Approach to Hematuria and Proteinuria in Children Adi








- Slides: 52
Approach to Hematuria and Proteinuria in Children Adi Alherbish
Objectives • To be able to define and recognize hematuria and proteinuria • To be able to generate a differential diagnosis of the commonest and most serious causes of hematuria and proteinuria • To have a clinical approach to both conditions.
Case 1 • 14 year old boy presenting with red urine since last night. Otherwise healthy. Normal BP, no flank pain, no ankle edema. • What’s the next step?
Case 1 • Urine dipstick: negative


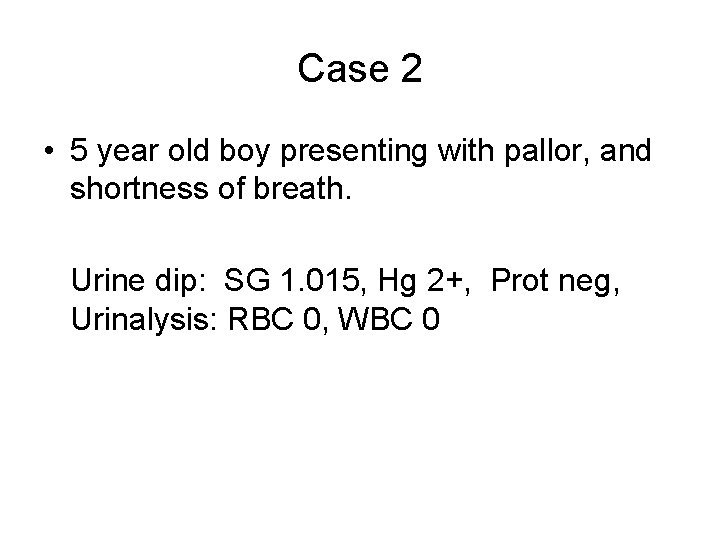
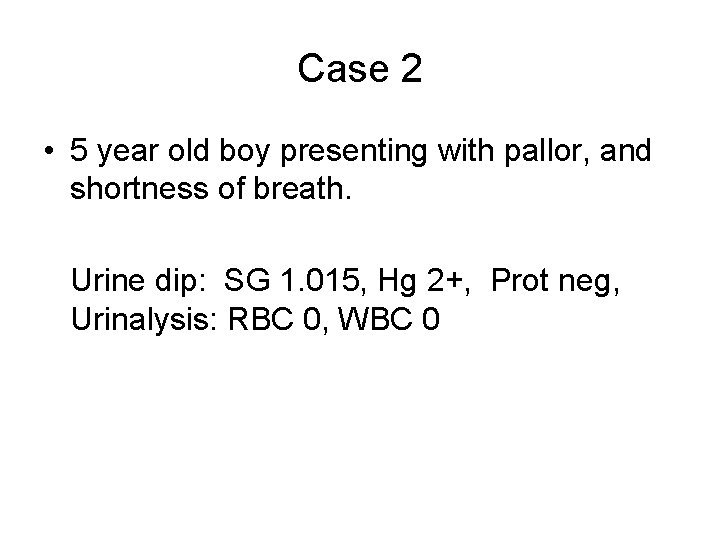
Case 2 • 5 year old boy presenting with pallor, and shortness of breath. Urine dip: SG 1. 015, Hg 2+, Prot neg, Urinalysis: RBC 0, WBC 0

Case 2 • CBC: Hg 80, WBC 5, Plt 180 • Retics: 3% Hemolytic Anemia • Send blood for: Hg electrophoresis, peripheral smear, Coombs test, G 6 PD
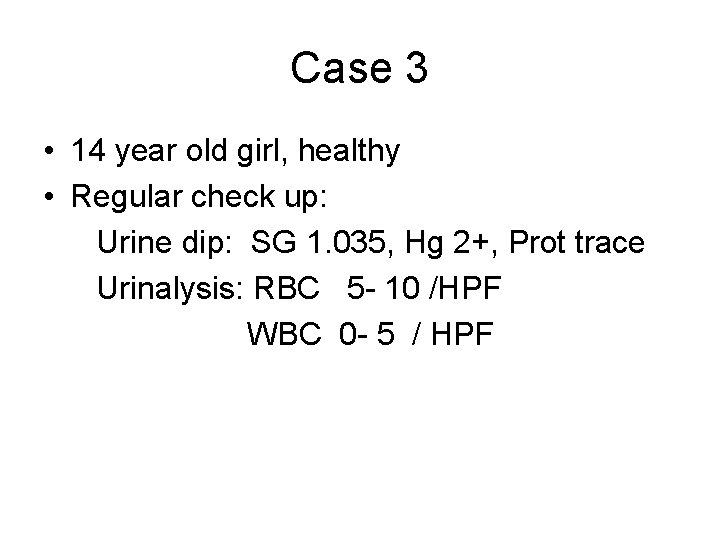
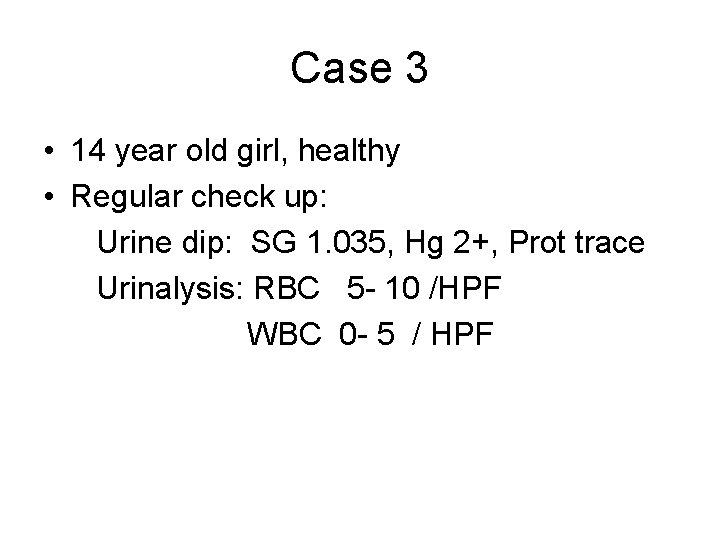
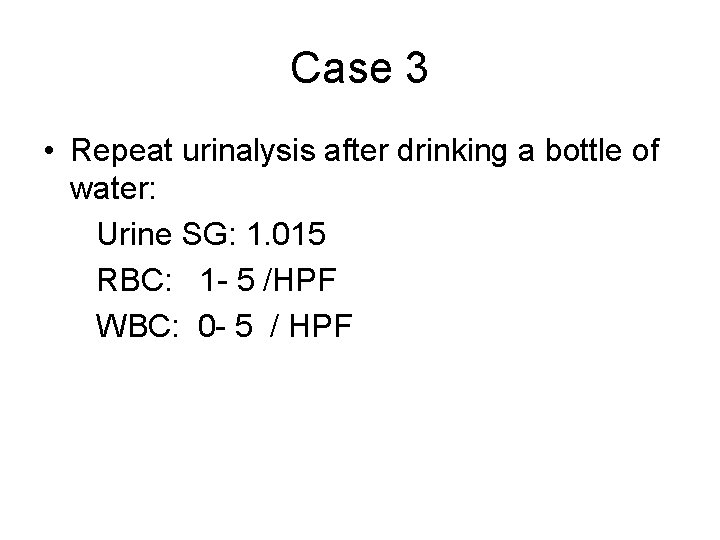
Case 3 • 14 year old girl, healthy • Regular check up: Urine dip: SG 1. 035, Hg 2+, Prot trace Urinalysis: RBC 5 - 10 /HPF WBC 0 - 5 / HPF
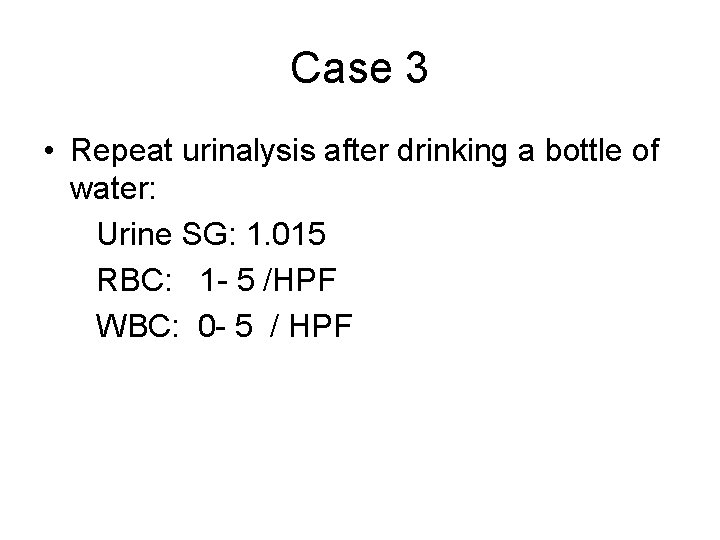
