Microcytic Hypochromic Anemia M Qari Differential diagnosis of
- Slides: 33
Microcytic Hypochromic Anemia • M Qari
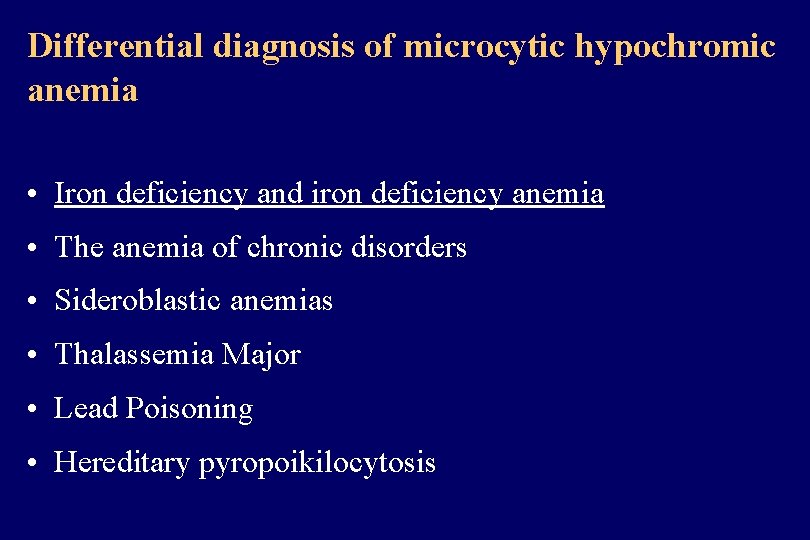
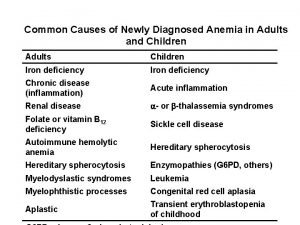
Differential diagnosis of microcytic hypochromic anemia • Iron deficiency and iron deficiency anemia • The anemia of chronic disorders • Sideroblastic anemias • Thalassemia Major • Lead Poisoning • Hereditary pyropoikilocytosis
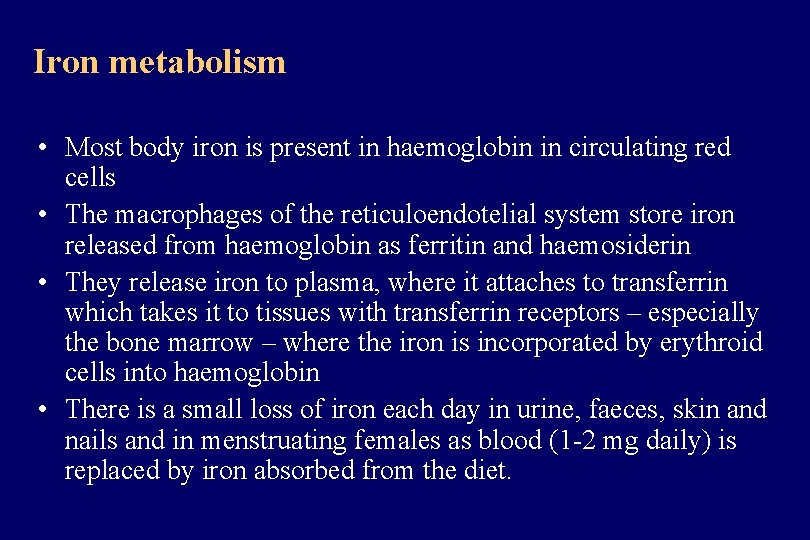
Iron metabolism • Most body iron is present in haemoglobin in circulating red cells • The macrophages of the reticuloendotelial system store iron released from haemoglobin as ferritin and haemosiderin • They release iron to plasma, where it attaches to transferrin which takes it to tissues with transferrin receptors – especially the bone marrow – where the iron is incorporated by erythroid cells into haemoglobin • There is a small loss of iron each day in urine, faeces, skin and nails and in menstruating females as blood (1 -2 mg daily) is replaced by iron absorbed from the diet.
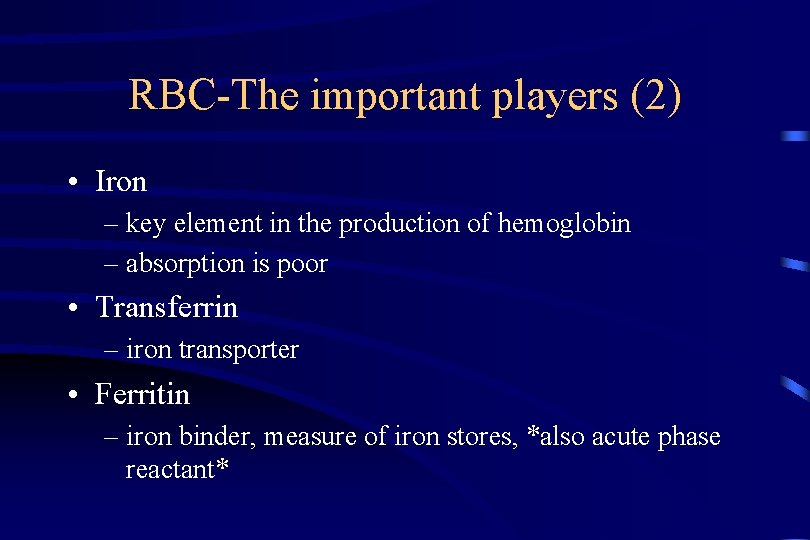
RBC-The important players (2) • Iron – key element in the production of hemoglobin – absorption is poor • Transferrin – iron transporter • Ferritin – iron binder, measure of iron stores, *also acute phase reactant*
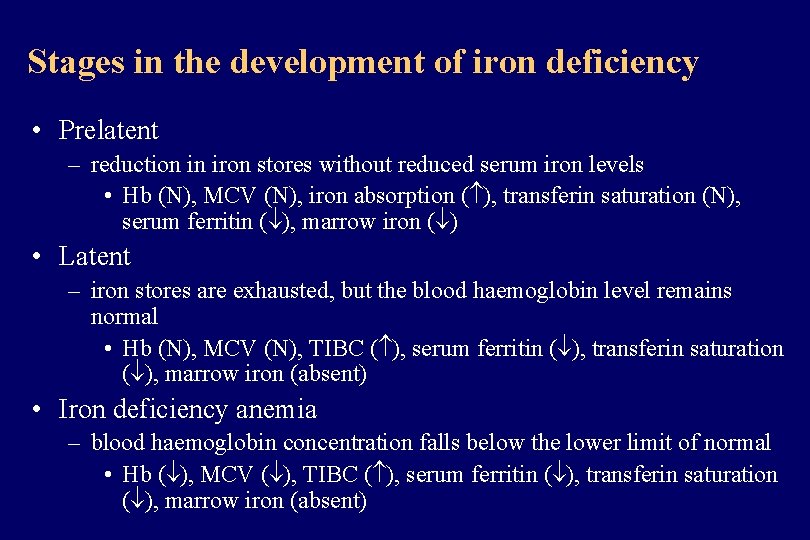
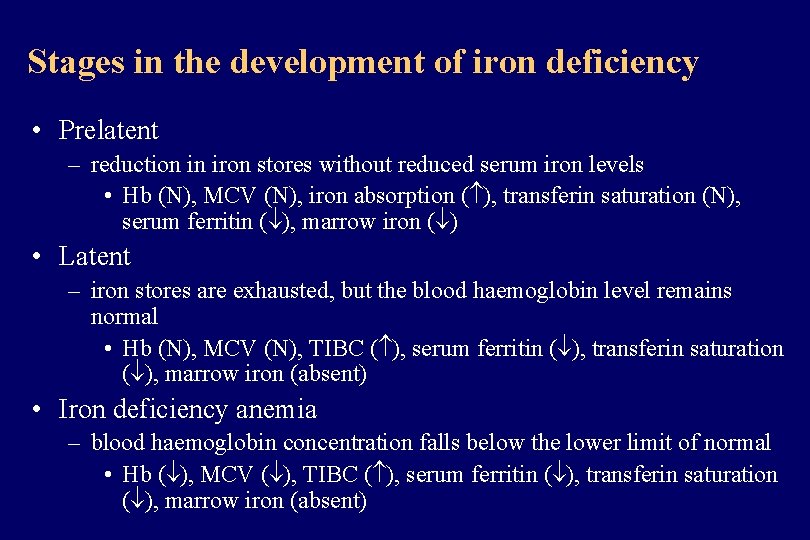
