Iron Deficiency Anemia Prof Dr Teoman SOYSAL Iron
- Slides: 34
Iron Deficiency Anemia Prof. Dr. Teoman SOYSAL
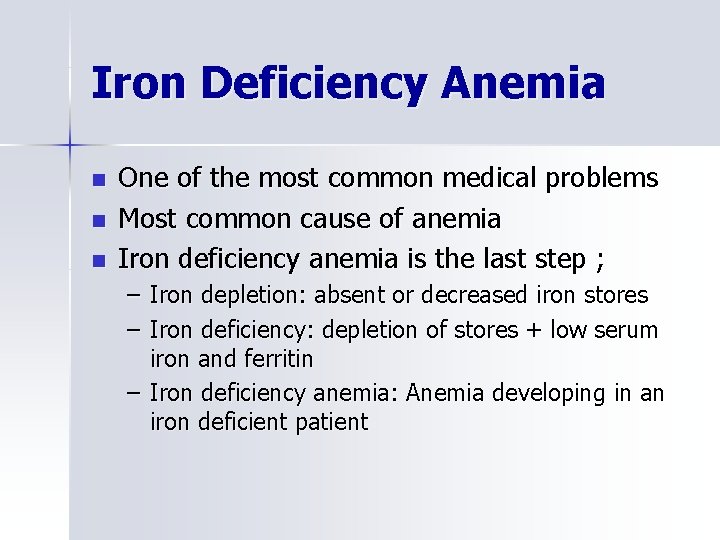
Iron Deficiency Anemia n n n One of the most common medical problems Most common cause of anemia Iron deficiency anemia is the last step ; – Iron depletion: absent or decreased iron stores – Iron deficiency: depletion of stores + low serum iron and ferritin – Iron deficiency anemia: Anemia developing in an iron deficient patient
Total amount of body iron: 3 -5 g
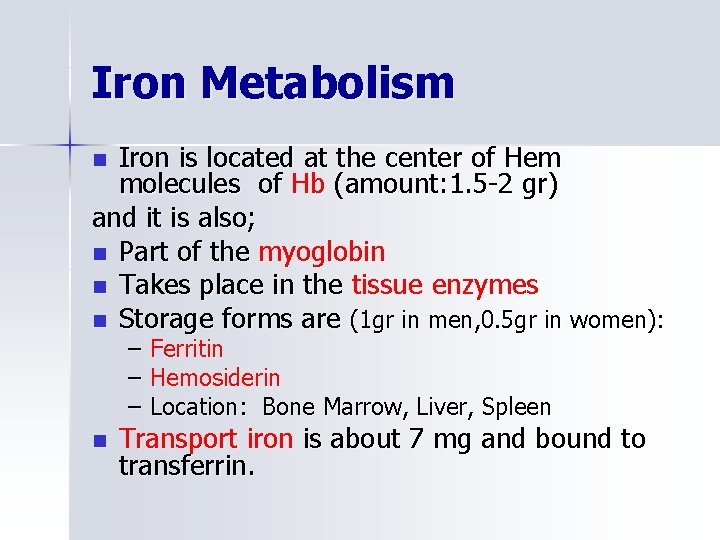
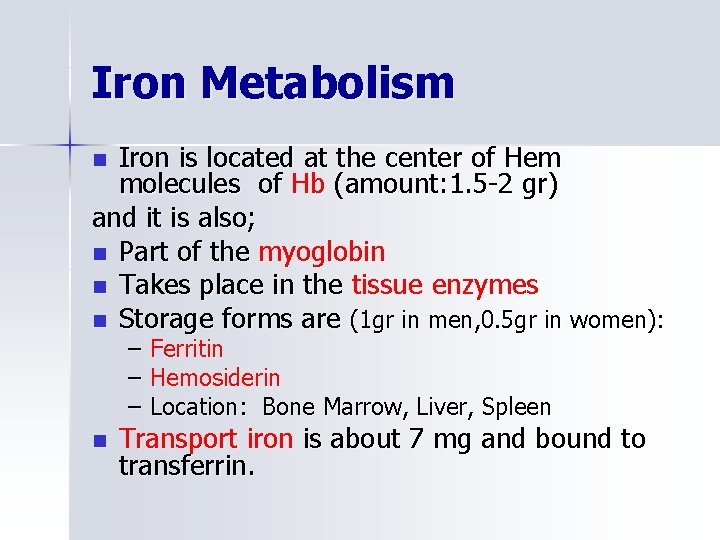
Iron Metabolism Iron is located at the center of Hem molecules of Hb (amount: 1. 5 -2 gr) and it is also; n Part of the myoglobin n Takes place in the tissue enzymes n Storage forms are (1 gr in men, 0. 5 gr in women): n – Ferritin – Hemosiderin – Location: Bone Marrow, Liver, Spleen n Transport iron is about 7 mg and bound to transferrin.
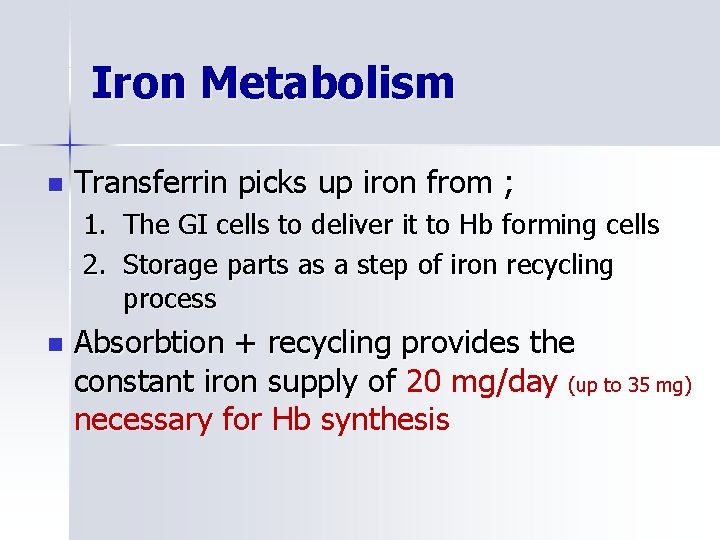
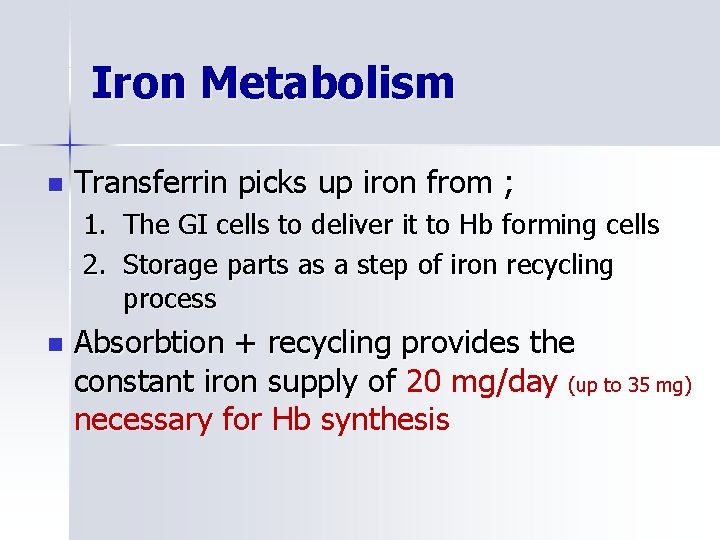
