Acute Ischemic Stroke Intervention Updates A Vascular Neurology



- Slides: 31

Acute Ischemic Stroke Intervention Updates: “A Vascular Neurology Perspective” Cardiovascular Research Technology Conference (CRT 19) Mach 5, 2019 Richard T. Benson, MD/Ph. D Associate Director, NIH Stroke Program @ MWHC Associate Professor of Clinical Neurology Georgetown University Medical Center
Disclosures: Abbott Laboratories Speaker’s Bureau
Topics § Extra-cranial carotid disease § Intra-cranial arterial disease § Acute LVO of the anterior circulation <6 hours § Acute LVO of the anterior circulation 6 – 24 hours
Carotid Endarterectomy Three large studies have shown the benefit of CEA in symptomatic patients with >70% stenosis (NASCET, ECST, VACST). For those with moderate stenosis, 50 – 69% and symptoms, other factors e. g. co-morbid conditions, gender, and risk factors must be considered.

Carotid Endarterectomy: Symptomatic stenosis Barnett HJM et al. , CMJ 2003
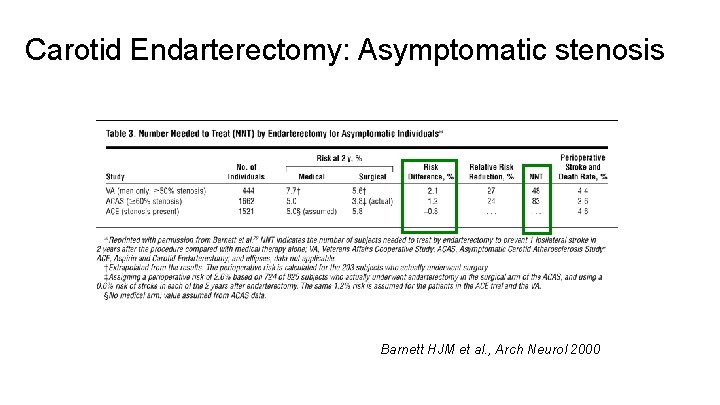
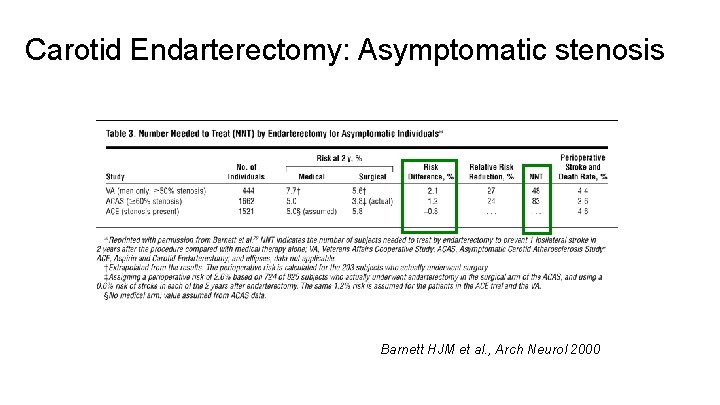
Carotid Endarterectomy: Asymptomatic stenosis Barnett HJM et al. , Arch Neurol 2000