Stages in the development of iron deficiency • Prelatent – reduction in iron stores without reduced serum iron levels • Hb (N), MCV (N), iron absorption ( ), transferin saturation (N), serum ferritin ( ), marrow iron ( ) • Latent – iron stores are exhausted, but the blood haemoglobin level remains normal • Hb (N), MCV (N), TIBC ( ), serum ferritin ( ), transferin saturation ( ), marrow iron (absent) • Iron deficiency anemia – blood haemoglobin concentration falls below the lower limit of normal • Hb ( ), MCV ( ), TIBC ( ), serum ferritin ( ), transferin saturation ( ), marrow iron (absent)
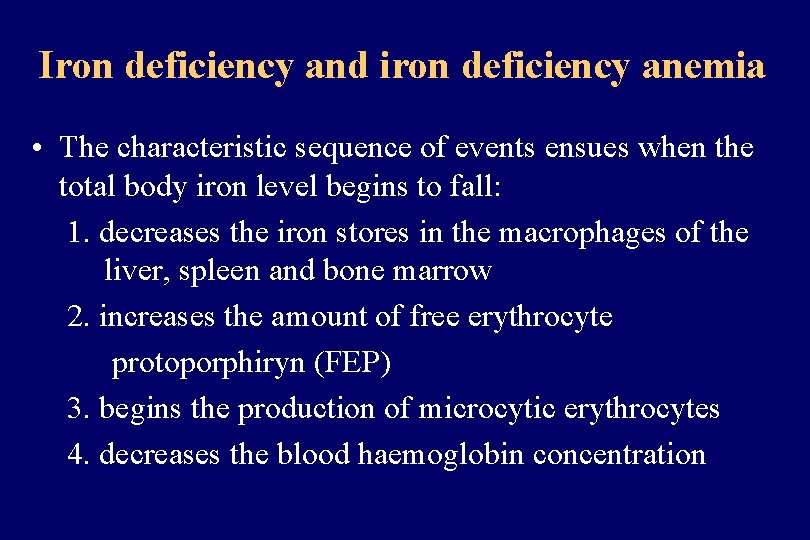
Iron deficiency and iron deficiency anemia • The characteristic sequence of events ensues when the total body iron level begins to fall: 1. decreases the iron stores in the macrophages of the liver, spleen and bone marrow 2. increases the amount of free erythrocyte protoporphiryn (FEP) 3. begins the production of microcytic erythrocytes 4. decreases the blood haemoglobin concentration
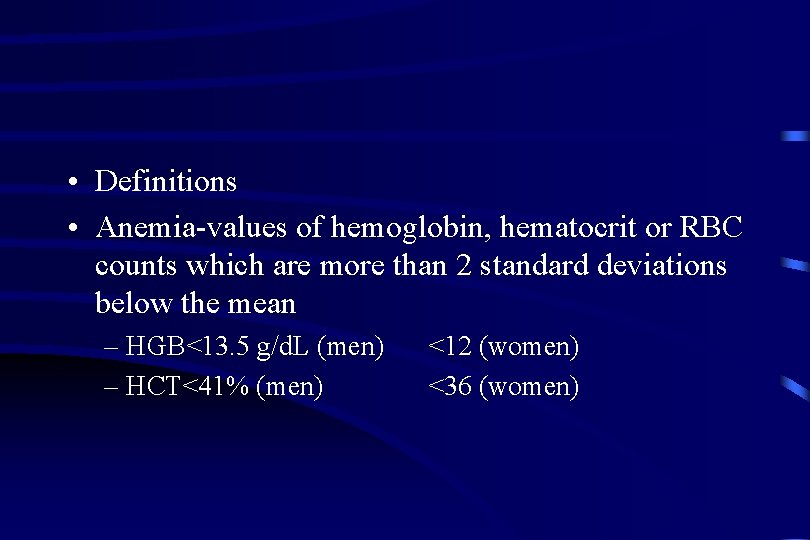
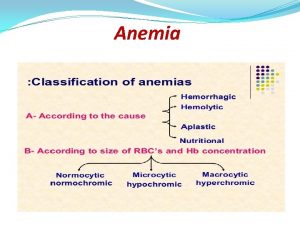
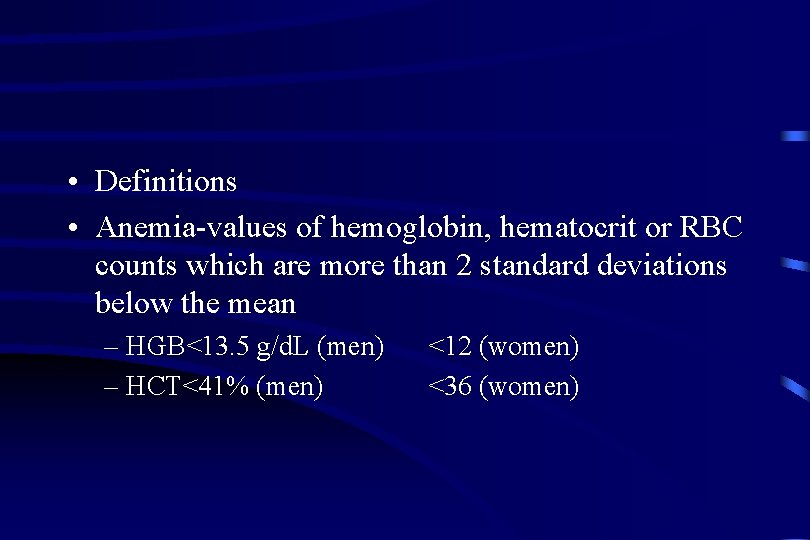
• Definitions • Anemia-values of hemoglobin, hematocrit or RBC counts which are more than 2 standard deviations below the mean – HGB<13. 5 g/d. L (men) – HCT<41% (men) <12 (women) <36 (women)
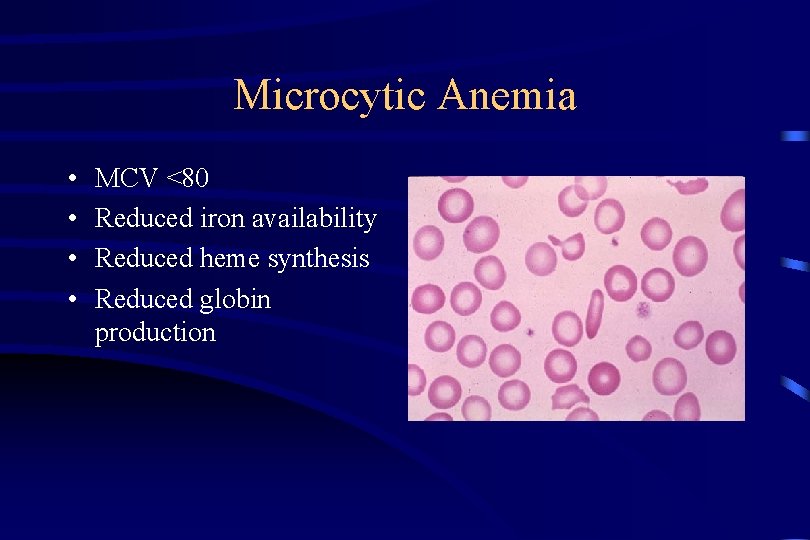
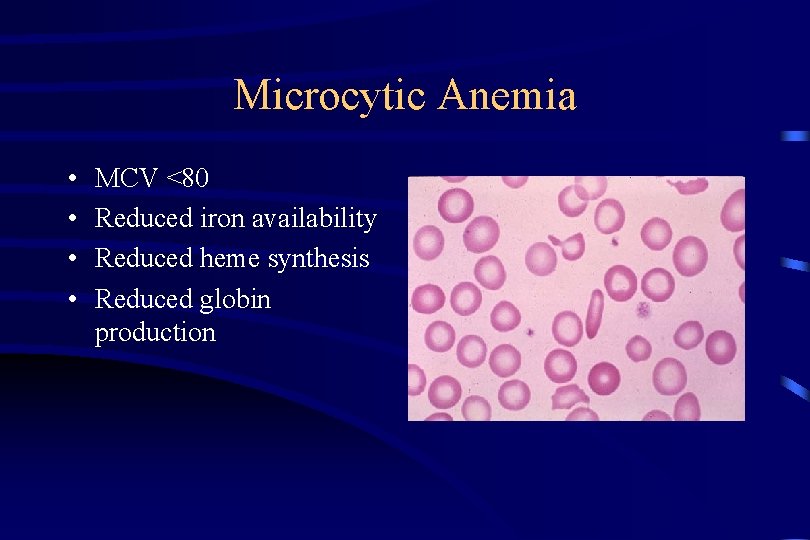
Microcytic Anemia • • MCV <80 Reduced iron availability Reduced heme synthesis Reduced globin production
