capillary Hemangioma Its differential Diagnosis F Fatemi MD






- Slides: 30
capillary Hemangioma & Its differential Diagnosis F. Fatemi, MD Isfahan University Of Medical Sciences
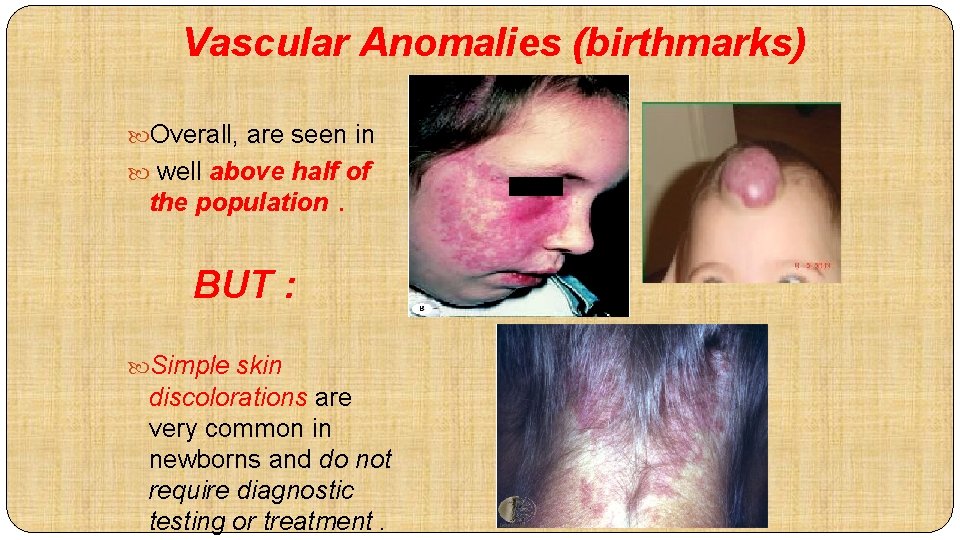
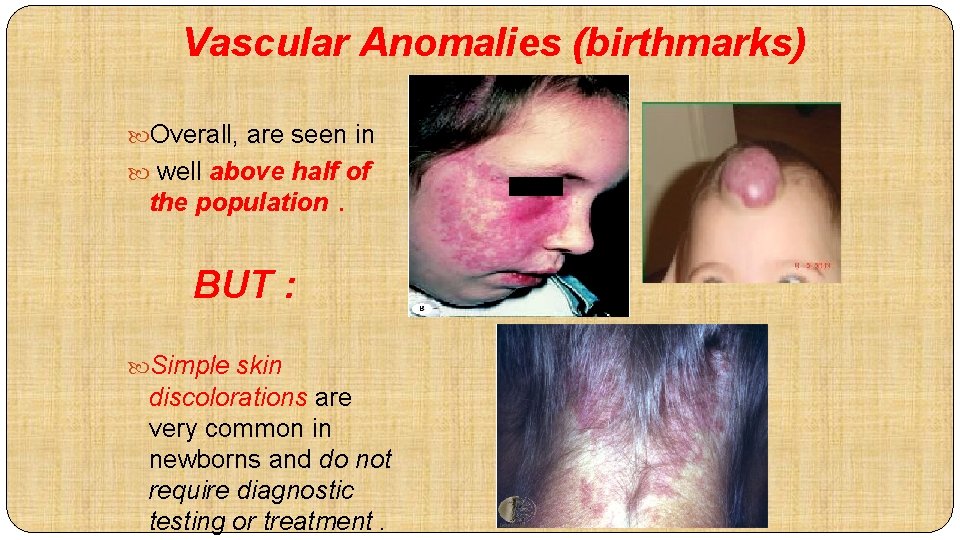
Vascular Anomalies (birthmarks) Overall, are seen in well above half of the population . BUT : Simple skin discolorations are very common in newborns and do not require diagnostic testing or treatment.

VBF Founded in 1994 by Linda Rozell- Shannon after her daughter Christine was diagnosed with a hemangioma and she found that there was no foundation, no website, no book and very few resources Linda searched for a surgeon to remove Christine’s hemangioma and found Dr. Waner. Together they formed VBF and wrote the first book on the subject “Birthmarks: A Guide to Hemangiomas and Vascular Malformations”

2011 – New Program Brings Hope �VBF establishes the ITEAM. �An international team of surgeons and treatment specialists who volunteer to travel to Russia, India, Asia and Africa to perform free surgeries and to train physicians in those countries to perform future treatments. �One i. TEAM trip will conducted every 9 month (based on funding)
