Assessment Management of Patients With Respiratory Tract Disorders







- Slides: 55
Assessment & Management of Patients With Respiratory Tract Disorders
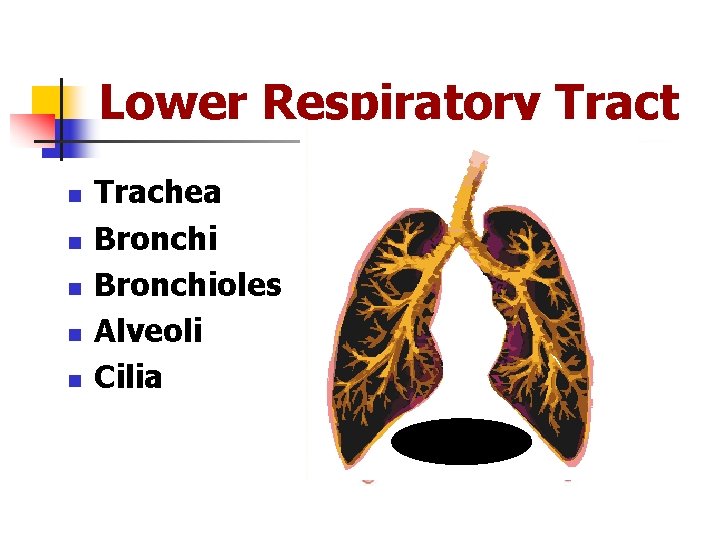
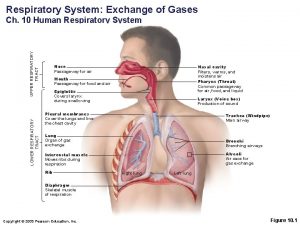
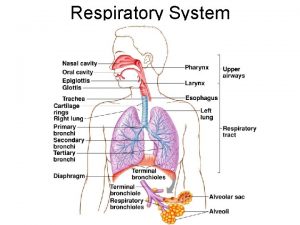
Lower Respiratory Tract n n n Trachea Bronchioles Alveoli Cilia
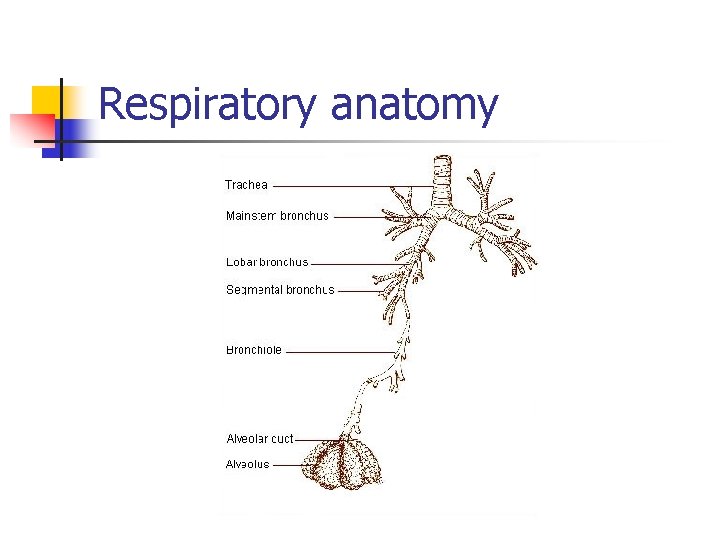
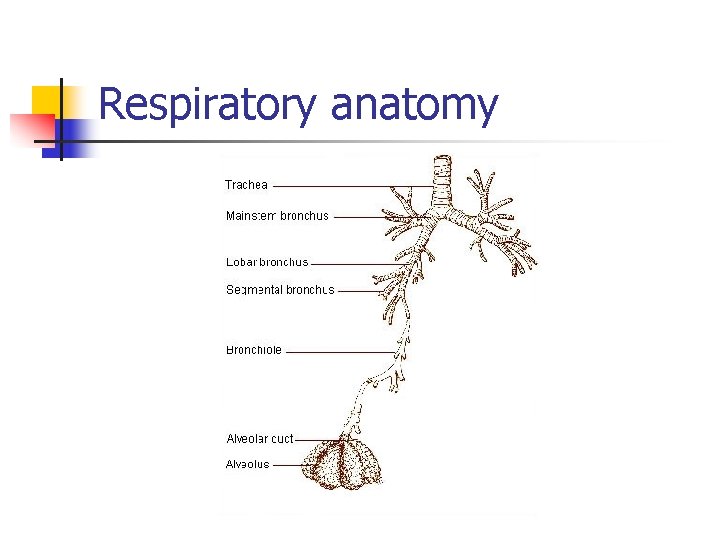
Respiratory anatomy
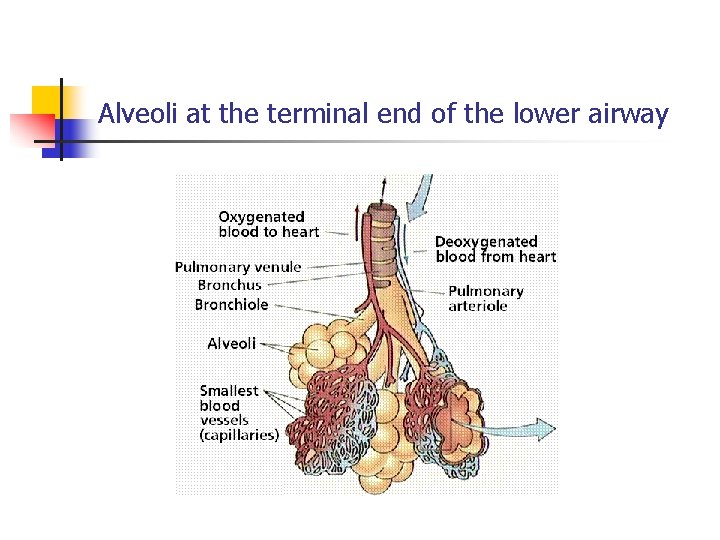
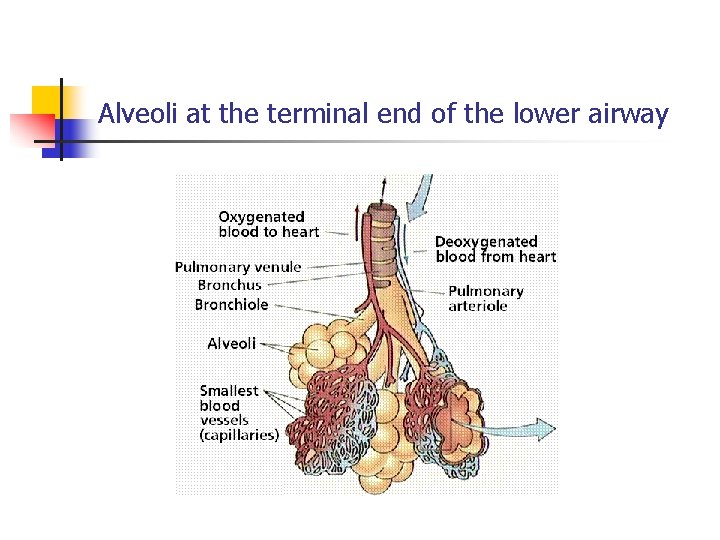
Alveoli at the terminal end of the lower airway
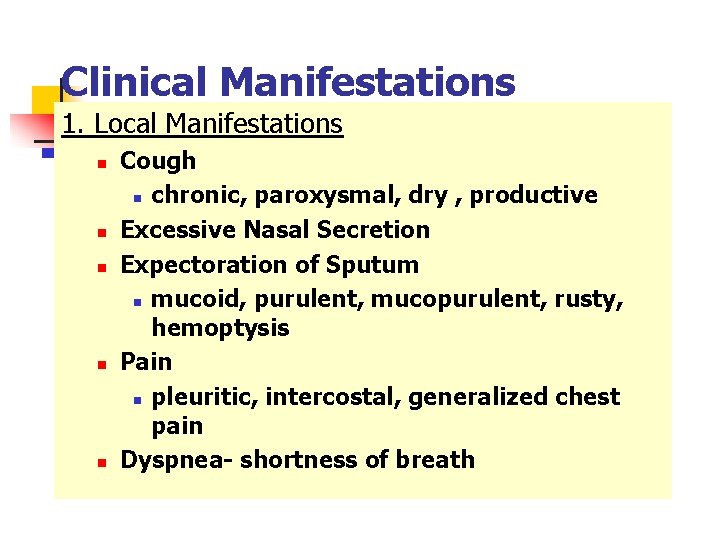
Clinical Manifestations 1. Local Manifestations n n n Cough n chronic, paroxysmal, dry , productive Excessive Nasal Secretion Expectoration of Sputum n mucoid, purulent, mucopurulent, rusty, hemoptysis Pain n pleuritic, intercostal, generalized chest pain Dyspnea- shortness of breath
Function Gases are moved in and out of the lung through pressure changes. Intrapleural pressure is negative (less than atmospheric pressure – 760 mm. Hg) Please refer to suggested reading notes
Clinical Manifestations 2. Systemic Manifestations n Hypoxemia n insufficient oxygenation of the blood n cyanosis- bluish, grayish discoloration of skin & mucous membranes n Hypoxia n inadequate tissue oxygenation n Hypercapnia n CO 2 in arterial blood above normal limits n Hypocapnia n CO 2 in arterial blood below normal limits n Respiratory Failure
Medical Terminology (Respiratory conditions) Respiratory Failure: The inability of n the cardovascular and pulmonary systems to maintain an adequate exchange of oxygen and carbondioxide in the lungs. Maybe caused by a failure in oxygen or n in ventilation. Can be hypoxemic or hypercapneic. n
