Clark County Nevada Understanding the Governance and County
- Slides: 29
Clark County Nevada Understanding the Governance and County Contributions of Public Hospitals Across the Country April 3, 2007
A Profile Of Hospitals Across The Country Project Overview and Approach University Medical Center Experience of Other Counties Summary 1
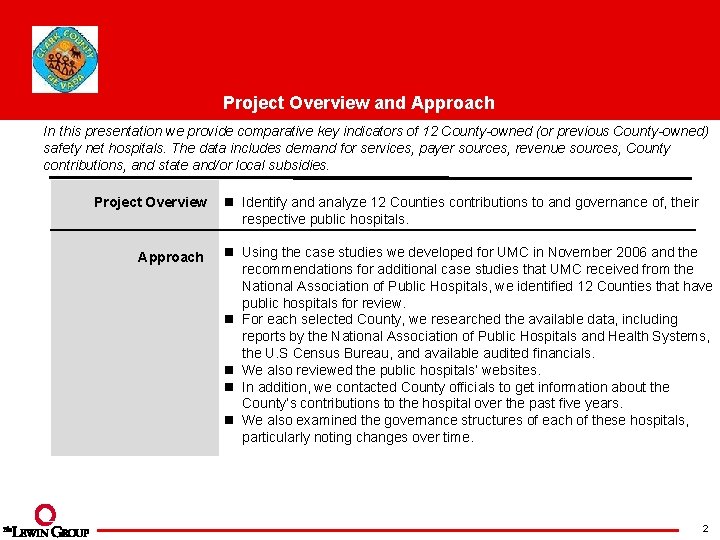
Project Overview and Approach In this presentation we provide comparative key indicators of 12 County-owned (or previous County-owned) safety net hospitals. The data includes demand for services, payer sources, revenue sources, County contributions, and state and/or local subsidies. Project Overview Approach n Identify and analyze 12 Counties contributions to and governance of, their respective public hospitals. n Using the case studies we developed for UMC in November 2006 and the recommendations for additional case studies that UMC received from the National Association of Public Hospitals, we identified 12 Counties that have public hospitals for review. n For each selected County, we researched the available data, including reports by the National Association of Public Hospitals and Health Systems, the U. S Census Bureau, and available audited financials. n We also reviewed the public hospitals’ websites. n In addition, we contacted County officials to get information about the County’s contributions to the hospital over the past five years. n We also examined the governance structures of each of these hospitals, particularly noting changes over time. 2
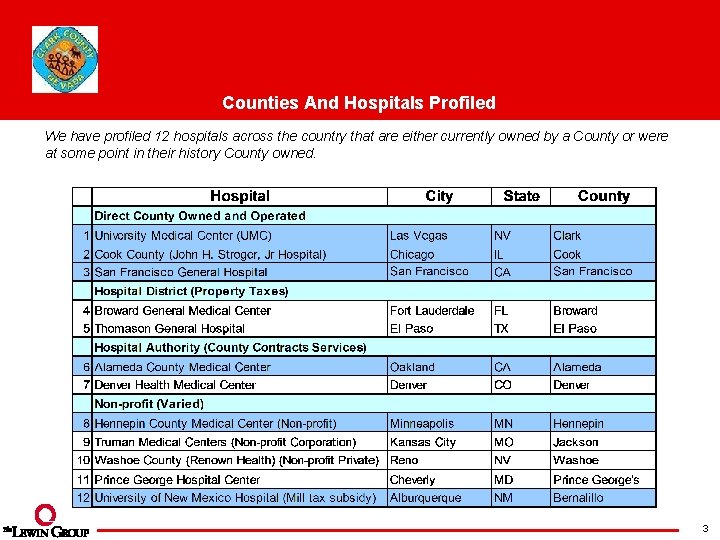
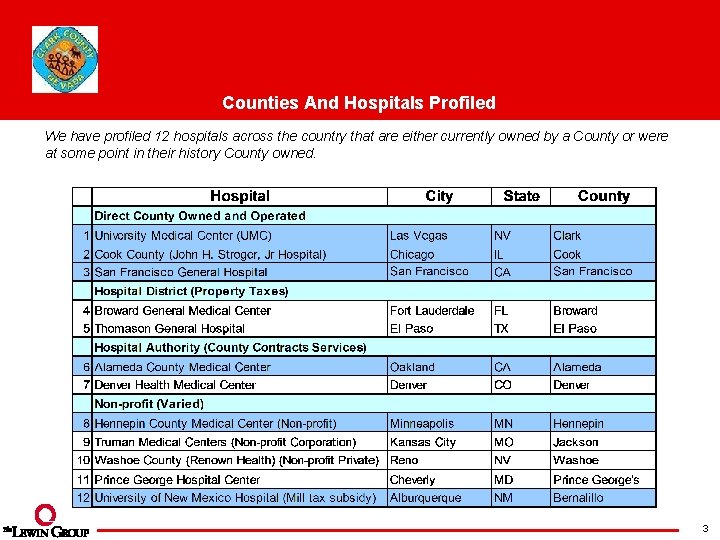
Counties And Hospitals Profiled We have profiled 12 hospitals across the country that are either currently owned by a County or were at some point in their history County owned. 3
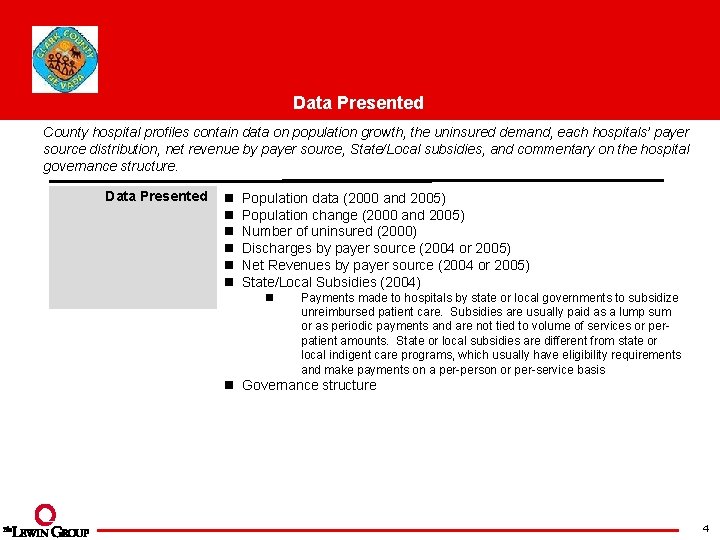
Data Presented County hospital profiles contain data on population growth, the uninsured demand, each hospitals’ payer source distribution, net revenue by payer source, State/Local subsidies, and commentary on the hospital governance structure. Data Presented n n n Population data (2000 and 2005) Population change (2000 and 2005) Number of uninsured (2000) Discharges by payer source (2004 or 2005) Net Revenues by payer source (2004 or 2005) State/Local Subsidies (2004) n Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a per-person or per-service basis n Governance structure 4
A Profile Of Hospitals Across The Country Project Overview and Approach University Medical Center Experience of Other Counties Summary 5
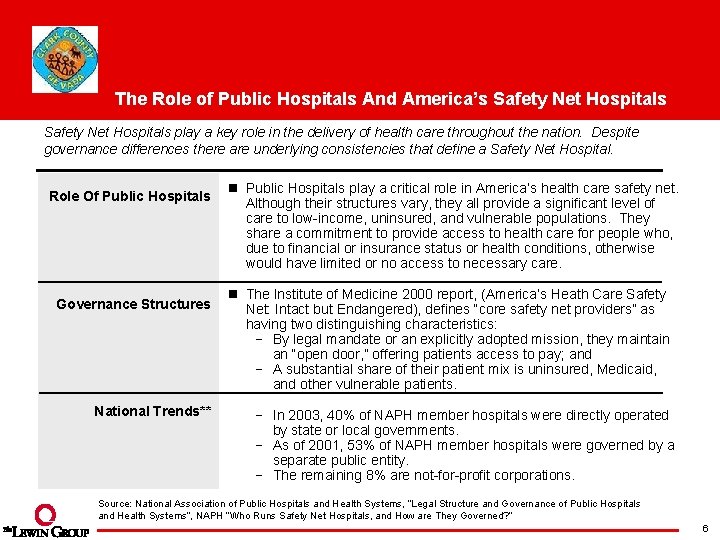
The Role of Public Hospitals And America’s Safety Net Hospitals play a key role in the delivery of health care throughout the nation. Despite governance differences there are underlying consistencies that define a Safety Net Hospital. Role Of Public Hospitals Governance Structures National Trends** n Public Hospitals play a critical role in America’s health care safety net. Although their structures vary, they all provide a significant level of care to low-income, uninsured, and vulnerable populations. They share a commitment to provide access to health care for people who, due to financial or insurance status or health conditions, otherwise would have limited or no access to necessary care. n The Institute of Medicine 2000 report, (America’s Heath Care Safety Net: Intact but Endangered), defines “core safety net providers” as having two distinguishing characteristics: By legal mandate or an explicitly