2011 and Beyond �Realizing the Vision……. �Bringing the i. TEAM to underserved countries �Babies With Birthmarks Guidelines established by major medical academies �Conference/Gala in NYC �Increased Awareness & Accessibility to Options �Discover Cause of Birthmarks through Research �Legislation passed to require insurance companies to cover treatment of all children with birthmarks. No Child Will Remain Untreated!
Capillary Hemangioma ØInfantile hemangioma ØCong hemangioma
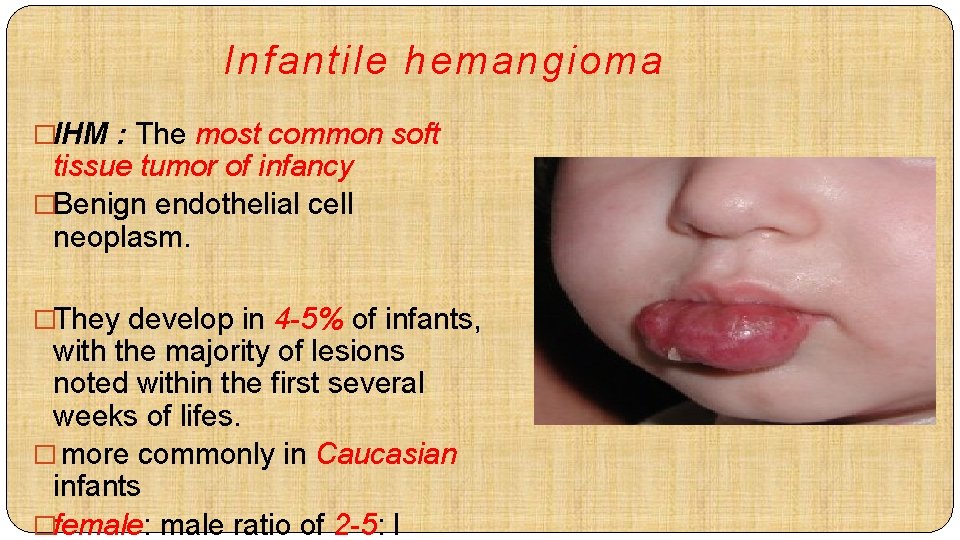
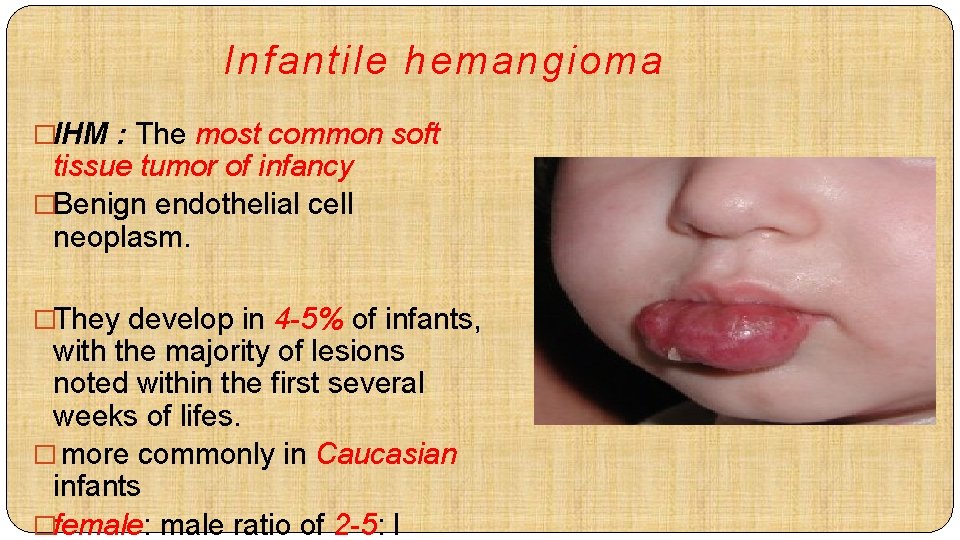
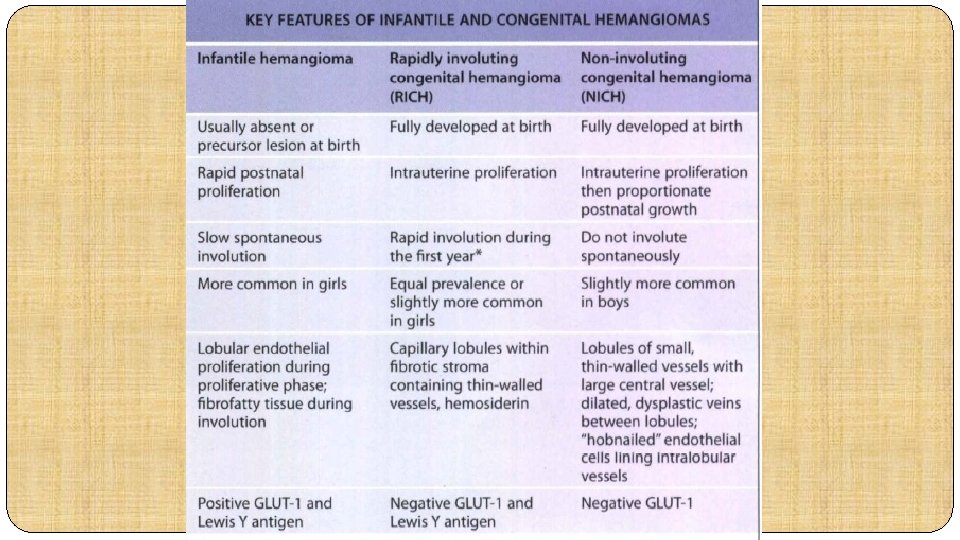
Infantile hemangioma �IHM : The most common soft tissue tumor of infancy �Benign endothelial cell neoplasm. �They develop in 4 -5% of infants, with the majority of lesions noted within the first several weeks of lifes. � more commonly in Caucasian infants �female: male ratio of 2 -5: I
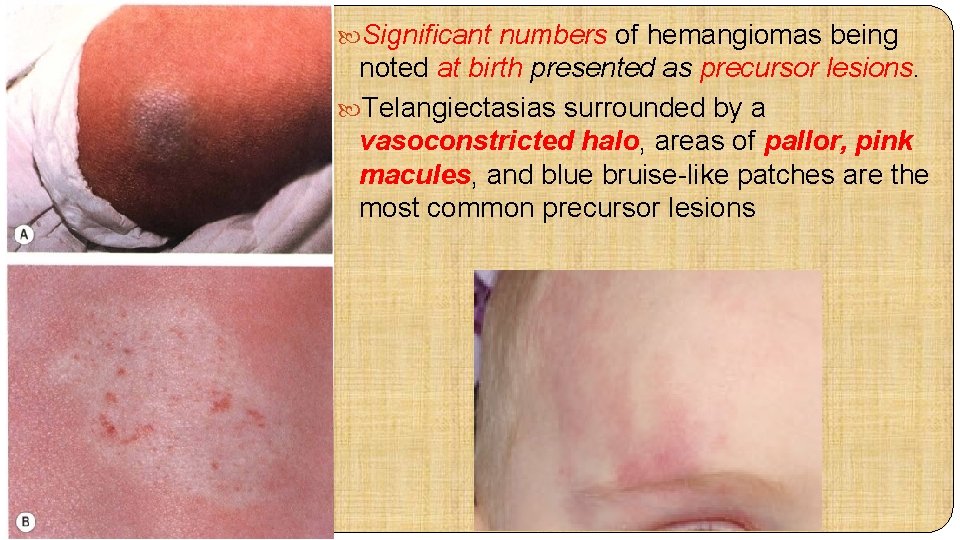
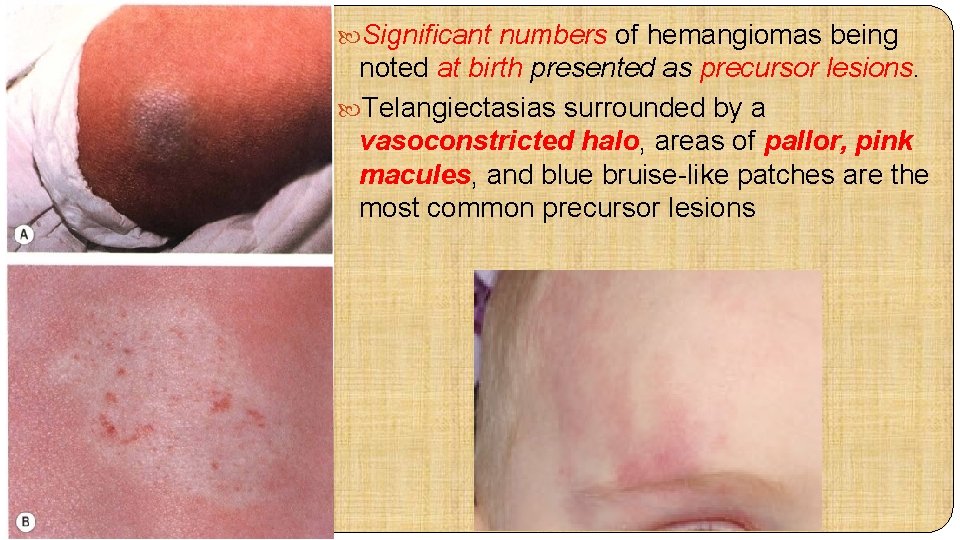
Significant numbers of hemangiomas being noted at birth presented as precursor lesions. Telangiectasias surrounded by a vasoconstricted halo, areas of pallor, pink macules, and blue bruise-like patches are the most common precursor lesions
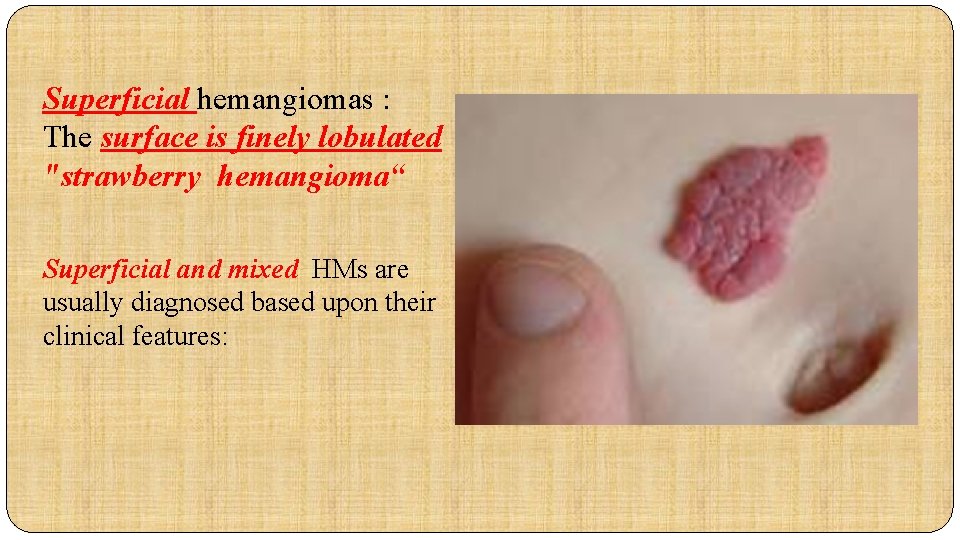
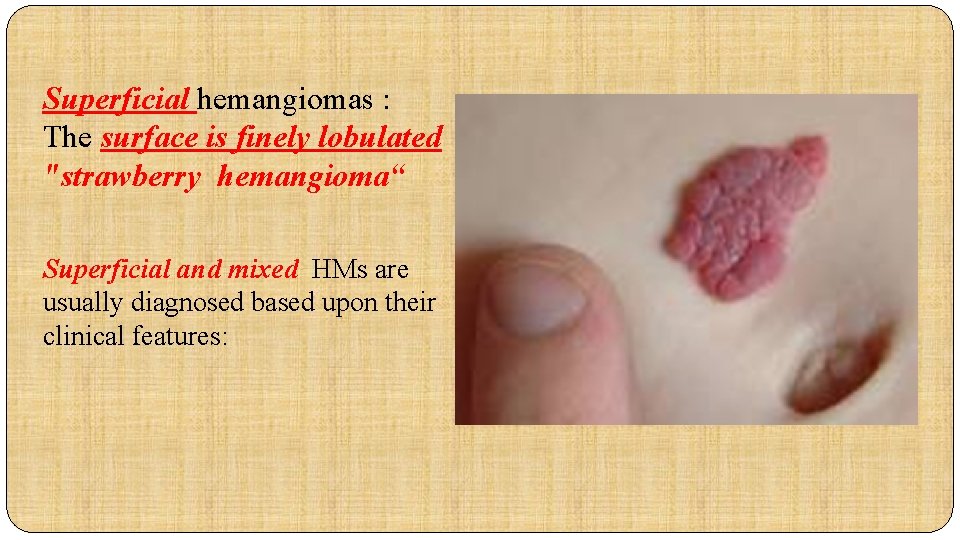