Medical terminology cont. Ventilation: the process of moving n gases into and out of the lungs Work of Breathing: The effort required for expanding and contracting of the lungs. The influencing factors: the rate and depth of breathing, the ease in which the lungs can be expanded and airway resistance
Assessment of Respiratory System Health History n n Risk Factors Major Clinical Manifestations n Cough n Sputum production n Chest pain n Wheezing n Clubbing of the fingers n Cyanosis
Assessment of Respiratory System Physical Examination n n Inspection n posture, shape, movement, dimensions of chest, flared nostrils, use of accessory muscles, skin color, and rate, depth, & rhythm of respiration Palpation n respiratory excursion, masses, tenderness Percussion n flat, dull, resonant, hyperresonant sounds Auscultation n breath sounds, voice sounds, crackles, wheezes
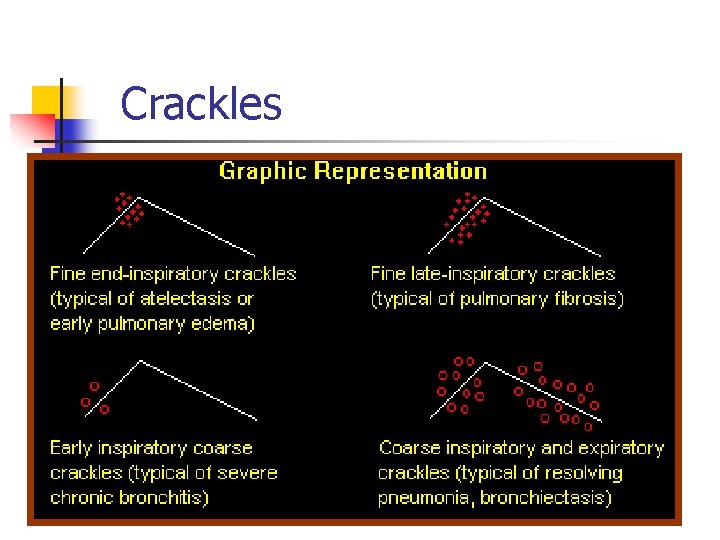
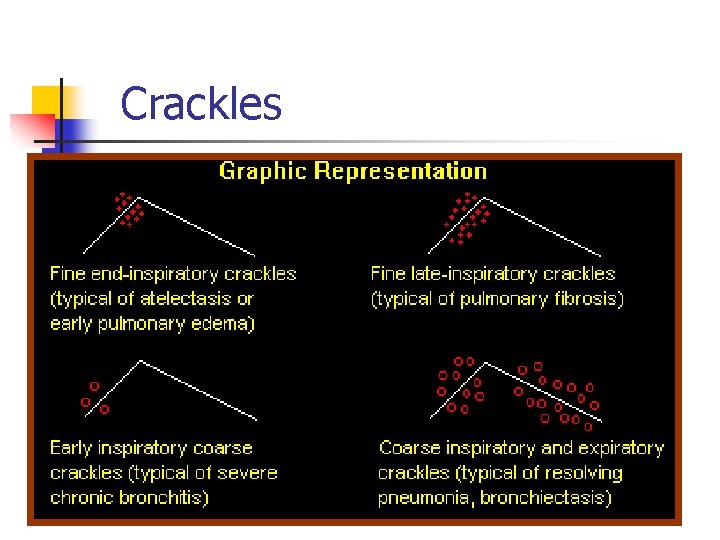
Crackles
Diagnostic Procedures n n n n Sputum Studies n Methods- standard, saline inhalation, gastric washing Arterial Blood Gases n measurements of blood p. H , arterial O 2 & CO 2 tensions, acid-base balance Pulse Oximetry Chest X-ray Bronchoscopy Thoracentesis Laryngoscopy

Lower Respiratory Disorders
Pneumonia n Inflammation & infection of lunginfecting organisms typically inhaledorganisms transmitted to lower airways and alveoli causing inflammation- impairs gas exchange Etiology: bacteria, virus, Mycoplasma, fungus, or from aspiration or inhalation of chemicals or other toxic substances n Risk factors: cigarette smoking, chronic underlying disorders, severe acute illness, suppressed immune system, & immobility

Pneumonia Assessment: Questions to ask n Have you been experiencing difficulty breathing? n Are you having pain? Where? n Do you have a cough? n Have you been running a fever? n Have you been feeling tired? Clinical Manifestations: n fever, pleuritic chest pain, tachypnea, SOB, tachycardia, cough, sputum production- rusty, blood-tingled or yellow-green, fatigue, poor appetite
