Anaemia In Pregnancy Iron Deficiency Dr Nivedita Malik






- Slides: 43
Anaemia In Pregnancy (Iron Deficiency) Dr Nivedita Malik
� Commonest medical disorder in pregnancy. � 18 -20 % pregnant women are anaemic in developed countries as compared to 40 -75 % in developing countries and Up to 88% in some states. � It is responsible(directly/contributory factor) for significant high maternal mortality throught out world, but more so in developing nations.
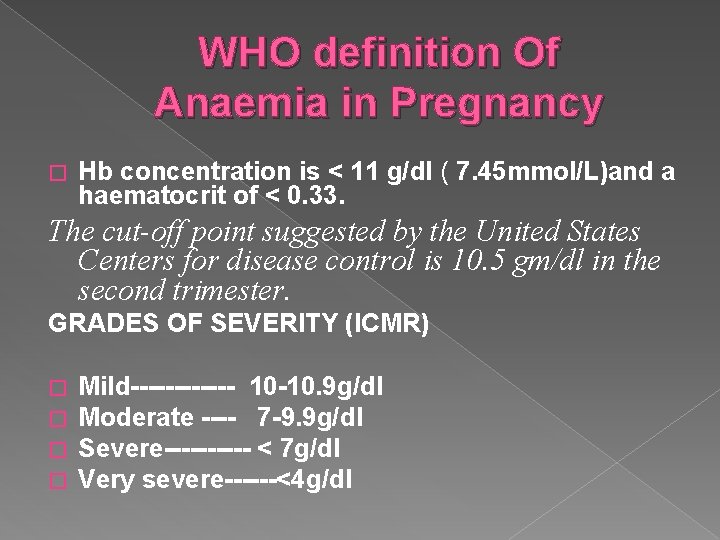
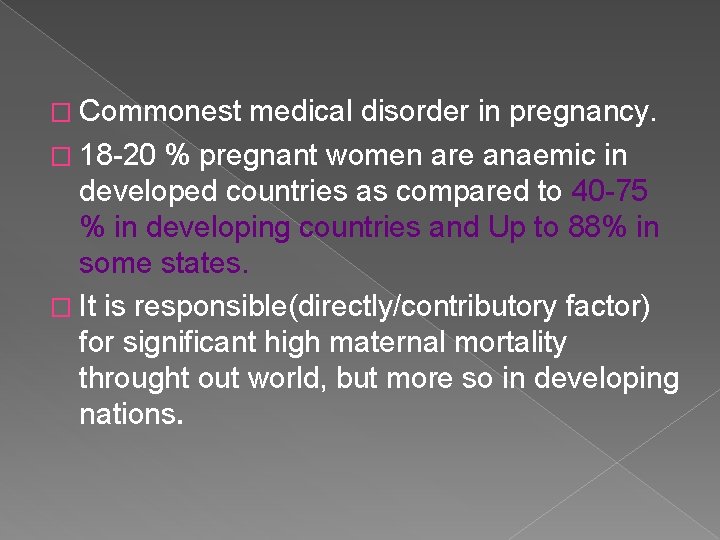
WHO definition Of Anaemia in Pregnancy � Hb concentration is < 11 g/dl ( 7. 45 mmol/L)and a haematocrit of < 0. 33. The cut-off point suggested by the United States Centers for disease control is 10. 5 gm/dl in the second trimester. GRADES OF SEVERITY (ICMR) � � Mild------ 10 -10. 9 g/dl Moderate ---- 7 -9. 9 g/dl Severe----- < 7 g/dl Very severe------<4 g/dl
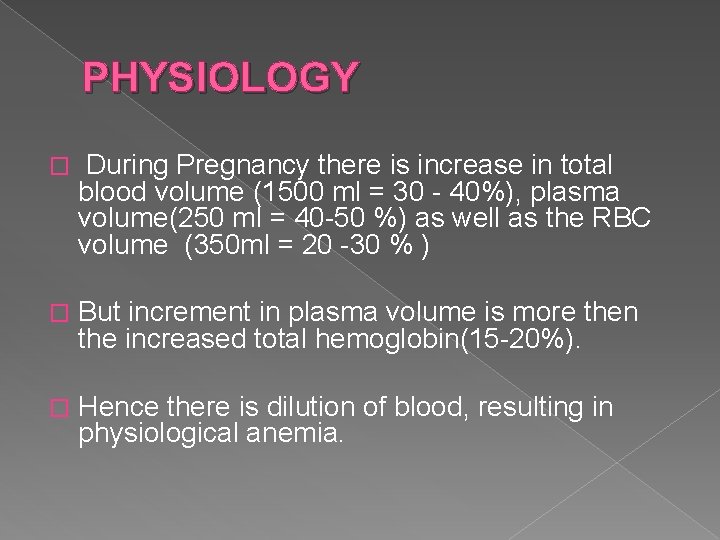
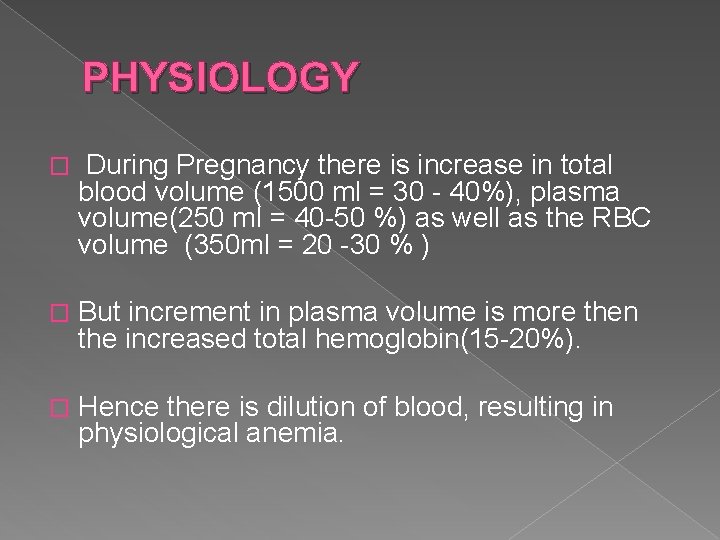
PHYSIOLOGY � During Pregnancy there is increase in total blood volume (1500 ml = 30 - 40%), plasma volume(250 ml = 40 -50 %) as well as the RBC volume (350 ml = 20 -30 % ) � But increment in plasma volume is more then the increased total hemoglobin(15 -20%). � Hence there is dilution of blood, resulting in physiological anemia.