Iron Metabolism n Transferrin picks up iron from ; 1. The GI cells to deliver it to Hb forming cells 2. Storage parts as a step of iron recycling process n Absorbtion + recycling provides the constant iron supply of 20 mg/day (up to 35 mg) necessary for Hb synthesis
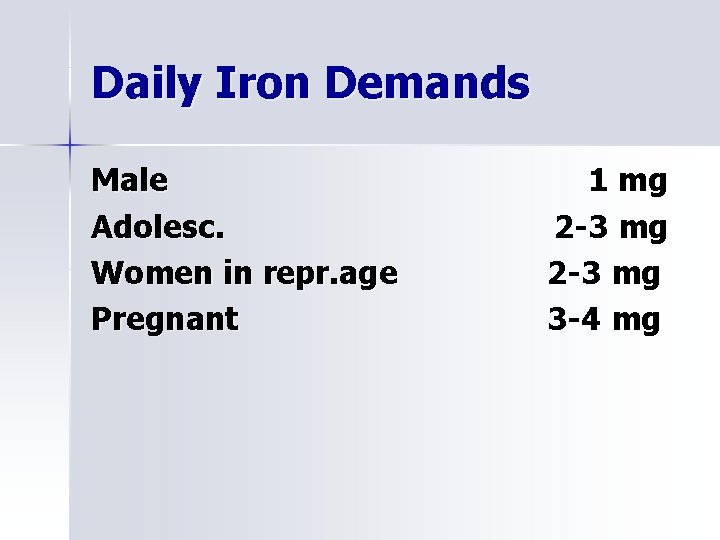
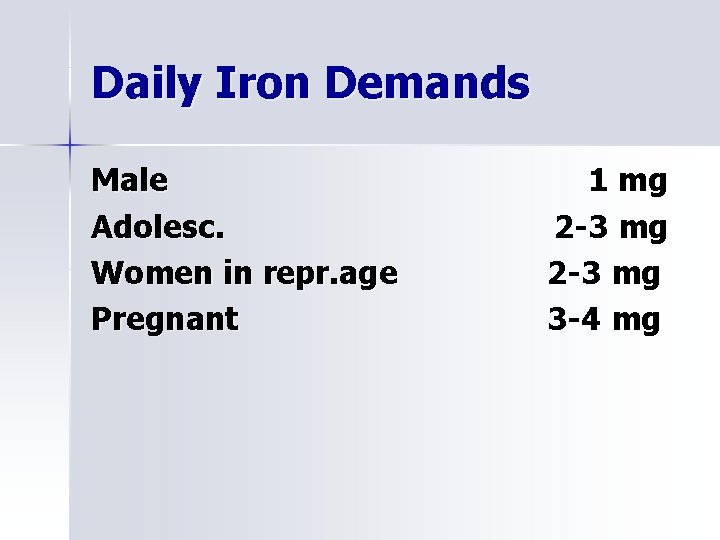
Daily Iron Demands Male Adolesc. Women in repr. age Pregnant 1 mg 2 -3 mg 3 -4 mg
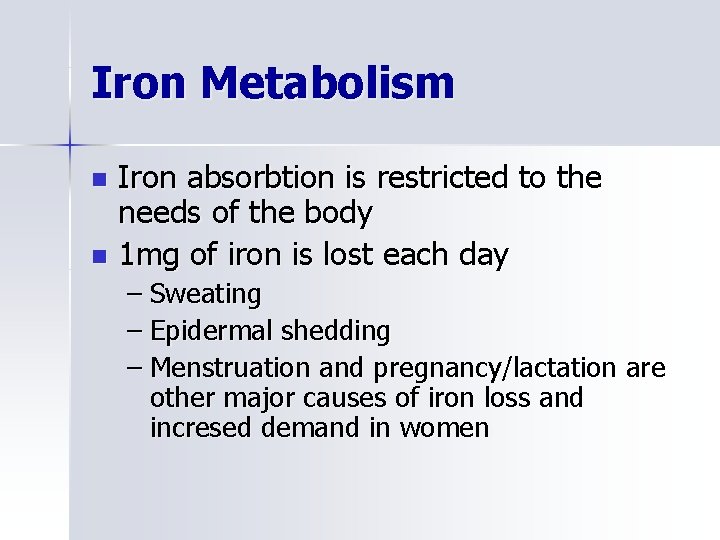
Iron Metabolism Iron absorbtion is restricted to the needs of the body n 1 mg of iron is lost each day n – Sweating – Epidermal shedding – Menstruation and pregnancy/lactation are other major causes of iron loss and incresed demand in women
Iron Metabolism n n n n Normal diet contains about 15 mg of iron/day 6 mg elemental iron/1000 cal 1/10 of ingested iron is absorbed Gastric acid releases iron from food Iron is absorbed in the reduced form Ascorbate increases absorbtion (by reducing) Phytates, tannates, antacids decrease absorbtion by making complexes with iron
Iron Metabolism n Main sites of absorbtion are; – Duodenum – Upper jejunum n Malabsorbtive states or gastrojejunostomy prevent absorbtion.
