CPC as Cinema The Producers starring Drs Troy

![The Setting • Polysubstance abuse [nicotine, alcohol, iv cocaine, pot] • Bipolar disorder • The Setting • Polysubstance abuse [nicotine, alcohol, iv cocaine, pot] • Bipolar disorder •](https://slidetodoc.com/presentation_image_h2/3fbe9d29998b2d7c1f9c889aa281e2ef/image-3.jpg)
![Toxicology studies • Opiates (expected, hydrocodone) - [ not cause of her liver disease] Toxicology studies • Opiates (expected, hydrocodone) - [ not cause of her liver disease]](https://slidetodoc.com/presentation_image_h2/3fbe9d29998b2d7c1f9c889aa281e2ef/image-7.jpg)






- Slides: 45
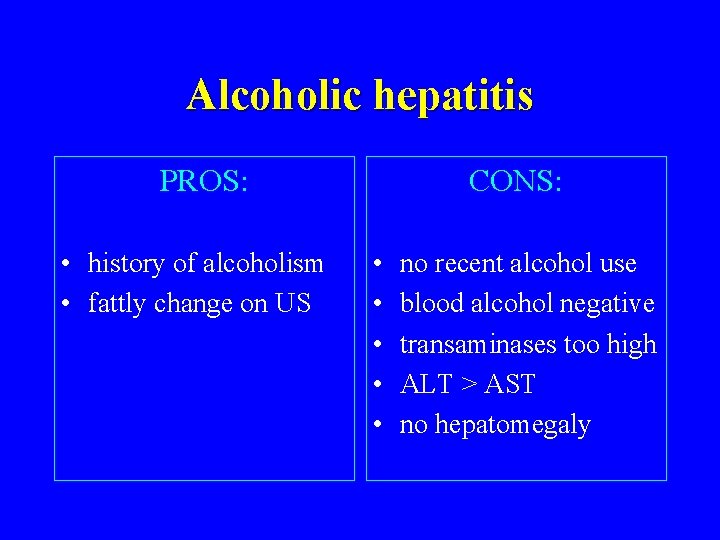
CPC as Cinema • “The Producers”, starring Drs. Troy Wadsworth and Nilam Soni • “Clueless”, starring Mark Feldman • “The Sting”, starring Dr. Dale Odell

The Plot: 45 year old divorcee with acute delirium • associated with hepatic • disease (jaundice, • • abnormal liver chemistries and asterixis). Asterixis (liver flap) Hepatic failure Respiratory acidosis Uremia Cerebrovascular disease
![The Setting Polysubstance abuse nicotine alcohol iv cocaine pot Bipolar disorder The Setting • Polysubstance abuse [nicotine, alcohol, iv cocaine, pot] • Bipolar disorder •](https://slidetodoc.com/presentation_image_h2/3fbe9d29998b2d7c1f9c889aa281e2ef/image-3.jpg)
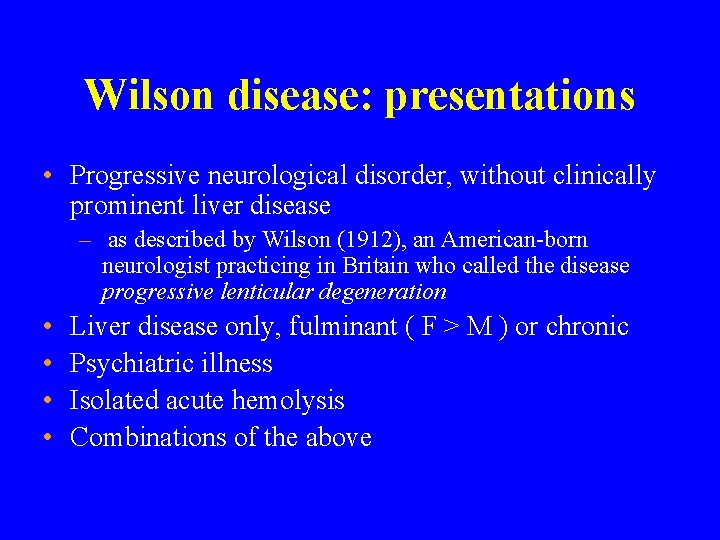
The Setting • Polysubstance abuse [nicotine, alcohol, iv cocaine, pot] • Bipolar disorder • Taking at least 6 other drugs: – hydrocodone and acetaminophen for back pain – risperidone, citalopram, carbamazepine, nefazodone – she is prone to drug OD if depressed • Grave’s disease treated with RAI twice- currently on T 4
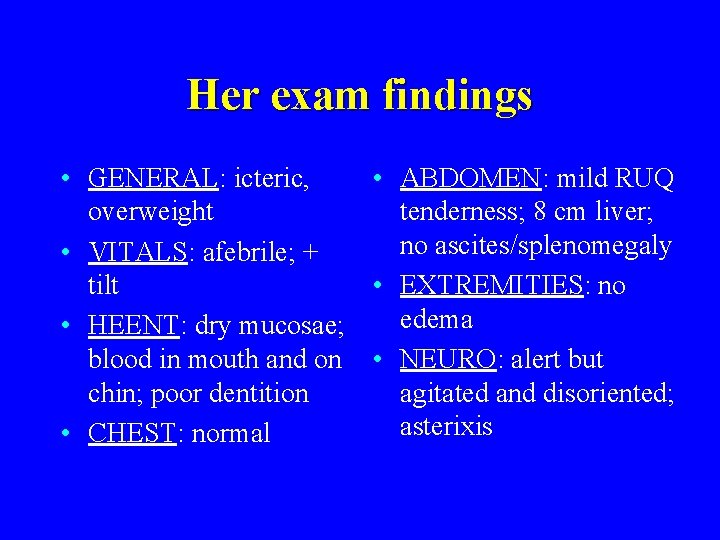
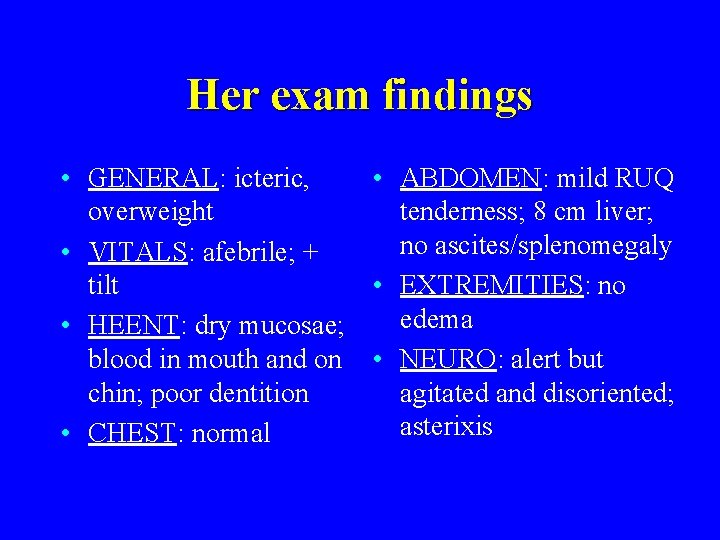
Her exam findings • GENERAL: icteric, • ABDOMEN: mild RUQ overweight tenderness; 8 cm liver; no ascites/splenomegaly • VITALS: afebrile; + tilt • EXTREMITIES: no edema • HEENT: dry mucosae; blood in mouth and on • NEURO: alert but chin; poor dentition agitated and disoriented; asterixis • CHEST: normal
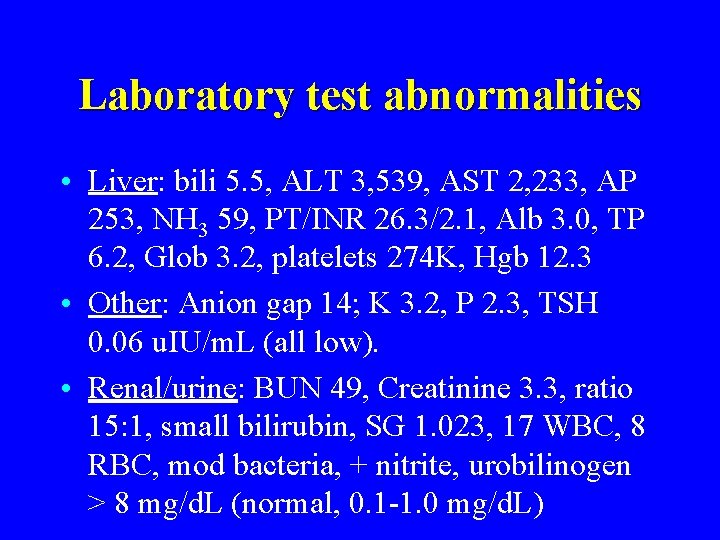
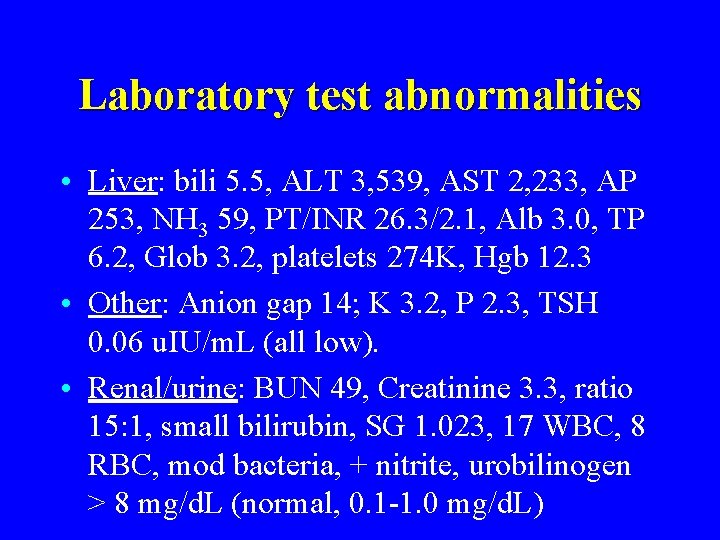
