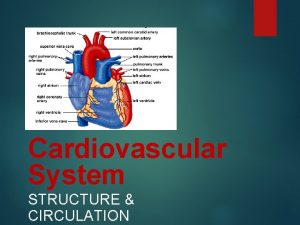
Cardiovascular System Part I The Heart Size of







- Slides: 40
Cardiovascular System Part I The Heart
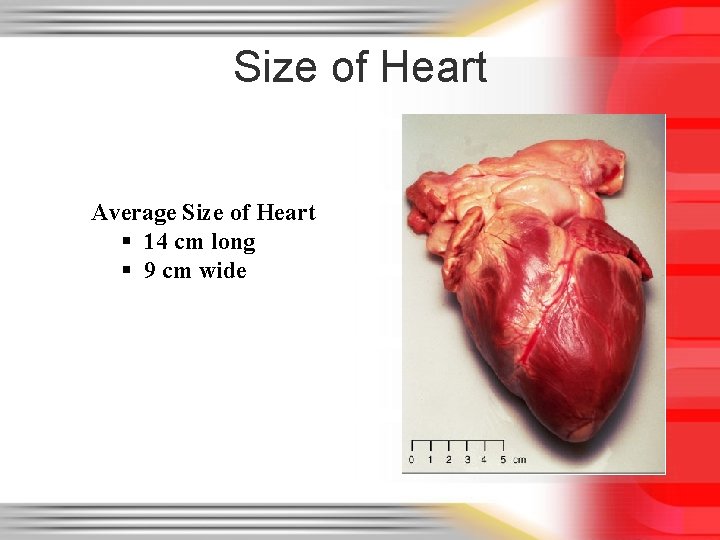
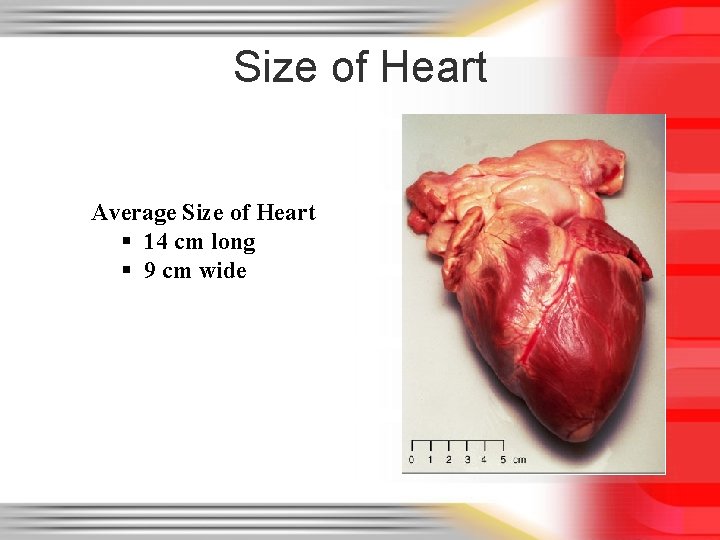
Size of Heart Average Size of Heart § 14 cm long § 9 cm wide
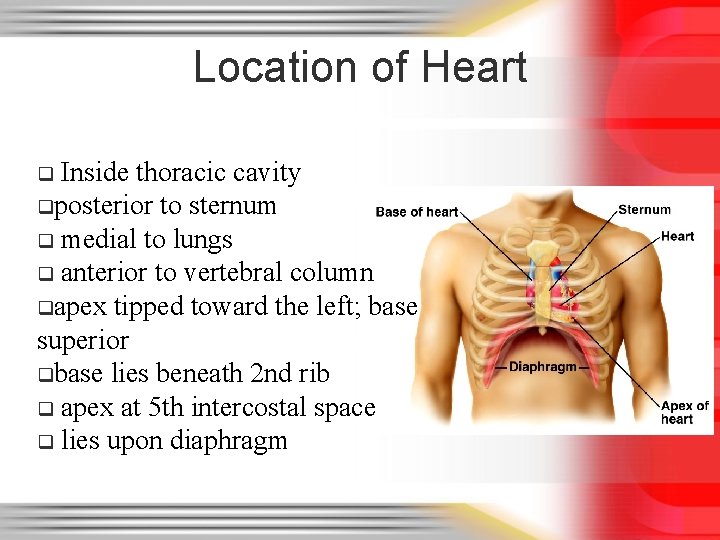
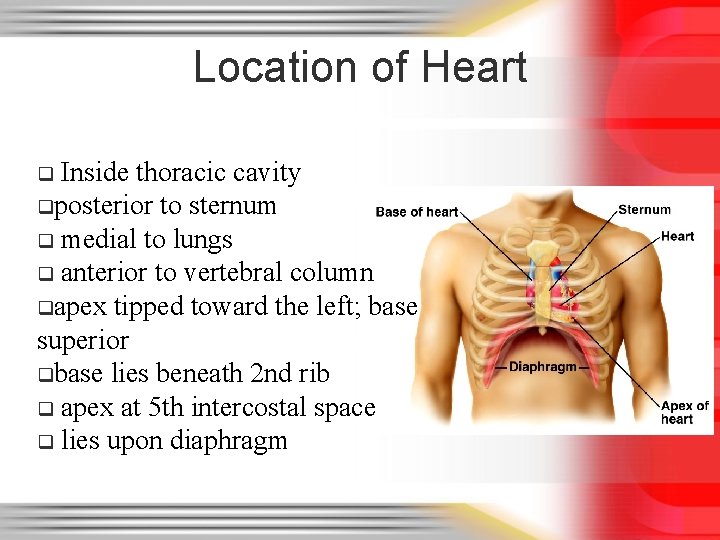
Location of Heart Inside thoracic cavity qposterior to sternum q medial to lungs q anterior to vertebral column qapex tipped toward the left; base superior qbase lies beneath 2 nd rib q apex at 5 th intercostal space q lies upon diaphragm q



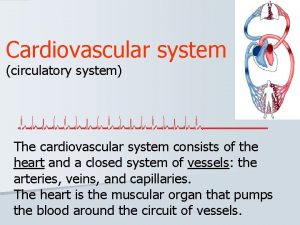
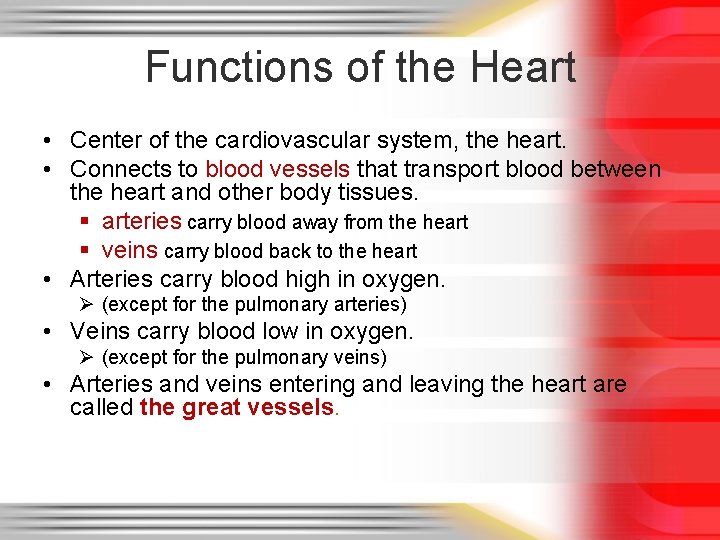
Functions of the Heart • Center of the cardiovascular system, the heart. • Connects to blood vessels that transport blood between the heart and other body tissues. § arteries carry blood away from the heart § veins carry blood back to the heart • Arteries carry blood high in oxygen. Ø (except for the pulmonary arteries) • Veins carry blood low in oxygen. Ø (except for the pulmonary veins) • Arteries and veins entering and leaving the heart are called the great vessels.
