Airway Clearance in Children Youth and Adolescents Does

- Slides: 58
Airway Clearance in Children Youth and Adolescents – Does The Device Really Matter? Chris Landon MD FAAP, FCCP, CMD Director of Pediatrics Ventura County Medical Center Pediatric Pulmonary Center Director Mid Coast Clinical Associate Professor of Pediatrics USC School of Medicine Pediatric Pulmonary Department Children’s Hospital Los Angeles
Disclaimer Scientific Advisory Boards • Hill-Rom
Objectives • I. Review of the rationale for airway clearance therapy and basic principles • II. Review the evidence for efficacy of airway clearance therapy in pediatrics • III. Minimal to no benefit in the treatment of children with acute asthma, bronchiolitis, hyaline membrane disease, and those on mechanical ventilation for respiratory failure in the pediatric intensive care unit, and it is not effective in preventing atelectasis in children immediately following surgery. •
Neuromuscular Diseases: Overview n Children who experience varying degrees of neurological/neuromuscular dysfunction n Diagnoses include: cerebral palsy, muscular dystrophy, spinal muscular atrophy, brain injury, consequences of infectious disease, inherited metabolic disorders, etc. – One child in 1000 is institutionalized as a result of profound disability
Neuromuscular Diseases: Overview Multi-system assessment necessary to determine risk of pulmonary involvement: n Neuromuscular n Gastroesophageal n Immune system n Respiratory n Psychosocial
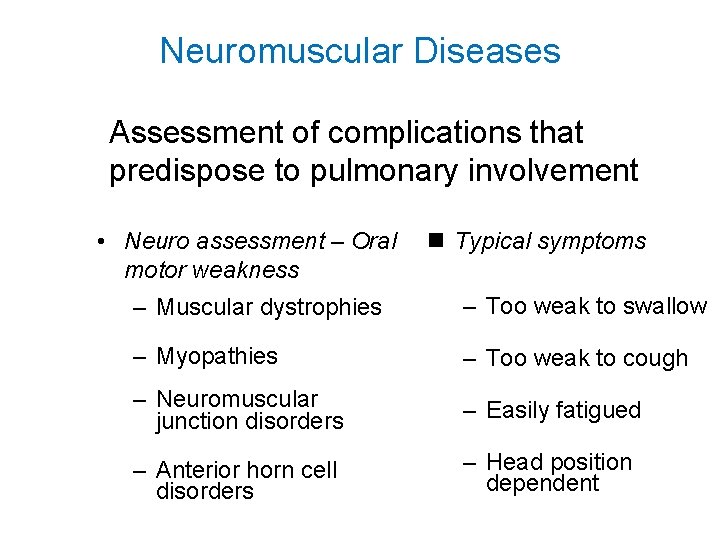
Neuromuscular Diseases Assessment of complications that predispose to pulmonary involvement • Neuro assessment – Oral motor weakness n Typical symptoms – Muscular dystrophies – Too weak to swallow – Myopathies – Too weak to cough – Neuromuscular junction disorders – Easily fatigued – Anterior horn cell disorders – Head position dependent
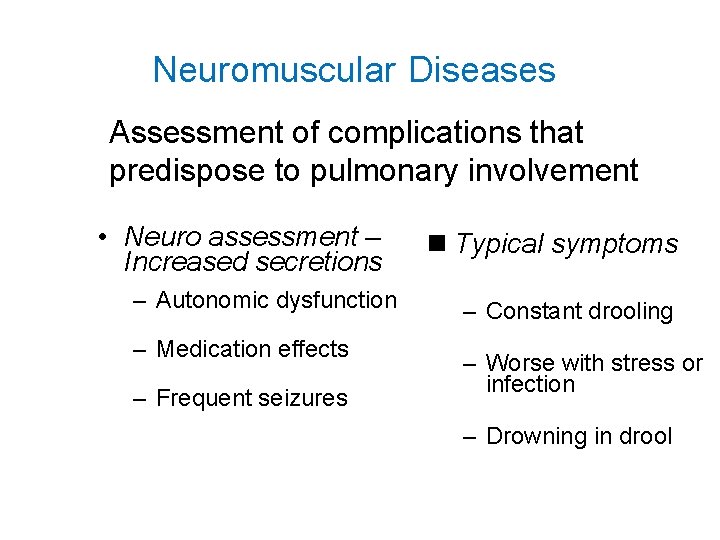
Neuromuscular Diseases Assessment of complications that predispose to pulmonary involvement • Neuro assessment – Increased secretions – Autonomic dysfunction – Medication effects – Frequent seizures n Typical symptoms – Constant drooling – Worse with stress or infection – Drowning in drool
Oral Motor Weakness n Myopathies n Muscular dystrophies n Neuromuscular junction disorders n Anterior horn cell disorders n Typical symptoms – Too weak to swallow – Too weak to cough – Easily fatigued – Head position dependent
Central Neurogenic Hypoventilation n Diffuse cortical damage n Poor hypoxic response n Poor hypercarbic response n Worse with stress or infection
Thoracic Weakness • • Myopathies Muscular dystrophies Neuromuscular junction disorders Anterior horn cell disorders
Gastroesophageal Function and Complications n The Upper Airway. Swallowing and Aspiration § Aspiration Associated Pneumonias § Lower Esophageal Aspiration, Gastric Distention and Airway Remodeling n Gastroesophageal Reflux Disease (GERD) § Fundoplication Versus Medication and Airway Clearance § Nutrition and the Immune System
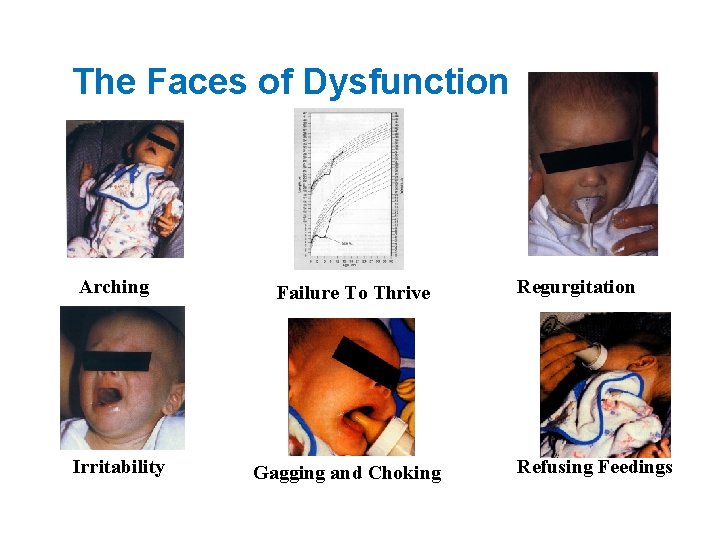
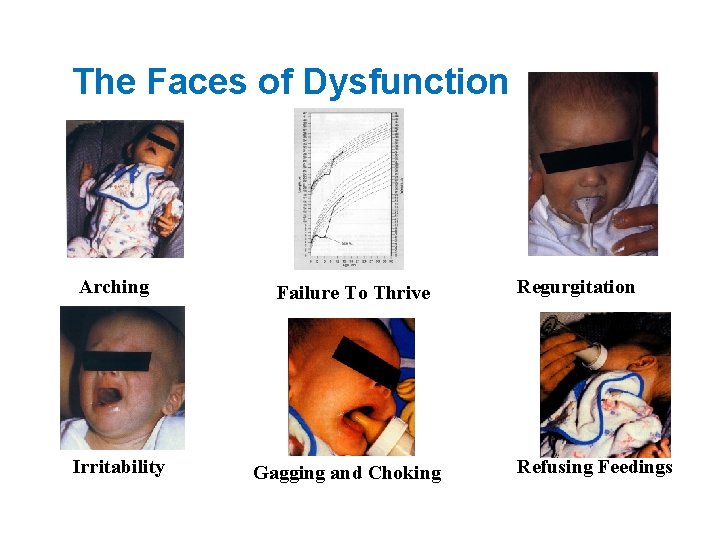
The Faces of Dysfunction Arching Irritability Failure To Thrive Gagging and Choking Regurgitation Refusing Feedings
The Immune System § Genetic § Abnormalities § § Nutritional Compromise of the § Immune System § Stress and Immune Response § Recurrent Infection and Frequent Use of Antibiotics: The Impacts Allergies Reactive Airway Disease (RAD) Airway Clearance Therapy
Respiratory Medical History – Number of Pulmonary Infections Annually – Number of Hospital Admissions Annually – Number of ER Admissions Annually – – – Number of Courses of Antibiotics for Respiratory Infections Annually Immunization History of Recurrent Infections with Respiratory Syncytial Virus (RSV)