Microcytic Anemia REDUCED IRON AVAILABILTY • Iron Deficiency – – Deficient Diet/Absorption Increased Requirements Blood Loss Iron Sequestration • Anemia of Chronic Disease – Low serum iron, low TIBC, normal serum ferritin – MANY!! • Chronic infection, inflammation, cancer, liver disease
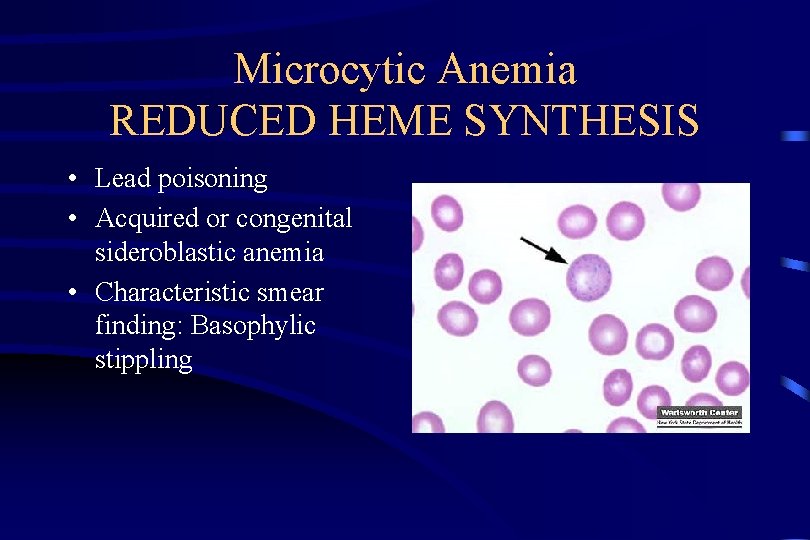
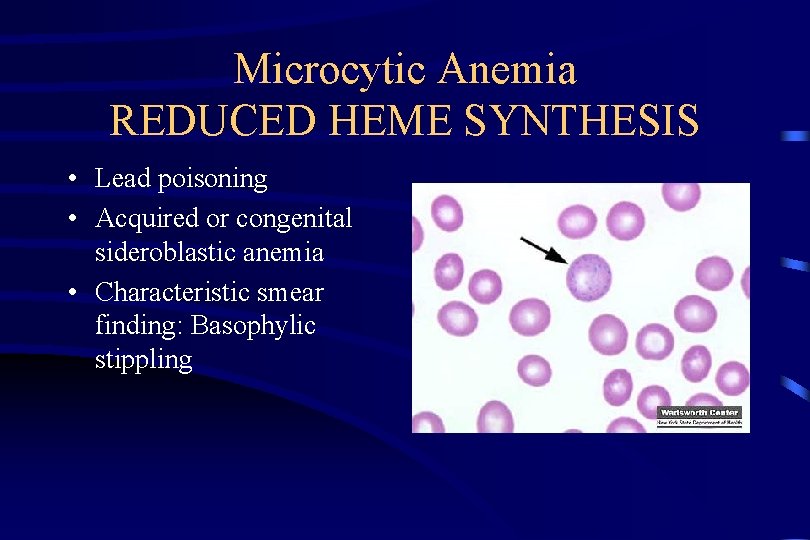
Microcytic Anemia REDUCED HEME SYNTHESIS • Lead poisoning • Acquired or congenital sideroblastic anemia • Characteristic smear finding: Basophylic stippling
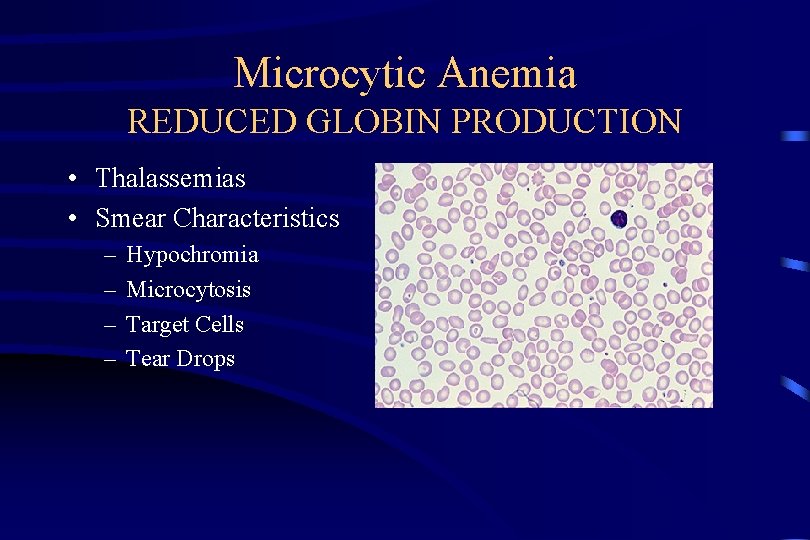
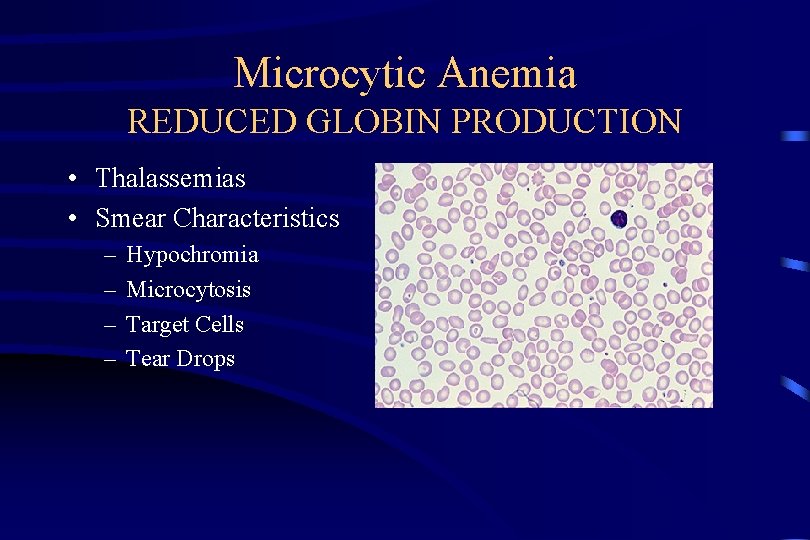
Microcytic Anemia REDUCED GLOBIN PRODUCTION • Thalassemias • Smear Characteristics – – Hypochromia Microcytosis Target Cells Tear Drops
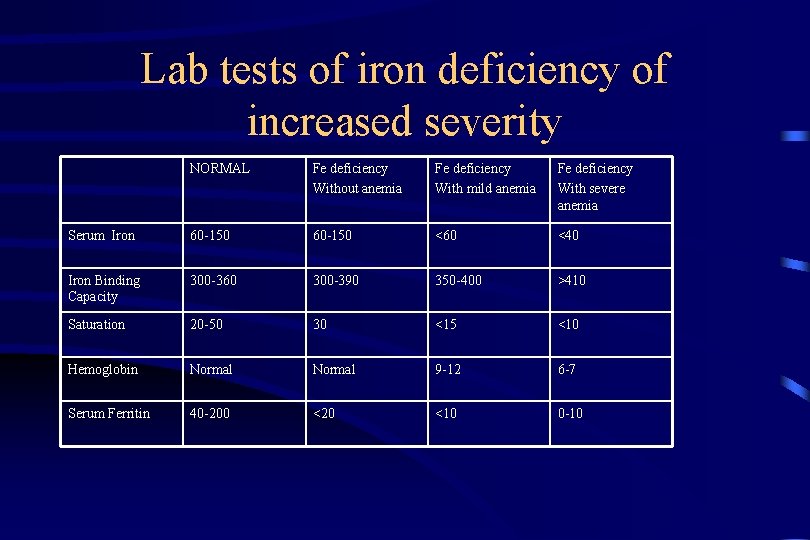
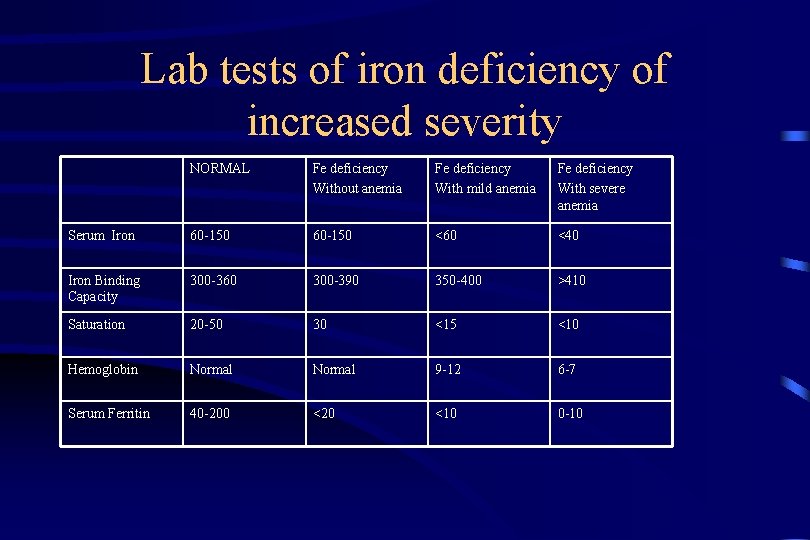
Lab tests of iron deficiency of increased severity NORMAL Fe deficiency Without anemia Fe deficiency With mild anemia Fe deficiency With severe anemia Serum Iron 60 -150 <60 <40 Iron Binding Capacity 300 -360 300 -390 350 -400 >410 Saturation 20 -50 30 <15 <10 Hemoglobin Normal 9 -12 6 -7 Serum Ferritin 40 -200 <20 <10 0 -10
Differential Diagnosis-Revisited • Classification by Pathophysiology – Blood Loss – Decreased Production – Increased Destruction
Iron deficiency anemia Definition and etiologic factors • The end result of a long period of negative iron balance – decreased iron intake • inadequate diet, impaired absorption, gastric surgery, celiac disease – increased iron loss • gastrointestinal bleeding (haemorrhoids, salicylate ingestion, peptic ulcer, neoplasm, ulcerative colitis) • excessive menstrual flow, blood donation, disorders of hemostasis – increased physiologic requirements for iron • infancy, pregnancy, lactation – cause unknown (idiopathic hypochromic anemia)