Superficial hemangiomas : The surface is finely lobulated "strawberry hemangioma“ Superficial and mixed HMs are usually diagnosed based upon their clinical features:
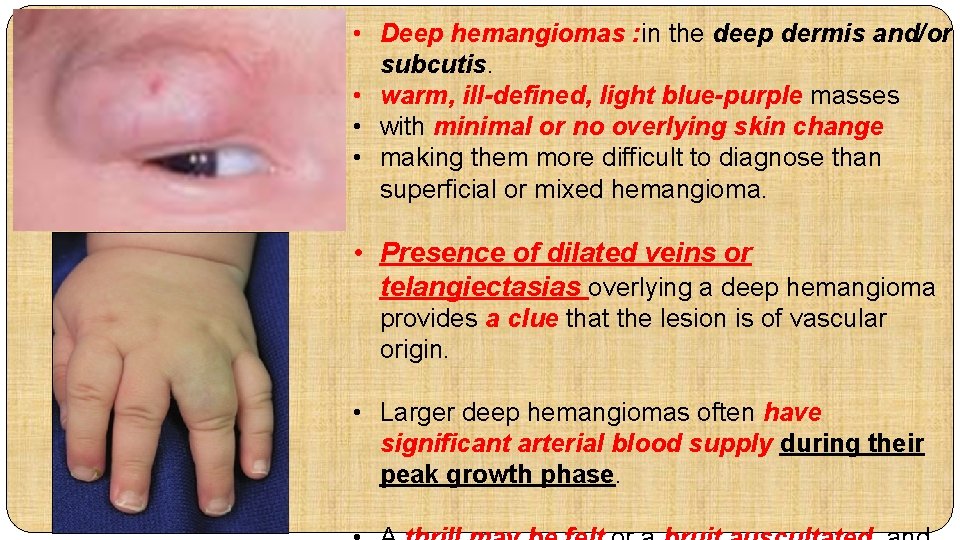
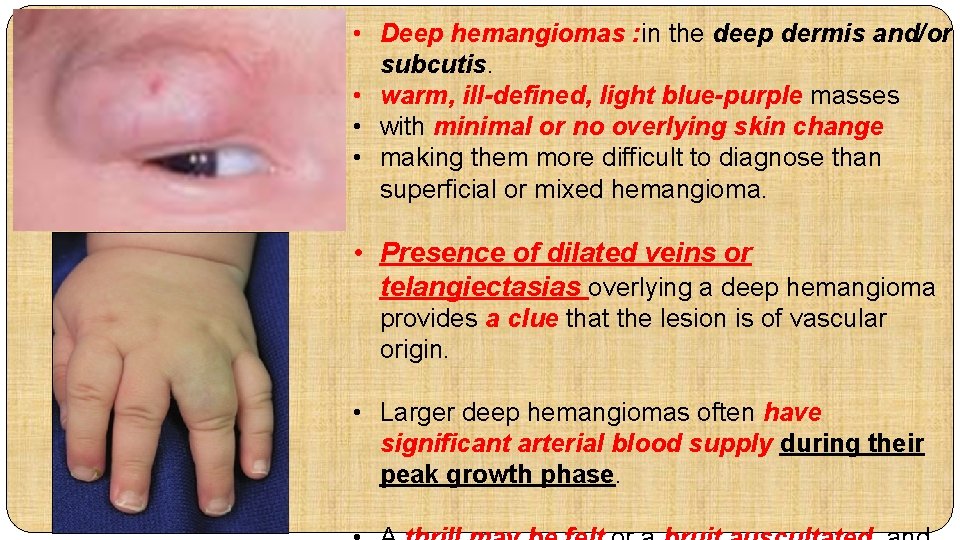
• Deep hemangiomas : in the deep dermis and/or subcutis. • warm, ill-defined, light blue-purple masses • with minimal or no overlying skin change • making them more difficult to diagnose than superficial or mixed hemangioma. • Presence of dilated veins or telangiectasias overlying a deep hemangioma provides a clue that the lesion is of vascular origin. • Larger deep hemangiomas often have significant arterial blood supply during their peak growth phase.
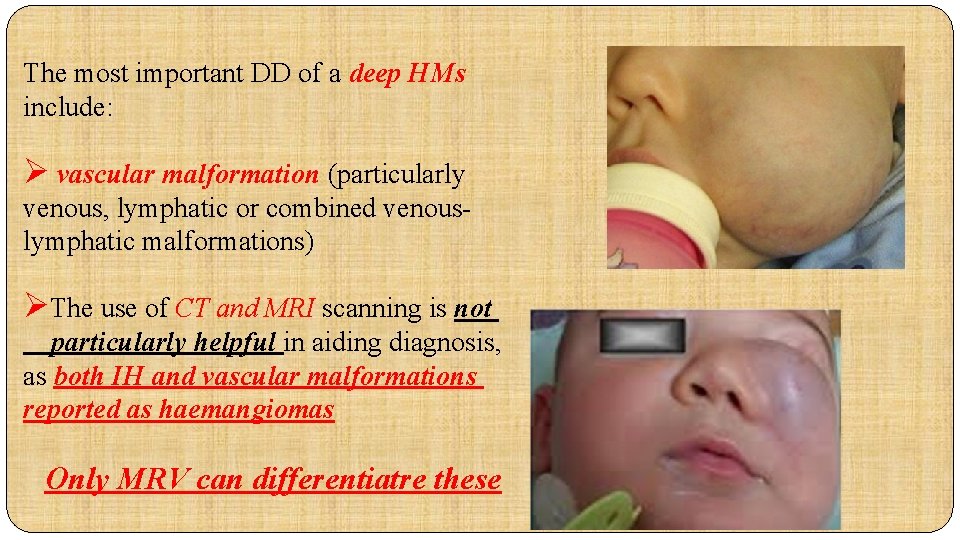
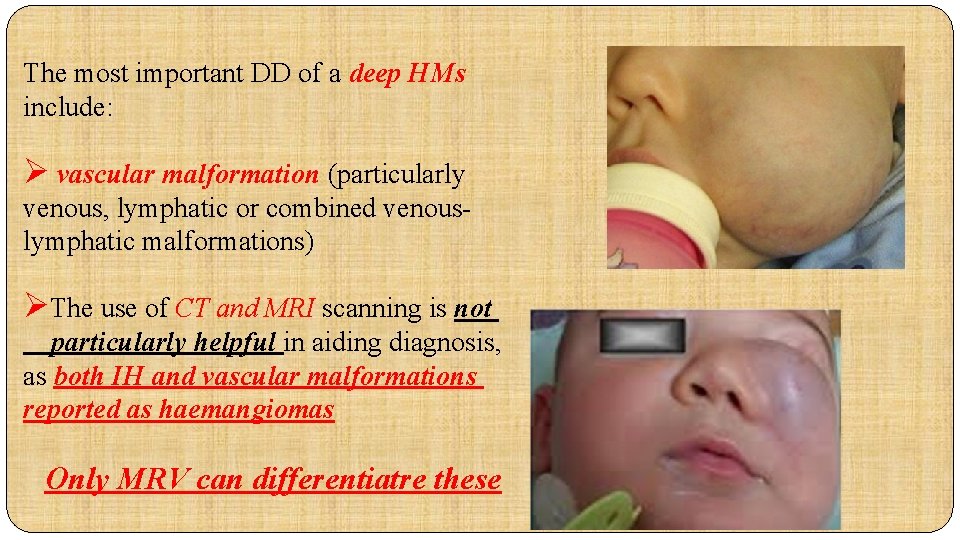
The most important DD of a deep HMs include: Ø vascular malformation (particularly venous, lymphatic or combined venouslymphatic malformations) ØThe use of CT and MRI scanning is not particularly helpful in aiding diagnosis, as both IH and vascular malformations reported as haemangiomas Only MRV can differentiatre these
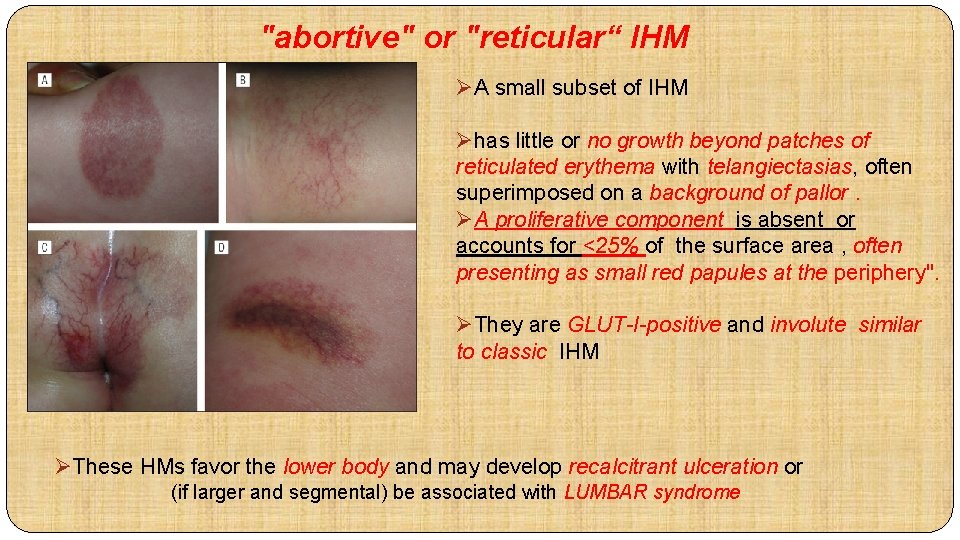
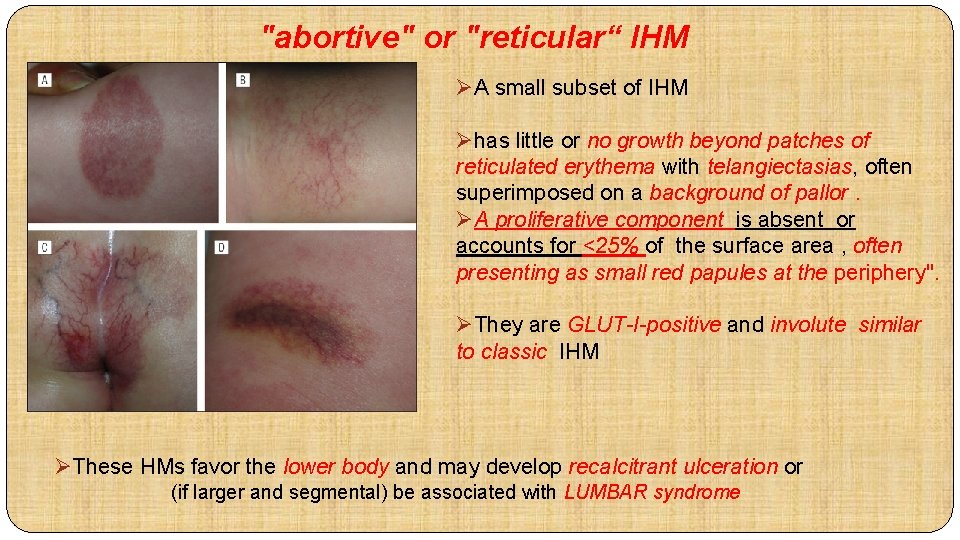
