Anticoagulation in Stroke Sanjeeva Reddy Onteddu Vascular Neurology
- Slides: 48
Anticoagulation in Stroke. Sanjeeva Reddy Onteddu. Vascular Neurology.
Disclosures. § Have a 3 year old. § We both worked on it. § No financial relations.
Objectives.
Objectives. § Who should be anticoagulated § When should be anticoagulated § What should be used to Anticoagulate. § Ultimate goal …. Will be revealed at the end
Ischemic Stroke
Who
All ischemic stroke patients. § 20 -30 years ago § MGH: § Acute stroke AC vs Antiplatelet study.
Easy ones first Need Neurology clearance § Has LV thrombus, No neurological deficits: § yes § Has A fib, no neurological deficits: § yes
Other thrombotic states § DVT/PE § Known hypercoagulable states.
Cardiac Causes § PFO- § No § PFO with large ASA – § may be, no large trials, case series and reports. § LV thrombus – § Yes but when § Mechanical Valve – § Yes and how soonish.
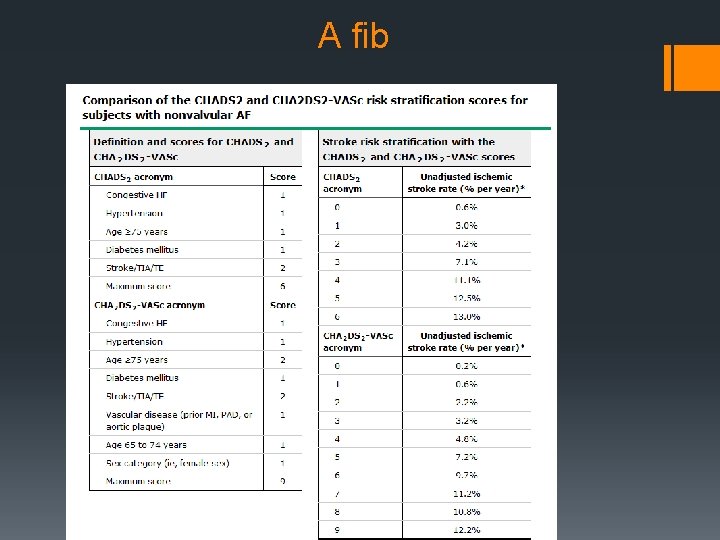
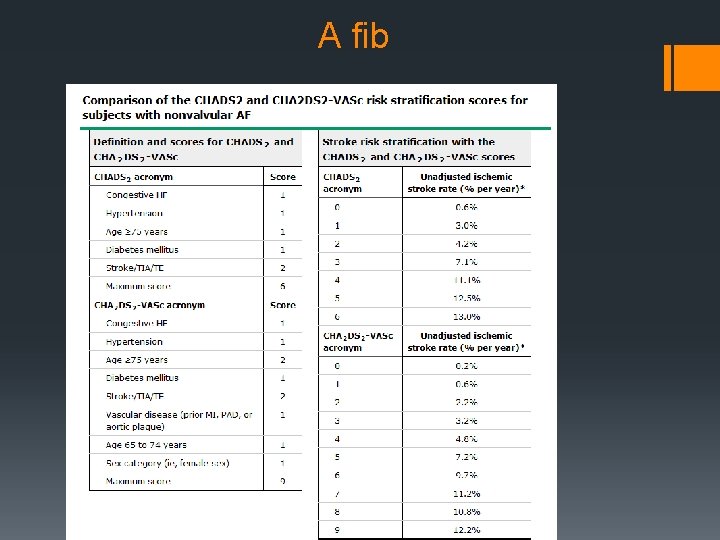
A fib
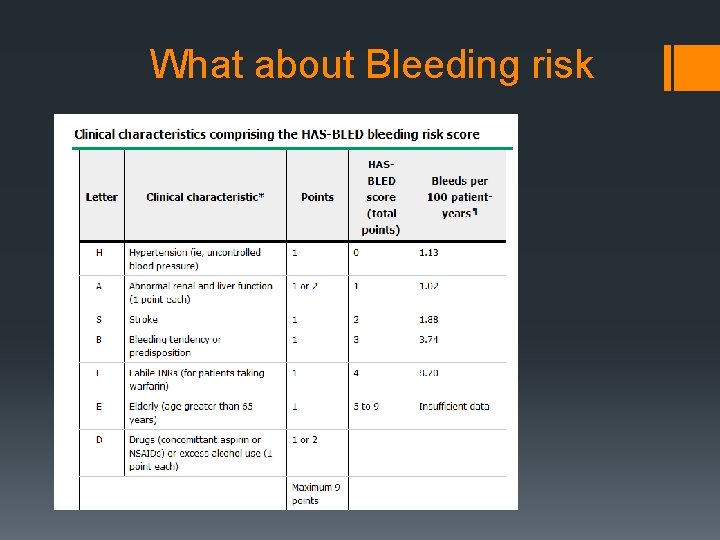
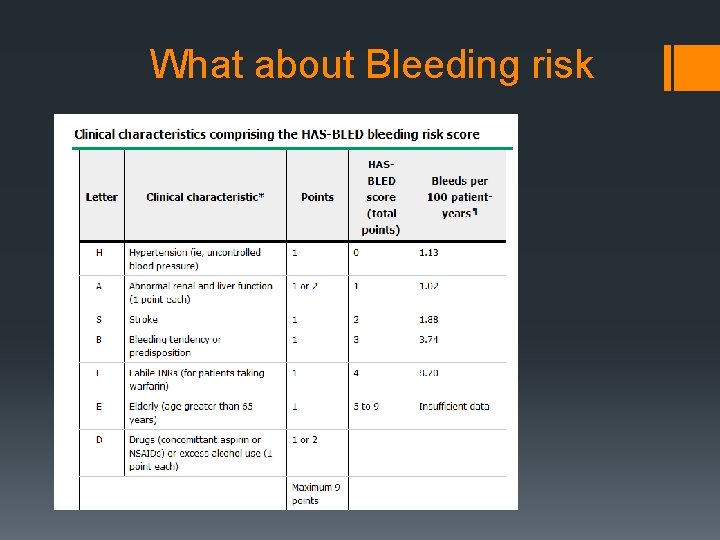
What about Bleeding risk
CHA 2 DS 2 -VASc Vs HAS-BLED § Other Bleeding Scores § ATRIA § HEMORR 2 HAGES § Use these to Identify factors which increase risk of bleeding and treat them.