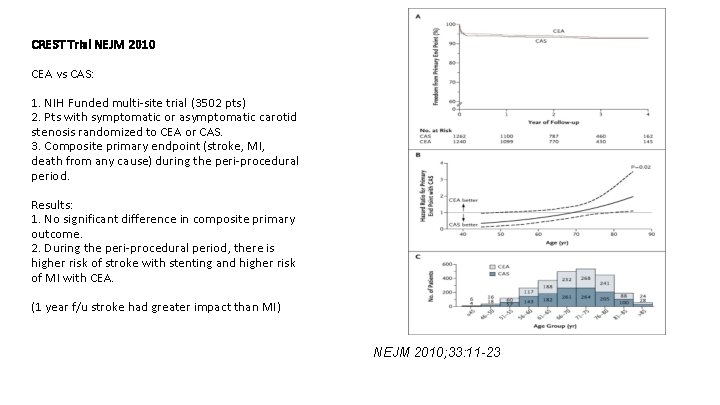
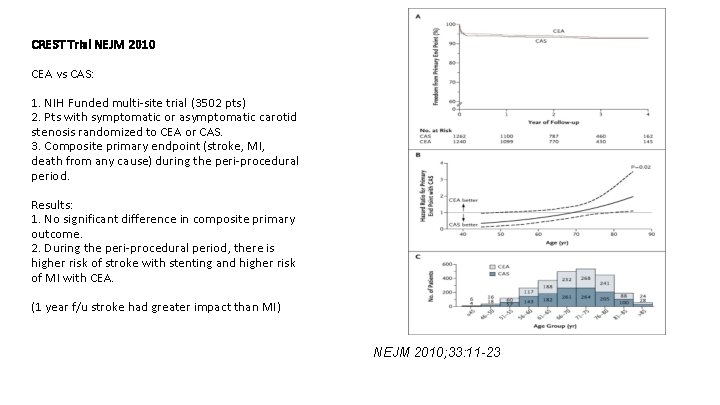
CREST Trial NEJM 2010 CEA vs CAS: 1. NIH Funded multi-site trial (3502 pts) 2. Pts with symptomatic or asymptomatic carotid stenosis randomized to CEA or CAS. 3. Composite primary endpoint (stroke, MI, death from any cause) during the peri-procedural period. Results: 1. No significant difference in composite primary outcome. 2. During the peri-procedural period, there is higher risk of stroke with stenting and higher risk of MI with CEA. (1 year f/u stroke had greater impact than MI) NEJM 2010; 33: 11 -23
AHA/ASA 2014 Guideline for the Prevention of Stroke in Patients with Stroke and TIA 1. For patients with TIA/IS within last 6 months and 70 -90% stenosis, CEA is recommended (if the perioperative morbidity mortality <6%). 2. For recent TIA/IS and 50 -69% stenosis, CEA is recommended based on patient specific factors 3. When degree of stenosis <50% CEA and CAS are not recommended. 