Definition Risk Factors of FGR FGR also called








- Slides: 37


Definition & Risk Factors of FGR
FGR, also called IUGR is the term used to describe a fetus that has not reached its growth potential because of genetic or environmental factors.
The origin of FGR may be fetal, placental, or maternal, with significant overlap among these entities. A major focus of prenatal care is to determine whether a fetus is at risk for growth restriction and to identify the growth restricted fetus.
This is important because these fetuses are at increased risk of adverse perinatal outcome. In addition, FGR appears to be an antecedent to some cases of hypertension, hyperlipidemia, coronary heart disease, and diabetes mellitus in the adult (Barker hypothesis)
In a cohort study in Sweden, a 10 -fold increase in late fetal deaths was found among very small fetuses. Similarly, Gardosi et al noted in 1998 that nearly 40% of stillborn fetuses that were not malformed were SGA.
DEFINITION The most common definition of FGR refers to a weight below the 10 th percentile for gestational age , although other definitions employing a variety of criteria have been advocated (eg, <5 th percentile, <3 rd percentile)
SGA birth is defined as EFW or AC less than the 10 th centile and severe SGA as an EFW or AC less than the 3 rd centile.
This definition is problematic because it does not make a distinction among fetuses who are (1) constitutionally small, (2) small because a pathologic process has kept them from achieving their genetic growth potential, and (3) not small but a pathologic process has kept them from achieving their genetic growth potential.

Of all fetuses at or below the 10 th percentile for growth, only approximately 40% are at high risk of potentially preventable perinatal death. Another 40% of these fetuses are constitutionally small.
The remaining 20% of fetuses that are SGA are intrinsically small secondary to a chromosomal or environmental etiology. Examples include fetuses with trisomy 18, cytomegalovirus infection, or fetal alcohol syndrome. These fetuses are less likely to benefit from prenatal intervention, and their prognosis is most closely related to the underlying etiology.
NORMAL AND ABNORMAL FETAL GROWTH Normal fetal growth reflects the interaction of the fetus's genetically and its modulation by the health of the fetus, placenta and the mother. Population-based studies of birth weight have reported that genetic factors contribute 30 to 50 % of the variation in birth weight, with the remainder due to environmental factors. Maternal genes influence birth weight more than paternal genes, but both have an effect.
Normal growth The process of fetal growth comprises three consecutive and somewhat overlapping phases. The first phase is the phase of cellular hyperplasia (the first 16 weeks of gestation). The second phase, known as the phase of concomitant hyperplasia and hypertrophy, (between the 16 th and 32 nd weeks). The third and final phase, called the phase of cellular hypertrophy ( between the 32 nd week and term)
Quantitatively, normal singleton fetal growth increases from approximately 5 g/day at 14 to 15 weeks of gestation to 10 g/day at 20 weeks and 30 to 35 g/day at 32 to 34 weeks, after which the growth rate decreases. The median growth rate in multiple gestations is lower than that of singletons during the third trimester.
Symmetric and asymmetric growth restriction The pattern of normal growth forms the basis for the clinical classification of FGR: ●Symmetric FGR (20 to 30 % ) ●Asymmetric FGR ( 70 to 80%)
Screening Measures
CLINICAL ASSESSMENT Clinical assessment is a reasonable screening tool for FGR in low risk pregnancies, as there is no high quality evidence that alternative approaches, such as routine ultrasound examination, improve outcome over clinical assessment alone.
Clinical assessment is based on assessment of past and present risk factors, physical examination, and ultrasound studies.
Symphysis-fundal height measurement: wide range of sensitivities: 13 to 86 % of small fetuses were reported
When ultrasound examination suggests a diagnosis of FGR, further evaluation to look for maternal, placental, or fetal disorders associated with impaired fetal growth is indicated.
This evaluation helps to (1) distinguish the IUGR from the constitutionally SGA, (2) guide management of the pregnancy
AC Most studies report reduced AC is the most sensitive single morphometric indicator of FGR.
Use of the 10 th centile had better sensitivities and specificities than other commonly used centiles. In a low risk population sensitivity (0– 10%) and specificity (66– 99%) for any parameter. In a high risk population, fetal AC < 10 th centile sensitivity( 72. 9– 94. 5%) and specificity 50. 6– 83. 8%. EFW < 10 th centile sensitivity ( 33. 3– 89. 2%) and specificity 53. 7– 90. 9%.
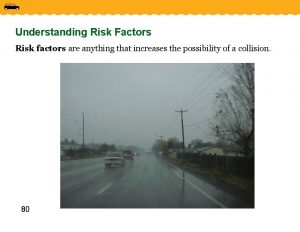
Risk factors for a SGA fetus/neonate : All women should be assessed at booking for risk factors for a SGA fetus/neonate to identify those who require increased surveillance. Women who have a major risk factor (OR > 2. 0) should be referred for serial ultrasound measurement of fetal size and assessment of wellbeing with umbilical artery Doppler from 26– 28 weeks of pregnancy.
Women who have three or more minor risk factors should be referred for uterine artery Doppler at 20– 24 weeks of gestation. Second trimester DS markers have limited predictive accuracy for delivery of a SGA neonate.
A low level (< 0. 415 Mo. M) of the first trimester marker PAPP–A should be considered a major risk factor for delivery of a SGA neonate. In high risk populations uterine artery Doppler at 20– 24 weeks of pregnancy has a moderate predictive value for a severely SGA neonate.
In women with an abnormal uterine artery Doppler at 20– 24 weeks of pregnancy, subsequent normalisation of flow velocity indices is still associated with an increased risk of a SGA neonate. Repeating uterine artery Doppler is therefore of limited value.
Women with an abnormal uterine artery Doppler at 20– 24 weeks (defined as a [PI]> 95 th centile) and/or notching should be referred for serial ultrasound measurement of fetal size and assessment of wellbeing with umbilical artery Doppler commencing at 26– 28 weeks of pregnancy.
Women with a normal uterine artery Doppler do not require serial measurement of fetal size and serial assessment of wellbeing with umbilical artery Doppler unless they develop specific pregnancy complications, for example antepartum haemorrhage or hypertension. However, they should be offered a scan for fetal size and umbilical artery Doppler during the third trimester
Serial ultrasound measurement of fetal size and assessment of wellbeing with umbilical artery Doppler should be offered in cases of fetal echogenic bowel.
Women with a single SFH which plots below the 10 th centile or serial measurements which demonstrates low or static growth by crossing centiles should be referred for ultrasound measurement of fetal size. Women in whom measurement of SFH is inaccurate (for example: BMI > 35, large fibroids, hydramnios) should be referred for serial assessment of fetal size using ultrasound





