Dual vs Triple Therapy in Patients Requiring PCI



- Slides: 21
Dual vs. Triple Therapy in Patients Requiring PCI and Oral Anticoagulation Dharam J. Kumbhani, MD, SM, MRCP, FACC, FAHA, FSCAI Section Chief, Interventional Cardiology Director, Cardiac Catheterization Laboratory, Clements University Hospital Associate Professor of Medicine UT Southwestern Medical Center, Dallas, TX
Disclosures Chair of upcoming ACC document on dual vs. triple therapy No industry conflicts
Case 70 yo male with history of: • Lung cancer secondary to smoking, treated with RUL lobectomy and XRT • COPD, mild to moderate • CKD III (creatinine 1. 3, e. GFR 56) • HTN • HPL • Chronic AF on apixaban 5 mg BID • EF 25% Presented to clinic after a recent admission for SOB and angina. No history of syncope. Had 3 admissions earlier in the year for heart failure exacerbation.
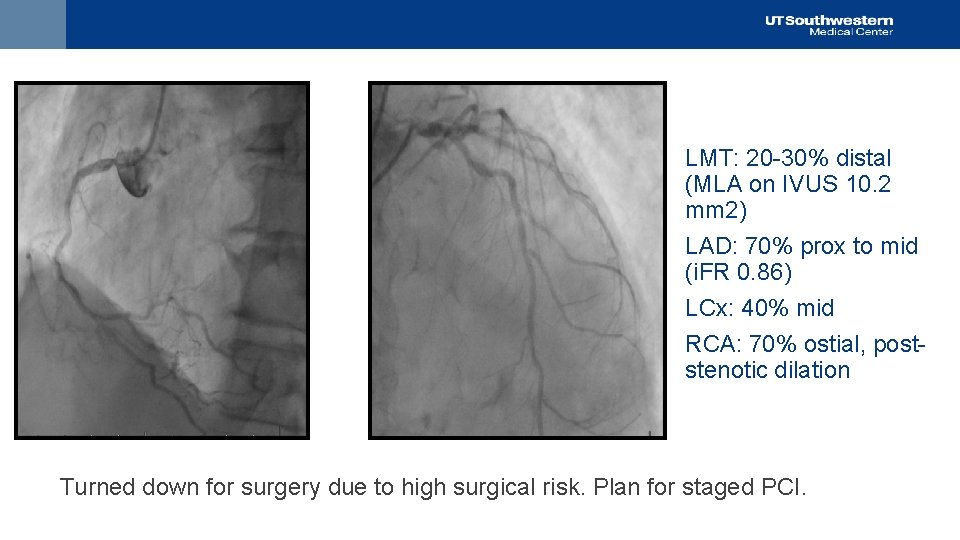
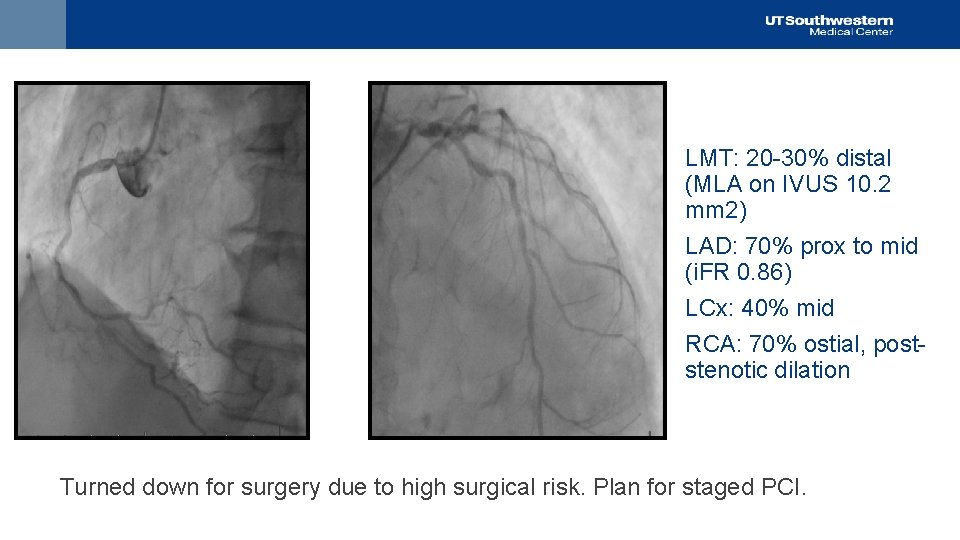
LMT: 20 -30% distal (MLA on IVUS 10. 2 mm 2) LAD: 70% prox to mid (i. FR 0. 86) LCx: 40% mid RCA: 70% ostial, poststenotic dilation Turned down for surgery due to high surgical risk. Plan for staged PCI.
