) – most common mass 2. Duplication cysts (a) bronchogenic, ass with carina (b) enteric – ass with GIT 3. Vascular – rings - encircle esoph. and trachea Pulmon. sling – between trachea and esoph. 4. ↑ L Atrium C. POST - Rare cause Neurogenic tumors • Ganglioneuroblastoma and ganglioneuroma (6 years) • Neuroblastoma (classic < 2 years)
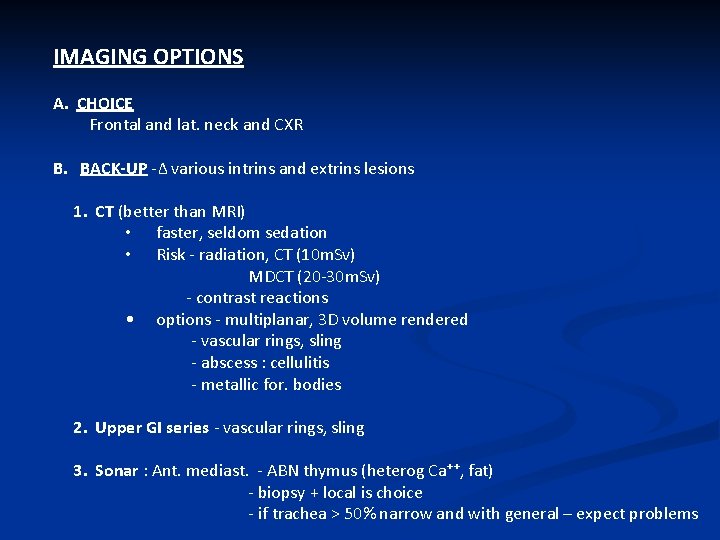
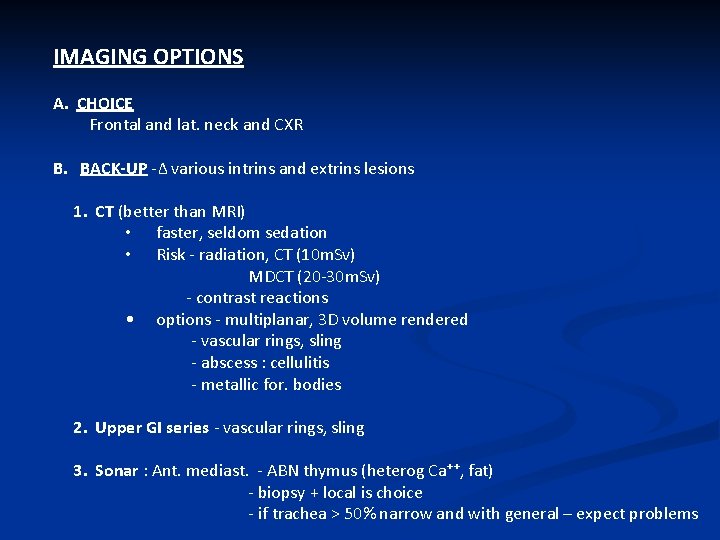
IMAGING OPTIONS A. CHOICE Frontal and lat. neck and CXR B. BACK-UP -Δ various intrins and extrins lesions 1. CT (better than MRI) • faster, seldom sedation • Risk - radiation, CT (10 m. Sv) MDCT (20 -30 m. Sv) - contrast reactions • options - multiplanar, 3 D volume rendered - vascular rings, sling - abscess : cellulitis - metallic for. bodies 2. Upper GI series - vascular rings, sling 3. Sonar : Ant. mediast. - ABN thymus (heterog Ca⁺⁺, fat) - biopsy + local is choice - if trachea > 50% narrow and with general – expect problems
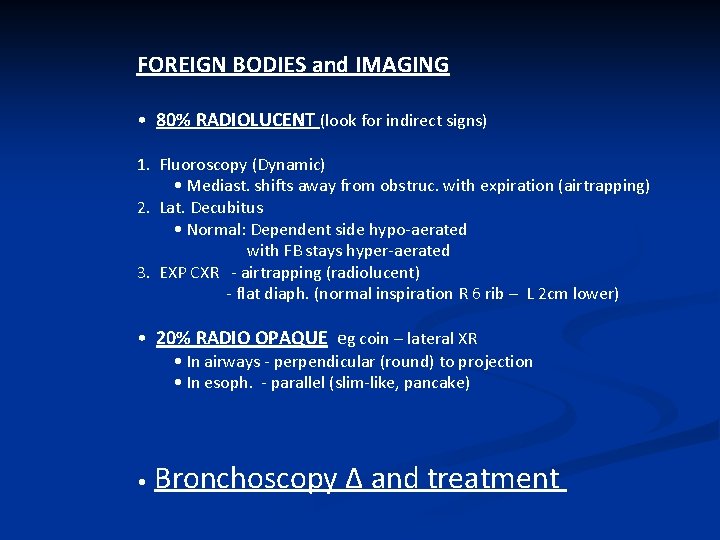
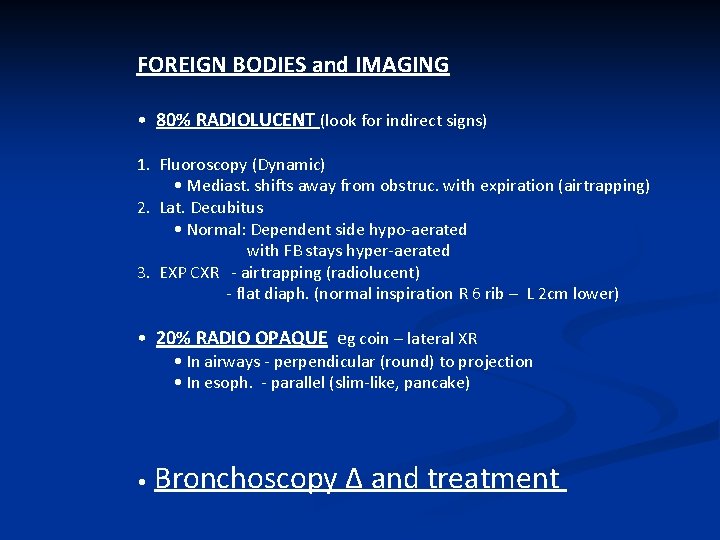