"abortive" or "reticular“ IHM ØA small subset of IHM Øhas little or no growth beyond patches of reticulated erythema with telangiectasias, often superimposed on a background of pallor. ØA proliferative component is absent or accounts for <25% of the surface area , often presenting as small red papules at the periphery". ØThey are GLUT-I-positive and involute similar to classic IHM ØThese HMs favor the lower body and may develop recalcitrant ulceration or (if larger and segmental) be associated with LUMBAR syndrome
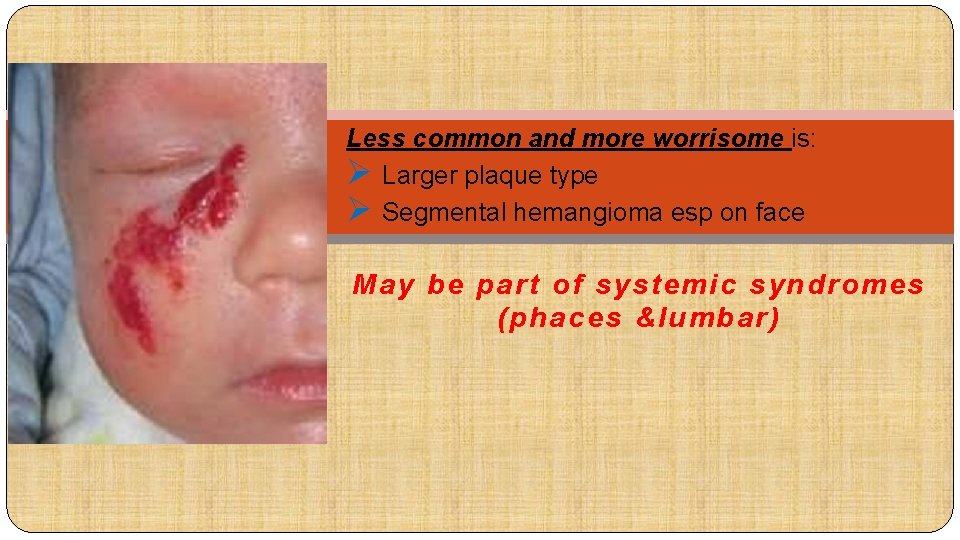
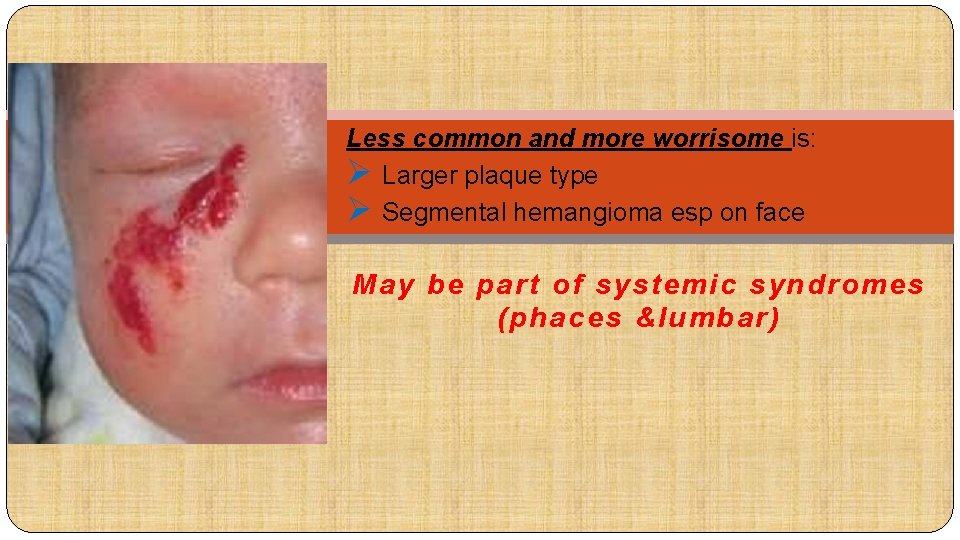
Less common and more worrisome is: Ø Larger plaque type Ø Segmental hemangioma esp on face May be part of systemic syndromes (phaces &lumbar)
congenital hemangioma -RICH -NICH
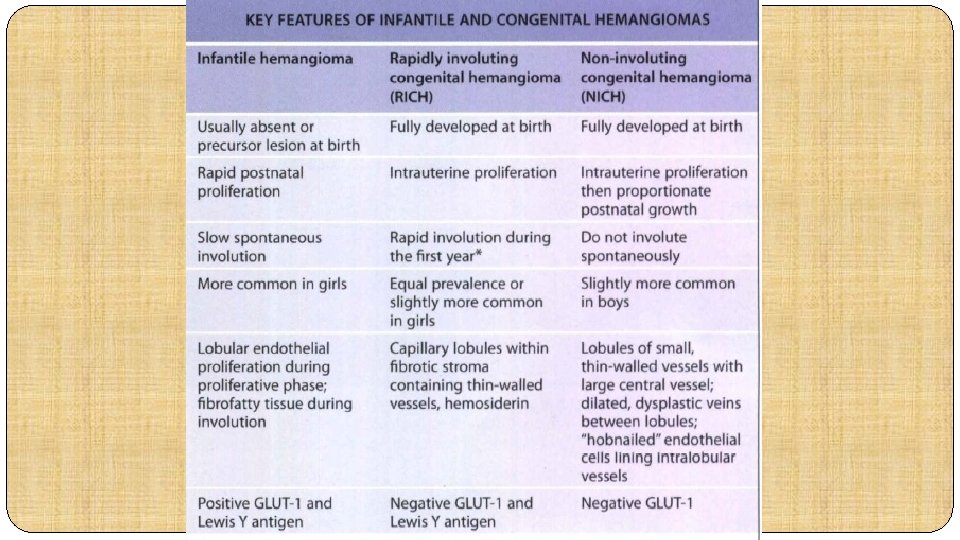
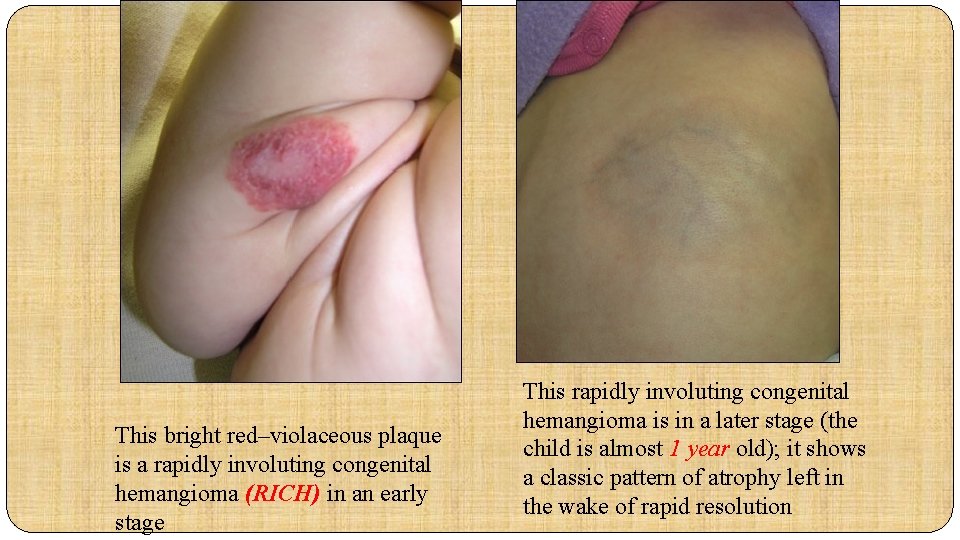
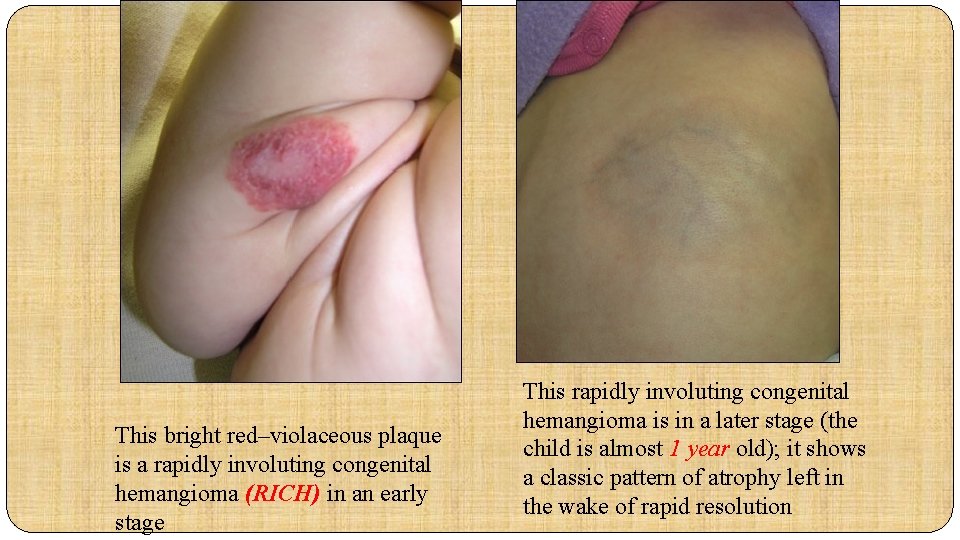
This bright red–violaceous plaque is a rapidly involuting congenital hemangioma (RICH) in an early stage This rapidly involuting congenital hemangioma is in a later stage (the child is almost 1 year old); it shows a classic pattern of atrophy left in the wake of rapid resolution

NICH lesions; ØThey consist of the classic telangiectatic patch with surrounding slight pallor. Ø unlike infantile HMs, grow proportionately with the child. ØThe lesions may worsen with maturity and do not involute spontaneously. ØThe diagnosis is often established retrospectively after the lesion is excised because involution fails to occur.