Other etiologies of ischemic Stroke § Lacunar – No § Stuttering Lacunar – give it a try. § Carotid Atherosclerosis – no § Carotid Dissection – § May be § Cryptogenic Strokes: § Not yet
Cryptogenic strokes § WARSS: No difference in cryptogenic pts with Coumadin vs ASA. § RESPECT-ESUS Study: We are Enrolling please send patients. § Second Cryptogenic strokes: Discuss with patients I usually do. § CLINICAL PRACTICE. Cryptogenic Stroke. Saver JL, N Engl J Med. 2016 May; 374(21): 2065 -74. § Some papers suggest Use CHA 2 DS 2 -VASc score even if A fib not detected.
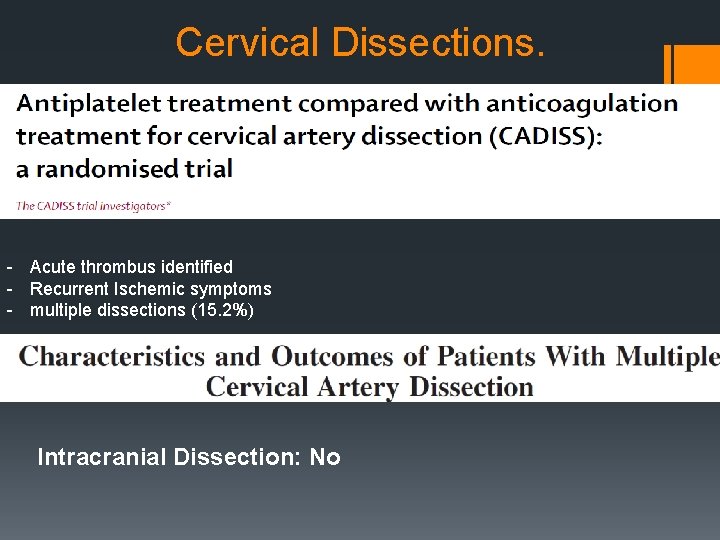
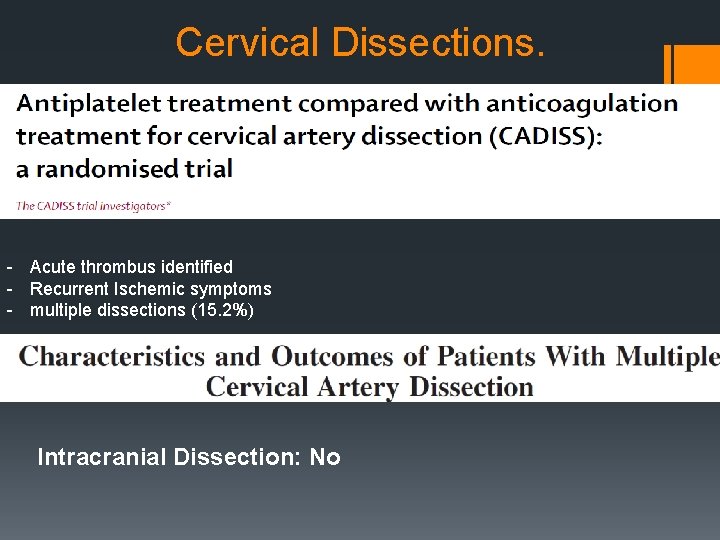
Cervical Dissections. - Acute thrombus identified - Recurrent Ischemic symptoms - multiple dissections (15. 2%) Intracranial Dissection: No
Cerebral Venous Thrombosis § Without ICH: § Yes § With ICH: § Yesissh
• Meta anyalsis: Recurrent CVT higher in patient who were taking Coumadin, no benefit. • • No Large Randomized controlled trials, Few studies non statistical significance. Few Question the need for AC. Expert Opinion/Guidelines 2011 AHA/ASA is to AC.