Iron deficiency anemia Clinical manifestation • Presentation of – underlying disease 37% – anemia symptoms 63%
Evaluation of the Patient • HISTORY – Is the patient bleeding? • Actively? In past? – Is there evidence for increased RBC destruction? – Is the bone marrow suppressed? – Is the patient nutritionally deficient? Pica? – PMH including medication review, toxin exposure
Evaluation of the Patient (2) REVIW OF SYMPTOMS • Decreased oxygen delivery to tissues – – Exertional dyspnea Dyspnea at rest Fatigue Signs and symptoms of hyperdynamic state • Bounding pulses • Palpitations – Life threatening: heart failure, angina, myocardial infarction • Hypovolemia – Fatiguablitiy, postural dizziness, lethargy, hypotension, shock and death
Evaluation of the Patient (3) PHYSICAL EXAM • Stable or Unstable? -ABCs -Vitals • Pallor • Jaundice -hemolysis • Lymphadenopathy • Hepatosplenomegally • Bony Pain • Petechiae • Rectal-? Occult blood
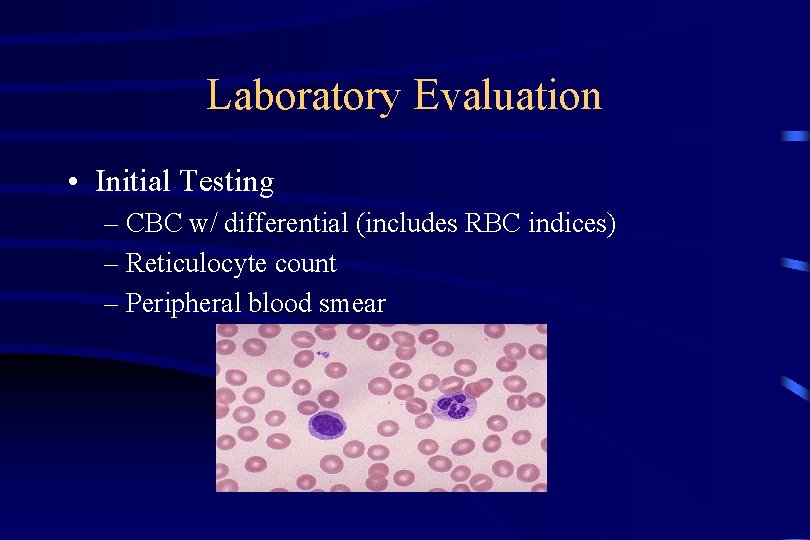
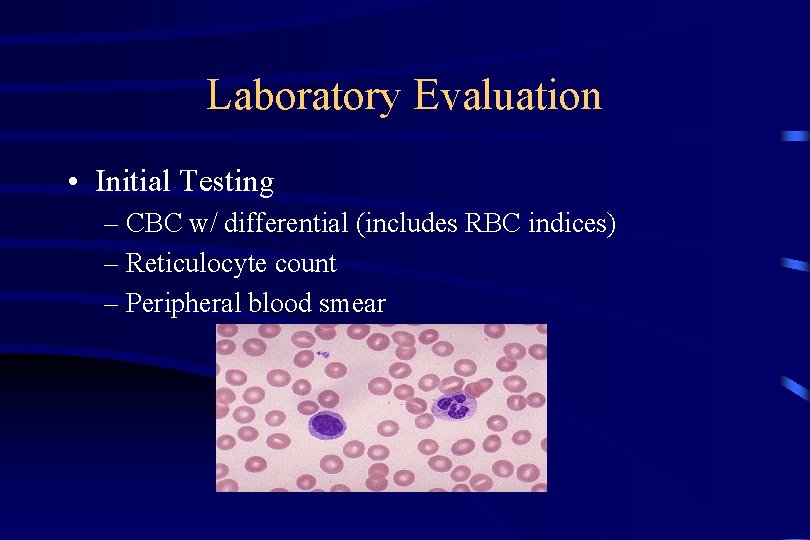
Laboratory Evaluation • Initial Testing – CBC w/ differential (includes RBC indices) – Reticulocyte count – Peripheral blood smear
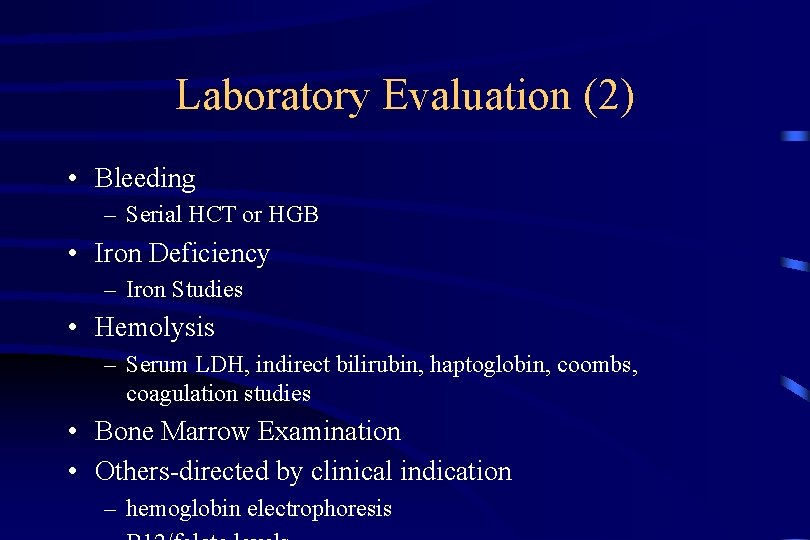
Laboratory Evaluation (2) • Bleeding – Serial HCT or HGB • Iron Deficiency – Iron Studies • Hemolysis – Serum LDH, indirect bilirubin, haptoglobin, coombs, coagulation studies • Bone Marrow Examination • Others-directed by clinical indication – hemoglobin electrophoresis
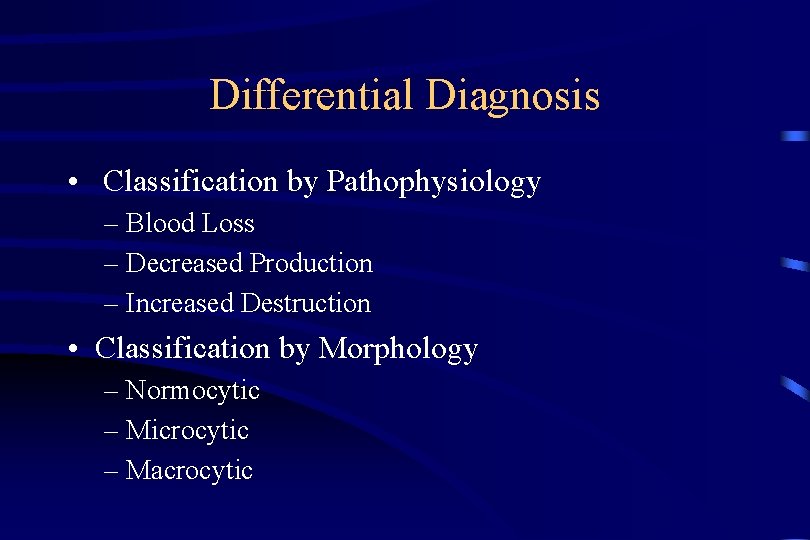
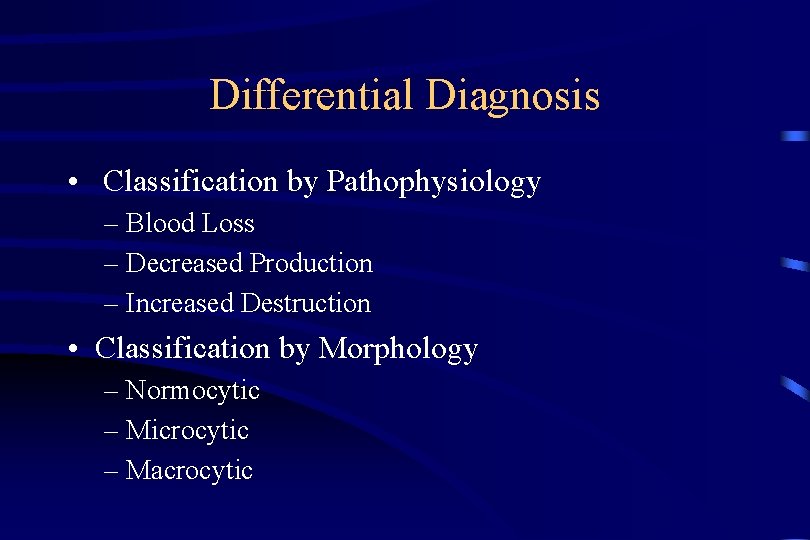
Differential Diagnosis • Classification by Pathophysiology – Blood Loss – Decreased Production – Increased Destruction • Classification by Morphology – Normocytic – Microcytic – Macrocytic
Symptoms of anemia • • Fatigue Dizziness Headache Palpitation Dyspnea Lethargy Disturbances in menstruation Impaired growth in infancy
Symptoms of iron deficiency • • Irritability Poor attention span Lack interest in surroundings Poor work performance Behavioural disturbances Pica Defective structure and function of epithelial tissue – especially affected are the hair, the skin, the nails, the tongue, the mouth, the hypopharynx and the stomach • Increased frequency of infection
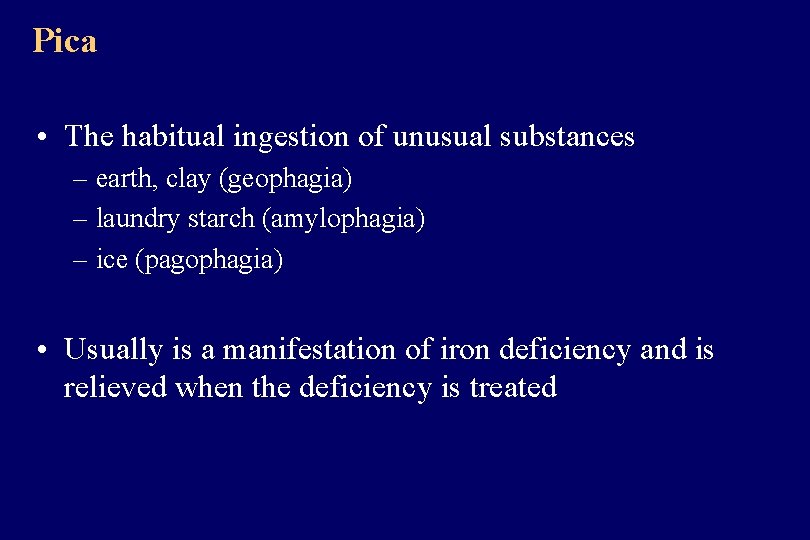
Pica • The habitual ingestion of unusual substances – earth, clay (geophagia) – laundry starch (amylophagia) – ice (pagophagia) • Usually is a manifestation of iron deficiency and is relieved when the deficiency is treated
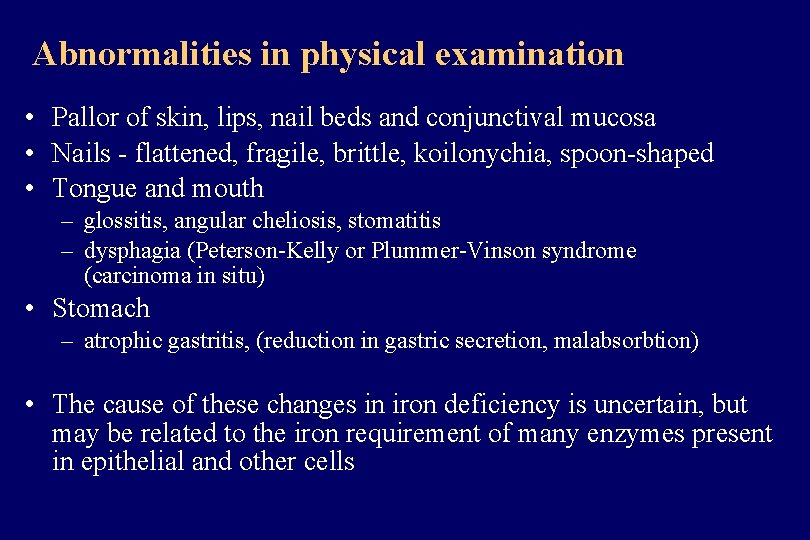
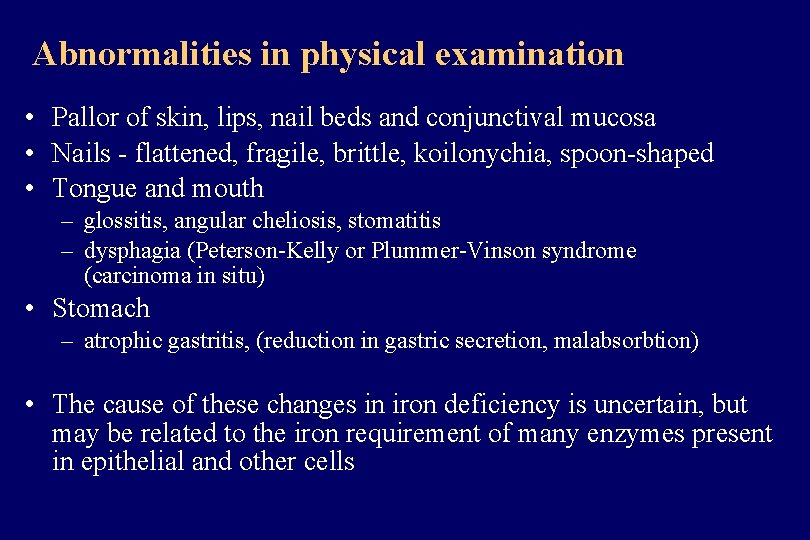
Abnormalities in physical examination • Pallor of skin, lips, nail beds and conjunctival mucosa • Nails - flattened, fragile, brittle, koilonychia, spoon-shaped • Tongue and mouth – glossitis, angular cheliosis, stomatitis – dysphagia (Peterson-Kelly or Plummer-Vinson syndrome (carcinoma in situ) • Stomach – atrophic gastritis, (reduction in gastric secretion, malabsorbtion) • The cause of these changes in iron deficiency is uncertain, but may be related to the iron requirement of many enzymes present in epithelial and other cells
