Celiac Disease and lactose Intolerance in North Indian







- Slides: 42

Celiac Disease and lactose Intolerance in North Indian Children Prof Satyavati Rana Department of Super Specialty of Gastroenterology, Post Graduate Institute of Medical Education & Research, Chandigarh, 160012, India
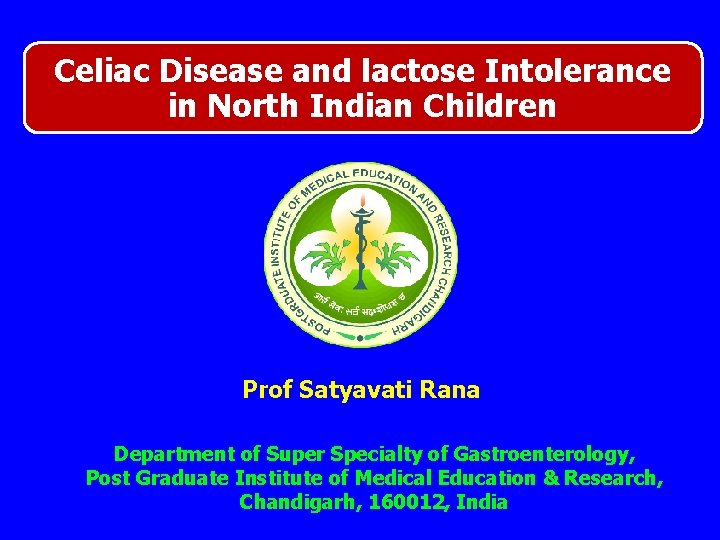
Introduction • Celiac disease is intestinal inflammatory disease that is triggered in genetically susceptible individuals by dietary gluten protein found in wheat, barley & rye • It is believed to be present in up to 1 in 100 of population
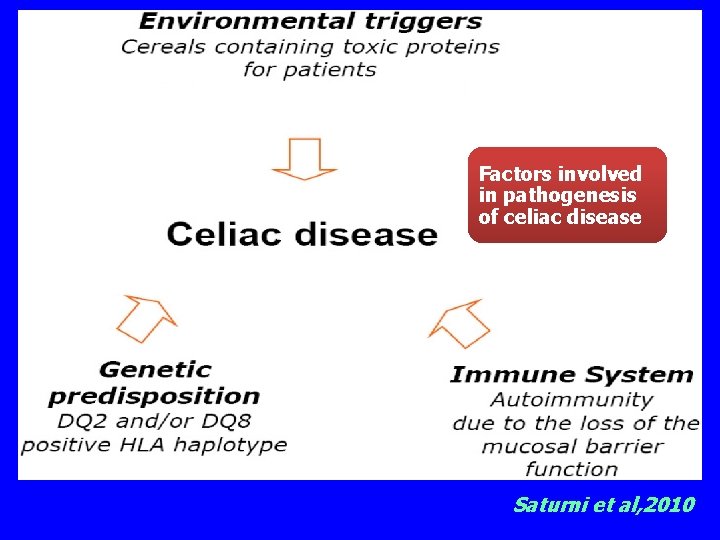
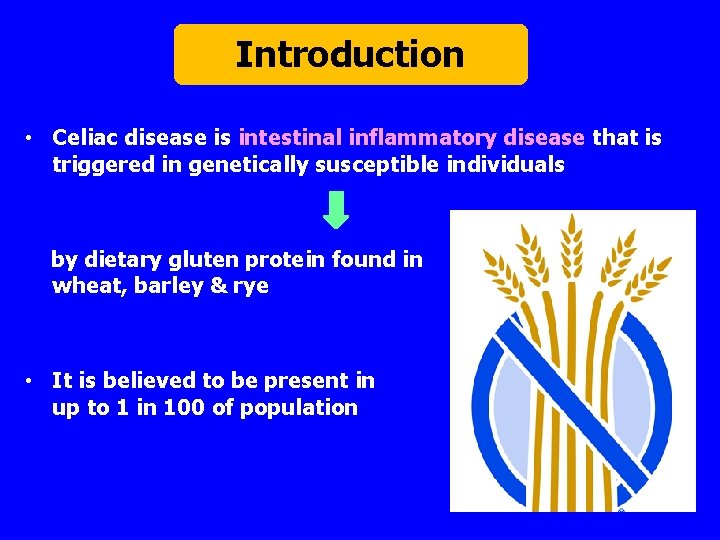
Factors involved in pathogenesis of celiac disease Saturni et al, 2010
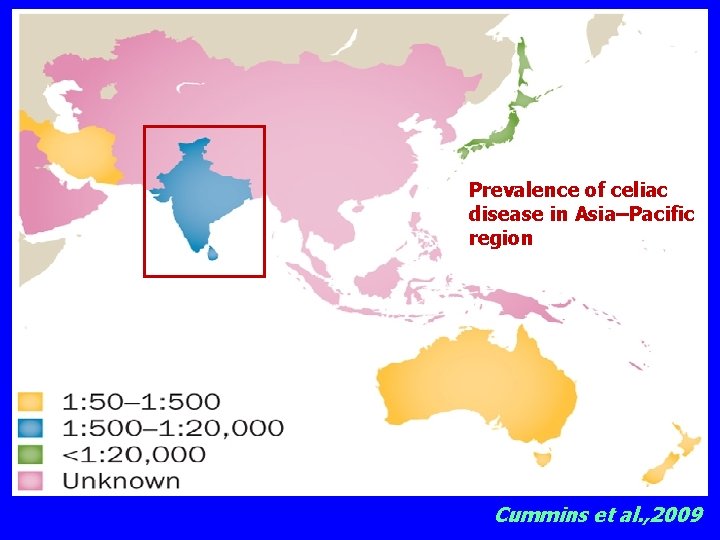
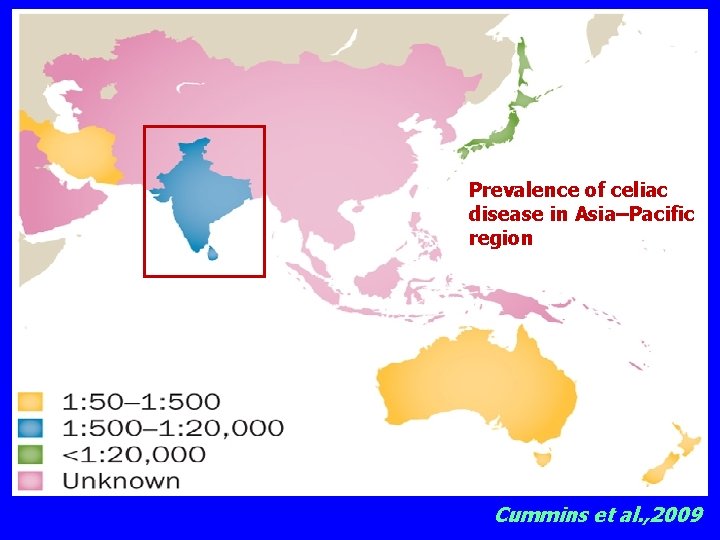
Prevalence of celiac disease in Asia–Pacific region Cummins et al. , 2009
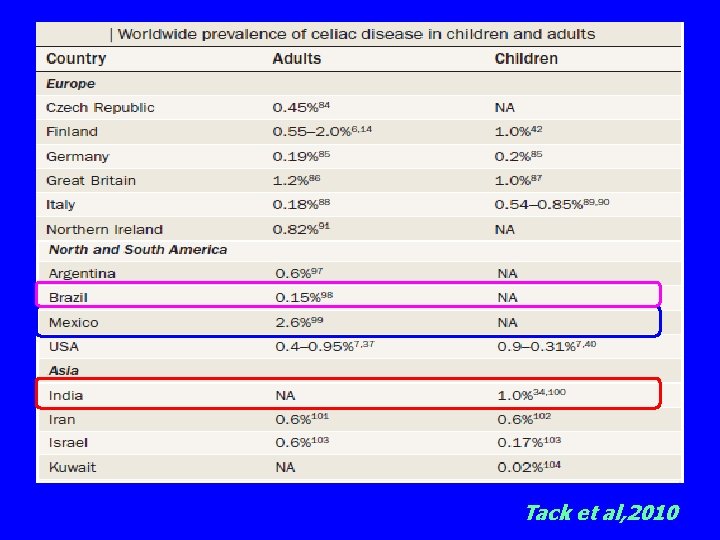
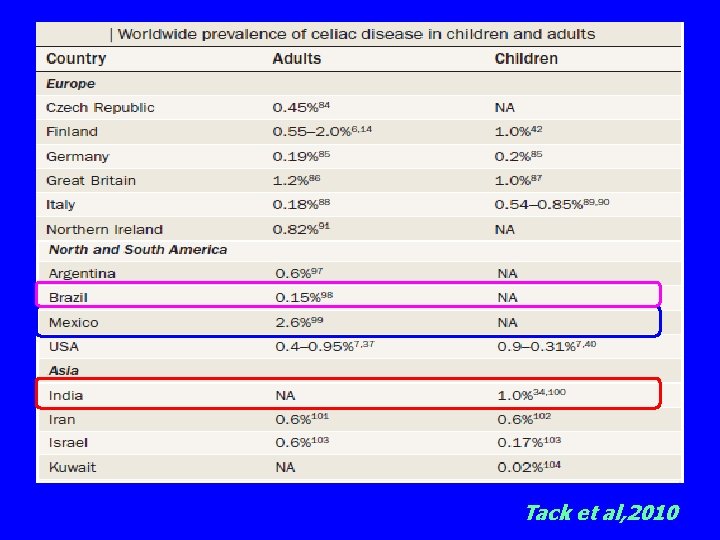
Tack et al, 2010
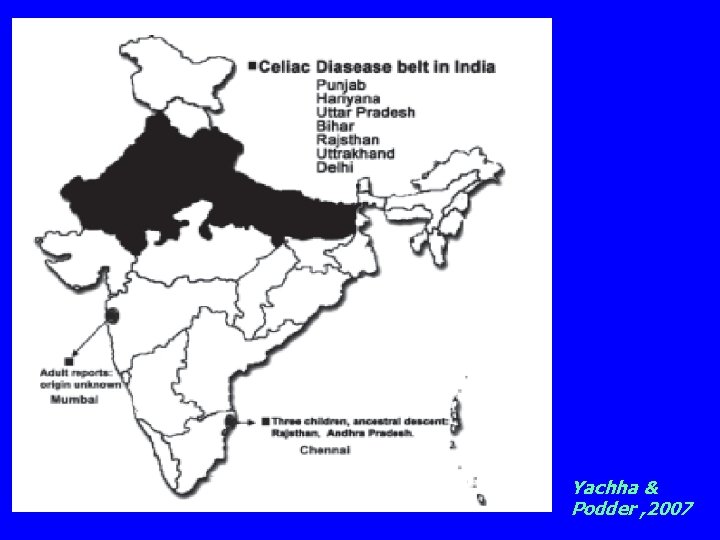
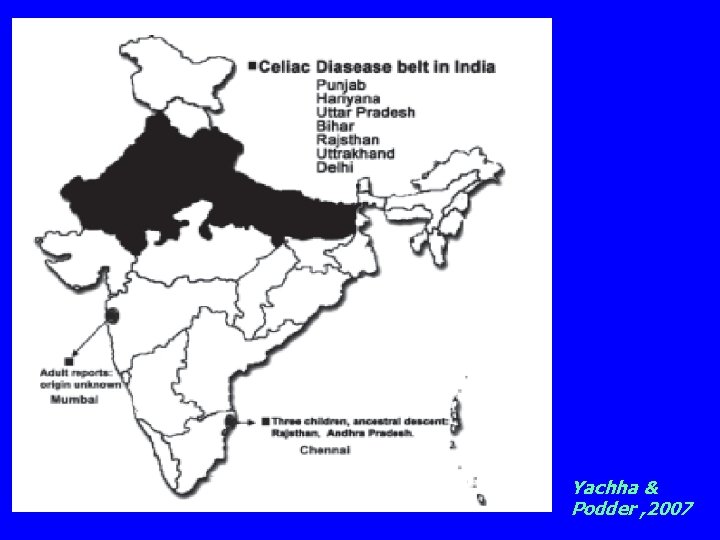
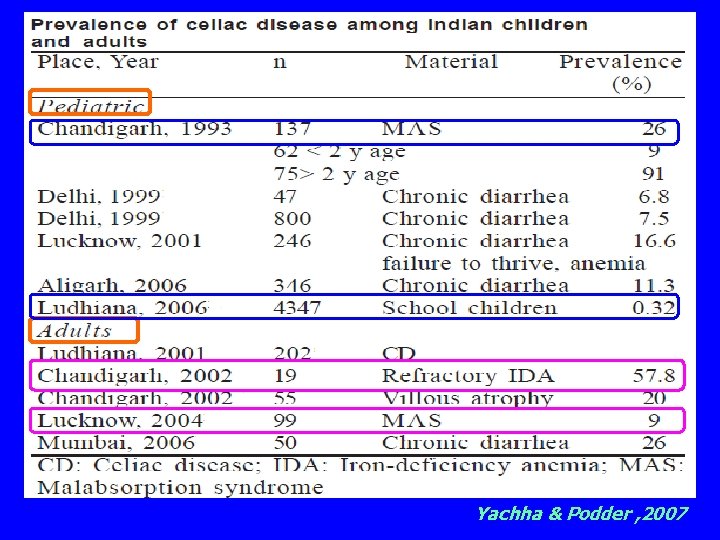
Yachha & Podder , 2007
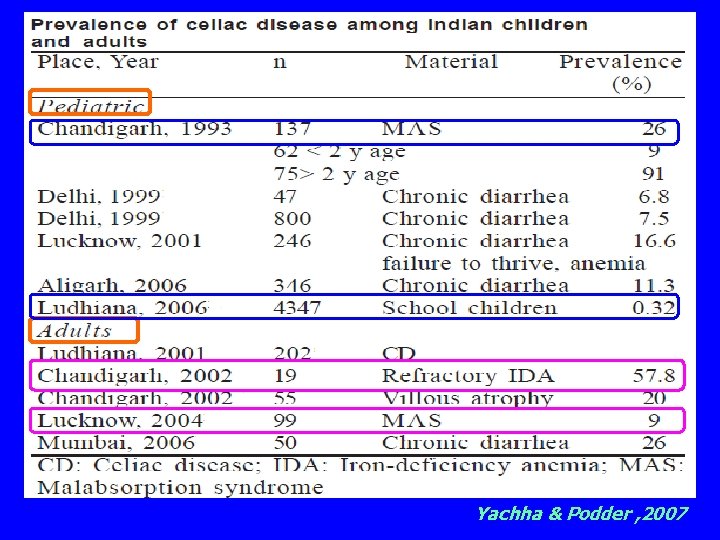
Yachha & Podder , 2007
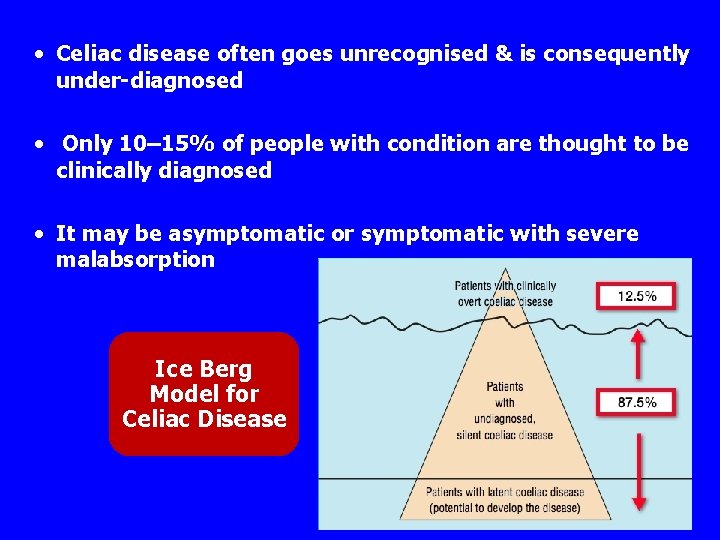
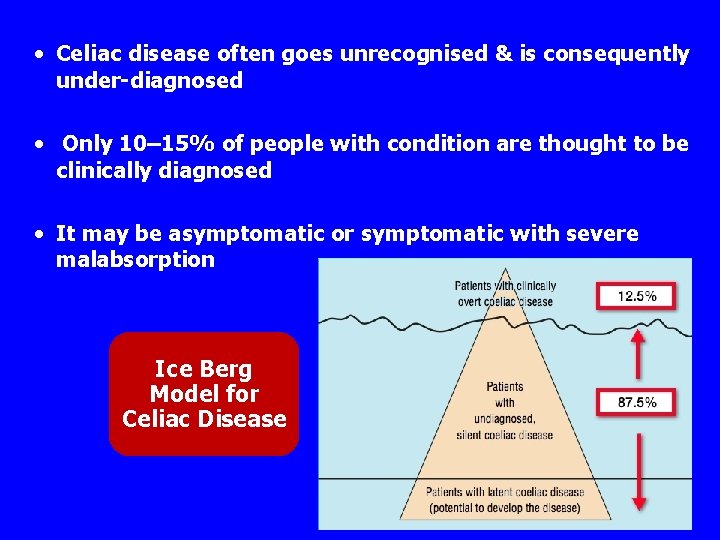
• Celiac disease often goes unrecognised & is consequently under-diagnosed • Only 10– 15% of people with condition are thought to be clinically diagnosed • It may be asymptomatic or symptomatic with severe malabsorption Ice Berg Model for Celiac Disease