Iron Metabolism Transport of iron – Transferrin is the main iron carrier in plasma – It is produced in liver cells with increased synthesis in iron deficiency – Transferrin binds 1 -2 ferric iron molecules – Transferrin-iron complex is endocytosed by Hb producing cells after linking to receptors.
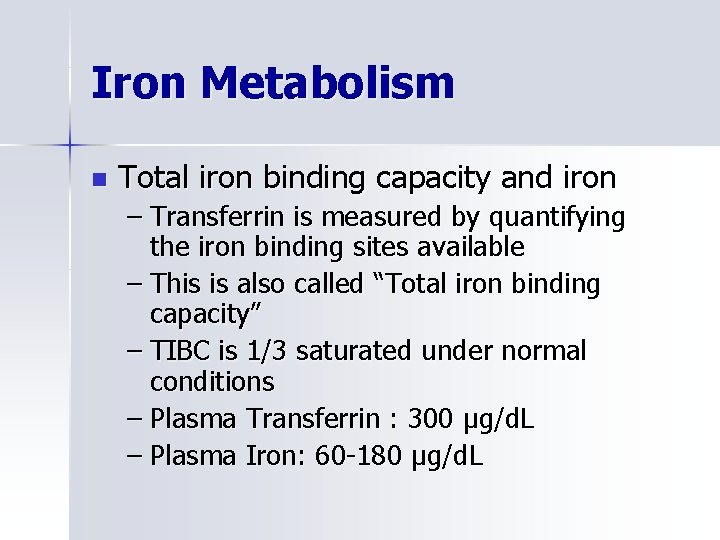
Iron Metabolism n Total iron binding capacity and iron – Transferrin is measured by quantifying the iron binding sites available – This is also called “Total iron binding capacity” – TIBC is 1/3 saturated under normal conditions – Plasma Transferrin : 300 μg/d. L – Plasma Iron: 60 -180 μg/d. L
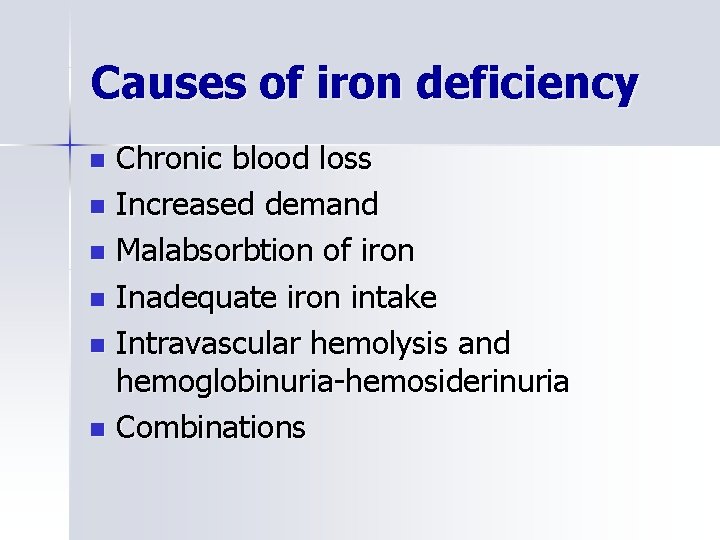
Causes of iron deficiency Chronic blood loss n Increased demand n Malabsorbtion of iron n Inadequate iron intake n Intravascular hemolysis and hemoglobinuria-hemosiderinuria n Combinations n
Increased demands n Pregnancy n Lactation n Rapid growth
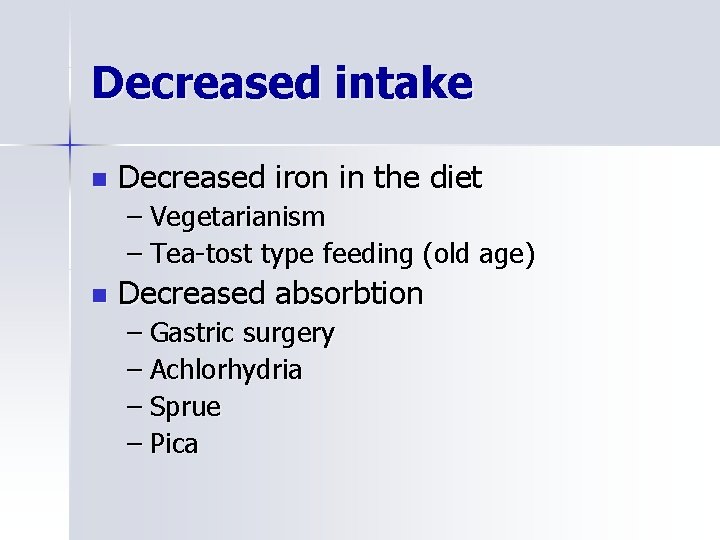
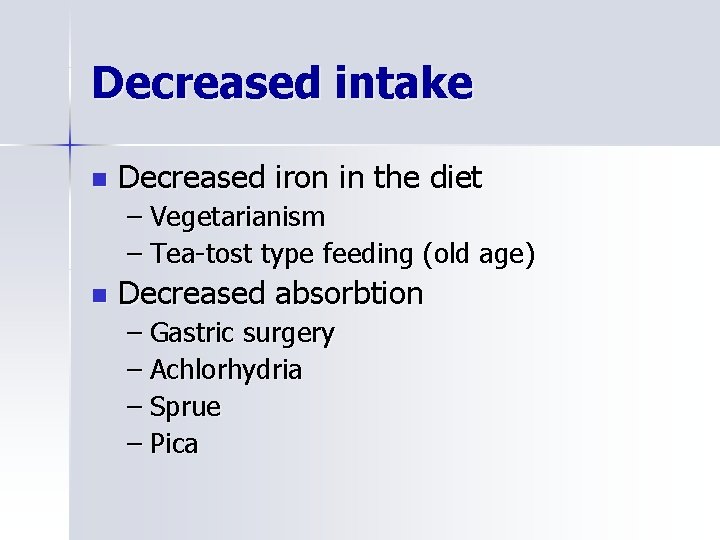
Decreased intake n Decreased iron in the diet – Vegetarianism – Tea-tost type feeding (old age) n Decreased absorbtion – Gastric surgery – Achlorhydria – Sprue – Pica
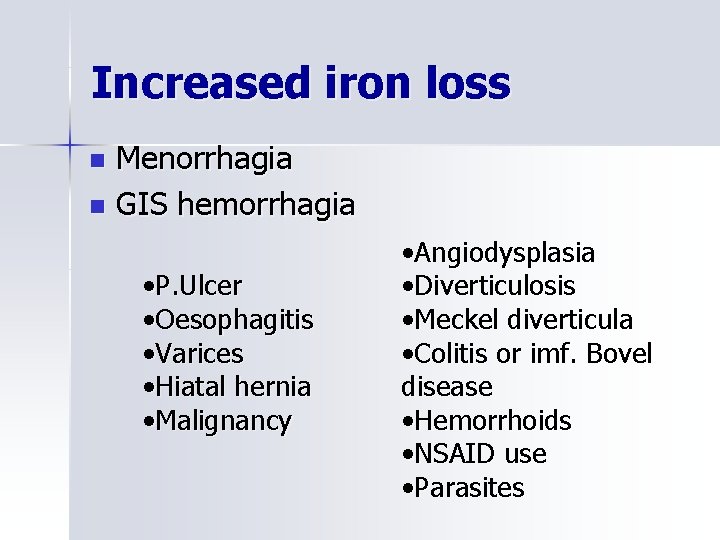