Pneumonia Diagnostic: n Sputum and blood cultures, CBC, ABGs, CXR, & Bronchoscopy Nursing Diagnoses: n Ineffective airway clearance r/t thick, tenacious sputum n Ineffective breathing pattern r/t tachypnea, chest pain, & airway inflammation n Impaired gas exchange r/t exudate in alveoli n Activity intolerance r/t hypoxemia, fatigue n Acute pain r/t disease process n Imbalanced nutrition less than body required
Pneumonia Planning: Client Outcomes n Maintain open & clear airway, normal RR, PO 2 level without supplemental O 2, complete physical care without frequent rest periods Interventions n Improve airway patency- auscultate lung sounds, monitor ABGs or pulse oximetry, elevate HOB, C & DB q 2 hrs, ambulate , O 2 as needed n Promote fluid intake & promote activity tolerance n Monitor & prevent complications n High fowler’s positioning to facilitate air exchange
Pneumonia n Pharmacology: n Antibiotic therapy based on sputum culture & sensitivity n n § § § Levaquin, Tequin, Rocephin, Primaxin, Zithromax, Ketek, Zinacef, Cipro, Tetracycline Instruct to finish all antibiotics at prescribed intervals Short acting beta 2 agonist such as Salbutamol Corticosteroids , Prednisolone to decrease inflammation Influenza vaccine, pneumococcal vaccine
n n Period of bed rest Promote adequate nutrition Provide support Evaluation: n n n breathing easier without chest pain temperature normal, activity level increased without frequent rest periods