Characteristics and Functions of the Heart • Ensures the unidirectional flow of blood through both the heart and the blood vessels. • Backflow of blood is prevented by valves within the heart. • Acts like two independent, side-by-side pumps that work independently but at the same rate. (double circuit) § one directs blood to the lungs for gas exchange § the other directs blood to body tissues for nutrient delivery
Characteristics and Functions of the Heart • Develops blood pressure through alternate cycles of heart wall contraction and relaxation. • Minimum blood pressure is essential to push blood through blood vessels to the body tissues for nutrient and waste exchange.
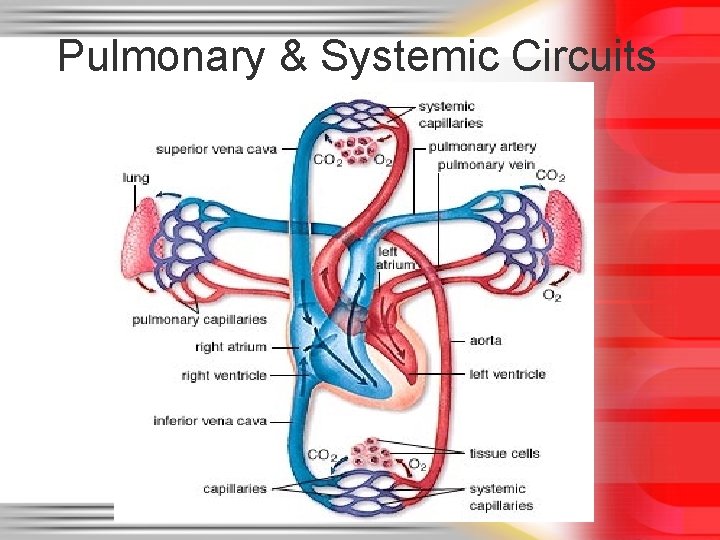
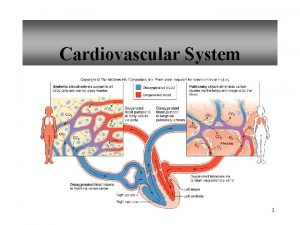
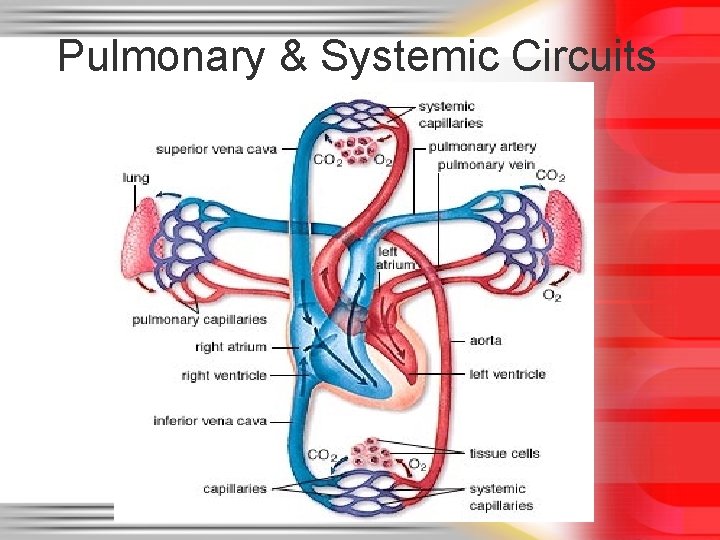
Pulmonary & Systemic Circuits
Pulmonary and Systemic Circuits • The pulmonary circuit consists of the chambers on the right side of the heart (right atrium and ventricle) as well as the pulmonary arteries and veins. § conveys blood to the lungs via pulmonary arteries § to reduce carbon dioxide and replenish oxygen levels in the blood § Blood returns to the heart in pulmonary veins
Pulmonary and Systemic Circuits • Blood returns to the left side of the heart, where it then enters the systemic circuit. • The systemic circuit consists of the chambers on the left side of the heart (left atrium and ventricle), along with all the other named blood vessels. § carries blood to all the peripheral organs and tissues of the body
Pulmonary and Systemic Circuits • Oxygenated blood from the left side of the heart is pumped into the aorta § the largest systemic artery in the body § then into smaller systemic arteries. • Gas exchange in tissues occurs from capillaries. • Systemic veins then carry deoxygenated blood (high in carbon dioxide) and waste products. • Most veins merge and drain into the superior and inferior venae cavae § drain blood into the right atrium. • There, the blood enters the pulmonary circuit, and the cycle repeats.
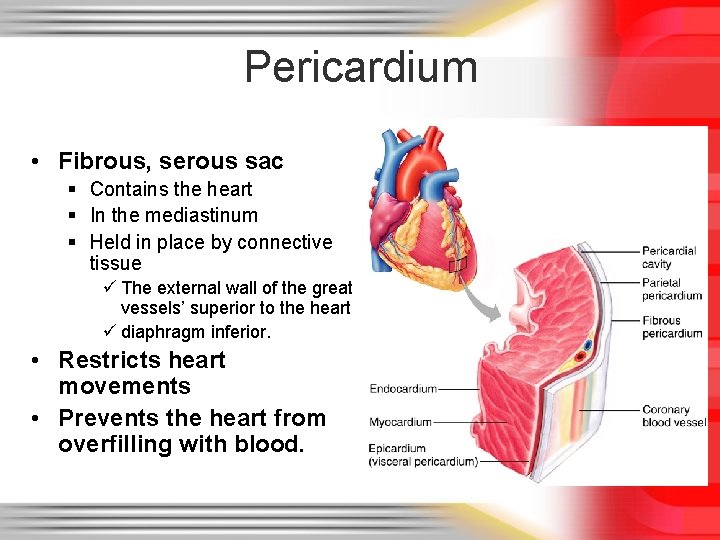
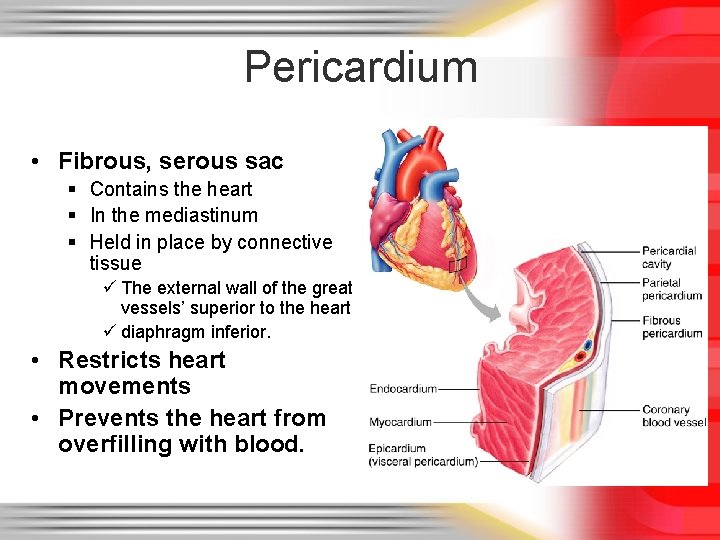
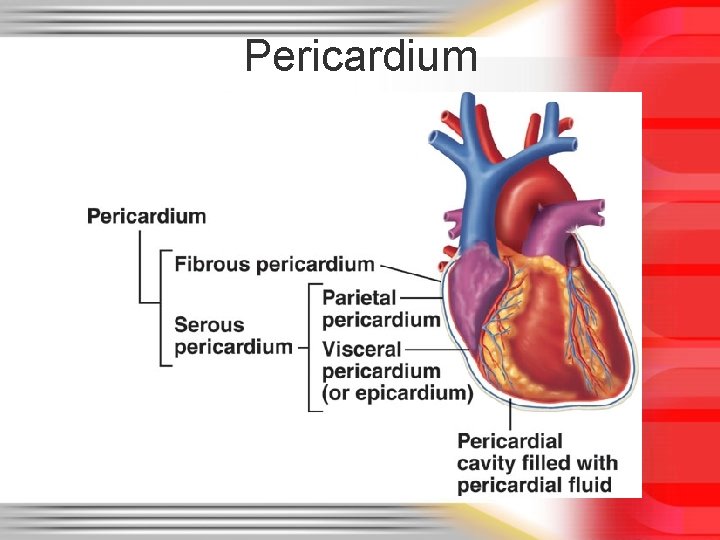
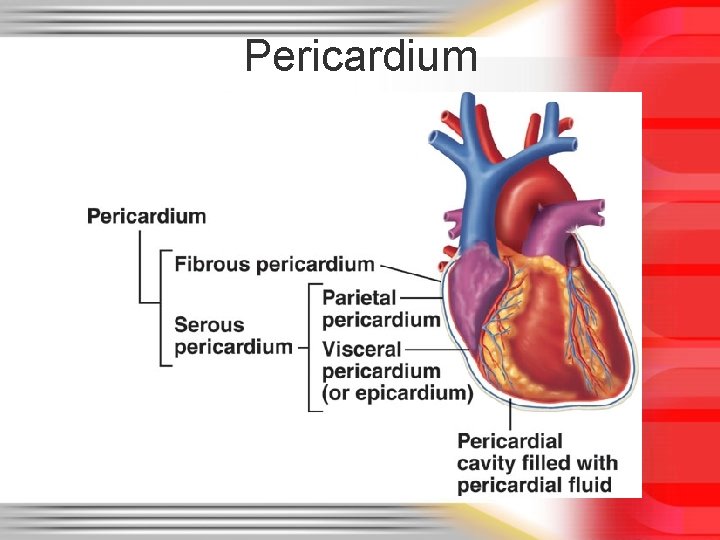
Pericardium • Fibrous, serous sac § Contains the heart § In the mediastinum § Held in place by connective tissue ü The external wall of the great vessels’ superior to the heart ü diaphragm inferior. • Restricts heart movements • Prevents the heart from overfilling with blood.