Complex patients
ICH patients § Wait…. . What…… § Not All § Only who are high risk of Thromboembolic events. § Patients with A fib, Hypercoag states Etc.
Hemorrhagic Stroke § Any Intracranial hemorrhage – Not acutely § ICH with A fib – May be things to consider § Etiology of ICH- Hypertensive vs others, § using AC at the time of incident ICH § Supra therapeutic/not supra therapeutic with Coumadin § Using NOAC’s
ICH Recurrence § More risk of Recurrence if § Uncontrolled hypertension § Lobar location of initial ICH § Ongoing anticoagulation § Greater number of micro bleeds on MRI § Recurrence of ICH after resumption of anticoagulation with VK antagonists, CHIRONE Study. § 7. 5% Recurrent Risk with median ICH recurrence time 16. 5 months.
Mechanical Valves and ICH § ICH with Mechanical Valve: Yes When § Safety vs Stroke
Mechanical Valves § Frequency of thromboembolic events: § 0. 7 to 1 percent per patient per year with Coumadin. § 2. 2 percent per patient per year with ASA § 4 percent with no anticoagulation. Mitral valve prostheses twice the risk compared with those aortic valve prostheses. valve thrombosis is 1. 8% a year Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation. 1994; 89(2): 635.
Cerebral Amyloid Angiopathy. § Can we AC patients with CAA: § NO § With Coumadin 7 -10 fold increased risk. § What about t. PA: no information might be bliss … § If more than 5 micro hemorrhages risk of Symptomatic ICH is high, should discuss with family. § Antiplatelet: Risk Vs benefit.
Stroke clearance for cardiac surgeries § Aortic dissection § Risk Vs Benefit. § Things to consider § Size of stroke § Need for surgery § Time since stroke § Presence of ICH/Petichial hemorrhage
§ Endocarditis with Septic Embolic/Mycotic Aneurysms. § Need Vessel imaging if mycotic aneurysm suspected. § t. PA with possible septic Emboli: § Contraindication
Afib + Falls ? AC § Need to fall 295 times a year for fall-related subdural hemorrhages to outweigh benefits of stroke prevention. § Choosing Antithrombotic Therapy for Elderly Patients With Atrial Fibrillation Who Are at Risk for Falls, Arch Intern Med. 1999; 159(7): 677685. doi: 10. 1001/archinte. 159. 7. 677
When to start it.
A fib and stroke § Treatment started with in 48 hrs of stroke § more bleeds § Non significant decreased ischemic strokes § Efficacy and safety of anticoagulant treatment in acute cardioembolic stroke: a meta-analysis of randomized controlled trials. AUPaciaroni M, Stroke. 2007; 38(2): 423.
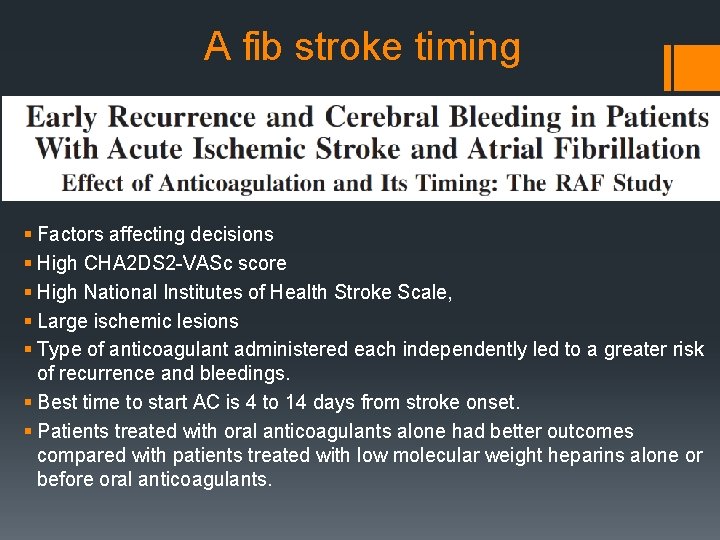
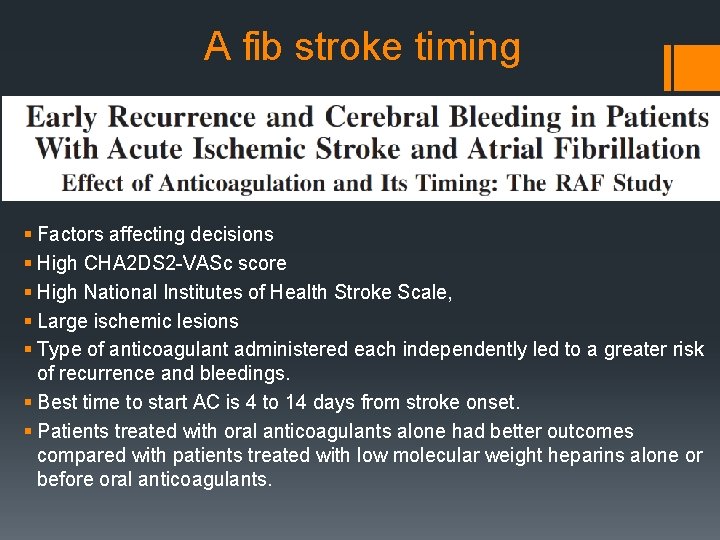
A fib stroke timing § Factors affecting decisions § High CHA 2 DS 2 -VASc score § High National Institutes of Health Stroke Scale, § Large ischemic lesions § Type of anticoagulant administered each independently led to a greater risk of recurrence and bleedings. § Best time to start AC is 4 to 14 days from stroke onset. § Patients treated with oral anticoagulants alone had better outcomes compared with patients treated with low molecular weight heparins alone or before oral anticoagulants.
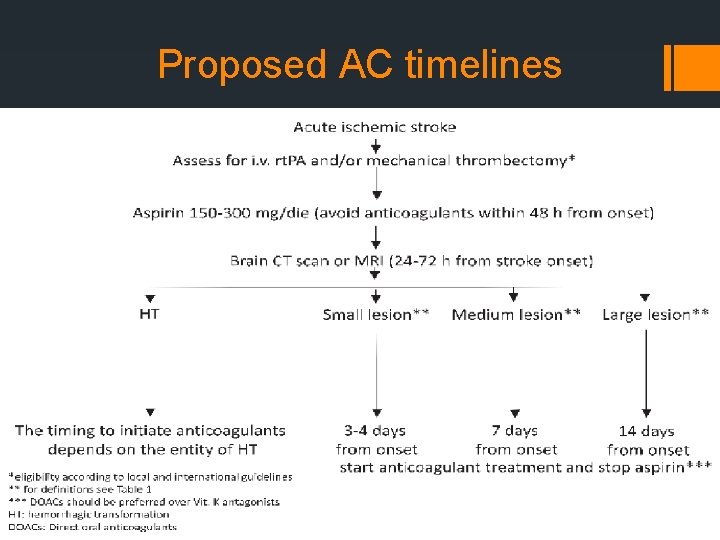
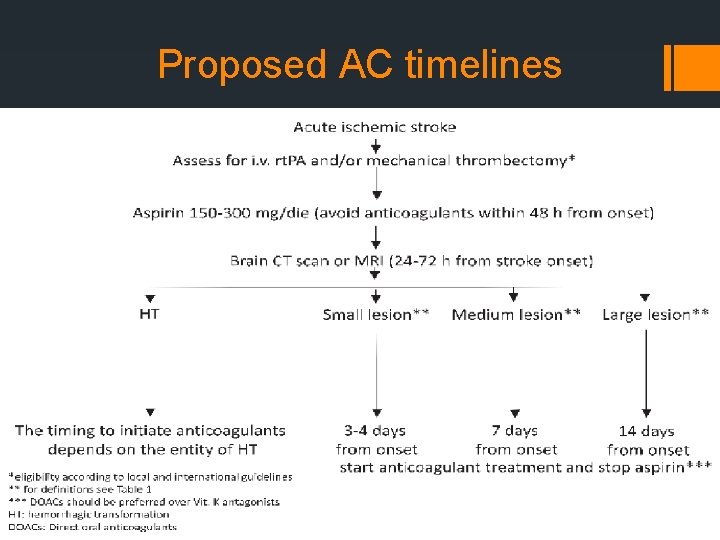
Proposed AC timelines
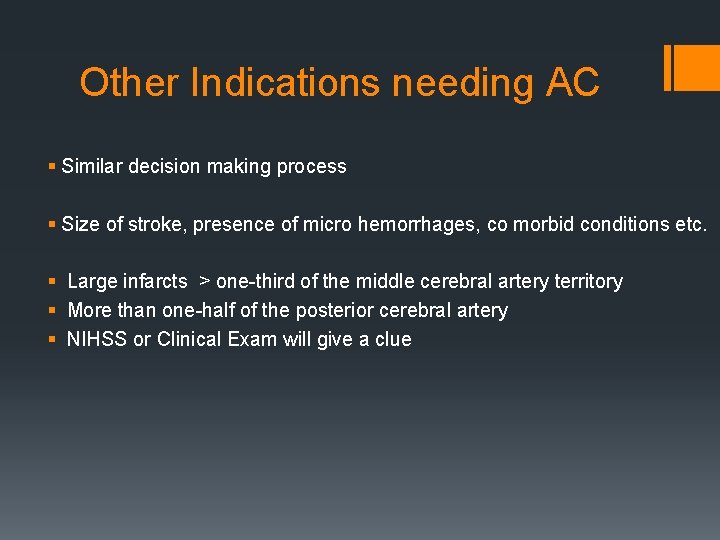
Other Indications needing AC § Similar decision making process § Size of stroke, presence of micro hemorrhages, co morbid conditions etc. § Large infarcts > one-third of the middle cerebral artery territory § More than one-half of the posterior cerebral artery § NIHSS or Clinical Exam will give a clue
ICH patients needing AC § Still Not Sure if we need to do it?
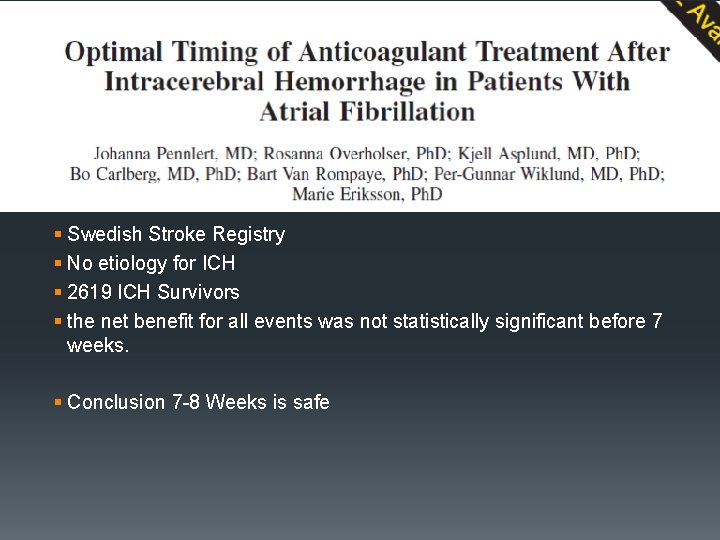
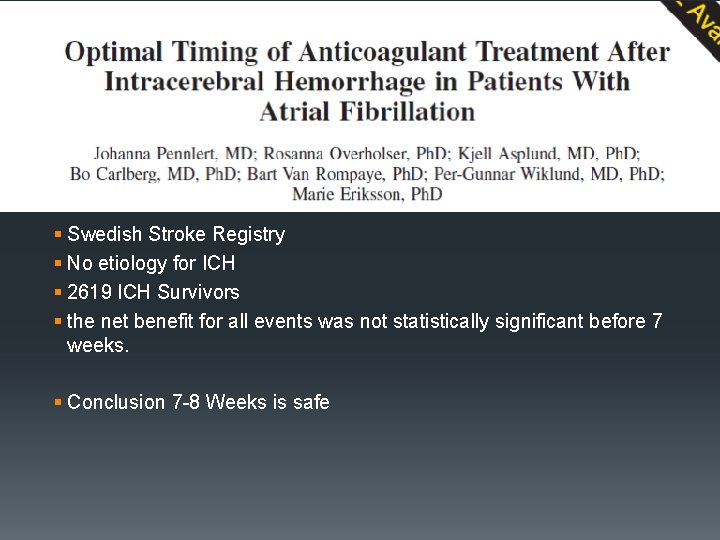
§ Swedish Stroke Registry § No etiology for ICH § 2619 ICH Survivors § the net benefit for all events was not statistically significant before 7 weeks. § Conclusion 7 -8 Weeks is safe
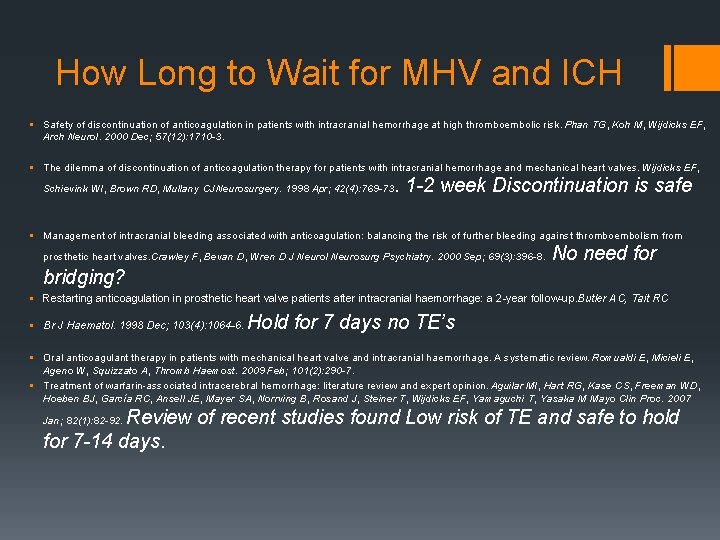
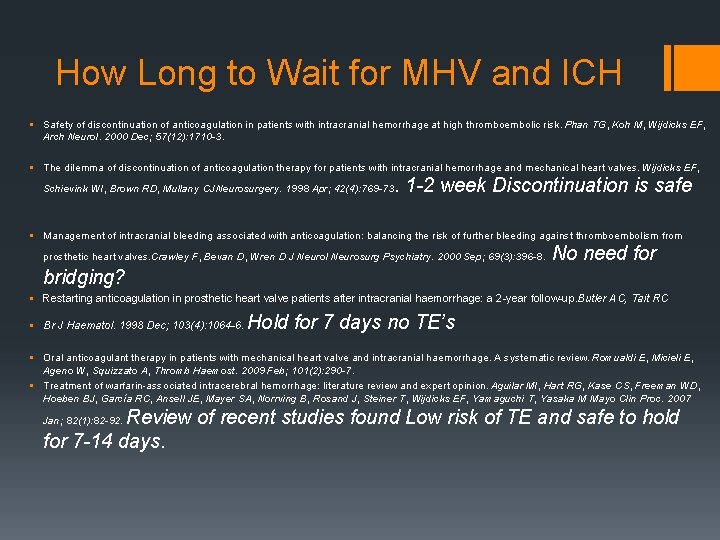
How Long to Wait for MHV and ICH § Safety of discontinuation of anticoagulation in patients with intracranial hemorrhage at high thromboembolic risk. Phan TG, Koh M, Wijdicks EF, Arch Neurol. 2000 Dec; 57(12): 1710 -3. § The dilemma of discontinuation of anticoagulation therapy for patients with intracranial hemorrhage and mechanical heart valves. Wijdicks EF, Schievink WI, Brown RD, Mullany CJNeurosurgery. 1998 Apr; 42(4): 769 -73 . 1 -2 week Discontinuation is safe § Management of intracranial bleeding associated with anticoagulation: balancing the risk of further bleeding against thromboembolism from prosthetic heart valves. Crawley F, Bevan D, Wren D J Neurol Neurosurg Psychiatry. 2000 Sep; 69(3): 396 -8. No need for bridging? § Restarting anticoagulation in prosthetic heart valve patients after intracranial haemorrhage: a 2 -year follow-up. Butler AC, Tait RC § Br J Haematol. 