4. When indicated, revascularization should be within 2 weeks of index event (if small stroke and no hemorrhage) 5. CAS is indicated as a alternative to CEA based on patient specific factors, anatomy, and neck morphology AHA/ASA 2018 Guideline for the Early Management of Patients with Acute Ischemic Stroke When revascularization is indicated for secondary stroke prevention in patients with minor, nondisabling stroke (m. RS 0 -2), it is reasonable to perform the procedure between 48 hours and 7 days of the index event rather than delay treatment if there are no contraindications to early revascularization.
AHA/ASA 2014 Guideline for the Prevention of Stroke in Patients with Stroke and TIA 1. For patients with TIA/IS within last 6 months and 70 -90% stenosis, CEA is recommended (if the perioperative morbidity mortality <6%). 2. For recent TIA/IS and 50 -69% stenosis, CEA is recommended based on patient specific factors 3. When degree of stenosis <50% CEA and CAS are not recommended. 4. When indicated, revascularization should be within 2 weeks of index event (if small stroke and no hemorrhage) 5. CAS is indicated as a alternative to CEA based on patient specific factors, anatomy, and neck morphology AHA/ASA 2018 Guideline for the Early Management of Patients with Acute Ischemic Stroke When revascularization is indicated for secondary stroke prevention in patients with minor, nondisabling stroke (m. RS 0 -2), it is reasonable to perform the procedure between 48 hours and 7 days of the index event rather than delay treatment if there are no contraindications to early revascularization. (CREST 2 on-going trial)
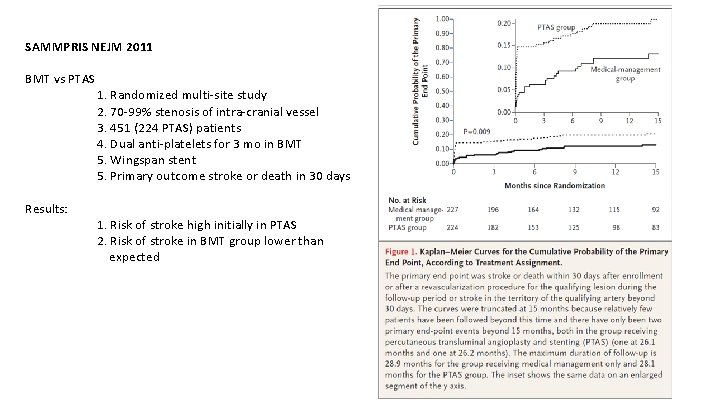
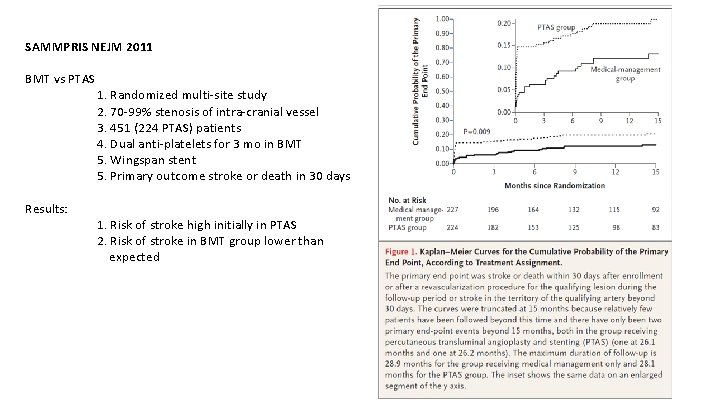
SAMMPRIS NEJM 2011 BMT vs PTAS Results: 1. Randomized multi-site study 2. 70 -99% stenosis of intra-cranial vessel 3. 451 (224 PTAS) patients 4. Dual anti-platelets for 3 mo in BMT 5. Wingspan stent 5. Primary outcome stroke or death in 30 days 1. Risk of stroke high initially in PTAS 2. Risk of stroke in BMT group lower than expected
AHA/ASA 2014 Guideline for the Prevention of Stroke in Patients with Stroke and TIA 1. For patients with TIA/IS with 50 -99% stenosis of a major intra-cranial artery ASA 325 mg is recommended over warfarin. 2. For patients with TIA/IS within 30 days attributable to 70 -99% stenosis of an intra-cranial artery, combination of ASA 325 mg/Plavix 75 mg for 90 days might be reasonable. 3. Stenting of intra-cranial arteries is not recommended