Case 3 • Repeat urinalysis after drinking a bottle of water: Urine SG: 1. 015 RBC: 1 - 5 /HPF WBC: 0 - 5 / HPF
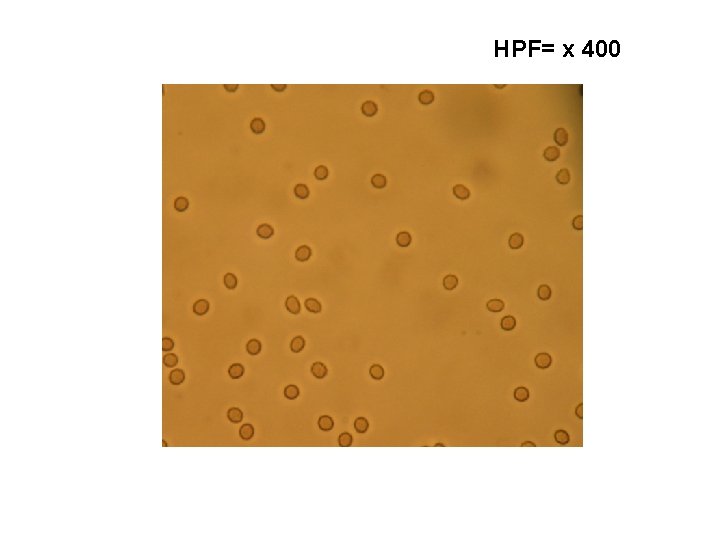
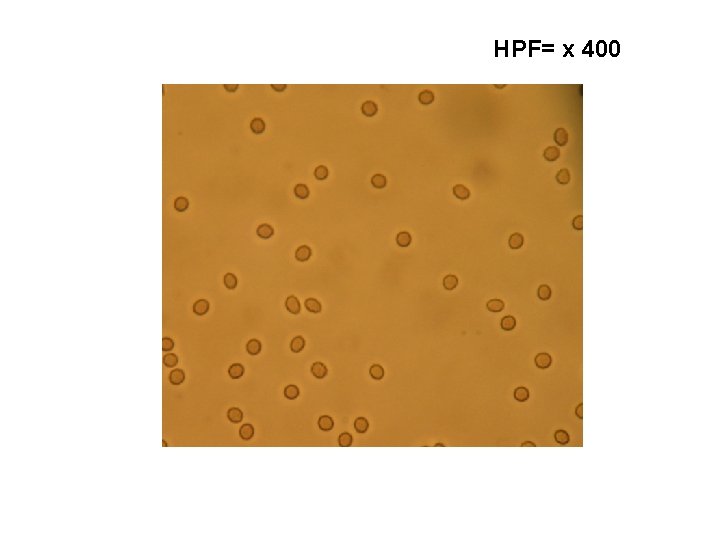
HPF= x 400
Case 5 • 9 year old girl, presenting with fever, rash, coryza, conjuctivitis, and dark urine. • Urine dip: SG 1. 015, Hg +3, Prot trace • Urinalysis: RBC > 100/ HPF WBC 10 - 25/ HPF
Case 5 • Urine positive for adenovirus
Case 6 • 14 year old girl, presenting with intermittent, sudden onset left flank pain and dark urine. • Urine SG: 1. 015, Hg 3+, Prot neg • Urinalysis: RBC 100/ HPF, WBC 0 Crystals present

Case 6 • In clinic: send urine for Ca/ Cr ratio, citrate, oxalate, uric acid, cystine
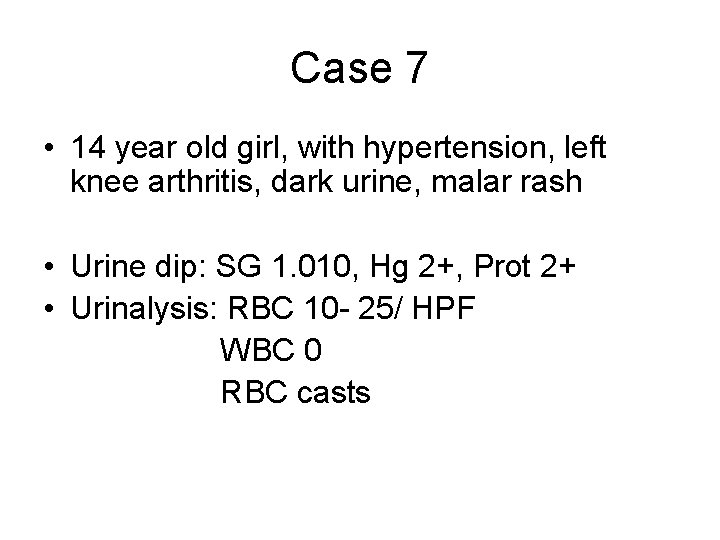
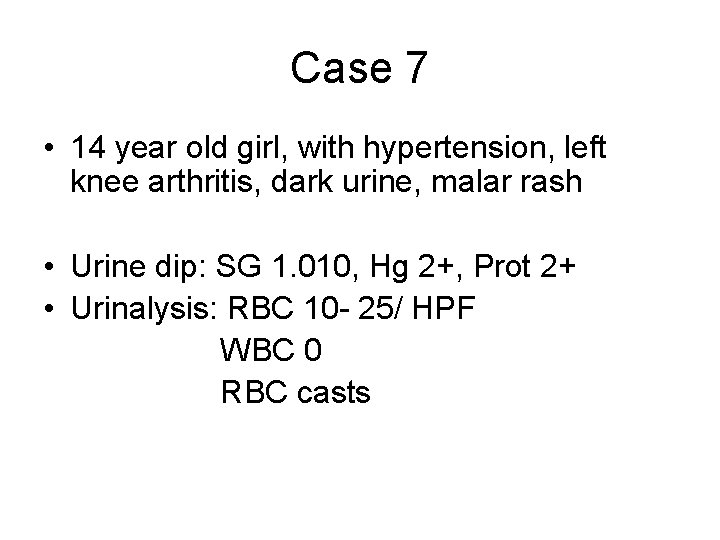
Case 7 • 14 year old girl, with hypertension, left knee arthritis, dark urine, malar rash • Urine dip: SG 1. 010, Hg 2+, Prot 2+ • Urinalysis: RBC 10 - 25/ HPF WBC 0 RBC casts


Case 7 • Send blood for: C 3, C 4, ANA, anti-ds DNA
Hematuria • Presence of > 5 RBC/ HPF, on more than two occasions, in the context of a normal urine specific gravity
The 3 Vital Questions 1 2 3 Is it true hematuria? Is it serious (urgent)? What is the cause?