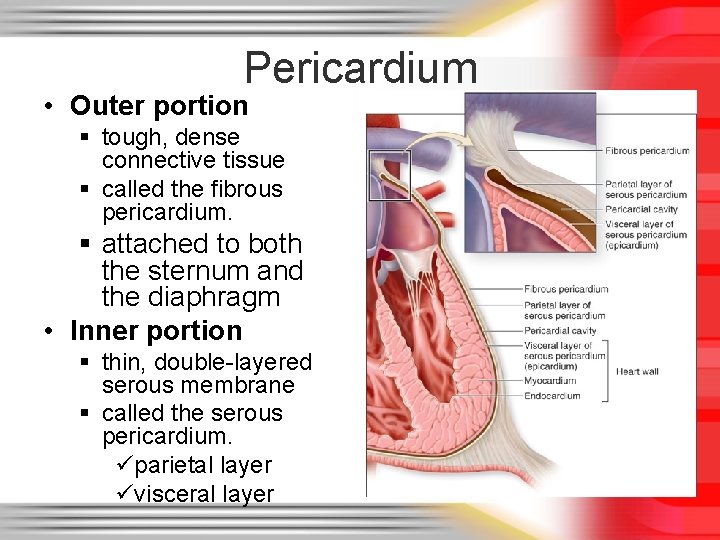
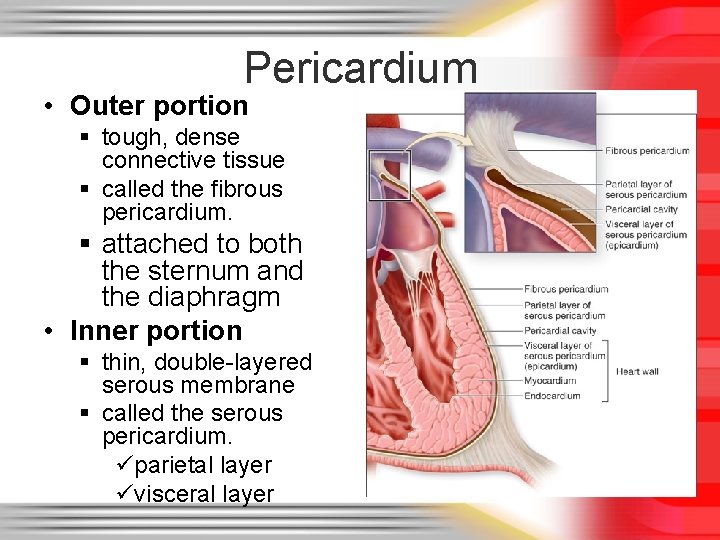
Pericardium • Outer portion § tough, dense connective tissue § called the fibrous pericardium. § attached to both the sternum and the diaphragm • Inner portion § thin, double-layered serous membrane § called the serous pericardium. üparietal layer üvisceral layer
Pericardium
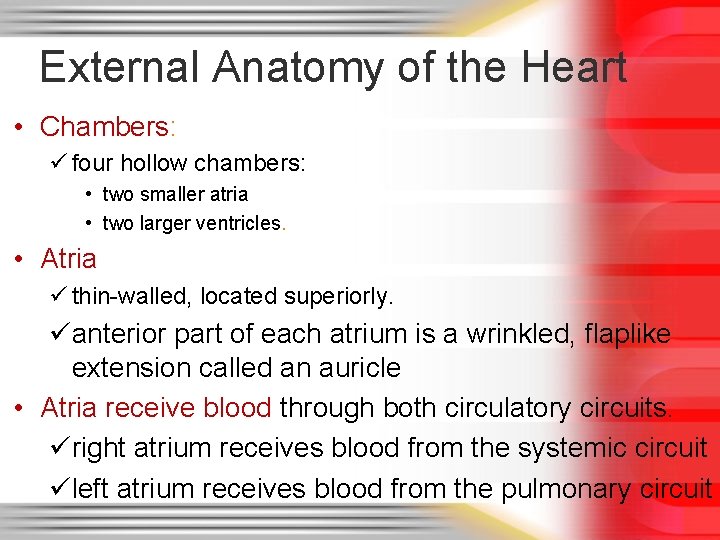
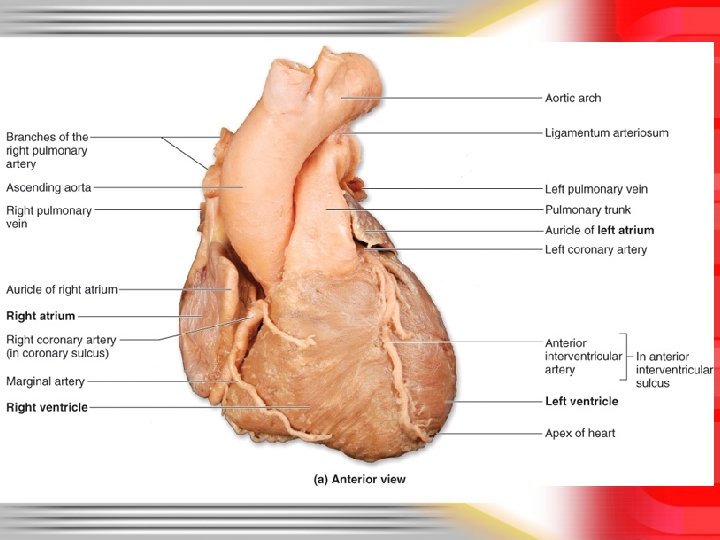
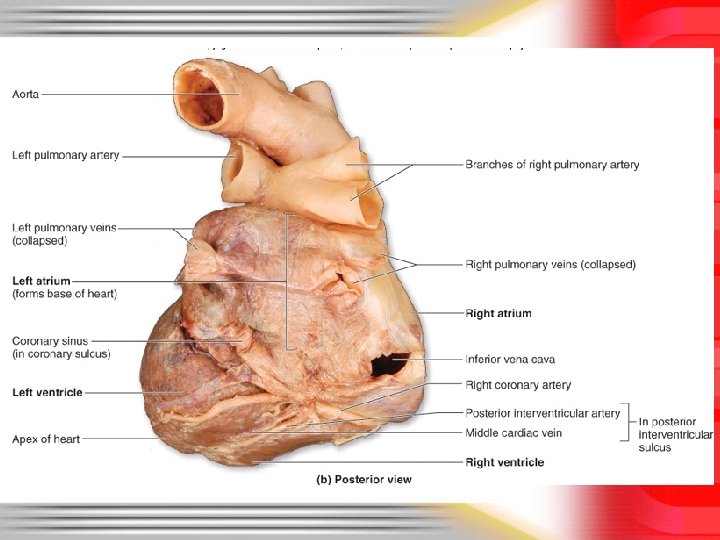
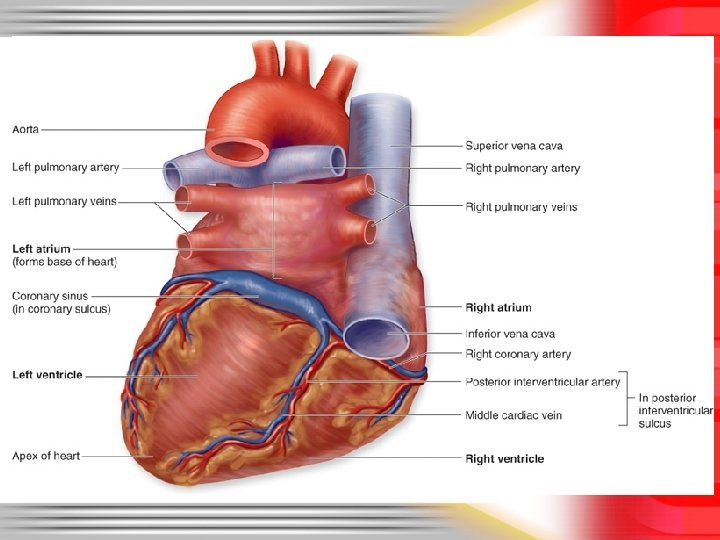
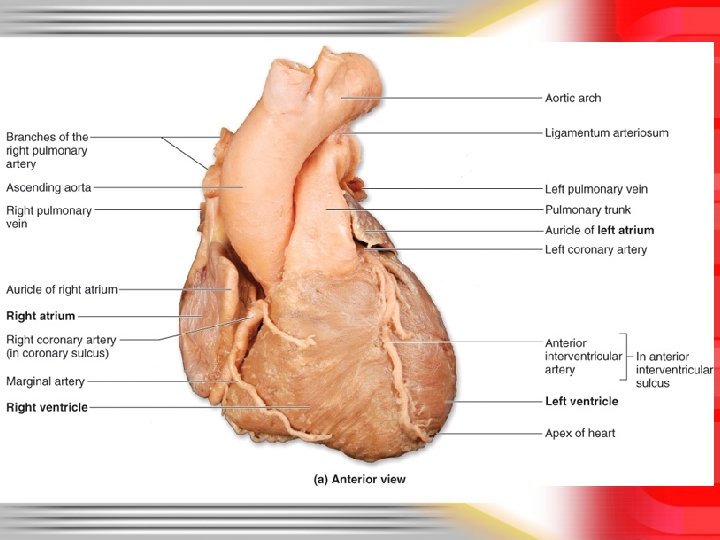
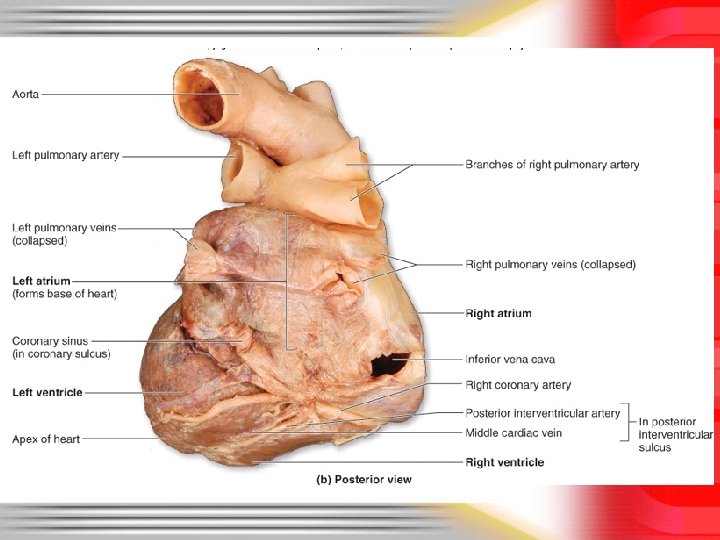
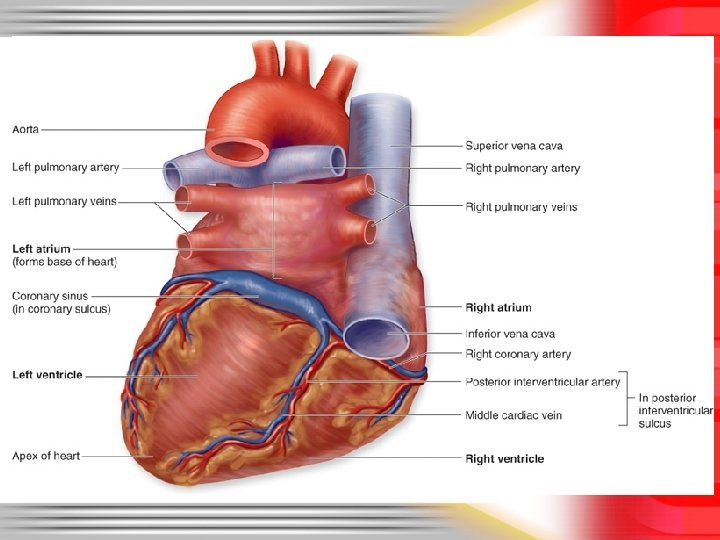
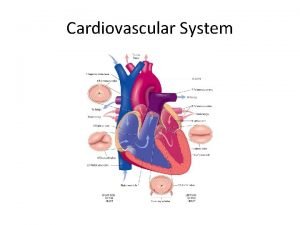
External Anatomy of the Heart • Chambers: ü four hollow chambers: • two smaller atria • two larger ventricles. • Atria ü thin-walled, located superiorly. üanterior part of each atrium is a wrinkled, flaplike extension called an auricle • Atria receive blood through both circulatory circuits. üright atrium receives blood from the systemic circuit üleft atrium receives blood from the pulmonary circuit
External Anatomy of the Heart • Blood that enters an atrium is passed to the ventricle on the same side of the heart. • Ventricles § the inferior chambers. § Two large arteries, the pulmonary trunk and the aorta exit the heart at the basal surface. • The pulmonary trunk carries blood from the right ventricle into the pulmonary circuit. • The aorta conducts blood from the left ventricle into the systemic circuit
External Anatomy of the Heart • Atria are separated from the ventricles externally by coronary sulcus (or atrioventricular sulcus) üextends around the circumference of the heart. • On both the anterior and posterior surfaces of the heart, the anterior interventricular sulcus and the posterior interventricular sulcus are located between the left and right ventricles. • These sulci extend inferiorly from the coronary sulcus toward the heart apex.

