2020 UnAnticipated difficult airway management in Pediatric Prof










- Slides: 60

2020 Un-Anticipated difficult airway management in Pediatric Prof. Mostafa Somri Director Anesthesiology Department Bnai Zion Medical Center Faculty of Medicine, Technion Institute of Technology Haifa, Israel
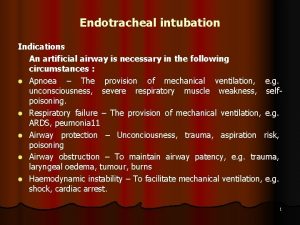
Airway management Endotracheal intubation is considered the definitive airway, it’s purposes is to create: • Mechanical ventilation of the lungs in anesthetized patients • Patient in ICU • In emergency situation
Pediatric Difficult Airway Definition • Difficult Face Mask Ventilation • Difficult Endotracheal Intubation • Can't Intubate Can't Ventilate/Oxygenate State (CICV/CICO)
States of Pediatric Difficult Airway Is rare • Overall incidence of 0. 58% in pediatric and 9 -13% in adult patient Paediatric Anaesthesia. 2013; 22: 1008 -1015 Anesthesiology. 2005; 103: A 1362 Can Anaesth Soc J. 1985; 32: 429 -434 Br J Anaesth. 1998; 80: 140 -46
Children at Risk of Difficult Airway Problems • Difficult face mask ventilation is very rare in children when performed by an experienced pediatric anesthesiologist • ET, intubation is a more frequent problem Paediatr Anaesth. 2012; 22: 1008– 1015 Anesthesiology. 1995; 82: 1063– 1064
States of Pediatric Difficult Airway • Anticipated Difficult Airway • Un -Anticipated Difficult Airway
Pediatric airway are different!! Specificity of natural anatomical conditions • • • Large head with protruding occiput Short and slender neck Small mouth Broad and short tongue Larynx being more superior Sharp angle between the base of the tongue and glottis, a long and narrow epiglottis • Physiological narrowing below the vocal cords

Signs of Anticipated Difficult Airway in Pediatric • Restricted head extension • Small mandibular space • Distinct distance from lower lib to the chin • Distinct distance from the ear tragus to the mouth • Mallampati of more than grade III and IV • limited availability of airway devices, Anesthetic experience Paediatric Anaesthesia 1996; 6: 251 -263