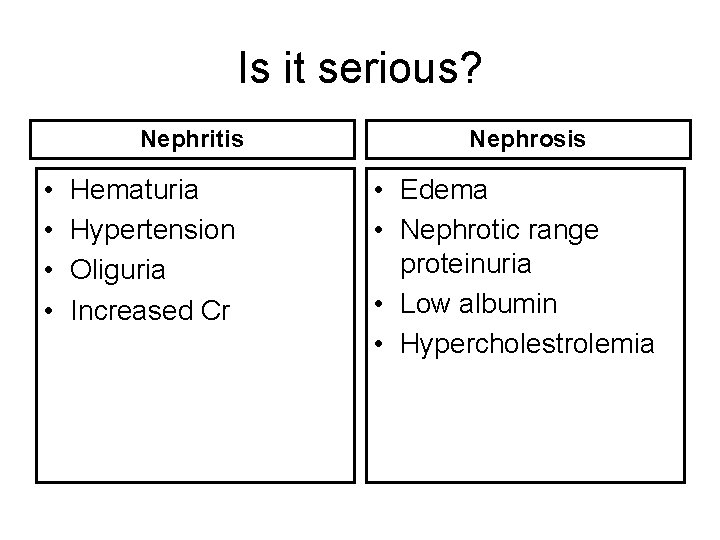
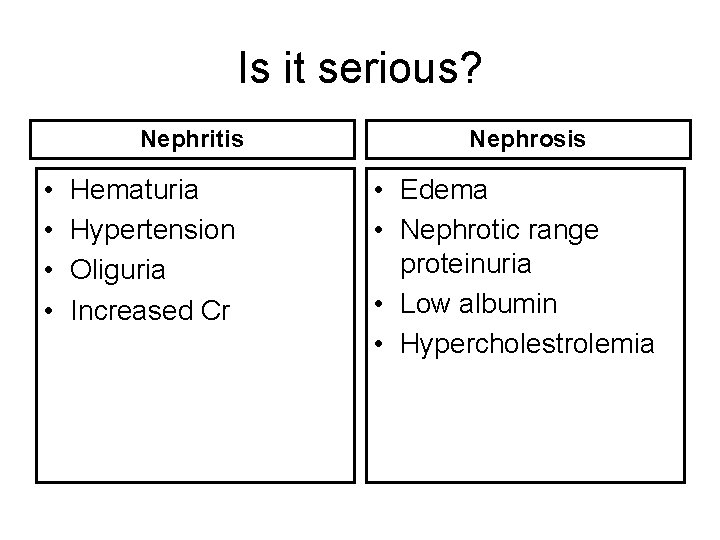
Is it serious? Nephritis • • Hematuria Hypertension Oliguria Increased Cr Nephrosis • Edema • Nephrotic range proteinuria • Low albumin • Hypercholestrolemia
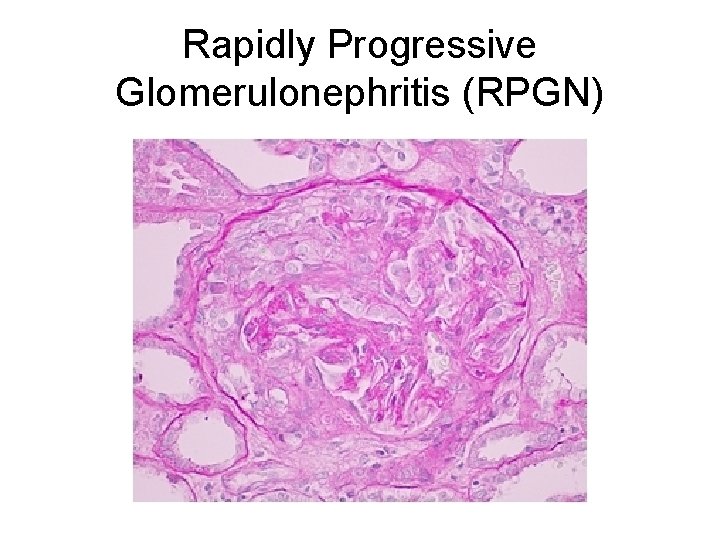
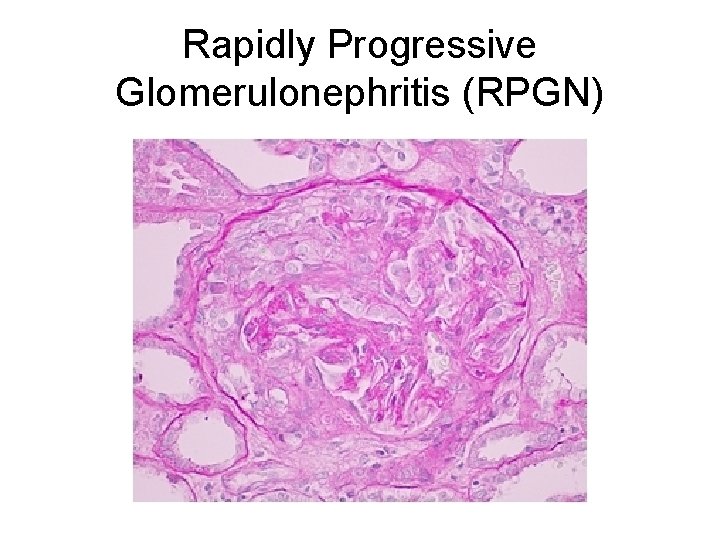
Rapidly Progressive Glomerulonephritis (RPGN)
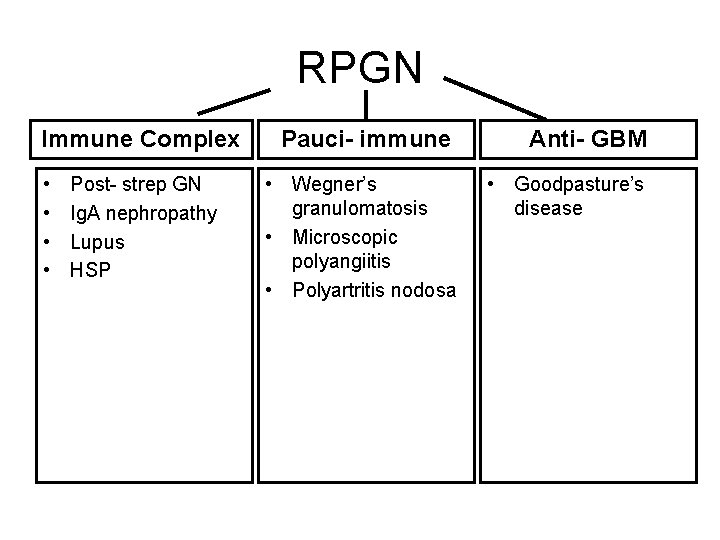
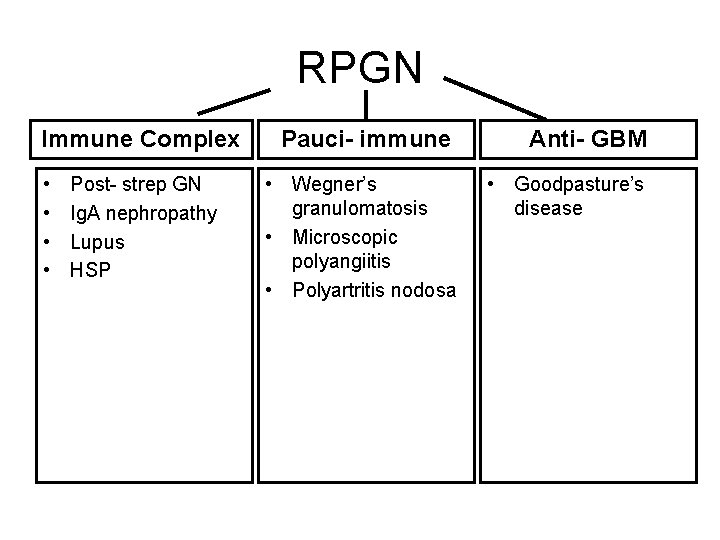
RPGN Immune Complex • • Post- strep GN Ig. A nephropathy Lupus HSP Pauci- immune Anti- GBM • Wegner’s granulomatosis • Microscopic polyangiitis • Polyartritis nodosa • Goodpasture’s disease
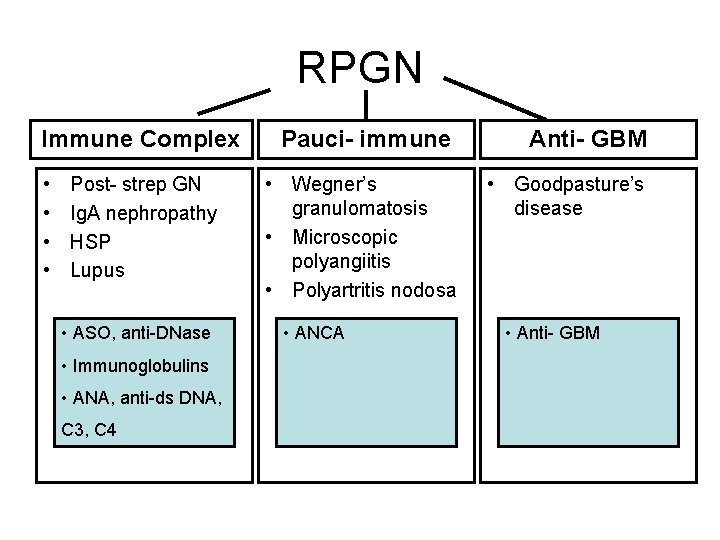
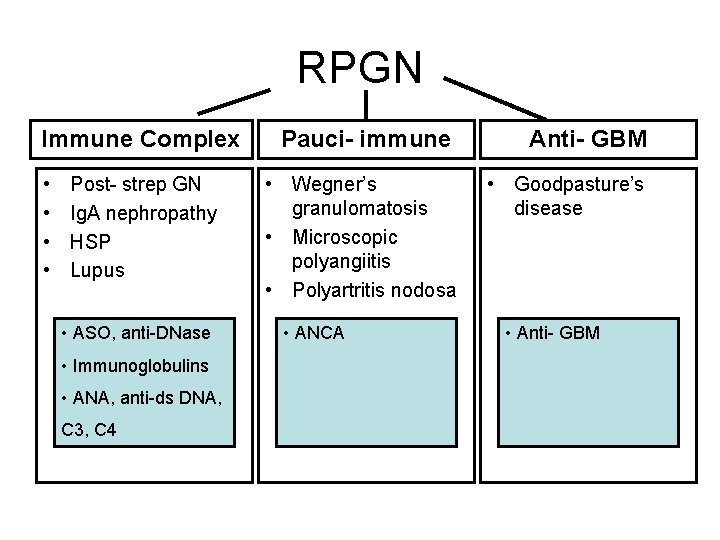
RPGN Immune Complex • • Post- strep GN Ig. A nephropathy HSP Lupus • ASO, anti-DNase • Immunoglobulins • ANA, anti-ds DNA, C 3, C 4 Pauci- immune Anti- GBM • Wegner’s granulomatosis • Microscopic polyangiitis • Polyartritis nodosa • Goodpasture’s disease • ANCA • Anti- GBM
Post strep Glomerulonephritis • Strep pharyngitis, or strep skin infection, followed 10 to 14 days by microscopic hematuria, nephritis, or nephrosis • Diagnosis: positive ASO low C 3 which normalize in 8 weeks • Management: supportive • Prognosis: Excellent (Vog et. Al: 137 cohort. ESRD: none, high Cr 10%)