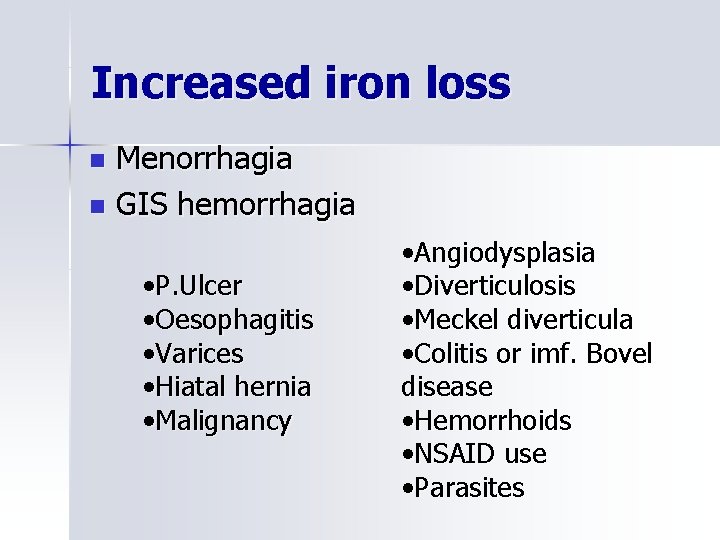
Increased iron loss Menorrhagia n GIS hemorrhagia n • P. Ulcer • Oesophagitis • Varices • Hiatal hernia • Malignancy • Angiodysplasia • Diverticulosis • Meckel diverticula • Colitis or imf. Bovel disease • Hemorrhoids • NSAID use • Parasites
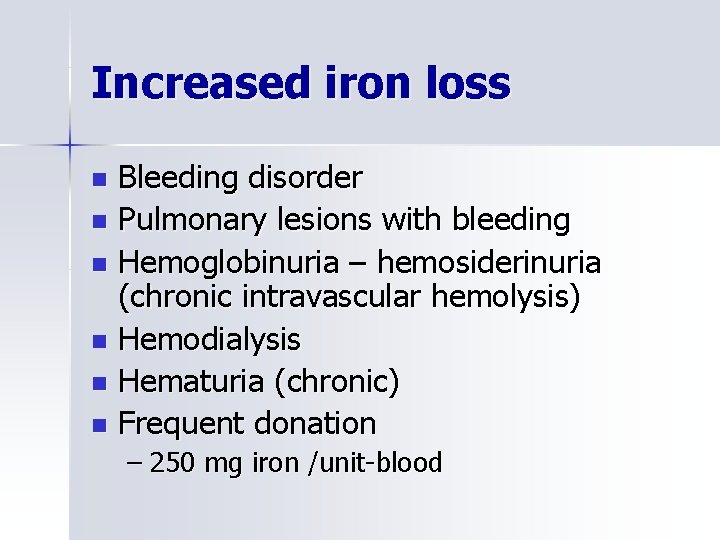
Increased iron loss Bleeding disorder n Pulmonary lesions with bleeding n Hemoglobinuria – hemosiderinuria (chronic intravascular hemolysis) n Hemodialysis n Hematuria (chronic) n Frequent donation n – 250 mg iron /unit-blood
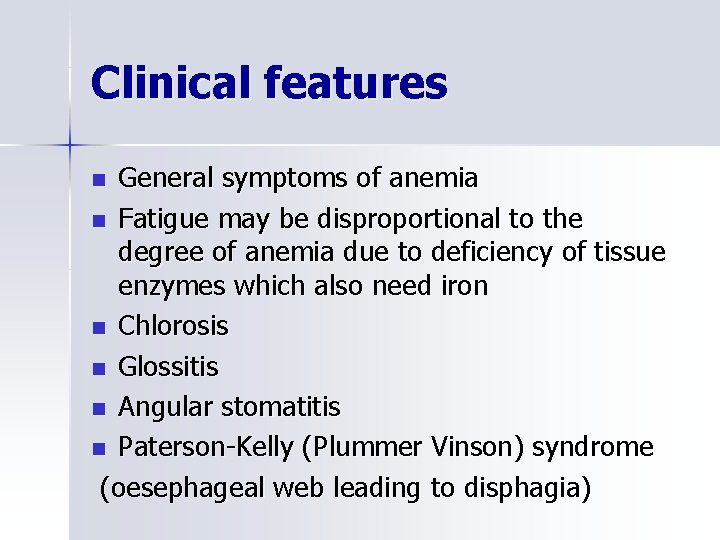
Clinical features General symptoms of anemia n Fatigue may be disproportional to the degree of anemia due to deficiency of tissue enzymes which also need iron n Chlorosis n Glossitis n Angular stomatitis n Paterson-Kelly (Plummer Vinson) syndrome (oesephageal web leading to disphagia) n
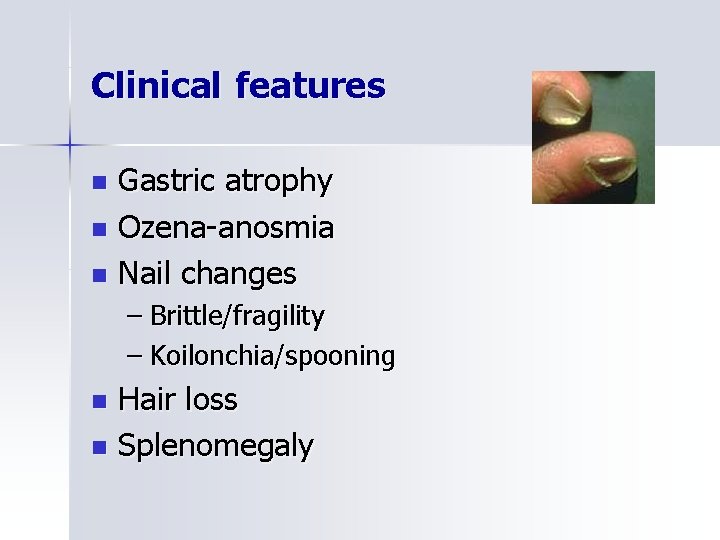
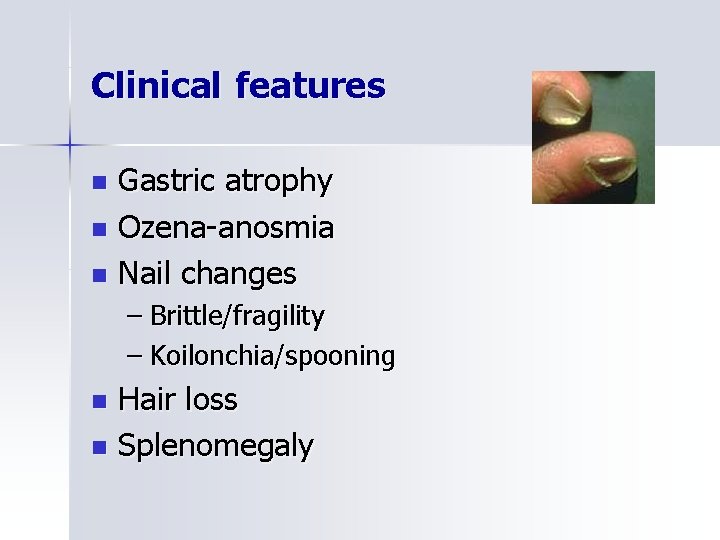
Clinical features Gastric atrophy n Ozena-anosmia n Nail changes n – Brittle/fragility – Koilonchia/spooning Hair loss n Splenomegaly n
Clinical features n Pica: Appetite for bizzare food/substances – Geophagy (earth, clay) – Pagophagia(ice) – Amylophagia(starch) Developmental problems n Splenomegaly n Tayanc-Prasad syndrome n (growth retardation, hypogonadism, hepatosplenomegaly, zinc and iron deficiency, geophagia) n Immun-deficiency
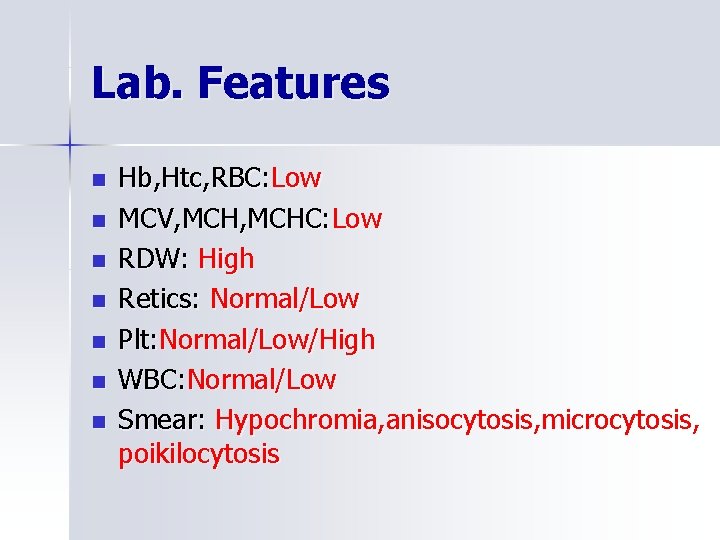
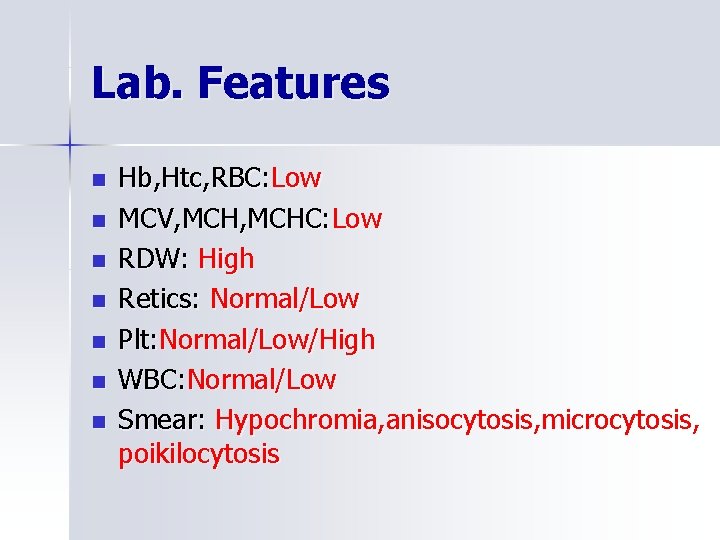
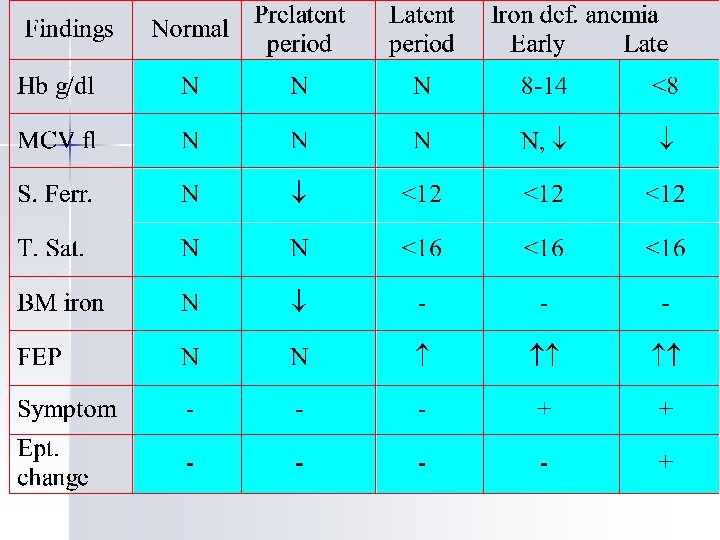
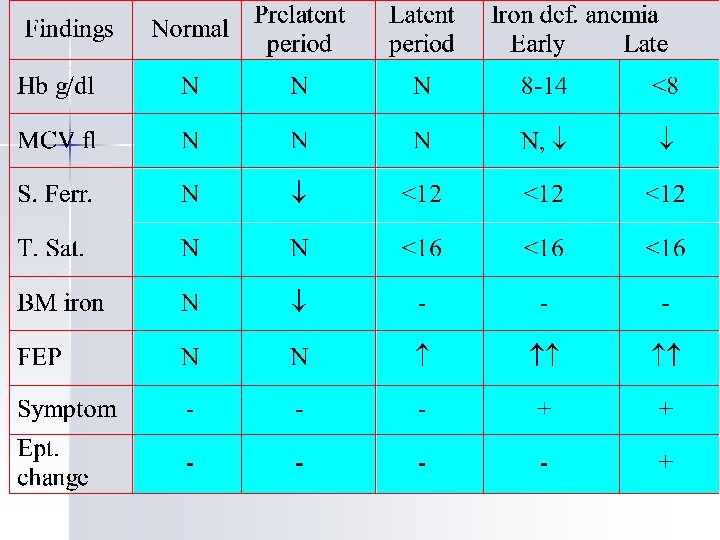
Lab. Features n n n n Hb, Htc, RBC: Low MCV, MCHC: Low RDW: High Retics: Normal/Low Plt: Normal/Low/High WBC: Normal/Low Smear: Hypochromia, anisocytosis, microcytosis, poikilocytosis
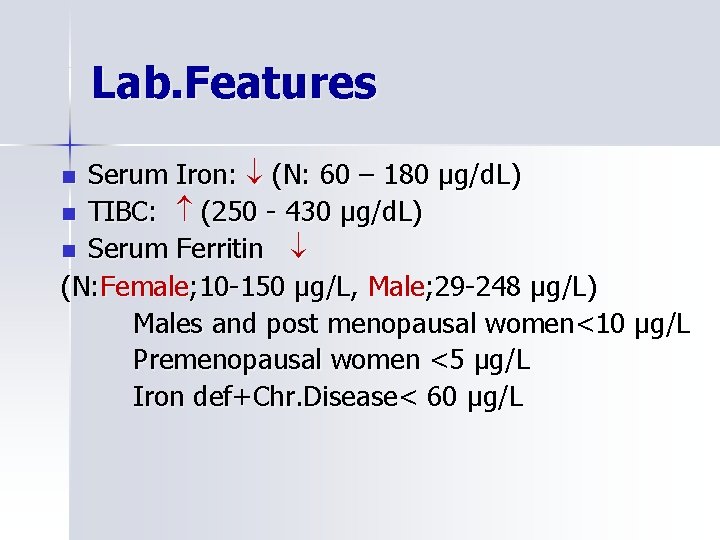
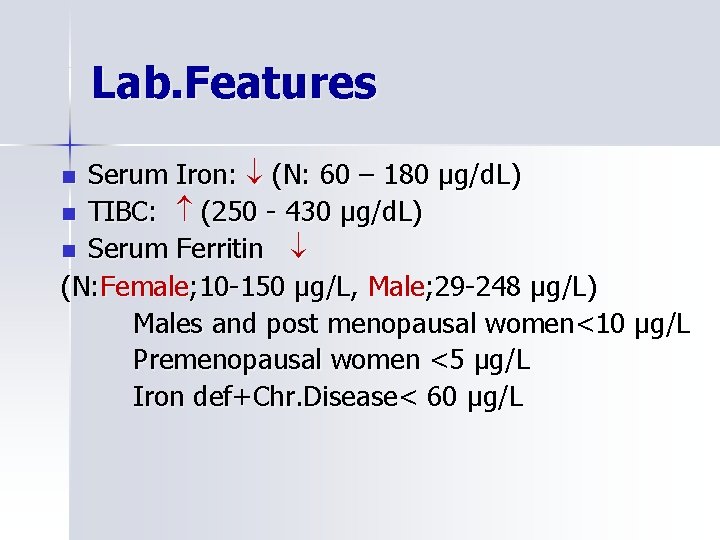
Lab. Features Serum Iron: (N: 60 – 180 μg/d. L) n TIBC: (250 - 430 μg/d. L) n Serum Ferritin (N: Female; 10 -150 μg/L, Male; 29 -248 μg/L) Males and post menopausal women<10 μg/L Premenopausal women <5 μg/L Iron def+Chr. Disease< 60 μg/L n
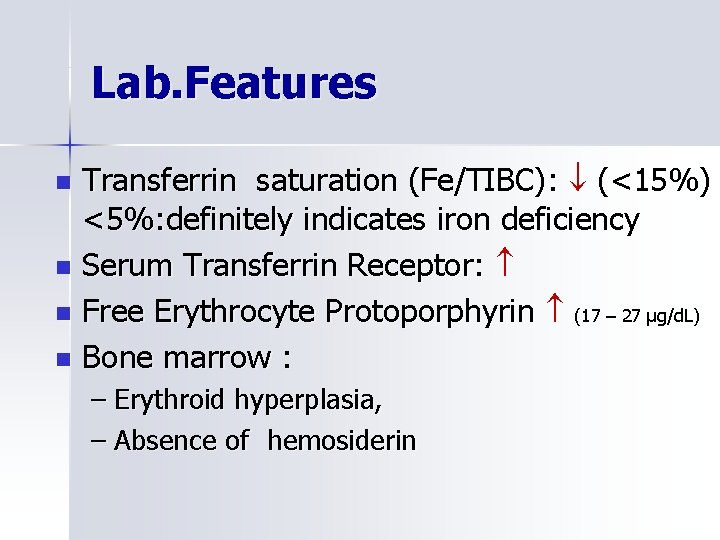
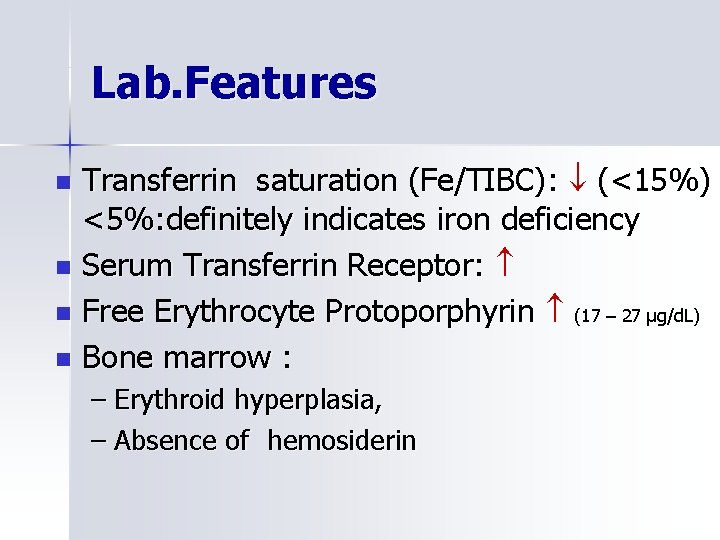
Lab. Features Transferrin saturation (Fe/TIBC): (<15%) <5%: definitely indicates iron deficiency n Serum Transferrin Receptor: n Free Erythrocyte Protoporphyrin (17 – 27 μg/d. L) n Bone marrow : n – Erythroid hyperplasia, – Absence of hemosiderin