FOREIGN BODIES and IMAGING • 80% RADIOLUCENT (look for indirect signs) 1. Fluoroscopy (Dynamic) • Mediast. shifts away from obstruc. with expiration (airtrapping) 2. Lat. Decubitus • Normal: Dependent side hypo-aerated with FB stays hyper-aerated 3. EXP CXR - airtrapping (radiolucent) - flat diaph. (normal inspiration R 6 rib – L 2 cm lower) • 20% RADIO OPAQUE eg coin – lateral XR • In airways - perpendicular (round) to projection • In esoph. - parallel (slim-like, pancake) • Bronchoscopy Δ and treatment
IMAGING FINDINGS UPPER AIRWAYS – ACUTE/CHRONIC
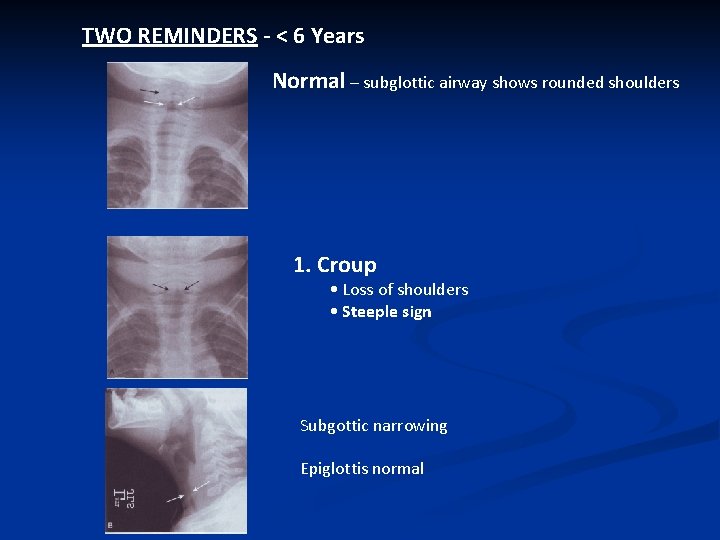
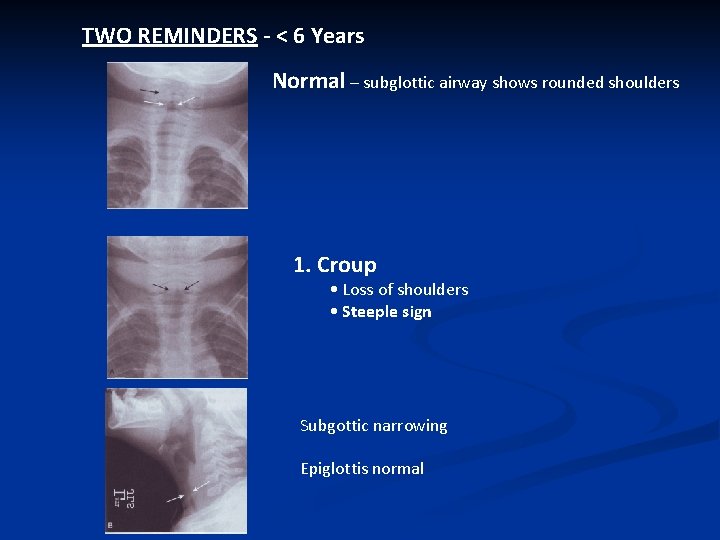
TWO REMINDERS - < 6 Years Normal – subglottic airway shows rounded shoulders 1. Croup • Loss of shoulders • Steeple sign Subgottic narrowing Epiglottis normal
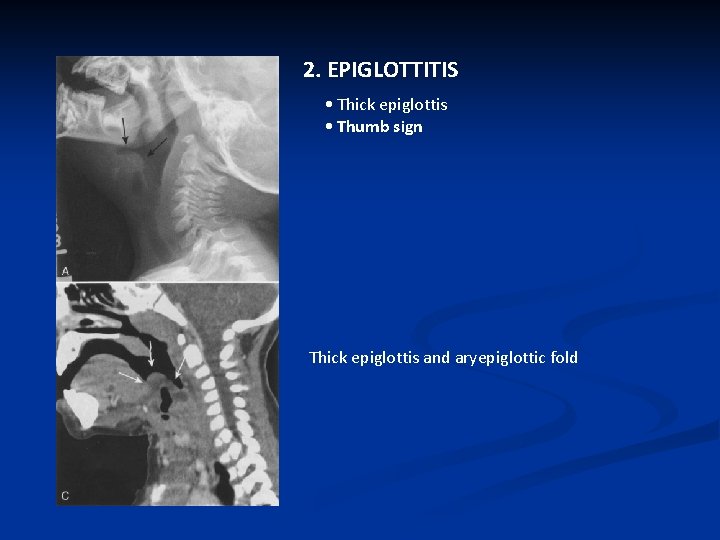
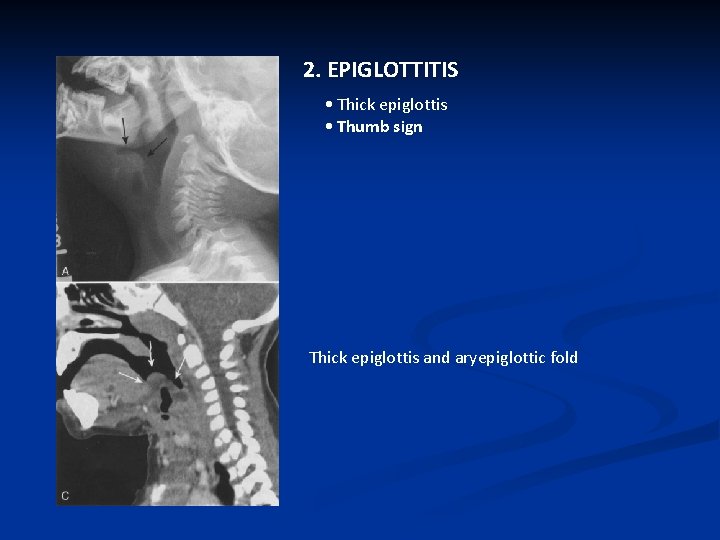
2. EPIGLOTTITIS • Thick epiglottis • Thumb sign Thick epiglottis and aryepiglottic fold
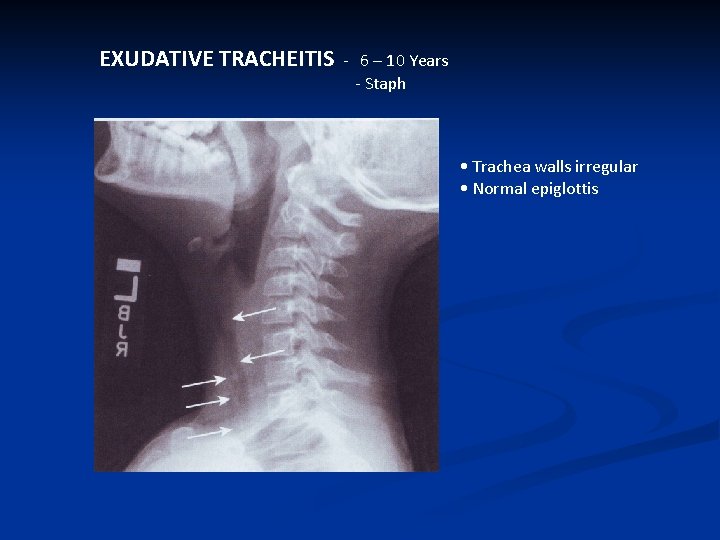
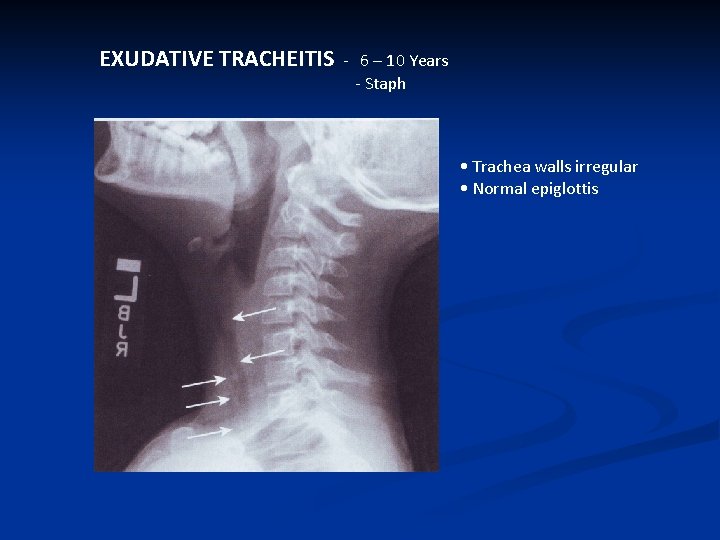
EXUDATIVE TRACHEITIS - 6 – 10 Years - Staph • Trachea walls irregular • Normal epiglottis
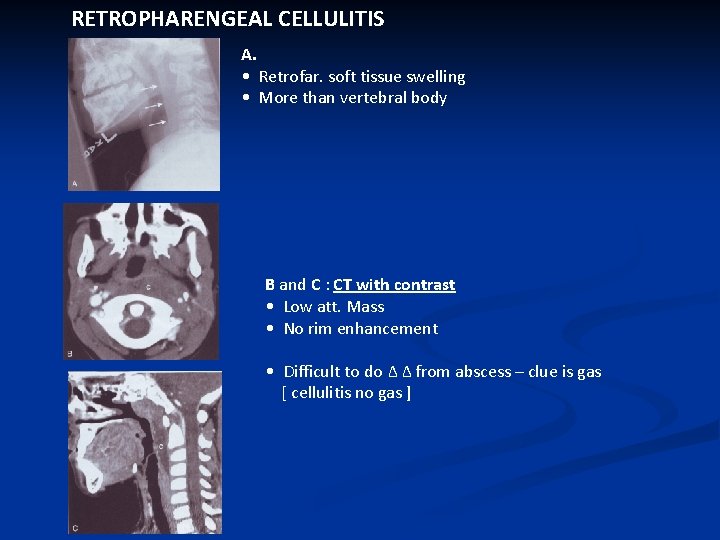