Acute Ischemic Stroke: Major thrombolytic Landmarks Lower rates of early recanalization and worse outcomes in patients with large vessel occlusion (LVO) with IV r-t. PA.
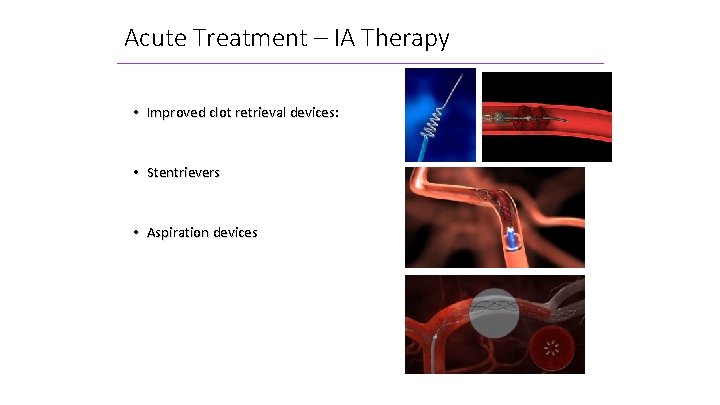
Acute Treatment – IA Therapy • Improved clot retrieval devices: • Stentrievers • Aspiration devices
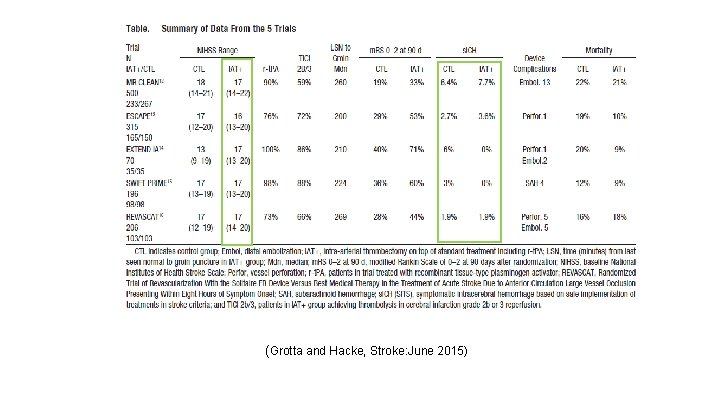
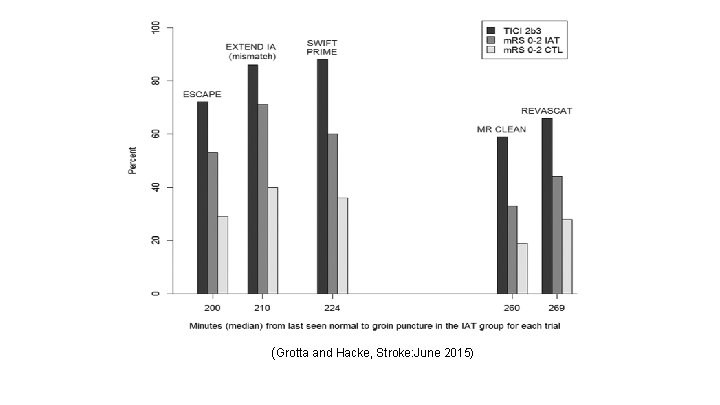
Acute Ischemic Stroke: Major Endovascular Landmarks 1. 2. 3. 4. 5. MR CLEAN (N Engl J Med 2015; 372: 11 -20) ESCAPE (N Engl J Med 2015; 372: 1010 -1030) EXTEND IA (N Engl J Med 2015; 372: 1009 -1018) SWIFT PRIME (N Engl J Med doi: 10. 1056/NEJMoa 1503780) REVASCAT (N Engl J Med doi. 1056/NEJMoa 1503780) HERMES A meta-analysis published in Lancet 2016 (confirmed the results).
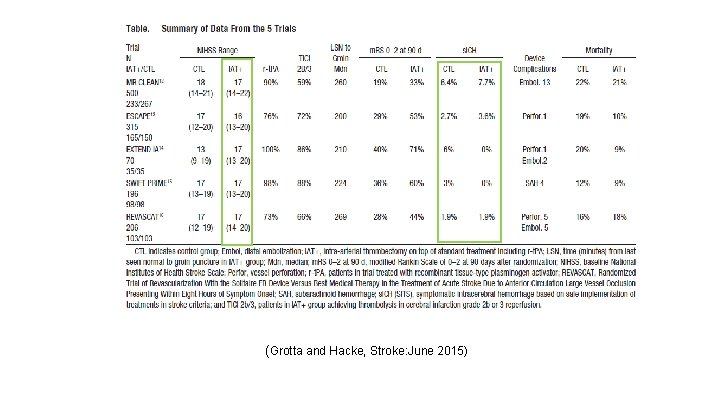
(Grotta and Hacke, Stroke: June 2015)
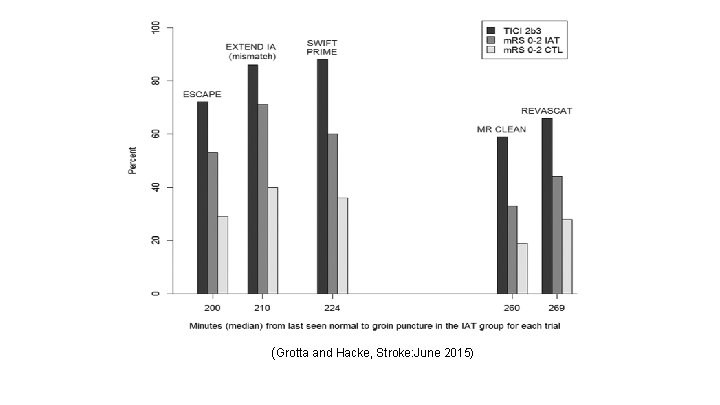
(Grotta and Hacke, Stroke: June 2015)
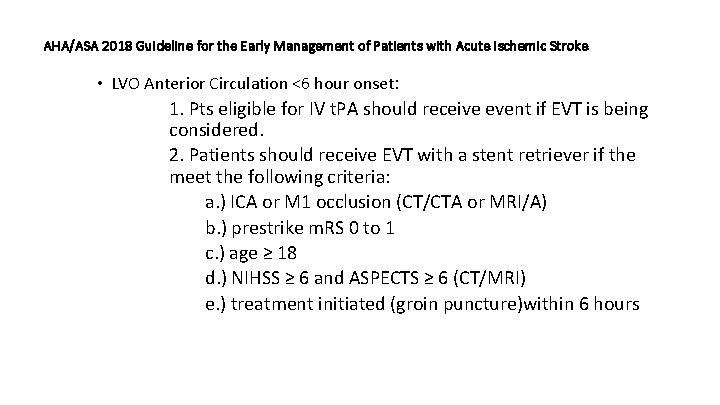
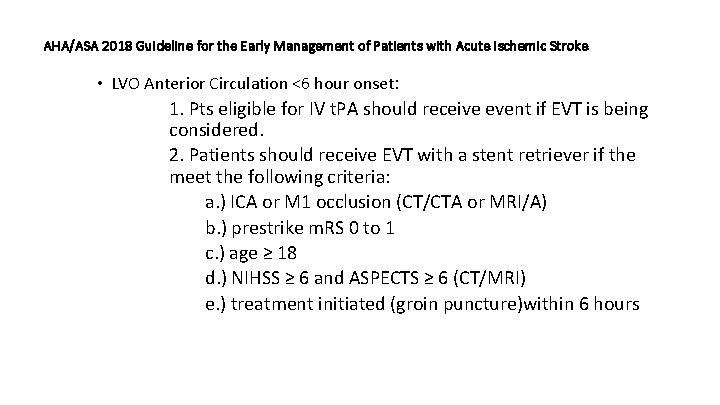