1998 Dec; 103(4): 1064 -6. Hold for 7 days no TE’s § Oral anticoagulant therapy in patients with mechanical heart valve and intracranial haemorrhage. A systematic review. Romualdi E, Micieli E, Ageno W, Squizzato A, Thromb Haemost. 2009 Feb; 101(2): 290 -7. § Treatment of warfarin-associated intracerebral hemorrhage: literature review and expert opinion. Aguilar MI, Hart RG, Kase CS, Freeman WD, Hoeben BJ, García RC, Ansell JE, Mayer SA, Norrving B, Rosand J, Steiner T, Wijdicks EF, Yamaguchi T, Yasaka M Mayo Clin Proc. 2007 Review of recent studies found Low risk of TE and safe to hold for 7 -14 days. Jan; 82(1): 82 -92.
What to Use § Bridge vs No Bridge § Warfarin vs NOAC § Which NOAC § Money matters
Bridge Vs no Bridge § Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation, N Engl J Med 2015; 373: 823 -833 August 27, 2015 DOI: 10. 1056/NEJMoa 1501035. § No benefit
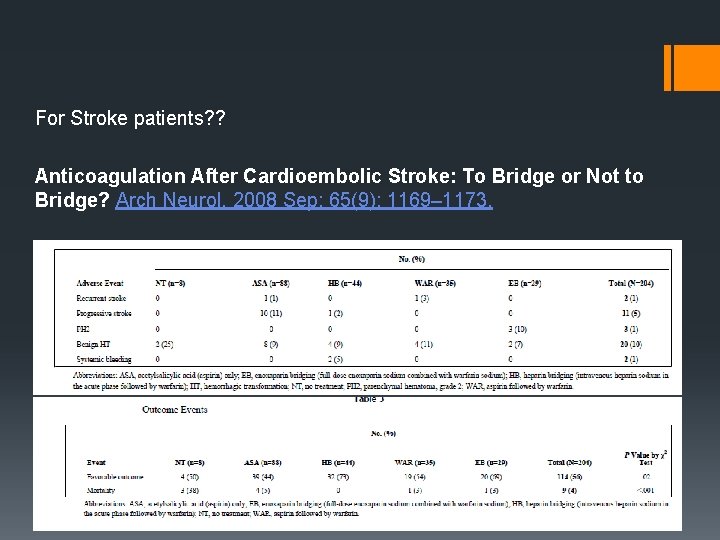
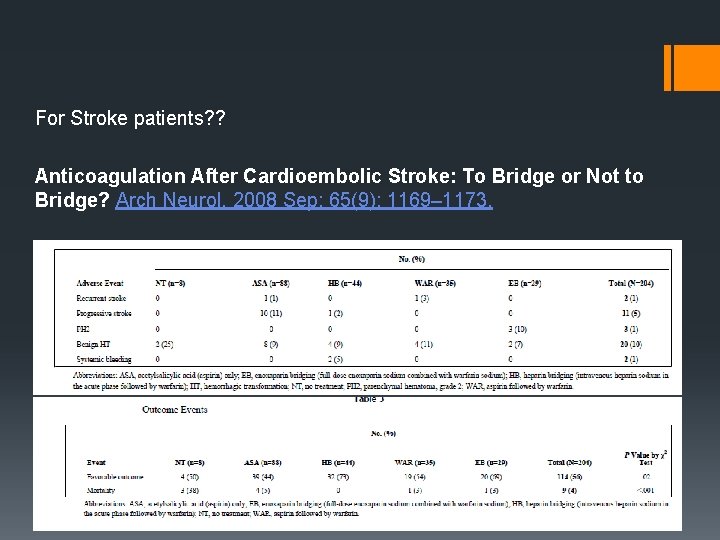
For Stroke patients? ? Anticoagulation After Cardioembolic Stroke: To Bridge or Not to Bridge? Arch Neurol. 2008 Sep; 65(9): 1169– 1173.