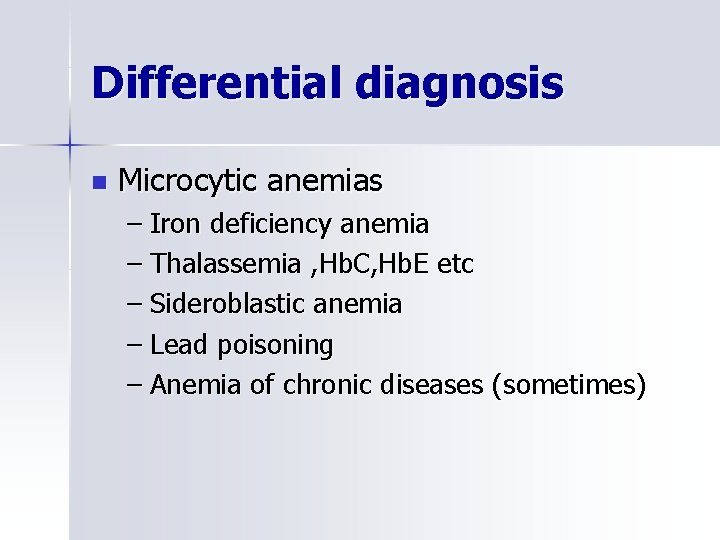
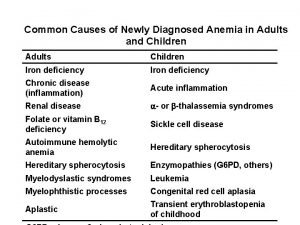
Differential diagnosis n Microcytic anemias – Iron deficiency anemia – Thalassemia , Hb. C, Hb. E etc – Sideroblastic anemia – Lead poisoning – Anemia of chronic diseases (sometimes)
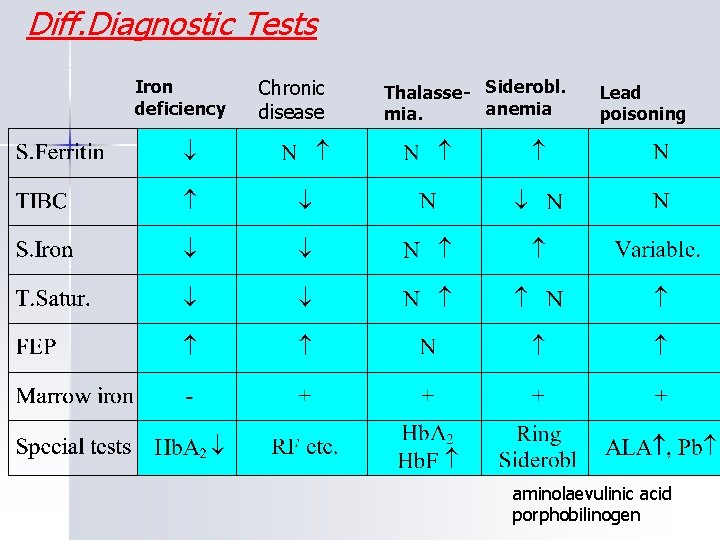
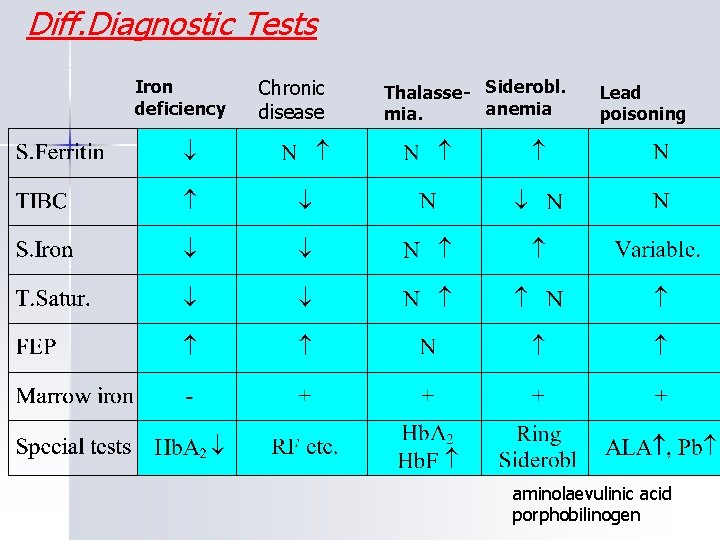
Diff. Diagnostic Tests Iron deficiency Chronic disease Thalasse- Siderobl. anemia mia. Lead poisoning aminolaevulinic acid porphobilinogen
Important !!!!!!! n The diagnostic procedure is not complete until the underlying pathology is disclosed.
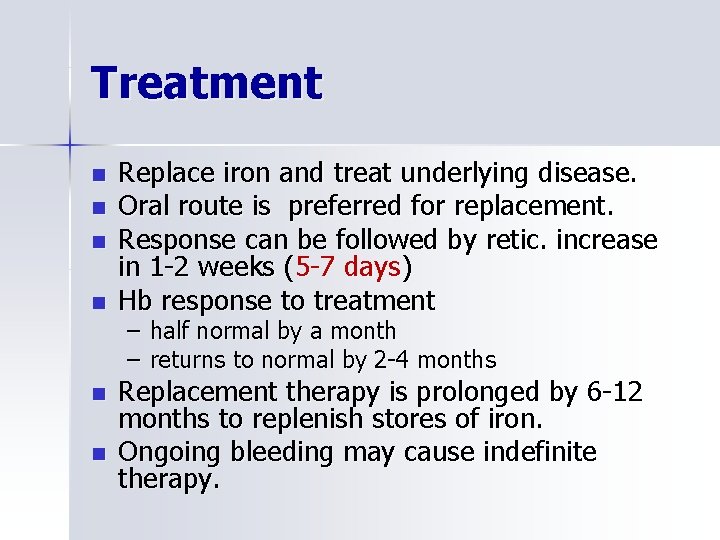
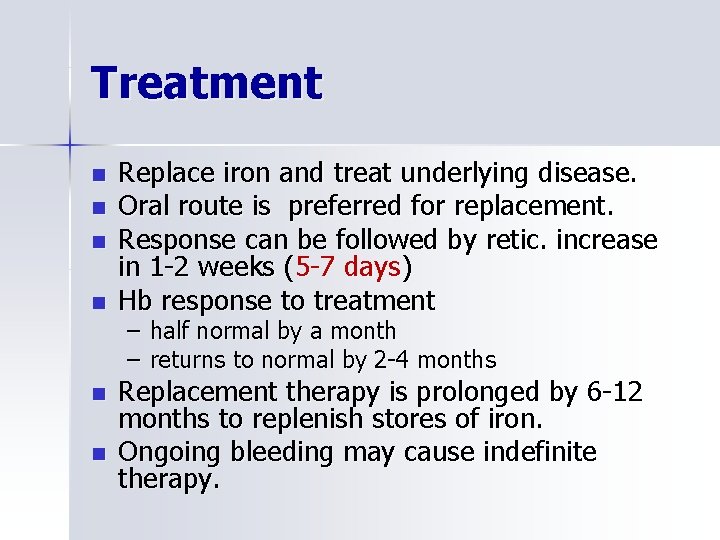
Treatment n n n Replace iron and treat underlying disease. Oral route is preferred for replacement. Response can be followed by retic. increase in 1 -2 weeks (5 -7 days) Hb response to treatment – – half normal by a month returns to normal by 2 -4 months Replacement therapy is prolonged by 6 -12 months to replenish stores of iron. Ongoing bleeding may cause indefinite therapy.