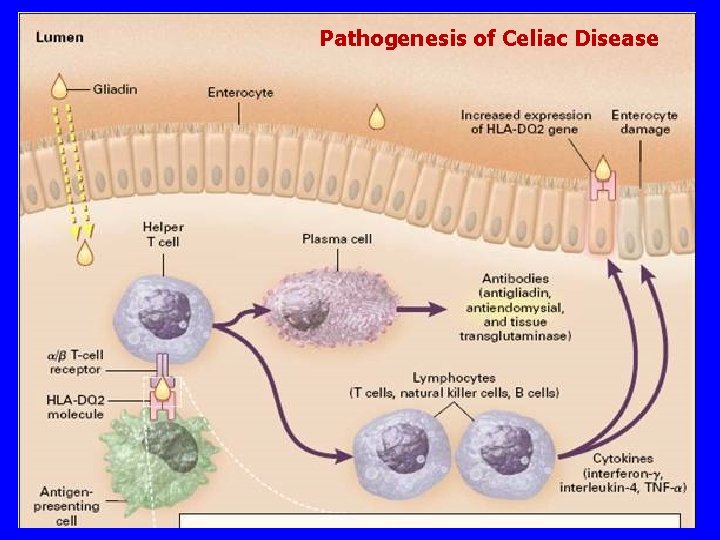
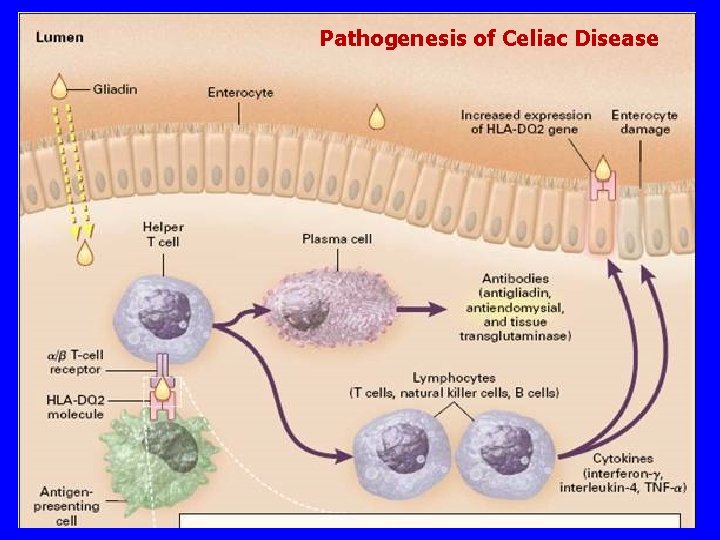
Pathogenesis of Celiac Disease
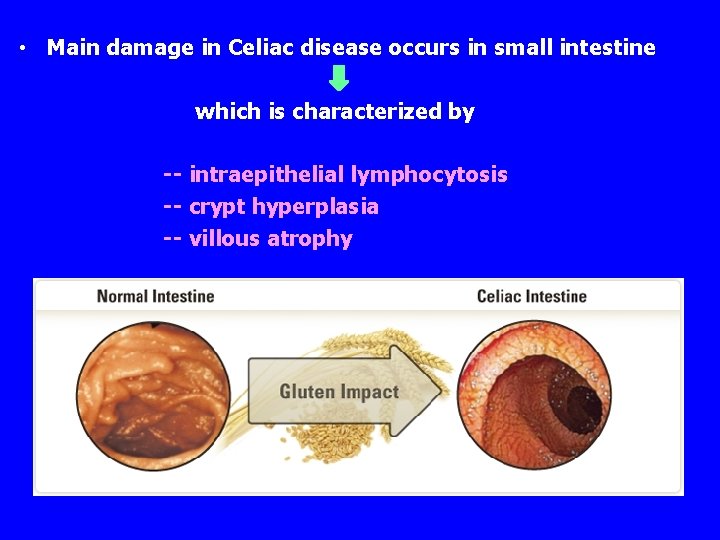
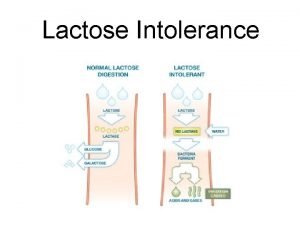
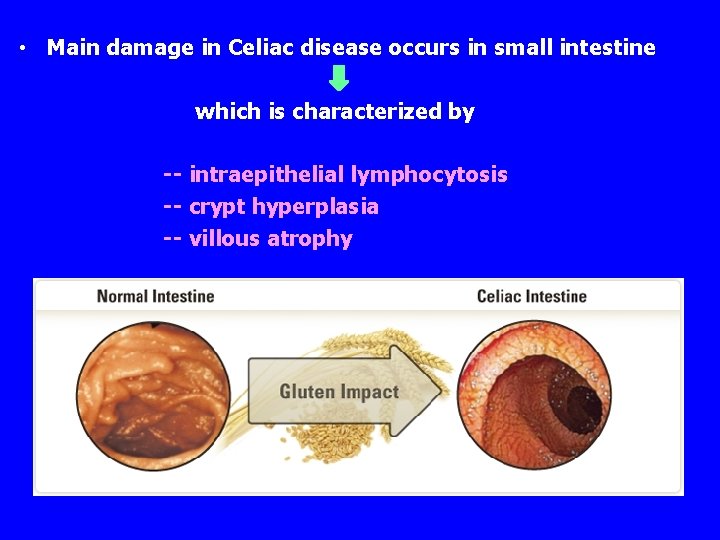
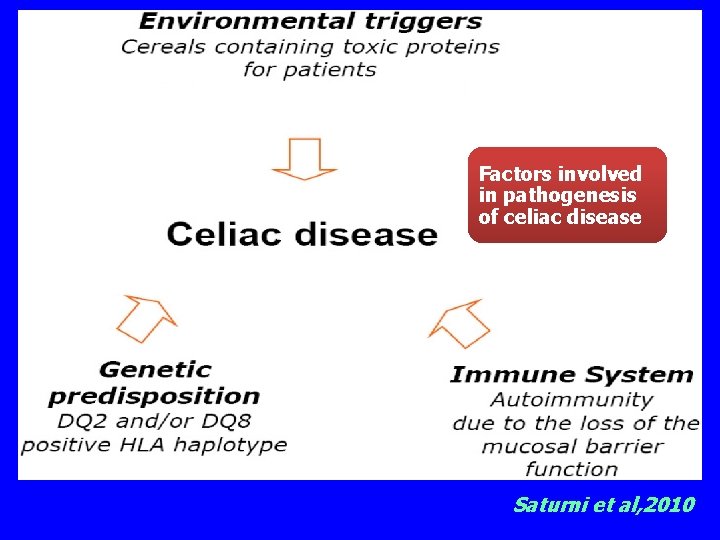
• Main damage in Celiac disease occurs in small intestine which is characterized by -- intraepithelial lymphocytosis -- crypt hyperplasia -- villous atrophy
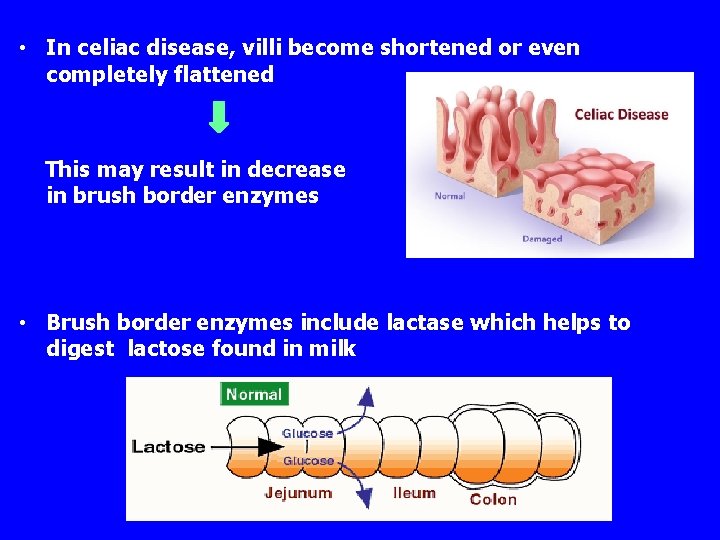
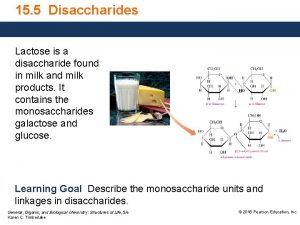
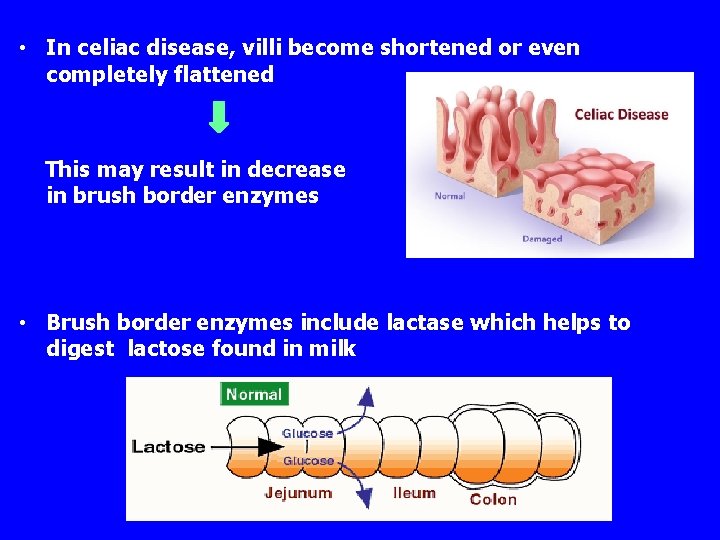
• In celiac disease, villi become shortened or even completely flattened This may result in decrease in brush border enzymes • Brush border enzymes include lactase which helps to digest lactose found in milk
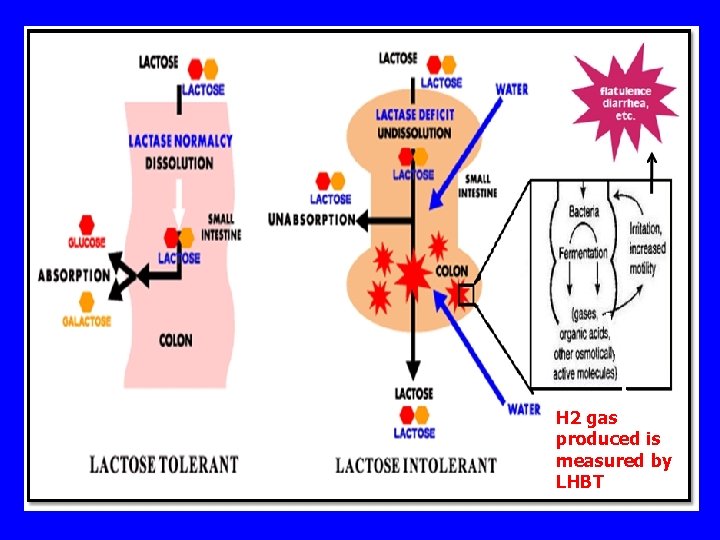
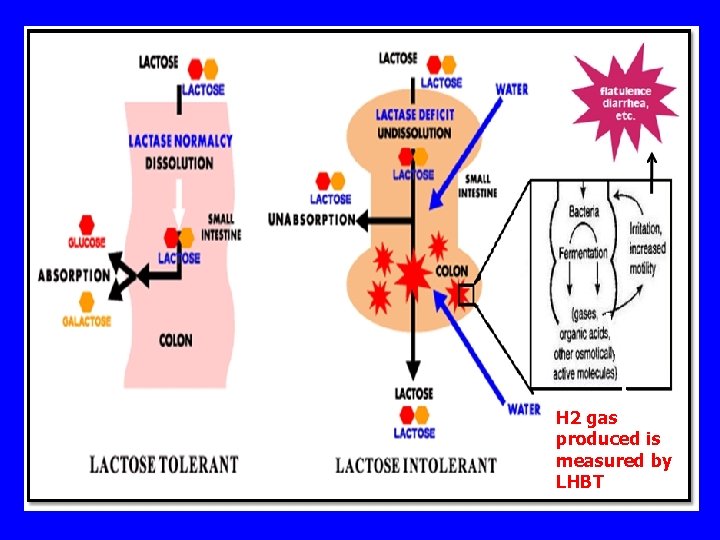
H 2 gas produced is measured by LHBT
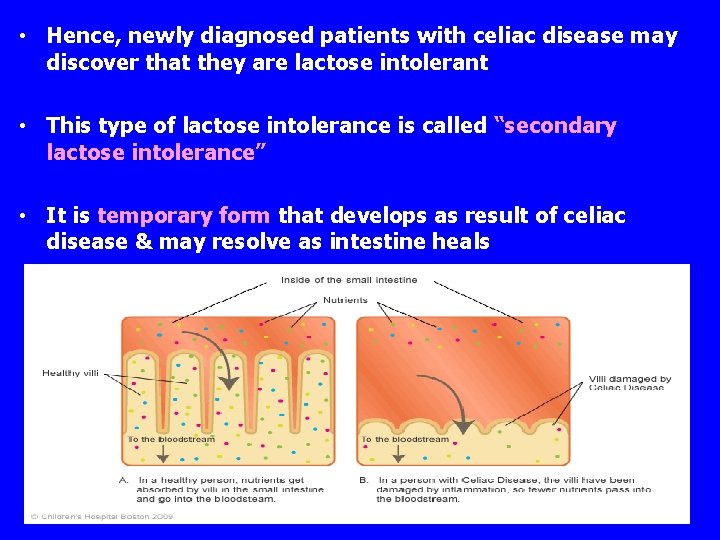
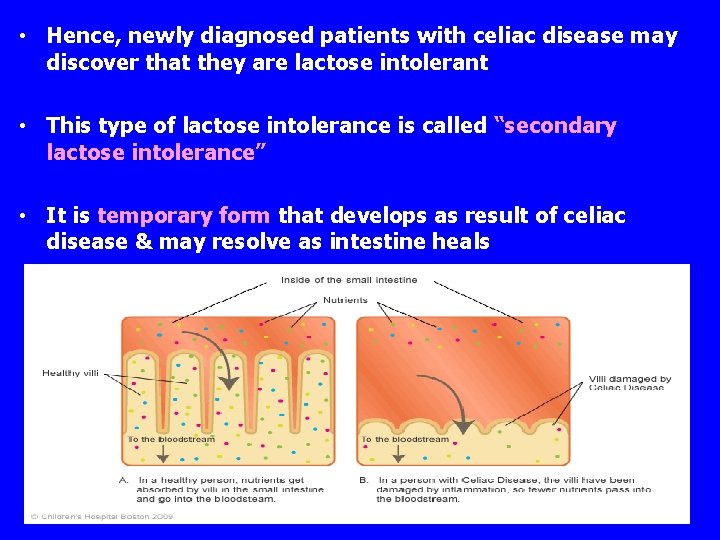
• Hence, newly diagnosed patients with celiac disease may discover that they are lactose intolerant • This type of lactose intolerance is called “secondary lactose intolerance” • It is temporary form that develops as result of celiac disease & may resolve as intestine heals
Aim of the study To elucidate lactose intolerance in children with celiac disease
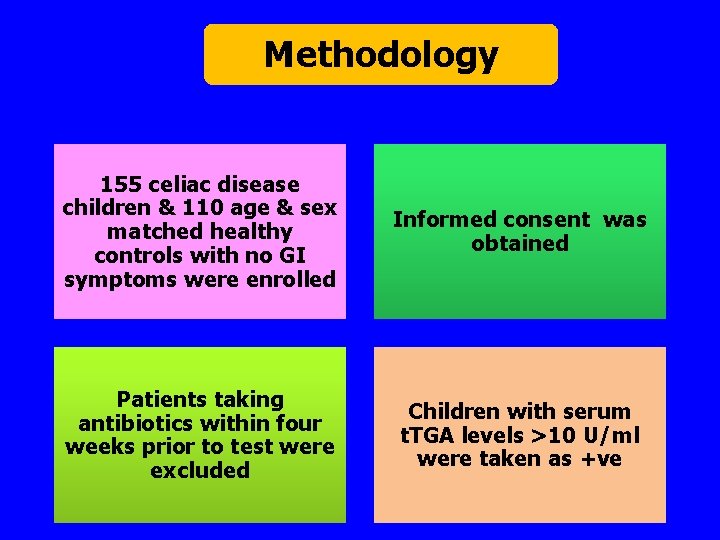
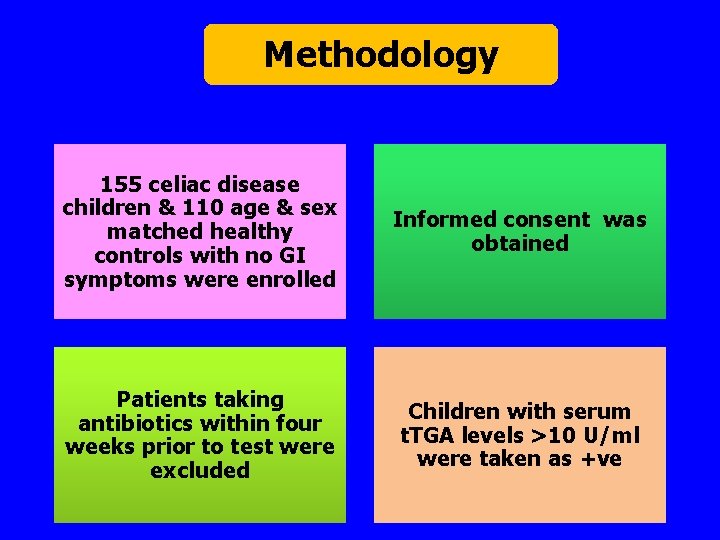