Differential Diagnosis of capillary hemangioma Most important : 1 -Kaposiformhemangioendothelioma 2 -Tuffted angioma

1 - Kaposiform hemangioendothelioma �Rare deeply seated , infiltrative vascular tumor �Involve the skin and subcutaneous as well as deep soft tissues, bone and even viscera �Locally aggressive �Expression of mixed blood vascular and lymphatic endothelial markers) � Glut 1 (-), CD 34+, LYVE 1+ �likely synonymous in pathogenesis with tufted angioma, with the latter ØDoes not spontaneously involute ØComplete surgical excision is recommended where feasible ØVAC : vincristine /actinomycin /cyclophosphamide , ….
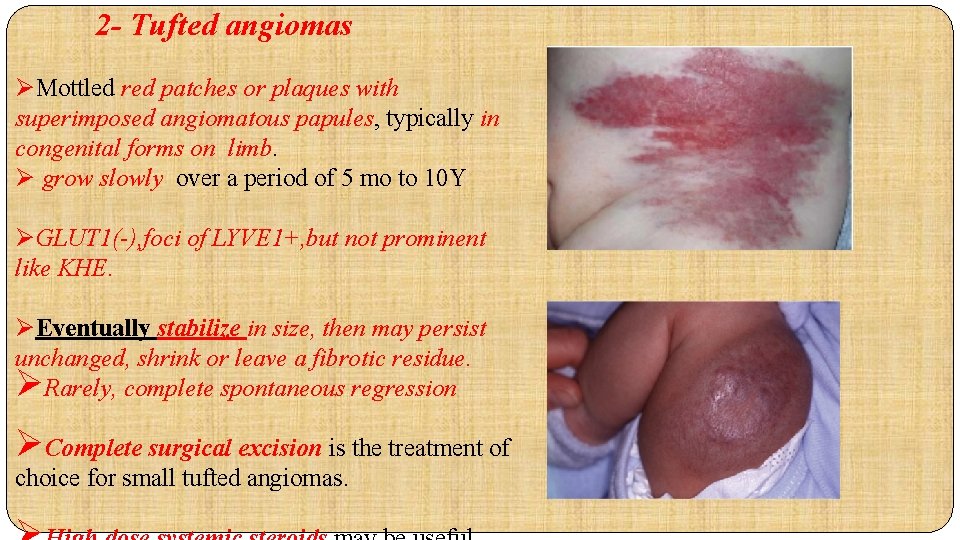
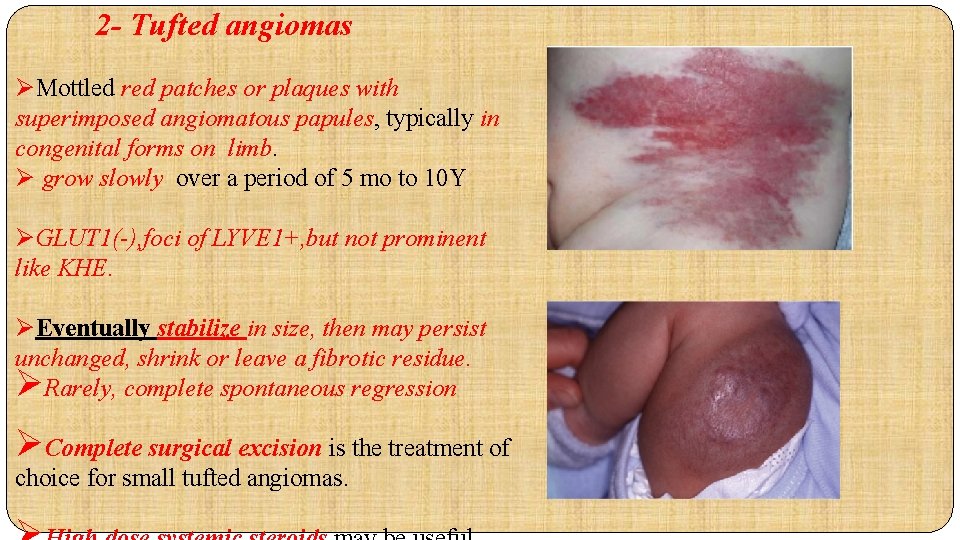
2 - Tufted angiomas ØMottled red patches or plaques with superimposed angiomatous papules, typically in congenital forms on limb. Ø grow slowly over a period of 5 mo to 10 Y ØGLUT 1(-), foci of LYVE 1+, but not prominent like KHE. ØEventually stabilize in size, then may persist unchanged, shrink or leave a fibrotic residue. ØRarely, complete spontaneous regression ØComplete surgical excision is the treatment of choice for small tufted angiomas.