adopted mission, they maintain an “open door, ” offering patients access to pay; and A substantial share of their patient mix is uninsured, Medicaid, and other vulnerable patients. In 2003, 40% of NAPH member hospitals were directly operated by state or local governments. As of 2001, 53% of NAPH member hospitals were governed by a separate public entity. The remaining 8% are not-for-profit corporations. Source: National Association of Public Hospitals and Health Systems, “Legal Structure and Governance of Public Hospitals and Health Systems”, NAPH “Who Runs Safety Net Hospitals, and How are They Governed? ” 6
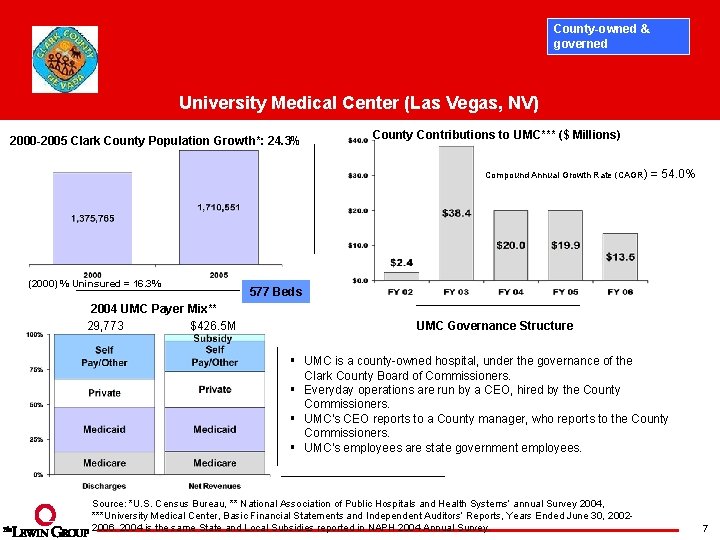
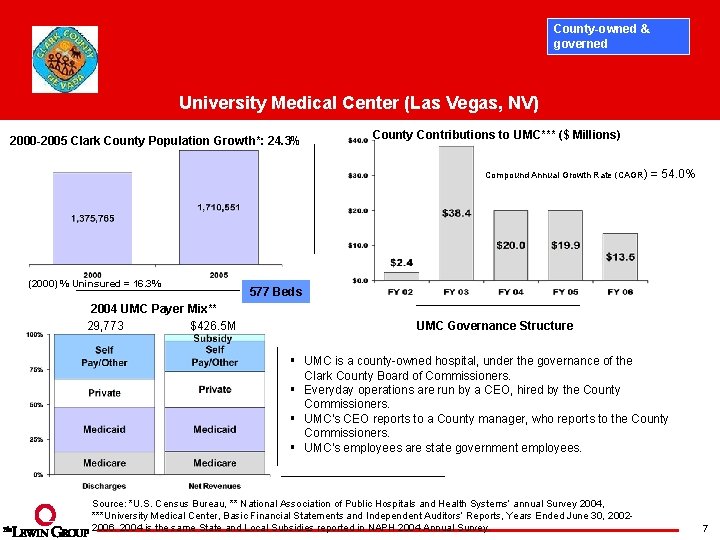
County-owned & governed University Medical Center (Las Vegas, NV) 2000 -2005 Clark County Population Growth*: 24. 3% County Contributions to UMC*** ($ Millions) Compound Annual Growth Rate (CAGR) = 54. 0% (2000) % Uninsured = 16. 3% 2004 UMC Payer Mix** 29, 773 $426. 5 M 577 Beds UMC Governance Structure § UMC is a county-owned hospital, under the governance of the Clark County Board of Commissioners. § Everyday operations are run by a CEO, hired by the County Commissioners. § UMC’s CEO reports to a County manager, who reports to the County Commissioners. § UMC’s employees are state government employees. Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, ***University Medical Center, Basic Financial Statements and Independent Auditors’ Reports, Years Ended June 30, 20022006. 2004 is the same State and Local Subsidies reported in NAPH 2004 Annual Survey. 7
A Profile Of Hospitals Across The Country Project Overview and Approach University Medical Center Experience of Other Counties Summary 8
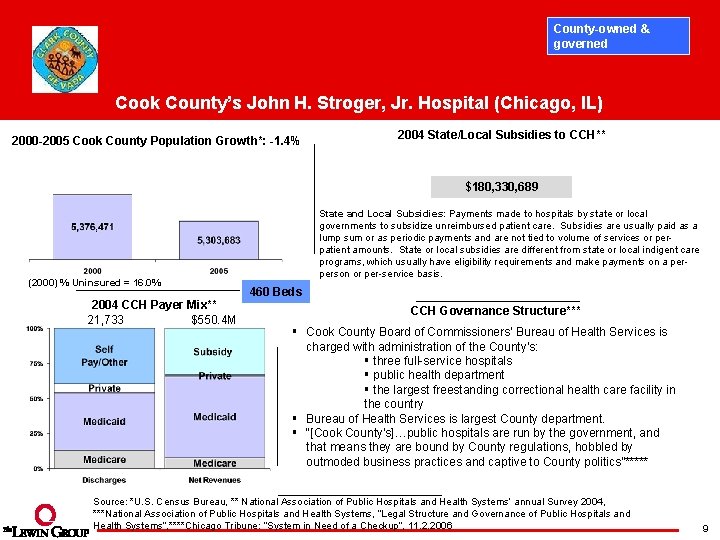
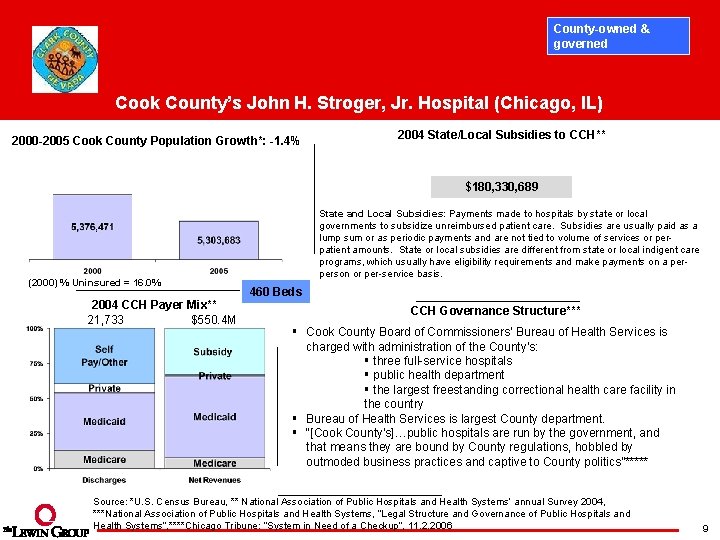
County-owned & governed Cook County’s John H. Stroger, Jr. Hospital (Chicago, IL) 2000 -2005 Cook County Population Growth*: -1. 4% 2004 State/Local Subsidies to CCH** $180, 330, 689 (2000) % Uninsured = 16. 0% 2004 CCH Payer Mix** 21, 733 $550. 4 M State and Local Subsidies: Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a perperson or per-service basis. 460 Beds CCH Governance Structure*** § Cook County Board of Commissioners’ Bureau of Health Services is charged with administration of the County’s: § three full-service hospitals § public health department § the largest freestanding correctional health care facility in the country § Bureau of Health Services is largest County department. § “[Cook County’s]…public hospitals are run by the government, and that means they are bound by County regulations, hobbled by outmoded business practices and captive to County politics”***** Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, ***National Association of Public Hospitals and Health Systems, “Legal Structure and Governance of Public Hospitals and Health Systems”, ****Chicago Tribune: “System in Need of a Checkup”, 11. 2. 2006 9
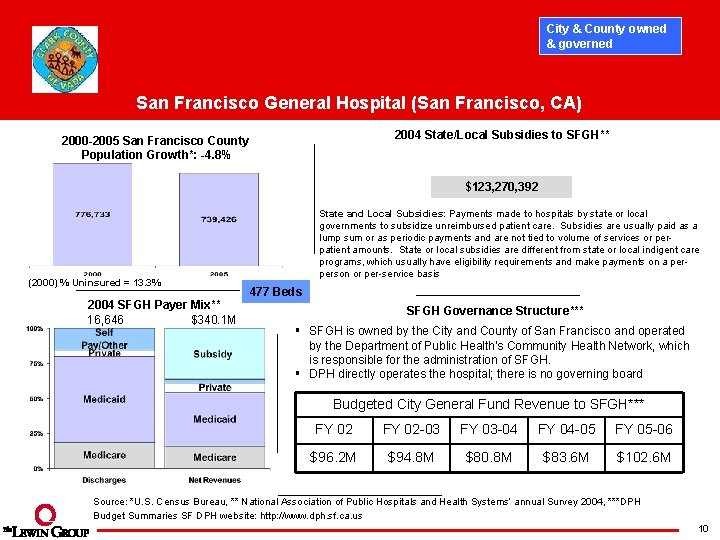
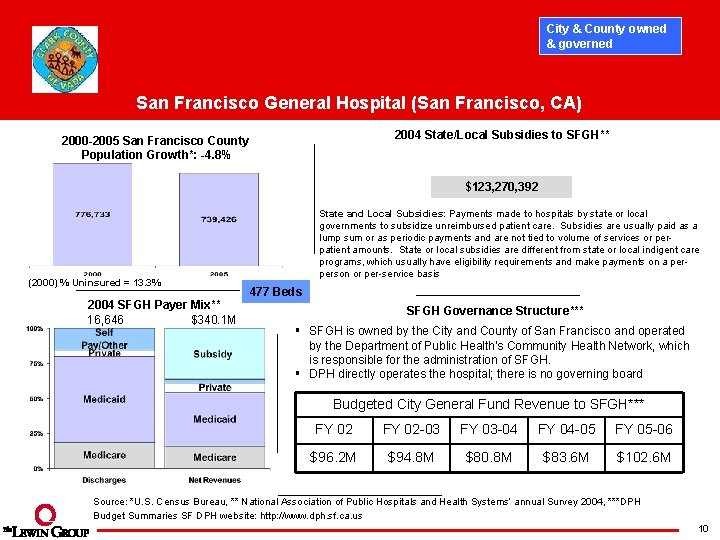
City & County owned & governed San Francisco General Hospital (San Francisco, CA) 2004 State/Local Subsidies to SFGH** 2000 -2005 San Francisco County Population Growth*: -4. 8% $123, 270, 392 (2000) % Uninsured = 13. 3% 2004 SFGH Payer Mix** 16, 646 $340. 1 M State and Local Subsidies: Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a perperson or per-service basis 477 Beds SFGH Governance Structure*** § SFGH is owned by the City and County of San Francisco and operated by the Department of Public Health's Community Health Network, which is responsible for the administration of SFGH. § DPH directly operates the hospital; there is no governing board Budgeted City General Fund Revenue to SFGH*** FY 02 -03 FY 03 -04 FY 04 -05 FY 05 -06 $96. 2 M $94. 8 M $80. 8 M $83. 6 M $102. 6 M Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, ***DPH Budget Summaries SF DPH website: http: //www. dph. sf. ca. us 10