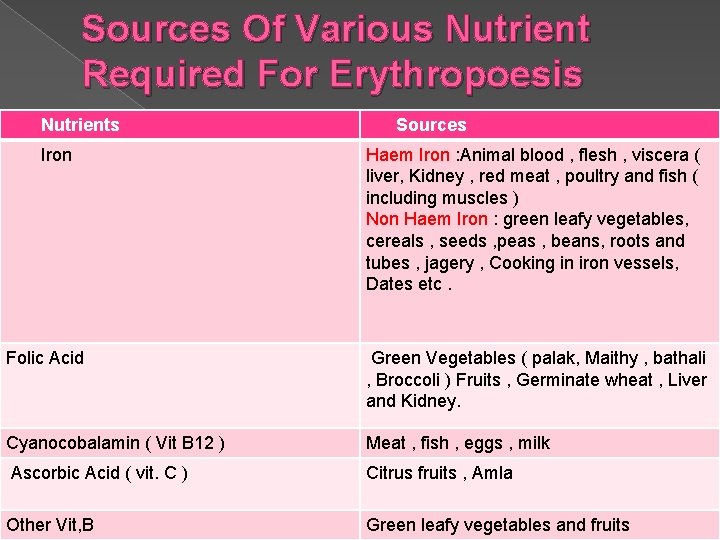
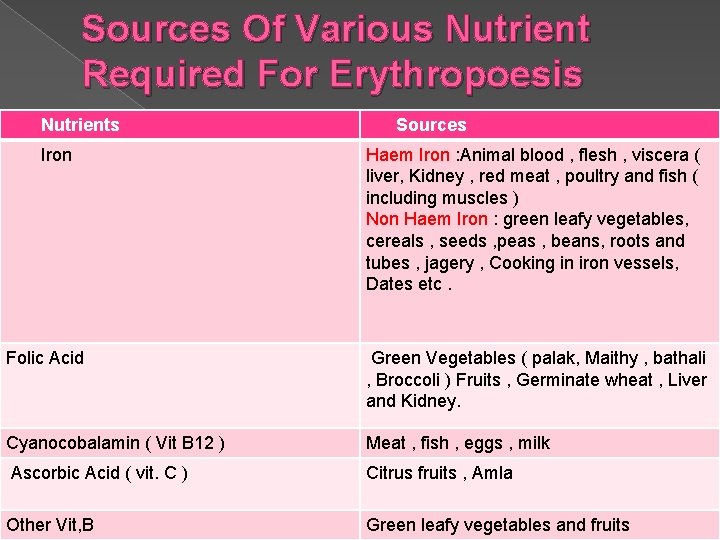
Sources Of Various Nutrient Required For Erythropoesis Nutrients Iron Sources Haem Iron : Animal blood , flesh , viscera ( liver, Kidney , red meat , poultry and fish ( including muscles ) Non Haem Iron : green leafy vegetables, cereals , seeds , peas , beans, roots and tubes , jagery , Cooking in iron vessels, Dates etc. Folic Acid Green Vegetables ( palak, Maithy , bathali , Broccoli ) Fruits , Germinate wheat , Liver and Kidney. Cyanocobalamin ( Vit B 12 ) Meat , fish , eggs , milk Ascorbic Acid ( vit. C ) Citrus fruits , Amla Other Vit, B Green leafy vegetables and fruits
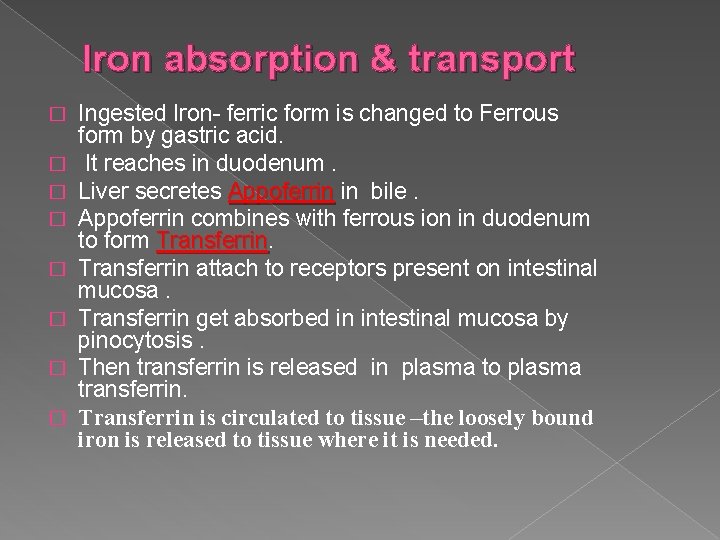
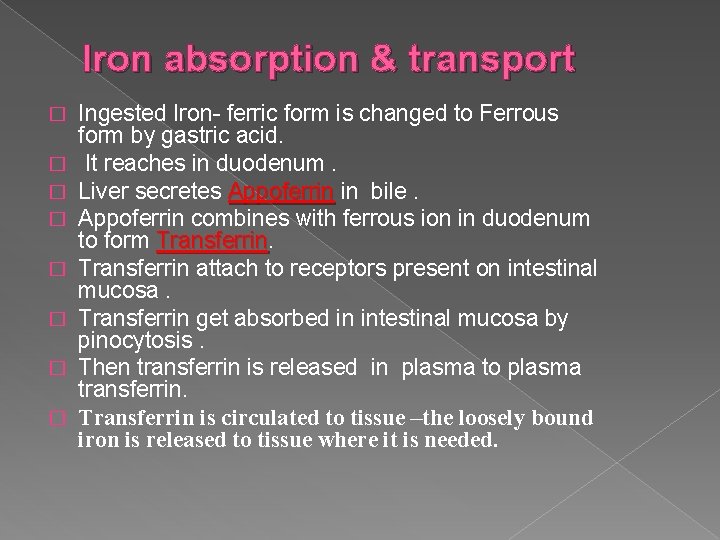
Iron absorption & transport � � � � Ingested Iron- ferric form is changed to Ferrous form by gastric acid. It reaches in duodenum. Liver secretes Appoferrin in bile. Appoferrin combines with ferrous ion in duodenum to form Transferrin attach to receptors present on intestinal mucosa. Transferrin get absorbed in intestinal mucosa by pinocytosis. Then transferrin is released in plasma to plasma transferrin. Transferrin is circulated to tissue –the loosely bound iron is released to tissue where it is needed.
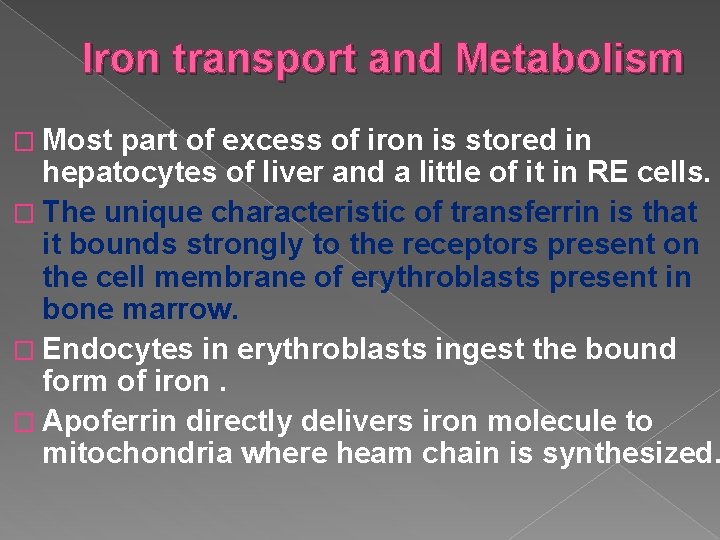
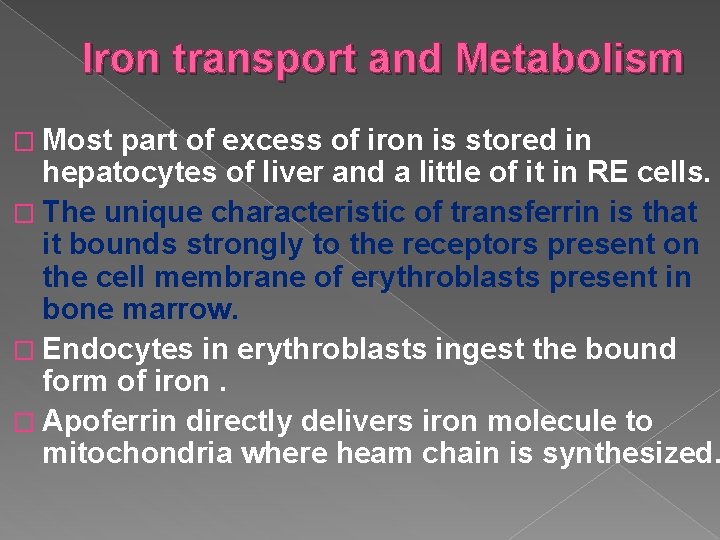
Iron transport and Metabolism � Most part of excess of iron is stored in hepatocytes of liver and a little of it in RE cells. � The unique characteristic of transferrin is that it bounds strongly to the receptors present on the cell membrane of erythroblasts present in bone marrow. � Endocytes in erythroblasts ingest the bound form of iron. � Apoferrin directly delivers iron molecule to mitochondria where heam chain is synthesized.

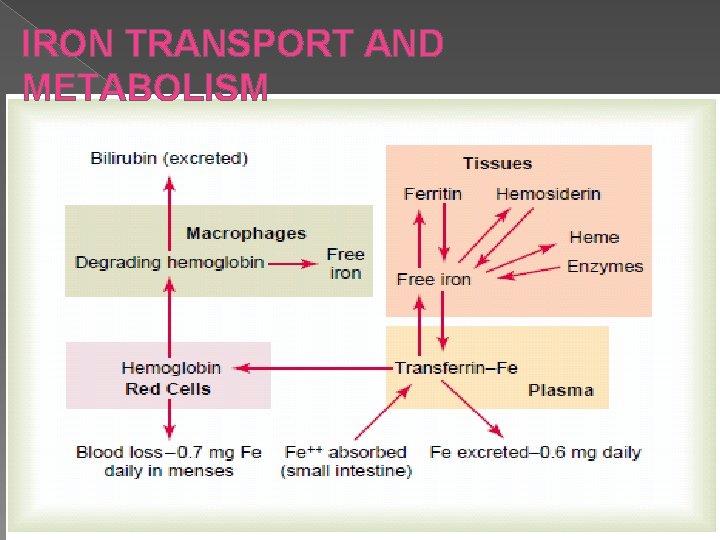
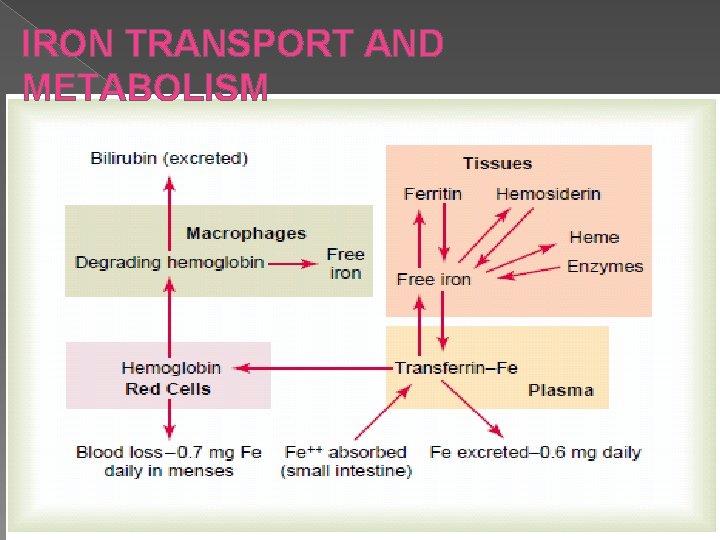
IRON TRANSPORT AND METABOLISM
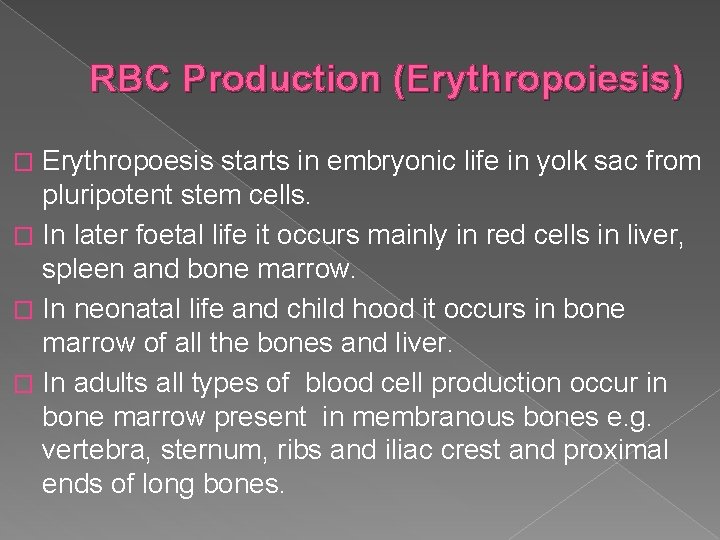
RBC Production (Erythropoiesis) Erythropoesis starts in embryonic life in yolk sac from pluripotent stem cells. � In later foetal life it occurs mainly in red cells in liver, spleen and bone marrow. � In neonatal life and child hood it occurs in bone marrow of all the bones and liver. � In adults all types of blood cell production occur in bone marrow present in membranous bones e. g. vertebra, sternum, ribs and iliac crest and proximal ends of long bones. �
The Hematinic Agents Erythropoietin Iron Vitamin B 12 & Folic acid
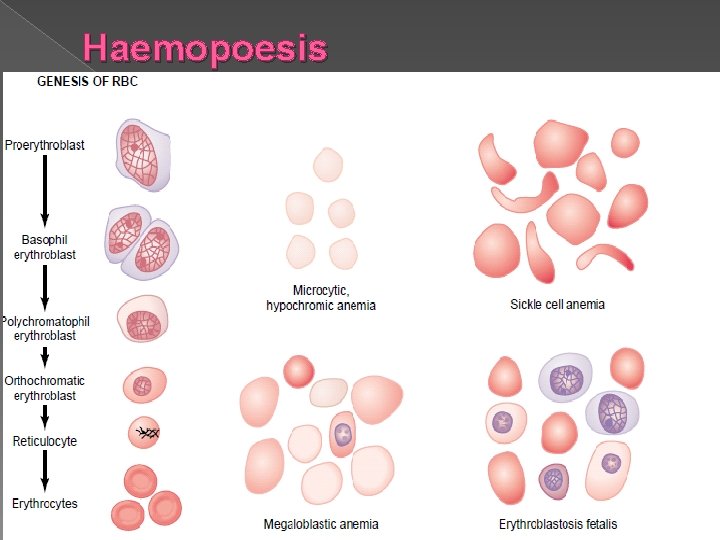
ERYTHROPOIESIS � Confined to the bone marrow in adults � RBCs are formed through stages of pro-normoblast – reticulocytes – mature non-nucleated eryhrocyte. � After a life span of 120 days RBCs degenerate and haemoglobin is broken down into haemosiderin and bile pigment.
ERYTHROPOIESIS (Contd. ) � For proper erythropoiesis adequate nutrients are needed: Minerals: Iron, traces of copper, cobalt and zinc. 2. Vitamins: Folic Acid, Vitamin B 12, Vitamin C, Pyridoxine and riboflavin 3. Proteins: For synthesis of globin moiety. 4. Hormones: Androgens and thyroxine, placental lactogen and progesterone. 1.

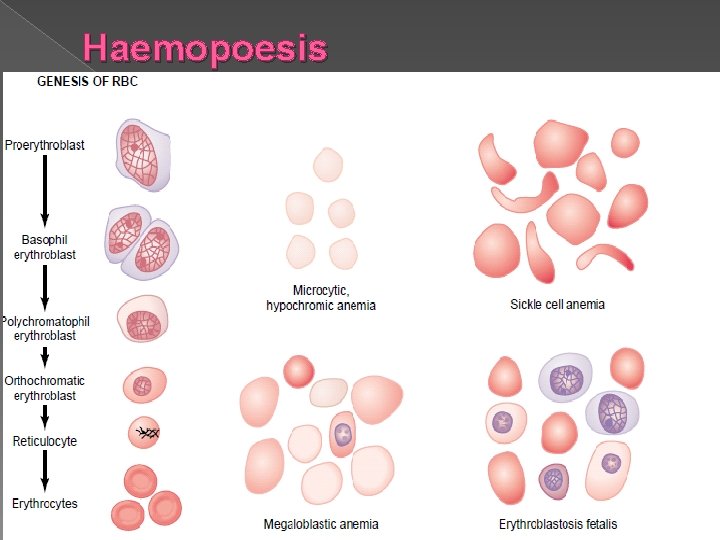
Haemopoesis
Life Span Of RBC And its destruction Mature RBC circulate and remain alive ( active )for 120 days. � RBC face wear and tear in circulation and get aged when they are engulfed by macrophages which dissociate iron from haem. � This iron is mainly stored in ferritin pool for Hb production. � Rest heam is denaturized in liver as bilrubin. � Daily loss of Iron- 0. 6 mg iron is lost in feces by male but iron loss is more in menstruating females (1. 3 mg). �
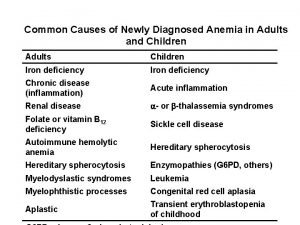
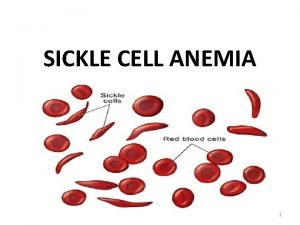
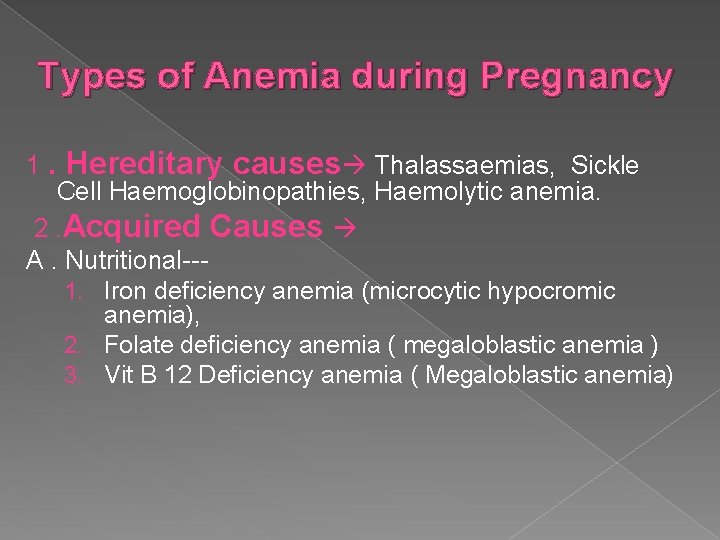
Types of Anemia during Pregnancy 1. Hereditary causes Thalassaemias, Sickle Cell Haemoglobinopathies, Haemolytic anemia. 2. Acquired Causes A. Nutritional--1. Iron deficiency anemia (microcytic hypocromic anemia), 2. Folate deficiency anemia ( megaloblastic anemia ) 3. Vit B 12 Deficiency anemia ( Megaloblastic anemia)
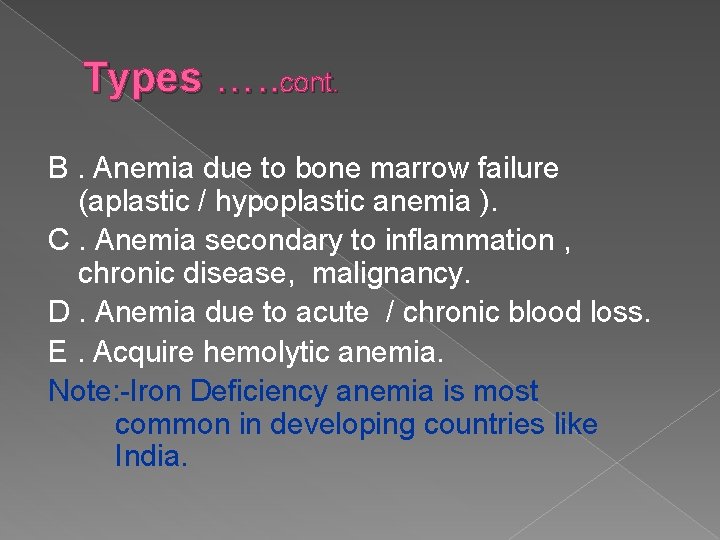
Types …. . cont. B. Anemia due to bone marrow failure (aplastic / hypoplastic anemia ). C. Anemia secondary to inflammation , chronic disease, malignancy. D. Anemia due to acute / chronic blood loss. E. Acquire hemolytic anemia. Note: -Iron Deficiency anemia is most common in developing countries like India.
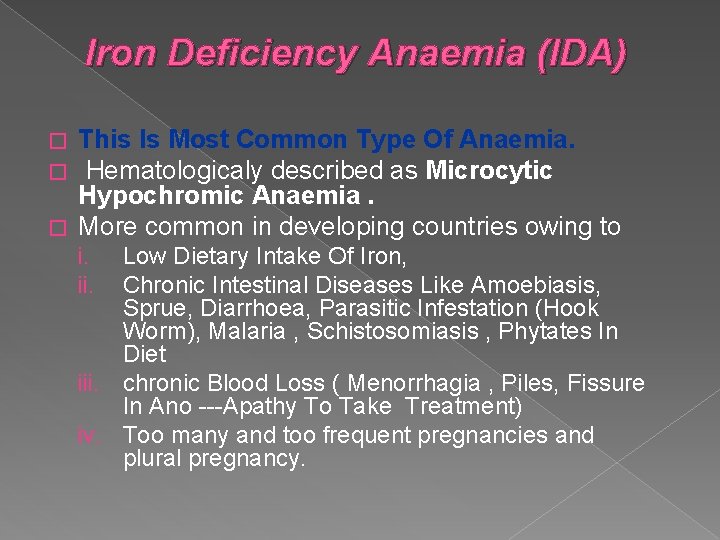
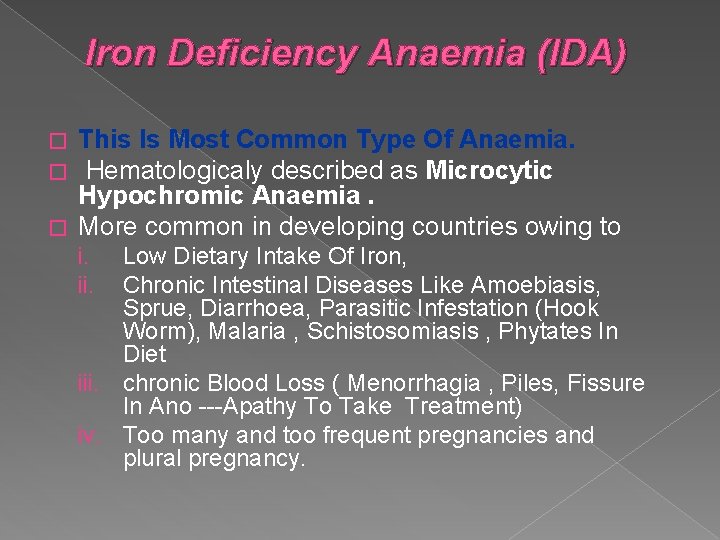
Iron Deficiency Anaemia (IDA) This Is Most Common Type Of Anaemia. Hematologicaly described as Microcytic Hypochromic Anaemia. � More common in developing countries owing to � � Low Dietary Intake Of Iron, Chronic Intestinal Diseases Like Amoebiasis, Sprue, Diarrhoea, Parasitic Infestation (Hook Worm), Malaria , Schistosomiasis , Phytates In Diet iii. chronic Blood Loss ( Menorrhagia , Piles, Fissure In Ano ---Apathy To Take Treatment) iv. Too many and too frequent pregnancies and plural pregnancy. i. ii.
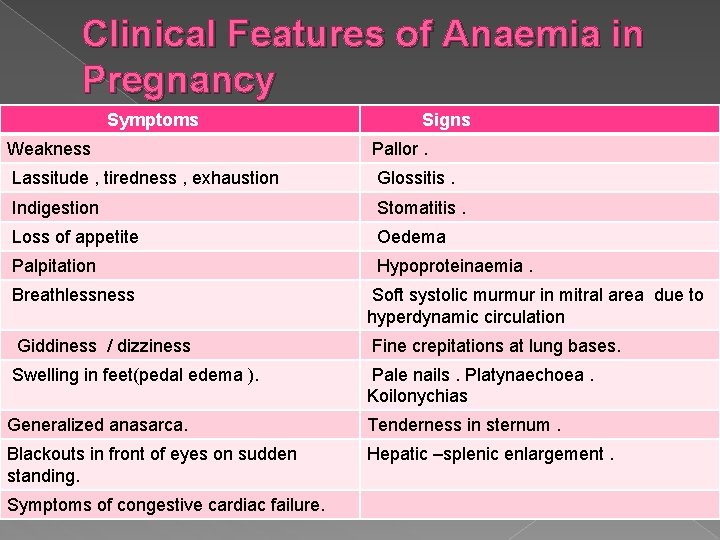
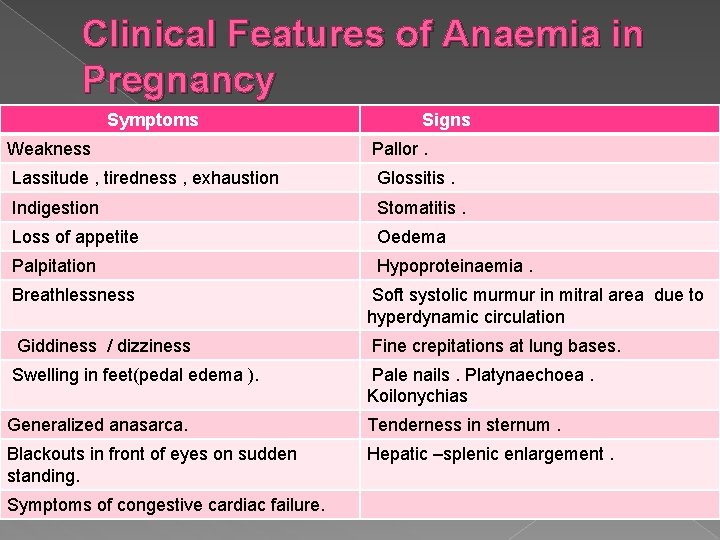
Clinical Features of Anaemia in Pregnancy Symptoms Signs Weakness Pallor. Lassitude , tiredness , exhaustion Glossitis. Indigestion Stomatitis. Loss of appetite Oedema Palpitation Hypoproteinaemia. Breathlessness Soft systolic murmur in mitral area due to hyperdynamic circulation Giddiness / dizziness Fine crepitations at lung bases. Swelling in feet(pedal edema ). Pale nails. Platynaechoea. Koilonychias Generalized anasarca. Tenderness in sternum. Blackouts in front of eyes on sudden standing. Hepatic –splenic enlargement. Symptoms of congestive cardiac failure.