Ig. A nephropathy • Typical presentation: intermittent gross hematuria that happen during colds • Other: gross hematuria microscopic hematuria nephritis nephrotic syndrome ESRD
Ig. A nephropathy • Diagnosis: clinical suspicion Ig. A level 20% sensitivity! Kidney biopsy- Ig. A in Immunoflorecence • Treatment: supportive in mild cases ACEI in proteinuria Steroids
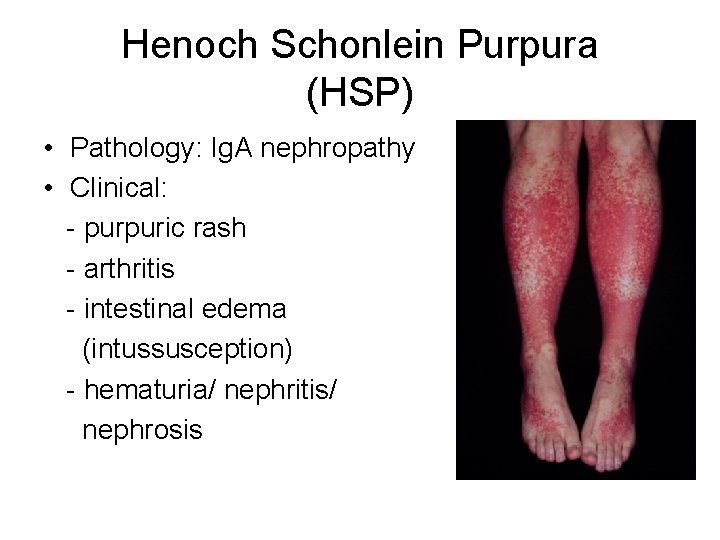
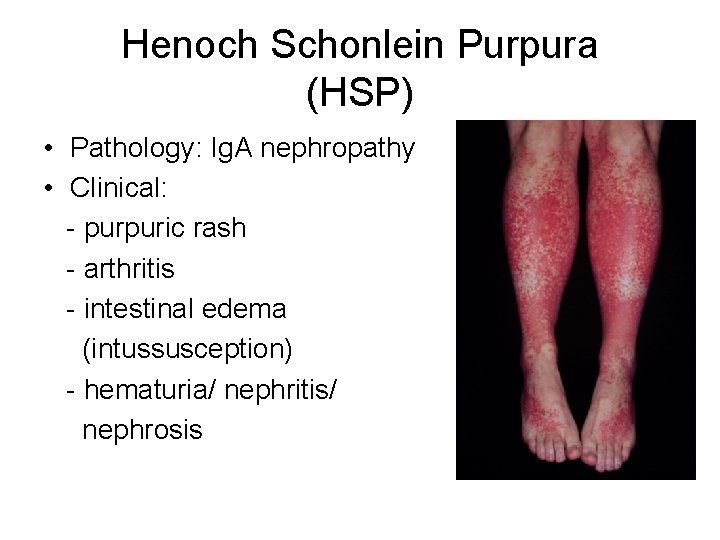
Henoch Schonlein Purpura (HSP) • Pathology: Ig. A nephropathy • Clinical: - purpuric rash - arthritis - intestinal edema (intussusception) - hematuria/ nephritis/ nephrosis
Hemolytic Uremic Syndrome • Pathogenesis: - typical (d+): E. coli O 157: H 7 shiga toxin 1 induced vascular injury - atypical (d-): alternative complement pathway defect • Clinical: triad of microangiopathic hemolytic anemia, thrombocytopenia, ARF
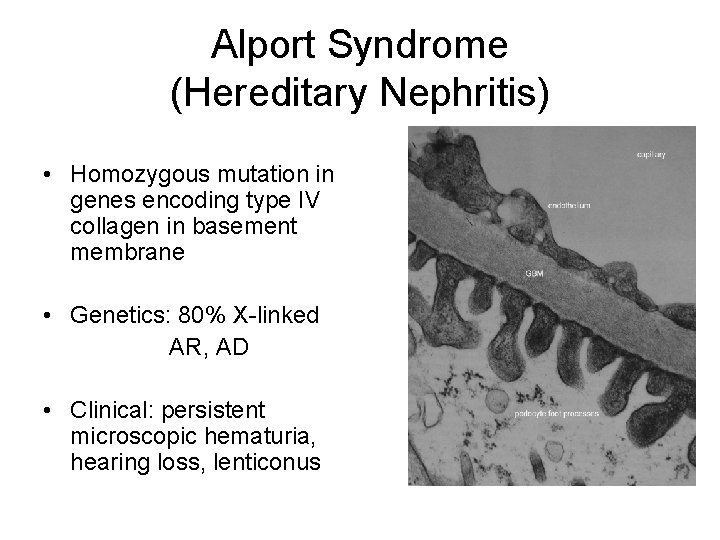
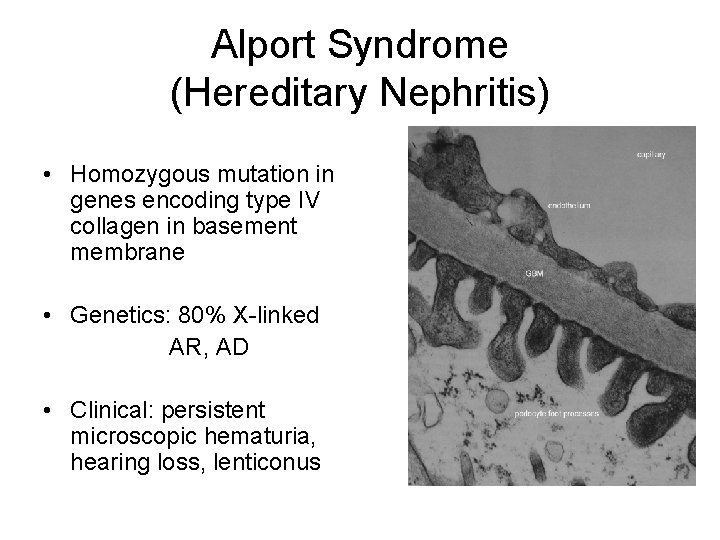
Alport Syndrome (Hereditary Nephritis) • Homozygous mutation in genes encoding type IV collagen in basement membrane • Genetics: 80% X-linked AR, AD • Clinical: persistent microscopic hematuria, hearing loss, lenticonus