Laboratory test abnormalities • Liver: bili 5. 5, ALT 3, 539, AST 2, 233, AP 253, NH 3 59, PT/INR 26. 3/2. 1, Alb 3. 0, TP 6. 2, Glob 3. 2, platelets 274 K, Hgb 12. 3 • Other: Anion gap 14; K 3. 2, P 2. 3, TSH 0. 06 u. IU/m. L (all low). • Renal/urine: BUN 49, Creatinine 3. 3, ratio 15: 1, small bilirubin, SG 1. 023, 17 WBC, 8 RBC, mod bacteria, + nitrite, urobilinogen > 8 mg/d. L (normal, 0. 1 -1. 0 mg/d. L)
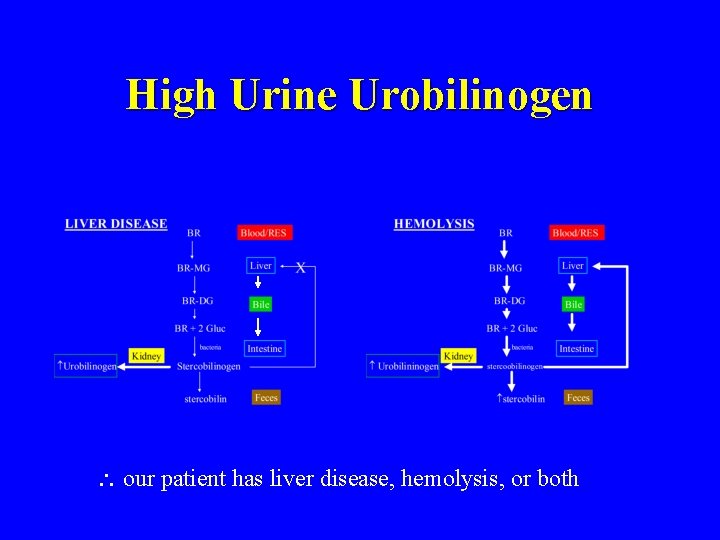
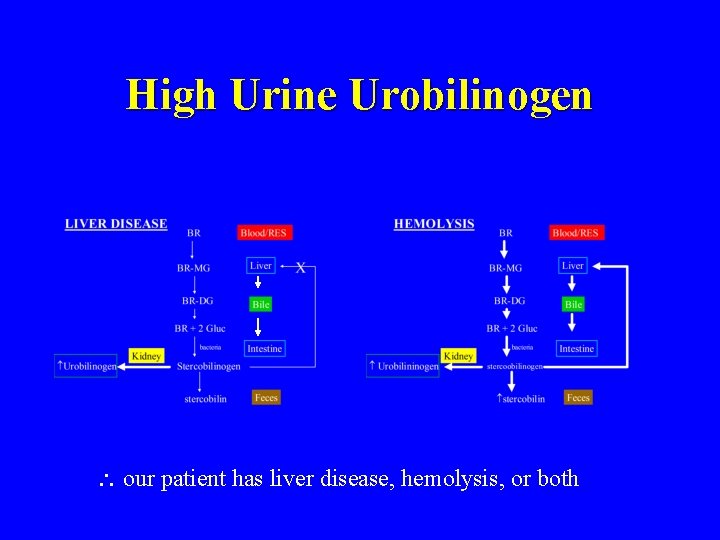
High Urine Urobilinogen our patient has liver disease, hemolysis, or both
![Toxicology studies Opiates expected hydrocodone not cause of her liver disease Toxicology studies • Opiates (expected, hydrocodone) - [ not cause of her liver disease]](https://slidetodoc.com/presentation_image_h2/3fbe9d29998b2d7c1f9c889aa281e2ef/image-7.jpg)
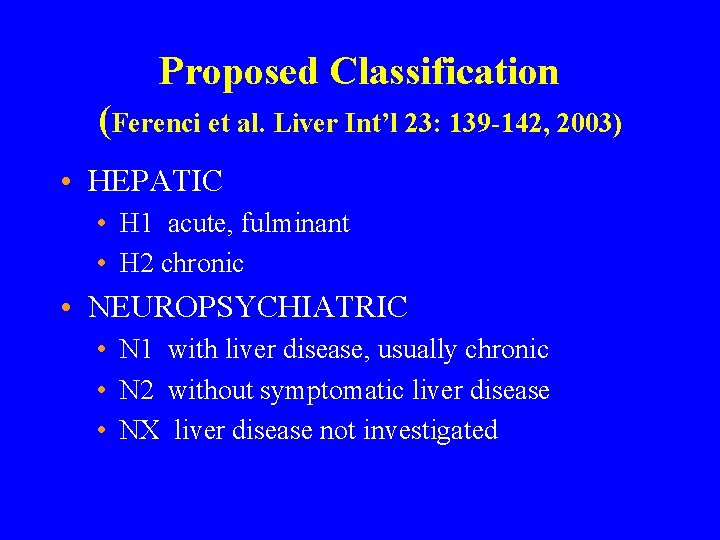
Toxicology studies • Opiates (expected, hydrocodone) - [ not cause of her liver disease] Aspirin - [ not cause of her gap acidosis] • APAP • • Carbamazepine- slightly toxic range signs of toxicity: clumsy, unsteady, confused, dizzy, drowsy – ? due to OD, liver failure with metabolism, or drug-drug interaction with nefazodone • Nefazodone-induced carbamazepine toxicity. Am J Psychiatry 153: 733, 1996 • Cabamazepine-nefazodone interaction in healthy subjects. J Clin Psychopharmacol 20: 46 -53, 2000 – ? role of carbamazepine in causing liver failure
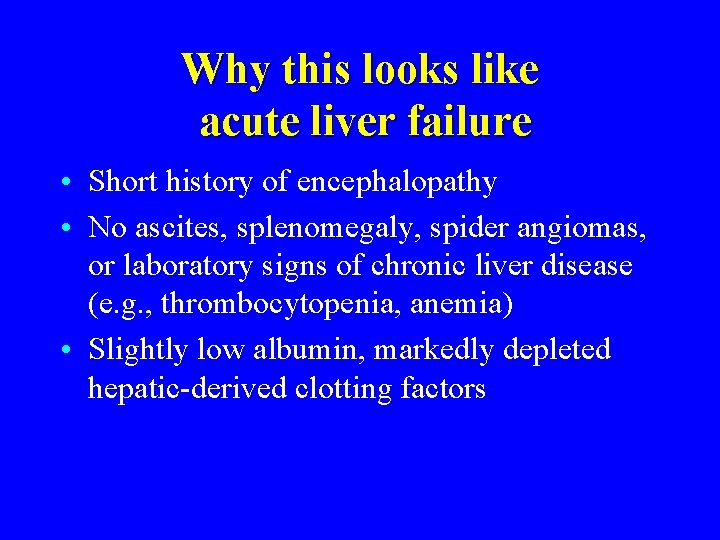
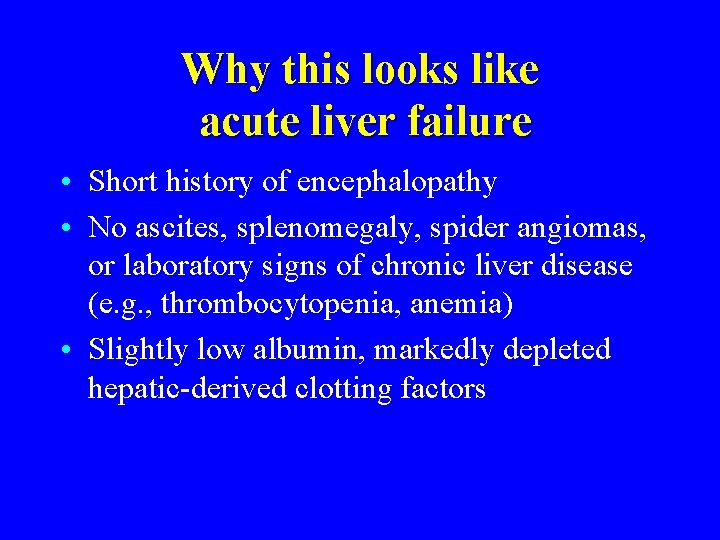
Why this looks like acute liver failure • Short history of encephalopathy • No ascites, splenomegaly, spider angiomas, or laboratory signs of chronic liver disease (e. g. , thrombocytopenia, anemia) • Slightly low albumin, markedly depleted hepatic-derived clotting factors
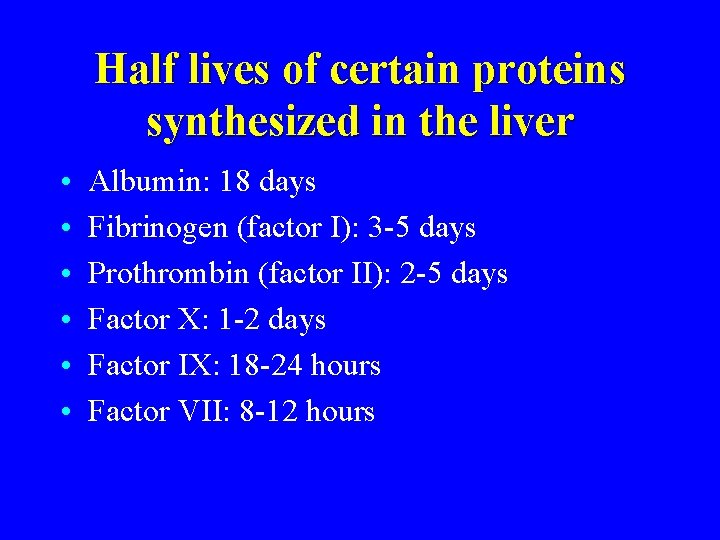
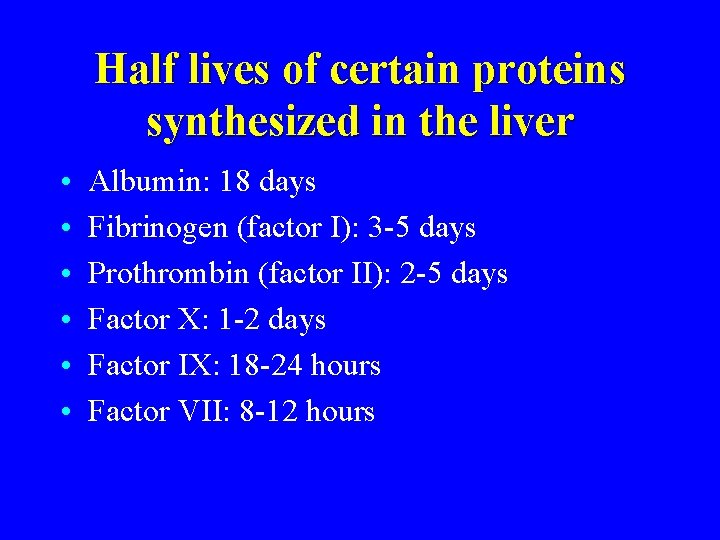
Half lives of certain proteins synthesized in the liver • • • Albumin: 18 days Fibrinogen (factor I): 3 -5 days Prothrombin (factor II): 2 -5 days Factor X: 1 -2 days Factor IX: 18 -24 hours Factor VII: 8 -12 hours
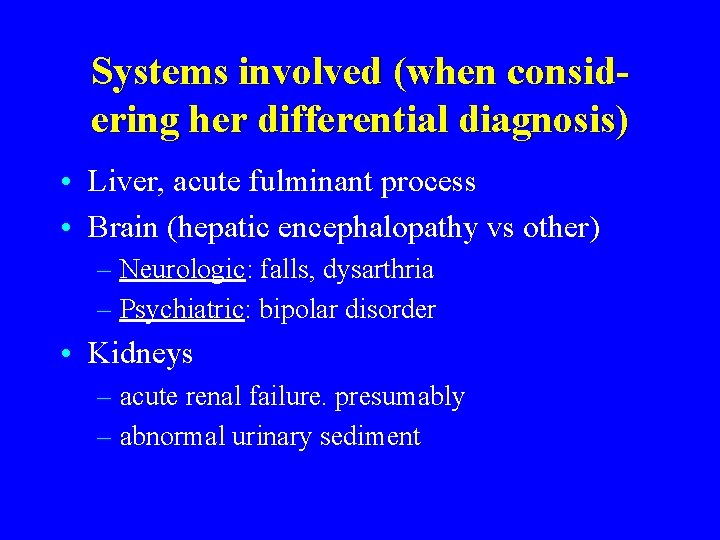
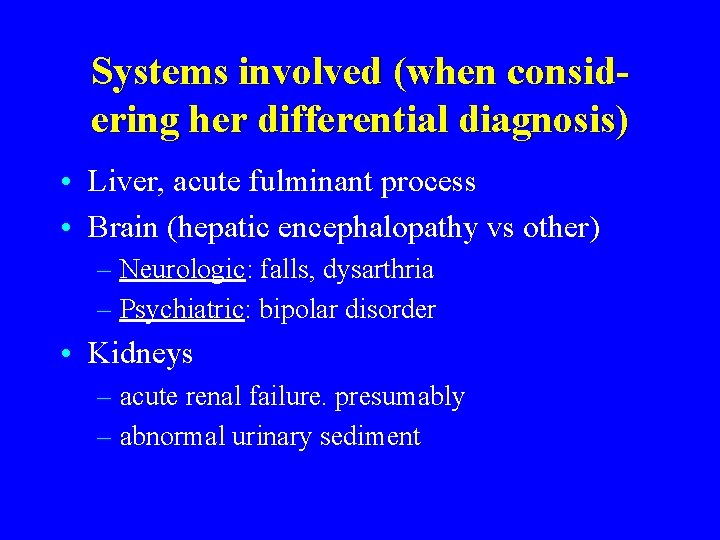
Systems involved (when considering her differential diagnosis) • Liver, acute fulminant process • Brain (hepatic encephalopathy vs other) – Neurologic: falls, dysarthria – Psychiatric: bipolar disorder • Kidneys – acute renal failure. presumably – abnormal urinary sediment
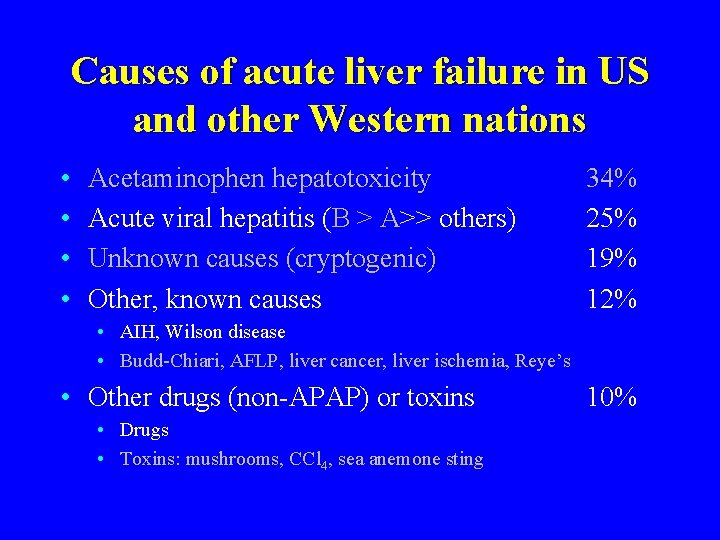
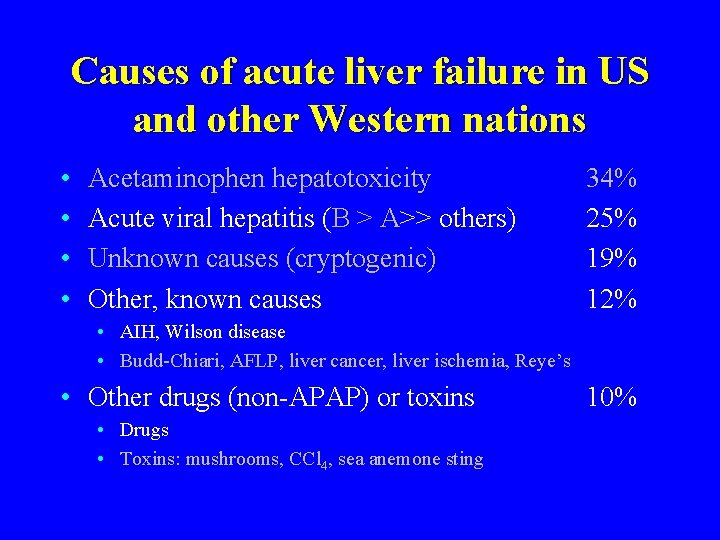