Tuberculosis n n Infectious disease that primarily affects the lungs; may be transmitted to other parts of the body Pulmonary infiltrates accumulate, cavities develop, & masses of granulated tissue form within the lungs Primary infectious agent- Mycobacterium Bacilli Transmitted by inhalation of droplets (talking, coughing, sneezing, & singing) Risk factors: immune system disorder, preexisting medical conditions, institutionalized, health care workers
ARDS Acute Respiratory Disease Syndrome A form of Acute Lung Injury n Diffused alveolar injury n An acute condition characterized by bilateral pulmonary infiltrates and severe hypoxemia Build up fluid in alveolar n n

ARDS - Causes Breathing vomit into lungs (aspirations) Inhaling chemicals n Lung transplannt n Pneumonia n Septic shock (infection thru body) n Trauma n n

ARDS -Characterstics Stiff heavy lungs(decreases the lungs n ability to expand) The level of oxygen in the blood can n stay dangerously low (even if oxygen is given via a ventilator)
ARDS - Symptoms usually develop 24 to 48 hrs of illness or injury Dyspnoea n Low blood pressure (infection) and n organ failure Rapid breathing n n
ARDS - Diagnostics Arterial Blood Gas n Blood Tests n Blood and Urine cultures n Bronchoscopy n Chest x-ray n Sputum culture and analysis

ARDS - Treatment Intensive Care Admission Antibiotic therapy n Steroid therapy n Diuretics n Ventilatory support n n
PULMONARY EMBOLISM Is a complication of an underlying n venous thrombosis Patient may not show classic signs and symptoms n
PE – SIGNS AND SYMPTOMS Classic presentation: Pleuretic chest pain n Dyspnoea n Hypoxia n n
PE – Signs and symptoms Seizures n Syncope n Abdominal pain n Fever n Productive cough n Wheezing n Altered level of consciousness n
PE – Signs and Symptoms New onset of atrial fibrillation Hemoptysis n Flank pain n Delirium n n
PE - Diagnosis ECG n Chest xray, CT, MRI, Echo, VQ scan n Blood tests –Dimer, coagulation profile, Arterial blood gas n