Benign familial hematuria (thin basment membrane nephropathy) • • • Autosomal dominant Hetrozygous mutation in type IV collagen Microscopic hematuria Screen the parents’ urine Benign course
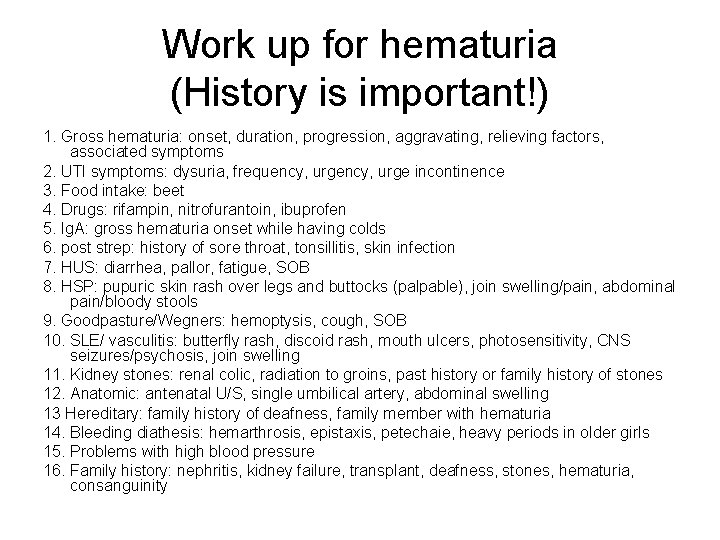
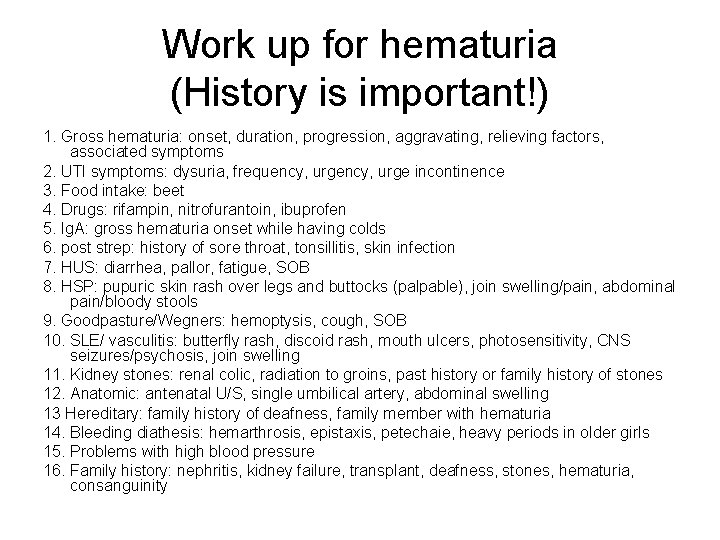
Work up for hematuria (History is important!) 1. Gross hematuria: onset, duration, progression, aggravating, relieving factors, associated symptoms 2. UTI symptoms: dysuria, frequency, urge incontinence 3. Food intake: beet 4. Drugs: rifampin, nitrofurantoin, ibuprofen 5. Ig. A: gross hematuria onset while having colds 6. post strep: history of sore throat, tonsillitis, skin infection 7. HUS: diarrhea, pallor, fatigue, SOB 8. HSP: pupuric skin rash over legs and buttocks (palpable), join swelling/pain, abdominal pain/bloody stools 9. Goodpasture/Wegners: hemoptysis, cough, SOB 10. SLE/ vasculitis: butterfly rash, discoid rash, mouth ulcers, photosensitivity, CNS seizures/psychosis, join swelling 11. Kidney stones: renal colic, radiation to groins, past history or family history of stones 12. Anatomic: antenatal U/S, single umbilical artery, abdominal swelling 13 Hereditary: family history of deafness, family member with hematuria 14. Bleeding diathesis: hemarthrosis, epistaxis, petechaie, heavy periods in older girls 15. Problems with high blood pressure 16. Family history: nephritis, kidney failure, transplant, deafness, stones, hematuria, consanguinity