Anticipated Difficult Airway Signs in Pediatric • Congenital abnormalities - (Pierre Robin , Goldenhar, Treacher Collins etc… ) • Metabolic- ( mucopolysaccharidosis) • Inflammatory – Rheumatoid Arthritis • Other Pathology – Tumor • Traumatic • limited availability of airway devices, Anesthetic experience
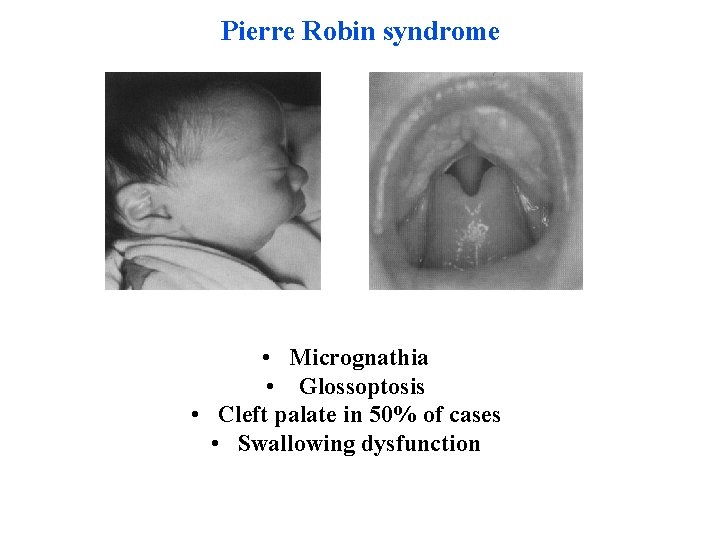
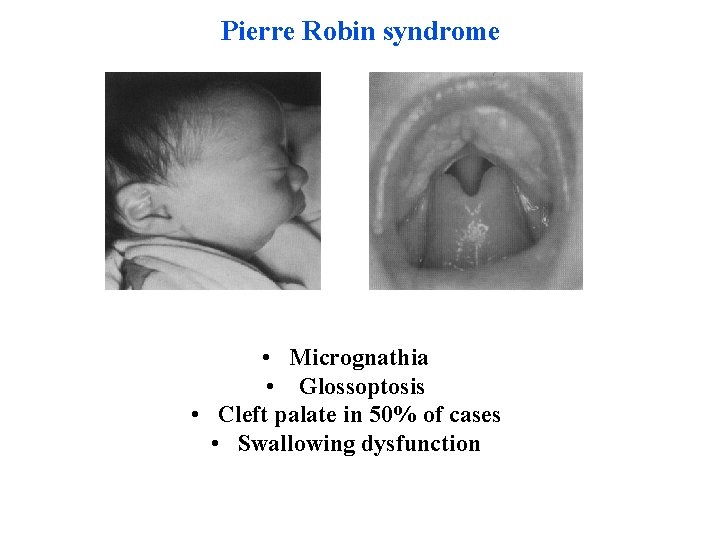
Pierre Robin syndrome • Micrognathia • Glossoptosis • Cleft palate in 50% of cases • Swallowing dysfunction
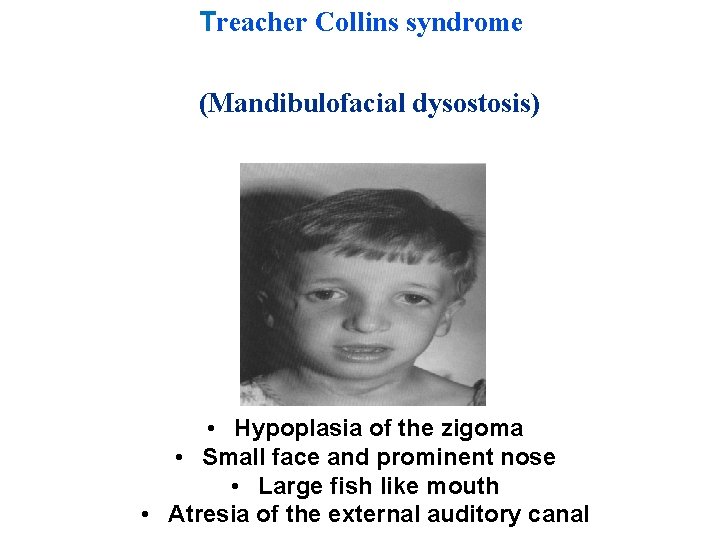
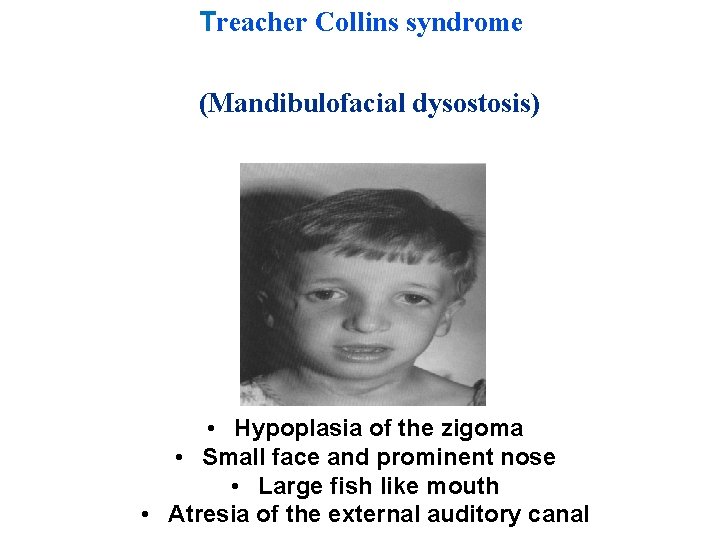
Treacher Collins syndrome (Mandibulofacial dysostosis) • Hypoplasia of the zigoma • Small face and prominent nose • Large fish like mouth • Atresia of the external auditory canal
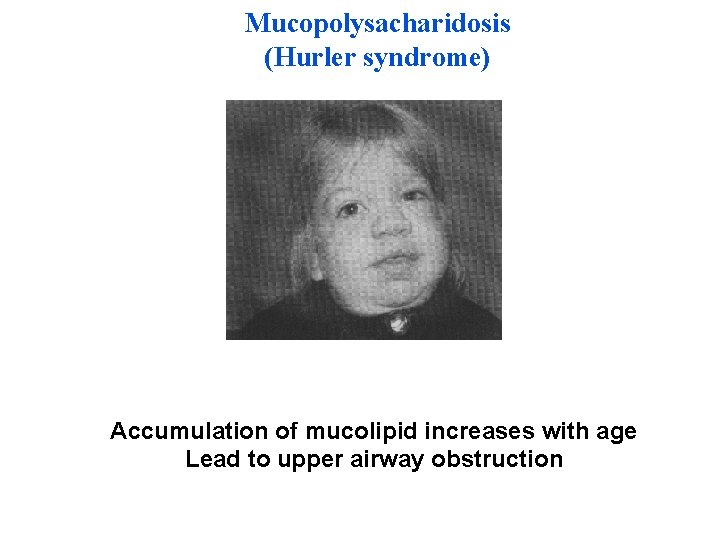
Mucopolysacharidosis (Hurler syndrome) Accumulation of mucolipid increases with age Lead to upper airway obstruction

Tumor Rhabdomyosarcoma
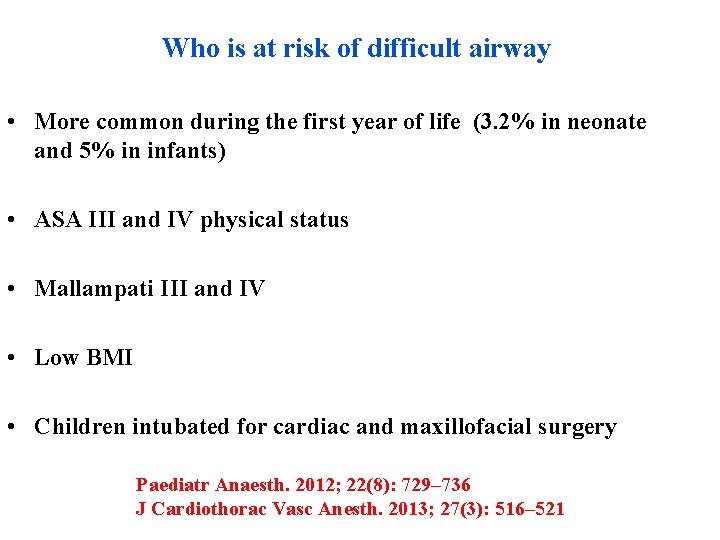
Who is at risk of difficult airway • More common during the first year of life (3. 2% in neonate and 5% in infants) • ASA III and IV physical status • Mallampati III and IV • Low BMI • Children intubated for cardiac and maxillofacial surgery Paediatr Anaesth. 2012; 22(8): 729– 736 J Cardiothorac Vasc Anesth. 2013; 27(3): 516– 521
Facts adds to difficult airway also because Children are characterized by: 1. Higher oxygen consumption 2. Less oxygen reserve. This leads to faster desaturation and subsequent bradycardia. Br J Anaesth. 2006; 97: 564– 570
Common Factors can attenuate difficult airway • Appropriate equipment • Credential anesthetic assistance and training that includes; • Simulation techniques. Paediatr Anaesth. 2016; 26(8): 784– 793 Anaesthesia. 2009; 64: 126 -30
