Diagnosis and management of Wilsons disease Richa Shukla





- Slides: 41
Diagnosis and management of Wilson’s disease Richa Shukla Faculty mentor: Dr. Pappas November 6, 2014
Case discussion • Reason for consult: Liver transplant evaluation for cirrhosis due to Wilson’s disease
HPI • 48 M with h/o Wilson’s disease diagnosed in 1995 - ↓ceruloplasmin, ↑ 24 hour urine copper and K-F rings • Treated with tetrathiomolybdate for 8 weeks in 1996, started on zinc acetate • Liver biopsy results 7/20/1999 consistent with cirrhosis • EGD 5/2009 and 6/2009 – non-bleeding varices
HPI • 2011 – patient blacked out while driving, killing a motorcyclist. Was subsequently incarcerated • Family reports irregular medical care during incarceration • Released in 2/2014 – family noted decline in mental status • Hospitalized x 2 for PSE and bleeding varices in 3/2014, 6/2014. Underwent TIPS 7/2014
HPI • 9/17/14 – hospitalized at OSH for AMS, transferred to a tertiary care hospital. • Mental status improved initially but subsequently patient refused lactulose and MS again decompensated • Transferred to a Houston hospital for OLT evaluation
HPI • Admitted to Houston hospital MICU due to obtundation • Started on lactulose and rifaximin via NG tube • Also started on zinc acetate and trientine
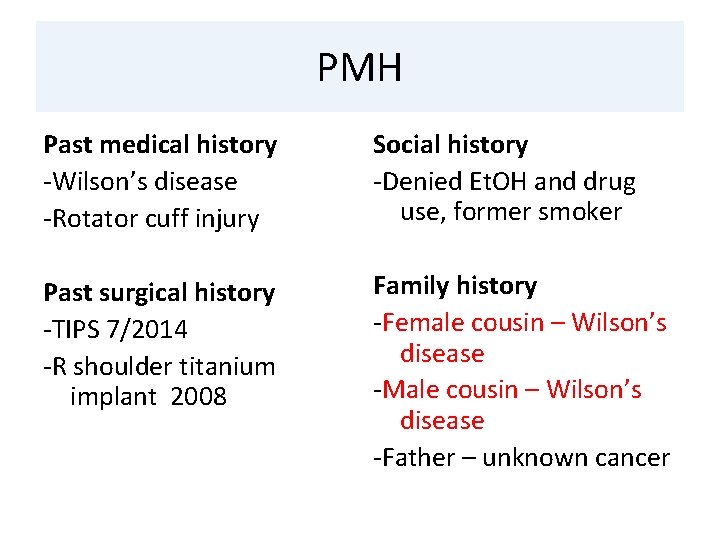
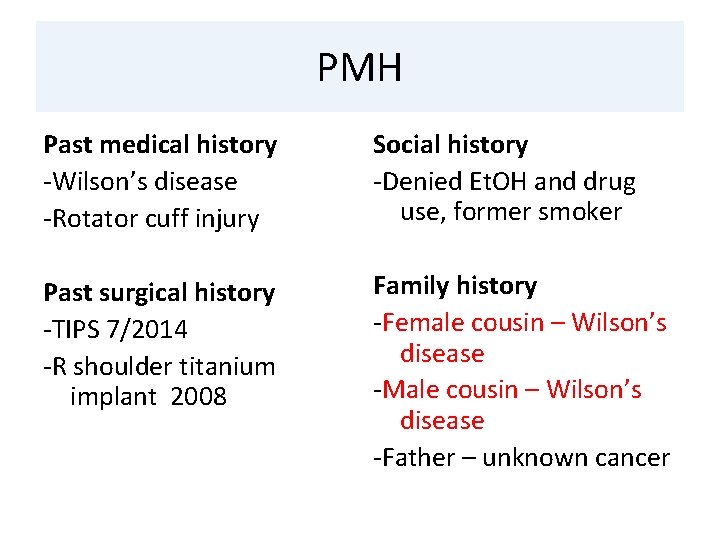
PMH Past medical history -Wilson’s disease -Rotator cuff injury Social history -Denied Et. OH and drug use, former smoker Past surgical history -TIPS 7/2014 -R shoulder titanium implant 2008 Family history -Female cousin – Wilson’s disease -Male cousin – Wilson’s disease -Father – unknown cancer
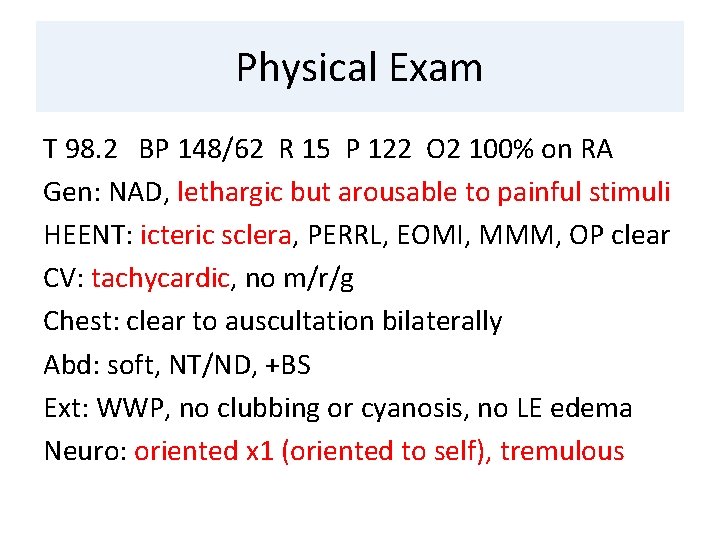
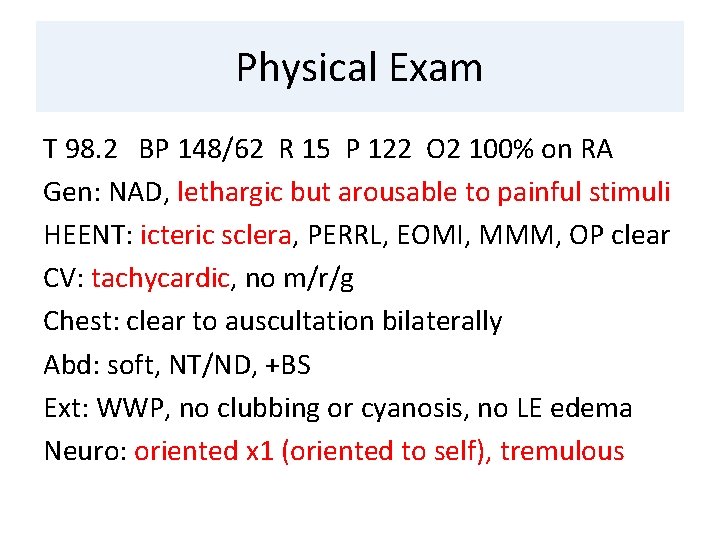
Physical Exam T 98. 2 BP 148/62 R 15 P 122 O 2 100% on RA Gen: NAD, lethargic but arousable to painful stimuli HEENT: icteric sclera, PERRL, EOMI, MMM, OP clear CV: tachycardic, no m/r/g Chest: clear to auscultation bilaterally Abd: soft, NT/ND, +BS Ext: WWP, no clubbing or cyanosis, no LE edema Neuro: oriented x 1 (oriented to self), tremulous