PE - Management Anticoagulation (warfarin, heparin, retaplse) Surgical intervention : n Emoblectomy n Vena Cava filters n n
Pulmonary Tuberculosis Mycobacterium tuberculosis n Airborne transmission n Tuberculin skin testing n Pharmacologic therapy- multidrug regimens and prophylaxis n
Tuberculosis Assessment: n Questions to ask - Are you suffering from night sweats? Have you lost weight? Have you been having low-grade fever? Have you been having SOB and coughing up anything from your lungs? Have you had chest pain? Where? Have you had weight loss? Clinical Manifestations- low-grade fever (late afternoon), night sweats, weight loss, anorexia, fatigue, chronic productive cough, pleuritic chest pain, hemoptysis
Tuberculosis Diagnostic: n Sputum culture- + acid-fast bacilli (AFB) n Skin testing- PPD n CBC- WBC elevated n CXR n Bronchoscopy Nursing Diagnosis: n Ineffective airway clearance r/t thick, tenacious secretions n Ineffective breathing pattern r/t airway inflammation

Tuberculosis Altered nutrition less than body requirements r/t anorexia and fatigue n Fatigue r/t disease process n Anxiety r/t social isolation secondary to isolation protocols Planning: Clients Outcomes n Maintain clear airway, normal RR, achieve weight gain, anxiety decreased Interventions: n Maintain respiratory isolation- infectious period - diversional activities n Barrier protection should be used n
Evaluation: n Client adheres to isolation precautions, takes medication as prescribed Complications v Miliary TB The organism invade the blood stream and can spread to multiple body organ n n Meningitis Pericarditis
Tuberculosis n n n n Promote airway clearance- bedrest, increase fluid intake, high humidity Pharmacology n First-line meds- Isoniazid, Rifampin, Ehtambutol, & Pyrazinamide for 4 months n Isoniazid and Rifampin continued for an additional 2 months or up to 12 months. Advocate adherence & prevention Monitor and manage potential complications Adequate nutrition Provide client and family education Provide emotional support