Standard Intubation • • • Effective pre-oxygenation Removal of upper airway secretions Effective anesthetic and paralysis Use of external laryngeal manoeuvres facilitating intubation Use of standard malleable airway stylet
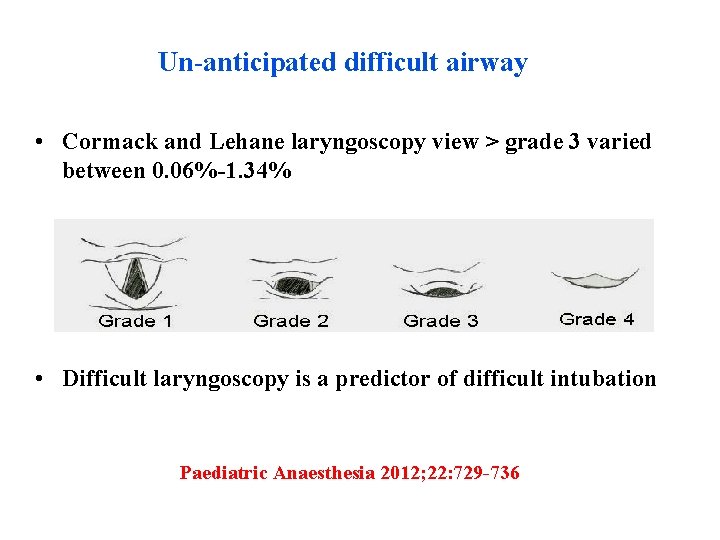
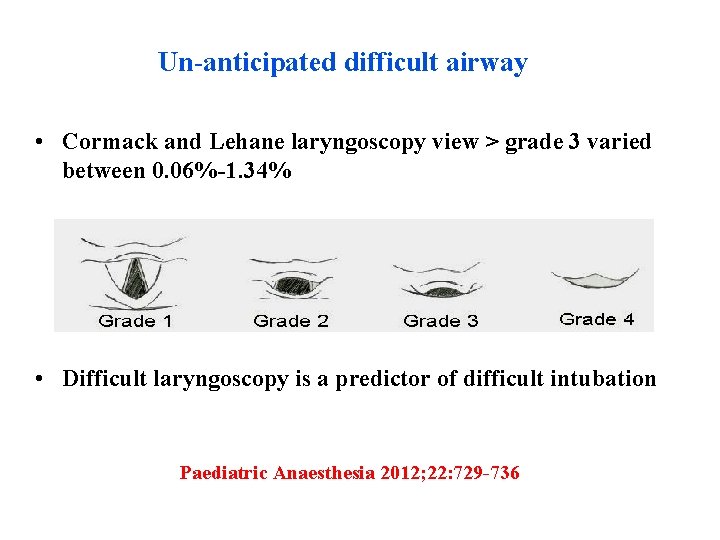
Un-anticipated difficult airway • Cormack and Lehane laryngoscopy view > grade 3 varied between 0. 06%-1. 34% • Difficult laryngoscopy is a predictor of difficult intubation Paediatric Anaesthesia 2012; 22: 729 -736
There are few pediatric difficult airway algorithms available in the literature. Paediatr Anaesth. 2015; 25(4): 346– 362 Paediatr Anaesth. 2010; 20(5): 454– 464

Practical algorithm For the Un-Anticipated difficult airway Stage 1
Achieve optimal conditions for face mask ventilation, laryngoscopy and tracheal intubation. • • How to hold the face mask Appropriate head and neck position Choice of an appropriate size and shape of a face mask Choice of both an appropriate laryngoscopy technique , size and shape of the laryngoscope blade • Choice of an appropriate tracheal tube
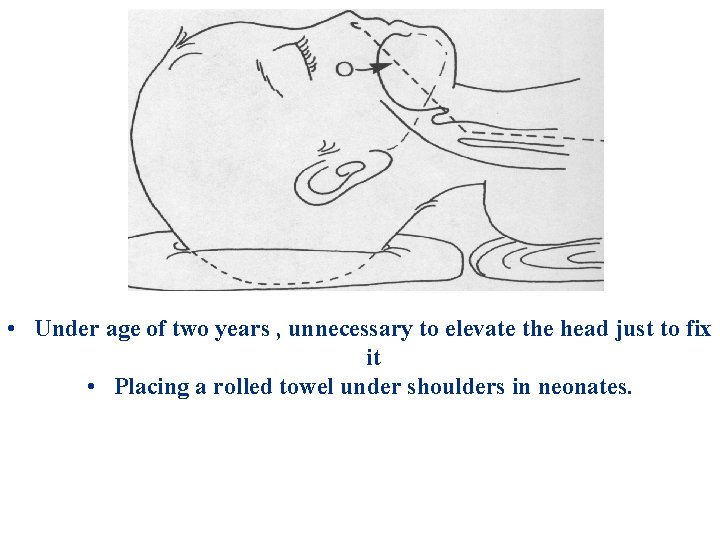
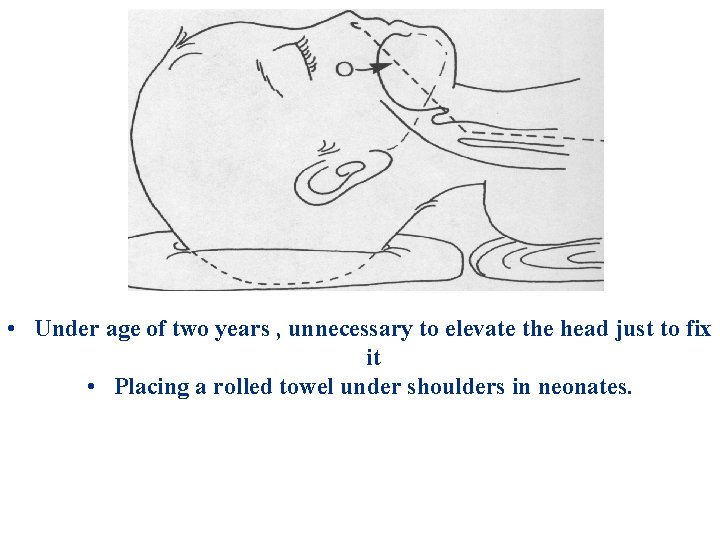
• Under age of two years , unnecessary to elevate the head just to fix it • Placing a rolled towel under shoulders in neonates.
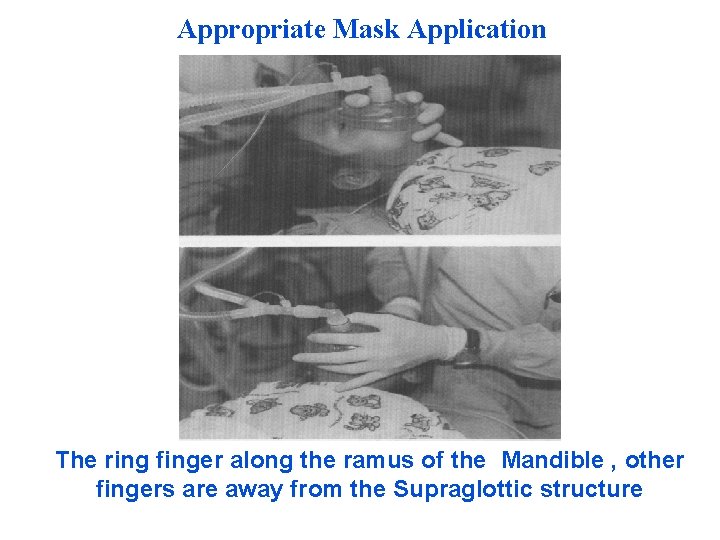
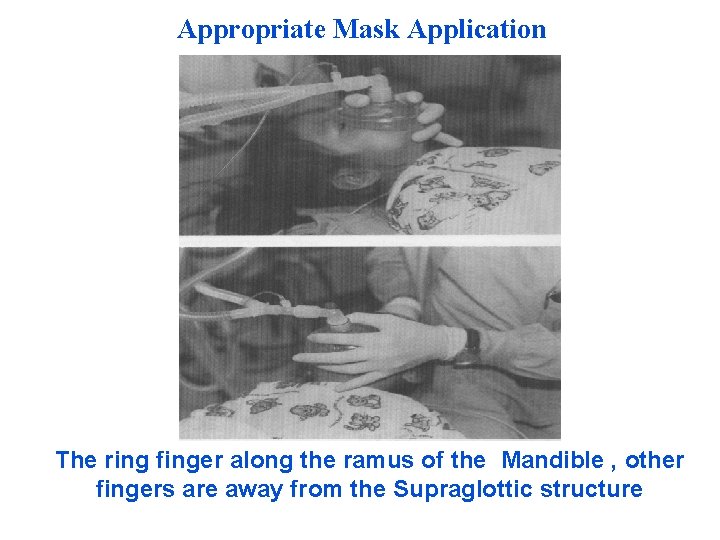
Appropriate Mask Application The ring finger along the ramus of the Mandible , other fingers are away from the Supraglottic structure
Improving conditions for face mask ventilation • Difficult Mask Ventilation (DMV) indicates unsatisfactory chest movements and inability to oxygenate the patient Sp. O 2 < 90% with Fi. O 2 = 1, 0. It’s rare in children. • laryngospasm, chest stiffness associated with opioid administration, excessive gastric insufflation with air & bronchospasm are the main causes. Paediatr Anaesth. 2012; 22(10): 1008 1015 Anesthesiology. 2007; 107: A 1637
• Sniffing position improves hypopharyngeal airway patency but does not necessarily change the position of the tongue • Upper airway obstruction is not primarily caused by changes in tongue position but rather by collapse of the pharyngeal structures. Cote’ & Lerman: A Practice of Anesthesia for Infants and Children – 2013; p. 246
• The jaw thrust maneuver is known to be the most effective to improve airway patency • Lateral positioning “recovery position”, enhances the effect of chin lift or the jaw thrust airway maneuvers Cote’ & Lerman: A Practice of Anesthesia for Infants and Children – 2013; p. 246
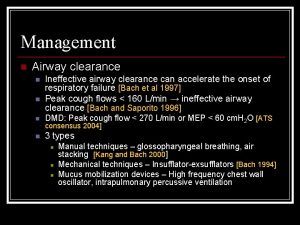
Actions should be taken in order to facilitate face mask ventilation • Solving of all equipment problems (air/gas leak) • Removal of secretions from the upper airways • Improved head and neck position, application of chin lift and jaw thrust • Improved seal around the face mask • Emptying the stomach (removal of excessive air/gas) • Use of oropharyngeal airway (OPA) or nasopharyngeal airway (NPA) • Cautious increase of pressure/volume of inspired air/gas during face mask ventilation • Administration of a bronchodilator in bronchospasm

Two hands face mask holder
External Laryngeal maneuver • The BURP maneuver, improves the laryngoscopic view by application of external pressure on the thyroid cartilage backwards, upwards and rightwards. • In neonates and infants the BURP may be performed by the intubator with the fifth finger of the hand holding the laryngoscope. BURP”. Can J Anaesth. 1993; 40(3): 279– 282
At this stage there may be two outcomes Success or failure
The causes of failure fall into two main groups: • Difficult laryngoscopy i. e. visualization of the laryngeal inlet • Difficulty in tracheal tube insertion into the trachea despite a good laryngoscopic view.
If Failure (max. 3 attempts in max. 10 minutes)
• A second experienced (consultant) anesthetist should be called • Ventilation should be continued with face mask and 100% oxygen

Stage II Maximizing the chances of successful intubation and further intubation attempts (max. 3 attempts in max. 10 minutes) Successful face mask ventilation results in satisfactory chest movements and good oxygenation of the patient (Sp. O 2 > 90%).
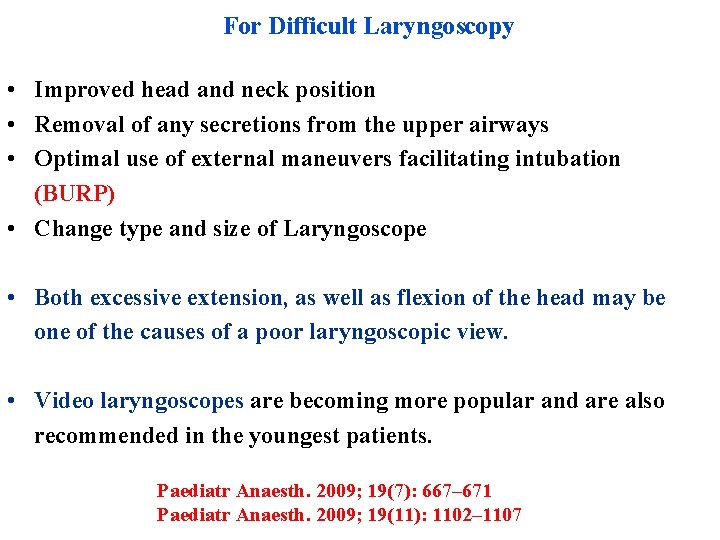
For Difficult Laryngoscopy • Improved head and neck position • Removal of any secretions from the upper airways • Optimal use of external maneuvers facilitating intubation (BURP) • Change type and size of Laryngoscope • Both excessive extension, as well as flexion of the head may be one of the causes of a poor laryngoscopic view. • Video laryngoscopes are becoming more popular and are also recommended in the youngest patients. Paediatr Anaesth. 2009; 19(7): 667– 671 Paediatr Anaesth. 2009; 19(11): 1102– 1107
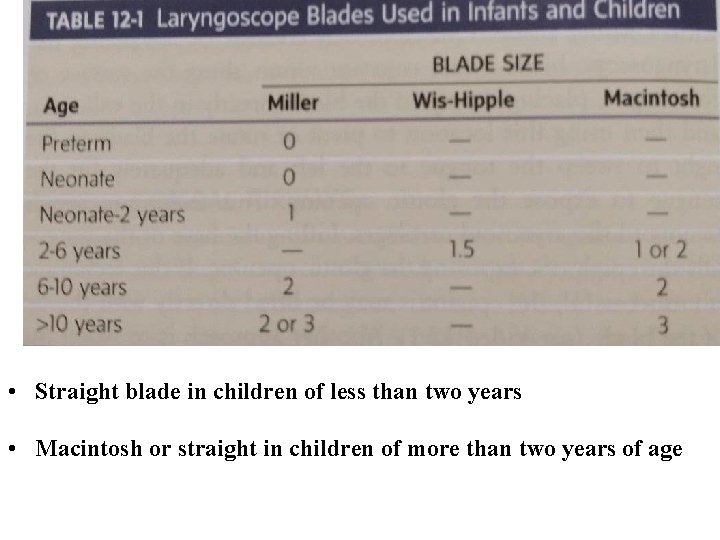
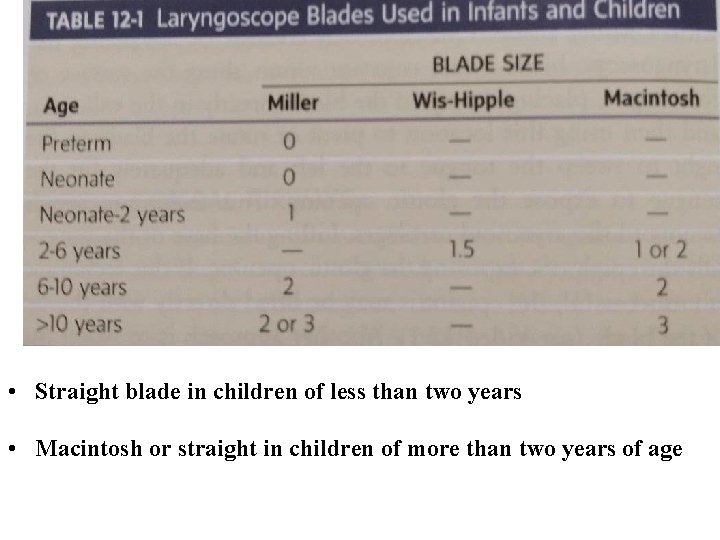
• Straight blade in children of less than two years • Macintosh or straight in children of more than two years of age
Difficult laryngoscopy NMBA • NMBA administration is considered safe and beneficial whenever face mask ventilation is effective. • Adequate muscle paralysis facilitates laryngoscopy. Paediatr Anaesth. 2010; 20: 454– 464 Anesthesiology. 2012; 117: 487– 493 Paediatr Anaesth. 2012; 22: 1147– 1149
Difficult insertion of the tracheal tube despite a good laryngoscopic view • The tip of the tracheal tube getting stuck in the anterior commisure of the vocal cords. A 90˚ anticlockwise rotation may solve the problem. • An introducer or airway stylet may be useful when there is difficulty with tracheal tube insertion below the level of the vocal cords. • A gum-elastic bougie (straight or curved) is useful when there is difficult intubation despite a good laryngoscopic view. Paediatr Anaesth. 2012; 22: 1147– 1149

IF Failure.

Keep always efficient mask oxygenation / ventilation with the right recommendation mentioned before
In this case we may have to awaken the child OR
In case of CICV/O In case of the inability to intubate and ventilate the patient, should be declared CICV (cann’t intubate and cann’t ventilate). It is a life-threatening situation and warrants a: prompt move to Stage III.
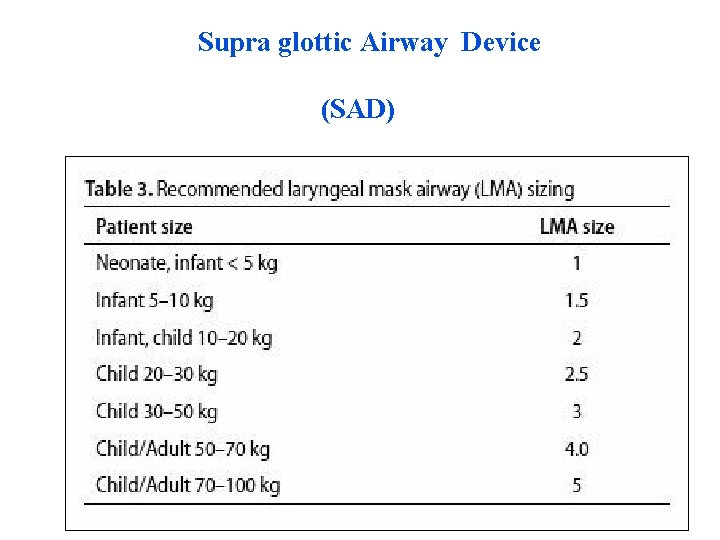
Stage III A: Use of a SAD (LMA) — a maximum of 3 attempts allowed • The most popular SADs are the laryngeal mask airways (LMA) and it’s various modifications • There also double-lumen SADs, e. g. LMA Supreme and LMA Pro. Seal , I gel & laryngeal tube which have a special channel used for NG tube insertion.

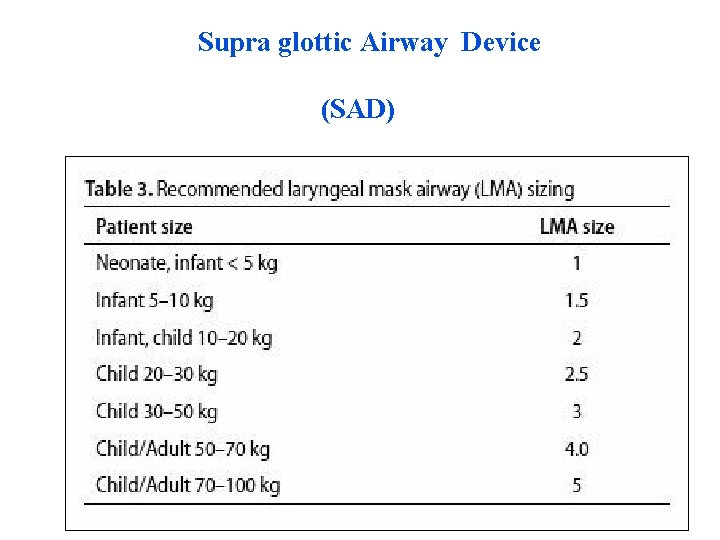
Supra glottic Airway Device (SAD)
Stage III : Use of a SAD (LMA) — a maximum of 3 attempts allowed There may be two outcomes at this stage: 1) Success — there is no immediate threat to life. 2) SAD for ET intubation guided.
Stage III : Use of a SAD (LMA) — a maximum of 3 attempts allowed If Failure
Stage III : Use of a SAD (LMA) — a maximum of 3 attempts allowed Failure Indicates a life-threatening situation and warrants a prompt move to Stage IV.