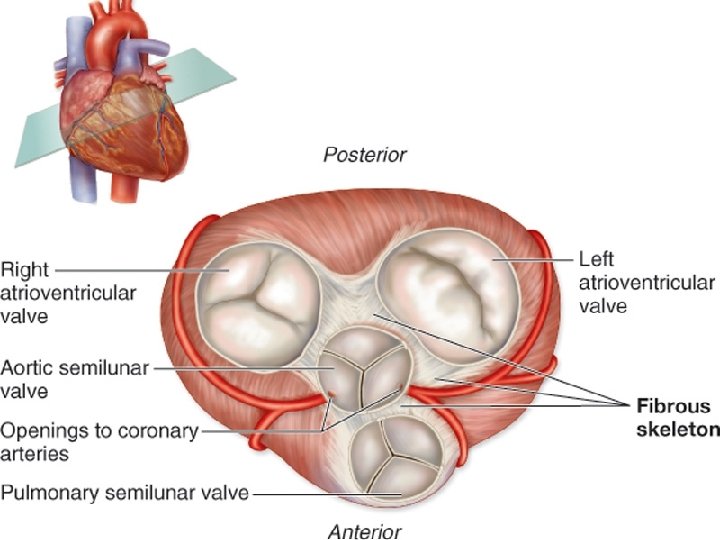
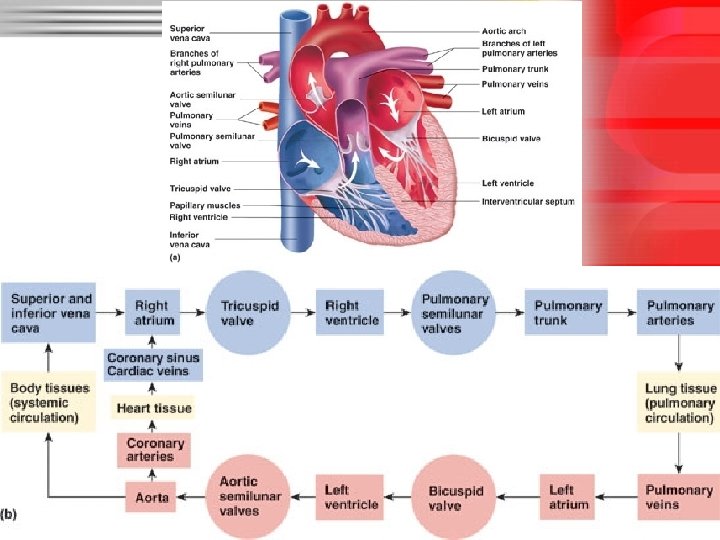
Internal Anatomy of the Heart • There are four heart chambers: – – right atrium right ventricle left atrium left ventricle • Each plays a role in the continuous process of blood circulation. • Valves permit the passage of blood in one direction and prevent its backflow.

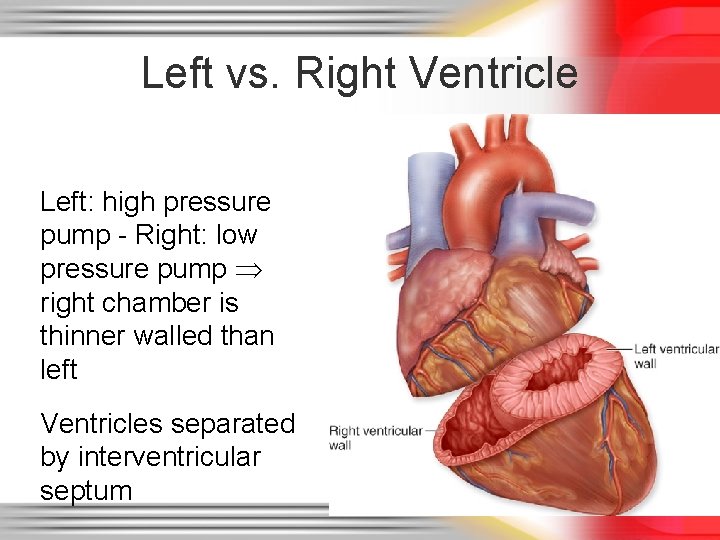
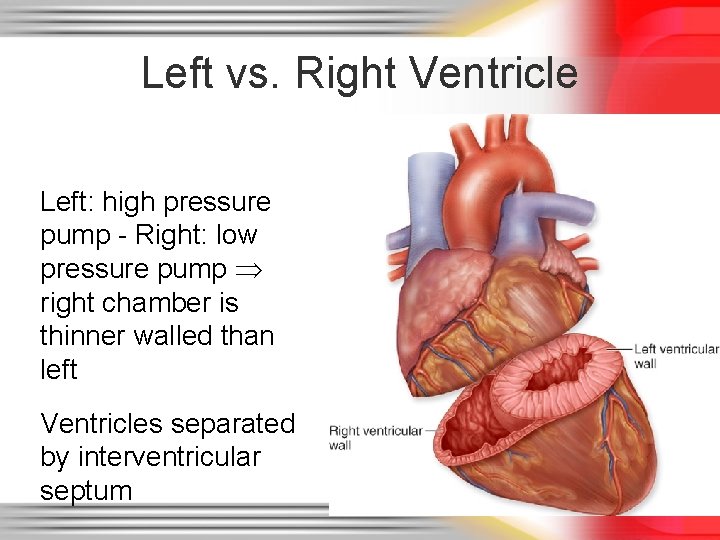
Left vs. Right Ventricle Left: high pressure pump - Right: low pressure pump right chamber is thinner walled than left Ventricles separated by interventricular septum
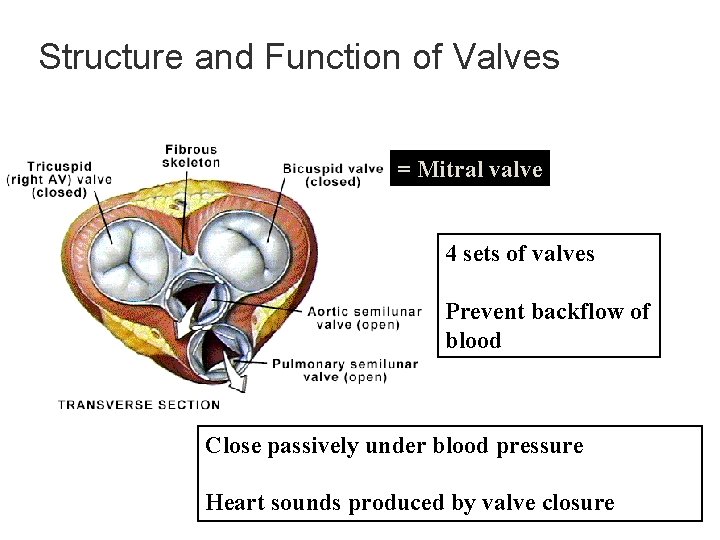
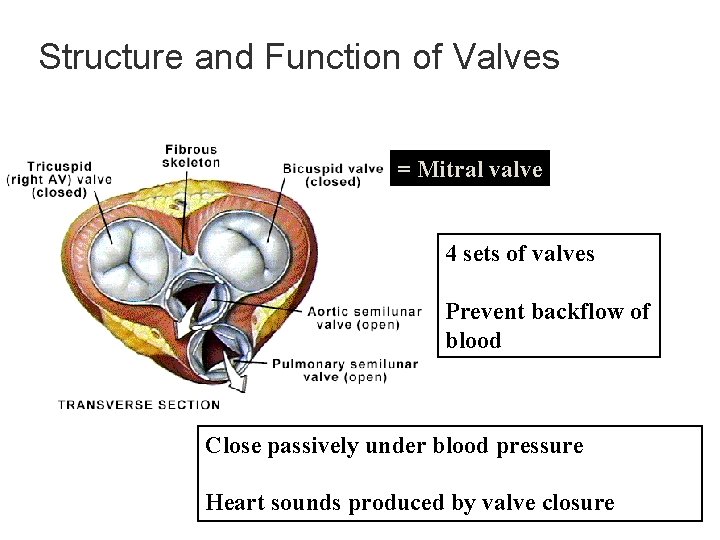
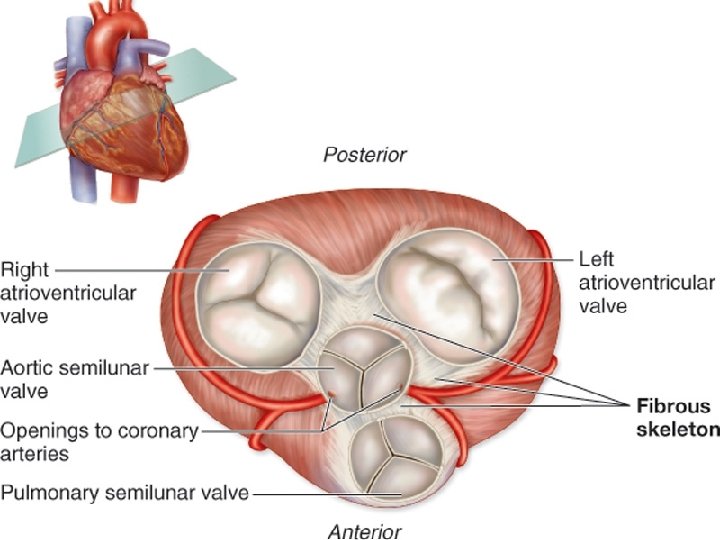
Structure and Function of Valves = Mitral valve 4 sets of valves Prevent backflow of blood Close passively under blood pressure Heart sounds produced by valve closure