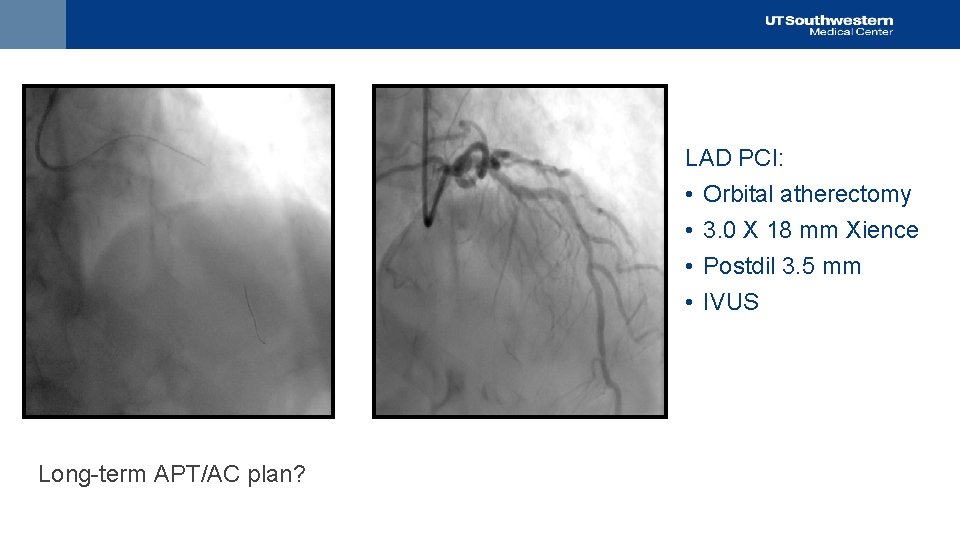
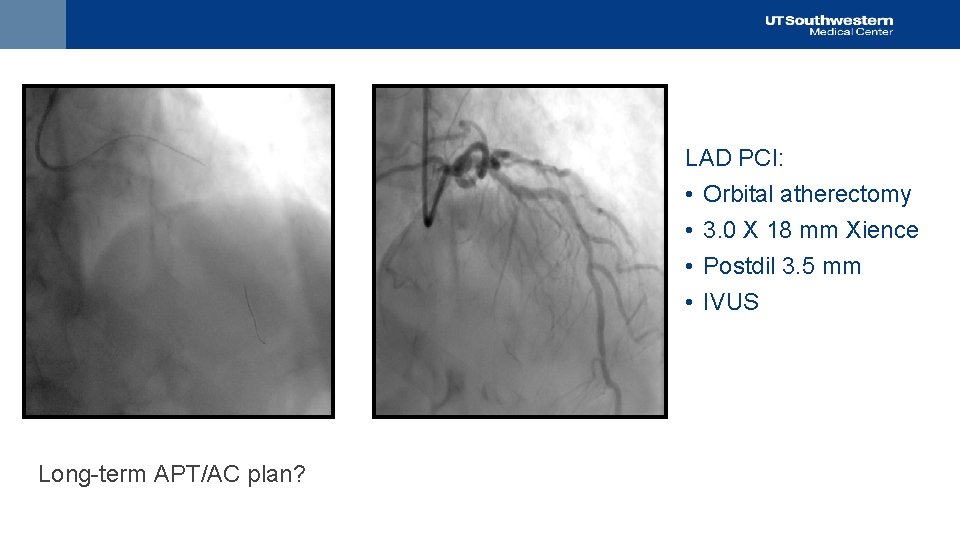
LAD PCI: • Orbital atherectomy • 3. 0 X 18 mm Xience • Postdil 3. 5 mm • IVUS Long-term APT/AC plan?
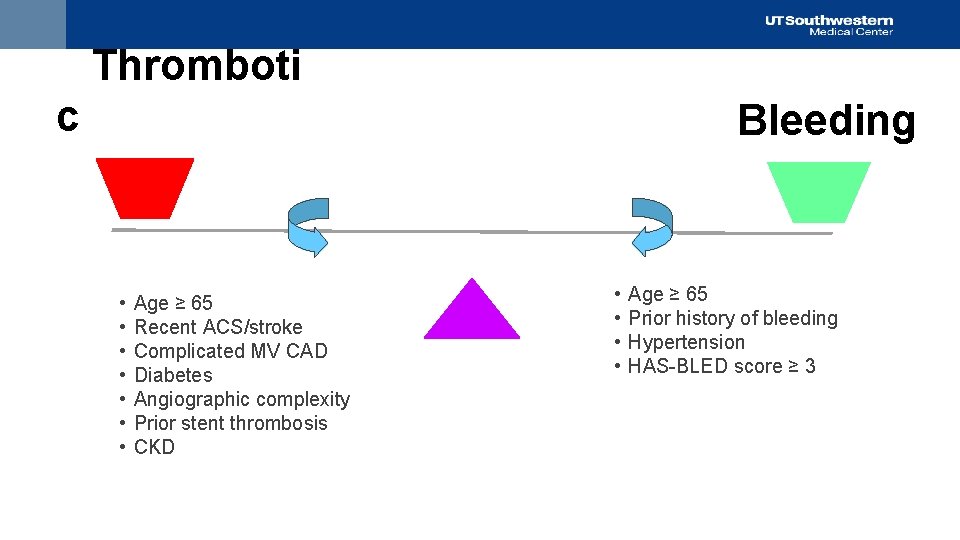
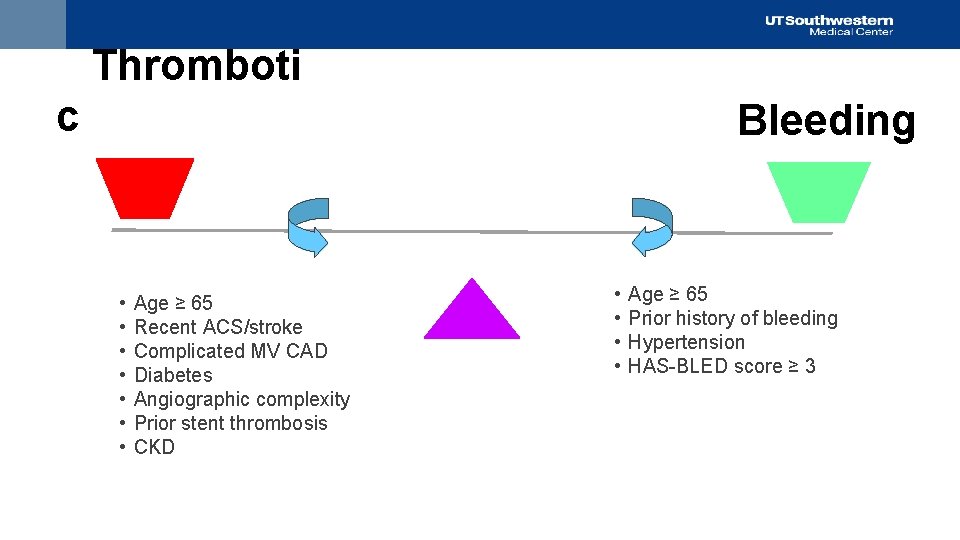
Thromboti c • • Age ≥ 65 Recent ACS/stroke Complicated MV CAD Diabetes Angiographic complexity Prior stent thrombosis CKD Bleeding • • Age ≥ 65 Prior history of bleeding Hypertension HAS-BLED score ≥ 3
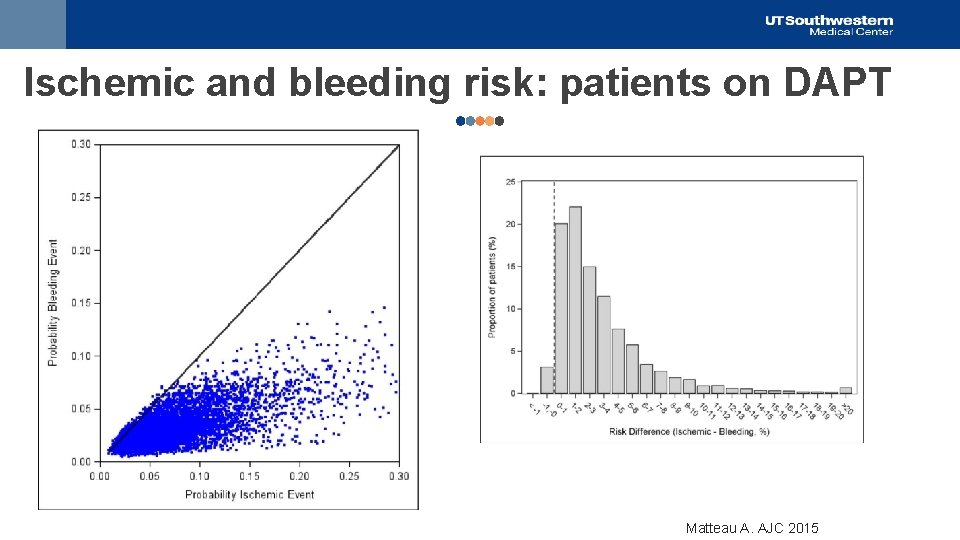
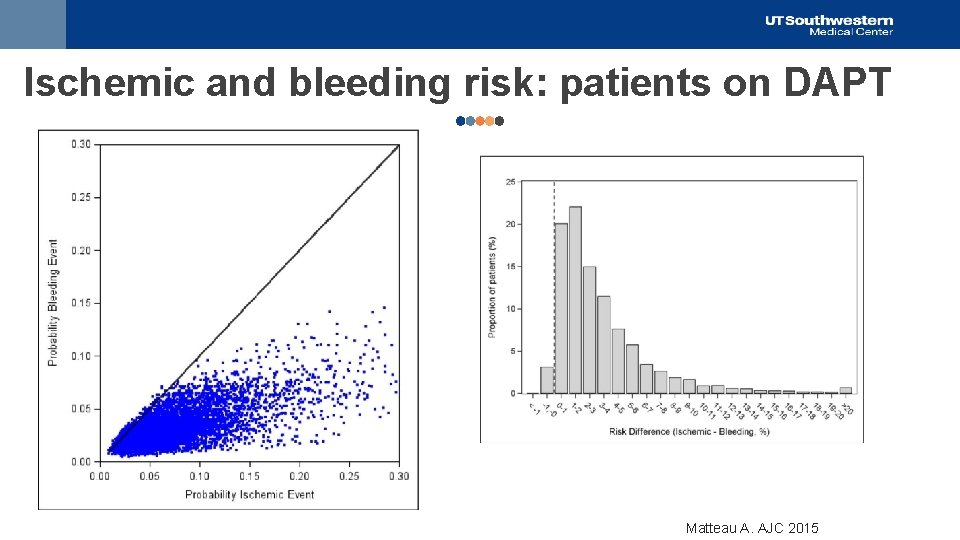
Ischemic and bleeding risk: patients on DAPT 200 400 Matteau A. AJC 2015

• Patients requiring long-term OAC and APT are a common clinical challenge • Estimated that 15 -30% of patients with AF will require APT/PCI • Patients on chronic oral anticoagulation therapy (OAC) with CAD are 7 x more likely to receive concomitant antiplatelet therapy • Atrial Fibrillation (ACTIVE W): The combination of aspirin and clopidogrel is not as effective as warfarin in patients with AF • Stenting (STARS): The combination of aspirin and a thienopyridine is more effective than warfarin in patients with coronary stents Hansen ML Arch Int Med 2010 Lip GY. Thromb Haemost 2010 Connolly S. Lancet. 2006 Leon MB. N Eng J Med. 1998
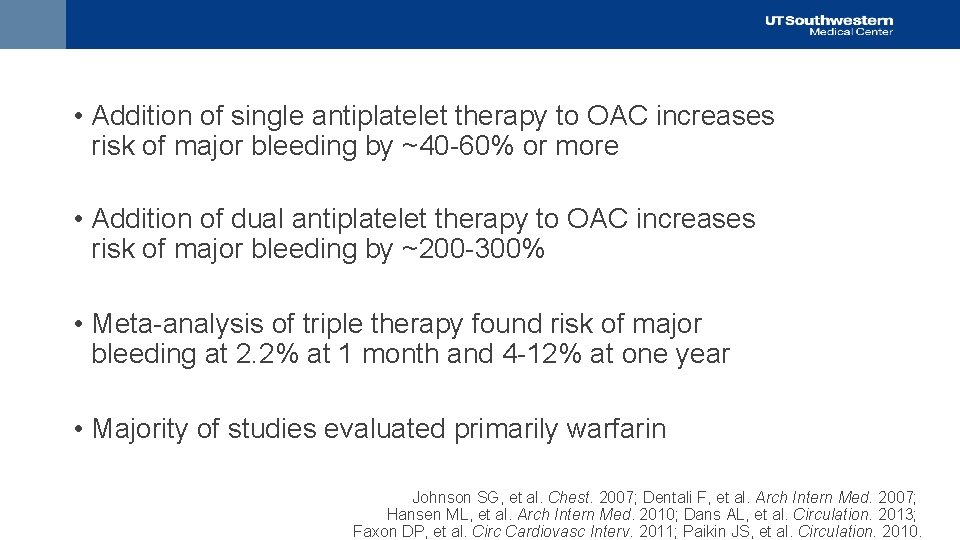
Triple Therapy • Addition of single antiplatelet therapy to OAC increases risk of major bleeding by ~40 -60% or more • Addition of dual antiplatelet therapy to OAC increases risk of major bleeding by ~200 -300% • Meta-analysis of triple therapy found risk of major bleeding at 2. 2% at 1 month and 4 -12% at one year • Majority of studies evaluated primarily warfarin Johnson SG, et al. Chest. 2007; Dentali F, et al. Arch Intern Med. 2007; Hansen ML, et al. Arch Intern Med. 2010; Dans AL, et al. Circulation. 2013; Faxon DP, et al. Circ Cardiovasc Interv. 2011; Paikin JS, et al. Circulation. 2010.