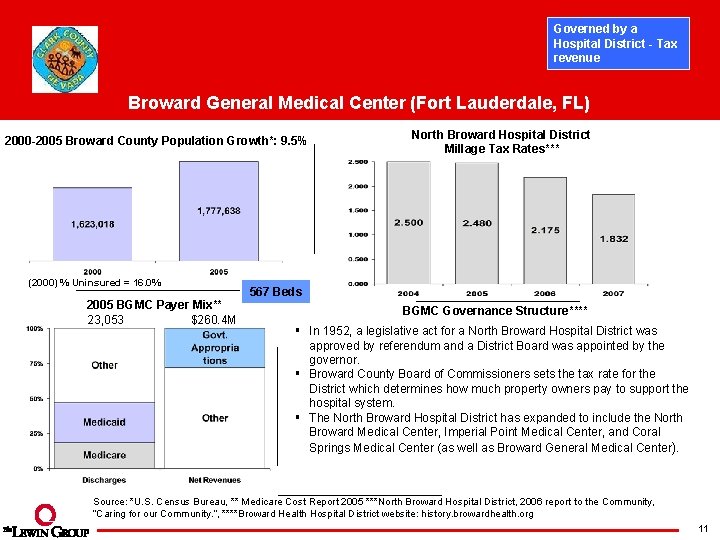
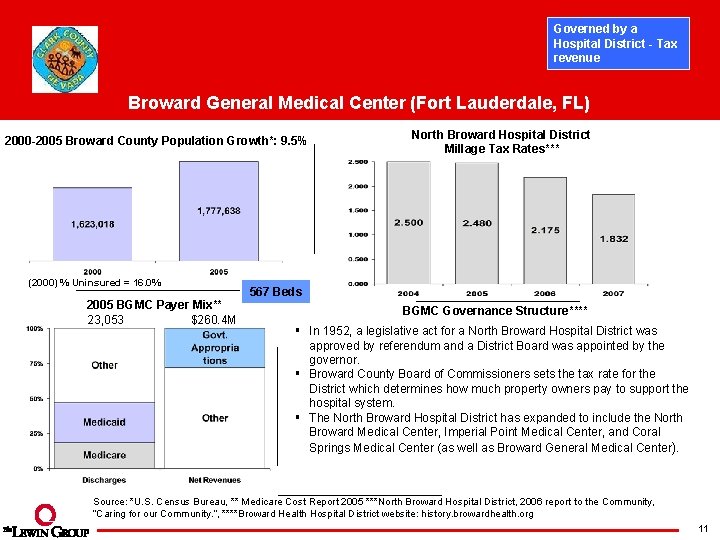
Governed by a Hospital District - Tax revenue Broward General Medical Center (Fort Lauderdale, FL) 2000 -2005 Broward County Population Growth*: 9. 5% (2000) % Uninsured = 16. 0% 2005 BGMC Payer Mix** 23, 053 $260. 4 M North Broward Hospital District Millage Tax Rates*** 567 Beds BGMC Governance Structure**** § In 1952, a legislative act for a North Broward Hospital District was approved by referendum and a District Board was appointed by the governor. § Broward County Board of Commissioners sets the tax rate for the District which determines how much property owners pay to support the hospital system. § The North Broward Hospital District has expanded to include the North Broward Medical Center, Imperial Point Medical Center, and Coral Springs Medical Center (as well as Broward General Medical Center). Source: *U. S. Census Bureau, ** Medicare Cost Report 2005 ***North Broward Hospital District, 2006 report to the Community, “Caring for our Community. ”, ****Broward Health Hospital District website: history. browardhealth. org 11
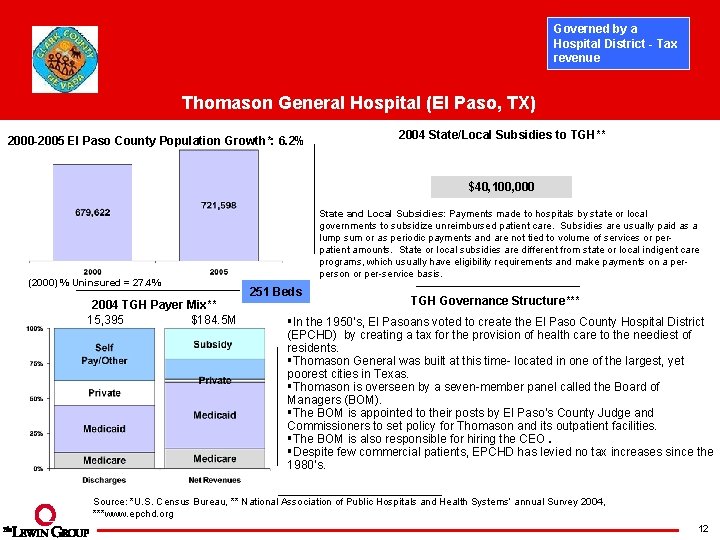
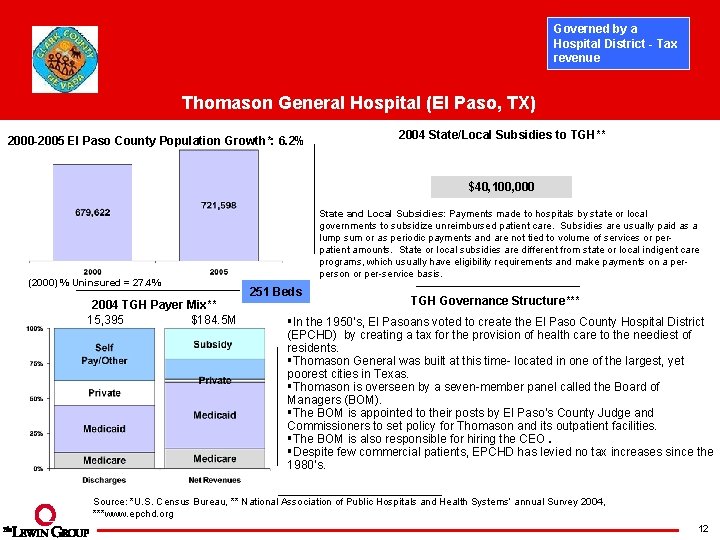
Governed by a Hospital District - Tax revenue Thomason General Hospital (El Paso, TX) 2000 -2005 El Paso County Population Growth*: 6. 2% 2004 State/Local Subsidies to TGH** $40, 100, 000 (2000) % Uninsured = 27. 4% 2004 TGH Payer Mix** 15, 395 $184. 5 M State and Local Subsidies: Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a perperson or per-service basis. 251 Beds TGH Governance Structure*** §In the 1950’s, El Pasoans voted to create the El Paso County Hospital District (EPCHD) by creating a tax for the provision of health care to the neediest of residents. §Thomason General was built at this time- located in one of the largest, yet poorest cities in Texas. §Thomason is overseen by a seven-member panel called the Board of Managers (BOM). §The BOM is appointed to their posts by El Paso’s County Judge and Commissioners to set policy for Thomason and its outpatient facilities. §The BOM is also responsible for hiring the CEO. §Despite few commercial patients, EPCHD has levied no tax increases since the 1980’s. Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, ***www. epchd. org 12
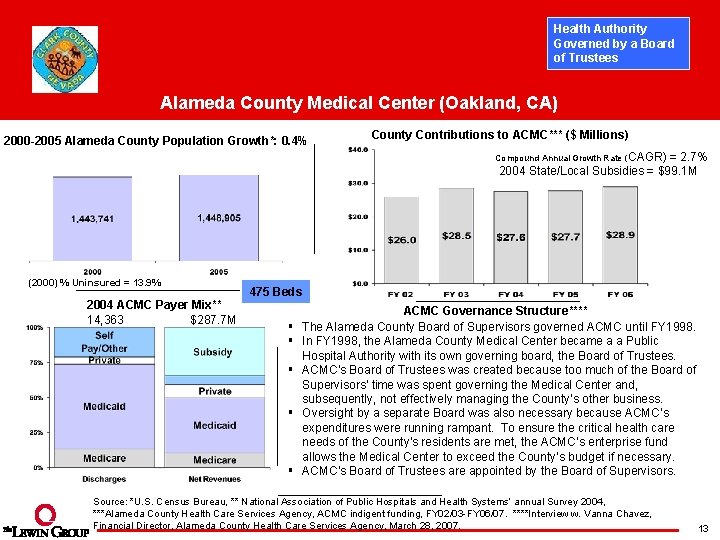
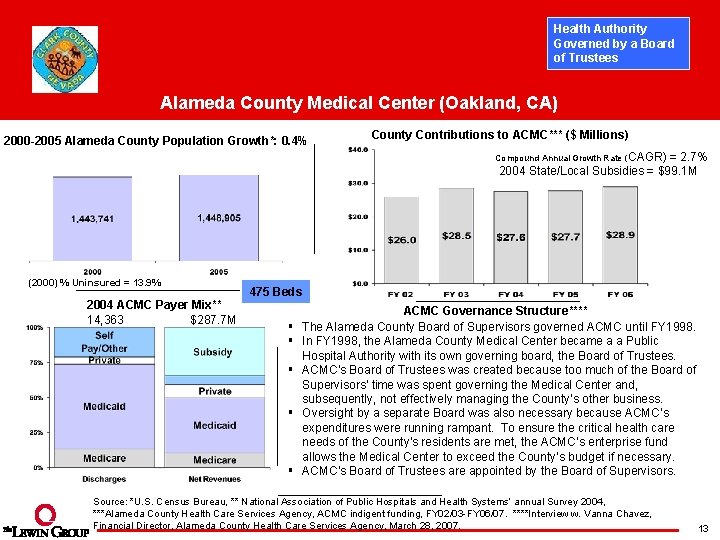
Health Authority Governed by a Board of Trustees Alameda County Medical Center (Oakland, CA) 2000 -2005 Alameda County Population Growth*: 0. 4% County Contributions to ACMC*** ($ Millions) Compound Annual Growth Rate (CAGR) = 2. 7% 2004 State/Local Subsidies = $99. 1 M (2000) % Uninsured = 13. 9% 2004 ACMC Payer Mix** 14, 363 $287. 7 M 475 Beds § § § ACMC Governance Structure**** The Alameda County Board of Supervisors governed ACMC until FY 1998. In FY 1998, the Alameda County Medical Center became a a Public Hospital Authority with its own governing board, the Board of Trustees. ACMC’s Board of Trustees was created because too much of the Board of Supervisors’ time was spent governing the Medical Center and, subsequently, not effectively managing the County’s other business. Oversight by a separate Board was also necessary because ACMC’s expenditures were running rampant. To ensure the critical health care needs of the County’s residents are met, the ACMC’s enterprise fund allows the Medical Center to exceed the County’s budget if necessary. ACMC’s Board of Trustees are appointed by the Board of Supervisors. Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, ***Alameda County Health Care Services Agency, ACMC indigent funding, FY 02/03 -FY 06/07. ****Interview w. Vanna Chavez, Financial Director, Alameda County Health Care Services Agency, March 28, 2007. 13
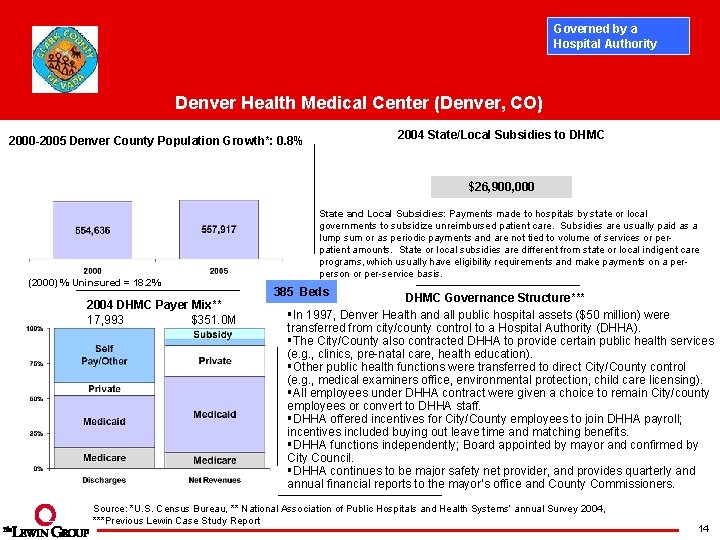
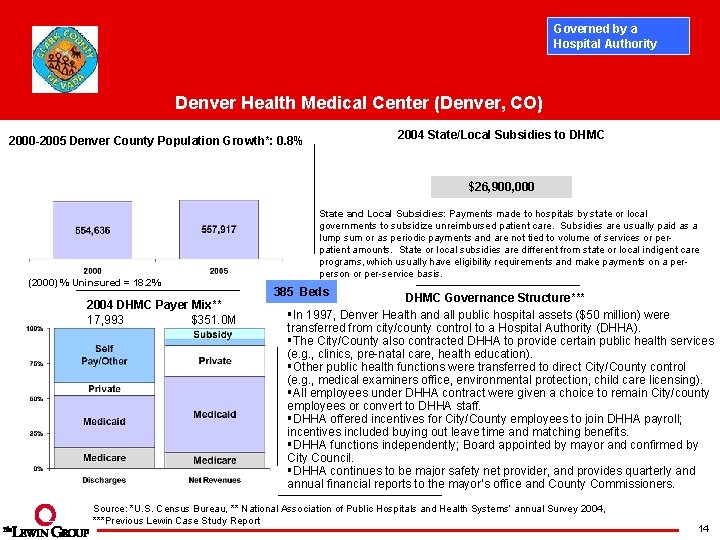
Governed by a Hospital Authority Denver Health Medical Center (Denver, CO) 2004 State/Local Subsidies to DHMC 2000 -2005 Denver County Population Growth*: 0. 8% $26, 900, 000 (2000) % Uninsured = 18. 2% 2004 DHMC Payer Mix** 17, 993 $351. 0 M State and Local Subsidies: Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a perperson or per-service basis. 385 Beds DHMC Governance Structure*** §In 1997, Denver Health and all public hospital assets ($50 million) were transferred from city/county control to a Hospital Authority (DHHA). §The City/County also contracted DHHA to provide certain public health services (e. g. , clinics, pre-natal care, health education). §Other public health functions were transferred to direct City/County control (e. g. , medical examiners office, environmental protection, child care licensing). §All employees under DHHA contract were given a choice to remain City/county employees or convert to DHHA staff. §DHHA offered incentives for City/County employees to join DHHA payroll; incentives included buying out leave time and matching benefits. §DHHA functions independently; Board appointed by mayor and confirmed by City Council. §DHHA continues to be major safety net provider, and provides quarterly and annual financial reports to the mayor’s office and County Commissioners. Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, ***Previous Lewin Case Study Report 14
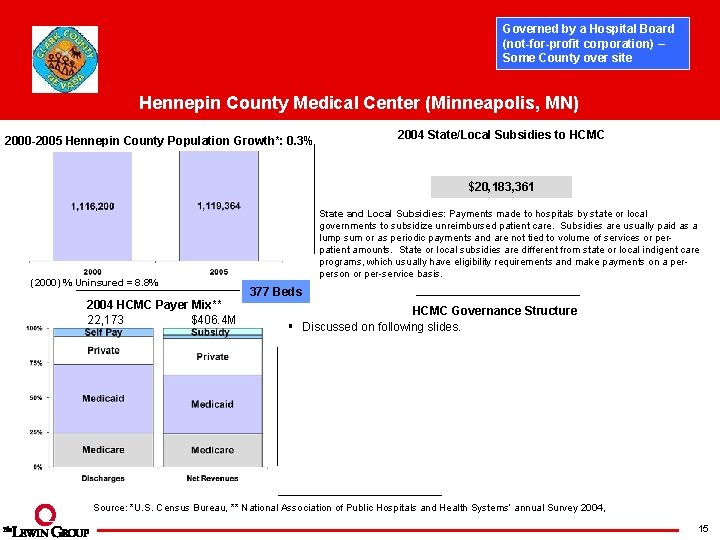
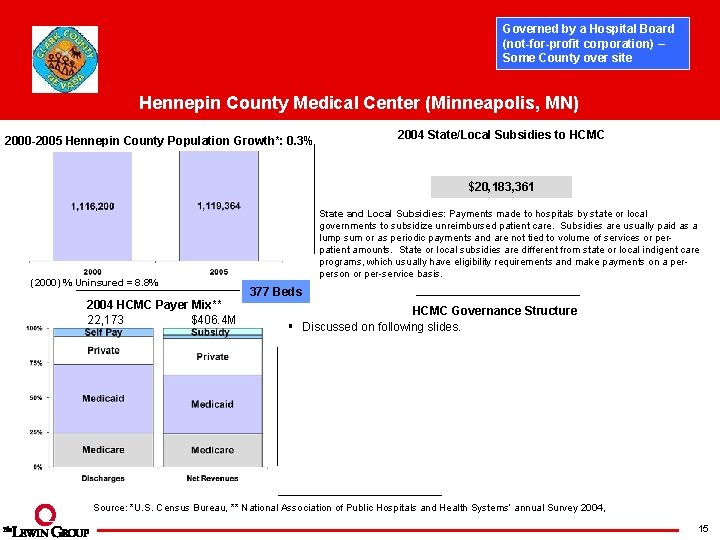
Governed by a Hospital Board (not-for-profit corporation) – Some County over site Hennepin County Medical Center (Minneapolis, MN) 2000 -2005 Hennepin County Population Growth*: 0. 3% 2004 State/Local Subsidies to HCMC $20, 183, 361 (2000) % Uninsured = 8. 8% 2004 HCMC Payer Mix** 22, 173 $406. 4 M State and Local Subsidies: Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a perperson or per-service basis. 377 Beds HCMC Governance Structure § Discussed on following slides. Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, 15
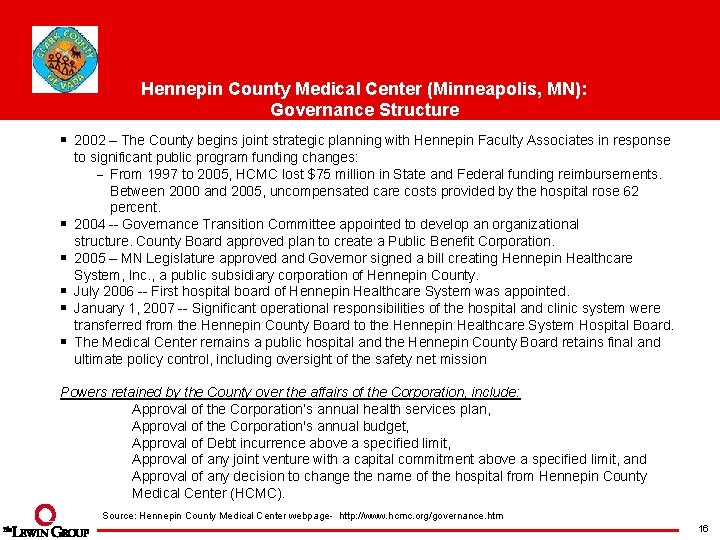
Hennepin County Medical Center (Minneapolis, MN): Governance Structure § 2002 – The County begins joint strategic planning with Hennepin Faculty Associates in response § § § to significant public program funding changes: From 1997 to 2005, HCMC lost $75 million in State and Federal funding reimbursements. Between 2000 and 2005, uncompensated care costs provided by the hospital rose 62 percent. 2004 -- Governance Transition Committee appointed to develop an organizational structure. County Board approved plan to create a Public Benefit Corporation. 2005 – MN Legislature approved and Governor signed a bill creating Hennepin Healthcare System, Inc. , a public subsidiary corporation of Hennepin County. July 2006 -- First hospital board of Hennepin Healthcare System was appointed. January 1, 2007 -- Significant operational responsibilities of the hospital and clinic system were transferred from the Hennepin County Board to the Hennepin Healthcare System Hospital Board. The Medical Center remains a public hospital and the Hennepin County Board retains final and ultimate policy control, including oversight of the safety net mission Powers retained by the County over the affairs of the Corporation, include: Approval of the Corporation’s annual health services plan, Approval of the Corporation's annual budget, Approval of Debt incurrence above a specified limit, Approval of any joint venture with a capital commitment above a specified limit, and Approval of any decision to change the name of the hospital from Hennepin County Medical Center (HCMC). Source: Hennepin County Medical Center webpage- http: //www. hcmc. org/governance. htm 16
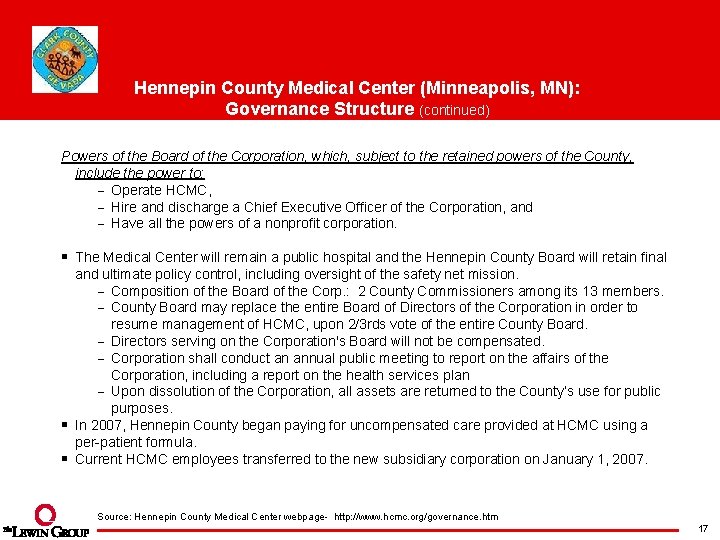
Hennepin County Medical Center (Minneapolis, MN): Governance Structure (continued) Powers of the Board of the Corporation, which, subject to the retained powers of the County, include the power to: Operate HCMC, Hire and discharge a Chief Executive Officer of the Corporation, and Have all the powers of a nonprofit corporation. § The Medical Center will remain a public hospital and the Hennepin County Board will retain final and ultimate policy control, including oversight of the safety net mission. Composition of the Board of the Corp. : 2 County Commissioners among its 13 members. County Board may replace the entire Board of Directors of the Corporation in order to resume management of HCMC, upon 2/3 rds vote of the entire County Board. Directors serving on the Corporation's Board will not be compensated. Corporation shall conduct an annual public meeting to report on the affairs of the Corporation, including a report on the health services plan Upon dissolution of the Corporation, all assets are returned to the County’s use for public purposes. § In 2007, Hennepin County began paying for uncompensated care provided at HCMC using a per-patient formula. § Current HCMC employees transferred to the new subsidiary corporation on January 1, 2007. Source: Hennepin County Medical Center webpage- http: //www. hcmc. org/governance. htm 17
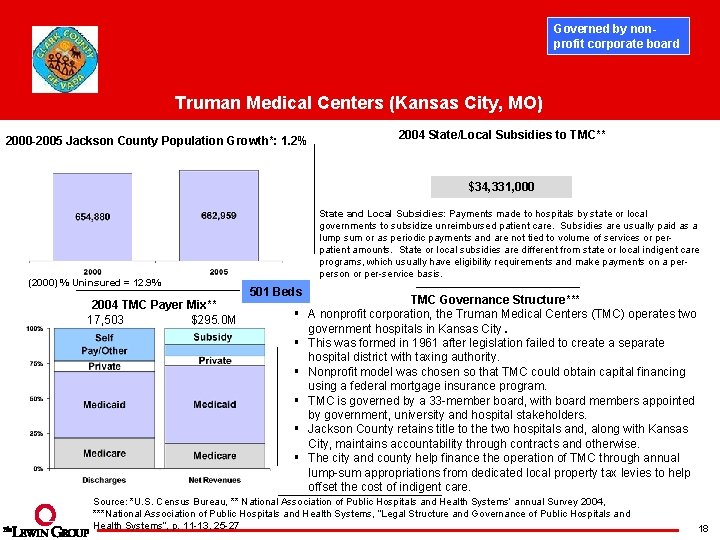
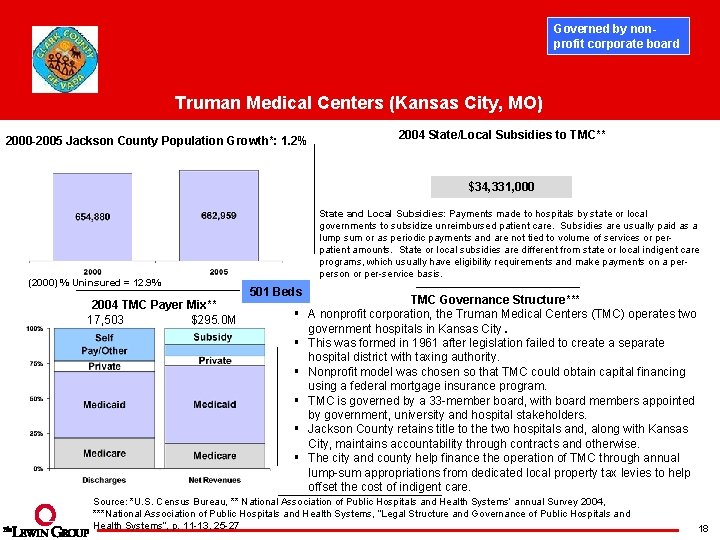
Governed by nonprofit corporate board Truman Medical Centers (Kansas City, MO) 2000 -2005 Jackson County Population Growth*: 1. 2% 2004 State/Local Subsidies to TMC** $34, 331, 000 (2000) % Uninsured = 12. 9% 2004 TMC Payer Mix** 17, 503 $295. 0 M State and Local Subsidies: Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a perperson or per-service basis. 501 Beds § § § TMC Governance Structure*** A nonprofit corporation, the Truman Medical Centers (TMC) operates two government hospitals in Kansas City. This was formed in 1961 after legislation failed to create a separate hospital district with taxing authority. Nonprofit model was chosen so that TMC could obtain capital financing using a federal mortgage insurance program. TMC is governed by a 33 -member board, with board members appointed by government, university and hospital stakeholders. Jackson County retains title to the two hospitals and, along with Kansas City, maintains accountability through contracts and otherwise. The city and county help finance the operation of TMC through annual lump-sum appropriations from dedicated local property tax levies to help offset the cost of indigent care. Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, ***National Association of Public Hospitals and Health Systems, “Legal Structure and Governance of Public Hospitals and Health Systems”, p. 11 -13, 25 -27 18
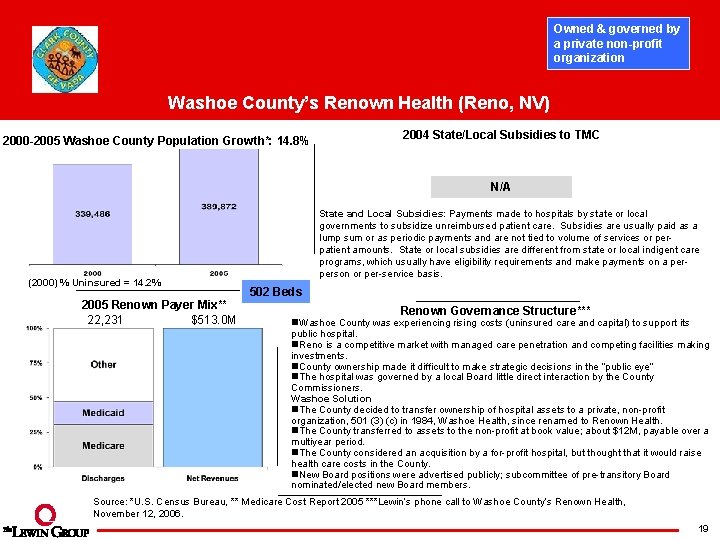
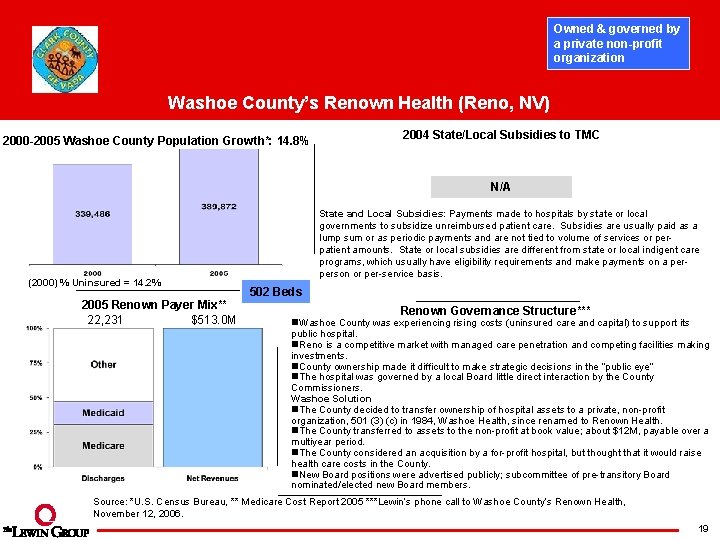
Owned & governed by a private non-profit organization Washoe County’s Renown Health (Reno, NV) 2000 -2005 Washoe County Population Growth*: 14. 8% 2004 State/Local Subsidies to TMC N/A (2000) % Uninsured = 14. 2% 2005 Renown Payer Mix** 22, 231 $513. 0 M State and Local Subsidies: Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a perperson or per-service basis. 502 Beds Renown Governance Structure*** n. Washoe County was experiencing rising costs (uninsured care and capital) to support its public hospital. n. Reno is a competitive market with managed care penetration and competing facilities making investments. n. County ownership made it difficult to make strategic decisions in the “public eye” n. The hospital was governed by a local Board little direct interaction by the County Commissioners. Washoe Solution n. The County decided to transfer ownership of hospital assets to a private, non-profit organization, 501 (3) (c) in 1984, Washoe Health, since renamed to Renown Health. n. The County transferred to assets to the non-profit at book value; about $12 M, payable over a multiyear period. n. The County considered an acquisition by a for-profit hospital, but thought that it would raise health care costs in the County. n. New Board positions were advertised publicly; subcommittee of pre-transitory Board nominated/elected new Board members. Source: *U. S. Census Bureau, ** Medicare Cost Report 2005 ***Lewin’s phone call to Washoe County’s Renown Health, November 12, 2006. 19
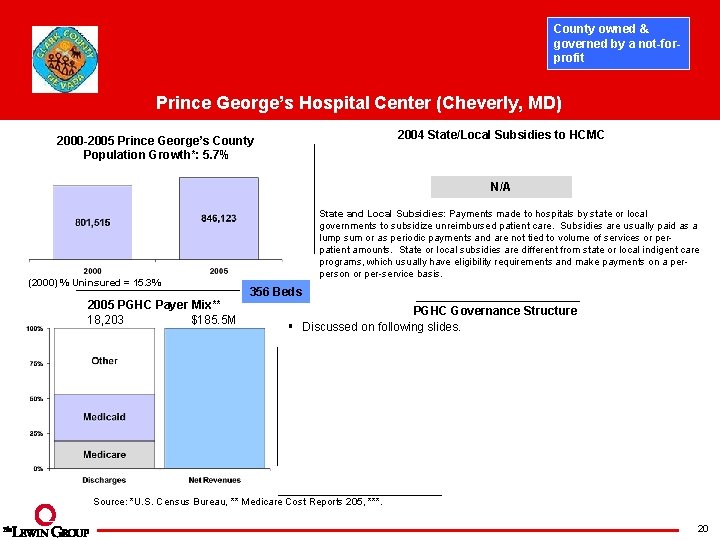
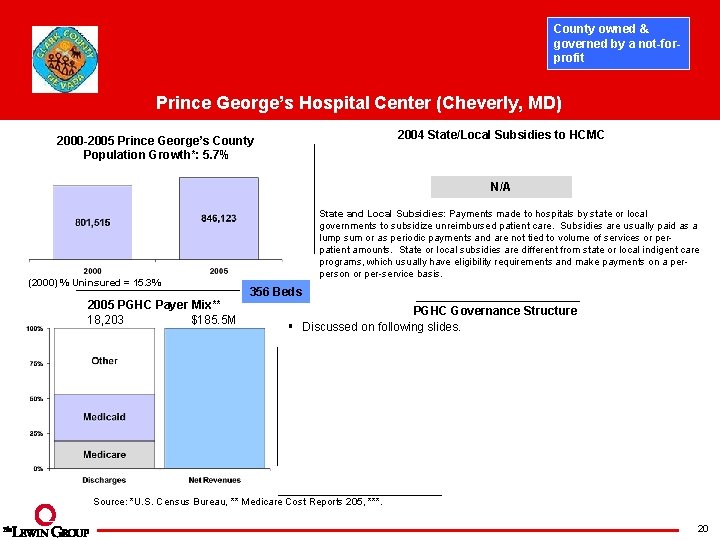
County owned & governed by a not-forprofit Prince George’s Hospital Center (Cheverly, MD) 2004 State/Local Subsidies to HCMC 2000 -2005 Prince George’s County Population Growth*: 5. 7% N/A (2000) % Uninsured = 15. 3% 2005 PGHC Payer Mix** 18, 203 $185. 5 M State and Local Subsidies: Payments made to hospitals by state or local governments to subsidize unreimbursed patient care. Subsidies are usually paid as a lump sum or as periodic payments and are not tied to volume of services or perpatient amounts. State or local subsidies are different from state or local indigent care programs, which usually have eligibility requirements and make payments on a perperson or per-service basis. 356 Beds PGHC Governance Structure § Discussed on following slides. Source: *U. S. Census Bureau, ** Medicare Cost Reports 205, ***. 20
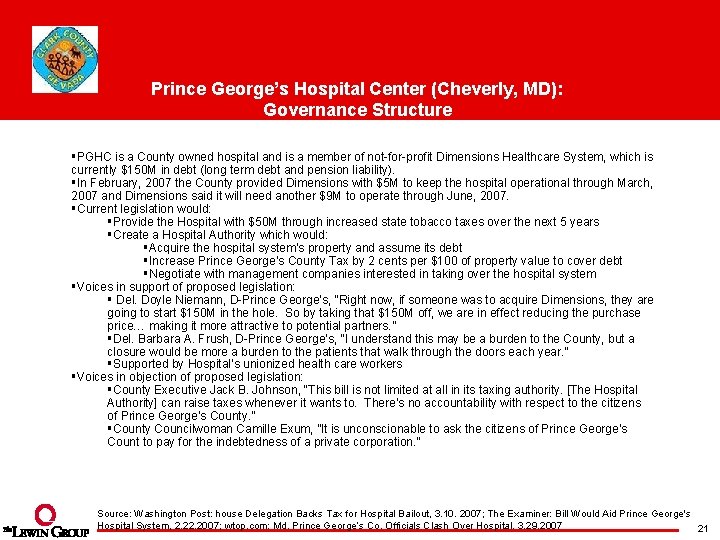
Prince George’s Hospital Center (Cheverly, MD): Governance Structure §PGHC is a County owned hospital and is a member of not-for-profit Dimensions Healthcare System, which is currently $150 M in debt (long term debt and pension liability). §In February, 2007 the County provided Dimensions with $5 M to keep the hospital operational through March, 2007 and Dimensions said it will need another $9 M to operate through June, 2007. §Current legislation would: §Provide the Hospital with $50 M through increased state tobacco taxes over the next 5 years §Create a Hospital Authority which would: §Acquire the hospital system’s property and assume its debt §Increase Prince George’s County Tax by 2 cents per $100 of property value to cover debt §Negotiate with management companies interested in taking over the hospital system §Voices in support of proposed legislation: § Del. Doyle Niemann, D-Prince George’s, “Right now, if someone was to acquire Dimensions, they are going to start $150 M in the hole. So by taking that $150 M off, we are in effect reducing the purchase price… making it more attractive to potential partners. ” §Del. Barbara A. Frush, D-Prince George’s, “I understand this may be a burden to the County, but a closure would be more a burden to the patients that walk through the doors each year. ” §Supported by Hospital’s unionized health care workers §Voices in objection of proposed legislation: §County Executive Jack B. Johnson, “This bill is not limited at all in its taxing authority. [The Hospital Authority] can raise taxes whenever it wants to. There’s no accountability with respect to the citizens of Prince George’s County. ” §County Councilwoman Camille Exum, ”It is unconscionable to ask the citizens of Prince George’s Count to pay for the indebtedness of a private corporation. ” Source: Washington Post: house Delegation Backs Tax for Hospital Bailout, 3. 10. 2007; The Examiner: Bill Would Aid Prince George's Hospital System, 2. 2007; wtop. com: Md. Prince George’s Co. Officials Clash Over Hospital. 3. 29. 2007 21
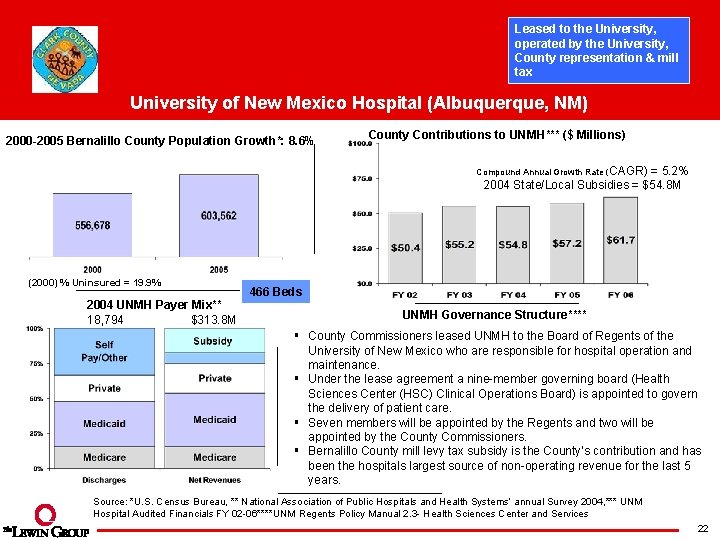
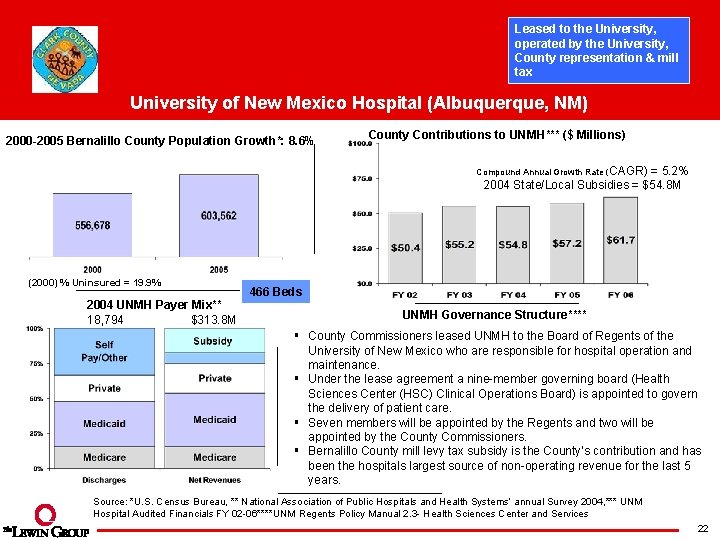
Leased to the University, operated by the University, County representation & mill tax University of New Mexico Hospital (Albuquerque, NM) 2000 -2005 Bernalillo County Population Growth*: 8. 6% County Contributions to UNMH*** ($ Millions) Compound Annual Growth Rate (CAGR) = 5. 2% 2004 State/Local Subsidies = $54. 8 M (2000) % Uninsured = 19. 9% 2004 UNMH Payer Mix** 18, 794 $313. 8 M 466 Beds UNMH Governance Structure**** § County Commissioners leased UNMH to the Board of Regents of the University of New Mexico who are responsible for hospital operation and maintenance. § Under the lease agreement a nine-member governing board (Health Sciences Center (HSC) Clinical Operations Board) is appointed to govern the delivery of patient care. § Seven members will be appointed by the Regents and two will be appointed by the County Commissioners. § Bernalillo County mill levy tax subsidy is the County’s contribution and has been the hospitals largest source of non-operating revenue for the last 5 years. Source: *U. S. Census Bureau, ** National Association of Public Hospitals and Health Systems’ annual Survey 2004, *** UNM Hospital Audited Financials FY 02 -06****UNM Regents Policy Manual 2. 3 - Health Sciences Center and Services 22
A Profile Of Hospitals Across The Country Project Overview and Approach University Medical Center Experience of Other Counties Summary 23
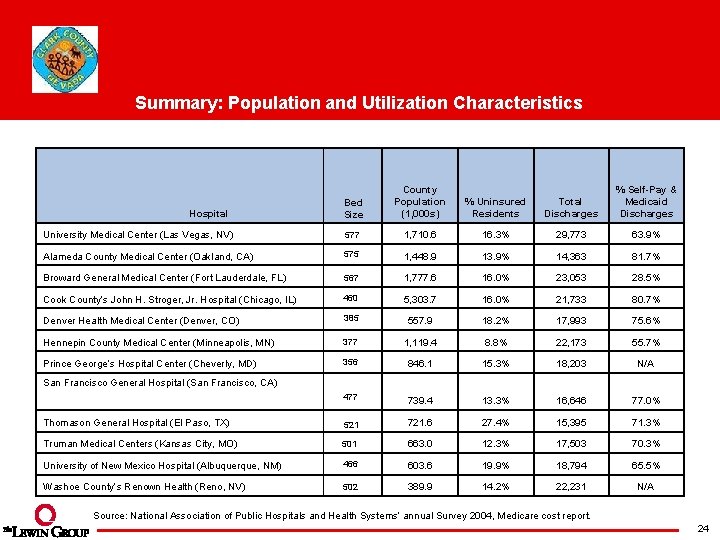
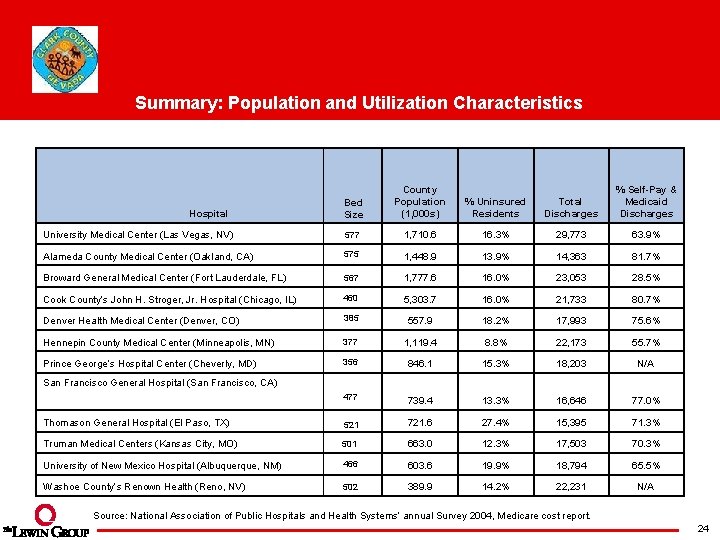
Summary: Population and Utilization Characteristics Bed Size County Population (1, 000 s) % Uninsured Residents Total Discharges % Self-Pay & Medicaid Discharges University Medical Center (Las Vegas, NV) 577 1, 710. 6 16. 3% 29, 773 63. 9% Alameda County Medical Center (Oakland, CA) 575 1, 448. 9 13. 9% 14, 363 81. 7% Broward General Medical Center (Fort Lauderdale, FL) 567 1, 777. 6 16. 0% 23, 053 28. 5% Cook County’s John H. Stroger, Jr. Hospital (Chicago, IL) 460 5, 303. 7 16. 0% 21, 733 80. 7% Denver Health Medical Center (Denver, CO) 385 557. 9 18. 2% 17, 993 75. 6% Hennepin County Medical Center (Minneapolis, MN) 377 1, 119. 4 8. 8% 22, 173 55. 7% Prince George’s Hospital Center (Cheverly, MD) 356 846. 1 15. 3% 18, 203 N/A 477 739. 4 13. 3% 16, 646 77. 0% Thomason General Hospital (El Paso, TX) 521 721. 6 27. 4% 15, 395 71. 3% Truman Medical Centers (Kansas City, MO) 501 663. 0 12. 3% 17, 503 70. 3% University of New Mexico Hospital (Albuquerque, NM) 466 603. 6 19. 9% 18, 794 65. 5% Washoe County’s Renown Health (Reno, NV) 502 389. 9 14. 2% 22, 231 N/A Hospital San Francisco General Hospital (San Francisco, CA) Source: National Association of Public Hospitals and Health Systems’ annual Survey 2004, Medicare cost report. 24
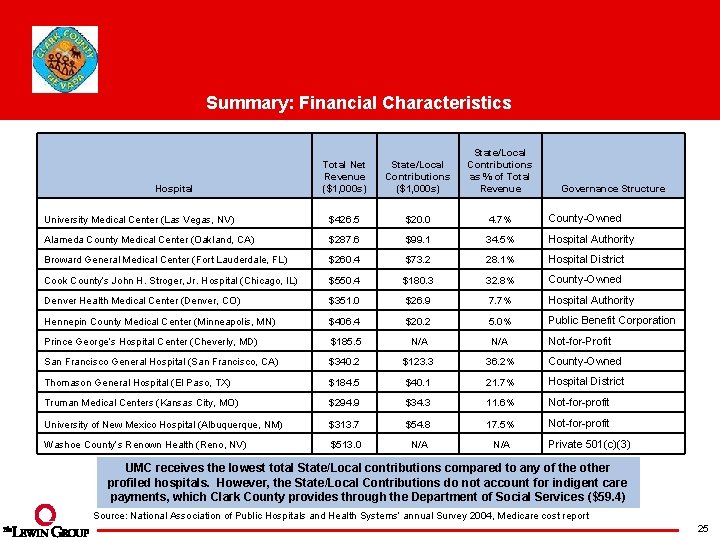
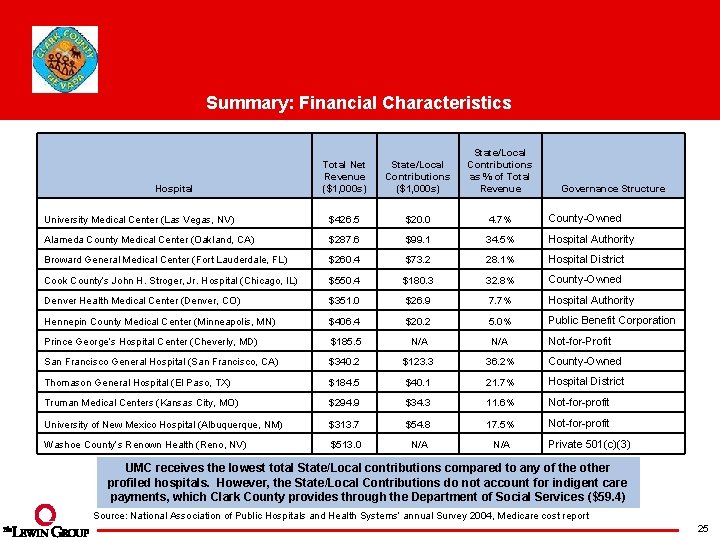
Summary: Financial Characteristics Total Net Revenue ($1, 000 s) State/Local Contributions as % of Total Revenue University Medical Center (Las Vegas, NV) $426. 5 $20. 0 4. 7% County-Owned Alameda County Medical Center (Oakland, CA) $287. 6 $99. 1 34. 5% Hospital Authority Broward General Medical Center (Fort Lauderdale, FL) $260. 4 $73. 2 28. 1% Hospital District Cook County’s John H. Stroger, Jr. Hospital (Chicago, IL) $550. 4 $180. 3 32. 8% County-Owned Denver Health Medical Center (Denver, CO) $351. 0 $26. 9 7. 7% Hospital Authority Hennepin County Medical Center (Minneapolis, MN) $406. 4 $20. 2 5. 0% Public Benefit Corporation Prince George’s Hospital Center (Cheverly, MD) $185. 5 N/A Not-for-Profit San Francisco General Hospital (San Francisco, CA) $340. 2 $123. 3 36. 2% County-Owned Thomason General Hospital (El Paso, TX) $184. 5 $40. 1 21. 7% Hospital District Truman Medical Centers (Kansas City, MO) $294. 9 $34. 3 11. 6% Not-for-profit University of New Mexico Hospital (Albuquerque, NM) $313. 7 $54. 8 17. 5% Not-for-profit Washoe County’s Renown Health (Reno, NV) $513. 0 N/A Hospital Governance Structure Private 501(c)(3) UMC receives the lowest total State/Local contributions compared to any of the other profiled hospitals. However, the State/Local Contributions do not account for indigent care payments, which Clark County provides through the Department of Social Services ($59. 4) Source: National Association of Public Hospitals and Health Systems’ annual Survey 2004, Medicare cost report 25
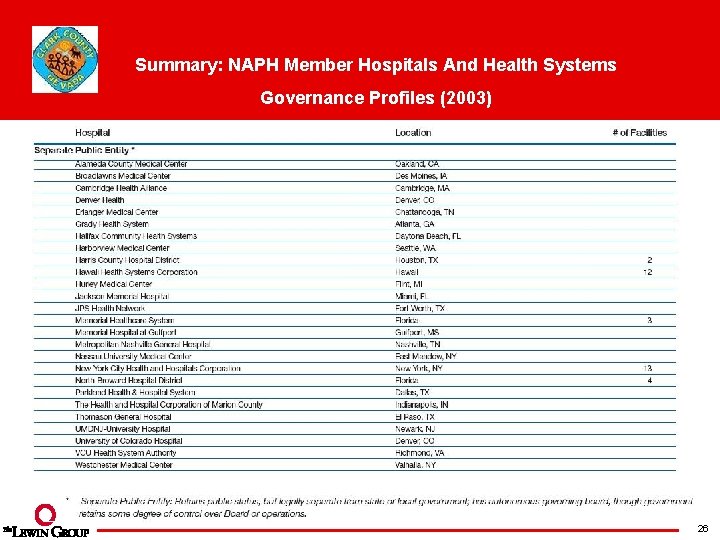
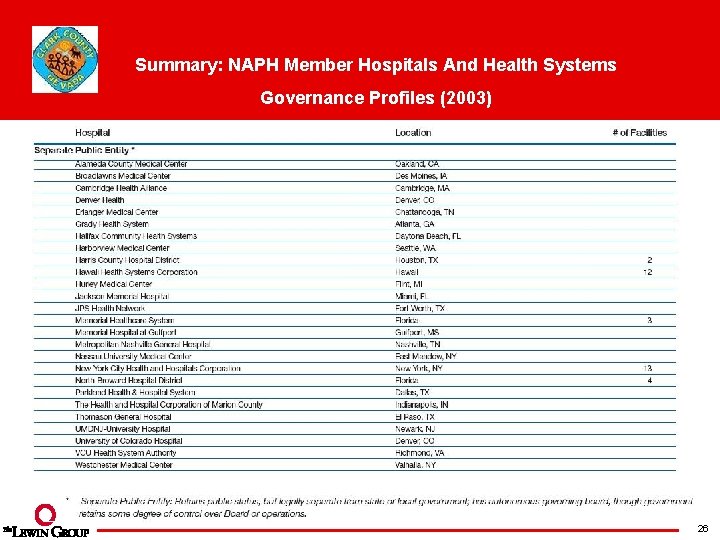
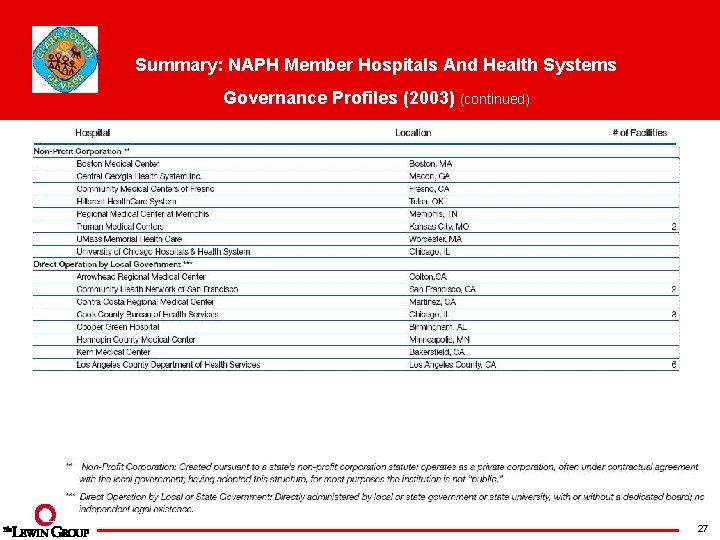
Summary: NAPH Member Hospitals And Health Systems Governance Profiles (2003) 26
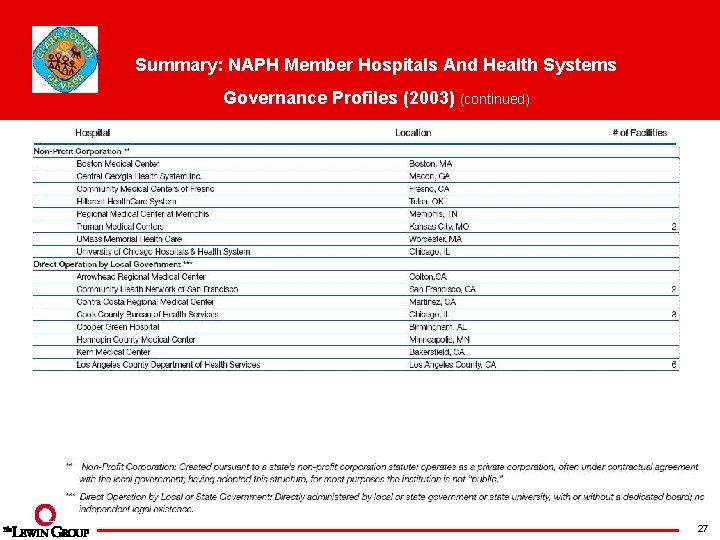
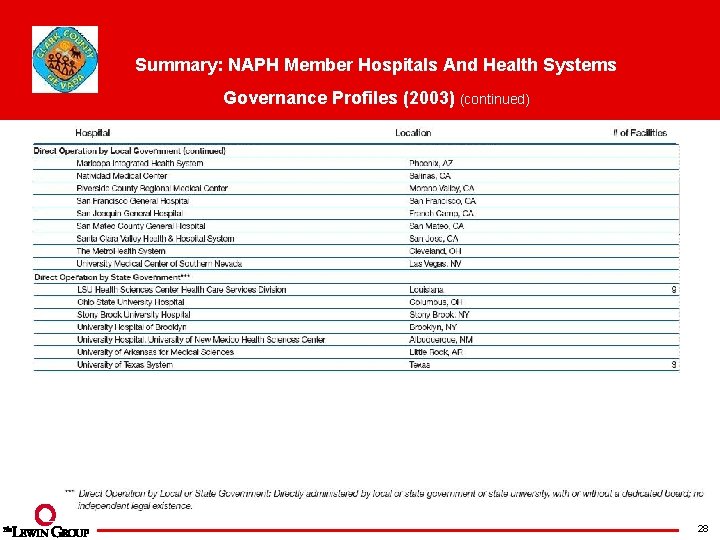
Summary: NAPH Member Hospitals And Health Systems Governance Profiles (2003) (continued) 27
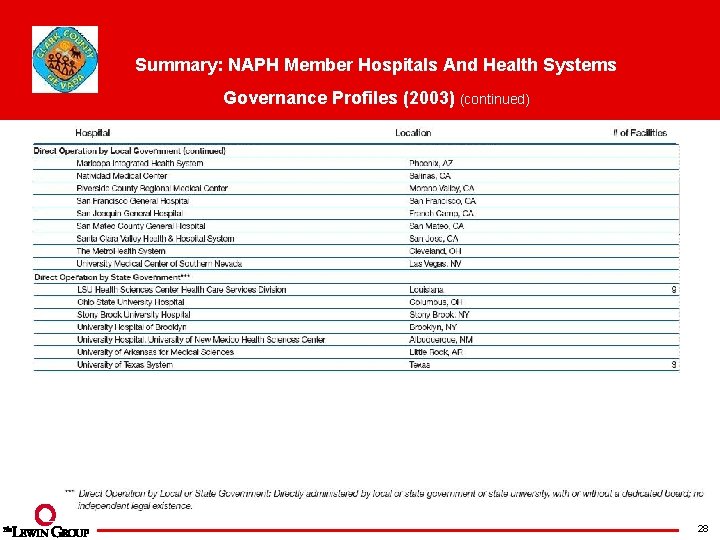
Summary: NAPH Member Hospitals And Health Systems Governance Profiles (2003) (continued) 28
 Functions of marketing by clark and clark
Functions of marketing by clark and clark Cook county nevada
Cook county nevada Lewis and clark county montana
Lewis and clark county montana Clark county youth football
Clark county youth football Clark county daq
Clark county daq Las vegas justice court efile
Las vegas justice court efile State of nevada department of business and industry
State of nevada department of business and industry Nevada department of business and industry
Nevada department of business and industry State of nevada department of business and industry
State of nevada department of business and industry Lewis and clark vocabulary
Lewis and clark vocabulary Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worm breton là gì
Tư thế worm breton là gì Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn