Acute Coronary Syndrome Nicholas Shaw ACS STEMI New


- Slides: 26
Acute Coronary Syndrome Nicholas Shaw
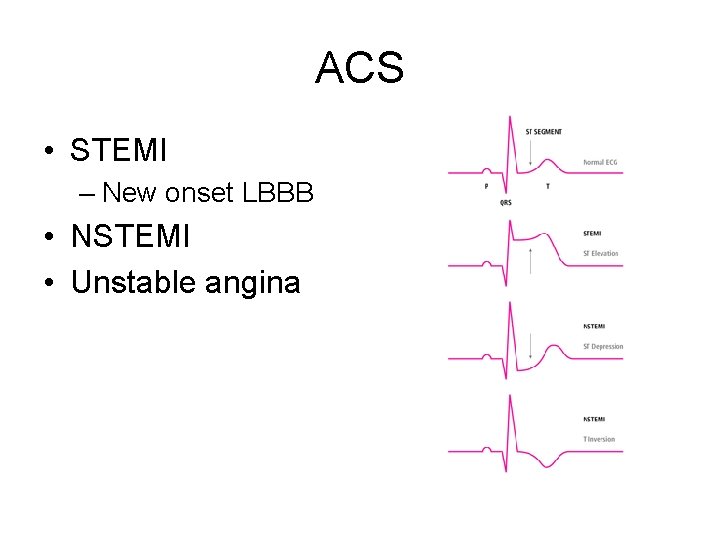
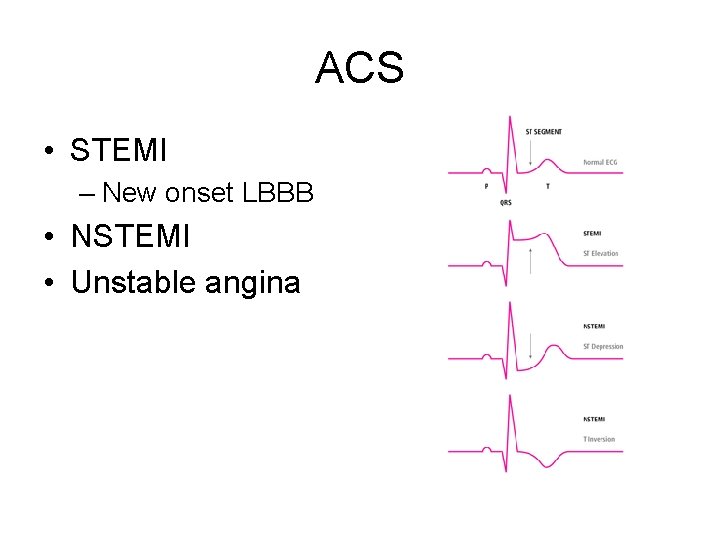
ACS • STEMI – New onset LBBB • NSTEMI • Unstable angina

Risk Factors for ACS • • Smoking Obesity Dyslipidaemia Hypertension • • • Age Male Ethnicity Family history CKD
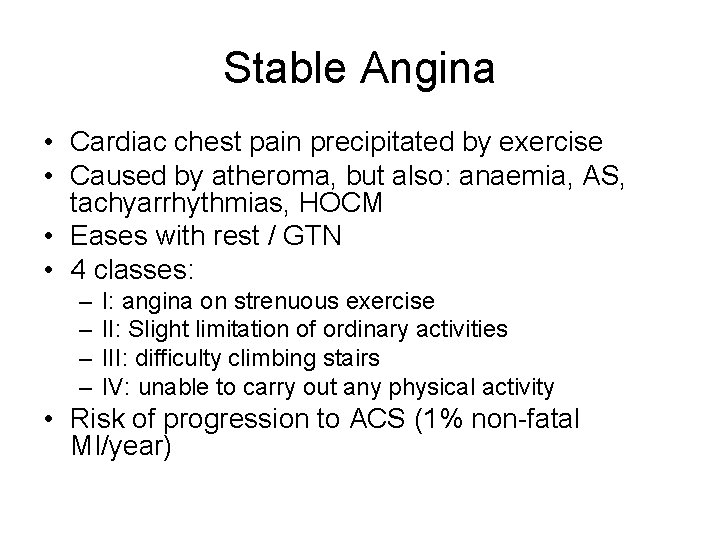
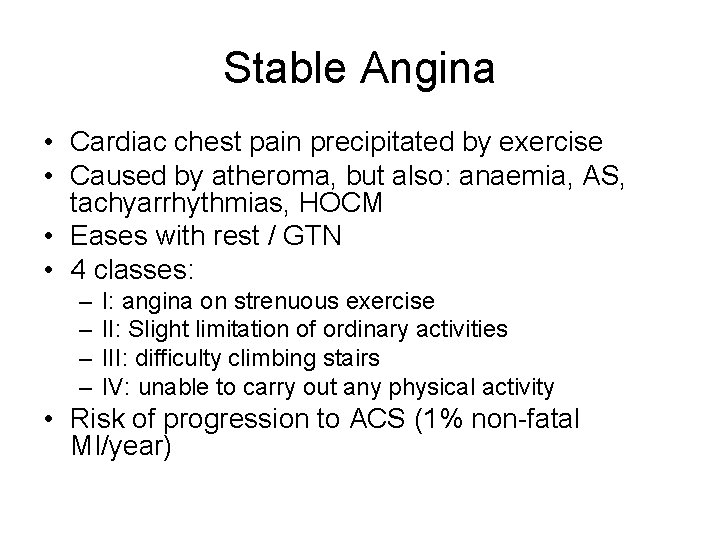
Stable Angina • Cardiac chest pain precipitated by exercise • Caused by atheroma, but also: anaemia, AS, tachyarrhythmias, HOCM • Eases with rest / GTN • 4 classes: – – I: angina on strenuous exercise II: Slight limitation of ordinary activities III: difficulty climbing stairs IV: unable to carry out any physical activity • Risk of progression to ACS (1% non-fatal MI/year)
Angina investigations • • • ECG Ecercise ECG FBC – anaemia Glucose – diabetes Lipids – dyslipidaemia TFTs - thyrotoxicosis
Angina Management • Lifestyle modification • Modifying risk factors • Medication – Aspirin – Beta blockers – Calcium channel blockers – Statins – Nitrates • Surgical – PTCA, CABG
Unstable Angina • Presence of angina without precipitating cause / at rest • Spectrum with stable angina and NSTEMI
Presentation of ACS • Typical chest pain – Male – Left sided chest pain – Radiating to left arm – Radiating to neck • Atypical chest pain – – – Right sided chest pain Abdominal pain Female Diabetic Elderly Silent MI • • • Cool Clammy Nausea Dyspnoea Pulmonary oedema Confusion Palpitations Collapse Death
Differential Diagnosis • • Musculoskeletal chest pain Pulmonary embolus Aortic dissection Gastric reflux
Diagnostic criteria of acute MI • 2/3 of: – ECG changes – Chest pain – Rise in cardiac enzymes
Investigations • ECG • Bloods – FBC – U&E – Trop T • CXR – Cardiomegaly – Pulmonary oedema – Widened mediastinum

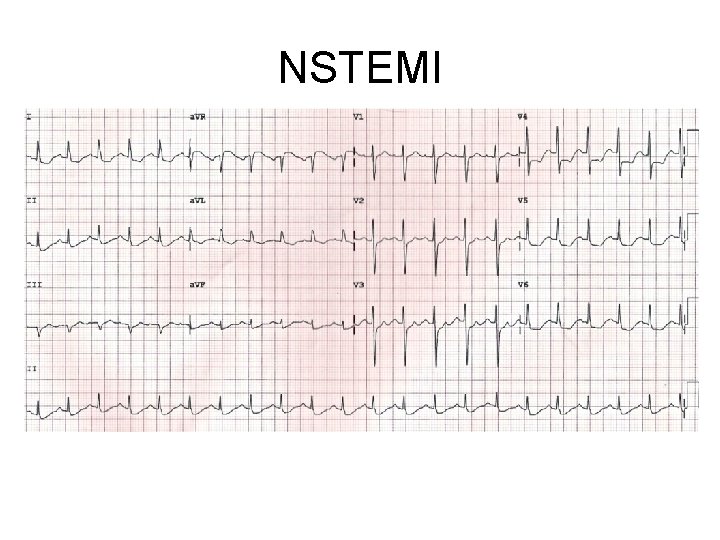
NSTEMI • Subocclusive thrombus • ECG changes: – ST depression – T wave inversion
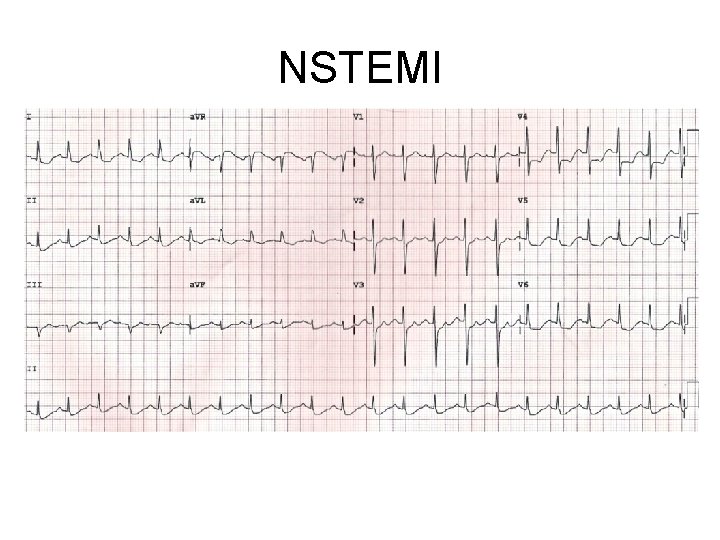
NSTEMI
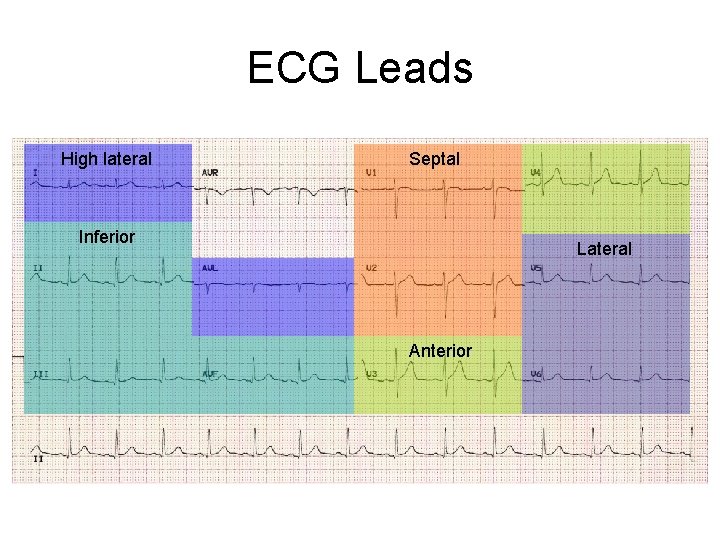
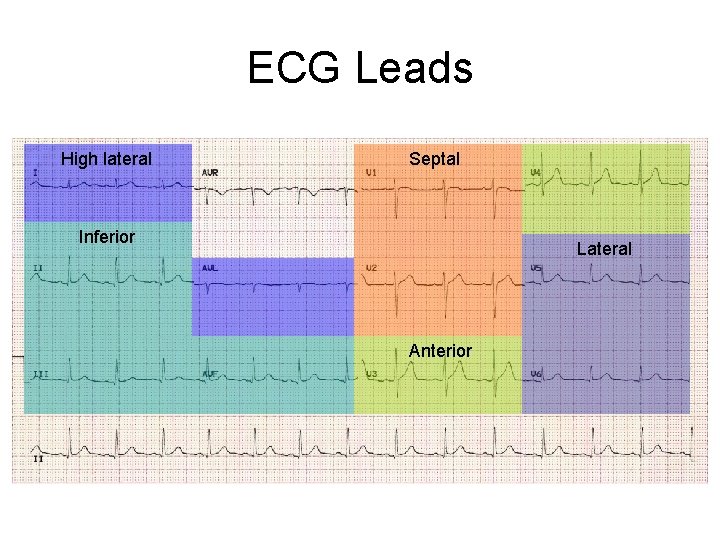
ECG Leads High lateral Septal Inferior Lateral Anterior
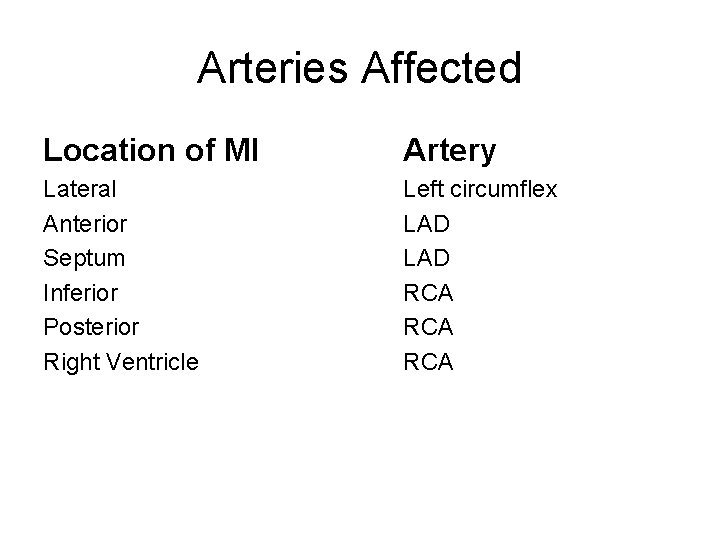
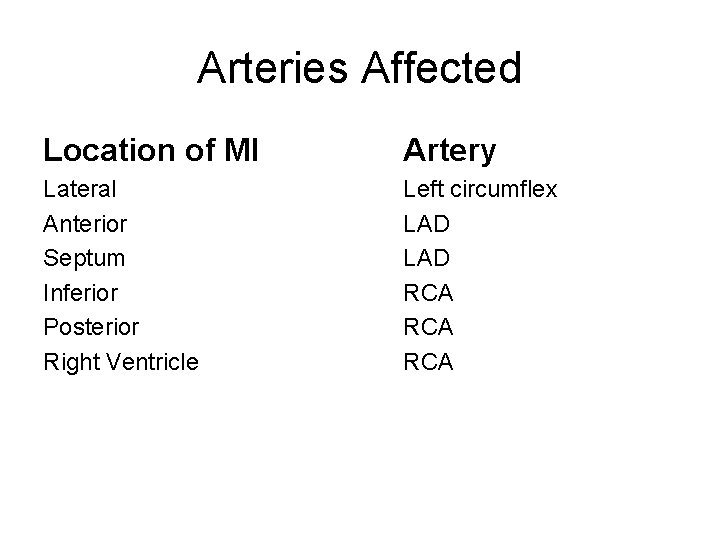
Arteries Affected Location of MI Artery Lateral Anterior Septum Inferior Posterior Right Ventricle Left circumflex LAD RCA RCA
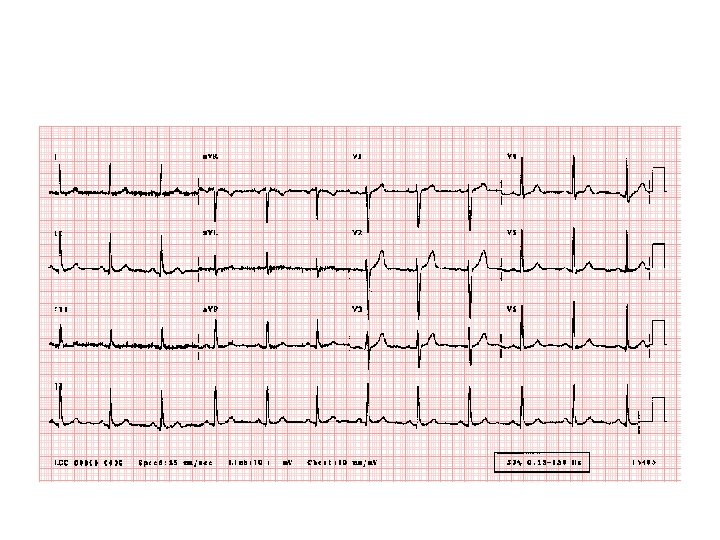
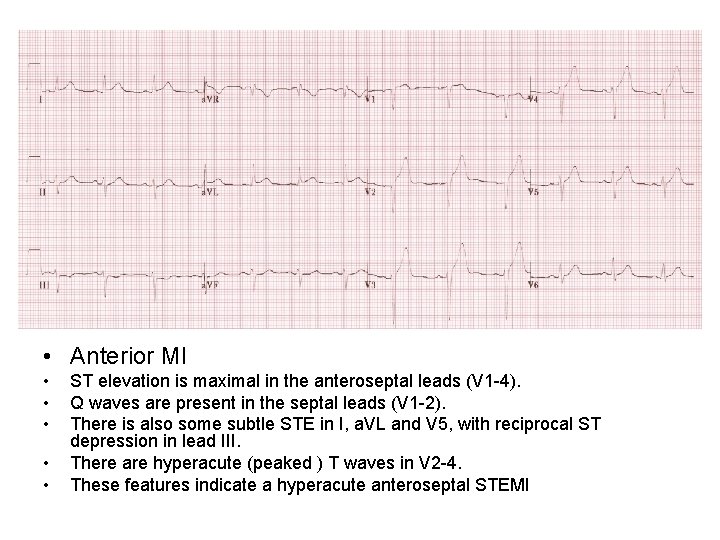
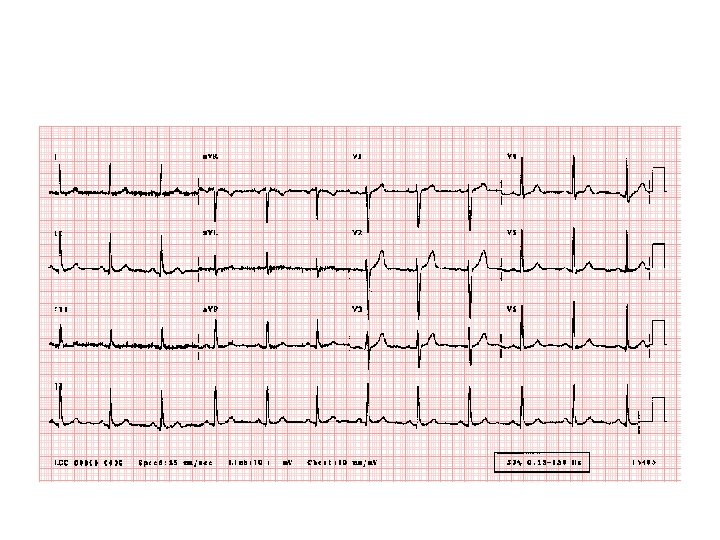
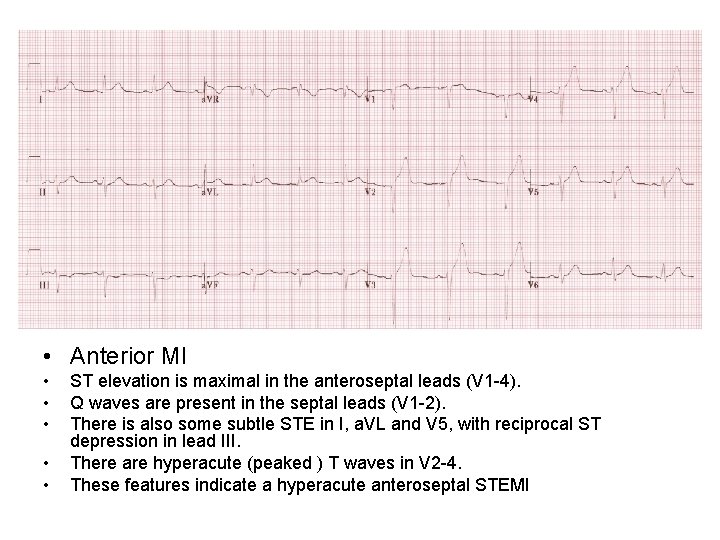
• Anterior MI • • • ST elevation is maximal in the anteroseptal leads (V 1 -4). Q waves are present in the septal leads (V 1 -2). There is also some subtle STE in I, a. VL and V 5, with reciprocal ST depression in lead III. There are hyperacute (peaked ) T waves in V 2 -4. These features indicate a hyperacute anteroseptal STEMI
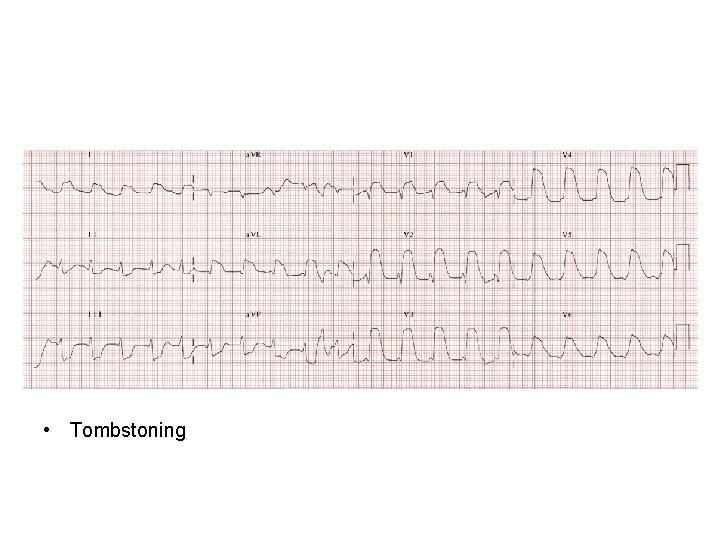
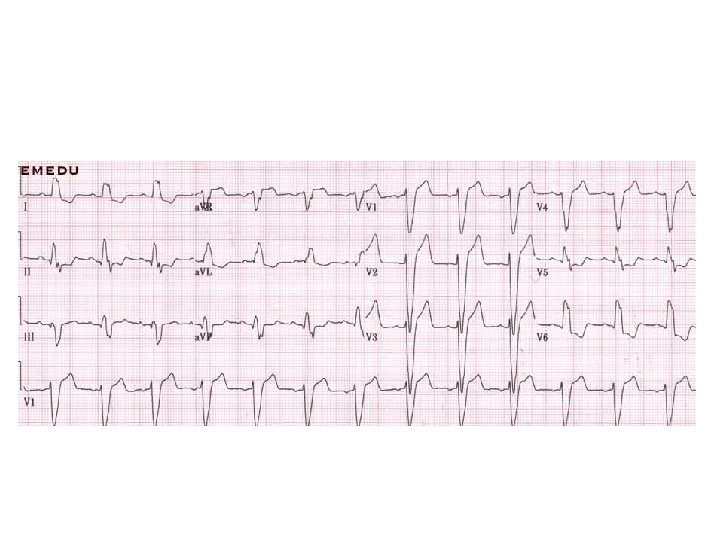
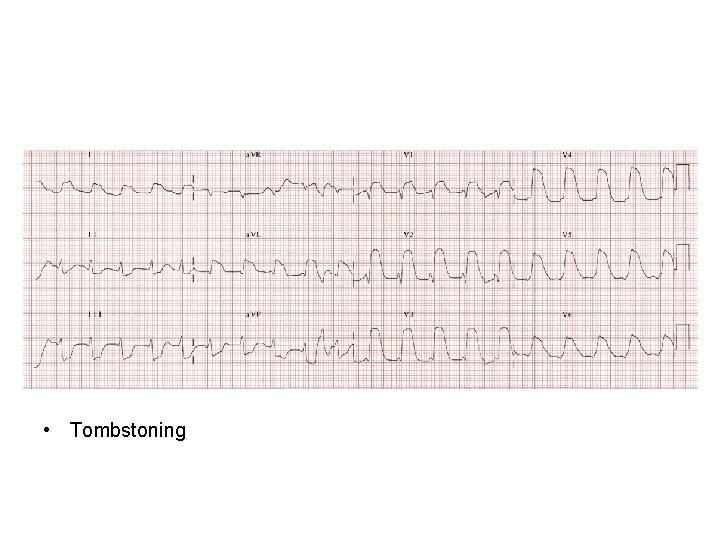
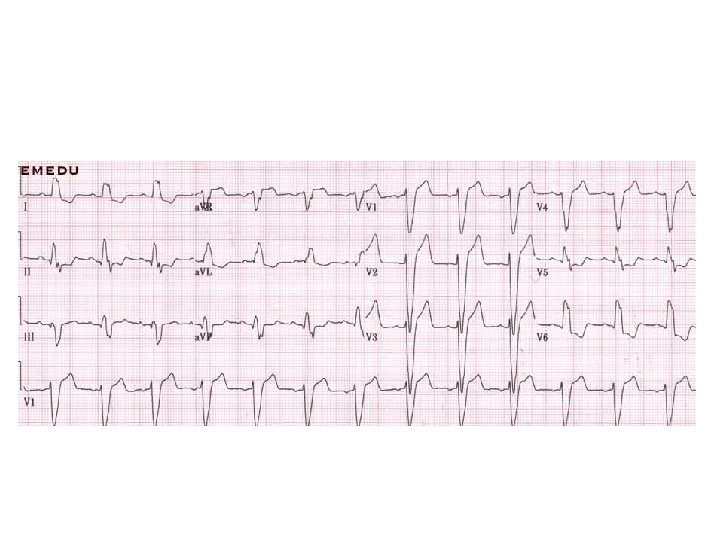
• Tombstoning
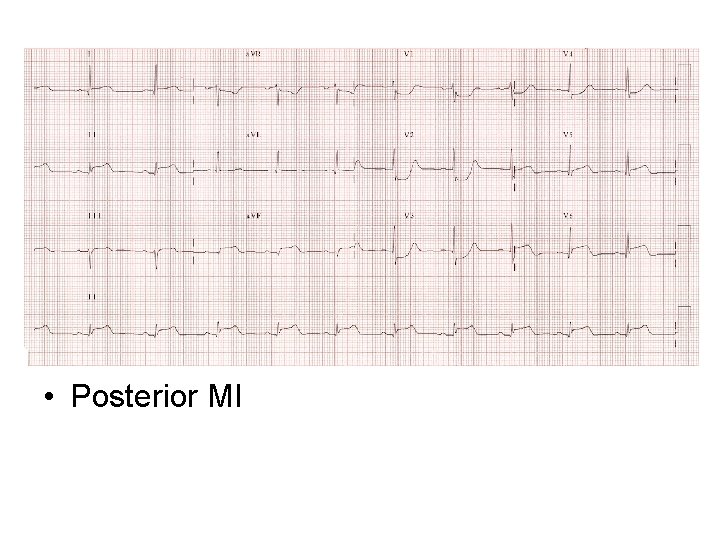
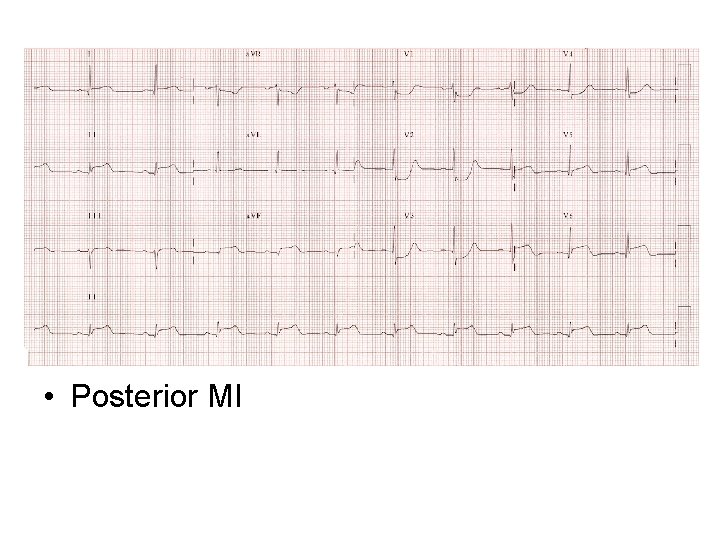
• Posterior MI
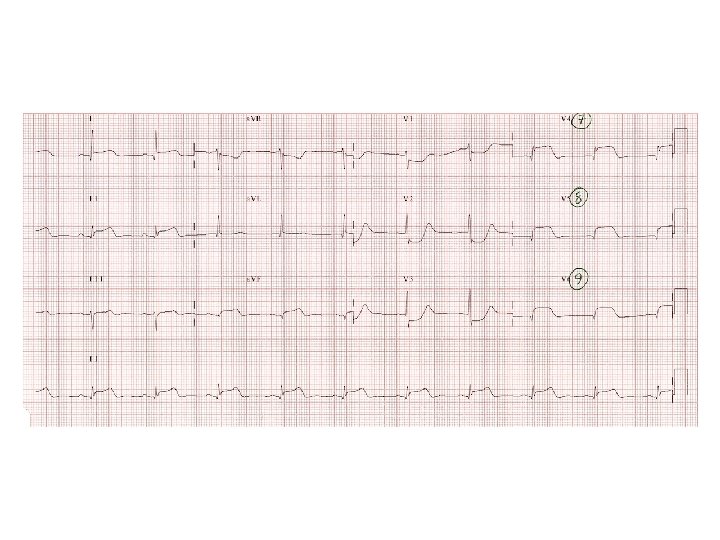
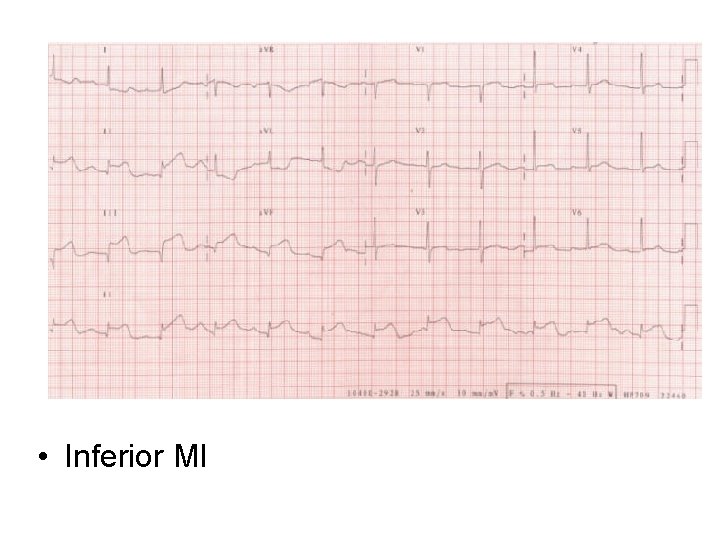
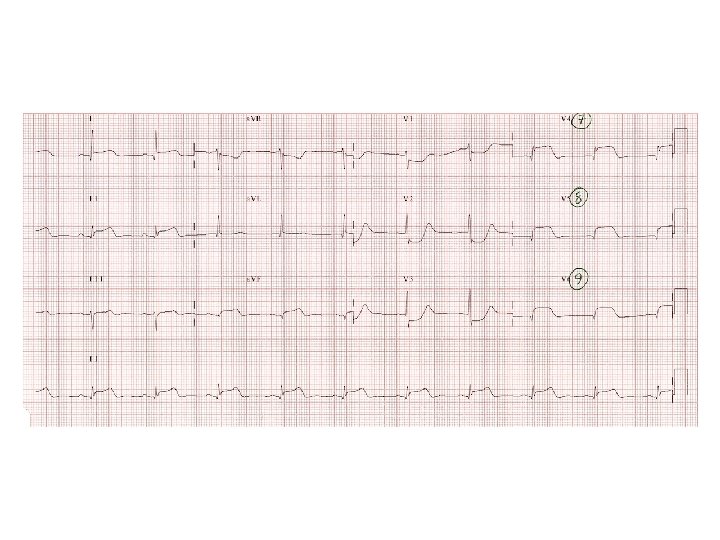
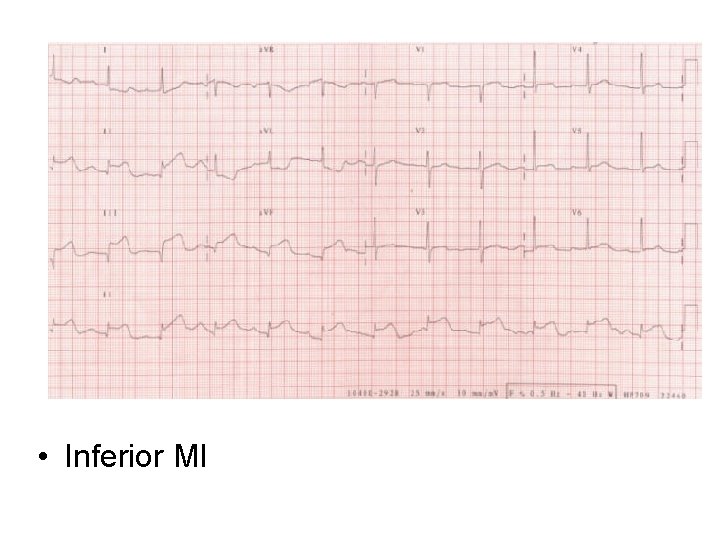
• Inferior MI
STEMI • - ST elevation > 1 mm in two or more limb leads and/or • - ST elevation > 2 mm in two or more consecutive precordial leads and/or • - Left Bundle Branch Block (LBBB) which is known or suspected to be of new onset and in the presence of cardiac symptoms
Treatment of STEMI • Morphine • Antiemetics (metoclopramide) • Antiplatelets – aspirin (300 mg) and ticagrelor (180 mg) • IV access • Bloods • Primary Coronary Intervention • Thrombolysis (t. PA / streptokinase)
Further inpatient management • • Education Echocardiogram (LV function) Clopidogrel (or ticagrelor) Beta blockers ACE-I Statins Risk factor modification