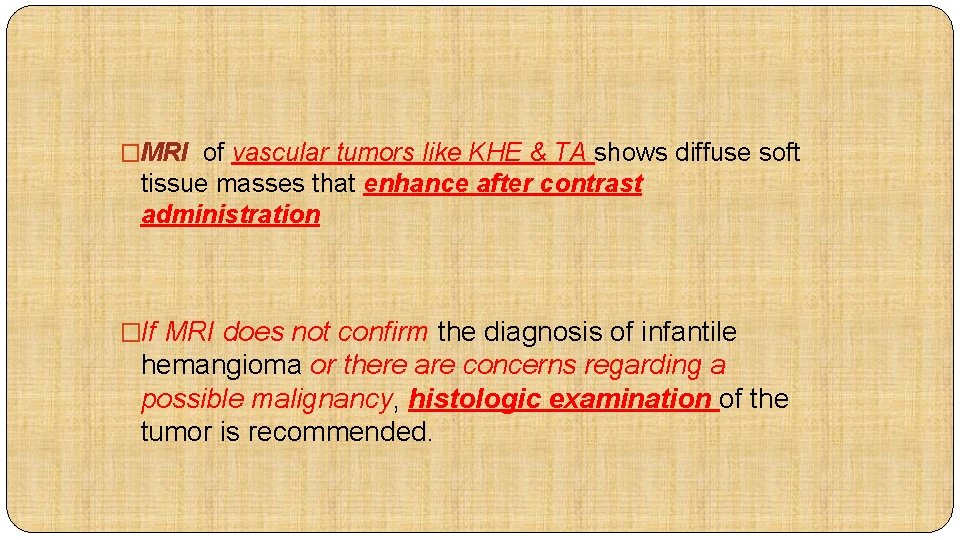
�MRI of vascular tumors like KHE & TA shows diffuse soft tissue masses that enhance after contrast administration �If MRI does not confirm the diagnosis of infantile hemangioma or there are concerns regarding a possible malignancy, histologic examination of the tumor is recommended.
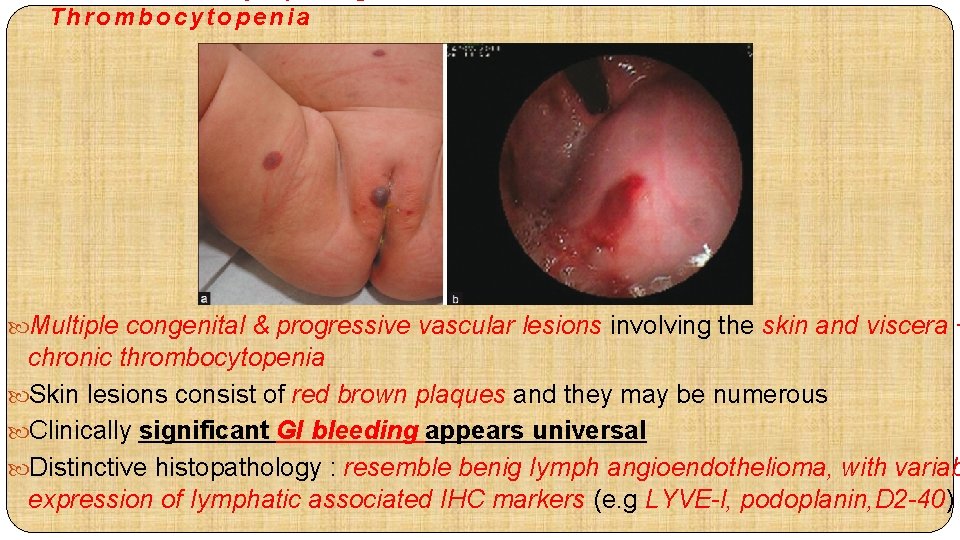
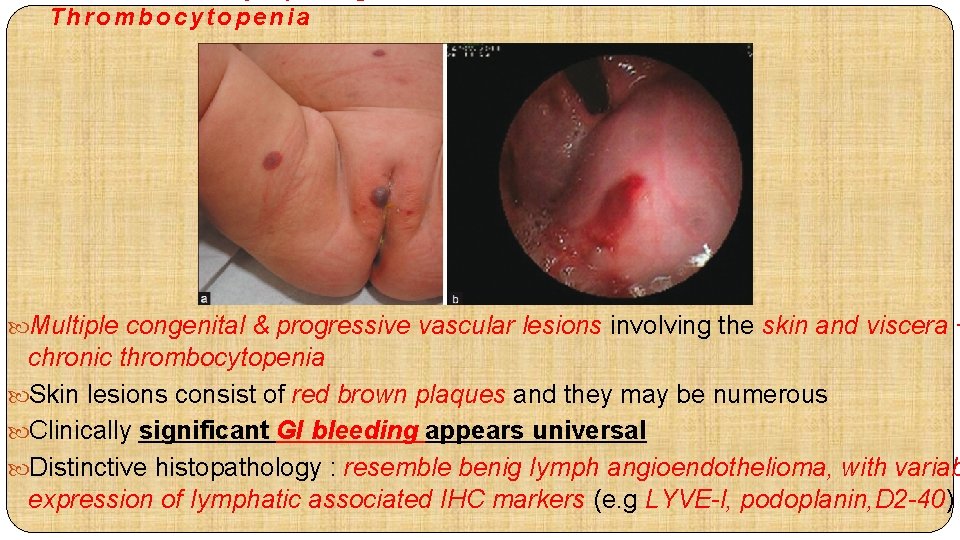
Thrombocytopenia Multiple congenital & progressive vascular lesions involving the skin and viscera + chronic thrombocytopenia Skin lesions consist of red brown plaques and they may be numerous Clinically significant GI bleeding appears universal Distinctive histopathology : resemble benig Iymph angioendothelioma, with variab expression of Iymphatic associated IHC markers (e. g LYVE-l, podoplanin, D 2 -40)
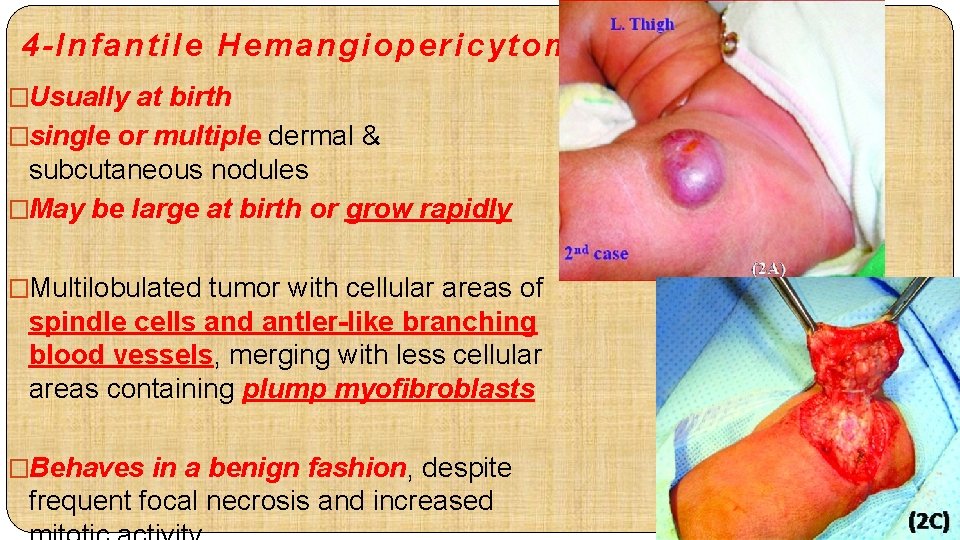