Tuberculosis n Questions to ask n Do you have difficulty breathing- all the time or is it caused by exertion? n Do you cough frequently and is it productive? n Have you had a weight loss? n Do you feel tired quite often and are your activities impaired by SOB or fatigue? n Do you have many respiratory infections? Over what period of time?
Tuberculosis Nursing Diagnosis n Ineffective airway clearance r/t thick, tenacious secretion and fatigue n Ineffective breathing pattern r/t fatigue and obstruction of the bronchial tree n Impaired gas exchange r/t increased sputum production n Activity intolerance r/t hypoxemia & fatigue n Altered nutrition r/t increased metabolic demands, fatigue, & anorexia n Anxiety r/t inability to breathe effectively
Tuberculosis Diagnostics: n ABGs, CBC, sputum culture, CXR, Pulmonary function tests Planning: Client Outcomes n Effectively clear airway and breathing pattern, maintain normal ABGs, increase activity with decrease SOB or fatigue, maintain weight, and less anxious with episodes of SOB
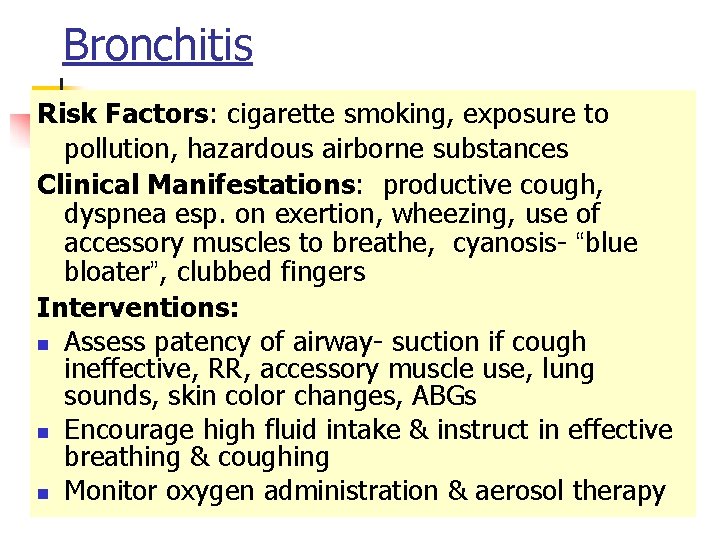
Bronchitis n n n Inflammation of the bronchi caused by irritants or infection hypertrophy & hypersecretion of mucous- cause increase in sputum production increase mucous- decrease airway lumen sizelumen becomes colonized with bacteria. Bronchial wall becomes scarred - leads to stenosis & airway obstruction Defined as a productive cough that lasts 3 months a year for 2 consecutive years with other causes excluded. Cough in the morning with sputum production is indicative of Chronic Bronchitis

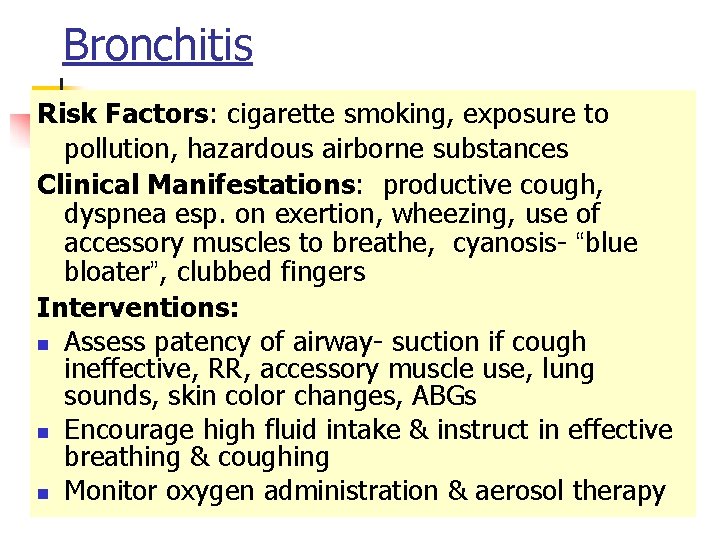