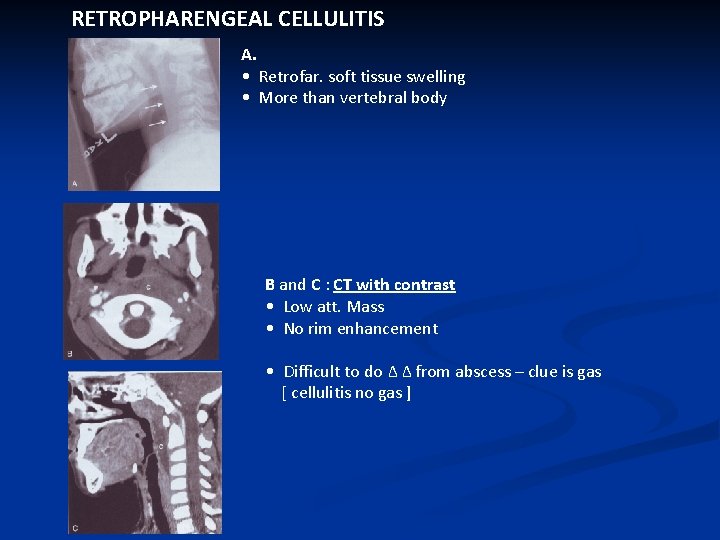
RETROPHARENGEAL CELLULITIS A. • Retrofar. soft tissue swelling • More than vertebral body B and C : CT with contrast • Low att. Mass • No rim enhancement • Difficult to do Δ Δ from abscess – clue is gas [ cellulitis no gas ]
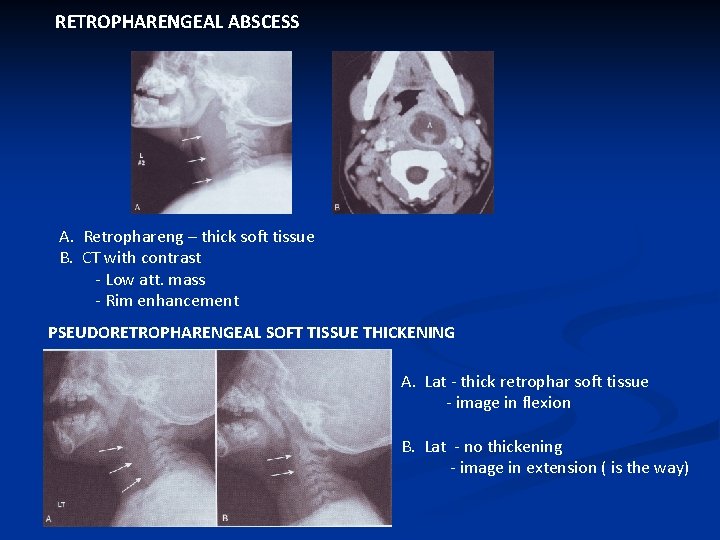
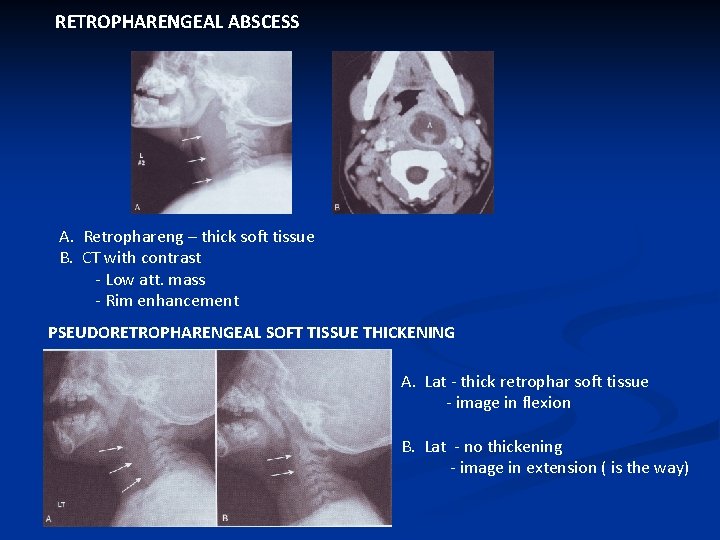
RETROPHARENGEAL ABSCESS A. Retrophareng – thick soft tissue B. CT with contrast - Low att. mass - Rim enhancement PSEUDORETROPHARENGEAL SOFT TISSUE THICKENING A. Lat - thick retrophar soft tissue - image in flexion B. Lat - no thickening - image in extension ( is the way)
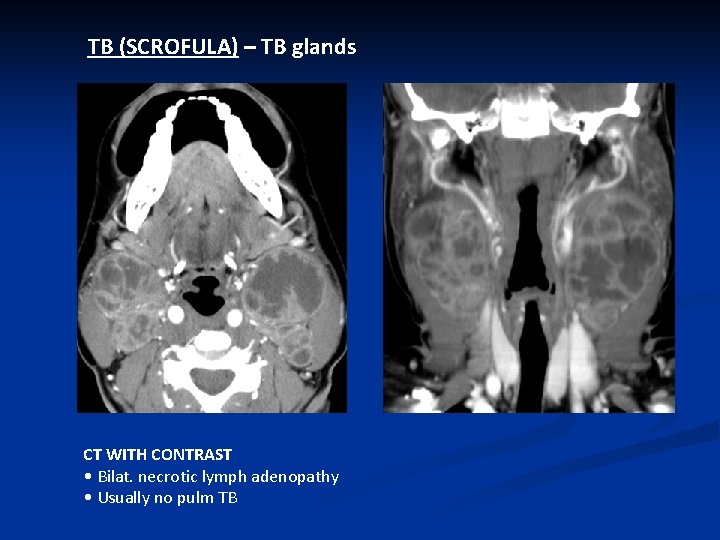
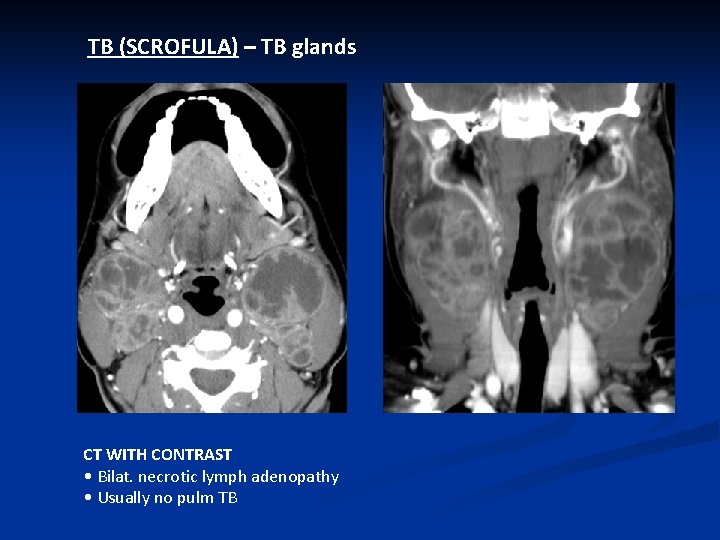
TB (SCROFULA) – TB glands CT WITH CONTRAST • Bilat. necrotic lymph adenopathy • Usually no pulm TB
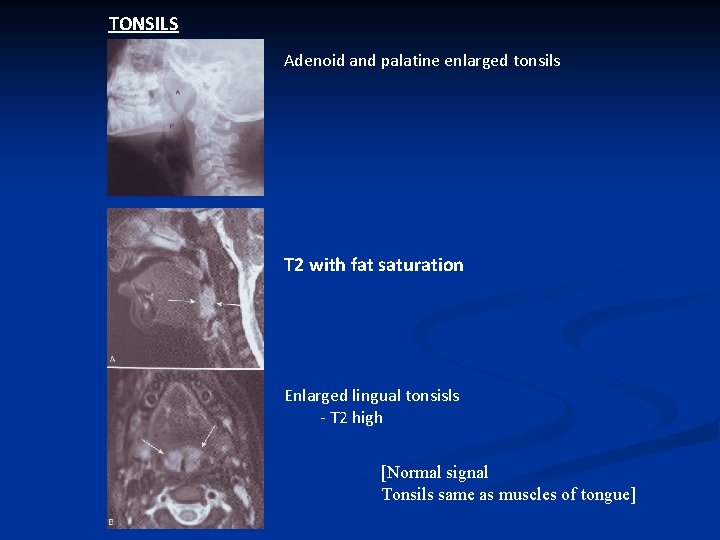
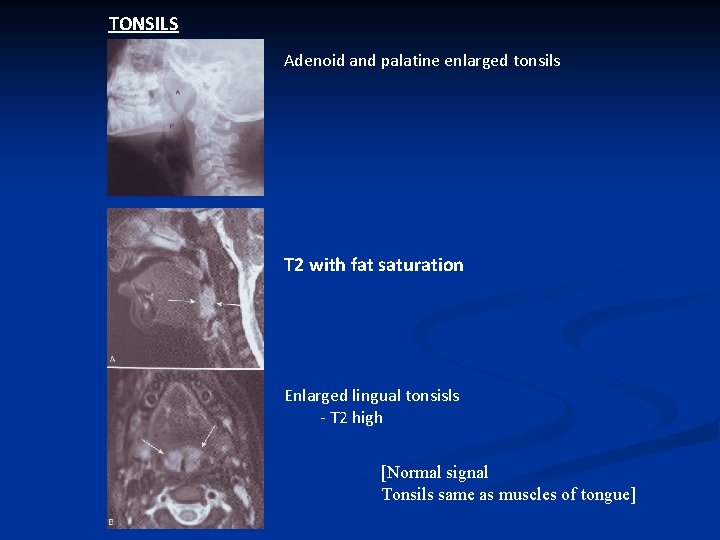
TONSILS Adenoid and palatine enlarged tonsils T 2 with fat saturation Enlarged lingual tonsisls - T 2 high [Normal signal Tonsils same as muscles of tongue]
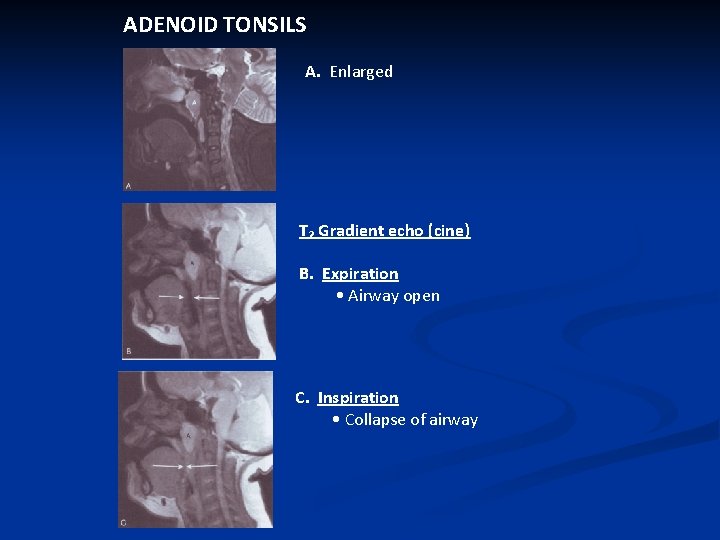
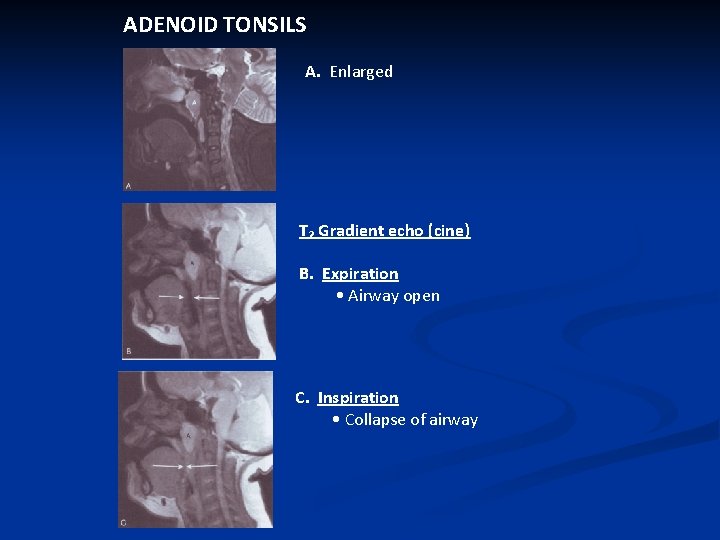