Methodology 155 celiac disease children & 110 age & sex matched healthy controls with no GI symptoms were enrolled Informed consent was obtained Patients taking antibiotics within four weeks prior to test were excluded Children with serum t. TGA levels >10 U/ml were taken as +ve
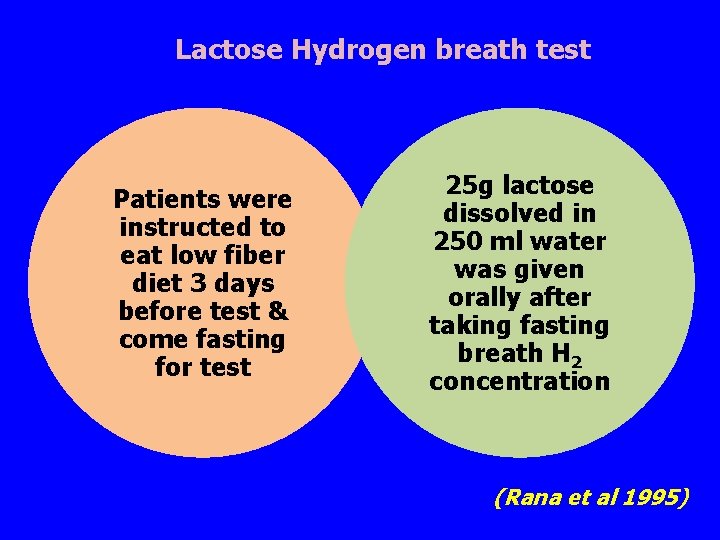
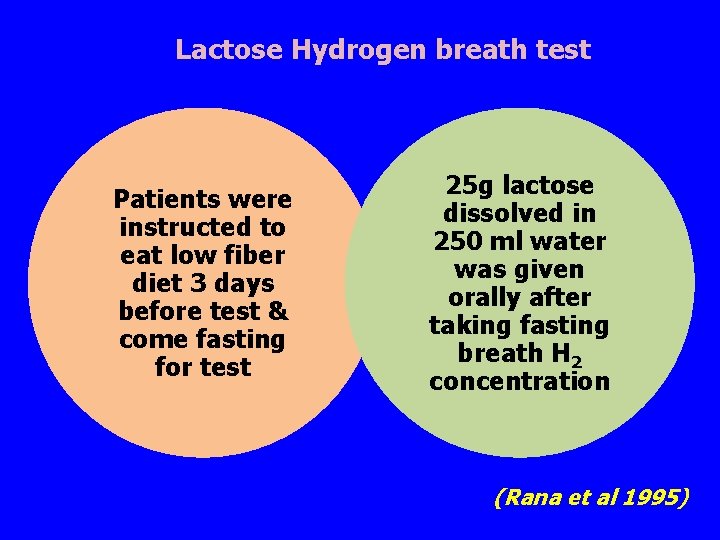
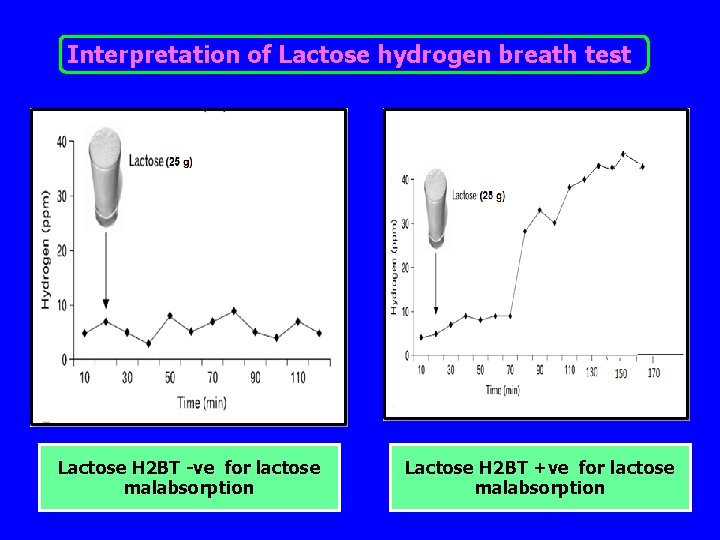
Lactose Hydrogen breath test Patients were instructed to eat low fiber diet 3 days before test & come fasting for test 25 g lactose dissolved in 250 ml water was given orally after taking fasting breath H 2 concentration (Rana et al 1995)
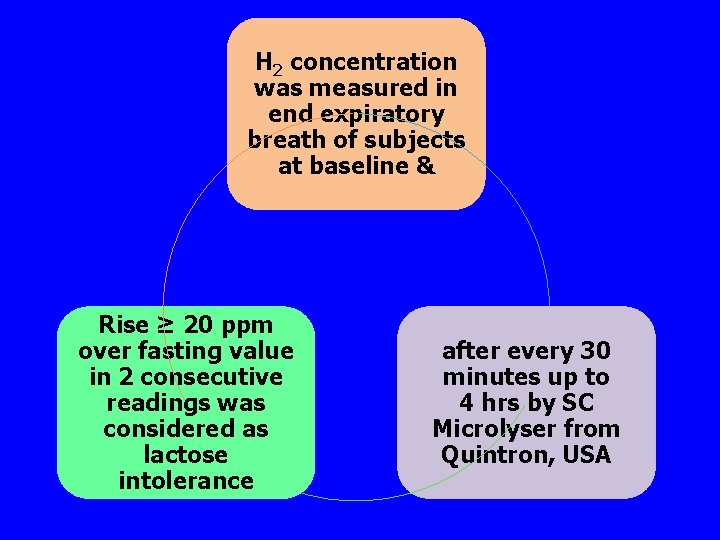
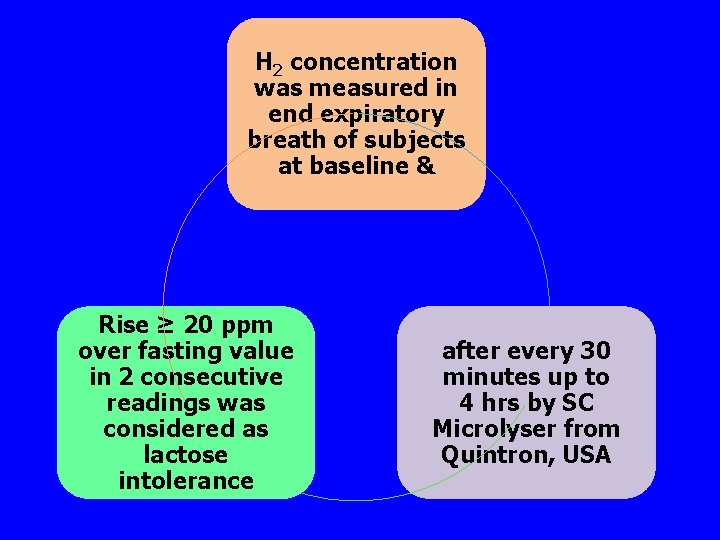
H 2 concentration was measured in end expiratory breath of subjects at baseline & Rise ≥ 20 ppm over fasting value in 2 consecutive readings was considered as lactose intolerance after every 30 minutes up to 4 hrs by SC Microlyser from Quintron, USA
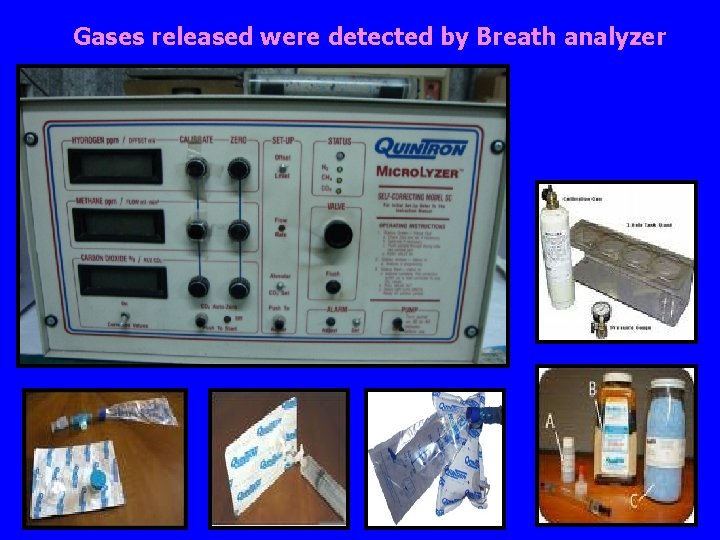
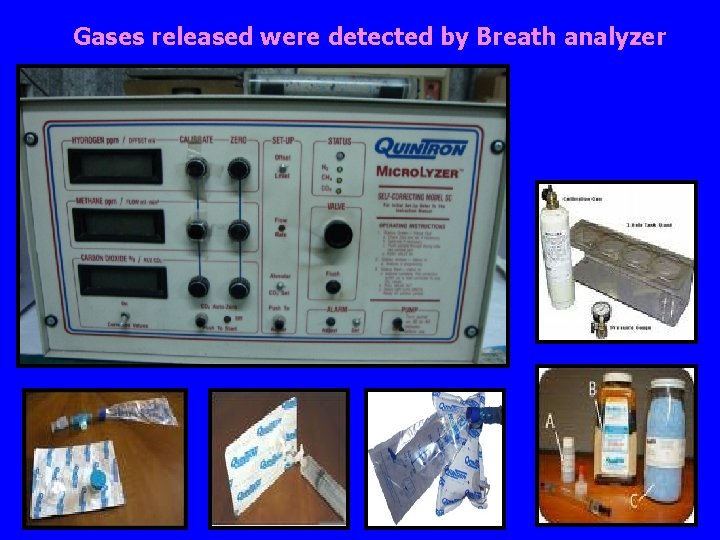
Gases released were detected by Breath analyzer
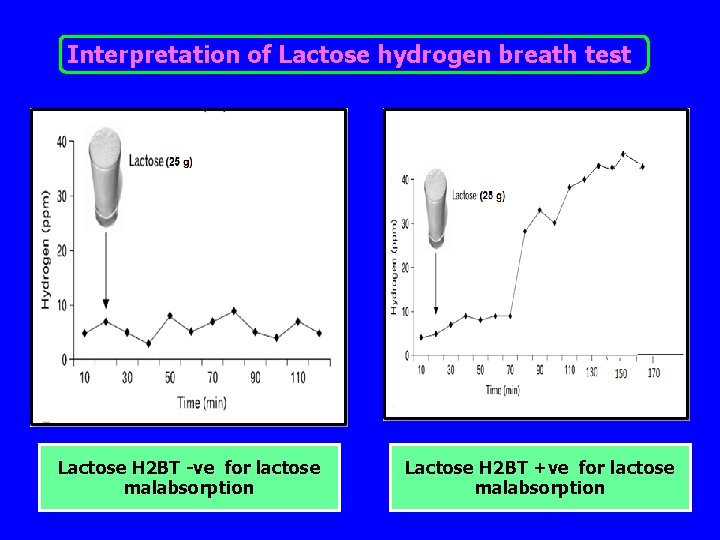
Interpretation of Lactose hydrogen breath test Lactose H 2 BT -ve for lactose malabsorption Lactose H 2 BT +ve for lactose malabsorption
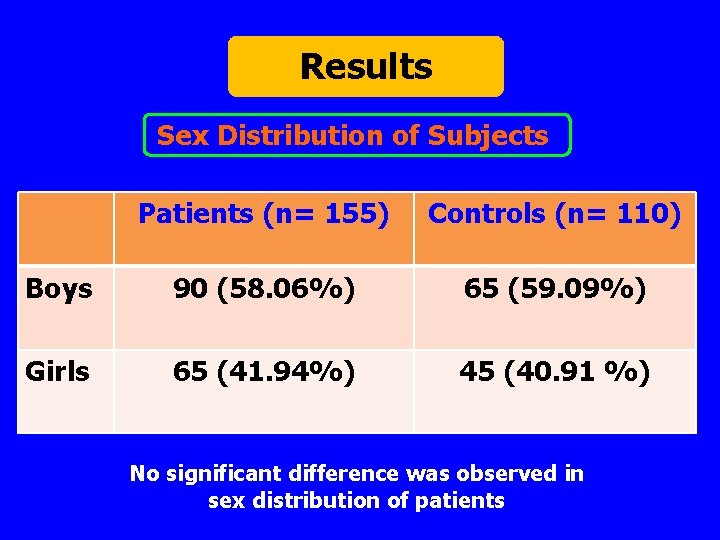
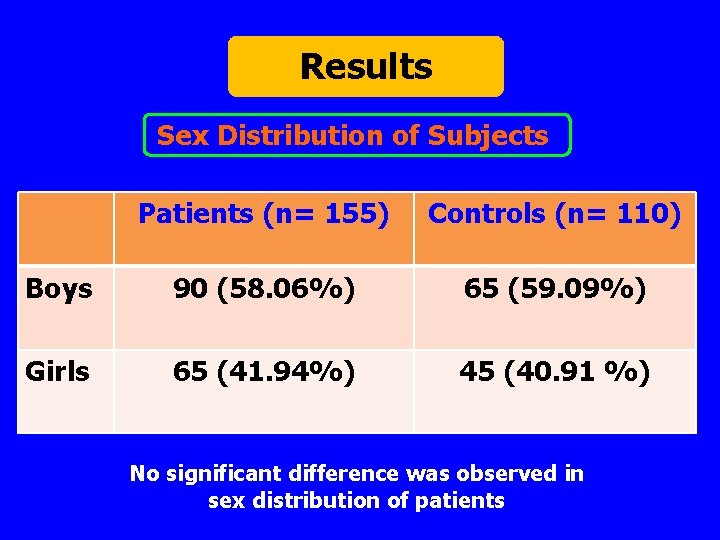