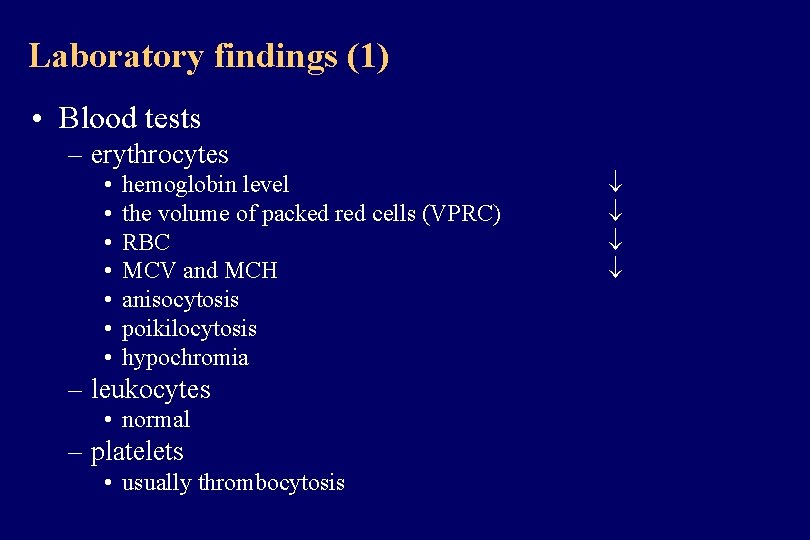
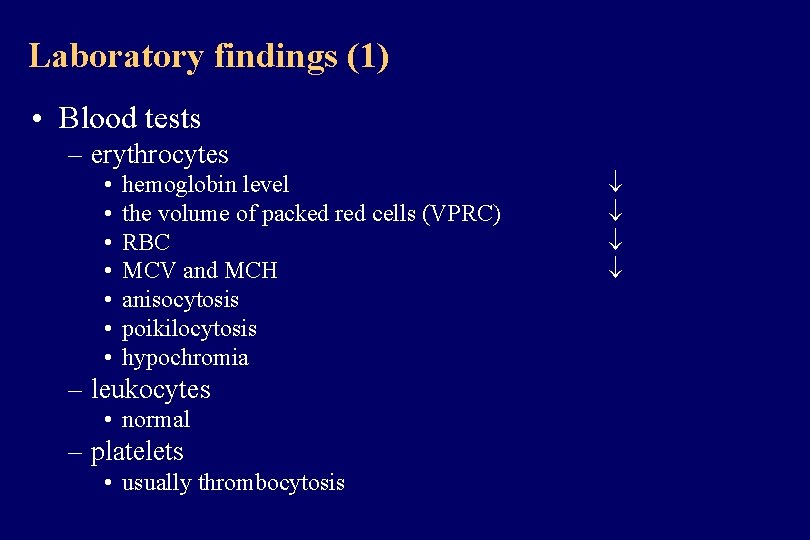
Laboratory findings (1) • Blood tests – erythrocytes • • hemoglobin level the volume of packed red cells (VPRC) RBC MCV and MCH anisocytosis poikilocytosis hypochromia – leukocytes • normal – platelets • usually thrombocytosis
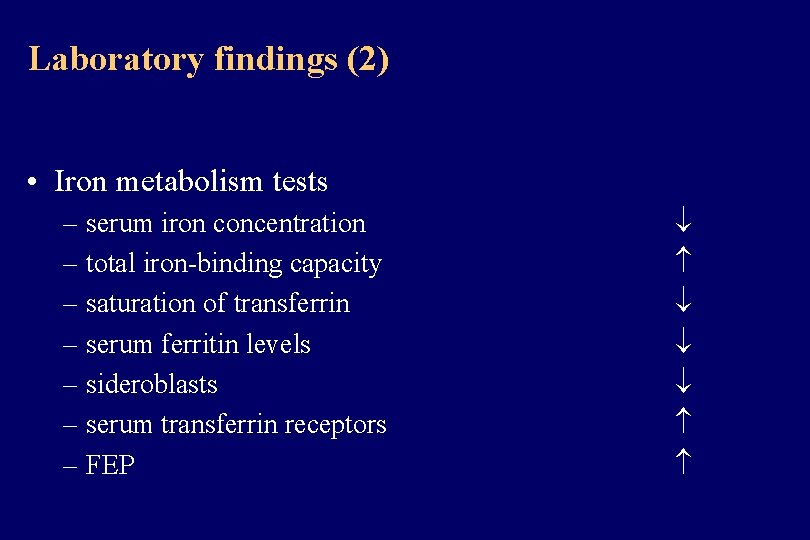
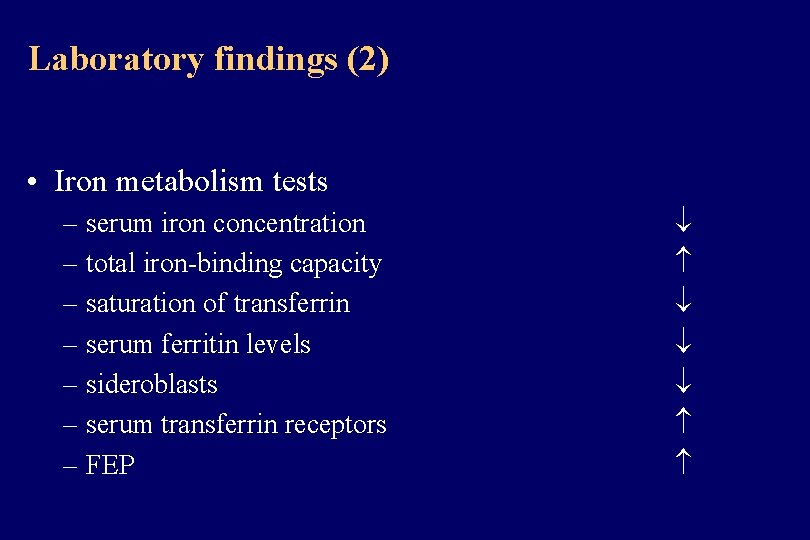
Laboratory findings (2) • Iron metabolism tests – serum iron concentration – total iron-binding capacity – saturation of transferrin – serum ferritin levels – sideroblasts – serum transferrin receptors – FEP
Management of iron deficiency anemia • Correction of the iron deficiency – orally – intramuscularly – intravenously • Treatment of the underlying disease
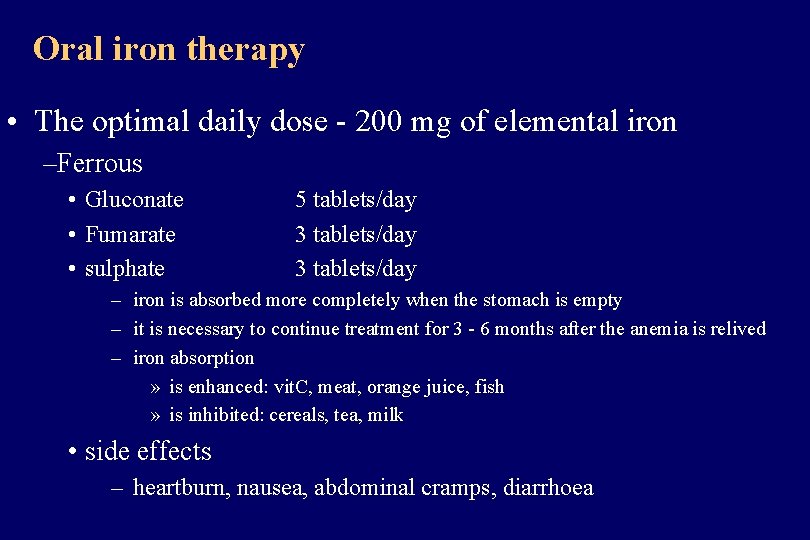
Oral iron therapy • The optimal daily dose - 200 mg of elemental iron –Ferrous • Gluconate • Fumarate • sulphate 5 tablets/day 3 tablets/day – iron is absorbed more completely when the stomach is empty – it is necessary to continue treatment for 3 - 6 months after the anemia is relived – iron absorption » is enhanced: vit. C, meat, orange juice, fish » is inhibited: cereals, tea, milk • side effects – heartburn, nausea, abdominal cramps, diarrhoea
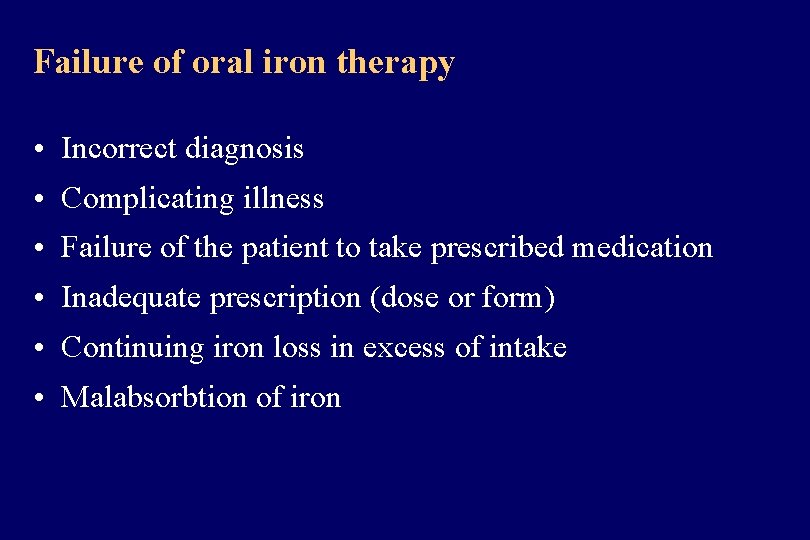
Failure of oral iron therapy • Incorrect diagnosis • Complicating illness • Failure of the patient to take prescribed medication • Inadequate prescription (dose or form) • Continuing iron loss in excess of intake • Malabsorbtion of iron
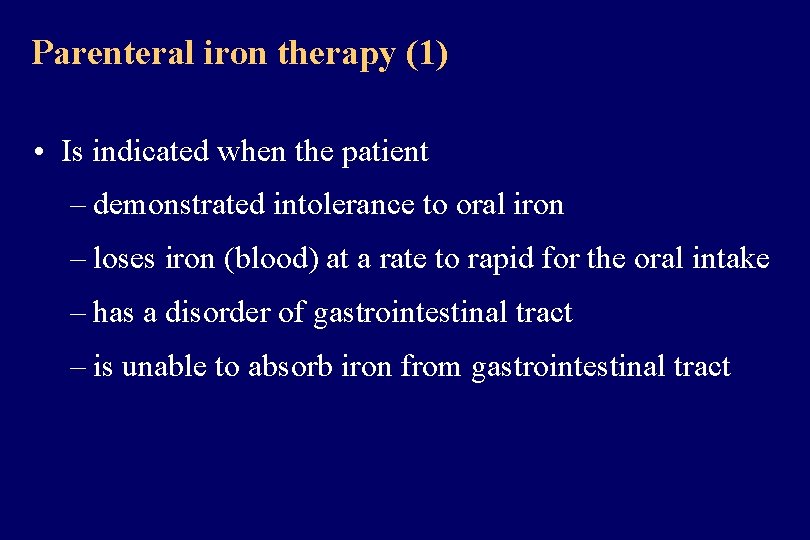
Parenteral iron therapy (1) • Is indicated when the patient – demonstrated intolerance to oral iron – loses iron (blood) at a rate to rapid for the oral intake – has a disorder of gastrointestinal tract – is unable to absorb iron from gastrointestinal tract
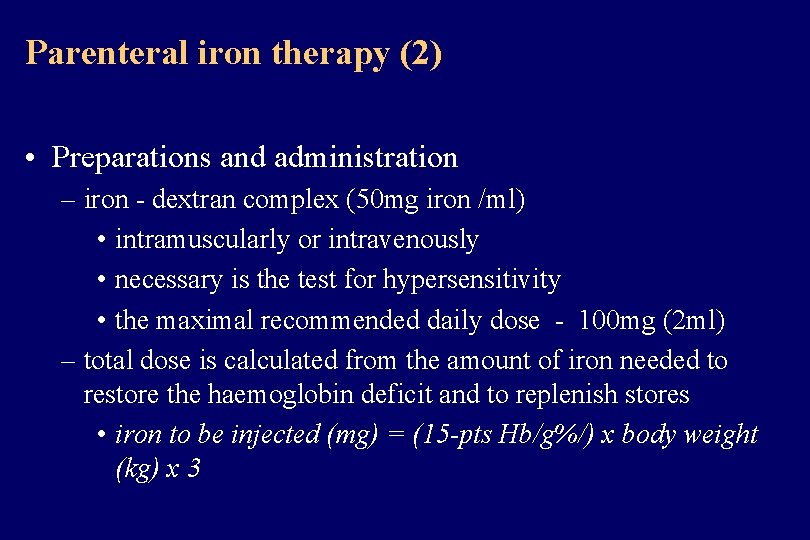
Parenteral iron therapy (2) • Preparations and administration – iron - dextran complex (50 mg iron /ml) • intramuscularly or intravenously • necessary is the test for hypersensitivity • the maximal recommended daily dose - 100 mg (2 ml) – total dose is calculated from the amount of iron needed to restore the haemoglobin deficit and to replenish stores • iron to be injected (mg) = (15 -pts Hb/g%/) x body weight (kg) x 3
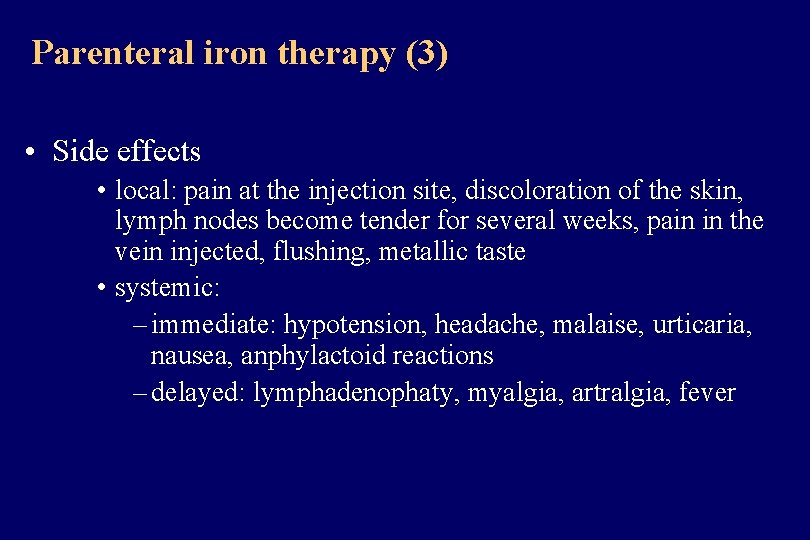
Parenteral iron therapy (3) • Side effects • local: pain at the injection site, discoloration of the skin, lymph nodes become tender for several weeks, pain in the vein injected, flushing, metallic taste • systemic: – immediate: hypotension, headache, malaise, urticaria, nausea, anphylactoid reactions – delayed: lymphadenophaty, myalgia, artralgia, fever
 Lab tests for anemia
Lab tests for anemia Causes of iron deficiency
Causes of iron deficiency Normocytic hypochromic anemia differential diagnosis