Who Needs Bridging § To consider § High Risk of Thrombo embolic events § Low risk of Hemorrhagic conversion or Hematoma Expansion. § Good Blood pressure Control § To avoid § Large ICH § High risk of bleeding, low platelets… § Renal failure…
Who Needs Bridging § Patients with LV thrombus. § Mechanical Valves? § Carotid Dissection with fresh thrombus, multiple recurrent strokes. § CVT: Sure
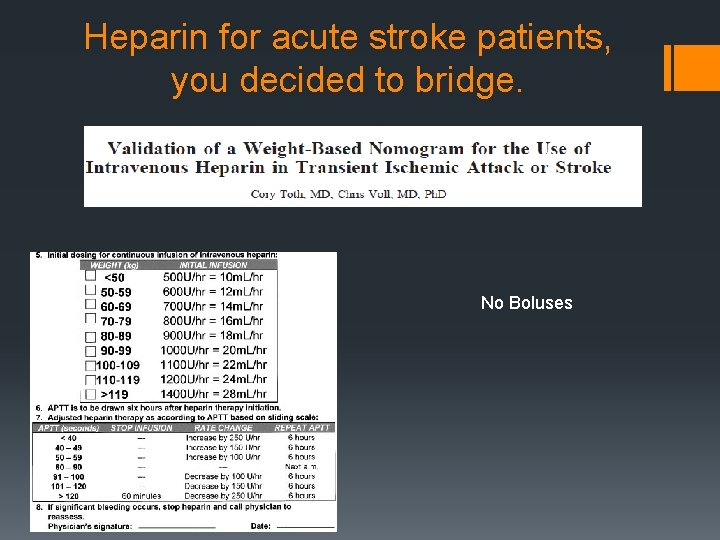
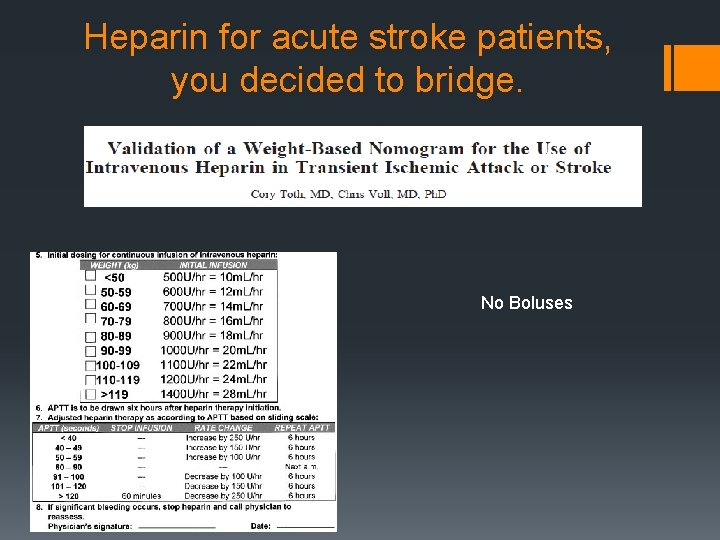
Heparin for acute stroke patients, you decided to bridge. No Boluses
Coumadin is Warfarin § BLEEDING OCCURS IN 2% TO 3% OF PATIENTS PER YEAR.
Still Coumadin § LV thrombus § APL § Cerebral venous Thrombosis § Mainly because they have not been studied § Mechanical Valve: Pradaxa worse than Coumadin, RE-ALIGN trial Others NOAC’s not studied.
For A fib Coumadin vs NOAC’s § All compared to Coumadin § No head – head comparisons. § Different rates of therapeutic INR’s § Recommendations now changing to NOAC’s as first line.
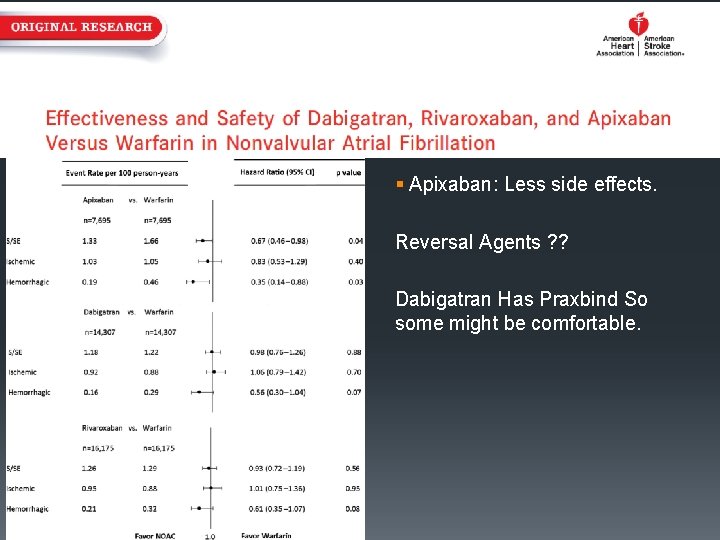
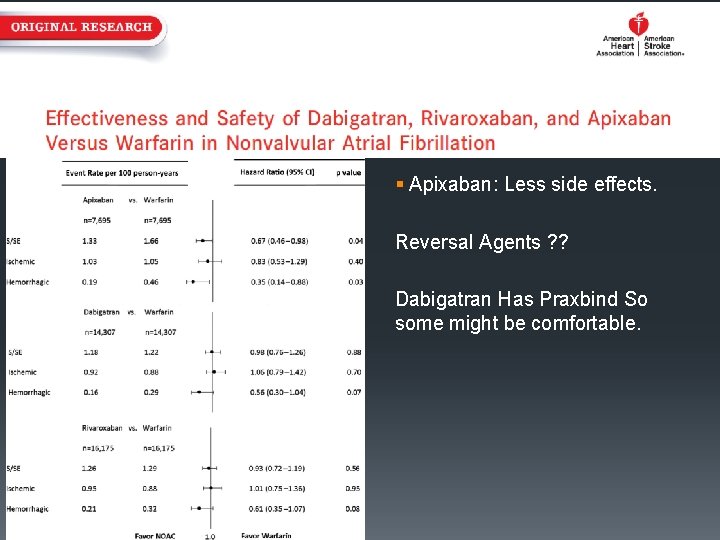
§ Apixaban: Less side effects. Reversal Agents ? ? Dabigatran Has Praxbind So some might be comfortable.