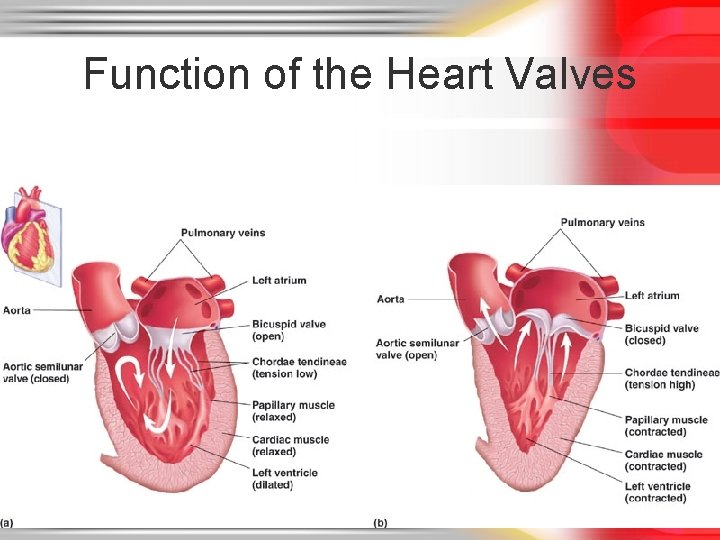
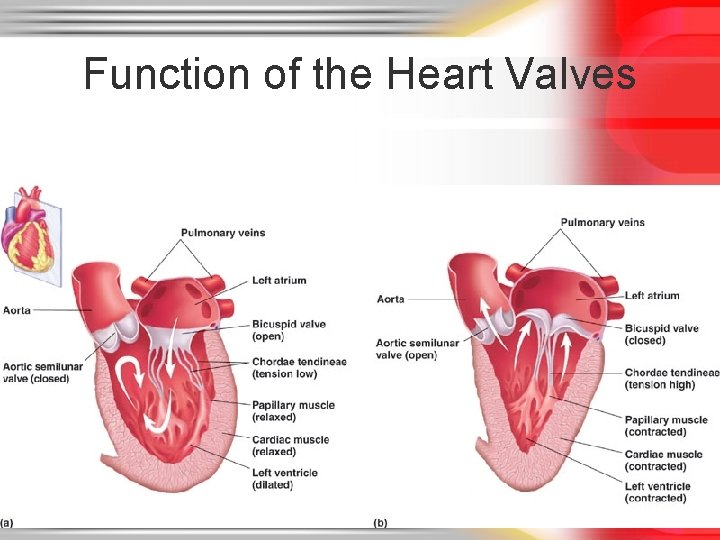
Function of the Heart Valves

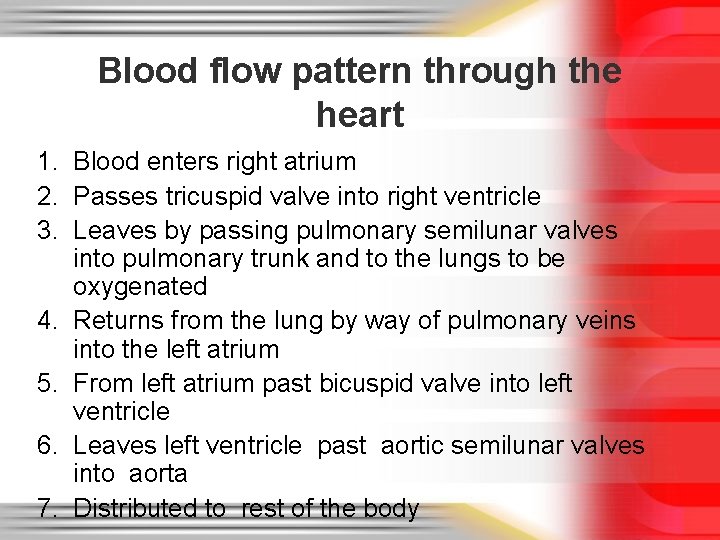
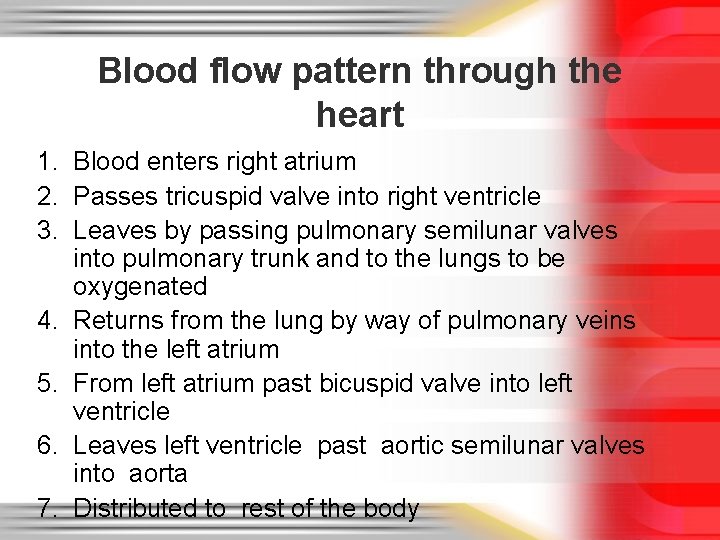
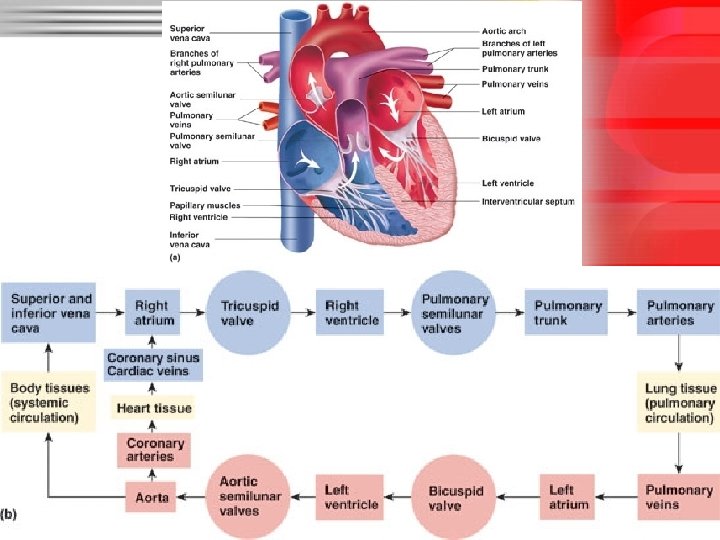
Blood flow pattern through the heart 1. Blood enters right atrium 2. Passes tricuspid valve into right ventricle 3. Leaves by passing pulmonary semilunar valves into pulmonary trunk and to the lungs to be oxygenated 4. Returns from the lung by way of pulmonary veins into the left atrium 5. From left atrium past bicuspid valve into left ventricle 6. Leaves left ventricle past aortic semilunar valves into aorta 7. Distributed to rest of the body
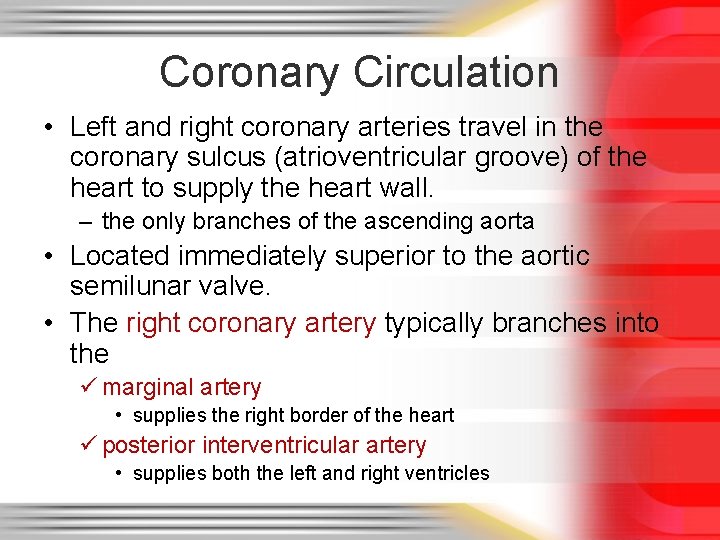
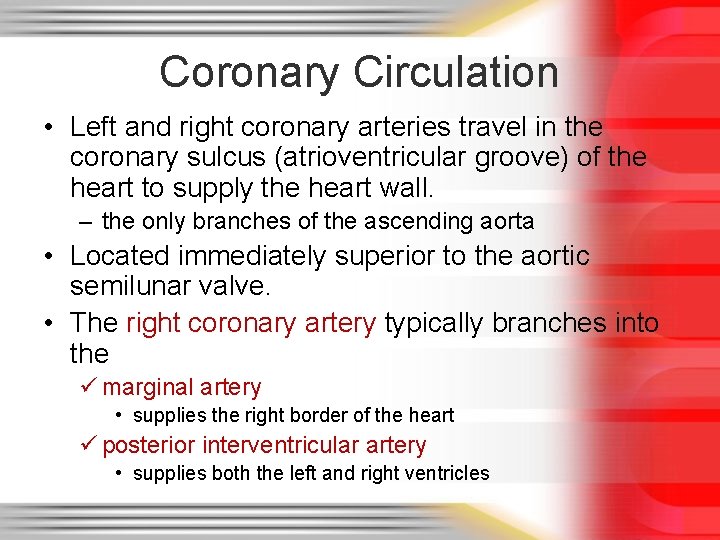
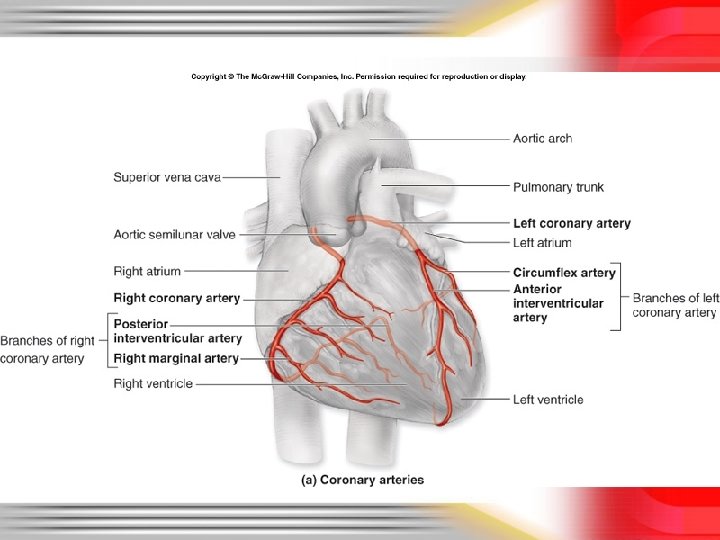
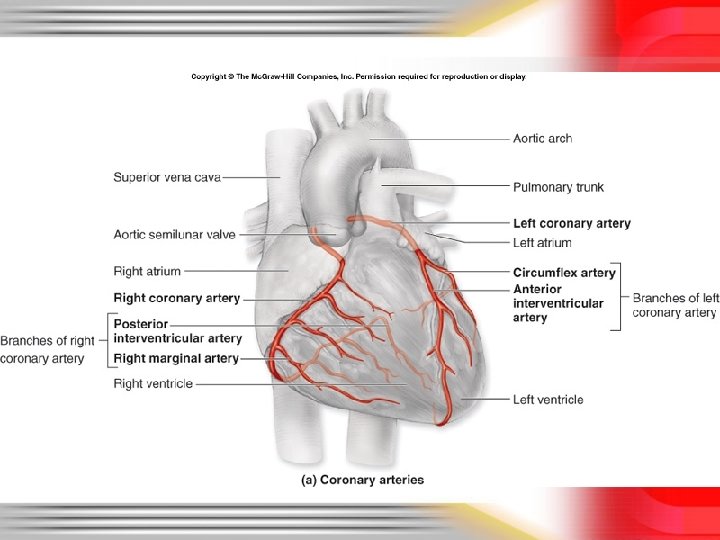