Normocytic hypochromic anemia differential diagnosis Microcytic hypochromic picture
Microcytic hypochromic picture Treatment of microcytic anemia
Treatment of microcytic anemia Macrocytic anemia symptoms
Macrocytic anemia symptoms Minal barve md
Minal barve md Macrocytic hypochromic anemia
Macrocytic hypochromic anemia Iron deficiency anemia differential diagnosis
Iron deficiency anemia differential diagnosis Aaaaeeeeoooo
Aaaaeeeeoooo Qari course syllabus
Qari course syllabus Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia Causes of macrocytic anemia
Causes of macrocytic anemia Low iron causes
Low iron causes Hematology cell counters
Hematology cell counters Feroba you
Feroba you Rbc inclusions
Rbc inclusions Hypochromic red cells
Hypochromic red cells Hypochromic red cells
Hypochromic red cells Hypochromic red cells
Hypochromic red cells Nursing process objectives
Nursing process objectives Steps of nursing process
Steps of nursing process Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Second phase of nursing process
Second phase of nursing process Medafile
Medafile Inguinal lymph nodes
Inguinal lymph nodes Hanifin rajka atopic dermatitis
Hanifin rajka atopic dermatitis Differential diagnosis for leukoplakia
Differential diagnosis for leukoplakia Tripple therapy
Tripple therapy Occlusio pupillae definition
Occlusio pupillae definition Coffee ground emesis
Coffee ground emesis Leukocoria differential diagnosis
Leukocoria differential diagnosis Bakers cyst differential diagnosis
Bakers cyst differential diagnosis