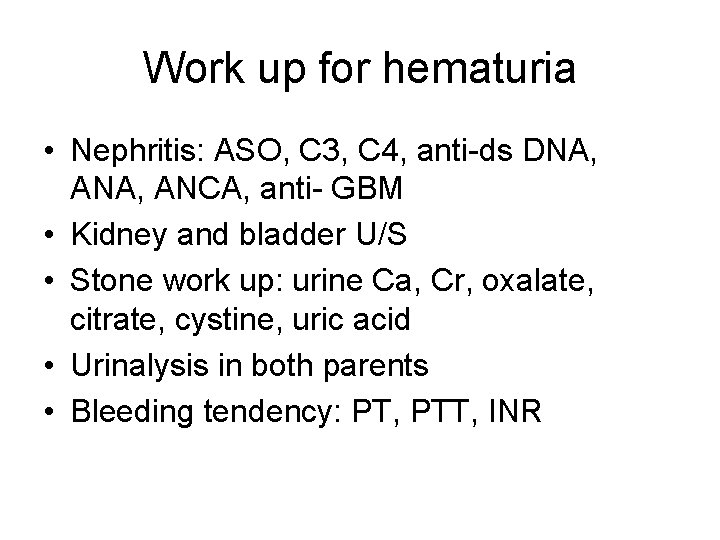
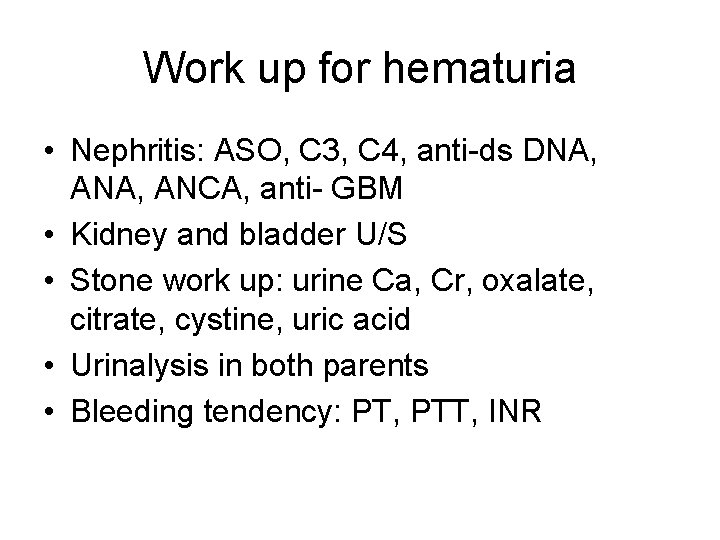
Work up for hematuria • Nephritis: ASO, C 3, C 4, anti-ds DNA, ANCA, anti- GBM • Kidney and bladder U/S • Stone work up: urine Ca, Cr, oxalate, citrate, cystine, uric acid • Urinalysis in both parents • Bleeding tendency: PT, PTT, INR
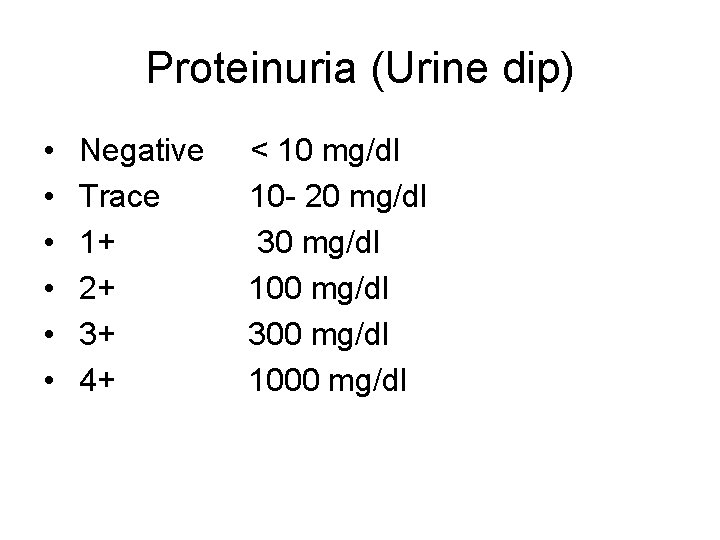
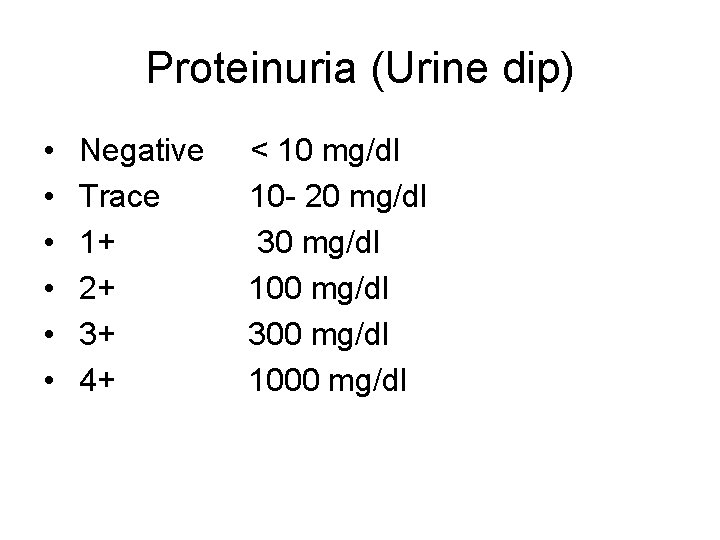
Proteinuria (Urine dip) • • • Negative Trace 1+ 2+ 3+ 4+ < 10 mg/dl 10 - 20 mg/dl 30 mg/dl 100 mg/dl 300 mg/dl 1000 mg/dl
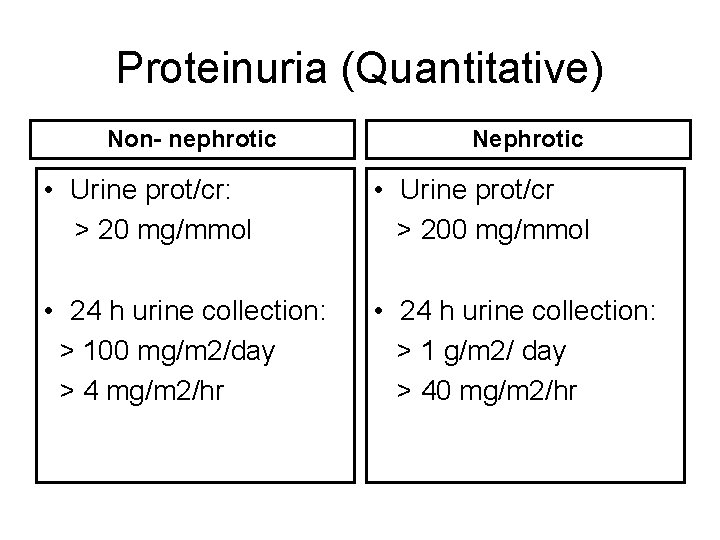
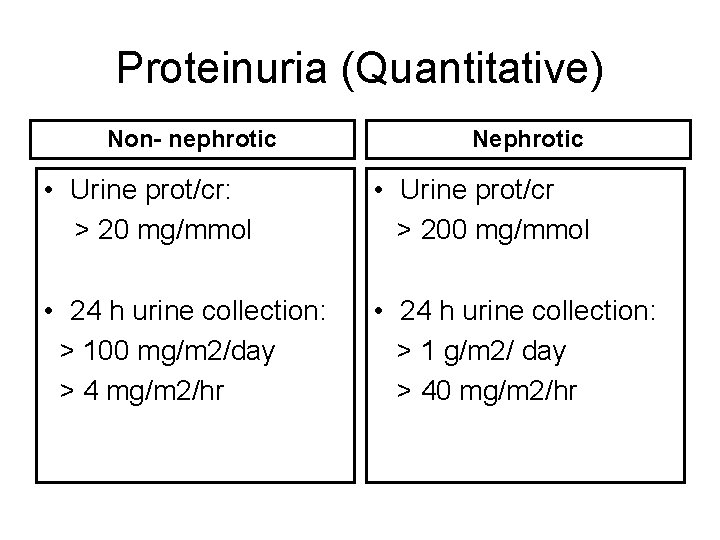
Proteinuria (Quantitative) Non- nephrotic Nephrotic • Urine prot/cr: > 20 mg/mmol • Urine prot/cr > 200 mg/mmol • 24 h urine collection: > 100 mg/m 2/day > 4 mg/m 2/hr • 24 h urine collection: > 1 g/m 2/ day > 40 mg/m 2/hr
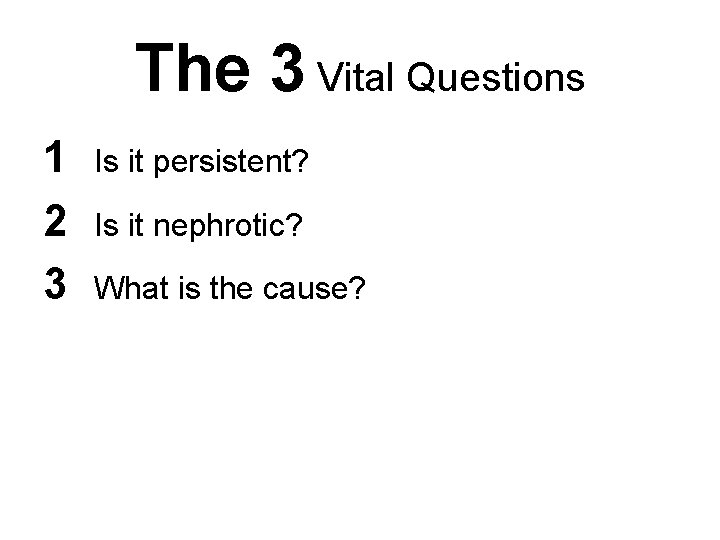
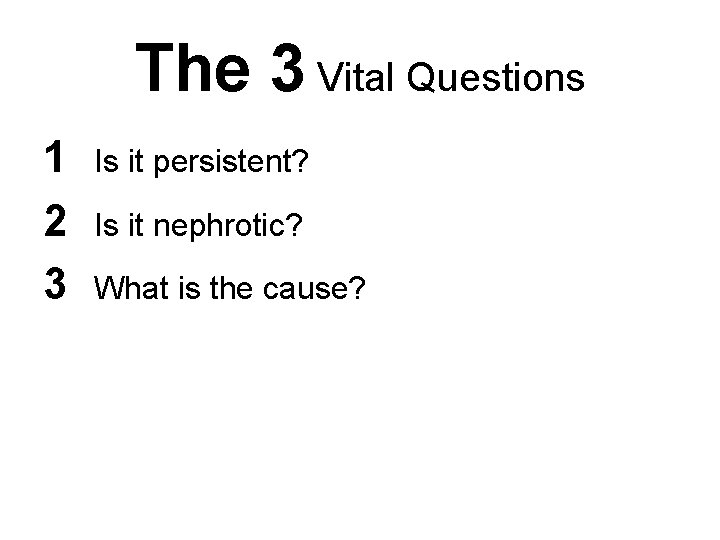
The 3 Vital Questions 1 2 3 Is it persistent? Is it nephrotic? What is the cause?
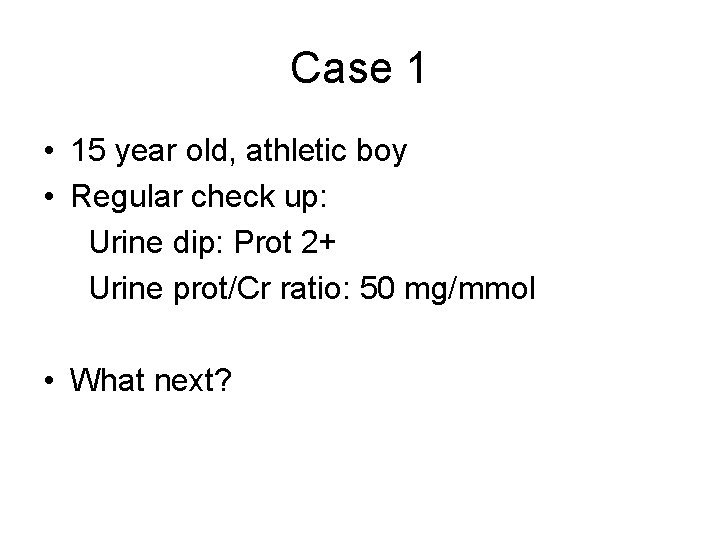
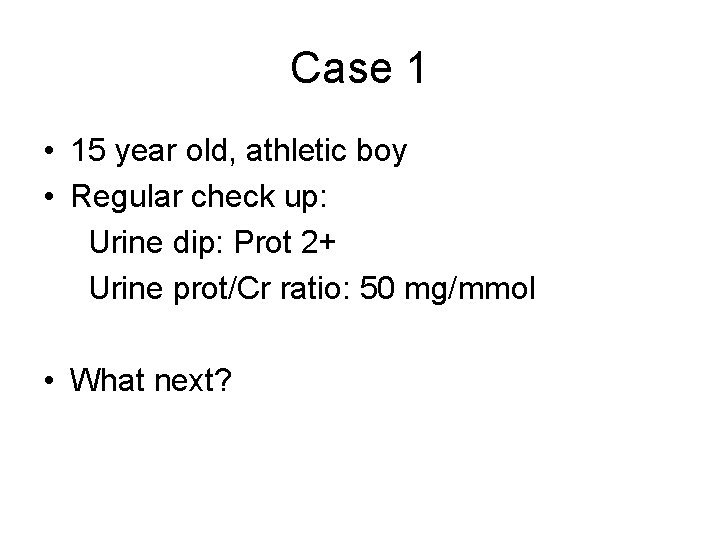
Case 1 • 15 year old, athletic boy • Regular check up: Urine dip: Prot 2+ Urine prot/Cr ratio: 50 mg/mmol • What next?