ADENOID TONSILS A. Enlarged T₂ Gradient echo (cine) B. Expiration • Airway open C. Inspiration • Collapse of airway
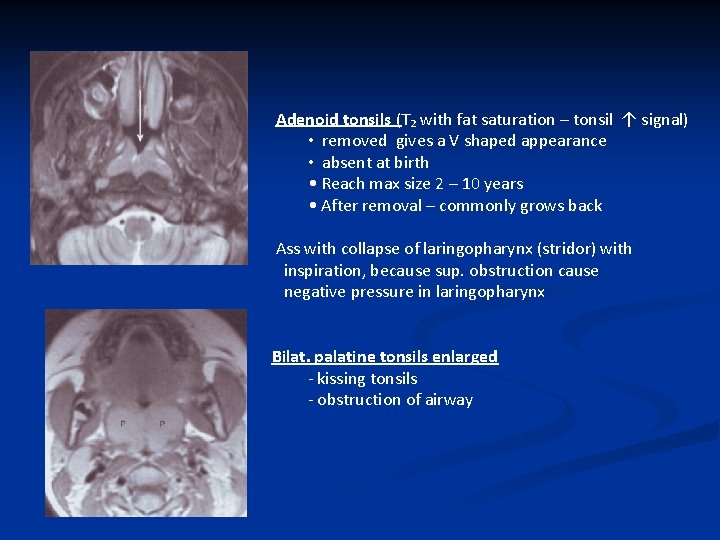
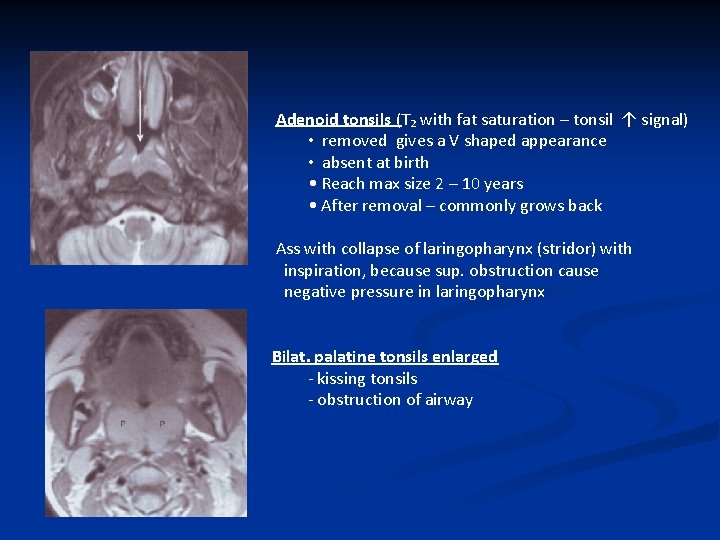
Adenoid tonsils (T₂ with fat saturation – tonsil ↑ signal) • removed gives a V shaped appearance • absent at birth • Reach max size 2 – 10 years • After removal – commonly grows back Ass with collapse of laringopharynx (stridor) with inspiration, because sup. obstruction cause negative pressure in laringopharynx Bilat. palatine tonsils enlarged - kissing tonsils - obstruction of airway
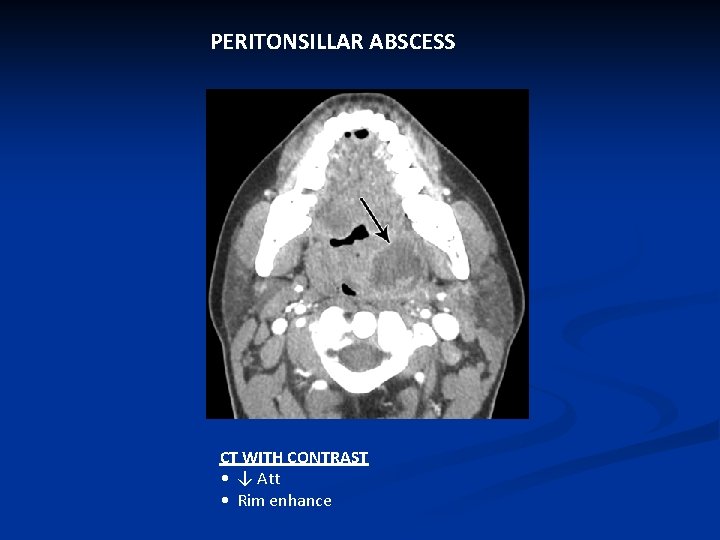
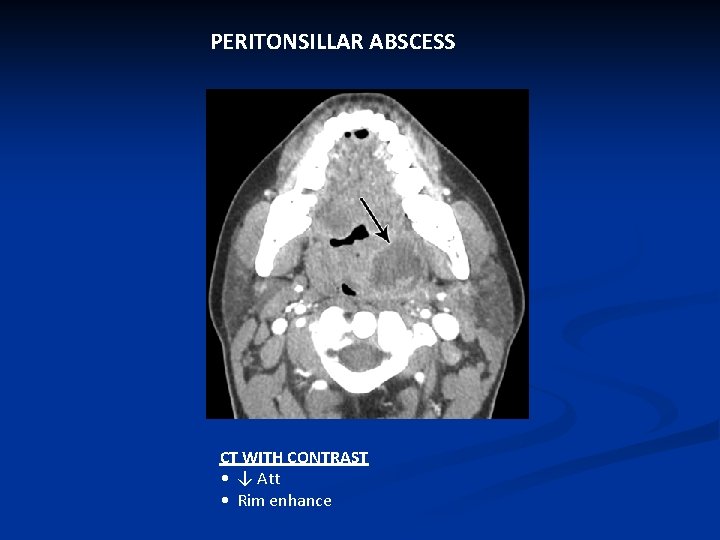
PERITONSILLAR ABSCESS CT WITH CONTRAST • ↓ Att • Rim enhance
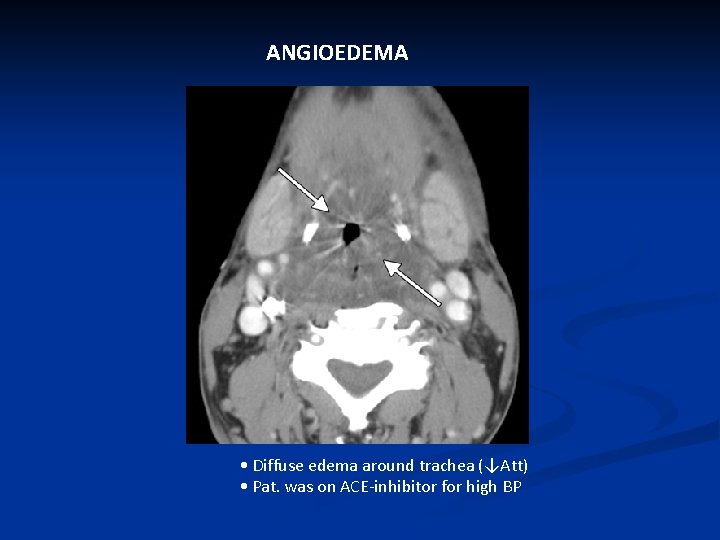
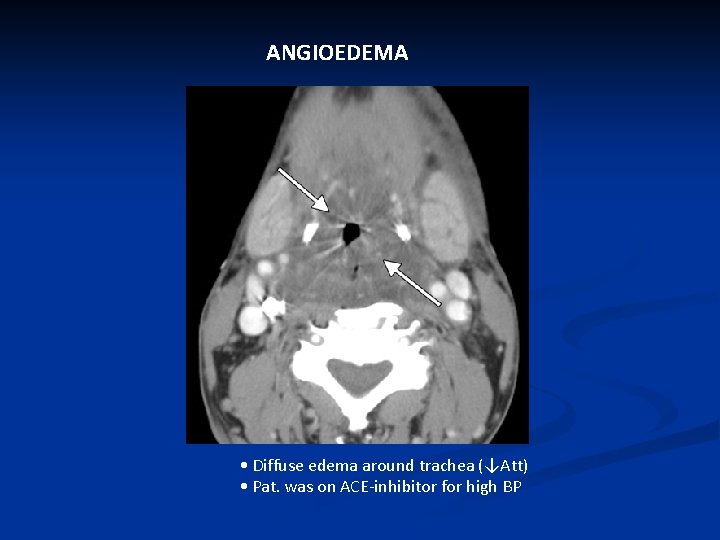
ANGIOEDEMA • Diffuse edema around trachea (↓Att) • Pat. was on ACE-inhibitor for high BP

GLOSSOPTOSIS – eg Down Obstruction of airway
LOWER AIRWAYS EXTRINSIC
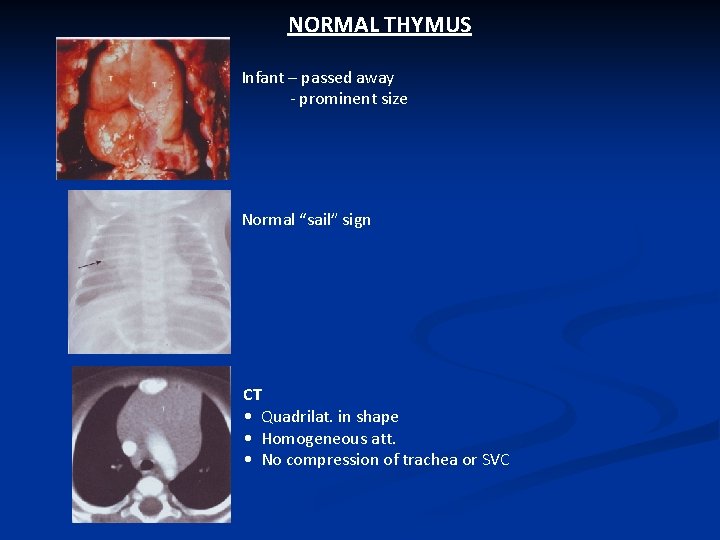
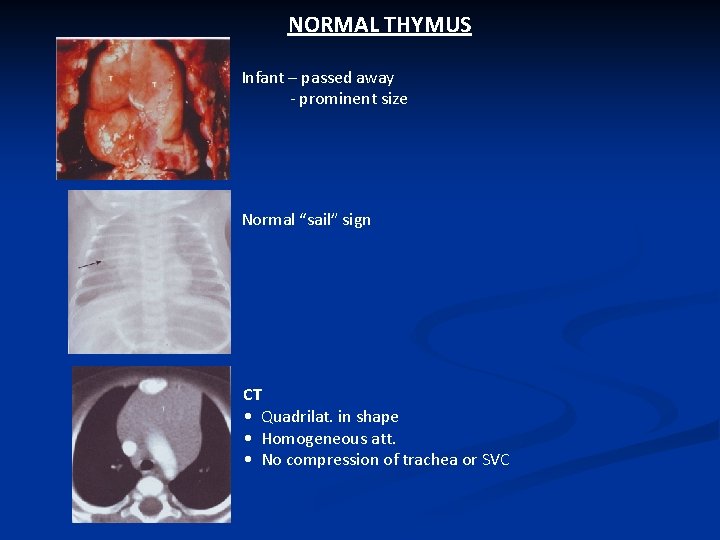