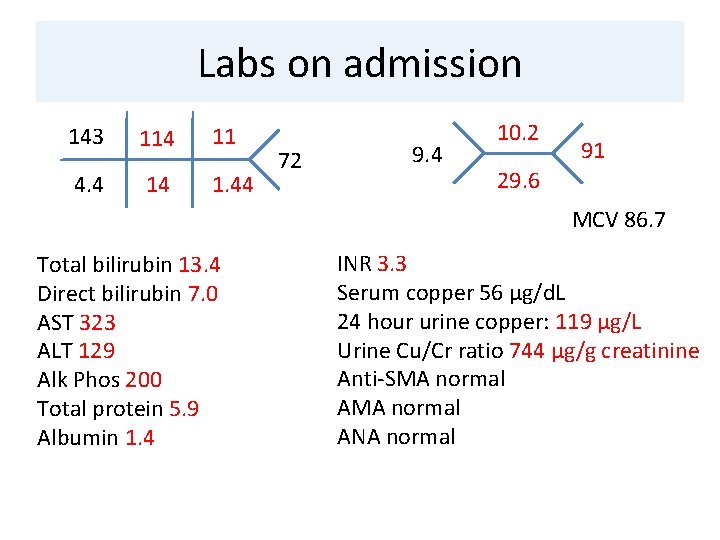
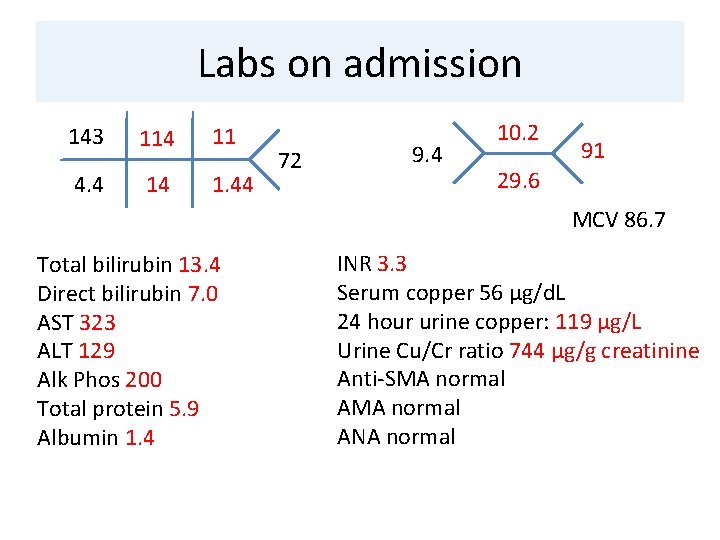
Labs on admission 143 114 11 4. 4 14 1. 44 72 9. 4 10. 2 91 29. 6 MCV 86. 7 Total bilirubin 13. 4 Direct bilirubin 7. 0 AST 323 ALT 129 Alk Phos 200 Total protein 5. 9 Albumin 1. 4 INR 3. 3 Serum copper 56 µg/d. L 24 hour urine copper: 119 µg/L Urine Cu/Cr ratio 744 µg/g creatinine Anti-SMA normal ANA normal
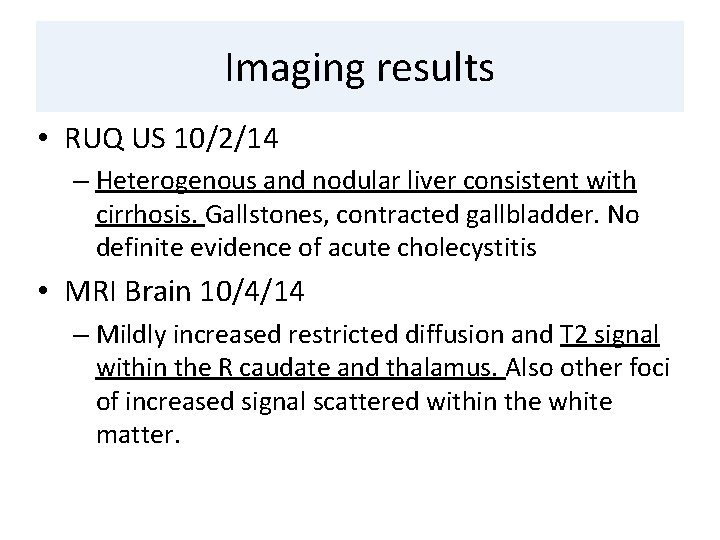
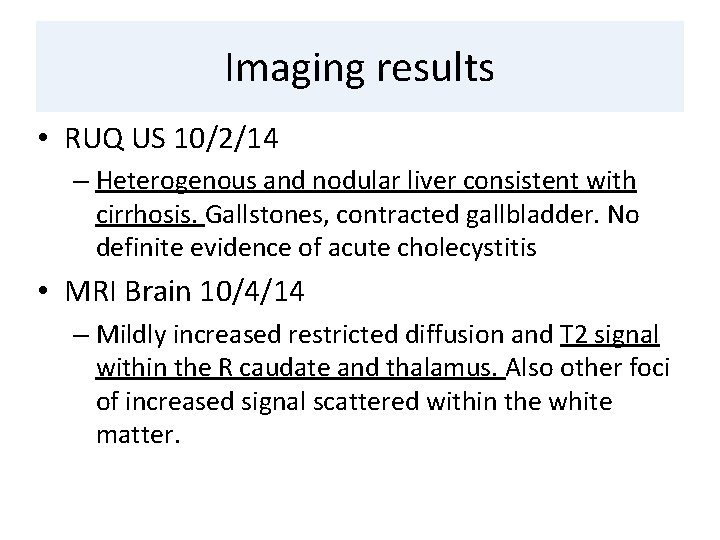
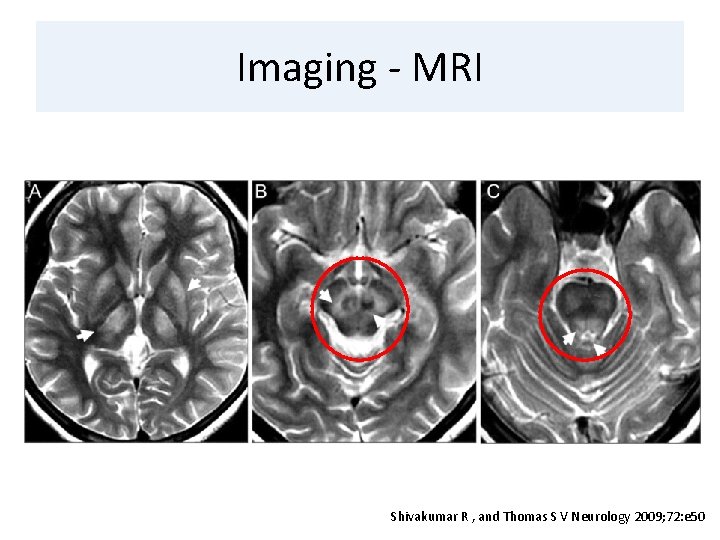
Imaging results • RUQ US 10/2/14 – Heterogenous and nodular liver consistent with cirrhosis. Gallstones, contracted gallbladder. No definite evidence of acute cholecystitis • MRI Brain 10/4/14 – Mildly increased restricted diffusion and T 2 signal within the R caudate and thalamus. Also other foci of increased signal scattered within the white matter.