Late Complications • • • Dresslers syndrome Papillary muscle rupture Fibrosis Aneurysm Heart failure Death
 Acute coronary syndrome
Acute coronary syndrome Global registry of acute coronary events
Global registry of acute coronary events Dipyrimadole
Dipyrimadole Classification of antianginal drugs
Classification of antianginal drugs Acute radiation syndrome
Acute radiation syndrome Acute aortic syndrome
Acute aortic syndrome Ace inhibitors in stemi
Ace inhibitors in stemi Loading dose of mi
Loading dose of mi Stemi imposters
Stemi imposters Dtu stemi trial
Dtu stemi trial Stemi chain of survival
Stemi chain of survival Stemi
Stemi Smoking myocardial infarction
Smoking myocardial infarction Vf coarse berapa joule
Vf coarse berapa joule Non stemi
Non stemi Kriteria framingham
Kriteria framingham Coronary groove
Coronary groove Trabeculae carinae
Trabeculae carinae Coronary personality
Coronary personality Right marginal artery
Right marginal artery Coronary sinusoids
Coronary sinusoids Cardiac plexus
Cardiac plexus Coronary artery disease
Coronary artery disease What is high quality cpr
What is high quality cpr Coronary sulcus
Coronary sulcus Good morning blood
Good morning blood Good morning blood
Good morning blood