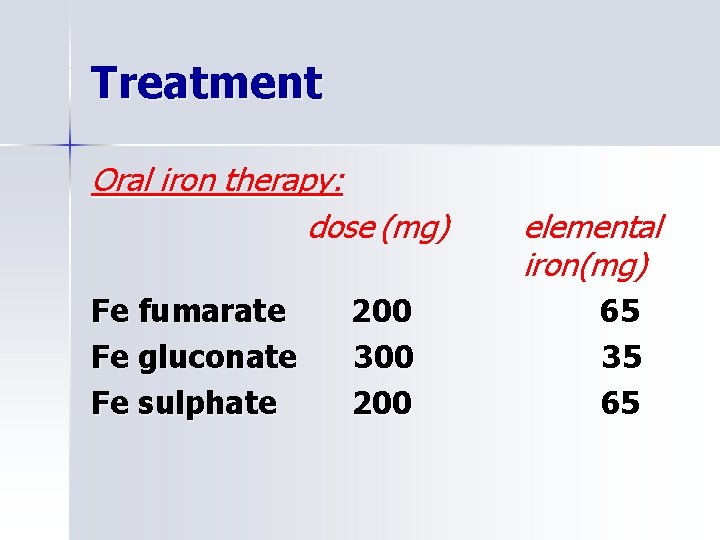
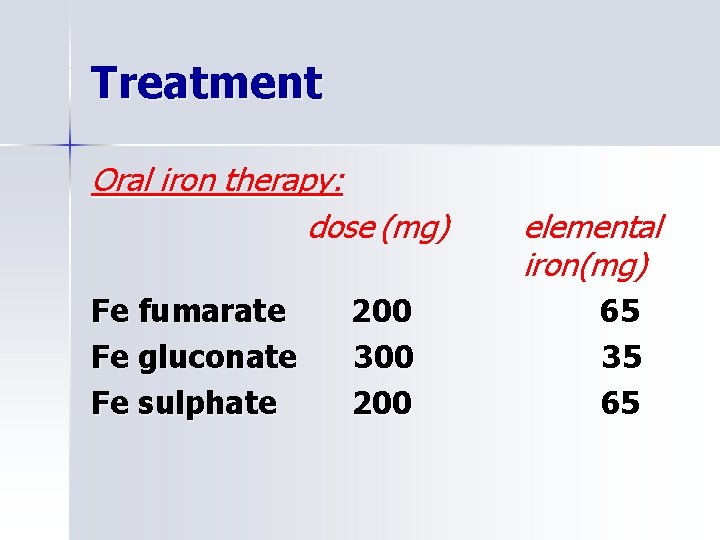
Treatment Oral iron therapy: dose (mg) Fe fumarate Fe gluconate Fe sulphate 200 300 200 elemental iron(mg) 65 35 65
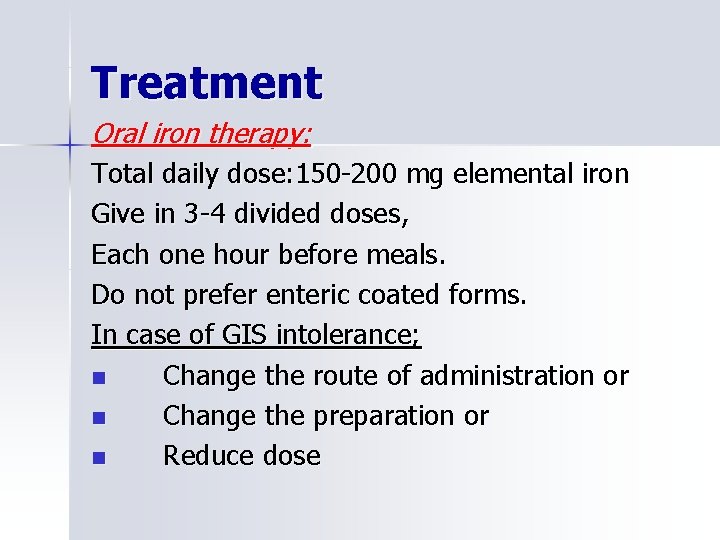
Treatment Oral iron therapy: Total daily dose: 150 -200 mg elemental iron Give in 3 -4 divided doses, Each one hour before meals. Do not prefer enteric coated forms. In case of GIS intolerance; n Change the route of administration or n Change the preparation or n Reduce dose
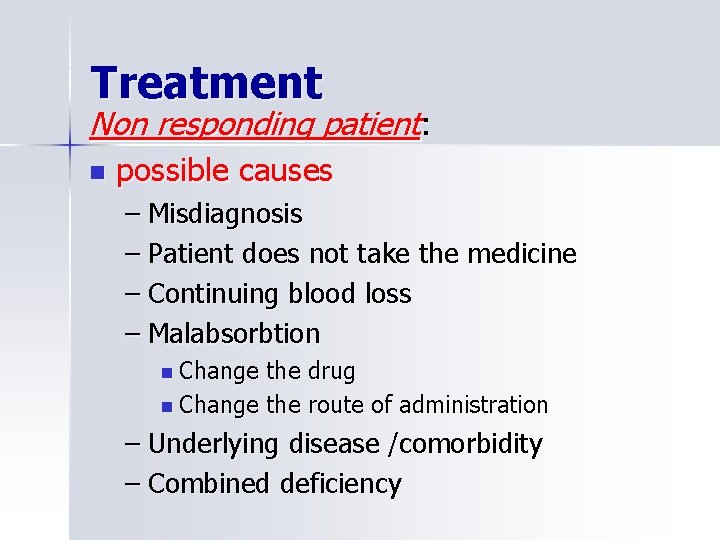
Treatment Non responding patient: n possible causes – Misdiagnosis – Patient does not take the medicine – Continuing blood loss – Malabsorbtion n Change the drug n Change the route of administration – Underlying disease /comorbidity – Combined deficiency
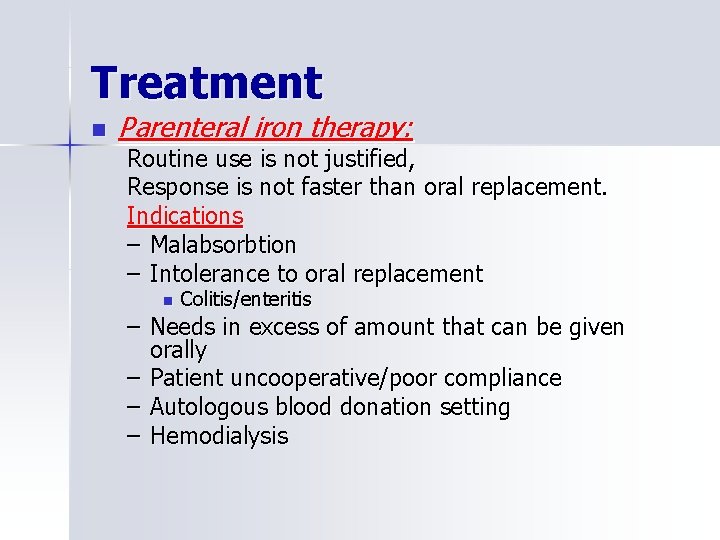
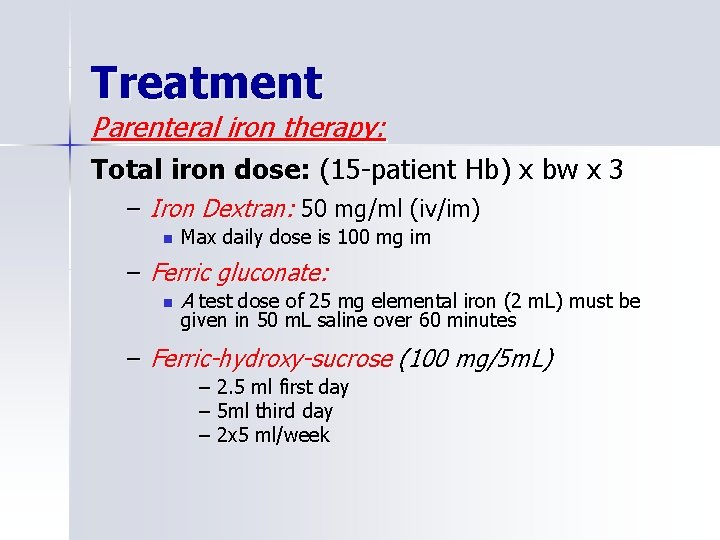
Treatment n Parenteral iron therapy: Routine use is not justified, Response is not faster than oral replacement. Indications – Malabsorbtion – Intolerance to oral replacement n Colitis/enteritis – Needs in excess of amount that can be given orally – Patient uncooperative/poor compliance – Autologous blood donation setting – Hemodialysis
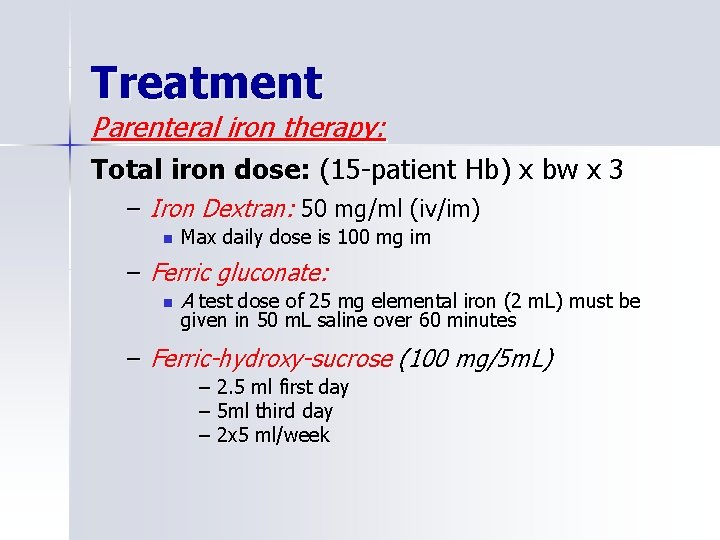
Treatment Parenteral iron therapy: Total iron dose: (15 -patient Hb) x bw x 3 – Iron Dextran: 50 mg/ml (iv/im) n Max daily dose is 100 mg im – Ferric gluconate: n A test dose of 25 mg elemental iron (2 m. L) must be given in 50 m. L saline over 60 minutes – Ferric-hydroxy-sucrose (100 mg/5 m. L) – 2. 5 ml first day – 5 ml third day – 2 x 5 ml/week
Treatment Parenteral replacement therapy may cause – allergic reactions, – local pain or induration, – serum sickness like disease, – lymphadenomegaly, – arthralgia, – myalgia etc.
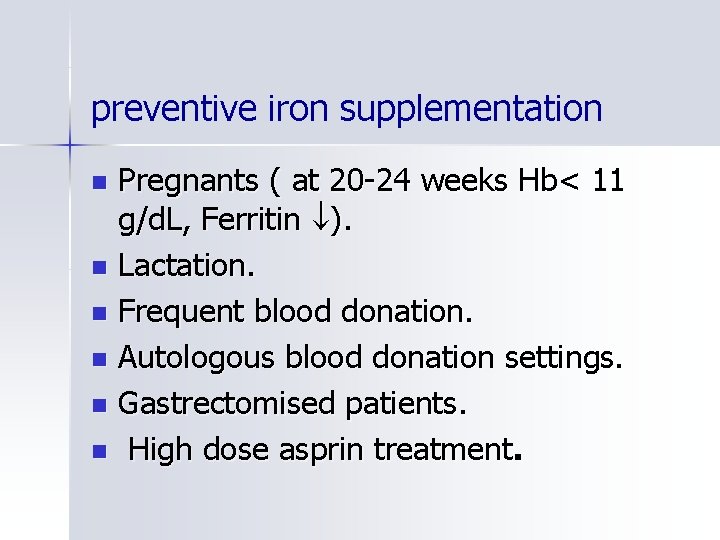
preventive iron supplementation Pregnants ( at 20 -24 weeks Hb< 11 g/d. L, Ferritin ). n Lactation. n Frequent blood donation. n Autologous blood donation settings. n Gastrectomised patients. n High dose asprin treatment. n