NORMAL THYMUS Infant – passed away - prominent size Normal “sail” sign CT • Quadrilat. in shape • Homogeneous att. • No compression of trachea or SVC
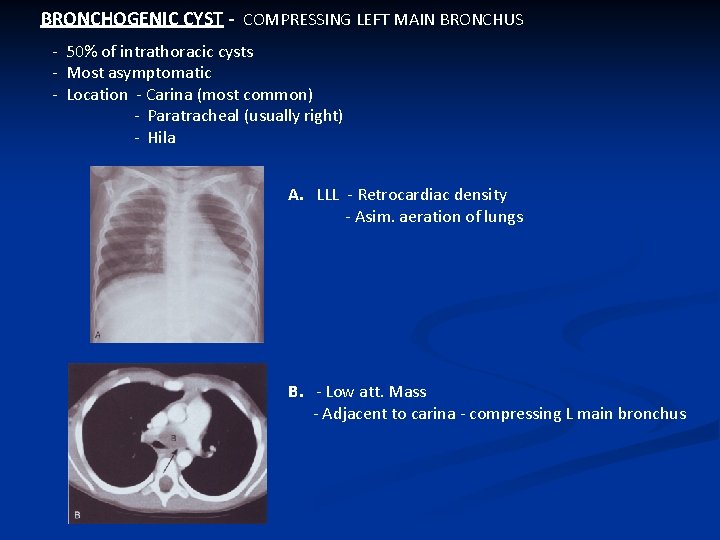
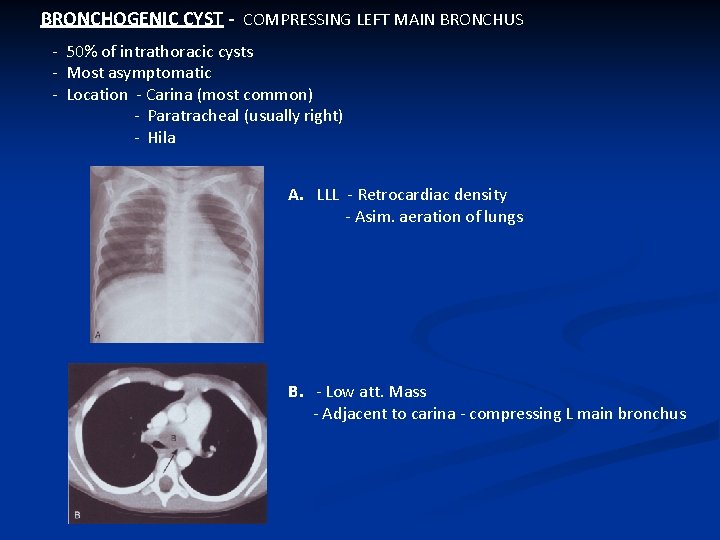
BRONCHOGENIC CYST - COMPRESSING LEFT MAIN BRONCHUS - 50% of intrathoracic cysts - Most asymptomatic - Location - Carina (most common) - Paratracheal (usually right) - Hila A. LLL - Retrocardiac density - Asim. aeration of lungs B. - Low att. Mass - Adjacent to carina - compressing L main bronchus
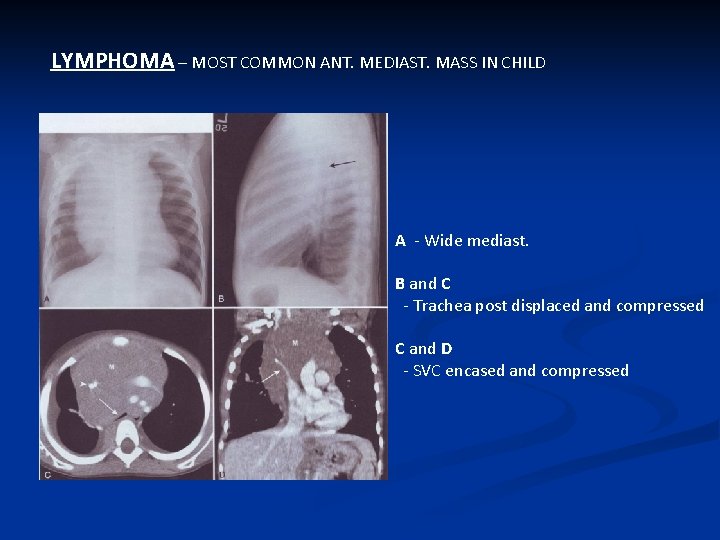
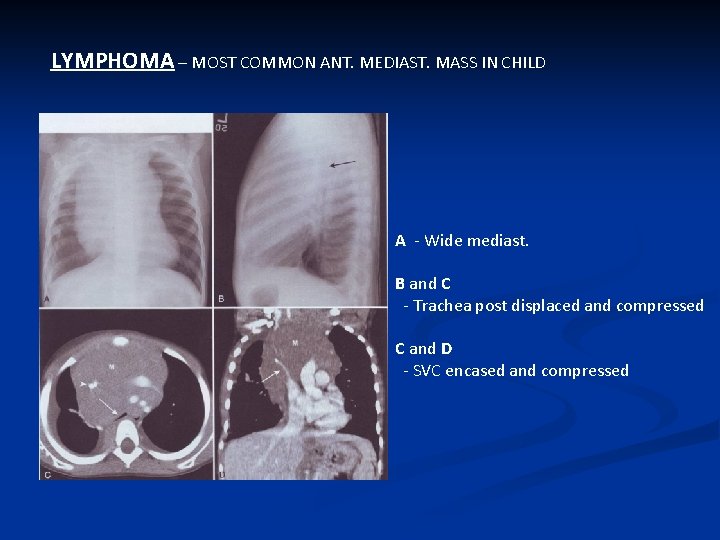
LYMPHOMA – MOST COMMON ANT. MEDIAST. MASS IN CHILD A - Wide mediast. B and C - Trachea post displaced and compressed C and D - SVC encased and compressed
VASCULAR RINGS/SLING • Some not found in 6 years • Some will not compress airways
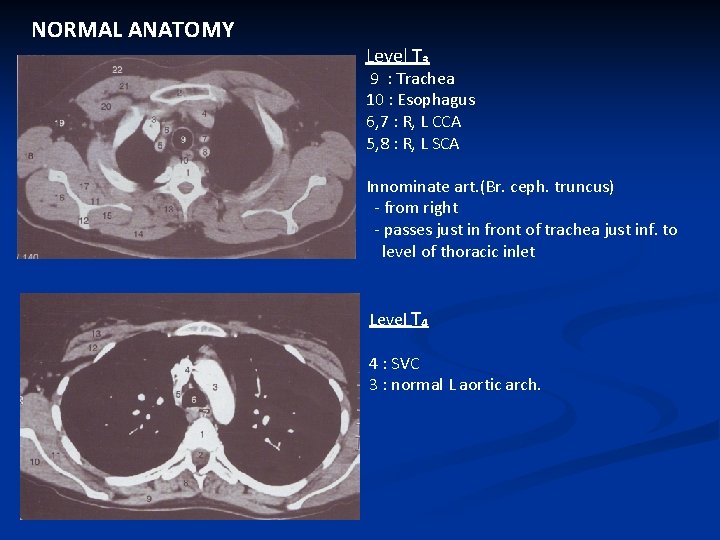
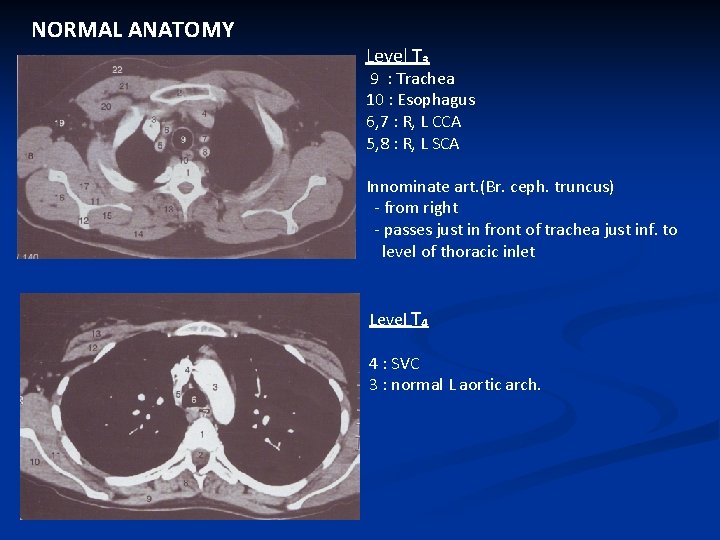
NORMAL ANATOMY Level T₃ 9 : Trachea 10 : Esophagus 6, 7 : R, L CCA 5, 8 : R, L SCA Innominate art. (Br. ceph. truncus) - from right - passes just in front of trachea just inf. to level of thoracic inlet Level T₄ 4 : SVC 3 : normal L aortic arch.