AHA/ASA 2018 Guideline for the Early Management of Patients with Acute Ischemic Stroke • LVO Anterior Circulation <6 hour onset: 1. Pts eligible for IV t. PA should receive event if EVT is being considered. 2. Patients should receive EVT with a stent retriever if the meet the following criteria: a. ) ICA or M 1 occlusion (CT/CTA or MRI/A) b. ) prestrike m. RS 0 to 1 c. ) age ≥ 18 d. ) NIHSS ≥ 6 and ASPECTS ≥ 6 (CT/MRI) e. ) treatment initiated (groin puncture)within 6 hours
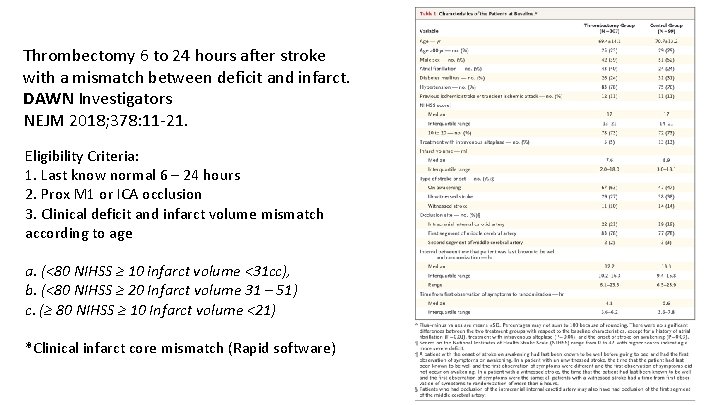
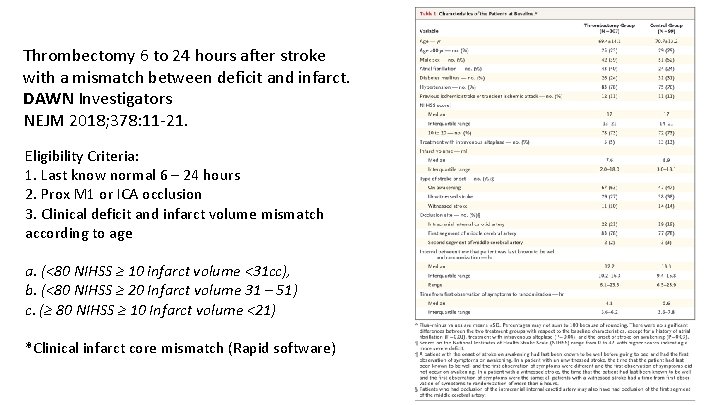
Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. DAWN Investigators NEJM 2018; 378: 11 -21. Eligibility Criteria: 1. Last know normal 6 – 24 hours 2. Prox M 1 or ICA occlusion 3. Clinical deficit and infarct volume mismatch according to age a. (<80 NIHSS ≥ 10 infarct volume <31 cc), b. (<80 NIHSS ≥ 20 Infarct volume 31 – 51) c. (≥ 80 NIHSS ≥ 10 Infarct volume <21) *Clinical infarct core mismatch (Rapid software)
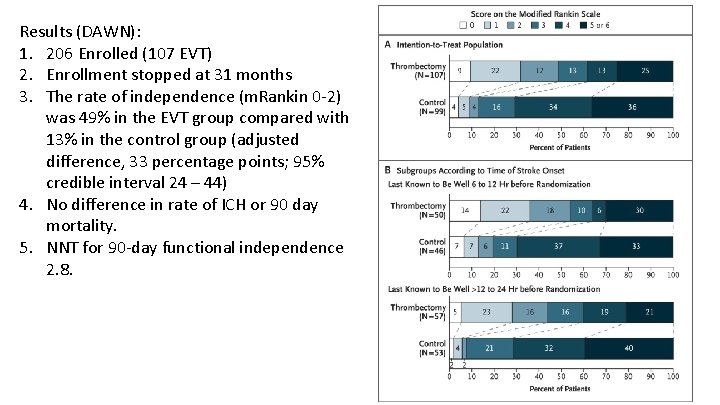
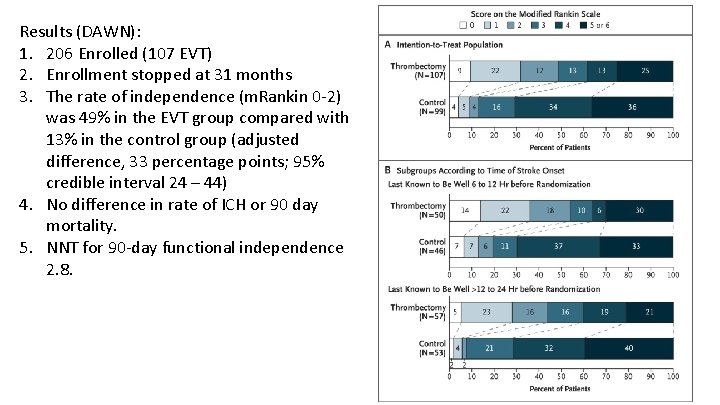