Causes of acute liver failure in US and other Western nations • • Acetaminophen hepatotoxicity Acute viral hepatitis (B > A>> others) Unknown causes (cryptogenic) Other, known causes 34% 25% 19% 12% • AIH, Wilson disease • Budd-Chiari, AFLP, liver cancer, liver ischemia, Reye’s • Other drugs (non-APAP) or toxins • Drugs • Toxins: mushrooms, CCl 4, sea anemone sting 10%
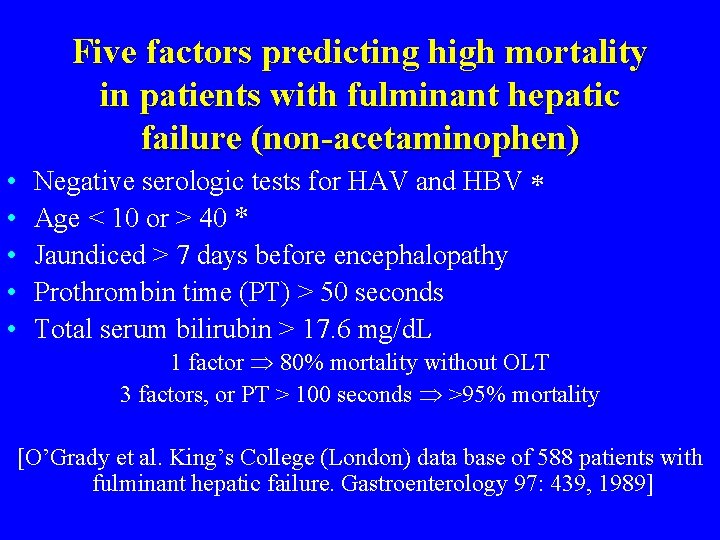
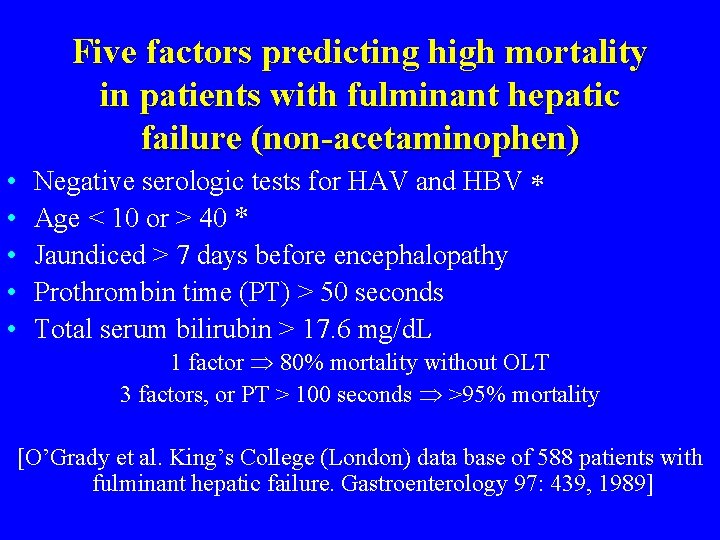
Five factors predicting high mortality in patients with fulminant hepatic failure (non-acetaminophen) • • • Negative serologic tests for HAV and HBV Age < 10 or > 40 * Jaundiced > 7 days before encephalopathy Prothrombin time (PT) > 50 seconds Total serum bilirubin > 17. 6 mg/d. L 1 factor 80% mortality without OLT 3 factors, or PT > 100 seconds >95% mortality [O’Grady et al. King’s College (London) data base of 588 patients with fulminant hepatic failure. Gastroenterology 97: 439, 1989]
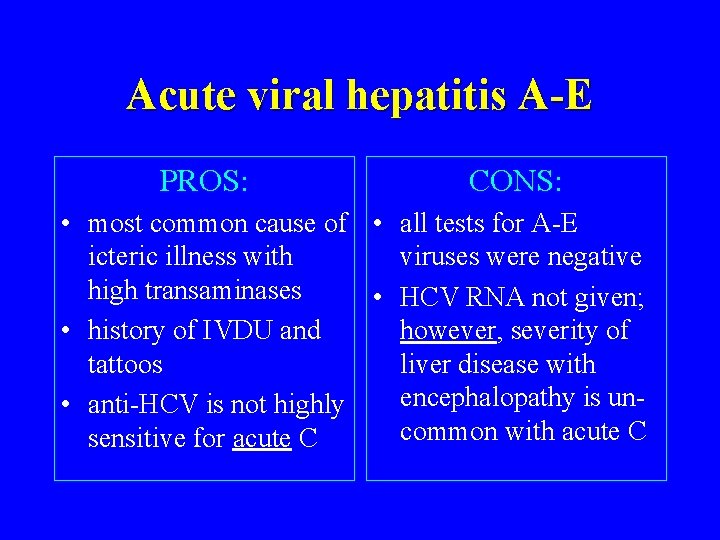
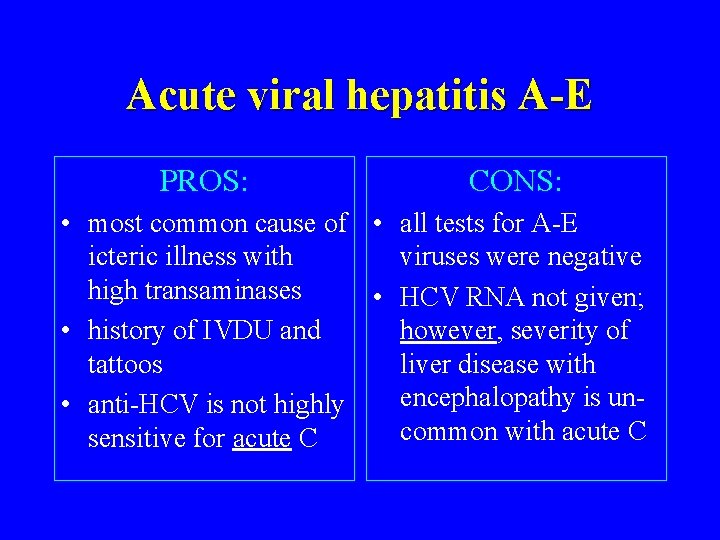
Acute viral hepatitis A-E PROS: CONS: • most common cause of • all tests for A-E icteric illness with viruses were negative high transaminases • HCV RNA not given; • history of IVDU and however, severity of tattoos liver disease with encephalopathy is un • anti-HCV is not highly common with acute C sensitive for acute C
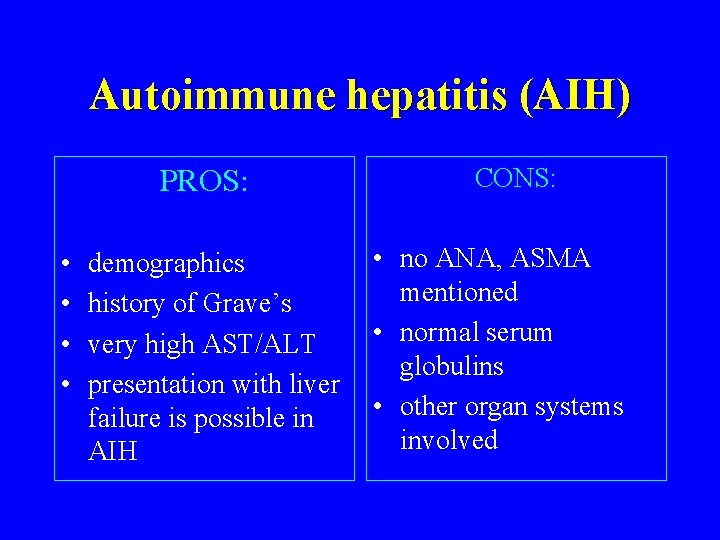
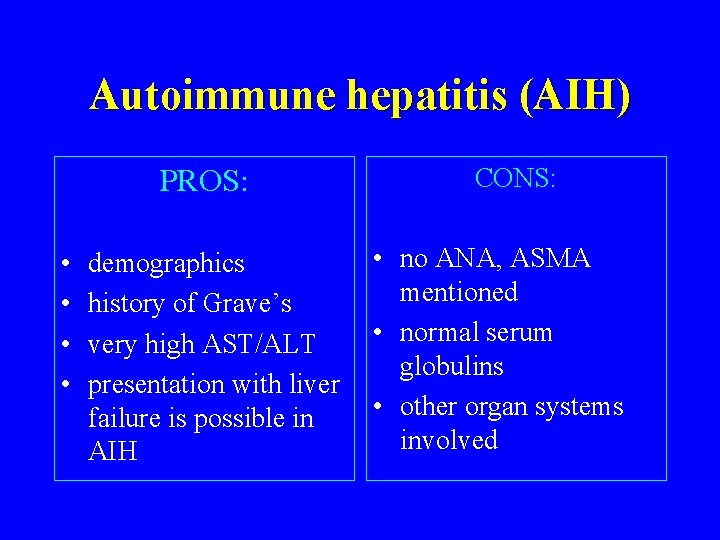
Autoimmune hepatitis (AIH) PROS: • • demographics history of Grave’s very high AST/ALT presentation with liver failure is possible in AIH CONS: • no ANA, ASMA mentioned • normal serum globulins • other organ systems involved
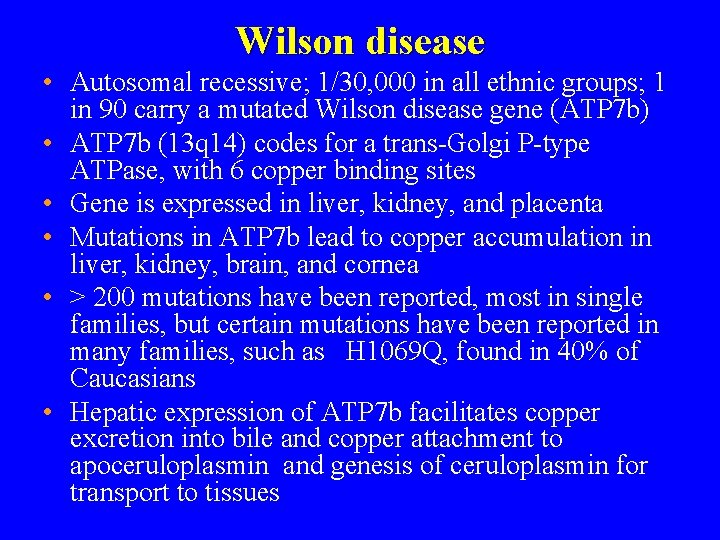
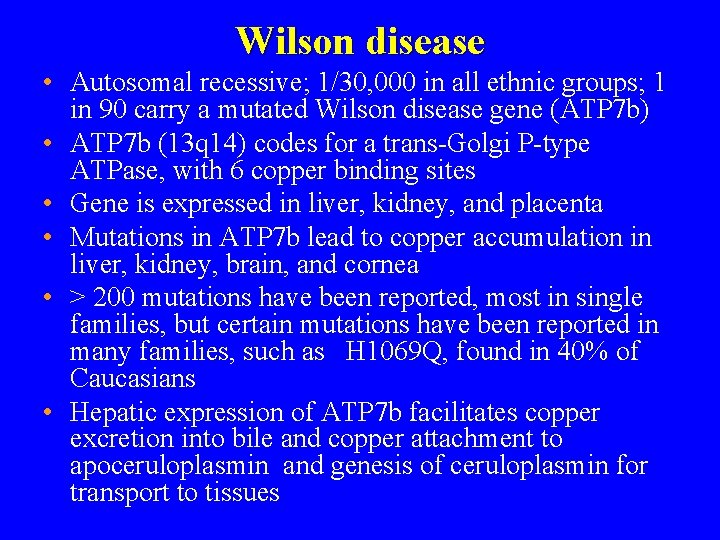
Wilson disease • Autosomal recessive; 1/30, 000 in all ethnic groups; 1 in 90 carry a mutated Wilson disease gene (ATP 7 b) • ATP 7 b (13 q 14) codes for a trans-Golgi P-type ATPase, with 6 copper binding sites • Gene is expressed in liver, kidney, and placenta • Mutations in ATP 7 b lead to copper accumulation in liver, kidney, brain, and cornea • > 200 mutations have been reported, most in single families, but certain mutations have been reported in many families, such as H 1069 Q, found in 40% of Caucasians • Hepatic expression of ATP 7 b facilitates copper excretion into bile and copper attachment to apoceruloplasmin and genesis of ceruloplasmin for transport to tissues