Results Sex Distribution of Subjects Patients (n= 155) Controls (n= 110) Boys 90 (58. 06%) 65 (59. 09%) Girls 65 (41. 94%) 45 (40. 91 %) No significant difference was observed in sex distribution of patients
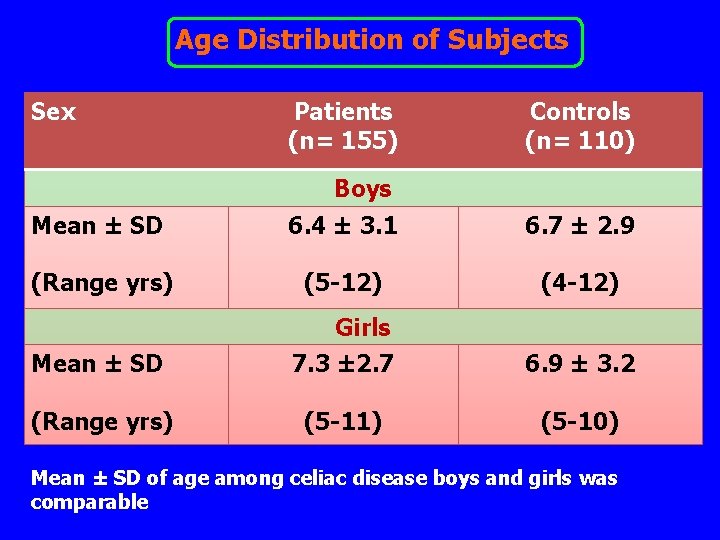
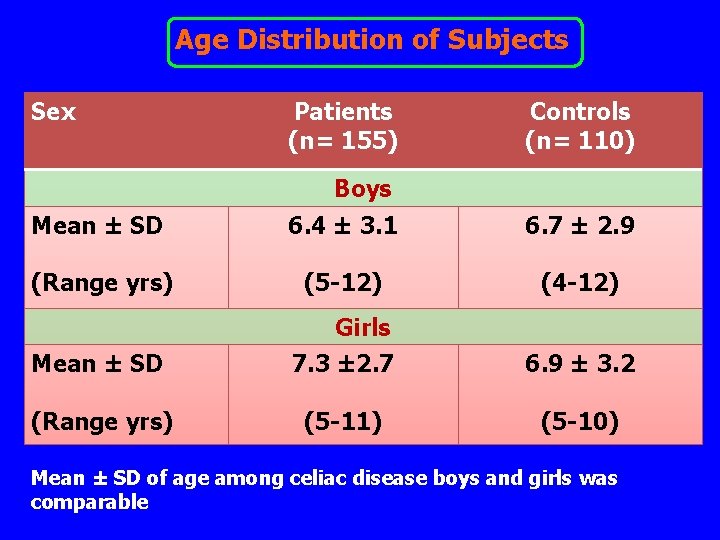
Age Distribution of Subjects Sex Patients (n= 155) Controls (n= 110) Boys Mean ± SD 6. 4 ± 3. 1 6. 7 ± 2. 9 (Range yrs) (5 -12) (4 -12) Mean ± SD Girls 7. 3 ± 2. 7 6. 9 ± 3. 2 (Range yrs) (5 -11) (5 -10) Mean ± SD of age among celiac disease boys and girls was comparable
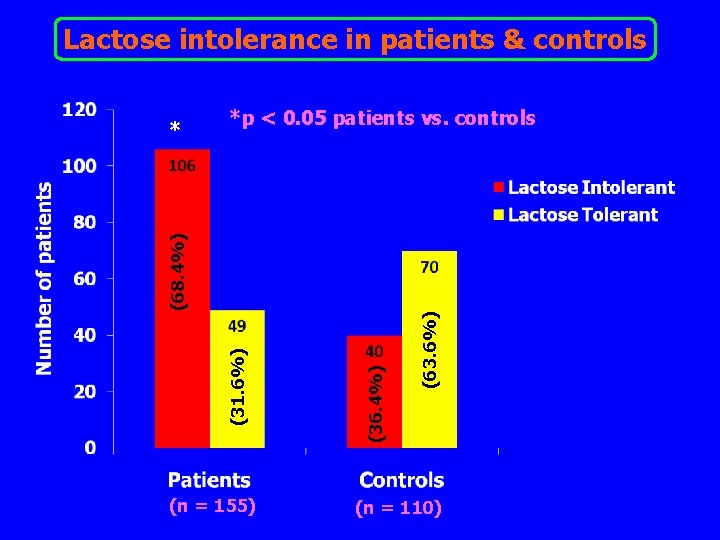
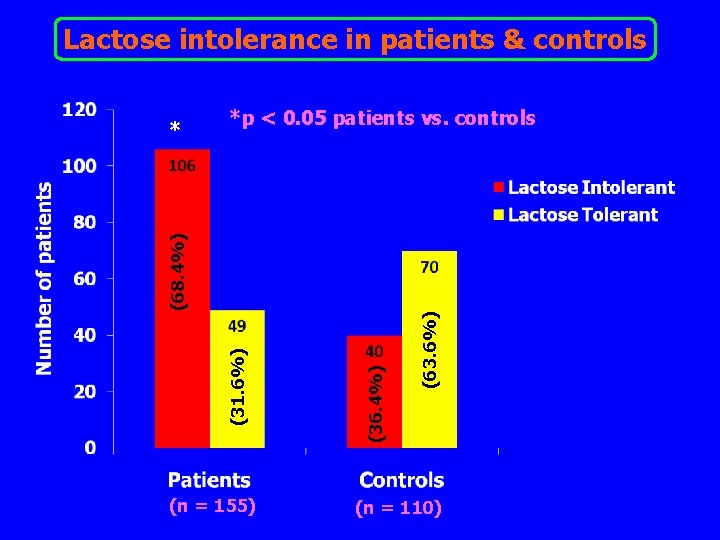
Lactose intolerance in patients & controls *p < 0. 05 patients vs. controls (n = 155) (63. 6%) (36. 4%) (31. 6%) (68. 4%) * (n = 110)
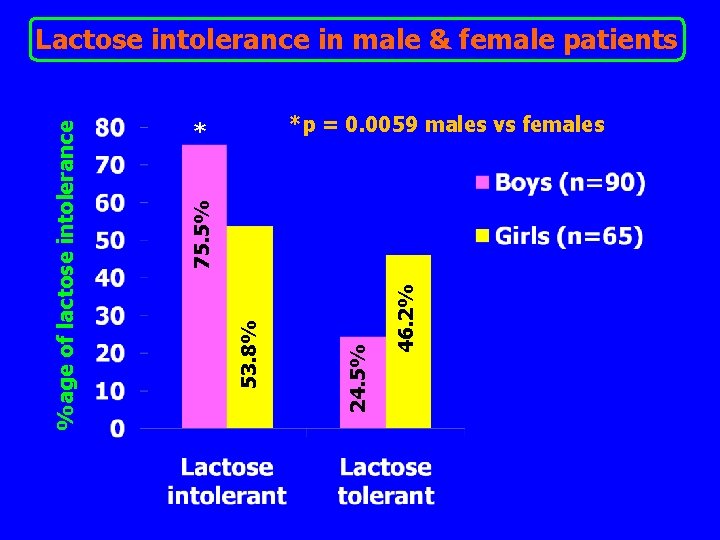
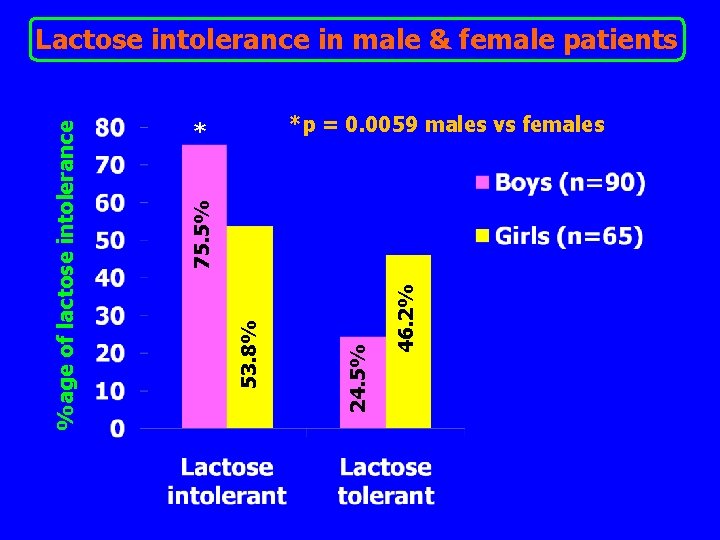
*p = 0. 0059 males vs females * 46. 2% 24. 5% 53. 8% 75. 5% %age of lactose intolerance Lactose intolerance in male & female patients
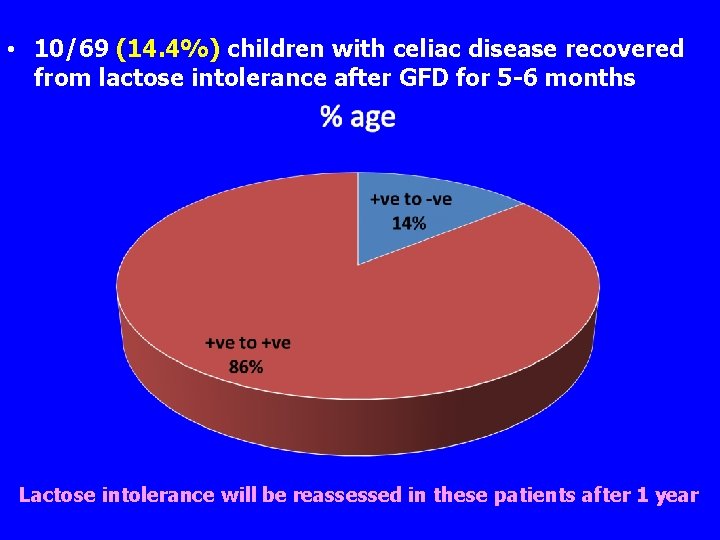
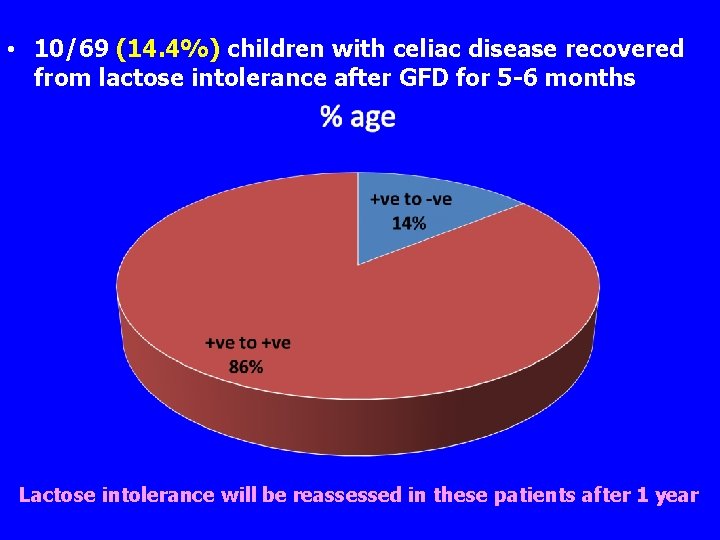
• 10/69 (14. 4%) children with celiac disease recovered from lactose intolerance after GFD for 5 -6 months Lactose intolerance will be reassessed in these patients after 1 year
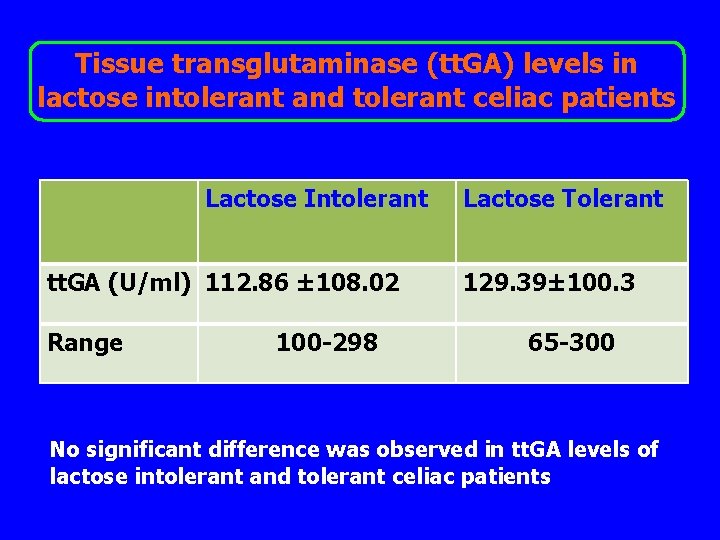
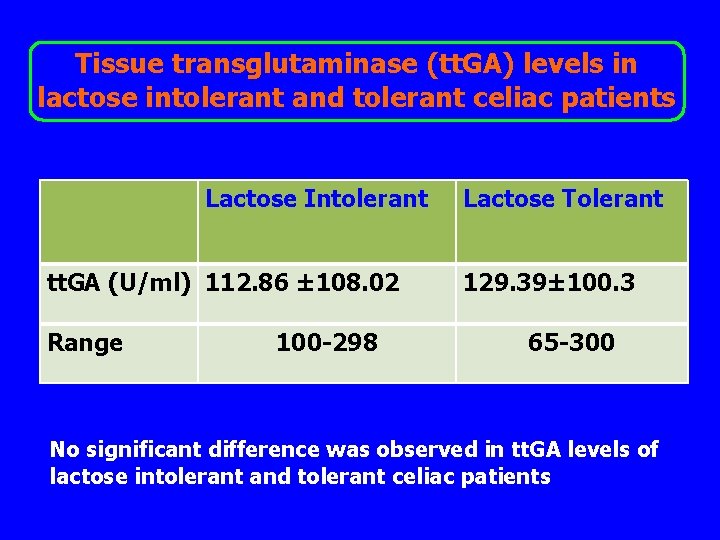
Tissue transglutaminase (tt. GA) levels in lactose intolerant and tolerant celiac patients Lactose Intolerant tt. GA (U/ml) 112. 86 ± 108. 02 Range 100 -298 Lactose Tolerant 129. 39± 100. 3 65 -300 No significant difference was observed in tt. GA levels of lactose intolerant and tolerant celiac patients