 Lenfadenomegali
Lenfadenomegali Anemia tibc ferritin iron
Anemia tibc ferritin iron Minerals are inorganic elements that the body
Minerals are inorganic elements that the body Osmosis iron deficiency anemia
Osmosis iron deficiency anemia Feroba-you sr tab
Feroba-you sr tab Elemental iron dose
Elemental iron dose Anemiam
Anemiam Labs for iron deficiency anemia
Labs for iron deficiency anemia Dietary iron
Dietary iron What is severe iron deficiency
What is severe iron deficiency Megaloblastic anemia causes
Megaloblastic anemia causes Indication of anemia
Indication of anemia Low iron causes
Low iron causes Hihtsek nedir
Hihtsek nedir Megaloblastic anemia is caused due to deficiency of
Megaloblastic anemia is caused due to deficiency of Megaloblastic anemia vs pernicious anemia
Megaloblastic anemia vs pernicious anemia Megaloblastic anaemia definition
Megaloblastic anaemia definition Iron deficiency in roses
Iron deficiency in roses Causes of iron deficiency
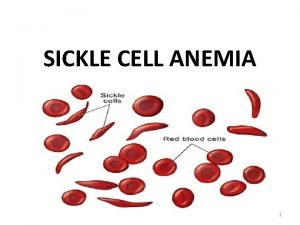
Causes of iron deficiency Sickle cell symptoms
Sickle cell symptoms Mass of iron in an iron tablet
Mass of iron in an iron tablet Iron sharpens iron friendship
Iron sharpens iron friendship Zinc deficiency rash
Zinc deficiency rash Chemistry of life summary
Chemistry of life summary Tyrosinase deficiency
Tyrosinase deficiency Versine of curve
Versine of curve Contamination and deficiency of a job performance measure
Contamination and deficiency of a job performance measure What are deficiency
What are deficiency Contract deficiency report
Contract deficiency report Rickets
Rickets Potassium deficiency symptoms
Potassium deficiency symptoms What is equilibrium cant
What is equilibrium cant Disclosure deficiency
Disclosure deficiency Von willebrand disease test
Von willebrand disease test Deficiency of vitamin
Deficiency of vitamin