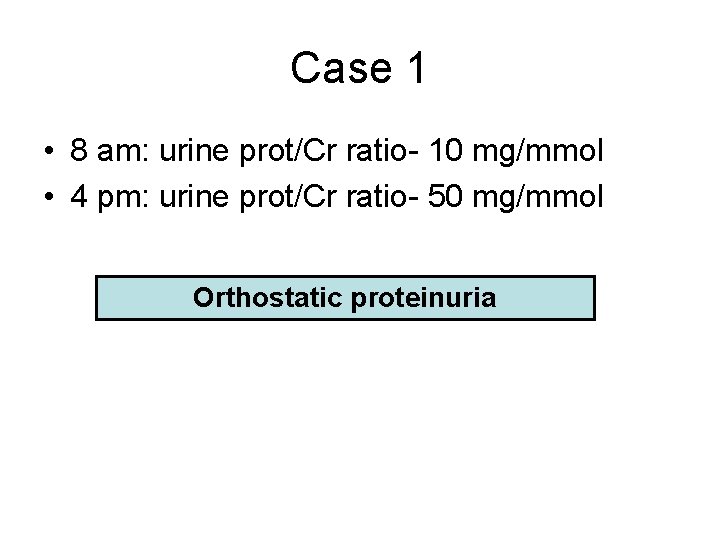
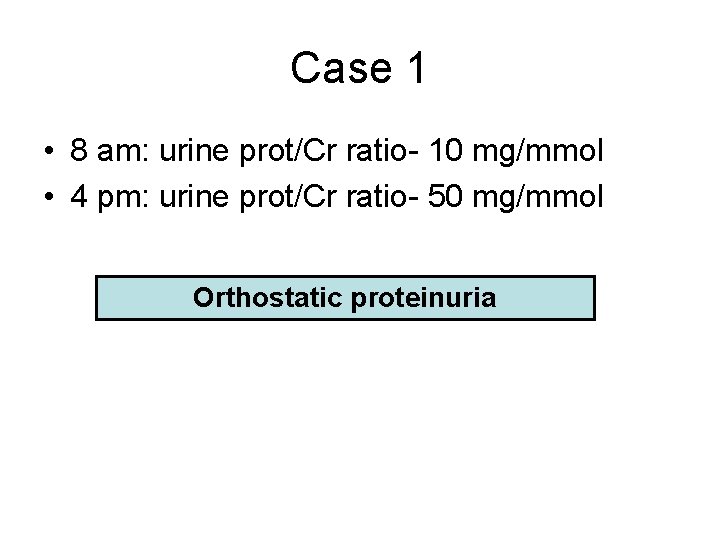
Case 1 • 8 am: urine prot/Cr ratio- 10 mg/mmol • 4 pm: urine prot/Cr ratio- 50 mg/mmol Orthostatic proteinuria
Non Persistant Proteinuria • • • Fever Strenuous exercise Cold exposure Epinephrine infusion Orthostatic
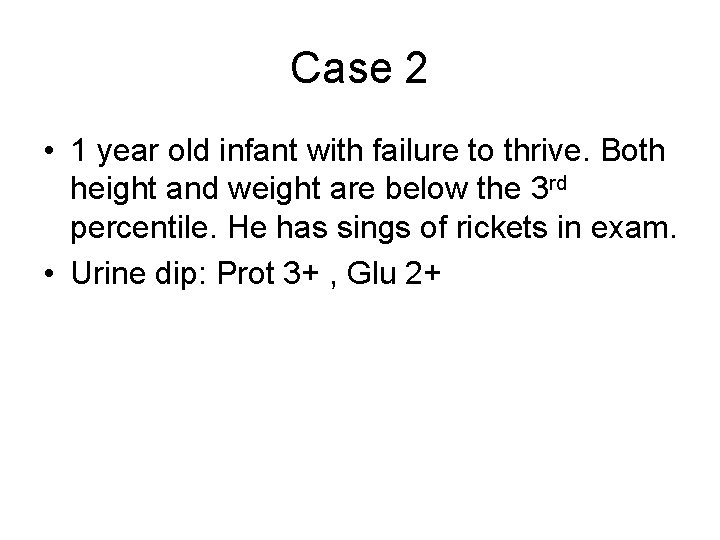
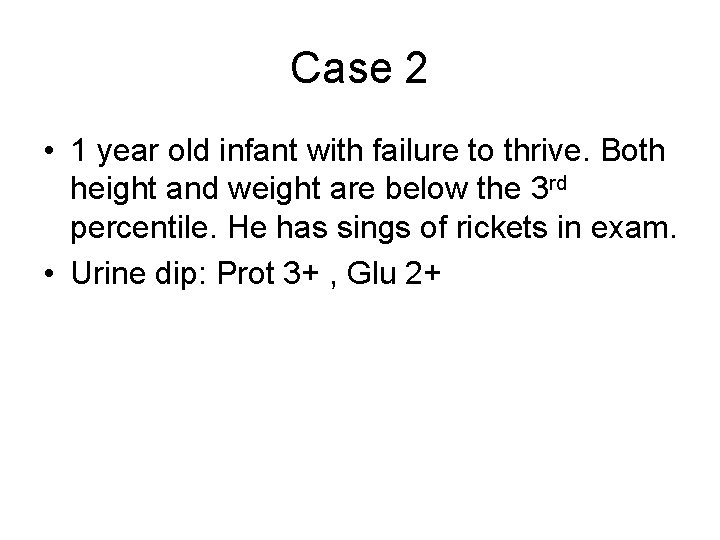
Case 2 • 1 year old infant with failure to thrive. Both height and weight are below the 3 rd percentile. He has sings of rickets in exam. • Urine dip: Prot 3+ , Glu 2+

Derakhshan Ali et al. Saudi J Kidney Dis Transpl. 2007 Oct-Dec; 18(4): 585 -9.