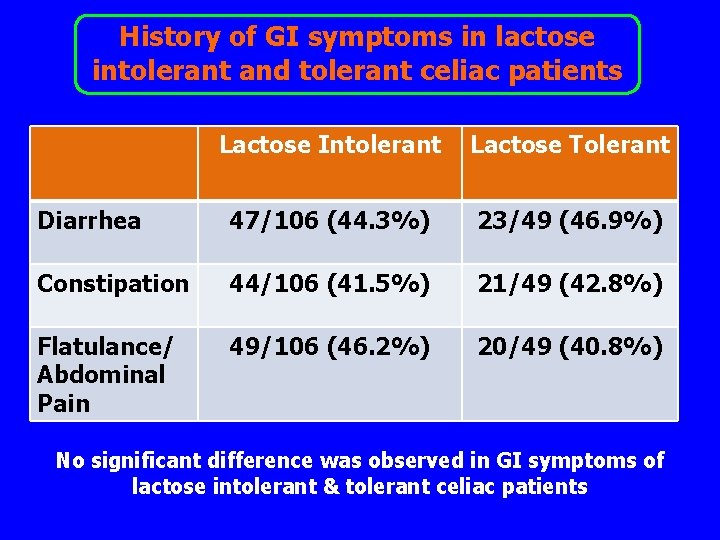
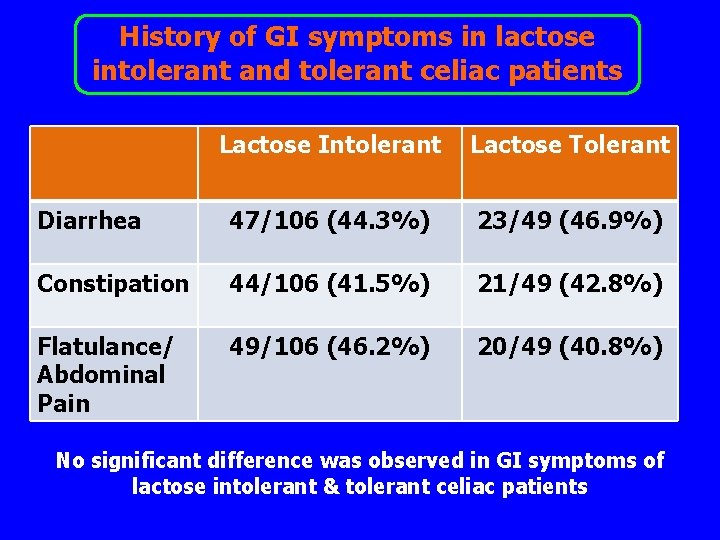
History of GI symptoms in lactose intolerant and tolerant celiac patients Lactose Intolerant Lactose Tolerant Diarrhea 47/106 (44. 3%) 23/49 (46. 9%) Constipation 44/106 (41. 5%) 21/49 (42. 8%) Flatulance/ Abdominal Pain 49/106 (46. 2%) 20/49 (40. 8%) No significant difference was observed in GI symptoms of lactose intolerant & tolerant celiac patients

VILLOUS ATROPHY LACTASE DEFICIENCY LACTOSE INTOLERANCE LACTOSE TOLERANT GLUTEN FREE DIET

Some Studies related to Celiac disease and Lactose intolerance
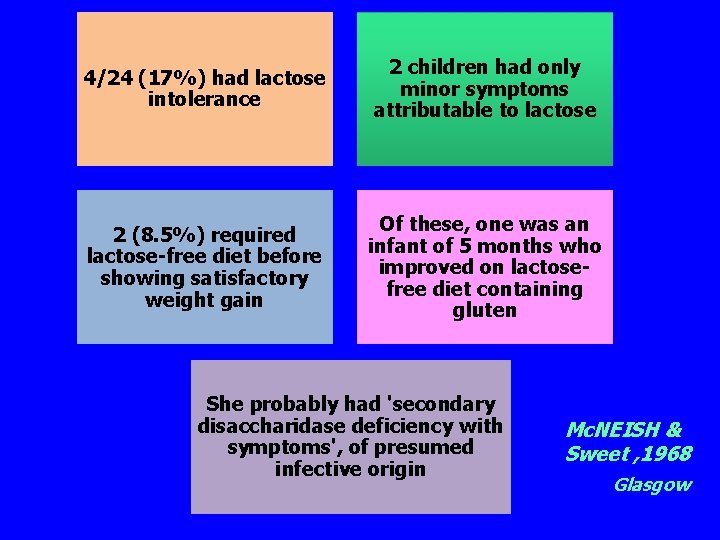
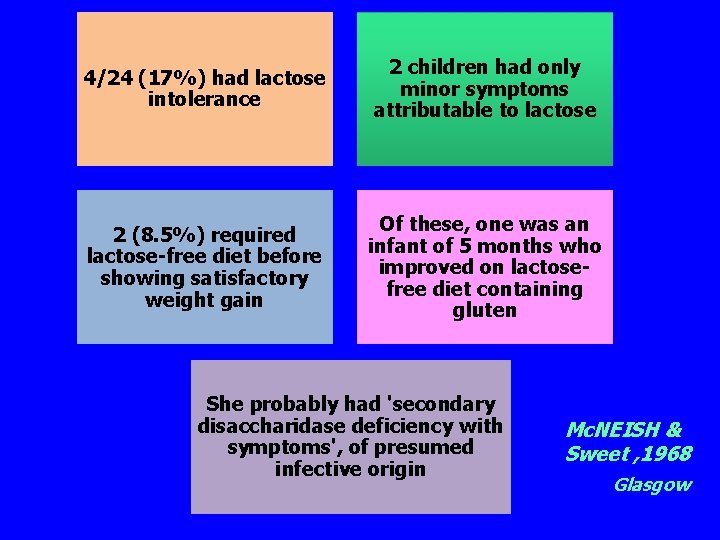
4/24 (17%) had lactose intolerance 2 children had only minor symptoms attributable to lactose 2 (8. 5%) required lactose-free diet before showing satisfactory weight gain Of these, one was an infant of 5 months who improved on lactosefree diet containing gluten She probably had 'secondary disaccharidase deficiency with symptoms', of presumed infective origin Mc. NEISH & Sweet , 1968 Glasgow
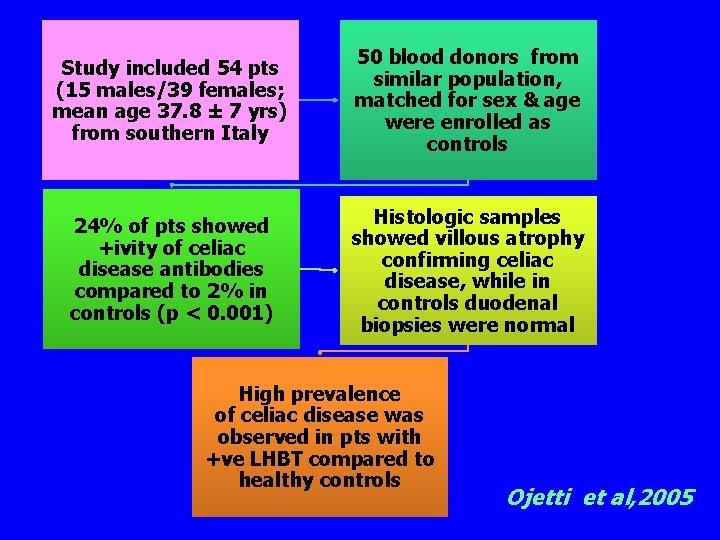
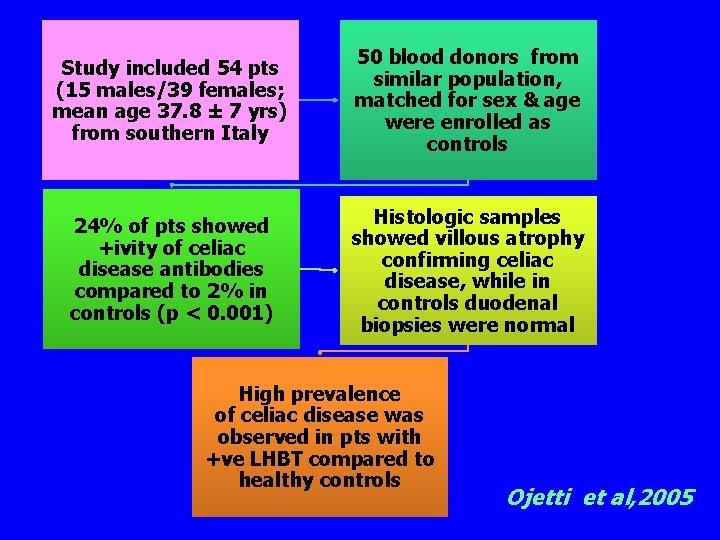
Study included 54 pts (15 males/39 females; mean age 37. 8 ± 7 yrs) from southern Italy 50 blood donors from similar population, matched for sex & age were enrolled as controls 24% of pts showed +ivity of celiac disease antibodies compared to 2% in controls (p < 0. 