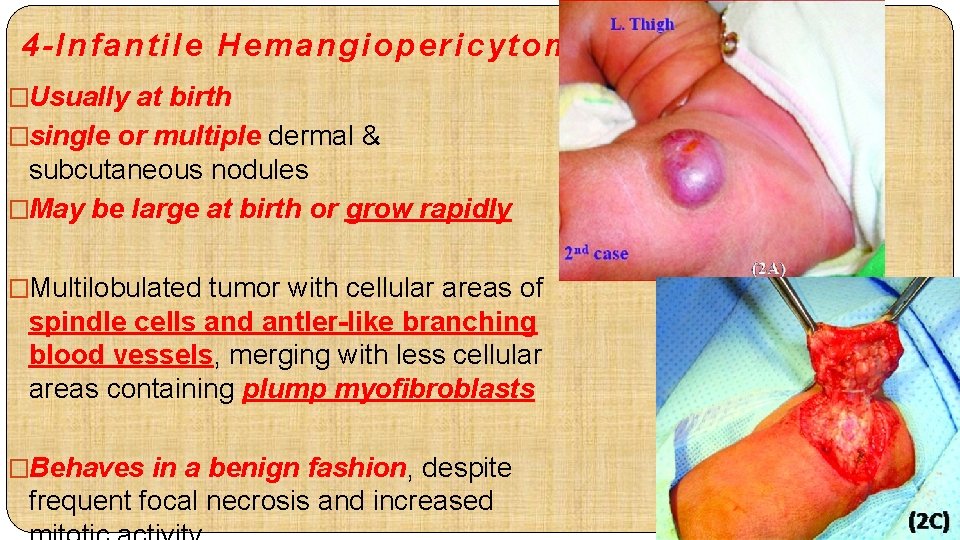
4 -Infantile Hemangiopericytoma �Usually at birth �single or multiple dermal & subcutaneous nodules �May be large at birth or grow rapidly �Multilobulated tumor with cellular areas of spindle cells and antler-like branching blood vessels, merging with less cellular areas containing plump myofibroblasts �Behaves in a benign fashion, despite frequent focal necrosis and increased
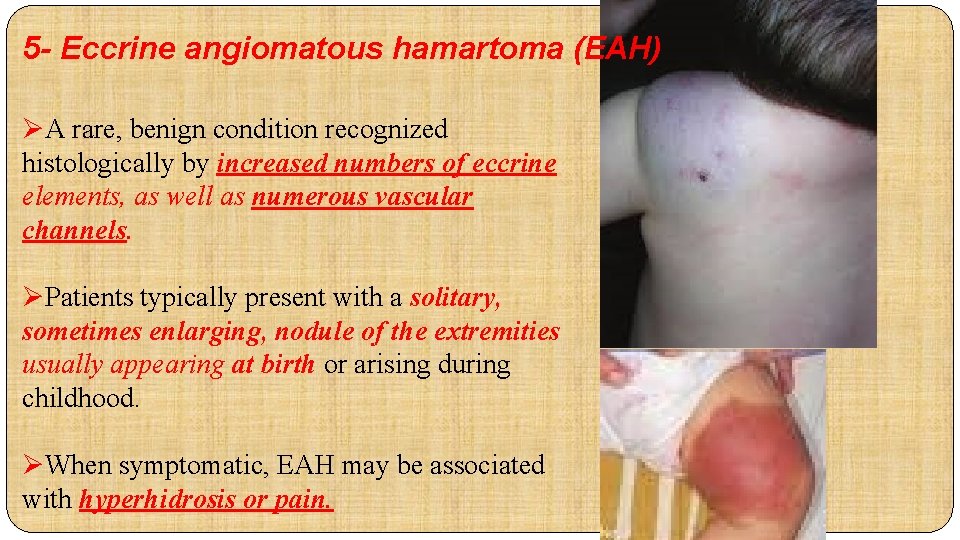
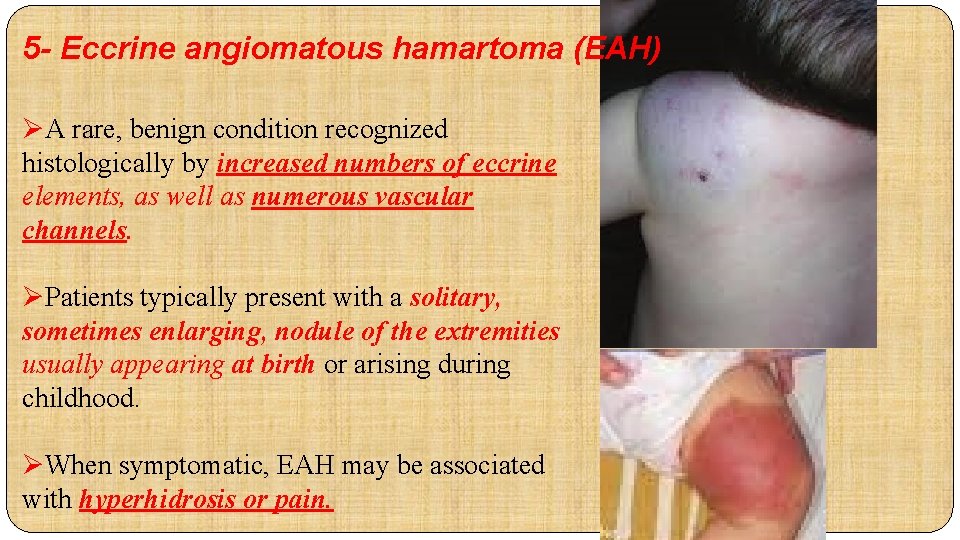
5 - Eccrine angiomatous hamartoma (EAH) ØA rare, benign condition recognized histologically by increased numbers of eccrine elements, as well as numerous vascular channels. ØPatients typically present with a solitary, sometimes enlarging, nodule of the extremities usually appearing at birth or arising during childhood. ØWhen symptomatic, EAH may be associated with hyperhidrosis or pain.