Results (DAWN): 1. 206 Enrolled (107 EVT) 2. Enrollment stopped at 31 months 3. The rate of independence (m. Rankin 0 -2) was 49% in the EVT group compared with 13% in the control group (adjusted difference, 33 percentage points; 95% credible interval 24 – 44) 4. No difference in rate of ICH or 90 day mortality. 5. NNT for 90 -day functional independence 2. 8.
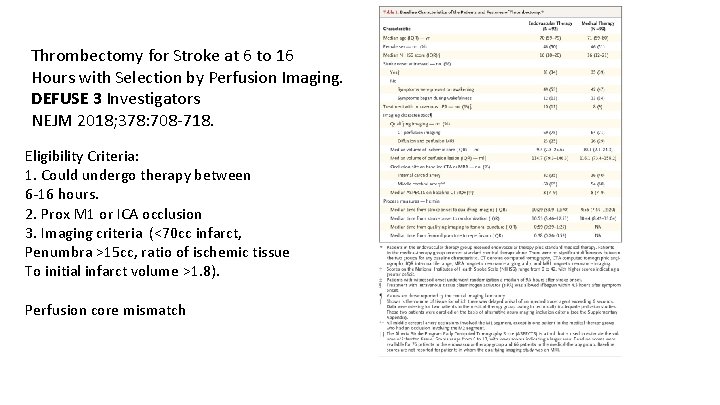
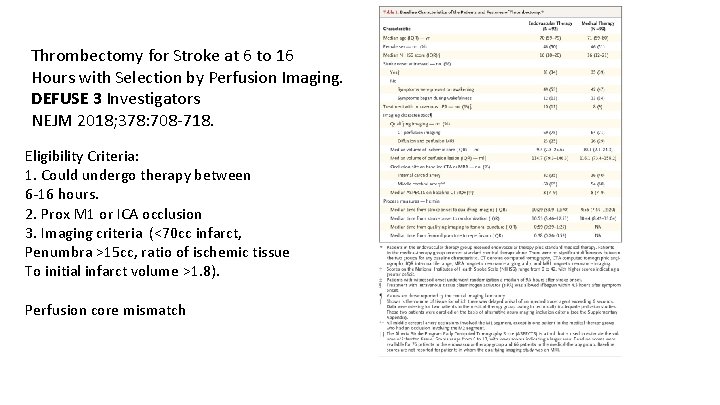
Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. DEFUSE 3 Investigators NEJM 2018; 378: 708 -718. Eligibility Criteria: 1. Could undergo therapy between 6 -16 hours. 2. Prox M 1 or ICA occlusion 3. Imaging criteria (<70 cc infarct, Penumbra >15 cc, ratio of ischemic tissue To initial infarct volume >1. 8). Perfusion core mismatch
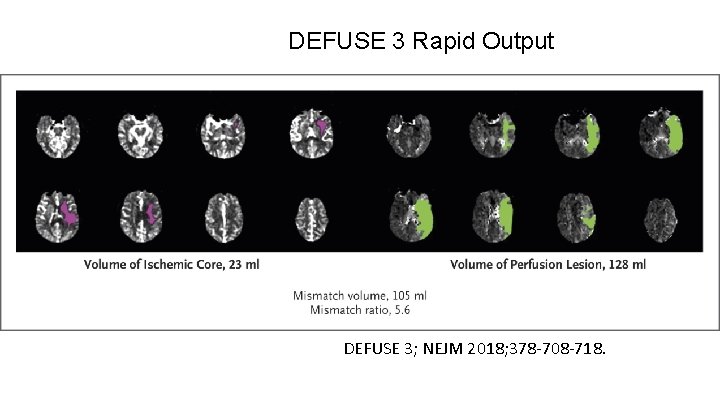
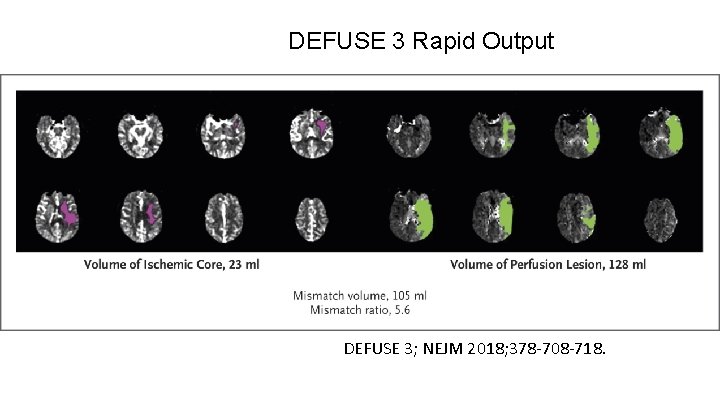
DEFUSE 3 Rapid Output DEFUSE 3; NEJM 2018; 378 -708 -718.
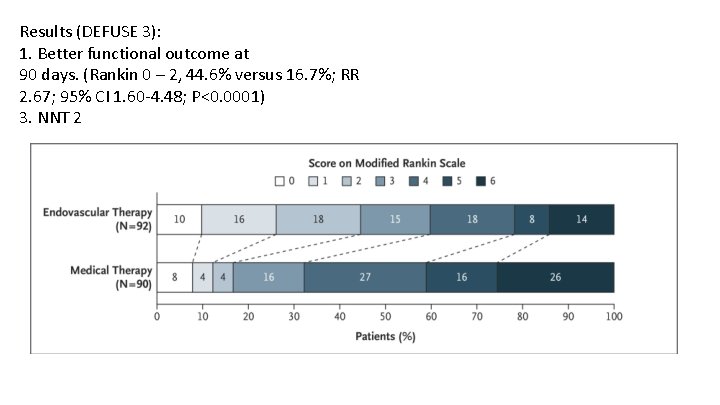
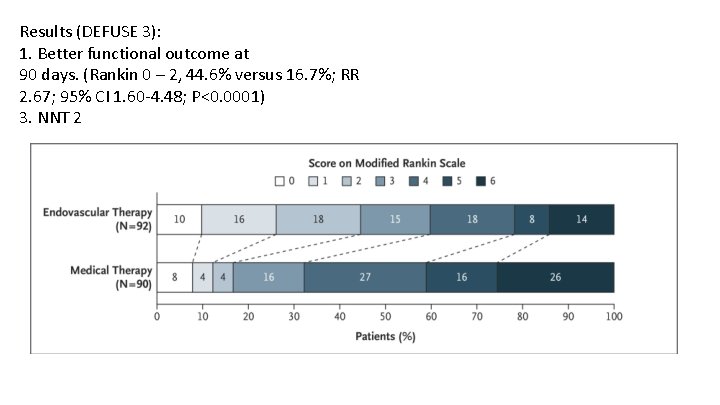
Results (DEFUSE 3): 1. Better functional outcome at 90 days. (Rankin 0 – 2, 44. 6% versus 16. 7%; RR 2. 67; 95% CI 1. 60 -4. 48; P<0. 0001) 3. NNT 2

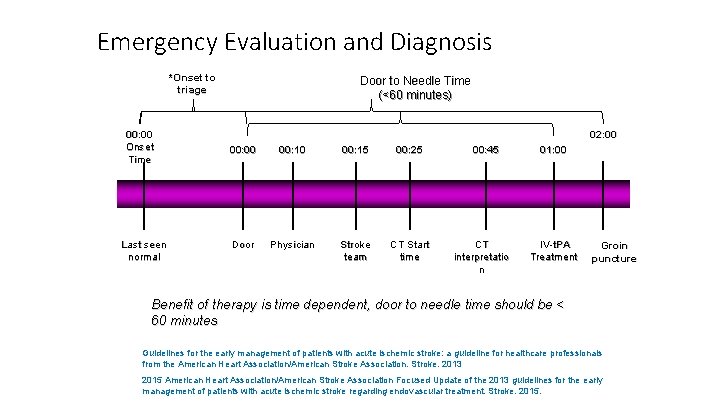