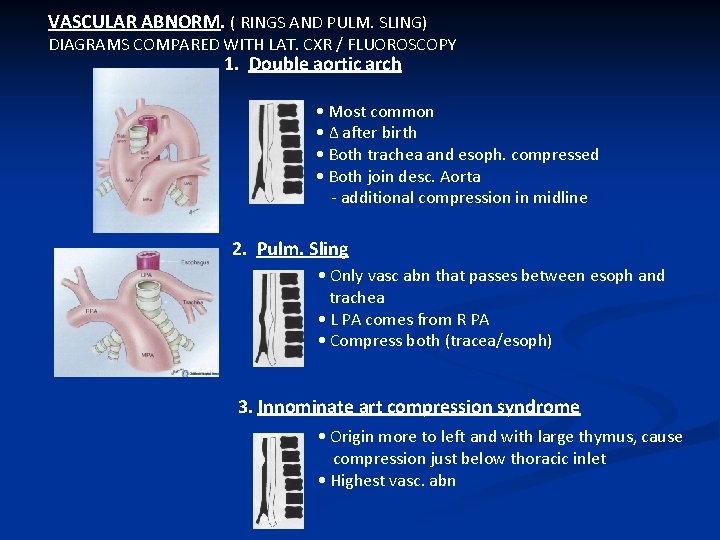
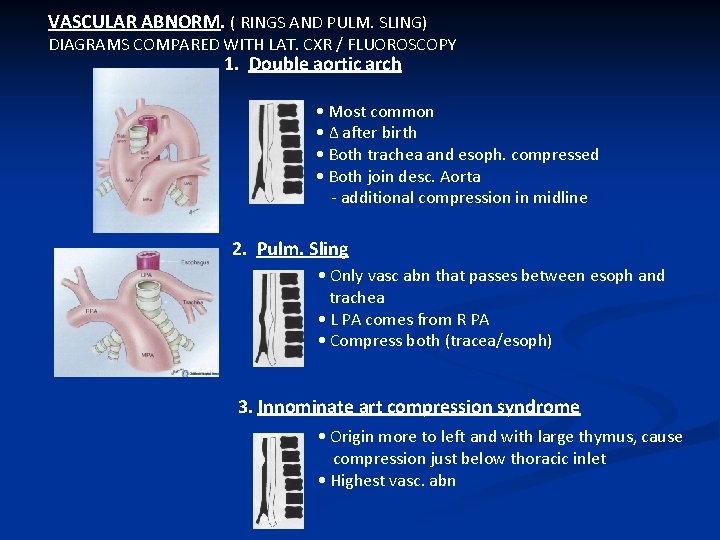
VASCULAR ABNORM. ( RINGS AND PULM. SLING) DIAGRAMS COMPARED WITH LAT. CXR / FLUOROSCOPY 1. Double aortic arch • Most common • Δ after birth • Both trachea and esoph. compressed • Both join desc. Aorta - additional compression in midline 2. Pulm. Sling • Only vasc abn that passes between esoph and trachea • L PA comes from R PA • Compress both (tracea/esoph) 3. Innominate art compression syndrome • Origin more to left and with large thymus, cause compression just below thoracic inlet • Highest vasc. abn
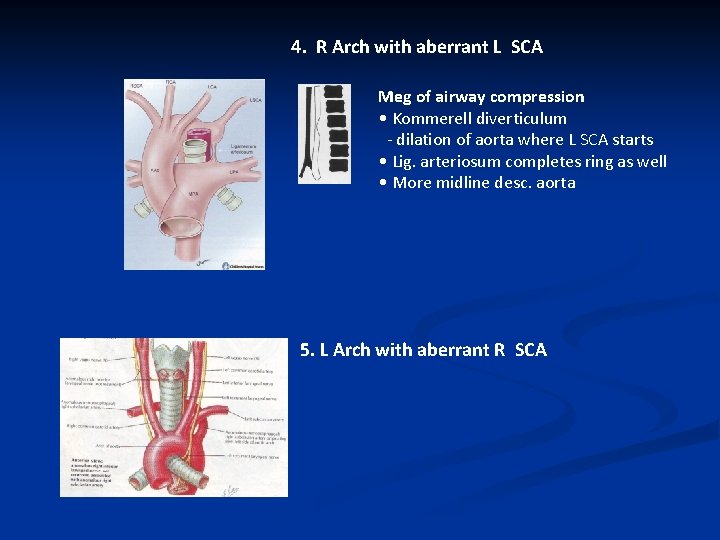
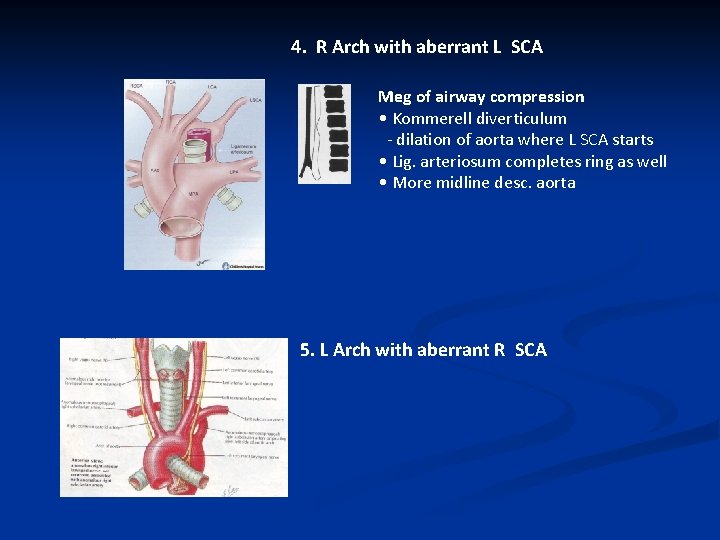
4. R Arch with aberrant L SCA Meg of airway compression • Kommerell diverticulum - dilation of aorta where L SCA starts • Lig. arteriosum completes ring as well • More midline desc. aorta 5. L Arch with aberrant R SCA
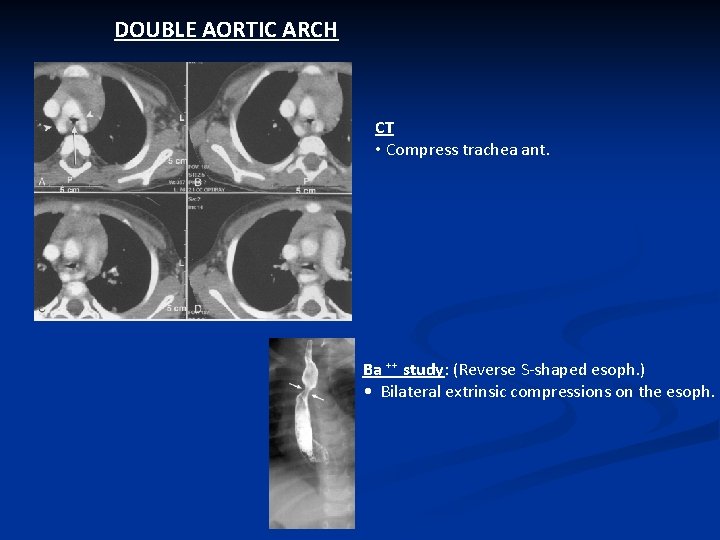
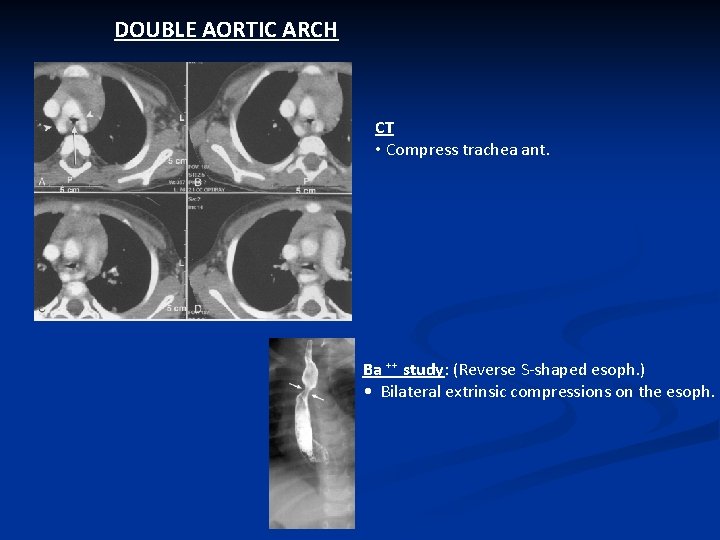
DOUBLE AORTIC ARCH CT • Compress trachea ant. Ba ⁺⁺ study: (Reverse S-shaped esoph. ) • Bilateral extrinsic compressions on the esoph.