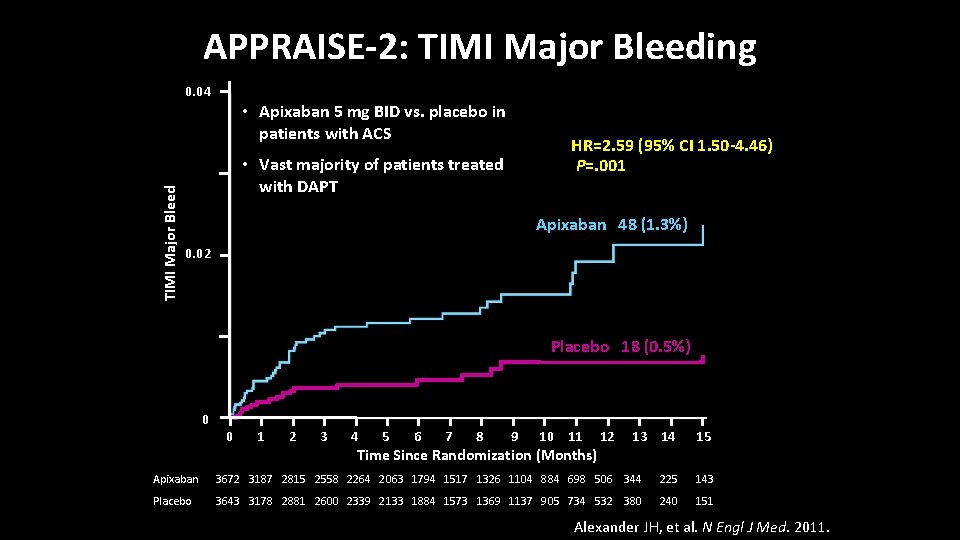
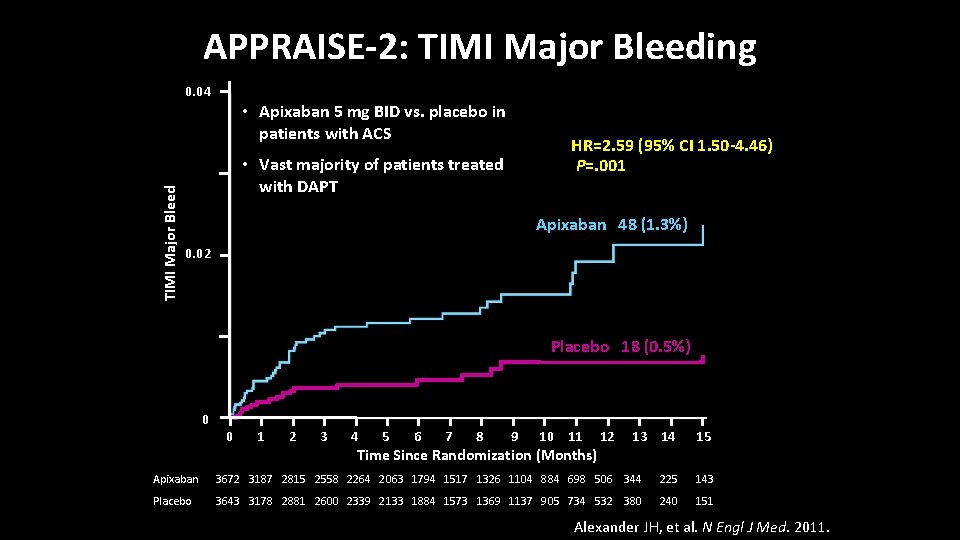
APPRAISE-2: TIMI Major Bleeding TIMI Major Bleed 0. 04 • Apixaban 5 mg BID vs. placebo in patients with ACS HR=2. 59 (95% CI 1. 50 -4. 46) P=. 001 • Vast majority of patients treated with DAPT Apixaban 48 (1. 3%) 0. 02 Placebo 18 (0. 5%) 0 0 1 2 3 4 5 6 7 8 9 10 11 Time Since Randomization (Months) 12 13 14 15 Apixaban 3672 3187 2815 2558 2264 2063 1794 1517 1326 1104 884 698 506 344 225 143 Placebo 3643 3178 2881 2600 2339 2133 1884 1573 1369 1137 905 734 532 380 240 151 Alexander JH, et al. N Engl J Med. 2011.