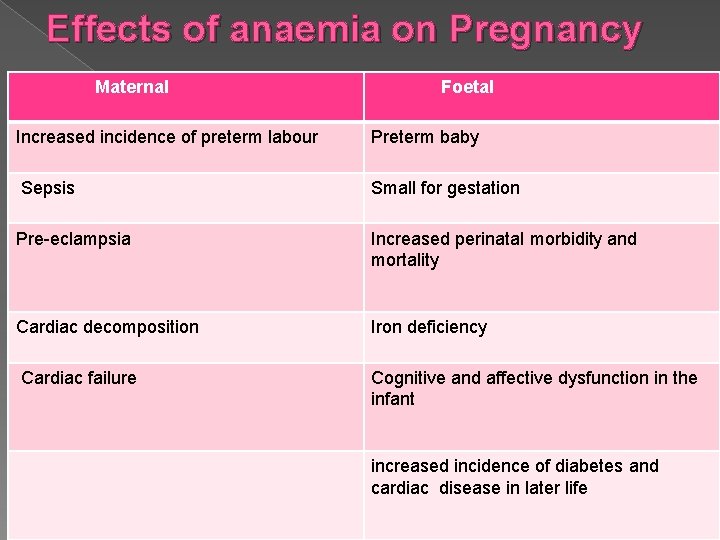
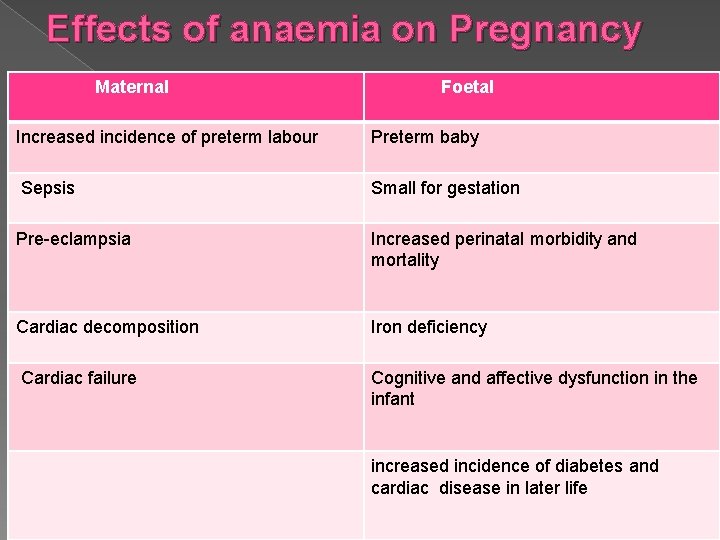
Effects of anaemia on Pregnancy Maternal Foetal Increased incidence of preterm labour Preterm baby Sepsis Small for gestation Pre-eclampsia Increased perinatal morbidity and mortality Cardiac decomposition Iron deficiency Cardiac failure Cognitive and affective dysfunction in the infant increased incidence of diabetes and cardiac disease in later life


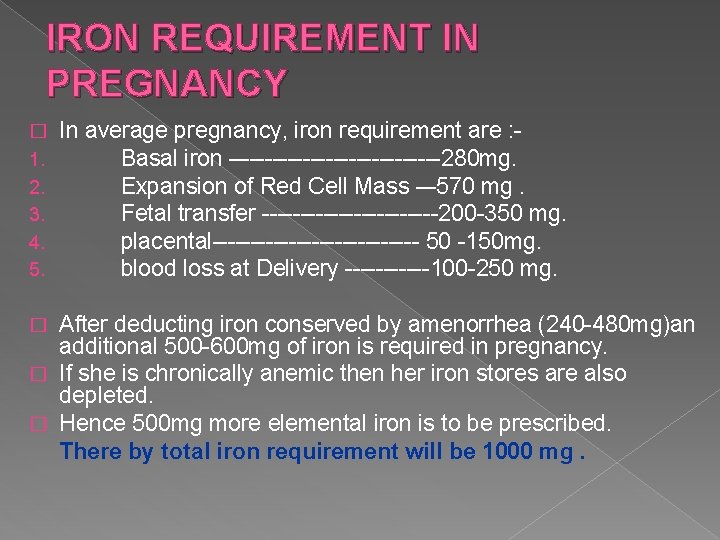
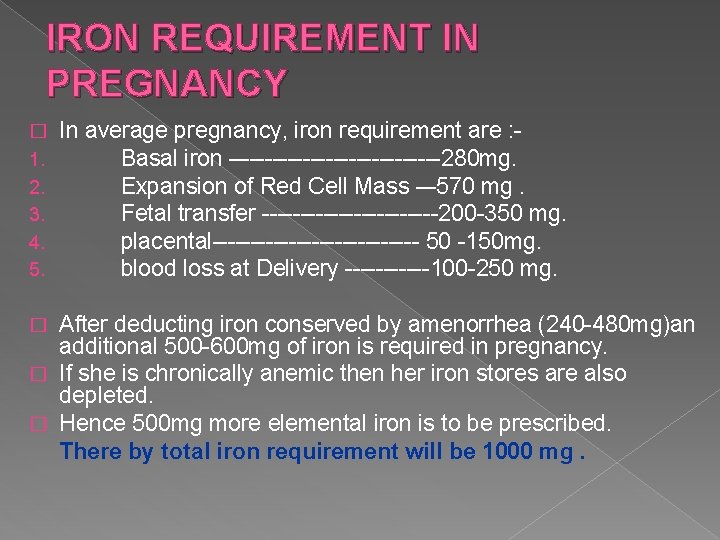
IRON REQUIREMENT IN PREGNANCY � 1. 2. 3. 4. 5. In average pregnancy, iron requirement are : Basal iron –-------------280 mg. Expansion of Red Cell Mass -– 570 mg. Fetal transfer ------------200 -350 mg. placental-------------- 50 -150 mg. blood loss at Delivery ------100 -250 mg. After deducting iron conserved by amenorrhea (240 -480 mg)an additional 500 -600 mg of iron is required in pregnancy. � If she is chronically anemic then her iron stores are also depleted. � Hence 500 mg more elemental iron is to be prescribed. There by total iron requirement will be 1000 mg. �
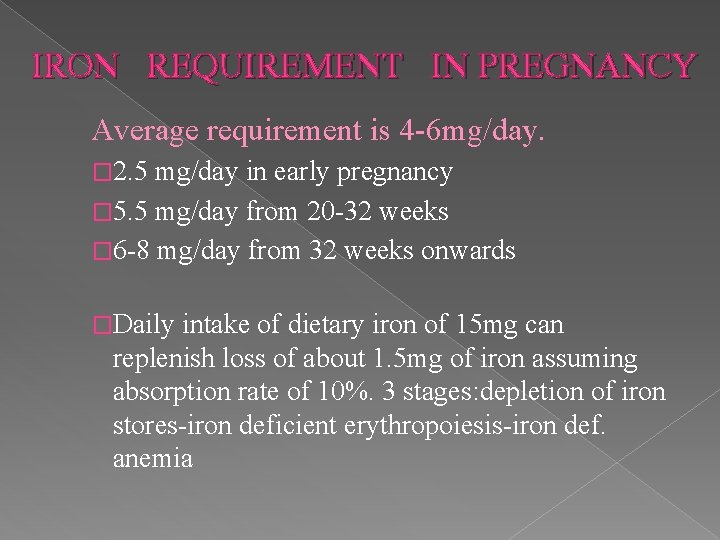
IRON REQUIREMENT IN PREGNANCY Average requirement is 4 -6 mg/day. � 2. 5 mg/day in early pregnancy � 5. 5 mg/day from 20 -32 weeks � 6 -8 mg/day from 32 weeks onwards �Daily intake of dietary iron of 15 mg can replenish loss of about 1. 5 mg of iron assuming absorption rate of 10%. 3 stages: depletion of iron stores-iron deficient erythropoiesis-iron def. anemia
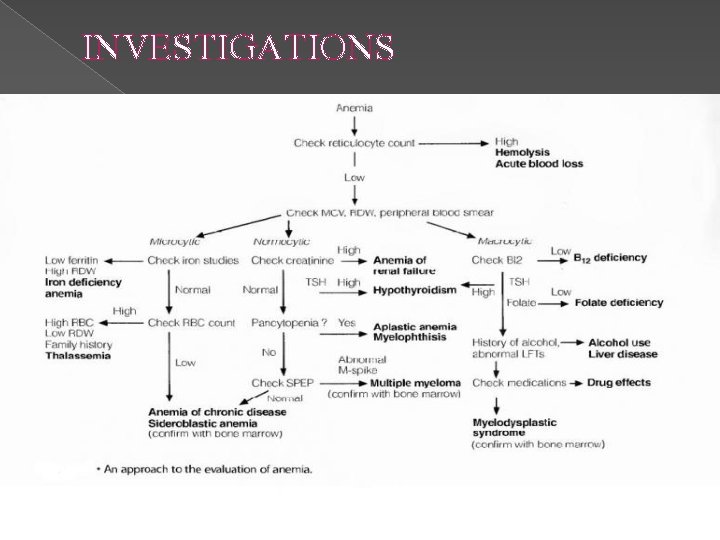
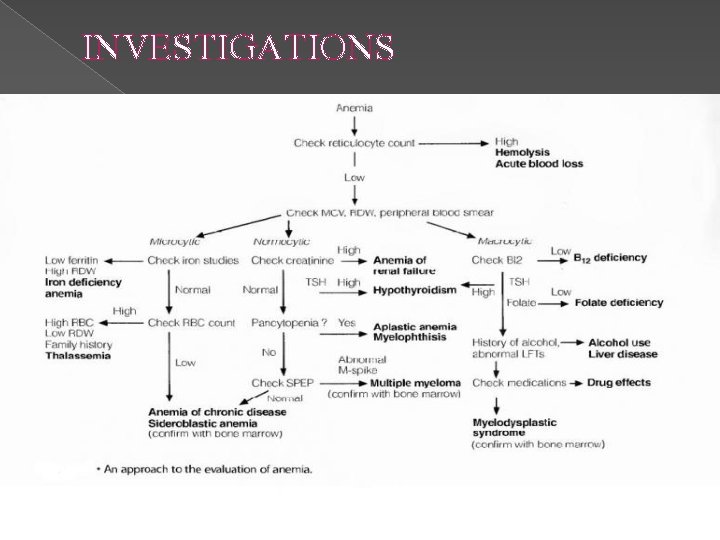
INVESTIGATIONS
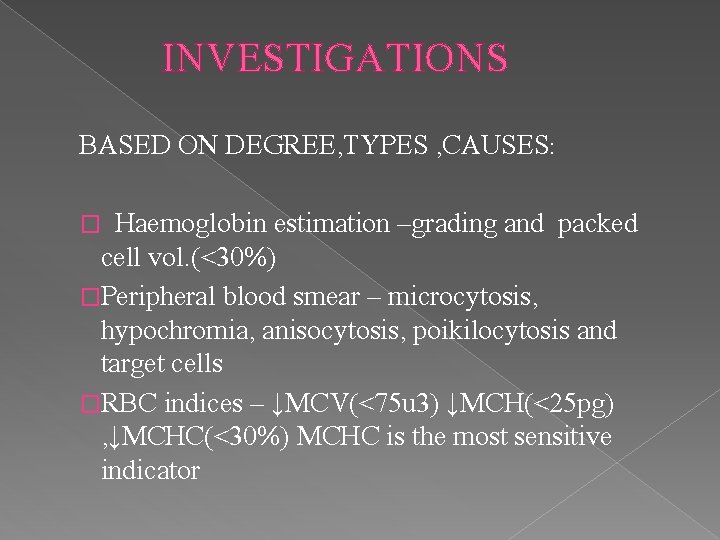
INVESTIGATIONS BASED ON DEGREE, TYPES , CAUSES: Haemoglobin estimation –grading and packed cell vol. (<30%) �Peripheral blood smear – microcytosis, hypochromia, anisocytosis, poikilocytosis and target cells �RBC indices – ↓MCV(<75 u 3) ↓MCH(<25 pg) , ↓MCHC(<30%) MCHC is the most sensitive indicator �
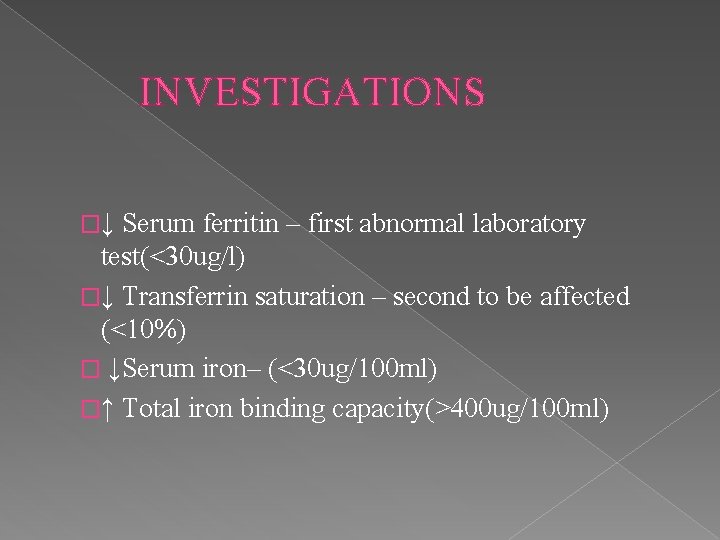