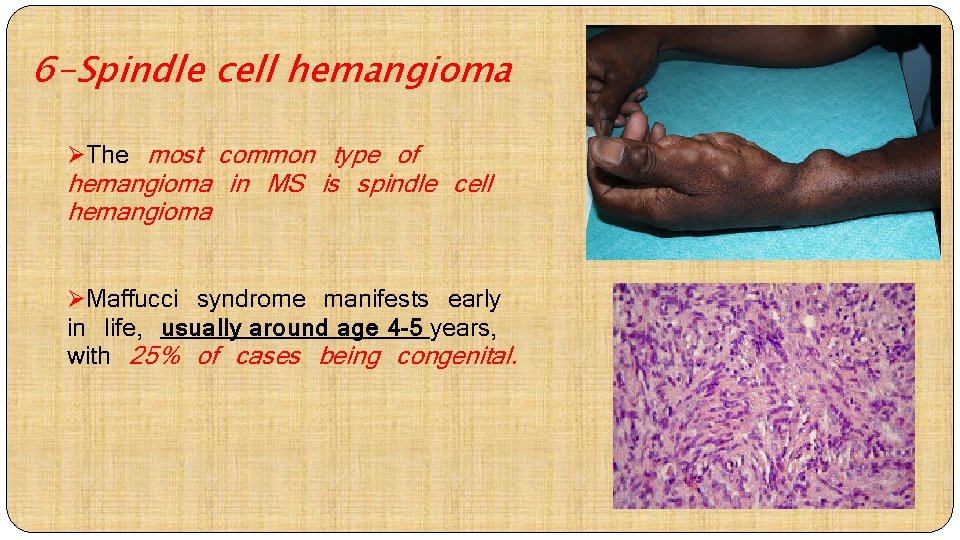
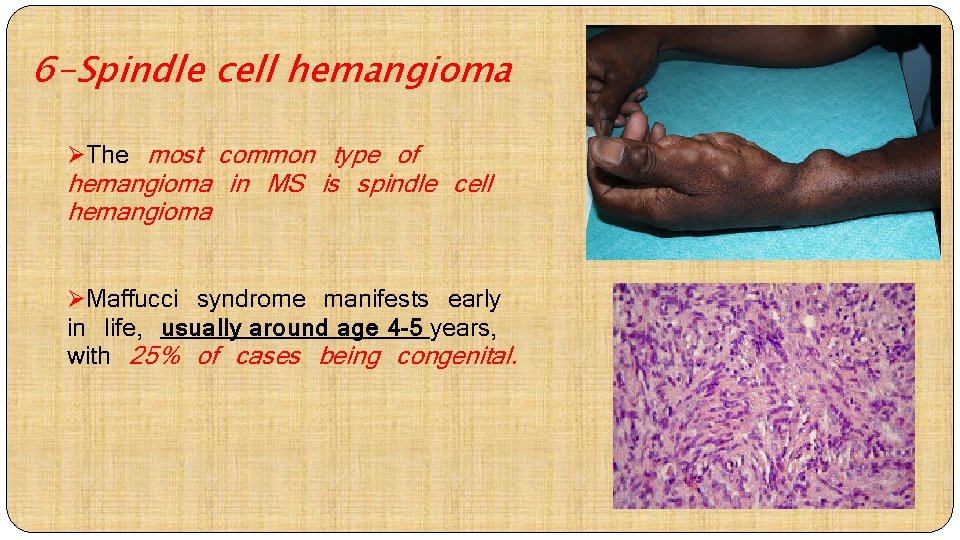
6 -Spindle cell hemangioma ØThe most common type of hemangioma in MS is spindle cell hemangioma ØMaffucci syndrome manifests early in life, usually around age 4 -5 years, with 25% of cases being congenital.
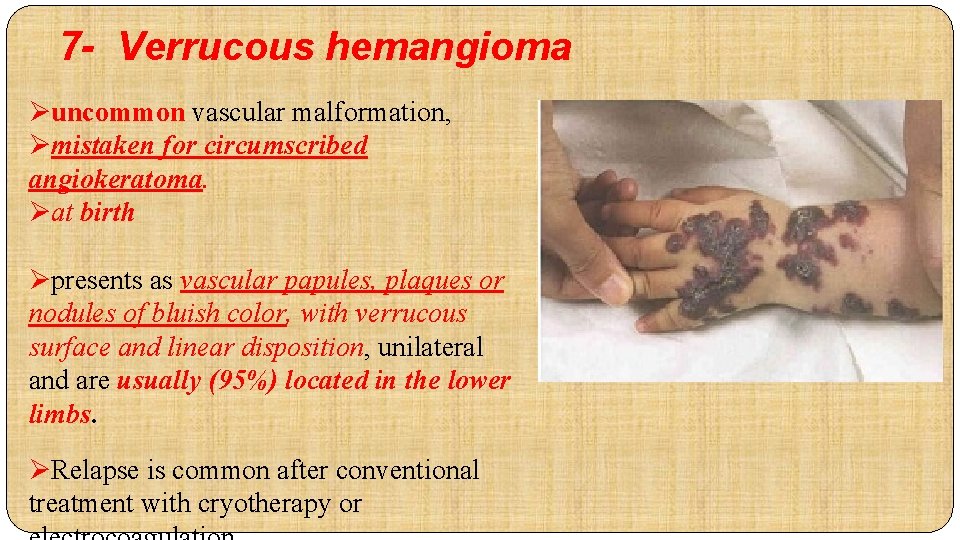
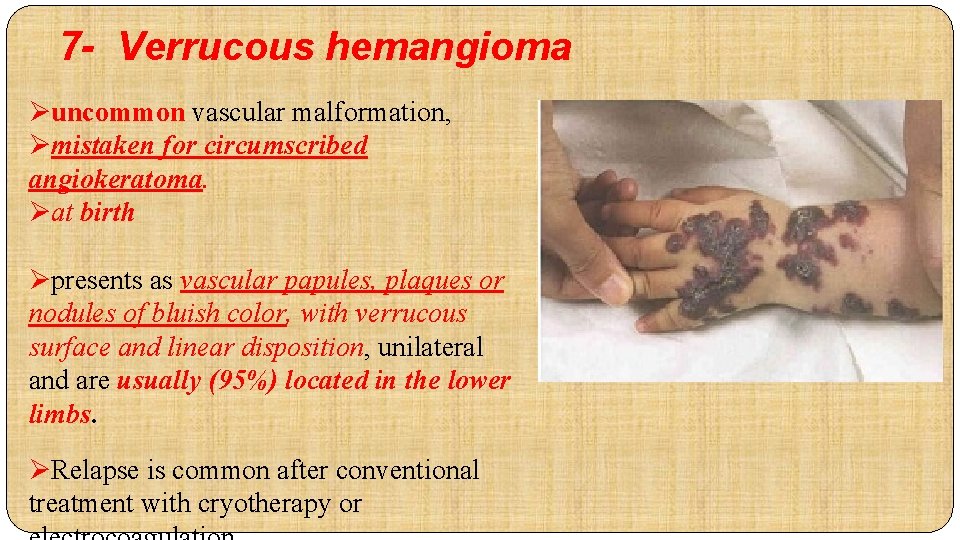
7 - Verrucous hemangioma Øuncommon vascular malformation, Ømistaken for circumscribed angiokeratoma. Øat birth Øpresents as vascular papules, plaques or nodules of bluish color, with verrucous surface and linear disposition, unilateral and are usually (95%) located in the lower limbs. ØRelapse is common after conventional treatment with cryotherapy or
other neoplasms that may have a vascular appearance due to overlying telangiectasias or a blue to red color : congenital fibrosarcoma Rhabdomyosarcoma Neuroblastoma primitive neuroectodermal tumor lymphoblastic lymphoma dermatofibrosarcoma protuberansinfantile myofibromatosis, which can present as solitary or multiple red to pink plaques or nodules; lipoblastoma, presents as an enlarging skin-colored or (less often) erythematous mass; Nasal glioma, often presenting as a congenital blue-red mass on the bridge of the nose.


 Pouya fatemi
Pouya fatemi Hemangioma
Hemangioma Pouya fatemi
Pouya fatemi Hemangioma arteriovenous malformation
Hemangioma arteriovenous malformation Non fatemi vedere i vostri palazzi ma le vostre carceri
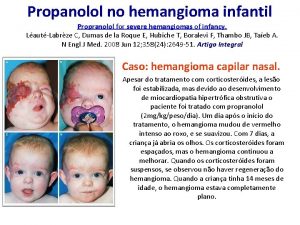
Non fatemi vedere i vostri palazzi ma le vostre carceri Hemangioma infantil fotos
Hemangioma infantil fotos Objectives of nursing process
Objectives of nursing process Define nursing process
Define nursing process Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Black stool pictures
Black stool pictures Chicken pix los pinos menu
Chicken pix los pinos menu Differential diagnosis for leukoplakia
Differential diagnosis for leukoplakia Vitamin c differential diagnosis mnemonic
Vitamin c differential diagnosis mnemonic Acute productive cough differential diagnosis
Acute productive cough differential diagnosis Leukocoria differential diagnosis
Leukocoria differential diagnosis 1152020
1152020 Best language nih
Best language nih Carcinoma in situ
Carcinoma in situ Broadbent sign in constrictive pericarditis
Broadbent sign in constrictive pericarditis Differential diagnosis of otitis externa
Differential diagnosis of otitis externa Gastric ulcer differential diagnosis
Gastric ulcer differential diagnosis Resolution of dka
Resolution of dka Occlusio pupillae definition
Occlusio pupillae definition Alarm signs of pud
Alarm signs of pud Normocytic hypochromic anemia differential diagnosis
Normocytic hypochromic anemia differential diagnosis Osteochondrosis
Osteochondrosis Nephrotic syndrome differential diagnosis
Nephrotic syndrome differential diagnosis Differential diagnosis of learning disabilities
Differential diagnosis of learning disabilities Differential diagnosis of dysphagia
Differential diagnosis of dysphagia