High Risk For Post-Operative Complications n Atelectasis n Pneumonia n Respiratory Failure n Need for prolonged ventilation n Tracheostomy n Death
Problems n Weak cough n Dyscoordinated swallow n Aspiration n Difficulty clearing secretions n Increased lower respiratory tract infections
Respiratory Weakness n May not be apparent on physical exam n Respiratory failure when work of breathing is increased
Chronic Respiratory Muscle Weakness n n n n n Reduced lung volumes Microatelectasis V/Q mismatch Scoliosis Decreased compliance of the chest wall Decreased pulmonary compliance Hypoxemia only during sleep Hypoventilation due to muscle weakness Hypoventilation due to central hypoventilation
Thorough History n Frequency and severity of respiratory tract infections n Pulmonary complications of previous surgeries n History suggestive of reactive airways disease – Even mildly increased airway obstruction may lead to respiratory failure in the postoperative period in a patient with severe respiratory muscle weakness
Physical Examination n Gag reflex n Cough n Adequacy of aeration n Presence of adventitial lung sounds
Ability To Cooperate With Post. Operative Pulmonary Therapy n General muscle strength n Physical and intellectual capacity
Laboratory Examinations n Chest x-ray n Arterial blood gases or mixed venous gas measurements and oximetry n Complete blood count
Pulmonary Function Tests n All children who are capable of performing them – Lung volumes – Pre and post bronchodilator – Maximal inspiratory and expiratory mouth pressures • frequently decreased more than lung volumes and flows • do not correlate with general muscle strength
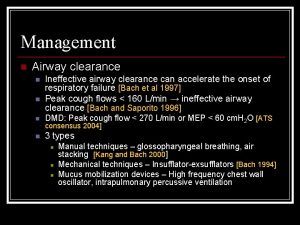
Impaired Airway Clearance: Factors • • Ineffective mucociliary clearance Excessive secretions Thick secretions Ineffective cough Restrictive lung disease Immobility / inadequate exercise Dysphagia / aspiration / gastroesophageal reflux
Results of Impaired Airway Clearance • • • Airway obstruction Mucus plugging Atelectasis Impaired gas exchange Infection Inflammation
Disease States with Compromised Airway Clearance • Primary Ciliary Dyskinesia • Neuromuscular Disease – Predisposes to respiratory failure – Distinct risk factor for morbidity and mortality • • • Severe neurologic insults Cystic Fibrosis Bronchiectasis v No proven benefit for airway clearance therapy in pneumonia, asthma not complicated by atelectasis, bronchiolitis
Airway Clearance Devices • • • CPT for infants PEP Valve Flutter Acapella Cough Assist The Vest System
Chest Physiotherapy for Infants • No definitive data to support use in asymptomatic CF infant. • Most likely age group to have adverse effects, especially GER + aspiration. • Must modify postural drainage to minimize side effects • Significant time commitment for families and Healthcare teams
PEP Valve • • • Positive Expiratory Pressure Action: Splints airways during exhalation Can be used with aerosolized medications Technique dependent Portable Time required: 10 -15 minutes
Flutter • Action: Loosens mucus through expiratory oscillation; positive expiratory pressure splints airways. • Used independently • Technique dependent – has to be held at a precise angle to maximize oscillation • Portable • May not be effective at low airflows • Time required: 10 -15 minutes
Acapella • Combines benefits of PEP and airway vibrations to mobilize secretions • Similar to flutter except has a valvemagnet device to interrupt expiratory flow and thus can be used at any angle.