INVESTIGATIONS �↓ Serum ferritin – first abnormal laboratory test(<30 ug/l) �↓ Transferrin saturation – second to be affected (<10%) � ↓Serum iron– (<30 ug/100 ml) �↑ Total iron binding capacity(>400 ug/100 ml)
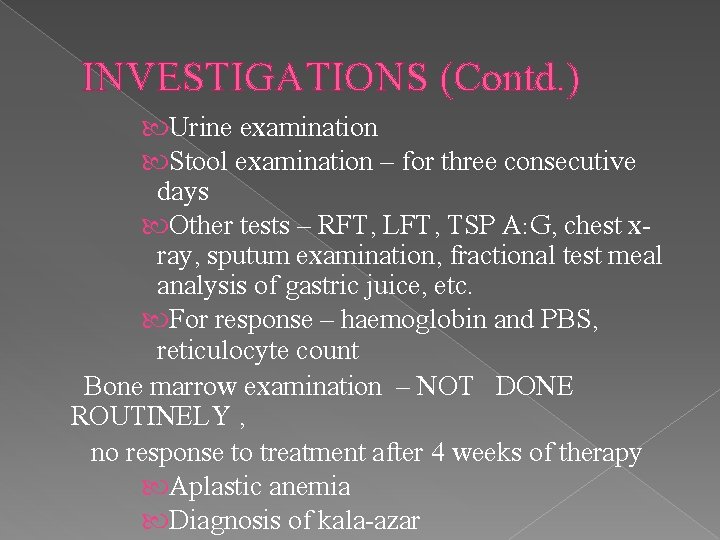
INVESTIGATIONS (Contd. ) Urine examination Stool examination – for three consecutive days Other tests – RFT, LFT, TSP A: G, chest xray, sputum examination, fractional test meal analysis of gastric juice, etc. For response – haemoglobin and PBS, reticulocyte count Bone marrow examination – NOT DONE ROUTINELY , no response to treatment after 4 weeks of therapy Aplastic anemia Diagnosis of kala-azar
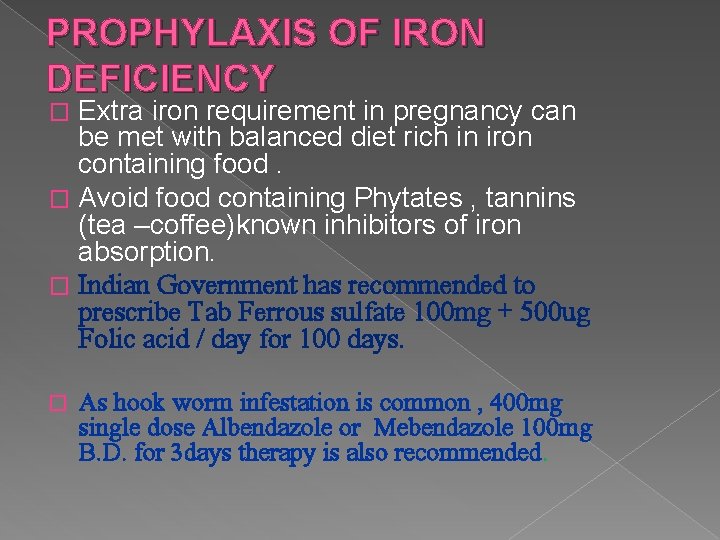
PROPHYLAXIS OF IRON DEFICIENCY Extra iron requirement in pregnancy can be met with balanced diet rich in iron containing food. � Avoid food containing Phytates , tannins (tea –coffee)known inhibitors of iron absorption. � Indian Government has recommended to prescribe Tab Ferrous sulfate 100 mg + 500 ug Folic acid / day for 100 days. � � As hook worm infestation is common , 400 mg single dose Albendazole or Mebendazole 100 mg B. D. for 3 days therapy is also recommended.
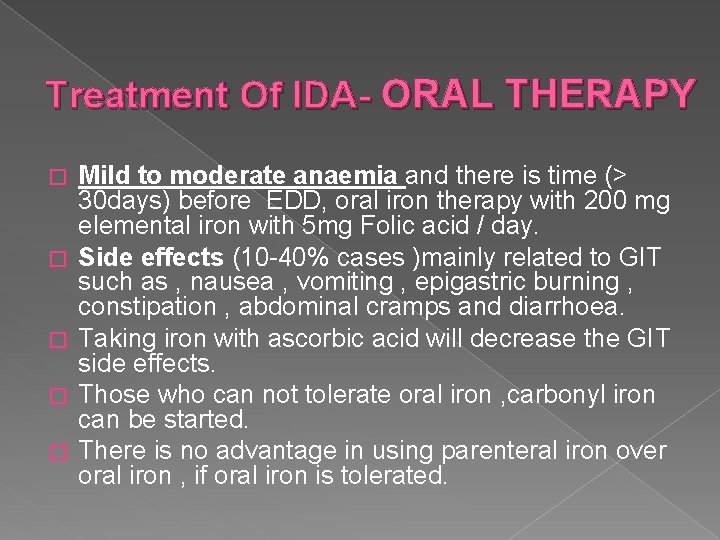
Treatment Of IDA- ORAL THERAPY � � � Mild to moderate anaemia and there is time (> 30 days) before EDD, oral iron therapy with 200 mg elemental iron with 5 mg Folic acid / day. Side effects (10 -40% cases )mainly related to GIT such as , nausea , vomiting , epigastric burning , constipation , abdominal cramps and diarrhoea. Taking iron with ascorbic acid will decrease the GIT side effects. Those who can not tolerate oral iron , carbonyl iron can be started. There is no advantage in using parenteral iron over oral iron , if oral iron is tolerated.

PARENTERAL THERAPY INDICATIONS: � Poor tolerance to oral therapy. � Poor absorption of iron like in chronic diarrhea, ulcerative colitis, coeliac disease or inflammatory bowel disease. � Non compliance � Oral iron is not effective � Women near term with severe anemia. � Presence of concurrent disease like chronic renal failure when patient is on hemodialysis or being treated with erythropoietin.