Coronary Circulation • Left and right coronary arteries travel in the coronary sulcus (atrioventricular groove) of the heart to supply the heart wall. – the only branches of the ascending aorta • Located immediately superior to the aortic semilunar valve. • The right coronary artery typically branches into the ü marginal artery • supplies the right border of the heart ü posterior interventricular artery • supplies both the left and right ventricles
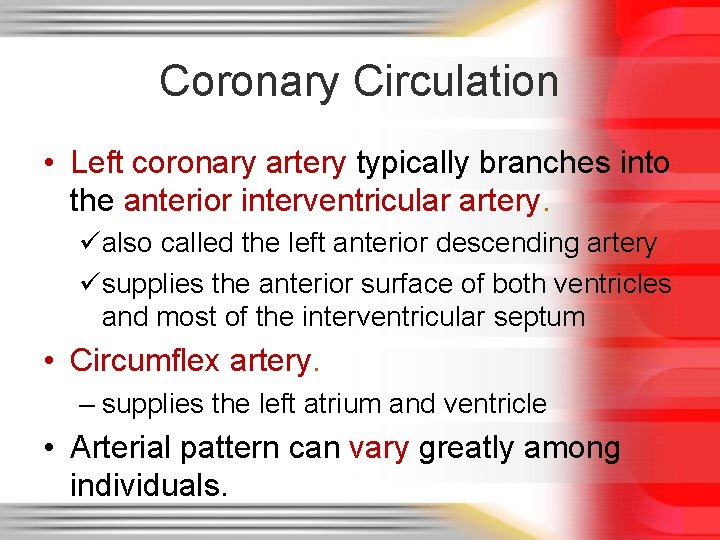
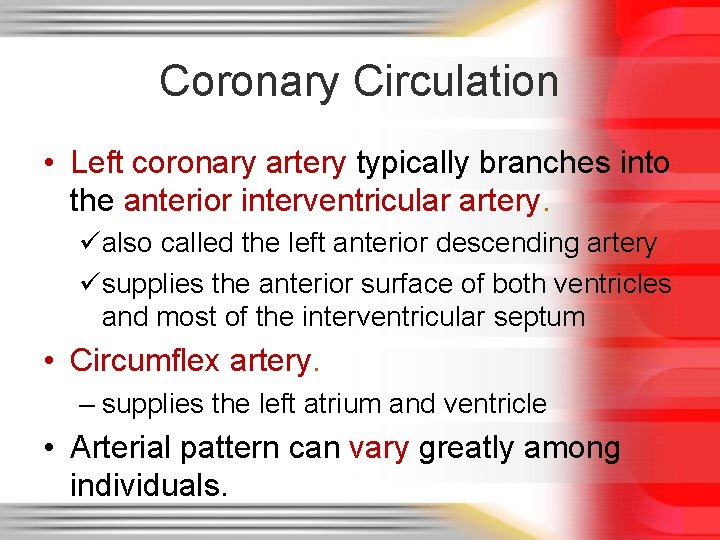
Coronary Circulation • Left coronary artery typically branches into the anterior interventricular artery. üalso called the left anterior descending artery üsupplies the anterior surface of both ventricles and most of the interventricular septum • Circumflex artery. – supplies the left atrium and ventricle • Arterial pattern can vary greatly among individuals.