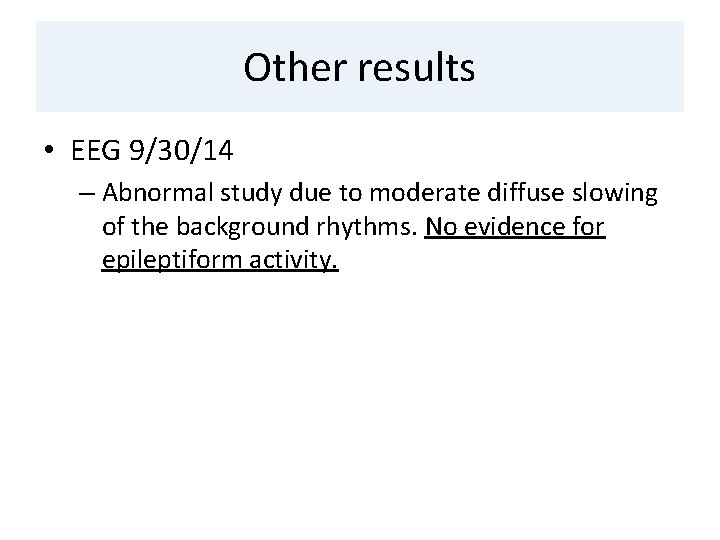
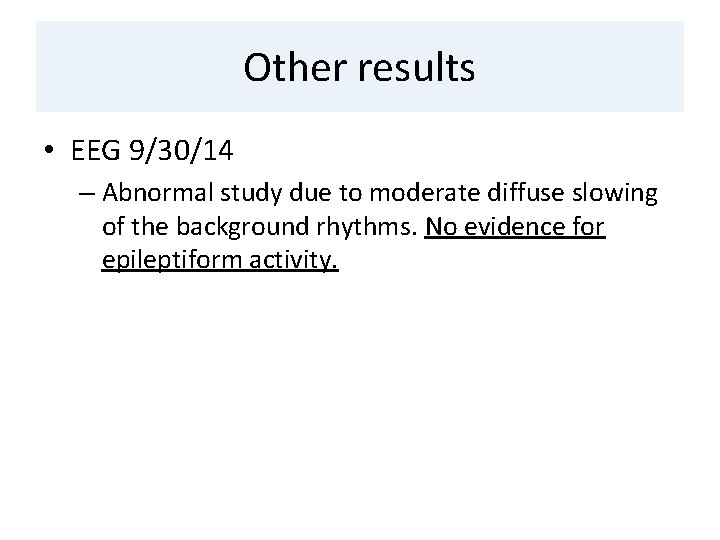
Other results • EEG 9/30/14 – Abnormal study due to moderate diffuse slowing of the background rhythms. No evidence for epileptiform activity.
Clinical Questions • How is Wilson’s disease diagnosed? • What treatment options are available for Wilson’s disease? • What is the role of liver transplantation in Wilson’s disease?
Clinical Questions • How is Wilson’s disease diagnosed? • What treatment options are available for Wilson’s disease? • What is the role of liver transplantation in Wilson’s disease?
Background • First written about in 1912 by Kinnier-Wilson • Autosomal recessive disease – mutation of ATP 7 B gene on chromosome 13 • Defective biliary excretion of copper • 30 affected individuals per million population • Majority diagnosed 15 -35 years of age • Children present with liver disease, adults with neurologic disease Wilson, S Brain 34: 295– 509. 1912 Lorincz. Annals of the New York Academy of Sciences. January 2010 Hilal Case Reports in Medicine September 2014 AASLD Criteria Diagnosis and Treatment of Wilson’s Disease: an update
Clinical presentation • Neurologic manifestations – 98% have Kayser-Fleischer rings – Classification: dysarthric, dystonic, tremulous, pseudosclerotic or parkinsonian – Chorea, dementia, seizures, hyperreflexia, autonomic dysfunction, risus sardonicus • Psychiatric symptoms – Earlier presentation – Depression most common

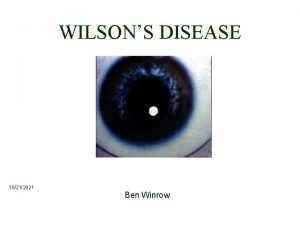
Kayser-Fleischer rings