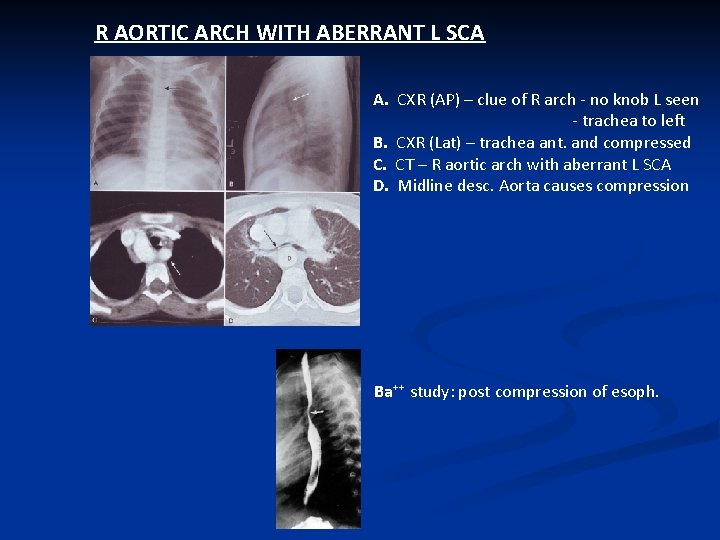
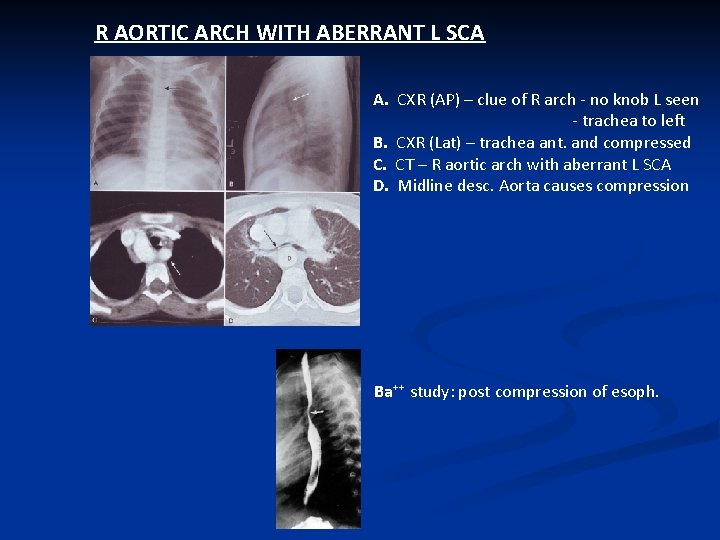
R AORTIC ARCH WITH ABERRANT L SCA A. CXR (AP) – clue of R arch - no knob L seen - trachea to left B. CXR (Lat) – trachea ant. and compressed C. CT – R aortic arch with aberrant L SCA D. Midline desc. Aorta causes compression Ba⁺⁺ study: post compression of esoph.
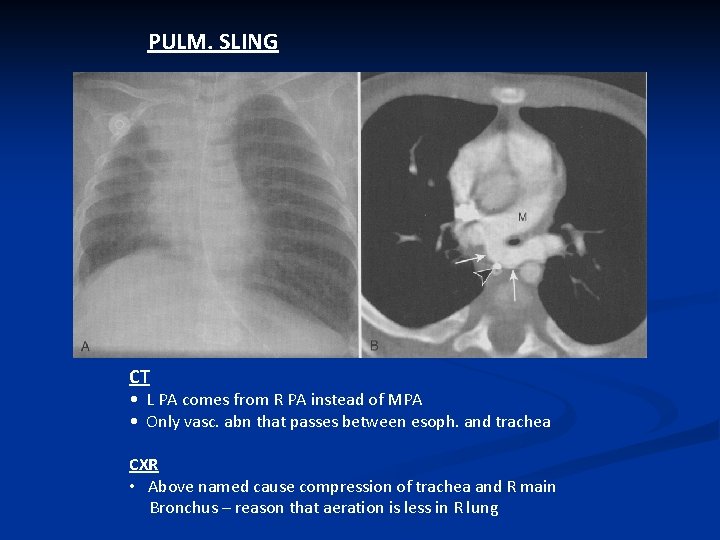
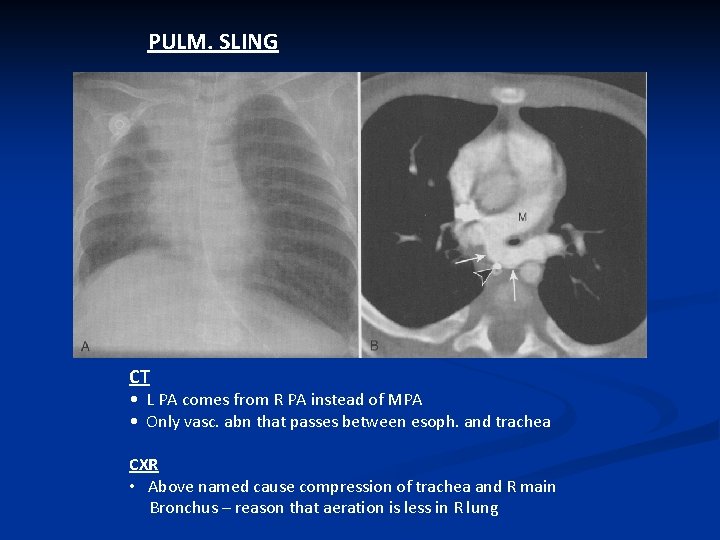
PULM. SLING CT • L PA comes from R PA instead of MPA • Only vasc. abn that passes between esoph. and trachea CXR • Above named cause compression of trachea and R main Bronchus – reason that aeration is less in R lung
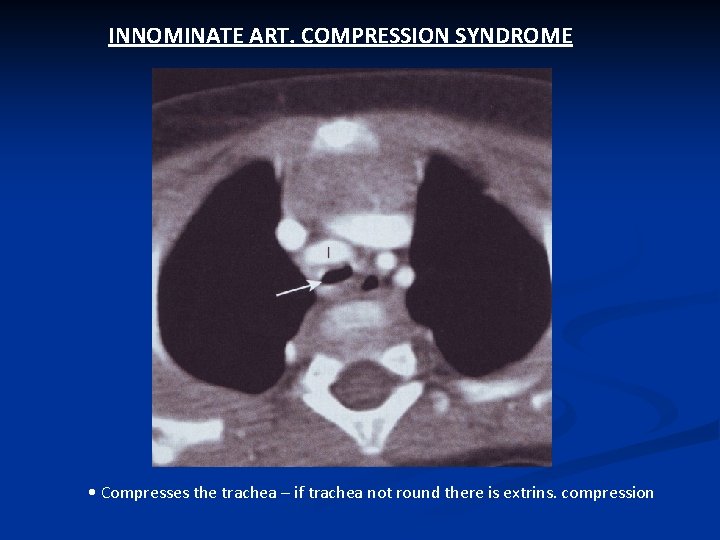
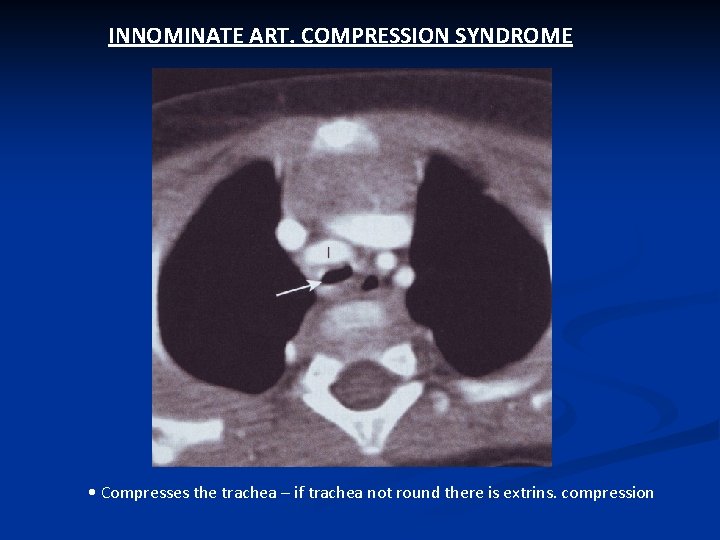
INNOMINATE ART. COMPRESSION SYNDROME • Compresses the trachea – if trachea not round there is extrins. compression
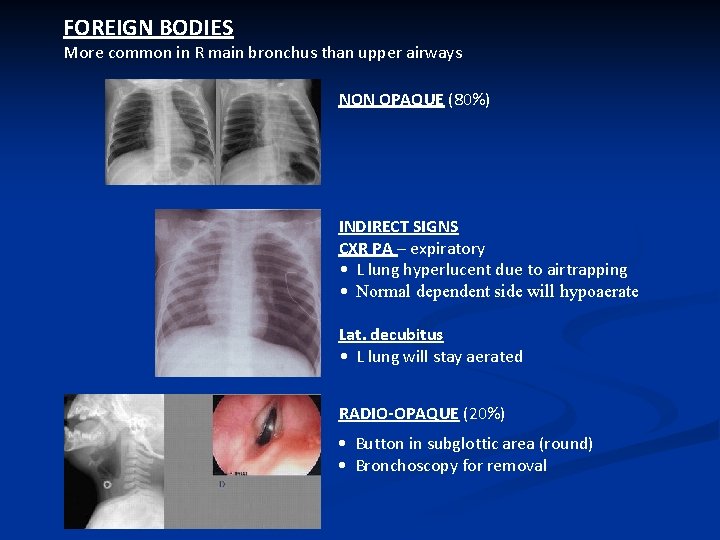
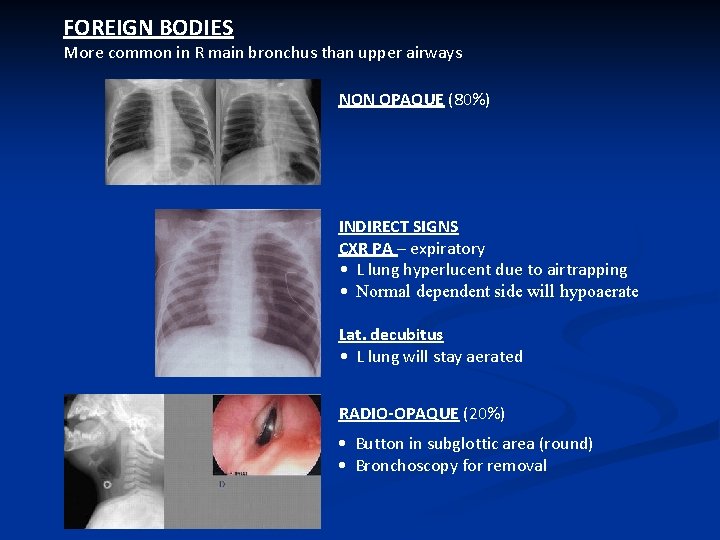
FOREIGN BODIES More common in R main bronchus than upper airways NON OPAQUE (80%) INDIRECT SIGNS CXR PA – expiratory • L lung hyperlucent due to airtrapping • Normal dependent side will hypoaerate Lat. decubitus • L lung will stay aerated RADIO-OPAQUE (20%) • Button in subglottic area (round) • Bronchoscopy for removal
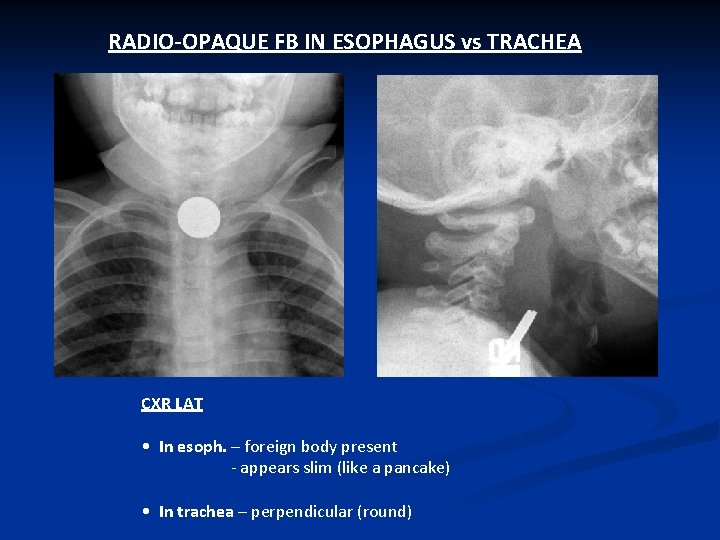
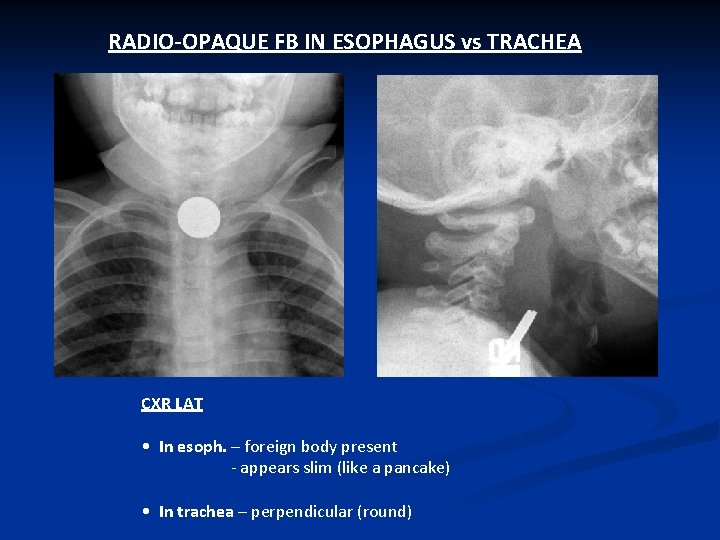