Contraindications for PEP, Acapella and Flutter • • Pneumothorax Perforated ear drum Hemoptysis Post-operative lung surgery as may lead to air leak or if fresh transplant may break down anastomoses site Severe cardiac disease Esophageal varices Pulmonary embolus
Cough Assist • Action: Creates mechanical “cough” through the use of high flows at positive and negative pressures. • Positive / negative pressures up to 60 cm of water • Used independently or with caregiver assistance • Technique independent • Portable • Primary use in muscular weakness
Airway Clearance Vest Systems (High Frequency Chest Wall Oscillation)
High Frequency Chest Wall Oscillating Devices • Action: Uses pulses of air pressure applied to the chest wall to produce shearing at the air-mucus interface and compression causes repetitive peak expiratory flows to expel mucus like small coughs • The chest wall is only compressed • The air in the airways only oscillates
Contraindications to Vest Therapy • Head and/or neck injury which has not been stabilized • Active pulmonary hemorrhage • Hemodynamic instability
Quality Airway Clearance Therapy Should § § § § Clear secretions effectively and consistently Preserve lung function Reduce infectious exacerbations Reduce dependence on antibiotic therapy and other medications Reduce need for hospitalization and auxiliary medical services Delay disease progression Reduce the burden of care Enhance the quality of life
Adverse Effects – Airway Clearance • • Oxygen desaturation Gastroesophageal reflux Aspiration Hyperventilation Airway obstruction from mobilized secretions Barotrauma Pain and discomfort Guilt from lack of adherence
Therapy Adjuncts • • • Antibiotics Bronchodilators Anti-inflammatory drugs Mucolytics Nutrition
HFCWO Clearance System Case 5 Year Old Girl With Spinal Muscular Atrophy Second PICU Hospitalization in Two Months
History Of Illness • • 5 year old girl with Spinal Muscular Atrophy Fever and oxygen saturations in the high 80’s Discharged from PICU two weeks prior Poor oral intake