Stage IV: Front-of-Neck Access • In life-threatening situations when bag-mask ventilation and ventilation through Laryngeal Mask Airway (LMA) is not possible : • The option to achieve the quickest possible oxygenation of the patient should be chosen, according to the available equipment and the physician’s experience.
Stage IV: Front-of-Neck Access The front-of-neck approach comprises the following methods : • • Needle cricothyroidotomy Surgical cricothyroidotomy Retrograde intubation Tracheotomy The front-of-neck access is rarely used in children.
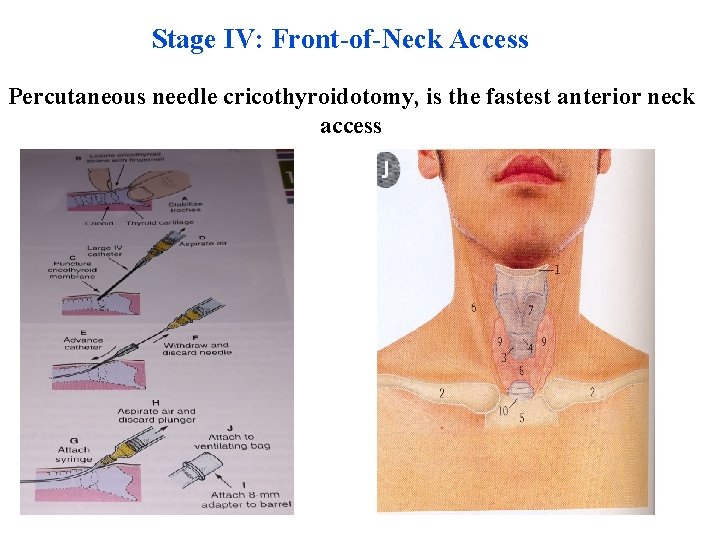
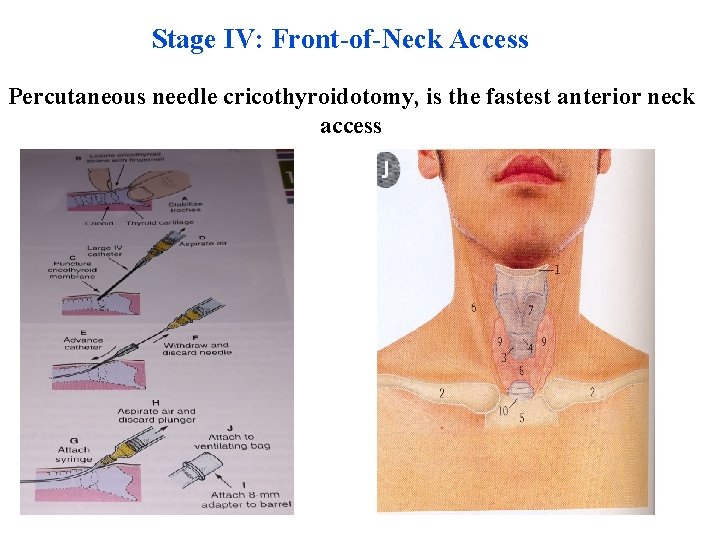
Stage IV: Front-of-Neck Access Percutaneous needle cricothyroidotomy, is the fastest anterior neck access

Stage IV: Front-of-Neck Access Surgical cricothyroidotomy is associated with high risk of complication – the smaller the child, the higher the risk. Paediatr Anaesth. 2009; 19 Suppl 1: 66– 76 Paediatr Anaesth. 2005; 15(5): 402– 406 J Pediatr Surg. 2007; 42(7): 1251– 1254
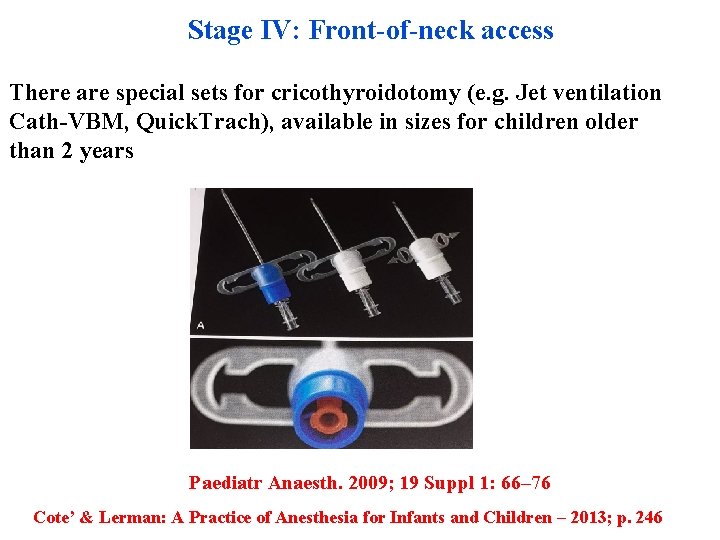
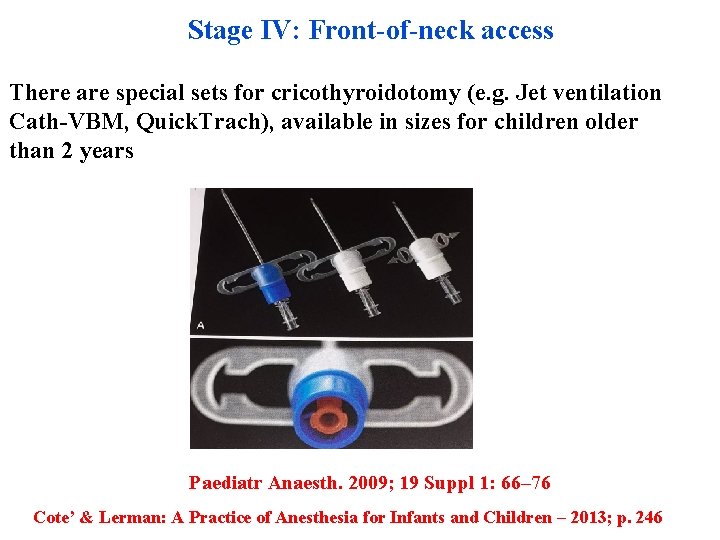
Stage IV: Front-of-neck access There are special sets for cricothyroidotomy (e. g. Jet ventilation Cath-VBM, Quick. Trach), available in sizes for children older than 2 years Paediatr Anaesth. 2009; 19 Suppl 1: 66– 76 Cote’ & Lerman: A Practice of Anesthesia for Infants and Children – 2013; p. 246
Stage IV: Front-of-neck access (FONA) • Only 8 of from the 30 physicians were able to cannulate the trachea within 4 minutes • High complication rate in children under 5 -6 years ( NAP 4) Br J Anaesth 2011; 106: 617 -613 Pediatr Anaesth 2005; 15: 402 -406 Paediatr Anaesth 2010; 20: 987 -993
Stage IV: Front-of-neck access Tracheotomy consists of making an incision on the anterior aspect of the neck, visualizing the tracheal wall and putting a tracheostomy tube inside the trachea through a created opening — usually at the level between the third and fourth tracheal cartilage.