13
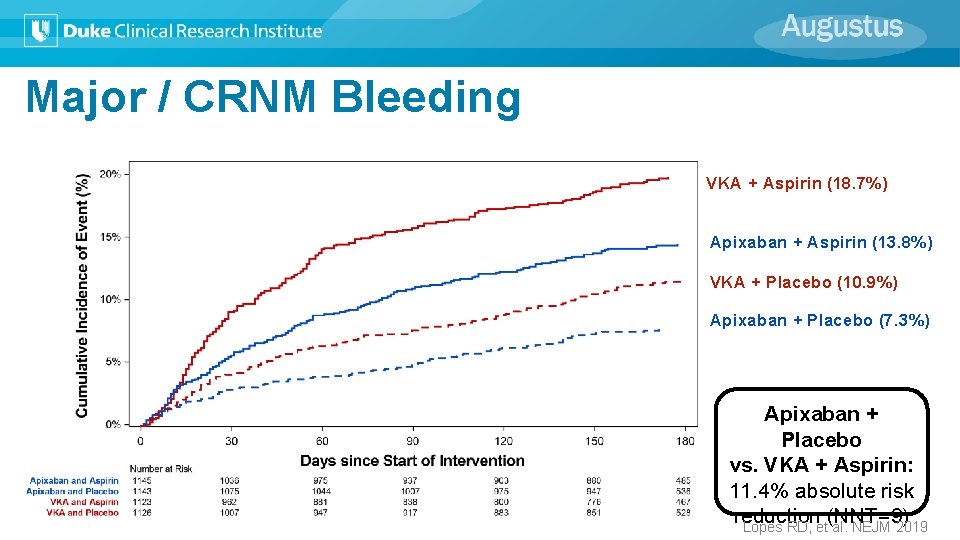
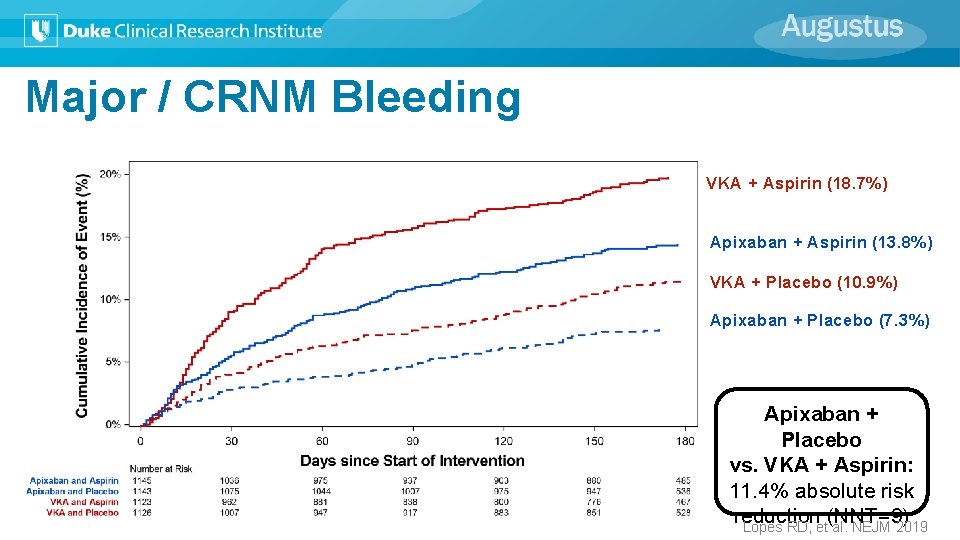
Major / CRNM Bleeding VKA + Aspirin (18. 7%) Apixaban + Aspirin (13. 8%) VKA + Placebo (10. 9%) Apixaban + Placebo (7. 3%) Apixaban + Placebo vs. VKA + Aspirin: 11. 4% absolute risk reduction (NNT=9) Lopes RD, et al. NEJM 2019
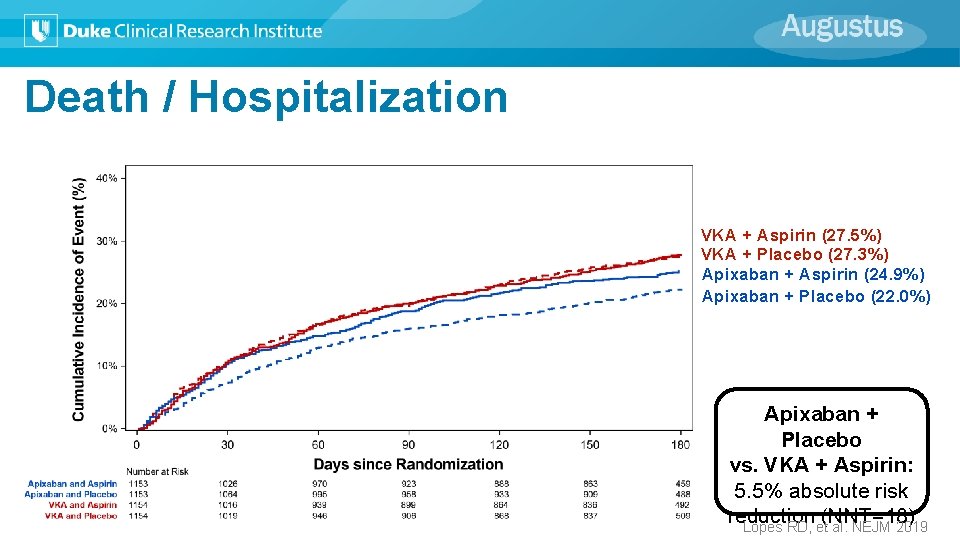
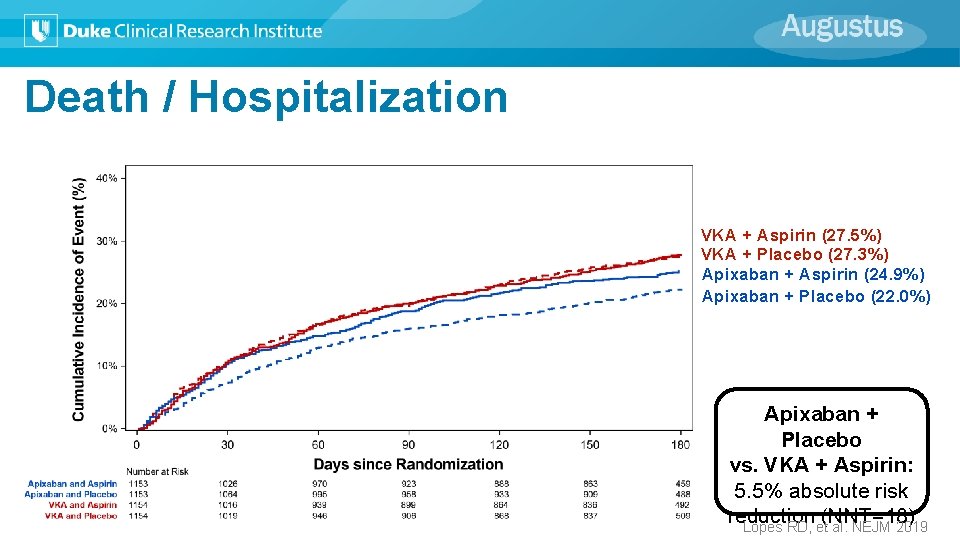
Death / Hospitalization VKA + Aspirin (27. 5%) VKA + Placebo (27. 3%) Apixaban + Aspirin (24. 9%) Apixaban + Placebo (22. 0%) Apixaban + Placebo vs. VKA + Aspirin: 5. 5% absolute risk reduction (NNT=18) Lopes RD, et al. NEJM 2019
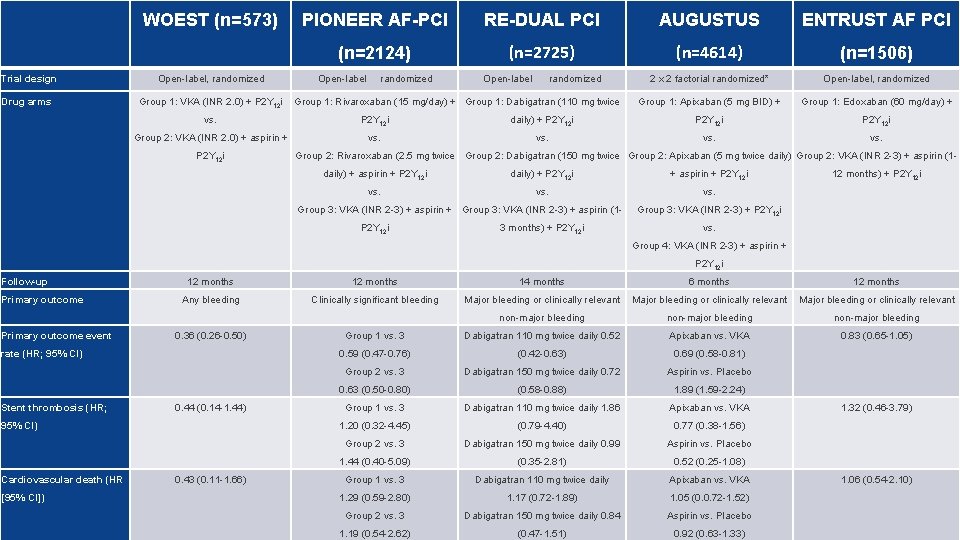
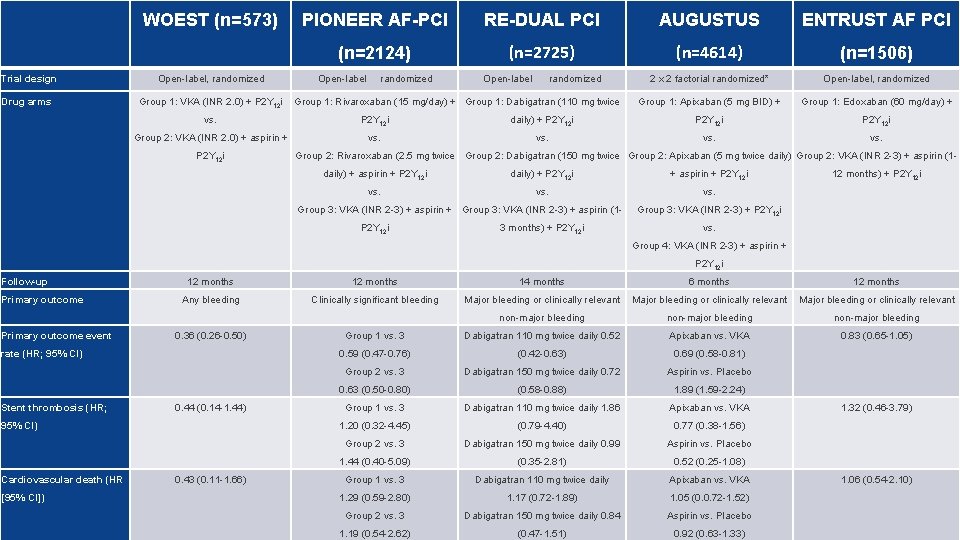
Trial design Drug arms WOEST (n=573) Open-label, randomized Group 1: VKA (INR 2. 0) + P 2 Y 12 i PIONEER AF-PCI RE-DUAL PCI AUGUSTUS ENTRUST AF PCI (n=2124) (n=2725) (n=4614) (n=1506) 2 x 2 factorial randomized* Open-label, randomized Group 1: Apixaban (5 mg BID) + Group 1: Edoxaban (60 mg/day) + Open-label randomized Group 1: Rivaroxaban (15 mg/day) + Group 1: Dabigatran (110 mg twice vs. P 2 Y 12 i daily) + P 2 Y 12 i Group 2: VKA (INR 2. 0) + aspirin + vs. P 2 Y 12 i Group 2: Rivaroxaban (2. 