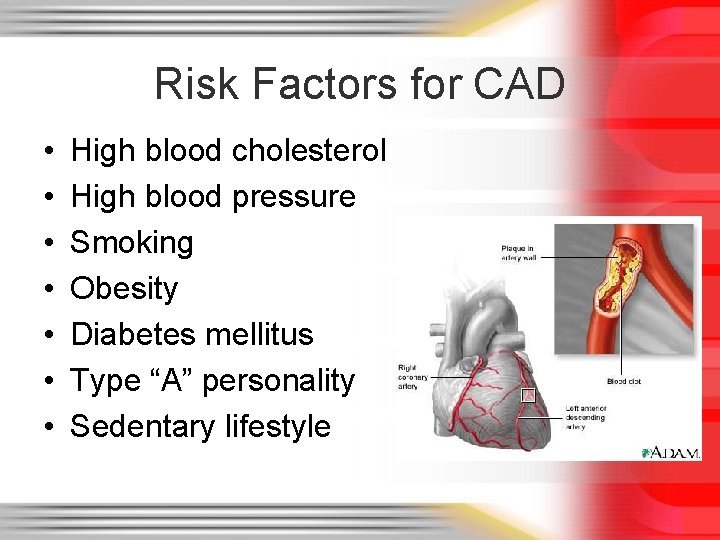
Risk Factors for CAD • • High blood cholesterol High blood pressure Smoking Obesity Diabetes mellitus Type “A” personality Sedentary lifestyle
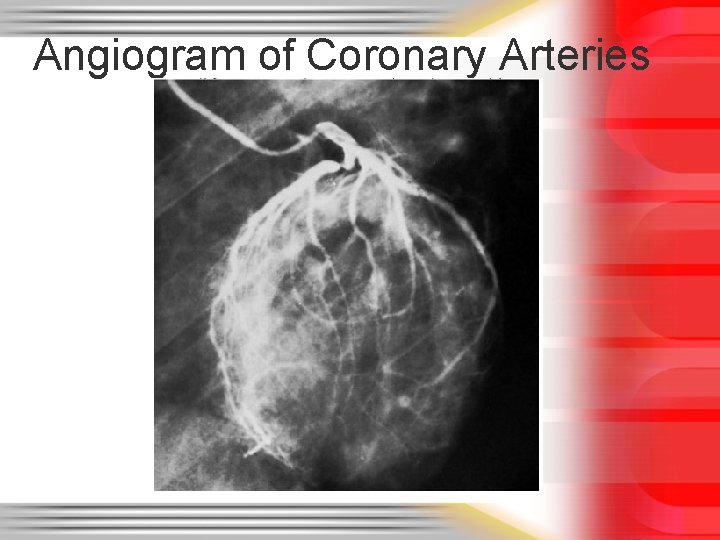
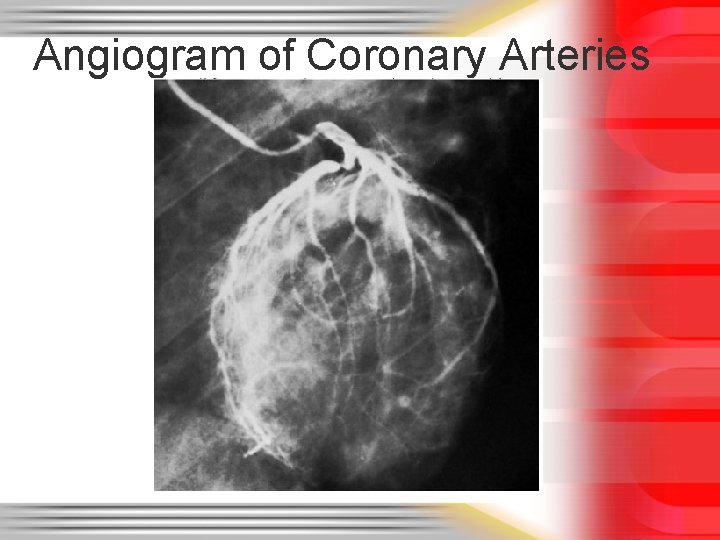
Angiogram of Coronary Arteries
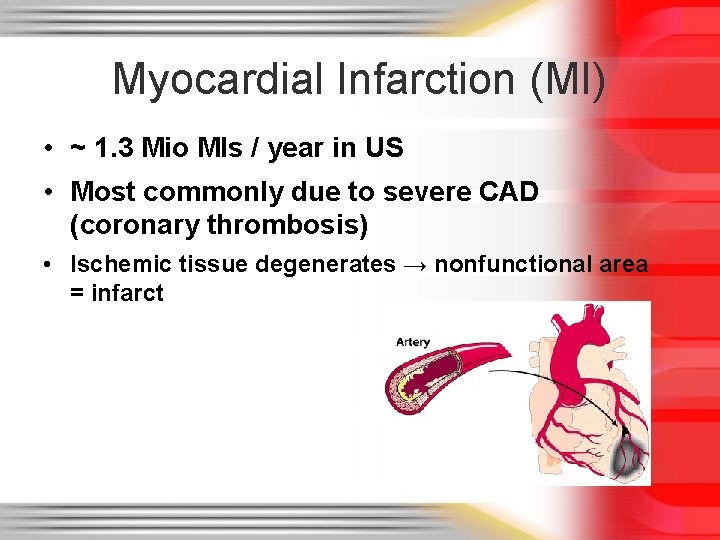
Myocardial Infarction (MI) • ~ 1. 3 Mio MIs / year in US • Most commonly due to severe CAD (coronary thrombosis) • Ischemic tissue degenerates → nonfunctional area = infarct
THE END
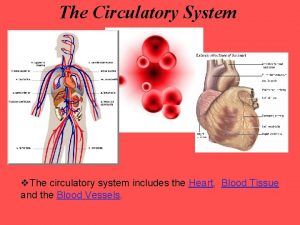
 Chapter 19 the circulatory or cardiovascular system
Chapter 19 the circulatory or cardiovascular system What makes up the circulatory system
What makes up the circulatory system Pithed rat meaning
Pithed rat meaning Totally tubular dude
Totally tubular dude Circulatory system crash course
Circulatory system crash course Chapter 5 the cardiovascular system labeling exercises
Chapter 5 the cardiovascular system labeling exercises Figure 11-7 veins labeled
Figure 11-7 veins labeled Figure 11-12 is a diagram of a capillary bed
Figure 11-12 is a diagram of a capillary bed Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Tissues in circulatory system
Tissues in circulatory system Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Introduction of heart
Introduction of heart Ptca
Ptca Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Chapter 13 cardiovascular system
Chapter 13 cardiovascular system Chapter 11 the cardiovascular system figure 11-2
Chapter 11 the cardiovascular system figure 11-2 The cardiovascular system includes the
The cardiovascular system includes the Blood vesel
Blood vesel True capillaries definition
True capillaries definition Heart is part of what system
Heart is part of what system![Const int size=18; string *tb12 = new string[size]; Const int size=18; string *tb12 = new string[size];](data:image/svg+xml,%3Csvg%20xmlns=%22http://www.w3.org/2000/svg%22%20viewBox=%220%200%20200%20200%22%3E%3C/svg%3E) Const int size=18; string *tb12 = new string[size];
Const int size=18; string *tb12 = new string[size]; Different methods
Different methods Cardiac dullness
Cardiac dullness Sheep heart labeled
Sheep heart labeled Hrt to hrt merrylands
Hrt to hrt merrylands Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Soplo protosistolico
Soplo protosistolico Rias hipertension arterial
Rias hipertension arterial Fresenius ncp
Fresenius ncp Cardiovascular drift
Cardiovascular drift Chapter 46 the child with a cardiovascular alteration
Chapter 46 the child with a cardiovascular alteration The child with a cardiovascular disorder chapter 26
The child with a cardiovascular disorder chapter 26 Wolters kluwer
Wolters kluwer American board of cardiovascular medicine
American board of cardiovascular medicine Life
Life Neuronas sensoriales
Neuronas sensoriales Sistema digestivo
Sistema digestivo Cardiovascular research institute basel
Cardiovascular research institute basel What is cardiovascular endurance in health related fitness
What is cardiovascular endurance in health related fitness






![Const int size=18; string *tb12 = new string[size]; Const int size=18; string *tb12 = new string[size];](https://slidetodoc.com/wp-content/uploads/2020/11/1588947_40cf3415d0afabae1c436a49b39f4ad0-300x225.jpg)