001) Histologic samples showed villous atrophy confirming celiac disease, while in controls duodenal biopsies were normal High prevalence of celiac disease was observed in pts with +ve LHBT compared to healthy controls Ojetti et al, 2005
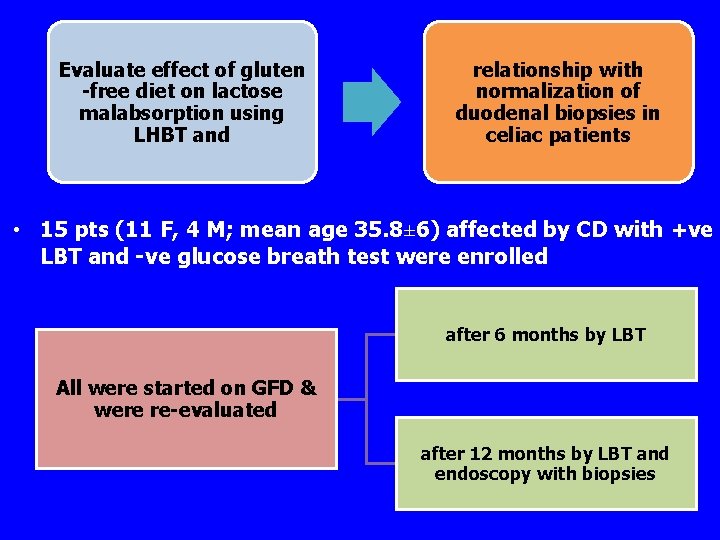
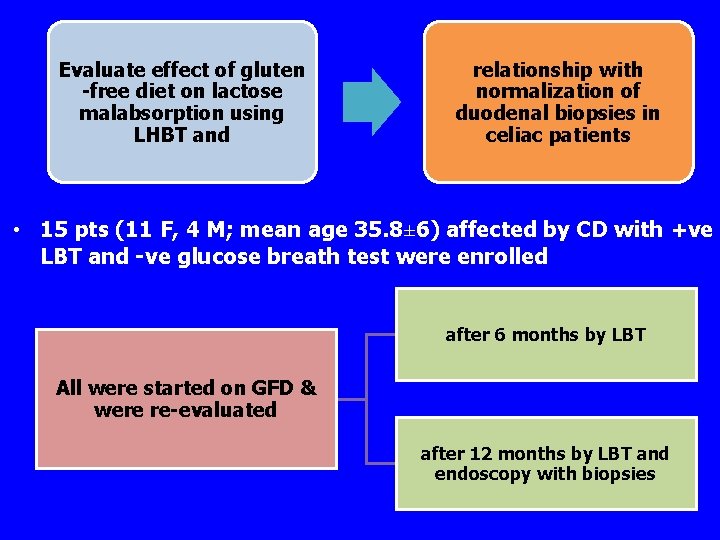
Evaluate effect of gluten -free diet on lactose malabsorption using LHBT and relationship with normalization of duodenal biopsies in celiac patients • 15 pts (11 F, 4 M; mean age 35. 8± 6) affected by CD with +ve LBT and -ve glucose breath test were enrolled after 6 months by LBT All were started on GFD & were re-evaluated after 12 months by LBT and endoscopy with biopsies
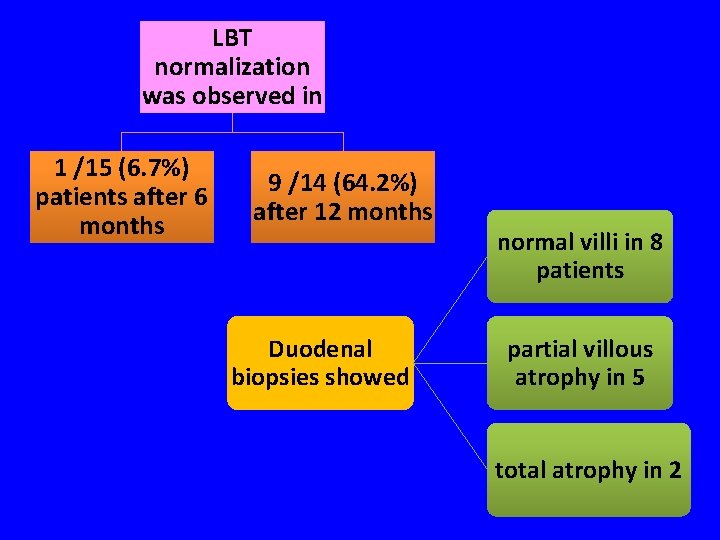
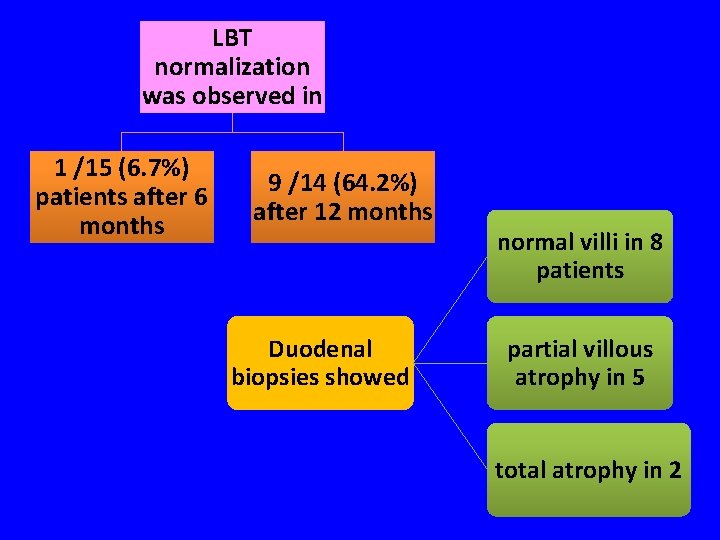
LBT normalization was observed in 1 /15 (6. 7%) patients after 6 months 9 /14 (64. 2%) after 12 months Duodenal biopsies showed normal villi in 8 patients partial villous atrophy in 5 total atrophy in 2
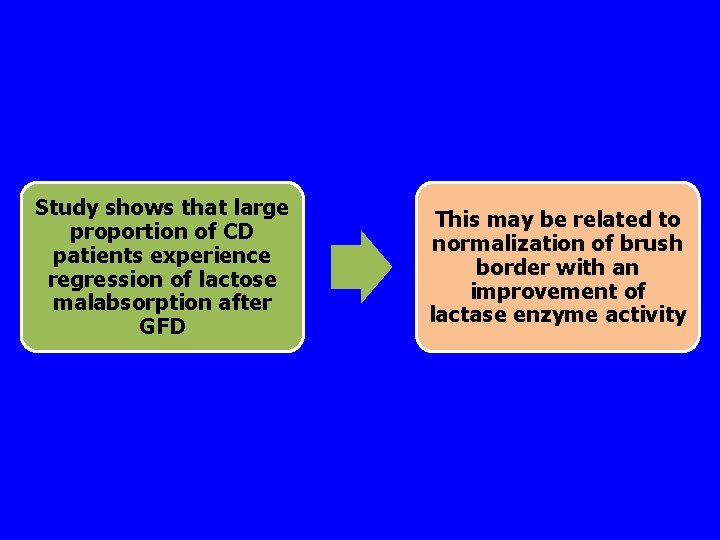
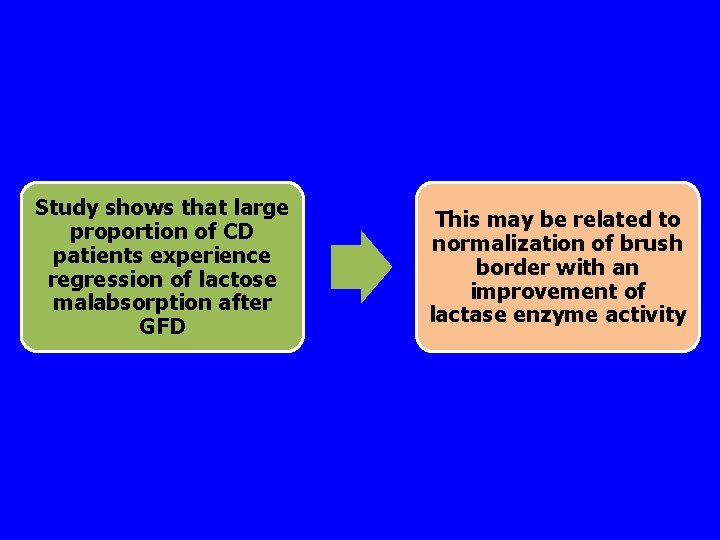
Study shows that large proportion of CD patients experience regression of lactose malabsorption after GFD This may be related to normalization of brush border with an improvement of lactase enzyme activity
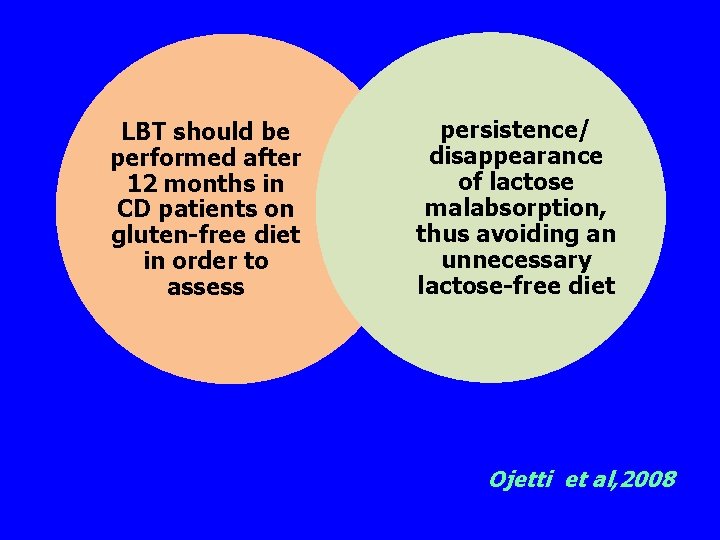
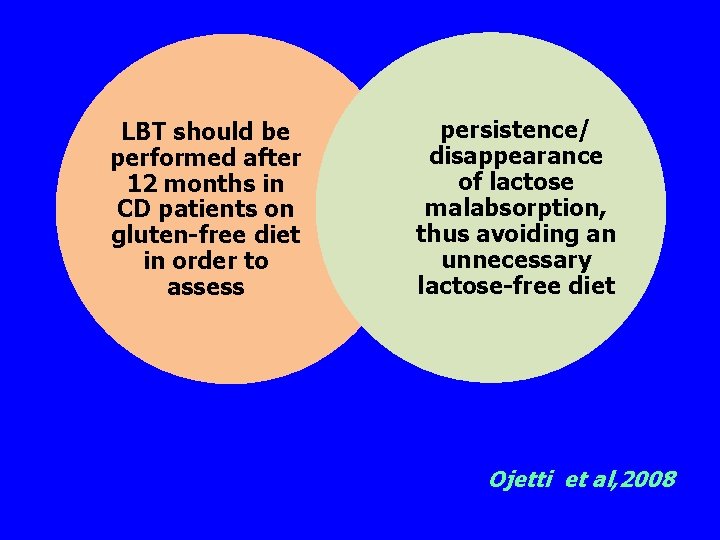