Bronchitis Risk Factors: cigarette smoking, exposure to pollution, hazardous airborne substances Clinical Manifestations: productive cough, dyspnea esp. on exertion, wheezing, use of accessory muscles to breathe, cyanosis- “blue bloater”, clubbed fingers Interventions: n Assess patency of airway- suction if cough ineffective, RR, accessory muscle use, lung sounds, skin color changes, ABGs n Encourage high fluid intake & instruct in effective breathing & coughing n Monitor oxygen administration & aerosol therapy
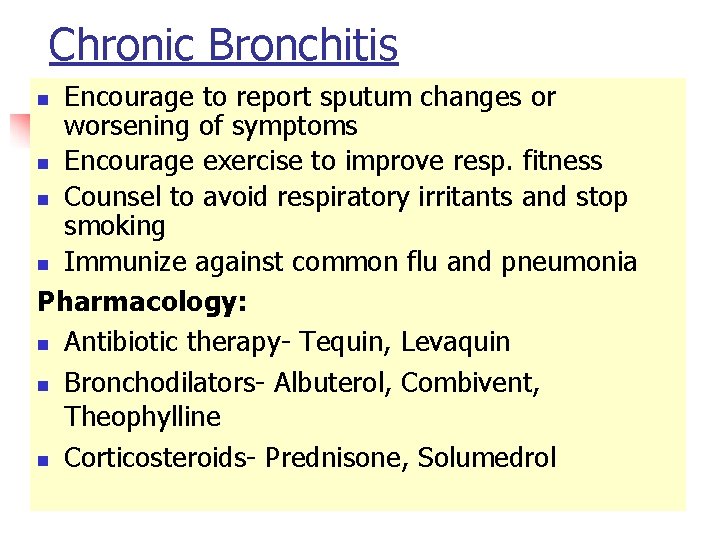
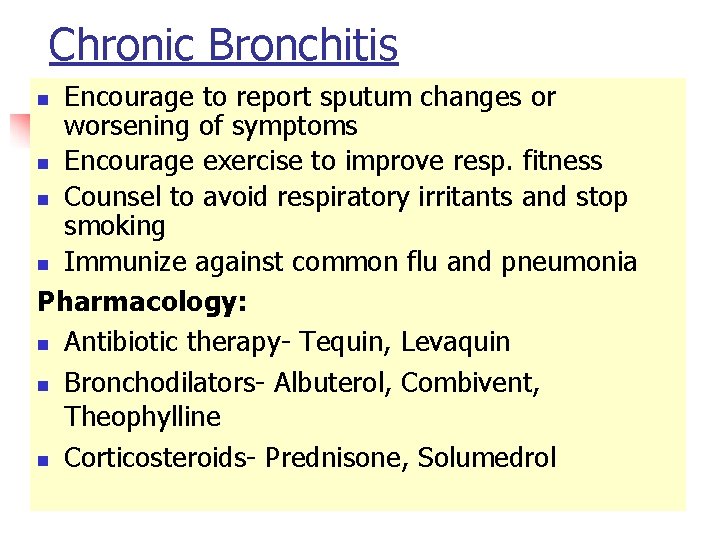
Chronic Bronchitis Encourage to report sputum changes or worsening of symptoms n Encourage exercise to improve resp. fitness n Counsel to avoid respiratory irritants and stop smoking n Immunize against common flu and pneumonia Pharmacology: n Antibiotic therapy- Tequin, Levaquin n Bronchodilators- Albuterol, Combivent, Theophylline n Corticosteroids- Prednisone, Solumedrol n
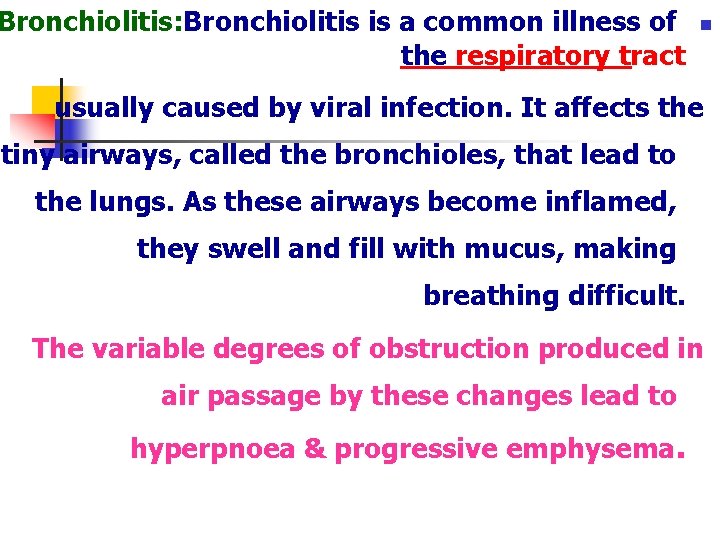
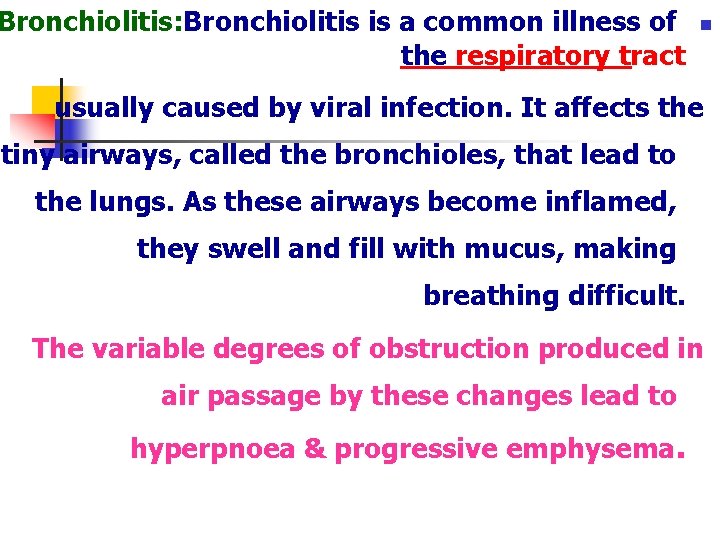
Bronchiolitis: Bronchiolitis is a common illness of the respiratory tract n usually caused by viral infection. It affects the tiny airways, called the bronchioles, that lead to the lungs. As these airways become inflamed, they swell and fill with mucus, making breathing difficult. The variable degrees of obstruction produced in air passage by these changes lead to hyperpnoea & progressive emphysema.
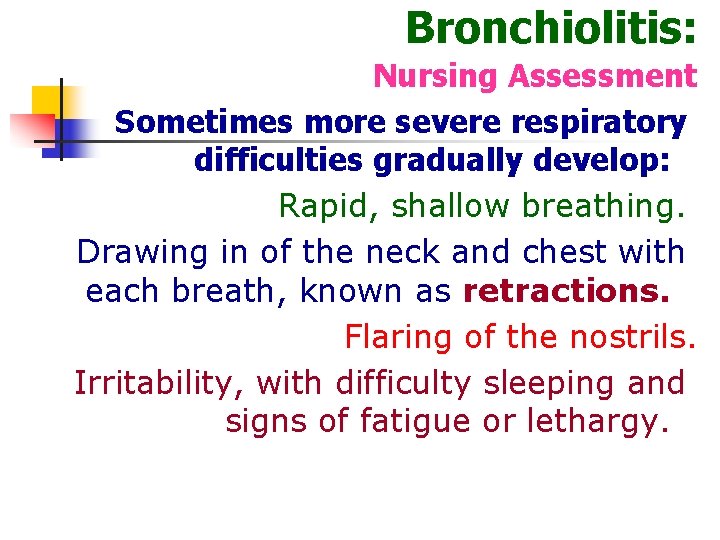
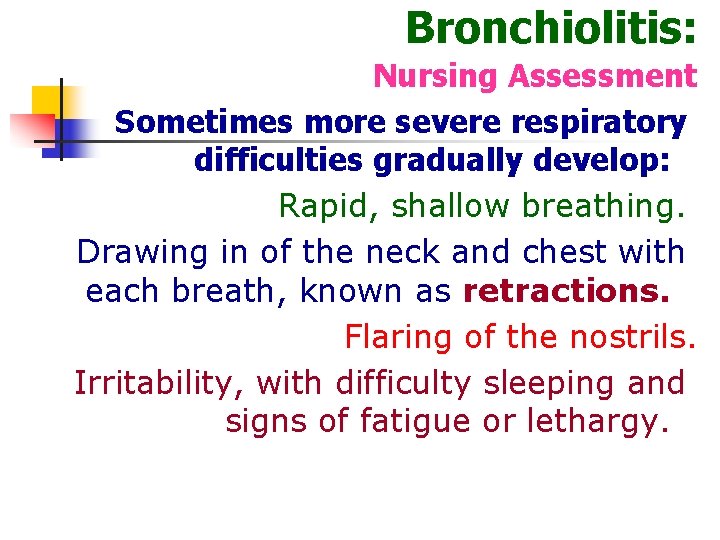
Bronchiolitis: Nursing Assessment Sometimes more severe respiratory difficulties gradually develop: Rapid, shallow breathing. Drawing in of the neck and chest with each breath, known as retractions. Flaring of the nostrils. Irritability, with difficulty sleeping and signs of fatigue or lethargy.