5 mg twice Group 2: Dabigatran (150 mg twice Group 2: Apixaban (5 mg twice daily) Group 2: VKA (INR 2 -3) + aspirin (1 daily) + aspirin + P 2 Y 12 i daily) + P 2 Y 12 i + aspirin + P 2 Y 12 i vs. Group 3: VKA (INR 2 -3) + aspirin + Group 3: VKA (INR 2 -3) + aspirin (1 P 2 Y 12 i 3 months) + P 2 Y 12 i 12 months) + P 2 Y 12 i Group 3: VKA (INR 2 -3) + P 2 Y 12 i vs. Group 4: VKA (INR 2 -3) + aspirin + P 2 Y 12 i Follow-up Primary outcome event 12 months 14 months 6 months 12 months Any bleeding Clinically significant bleeding Major bleeding or clinically relevant non-major bleeding Group 1 vs. 3 Dabigatran 110 mg twice daily 0. 52 Apixaban vs. VKA 0. 83 (0. 65 -1. 05) 0. 59 (0. 47 -0. 76) (0. 42 -0. 63) 0. 69 (0. 58 -0. 81) Group 2 vs. 3 Dabigatran 150 mg twice daily 0. 72 Aspirin vs. Placebo 0. 63 (0. 50 -0. 80) (0. 58 -0. 88) 1. 89 (1. 59 -2. 24) Group 1 vs. 3 Dabigatran 110 mg twice daily 1. 86 Apixaban vs. VKA 1. 20 (0. 32 -4. 45) (0. 79 -4. 40) 0. 77 (0. 38 -1. 56) Group 2 vs. 3 Dabigatran 150 mg twice daily 0. 99 Aspirin vs. Placebo 1. 44 (0. 40 -5. 09) (0. 35 -2. 81) 0. 52 (0. 25 -1. 08) Group 1 vs. 3 Dabigatran 110 mg twice daily Apixaban vs. VKA 1. 29 (0. 59 -2. 80) 1. 17 (0. 72 -1. 89) 1. 05 (0. 