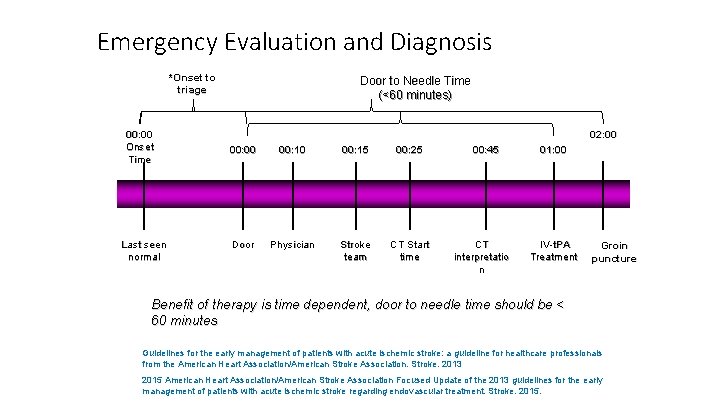
Emergency Evaluation and Diagnosis *Onset to triage 00: 00 Onset Time Last seen normal Door to Needle Time (<60 minutes) 02: 00 00: 10 00: 15 00: 25 Door Physician Stroke team CT Start time 00: 45 CT interpretatio n 01: 00 IV-t. PA Treatment Groin puncture Benefit of therapy is time dependent, door to needle time should be < 60 minutes Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013 2015 American Heart Association/American Stroke Association Focused Update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment. Stroke. 2015.
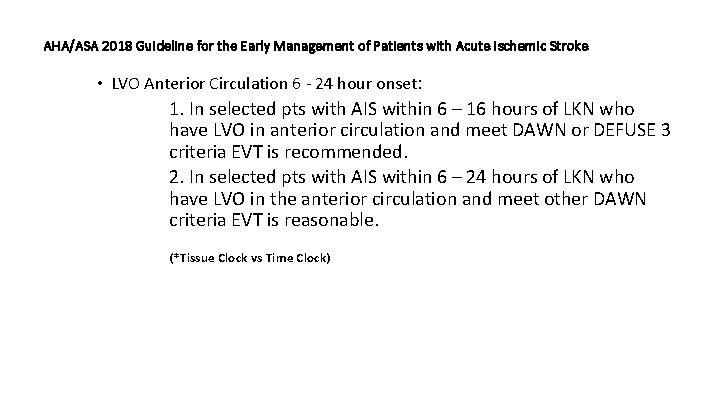
AHA/ASA 2018 Guideline for the Early Management of Patients with Acute Ischemic Stroke • LVO Anterior Circulation 6 - 24 hour onset: 1. In selected pts with AIS within 6 – 16 hours of LKN who have LVO in anterior circulation and meet DAWN or DEFUSE 3 criteria EVT is recommended. 2. In selected pts with AIS within 6 – 24 hours of LKN who have LVO in the anterior circulation and meet other DAWN criteria EVT is reasonable. (*Tissue Clock vs Time Clock)
**Discussion between Neuro-IR attending and stroke Attending**