Stage IV: Front-of-neck access While it can be performed at any age, there are very limited indications in neonates. Paediatr Anaesth. 2015; 25(4): 346– 362 Paediatr Anaesth. 2010; 20(5): 454– 464
If one is unable to secure tracheal intubation it is important to: • Recognize the limits of one’s ability • Do not hesitate to seek assistance from a colleague or request the surgeon to preform a tracheostomy or bronchoscopy • As an alternative, the child can be awakened and referred to a major pediatric center • In an urgent, life-threatening situation, placement of an SGA device or percutaneous cricothyroidotomy can be lifesaving Cote’ & Lerman: A Practice of Anesthesia for Infants and Children – 2013; p. 246
2020 Thank you very much for your attention! V- SIATTIP MEETING 2020
 Upper airway and lower airway
Upper airway and lower airway Cricoid pressure
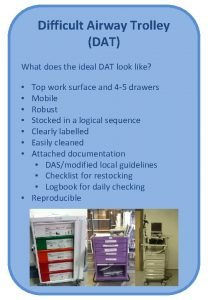
Cricoid pressure Ideal dat
Ideal dat Asa difficult airway algorithm
Asa difficult airway algorithm Difficult airway ppt
Difficult airway ppt Unanticipated problem vs adverse event
Unanticipated problem vs adverse event Who is hurt and who is helped by unanticipated inflation
Who is hurt and who is helped by unanticipated inflation Define unanticipated inflation
Define unanticipated inflation New trends in pediatric nursing
New trends in pediatric nursing Indikasi nasopharyngeal airway
Indikasi nasopharyngeal airway Chapter 10 airway management
Chapter 10 airway management Opa and npa
Opa and npa Npa measurement
Npa measurement Basic airway management equipment
Basic airway management equipment Airway breathing management
Airway breathing management Stepwise approach to airway management
Stepwise approach to airway management Upper airway anatomy
Upper airway anatomy Mechanism of respiration
Mechanism of respiration Respiratory airway secretary
Respiratory airway secretary Soap me airway
Soap me airway Grade view intubation
Grade view intubation Jarak thyromental adalah
Jarak thyromental adalah What is mean airway pressure
What is mean airway pressure Head tilt chin lift jaw thrust
Head tilt chin lift jaw thrust Mean airway pressure
Mean airway pressure Lma boyutları
Lma boyutları Vareculla
Vareculla Intubating lma
Intubating lma Lemon law airway assessment
Lemon law airway assessment Mean airway pressure formula
Mean airway pressure formula Automatic positive airway pressure
Automatic positive airway pressure Asp medical clinic
Asp medical clinic Airway numaraları
Airway numaraları Asa airway classification
Asa airway classification Aprv indications
Aprv indications Airway view
Airway view Pharyngo-tracheal lumen airway
Pharyngo-tracheal lumen airway Rae
Rae Thyromental
Thyromental Smart goals for ineffective airway clearance
Smart goals for ineffective airway clearance Indications for artificial airway
Indications for artificial airway Emergency action steps
Emergency action steps Airway gym
Airway gym Airway breathing c
Airway breathing c Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Moans airway
Moans airway Asa airway fire algorithm
Asa airway fire algorithm Generations of supraglottic airway devices
Generations of supraglottic airway devices Nasopharyngeal airway
Nasopharyngeal airway Nasopharyngeal airway
Nasopharyngeal airway Pulmonary arteriole
Pulmonary arteriole Mouth gag airway
Mouth gag airway How will you open the casualty's airway
How will you open the casualty's airway Abcde environment
Abcde environment Mellampati
Mellampati Noratbj
Noratbj Lethal triad
Lethal triad Is ap seminar difficult
Is ap seminar difficult Why is software difficult to build?
Why is software difficult to build? Beaumol
Beaumol Scripture the way of the transgressor is hard
Scripture the way of the transgressor is hard