0. 72 -1. 52) Group 2 vs. 3 Dabigatran 150 mg twice daily 0. 84 Aspirin vs. Placebo 1. 19 (0. 54 -2. 62) (0. 47 -1. 51) 0. 92 (0. 63 -1. 33) 0. 36 (0. 26 -0. 50) rate (HR; 95% CI) Stent thrombosis (HR; 0. 44 (0. 14 -1. 44) 95% CI) Cardiovascular death (HR [95% CI]) 0. 43 (0. 11 -1. 66) 1. 32 (0. 46 -3. 79) 1. 06 (0. 54 -2. 10) 16
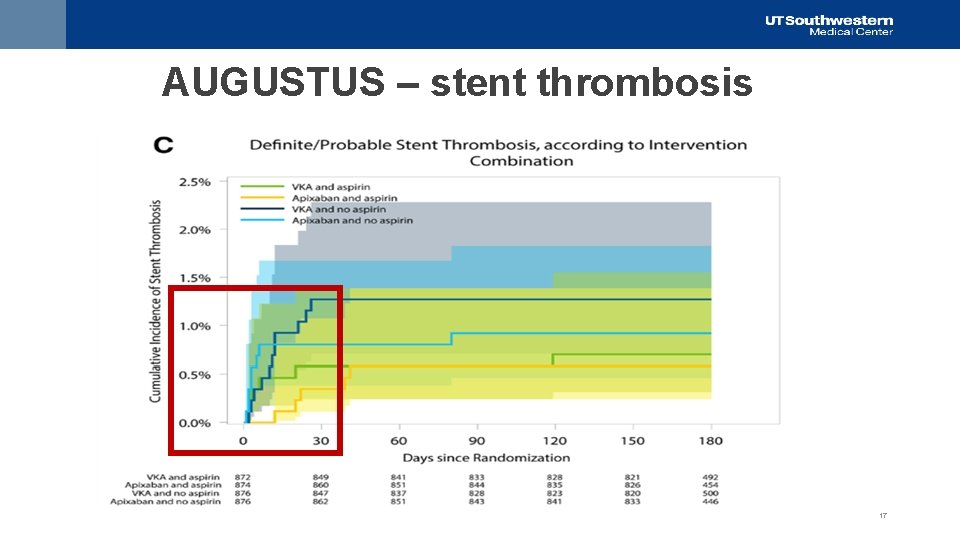
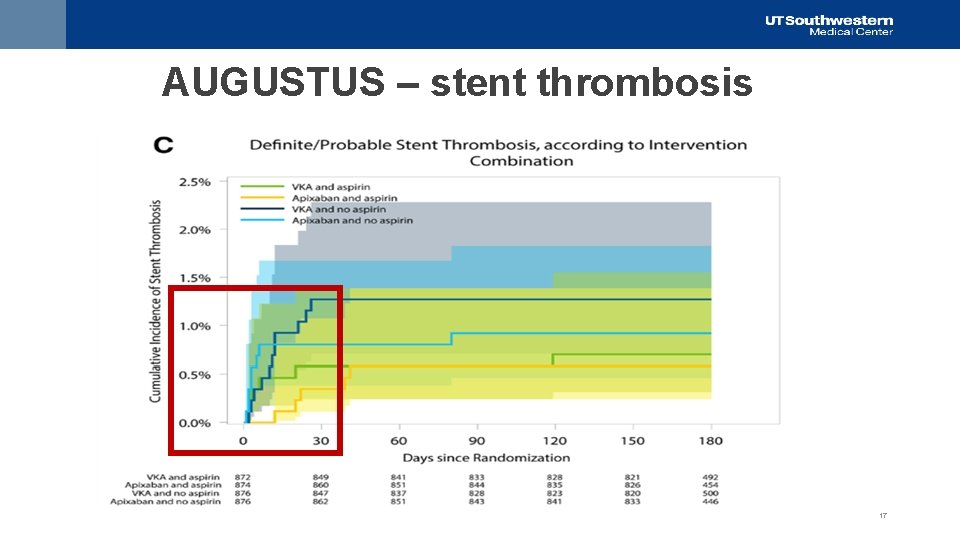
AUGUSTUS – stent thrombosis 17
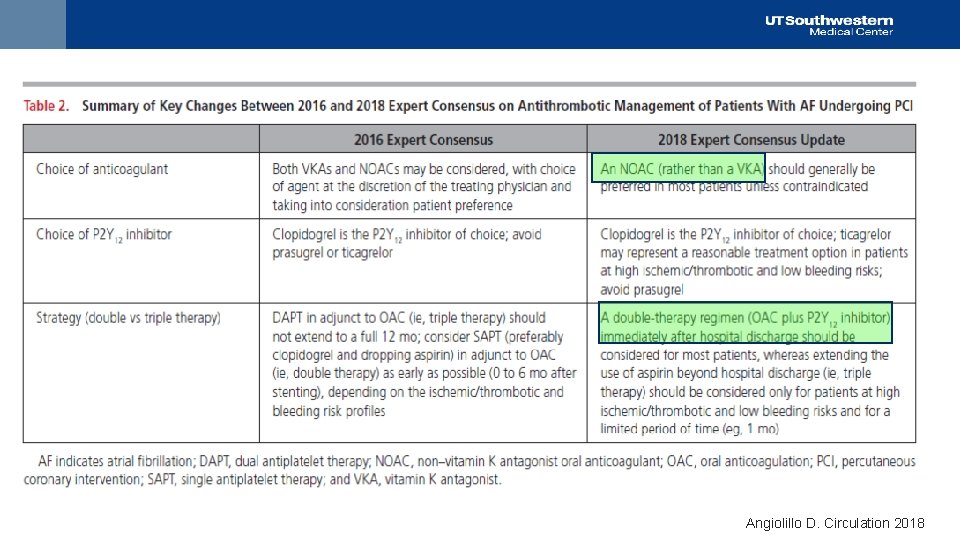
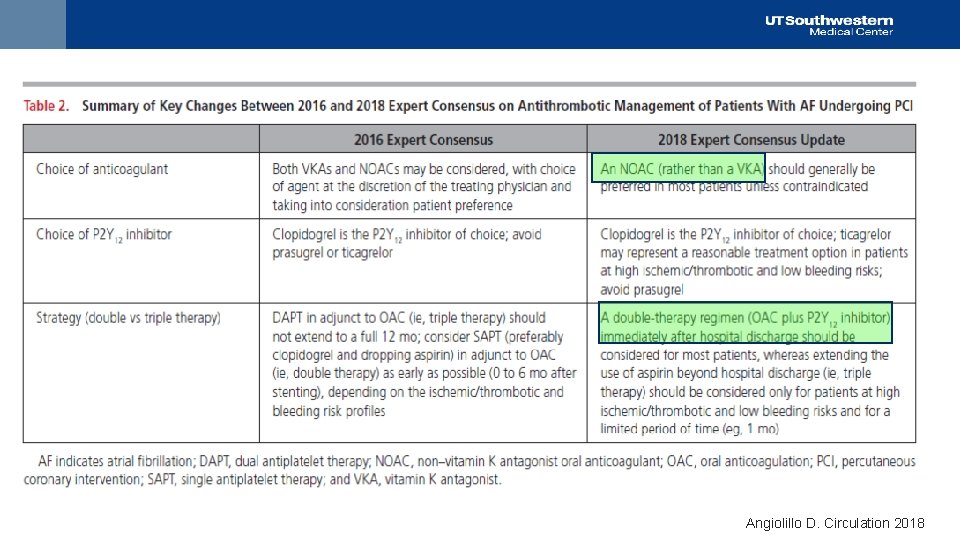
Angiolillo D. Circulation 2018

Angiolillo D. Circulation 2018
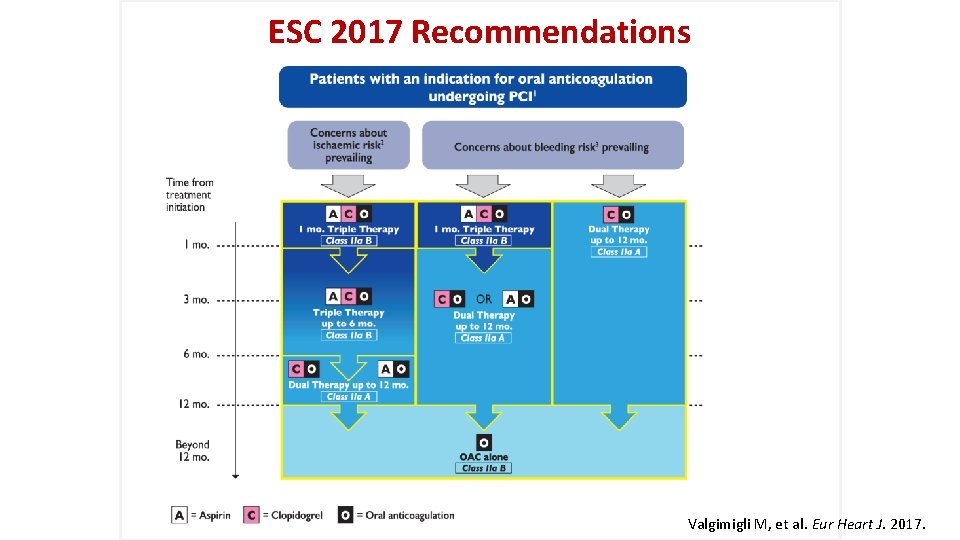
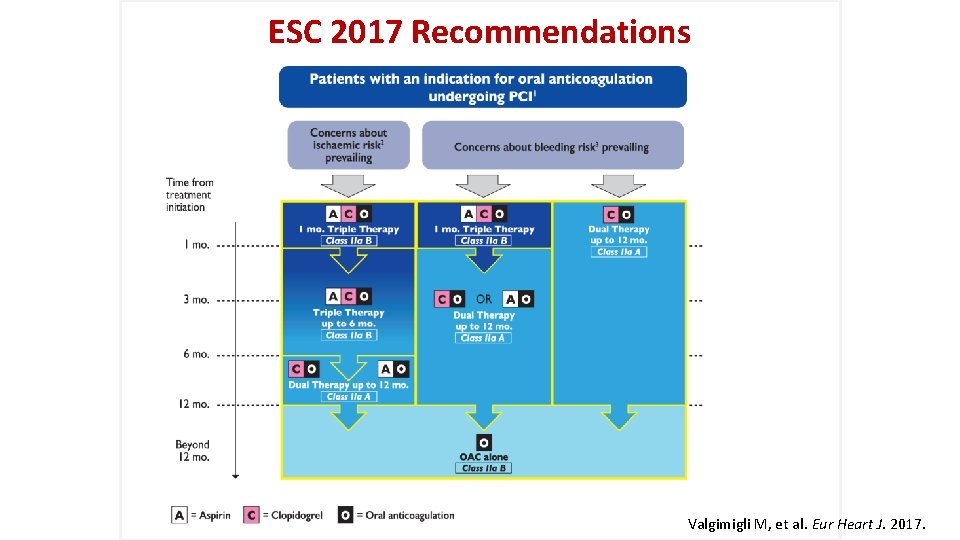
ESC 2017 Recommendations Valgimigli M, et al. Eur Heart J. 2017.
21
Case update • Patient discharged on apixaban 5 mg BID and clopidogrel 75 mg daily, based on ARISTOTLE • ASA 325 mg on day of PCI, none after that • Doing well at 30 days
Concluding thoughts • Need for OAC and APT remains a common clinical dilemma • Rapidly evolving evidence-base • DOACs better than VKA, dosing considerations important • “Dual therapy less bleeding than triple therapy long-term, efficacy preserved • Clopidogrel is P 2 Y 12 i of choice, ticagrelor in some instances • ASA 81 can be considered if high stent thrombosis risk and low bleeding risk for short durations
 Triple entente ww1
Triple entente ww1 антанта
антанта Triple entente vs triple alliance
Triple entente vs triple alliance Alianzas de la primera y segunda guerra mundial
Alianzas de la primera y segunda guerra mundial Triple alianza y triple entente
Triple alianza y triple entente Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Perimylolysis
Perimylolysis Dsdm models
Dsdm models Excellent choice for systems requiring high reliability
Excellent choice for systems requiring high reliability What is virtual memory
What is virtual memory Industries requiring compulsory licensing *
Industries requiring compulsory licensing * Syngenta corn herbicides
Syngenta corn herbicides Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Stomach ulcer
Stomach ulcer Pud triple therapy
Pud triple therapy Pud triple therapy
Pud triple therapy Triple therapy anticoagulation
Triple therapy anticoagulation Triple therapy dose
Triple therapy dose Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness bits cost
Bioness bits cost What are the major humanistic therapies
What are the major humanistic therapies ç
ç