LBT should be performed after 12 months in CD patients on gluten-free diet in order to assess persistence/ disappearance of lactose malabsorption, thus avoiding an unnecessary lactose-free diet Ojetti et al, 2008
Conclusion This study indicates that lactose intolerance is common among children with celiac disease which can be one of the causes for gastrointestinal symptoms
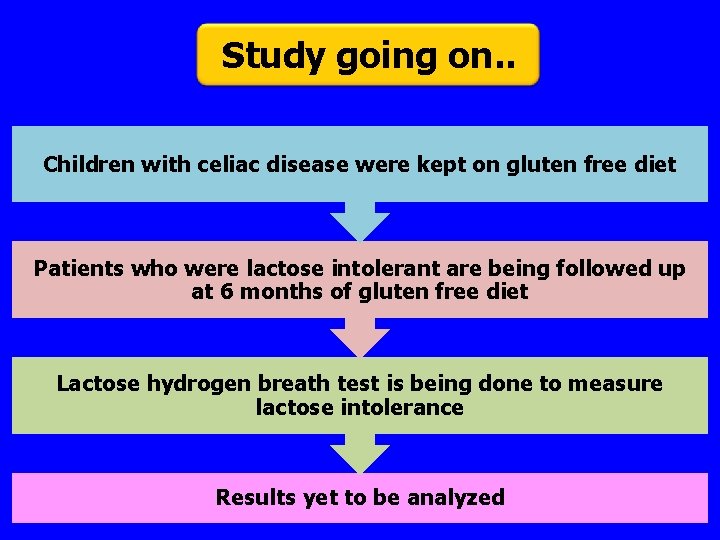
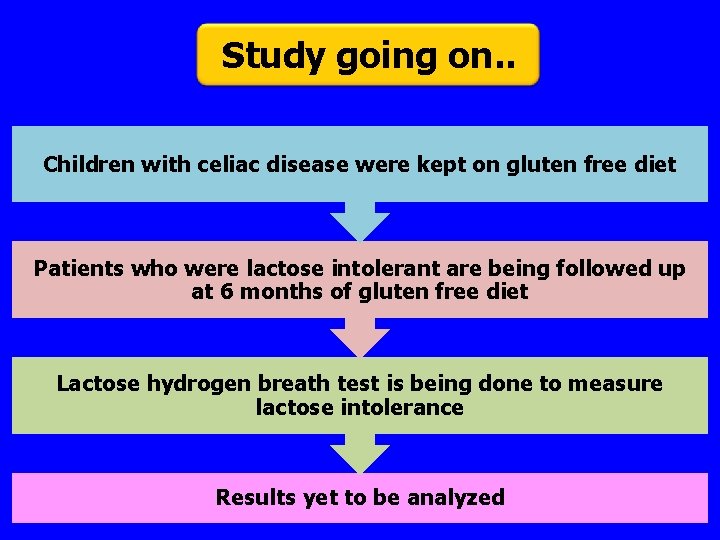
Study going on. . Children with celiac disease were kept on gluten free diet Patients who were lactose intolerant are being followed up at 6 months of gluten free diet Lactose hydrogen breath test is being done to measure lactose intolerance Results yet to be analyzed

Thank you…
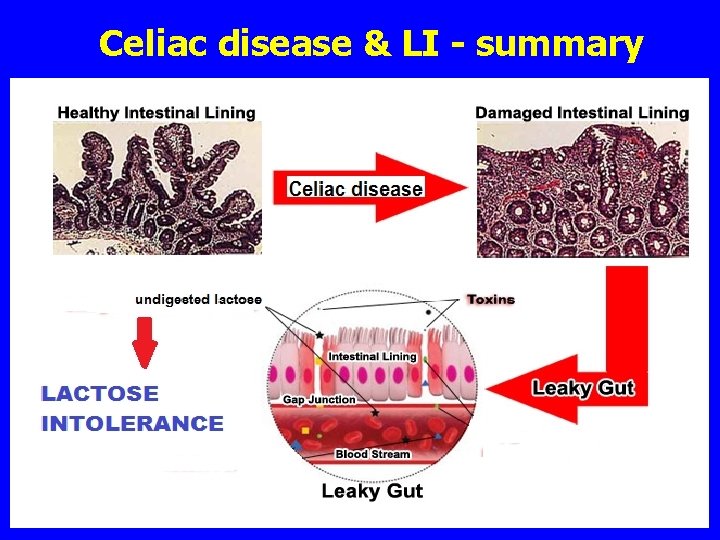
Celiac disease & LI - summary
 Enzymes and lactose intolerance lab answers
Enzymes and lactose intolerance lab answers Intolérance au lactose
Intolérance au lactose Lactose intolerance countries
Lactose intolerance countries Lactose intolerance
Lactose intolerance Lactose intolerance histology
Lactose intolerance histology Lactose intolerance gene
Lactose intolerance gene Hoch₂
Hoch₂ Prof tufan kutlu
Prof tufan kutlu Causes of malabsorption
Causes of malabsorption Celiac disease in french
Celiac disease in french Celiac disease pes statement
Celiac disease pes statement Marsh classification of celiac disease
Marsh classification of celiac disease Pes statement for celiac disease
Pes statement for celiac disease Case study celiac disease