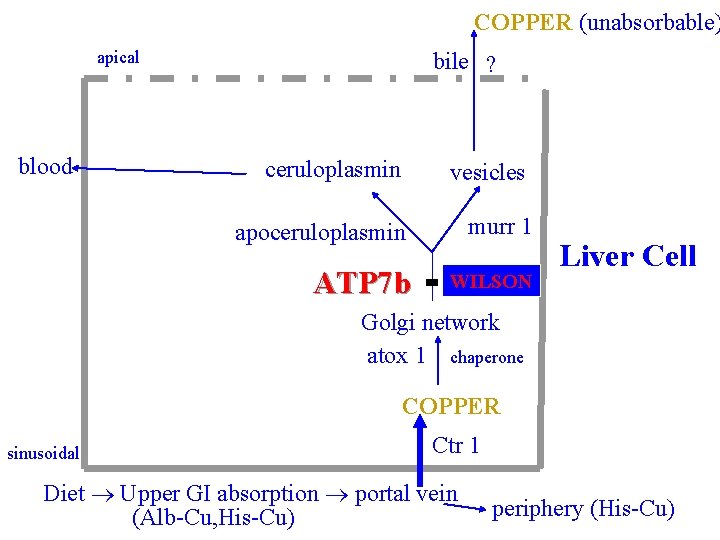
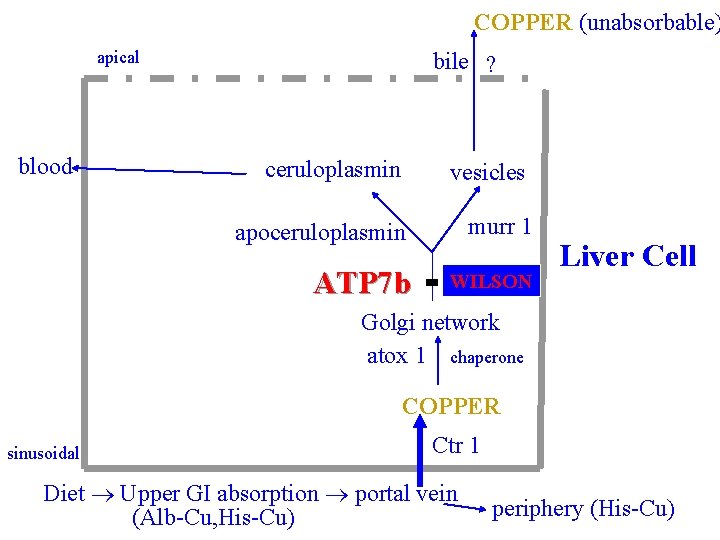
COPPER (unabsorbable) apical blood bile ? ceruloplasmin vesicles apoceruloplasmin murr 1 ATP 7 b WILSON Liver Cell Golgi network atox 1 chaperone COPPER sinusoidal Ctr 1 Diet Upper GI absorption portal vein (Alb-Cu, His-Cu) periphery (His-Cu)
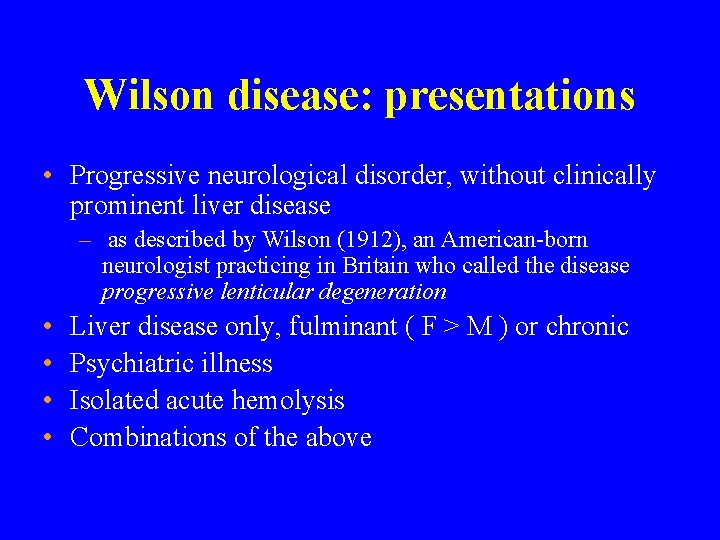
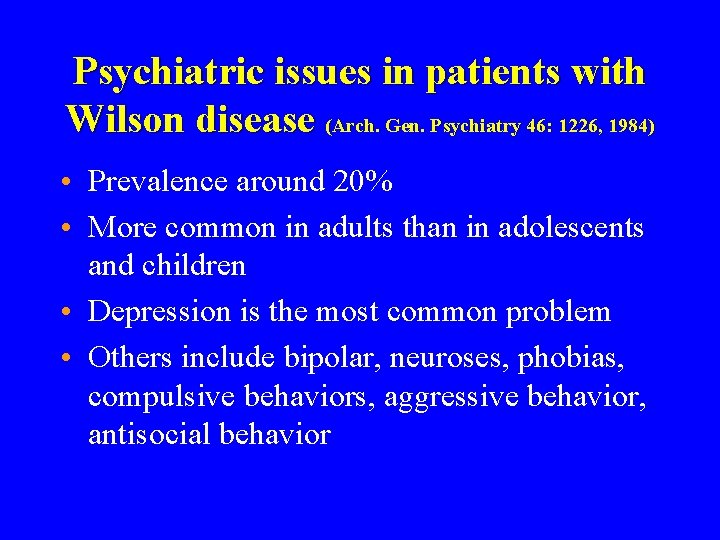
Wilson disease: presentations • Progressive neurological disorder, without clinically prominent liver disease – as described by Wilson (1912), an American-born neurologist practicing in Britain who called the disease progressive lenticular degeneration • • Liver disease only, fulminant ( F > M ) or chronic Psychiatric illness Isolated acute hemolysis Combinations of the above

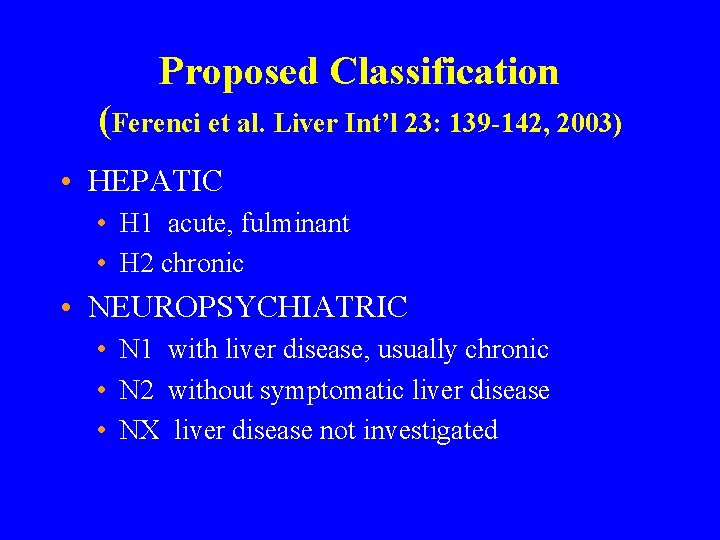
Proposed Classification (Ferenci et al. Liver Int’l 23: 139 -142, 2003) • HEPATIC • H 1 acute, fulminant • H 2 chronic • NEUROPSYCHIATRIC • N 1 with liver disease, usually chronic • N 2 without symptomatic liver disease • NX liver disease not investigated
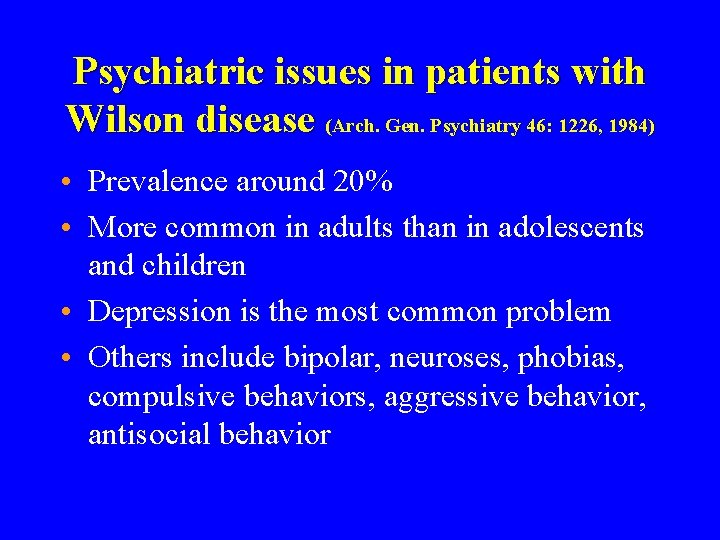
Psychiatric issues in patients with Wilson disease (Arch. Gen. Psychiatry 46: 1226, 1984) • Prevalence around 20% • More common in adults than in adolescents and children • Depression is the most common problem • Others include bipolar, neuroses, phobias, compulsive behaviors, aggressive behavior, antisocial behavior
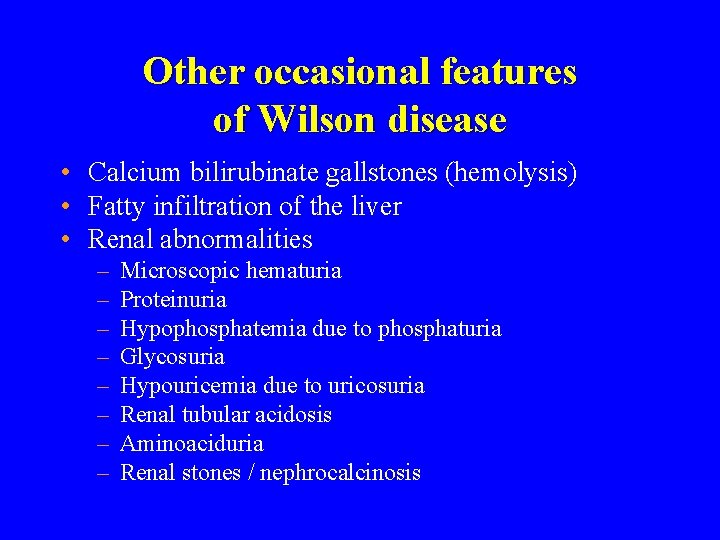
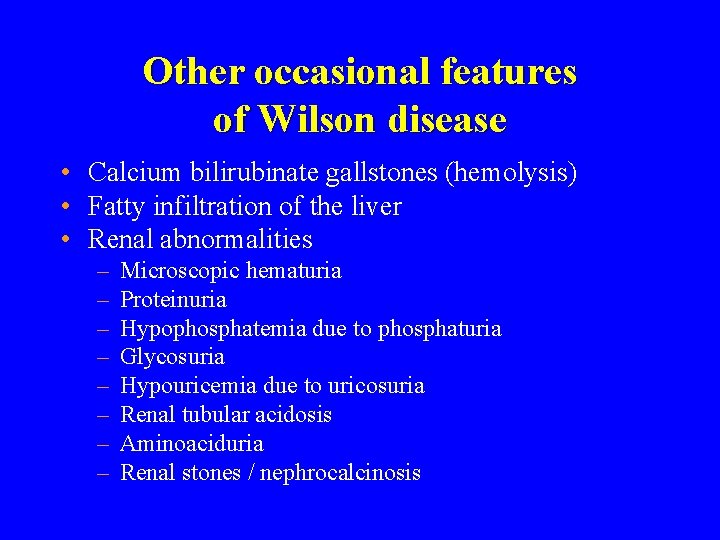
Other occasional features of Wilson disease • Calcium bilirubinate gallstones (hemolysis) • Fatty infiltration of the liver • Renal abnormalities – – – – Microscopic hematuria Proteinuria Hypophosphatemia due to phosphaturia Glycosuria Hypouricemia due to uricosuria Renal tubular acidosis Aminoaciduria Renal stones / nephrocalcinosis
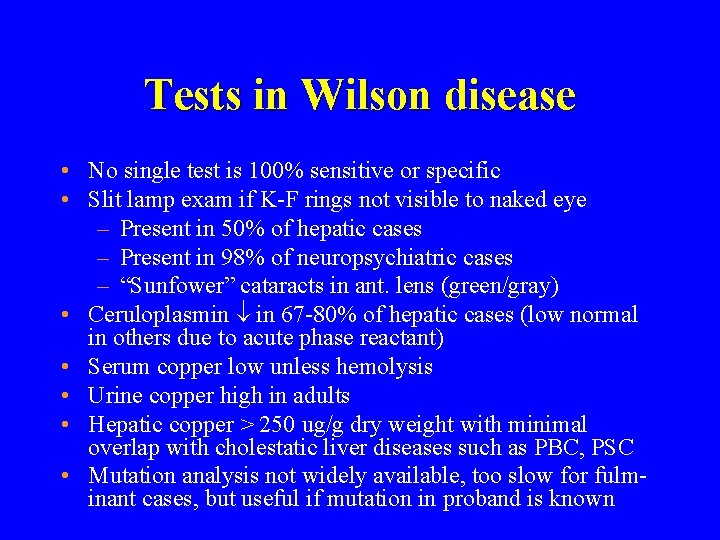
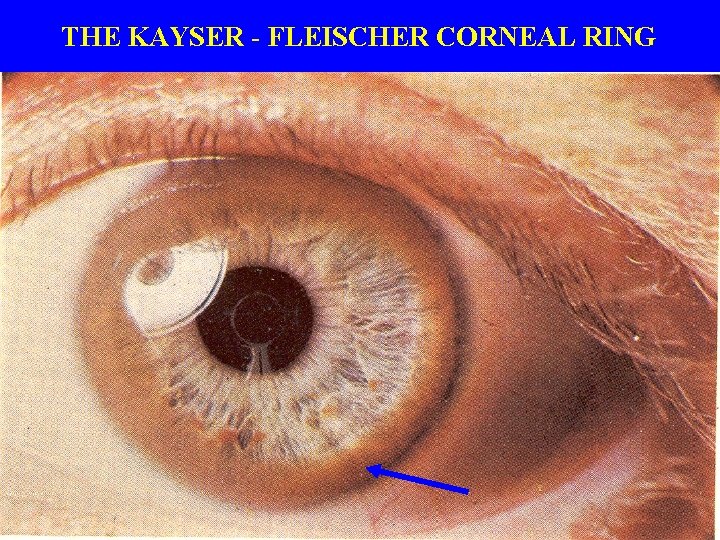
Tests in Wilson disease • No single test is 100% sensitive or specific • Slit lamp exam if K-F rings not visible to naked eye – Present in 50% of hepatic cases – Present in 98% of neuropsychiatric cases – “Sunfower” cataracts in ant. lens (green/gray) • Ceruloplasmin in 67 -80% of hepatic cases (low normal in others due to acute phase reactant) • Serum copper low unless hemolysis • Urine copper high in adults • Hepatic copper > 250 ug/g dry weight with minimal overlap with cholestatic liver diseases such as PBC, PSC • Mutation analysis not widely available, too slow for fulminant cases, but useful if mutation in proband is known