Clinical Findings • X-ray at PMD’s office showed RUL Pneumonia • Transferred by PMD to Santa Barbara PICU by ambulance from the office • Temperature 38. 7 Pulse 158 BP 105/53 • Respiratory Rate 29 • Chest clear to auscultation bilaterally. No audible wheezing • Neuro – Alert and cooperative, extremely thin with muscular atrophy
Treatment Issues • Social stressors of divorcing parents • Parents not recognizing that patient is having difficulties with eating • Last authorized Pediatric Pulmonary visit 1/23/05 VEST prescribed • Despite multiple attempts to fit VEST, patient reported to mother it was uncomfortable. Mother blamed father for imposing it. Parents feel uncomfortable with CPT due to patients reported discomfort • Unable to generate sufficient flow for Flutter and Acapella • Patient has nebulizer for albuterol and uses 1992 Coffalator left by DME company
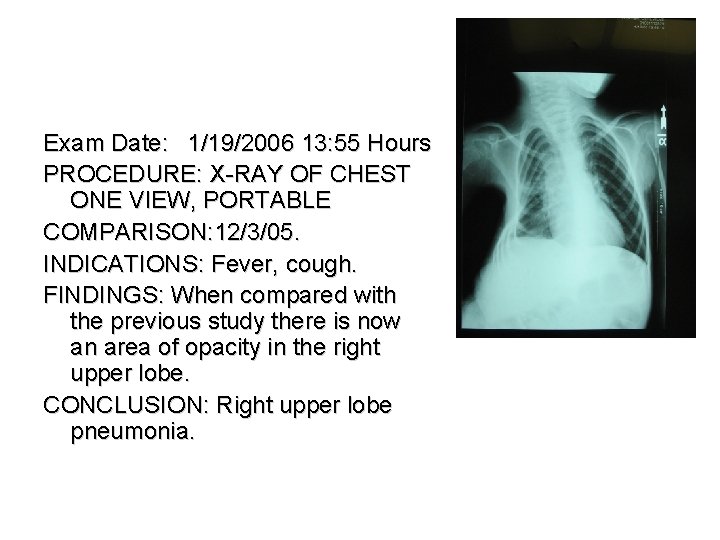
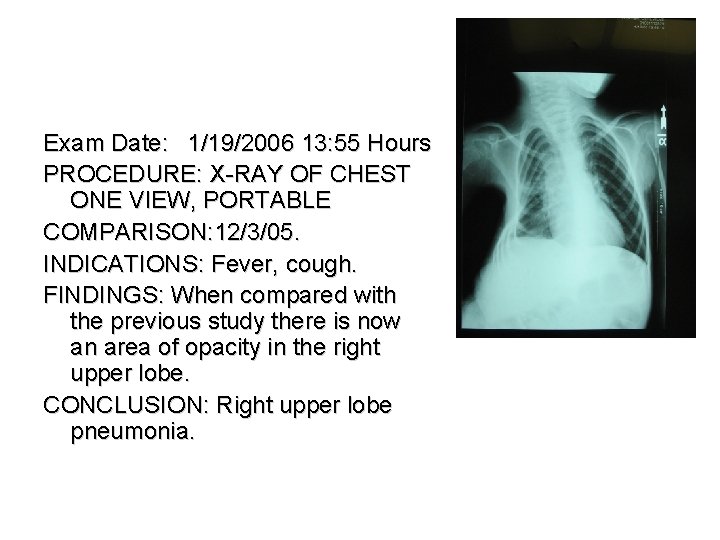
Exam Date: 1/19/2006 13: 55 Hours PROCEDURE: X-RAY OF CHEST ONE VIEW, PORTABLE COMPARISON: 12/3/05. INDICATIONS: Fever, cough. FINDINGS: When compared with the previous study there is now an area of opacity in the right upper lobe. CONCLUSION: Right upper lobe pneumonia.
Medical Interventions at Time of Presentation • Bi. Pap with supplemental oxygen for sleeping and napping • Cefuroxime and Azithromycin • Patient receives albuterol and CPT to upper lobe
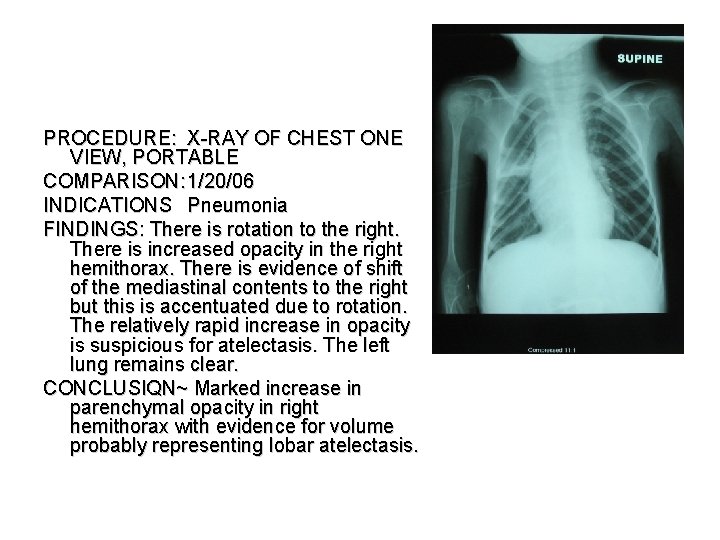
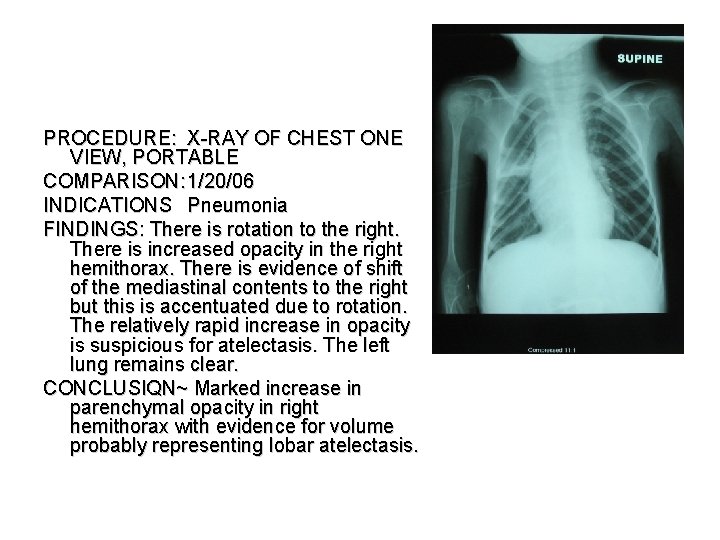
PROCEDURE: X-RAY OF CHEST ONE VIEW, PORTABLE COMPARISON: 1/20/06 INDICATIONS Pneumonia FINDINGS: There is rotation to the right. There is increased opacity in the right hemithorax. There is evidence of shift of the mediastinal contents to the right but this is accentuated due to rotation. The relatively rapid increase in opacity is suspicious for atelectasis. The left lung remains clear. CONCLUSIQN~ Marked increase in parenchymal opacity in right hemithorax with evidence for volume probably representing lobar atelectasis.