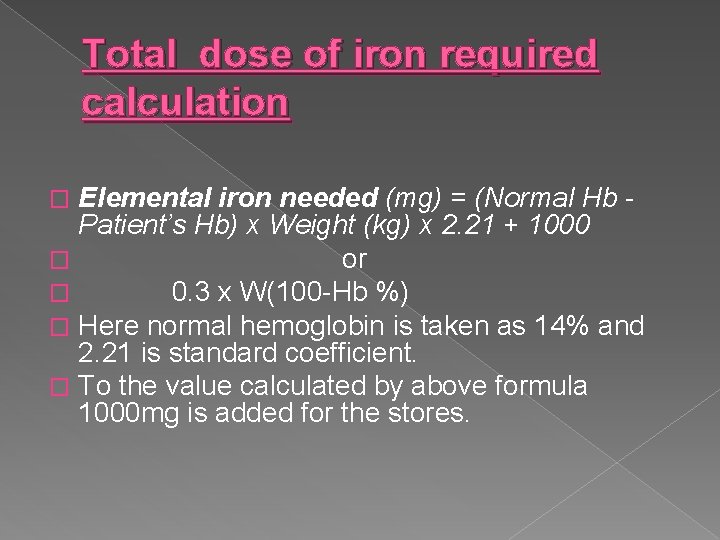
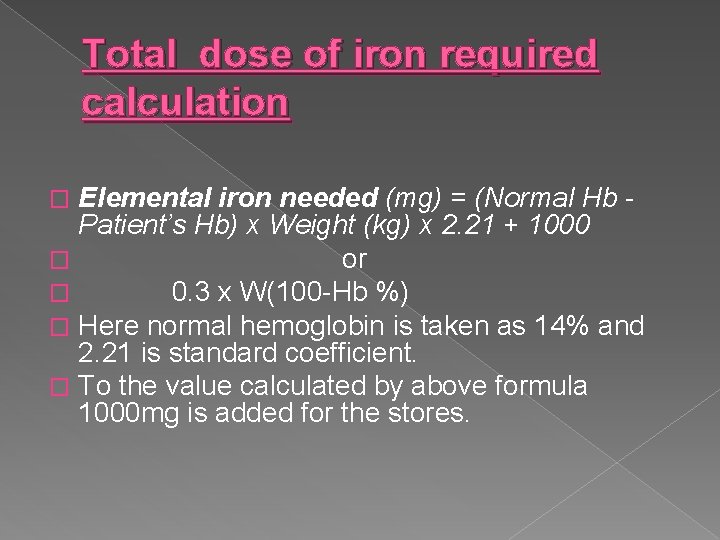
Total dose of iron required calculation Elemental iron needed (mg) = (Normal Hb Patient’s Hb) x Weight (kg) x 2. 21 + 1000 � or � 0. 3 x W(100 -Hb %) � Here normal hemoglobin is taken as 14% and 2. 21 is standard coefficient. � To the value calculated by above formula 1000 mg is added for the stores. �
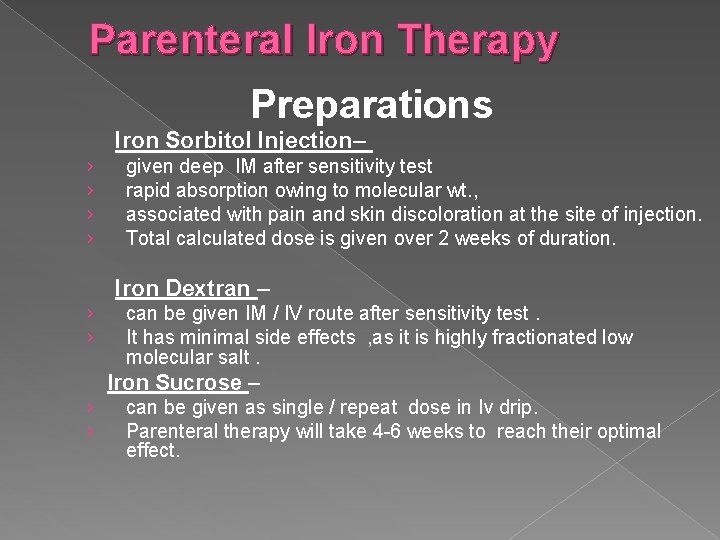
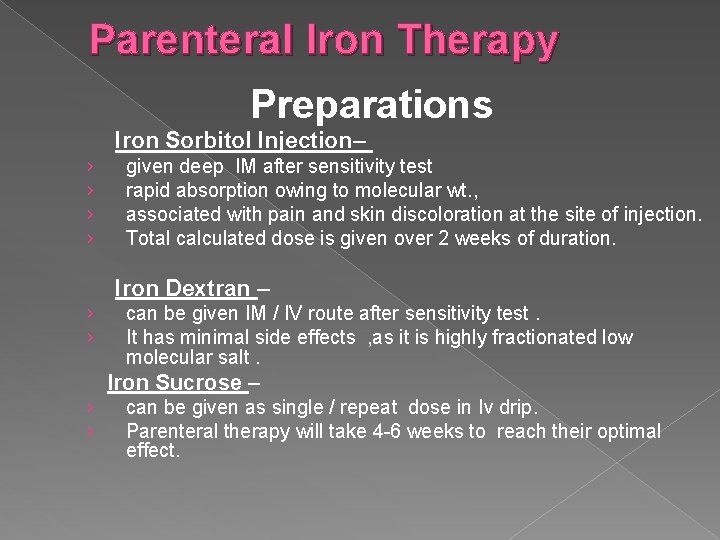
Parenteral Iron Therapy Preparations Iron Sorbitol Injection– › › given deep IM after sensitivity test rapid absorption owing to molecular wt. , associated with pain and skin discoloration at the site of injection. Total calculated dose is given over 2 weeks of duration. Iron Dextran – › › can be given IM / IV route after sensitivity test. It has minimal side effects , as it is highly fractionated low molecular salt. Iron Sucrose – › › can be given as single / repeat dose in Iv drip. Parenteral therapy will take 4 -6 weeks to reach their optimal effect.
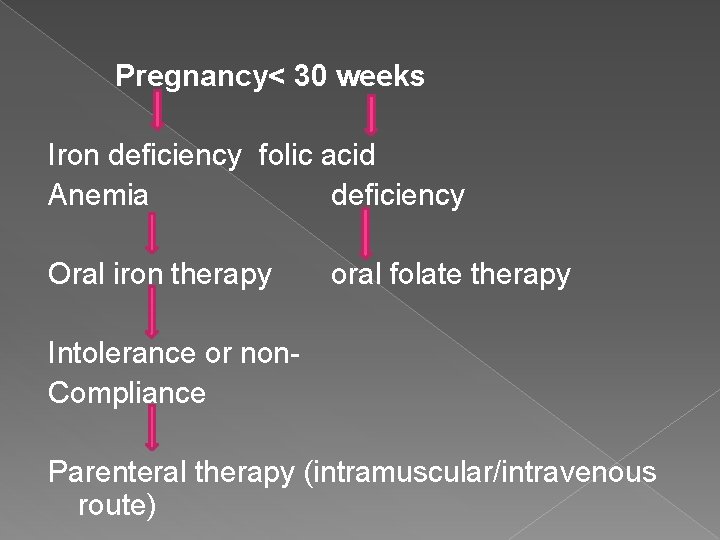
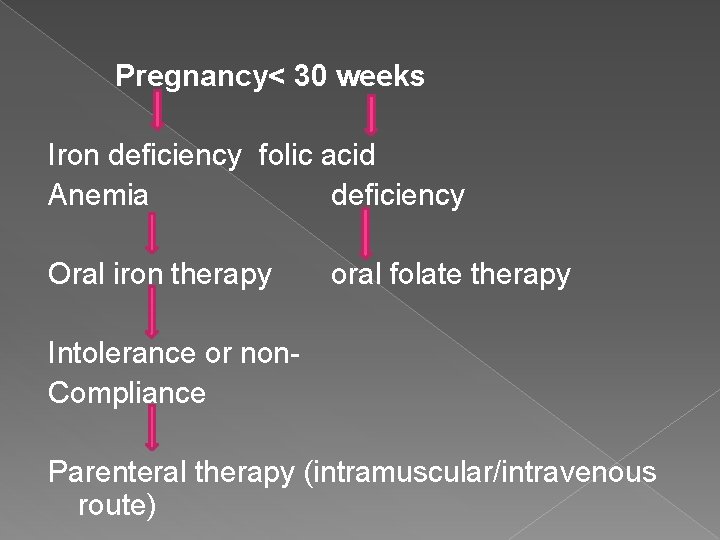
Pregnancy< 30 weeks Iron deficiency folic acid Anemia deficiency Oral iron therapy oral folate therapy Intolerance or non. Compliance Parenteral therapy (intramuscular/intravenous route)
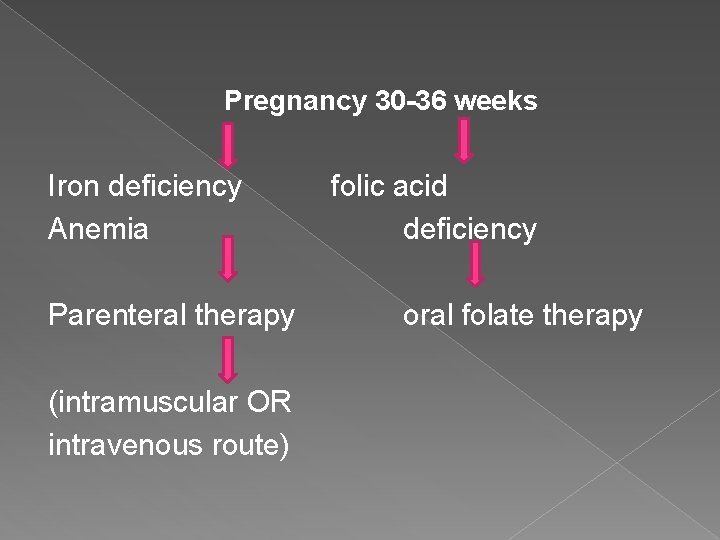
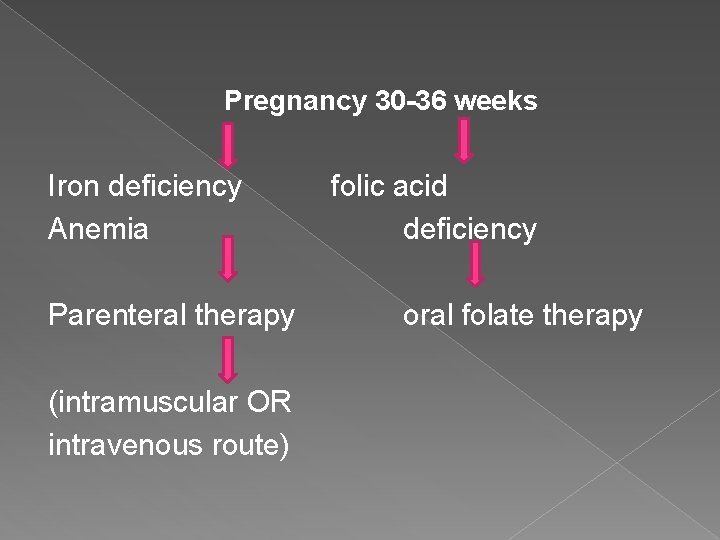
Pregnancy 30 -36 weeks Iron deficiency Anemia Parenteral therapy (intramuscular OR intravenous route) folic acid deficiency oral folate therapy
Pregnancy >36 weeks BLOOD TRANSFUSION
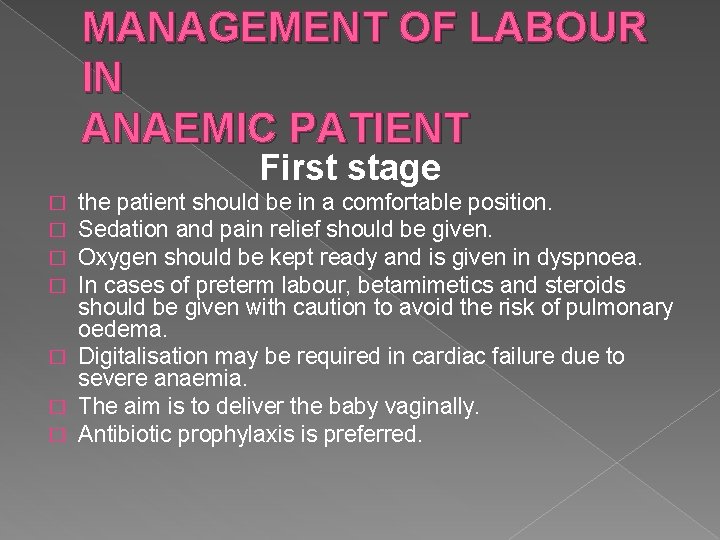
MANAGEMENT OF LABOUR IN ANAEMIC PATIENT First stage the patient should be in a comfortable position. Sedation and pain relief should be given. Oxygen should be kept ready and is given in dyspnoea. In cases of preterm labour, betamimetics and steroids should be given with caution to avoid the risk of pulmonary oedema. � Digitalisation may be required in cardiac failure due to severe anaemia. � The aim is to deliver the baby vaginally. � Antibiotic prophylaxis is preferred. � �
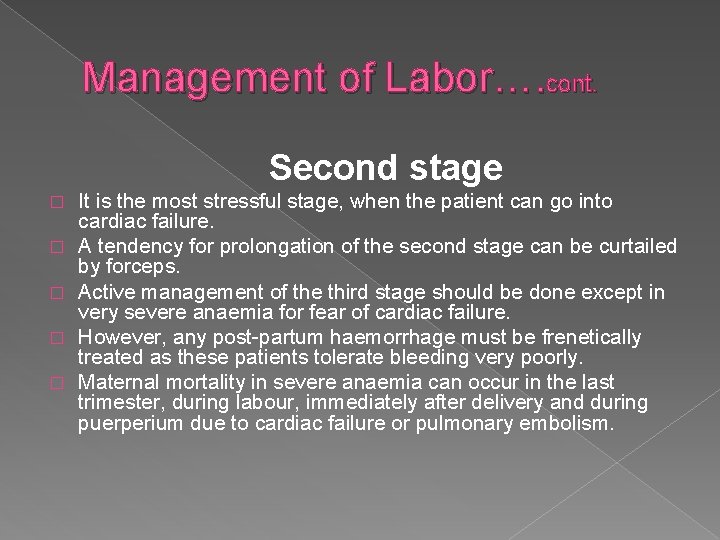
Management of Labor…. cont. Second stage � � � It is the most stressful stage, when the patient can go into cardiac failure. A tendency for prolongation of the second stage can be curtailed by forceps. Active management of the third stage should be done except in very severe anaemia for fear of cardiac failure. However, any post-partum haemorrhage must be frenetically treated as these patients tolerate bleeding very poorly. Maternal mortality in severe anaemia can occur in the last trimester, during labour, immediately after delivery and during puerperium due to cardiac failure or pulmonary embolism.