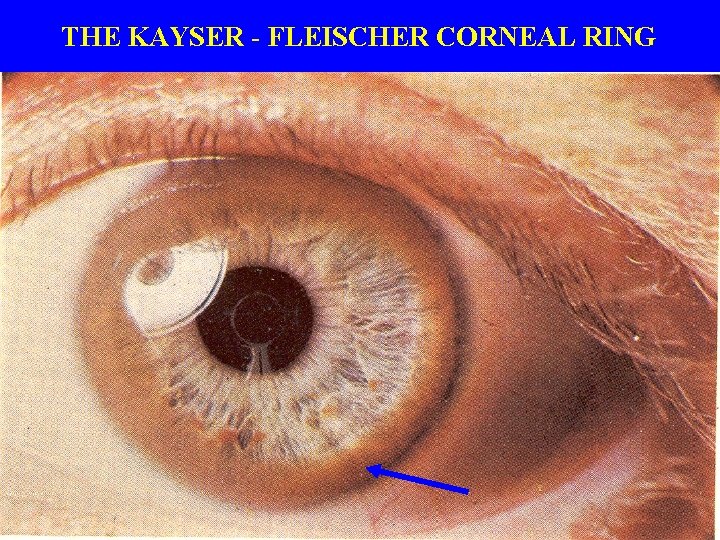
THE KAYSER - FLEISCHER CORNEAL RING
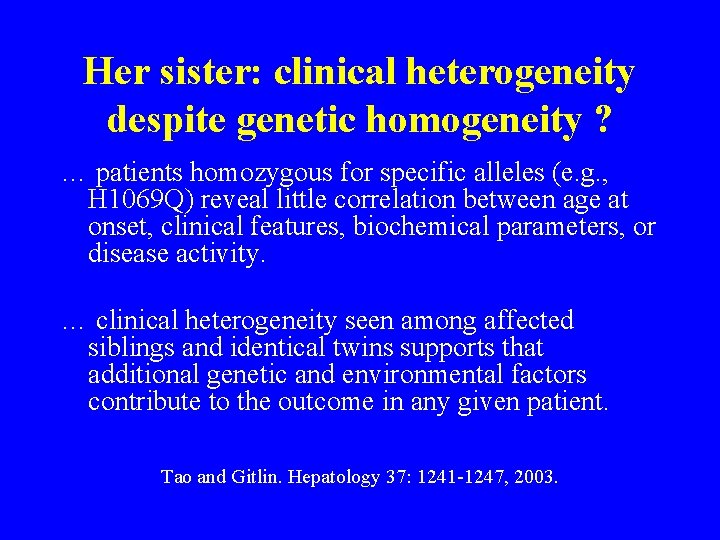
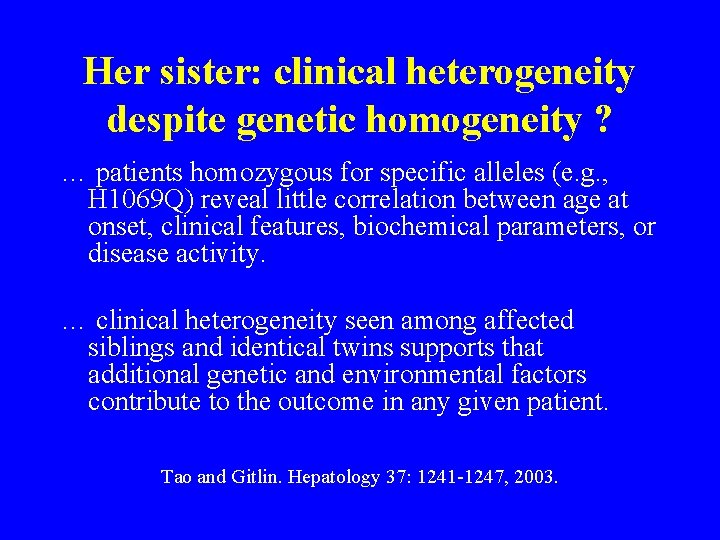
Her sister: clinical heterogeneity despite genetic homogeneity ? … patients homozygous for specific alleles (e. g. , H 1069 Q) reveal little correlation between age at onset, clinical features, biochemical parameters, or disease activity. … clinical heterogeneity seen among affected siblings and identical twins supports that additional genetic and environmental factors contribute to the outcome in any given patient. Tao and Gitlin. Hepatology 37: 1241 -1247, 2003.
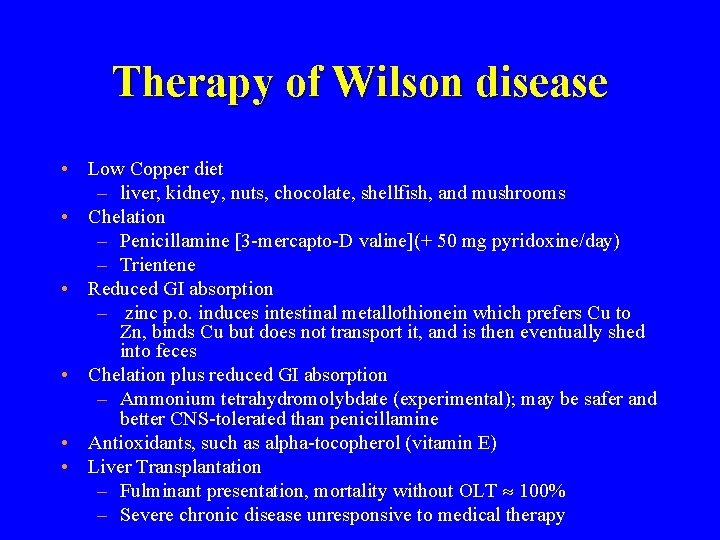
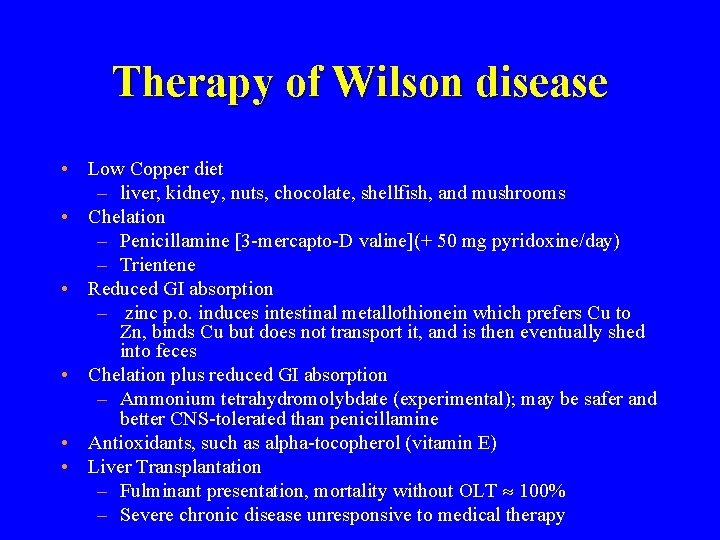
Therapy of Wilson disease • Low Copper diet – liver, kidney, nuts, chocolate, shellfish, and mushrooms • Chelation – Penicillamine [3 -mercapto-D valine](+ 50 mg pyridoxine/day) – Trientene • Reduced GI absorption – zinc p. o. induces intestinal metallothionein which prefers Cu to Zn, binds Cu but does not transport it, and is then eventually shed into feces • Chelation plus reduced GI absorption – Ammonium tetrahydromolybdate (experimental); may be safer and better CNS-tolerated than penicillamine • Antioxidants, such as alpha-tocopherol (vitamin E) • Liver Transplantation – Fulminant presentation, mortality without OLT 100% – Severe chronic disease unresponsive to medical therapy

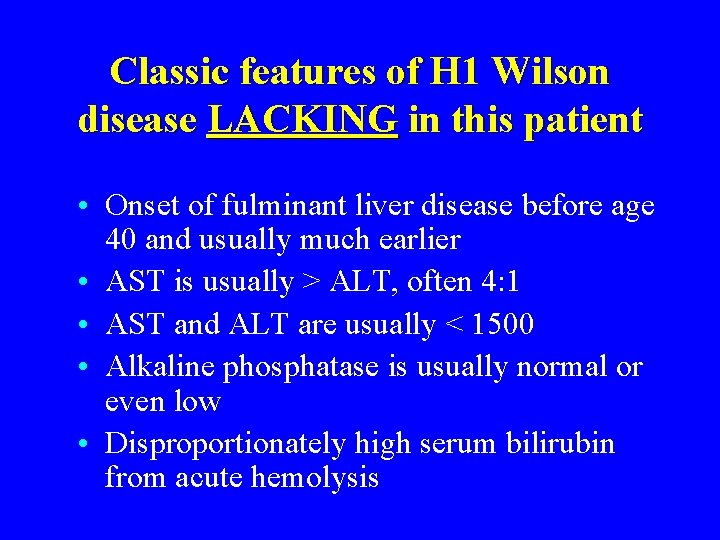
Wilson disease PROS: • Fulminant hepatic failure presentation • Sister died age 14 of fulminant disease • Concomitant neuropsychiatric and renal abnormalities CONS: • Many classic features of Wilson disease are lacking in this patient
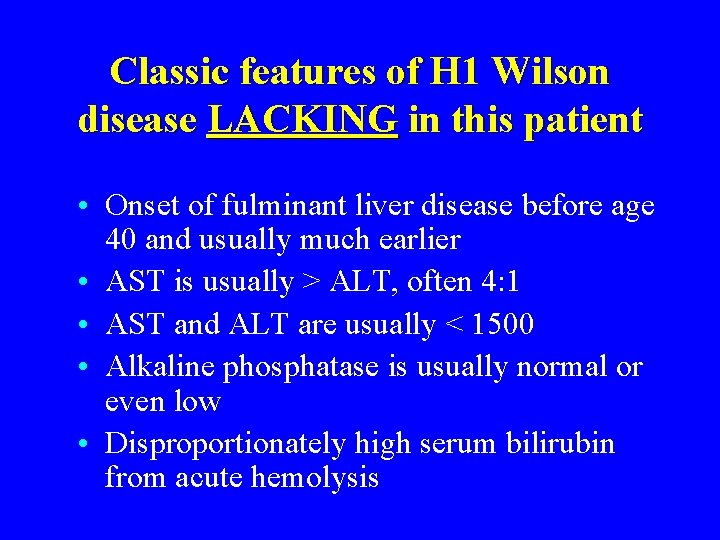
Classic features of H 1 Wilson disease LACKING in this patient • Onset of fulminant liver disease before age 40 and usually much earlier • AST is usually > ALT, often 4: 1 • AST and ALT are usually < 1500 • Alkaline phosphatase is usually normal or even low • Disproportionately high serum bilirubin from acute hemolysis
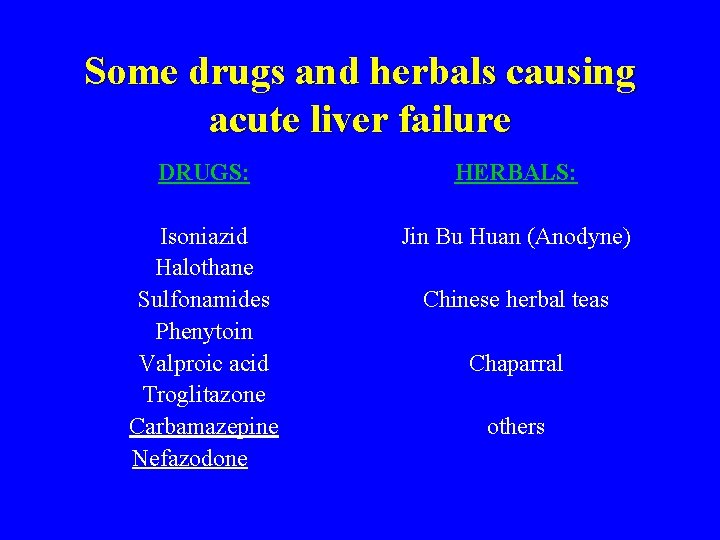
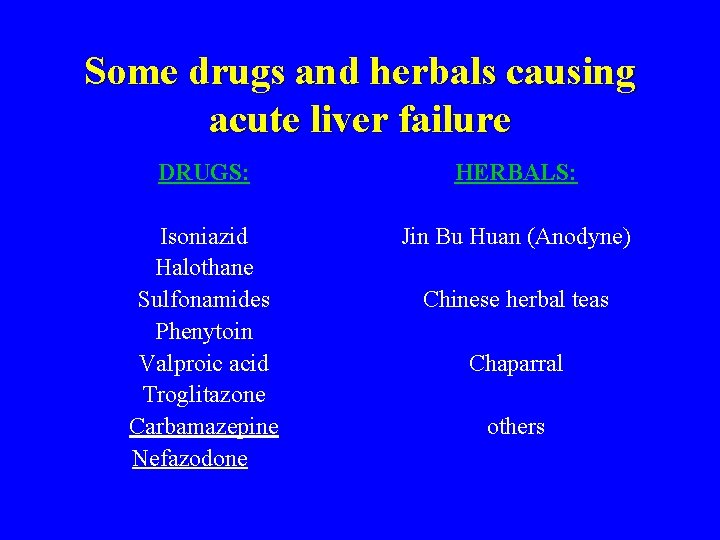
Some drugs and herbals causing acute liver failure DRUGS: HERBALS: Isoniazid Halothane Sulfonamides Phenytoin Valproic acid Troglitazone Carbamazepine Nefazodone Jin Bu Huan (Anodyne) Chinese herbal teas Chaparral others
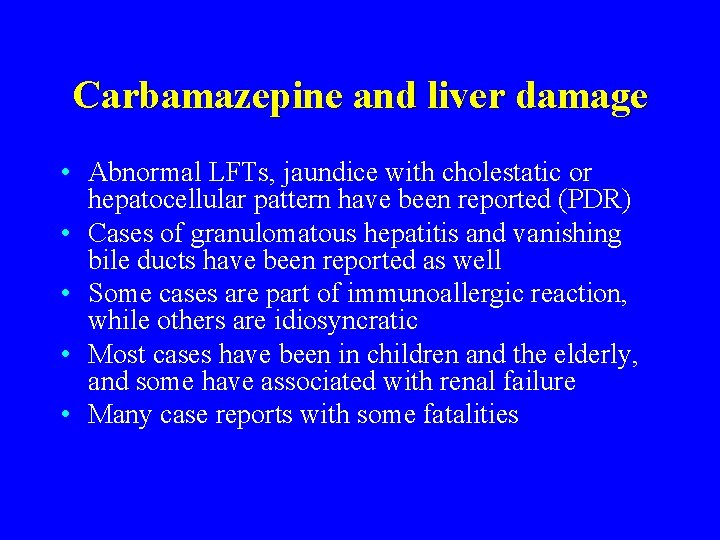
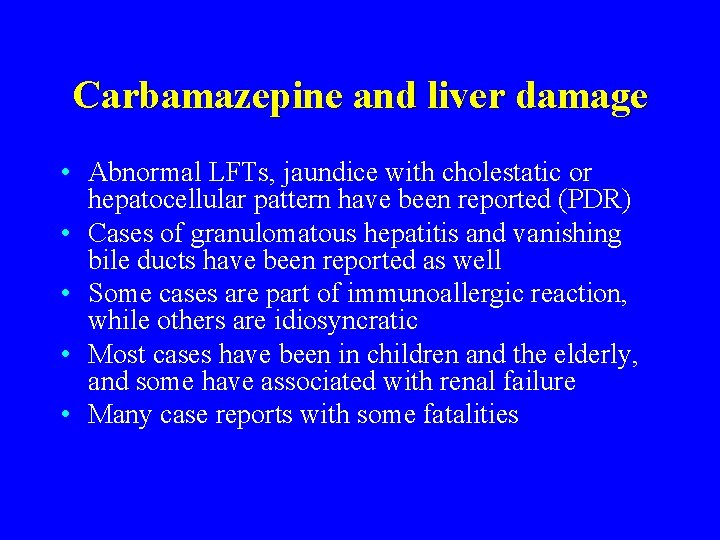
Carbamazepine and liver damage • Abnormal LFTs, jaundice with cholestatic or hepatocellular pattern have been reported (PDR) • Cases of granulomatous hepatitis and vanishing bile ducts have been reported as well • Some cases are part of immunoallergic reaction, while others are idiosyncratic • Most cases have been in children and the elderly, and some have associated with renal failure • Many case reports with some fatalities
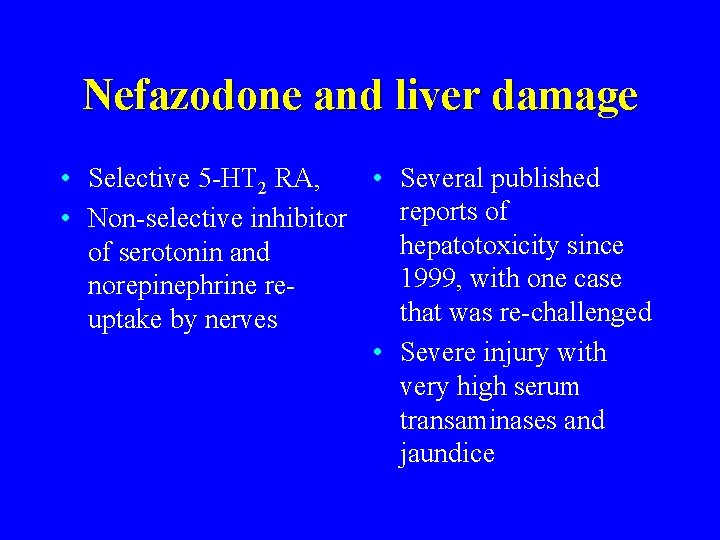
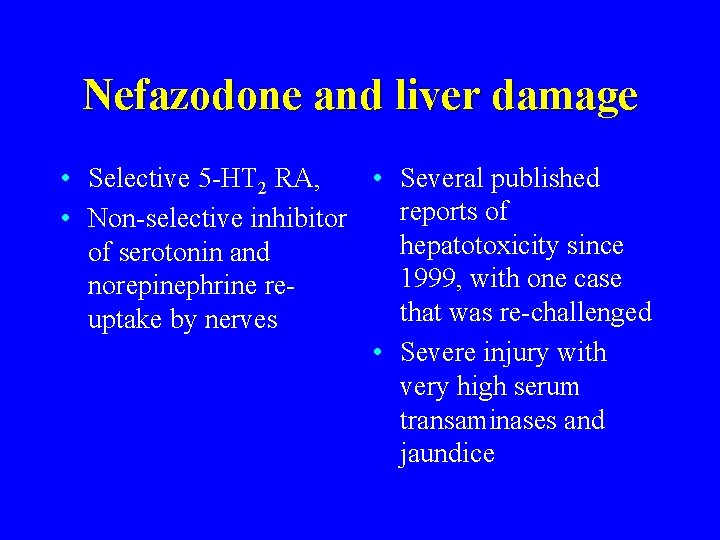
Nefazodone and liver damage • Selective 5 -HT 2 RA, • Several published reports of • Non-selective inhibitor hepatotoxicity since of serotonin and 1999, with one case norepinephrine rethat was re-challenged uptake by nerves • Severe injury with very high serum transaminases and jaundice
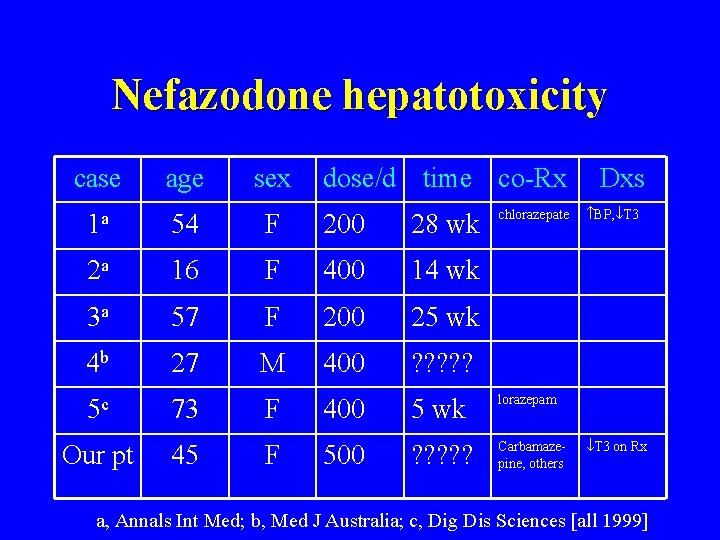
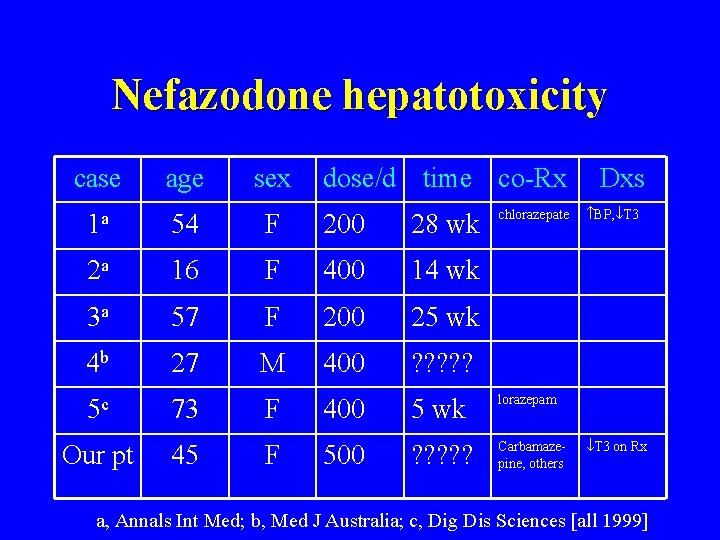
Nefazodone hepatotoxicity case age sex dose/d time co-Rx chlorazepate 1 a 54 F 200 28 wk 2 a 16 F 400 14 wk 3 a 57 F 200 25 wk 4 b 27 M 400 ? ? ? 5 c 73 F 400 5 wk lorazepam ? ? ? Carbamazepine, others Our pt 45 F 500 Dxs BP, T 3 on Rx a, Annals Int Med; b, Med J Australia; c, Dig Dis Sciences [all 1999]
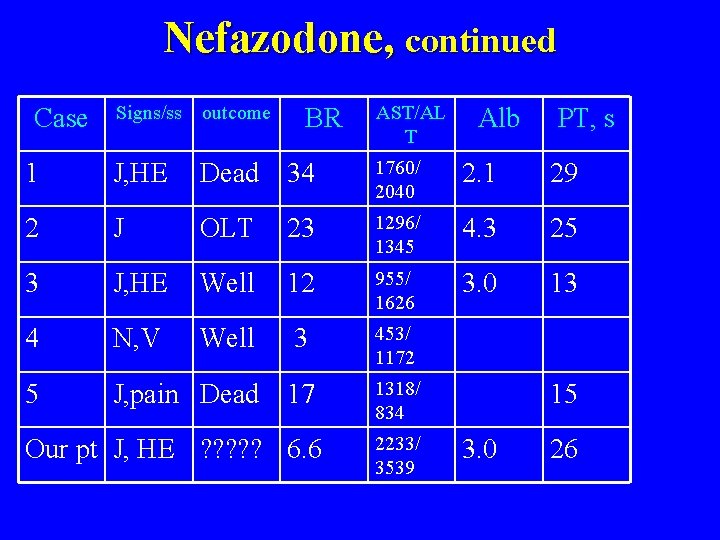
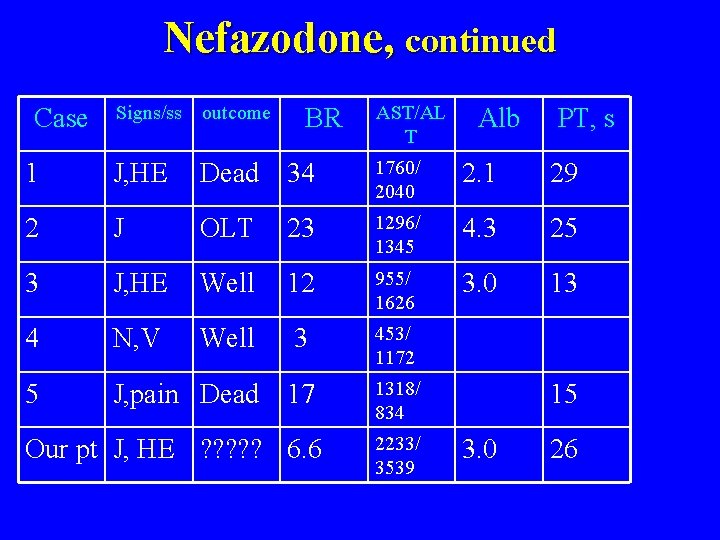
Nefazodone, continued Signs/ss outcome 1 J, HE Dead 34 1760/ 2040 2. 1 29 2 J OLT 23 1296/ 1345 4. 3 25 3 J, HE Well 12 955/ 1626 3. 0 13 4 N, V Well 3 453/ 1172 5 J, pain Dead 17 1318/ 834 Case BR Our pt J, HE ? ? ? 6. 6 AST/AL T 2233/ 3539 Alb PT, s 15 3. 0 26
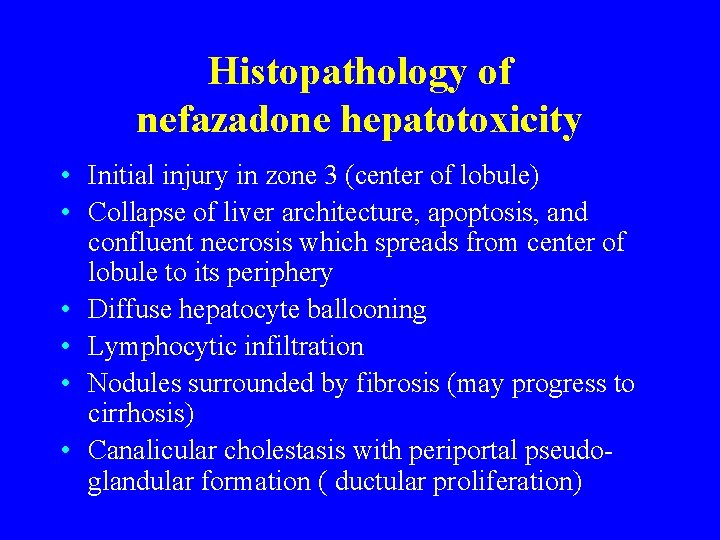
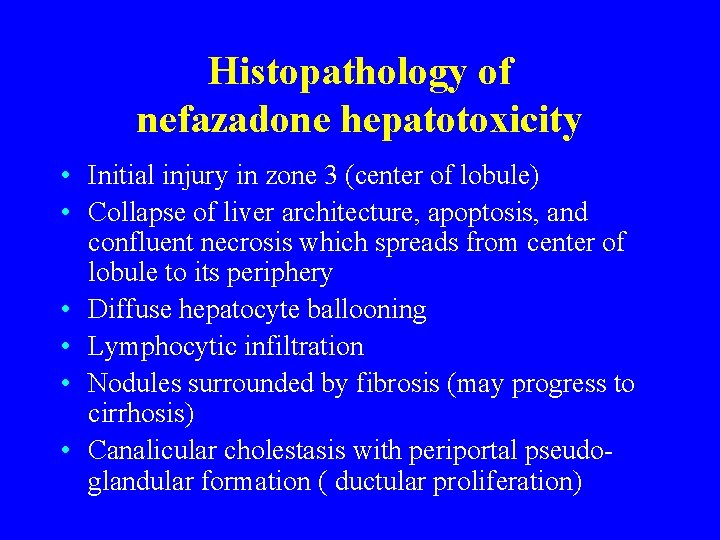
Histopathology of nefazadone hepatotoxicity • Initial injury in zone 3 (center of lobule) • Collapse of liver architecture, apoptosis, and confluent necrosis which spreads from center of lobule to its periphery • Diffuse hepatocyte ballooning • Lymphocytic infiltration • Nodules surrounded by fibrosis (may progress to cirrhosis) • Canalicular cholestasis with periportal pseudoglandular formation ( ductular proliferation)
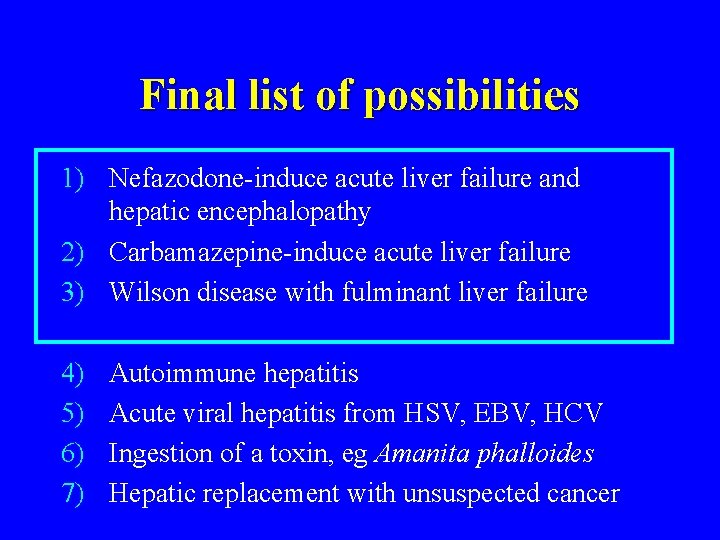
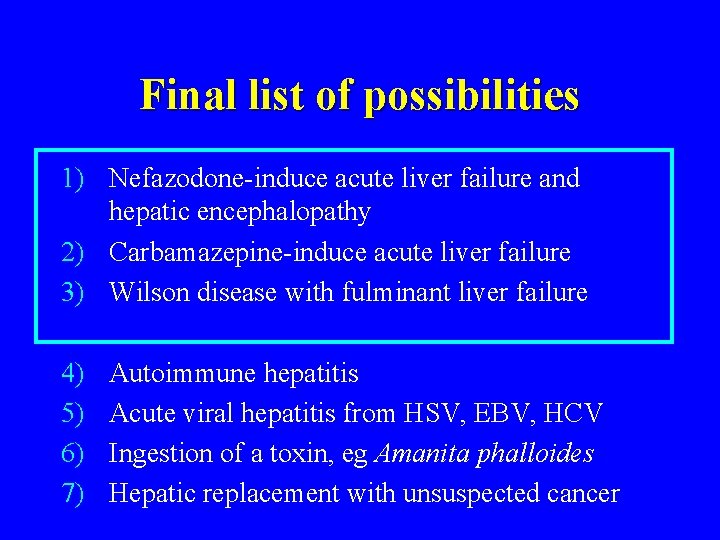
Final list of possibilities 1) Nefazodone-induce acute liver failure and hepatic encephalopathy 2) Carbamazepine-induce acute liver failure 3) Wilson disease with fulminant liver failure 4) 5) 6) 7) Autoimmune hepatitis Acute viral hepatitis from HSV, EBV, HCV Ingestion of a toxin, eg Amanita phalloides Hepatic replacement with unsuspected cancer
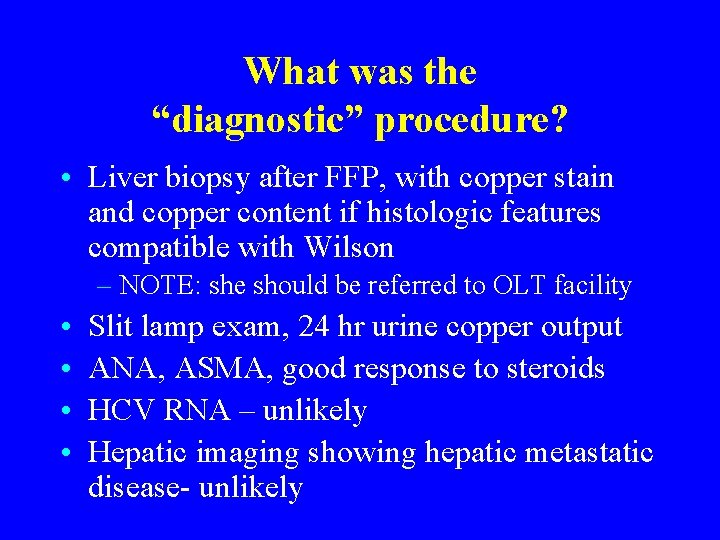
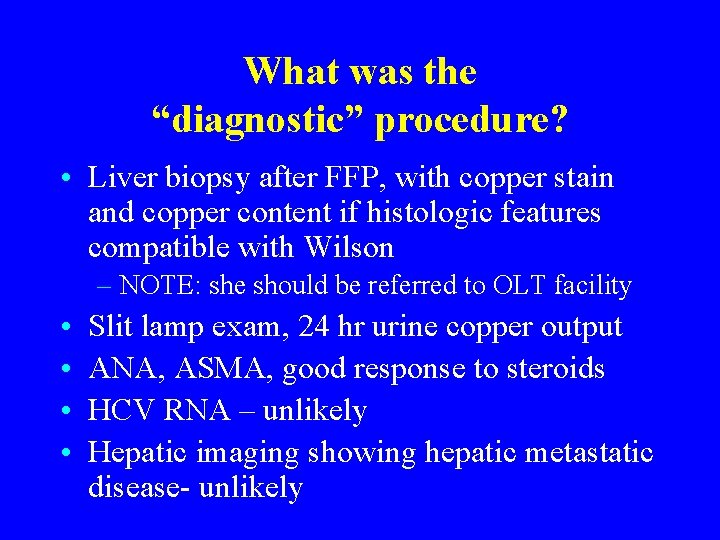
What was the “diagnostic” procedure? • Liver biopsy after FFP, with copper stain and copper content if histologic features compatible with Wilson – NOTE: she should be referred to OLT facility • • Slit lamp exam, 24 hr urine copper output ANA, ASMA, good response to steroids HCV RNA – unlikely Hepatic imaging showing hepatic metastatic disease- unlikely

CPC as cinema. It’s show time!

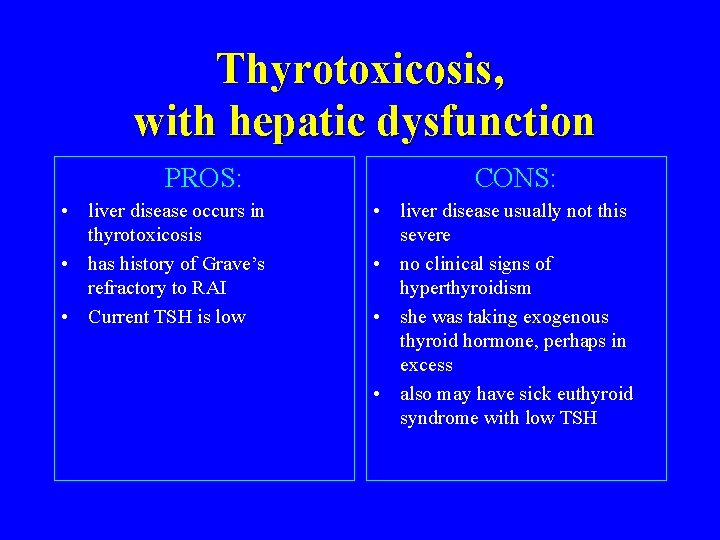
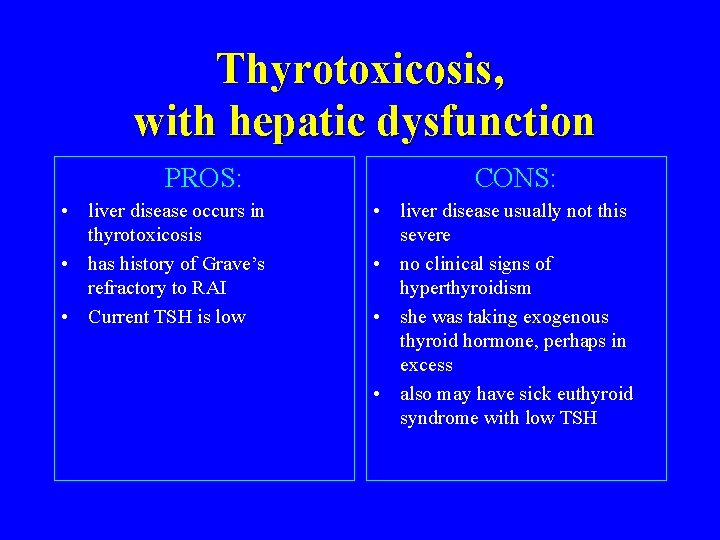
Thyrotoxicosis, with hepatic dysfunction PROS: • liver disease occurs in thyrotoxicosis • has history of Grave’s refractory to RAI • Current TSH is low CONS: • liver disease usually not this severe • no clinical signs of hyperthyroidism • she was taking exogenous thyroid hormone, perhaps in excess • also may have sick euthyroid syndrome with low TSH
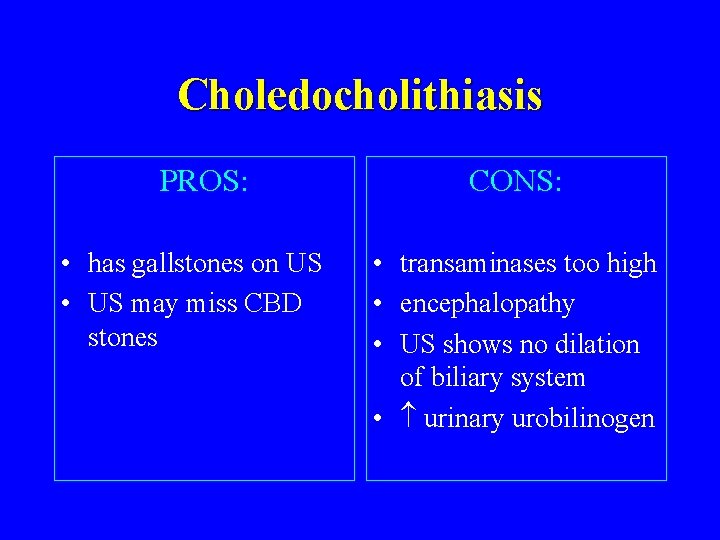
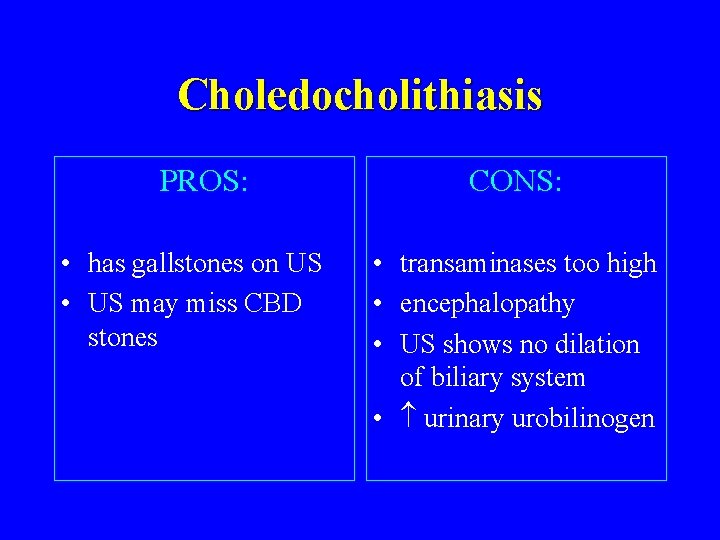
Choledocholithiasis PROS: • has gallstones on US • US may miss CBD stones CONS: • transaminases too high • encephalopathy • US shows no dilation of biliary system • urinary urobilinogen
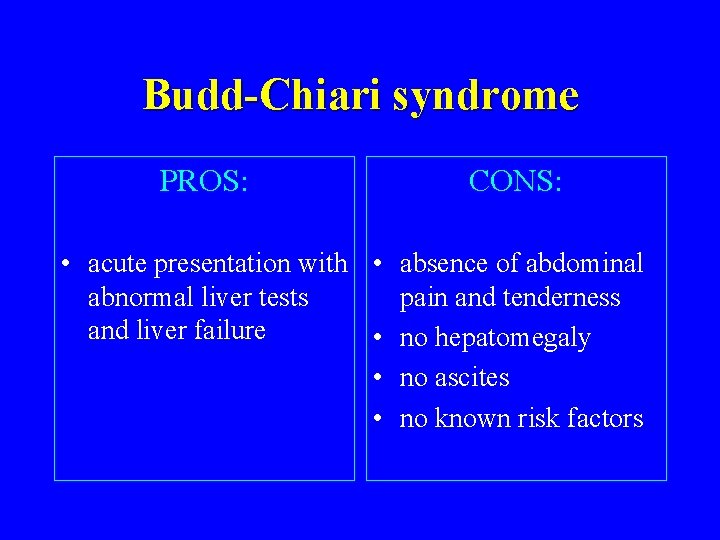
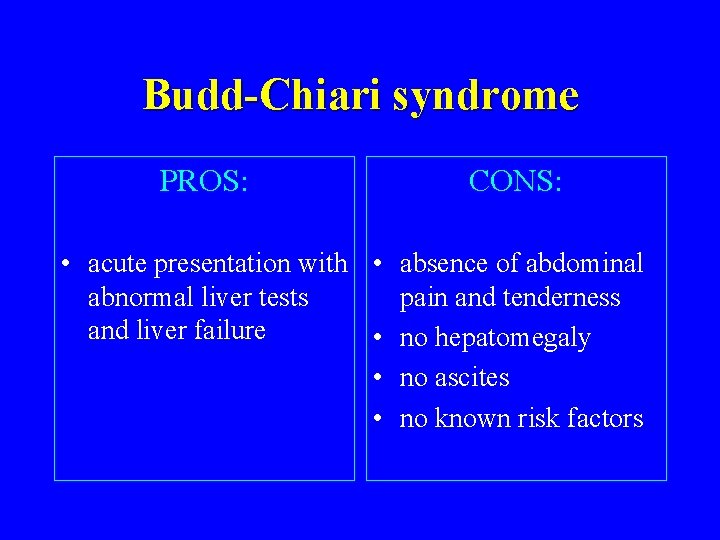
Budd-Chiari syndrome PROS: CONS: • acute presentation with • absence of abdominal abnormal liver tests pain and tenderness and liver failure • no hepatomegaly • no ascites • no known risk factors
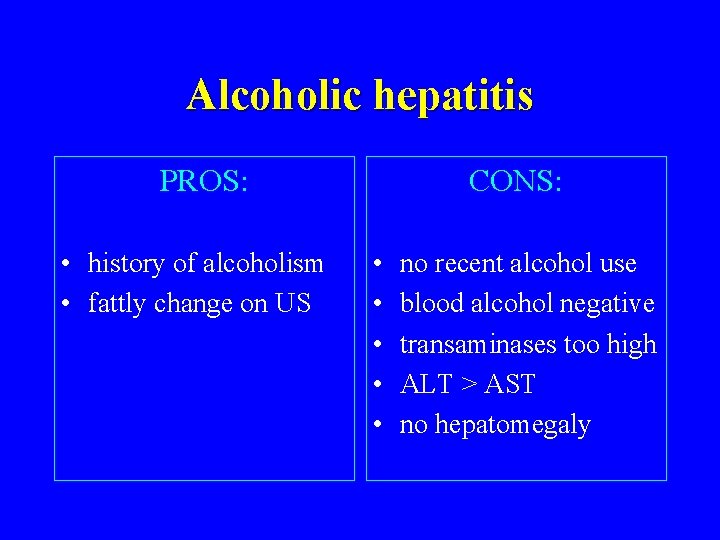
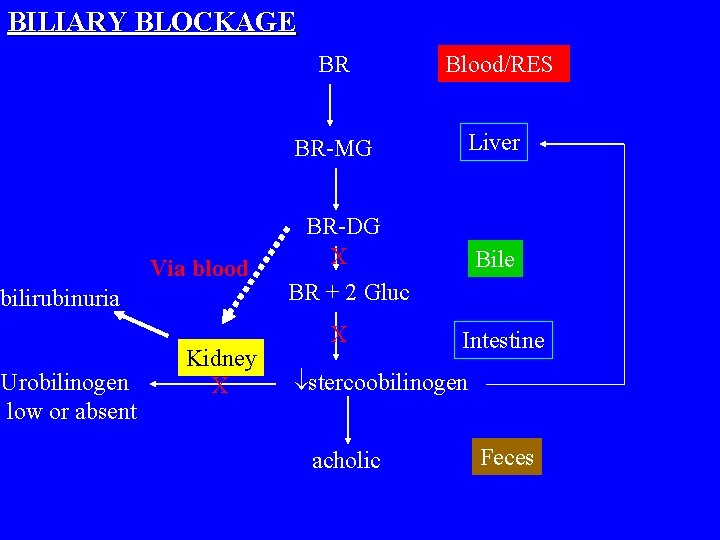
Alcoholic hepatitis PROS: • history of alcoholism • fattly change on US CONS: • • • no recent alcohol use blood alcohol negative transaminases too high ALT > AST no hepatomegaly

NAFLD / NASH • • PROS: CONS: not currently drinking obese fatty liver on US ALT > AST • liver is not large • encephalopathy rare • transaminases too high
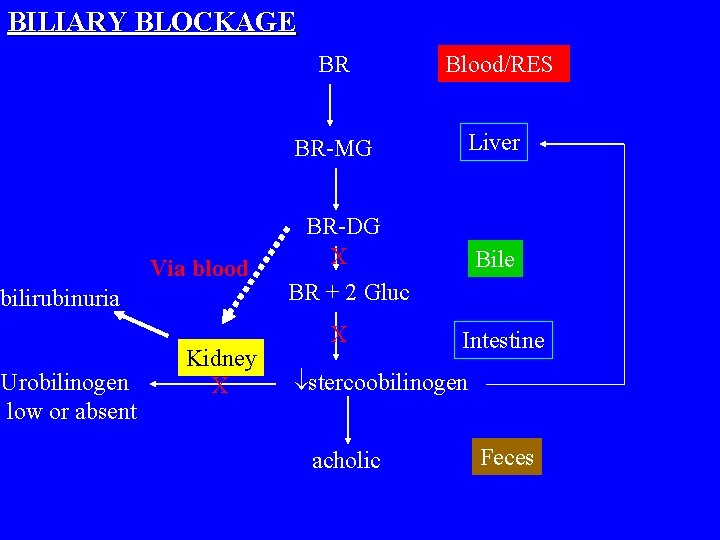
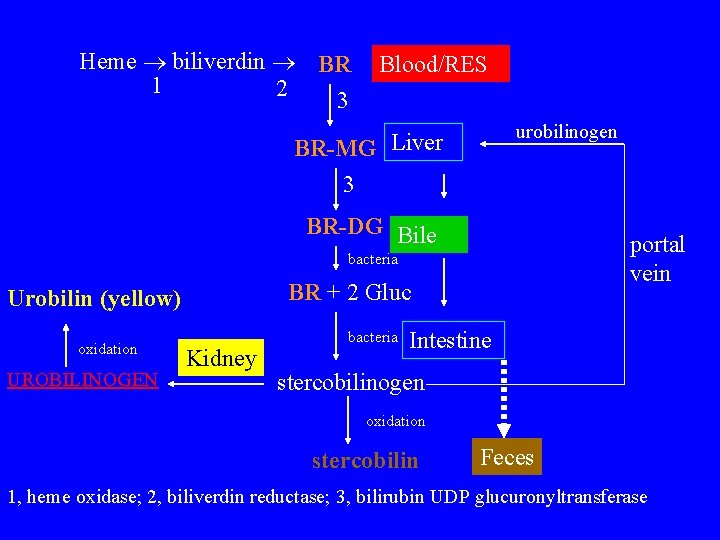
BILIARY BLOCKAGE Via blood bilirubinuria Urobilinogen low or absent Kidney X BR Blood/RES BR-MG Liver BR-DG X BR + 2 Gluc X Bile Intestine stercoobilinogen acholic Feces
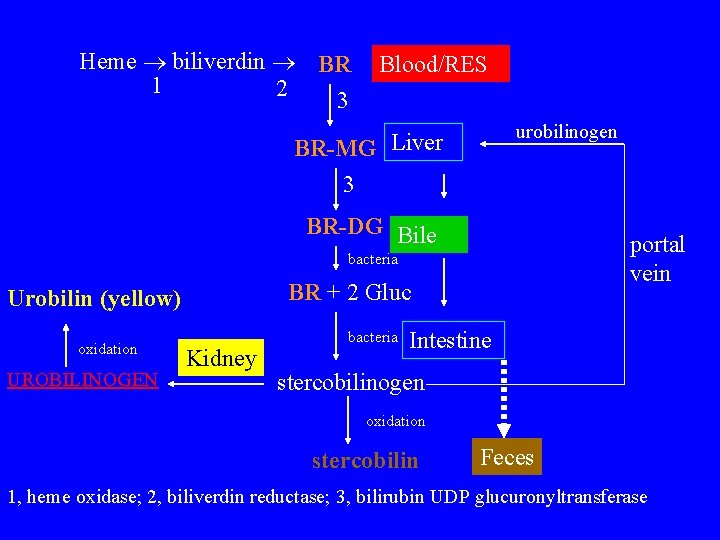
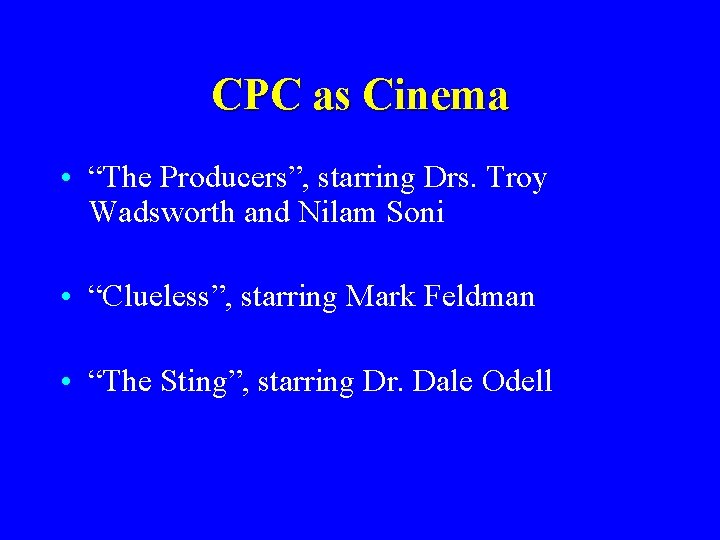
Heme biliverdin BR 1 2 3 Blood/RES urobilinogen BR-MG Liver 3 BR-DG Bile portal vein bacteria BR + 2 Gluc Urobilin (yellow) oxidation UROBILINOGEN Kidney bacteria Intestine stercobilinogen oxidation stercobilin Feces 1, heme oxidase; 2, biliverdin reductase; 3, bilirubin UDP glucuronyltransferase
 La vrit
La vrit Drs atypique
Drs atypique Pendapat dari drs. wasty soemanto, m.pd
Pendapat dari drs. wasty soemanto, m.pd Drs.wa.gov/oaa
Drs.wa.gov/oaa Temple university drs
Temple university drs Melanie cosby
Melanie cosby Score de heart
Score de heart Drs hardwarezone
Drs hardwarezone Cisco drs backup
Cisco drs backup Drs
Drs Amalgaamafscheider
Amalgaamafscheider Drs abcdefg
Drs abcdefg Dr koh and trory
Dr koh and trory Dr grace ng
Dr grace ng Cpc long range forecast
Cpc long range forecast Introduction to cpc
Introduction to cpc Noaa corps cpc
Noaa corps cpc Testamento particular novo cpc
Testamento particular novo cpc Cab abstracts ebsco
Cab abstracts ebsco Art 294 a 311 novo cpc
Art 294 a 311 novo cpc Imprimir rup
Imprimir rup Artigo 775 cpc
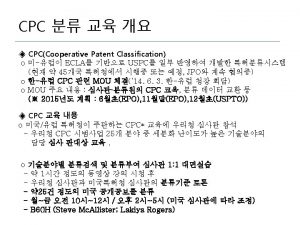
Artigo 775 cpc Cpc vs ipc
Cpc vs ipc Cpc 02
Cpc 02 Cpc pathology
Cpc pathology Cpc moodle
Cpc moodle Cpc monitoring
Cpc monitoring Art. 131 cpc
Art. 131 cpc Cpc pna
Cpc pna Cpc assessment tools
Cpc assessment tools Artigo 775 cpc
Artigo 775 cpc Cpc vale do rio doce
Cpc vale do rio doce Importancia de la demanda
Importancia de la demanda Organization corollary
Organization corollary Cpc cabi
Cpc cabi Noaa corps cpc
Noaa corps cpc Que es c.p.c. en contabilidad
Que es c.p.c. en contabilidad Gmod surfing
Gmod surfing Prazo para abertura de inventário novo cpc
Prazo para abertura de inventário novo cpc Art 610 cpc
Art 610 cpc Prezentare google
Prezentare google Cpc cpma
Cpc cpma Artigo 783 do cpc
Artigo 783 do cpc Fraude contra credores cpc
Fraude contra credores cpc Cpc cycle kelly
Cpc cycle kelly Ruy pereira camilo junior
Ruy pereira camilo junior