Medical Interventions at Time of Presentation • Bi. Pap with supplemental oxygen for sleeping and napping • Cefuroxime and Azithromycin • Changed to cefepime on Day 3 • Pediatric Hospitalist reviews care and Xray reports by phone with Pediatric Pulmonologist • Coffalator brought from home
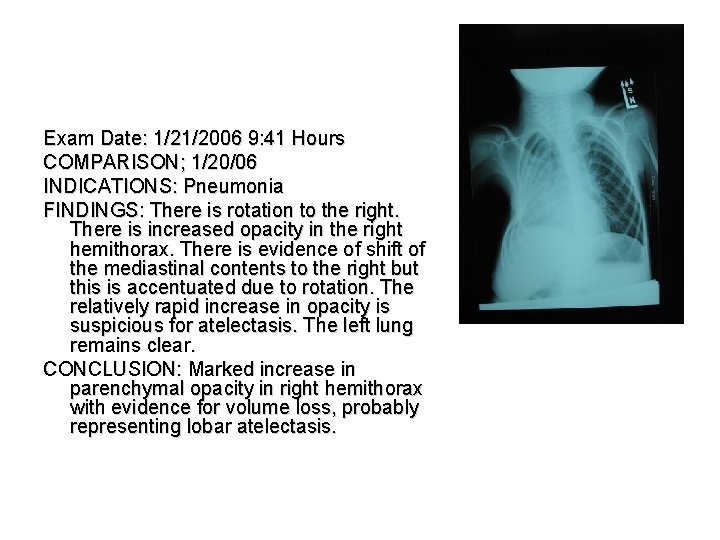
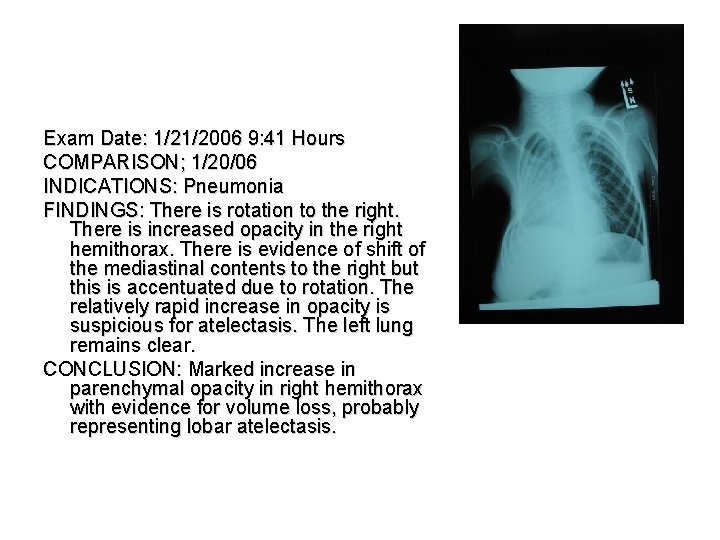
Exam Date: 1/21/2006 9: 41 Hours COMPARISON; 1/20/06 INDICATIONS: Pneumonia FINDINGS: There is rotation to the right. There is increased opacity in the right hemithorax. There is evidence of shift of the mediastinal contents to the right but this is accentuated due to rotation. The relatively rapid increase in opacity is suspicious for atelectasis. The left lung remains clear. CONCLUSION: Marked increase in parenchymal opacity in right hemithorax with evidence for volume loss, probably representing lobar atelectasis.
Medical Interventions at Time of Presentation • Bi. Pap with supplemental oxygen for sleeping and napping • Cefuroxime and Azithromycin • Changed to cefepime on Day 3 • Coffalator brought from home • Custom VEST brought from home and used in conjunction with Coffalator
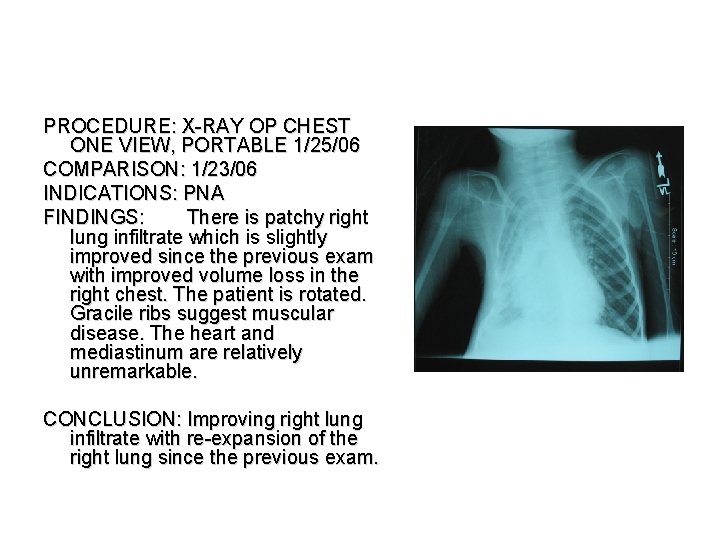
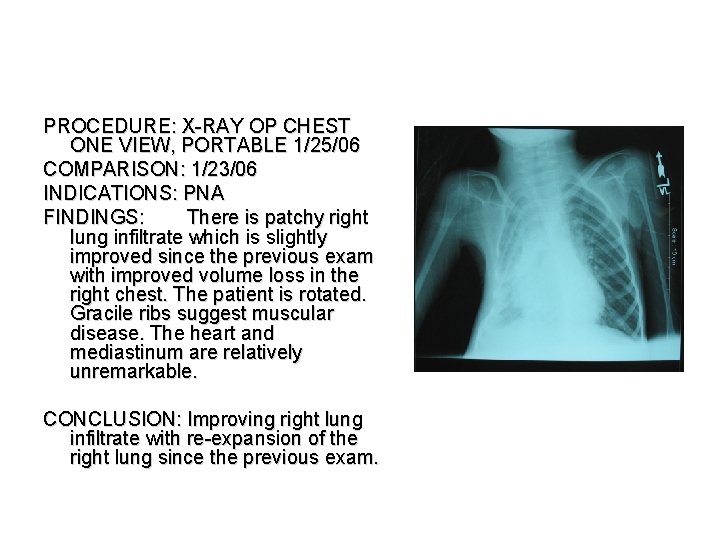
PROCEDURE: X-RAY OP CHEST ONE VIEW, PORTABLE 1/25/06 COMPARISON: 1/23/06 INDICATIONS: PNA FINDINGS: There is patchy right lung infiltrate which is slightly improved since the previous exam with improved volume loss in the right chest. The patient is rotated. Gracile ribs suggest muscular disease. The heart and mediastinum are relatively unremarkable. CONCLUSION: Improving right lung infiltrate with re-expansion of the right lung since the previous exam.
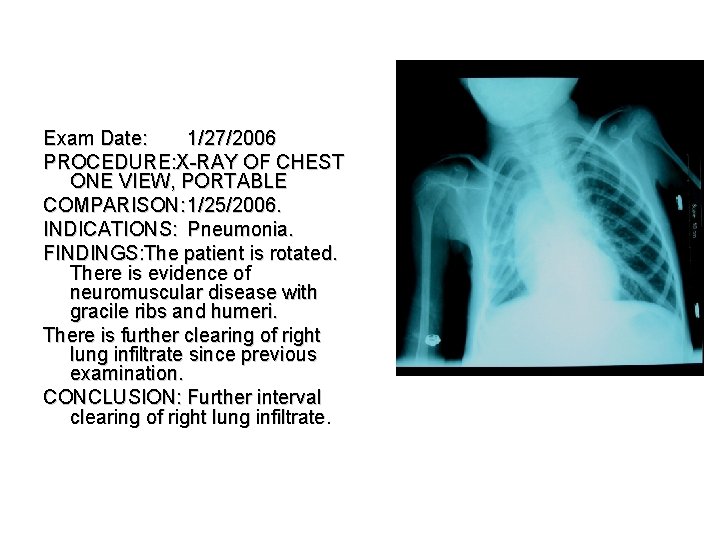
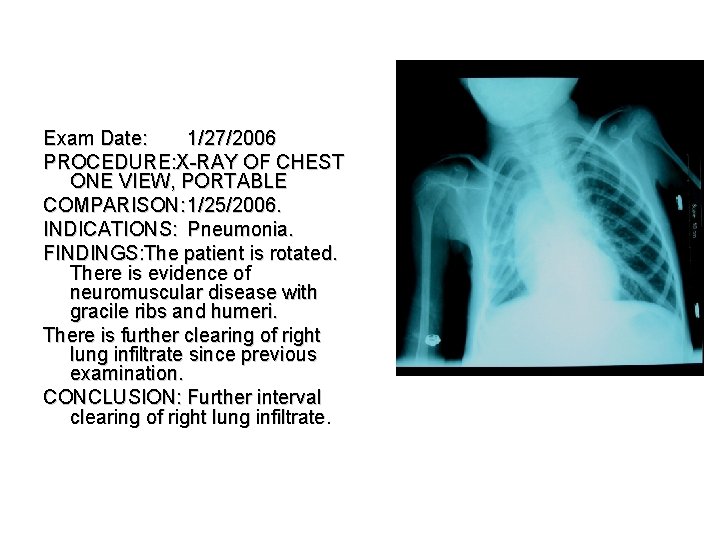
Exam Date: 1/27/2006 PROCEDURE: X-RAY OF CHEST ONE VIEW, PORTABLE COMPARISON: 1/25/2006. INDICATIONS: Pneumonia. FINDINGS: The patient is rotated. There is evidence of neuromuscular disease with gracile ribs and humeri. There is further clearing of right lung infiltrate since previous examination. CONCLUSION: Further interval clearing of right lung infiltrate.