PUERPERIUM � The mother should have adequate rest; � Iron and folate therapy should be continued for least 3 months. � Any infection must be treated. � Puerperal sepsis, failing lactation, subinvolution of uterus and thromboembolism are more common in these patients.
CONTRACEPTION � � � The anemic patient must use an effective method of contraception and should not conceive for at least 2 years giving time for Iron stores to recover. Sterilization is preferred if the family is completed. If there is no history of menorrhagia, an intra-uterine device can be inserted. Levonorgestrel intrauterine device (Mirena) can be used in presence of menorrhagia for contraception. It reduces blood loss but is expensive. Barrier methods can be safely given, but their higher failure rate is a disadvantage.

THANK YOU
 Priya malik and tanu malik
Priya malik and tanu malik Definition of spotting during pregnancy
Definition of spotting during pregnancy Nucleosome
Nucleosome Iron deficiency anemia
Iron deficiency anemia Kolonychia
Kolonychia Causes of iron deficiency
Causes of iron deficiency Anemia tibc ferritin iron
Anemia tibc ferritin iron Iron deficiency anemia smear
Iron deficiency anemia smear Iron deficiency anemia smear
Iron deficiency anemia smear Dactylitis
Dactylitis Dashod dog
Dashod dog Microcytic hypochromic anemia
Microcytic hypochromic anemia Labs for iron deficiency anemia
Labs for iron deficiency anemia Osmotic fragility test tube color
Osmotic fragility test tube color Low ferritin symptoms
Low ferritin symptoms Iron studies interpretation
Iron studies interpretation Investigation of megaloblastic anemia
Investigation of megaloblastic anemia Nutrient deficiency
Nutrient deficiency Iron sharpens iron friendship
Iron sharpens iron friendship Mass of iron in an iron tablet
Mass of iron in an iron tablet Types of anaemia
Types of anaemia Acute megaloblastic anemia
Acute megaloblastic anemia Koilonchiya
Koilonchiya Grades of anemia
Grades of anemia Codominance
Codominance Macrocytic non megaloblastic anemia
Macrocytic non megaloblastic anemia Difference between sickle cell anaemia and thalassemia
Difference between sickle cell anaemia and thalassemia Ovalomacrocytosis
Ovalomacrocytosis Microcytic tails
Microcytic tails Twin anaemia polycythaemia sequence
Twin anaemia polycythaemia sequence Sickle cell anemia codominance
Sickle cell anemia codominance Zaid malik md
Zaid malik md Malik jahan khan
Malik jahan khan Deja and malik
Deja and malik Angel izraeel duty in islam
Angel izraeel duty in islam Ali afzal malik
Ali afzal malik Riena malik
Riena malik Jessup malik abkommen
Jessup malik abkommen Kisah suraqah bin malik
Kisah suraqah bin malik Phenylketoneuria
Phenylketoneuria Saadat malik
Saadat malik Dr salwa malik
Dr salwa malik Avinash lakshman prashant malik
Avinash lakshman prashant malik Rimsha malik
Rimsha malik