Bronchiolitis Nursing care: Follow strict precautions to prevent spread of infection. Administer high humidified oxygen. Clear nasal congestion, try a bulb syringe and saline (saltwater) nose drops. Provide adequate Ng. Care for vomiting, fever, & diarrhea. Small frequent diet, & increase fluid intake.
Lung abscess n n n A lung abscess is a localized area of lung destruction liquefaction necrosis usually related to pyogenic bacteria Cavity formation n n Clinical manifestation Dyspnoea Chest pain Tachycardia
Diagnosis Method CT n Chest X ray n Encourage exercise to improve resp. fitness n Counsel to avoid respiratory irritants and stop smoking n Immunize against common flu and pneumonia Pharmacology: n Antibiotic therapy- Tequin, Levaquin n Bronchodilators- Albuterol, Combivent, Theophylline n
 Pyramidal tract vs extrapyramidal tract
Pyramidal tract vs extrapyramidal tract Olivospinal tract vs tectospinal tract
Olivospinal tract vs tectospinal tract Nursing care of male patients with genitourinary disorders
Nursing care of male patients with genitourinary disorders Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Anatomical structures of the upper respiratory tract
Anatomical structures of the upper respiratory tract Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Passage of air through the respiratory tract
Passage of air through the respiratory tract Classification of pneumonia
Classification of pneumonia Upper and lower respiratory system
Upper and lower respiratory system Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Phelebetomy
Phelebetomy Upper respiratory tract
Upper respiratory tract Upper respiratory tract
Upper respiratory tract Carina nasal
Carina nasal Lrti
Lrti Normal flora of respiratory tract
Normal flora of respiratory tract Respiratory zone
Respiratory zone Bristolian douglas rys
Bristolian douglas rys Nottingham city hospital respiratory assessment unit
Nottingham city hospital respiratory assessment unit Lippincott williams & wilkins
Lippincott williams & wilkins Management of patients with neurologic trauma
Management of patients with neurologic trauma Cva
Cva Urised otc
Urised otc Sexually transmitted diseases
Sexually transmitted diseases Who analgesic ladder
Who analgesic ladder Pathophysiology of intestinal obstruction
Pathophysiology of intestinal obstruction Life expectancy of sickle cell patients
Life expectancy of sickle cell patients Position in bed nursing
Position in bed nursing Perimylolysis
Perimylolysis The factors of care that patients can expect to receive
The factors of care that patients can expect to receive Patients rights charter
Patients rights charter 6 malaysian safety goals
6 malaysian safety goals Cataract care plan
Cataract care plan Nursing interventions for hoarding disorder
Nursing interventions for hoarding disorder Daily intentional nurse leader rounding on patients
Daily intentional nurse leader rounding on patients Module 70 introduction to therapy
Module 70 introduction to therapy Emergency patient move
Emergency patient move Chapter 36 patients with special challenges
Chapter 36 patients with special challenges How does nurse ratched manipulate the patients
How does nurse ratched manipulate the patients Procedure of admission
Procedure of admission Moving and handling dementia patients
Moving and handling dementia patients Leader rounding on patients
Leader rounding on patients Ethical issues in treating lgbt patients
Ethical issues in treating lgbt patients House classification of soft palate
House classification of soft palate Prevention of vte in nonorthopedic surgical patients
Prevention of vte in nonorthopedic surgical patients Emergency move vs rapid extrication
Emergency move vs rapid extrication Dealing with challenging patients
Dealing with challenging patients Rothberg position
Rothberg position Pico questions
Pico questions Handling patients
Handling patients Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Broadmoor patients
Broadmoor patients 10 patients' rights
10 patients' rights Guideline clinical nutrition in patients with stroke
Guideline clinical nutrition in patients with stroke Type 2 diabetes diet sheet
Type 2 diabetes diet sheet Nursing management of liver abscess
Nursing management of liver abscess