Questions
§ Anticoagulation and stroke. § Anticoagulants versus antiplatelet agents for acute ischaemic stroke. Berge E, Sandercock P 2014 § Anticoagulants for acute ischaemic stroke. Sandercock PA, 2015. § CAA and Anticoagulation § Warfarin-associated hemorrhage and cerebral amyloid angiopathy: a genetic and pathologic study. § Rosand J, Neurology. 2000; 55(7): 947. § How to AC § Validation of a weight-based nomogram for the use of intravenous heparin in transient ischemic attack or stroke. AUToth C, . 2002; 33(3): 670. § PFO References § Lamy C, Giannesini C, Zuber M, et al. Clinical and imaging findings in cryptogenic stroke patients with and without patent foramen ovale: the PFO-ASA Study. Atrial Septal Aneurysm. Stroke 2002; 33: 706. § Serena J, Marti-Fàbregas J, Santamarina E, et al. Recurrent stroke and massive right-to-left shunt: results from the prospective Spanish multicenter (CODICIA) study. Stroke 2008; 39: 3131. § Homma S, Sacco RL, Di Tullio MR, et al. Effect of medical treatment in stroke patients with patent foramen ovale: patent foramen ovale in Cryptogenic Stroke Study. Circulation 2002; 105: 2625. § Dissection Reference § Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial The CADISS trial investigators* § Characteristics and Outcomes of Patients With Multiple Cervical Artery Dissection § Yannick Béjot, MD, Ph. D on behalf of the CADISP Group
 Nonvascular plants reproduction
Nonvascular plants reproduction Nonvascular plants
Nonvascular plants Vascular and non vascular difference
Vascular and non vascular difference Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Anticoagulation
Anticoagulation Lahey anticoagulation clinic
Lahey anticoagulation clinic Anticoagulation
Anticoagulation Hospital medication chart
Hospital medication chart Triple therapy anticoagulation
Triple therapy anticoagulation Classification of antiarrhythmic drugs
Classification of antiarrhythmic drugs Heparin drip protocol
Heparin drip protocol Overlake senior health clinic
Overlake senior health clinic Emory clinic - school of medicine faculty
Emory clinic - school of medicine faculty Prof raj reddy
Prof raj reddy Ketan reddy
Ketan reddy Konda madhava reddy
Konda madhava reddy Bheemarjuna reddy tamma
Bheemarjuna reddy tamma Raj reddy inventions
Raj reddy inventions Dr dn reddy
Dr dn reddy Conduit metaphor meaning
Conduit metaphor meaning Swarith
Swarith I am woman helen reddy lyrics meaning
I am woman helen reddy lyrics meaning Jessica reddy x
Jessica reddy x Sahithya reddy periodontics
Sahithya reddy periodontics Joseph berger md neurology
Joseph berger md neurology Mary bridge neurology clinic
Mary bridge neurology clinic Nbme shelf percentiles 2021
Nbme shelf percentiles 2021 Midwest neurology
Midwest neurology Neurology near loomis
Neurology near loomis Department of neurology
Department of neurology Motor strength scale
Motor strength scale Midwest neurology
Midwest neurology Jung
Jung Duplex ultrasound vs doppler
Duplex ultrasound vs doppler Nlff neurology
Nlff neurology Neurology
Neurology Tufts anesthesia residency
Tufts anesthesia residency Ulster hospital neurology consultants
Ulster hospital neurology consultants Dr kirk kleinfeld
Dr kirk kleinfeld Erlanger neurology
Erlanger neurology Nheent
Nheent Nlff neuro
Nlff neuro Oregon neurology associates
Oregon neurology associates Difference between fine touch and crude touch
Difference between fine touch and crude touch Dr nin bajaj
Dr nin bajaj Pmg neurology
Pmg neurology Dr robert layzer
Dr robert layzer Neurology
Neurology Umass nurse residency program
Umass nurse residency program