New Achievements • PROBLEM: • Recurrent Intensive Care Unit Admissions for Patients with Neuromuscular Disease, Cerebral Palsy, and Anoxic Brain Damage
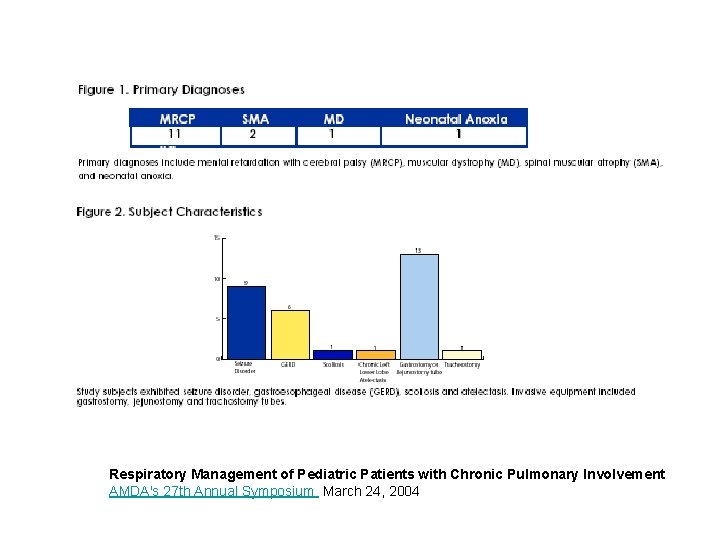
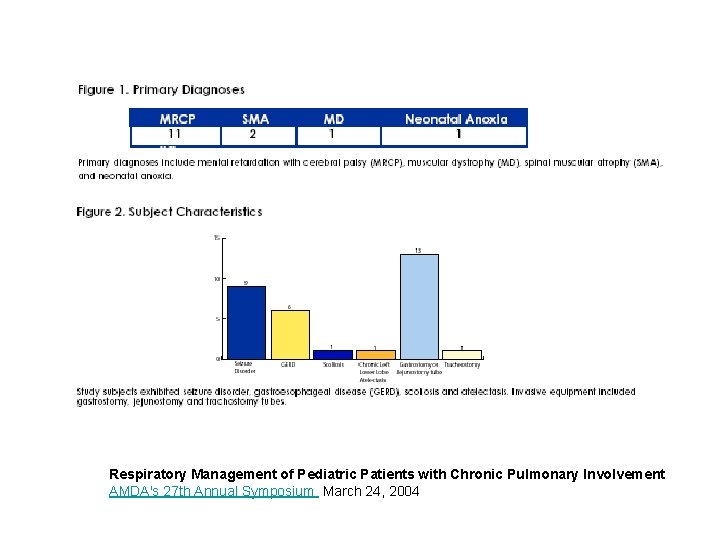
Respiratory Management of Pediatric Patients with Chronic Pulmonary Involvement AMDA's 27 th Annual Symposium March 24, 2004

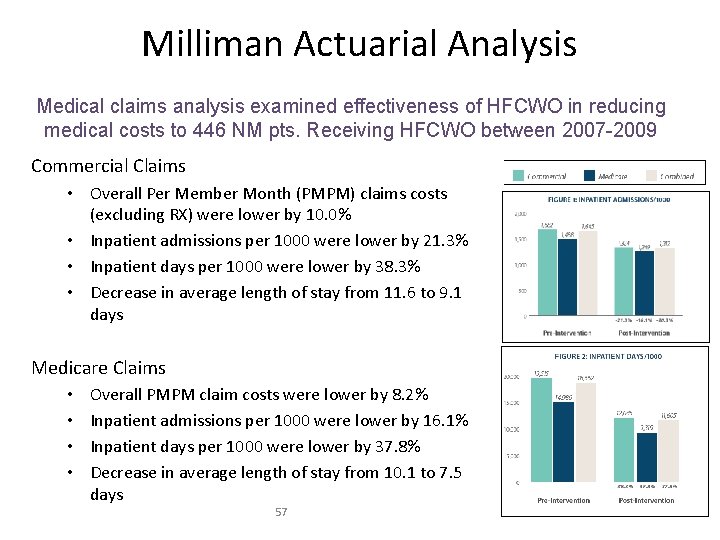
Data Sources • Medical claims data from 2007 -2009. 233, 562 patients identified with neuromuscular diseases. 446 patients received The Vest System. • Thomson Reuters Market. Scan Data Base reflecting the health experiences of employees and dependents covered by the health benefits of large employers. • Milliman’s Consolidated HCG Database (CHSD) containing detailed claims and membership information from Milliman’s data contributors • Claims and membership from the Center of Medicare and Medicaid Services (CMS) 5% sample of the Medicare population This report was prepared by Milliman on January 16, 2012
Medical Claims Analysis • Medical claims analysis to examine the effectiveness of High Frequency Chest Wall Oscillation (HFCWO) in reducing medical costs. • The analysis covered 446 neuromuscular disease patients that had received HFCWO therapy between 2007 and 2009 comparing health care costs incurred before and after HFCWO therapy intervention. • The results of the study show lower claim costs for patients with neuromuscular disorders after the initial insurance claim for HFCWO. This report was prepared by Milliman on January 16, 2012
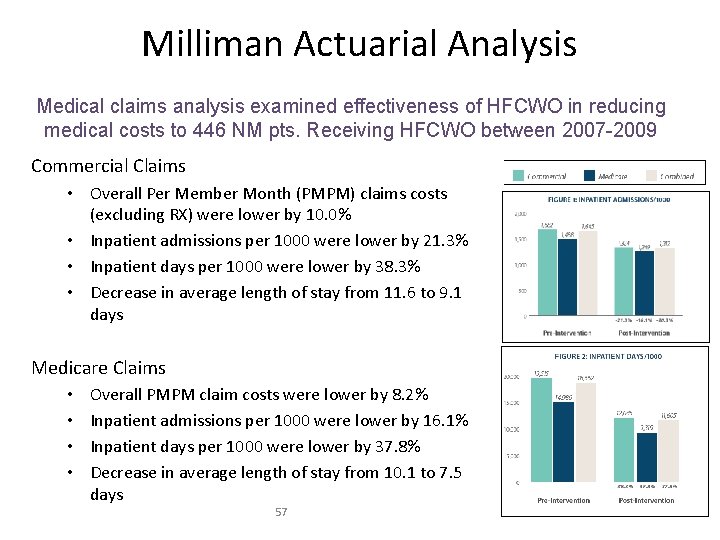
Milliman Actuarial Analysis Medical claims analysis examined effectiveness of HFCWO in reducing medical costs to 446 NM pts. Receiving HFCWO between 2007 -2009 Commercial Claims • Overall Per Member Month (PMPM) claims costs (excluding RX) were lower by 10. 0% • Inpatient admissions per 1000 were lower by 21. 3% • Inpatient days per 1000 were lower by 38. 3% • Decrease in average length of stay from 11. 6 to 9. 1 days Medicare Claims • • Overall PMPM claim costs were lower by 8. 2% Inpatient admissions per 1000 were lower by 16. 1% Inpatient days per 1000 were lower by 37. 8% Decrease in average length of stay from 10. 1 to 7. 5 days 57
References • Deboeck et al. Airway clearance techniques to treat acute respiratory disorders in previously healthy children – where is the evidence? European Journal of Pediatrics. 2009 • Fuhrman et al. Pediatric Critical Care. 4 th Edition. 2011. • Light et al. Pediatric Pulmonology. 2011 • Mcilwaine, M. Physiotherapy and airway clearance techniques and devices. Pediatric Respiratory Review. 2007. • Morrison and Agnew. Oscillating devices for airway clearance in people with cystic fibrosis. Cochrane Database of Systematic Reviews. 2009. • Taussig et al. Pediatric Respiratory Medicine. 1999. • West. Respiratory Physiology – The Essentials. 8 th Edition 2008. • Landon. Novel methods of ambulatory physiologic monitoring in patients with neuromuscular disease. Pediatrics 2009
 Laryngoscopy view grades
Laryngoscopy view grades Infants, children, and adolescents 8th edition
Infants, children, and adolescents 8th edition Infants, children, and adolescents 8th edition
Infants, children, and adolescents 8th edition Actual diagnosis
Actual diagnosis American youth football medical clearance form
American youth football medical clearance form Florida children and youth cabinet
Florida children and youth cabinet What is the difference between courting and dating
What is the difference between courting and dating Anatomy of upper respiratory tract
Anatomy of upper respiratory tract Maximum metal condition (mml) corresponds to the
Maximum metal condition (mml) corresponds to the Max clearance formula
Max clearance formula Canadian controlled goods program
Canadian controlled goods program Rake angle and clearance angle in dentistry
Rake angle and clearance angle in dentistry Clearance between bearing and shaft
Clearance between bearing and shaft Cgp and itar clearance
Cgp and itar clearance Cricothyroidotomy
Cricothyroidotomy Airway management acls
Airway management acls Respiration
Respiration Respiratory airway secretary
Respiratory airway secretary King airway
King airway Cormack lehane score
Cormack lehane score Skor mallampati
Skor mallampati Servo pressure on hfjv
Servo pressure on hfjv Head tilt chin lift jaw thrust
Head tilt chin lift jaw thrust Mean airway pressure
Mean airway pressure Hava yolu anatomisi
Hava yolu anatomisi Mallampati score intubation
Mallampati score intubation Triple airway maneuver
Triple airway maneuver Larangoscopy
Larangoscopy Tracheostomy stoma
Tracheostomy stoma Mean airway pressure formula
Mean airway pressure formula Ahi cpap
Ahi cpap Asp medical clinic
Asp medical clinic Airway numaraları
Airway numaraları Lemon law anesthesie
Lemon law anesthesie Aprv indications
Aprv indications Airway view
Airway view Ztechnique
Ztechnique Head tilt chin lift
Head tilt chin lift Opa and npa
Opa and npa Airway anatomy intubation
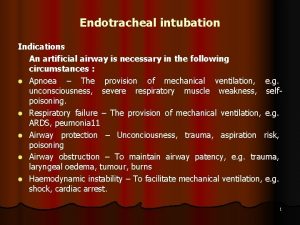
Airway anatomy intubation Indications for artificial airway
Indications for artificial airway Chapter 9 airway management
Chapter 9 airway management 3 emergency action steps
3 emergency action steps Airway gym
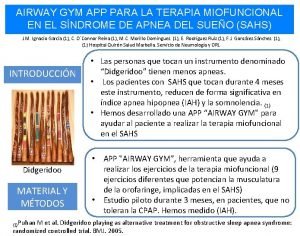
Airway gym Airway abcde
Airway abcde Airway breathing c
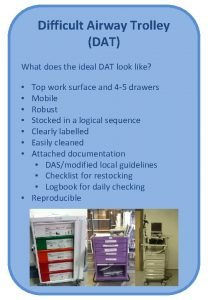
Airway breathing c Difficult airway trolley
Difficult airway trolley Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Moans airway
Moans airway Asa airway fire algorithm
Asa airway fire algorithm Generations of supraglottic airway devices
Generations of supraglottic airway devices Nasopharyngeal airway
Nasopharyngeal airway Nasopharyngeal airway
Nasopharyngeal airway Sandwich manuver
Sandwich manuver Thin
Thin Difficult airway algorithm asa
Difficult airway algorithm asa Mouth gag airway
Mouth gag airway Stepwise approach to airway management
Stepwise approach to airway management How will you open the casualty's airway
How will you open the casualty's airway