Case study celiac disease Celiac disease colville
Celiac disease colville Communicable disease and non communicable disease
Communicable disease and non communicable disease The crucible intolerance
The crucible intolerance Stibio intolérance
Stibio intolérance Reverend hale quotes
Reverend hale quotes Maltose intolerance
Maltose intolerance Galctosemia
Galctosemia Function of polysaccharides
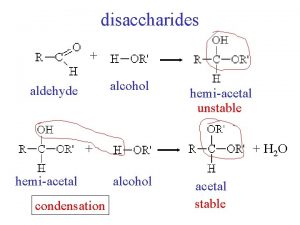
Function of polysaccharides Hemiacetal group in lactose
Hemiacetal group in lactose What is vikramsheel vihar
What is vikramsheel vihar Niohc
Niohc Mutual self help housing
Mutual self help housing Celiac artery and mesenteric artery
Celiac artery and mesenteric artery North east and north cumbria integrated care system
North east and north cumbria integrated care system Chapter 14 north and south
Chapter 14 north and south Cheese lactose chart
Cheese lactose chart Pont oxydique
Pont oxydique Lactose
Lactose Sucrosazone
Sucrosazone Antigenic structure of e coli
Antigenic structure of e coli Chemical properties of monosaccharides
Chemical properties of monosaccharides Lactose is a disaccharide found in milk
Lactose is a disaccharide found in milk Lactose
Lactose ágar sangue
ágar sangue Lactosen
Lactosen Lactose
Lactose Lactose glycemic index
Lactose glycemic index Untuk mengamati ekspresi gen lactose
Untuk mengamati ekspresi gen lactose Lactobacillus bulgaricus converts lactose to *
Lactobacillus bulgaricus converts lactose to *