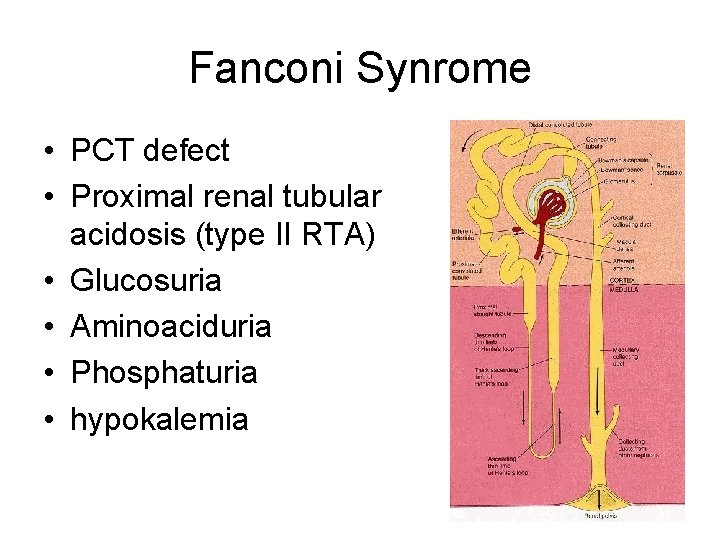
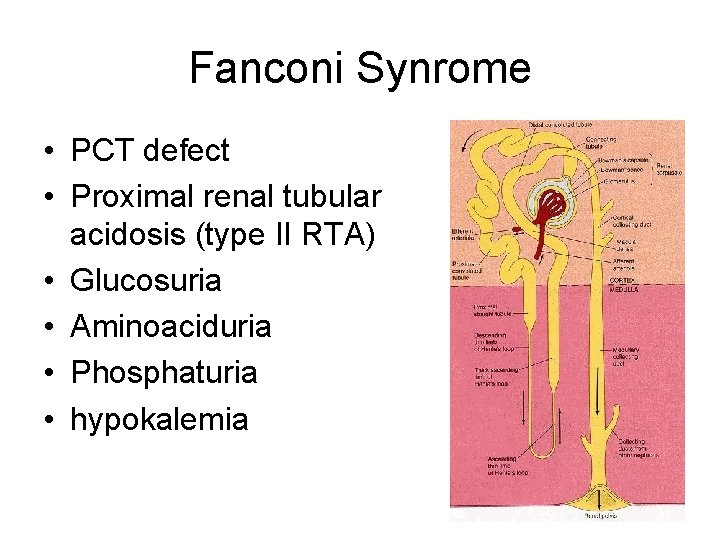
Fanconi Synrome • PCT defect • Proximal renal tubular acidosis (type II RTA) • Glucosuria • Aminoaciduria • Phosphaturia • hypokalemia
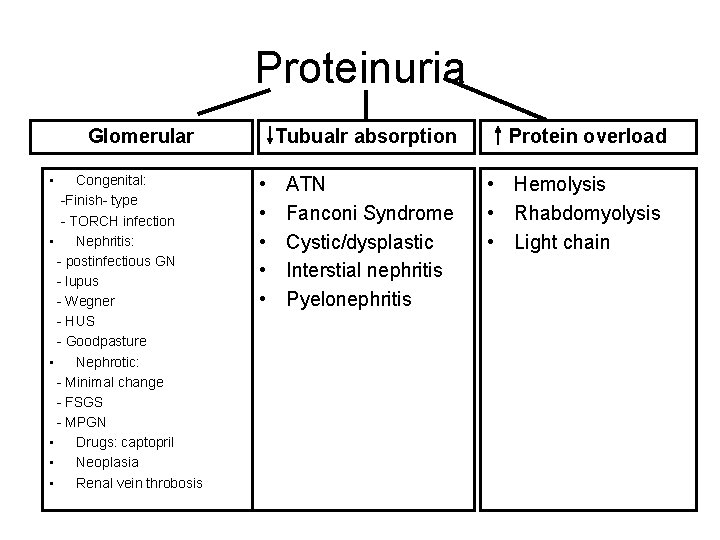
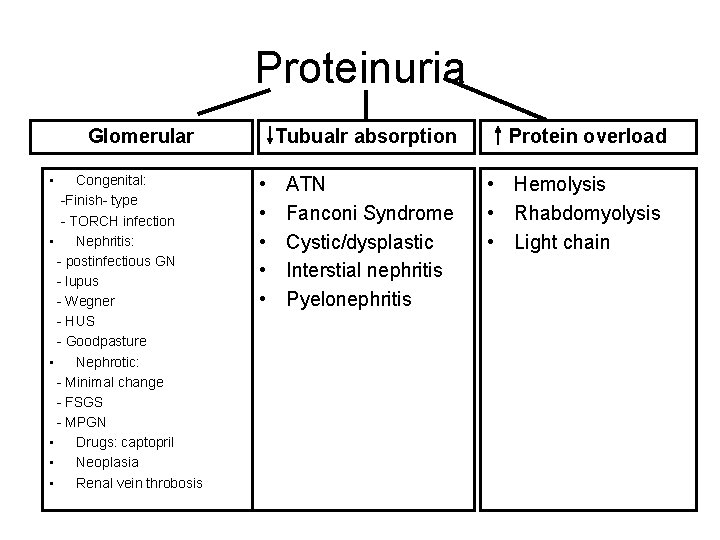
Proteinuria Glomerular • Congenital: -Finish- type - TORCH infection • Nephritis: - postinfectious GN - lupus - Wegner - HUS - Goodpasture • Nephrotic: - Minimal change - FSGS - MPGN • Drugs: captopril • Neoplasia • Renal vein throbosis • • • Tubualr absorption Protein overload ATN Fanconi Syndrome Cystic/dysplastic Interstial nephritis Pyelonephritis • Hemolysis • Rhabdomyolysis • Light chain

Proteinuria Glomerular • Congenital: -Finish- type - TORCH infection • Nephritis: - postinfectious GN - lupus - Wegner - HUS - Goodpasture • Nephrotic: - Minimal change - FSGS - MPGN • Drugs: captopril • Neoplasia • Renal vein throbosis • • • Tubualr absorption Protein overload ATN Fanconi Syndrome Cystic/dysplastic Interstial nephritis Pyelonephritis • Hemolysis • Rhabdomyolysis • Light chain Urine electrophoresis: • Glomerular: albumin • Tubular: other proteins. .
Case 3 • 5 year old boy, presenting with puffy eyes, enlarged tummy, and feet swelling. • Exam: normal BP, ascites, pitting edema • Urine dip: Prot 4+ • What’s the next step?
Case 3 • Urine prot/cr 1500 mg/mmol • Serum albumin 15 g/l • High cholesterol
Nephrotic Syndrome • • Urine Prot/Cr > 200 mg/mmol Serum albumin < 25 g/l Edema Hyperlipedemia
Nephrotic Syndrome • • • Minimal change disease Focal segmental glomerulosclerosis Membranoproliferative Membranous GN Infection: HIV, hepatits, syphilis Lupus, Ig A, HSP, post strep
Initial therapy • • Supportive: albumin 25% and lasix prn Salt restriction Fluid restriction while nephrotic Prednisone 60 mg/m 2/day for 6 weeks followed by 40 mg/m 2/day for 6 weeks then wean. .
Indications for biopsy • Steroid resistant: fail to enter remission after 8 weeks of therapy • Steroid dependent: intially enter remission, but develping relapse while on therapy, or within 2 weeks of steroid discontinuration • • Hematuria Increased Cr (when intravasculary repleted) Low complement Positive lupus serology
 Ratio
Ratio Proteinuria overflow
Proteinuria overflow Reabsorbcia
Reabsorbcia Prerenal proteinuria
Prerenal proteinuria Proteinuria
Proteinuria Proteinuria
Proteinuria Hemoglobinuria vs hematuria
Hemoglobinuria vs hematuria Macroscopic hematuria causes
Macroscopic hematuria causes Fountain valley hematuria
Fountain valley hematuria Eritrocitos isomorficos
Eritrocitos isomorficos Abdullah alsalloum
Abdullah alsalloum Hematuria
Hematuria Hematuria causes
Hematuria causes Anuria disuria poliuria oliguria hematuria
Anuria disuria poliuria oliguria hematuria Hemoglucosa
Hemoglucosa Oxibutinina dosis
Oxibutinina dosis Hematuria
Hematuria Differentiate between virtual circuit and datagram network
Differentiate between virtual circuit and datagram network Tony wagner's seven survival skills
Tony wagner's seven survival skills Theoretical models of counseling
Theoretical models of counseling Waterfall approach in international marketing
Waterfall approach in international marketing Approach approach conflict
Approach approach conflict Bandura's reciprocal determinism
Bandura's reciprocal determinism Approach research meaning
Approach research meaning Traditional approach vs object oriented approach
Traditional approach vs object oriented approach Ron rivest, adi shamir, and leonard adleman
Ron rivest, adi shamir, and leonard adleman Adı soyadı
Adı soyadı Baskoro adi pratomo
Baskoro adi pratomo Rahmulyo adi wibowo
Rahmulyo adi wibowo Ataturkun babasinin adi
Ataturkun babasinin adi Hışman çizik
Hışman çizik 10101010010
10101010010 Adi bin hatim
Adi bin hatim Aldehit kapalı formülü
Aldehit kapalı formülü Gemi dümen çeşitleri
Gemi dümen çeşitleri Silisyum tetraflorür
Silisyum tetraflorür Cumhuriyetten önceki devletimizin adı neydi
Cumhuriyetten önceki devletimizin adı neydi Cumhuriyet ilan edilmeden önce devletimizin adı neydi
Cumhuriyet ilan edilmeden önce devletimizin adı neydi Cumhuriyetten önceki devletimizin adı neydi
Cumhuriyetten önceki devletimizin adı neydi At&t adi with managed router
At&t adi with managed router Cal2 bileşiğinin adı
Cal2 bileşiğinin adı Hızınız 110 yavaş aq
Hızınız 110 yavaş aq Eskiden devletimizin adı neydi
Eskiden devletimizin adı neydi Rsul
Rsul Adi load data
Adi load data çapraz köprü döngüsü
çapraz köprü döngüsü Tuzlu topraklar diğer adı
Tuzlu topraklar diğer adı Kelenjar littre
Kelenjar littre Teleskobun optik parçalarını bulunduran yapıdır
Teleskobun optik parçalarını bulunduran yapıdır Parienteral
Parienteral Adi karışım
Adi karışım Kəsr üstlü qüvvət
Kəsr üstlü qüvvət Peygamberimizin aile büyükleri
Peygamberimizin aile büyükleri