 Credit risk market risk operational risk
Credit risk market risk operational risk Which search strategy is also called as blind search?
Which search strategy is also called as blind search? Citric acid cycle also called
Citric acid cycle also called Specification-based techniques
Specification-based techniques Parts of the pharynx
Parts of the pharynx A workbook is also called a
A workbook is also called a Fungi are also called multicellular decomposers
Fungi are also called multicellular decomposers Glasses also called eyeglasses (formal)
Glasses also called eyeglasses (formal) It is also called figurative language
It is also called figurative language Vowel phonemes that glide in the middle
Vowel phonemes that glide in the middle Citric acid cycle also called
Citric acid cycle also called Examples of axial movement
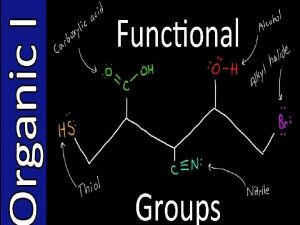
Examples of axial movement Alkanes are also called
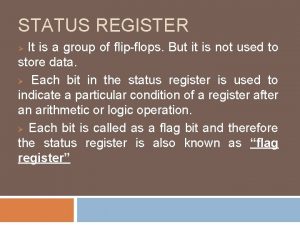
Alkanes are also called Status register
Status register Short division bus stop method
Short division bus stop method Womb is also called
Womb is also called Raster scan display and vector scan display
Raster scan display and vector scan display Is also called as data selector.
Is also called as data selector. The circle graphs are commonly called
The circle graphs are commonly called Womb is also called
Womb is also called Dynamic equivalent translation
Dynamic equivalent translation Womb is also called
Womb is also called Womb is also called
Womb is also called 4-adjacency 8-adjacency m-adjacency
4-adjacency 8-adjacency m-adjacency Womb is also called
Womb is also called Bytestuffing
Bytestuffing Ac voltage controller applications
Ac voltage controller applications Shark skates and rays are also called
Shark skates and rays are also called Irony in literature
Irony in literature Dominance emphasis
Dominance emphasis Economic resources are also called:
Economic resources are also called: Direct english method
Direct english method What is physiological density ap human geography
What is physiological density ap human geography Which vitamin is antihemorrhagic
Which vitamin is antihemorrhagic Permanent hardness is also called as
Permanent hardness is also called as Royalty receivable account
Royalty receivable account Why are they called modal verbs
Why are they called modal verbs What are the osha construction standards also called
What are the osha construction standards also called