RADIO-OPAQUE FB IN ESOPHAGUS vs TRACHEA CXR LAT • In esoph. – foreign body present - appears slim (like a pancake) • In trachea – perpendicular (round)

POST INTUBATION STRICTURE AND GRANULOMA
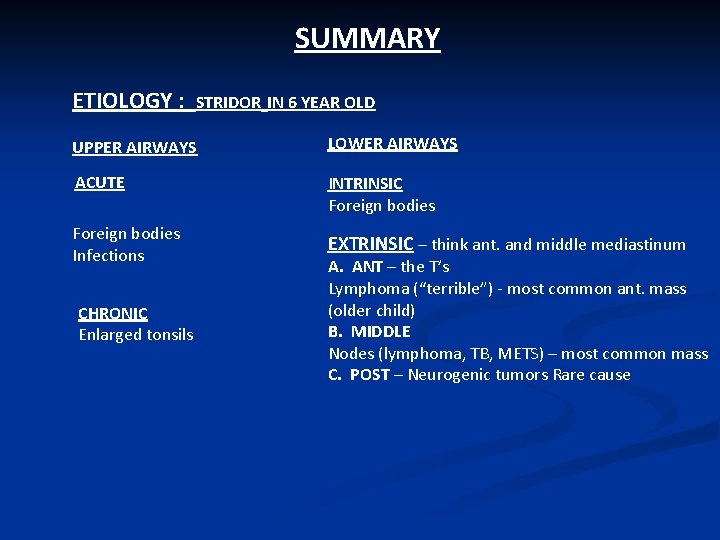
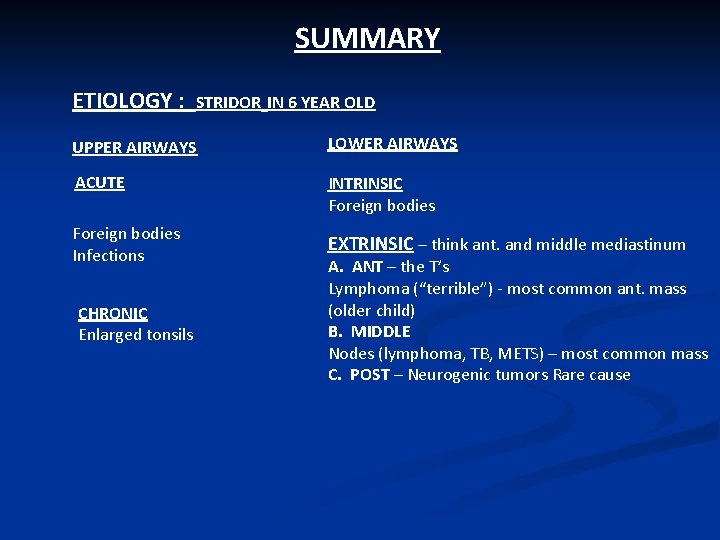
SUMMARY ETIOLOGY : STRIDOR IN 6 YEAR OLD UPPER AIRWAYS LOWER AIRWAYS ACUTE INTRINSIC Foreign bodies Infections EXTRINSIC – think ant. and middle mediastinum CHRONIC Enlarged tonsils A. ANT – the T’s Lymphoma (“terrible”) - most common ant. mass (older child) B. MIDDLE Nodes (lymphoma, TB, METS) – most common mass C. POST – Neurogenic tumors Rare cause
It has been said that one of the differentiating features between a pediatric and a general radiologist is that a pediatric radiologist remembers to look at the airway. Problems with the airway are much more common in children than in adults.
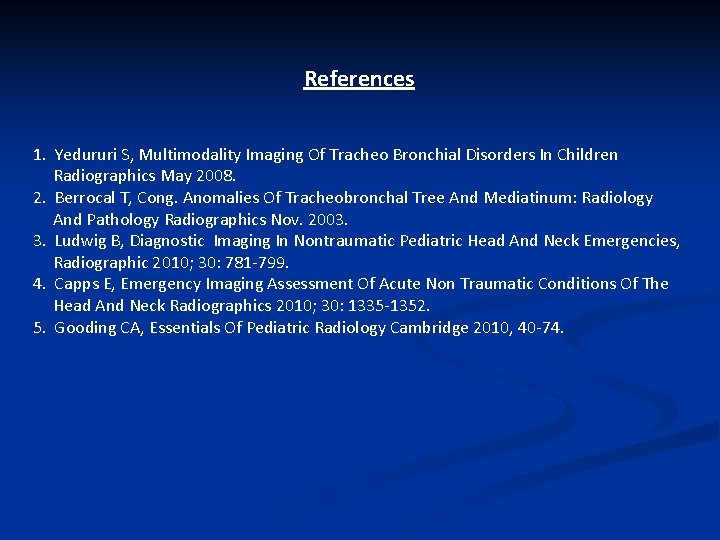
References 1. Yedururi S, Multimodality Imaging Of Tracheo Bronchial Disorders In Children Radiographics May 2008. 2. Berrocal T, Cong. Anomalies Of Tracheobronchal Tree And Mediatinum: Radiology And Pathology Radiographics Nov. 2003. 3. Ludwig B, Diagnostic Imaging In Nontraumatic Pediatric Head And Neck Emergencies, Radiographic 2010; 30: 781 -799. 4. Capps E, Emergency Imaging Assessment Of Acute Non Traumatic Conditions Of The Head And Neck Radiographics 2010; 30: 1335 -1352. 5. Gooding CA, Essentials Of Pediatric Radiology Cambridge 2010, 40 -74.