Clinical presentation • Hepatic manifestations – Range from asymptomatic disease to acute liver failure – Younger patients develop acute hepatitis with ↑AST, jaundice, abdominal pain – Acute liver failure – Coomb’s negative hemolytic anemia, low uric acid, normal/low-normal alkaline phosphatase, coagulopathy, renal failure
Diagnosis • Classic Wilson’s disease: Age 5 -40, decreased ceruloplasmin, Kayser-Fleischer rings • High index of clinical suspicion, multisystem symptomatology • Family screening of first-degree relatives must be undertaken Ala et al. Lancet February 2007
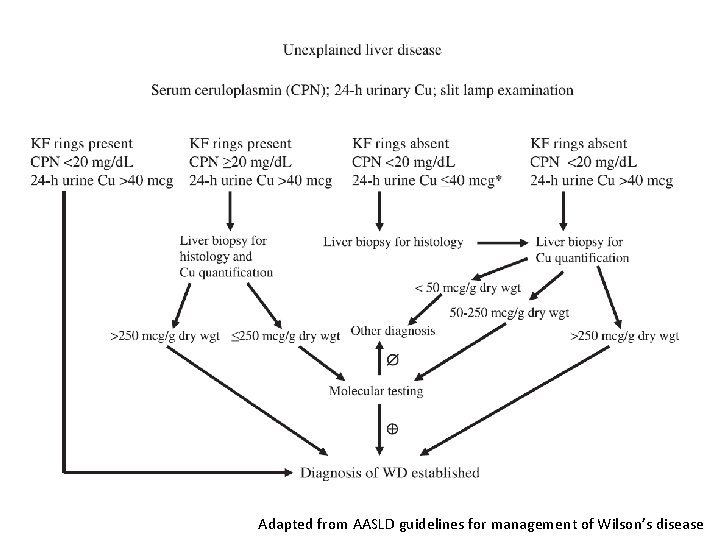
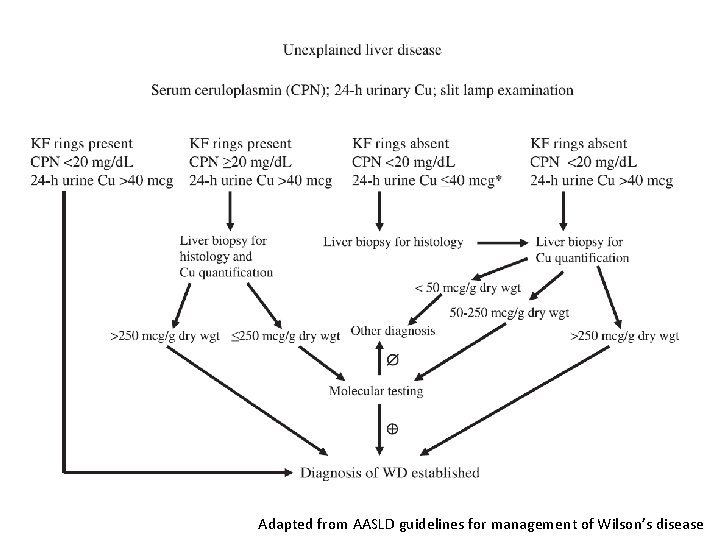
Adapted from AASLD guidelines for management of Wilson’s disease
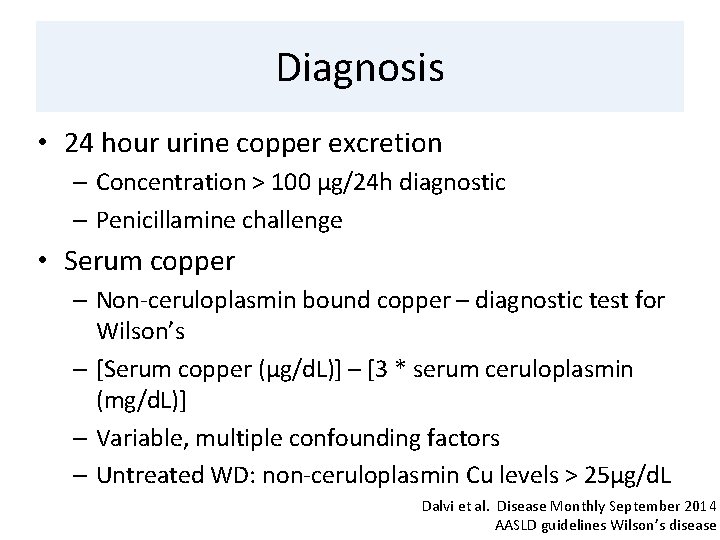
Diagnosis • 24 hour urine copper excretion – Concentration > 100 µg/24 h diagnostic – Penicillamine challenge • Serum copper – Non-ceruloplasmin bound copper – diagnostic test for Wilson’s – [Serum copper (µg/d. L)] – [3 * serum ceruloplasmin (mg/d. L)] – Variable, multiple confounding factors – Untreated WD: non-ceruloplasmin Cu levels > 25µg/d. L Dalvi et al. Disease Monthly September 2014 AASLD guidelines Wilson’s disease
Diagnosis • Serum ceruloplasmin – Level below 20 mg/d. L SUGGESTIVE – Low levels seen: 1% normal population, 10% of heterozygous carriers for WD, Menke’s disease, nephrotic syndrome – Normal ceruloplasmin seen in 20% WD patients • Cauza et al. –PPV of low ceruloplasmin 5. 9% Cauza et al. J Hepatol 1997; 27: 358 -362.
Use of ceruloplasmin • AASLD guidelines: – Extremely low serum ceruloplasmin level (<50 mg/L or <5 mg/d. L) should be taken as strong evidence for the diagnosis of WD. – Modestly subnormal levels suggest further evaluation is necessary. – Serum ceruloplasmin within the normal range does not exclude the diagnosis

Other diagnostic tests • Hepatic copper concentration - > 250 µg/g dry weight • Kayser-Fleischer rings – slit-lamp exam – Most patients with neuropsychiatric symptoms will show KF rings – 50– 60% of patients with hepatic WD
Genetic testing • 25% probability that sibling of affected patient has WD • Genetic testing – standard of screening in family members • Direct sequencing of ATP 7 B for disease specific mutations – standard for molecular diagnosis • Finding of two mutations or homozygosity for one mutation highly suggestive of WD Schilsky et al Curr Gastroenterol Rep (2010) 12: 57– 61
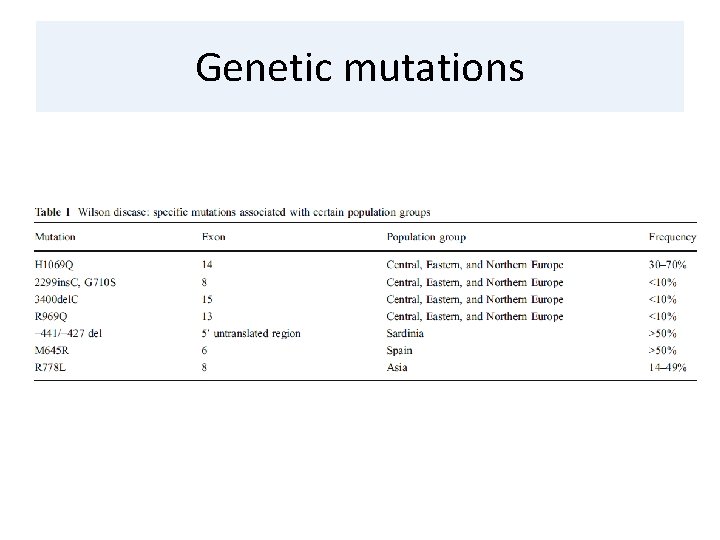
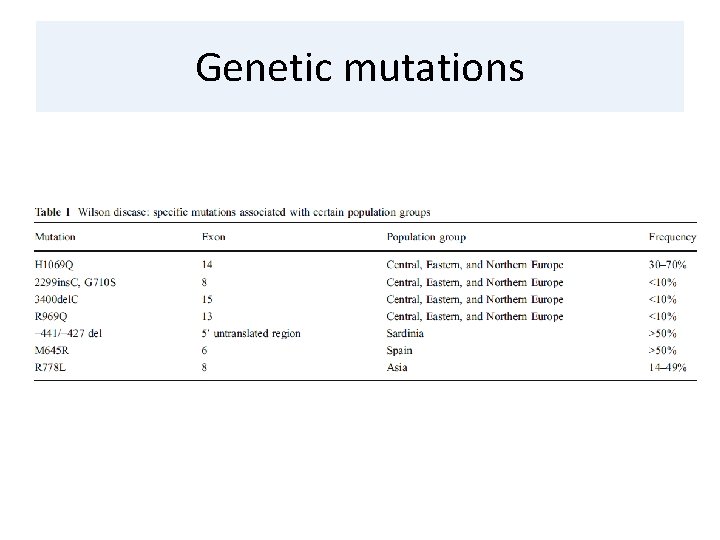
Genetic mutations
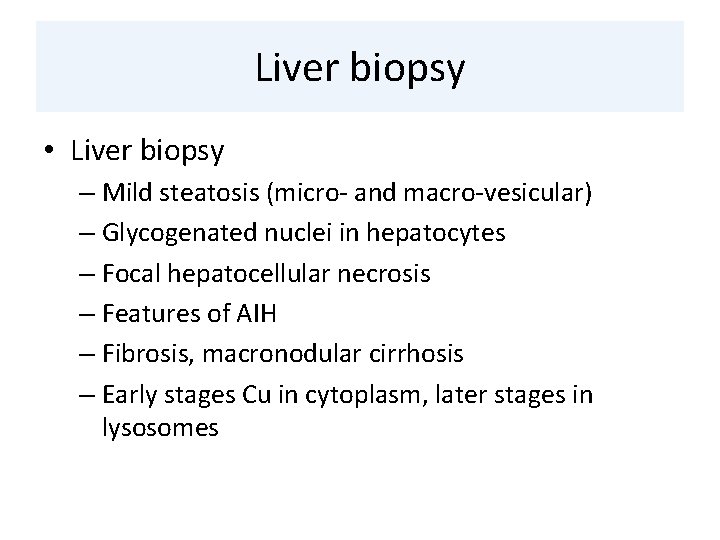
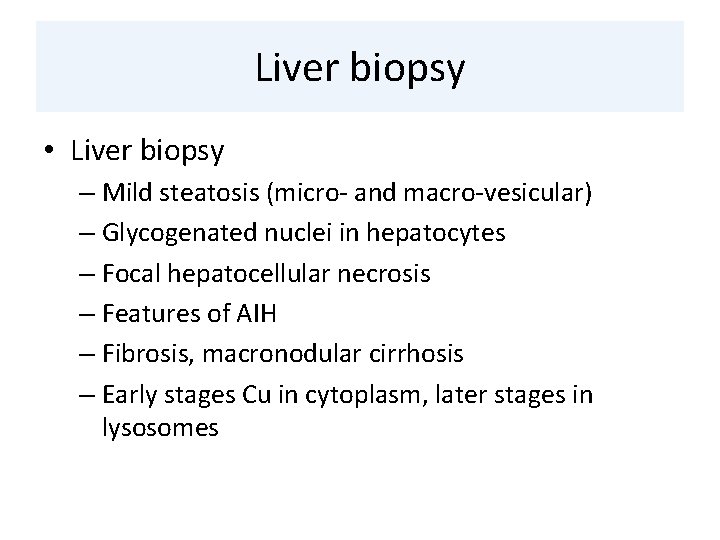
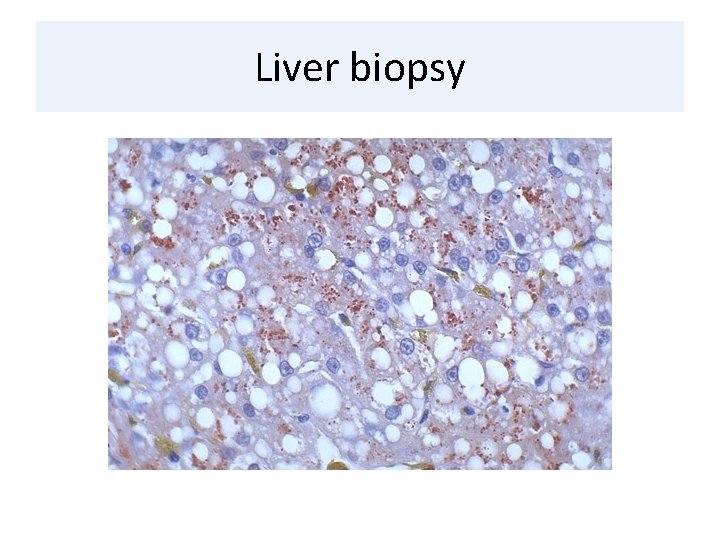
Liver biopsy • Liver biopsy – Mild steatosis (micro- and macro-vesicular) – Glycogenated nuclei in hepatocytes – Focal hepatocellular necrosis – Features of AIH – Fibrosis, macronodular cirrhosis – Early stages Cu in cytoplasm, later stages in lysosomes
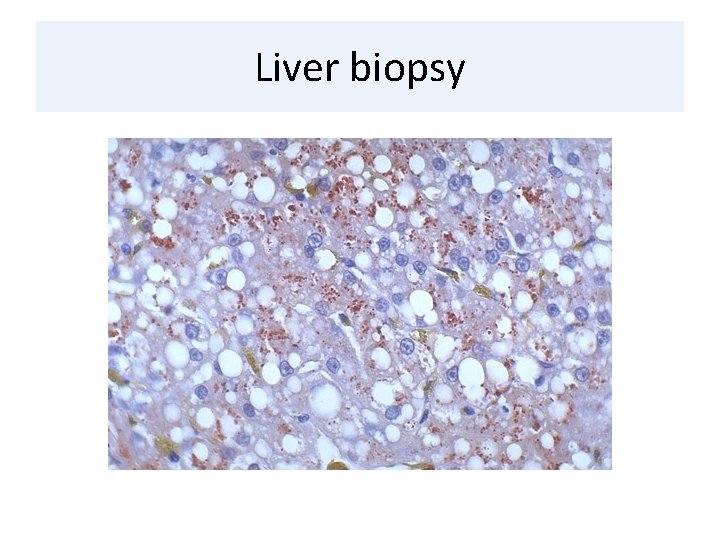
Liver biopsy
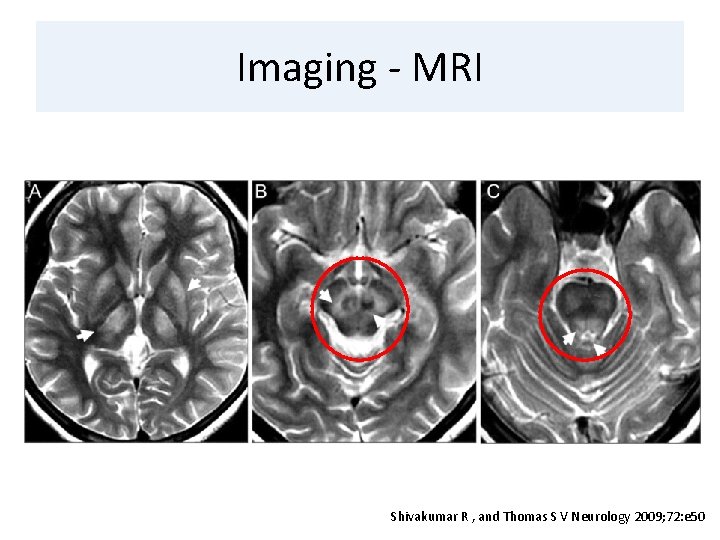
Imaging - MRI Shivakumar R , and Thomas S V Neurology 2009; 72: e 50

Diagnostic Index Dalvi et al. Disease A Month Sept 2014
Clinical Questions • How is Wilson’s disease diagnosed? • What treatment options are available for Wilson’s disease? • What is the role of liver transplantation in Wilson’s disease?

Treatment • Goal of treatment – Removal of copper from various organs – Symptomatic control
Treatment - chelation • Pencillamine – First oral agent to treat WD – Side effects: neurologic deterioration, bone marrow suppression, hypersensitivity, lupus-like syndrome • Trientine – Promotes urinary excretion of copper – Fewer side effects than penicillamine – Combine with zinc for maintenance therapy
Treatment - chelation • Zinc – Sequesters copper within enterocytes, also complexes copper in hepatocytes in non-toxic form – Used in pre-symptomatic, maintenance phase • Ammonium tetrathiomolybdate – Complexes with dietary copper when given with meals – reducing absorption – Complexes with free copper and serum albumin when given between meals – excreted in bile
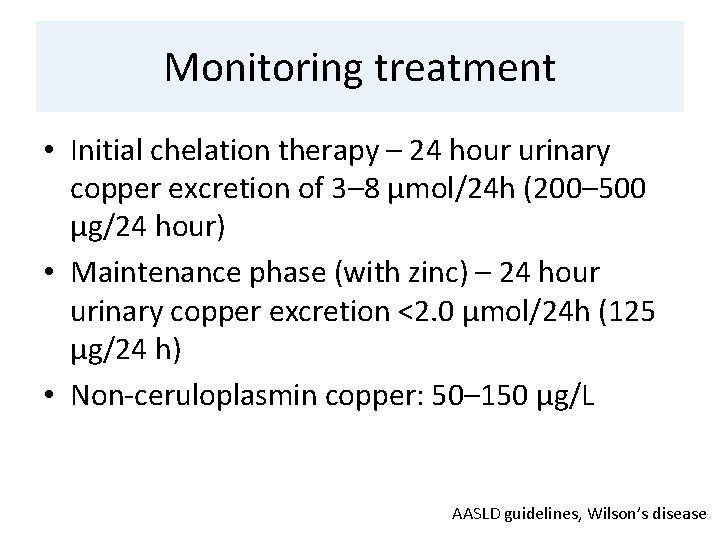
Monitoring treatment • Initial chelation therapy – 24 hour urinary copper excretion of 3– 8 μmol/24 h (200– 500 μg/24 hour) • Maintenance phase (with zinc) – 24 hour urinary copper excretion <2. 0 μmol/24 h (125 μg/24 h) • Non-ceruloplasmin copper: 50– 150 μg/L AASLD guidelines, Wilson’s disease
Clinical Questions • How is Wilson’s disease diagnosed? • What treatment options are available for Wilson’s disease? • What is the role of liver transplantation in Wilson’s disease?
Role for liver transplantation • Acute liver failure • Decompensated liver disease unresponsive to medical therapy • One-year survival following liver transplantation 79%-87% Eghtesad et al. Liver Transplant Surgery November 2009
Long-term outcomes in WD • Beinhardt et al. – retrospective cohort study of 229 patients between 1961 -April 2013 • Long term treatment outcomes studied in 162 patients, average follow-up of 14. 8 ± 11. 4 yrs • 26% fully recovered, 24% improved, 25% stable • 13% of patients required OLT during study period • Overall shows long-term favorable outcomes in WD patients receiving regular care Beinhardt et al. CGH April 2014

OLT in neurologic disease • Stracciari et al : 44 M with WD, cirrhosis and neurologic manifestations – post OLT showed improvement in motor function, disappearance of K-F rings, normalization of copper balance, reversal of MRI abnormalities Stracciari et al. JAMA Neurology March 2000
OLT in neurologic disease • Guarino et al – presented case of rapid deterioration in neurological function after OLT in patient with hepatic and neurologic involvement – basal ganglia damage is irreversible – early post-operative central pontine and extrapontine myelinolysis Guarino et al. Acta Neurologica Scandinavica November 1995
Summary • Diagnosis – serum ceruloplasmin, 24 hour urine copper, K-F rings, liver biopsy, imaging • Treatment – chelation agents (D-penicillamine v. trientine), symptomatic treatment • Liver transplantation for ALF, refractory disease • Unclear benefits and possible harm of OLT in neurologic disease • With chelation therapy and OLT, prolonged survival has become the norm
Thank you!
 Richa shukla pregnant
Richa shukla pregnant Richa colon
Richa colon Ruchi shukla ukraine
Ruchi shukla ukraine Amol shukla
Amol shukla Rekha shukla joint secretary
Rekha shukla joint secretary Dr bk shukla
Dr bk shukla Jagadish shukla
Jagadish shukla Wilson's fourteen points and the treaty of versailles
Wilson's fourteen points and the treaty of versailles Ongoing planning in nursing
Ongoing planning in nursing Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Objectives of nursing process
Objectives of nursing process Reservoir system
Reservoir system Dr richa goyal
Dr richa goyal Dr richa tiwari
Dr richa tiwari Richa rai
Richa rai Bharathi viswanathan
Bharathi viswanathan Gange med brøk
Gange med brøk Woodrow wilsons new freedom
Woodrow wilsons new freedom Woodrow wilsons 14 punkter
Woodrow wilsons 14 punkter Annual order cost formula
Annual order cost formula Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Nursing diagnosis for meniere's disease
Nursing diagnosis for meniere's disease Nursing diagnosis for meniere's disease
Nursing diagnosis for meniere's disease Behcet disease diagnosis
Behcet disease diagnosis Diagnosis of periodontal disease
Diagnosis of periodontal disease Type 1 diabetes in adults diagnosis and management
Type 1 diabetes in adults diagnosis and management Nursing care for gastrointestinal disorders
Nursing care for gastrointestinal disorders Phototherapy for newborn's nursing interventions
Phototherapy for newborn's nursing interventions Kate lorig stanford
Kate lorig stanford Disease management association of america
Disease management association of america Wagner model of chronic disease management
Wagner model of chronic disease management Decompensated cirrhosis
Decompensated cirrhosis Disease management roi
Disease management roi Deka vitaminok
Deka vitaminok Disease management roi
Disease management roi Top management and middle management
Top management and middle management Management pyramid
Management pyramid Top management middle management first line management
Top management middle management first line management Charting identification chapter 28
Charting identification chapter 28 Pendulous tuberosity
Pendulous tuberosity Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning